PowerPoint
advertisement
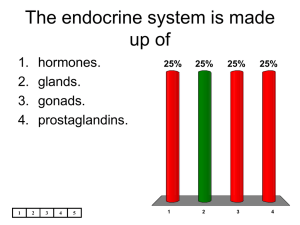
Male Reproduction: Learning Objectives 1. How are requirements and timing for meiosis different in males compared to females? 2. What events are required for formation of sperm? What roles do hormones and accessory cells play? What are normal sperm counts and how long does it take to affect sperm numbers? 3. What structures and glands are required for sperm to exit the body? 4. How might novel methods of male contraception take advantage of these required events and structures? Current Male Contraceptives • 1. 2. 3. • 1. Three methods currently available: Withdrawal: 27% pregnancy rate/year Vasectomy: permanent sterilization Condoms: great for preventing STDs Do we need more? Persistently high teen pregnancy rate, abortions, dissatisfaction with choices. 2. 1/7 women worldwide die in childbirth, aid to developing countries can only provide about 1 condom/man per year. Clicker Question 1 • Would you use a new method of contraception for men or encourage your partner to use one? 1. Yes 2. No Methods in Development 1. Affect formation of sperm 2. Affect ability of sperm to exit the body 3. Affect the ability of sperm to fertilize an egg. Type 1: Formation of Sperm Meiosis in testis, external in mammals Scrotum creates heat exchange to lower temperature to below 95°F. Type 1: Formation of Sperm Heat Methods of Contraception Protein Heat Shock Factor initiates cell death in sperm over 95°F 1. Simple wet heat: 1946 Dr. M. Voegeli reported 10 years of experiments on 9 male volunteers that showed method was effective and reversible. “Sits in a shallow or testes-only bath of 116°F for 45 minutes daily for 3 weeks. Six months of sterility results, after which normal fertility returns.” Type 1: Formation of Sperm How Hot is 116°F? Temperature Typical Usage Sensation 120°F Recommended home faucet temp Burn in 10 minutes Pain threshold for adults 116°F Testes-only bath 110°F Hot shower Very hot but not painful Very warm 105°F Maximum tolerable bath temp Hot tub temp 118°F 101°F warm warm Type 1: Formation of Sperm Heat Methods of Contraception Protein Heat Shock Factor initiates cell death in sperm over 95°F 2. Artificial cryptochordism/suspensories: John Rock and Derek Robinson of Harvard built on Voegeli’s work in the 1960s to investigate insulated underwear. Two pieces of evidence, heat effects and the fact that men with undescended testis (cryptochordid) were often infertile. Method: keep the testes close to the inguinal canal (the tube into which retractile testes withdraw) during waking hours. Type 1: Formation of Sperm Suspensories Publication 1987 Average sperm count 12 million/ml Average motility 22-30% 1991 3 million/ml 15% 1997 <2 million/ml Method briefs Rubber ring Type 1: Formation of Sperm Clicker Question 2 • A. B. C. D. E. How many sperm are normally present in a milliliter (1/5 tsp)of semen? 100,000 1 million 10 million 50 million 100 million Type 1: Formation of Sperm Clicker Question 3 • • A. B. C. D. Still sounds like plenty of sperm! No, men are often diagnosed with infertility with sperm counts as low as: 15 million sperm/ml 20 million sperm/ml 40 million sperm/ml 50 million sperm/ml Type 1: Formation of Sperm • The following figure shows the process of meiosis in the seminiferous tubules in the male testis. Annotate the figure to indicate names for the sperm precursor cells (spermatogonium, primary and secondary spermatocytes, spermatids, and immature sperm) and write the names for the type of division that the arrows are indicating (mitosis, meiosis I, and meiosis II). Type 1: Formation of Sperm Type 1: Formation of Sperm Typical Test Question 4 A. B. C. D. E. Which choice is true about both sperm and ova production? Initiation of meiosis is continuous after puberty. Millions of mature gametes are produced daily. All resulting gametes are the same size. All resulting gametes are haploid. All cells that result from meiosis will function as gametes. Type 1: Formation of Sperm How long would heat take? • Should take 2-2.5 months to become effective. • Reversible after 12-18 months. • Concerns: 1. Potential cancer risk: permanent natural cryptorchidism since childhood is associated with increase risk of testicular cancer 2. Sperm DNA damage even after cessation? Type 1: Formation of Sperm How’d you know it’s working? • $44.95 for two tests, 15 minutes • Works by staining the cells in the sperm sample to produce a color, intensity then compared to color reference to determine if above or below 20 million sperm/ml Type 1: Formation of Sperm Hormonal Contraceptives Three Major Classes: 1. Androgens 2. GnRH antagonist with androgen replacement 3. Progestin with androgen replacement Type 1: Formation of Sperm Typical Test Question 5 • A. B. C. D. Androgens, like testosterone can effectively reduce sperm production because they act to lower production of GnRH by the hypothalamus and LH by the pituitary. This effectively prevents sperm production because LH is needed to stimulate Leydig cells to make adequate amounts of testosterone needed to stimulate spermatogenesis in the testis. LH is needed to stimulate Sertoli cells that are required to nuture maturation of spermatids. LH normally boosts to GnRH levels, so without LH, there will not be enough GnRH to stimulate sperm production. LH boosts the production of inhibin which normally lowers sperm counts. Type 1: Formation of Sperm Status of male pill • Nothing available right now, may reach European market in 10 years. • Problems: – Take 11/2 - 21/2 months to start. – Progestins most well researched, good delivery, therapeutic dose extremely narrow. – Some of the androgens are only effective if injected into muscle, working for time release. – TE (10 days, but 100% reduction, Testosterone buciclate (3 months, but only 40% reduction) • Side effects of depressing “good” HDL cholesterol. • Reversible in 3-5 months • Non-response rates: 5-20% Type 1: Formation of Sperm Testis: full of Seminiferous Tubules • Hollow tubes coiling through testis. • Location of the divisions of meiosis. • Location of cells needed to produce testosterone, Leydig cells Sertoli cells nurture developing sperm cells Type 1: Formation of Sperm Adjudin: Sertoli Cells • Derived from anti-cancer medication, Lonidamine • Changes sertoli cell connection to developing spermatids so they break down before maturation is complete. • Problems: – Delivery difficult, so attaching it to altered, nonfunctional FSH. FSH only binds to sertoli cells. – Still has to be injected. – Only tested in rats so far Type 2: Sperm Exit Type 2: Sperm Exit Typical Test Question 6 A. B. C. D. E. A man who was diagnosed with a very low sperm count was given an vasograph (dye was placed in his reproductive tract) and X-rays revealed the location of a blockage in his vas deferens. What would this mean? sperm are formed and mature normally, but they are blocked from exiting the body and build up in the epididymis. sperm cannot form because the cells that manufacture testosterone in the vas deferens are prevented from functioning. sperm are made normally but cannot reach the vas deferens where they complete the final steps in maturation. sperm cannot form normally because the blockage in the vas deferens prevents the products of meiosis, the spermatids, from reaching the epididymis where the must finish maturation. this man can never have children because sperm form in the vas deferens, and this blockage prevents the steps of meiosis from occurring. Type 2: Sperm Exit Current Methods 1. Vasectomy (expensive to reverse, granulomas (10%) and autoimmune response) 2. RISUG: (Reversible Inhibition of Sperm Under Guidance) injected powdered styrene maleic anhydride forms partial plug which can be later flushed out. Phase III clinical trials India. 3. Injected plugs (clinical trial in 12,000 Chinese men, 30-minute outpatient procedure, takes 12-18 months to work, epididymis rupture 4. Intra vas device (phase II clinical trials, China, here in US by 2010, $1000 Type 2: Sperm Exit Block Semen Exit • Dry Orgasm • Phenoxybenzamine (blood pressure) /Thioridazine: 2006, block smooth muscle contractions in reproductive tract. – Seminal Vesicles: fructose (energy) prostaglandins, basic fluids – Prostate: enzymes, antibiotic – Bulbourethral gland: mucus Type 3: Block Fertilization • Nifedipine, hypertension/migraine medicine discovered in 1992 to cause infertility, apparently through damage to sperm cell membrane (lacked egg binding sugar and had too much cholesterol in membrane. No clinical trials, patents expired. • Sperm enzyme inhibitors, 90% effective when dissolved in rats drinking water. Clicker Question 7 • 1. 2. 3. 4. 5. 6. 7. 8. Which of the methods mentioned could you see yourself (or your spouse using) in the future? Wet heat Suspensories Male Pill Adjuvin (anti sperm maturation) RISUG (reversible block in vas deferens Smooth muscle contraction inhibitors Sperm incapacitators None of the above