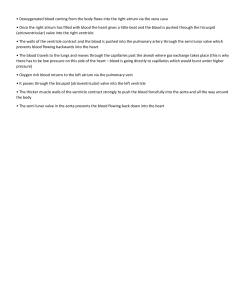
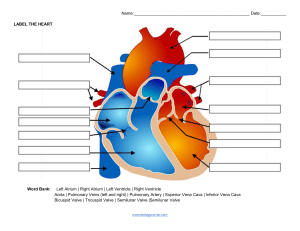
CVS MODULE The heart consists of four chambers, two atria (upper chambers) and two ventricles (lower chambers). There is a valve through which blood passes before leaving each chamber of the heart. The valves prevent the backward flow of blood. These valves are actual flaps that are located on each end of the two ventricles (lower chambers of the heart). They act as one-way inlets of blood on one side of a ventricle and one-way outlets of blood on the other side of a ventricle. Normal valves have three flaps, except the mitral valve, which has two flaps. The four heart valves include the following: • • • • tricuspid valve: located between the right atrium and the right ventricle. pulmonary valve: located between the right ventricle and the pulmonary trunk. mitral valve: located between the left atrium and the left ventricle. aortic valve: located between the left ventricle and the aorta. As the heart muscle contracts and relaxes, the valves open and shut, letting blood flow into the ventricles and atria at alternate times. 1) Tricuspid valve which has 3 cups: Each cup consists of 2 layers of endocardium and thin fibrous tissue layer in between, The cup attached by its base to the fibrous ring surrounds the orifice while its apex hangs into ventricular cavity which gives insertion to the Chordae tendineae. The atrial surface is smooth, and the ventricular surface is rough. Between the right atrium and right ventricle. 1 | Page 2)pulmonary valve: It guards the pulmonary trunk, exists between the right ventricle and the pulmonary trunk. Consists of 3 semilunar cusps, its base attached to the wall of wall the pulmonary trunk while its free edges directed upwards into the lumen of the trunk. 3) Mitral valve (bicuspid): Opens into the left ventricle, has only 2 cusps. 4) Aortic valve: A 3 semilunar valve between the left ventricle and the aorta. They are all part of the endocardium. The most common organism of Rheumatic fever is Streptococcus. Especially streptococcus pyogenes. It’s a major humanspecific bacterial pathogen that causes a wide array of manifestations ranging from mild localized infections to lifethreatening invasive infections. gram-positive, catalase-negative, oxidase negative, non-sporulated, non-motile, has a hyaluronic acid capsule which is chemically similar to that of host connective tissue. β-hemolytic streptococci. It is a facultative anaerobe, grows best in 5 to 10% carbon dioxide, and forms pinpoint colonies on blood agar 2 | Page plates. Lancefield serological grouping system is used to differentiate group A streptococci (GAS) from other streptococci. The type A antigen of S. pyogenes is a polysaccharide which is comprised of N-acetylglucosamine attached to a rhamnose polymer backbone. M protein is the major surface protein presents on S. pyogenes cell wall, S. pyogenes usually colonizes, pharynx, anus, and genital mucosa. Infections caused by S. pyogenes are highly contagious. Transmission can occur through airborne droplets, hand contact with nasal discharge or with objects or surfaces contaminated with bacteria, skin contact with contaminated lesions, or contaminated food sources. Multiple virulence factors are responsible for clinical manifestations of the S. pyogenes. The bacterial capsule consisting of hyaluronic acid provides protection against phagocytosis. M protein, lipoteichoic acid, and protein F are responsible for the attachment of the bacteria to host cells. M protein is also responsible for inhibiting opsonization by binding to complement regulators and to fibrinogen. M protein is the most important virulence factor for S. pyogenes since experiments have shown that M mutants cannot survive in phagocyte-containing human blood. S. pyogenes also produce exotoxins, like a pyrogenic (erythrogenic) toxin, which is responsible for the rash of scarlet fever and toxic shock syndrome. Other virulent factors include streptokinase, streptodornase, hyaluronidase, and streptolysins, which help in the invasion of tissues. What is rheumatic? Its an acute immunologically mediated, multisystem inflammatory diseases that occurs after group A β-hemolytic streptococcal infections usually pharyngitis or skin infections. Rheumatic valvular disease is the cardiac manifestation of rheumatic fever, its associated with inflammation of all parts of the heart, valvular inflammation and scarring produce the most important clinical features. The valvular disease takes the form of deforming fibrotic mitral stenosis. Rheumatic heart disease is essentially the only cause of acquired mitral stenosis. How rheumatic valvular disease happens? Acute rheumatic fever is a hypersensitivity reaction, the antibodies of Astreptococcal molecules cross react with the host myocardial antigen because of antigenic similarity between the streptococcal and human connective tissue. 3 | Page Antibodies against M protein bind to proteins in myocardium and cardiac valves, this binding causes injury through activation of complement and Fc receptorsbearing cells, CD4+T cells that recognize streptococcal peptides can cross-react with host antigens and elicit cytokine-mediated inflammatory responses. Deforming fibrotic lesions develop after healing its associated with resolution of acute inflammation. The pathological changes in the valves: Fibrinoid necrosis and fibrin deposition along lines of closure forming 1-2 mm vegetations (verrucae) which cause disturbance in cardiac function. In chronic rheumatic fever the most important functional consequence of RHD is: Valvular stenosis and regurgitation, stenosis tends to predominate. Mitral valve alone involved in 70% of cases, combined with aortic is 25%. With the pressure overload the atrium progressively dilates leading to atrial fibrillation and thrombosis 4 | Page With left sided heart failure because of the long standing passive venous congestion leads to right ventricular hypertrophy and failure. Prevention measures and role of long acting penicillin: Treatment of acute rheumatic fever consists of antibiotic therapy, antiinflammatory therapy, heart failure management, and commencement of ongoing care (secondary prevention and provision of education), Hospitalization is advisable for optimal management of ARF, especially for an initial episode, so that all tests can be completed, response to therapy can be observed, and long-term preventative measures can be started with appropriate education for the patient and their caregivers. Prevention of initial development of rheumatic fever (primary prevention) is accomplished by prompt diagnosis and antibiotic treatment of group A Streptococcus (GAS) tonsillopharyngitis and, in some settings, GAS pyoderma. Appropriate antibiotic treatment of pharyngitis prevents ARF in most cases, However, at least one-third of ARF episodes occur in the setting of subclinical streptococcal infection, In addition, ARF is not preventable in symptomatic patients who are not able to access medical care. Patients who have had an attack of ARF and develop subsequent group A Streptococcus (GAS) pharyngitis are at high risk for a recurrent attack of ARF. Rheumatic heart disease (RHD) becomes more severe with each recurrent episode. Thus, the most effective method to limit progression of RHD severity is prevention of recurrent GAS pharyngitis. long-term antimicrobial prophylaxis better than recognition and treatment of acute GAS pharyngitis episodes, because GAS infection does not need to be symptomatic to trigger a recurrent attack of ARF. Long-term prophylaxis is warranted for patients with a well-documented history of ARF (including cases with Sydenham chorea [SC] as the sole manifestation), as 5 | Page well as those with definite evidence of RHD. Antibiotic prophylaxis is usually provided in the primary care. Antibiotic selection — For most patients, long-acting penicillin G benzathine administered intramuscularly (IM) every 28 days rather than other regimens, However, there is regional variation in use of penicillin G benzathine depending upon availability and cost. In regions where ARF is endemic, penicillin G benzathine continues to be the preferred agent since it is highly effective, low cost, and readily available. By contrast, in nonendemic regions (eg, the United States and Europe), penicillin G benzathine is more costly, and recurrent shortages are a substantial and recurring problem, Thus, oral agents (eg, penicillin V) are more commonly used in nonendemic compared with endemic regions. Oral agents are also appropriate for patients with the following features: ●Proven penicillin allergy (where a macrolide such as azithromycin is used) ●Severe valvular disease from RHD due to increased risk for sudden death following IM injections ●Bleeding problems following injections that cannot be addressed 6 | Page References https://www.columbiadoctors.org/treatments-conditions/heart-valves-anatomyandfunction#:~:text=tricuspid%20valve%3A%20located%20between%20the,left% 20v entricle%20and%20the%20aorta https://www.ncbi.nlm.nih.gov/books/NBK554528/ https://www.uptodate.com/contents/acute-rheumatic-fever-treatmentandprevention?sectionName=PRIMARY%20PREVENTION&topicRef=114019& anc hor=H7&source=see_link#H7 7 | Page