The Comprehensive Stuttering Therapy Program: Development
advertisement
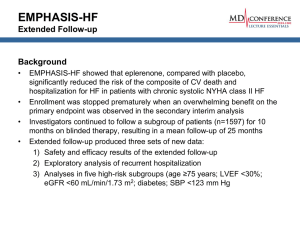
The Comprehensive Stuttering Therapy Program : Development & Initial Outcomes Farzan Irani Assistant Professor Department of Communication Disorders “Share & Tell” College of Health Professions February 16th, 2012 OUTLINE Discussion of Objectives/Learner Outcomes CSTP-A Overview – – – – History & Development Research Objectives Program Structure Initial Outcome Data Discussion/Evaluation of Program Future Clinical and Research Directions OBJECTIVES As a result of this presentation participants will be able to: – – – – – Describe the nature of stuttering. Identify methods to behaviorally assess and treat stuttering. Identify the pros and cons of intensive therapy for adults who stutter. Identify the importance of providing regular follow-up therapy for clients attending an intensive stuttering therapy program. Identify the pros and cons of providing therapy for Adults Who Stutter via telepractice. STUTTERING Let’s see! Core & Secondary behaviors Often described as an “Iceberg” A-B-C http://www.citylit.ac.uk/resources/media/image/Iceberg.jpg BEHAVIORAL ASSESSMENT Important to measure: – Severity of overt behaviors. – Impact of stuttering on communication attitude and Quality of Life (QOL). Measures of severity: – Calculating Percentage of Syllables Stuttered (%SS) from a variety of speech samples. – Stuttering Severity Instrument – 4th Edition (SSI-4). Measures of Communication Attitude & QOL: – Erickson S-24 Scale of Communication Attitudes (S-24) – Overall Assessment of the Speakers Experience of Stuttering (OASES). • Both questionnaires to be completed by the client/participant. BEHAVIORAL TREATMENT Important to remember that stuttering is a multidimensional disorder –hence treatment must address all aspects: – Stuttering Severity: Addressed by the use of a variety of methods to enhance the forward flow of speech and fluency. – Attitudes and QOL: Addressed by the use of Cognitive Behavioral Therapy principles, Mindfulness, and more recently the use of principles from “Acceptance and Commitment Therapy” and “Dialectical Behavioral Therapy.” Very limited data to support the benefits of addressing attitudes and QOL; however, it is strongly recommended by newer qualitative studies, anecdotal data, self-help/advocacy groups, and experiential experts. CSTP-A: HISTORY & DEVELOPMENT Offered at Texas State University – San Marcos in Summer 2011 for the first time. Largely influenced and builds on the Intensive Stuttering Clinic for Adolescents and Adults (ISCAA) offered by Rodney Gabel Ph.D., BRS-FD since 2003. Developed and builds from my research and clinical experiences: – – – Investigation and application of telepractice follow-up to supplement Intensive Stuttering therapy (Irani & Gabel, 2011). Qualitative investigation of factors that client report as helpful and not helpful in the therapy process (Irani, 2010; unpublished dissertation). The need for better documentation and reporting of clinical outcome data. Developed during 2010 as part of a fluency cognate for graduate students in the Department of Communication Disorders Purpose of the program: – – – Offer quality services for clients. Increase/improve student training and clinical education in the area of fluency disorders. Develop a systematic research program to assess: a) Treatment outcomes for intensive stuttering therapy; b) Treatment outcomes for telepractice; c) Evaluate student learning as part of participating in an intensive therapy program. RESEARCH OBJECTIVES Measure quantitative and qualitative treatment outcomes that account for the multifaceted nature of stuttering, including: – Measures of stuttering severity including the Stuttering Severity Instrument, 4th Edition (SSI-4), and percentage of syllables stuttered (%SS) in a variety of speaking tasks, client and clinician perceptual ratings of stuttering severity. – Measures of the clients’ attitudes toward speech and communication and impact on Quality of Life measured the Erickson’s S-24 scale of communication attitudes and the Overall Assessment of the Speaker’s Experience of Stuttering (OASES, Yaruss & Quesal, 2008) . – Qualitative Data gathered from: • Clients • Graduate Student Clinicians. RESEARCH OBJECTIVES Secondary research objective: Student learning outcomes and clinical preparation. – Qualitative study under development – Semi-structured interviews – Gather student perceptions of benefits from participating in the program, including: academic, clinical, and other benefits derived from this program. – All interviews to be conducted after completion of the program . PROGRAM STRUCTURE STRUCTURE– INTENSIVE CLINIC 10-days (2-weeks) Programmatic in nature – – Includes manual, adapted from ISCAA manual developed by Rodney Gabel. Flexible to accommodate unique client needs during individual sessions. Total 60 hours of therapy – – – 20 hours group therapy; 10 AM to 12 PM (program coordinator/supervisors) 40 hours individual therapy 1 PM to 5 PM (student clinicians) 5 days/per week 3 follow-up sessions the week following Intensive Clinic – Supports transfer and stabilization of skills learned during the intensive clinic G ) RI N P - A T T E ( C ST U T E S ULTS D SI V EN O R A H E PR AM F Manual M O OGR nician 11 EC Cli r, 20 TH Y PR me Sum P A ER TH LP C-S SLP ., CC CC., C Ph.D i, .D n h a Ir ,P n tz a r z a ar w ic S r: F ato : Er ant rdin sult Coo Con l : s a n ic Clin nicia t Cli den er Stu eath H , am gr inia ard ro y P Ball Virg ap er ort, Th enp v in g a a r D in tte tu Katr d S te ris, ce a Har i- fa u lt Haly e M ard, th e . n k f e D L -F l o oo RS ua , Br an P, B and e m -S L th C Rutl o m ., C C fr h .D ie d d if e l, P b mo Ga is al ey nu dn ma y Ro b h is * T cted e d ir STRUCTURE– INTENSIVE CLINIC Goals Addressed (overlap present): – Education – Awareness/identification – Desensitization – Mindfulness – Fluency Shaping – Stuttering Modification – Becoming one’s own clinician (transfer & maintenance of skills) STRUCTURE: FOLLOW-UP Tailored to individual client needs. Preferably offered via telepractice to accommodate for Scheduling conflicts and distance from clinic (overall cost). Offered for up to 10 months (2 academic semesters) after completion of the Intensive Clinic. At least one semester of follow-up strongly recommended for all clients. – Research indicates (St. Louis & Westbrook, 1987; Andrews, Guitar, & Howie; Irani, 2010) that intensive programs are good for quick gains; however, follow-up therapy is important to long-term maintenance of gains. TELEPRACTICE DEMONSTRATION INITIAL OUTCOME DATA Program will be completed in May 2012. 3 clients attended the program in Summer 2011, and continue receiving follow-up services. Data collection, organization, and analysis is still underway. Initial outcome measures gathered from the baseline sessions, intensive clinic, and first semester of follow-up are presented. Qualitative interviews to evaluate the intensive clinic completed. Data is not available at this time. – A second interview to evaluate the follow-up program will be conducted after its completion in May. Qualitative interviews with students will be completed after the program completion in May 2012. DATA ANALYSIS Descriptive data presented (visual where possible) Dataset analyzed statistically includes the following measures: – Severity Measures (%SS for conversation, monologue, and reading & SSI-4). – Attitude Measures (S-24 & OASES). All %SS data independently analyzed by 2 trained RA’s – Intra-Class Correlation Coefficient (ICC, Shrout & Fleiss, 1979) calculated – ICC (2, 1)=.854, p=.000. Wilcoxon Signed-Ranks test used to measure statistically significant changes in outcome measures (non-parametric selected due to small n). – Statistics done for major data points including pre-intensive (pre), Post-Intensive (post); follow-up 1 (F1), and follow-up 2 (F2). • Non-parametric equivalent of t-test. DATA POINTS Pre F2 Post F1 PARTICIPANT PROFILE 3 clients: 2 male, 1 female Age ranged from 17:12 years to 43 years Stuttering severity at baseline (SSI-4) ranged from Mild to Very Severe Quantitative data available for baseline measures, postintensive, and 6 month follow-up. – Includes SSI-4 scores, %SS, S-24, and OASES. • OASES and S-24 scores only gathered at major data points to address test-retest reliability. DESCRIPTIVE DATA: %SS CONVERSATION %SS Conversation 18.00 15.90 16.00 14.13 12.00 13.46 13.33 14.00 11.83 11.23 10.00 %SS Conversation 6.33 8.00 6.00 4.00 Cohen’s d = .64 2.00 Cohen’s d = 1.83 0.00 Baseline 1 Baseline 2 Baseline 3 Pre Post F1 F2 DESCRIPTIVE DATA: %SS MONOLOGUE %SS Monologue 20.00 18.27 18.00 16.00 14.20 14.97 13.27 14.00 12.13 12.00 11.50 10.00 %SS Monologue 7.63 8.00 6.00 Cohen’s d = .69 4.00 2.00 Cohen’s d = 1.83 0.00 Baseline 1 Baseline 2 Baseline 3 Pre Post F1 F2 DESCRIPTIVE DATA: %SS READING %SS Reading 16.00 13.63 14.00 11.70 12.00 10.00 11.77 9.47 7.90 8.00 %SS Reading 6.00 3.90 4.00 3.55 Cohen’s d = .36 2.00 Cohen’s d = .97 0.00 Baseline 1 Baseline 2 Baseline 3 Pre Post F1 F2 DESCRIPTIVE DATA: SSI-4 SSI-4 30.00 27.67 MODERATE 26.33 24.67 25.00 22.67 20.33 20.00 MILD 19.00 18.67 15.00 SSI-4 Cohen’s d = .54 V. MILD Cohen’s d = .56 10.00 Intensive 5.00 Withdrawal 0.00 Baseline 1 Baseline 2 Baseline 3 Pre Post F1 F2 DESCRIPTIVE DATA: S-24 S-24 18.00 16.00 16.00 14.00 12.67 12.33 12.00 10.00 7.33 8.00 6.00 4.00 2.00 0.00 Pre Post F1 Cohen’s d = .72 Cohen’s d = 2.94 F2 S-24 DESCRIPTIVE DATA: OASES OASES 5.00 4.50 SEVERE 4.00 3.50 MOD/SEVERE 3.12 3.00 2.50 2.00 MOD 2.11 2.20 Post F1 1.95 MILD/MOD 1.50 1.00 0.50 MILD 0.00 Pre Cohen’s d = 1.83 Cohen’s d = 2.25 F2 OASES RESULTS: STATISTICAL ANALYSES Wilcoxon Signed-Ranks Test conducted to measure whether treatment resulted in statistically significant changes in a variety of outcome measures: – Severity (based on %SS and SSI-4) • Intensive Clinic, Pre-Post Comparison: Z= -2.982, p =.003 • Follow-up, Pre-F2 Comparison: Z=-2.407, p=.016 – Attitude Change (based on OASES and S-24) • Intensive Clinic, Pre-Post Comparison: Z=-1.051, p=.293 • Follow-up, Pre-F2 Comparison: Z=-2.201, p=.028 EVALUATION Initial outcomes data indicates the intensive clinic and follow-up package were effective. – Statistically & Clinically significant changes made at 6 mo. follow-up Intensive clinic good for making gains in outcomes related to stuttering severity. Follow-up services important to maintaining outcomes related to severity and improving outcomes related to attitudes toward speech/communication. Both components of the program appear to help with different aspects of stuttering management: – – Intensive appears to help make rapid changes in severity measures and begin the process of attitude change. Follow-up helps with maintenance of speech related changes and continued improvement with regards to attitude change. • Telepractice appears to be an effective means to deliver follow-up, no comparison data available at this time. INTERESTING TRENDS Pre-Post Intensive Clinic: – – Significant changes on all outcome measures of overt behavior (frequency of stuttering, severity) Clinically significant changes on outcome measures of attitude; however, comparatively small magnitude as measured by Cohen’s d 6-month follow-up data: – – Reduction in the magnitude of change on all outcome measures of overt behavior as measured by Cohen’s d. Increased magnitude and significance on all outcome measures related to attitude. Outcomes data appears to conflict! – – – Qualitative interview = missing piece. Often, as clients become more comfortable with stuttering (increased acceptance) they “take control” and modify their stuttering behaviors. Quantitative data appears to show relapse as a result. Stuttering variability needs to be accounted for. FUTURE DIRECTIONS Major limitation = n – Continue data collection over a period of years to increase n. Continue to offer the program as a package with future changes: – – Inclusion of adolescents Flexibility with follow-up program: choice between in-person and telepractice • Allow for comparison between telepractice and regular follow-up therapy. Possibly offer a “hybrid” version of the program where contact time during the intensive is reduced to ~5 days. – Part of the intensive program offered as a series of online modules. Offer an online only version of the CSTP, compare with existing CSTP outcomes data. ACKNOWLEDGMENT CHP Start-up Monies supported the Clinical Program Texas State University – San Marcos Research Enhancement Program (REP) supported Research Program and supplemented CHP Start-up money. Department of Communication Disorders for supporting this project. Speech-Language-Hearing Clinic and CDIS graduate students for involvement. Special thanks to: – – – – – Dean Ruth Wellborn & Dr. Diana Gonzales for making the project possible. Ms. Renee Wendell for supporting the program as clinical director. Ms. Irene Talamantes for administrative help, and general help setting up the program, providing direction! CDIS graduate Students: Heather Ballard, Virginia Davenport, Katrina Harris, Halya Lenard, and Brooke Lenard for their hard work and devotion. Dr. Eric Swartz from Texas A&M University at Kingsville for supervision support during the intensive clinic. THOUGHTS? QUESTIONS? My Contact Information: – firani@txstate.edu; (512)245-6599 – Yes, the CSTP will be offered again this summer. Adolescents, age 12 years and above are welcome – www.health.txstate.edu/slhclinic/cstp.html