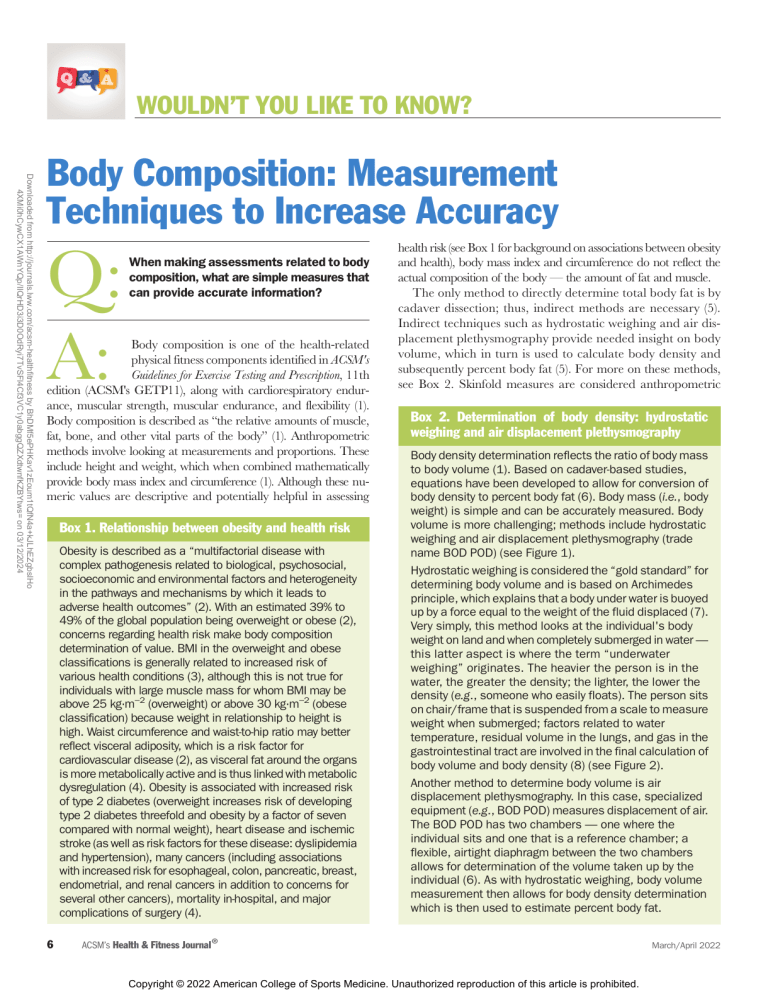
WOULDN’T YOU LIKE TO KNOW? Downloaded from http://journals.lww.com/acsm-healthfitness by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo 4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 03/12/2024 Body Composition: Measurement Techniques to Increase Accuracy Q: A: When making assessments related to body composition, what are simple measures that can provide accurate information? Body composition is one of the health-related physical fitness components identified in ACSM's Guidelines for Exercise Testing and Prescription, 11th edition (ACSM's GETP11), along with cardiorespiratory endurance, muscular strength, muscular endurance, and flexibility (1). Body composition is described as “the relative amounts of muscle, fat, bone, and other vital parts of the body” (1). Anthropometric methods involve looking at measurements and proportions. These include height and weight, which when combined mathematically provide body mass index and circumference (1). Although these numeric values are descriptive and potentially helpful in assessing Box 1. Relationship between obesity and health risk Obesity is described as a “multifactorial disease with complex pathogenesis related to biological, psychosocial, socioeconomic and environmental factors and heterogeneity in the pathways and mechanisms by which it leads to adverse health outcomes” (2). With an estimated 39% to 49% of the global population being overweight or obese (2), concerns regarding health risk make body composition determination of value. BMI in the overweight and obese classifications is generally related to increased risk of various health conditions (3), although this is not true for individuals with large muscle mass for whom BMI may be above 25 kg·m−2 (overweight) or above 30 kg·m−2 (obese classification) because weight in relationship to height is high. Waist circumference and waist-to-hip ratio may better reflect visceral adiposity, which is a risk factor for cardiovascular disease (2), as visceral fat around the organs is more metabolically active and is thus linked with metabolic dysregulation (4). Obesity is associated with increased risk of type 2 diabetes (overweight increases risk of developing type 2 diabetes threefold and obesity by a factor of seven compared with normal weight), heart disease and ischemic stroke (as well as risk factors for these disease: dyslipidemia and hypertension), many cancers (including associations with increased risk for esophageal, colon, pancreatic, breast, endometrial, and renal cancers in addition to concerns for several other cancers), mortality in-hospital, and major complications of surgery (4). 6 health risk (see Box 1 for background on associations between obesity and health), body mass index and circumference do not reflect the actual composition of the body — the amount of fat and muscle. The only method to directly determine total body fat is by cadaver dissection; thus, indirect methods are necessary (5). Indirect techniques such as hydrostatic weighing and air displacement plethysmography provide needed insight on body volume, which in turn is used to calculate body density and subsequently percent body fat (5). For more on these methods, see Box 2. Skinfold measures are considered anthropometric Box 2. Determination of body density: hydrostatic weighing and air displacement plethysmography Body density determination reflects the ratio of body mass to body volume (1). Based on cadaver-based studies, equations have been developed to allow for conversion of body density to percent body fat (6). Body mass (i.e., body weight) is simple and can be accurately measured. Body volume is more challenging; methods include hydrostatic weighing and air displacement plethysmography (trade name BOD POD) (see Figure 1). Hydrostatic weighing is considered the “gold standard” for determining body volume and is based on Archimedes principle, which explains that a body under water is buoyed up by a force equal to the weight of the fluid displaced (7). Very simply, this method looks at the individual's body weight on land and when completely submerged in water — this latter aspect is where the term “underwater weighing” originates. The heavier the person is in the water, the greater the density; the lighter, the lower the density (e.g., someone who easily floats). The person sits on chair/frame that is suspended from a scale to measure weight when submerged; factors related to water temperature, residual volume in the lungs, and gas in the gastrointestinal tract are involved in the final calculation of body volume and body density (8) (see Figure 2). Another method to determine body volume is air displacement plethysmography. In this case, specialized equipment (e.g., BOD POD) measures displacement of air. The BOD POD has two chambers — one where the individual sits and one that is a reference chamber; a flexible, airtight diaphragm between the two chambers allows for determination of the volume taken up by the individual (6). As with hydrostatic weighing, body volume measurement then allows for body density determination which is then used to estimate percent body fat. ACSM’s Health & Fitness Journal ® Copyright © 2022 American College of Sports Medicine. Unauthorized reproduction of this article is prohibited. March/April 2022 Figure 1. Body volume measurement using air displacement plethysmography (trade name BOD POD). Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved. Downloaded from http://journals.lww.com/acsm-healthfitness by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo 4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 03/12/2024 measures and have been described as “doubly indirect” given that the skinfold thickness is used in prediction equations along with an individual's age to estimate body density, which in turn allows for calculation of body fat percentage (i.e., the percent of the total body weight that is fat) (1,5). Given the specialized equipment and costs associated with hydrostatic weighing and air displacement plethysmography, the focus of this article will be on anthropometric measures that are relatively simple and inexpensive, providing valuable insights when done carefully and consistently according to standardized procedures. Figure 2. Hydrostatic weighing is used to measure body density in order to obtain measures of body composition. Photo courtesy of the Department of Exercise Science and Sport Management at Kennesaw State University. Used with permission. BODY MASS INDEX (BMI) BMI is a mathematical calculation that reflects an individual’s body weight relative to height; the calculation is as follows: body weight in kilograms (kg) divided by height in meters squared (m2). The unit of measure is kilograms per square meter (or this may be written as kg·m−2). Body weight should be determined on a calibrated scale (balance beam or electronic) with no shoes and minimal clothing (i.e., shorts and T-shirt) (7). A stadiometer is a device with a vertical ruler and sliding horizontal platform that is lowered to the top of the person’s head to measure height. Height should be determined with shoes off, heels together, standing with head, buttocks, and heels in contact with the vertical ruler; the individual should breathe in and hold breath while looking forward while the horizontal platform is lowered to touch the top of the head (7). With accurate height and weight measures, BMI can be calculated. A sample calculation is shown in Box 3. Classification by BMI includes the following: underweight is less than 18.5 kg·m−2, normal is 18.5–24.9 kg·m−2, overweight is 25–29.5 kg·m−2, and obesity is 30 kg·m−2 and above (1). Although often used Volume 26 | Number 2 www.acsm-healthfitness.org Copyright © 2022 American College of Sports Medicine. Unauthorized reproduction of this article is prohibited. 7 WOULDN’T YOU LIKE TO KNOW? Box 3. BMI calculation For an individual with a weight of 154 lbs and a height of 70 inches: Downloaded from http://journals.lww.com/acsm-healthfitness by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo 4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 03/12/2024 First convert weight from pounds to kilograms (kg); there are 2.2 lbs in each kilogram: 154/2.2 = 70 kg Then convert height from inches to meters (m); there are 0.0254 meters in each inch: 70 inches 0.0254 = 1.78 m To complete the calculation, take the weight in kilograms and divide by the height squared BMI = 70/(1.782) BMI = 70/(3.17) BMI = 22.1 kg·m−2 Another option for determining BMI is to use an online calculator. This calculator allows you to enter either standard or metric units and then the BMI is provided in kg·m−2: https://www.nhlbi.nih.gov/health/educational/ lose_wt/BMI/bmicalc.htm. on a population level to determine “obesity,” a shortcoming of BMI is the inability to look at composition or to differentiate fat from muscle (1). For example, a muscular strength-trained individual with a low percent body fat can have a BMI above 30 kg·m−2. An obesity classification for this individual would be inappropriate as the “excess” weight relative to height is muscle rather than fat. Other assessments, including girth (circumference) or skinfold measures, would be more helpful in this situation. CIRCUMFERENCE Measurement of waist circumference, or determination of the ratio of waist and hip circumference, can be used to reflect the pattern of body fat distribution (1). Body fat that dominates on the trunk is referred to as android obesity; body fat in the hip and thigh area is referred to as gynoid obesity (1). Android obesity 8 is associated with increased risk of hypertension, type 2 diabetes, dyslipidemia, cardiovascular disease, and metabolic syndrome, among other health concerns (1). Circumference measures are simple and can be used to reflect general distribution of body fat. Ideally, the measurements should be made with a tape measure with spring-loaded handle (see Figure 3 for an example), which allows for better consistency between measures as the tension on the tape can be standardized (1). Without the spring mechanism, differing measures could result simply by altering the amount of tension on the tape (i.e., holding it tightly or more loosely). Two measures should be taken, allowing for time between a single measure or rotating through sites, with an average of two measures within 5 mm being used. The waist circumference focuses on central obesity. The location of “waist” is not universally defined (9); for more insights into the various definitions, see the prior ACSM's Health & Fitness Journal® article “A Simple yet Complicated Tool: Measuring Waist Circumference to Determine Cardiometabolic Risk.” ACSM's GETP11 defines waist as “at the level of the iliac crest” (1), as shown in Figure 3. High risk according to this measurement site begins at 90 cm (35.5 inches) for women and 100 cm (39.5 inches) for men (1). Note that the population on which these risk criteria are based is limited (Caucasian), and thus values reflecting risk may be different for other racial and ethnic groups (1). Waist-to-hip ratio involves a slightly different measure for “waist” along with hip circumference (1,7). The ratio requires a calculation: waist circumference divided by hip circumference (1). The individual should be standing with arms at sides and feet together. The abdomen should be relaxed, in a neutral position. For this ratio, waist is measured as the narrowest part of the torso above the umbilicus and below the xiphoid process. The hip is measured with the tape ACSM’s Health & Fitness Journal ® Copyright © 2022 American College of Sports Medicine. Unauthorized reproduction of this article is prohibited. March/April 2022 Box 4. Description of skinfold sites (adapted from ACSM [1]) (https://youtu.be/cEsuxgX2Udg). Figure 4. Components of a fold (skin and subcutaneous fat) and location of caliper (blue mark). Photo courtesy of Barbara Bushman. Downloaded from http://journals.lww.com/acsm-healthfitness by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo 4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 03/12/2024 Abdominal: vertical fold located 2 cm to the right of the umbilicus Suprailiac: diagonal fold located above the anterior superior iliac spine (i.e., anterior axillary line immediately above the iliac crest) Triceps: vertical fold located midway between the acromion process of the scapula and the olecranon process of the ulna in the posterior midline with arm held freely at the side Thigh: vertical fold located midway between the inguinal crease and the proximal border of the patella in the anterior midline Subscapular: diagonal fold located 1–2 cm below the inferior angle of the scapula Chest (for males): diagonal fold located midway between the anterior axillary line and the nipple in men at the maximal circumference of the buttocks. For both the waist and the hip girth measures, ensure that the tape measurement is in a horizontal orientation around the entire circumference of the waist and hip, respectively. For individuals younger than 60 years of age, health risk is high when the ratio is >0.95 for men and >0.86 for women (1). For individuals 60 to 69 years of age, high risk is >1.03 for men and >0.90 for women (1). SKINFOLD MEASURES Skinfold measures correlate with more technical methods of body fat determination (i.e., hydrodensitometry and air displacement plethysmography). The basic premise is that the amount of subcutaneous fat is proportional to the total body fat (1). Although generally about one-third of body fat is subcutaneous, many factors can affect this, including differences in intra- and intermuscular fat and fat deposits in internal organs along with variations for males and females, age, and race (1). Figure 3. Waist measurement with spring-loaded handle. Skinfold assessment can predict percent body fat within ±3.5% fat (1). That level of accuracy assumes proper techniques were used with correct determination of skinfold location and properly calibrated skinfold calipers (1). A “fold” should include two layers of skin and the underlying subcutaneous fat (see Figure 4). Locations of selected sites are defined in Box 4. Pictures of the sites are found in Figures 5 to 9. Note that the marks on the skin are oriented to allow for consistent placement of the caliper (on the “cross bar”), while the other line should be the “top” of the fold (see Figure 10 A and B). Taking care in measuring and marking these locations will improve accuracy and is a key aspect of skinfold measures. Standardized testing is key for accuracy and includes the following (1): Figure 5. Abdominal and suprailiac skinfold locations. Photo courtesy of Barbara Bushman. Photo courtesy of Barbara Bushman. Volume 26 | Number 2 www.acsm-healthfitness.org Copyright © 2022 American College of Sports Medicine. Unauthorized reproduction of this article is prohibited. 9 WOULDN’T YOU LIKE TO KNOW? Downloaded from http://journals.lww.com/acsm-healthfitness by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo 4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 03/12/2024 • Measures should be done on the right side of the client’s body • The pinch should be maintained throughout the measurement • Caliper placement should be directly on the skin (not over clothing) • Caliper should be 1 cm away from the fingers pinching the fold to avoid compressing the fold being measured (see Figure 10 for correct and incorrect distancing) • Caliper should be placed halfway between the top of the fold and the base (see blue bar in Figure 4) • Allow the caliper to settle for 2 seconds before taking the reading, open caliper jaws to remove from skin after measurement is noted • Repeat measurements should be taken by rotating through the sites to allow for each area to return to normal between measures • Measures should be within 2 mm Figure 7. Thigh skinfold location. Photo courtesy of Barbara Bushman. At least two measures per site are required, within 2 mm of one another. If the initial two measures are not within 2 mm, take an additional measurement, using the mean of whichever two measures were within 2 mm of one another for the calculations. Figure 6. Triceps skinfold location. Photo courtesy of Barbara Bushman. Skinfold equations have been developed for males and females with various combinations of skinfold measures, along with age, allowing for calculation of body density. Box 5 shows two options that each require three skinfold site measurements for men and women. The calculated body density is then used to estimate percent body fat. One commonly used equation is as follows (1): Figure 8. Subscapular skinfold location. Photo courtesy of Barbara Bushman. 10 ACSM’s Health & Fitness Journal ® Copyright © 2022 American College of Sports Medicine. Unauthorized reproduction of this article is prohibited. March/April 2022 Figure 9. Chest skinfold location (male). Photo courtesy of Barbara Bushman. Downloaded from http://journals.lww.com/acsm-healthfitness by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo 4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 03/12/2024 although normative values suggest a range of 12% to 23% for males and 17% to 26% for females as “good” (1). Other factors, including age, sex, race, and athletic level, are additional considerations regarding what best reflects a healthy percentage of body fat (1). SUMMARY Anthropometric measures allow for indirect determination of aspects related to body composition. Weight in relation to height (i.e., BMI) provides general insight, although BMI is unable to discriminate between difference in weight due to excess fat compared with muscle. Circumference measures (hip girth and waist-to-hip ratio) are helpful in gauging distribution of body fat and, thus, may be of better insight than BMI regarding health. An indirect assessment of body composition is possible with the skinfold technique, which requires care in measurements of subcutaneous fat to calculate an estimate of percent body fat. The determination of body composition may thus be made with simple tools and is a valuable addition within fitness assessments. Box 6. Example skinfold test results with calculation of percent body fat 33-year-old male Percent body fat = [(4.95/body density) − 4.50] 100. Thus, the steps are to record the skinfolds required, complete the matching calculation for body density, and then mathematically convert body density to percent body fat. An example is found in Box 6. A healthy percent body fat has not been defined, Box 5. Equations to determine body density from skinfold measures (1) Male Three-site formula requiring sum of chest, abdominal, and thigh measures (SS) and age in years Body density = 1.10938 − (0.0008267 SS) + (0.0000016 SS2) − (0.0002574 age) Three-site formula requiring sum of chest, triceps, and subscapular measures and age in years Body density = 1.1125025 − (0.0013125 SS) + (0.0000055 SS2) − (0.000244 age) Female Three-site formula requiring sum of triceps, suprailiac, and thigh measures and age in years Body density = 1.0994921 − (0.0009929 SS) + (0.0000023 SS2) − (0.0001392 age) Three-site formula requiring sum of triceps, suprailiac, and abdominal measures and age in years Body density = 1.089733 − (0.0009245 SS) + (0.0000025 SS2) − (0.0000979 age) Volume 26 | Number 2 Site Measurement 1 (mm) Measurement 2 (mm) Mean (mm) Chest 12 14 13 Abdomen 14 14 14 Thigh 16 18 17 For the calculation, the sum of the three skinfolds is 44 mm (13 + 14 + 17 = 44). The next step is to enter the sum of the skinfolds and age in years into the equation from Box 5 reflecting these three sites (these values are shown in bold; other values are the constants in the regression equation) Body density = 1.10938 − (0.0008267 44) + (0.0000016 442) − (0.0002574 33) Body density = 1.10938 − (0.0008267 44) + (0.0000016 1936) − (0.0002574 33) Body density = 1.10938 − (0.0363748) + (0.0030976) − (.0084942) Body density = 1.0676086 The body density (do not round this number) then can be entered into the equation to convert to percent body fat: Percent body fat = [(4.95/body density) − 4.50] 100 Percent body fat = [(4.95/1.0676086) − 4.50] 100 Percent body fat = 13.7% For a 33-year-old male, this is in the “excellent” fitness classification category, per ACSM's GETP11 (1). www.acsm-healthfitness.org Copyright © 2022 American College of Sports Medicine. Unauthorized reproduction of this article is prohibited. 11 WOULDN’T YOU LIKE TO KNOW? Figure 10 A and B. Skinfold showing proper distance of 1 cm between pinch and caliper and incorrect technique. A, Proper. B, Incorrect. See video for both improper and proper skinfold technique: https://youtu.be/RdQ0UUblQ8E. Photos and video courtesy of Barbara Bushman. Downloaded from http://journals.lww.com/acsm-healthfitness by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo 4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 03/12/2024 1. American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 11th ed. Philadelphia (PA): Wolters Kluwer; 2021, 513p. 2. Powell-Wiley TM, Poirier P, Burke LE, et al, American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143:e984–1010. doi:10. 1161/CIR.0000000000000973 Available from: https://www.ahajournals.org/ doi/epub/10.1161/CIR.0000000000000973. 3. National Heart, Lung, and Blood Institute web site [Internet]. Assessing Your Weight and Health Risk. Bethesda (MD): National Heart, Lung, and Blood Institute; [cited 2011 Nov 4]. Available from: https://www.nhlbi.nih.gov/health/educational/lose_ wt/risk.htm. 4. Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33(7):673–89. Available from: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4859313/. 5. Kasper AM, Langan-Evans C, Hudson JF, et al. Come back skinfolds, all is forgiven: a narrative review of the efficacy of common body composition methods in applied sports practice. Nutrients. 2021;12:1075. Available from: https://www.mdpi. com/2072-6643/13/4/1075. 6. Fosbøl MØ, Zerahn B. Contemporary methods of body composition measurement. Clin Physiol Funct Imaging. 2015;35:81–97 Available from: Contemporary methods of body composition measurement (wiley.com). 7. American College of Sports Medicine. ACSM's Fitness Assessment Manual. 6th ed. Philadelphia (PA): Wolters Kluwer; 2022, 193 p. 12 8. Brodie D, Moscrip V, Hutcheon R. Body composition measurement: a review of hydrodensitometry, anthropometry, and impedance methods. Nutrition. 1998; 14(3):296–310. 9. Serviente C, Sforzo GA. A simple yet complicated tool: measuring waist circumference to determine cardiometabolic risk. ACSMs Health Fit J. 2013;17(6):29–34. Available from: https://journals.lww.com/acsm-healthfitness/Fulltext/2013/11000/A_ Simple_Yet_Complicated_Tool__Measuring_Waist.7.aspx. Barbara A. Bushman, Ph.D., FACSM, ACSM-CEP, ACSM-EP, ACSM-CPT, is a professor at Missouri State University. Dr. Bushman has authored papers related to menopause, factors influencing exercise participation, and deepwater run training; she authored ACSM’s Action Plan for Menopause (Human Kinetics, 2005), edited both the first and second editions of ACSM’s Complete Guide to Fitness & Health (Human Kinetics, 2011 and 2017), and promotes health/fitness at www. Facebook.com/FitnessID. ACSM’s Health & Fitness Journal ® Copyright © 2022 American College of Sports Medicine. Unauthorized reproduction of this article is prohibited. March/April 2022