RoleSpeechPathology_PD - Pakistan Parkinson`s Society
advertisement
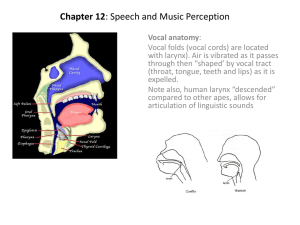
Parkinson’s Disease Role of Speech Language Pathology Dr. Mariam H Syeda Speech-Language Pathologist MBBS, CCC-SLP Ziauddin College of Speech Language Therapy Cognition Voice swallow language speech Speech Language Pathology Areas Affected in Parkinson’s • • • • Voice Speech Swallow Cognition Outline • Area Affected in PD – Symptoms – Causes – Evaluation/Treatment – Tips to take home • Available Resources – ZCSLT • Projects VOICE Voice symptoms • Voice Quality – Hoarse or breathy – caused by the vocal folds not firmly meeting in a regular rhythm or closing pattern (bowing of vocal folds) Voice symptoms • Loudness – Reduced loudness • Evidence suggests breakdown in patient’s sensory processing – “My wife is hard of hearing.” • Inaccurate sense of vocal effort – “It feels shouting.” like I am shouting. • Individuals with PD “overhear” themselves Voice symptoms • Pitch: – Speech has very little melody or pitch variation. – Monotone pitch (decreased up and down movement of the larynx) – can be hard to listen to because it is the inflection of speech that keeps listeners involved in a conversation – lacks liveliness, can be boring to listen to and sometimes it is misunderstood. Evaluation • Informal – Recordings – Voice tasks • Formal – DRS (Dr. Speech) – Virtual Voice Trainer Treatment • Traditional Voice Therapy • Specific voice rehabilitation programs – LSVT • Voice evaluation/treatment software – DRS Lee Silverman Voice Treatment (LSVT) • Intensive voice treatment program: – Designed to teach an individual with PD to improve functional intelligible oral communication by increasing vocal loudness • Treatment Duration: – 16 intensive individual sessions, 4x/week – Maintenance: 6 to 12 months (daily practice) Lee Silverman Voice Treatment • Theory: – Model of Intention: – When subjects speak with intent, their speech was observed as slower and louder with better articulation and increased quality. – “Think Loud, Think Shout” LSVT Outcomes • Improvements subsequent to LSVT treatment have included changes in – facial expression (Spielman, Borod, & Ramig, 2003), – speech intensity (Ramig et al., 1995), – vocal cord adduction (Smith et al., 1995) and – sub-glottal air pressure (Ramig & Dromey, 1996). – Positive improvements in swallowing (Sharkawi et al 2002) LSVT Cognitive Perspective – LSVT is not a cognitively demanding intervention approach (Sapir & colleagues, 2003). • Some individuals with PD present with symptoms of dementia (Sapir & colleagues, 2003). • may have difficulty completing multi-step tasks (Yorkston, Miller, & Strand, 2004). • LSVT simple intervention tasks that are motivating to the individual (Yorkston, Miller, & Strand, 2004). Dr. Speech • Dr. Speech is a comprehensive real-time speech and voice assessment and training software system • It helps to teach, reinforce, document and report speech production in various animated tasks. • 6 components, each targeting a different function DRS – Dr. Speech • This game-like tool; Provides immediate visual feedback to the client on their performance Is versatile and has unique features Enables a quick review of the graphical display or statistical data of the client’s performance. Provide real-time recording and playback help maximize the client’s therapy. 6 Components of DRS Voicing Onset Voicing Phonetic Exercise Maximum Phonation Time (MPT) Pitch Loudness Tips to improve….. Quality • ❑ Try to produce a sharp sound while producing voice • ❑ Keep the loudness level of the voice up by pushing air from the abdomen. • ❑ Practice speech drills and lip/tongue strengthening exercises • ❑ avoid excessive coughing, throat clearing or yelling. • ❑ Protect the vocal folds by keeping the home air moist (humidifier) Tips to improve….. Loudness Take a big breath before beginning to speak. Use short sentences/phrases Use abdominal muscles when yelling/screaming Maintain good posture Open mouth behavior when speaking Tips to improve….. Pitch • Question- Statement Contrast: • When making a statement, start the sentence at a slightly higher pitch, and bring it down at the end – I am not going home. ➷ • When asking a question, start lower and raise the pitch at the end. – I am not going home? ➹ Tips to improve….. Pitch • ❑ Emphasize important words by increasing the pitch when they are said. – Turn right at the signal • ❑ When reading the speech practice material, draw arrows to aid in indicating when to change the pitch. • ❑ Practice pitch changes when singing. Try to exaggerate the pitch range when singing. SPEECH Speech Characteristics • Hypokinetic Dysarthria • Fast Rate of Speech – Sometimes people with PD experience “rushes” of speech – • very rapid speech • And an uneven tempo. – Speech becomes difficult to understand. • Unclear Speech – individual speech sounds are not made clearly or precisely speech sounds “slurred” Speech characteristics • • • • • • • • Hypokinetic Dysarthria: Monopitch Monoloudness Reduced stress Short phrases Variable rate Short rushes of speech Imprecise consonants Cause of unclear speech: • • • • Decreased mouth opening Slow and imprecise lip movements Slow and imprecise tongue movements Poor ability to move the tongue and lips together in a way that is coordinated and rapid enough to be able to produce all of the speech sounds clearly Speech Evaluation • Oro-motor Examination • Speech Assessment Batteries • DRS – – Quantitative data Therapy for Clear Speech • Conventional speech therapy exercises • DRS • Delayed Auditory Feedback (DAF) – Rate of speech • Voice Amplifiers Speech Exercises • lip strength and flexibility exercises • tongue strength and flexibility exercises Example… Purse lips, pucker and say OOO… Example… Blow air through straw while putting up cheeks as much as possible. Clear Speech Tips • Before starting to speak, swallow all excess saliva in the mouth. • Say all sounds clearly and firmly – exaggerate the sounds and do not leave any sounds of any words out. • Start by practicing single words, then two and three word phrases, short sentences and paragraphs Clear Speech Tips • Pause between words • keep the vocal loudness up until the end of the sentence • Try making a fist when speaking, or pushing • use shorter sentences • Simplify the message for the listener • Speak at a slightly slower than normal rate • Do not strain to say every word perfectly SWALLOW Swallowing • Oral Phase • Pharyngeal Phase • Esophageal Phase • Swallowing Dysphagia • A disorder of swallowing • common consequence of PD, with reports of 40% to 100% of patients in the later stages experiencing symptoms like – ❑ Slow rate of eating. – ❑ Fatigue during eating. – ❑ Food “sticking” in the throat. – ❑ Coughing or choking on food or liquid. – ❑ Difficulty in swallowing pills. • May lead to aspiration pneumonia Effects of PD on swallowing Oral • typical repetitive, AP rolling pattern in lingual propulsion of the bolus (rockingrolling motion) • excessive tongue pumping movements • anterior loss due to poor lip seal • Posterior spillage pharyngeal • delays in the triggering of the pharyngeal phase • Larygeal elevation and closure incomplete • impaired pharyngeal motility • deficient epiglottic retroflexion • laryngeal penetration/aspiration , pooling/residue in sinuses esophageal • incomplete UES relaxation and reduced UES opening during swallowing • stasis of bolus aspiration after swallow • These behaviors were more prevalent in liquid than in semi-solids or solids. Effects of PD on Cough Reflex • desensitization of pharyngeal, laryngeal or tracheal mucosa – resulting in failure to clear substances from the upper airway – thought to be the result of impairment to the sensory components of the vagus and glossopharyngeal nerves. • This may account for the high incidence of – silent aspiration – aspiration pneumonia Evaluation • Evaluation – Informal • Bedside Swallow Evaluation – Formal • Modified Barium Swallow Treatment • Treatment – Compensatory strategies – Diet modification • Liquids are the toughest • Pureed diet is easier – Therapeutic strategies – VitalStim Therapy • Neuromuscular electrical stimulation for Swallowing CONSISTENCY EXAMPLES Thin liquid Milk, fruit juice Thick liquid Soup, milkshake Puree Yogurt, custard Soft solid Mashed potato, porridge, khichdi Hard solid Biscuits, chappati, toast, salads VitalStim Neuromuscular Electrical Stimulation for Dysphagia Proven safe (the only FDA approved device for swallow) Remarkably successful ZCSLT has the only certified VitalStim provider in Pakistan Dysphagia management Safe Swallow Tips • Eat only those consistencies that have been recommended as being safe • Sit upright at 90 degrees • Stay upright for at least 30 mins after taking anything by mouth • Chin tuck – when swallowing • No distractions ZIAUDDIN COLLEGE OF SPEECH LANGUAGE THERAPY Evaluation & Therapy for all areas in PD: Voice Swallow Speech Cognition Sessions - One-on-one & Group - Each is session is for 30-45 mins NEW PROJECTS VitalStim Therapy Modified Barium Swallow Study VOICE & SWALLOW LAB Video Stroboscopy Unit Digital Swallowing Station


![Dysphagia Webinar, May, 2013[2]](http://s2.studylib.net/store/data/005382560_1-ff5244e89815170fde8b3f907df8b381-300x300.png)