![GROUP 4 CARDIOVASCULAR SYSTEM PATHOLOGY[1]](http://s2.studylib.net/store/data/027458027_1-ab2511ff13deaf6beb1489324605f5fe-768x994.png)
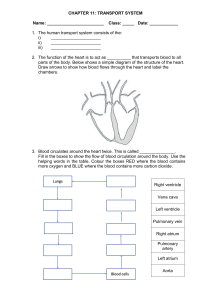
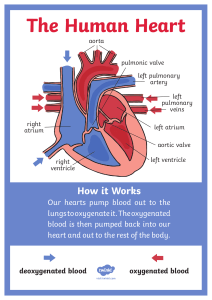
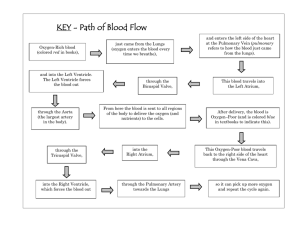
CARDIOVASCULAR SYSTEM Group 4 Terms Ischemia-refers to an interference with blood supply to an organ or part of an organ, depriving the organ’s cells and tissues of oxygen and nutrients. Causes: Narrowing of arterial structures Thrombotic or embolic occlusions Infarction- is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct Haemorrhage- ilocalized area of ischemic necrosis within a tissue or organ produced by occlusion and rupture of a blood vessel Causes Injury such as trauma Atherosclerosis Inflammatory or neoplastic erosions of the vessel wall. CONGENITAL HEART DISEASES DEF: Abnormalities of the heart or great vessels that are present at birth and result in either shunting of blood between the Rt and Lt circulation and/or cause outflow obstruction. They originate from faulty embryogenesis during week 3-8 when major CVS structures develop. Cause unknown in 90%, Environmental factors e.g congenital rubella, maternal DM, alcohol, drugs e.g thalidomide. Genetic factors e.g trisomies 13,15,18,21, Turners syndrome CLASSIFICATION 1.An abnormal communication: ASD, VSD, PDA. atreal septal defect, ventricular septal defect, patent ductus arteriousus 2. An obstruction eg. tricuspid atresia, pulmonary, mitral, aortic valve stenosis, coarctation of aorta. 3. Common chambers- common atrium, common ventricle 4. Abnormal connections (discordance)- Transposition of great arteries. 5. Abnormal situs (position) of heart chambers. LEFT-TO-RIGHT SHUNTS Atrial septal defect(ASD) The most common congenital cardiac lesions are left-to-right shunts which permit mixing of blood in the systemic and pulmonary circulations. Is the most common congenital cardiac lesion which permits free communication btw the two atria as a result of either lack of closure of the foramen ovale after birth or its improper closure during gestation Because the left atrium pressure is usually higher than the pressure in the right atrium, the resulting shunt is from left to right and causes increased pulmonary blood flow and overloading of the right ventricle. This produces the radiographic appearance of enlargement of the rt ventricle, rt atrium and pulmonary outflow tract Apical 4 chamber view echo. Note the enlarged right chambers. Ventricular septal defect(VSD) In pts with vsd, the resulting shunt is also from left to right because the left ventricular pressure is usually higher than the pressure in the right ventricle The shunt causes increased pulmonary blood flow and consequently increased pulmonary venous return. This leads to diastolic overloading and enlargement of the lt atrium and lt ventricle Because shunting occurs primarily in systole and any blood directed to the rt ventricle immediately goes into the pulmonary artery, there is no overloading of the rt ventricle and radiographically no right ventricular enlargement is seen. Patent ductus arteriosus(PDA) Is the third major type of lt-to-rt shunts The ductus arteriosus is a vessel that extends from the bifurcation of the pulmonary artery to joint the aorta just distal to the left subclavian artery. It serves to shunt blood from the pulmonary artery into the systemic circulation during intrauterine life. Persistence of the d.a, which normally closes soon after birth results in a lt-to-rt shunt. The flow of blood from the higher-pressure aorta to the lower-pressure pulmonary artery causes increased pulmonary blood flow, and an excess volume of blood is returning to the lt atrium and ventricle. Radiographically, there is enlargement of the lt atrium, lt ventricle and the central pulmonary arteries, along with diffuse increase in pulmonary vascularity The increased blood flow through the aorta proximal to the shunt produces a prominent aortic knob in contrast to a small- or normal size aorta seen in atrial and ventricular SD All lt-to-rt shunts can be complicated by development of pulmonary hypertension(Eisenmenger’s syndrome) R/A PA chest ASD-enlarged rt ventricle, rt atrium and pulmonary outflow tract VSD-pulmonary trunk enlargement, no rt ventricular enlargement PDA- enlargement of lt atrium, lt ventricle with an increase in pulmonary vascularities US- atrial defect has common atria; ventricular defect demonstrate lack of closure MRI- spin echo MRA breath-hold and cine to investigate morphological and functional anomalies when US is not visible or not diagnostic Tetralogy of Fallot Is the most common cause of cynotic congenital heart disease. It consists of four( thus “tetra”) abnormalities: i) high ventricular septal defect ii) pulmonary stenosis iii) overriding of the aortic orifice above the ventricular defect and iv) right ventricular hypertrophy Pulmonary stenosis cause an elevation of pressure in the rt ventricle and hypertrophy of that chamber Because of the narrow opening of the pulmonary valve, an inadequate amount of blood reaches the lungs to be oxygenated. The VSD and the overriding of the aorta produce rt-to- lt shunting of unoxygenated blood into the lt ventricle and the into the systemic circulation, thus increasing degree of cyanosis R/A PA chest- enlarged right ventricle causes upward and lateral displacement of the heart apex Echocardiography- demonstrates the four abnormalities of the disease. MRI- demonstrates the morphological conditions; spin- echo scans to identify abnormalities, and cine to demonstrate flow void in pulmonary stenosis TETRALOGY OF FALLOT(TOF) Boot shaped heart -. Due to uplifting of the cardiac apex due to right ventricular hypertrophy and concavity of the main pulmonary artery. Coarctation of the aorta Refers to narrowing or constriction of the aorta that most commonly occurs just beyond the branching of the blood vessels to the head and arms ( just beyond the origin of LSA) The blood supply and the pressure to the upper extremities are higher than normal As a result, there is decreased blood flow through the constricted area to the abdomen and legs. Classically the pt has normal blood pressure in the arms, but very low blood pressure in the legs. It is the most common frequent cause of hypertension in children. The relative obstruction of aortic blood flow leads to progressive development of Collateral circulation- the enlargement of normally tiny vessels in an attempt to compensate for the inadequate blood supply to the lower portion of the body R/A PA chest- rib notching Ba. Swallow- opposite of above Echo – demonstrate the severity of the stricture Doppler echo-determines flow gradient and possible collateral vessels Aortography( angiography)- localizes obstruction, determines length of coarctation and identifies an associated malformation MRI-demonstrate narrowing, used for follow-up of corrective surgery Oblique-sagittal ‘black blood’ Turbo-spin echo showing severe discrete coarctation Transposition of the great arteries The common form is the D-loop transposition in which the ventricular anatomy is normal. There is simple reversal of connection of the great arteries, with the aorta arising from the morphologically right ventricle and the pulmonary artery arising from the morphologically left ventricle. The exact orientation is variable, but the most common arrangement is with aortic valve arising from a high anterior position from the rt ventricle, and the pulmonary valve arising from the lower position behind the rt ventricular outflow tract. The normal arrangement where the rt ventricular outflow tract and main pulmonary artery twists around the lt ventricular outflow tract and the aorta, is lost and the two great arteries run upwards parallel to their respective chambers R/A PA chest- heart is slightly enlarged and rounded Echo- clearly show the two great vessels but care must be taken to correctly identify the great arteries, which usually lie in parallel Angiography- will clearly show the abnormal connections and clarify other associated anomalies TGA( TRANSPOSITION OF GREAT ARTERIES)EGG ON STRING, EGG ON SIDE SIGN TRANSPOSITION OF THE GREAT ARTERIES(TGA) MR sagittal: Aorta arises anteriorly from hypertrophied right ventricle. Posterior PA arises from left ventricle. Read other congenital anomalies Double inlet left ventricle Double outlet left ventricle Dextrocardia Tricuspid atresia Pulmonary stenosis Aortic stenosis Congenital cardiomyopathies Truncus arteriosus etc Coronary Artery Disease(CAD) Narrowing of coronary arteries causes oxygen deprivation of the myocardium and ischemic heart diseases. In most patients, narrowing of the lumen of one or more of the coronary arteries is attributable to the deposition of fatty material on the inner arterial wall (atherosclerosis) Predisposing factors to development of CAD; HTN Obesity Smoking A high-cholesterol diet Lack of exercise. The speed and degree of luminal narrowing determine whether an atherosclerotic lesion causes significant and clinically evident ischemia. Temporary oxygen insufficiency causes angina pectoris, a feeling of severe chest pain that may radiate to the neck, jaw and left arm( sometimes both arms), and that is often associated with the sensation of chest tightness or suffocation Occlusion of coronary arteries deprives an area of myocardium of its blood supply and leads to the death of muscle cells (myocardial infarction) in the area of vascular distribution. The size of the coronary artery that is occluded and the myocardium that it supplies determine the extent of heart muscle damage. The greater the area affected, the poorer the prognosis because of the increase loss of pumping function that may result in CHF . A favourable prognosis is the development of collateral circulation, through which blood from surrounding vessels is channeled into the damaged tissue. if pt survives, the infarcted region heals with fibrosis. Long term complication include the development of thrombi on the surface of the damage area and the production of a local bulge ( ventricular aneurysm)at the site of weakness of the myocardial wall R/A PA chest- vessel calcifications SPECT- classifies myocardial necrosis CT-decreased attenuation in the affected myocardial tissue Calcium scoring to visualized hard plaque , CTA to visualize soft plague MRI- increased T2W signal intensity in affected myocardial tissue NM- focal defects(cold spots) after exercise with filling at rest indicate stenosis IVUS( intravascular ultrasound)- vessel size and length of lesion Angiogram- strictures or narrowing are filling defects CT With MDCTA imaging of the more proximal coronary arteries allows reliable exclusion or detection CAD. Oblique coronal MIP reconstruction shows Ca++ of LAD Congestive Cardiac Failure(CCF) Refers to the inability of the heart to propel blood at a volume sufficient to the tissues. Causes Intrinsic cardiac abnormality( include insufficient or defective cardiac filling and impaired contractions for emptying) HTN hypertension Any obstructive process that abnormally increases the peripheral resistance to bood flow PA chest- CTR > 50% Left sided cardiac enlargement, pulmonary oedema, pulmonary effusion Right sided widened mediastenum and elevated right hemidiaphragm Echo – measuring left ventricular performance, ejection fraction and filling pressures of the pulmonary artery and ventricles Hypertension Blood pressure is the function of cardiac output ( the amount of blood pumped per unit time by the heart) and the total peripheral resistance, which reflects the condition of the walls of the blood vessels throughout the body Although the peripheral resistance and the cardiac output may fluctuate rapidly Depending on such factors as whether a person sits or stands and is quiet or excited, the systemic bp remains remarkably constant in a healthy person. Bp reading consists of systolic(highest pressure in the peripheral arteries that occurs when the lt ventricle contracts), and diastolic ( pressure in the peripheral arteries when the lt ventricle is relaxing and filling with the blood form the lt atrium HTN is defined as elevation of systolic pressure above 140mmHg and of diastolic pressure above 90mmHg Forms Most pts with elevated bp has essential or idiopathic htn – characterized by gradual onset and a prolonged course, often of many years A much less common malignant form characterised by abrupt onset, runs a rapid cause and often leads to renal failure or cerebral haemorrhage About 6% of pts have secondary htn resulting from another disease. Underlying causes: renal parenchyma disease Vascular disease Adrenal abnormalities Abnormality involving the secretion of a substance the increases vascular tone and and peripheral arterial substance R/A P/A chest- aortic knuckle prominence Arteriography detects renovascular lesions RN renogram-demonstrate lesions Hypertensive heart disease Long standing HTN causes narrowing of systemic blood vessels and an increase resistance in blood flow. The left ventricle is forced to assume a larger workload, which initially causes hypertrophy and little if any change in radiographic appearance of cardiac silhoutte. R/A PA chest- enlarged lt ventricle, inferior displacement of cardiac apex, aortic tortuosity Aneurysm Is a localized dilatation of an artery that most commonly involves the aorta, especially its abdominal portion It represents a weakness in the wall (decrease elastin and increased collagen production) Types Saccular aneurysm- involves only one side of the arterial wall Fusiform aneurysm Is bulging of the entire circumference of the vessel wall Of a blood vessel caused by atherosclerosis , syphilis or other infection, trauma, or a congenital defect such as Marfan’s syndrome Presence of multiple small anerysms is suggestive of a generalized arterial inflammation (arteritis) R/A Radiograph- calcification outlining vessel Extensive calcification of the Aorta 53 54 Atherosclerosis Arteriosclerosis occurs when arteries become marked by thickening, hardening and lack of elasticity in the arterial wall. Atherosclerosis is one form of arteriosclerosis The major cause of vascular disease of the extremities is atherosclerosis, in which fatty deposits called plaques develop in the intima and produce progressive narrowing and often And often complete occlusion of large and medium size arteries. R/A Plain- calcification demonstrating hardening of the artery Colour Doppler- demonstrates plaque and degree of luminal stenosis MRA- two-dimensional time-of-flight view Demonstrates narrowing and flow changes in infrapopliteal vessels 3-D images demonstrate narrow occlusions as signal absence Traumatic rupture of the aorta Is potentially a fatal complication of closed-chest trauma. In almost all cases(90-95%), the aortic tear occurs just distal to the left subclavian artery at the site of the ductus venosus R/A PA chest – widened mediastinum, deviation of the NG tube to right, apical pleural cap C TA/Aortography- demonstrates tear and heamorrhage A traumatic pseudoaneurysm at the isthmus on arch aortography. A. Aortogram – shows aortic laceration at the isthmus 59 Dissection of the aorta Is a potentially life threatening condition in which disruption of the intima( inner layer) permits the blood to enter the wall of the aorta and separate its layers. As a result of the disruption, the aorta is divided into true and false lumens Most occur in pts with arterial HTN, some are a result of trauma or congenital defect Radiographic appearance Plain.- widening of aortic shadow which may be irregular CT- double-barrel channel with linear filling defect within the lumen(intimal flap) MRI- intimal flap causes medium intensity signal separating true and false lumina; blood flow causes signal void TEE(transesophageal echocardiography)- demonstrates intimal tear, extension of dissection and pleural effusion Aortography-extend of true and false lumina VALVULAR DISEASES Review anatomy of major valves Rheumatic Heart Disease(RHD) Rheumatic fever is an autoimmune disease that results from reactions of a pts antibodies against antigens from a previous streptococci infection(of throat and ear). The symptoms( fever, rash, inflamed and painful joints) typically develop several weeks after the streptococcal infection The major damage of RF is to the valves of the heart, most frequently the mitral and aortic valves. It is the major cause of acquired valvular disease. The allergic response causes inflammation of the valves Deposits of blood platelets and fibrin from blood flowing over the valve produce small nodules (vegetations) along the margins of the valve cusps. The thickened valves may stick together, so that the valvular opening remains permanently narrowed(stenosis) rather than opening properly when blood flows through. Fibrous scarring may cause retraction of the valves cusps so that the cusps are unable to meet when the valves tries to close; this is insufficiency, and blood leaks through the valve when it should be closed. Imaging Doppler echocardiography- quantify valvular insufficiencies Mitral stenosis Almost always a complication of rheumatic disease, results from diffuse thickening of the valve by fibrous tissue, calcific deposits, or both. R/A PA chest- left atrium enlargement Lateral,RAO- posterior displacement of oesophagus, left main bronchus and calcification of valves Echocardiography-chamber enlargement, wall thickness and size of valvular orifices Sine MRI- demonstrates and quantitates abnormal flow patterns Read mitral insufficiency Aortic stenosis May be caused by: RHD Congenital valvular deformity(esp of bicuspid origin) Degenerative process of aging( idiopathic calcific stenosis The obstruction to lt ventricular outflow in aortic stenosis increases the workload of the lt ventricle R/A PA chest- enlargement of lt ventricle, rounding of the cardiac apex Posterior displacement of the cardiac apex in the lateral projection Lateral- posterior displacement of cardiac apex , bulging of ascending aorta Aortic valve calcification Read aortic insufficiency Infective endocarditis Refers to the formation of nodules or vegetations on heart valves by deposits of bacteria or fungi. Unlike the small nodules in rheumatic fever, the vegetations in I.E are filled with bacteria and tend to break easily to enter the bloodstream and form septic emboli that Travel to the brain, kidney, lung or other vital organs. R/A Echocardiography- shaggy echoes produce by irregular thickening of affected valves Electron-beam CT- vegetations in valve,valvular calcifications, distirted orifices Pericardial effusion Refers to accumulation of fluid within the pericardial space surrounding the heart. Causes include: Bacteria Viruses Neoplastic involvement idiopathic Imaging PA chest- enlargement of cardiac silhouette Echocardiography- posterior sonolucent fluid collection CT- loculated fluid accumulation around the heart MRI- differentiate serous from hemorrhagic fluid as decreased signal intensity 2.PERICARDIAL EFFUSSION Pericardial effusion in a 40year-old woman with shortness of breath. Axial contrastenhanced CT scan shows an effusion (∗) with the same attenuation as water (0 HU). Deep venous thrombosis DVT which is primarily the major source of potentially fatal pulmonary embolism. Risk factors are related to Virchow's triad: stasis, hypercoagulability, and venous injury. VENOUS DISEASES At times, DVT may be the earliest symptom of an unsuspecting malignancy of the pancreas, lung or G.I.T R/A Venography- constant filling defects or an abrupt ending of the opaque column in a vein, nonfilling of one or more veins, extensive SONOGRAPHIC FEATURES 1. Noncompressibility of vein (loss of “wink” sign) 2. Echogenic lumen 3. Enlarged vein 4. Color Doppler allows differentiation of occlusive and nonocclusive thrombi. 5. Indirect iliac evaluation is possible by evaluating the pulse wave Doppler form. The waveform changes with respiration, augmentation, and Valsalva. 80 Varicose veins Are dilated, elongated and tortuous vessels that most commonly involve the superficial veins of the leg just under the skin. If the venous dilatation becomes extreme, the valves that normally prevent backflow of blood due to gravity become incompetent and cease to function, thus increasing the volume of blood in these slowflowing vessels R/A Venography- demonstrates patency of the deep venous system and degree of collateral circulation from the superficial to deep veins. THANK YOU END