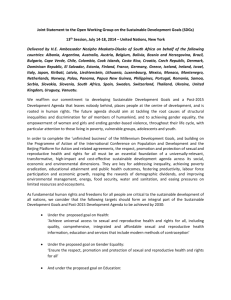
SOCIOL 3HH3: SOCIOLOGY OF HEALTH ROOM FOR IMPROVEMENT: Reproductive Health Needs A Revamp Name: Alice Xue Student Number: 1138724 Introduction For the vast majority of all living species, sexual reproduction is the fundamental source of their continued survival. However, sexuality for humans is much more complex than this functionalistic definition would suggest. Sexuality is often considered part of an individual’s identity and hold significant social value, affecting the way one views themselves and their interactions with others. For this reason, reproductive health is a very important pillar in determining the physical, mental and social wellbeing of an individual. The World Health Organization defined reproductive health as the reproductive processes, functions and system at all stages of life. UN agencies goes further to claim that sexual and reproductive health includes “physical, as well as psychological well-being vis-a-vis sexuality” (Joint United Nations Programme on HIV/AIDS et al 2018). In real life application, reproductive health may include, but is not limited to, being informed about safe sex practices through well implemented sexual education programs, having easy and affordable access to birth control options and sexual healthcare. For women, reproductive healthcare may be particularly important as it not only pertains to managing pregnancy and childbirth, but is also inseparable from gender equality. Proper reproductive health allows for crucial decision making in regards to a woman’s body and future. Institutions such as education, healthcare and government all play important roles in achieving reproductive health for its citizens. Therefore, it would be in the best interest for social institutions to implement legislation that advocates for reproductive health and help citizens attain a happier and healthier standard of living. . Thesis This inquiry argues that current institutional legislations surrounding reproductive health are inadequate. Reproductive health needs to be better established as a topic in social institutions, such as education and healthcare, in order to promote better sexual agency and a healthier attitude towards sexuality. Theoretical Approach A feminist perspective will be used to understand the impacts of current reproductive health legislations on sexual agency, particularly for women in health care institutions. The feminist tradition, at its core, is focused on a humane system of justice that acknowledges that women are placed at a disadvantage in a patriarchal society (Inderbitzin et al 2015). More specifically, the effects of these patriarchal institutions will be examined in context of the structure agency debate; a debate concerning individual choice versus determination by outside forces and of the need to understand an issue that has such important implications for politics and social life (Hornosty and Germov 2012). This theoretical approach is important in understanding the effects of a insufficient sex education curriculum for both male and female adolescents as well as the implications of gender inequality found in health care. The inquiry will delve into how these social institutions limit an individual’s ability to make well informed decisions and fail to provide the required resources to achieve reproductive health. Education Abstinence Only Programs Sex education is one of the few reliable sources for sexuality and sexual health for youth. However, there is no standardized sex education policy in the US, leading to curriculums that are factually lacking and often riddled with misinformation, hindering an adolescent’s development of a healthy attitude towards sexuality. There are three main types of programs found in the American sex education system; abstinence-only, abstinence-plus, and comprehensive sex education (Lindberg et Al 2016). Abstinence centered education focus on providing instruction on saying no to sex without providing information on birth control. A study done by Advocates for Youth state, “many of the curricula commonly used in abstinence-only programs distort information about the effectiveness of contraceptives, misrepresent the risks of abortion, blur religion and science, treat gender stereotypes as scientific fact, and contain basic scientific errors" (Blanton 2018). These curriculums may also enforce the idea that an individual may “lose part of their worth everytime they sleep with someone”, a message that is particularly directed at the female gender. This idea feeds into the sexual double standard that women are more harshly judged for their number of sexual partners compared to their male counterparts (Kreager and Staff 2009). This kind of sex education spreads misinformation and assigns morality to sexual behaviour. By presenting subjective belief systems as objective facts, adolescents are impaired in their decision making when it comes to their sexuality. Comprehensive Programs Still, abstinence only programs are more prominent in American schools even though comprehensive programs are proven to be more effective and promote better decision making in adolescents (Lindberg et Al 2016). Comprehensive program curriculums commonly include topics on sexual health topics suchs as human sexuality, HIV or STD prevention and pregnancy prevention through birth control options. But even the comprehensive programs take a traditional disease model when approaching the topic of sexual activity, resorting to fear tactics to scare adolescents away from the consequences of being sexually active. This kind of educational program is grossly lacking from a dynamic relationship perspective as it fails to address adolescents’ social and emotional concerns regard sex and could lead to more serious adverse outcomes after having sex (Brady and Halpern-Felsher 2007). Being sexually active encompasses far more than the biological risks of pregnancy and sexually transmitted diseases, the social and emotional consequences can cause equal if not greater impact on the psychological well being of adolescents. By forgoing such an important component, adolescents are not able to proper assess situations and may not act in their best interest out of ignorance. It would be far more beneficial for sex education curriculums to address these social and psychological factors, which encourage for a better understanding of sexuality and promote well informed decisions. Lack of LGBTQ Curriculums Additionally, sex education curriculums are largely heteronormative, disregarding alternative sexual identities and alternative definitions of sex. This may be particularly distressing to individuals that identify as part of the LGBTQ demographic, an already marginalized group, whose experiences and identities are not being adequately addressed as part of the curriculum. According to a Human Rights Campaign survey conducted in 2015, only 12% of millennials recall learning about same-sex relationships as part of their sex education curriculum (Blanton 2018). Certain abstinence only curriculums may even promote fear of same sex attraction, creating a hostile environment for LGBTQ youth. Queer youth need a safe and reliable source of information regarding their sexual health, positive representation of LGBTQ individuals and guidance in understanding their gender identity or sexual orientation. The absence of these topics may cause queer youth to frequently seek information online or from peers. However, much of the sexual health information online is neither age-appropriate nor medically accurate, and peers may be misinformed. This may result in detrimental impacts to the physical and psychological well being of LGBTQ youth. Future sex education curriculums would greatly benefit from including topics that address queer sexuality and positively influence the development of sexual identity among the LGBTQ demographic. Thus, given the lack of information in sex education curriculums, it would be very difficult for an adolescent to develop a healthy and well informed attitude towards their own developing sexuality. While it could be argued that parents may take on the role of educating their children on sexuality, it is unlikely that they would be able to provide accurate and unbiased information on the topic given the historical lack of well implemented sex education curriculums. The parents themselves are also unlikely to have been formally educated on the topic of sexuality (Brown et al. 2014). Additionally, the existing social taboos around discussion of sex does not encourage a safe and comfortable environment for children to ask questions and engage in open conversation. The remaining sources of information that adolescents commonly turn to are what is told to them by peers and what is shown in mass media. Both of these sources are littered with misinformation and ignorance towards a sensitive topic which may increase the likelihood of poor decision making when faced with a sexual scenario and negatively impact an individual’s future attitudes and mindset regarding sexuality. The Government of Canada website reports that comprehensive sexuality education can contribute to a reduction in rates of adolescent pregnancy and rates of HIV (Government of Canada 2018). Both pregnancy and disease during adolescence can inhibit workforce participation later in life. Therefore, a comprehensive sexual education program should be implemented as part of the health curriculum at schools in order to encourage well informed decision making in sexual matters and provide better opportunities in the future. Health Care Access to Birth Control Having access to safe, affordable birth control options is a big contributor to women’s sexual health and agency. However, female contraceptive options that are commercially available still lack accessibility for all social classes and come at the cost of adverse health effects. Legislative regulations in healthcare make it especially difficult for citizens of lower classes to obtain contraceptives methods and offer few options in the event of a unplanned pregnancy. This holds especially true for women who wish to have sexual agency without becoming pregnant as female contraceptives are controlled by medical institutions, costly without insurance and come with a slew of side effects. Male condoms only offer 84% effectiveness with perfect use and require cooperation from sexual partners (Planned Parenthood 2019), so female contraception is a better option for sexually active women who desire more control and higher reliability. Additionally, virtually all of the aforementioned contraceptive methods require prescription through a medical consultation and is not always covered by insurance. Without insurance coverage, contraceptive options range from $50/month to initial costs of $1300, this is in addition to any fees required for regular consultations, check ups and prescriptions (Planned Parenthood, 2019). This is simply not feasible for women who are unemployed or employed without insurance coverage; this concern is compounded for women in lower social classes, who are also less likely to receive proper sex education and are more vulnerable to unplanned pregnancies (Chandra-Mouli et al. 2014). Access to family planning enables women to choose the timing and spacing of their pregnancies. Fewer pregnancies lead to greater workforce participation for women. With each additional child born to a woman between the ages of 25 and 39, it is estimated that labor participation decreases 10%-15% (Government of Canada 2018). For lower income classes, lower labor participation exacerbates the lack of financial resources and better employment opportunities, which in turn feeds into their inability to attain access better health care. This is especially true for the vulnerable demographic of working class teenage mothers. Adolescent pregnancy can have negative social and economic effects on girls, their families, and their communities. Often, girls who become pregnant have to drop out of school, and girls with little or no education have fewer skills and opportunities to find a job (Government of Canada 2018). The current institutional system has no place for the single, pregnant teenager; and without some form of significant social and financial support from a partner or family, will find themselves trapped in a vicious cycle of poverty and poor health. Alternatively, easy and affordable access to contraceptive options combined with proper sex education will decrease pregnancies, allowing for more labour participation and financial stability. This will serve to increase a woman’s independence and grant access to both better employment and healthcare opportunities. Side Effects of Contraceptives The most common female contraception methods offered to women such as oral contraceptives, intrauterine devices (IUD) and hormonal patches are known to cause adverse health effects, including: irregular bleeding; amenorrhea; weight gain; headache; skin changes; nervousness; stomach pain; nausea; libido changes; dizziness; weakness; depression (Barr 2015). However, many side effects are withheld from websites that are specifically designed to provide information regarding available contraception options. Bedsider.org, a research based non profit, non partisan organization designed to provide a birth control support network for women, features an article titled “ Side effects: The good, the bad, and the temporary” in an attempt to outline the side effects of common birth control options. However, the negative side effects listed are glossed over or presented in a “you may experience this certain side effect but there is no clear relationship” tone (Bedsider 2018). One look at the comment section for this article shows many women frustrated with this kind of disregard, voicing that negative side effects have been downplayed. A user under the name Peg shares her experiences with oral contraceptives, saying “I have had a horrible time with birth control - depression, anxiety, loss of libido from the Pill has really done some damage in my life. Does everyone experience these side effects? No. But that doesn't mean they don't exist and are not important.” Another user by the name of Opal also echoes this sentiment, commenting; “My sister and I both suffered crippling depression when we tried the Pill back in college, and we both struggled with it for months before we figured out what the problem was. If the potential mood-altering side effects of the Pill were more widely reported, we might both have solved our problem a lot sooner! I've looked at the individual entry for the Pill and that information is not there. Please don't talk down to women or try to sweep this stuff under the rug” (Bedsider 2018). In fact, a quick google search online shows countless women sharing similar experiences with contraceptives, many who experienced severe negative side effects that were not listed on the label and whose concerns brushed off by medical professionals as unfounded by evidence. Unfortunately, the reality of medical professionals minimizing women’s pain compared to their male counterparts is a well documented phenomenon (Hoffman and Tarzian 2003) and the impacts of this inequality spans far wider than just reproductive health. But in the context of contraceptive options, if the concerns around current contraceptive options are not heard, there is no push to come up with new ones. These side effects are severe enough to drastically decrease one’s quality of life and it can be emotionally and financially exhausting to test out options in hopes of finding one that is well tolerated. The lack of institutional support in women’s reproductive health also limits sexual agency, as the responsibility of preventing and dealing with pregnancy is almost solely assigned to women. Women may choose to avoid casual sexual encounters in order to create the best chances of avoiding these repercussions, creating an unequal balance of power in sexual agency between the sexes. Reproductive health should invest further resources into developing commercially available male contraception methods that is non surgical in nature, lessening this inequality by dividing up the responsibility of pregnancy prevention. Therefore, having access to contraception that is effective, inexpensive and with minimal negative health impacts, is an important factor in establishing gender equality. With the ability to choose and plan pregnancies, women can have better employment opportunities and improved overall agency in making choices regarding their body and future. Conclusion In conclusion, social institutions such as education and healthcare should revise their reproductive health legislations to more effectively ensure health and equality among its citizens. The current sex education system is outdated and hinders the development of healthy sexuality. A comprehensive sex education curriculum should be implemented in schools, the program include factually correct information regarding safe sex, address the social and emotional consequences of being sexually active and be inclusive of alternative sexual orientations and identities. Sex education programs should be a reliable source of information for youth, build the foundation to making well informed choices that lead to happier and more successful lives in adulthood. Reproductive healthcare would also benefit from providing easy and affordable access to birth control options for women of all social classes. More research should be conducted for contraceptive options, the concerns of side effects need to be taken seriously by healthcare professionals in order to provide improved contraceptive alternatives that minimize adverse impacts on the health of users. Having the ability to plan pregnancies gives women greater autonomy in their life, leading to higher financial independence and promotes gender equality. The reader should note that this paper is written under certain contextual limitations in order to better narrow down the scope of understanding. The educational aspects discussed are Western centric, focusing on the sex education curriculums in North America and not comprehensive of other education systems. The healthcare portion of this paper places heavy focus on the heterosexual definition and understanding of sex and does not fully consider alternative sexualities or alternative definitions of sex. Further research should be conducted on already existing sex education programs that are well implemented successful in promoting good decision making and healthy attitudes towards sexuality. In healthcare, male contraception options should be explored as a way to share the responsibility of pregnancy prevention and even the balance of power between sexes. Social institutions could be a driving force in improving the reproductive health of citizens and should definitely work towards implementing better practices in its legislation. References Barr, Nancy Grossman. 2010. “Managing Adverse Effects of Hormonal Contraceptives.” David Geffen School of Medicine at the University of California, Los Angeles, California. Bedsider. 2018. “Side Effects: The Good, the Bad, the Temporary.” Bedsider, September 1. Blanton, Kayla. 2018. “5 Inaccurate Things You Were Probably Taught in Sex Ed.” Insider Inc, September 18. Brady, S. S. and B. L. Halpern-Felsher. 2007. “Adolescents’ Reported Consequences of Having Oral Sex Versus Vaginal Sex.” PEDIATRICS 119(2):229–36. Brown, Verena W., Susan M. Lamb, Amy M. Perkins, Diana W. Naim, and Suzanne P. Starling. 2014. “Knowledge Regarding Hymens and the Sex Education of Parents.” Journal of Child Sexual Abuse 23(6):674–89. Chandra-Mouli, Venkatraman, Donna R. McCarraher, Sharon J. Phillips, Nancy E. Williamson, and Gwyn Hainsworth. 2014. “Contraception for Adolescents in Low and Middle Income Countries: Needs, Barriers, and Access.” Reproductive Health 11(1). Government of Canada. 2018. “Sexual and Reproductive Health and Rights.” November 12. Guttmacher Institute. 2019. “Parental Involvement in Minors.” Guttmacher Institute. Hoffman, Diane and Anita Tarzian. 2003. “The Girl Who Cried Pain: A Bias Against Women in the Treatment of Pain.” Journal of Law 29:13–27. Hornosty, Jennie Mary and John Germov. 2012. Second Opinion: An Introduction to Health Sociology. Don Mills, Ont.: Oxford University Press. Inderbitzin, Michelle Lee, Kristin Ann Bates, and Randy R. Gainey. 2015. Perspectives on Deviance and Social Control. Los Angeles: SAGE. Joint United Nations Programme on HIV/AIDS, World Health Organization, and UNESCO, Director General. 2018. International Technical Guidance on Sexuality Education: An Evidence-Informed Approach. Paris: United Nations Educational, Scientific and Cultural Organization. Kreager, Derek A. and Jeremy Staff. 2009. “The Sexual Double Standard and Adolescent Peer Acceptance.” Social Psychology Quarterly 72(2):143–64. Lindberg, Laura Duberstein, Isaac Maddow-Zimet, and Heather Boonstra. 2016. “Changes in Adolescents’ Receipt of Sex Education, 2006–2013.” Journal of Adolescent Health 58(6):621–27. Onyehalu, A. S. 1983. “Inadequacy of Sex Knowledge of Adolescents: Implications for Counselling and Sex Education.” Adolescence 18(71):627–30. Planned Parenthood. 2019. “Birth Control.” Planned Parenthood Federation of America Inc.