Cooling off on Therapeutic Hypothermia
advertisement
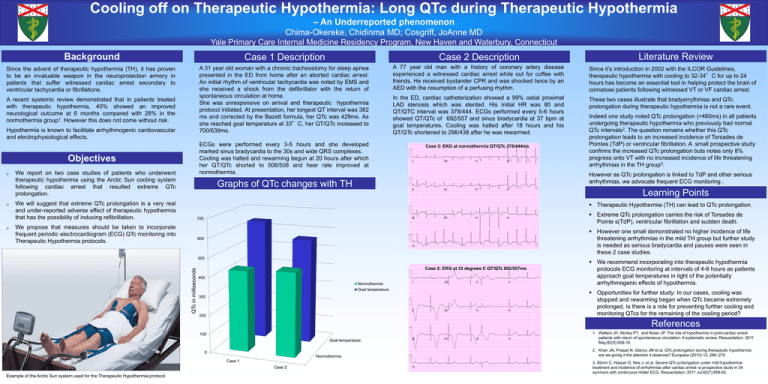
Cooling off on Therapeutic Hypothermia: Long QTc during Therapeutic Hypothermia – An Underreported phenomenon Chima-Okereke, Chidinma MD; Cosgriff, JoAnne MD Yale Primary Care Internal Medicine Residency Program, New Haven and Waterbury, Connecticut Background Case 1 Description Case 2 Description Since the advent of therapeutic hypothermia (TH), it has proven to be an invaluable weapon in the neuroprotection armory in patients that suffer witnessed cardiac arrest secondary to ventricular tachycardia or fibrillations. A 31 year old woman with a chronic tracheostomy for sleep apnea presented in the ED from home after an aborted cardiac arrest. An initial rhythm of ventricular tachycardia was noted by EMS and she received a shock from the defibrillator with the return of spontaneous circulation at home. She was unresponsive on arrival and therapeutic hypothermia protocol initiated. At presentation, her longest QT interval was 382 ms and corrected by the Bazett formula, her QTc was 429ms. As she reached goal temperature at 33°C, her QT/QTc increased to 700/639ms. A 77 year old man with a history of coronary artery disease experienced a witnessed cardiac arrest while out for coffee with friends. He received bystander CPR and was shocked twice by an AED with the resumption of a perfusing rhythm. Since it’s introduction in 2002 with the ILCOR Guidelines, therapeutic hypothermia with cooling to 32-34°C for up to 24 hours has become an essential tool in helping protect the brain of comatose patients following witnessed VT or VF cardiac arrest. In the ED, cardiac catheterization showed a 99% ostial proximal LAD stenosis which was stented. His initial HR was 80 and QT/QTC interval was 378/444. ECGs performed every 5-6 hours showed QT/QTc of 692/557 and sinus bradycardia at 37 bpm at goal temperatures. Cooling was halted after 18 hours and his QT/QTc shortened to 298/438 after he was rewarmed. These two cases illustrate that bradyarrythmias and QTc prolongation during therapeutic hypothermia is not a rare event. A recent systemic review demonstrated that in patients treated with therapeutic hypothermia, 40% showed an improved neurological outcome at 6 months compared with 28% in the normothermia group1. However this does not come without risk. Hypothermia is known to facilitate arrhythmogenic cardiovascular and electrophysiological effects. ECGs were performed every 3-5 hours and she developed marked sinus bradycardia to the 30s and wide QRS complexes. Cooling was halted and rewarming begun at 20 hours after which her QT/QTc shorted to 508/508 and hear rate improved at normothermia. Objectives Indeed one study noted QTc prolongation (>460ms) in all patients undergoing therapeutic hypothermia who previously had normal QTc intervals2. The question remains whether this QTc prolongation leads to an increased incidence of Torsades de Pointes (TdP) or ventricular fibrillation. A small prospective study confirms the increased QTc prolongation buts notes only 8% progress onto VT with no increased incidence of life threatening arrhythmias in the TH group3. However as QTc prolongation is linked to TdP and other serious arrhythmias, we advocate frequent ECG monitoring . Graphs of QTc changes with TH Learning Points We will suggest that extreme QTc prolongation is a very real and under-reported adverse effect of therapeutic hypothermia that has the possibility of inducing refibrillation. Therapeutic Hypothermia (TH) can lead to QTc prolongation. Extreme QTc prolongation carries the risk of Torsades de Pointe s(TdP), ventricular fibrillation and sudden death. We propose that measures should be taken to incorporate frequent periodic electrocardiogram (ECG) QTc monitoring into Therapeutic Hypothermia protocols. However one small demonstrated no higher incidence of life threatening arrhythmias in the mild TH group but further study is needed as serious bradycardia and pauses were seen in these 2 case studies. QTc in milliseconds We report on two case studies of patients who underwent therapeutic hypothermia using the Arctic Sun cooling system following cardiac arrest that resulted extreme QTc prolongation. Case 2: EKG at normothermia QT/QTc 378/444ms Literature Review Case 2: EKG at 33 degrees C QT/QTc 692/557ms We recommend incorporating into therapeutic hypothermia protocols ECG monitoring at intervals of 4-6 hours as patients approach goal temperatures in light of the potentially arrhythmogenic effects of hypothermia. Opportunities for further study: In our cases, cooling was stopped and rewarming began when QTc became extremely prolonged. Is there is a role for preventing further cooling and monitoring QTcs for the remaining of the cooling period? References 1. Walters JH, Morley PT, and Nolan JP. The role of hypothermia in post-cardiac arrest patients with return of spontaneous circulation: A systematic review. Resuscitation. 2011 May;82(5):508-16. 2. Khan JN, Prasad N, Glancy JM et al. QTc prolongation during therapeutic hypothermia: are we giving it the attention it deserves? Europace (2010) 12, 266–270 Example of the Arctic Sun system used for the Therapeutic Hypothermia protocol 3. Storm C, Hasper D, Nee J, et al. Severe QTc prolongation under mild hypothermia treatment and incidence of arrhythmias after cardiac arrest--a prospective study in 34 survivors with continuous Holter ECG. Resuscitation. 2011 Jul;82(7):859-62.