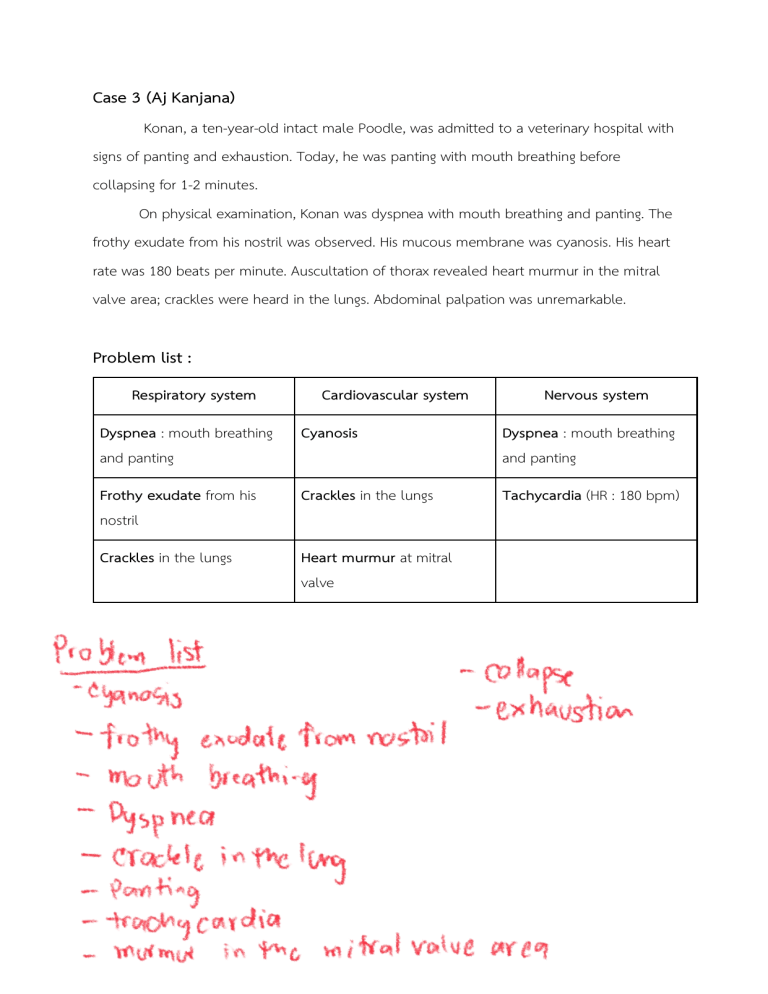
Case 3 (Aj Kanjana)
Konan, a ten-year-old intact male Poodle, was admitted to a veterinary hospital with
signs of panting and exhaustion. Today, he was panting with mouth breathing before
collapsing for 1-2 minutes.
On physical examination, Konan was dyspnea with mouth breathing and panting. The
frothy exudate from his nostril was observed. His mucous membrane was cyanosis. His heart
rate was 180 beats per minute. Auscultation of thorax revealed heart murmur in the mitral
valve area; crackles were heard in the lungs. Abdominal palpation was unremarkable.
Problem list :
Respiratory system
Cardiovascular system
Nervous system
Dyspnea : mouth breathing
and panting
Cyanosis
Dyspnea : mouth breathing
and panting
Frothy exudate from his
nostril
Crackles in the lungs
Tachycardia (HR : 180 bpm)
Crackles in the lungs
Heart murmur at mitral
valve
Cardiovascular system
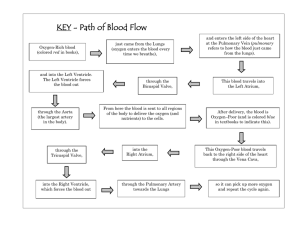
Anatomy of the heart
Picture 1 : The anatomy of the heart includes four chambers
( References : https://my.clevelandclinic.org/health/body/21704-heart )
the parts of the heart
● Walls.
● Chambers that are like rooms.
● Valves that open and close like doors to the rooms.
● Blood vessels like plumbing pipes that run through a building.
● An electrical conduction system like electrical power that runs through a
building.
Heart walls
Heart walls are the muscles that contract (squeeze) and relax to send blood throughout the
body. A layer of muscular tissue called the septum divides heart walls into the left and right
sides.
heart walls have three layers:
1. Endocardium: Inner layer.
2. Myocardium: Muscular middle layer.
3. Epicardium: Protective outer layer.
The epicardium is one layer of pericardium. The pericardium is a protective sac that covers
the entire heart. It produces fluid to lubricate the heart and keep it from rubbing against
other organs.
Heart chambers
Dog’s heart has four separate chambers. have two chambers on the top (atrium, plural atria)
and two on the bottom (ventricles), one on each side of the heart.
●
Right atrium: Two large veins deliver oxygen-poor blood to the right atrium. The
superior vena cava carries blood from the upper body. The inferior vena cava brings
blood from the lower body. Then the right atrium pumps the blood to the right
ventricle.
●
Right ventricle: The lower right chamber pumps the oxygen-poor blood to lungs
through the pulmonary artery. The lungs reload the blood with oxygen.
●
Left atrium: After the lungs fill blood with oxygen, the pulmonary veins carry the
blood to the left atrium. This upper chamber pumps the blood to the left ventricle.
●
Left ventricle: The left ventricle is slightly larger than the right. It pumps oxygen-rich
blood to the rest of the body.
Heart valves
Dog’s heart valves are like doors between heart chambers. They open and close to allow
blood to flow through. They also keep blood from moving in the wrong direction.
Atrioventricular valves
The atrioventricular (AV) valves open between upper and lower heart chambers. They
include:
●
Tricuspid valve: Door between right atrium and right ventricle.
●
Mitral valve: Door between left atrium and left ventricle.
Semilunar valves
Semilunar (SL) valves open when blood flows out of ventricles. They include:
●
Aortic valve: Opens when blood flows out of the left ventricle to the aorta (artery
that carries oxygen-rich blood to body).
●
Pulmonary valve: Opens when blood flows from the right ventricle to pulmonary
arteries (the only arteries that carry oxygen-poor blood to lungs).
Blood vessels
heart pumps blood through three types of blood vessels:
●
Arteries carry oxygen-rich blood from heart to body’s tissues. The exception is
●
pulmonary arteries, which go to the lungs.
Veins carry oxygen-poor blood back to the heart.
●
Capillaries are small blood vessels where the body exchanges oxygen-rich and
oxygen-poor blood.
Electrical conduction system
Picture 2 : Diagram of the cardiac conduction system
( References : https://my.clevelandclinic.org/health/body/21704-heart )
The heart's conduction system is like the electrical wiring of a building. It controls the
rhythm and pace of the heartbeat. Signals start at the top of the heart and move down to
the bottom. Dog’s conduction system includes:
●
Sinoatrial (SA) node: Sends the signals that make the heart beat.
Atrioventricular (AV) node: Carries electrical signals from heart’s upper chambers to
its lower ones.
●
Left bundle branch: Sends electric impulses to the left ventricle.
●
Right bundle branch: Sends electric impulses to the right ventricle.
●
Bundle of His: Sends impulses from AV nodes to the Purkinje fibers.
Purkinje fibers: Make heart ventricles contract and pump out blood.
●
●
Auscultation
structure
Dogs
Mitral valve
L,5th ICS at CCJ
Aortic valve
L,4th ICS above CCJ
Pulmonic valve
L,2nd-4th ICS at CCJ just above the sternum
Tricuspid valve
R,3rd-5th ICS at CCJ
ICS = intercostal space
L = left
CCJ = costochondral junction
R = right
Picture 3 : Diagram showing approximate valve locations for auscultation
(copyright J.M. Naylor 2001 University of Saskatchewan)
(References : https://www.vetvisions.com/small-animal-cardiology-auscultation/ )
Mitral Regurgitation ; pathogenesis and clinical finding
1. If mitral regurgitation occurs while the left ventricle is systolic, some blood will flow back
to the left atrium, increasing volume and pressure in the left atrium. Later, when the left
ventricle is diastolic, the blood from the left atrium will be sent to the left ventricle, causing
increased volume to push back into the left ventricle. At this time, it will cause S3 heart
sound, which is the sound caused by rapid ventricular filling. When the blood enters the left
ventricle more than normal, the heart will expand to support more blood, which causes
eccentric left ventricular hypertrophy.
Picture 4 : Mitral regurgitation
(References : https://www.mayoclinic.org/diseases-conditions/mitral-valveregurgitation/symptoms-causes/syc-20350178)
2. Apical impulse, also known as the point of maximal impulse (PMI) and the apex beat, is
the pulse point on the chest at the point over the apex of the heart. It is different from the
other pulse. When palpation, another pulse point located in the arteries throughout the
body senses the heart rate, while apical impulse, palpated in the mitral area in dogs, senses
the contraction of the left ventricle that pumps blood from the heart through the aorta to
the rest of the body. Apical impulse on palpation and auscultation is one of the clinical
findings that provide many contents such as heart rhythm or the strength of pulse directly
to the left ventricle. Therefore, apical pulse is the most accurate reading of heart rate and it
can indicate heart health.
3. The consequences associated with common cardiac defects, mitral regurgitation. With each
contraction of the left ventricle, a normal volume of blood is ejected into the aorta, and an
additional volume of blood is ejected backward (through the regurgitant valve) into the left
atrium. As a result, there is an increase in the volume work performed by the left ventricle.
Therefore mild-to-moderate left ventricular hypertrophy develops. Also, in a heart with mitral
regurgitation, the left atrium becomes distended, and left atrial pressure increases, as does
pulmonary venous pressure. Elevated pressure in the pulmonary blood vessels forces water
and electrolytes out of the bloodstream and into the pulmonary interstitial space, causing
pulmonary edema.
In the lung, as in other organs, there is continual movement of water and solutes from the
capillary bed into the lung interstitium. Forces describes in starling's equation govern the
movement of fluid across the pulmonary capillary endothelium as follows:
𝐹𝑙𝑢𝑖𝑑 𝑖𝑛𝑓𝑙𝑢𝑥
= 𝐾{(𝑃𝑐𝑎𝑝 − 𝑃𝑖𝑓) − 𝜎(𝛱𝑐𝑎𝑝 − 𝛱𝑖𝑓)}
Where 𝐾 is the rate of flow (mL/h) per unit of pressure across the endothelium and is
referred to as the filtration coefficient; 𝑃𝑐𝑎𝑝 is capillary hydrostatic pressure; 𝑃𝑖𝑓 is
interstitial fluid hydrostatic pressure; 𝛱𝑐𝑎𝑝 and 𝛱𝑖𝑓 are capillary and interstitial colloid
osmotic (oncotic) pressure respectively; and 𝜎 is the reflection coefficient,which indicates
how effective the capillary endothelium is at preventing the movement of proteins and
other solutes. When the normal values shown in picture 5 are inserted into Starling’s
equation, the net force is positive and favors fluid filtration out of the capillaries and into
the interstitium.
Picture 5 : Diagrammatic representation of a pulmonary capillary in the alveolar septum.
Top, on the “thin” side of the septum, capillary endothelium and alveolar epithelium share
a basement membrane. Bottom, on the “thick” side of the septum, endothelium and
epithelium are separated by a layer of interstitial tissue. Typical values for capillary and
interstitial fluid hydrostatic pressures (𝑃𝑐𝑎𝑝 and 𝑃𝑖𝑓) and oncotic pressures (𝛱𝑐𝑎𝑝 and
𝛱𝑖𝑓) are shown.
(Reference: Klein BG: Cunningham’s Textbook of Veterinary Physiology, 6th ed.,2020,p 572)
Increases in capillary hydrostatic pressure occur in animals with left-sided heart failure. These
elevated pressures result in an increased fluid influx into the interstitium. As fluid transfer out
of capillaries increase even further, excess fluid accumulates around the bronchi and large
vessels in the compliant peribronchial and perivascular spaces. Fluid flux across the
pulmonary capillary endothelium, the proteoglycan bridge in the alveolar septum break,
which greatly allows greater fluid movement into the interstitium. This fluid is termed
pulmonary interstitial edema and is seen radiographically as peribronchial cuffing.
Picture 6: Peribronchial cuffing refers to a radiographic term used to describe haziness or
increased density around the walls of a bronchus or large bronchiole.
(Reference: https://www.teachingmedicine.com/tutorial/CHF/Peribronchial_cuffing )
When fluid pressure within pulmonary interstitium exceeds the barrier capacity of the
alveolar epithelium,the clinically evident alveolar edema occurs as fluid enters the air
spaces across the alveolar epithelial cells or at the level of the bronchioles
.
Picture 6: The development of pulmonary interstitial edema and alveolar edema
(Reference:https://www.semanticscholar.org/paper/Diagnosis-and-management-ofcardiogenic-pulmonary-Alwi/9a1c410cfb48e56ea1b28447473758966988a799)
Pulmonary edema may cause crackling sounds in your lungs. People or animals with
congestive heart failure (CHF) often have pulmonary edema. CHF occurs when the heart
cannot pump blood effectively. This results in a backup of blood, which increases blood
pressure and causes fluid to collect in the air sacs in the lungs.
4.Mitral regurgitation is incompetency of the mitral valve causing flow from the left ventricle
into the left atrium during ventricular systole. This leads to a reduction in stroke volume
ejected into the aorta, resulting in decreased cardiac output, causing insufficient blood to
supply various organs.When there is not enough blood flowing to the organs, it stimulates
the The renin-angiotensin-aldosterone system (RAAS) .RAAS is the system of hormones,
proteins, enzymes and reactions that regulate blood pressure and blood volume on a longterm basis. It regulates blood pressure by increasing sodium (salt) reabsorption, water
reabsorption (retention) by kidney and vascular tone (the degree to which blood vessels
constrict, or narrow) leading to an increase in intravascular hydrostatic pressure systemically.
This causes water to be driven out of the blood vessels into the interstitial space, resulting
in peripheral edema.
The renin-angiotensin-aldosterone system (RAAS)
The first stage of the RAAS is the release of the enzyme renin. Renin released from
granular cells of the renal juxtaglomerular apparatus (JGA) in response to one of three
factors:
● Reduced sodium delivery to the distal convoluted tubule detected by macula densa
cells.
● Reduced perfusion pressure in the kidney detected by baroreceptors in the afferent
arteriole.
● Sympathetic stimulation of the JGA via β1 adrenoreceptors.
Angiotensinogen is a precursor protein produced in the liver and cleaved by renin to form
angiotensin I. Angiotensin I is then converted to angiotensin II by angiotensin converting
enzyme (ACE). This conversion occurs mainly in the lungs. Angiotensin II exerts its action by
binding to various receptors throughout the body.
The table below outlines its effect at different points.
Site
Main Action
Arterioles
Vasoconstriction
Kidney
Stimulates Na+ reabsorption
Sympathetic nervous system
Increased release of noradrenaline (NA)
Adrenal cortex
Stimulates release of aldosterone
Hypothalamus
Increases thirst sensation and stimulates antidiuretic hormone (ADH) release
5. Blood consistently flows backward throughout the systole, resulting in Holosystolic
murmur at mitral valve which is to hear the murmur throughout the compression period.
And it usually Radiates to the axilla. In addition, the amount of blood that goes to the body
decreases or the stock volume decreases so the heart muscle has to contract more.
Therefore, increase afterload.
6. The serum creatinine is increased. Creatinine is the wasted product in metabolism of
protein and the beaking down of muscular tissue. Due to the decreased cardiac output
cause the decreasing amount of oxygen to the kidney, this lead to renal dysfunction. The
kidney parenchyma are injured due to oxygen insufficient which result in decreasing of
Glomerula filtration rate (GFR) and ability of kidney to clear out creatinine.
Nervous system
The nervous system includes the brain, spinal cord, and a complex network of nerves.
This system sends messages back and forth between the brain and the body.
The brain is what controls all the body's functions. The spinal cord runs from the brain
down through the back. It contains threadlike nerves that branch out to every organ and
body part. This network of nerves relays messages back and forth from the brain to different
parts of the body.
The nervous system is made up of the central nervous system and the peripheral
nervous system:
The central nervous system includes the brain and spinal cord.
● The peripheral nervous system includes the nerves that run throughout the whole
body.
The nervous system uses tiny cells called neurons to send messages back and forth from
the brain, through the spinal cord, to the nerves throughout the body.
●
Billions of neurons work together to create a communication network. Different neurons
have different jobs. For example, sensory neurons send information from the eyes, ears,
nose, tongue, and skin to the brain. Motor neurons carry messages away from the brain to
the rest of the body to allow muscles to move. These connections make up the way we
think, learn, move, and feel. They control how our bodies work — regulating breathing,
digestion, and the beating of our hearts.
The CNS
The CNS (Central Nervous System) components involved in regulating the heart and lungs
Hypothalamus
The hypothalamus is a crucial region of the brain located below the thalamus, forming the
floor of the third cerebral ventricle. It's a small, cone-shaped structure that extends
downward from the brain, terminating in the pituitary stalk, which connects it to the pituitary
gland. Functionally, the hypothalamus serves as a control center for numerous autonomic
nervous system functions and interacts intricately with the endocrine system through its
connections with the pituitary gland.
The brainstem
The brainstem, located in the middle of the brain, is the stalk-like part of the brain that
connects the brain to the spinal cord and is only about one inch long. This region regulates
essential functions such as blood pressure, breathing, heart rhythms, and swallowing.
The brainstem can be further subdivided into the midbrain, pons, and medulla.
The midbrain, otherwise known as the mesencephalon, is crucial for regulating eye
movements, emotions, hearing, and long-term memory. Notably, the substantia nigra, rich in
dopamine neurons, is located within the midbrain and is often affected by Parkinson's
disease.
The pons is the starting location for four of the 12 cranial nerves. Some of the different
functions regulated by the pons include facial movements, hearing, breathing, and balance.
The medulla is located at the bottom of the brainstem where the brain and spinal cord
meet. This region of the brainstem regulates breathing, heart rate, and blood pressure.
Additionally, the medulla maintains reflective activities such as sneezing, vomiting, coughing,
and swallowing.
The PNS
The PNS consists of both the somatic and autonomic nervous systems. Taken together,
these systems transmit information from different areas of the body to the brain and ensure
that signals sent from the brain are transmitted to other areas of the body.
(Reference : https://en.wikivet.net/Autonomic_Nervous_System_-_Anatomy_%26_Physiology)
The somatic nervous system
The somatic nervous system (SNS) consists of peripheral nerve fibers that carry sensory
information or sensations from peripheral organs to the CNS. The SNS also includes motor
nerve fibers that exit the brain to carry commands for movement to the skeletal muscles.
For example, upon touching a hot object, sensory nerves carry information about the heat
to the brain. Subsequently, the brain, through motor nerves, commands the hand muscles
to withdraw it immediately. This process takes less than one second to complete. The
neural cell body that carries this information often lies within the brain or spinal cord and
projects directly to a skeletal muscle.
The autonomic nervous system
The autonomic nervous system (ANS) controls the nerves of the body's inner organs that
cannot be controlled consciously. The ANS can be further subdivided into the sympathetic,
parasympathetic, and enteric nervous systems. Some of the different activities controlled by
the ANS include the heartbeat, digestion, subconscious breathing, blood pressure, and
sexual arousal.
(Reference : https://www.pinterest.com/pin/autonomic-nervous-system-nervous-system-ofanimals--263390278180895432/)
The sympathetic pathway is associated with the heart and lungs.
The sympathetic pathway originating from the medulla➝spinal cord➝preganglionic
neurons ➝ middle cervical ganglia➝cardiac plexus and the vagosympathetic
trunk➝heart, bronchiole smooth muscle, and blood vessels ➝ heart rate increase dilation
of the trachea and bronchi, dilation of bronchioles in the lungs, vasodilation (increasing
blood flow in the cardiac muscle), and systemic vasoconstriction.
Backward Heart Failure → Mitral Regurgitation (MR)
The activation of the sympathetic nervous system (SNS) increases stroke volume by
providing inotropic support to the failing heart, while also inducing peripheral
vasoconstriction to maintain mean arterial perfusion pressure.
Heart
Mitral regurgitation (MR)➝cardiac output decreases➝ leading to a drop in blood pressure
➝ Baroreceptor and chemoreceptor reflexes detect➝signaling the hypothalamus and
medulla oblongata ➝ activates the sympathetic tone➝increasing sympathetic pathway
activity➝heart rate raises ➝tachycardia.
Kidney
Mitral regurgitation (MR)➝cardiac output decreases ➝ causing a drop in blood pressure
➝ Baroreceptor and chemoreceptor reflexes detected ➝ signaling the hypothalamus and
medulla oblongata➝sympathetic tone increase➝activates the Renin-AngiotensinAldosterone System (RAAS).
Lungs
Mitral regurgitation (MR)➝pulmonary edema ➝ Blood gas abnormality (O2↓ CO2↑) ➝
Chemoreceptors(carotid bodies and medulla oblongata) detected ➝afferent
impulses➝the brainstem respiratory center for processing (pons and medulla) ➝generates
efferent impulses ➝ resulting in dyspnea.
Pulmonary edema can cause disturbances in the airway epithelium➝triggering sensory
receptors like the juxtacapillary receptors➝receptors detect➝send afferent
impulses➝brainstem, specifically the pons and medulla ➝ efferent impulses ➝ the
lungs ➝ leading to dyspnea.
Pulmonary edema➝mechanical respiratory load➝increasing airway resistance and
elastance➝Mechanoreceptors and chest wall receptors, such as muscle spindles and Golgi
tendon organs detected ➝ generating afferent impulses➝brainstem➝The somatosensory
cortex processes this information ➝ efferent impulses➝chest wall and
diaphragm➝resulting in dyspnea.
Respiratory system
Frothy exudate
In heart failure (HF), pleural effusion results from increased interstitial fluid in the
lung due to elevated pulmonary capillary pressure.then plasma will leak to alveolar space
and mix with surfactant in the alveolar surface.the mixture of fluid is beated in one
direction toward the pharynx by ciliary escalator mechanism.eventually the mixture of fluid
is frothy by ciliary movement
Dyspnea
Dyspnea refers to labored or difficult breathing and is often associated with
hypoventilation. A person suffering from dyspnea is aware, or conscious, of the breathing
pattern and is generally uncomfortable and in distress. Orthopnea refers to dyspnea while
lying down. It is relieved by sitting or standing up. This condition is common in patients with
heart disease.
Crackles in the lungs
Crackles are adventitious or abnormal breath sounds that sound like bubbling or
popping and can reflect fluid overload in the lungs because of an acute exacerbation of or
onset of heart failure
References
1. Yu Y. Mitral Regurgitation: Pathogenesis and clinical findings | Calgary Guide [Internet].
The Calgary Guide to Understanding Disease. 2023. Available from:
https://calgaryguide.ucalgary.ca/mitral-regurgitation-pathogenesis-and-clinical-findings/
2. Professional CCM. Apical Pulse [Internet]. Cleveland Clinic. Available from:
https://my.clevelandclinic.org/health/articles/23346-apical-pulse
3. Eske J. Where is the apical pulse, and what can it indicate? [Internet]. 2020. Available
from: https://www.medicalnewstoday.com/articles/apical-pulse
4. Domocmat C. Assessments heart & neck vessel [Internet]. SlideShare. 2017. Available
from: https://www.slideshare.net/kharr/assessments-heart-neck-vessel
5. The Renin-Angiotensin-Aldosterone-System - TeachMePhysiology [Internet].
TeachMePhysiology. 2023. Available from: https://teachmephysiology.com/urinarysystem/regulation/the-renin-angiotensin-aldosterone-system/
6. Douedi S, Douedi H. Mitral regurgitation [Internet]. StatPearls - NCBI Bookshelf. 2023.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK553135/
7. Professional CCM. Renin-Angiotensin-Aldosterone System (RAAS) [Internet]. Cleveland
Clinic. Available from: https://my.clevelandclinic.org/health/articles/24175-reninangiotensin-aldosterone-system-raas
8. Airway clearance in the normal lung (2022) Bronchiectasis. Available at:
https://bronchiectasis.com.au/physiotherapy/principles-of-airway-clearance/airwayclearance-in-the-normal-lung (Accessed: 21 March 2024).
9. O’Brien, P. (2021) How does mucociliary clearance work, AirPhysio. Available at:
https://www.airphysio.com/mucociliary-clearance-and-removal/ (Accessed: 21 March
2024).
10. Hirsch L, editor. Nervous system (for parents) | nemours kidshealth [Internet]. The
Nemours Foundation; 2022 [cited 2024 Mar 21]. Available from:
https://kidshealth.org/en/parents/brain-nervous-system.html
11. Utiger RD. Hypothalamus [Internet]. Encyclopædia Britannica, inc.; 2024 [cited 2024
Mar 21]. Available from: https://www.britannica.com/science/hypothalamus
12. Paharia PT. What is the nervous system? [Internet]. 2022 [cited 2024 Mar 21].
Available from: https://www.news-medical.net/health/What-is-the-NervousSystem.aspx
13. Hasenfuss G, Mann DL. Pathophysiology of heart failure [Internet]. 2016 [cited 2024
Mar 21]. Available from: https://thoracickey.com/pathophysiology-of-heart-failure/
14. Manolis AA, Manolis TA, Manolis AS. Neurohumoral activation in heart failure
[Internet]. Multidisciplinary Digital Publishing Institute; 2023 [cited 2024 Mar 21].
Available from: https://www.mdpi.com/1422-0067/24/20/15472
15. Gifford AH, Mahler DA. Dyspnea [Internet]. 2016 [cited 2024 Mar 21]. Available from:
https://thoracickey.com/dyspnea/
16. Dypsnea [Internet]. Slideshare; 2018 [cited 2024 Mar 21]. Available from:
https://www.slideshare.net/yuyuricci/dypsnea
17. Manning HL. pathophysiology of Dyspnea [Internet]. 1996 [cited 2024 Mar 21].
Available from:
https://www.researchgate.net/publication/15722272_Pathophysiology_of_Dyspnea
18. Lo, K. B., Dayanand, S., Ram, P., Dayanand, P., Slipczuk, L. N., Figueredo, V. M., &
Rangaswami, J. (2019). Interrelationship Between Kidney Function and Percutaneous
Mitral Valve Interventions: A Comprehensive Review. Current cardiology reviews,
15(2), 76–82. https://doi.org/10.2174/1573403X14666181024155247
19. Jennifer Dekerlegand,Chapter 25 - Congestive Heart Failure,Editor(s): Michelle H.
Cameron, Linda G. Monroe,Physical Rehabilitation,W.B. Saunders,2007,Pages 669688,ISBN9780721603612,https://doi.org/10.1016/B978-072160361-2.500284.(https://www.sciencedirect.com/science/article/pii/B9780721603612500284)
20. Bronchiectasis. Airway clearance in the normal lung - bronchiectasis [Internet].
Bronchiectasis. 2022. Available
from: https://bronchiectasis.com.au/physiotherapy/principles-of-airwayclearance/airway-clearance-in-the-normal-lung
21. O’Brien P, O’Brien P. How does mucociliary clearance work – Mucus clearance and
removal [Internet]. AirPhysio. 2021. Available
from: https://www.airphysio.com/mucociliary-clearance-and-removal/