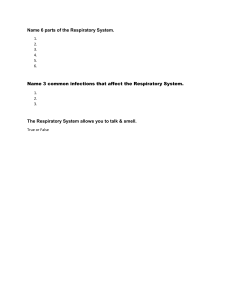
Exam 2 Study Guide Chapter 26 – Respiratory Condi3ons of Childhood - Distinguish between clinical manifestations of various respiratory conditions Respiratory system overview Normal physiology Essential functions o Ventilation o Oxygenation o Removal of waste gases o Protection of airway from harm, infections - Nursing assessment (Box 26.1) o Review of systems: Cough, Wheeze, Cyanosis, Chest Pain, Sputum Production, Halitosis Respiratory distress identification, management (Box 26.1) Anatomical differences in childhood o Normal 4 mm in diameter o Edema 1 mm significant closer - Respiratory infec3ons - Very common in childhood Infectious agents o Most infections caused by viruses Age o Characteristics of infection often vary by age Size o Anatomic differences Resistance Seasonal variations Clinical manifesta3ons (esp. Box 26.1) - Fevers: o May be absent in neonates (<28 days) o Greatest at ages 6 months to 3 years o Temperature may reach 103° to 105 °F (39.5° to 40.5°C) even with mild infecOons o OQen appears as first sign of infecOon o May leave child listless and irritable or somewhat euphoric and more acOve than normal, temporarily; leads some children to talk with unaccustomed rapidity o Tendency to develop high temperatures with infecOon in certain families o May precipitate febrile seizures (see Chapter 30) - Meningismus: o o o Meningeal signs without infection of the meninges Occurs with abrupt onset of fever Accompanied by • Headache o - Anorexia: o o o - Small nasal passages of infants easily blocked by mucosal swelling and exudation Can interfere with respiration and feeding in infants May contribute to the development of otitis media and sinusitis Nasal Discharge Common feature May be thin and watery (rhinorrhea) or thick and purulent Depends on the type and stage of infection Associated with itching May irritate upper lip and skin surrounding the nose Cough: o o o - Common complaint Sometimes indistinguishable from pain of appendicitis in older child May be caused by mesenteric lymphadenitis May represent referred pain (e.g., chest pain associated with pneumonia) May be related to muscle spasms from vomiting, especially in nervous, tense children Nasal congesOon / rhinorrhea: o o o o o o o o o - Usually mild, transient diarrhea, but may become severe Often accompanies viral respiratory tract infections Abdominal pain: o o o o o - Occurs readily in small children with illness A clue to the onset of infection May precede other signs by several hours Usually short lived but may persist during the illness Is frequent cause of dehydration Diarrhea: o o - Common with most childhood illnesses Frequently the initial evidence of illness Persists to a greater or lesser degree throughout febrile stage of illness; often extends into convalescence VomiOng: o o o o o - • Pain and stiffness in the back and neck • Presence of Kernig and Brudzinski signs Subsides as the temperature drops Common feature May be evident only during the acute phase May persist several months after a disease Respiratory sounds: o Sounds associated with respiratory disease: • Cough o - • Hoarseness • Grunting • Stridor • Wheezing Findings on auscultation: • Wheezing • Crackles • Absence of air movement Sore throat: o o o o Frequent complaint of older children Young children (unable to describe symptoms) may not complain even when highly inflamed Increased drooling noted by parents Refusal by child to take oral fluids or solids Nursing care of child with respiratory tract infec3on (pp. 875 – 877) - Ease respiratory efforts • oxygen supplementation, HUMIDIFICATION- soothe inflamed mucosa, suctioning Promote rest and comfort • hydration, pain relief, fever support Prevent infection spread Reduce body temperature Promote hydration and nutrition Provide family support and teaching Observe for deterioration NO cold remedies should be used in children Acute Viral Nasopharyngi3s (common cold) - - - - Pathophysiology (common causes) o Rhinovirus o Respiratory syncytial virus (RSV) o Adenovirus o Influenza / Parainfluenza Diagnostic evaluation Clinical manifestations o Based on age o Cough is Protective* Therapeutic management o Promote hydration, rest, comfort o Symptom management (e.g., fevers) o Avoid OTC cough suppressants • Limited evidence of effectiveness of OTC cough/cold preps for <6 years old Nursing care management § Evidence of early complications (Box 26.3) Pharyngi3s - - - - - Pathophysiology (common causes) o Group A beta-hemolytic streptococci (GABHS) o Diagnostic evaluation o Diagnosed by rapid swab or culture • 80-90% of cases of acute pharyngitis are viral Clinical manifestations o Sore throat o Cervical lymphadenopathy o Headache o Fever o Abdominal pain o Exudate o Palatal petechiae o Strawberry tongue o Scarlet fever is a sand papery rash o Brief illness varying in severity from asymptomatic to severe o Complications: sinusitis, abscess Therapeutic management o PCN x 10days o Analgesics o Antipyretics o Saline gargles Nursing care management o Carriers may have +culture in setting of another virus, rarely need therapy; minimal transmission to others o Tonsilli3s - InflammaOon of the tonsils - TonsilliOs oQen occurs with pharyngiOs - ManifestaOons o Edema, enlargement of the tonsils o Sore throat o Difficulty swallowing and breathing o Tender lymph nodes o May be viral or bacterial in eOology - Treatments include anObioOcs for GABHS, analgesia, surgery in some cases Tonsillectomy and adenoidectomy (Post-op care) - Assessment o Inspect secreOons and emesis o S/S of bleeding (tachycardia, pallor, bright red blood in emesis, frequent swallowing or throat clearing) o S&S of respiratory distress (agitaOon, stridor, drooling) - Intervention o o o o o o Abdomen/side lying unOl fully awake Avoid/limit sucOon Discourage coughing/clearing throat/blowing nose Ice collar Administer: analgesics, anOemeOcs SucOon & O2 at bedside o Restart clears when awake, not bleeding § SoQ diet § Avoid red foods, straws, cream based unOl toleraOng clears - Discharge Teaching o ***Bleeding risk 5-10 days post-op o Proper fluid and foods o Rest o Nothing in the mouth, straws etc. o Pain control Influenza - - - - Pathophysiology o Influenza (flu) is a contagious respiratory illness spread by droplets and contact o Two main types of influenza viruses: A & B o Influenza type C: asymptomatic or mild respiratory illness o Antigenic shift/drift Diagnostic evaluation o Diagnosed by nasal swab Clinical manifestations (compared to cold, COVID, allergies) o Range of severity from asymptomatic to severe disease o Sudden onset o Complications in children Young children are at higher risk for developing serious flu related complications, Children <5years, Especially infants and toddlers (<2years old) o Pneumonia (often hemorrhagic) o Febrile seizures o Exacerbation of known health conditions like heart disease or asthma o Encephalopathy / Encephalitis o Secondary bacterial infections (OM, myocarditis, sinusitis) Therapeutic management o Treatment depends on age and severity o Rest, hydration, ease symptoms o Antipyretics o Analgesics o Antiviral medication o Oseltamivir (>2wks old) most effective when given within 48 hours of symptom onset o 5-day course o Ibuprofen more helpful d/t muscle aches o Oseltamivir – for infants and children o Yearly vaccine reduce risk Nursing care management (Important considerations) o Special care is needed to prevent flu infections in infants ≤6 months o Avoid contact (including feeding) with anyone with flu or flu-like symptoms o If exposure occurs, notify provider o Breastfeeding considerations: o Mother is not infected – direct breastfeeding encouraged o o Mother is infected – pumping, bottle-feeding by healthy caregiver is ok No flu vaccine under 6 months Ear infec3ons The most common trigger of ear infecOons in children is an upper respiratory infecOon such as a cold, the flu, or strep throat In infants and children, the eustachian tube is prone to becoming obstructed due to swelling and inflammaOon that accompanies URIs and other respiratory condiOons (like allergies) à poor venOlaOon of middle ear à moist, warm environment à infecOon Middle Ear infec3on (O33s Media) - Pathophysiology o Otitis media is the presence of fluid within the middle ear along with s/s of middle ear inflammation o Often preceded by viral respiratory illness o Acute otitis media (AOM) vs. otitis media with effusion (OME) - § AOM is fluid in middle ear with presenting signs and symptoms of illness § OME is middle ear fluid without signs of acute infection Risk factors AOM o Young age o Genetic or familial history of AOM o Craniofacial anomalies (e.g., cleft lip, palate) o Poor access to primary healthcare o Low socioeconomic status o Exposure to tobacco smoke o Having older siblings o Day-care attendance o Use of a pacifier o Protective factor: breastmilk fed - Diagnostic evaluation Clinical manifestations o Acute otitis media § Preceded by upper respiratory infection § Otalgia (earache) § ± Fever § ± Otorrhea (purulent discharge) o Chronic otitis media § Hearing loss § Difficulty communicating § Fullness sensation, tinnitus, or vertigo - Therapeutic management o Guidelines emphasize need for accurate diagnosis, pain management, and watchful waiting in children with non-severe AOM, i.e. delayed prescription for those >6mos with mild/mod unilateral OM o Exceptions include: § Infants <6 months old § Infants 6 months and older with drainage, fever >39, pain for >48 hours, mod/severe ear pain § Bilateral AOM in child 6-23 months old o Amoxicillin 80-90mg/kg/day divided twice daily for up to 10 days § Children 2 years and older: 5 to 7 days § Children <2 years and high-risk comorbidities: 10 days o Supportive care and symptom management includes: § Fever reduction § Pain management (may include benzocaine ear drops) § Decongestants/antihistamines NOT recommended o Other interventions include external application of heat or cold, promote rest and hydration - - Complications o Hearing loss § Speech, language, cognitive development impairment o Tympanic membrane perforation o Chronic suppurative otitis media o Cholesteatoma o Tympanosclerosis o Mastoiditis o Labyrinthitis o Facial paralysis Nursing care management § Medical vs surgical o Myringotomy – surgical incision of the eardrum to alleviate severe pain, and drainage of fluid built up in middle ear o Tympanostomy tube placement (oQen with adenoidectomy) § Pressure-equalizing tubes facilitate drainage from middle ear & promote venOlaOon Outer ear infec3ons (O3s Externa) - - - Pathophysiology o Infection of the external ear canal most commonly caused by Pseudomonas aeruginosa, Staphylococcus epidermidis or Staphylococcus aureus o External ear canal becomes inflamed, irritated, and macerated when exposed during swimming or increased environmental humidity o More frequently occurring in 5- to 14-year-olds, esp. in the summer § Risk factors Diagnostic evaluation Clinical manifestations o Ear pain with manipulation of the pinna (esp. pressure on the tragus) o Pain out of proportion with degree of inflammation o Conductive hearing loss may be present o Itching o Edema o Erythema o Cheesy green-blue-gray discharge o Tenderness o Fever o Pain can progress to jaw, ear Treatment o o o Relieve symptoms, restore normal flora, cerumen, tissue External ear canal cleaning Otic medications used to treat infection - § Antibiotics and steroids o Sterile gauze wick inserted if edema present to help facilitate ear drops to penetrate deep enough into external ear canal Prevention and Education o Use well-fitting ear plugs while swimming o Thoroughly drying ears after swimming o Consider ear drop solution with 1-part white vinegar to 1-part isopropyl alcohol (only if tympanic membrane is intact) o Avoid temptation to itch or pick affected ear with cotton swab or other objects which can lead to further damage Croup syndromes (Table 26.4) - Croup is a general term applied to a cluster of symptoms characterized by: o Hoarseness o Resonant cough (“barky” “brassy” “croupy”) o Inspiratory stridor (varying degrees) o Respiratory distress (varying degrees) o Swelling or obstrucOon in larynx and subglois of upper airway - Most cases are caused by viruses Acute epigloQ3s Medical emergency Serious obstructive inflammatory process Most common in children 2- to 5-years-old Historically caused by H. influenzae § Incidence has declined due to availability of Hib conjugate vaccine § Now often caused by viruses Clinical Manifestations o Abrupt onset, rapidly progressive o Asymptomatic at bedtime, then… o Awakened with painful swallowing, sore throat, absent URI symptoms o Febrile, appears suddenly very sick o Tripod positioning o Drooling o Irritable, restless, anxious/apprehensive, frightened o “Froglike” croaking on inspiration o May lead to complete airway obstruction rapidly o Child does not sound hoarse (unlike with LTB) o Suprasternal and substernal retractions may be visible o Better air exchange achieved with slow, quiet breaths o Mild hypoxia will progress to cyanosis without immediate treatment o Throat appears red, inflamed o Epiglottis appears enlarged, cherry red, and swollen Predictive Signs of Epiglottitis o o o o - - - - o Absence of spontaneous cough o Presence of drooling o Agitation Key Assessment Considerations o When epiglottitis is suspected, throat inspection should be performed only when immediate endotracheal intubation or an emergency tracheotomy can be performed if needed. o Don’t do anything that upsets them o Separate from parents o IV placement o Look in the mouth o Lie them flat o Cry** Therapeutic Management o o o o o Priority intervention o Protect or re-establish airway o Deliver supplemental oxygen Diagnostic evaluation to determine underlying cause (e.g., throat culture, once airway secured) Administer antibiotics Administer supportive medications (e.g., corticosteroids) and IV fluids Prevention with routine immunizations; HiB Laryngotracheobronchi3s - Pathophysiology o Caused by viral infection (esp. parainfluenza viruses, adenoviruses, RSV) and sometimes bacteria (esp. M. pneumoniae) o Most common croup syndrome o Common age 6 mos-3 yrs; rare after age 6 yrs o o - Usually preceded by an upper airway infection, which descends to adjacent structures Inflammation of mucosal lining of larynx and trachea...leads to narrowing airway Diagnostic evaluation Clinical manifestations o Gradual onset of low-grade fever o “Barky” “Brassy” “Croupy” cough (see video #2) o Inspiratory stridor o Suprasternal retractions o Hoarseness o Worse at night and with agitation/crying o Respiratory distress symptoms: o Nasal flaring, intercostal retractions, tachypnea, continuous stridor o Progresses to obstruction, impaired ventilation and respiratory failure - • Warning signs Therapeutic management Cool mist humidified air – no evidence Not indicated: Anti-tussive or decongestant · Antibiotics D/C no stridor at rest - Nursing care management Bronchi3s - esp. respiratory syncy3al virus - - Pathophysiology o Inflammation of the large airways (trachea and bronchi) o Frequently associated with URIs o Most commonly caused by viruses § Flu, parainfluenza, coronavirus, rhinovirus, RSV, human metapneumovirus § Bacterial causes include pertussis, M. pnuemoniae, Chlamydia pneumoniae Diagnostic evaluation Clinical manifestations (Box 26.6) o Usually mild, self-limiting symptoms o Cough § Dry § Hacking § Nonproductive § Worsened at night § Lasting > 5 days § May persistent for 1 to 3 weeks - Therapeutic management o Symptom management § Analgesics § Antipyretics § Humidified air § No other medications are effective o Consider evaluating teens for vaping, marijuana - Nursing care management § Oxygen delivery devices Bronchioli3s - Pathophysiology o Acute viral infection mostly caused by respiratory syncytial virus (RSV) o Also, adenovirus, parainfluenza, human metapneumovirus o Occurs less frequently in breastfed infants, more frequently in crowded conditions o o o o - Most common cause of hospitalization in children < 2 yrs Severe RSV in first year sig risk factor for asthma Spread via direct contact with respiratory droplets Peak incidence younger than 3 mos Disease process o Disease progression leads to inflammation of epithelial lining the small airways (bronchioles) causing... § ↑ Mucus production § ↑ Inflammation § ↑ Cellular necrosis RSV - Hospitalization o Children younger than 6 months of age with RSV infection may need to be hospitalized o Likely admission <1 mos o Poor feeding, lethargy, dehydration, moderate to severe distress, apnea, cyanosis o Underlying conditions - o o Lung or heart disease o Prematurity Hospital Management o Oxygen (often high flow nasal cannula) o Frequent oral, nasal, nasopharyngeal suction o Noninvasive positive pressure ventilation (e.g. CPAP, BiPAP) o Intubation and mechanical ventilation o Nasogastric feeds or o IV fluid / NPO o AAP does not recommend use of nebulizers (Albuterol, Racemic Epi) or steroids Home Treatment Most RSV infections are self-limiting and can be managed at home o Manage fever and discomfort o Maintain hydration o Watch for respiratory distress SARS-COV-2/COVID-19/MISC o Clinical manifestaOons similar to other viruses, i.e. flu o Fever, sore throat, muscle aches, GI upset, headache, malaise o Also loss of taste/smell, progression to dyspnea o Severe cases include coagulopathy, cardiac impairment, liver or renal disease, increased WBC counts o More likely with preexisOng condiOons, < 1yr, asthma, CLD, oncology, immunosuppression, anemia, low platelets, CV disease o TherapeuOc management (hospital-based) o Remdesivir (MAB therapy) & Dexamethasone o Key is prevenOon: vaccines, hygiene MIS-C (MulOsystem Inflammatory Syndrome in Children) o Hyperinflammatory system occurring 2-4 weeks post COVID-19 infecOon o Clinical manifestaOons o Fever plus…any of the following: o Abd, chest, or neck pain; V/D; injected conjuncOva, redness or swelling of lips, tongue - Therapeutic Management o Vasoactive medications (50%) o Oxygen/ventilation support (20%) o Anticoagulation agents o Steroids o Immunoglobulin o Immunosuppressants o Antibiotics Pneumonia - Pathophysiology o Viral (most common) o COVID-19, flu, adenovirus, parainfluenza o Bacterial o S. pnuemoniae, M. catarrhalis o Atypical o Aspiration (stay tuned) o Occurs more frequently in infancy and early childhood o Different pathogens based on age o May be primary or secondary illness - - Diagnostic evaluation o Covid Test, Nasal Swab Clinical manifestations (Box 26.8) Therapeutic management o Viral pneumonia is self-limiting, symptom management o Oxygen, analgesics, antipyretics, monitoring fluid intake o Bacterial pneumonia is treated with antibiotics and symptom management o High dose amoxicillin or 2nd/3rd generation cephalosporin o Atypical pneumonia is treated is with antibiotics and symptom management - o Azithromycin, erythromycin § Complications: Pleural effusions, Emphysema, Pneumothorax, and AOM Nursing care management o Symptom Management Pertussis (whooping cough) - - - - - Pathophysiology o Acute respiratory tract infection caused by Bordatella pertussis o Primarily in children <4 years old who are not immunized o Highly contagious o Highest morbidity, mortality for young infants Diagnostic evaluation Clinical manifestations o Classic whoop o Apnea (young infants) o Cough o Coryza (rhinitis - inflammation of mucosal lining of nose) o Sneezing Therapeutic management o Antibiotics o Supportive care o Complications include encephalopathy, seizures, pneumonia, hypoxia, rib fractures, bleeding into conjunctiva, hernia o Death risk higher for infants (particularly unimmunized) Nursing care management Non-infec3ous respiratory dysfunc3on - Aspiration - esp. foreign body Pathophysiology o Two common types of aspiration in children: o Foreign body aspiration o Aspiration pneumonia Foreign Body Aspira3on o o o o o o o 80% of FBA occurs in children younger than 3 years o Peak age: 1-2 years Majority of FBA are lodged in bronchi Larynx and trachea less common, higher morbidity and mortality S/S depend on site of obstruction and time elapsed Almost 50% of children will be asymptomatic Able to stand, explore world via oral route, have fine motor skills to put objects in mouth, do not yet have molars to chew adequately Small airway diameter prone to obstruction Laryngotracheal ObstrucOon o o o o o Dyspnea Cough Stridor Hoarseness Cyanosis Bronchial ObstrucOon o o o o o Cough (frequently paroxysmal) Wheezing Asymmetrical breath sounds Decreased air entry Dyspnea - Diagnostic evaluation o Witnessed or reported event o Onset of coughing o Unilateral wheezing or decreased aeration o FB aspiration in mainstem or lower bronchi o Witnessed event using choking or gagging o Complete obstruction of trachea or larynx can occur from mechanical blockage or induced laryngospasm o History of choking, when asked specifically, found in 80-90% of confirmed choking cases o Clinical Pearls o Many aspiration events are unwitnessed o Consider FBA in any infant/toddler with acute onset respiratory distress o Safest removal is in the OR with appropriate personnel & resources o Reflexive coughing is likely the most successful mechanism to clear FB o Minimize interventions Therapeutic management Nursing care management - - Aspira3on pneumonia o An inflammaOon of the lungs due to aspiraOon of a foreign substance such as food, liquid, vomit, or mucus o Clinical manifestaOons include o Increased cough or fever with foul-smelling sputum o Other signs of lower airway involvement o Treatment o AnObioOcs o Resp support Conditions that increase risk ARDS, or Acute Respiratory Distress Syndrome, is an inflammatory lung condiOon involving both lungs that may complicate severe pneumonia (including influenza), trauma, sepsis, aspiraOon of gastric contents, and many other condiOons. InflammaOon leads to injury of lung Ossue and leakage of blood and plasma into the airspaces resulOng in low oxygen levels in the blood. Mechanical venOlaOon is required both to deliver higher concentraOons of oxygen to and provide venOlaOon to remove carbon dioxide from the body. InflammaOon in the lung may lead to inflammaOon elsewhere causing shock and injury or dysfuncOon in the kidneys, heart, and muscles. There is no proven drug treatment for ARDS per se. Current management of ARDS begins with treatment and stabilizaOon of the underlying disease that caused ARDS, such as early and effecOve anObioOcs for pneumonia or sepsis. The injured lung should be managed gently with small breaths and low pressures from the venOlator (so called low Odal volume and pressure venOlaOon). In addiOon, conservaOve use of intravenous fluids combined with removal of excess fluids with diureOcs lessens the need for mechanical venOlaOon. With these supporOve measures, the lung may heal quickly and the paOent can return to normal breathing in days; in severe cases ARDS may enter a prolonged phase of healing that may require weeks to resolve. In even more severe cases, devastaOng lung injury cannot support life or other organs fail along with the lung (a condiOon known as mulOple organ failure). Death may occur in up to 40 percent of cases in this severe form. Congenital Diaphragma3c Hernia - - - Pathophysiology o Diaphragm does not form completely, resulting in an opening between the thorax and the abdominal cavity o Lung hypoplasia (underdevelopment) occurs on affected side o Ventilation compromised by hypoplasia and compression; pulmonary hypertension o High mortality o Prenatally diagnosed with appropriate prenatal care; otherwise, severe resp distress at birth with scaphoid abdomen Diagnostic evaluation Clinical manifestations Therapeutic management (big picture items) o Fetal surgery o Post birth o Immediate intubation o Gastric decompression o Transfer to ECMO center o Surgery o Long term complications o Chronic lung disease, gastroesophageal reflux, feeding problems, recurrent diaphragmatic herniation, intestinal obstruction, pneumonia, FTT, hearing loss, scoliosis, and impaired motor and cognitive function o Nursing care management Asthma - Pathophysiology o Inflammation in response to a trigger o Airway edema and accumulation of mucus o Smooth muscle spasm of the bronchi and bronchioles o Airway remodeling leading to permanent changes Airway impact o o Airway lumen is narrowed, so expiration is forced Air trapping occurs o o o o o o § Results in fatigue, poor ventilation, and poor oxygenation Chronic inflammatory disorder o Recurrent wheezing, breathlessness, chest tightness, and cough Most have first symptoms before 4-5 years of age Most common chronic disease of childhoods, primary cause of school absences, 3rd leading cause of hospitalizations SES, geography, pollution, prematurity, limited access to health care, under diagnosis, under treatment all increased risk, morbidity, and mortality Ask about time of onset/exacerbation, potential causes, triggers, severity of symptoms, response to treatments at home, all current medications, last doses, Triggers (Box 26.16) - Diagnostic evaluation o Symptoms are critical part of asthma diagnosis (Classification Box 26.15) o Pulmonary function tests (PFTs) o Children need to follow instructions o Conduct at initial diagnosis, when treatment is started, when stable on treatment, and then every 1-2 years o Peak expiratory flow rates (PEFR; p. 923) o Maximum forced expiration o Allergen testing o CXR not routinely indicated - Clinical manifestations o May be associated with URI symptoms o Cough: hacking, paroxysmal, may be productive, can be chronic Dyspnea, SOB, prolonged expiration, cyanosis, restless, nervousness, sweating, panting o Wheezing, hyperresonance, coarse breath sounds, crackles o Positioning to maintain a patent airway (tripod, on next slide) Therapeutic management o Anti-inflammatory o Can be given IV, enterally, and inhalation o Onset varies depending on route o Used in children > 5 y/o o Can lead to improved asthma symptoms o S/E o Cough, dysphonia, and oral thrush o Growth needs to be monitored o Ex. budesonide and fluticasone o - o o Long term: Inhaled steroids, long acting β2 agonists, and leukotriene modifiers Short acting: β2 agonists, anticholinergics, systemic corticosteroids B2 Adrenergic Agonists o o o o Allows smooth muscles to relax by reducing availability of calcium Eliminate bronchospasms S/E: tachycardia, GI disturbances, irritability, tremors, nervousness, and insomnia Ex. Albuterol, levalbuterol, terbutaline Other MedicaOons § - o Long-acting beta agonists (single and combo products with steroids) o Leukotrienes o Anticholinergics o Monoclonal antibodies Asthma exacerbation emergency management Nursing care management Status asthmaticus o Goal is to improve ventilation and oxygenation o Decrease airway resistance, relieve bronchospasm, correct dehydration and acidosis, relieve anxiety o Treatment o Humidified O2 o Medication § Inhaled short acting β agonist: initially q20-30 min or continuous § Systemic corticosteroid § Ipratropium bromide § IV fluids o Other medications o o o IV magnesium Inhaled heliox Ketamine: smooth muscle relaxant Cys3c fibrosis - Pathophysiology (Fig 26.15) o Exocrine gland dysfunction that produces multisystem involvement o Pulmonary sequelae o Digestive sequelae o Autosomal recessive trait - Diagnostic evaluation o At least one of the typical features of CF: chronic sinusitis, GI and nutritional abnormalities, salt-loss syndromes, obstructive azoospermia o Sibling with CF o Positive newborn screening o Plus at least one of the following: o Elevated sweat chloride o o - - Two known CFTR gene mutations on separate alleles Abnormal testing for nasal epithelial ion transport Clinical manifestations o Progressive chronic obstructive lung disease associated with infection o Initial wheezing, dry, non-productive cough o Maldigestion from exocrine pancreatic insufficiency o Initial meconium ileus o Growth failure from malabsorption and anorexia o Diabetes symptoms of hyperglycemia, polyuria, glycosuria, and weight loss from pancreatic insufficiency o Salty kiss - Therapeutic management Pulmonary o Typical findings could be absent o Fever o Tachypnea o Chest pain o Eval for anorexia, weight loss, and decreased activity o Send respiratory culture and other appropriate studies o Use of inhaled antibiotics (Tobramycin) o Secretions are very viscous and thick, o Dornase thins secretions o 7% hydrate and thin sections o Streaking incr pulm infection or advanced lung disease o Hemoptysis – greater than 250mL/24 hr is life threatening Management of Pulmonary InfecOons o o o o - Typical findings could be absent o Fever o Tachypnea o Chest pain Eval for anorexia, weight loss, and decreased activity Send respiratory culture and other appropriate studies Use of inhaled antibiotics (Tobramycin) GI o o Replace pancreatic enzymes o Administer with meals and snacks, or within 30 min § Varying dose, depending on child’s response and meal (less capsules for a snack, for example) § If dosage of pancreatic enzymes is correct, the patient’s stools should not float Well balanced, high protein, high calorie diet for growth o o - Reflux management Constipation/rectal prolapse o MiraLAX o Other laxatives, stool softeners, rectal gastrografin Endocrine o o o Unstable glucose homeostasis, insulin deficiency, insulin resistance o Will discuss these issues more generally in the Endocrine lecture 95% chance of reproductive issues Osteoporosis and osteopenia o Chronic steroids and pancreatic insufficiency lead to poor bone growth o Need monitoring of bone mass density o Nutrition optimization, exercise, bisphosphonates Chapter 19 – Children with Special Needs - Scope of the problem - Considerations o Care in the home o Supplies, backup plans o Subspecialist involvement o PT, OT, speech therapy, skilled nursing, etc o School o Social/emotional growth o Impact on family o Caregiver stress o Siblings Family-centered care o o o o o o Importance of the family as the “consistent” unit Parents become the expert à form partnerships with healthcare team Family-Health Care Provider Communication Establishing Therapeutic Relationships Shared Decision Making Normalization - Communication Shared decision making (Box 19.1) Normalization Impact (Box 19.3) - Family, siblings Times of crisis o o o o o Diagnosis of the condition Exacerbations of the condition Developmental milestones/recognizing limitations Start of school Death of child Pallia3ve care in childhood - Ethical dilemmas o Pain control o Chemotherapy/experimental therapies o Supplemental nutrition/hydration o Resuscitation o Autopsy Chapter 10 – Infant Health Promo3on Biologic development in infancy (Table 10.3) - - - Proportional changes (e.g., weight, height, head circumference) Sensory changes o Visual acuity improves o Binocular vision established o Depth perception develops 7-9 months o Visual preference for human face Maturation of systems o Respiratory – rate slows, abd breathing, short trachea-lung distance, short straight eustachian tubes o CV- rate slow, increased BP o Hematopoietic- transition from fetal Hb to adult Hb, 6 mos physiologic anemia (nadir), maternal iron stores deplete o GI- immature processes, stomach grow, amylase/lipase limited early on for fat absorption, solids may be incompletely digested o Immunologic– higher risk for infection due to low Ig, breastmilk helps in IgA o Thermoregulation- becomes more efficient, vernix plays role in thermoregulation and immune properties (protects skin/barrier), capillaries learn to respond to changes in temperature o Renal- 78% term infants body is water, decreases over time, void frequently and dilute urine o Sensory- every sense is present at birth, auditory is most advanced and adult levels at birth, vision least mature, binocular vision and depth perception take time to develop o Gross motor milestones o Head lag in first 2 months o Head control at 4 months o Rolling over (from abdomen to back) at 5 to 6 month o o o o o o o o - Parachute reflex by 7 months (Parachute reflex – arms out in anticipation of falling) Sit alone by 7 months Move from prone to sitting position by 10 months Movement and Activity Cephalocaudal direction of development Increased coordination of extremities at 4 months Crawling at 6 to 7 months (usually backward) Walk with assistance at 11 months Walk alone at 12 months Fine motor milestones o From palmar to pincer grasp o Grasping object at 2 to 3 months o Palmar grasp at 6 months o Transfer object between hands at 7 months o Pincer grasp at 10 months o Remove objects from container at 11 months o Build tower of two blocks at 12 months Psychosocial development (Erikson) - Trust vs mistrust o Infants learn basic trust if the world is a secure place where their basic needs are met. Cogni3ve development (Piaget) - Sensorimotor phase o Piaget's term for the way infants think—by using their senses and motor skills—during the first period of cognitive development. Stage One o Reflexes- suck to drink from a bottle (Birth to 1 month) o Stage Two (1 to 4 months) – Primary circular reactions – replaced reflexes with voluntary behavior o Stage of first habits- suck in some ways for hunger, others for comfort o Stage Three (4 to 8 months)– primary circular actions become prolonged o Responding to people and objects- clapping when mom says patty-cake o Stage Four(8 to 12 months)- Means to the end; more attuned to goals of others; increased social understanding-putting mom’s hands together to get her to play patty cake, waving bye bye, o Object permanence o o o o o Stage Five - toddler Little scientists; trial and error- putting teddy in toilet and flushing. No hesitation Stage Six - toddler Mental combination use; intellectual experimentation via imagination; deferred imitation Hesitation before acting o Remembering mom’s reaction to teddy flushed in toilet Social development - - Attachment o The connection between one person and another, measured by how they respond to one another Attachment – 2 components required – ability to discriminate mother from others and object permanence o Begins to form in early infancy and influences a person's close relationships throughout life. o Remember trust vs. mistrust Secure attachment (Type B) o An infant obtains both comfort and confidence from the presence of his or her caregiver. (~ 50-70% toddlers o Disorders – result from abuse/ neglect …develop lack of warmth, do not response to comfort, lack of emotional regulation Separation anxiety, stranger fear o Separation anxiety – 4-8 months o Stranger – 6-8 months Language development o o o o o o o Crying is the first verbal communication Vocalizations by 6 weeks Coo, gurgle, laugh aloud at 3 to 4 months Imitate sounds and add consonants at 8 months Comprehend “No”; follow commands at 9 to 10 months Ascribe meaning to a word at 10 to 11 months Three to five words with meaning by age 1 year Temperament dimensions o o o Effortful control (regulating attention and emotion, self-soothing) Negative mood (fearful, angry, unhappy) Exuberant (active, social, not shy) Coping with common concerns of infant growth / development - Separation/stranger fear Limits/discipline Childcare Teething o Pacifier use – no absolute certainty – sids, nipple confusion, incr OM, Promo3ng op3mal health during infancy - Nutrition o First 6 months o o o o o Human milk is first choice o No need for additional fluids in the first 4 months o Daily supplements (vitamin D, iron) Second 6 months o Selection and preparation of solid foods o Introduction of solid foods, progression § intervals of 4 to 7 days to allow for identification of food allergies o May need fluoride supplements o NO honey in the first year of life Weaning o Weaning from breast or bottle to cup after 1 year Dental health Introduction of Solids o Rice or oatmeal cereal starting at 4-6 mo (iron) o Then move to vegetables & fruit (roughly at 6-8 mo, depending on baby and family) o One new food every few days o If no known allergy or high risk for allergy, introduce peanuts, eggs in the 4-6 months range o Meat, fish, poultry: start at 8-10 months o NO honey before 12 mo (botulism) Weaning from breast or bottle à easiest if child decides; substitute one bottle or sippy cup at a time for a feeding, gradually increase Sleeping patterns o Sleep duration changes o Total daily sleep: 16-18 hours (newborn); 15 hours (2 mos); 13 hours (6-12 mos) o Nocturnal pattern of 9 to 11 hours by 3 to 4 months o As nighttime sleep increases, daytime sleep decreases o Sleeping through the night Usually between 3-4 months o Back to Sleep campaign o Sleep problems o Sleeping arrangements o Anticipatory Guidance: o Sleeping habits may change/become disrupted during attachment/separation anxiety phase o Sleep training: routine is important! o - Safety and injury preven3on - Family-Centered Care Box Child Safety Home Checklist o Suffocation o Aspiration, asphyxia, animal bites o Falls o Electrical & other burns o Poisoning and Ingestions o o Automobile Safety Drowning Chapter 11 – Common Health Problems of Infancy Health problems related to nutriOon - - - Nutritional imbalance o Vitamin imbalances Vit D- exclusively breastfed, for longer than 6 mos, poor diets without milk products o Specific d/o or diets- fat soluble vitamins A & D o Iron Calcium o Mineral imbalances o Protein- energy malnutrition o Kwashiorkor- protein deficiency o Marasmus- calorie deficiency o Nursing care management- education, immunizations, well visits, appropriate nutrition per age Food sensitivity o Immunoglobulin E (IgE)–mediated immune response (e.g., cow’s milk allergy) o Food intolerance o Non- IGE- mediated immune response (E.G, Lactose intolerance) o Diagnosis and therapeutic management o Nursing care management - advising for breastfeeding, do not delay highly allergic food introduction, safety in day care (then school), what to do when allergic rxn o Mgmt- Avoiding offender, sensitization therapy Failure to thrive (FTT) o Deceleration of growth in both height and weight o < 5th%tile weight o Z-score -2 o Crosses 2+ growth curve lines (down) o Multifactorial, Dianosis of exclusion o Classifications- Previous classification of organic or nonorganic may be too simple because most cases of FTT are complex and have mixed causes. o Inadequate caloric intake – incorrect formula prep, neglect, lack o Inadequate absorption – CF, celiac, crohns, allergy o Increased metabolism – hyperthyroid, heart disease o Defective utilization – various genetic anomalies, metabolic storage dx o Dx- diet hx, labs, o Reverse cause, diets , medication o Diagnostic evaluation o Diagnostics focus on ruling out underlying causes (history, labs, environmental & dietary assessments) o Therapeutic management o Treatment involves treating underlying cause plus: o High caloric density feedings o Vitamin & mineral supplements o o Family intervention if indicated Chronic Disease o Cardiac § Cardiac Failure o Neoplasia o Pulmonary § Bronchopulmonary Dysplasia § Cystic Fibrosis o Renal § Renal Failure § Renal Tubular Acidosis o Rheumatology § Systemic Lupus Erythematosus o Congenital/Genetic/Neurological Disease § Cerebral Palsy § Craniofacial Abnormalities § Fetal Alcohol Syndrome § Intrauterine Growth Retardation § Mental Retardation § Myopathies § Neurocutaneous Syndromes • Neurofibromatosis § Prematurity § Primary CNS abnormality § Genetic Syndromes • Cystic Fibrosis • Russell-Silver Syndrome • Williams Syndrome § Muscle weakness • Prader Willi Syndrome § Inborn Error of Metabolism o Endocrinological Disease § Diabetes Mellitus § Hypopituitarism § Hyperthyroidism § Growth hormone Deficiency o Gastrointestinal Disease § Celiac Disease § Chronic Diarrhea § Chronic Emesis § Esophagitis § Gastrointestinal Reflux § Inflammatory Bowel Disease § Malabsorption o o o o o o o o o § Protein Losing Enteropathies Infectious Disease § Congenital infections § HIV/AIDS § Recurrent infections § Parasites § Tuberculosis Immunological/Rheumagological Disease § Immunodeficiencies Other § Anemia § Heavy Metals • Lead • Drugs o Amphetamine o Cocaine o Hydantoin o Phenobarbital § Dental Caries Nutritional Problems § Inadequate Calories § Inadequate Protein § Poor Appetite § Maternal Malnutrition Psychiatric Problems § Depression § Eating Disorders in Patient or Mother § Munchausen’s Disease by Proxy § Psychosis Social Problems § Child Abuse § Caregiver/Child Interaction Abnormalities • Emotional Deprivation • Difficult Child § Family Stress § Parenting, Ineffective § Poverty Nursing Care Management: Assessment & observation: anthropometrics, 3-5 day food record, family interactions, mealtime behaviors, signs of disordered eating Planning & Intervention: Provide accepting, caring, positive environment; provide continuity of care for establishment of trust & rapport; actively feed child; referral to social work and/or counseling o Colic o o o o o - - Reassessment & discharge: continued anthropometrics, signs of improved behavior, education on feeding child Excessive crying (rule of 3s) thought to be caused by abdominal pain in infants o Most common in infants <3 mo, no other consistent risk factors but many proposed o <5% have identified organic cause o Self-limiting, usually resolves by 12-16 wks Rule out potential causes Most management = supportive Feeding too rapidly, excessive air, improper feeding technique, emotion distress Determining feeding characteristics, breast milk – mother’s diet Nursing Assessment o Circumstances of crying § Onset, location, duration, characteristics, aggravating factors, relieving factors, treatment o Family situation: who’s around, how they respond Nursing Intervention: o Parental reassurance – not doing anything wrong, very unlikely child will experience negative long-term outcomes o Parental education – changing positions, rocking swing, massaging, soothing sounds, pacifier for sucking, swaddling, trial off foods or cows milk products, air-minimizing bottles Sleep problems o o o Nighttime feeding Developmental night crying o Awaken abruptly newly Trained night crying (inappropriate sleep association) o Falling asleep outside of own bed Sudden Infant Death Syndrome (SIDS) o o o o o o o o o Death during sleep unexplained after postmortem exam and history taking Likely multifactorial, environmental & genetic risk #1 cause of death among infants 1-12 months #1 Goal: Prevention Back-to-Sleep (or Safe-to-Sleep) campaign, 1994 Genetic predisposition new research area Brainstem abnormalities and cardio resp control, Infant Risk Factors SIDS Male, African American, American Indian, Preterm labor (LBW), Low APGARs, Sibling of SIDS victim Risk factors Maternal Smoking, Co-sleeping, Prone sleeping, Soft bedding, Substance use, Recent illness, Prolonged QT Protective Factors o Sleeping in supine, Flat, alone space, breastfeeding, Pacifier use, Up-to date Immunizations Brief Resolved Unexplained Event (BRUE) o o o o o o Infant exhibits a combination of: o Apnea, irregular respirations o Change in color or muscle tone, mental status o Choking, gagging, or coughing o Usually involves significant intervention Diagnostic evaluation o Assess for underlying cause (GERD, arrhythmia, seizure disorder, sepsis, other infections) o History o Monitoring o Infection evaluation, chemistries o +/- EKG, chest xray, cranial imaging o Further evaluation depending on signs/symptoms Therapeutic management Educate regarding evaluation Provide emotional support to the parents (fear, anxiety, uncertainty, frustration, depression) Discharge teaching: o CPR o At-home apnea monitors: not routinely used Skin disorders o o o - - Common conditions: o Diaper dermatitis o Atopic dermatitis (eczema) o Seborrheic dermatitis o Urticaria (HIVES) Clinical manifestations Nursing care management Diaper dermatitis treatment o Basic Irritant: o Keep skin dry/change diaper as soon as wet o Leave open to air if possible o Use barrier cream (zinc oxide, petrolatum) 2-4 times a day § Clean and dry skin prior to application o Do not use diaper wipes on open areas o Avoid over-washing § Soft cloth, warm water, gentle non-soap cleanser o Candidiasis: o Nystatin diaper cream - topical 3-4 times/day Atopic dermatitis (eczema) o Usually in the context of fam hx eczema, asthma, allergies, allergic rhinitis o Major treatment goals: o o o o o o o o o Rehydrate o Relieve itching o Prevent/treat 2° infection Treatments: topical treatment (aquaphoR, hydrolateum, eucerin, cetaphil, corticosteriod) for inflammation, antibiotics for infections, oral antihistamine for itching Therapeutic treatments: Baths, moisture locking lotions, cool compresses Education: Use nondrying soaps Use lotions immediately after bath Keep nails short, don’t scratch Wear soft cotton pajamas, avoid itchy fabrics/stuffed animals Sign of infection (impetigo): Assess for honey colored crusting on top of rash, or red edged pustules – contact provider Administration of medical ointments: appropriate amount, frequency, contact MD if reoccurs/doesn’t resolve Seborrheic DermaOOs Chronic, recurrent inflammatory reaction of skin o Usually of scalp o Thick, yellow, adherent scaly patches o Scalp Hygiene o Shampoo and physical removal Food allergies o Oral Allergy Syndrome: Swelling & itching of lips, tongue, throat o Immediate GI Hypersensitivity: Nausea, cyclic vomiting, diarrhea, abdominal cramping o Cutaneous Symptoms: Hives, red rash, flushing o Anaphylaxis: facial or throat swelling of any kind, uticaria, wheeze or noisy breathing, croupy cough, difficulty swallowing, excessive drool, dizziness o - Intervening on Food Alergies Pharmacological and Medical TesOng o o o o Diphenhydramine, <2yr old only w/ MD supervision Cetirizine, Fexofenadine, Loratadine Epinephrine 0.01mg/kg, max 0.5mg Pin-prick testing, food challenges Non- pharmacological and Nursing IntervenOons o o Education for families & professionals working with kids on recognition, medical intervention, avoidance Advocacy & policy-making for allergy awareness, allergen-free zones, action plans Chapter 12 – Toddler Health Promo3on Biologic development in toddlers (Table 12.2) - Proportional changes Sensory changes - - - o Visual acuity of 20/40 is acceptable o Full binocular vision well developed o Still gaining depth perception o Development of hearing, smell, taste, and touch increases o Uses all senses to explore the environment Maturation of systems o Neuro - All brain cells present, but continue to grow in size, brain 75% of adult size by age 2 yrs, myelination almost complete by age 2 yr o Resp – Volume of resp tract grows; inner ear structures are short and straight, tonsils are large and therefore, upper respiratory tract infections, otitis media, and tonsillitis are common; decr RR, still have abd breathing o CV – decrease in HR, Inc BP o GI – voluntary control of elimination key change in this age group, bladder capacity increases o Immune- defense mechanisms of skin and blood far more efficient, exposure to new pathogens o Thermo- rarely issues in mod temp regulation- capillaries fully functioning Gross motor milestones o Locomotion o Walks by 12-13 months; runs by 18 months o Climbs stairs by 2 yrs o Jump, stand on one foot, tiptoe o Improved coordination between 2 and 3 yrs Fine motor milestones o Has improved manual dexterity at 12 to 15 months o Throws a ball by 18 months o Building growing towers of blocks o Scribble at 15 months o Draws circles by age 3 years Psychosocial development (Erikson) - - Autonomy vs self-shame and doubt o Developing a sense of personal control over physical skills and a sense of independence o If children in this stage are encouraged and supported in their increased independence, they become more confident and secure in their own abilities o If children are criticized, overly controlled, or not given the opportunity to assert themselves, they begin to feel inadequate in their ability to survive, and may then become overly dependent upon others, lack self-esteem, and feel a sense of shame or doubt in their abilities Negativism, ritualism o Negativism: giving negative response to requests o "No" or "me do" o Asserting independence and autonomy o Emotional liability o "Terrible Twos" o Ritualism the need to maintain sameness and reliability o Provides sense of comfort CogniOve development (Piaget) - - Sensorimotor phase (12 – 24 months) o Sensorimotor phases o Tertiary circular reactions at 13 to 18 months (5th stage) § Causal relationships, trial and error; problem solving and operations o Invention of new means through mental combinations at 19 to 24 months (6th stage) § Symbolic thought and imagination; hesitating before acting; spatial relationships; objective permanence o Increasing awareness of others' actions and copy § Imitation gestures and words § Domestic mimicry o Stage Five - toddler o Liple scienOsts; trial and error- puing teddy in toilet and flushing. No hesitaOon o Stage Six - toddler o Mental combinaOon use; intellectual experimentaOon via imaginaOon; deferred imitaOon o HesitaOon before acOng o Remembering mom’s reacOon to teddy flushed in toilet Preoperational – preconceptual phase (2 – 4 years) – Table/Box 12.1 o Preoperational Stage (2-7 yrs) o Divided into two stages § Preconceptual phase at 2 to 4 years § Intuitive thought phase at 4 to 7 years o Children do not use operations (logical reasoning) o Transition between self-satisfying behaviors of infancy and socialized relationships o Increased use of language o Concern with “why” and “how” o Prelogical thinking CharacterisOcs of PreoperaOonal Thought o o o o o o Obstacles to Logic Animism – belief that natural objects and phenomena are alive with sensations and abilities like humans Egocentrism - self-centeredness, contemplating the world from personal perspective Transductive reasoning – applying a connection to unrelated things, not inductive or deductive Global organization -Reasoning that changing any one part of the whole will changes the whole (move bed, won’t sleep in room) Centration -Tendency to focus on one aspect of a situation to the exclusion of all others o Irreversibility - Fail to recognize that reversing a process may restore what existed before; nothing can be undone Social development o o o o o Differentiation of self from mother and from significant others is a major task o Separation o Individuation Increased understanding and awareness of object permanence Some ability to tolerate frustration à diminished stranger fear Some ability to delay gratification Transitional objects provide security Language development o o o o o o Increasing level of comprehension Increasing ability to understand Comprehension of 300 words by age 2 yrs At age 2 yrs, can use two- or three-word phrases At age 3 yrs, can use simple sentences and acquires five to six new words a day Gestures precede each language milestone up to 30 months of age (putting phone to ear; pointing) Personal-social behavior o o o o Play o o o o o o o o Toddler develop skills of independence Sudden mood swings are common Skills of independence may result in tyrannical, strong willed, volatile Behavior Skills include feeding, playing, dressing, and undressing self Parallel play Imitation Little emphasis on gender-stereotyped toys Increased locomotive skills Educational toys and books Tactile play Appropriate safety in relation to size, shape, risk for toxins, and sturdiness of toys AAP- no screen time until 2 yrs; then <1 hr educational programming per day Coping with common concerns of toddlerhood - - - Toilet training – a major task of toddlerhood; 3 markers include: aware of urge, interest/motivation, dry at least 2 hours during day; also fine motor skills to remove clothing, impatience with wet or soiled diapers; daytime dryness occurs long before nighttime Temper tantrums – linked to anger and distress; asserting independence, set clear boundaries and expectations, *consistency and routine and developmentally appropriate expectations and rewards, offering choices Negativism – reduce the opportunity for a no answer - Stress – small amounts beneficial to develop coping strategies, excess is destructive; best approach is prevention Regressive behavior – often response to stress; best approach is to ignore and praise appropriate behavior Sibling rivalry – typically when new baby enters family, jealousy, dethronement PromoOng opOmal health - Nutrition o Growth rate slows, decreasing need for calories, protein, fluid o Physiologic anorexia o Ritualism o Lifetime habits are developed early o Avoid food as reward o MyPlate recommendations (replaced food pyramid) o Transition to whole milk at 1 yr and low-fat milk at 2 yrs o Need for iron, calcium and vit D o Picky, fussy eaters with strong taste preferences o Same dish, same cup, same seat at table Specialized Diets/ AlternaOve Medicine Vegetarian diets increasing in US Adequate vegetarian diet can be achieved Strict (vegan) diets are often inadequate in protein, calories for growth and energy; iron deficiency anemia and rickets o Supplements not always safe for children Sleep/activity o Average sleep of 11 to 12 hours per day o One nap typically distinguishes by age 2 or 3 yrs o Bedtime resistance, nighttime waking o Transition from crib to bed o Activity is very high o Newer concern with decreased activity and increased screen time o o o - Safety and injury prevenOon - Motor vehicle safety (e.g., use of car seats) Accidental ingestions, burns, aspiration, drowning, etc. o Unintentional injuries leading cause of death age 1-4 yrs o MVC deaths are caused by improper car restraints or lack of; children in front seat highest risk for injury o Recs: children up to age 2 in rear facing seat until outgrow seat’s recommendations, then forward facing in back seat – never in bulky jackets or clothing, then booster seats, o Children should be in a car seat until 4’9”, or 8-12 yrs old o Children with disabilities may require specialized restraint system o Also concern for children in open beds of pick ups trucks, left in hot cars, children crawling in trunks and asphyxiating o o o o o o o Drowning: males have higher rate of drowning, infants in buckets and tubs; toddlers in pools, tubs, ponds/lakes, hot tubs Burns: scald burns most common type of thermal injury, water heaters should be adjusted, sunburns, keeping things out of reach, covers on electric sockets Poisoning: toddlers highest risk, innate curiosity; major reason is improper storage Falls: most non lethal injuries, from stairs, jungle gyms Aspiration: new foods, toys Bodily harm (ped vs car, bites, knives, scissors, firearms) Anticipatory guidance AnOcipatory guidance for family of toddler - Family-Centered Care Box – Guidance During Toddler Years (p. 422) Chapter 13 – Preschooler Health Promo3on Biologic development of preschool-age children (Table 13.1) - - - Proportional changes o Physical growth slows and stabilizes o Average weight gain remains about 5 lbs/yr o Average height increases 2½ to 3 in/yr o Physical proportions slender and sturdy o Body systems mature and stabilize; can adjust to moderate stress and change Gross motor milestones o Gross motor skills should be well-established o Walking o Running o Climbing o Jumping, skipping o Ride tricycle o Balance o Catch ball Fine motor milestones o Fine motor skills include refinement in eye–hand and muscle coordination o Drawing, dressing, artwork, skillful manipulation o Readiness for learning and independence in school Psychosocial development (Erikson) - Initiation vs. guilt o Chief psychosocial task of the preschool period o Initiative includes saying something new, beginning a new project, or expressing an emotion o Feelings of guilt, anxiety, and fear may result from thoughts that differ from expected behavior o Development of superego (conscience) o Learning right from wrong; moral development CogniOve development (Piaget) - - Preoperational – preconceptual phase (2 – 4 years) o Preoperational phase spans age 2 to 7 years o Divided into two stages o Preconceptual phase at 2 to 4 years Preoperational – intuitive thought phase (4 – 7 years) o Shifts from egocentric thought to social awareness o Able to consider other viewpoints o Egocentricity is still evident Development of body image o o o Increasing comprehension of “desirable” appearances Aware of racial identity, differences in appearances, and biases Poorly defined body boundaries o Fear that if the skin is “broken,” all one’s blood and “insides” can leak out o Frightened by intrusive experiences Social development o o o o o Individuation–separation process is completed Overcomes stranger anxiety and fear of separation from the parents Still needs parental security and guidance Security from familiar objects Play therapy is beneficial for working through fears, anxieties, and fantasies Language development o o o o o Major mode of communication and social interaction Vocabulary increases dramatically between age 2 and 5 yrs Complexity of language use increases between age 2 and 5 yrs Form 3-4 word sentence between ages 3-4 yr olds; 4-5 word sentences for 4-5 yr olds 2 yrs – 300 words, 5 yrs – 2100 words Personal-social behavior o o o o Play o o o o o Less help with toileting, eating, or dressing More sociable and willing to please Has internalized values and standards of family and culture May begin to challenge parental values Associative play- interact, sharing toys, but not taking turns Imitative play Imaginative play and imaginative playmates Dramatic play- Dress up clothes, props, dolls, housekeeping toys Manipulative, constructive, creative, educations toys good for this age Coping with common concerns of preschool-age children - School experience: Preschool and kindergarten – adjustment to school, peer experiences, social emotional physical development Sex – find out what the children know and think/ be honest - - Gifted children can present unique challenges, require increased attention and stimulation Aggression – Behavior that attempts to hurt another person or destroy property, avoiding media exposure, using appropriate behavior to reply- non-negative appropriate discipline, May be influenced by biologic, sociocultural, and familial variables, Factors that affect aggressive behavior include gender, frustration, modeling, and reinforcement Speech- most critical period for speech development occurs between 2-4 yrs; early detection, prevention, an intervention; Stuttering Stammering Stress – especially vulnerable because of inability to cope, best approach is prevention, Minimum amounts of stress can be beneficial, Parental awareness of signs of stress in the child’s life Schedule adequate rest, Prepare the child for upcoming changes to maximize coping strategies Fears – greatest during school age years; dark, alone, animals, ghosts, sexual matters…concept of animism. Actively involve children in finding solutions, practical desensitization PromoOng opOmal health - - - Nutrition o Caloric requirements are approximately 1200-1400 calories o Fluid requirements depend on activity, climate, state of health o Total fat should be reduced (30-40% total caloric intake) > 2 yrs o Limiting sugar sweetened beverages and juices o MyPlate (USDA recs) o Food fads and strong tastes still common o Finicky eaters o Help prepare meals o Obesity, DM, metabolic syndrome, CV dx Sleep/activity o Patterns vary widely o Sleeps 10-13 hrs (including naps) o Nighttime waking still common o Consistency is key o Free active play is encouraged o Emphasis is on fun and safety Injury prevention/education o Slightly less prone to injury/falls due to matured motor skills, coordination and balance o Safety education and setting good examples o Development of long-term safety behaviors o Bike helmets AnOcipatory guidance for families of preschoolers - Family-Centered Care Box - Guidance During Preschool Years (p. 440) o Injury prevention shifts from protection to education o Children begin questioning previous teachings of parents o Children begin to prefer the companionship of peers o Entry into school marks separation for parents and children Chapter 14 – Common Health Problems of Early Childhood Sleep problems - Nightmares vs night terrors (Table 14.1) o Prime time for sleep disturbances o Going to sleep o Waking during the night o Nightmares/sleep terrors o Prolong bedtime o Interventions based on cause o Increasing autonomy, negative sleep associations, nighttime fears, inconsistent sleep routines, lack of limits, media exposure o Avoid violent media at all times, limit media in evening o Consistent bedtime routines, do not take into parents bed or stay up too late, night lights, comfort object o Start wind down time early o If they’re having a night terror, though, your child won’t really be awake. They may try to talk or yell, but they probably won’t be forming full sentences or even words. o Other signs of a night terror include: o Appearing frightened. o Being difficult to console. o Moving wildly or erratically. o Screaming, shouting or wailing. o Staring blankly. o Sweating It’s best to allow a sleep terror to run its course. Trying to awaken your child in the midst of a sleep terror probably won’t work. If you do rouse your child, they’ll probably be confused or frightened to wake up so suddenly. Remember, they were sleeping during the night terror, so waking up to you in their room worrying about them will likely be concerning for them. That means more Ome and consoling to get back to sleep. Accidental / injurious ingesOons - - Emergent management (p. 446) o Poison control center o Call first, before initiating any interventions o Assessment o Vitals, mental status, resp & circ support o Gastric decontamination o Induce vomiting, activated charcoal, absorb toxin, or use gastric lavage, depending on the agent ingested o Prevention of recurrence o Passive vs active measures o Passive – no active participation, child safety caps on meds Prevention (Nursing Care Guidelines Box) Lead poisoning o o o o o o o o o o o o Lead-based paint in older homes o Impoverished, urban area; older rental homes Microparticles of lead contaminate bare soil Food and water contamination o Pottery and dishes Folk remedies Can be inhaled or ingested Rarely symptomatic (even at high levels) but affects renal, neurologic, and hematologic systems (bone marrow) Highly problematic for growing brain and nervous system Diagnosis o Anemia o Blood lead level >5 μg/dl (venous sample) Screening for lead poisoning at age 1 and 2 years Chelation therapy Prognosis o Permanent CNS damage Nursing priorities of care o Prevent o Identify (iron deficiency) o Lead settles in teeth and bones o Children who are iron deficient absorb more readily Child maltreatment (Box 14.5, 14.6) - - Neglect o Failure to provide for basic needs and adequate level of care o Physical neglect o Emotional neglect Physical abuse o Deliberate infliction of injury o Minor injuries more frequently reported o Major injuries lead to more death o Abusive head trauma o AKA shaken baby syndrome o 1300 children affected per yr, 25% die, 80% severe sequelae o Violent shaking and shearing forces of blood vessels and neurons • Intracranial bleeds, retinal hemorrhages o Rib fractures, long bone fractures o Often no outward signs of injury and presents with non-specific symptoms o Poor outcomes – seizure d/o, visual impairments, hearing loss, cerebral palsy, mental, cognitive, motor impairments o large head, weak neck muscles o Vomiting, irritability, poor feeding, listlessness o Severe – seizures, alterations in LOC, apnea, bradycardia Risk factors: Parental characteristics • Young parent, single parent • Socially isolated/few supportive relationships • Low income/little education • Substance abuse • Low self-esteem • Limited parenting skills • Hx of abuse o Child characteristics • Birth - 1 yr • Need for constant attention • Unplanned, unwanted • Hyperactive • Disabled o Environmental characteristics • Chronic stress • Divorce • Poverty • Unemployment • Poor housing • Alcoholism/drug addiction • Substitute caregivers Sexual abuse o Most devastating o Increasing over past decade Clinical manifestations o Growth failure/signs of malnutrition o Poor hygiene o Enuresis o Sleep disorders o Bruising in various stages of healing o Burns o Patterns of objects in bruising/burns o Specific types/location of fractures o Multiple o Spiral, twisting o Skull, face, nose o Recurrent UTI o Rash/bleeding genitals o Abnormal affect o Withdrawn o Self-stimulating behaviors o Lack of social smiles in infants o - - - o Antisocial behavior o Inappropriate reactions (no response to scary stimuli) o Fear of parents/home o Age-inappropriate sexual play o Sudden change in behavior o Regressive behavior o Decline in school performance Nursing Care o Physical assessment documentation o Identify all injuries o Ensure whole body is evaluated § Scalp, behind ears, frenulum o Very clear and detailed description o Genital exam findings may be normal in sexual abuse § Consider bed linens, clothing o Strict adherence to evidence collection guidelines o Assess behavioral indicators Chapter 15 - Health Promo3on of the School-Age Child Biologic development (Table 15.1) - Maturation of systems o GI- Fewer stomach upsets, stable glucose levels, increased capacity; caloric needs less than preschool o GU- Larger bladder capacity (girls>boys) o CV- Steady increase in BP and decrease in HR o Immune- More competence in localizing infections & producing antibody response o MS- Bones continue to ossify, but still yield to pressure and muscle pulls Psychosocial development (Erikson) - Industry vs inferiority o o o o Crisis between productivity (competence) and inadequacy (incompetence) Attempt to master many skills; simply trying new things is insufficient Sustained activity leading to accomplishment is the goal Self-pride as well as peer feedback CogniOve development (Piaget) - Concrete operational stage (7 – 11 years) o Concrete thought arises from what is visible, tangible and real, not abstract and theoretical o Grounded in actual experiences o New, logical thought o Classification – organization into groups according to some characteristic they have in common o Seriation – concept that things can be arranged in a logical series o Master concept of conservation Social development - - Play o o o o Peers o Social relationships and cooperation o Peer groups have own culture o Appreciate multiple viewpoints o Sensitive to social norms o Forming friendships o Formalized groups o Peer pressure/bullying Relationship with families o Parents still primary influence o Transition to prefer peers Rules and rituals Team play Quiet games and activities Ego mastery Coping with common concerns of school-age children - - - School experience, teacher, and parent roles o Important socializing agent o Role of teachers o Role of parents Latchkey children o Increased risk for injury & delinquency, social/ emotional issues o After school programs Discipline o Effective in positive, supportive environment; guide desired behaviors Dishonest behavior - o Lying, cheating, stealing Stress and fear o Significant from many sources o Risk factors and solutions PromoOng opOmal health - - - - Nutrition o Importance of balanced diet to promote growth o Quality of the diet related to the family’s pattern of eating o Quality of dietary choices in the school cafeteria Sleep/rest o Total sleep varies o Depends upon age, activity levels, health status o Naps extinguished o Average at 5 yrs: 10-13 hrs o Average at 11 yrs: 9-12 hrs o Bedtime resistance o Common until age 12 Exercise/ activity o Sports and injury prevention o Essential for muscle development and tone, balance and coordination, strength and endurance o Sports o Controversy regarding early participation in competitive sports o Concerns with physical and emotional maturity in competitive environment o Acquisition of skills o Generally, like competition o Limit media/screen time Injury prevention (Table 15.2) o Motor vehicle accidents o Bicycle safety o Skateboard, in-line skating, scooter, ATVs o Trampolines o Drowning AnOcipatory guidance for families of school-age children - Family-Centered Care Box - Guidance During School Years (p. 480) o Education, proper equipment o Account for child’s increasing independence Chapter 16 – Health Problems of the School-Age Child Obesity o o Increase in body weight from excessive accumulation of body fat relative to lean body mass o > 95th BMI for age, per CDC Overweight: weighing more than average for height and body build o o o o - - Significant number of overweight/obese children in US (1 in 3) Disproportionately high among non-Hispanic black and Hispanic youth Also affected by parent education <5% cases attributed to underlying disease Complications o Low self-esteem o Social isolation o Anxiety o Depression o Eating disorders o Hypercholesterolemia o HTN o Respiratory disorders (OSA) o Orthopedic conditions (SCFE) o Cholelithiasis o Cancer o Non-alcoholic fatty liver disease o T2DM o Metabolic syndrome Recommendations for prevention (Box 16.1) Dental care o o o o o Caries one of most common chronic diseases affecting all children Periodontal disease Malocclusion Trauma EliminaOon - - ADHD o o o o - - Enuresis o Repeated inappropriate voiding in a child who has reached an age where bladder control is expected (5 yrs) o Primary: has never obtained bladder control for extended periods o Ex. Maturational delay, functionally small bladder o Secondary: onset of wetting after established urinary continence o Ex. Stress, infection, sleep disorder o Monosymptomatic (only at night) or non-monosymptomatic (daytime with emotional stressors) Etiology o Sleep theory – deep sleepers o Functional bladder capacity theory – maximum volume of urine voided following micturition o Failure to concentrate urine, insufficient ADH o Dysfunctional detrusor activity Encopresis o Repeated inappropriate stooling in a child who has reached an age where bowel control is expected (4 yrs) o Primary: has never obtained bowel control (>4yrs) o Ex. Autism spectrum, spina bifida, neglect, lax training o Secondary: had reliably had bowel control for 6+ months before onset o Ex. Emotional or psychological concerns, stress o More common males Etiologies o Most common cause is constipation o Often precipitated by environment change o Impairs usual movement and contraction of colon o Abnormalities in digestive tract o Medical conditions o Psychogenic encopresis 3 Subtypes, per APA Combined Predominantly inattentive Predominantly hyperactive-impulsive Clinical manifestations (Box 16.5) o Poor impulse control, difficulty sitting still, fidgeting, difficulty sustaining attention, disorganized Therapeutic management o Based on age and severity o Behavioral o Collaboration between home, school, and other environments Medications- Other medications may be used if comorbidities exist Ritaline (methyphenidate), Concerta, Vyvanse o Pharmacologic: stimulants vs nonstimulants • Dose based on response • Common side effects o Appetite loss o Abd pain o Headaches o Sleep disturbance o Growth velocity issues o Avoid in Tourette syndrome Nursing care management o School nurses particularly involved in management o Instituting behavioral modifications & environmental manipulation o Classroom placement o Medication education o Diet monitoring o - Learning disabiliOes o o o o Tics o o o o o o 3 characteristics o Lower intellectual ability o Childhood onset o Significant impairment of social functioning or adaptation Dyslexia, Dysgraphia, Dyscalculia Multiple tests to diagnose Therapeutic management depends on which type Involuntary, recurrent, random, rapid stereotypes movement of vocalization 1 in 5 children PANDAS Most resolve by late childhood/adolescence without intervention Support to child and famil * Pediatric autoimmune neuropsychiatric d/o with strep infections Stress - - Functional abdominal pain o Often attributed to psychogenic causes, organic cause in very few cases; real pain o Assess risk factors – somatic predisposition, lifestyle, routines, diet, learned behaviors o Tend to be high achievers with high expectations o Reassurance and reduce symptoms o High fiber diet, bowel regimen, CBT Conversion reaction o Psychophysiologic disorder with sudden onset often related to major family crisis o May experience physical manifestations o Abd pain, pseudoseizures, fating, paralysis, h/a, visual field deficits o Nursing care includes education and support o Conversion – dealing with the stressor, ruling out other etiologies o Schizo – requires highly specialized care, education on medications (multiple side effects), clarify abnormal perceptions Mood and affect - - Depression (Box 16.7) o Low self-esteem, hopelessness, poor social engagement; manifests differently o Assess need for inpatient care o Can interrupt normal G&D, must be recognized, assess for suicide risk, adherence to care plans, detection as it can affect normal G&D o Medications can take time to work, close monitoring during initial medication Schizophrenia- rare, genetic, gestational and birth complications Anxiety o Most common mental health d/o o Excessive worry, fearfulness; difficulty functioning o Often unrecognized Chapter 17 – Health Promo3on of the Adolescent Biologic development (Table 17.1) o o Physical growth o Dramatic increase in growth § Second only to the infant period o Final 20-25% of linear growth achieved o Up to 50% of ideal body weight gained – in growth spurt o Height spurt follows a weight spurt, and then a muscle spurt occurs Neuroendocrine events of puberty o Hypothalamus> pituitary> gonads> estrogen/testosterone o Gonads- paired sex glands (ovaries in female, testicles in males produce hormones and gamates o Estradiol- Sex hormone considered the chief estrogen, Females produce more estradiol than males o Testosterone- Sex hormone, the best known of the androgens (male hormones). Secreted in far greater amounts by males than by females o o o * Hypothalamus produces GnRH à ant pituitary gland à FSH/LH --> gonadsm Sexual Maturation o Orderly sequence o Age of onset varies; genetics important in determining timing o Primary sex characteristics § Parts of the body that are directly involved in reproduction, including the vagina, uterus, ovaries, testicles, and penis o Secondary sex characteristics § Observable physical traits that are not directly involved in reproduction but that indicate sexual maturity, such as a man's beard and a woman's breasts o Precocious puberty is a concern if occurs before age 8 Other physiologic changes o Size and strength of heart increase o HR decreases o Blood volume and BP increases o Adult blood values achieved o Lung volume increases o RR reaches adult rates o Frontal cortex still not fully developed CogniOve development (Piaget) - - - - Formal operational thought o Fourth and final stage of cognitive development o Characterized by: o Systematic logic o Ability to think abstractly o Consider consequences to actions o Hypothesize possibilities Deductive reasoning- Reasoning from a general statement, premise, or principle, through logical steps to figure out, Top-down reasoning § Deductive- all students in the class like pizza, Jane is in the class, Therefore, Jane likes pizza, At the conference, all those presenting have a PhD, Maria is presenting at the conference, Therefore, Maria has. PhD Inductive reasoning- Reasoning from one or more specific experiences or facts to a general conclusion; maybe less cognitively advanced than deduction, bottom-up reasoning § Inductive – every quiz has been easy…the exam should be easy teacher used ppt in the last few lectures, therefore the teacher will use PowerPoint tomorrow Hypothetical thought- Reasoning that includes propositions and possibilities that may not reflet reality, If-then propositions Hallmark of formal operational thought is capacity to think of possibility not just reality Psychosocial development (Erikson) - Identity vs role confusion o Fifth stage of development/psychosocial crisis o Finding one’s own identity but confused by many possible roles to adopt o o o “Who am I?” Identity Consistent definition of one's self as a unique individual, in terms of roles, attitudes, beliefs, and aspirations Identity achievement Erikson's term for the attainment of identity, or the point at which a person understands who they are as a unique individual, in accord with past experiences and future plans Social environments - - Families o Changes in family microsystems lead to more unsupervised time o Increase in risk taking behaviors, poor diet, more screen time, substance use, sexual intercourse, etc o Decrease opportunities for communication and intimacy with parents o Adolescents who eat meals together 5-7 times/week are more connected with family, perform better academically, participate in fewer risky behaviors o Family belonging leads to less susceptibility to peer pressure o Parenting style affects development o Authoritative is preferred o Microsystems – more divorce, remarriage, single parents, older parents, working parents o Roles change from “protection–dependency” to “mutual affection and equality” o Conflicts with parents o Parent–adolescent conflict typically peaks in early adolescence and is more a sign of attachment than of distance o Most often mothers & daughters o Bickering- Repeated petty arguments (more nagging than fighting) about routine, dayto-day concerns o Neglect- Although teenagers may act as if they no longer need their parents, neglect can have adverse effects. More important that conflict -- family closeness and cohesiveness o Communication: Do family members talk openly and honestly? o Support: Do they rely on each other? o Connectedness: How emotionally close are family members? o Control: Do parents undermine independence? Peer groups o Critically important in adolescence, may have positive and negative effects o Adolescents spend more time with peers than children o Peers serve as credible source of information, role models of social behaviors, social reinforcement o Help navigate physical changes of puberty, the intellectual challenges of high school & the social changes of leaving childhood o Do not negate the need for parental support o Tech may bring peers together- provide outlet for those who feel alone o o o o - - Encouragement to conform to one’s friends in behavior, dress and attitude, usually considered a negative force Deviancy training – destructive peer support in which one person shows another how to rebel against authority Controlling for environment and genes, if one twin is delinquent, the other will likely follow Study showed twins - controlling for genes and environment, if one is delinquent, the other will likely be as well Romantic Partners First romance typically occurs in high school with steady relationships Exclusive commitment is ideal, but often difficult; breakups are common More closely related to emotional state than actual interactions Sexual intercourse more or less likely dependent upon peer support o o o o School o Essential for successful future o Failure to complete high school reduces employment opportunities and probability to earning adequate income o Lack of parental involvement in school o Social environment, practices and conditions impact outcomes o Smaller classes and school size o Foster positive peer group relationships o Promote health and fitness o Encourage family involvement Work o Media, technology use o Most adolescents employed o Mostly restricted jobs, but some may promote social skills, autonomy o May have detrimental effects (esp working >20 hrs/wk) o Jobs that link to adults who serve as vocational mentors are valuable Technology o 95% of teens have smart phones; 45% online on constant basis o Provide a connection, but have many downsides o Cyberbullying, sexting o Multitasking with technology • Unclear how this will affect the brain o Increased concern for distracted driving • 59.5% of 12th graders report texting/emailing while driving PromoOng opOmal health o o o Comprehensive approach o Individuals, families, communities o Physical, cognitive, emotional, social Focus based on morbidity and mortality of age group Mortality: o MVC, accidental injuries, homicide, suicide o o - - - Morbidity o Motor and recreational vehicles, sexual and physical abuse, unwanted pregnancy, STIs, substance use, mental health issues Inequities exist o Gap in life expectancy between African American and white adolescents o African American and native American males have highest risk of premature death Adolescent perspective o To be effective, health promotion must include adolescent perspective and involvement o Many are reluctant to seek services for social and psychologic problems o Unwilling to seek health care for fear parents will find out Context o Schools o Health promotion and disease prevention § Healthy eating, fitness, assignments o School-based and school-linked health services o Communities o Media campaigns, raise awareness o Health care settings o Internet and other technologies Parenting/family adjustment Psychosocial adjustment Intentional and unintentional injury Dietary habits/ eating disorders Physical fitness Sexual health Substance use Mental health and suicide Sleep deprivation LGBTQ++ o Unique considerations for care o Higher prevalence of bullying, dating violence, eating disorders, suicidal behaviors o Ensuring safety in disclosure, sensitive care AnOcipatory guidance for adolescents and their families - Family-Centered Care Box – Guidance During Adolescence (p. 534) Chapter 18 – Health Problems of the Adolescent Varicocele - Enlarged veins of spermatic cord, may impair fertility (impaired spermatogenesis) Palpated as worm like mass above the testicle Surgery (if growth of testicle is arrested) EpididymiOs - Inflammatory response of epididymis; may be infectious (viral or bacterial) Urethral d/c, pyuria, dysuria, fever - Most common causes Chalmydia and Gonorrhea Abx, rest, analgesics, scrotal support GynecomasOa - Breast enlargement; unilateral or bilateral Normally occurs transiently; may be pathologic May also be drug-induced Prepubertal should be evaluated for rare tumors, Klinefelter Plastic surgery in severe cases Drugs: spironolactone, cimeOdine, ketoconazole, estrogens, TesOcular torsion - Occurs when a testicle rotates, twisting the spermatic cord that brings blood to the scrotum Reduced blood flow causes sudden and often severe pain and swelling, redness, absent cremasteric reflex Fever and urinary symptoms typically absent Most common between ages 12 and 18, but it can occur at any age, even before birth Surgical emergency Menstrual disorders - - Amenorrhea o Absence of menstruation o Primary - age 14 w/o secondary sexual characteristics or 16 w/ secondary sex characteristics o Secondary- absence of menses after menstruation was previously established for more than 3 menstrual cycles or irregular menses for 6 months after the establishment of normal menses o Female athlete triad – reduced calorie intake, amenorrhea, low bone mineral density Dysmenorrhea o Pain during or shortly before menstruation o May be primary or secondary (pathological) o Therapeutic management § NSAIDs § Estrogen therapy § Oral contraceptives § Dietary changes § Exercises, comfort measures Sexually transmiped infecOons (Box 18.2) - Gonorrhea Symptoms Males: yellow discharge, painful urination, urinary frequency/urgency/nocturia Females: may be asymptomatic or yellow discharge, painful urination, pain with intercourse Rectal pain, purulent discharge, bloody stool Treatment - Drug resistant strains increasing Single dose IM ceftriaxone plus single dose PO azithromycin Treat for concomitant chlamydia Chlamydia (Most common bacterial) Symptoms Males: may be asymptomatic, or redness of urethral meatus, tenderness, itching, discharge Females: may be asymptomatic, or purulent discharge, cervical redness, edema, pelvic congestion Increased risk of HIV if damage to cervix Treatment Single dose PO azithromycin or 7 days PO doxycycline BID Abstain for 7 days Notify partners Syphilis Symptoms Increasing in MSM population Primary – painless chancre Secondary – (6wks-mos) widespread rash and generalized LAD, fever, h/a, malaise, wart like lesions Tertiary – Neuro, CV, MS effects Treatment Penicillin G Human papillomavirus Most common viral Symptoms Types 16, 18 can lead to cervical cancer Types 6, 11 cause genital warts (may appear cauliflower like) Males: lesions on penis, anus Females: lesions posterior to genitals, anus, buttocks Treatment Palliate, not curative Topical medications Cryotherapy Surgery Herpes Simplex Virus Symptoms May be asymptomatic or painful lesions, fever, chills, malaise, LAD, headaches Lesions: vesicles, pustules, ulcers Females have more severe symptoms, cervix involvement May be passed form motheràinfant Treatment Palliative not curative Oral antivirals Oral analgesic Consistent condom use - Flares trigger with stress Trichomoniasis (protozoa) Symptoms Males: asymptomatic or urethritis Females: yellow/green frothy, malodorous discharge, cervix with “strawberry spots”, acute inflammation Treatment Metronidazole (flagyl) oral Pelvic inflammatory disease Pregnancy o o o Adolescent pregnancy o Slight rate decline in US o Considered socially, educationally, psychologically, and economically disadvantageous to both mother and child o Delayed or inadequate prenatal care common Contraception o Methods should be safe, effective, and suited to the individual o Contraception use is variable o Less familiar with partner less likely to use contraception o Dissatisfaction with conception side effects Nursing care management Sexual assault o o o o o o Unwanted sexual activity by force or manipulation High risk population Often committed by known perpetrator Diagnostic evaluation o Consider pediatric SANE Therapeutic management Nursing care management EaOng Disorders (Table 18.5) o o o o o o o o Multifactorial etiology Genetic predisposition Psychological: Fear, anxiety, obsessive compulsiveness, depression, other disorders Sociocultural: Body dissatisfaction, family dysfunction Environmental: Involvement with sports or activities with aesthetic or athletic expectations Anorexia/Bulimia Anorexia nervosa (AN) characterized by: § Refusal to maintain a minimally normal body weight § Intense fear of weight gain § Disturbed body perception and denial of the problem Bulimia nervosa (BN) characterized by: Binge eating followed by inappropriate compensatory behaviors such as selfinduced vomiting, misuse of laxatives, diuretics, fasting, exercise § Secretive frenzied consumptions large amounts high-calorie food Eating disorder NOS (EDNOS) Binge eating disorder § Similar to BN, but no purging § o o Substance abuse - Self-harm Suicide Motivation – often initial experimentation, curiosity Goal is often peer acceptance Two broad categories often – experimenters and compulsive users, or recreational users Abused drugs o Tobacco and smokeless tobacco o Alcohol o Cocaine o Narcotics o CNS depressants, stimulants o Mind-altering drugs - By age 18, 80-90% of adolescents have tried alcohol - CNS depressants: hypnotic drugs, barbiturates, non-barbiturates, alcohol, Rohypnol (10x more powerful than Valium) - CNS stimulants: amphetamines, cocaine - Mind-altering – cannabis included, LSD - Self-injury or self-mutilation, without intent to die Excludes eating disorders, drug abuse & socially accepted behaviors (piercing & tattoos) Peaks age 15-16 years, declines at 18 yrs Prominent in females, those with sexual orientation confusion, hx of physical/sexual abuse Rarely seek treatment Therapeutic management Nursing Alert The S.A.F.E. Alternatives offers a helpline, (1-800-DON'T-CUT [366-8288]) & hosts a website (http://www.selfinjury.com) with information about treatment programs & other resources - Terms: Suicide/Suicidal ideation/ Suicide attempt Methods • Firearms – most commonly used instrument for completed suicide by males • Cutting/piercing – by females • Hanging - - Depression - • Overdose – most common method for attempt • • Most important indicator is active psychiatric d/o Individual, family, social, environmental factors • • • • • • • • Fantasy based Relief from suffering, gain comfort and sympathy, revenge Return and witness grief Therapeutic management Threats require immediate action Medications SSRIs Therapy Etiology Motivation Dip in self-esteem occurs at puberty Common for every ethnicity and gender Less confidence, sadness Family and cultural norms are protective Feelings of hopelessness, lethargy, and worthlessness that last two weeks or more Disrupts normal activities Girls have much higher rates than boys (2x) Biological and cultural difference Rumination - repeatedly thinking and talking about past experiences o Can contribute to depression o More common in girls