Road to UHC and Beyond: Japan`s 50-year Experience
advertisement
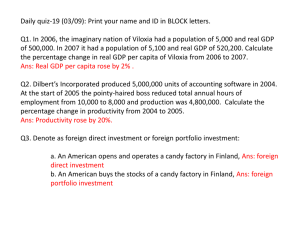
Road to UHC and Beyond: Japan’s 50-year Experience 10th Anniversary Conference Towards Universal Health Coverage: Increasing Enrolment Whilst Ensuring Sustainability Tomoko Ono OECD Health Division Accra, 5th November, 2013 Tokyo Station Tokyo Tower Sky Tree 1961: 2011:50th Achievement Year Anniversary of Achieving Health Coverage UHC 1920s: Introduction of Universal Health of Insurance Scheme UHC helped Japan to achieve good health results with relatively low health expenditures Outline of Presentation • Health system of Japan at a glance • Financing: Multiple insurances schemes • Payment: FFS with unified fee-schedule • Current challenges Health System of Japan at a Glance Recap historical development 1958:Nation al insurance law (mandate) 1956:30% not covered 1922: Health insurance law 1938: National Insurance law 1945: End of WWII Universal Health Coverage Source: WHO, World Health Report 2013 Population coverage: • 100% achieved in 1961 Cost coverage: • 82% by government or social security in 2011 Service coverage: • Outpatient, Inpatient, Dental, Pharmaceuticals Key Feature of Health Systems • Financing: • Multiple health insurance schemes, contribution + general tax + co-payment (with ceiling and exemption for low-income group) • Payment: • Managed FFS system through unified fee-schedule for all providers/insurance schemes in Japan • Service delivery: • Predominantly private providers (although public providers exists) • Roles of hospitals/clinics and GPs/specialists functions are not well defined in practice • Access: • Free choice of provider by patients (no gate keeping) Health Insurance Schemes 4 Different Insurance Schemes • Over 3,000 insurance plans in Japan, grouped into • Citizens’ Health Insurance (CHI): farmers, selfemployed, unemployed and elderly (later separated) • National Health Insurance Associations (NHIA): mainly small and medium enterprise employees and their dependent • Society Managed Health Insurance (SMHI): mainly employees of large firms and their dependent • Mutual Aid Association (MAA): mainly public sector employees and their dependent • Limited role for private insurance Achieving Universal Coverage UHC in 1961 Source: Takagi 1994, World Bank 2013 (forthcoming) UHC: Citizen’s Health Insurance’s Role • Historical Development of CHI • Build upon the existing community-based health insurance scheme: voluntary participation and expanded through government subsidies • Participation was mandated in 1961 for all residents, management moved to municipalities • Current financial sources: contribution from beneficiary, cross-subsidy from other schemes, subsidies from national and local government and copayment Revenues for Social Health Insurance cross-subsidies Elderly CHI NHIA Individual MAA Employee Government Individual SMHI Individual Individual Individual Financial Sources for Health Services UHC Managed FFS System with Unified Fee-Schedule Single Payment System: Fee-Schedule • Fee-schedule • Sets prices for each services, pharmaceuticals and devices for virtually all providers • Defines the benefits and conditions for reimbursement • Auditing for these conditions • For most providers, these are the only sources of revenue • Fee schedule revisions (every 2 years) • Managed by national government • Institutionalized process of negotiating benefits and resource allocation among key stake holders • Continuous process of adaptation and adjustment Biennial Fee-Schedule Revisions Government Ministry of Health, Labour and Welfare Ministry of Finance Macro: Global Revision Rate Central Social Insurance Medical Council Micro: Fee negotiation for item-by-item Medical services Medical devises Pharmaceuticals Pharmaceuticals Pricing Mechanisms • In 1982, 39% of national medical expenditure was spent on pharmaceuticals. • It went down to 27% in 1988 and 21% in 1998, then went up again to 25% in 2009 • We set a price in fee schedule, but providers purchase products for which bigger discounts can be negotiated and earned. • Government conduct survey of pharmaceutical prices of each products and set new fee schedule price at a certain percentile. Cost Containment Mechanism • Cost containment tools • Price control via negotiation, by monitoring volume • New technology - setting the initial price low, restriction to patients with specific conditions • Other restrictions • Balanced-billing (charging more than the fees set in the fee schedule): banned • Extra-billing (billing services and pharmaceuticals not listed in the fee schedule with those listed): only allowed for amenity and a few new technologies still being evaluated Current Challenges Slow economic growth and increasing social security expenditure Real GDP Growth Rate and Social Security Expenditures Real GDP Growth Rate 8 14 % % 22 Real GDP growth (left) % Social security expenditures / GDP (right) average 9.6% in 1955-70 6 20 4 18 2 16 0 14 -2 12 -4 10 12 10 8 average 4.5% in 1970-90 6 4 2 0 -2 -4 average 0.9% in 1990-2011 -6 1955 1960 1965 1970 1975 1980 1985 1990 1995 2000 2005 2010 Source: Cabinet Office of Japan 1990 1995 2000 2005 2010 Ageing Population and Inequality between Insurance Schemes Age structure of CHI beneficiary, 1975, 2001 and 2007 Take Home Message UHC in Japan was achieved through... • Long-term political commitment for UHC, supported by political groups with different ideologies • Democratic movements and commitment to social solidarity in post-war Japan provided impetus to expand coverage • Incremental expansion of health insurance coverage • Harmonization of benefits and established redistribution schemes Cost Containment despite FFS system • Institutionalized fee-schedule revision process • Global revision rate • Item-by-item fee negotiation: mitigate increase in expenditure, maintain appropriate solvency for providers, and reflect government priority • Stringent and disciplined payment system • Unified fee-schedule for all health services and conditions of its use • Ban on balanced-billing and restriction on extrabilling Acknowledgement: Ghana Health Insurance Authority Prof. Naoki Ikegami, Keio University School of Medicine Japan-World Bank Partnership Program on UHC Kyoto, Japan Japan Kagoshima, Niigata, Acknowledgement for picture • Slide 2 • Tokyo Station http://www.oldphotosjapan.com/ja/photos/78/tokyo-eki • Tokyo Tower http://showa.mainichi.jp/photo/2008/12/post-1b55-23.html • Sky Tree • Slide • Niigata, http://uonuma.biz/blog/9927 • Kyoto, http://futuretihing.net/futurething/wpcontent/uploads/2013/08/63bf16f29e082d9d510aac6e4fd47ea6.jpg Total Health Expenditure (% of GDP) Source: OECD, Health at a Glance 2011 Total Expenditure on Health in 2011 by type of financing Japan attained UHC while still a middle income country, and at the start of its rapid economic growth period Real GDP and GDP per Capita (in 1990 Geary-Khamis Dollar) Billions of $ GDP per capita (right) Real GDP (left) $ per capita Attainment of Universal Health Coverage (1961) ($420B, $4291per capita) 1955 1960 1965 1970 1975 1980 1985 Source: Angus Maddison (2001) “The World Economy – A Millennial Perspective” 30