MTiD - presentation - Faculty Development
advertisement
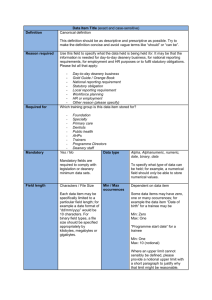
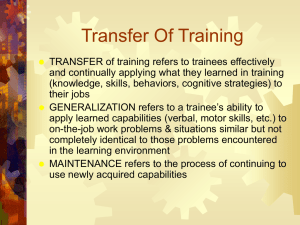
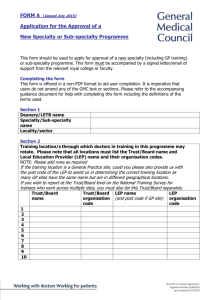
Faculty Development MANAGING TRAINEES IN DIFFICULTY www.londondeanery.ac.uk INTRODUCTIONS • Your name • Your role • What you want to get out of the session LEARNING OBJECTIVES By the end of the course participants will have: • Identified the common symptoms and situations that lead to trainee difficulties • Identified common signs of trainees experiencing difficulty • Discussed principles central to the early identification and management of a trainee in difficulty using the Deanery framework • Discussed recent developments related to revalidation EXPLORING AND DEFINING THE CHALLENGES Identifying poor performance • A good supervisor will support the majority of trainees and clearly identify the struggling minority • But what do we do with this struggling minority? POOR PERFORMANCE From your own experience with trainees: • What are the characteristics of poor performers? • What are the early warning signs (even if you didn’t recognise them at the time) of a trainee in difficulty? EARLY WARNING SIGNS • The disappearing act • Rigidity in thinking • Very slow • Inappropriate emotional outbursts • Failing to gain the trust of others • Colleagues don’t want to call on them • Lack of insight • Problems with probity Paice & Orton (2004) . MANAGING TRAINEES IN DIFFICULTY • Poor performance is a symptom not a diagnosis • Exploration of underlying causes is essential ASSESSMENT DOMAINS Health and home Personality and behaviour Clinical capability Organisational issues HEALTH AND HOME • High workloads and time pressures in clinical practice may lead to depression and anxiety • Firth-Cozens (2003) found significant levels of stress among junior doctors – 28% above threshold levels of stress, compared with18% of the general population • Like anyone else, doctors experience ‘life events’ – family, relationships, finance, etc. PERSONALITY AND BEHAVIOUR • Personality types and learning styles are associated with different responses to working conditions McManus et al. (2004) • Personality strengths under pressure may become problematic, e.g. enthusiastic – volatile Hogan & Hogan (1997) ORGANISATIONAL ISSUES • Poor educational infrastructure, e.g. poor induction, rotation, staffing/workload issues, training and support of supervisors • Bullying, harassment • Service reconfiguration CLINICAL COMPETENCE • Lack of specific practical skills or knowledge, attitudes • Capability • Limited experience in a specific clinical area KEY QUESTIONS • Can the trainee normally perform procedures and work well? • If so, why can’t they perform well now? • Is there a health issue? • Personality and behaviour issues? • Organisational issues? • A combination of issues? RESPONSIBILITIES OF THE EDUCATIONAL SUPERVISOR What are our responsibilities: • to the trainee? • to the rest of the clinical team? • to patients and society in general? • to the Deanery? FRAMEWORK FOR THE MANAGEMENT OF TRAINEES IN DIFFICULTY DEANERY MTID FRAMEWORK Key sections • Identifying that there is a problem • Further considerations • Educational interventions • Record keeping • Formal investigation of clinical performance • Deanery internal processes • Self-help and additional resources CASE STUDIES • Individually, think of a trainee you have supervised and considered to be in difficulty • Briefly present your experience to the group (without breaching confidentiality) • As a group, choose one of the examples presented and use the London Deanery framework to consider how you could address this situation RESOURCES AND SUPPORT London Deanery website • Mednet (confidential, self-referral) • The London Deanery Coaching and Mentoring Service • Careers Unit • Language and Communication Resource Unit Be aware of local resources, including occupational health, trainee’s GP See London Deanery ‘Framework for Managing a Trainee in Difficulty’ for a comprehensive list of resources The Medical Professional Support Unit for London…coming soon RECOMMENDED APPROACH • Act early • No surprises – involve learner • If it isn’t written down it hasn’t happened • Objective – fact not opinion EFFECTIVE EDUCATIONAL SUPERVISION CAN HELP TO PREVENT POOR PERFORMANCE • Clarity of purpose/role with clear objectives • Clear induction programme • Mentoring • Regular review of progress with effective feedback • Encourage reflective practice • 360-degree appraisal • Early identification of difficulty IMPORTANCE OF EFFECTIVE FEEDBACK • Ask trainee’s point of view and encourage reflection • Phrase feedback in descriptive, non-evaluative language • Be specific not general • Address decisions and actions rather than assumed intentions and interpretations • Be constructive – acknowledge appropriate behaviour as well as areas for improvement PERFORMANCE IN PRACTICE – LEARNING PROGRAMME PERFORMANCE IN PRACTICE – LEARNING PROGRAMME Revalidation for trainees Doctors in postgraduate training will hold licences Therefore… Will need to revalidate Every 5 years AND at CCT The Postgraduate Dean is the Responsible Officer for trainees GMC consultation Revalidation: the way ahead March 2010 Findings – October 2010 • Streamlined process • Straightforward • Proportionate • Cost-effective • Efficient What is revalidation? 1. Five-yearly cycle commencing April 2013 2. The cornerstone will be a strengthened version of the appraisal cycle 3. Provides a focus for doctors’ efforts to maintain and improve their practice 4. Facilitates the organisations in which doctors work to support them in keeping their practice up to date 5. Encourages patients and the public to provide feedback about the medical care they receive 6. Contributes to improving the quality of patient care and providing assurance to patients, the public and employers Good Medical Practice Has 7 domains: 1. Good clinical care 2. Maintaining good medical practice 3. Teaching and training, appraising and assessing 4. Relationships with patients 5. Working with colleagues 6. Probity 7. Health New GMC Domains for GMP Domain 1: Knowledge, skills, performance Domain 2: Safety and quality •Maintain your professional performance •Contribute to and comply with systems to protect patients •Apply knowledge and experience to practice •Respond to risks to safety •Ensure that all documentation (including clinical records) formally recording your work is clear, accurate and legible •Protect patients and colleagues from any risk posed by your health Domain 3: Communication, partnership & teamwork Domain 4: Maintaining trust •Communicate effectively •Work constructively with colleagues and delegate effectively •Establish and maintain partnerships with patients •Show respect for patients •Treat patients and colleagues fairly and without discrimination •Act with honesty and integrity ARCP and revalidation Additional information that is likely to be needed at ARCP includes: • Serious incidents (SI) and complaints involving the trainee: – the investigation reports – the trainee’s reflection – consequent education planning arising from the incident and progress made • Employer reports of routine clinical performance of the trainee: – training posts – any out-of-training/locum posts taken in year • Reports of other incidents or events relating to the trainee: – that reflect key aspects of their health conduct or behaviour that relates to Good Medical Practice – includes criminal convictions KEY LEARNING POINTS • Causes of poor performance are usually multifactorial • Poor performance often has early warning signs • An educational supervisor needs to be able to make informed judgements about the next steps once poor performance has been identified • Thoughtful support will help most individuals to improve performance