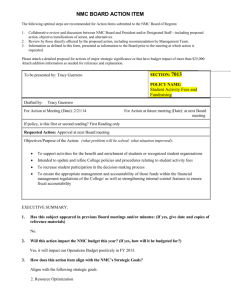
NMC new rules
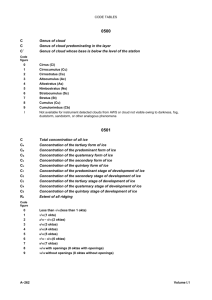
advertisement
NMC Helping Activists support members Roz Hooper Senior Legal Officer RCN Legal Directorate RCN Joint Representatives’ Conference 15th June 2013 Aims of the day: • Understand NMC processes • Recent case types • How can you help members facing NMC proceedings? • CRB/DBS… news How nurses are regulated • • • • Employment contract NMC registration: Fitness to Practise DBS Criminal justice system Who refers nurses to the NMC? NMC in numbers: • Year NMC new referrals New interim orders • 2007/8 1,487 199 (13%) • 2008/9 2,178 252 (14%) • 2009/10 2,988 345 (13%) • 2010/11 4,211 424 (12%) • 2011/12 4,407 922 (21%) Are nurses getting worse? • Nearly 600 nurses and midwives were banned from practising last year by the Nursing and Midwifery Council, Nursing Standard has learned. • A total of 589 nurses were removed from the NMC register following fitness to practise (FtP) hearings in 2012/13, up from 365 in 2011/12. • Real reason: Up to Jan 2012, 9 cases being heard a day, now 22.. Clearing Outcomes in the NMC: • RCN secures a no case to answer or no sanction finding in 85% of cases. NMC equivalent for all cases is 81% (but not quite like for like as figure includes 40% screened out, many without notification) • Rest were no sanction/ cautions /Conditions of practice/ suspensions/ strike off NMC: The practicalities • Court room set up: Panellists and Legal Assessor • Standard of proof: Balance of probabilities • RCN representation: Usually specialist barrister Fitness to Practise Cases • “Fitness to practise is a registrant’s suitability to be on the register without restrictions.” • Reporting a case of unfitness to practise to the NMC is only appropriate if the conduct, practice or health of a registrant is impaired to the extent that public protection may be compromised • (Reporting unfitness to practise: A guide for employers and managers. NMC 2004) NMC Advice to employers • Do all you can at a local level • We will not normally become involved in a case if you cannot demonstrate that you have already taken measures to tackle the situation at a workplace level. • Before contacting us, make sure you: • carry out your own internal investigations • carefully collect and manage evidence • make use of your own disciplinary and competence procedures Types of cases: • Misconduct • Lack of competence • Health • Conviction or caution • Determination by another body It is current fitness that is assessed Typical misconduct cases • Clinical: drug errors, neglect, recording errors, missed observations, home manager failings etc • Dishonesty: working while on sick leave, sleeping on duty, misleading on CV, failing to disclose NMC referral to employer, altering a record • Abuse of patients : shouting, rough handling • Boundaries: flings with patients, language, social network sites, colleagues Case study 1 Comments to Colleagues (not malicious): ‘This response would not have been given to a white woman and the fact that Ms Rowe was a black woman was fundamental to the listener’s perception of humour. This had the effect of isolating Ms X and making her feel different. For these reasons the panel concludes that the joke was a racist joke and thus a racist remark as charged’ Sanction: 2 year caution Case study 2 • 4 failures to administer medication, and record that she had administered it • 12 month Conditions of practice • “You must not carry out the administration of medication unless under the direct supervision of another registered nurse” Case study 3 Sexual relationships with 2 student nurses registrant was mentoring “Both of the relationships that Mr Y had with Student A and Student B were consensual. The panel has heard from Mr Y today and he has expressed remorse and shame for his failings” Sanction: 12 month caution order Case Study 4 • Some poor practice, and undertook invasive procedures that were unjustified and made an inappropriate comment to Patient B with words to the effect “It’s time to go for the big sleep” • Did not attend, so no insight or attempts to remedy • Sanction: Struck off Danger areas: Social networking sites • Badmouthing your workplace, identifying yourself as a nurse and commenting on your Trust’s policies, commenting on colleagues (Where I work they are all a load of…) • Communicating with patients (eg ‘Hi Sweetie’) • Commenting on your activities (eg I’m on duty in 4 hours and I am trashed…) Danger areas: Boundaries • You share personal problems or aspects of your intimate life with patients or keep secrets with patients or take gifts. • You become defensive when someone questions your interaction with the patient. • You speak to the patient about your own professional needs or inability. • You speak poorly of co-workers or the hospital to patients. • You speak poorly of co-workers or the hospital to patients. • You talk to patients/families about things that are out of your scope of practice. • You give patients personal contact information/ money or extra attention. • You feel that you understand the patient’s problems better than other members of the healthcare team. DBS (the Disclosure and Barring Service).. Formerly CRB and ISA • Everyone in a nursing role (including HCAs) requires a CRB certificate.. In future to be called a DBS check • Checks contain convictions, cautions and enhanced disclosure, which includes any information that the chief police officer believes ‘might be relevant’ and ‘ought to be included’... so unproven allegations can go in DBS/ISA 2 • If a member is unhappy with the entry in the DBS check, refer to RCND immediately • DBS can also bar people (not just nurses) from working with children or vulnerable adults • If a member is referred, refer to RCND • The new update service Cautions • Police do refer on to the NMC and DBS • NMC treats a caution as an admission that they cannot go behind • The olive oil incident… Advice to a member facing an NMC referral • Contact RCND immediately.. Should be with the lawyer within a day • Tell employer immediately (a duty under the code) • Write reflective pieces.. Consider how to demonstrate remorse and remediation (courses and work) • Keep the evidence/witness details.. but don’t breach patient confidentiality Any questions or comments?