Slow repetitive Transcranial Magnetic Stimulation
advertisement
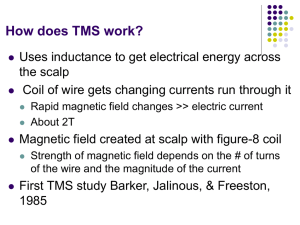
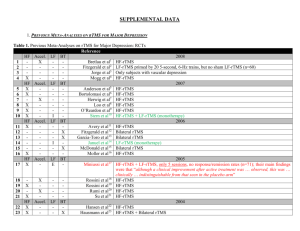
Slow repetitive Transcranial Magnetic Stimulation A Treatment for Auditory Hallucinations in Schizophrenia Transcranial Magnetic Stimulation (TMS) Historical Background: About a century ago researchers first stimulated retinal nerve cells with magnetic fields to produce flashes of light in subjects 1985 Barker and colleagues first stimulate brain cells in the motor cortex of subjects. By 1990’s develop repetitive TMS where repeated magnetic pulses can be delivered up to 50 times a second (50 hertz) Thompson, 1910 Transcranial Magnetic Stimulation (TMS) About the intervention: Principle behind TMS is if an electrical current is passed through a wire coil, then it momentarily generates a magnetic field. This magnetic field can easily penetrate the skull and induce electrical currents in the brain that can depolarize superficial neurons The magnetic field rapidly declines with distance Stimulates about 2-3 cm of cortex but depends on shape and configuration of coil (Hoffman & Cavus, 2002) So this is a relatively painless and non-invasive way to stimulate the brain Transcranial Magnetic Stimulation (TMS) About the intervention: 2 types of rTMS: fast rTMS is >1 hertz slow rTMS is ≤ 1 hertz Fast rTMS induces excitation whereas slow rTMS induces inhibition in brain cells. Reasons for this isn’t clear Slow rTMS may bring about lasting changes as well (Chen et al, 1997) Based on this researchers have begun to use slow rTMS to treat brain hyperexcitability disorders like auditory hallucinations (AH) in Schizophrenia Procedure of Studies Slow rTMS (1 hertz), was administered to the left temporoparietal cortex, (which has been shown to be active during AH), of right handed patients for up to about 15min a session for about 1-2 weeks Patients had Schizophrenia and reported AH on a daily basis Patients AH were assessed by the Auditory Hallucinations Rating Scale (AHRS), developed by Hoffman et al., before, during and after the treatment In a double blind protocol, patients were randomly assigned to either the treatment or sham condition Sham condition was the same as treatment except the coil was angled 45° from the scalp. This produced the same sounds and feeling of ‘knocking on the scalp’, but without the brain stimulation. Research studies Transcranial magnetic stimulation and auditory hallucinations in schizophrenia (Hoffman et al, 2000) Studied 12 Schizophrenic patients with AH and used a double-blind crossover design with a sham-stimulation control condition the effects of 4, 8, 12, and 16 minutes of stimulation administered on four separate days were assessed. Improvements in AH were significantly greater for rTMS than sham in the 12 and 16 Research studies Transcranial magnetic stimulation and auditory hallucinations in schizophrenia (Hoffman et al, 2000) Possible Limitations: Possible individual differences in anatomical location of primary speech area Patients who receive rTMS condition first might have effects on sham condition 5 patients were taking anticonvulsant drugs and this seemed to have an affect on reduction of AH after rTMS rTMS at 45° in sham condition may still be active on cortex Research studies Temporoparietal Transcranial Magnetic Stimulation for Auditory Hallucinations: Safety, Efficacy and Moderators in a Fifty Patient Sample (Hoffman et al., 2005) Studied 50 schizophrenic patients with AH and used a double-blind random assignment to either active or sham condition Excluded patients with history of seizures Trials lasted 8mins on day 1, 12mins on day 2, and 16mins on subsequent 7days AH were significantly reduced in active compared to sham condition Research studies Temporoparietal Transcranial Magnetic Stimulation for Auditory Hallucinations: Safety, Efficacy and Moderators in a Fifty Patient Sample (Hoffman et al., 2005) Possible Limitations: Possible individual differences in anatomical location of primary speech area Half the patients were recruited on a previous study so recruiting procedures could have changed Patients were taking various neuroleptics during this study which might have had an interaction rTMS at 45° in sham condition may still be active on cortex Research studies Slow Transcranial Magnetic Stimulation Can Rapidly Reduce Resistant Auditory Hallucinations in Schizophrenia (Poulet et al., 2005) Studied 10 Schizophrenic patients with AH in a double-blind cross over Gave 1000 stimulations twice a day for 5 days, for each condition Roughly twice as much stimulation as Hoffman et al., in half the time Found a significant reduction in AH Also used a real sham stimulator Research studies Slow Transcranial Magnetic Stimulation Can Rapidly Reduce Resistant Auditory Hallucinations in Schizophrenia (Poulet et al., 2005) Possible Limitations: Possible individual differences in anatomical location of primary speech area Patients who receive rTMS condition first might have effects on sham condition The more intense sessions might have increased risk of adverse effects A few patients were taking anticonvulsant drugs which was shown in Hoffmann et al., (2000) to affect rTMS on AH Research studies Transcranial magnetic stimulation for auditory hallucinations in Schizophrenia (McIntosh et al., 2004) Replicated Hoffman et al, 2000 Studied 16 Schizophrenic patients with AH and used a double-blind crossover design the effects of 4, 8, 12, and 16 minutes of stimulation administered on four separate days were assessed Each minute of stimulation was followed by 15 seconds of rest to check coil position and allow patients to move Patients AH improved in both active and sham with no significant difference So they failed to replicate Hoffman et al., results Research studies Transcranial magnetic stimulation for auditory hallucinations in Schizophrenia (McIntosh et al., 2004) Possible Limitations: The 15 seconds of rest after each minute may have curtailed the physiological effects of rTMS Possible individual differences in anatomical location of primary speech area Patients who receive rTMS condition first might have effects on sham condition rTMS at 45° in sham condition may still be active on cortex Research studies Neuronavigated transcranial magnetic stimulation and auditory hallucinations in a schizophrenic patient: Monitoring of neurobiological effects (Langguth et al., 2005) A case study of a male with disorganized Schizophrenia with AH who was not responding to neuroleptics or CBT Decided to try rTMS First a PET and MRI was done to find the exact area of activation during AH This allowed the TMS coil to be exactly positioned over the site of increased activation in the left temporal cortex 28 sessions of 2000 stimuli were administered and PET was followed up after 2 and 5 weeks The PET scans revealed an attenuation of the initial increased activation compared with normals Research studies Neuronavigated transcranial magnetic stimulation and auditory hallucinations in a schizophrenic patient: Monitoring of neurobiological effects (Langguth et al., 2005) This study shows that neuroimaging is suitable for detecting changes in auditory processing and for AH This study and previous studies show that the superior temporal gyrus is important in the pathophysiology of AH Also neuroimaging before rTMS can circumvent the problem of individual differences in anatomical location of auditory area’s involved in AH Although this is only a case study Neurobiology of the Disorder Auditory Hallucinations (AH) occur in 60 – 80% of people with Schizophrenia (Hoffman et al., 2005) Neuroimaging studies show that activation of brain areas involved in speech perception play a role in producing AH Dierks et al., (1999) showed that primary auditory cortex is activated in hemisphere dominant for handedness during AH and bilaterally during acoustic stimulation Lennox et al., (2000) showed that superior temporal, middle frontal and inferior parietal gyri were activated during AH Neurobiology of the Disorder Slow rTMS is thought to reduce AH because it induces long term depression (Hoffman et al., 2002) Long-term depression (LTD) and long-term potentiation (LTP), are hypothesized to mediate information storage in the brain, by enduring modifications in synaptic strength LTP can be induced by high-frequency stimulation (40-100 hertz), where potentiated synapse are more likely to produce an action potential and can last from hours up to years Whereas LTD can be induced by low-frequency stimulation (1 hertz), and synapses are weakened making it less likely for an action potential. Furthermore, low-frequency stimulation is able to reverse high-frequency-induced potentiated synaptic responses, a phenomenon referred to as “depotentiation,” (Hoffman et al., 2002) Neurobiology of the Disorder Slow rTMS is thought to induce LTD because it produces the same low frequency (1 hertz) stimulation in brain cells as direct electrical stimulation This would explain why Slow rTMS (≤ 1 hertz) induces inhibition whereas fast rTMS (>1 hertz) induces excitation. Also low frequency direct electrical stimulation over many days has been shown to induce longer periods of LTD, which is also seen in slow rTMS over many days (Hoffman et al., 2002) So this means that slow rTMS reduces AH by reducing the synaptic strength in the auditory cortex through LTD Although LTD is simply not enough to completely explain the effects of slow rTMS on the complex intracortical circuitry Evaluation Advantages: It’s a non-invasive way that may produce somewhat long lasting changes in brain disorders like Schizophrenia, through depotentiation Doesn’t have the side effects of drugs, as long as safety guidelines are followed Provides precise information on functional significance of specific brain regions Can establish causal link between brain activation and behaviour Evaluation Disadvantages: Strict ethical guidelines must be followed Magnetic fields will disrupt electrical devises like pace makers, etc. Can cause hearing loss because sound emitted is in the frequency range 2–7 kHz where the human ear is the most sensitive, so must wear ear plugs Can cause headache because of activation of scalp and neck muscles TMS operates at high voltages so must be careful around equipment Can possibly cause seizure with fast rTMS Conclusion I believe that TMS is a very promising new method to study normal and abnormal brain functioning and to treat various mental disorders Although not all patient groups can receive TMS (i.e. patients with seizure disorders) More studies need to be done to clarify the effects of slow rTMS on the brain Intervention studies with TMS should use patient specific neuroimaging to circumvent individual anatomical differences and to enhance outcome