• Meeting the Standards cases, at the end of each unit, help students revisit and
revise concepts and theories.
• Evidence-based Practice boxes show students how to apply current research to
clinical practice in order to establish action plans that satisfy client preferences and
values.
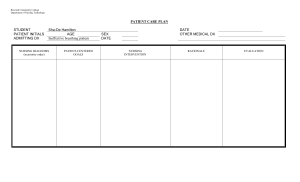
• Concept Map flowcharts represent nursing processes and care plans as well as coach
students through complex topics.
• Step-by-Step Skills boxes set the foundation for clinical competence by explaining
techniques and procedures in detail.
• End-of-chapter Test Your Knowledge questions encourage students to develop
critical thinking skills and prepare for exams.
• Updated samples of model electronic health records give students an overview
of contemporary effective nursing care.
CVR_BERM9793_11_GE_CVR (47.2 mm).indd 1
Kozier & Erb’s
Fundamentals of Nursing
Concepts, Process, and Practice
Berman
Snyder
Frandsen
Available separately for purchase (for the very first time with this edition) is MyLab
Nursing, the teaching and learning platform that empowers instructors to personalize
learning for every student. A supplement on COVID-19 provides guidance on how
nurses should care for patients with COVID-19 and take precautions to keep themselves
and their families safe.
ELEVENTH
EDITION
• Newly added global examples—such as licensure regulations in Nepal and the
United Kingdom and accreditation processes of programs in Denmark, Ireland, and
Taiwan—make the text more relevant than ever to students across the world.
Kozier & Erb’s
• Lifespan Considerations and Client Teaching boxes discuss standards of care and
safety that nurses must uphold while caring for their clients.
Fundamentals of Nursing
Key Features
Concepts, Process, and Practice
Nurses need to not only be aware of the medical, legal, and ethical aspects of nursing
but also be skilled in communicating, teaching, leading, managing, and applying critical
thinking. Now in its eleventh edition, Kozier & Erb’s Fundamentals of Nursing continues to
prepare student nurses to carry out their multifaceted roles in varied healthcare settings.
With its focus on disease prevention, health promotion, holistic care, clinical reasoning,
multiculturalism, ethics, and advocacy, this edition highlights the integral aspects of
contemporary nursing.
GLOBAL
EDITION
GLOB AL
EDITION
GLOBAL
EDITION
This is a special edition of an established title widely used by colleges and
universities throughout the world. Pearson published this exclusive edition
for the benefit of students outside the United States and Canada. If you
purchased this book within the United States or Canada, you should be aware
that it has been imported without the approval of the Publisher or Author.
ELEVENTH EDITION
Audrey Berman • Shirlee Snyder • Geralyn Frandsen
04/02/21 10:30 AM
Kozier & Erb’s
Eleventh Edition
Global Edition
Fundamentals
of Nursing
Concepts, Process, and Practice
Audrey Berman, PhD, RN
Professor, School of Nursing
Samuel Merritt University
Oakland, California
Shirlee J. Snyder, EdD, RN
Retired Dean and Professor, Nursing
Nevada State College
Henderson, Nevada
Geralyn Frandsen, EdD, RN
Professor of Nursing
Maryville University
St. Louis, Missouri
A01_BERM9793_11_GE_FM.indd 1
05/02/2021 17:07
Please contact https://support.pearson.com/getsupport/s/contactsupport with any queries on this content.
_________________________________________________________________________
Pearson Education Limited
KAO Two
KAO Park
Hockham Way
Harlow
Essex
CM17 9SR
United Kingdom
and Associated Companies throughout the world
Visit us on the World Wide Web at: www.pearsonglobaleditions.com
© Pearson Education Limited 2022
The rights of Audrey Berman, Shirlee J. Snyder, and Geralyn Frandsen to be identified as the authors of this work have been asserted by them in
accordance with the Copyright, Designs and Patents Act 1988.
Authorized adaptation from the United States edition, entitled Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice, 11th
Edition, ISBN 9780135428733, by Audrey Berman, Shirlee J. Snyder, and Geralyn Frandsen, published by Pearson Education © 2021.
All rights reserved. This publication is protected by copyright, and permission should be obtained from the publisher prior to any prohibited
reproduction, storage in a retrieval system, or transmission in any form or by any means, electronic, mechanical, photocopying, recording, or
otherwise. For information regarding permissions, request forms and the appropriate contacts within the Pearson Education Global Rights &
Permissions department, please visit www.pearsoned.com/permissions/.
Attributions of third-party content appear on the appropriate page within the text.
PEARSON, ALWAYS LEARNING, and MYLAB are exclusive trademarks owned by Pearson Education, Inc. or its affiliates in the U.S. and/or other
countries.
Notice: Care has been taken to confirm the accuracy of information presented in this book. The authors, editors, and the publisher, however, cannot
accept any responsibility for errors or omissions or for consequences from application of the information in this book and make no warranty, express
or implied, with respect to its contents.
The authors and publisher have exerted every effort to ensure that drug selections and dosages set forth in this text are in accord with current
recommendations and practice at time of publication. However, in view of ongoing research, changes in government regulations, and the constant
flow of information relating to drug therapy and drug reactions, and differences in standards and practices across various regions, the reader is urged
to check the package inserts of all drugs for any change in indications of dosage and for added warnings and precautions. This is particularly
important when the recommended agent is a new and/or infrequently employed drug.
Unless otherwise indicated herein, any third-party trademarks that may appear in this work are the property of their respective owners, and any
references to third-party trademarks, logos or other trade dress are for demonstrative or descriptive purposes only. Such references are not intended
to imply any sponsorship, endorsement, authorization, or promotion of Pearson’s products by the owners of such marks, or any relationship between
the owner and Pearson Education, Inc. or its affiliates, authors, licensees or distributors.
This eBook is a standalone product and may or may not include all assets that were part of the print version. It also does not provide access to other
Pearson digital products like MyLab and Mastering. The publisher reserves the right to remove any material in this eBook at any time.
British Library Cataloguing-in-Publication Data
A catalogue record for this book is available from the British Library
Print ISBN 10: 1-292-35979-X
Print ISBN 13: 978-1-292-35979-3
eBook ISBN 13: 978-1-292-35980-9
Typeset by SPi Global
Dedication
Audrey Berman
dedicates this eleventh edition to her mother, Lotte Henrietta
Julia Sarah Rosenberg Berman Isaacs (1926–2017), who raised two strong daughters
and served as a role model to each of them and also to her grandchildren, Brian and
Jordanna, and great-grandsons, Benjamin and Adam. May her memory be a blessing.
Shirlee Snyder
dedicates this eleventh edition in memory of her older brother,
Ted Snyder, whose legacy is his loving and caring family; to her younger brother, Dan
Snyder, who enjoys his retirement with his wife, children, and grandchildren; to Kelly
Bishop, the best daughter ever and her first great-grandchild, Oliver; to her stepson,
Steven Schnitter; to all the nurses who contribute to the nursing profession; and
always, to her husband, Terry J. Schnitter, for his continual love and support.
Geralyn Frandsen dedicates this eleventh edition to her loving husband and fellow
nursing colleague, Gary. He is always willing to answer questions and provide editorial
support. She also dedicates this edition to her children, Claire and Joe; son-in-law,
John Conroy; and daughter-in-law, Allyson Angelos.
A01_BERM9793_11_GE_FM.indd 3
05/02/2021 17:07
About the Authors
Audrey Berman, PhD, RN
Shirlee J. Snyder, EdD, RN
A San Francisco Bay Area native, Audrey Berman received her BSN from the University
of California–San Francisco and later returned to that campus to obtain her MS in physiologic nursing and her PhD in nursing. Her dissertation was entitled Sailing a Course
Through Chemotherapy: The Experience of Women with Breast Cancer. She worked in oncology at Samuel Merritt Hospital prior to beginning her teaching career in the diploma
program at Samuel Merritt Hospital School of Nursing in 1976. As a faculty member,
she participated in the transition of that program into a baccalaureate degree and in the
development of the master of science and doctor of nursing practice programs. Over the
years, she has taught a variety of medical–surgical nursing courses in the prelicensure
programs on three campuses. She served as the dean of nursing at Samuel Merritt University from 2004 to 2019 and was the 2014–2016 president of the California Association
of Colleges of Nursing.
Dr. Berman has traveled extensively, visiting nursing and healthcare institutions in
Australia, Botswana, Brazil, Finland, Germany, Israel, Japan, Korea, the Philippines, the
Soviet Union, and Spain. She is a senior director of the Bay Area Tumor Institute and
served 3 years as director on the Council on Accreditation of Nurse Anesthesia Educational Programs. She is a member of the American Nurses Association and Sigma Theta
Tau and is a site visitor for the Commission on Collegiate Nursing Education. She has
twice participated as an NCLEX-RN item writer for the National Council of State Boards
of Nursing. She has presented locally, nationally, and internationally on topics related to
nursing education, breast cancer, and technology in healthcare.
Dr. Berman authored the scripts for more than 35 nursing skills videotapes in the
1990s. She was a coauthor of the sixth, seventh, eighth, ninth, tenth, and eleventh editions of Fundamentals of Nursing and the fifth, sixth, seventh, eighth, and ninth editions
of Skills in Clinical Nursing.
Shirlee J. Snyder graduated from Columbia Hospital School of Nursing in Milwaukee,
Wisconsin, and subsequently received a bachelor of science in nursing from the University of Wisconsin–Milwaukee. Because of an interest in cardiac nursing and teaching, she
earned a master of science in nursing with a minor in cardiovascular clinical specialist
and teaching from the University of Alabama in Birmingham. A move to California
resulted in becoming a faculty member at Samuel Merritt Hospital School of Nursing
in Oakland, California. Shirlee was fortunate to be involved in the phasing out of the
diploma and ADN programs and development of a baccalaureate intercollegiate nursing program. She held numerous positions during her 15-year tenure at Samuel Merritt College, including curriculum coordinator, assistant director–instruction, dean of
instruction, and associate dean of the Intercollegiate Nursing Program. She is an associate
professor alumnus at Samuel Merritt College. Her interest and experiences in nursing
education resulted in Shirlee obtaining a doctorate of education focused on curriculum
and instruction from the University of San Francisco.
Dr. Snyder moved to Portland, Oregon, in 1990 and taught in the ADN program at
Portland Community College for 8 years. During this teaching experience she presented
locally and nationally on topics related to using multimedia in the classroom and promoting the success of students of diverse ethnic backgrounds and communities of color.
Another career opportunity in 1998 led her to the Community College of Southern
Nevada in Las Vegas, Nevada, where Dr. Snyder was the nursing program director with
4
A01_BERM9793_11_GE_FM.indd 4
05/02/2021 17:07
Loss, Grieving, and Death
43
LEA R N IN G OU TC OME S
After completing this chapter, you will be able to:
1. Describe types and sources of losses.
2. Discuss selected frameworks for identifying stages of grieving.
3. Identify clinical symptoms of grief.
4. Discuss factors affecting a grief response.
5. Identify measures that facilitate the grieving process.
6. List clinical signs of impending and actual death.
7. Describe the process of helping clients die with dignity.
8. Describe the role of the nurse in working with families or caregivers of dying clients.
9. Describe nursing measures for care of the body after death.
K EY T E RMS
actual loss, 1085
algor mortis, 1101
anticipatory grief, 1086
anticipatory loss, 1086
bereavement, 1086
cerebral death, 1094
closed awareness, 1096
complicated grief, 1086
end-of-life care, 1099
grief, 1086
heart-lung death, 1094
higher brain death, 1094
hospice, 1098
livor mortis, 1101
Introduction
Everyone experiences loss, grieving, and death during his
or her life. Individuals may suffer the loss of valued relationships through life changes, such as moving from one
city to another; separation or divorce; or the death of a parent, spouse, or friend. Individuals may grieve changing
life roles as they watch grown children leave home or they
retire from their lifelong work. Losing valued material
objects through theft or natural disaster can evoke feelings of grief and loss. When individuals’ lives are affected
by civil or national violence, they may grieve the loss of
valued ideals such as safety, freedom, or democracy.
In the clinical setting, the nurse encounters clients who
may experience grief related to declining health, loss of a
body part, terminal illness, or the impending death of self
or a significant other. The nurse may also work with clients in community settings who are grieving losses related
to a personal crisis (e.g., divorce, separation, financial loss)
or disaster (war, earthquakes, or terrorism). Therefore, it is
important for the nurse to understand the significance of
loss and develop the ability to assist clients as they work
through the grieving process.
Nurses may interact with dying clients and their
families or caregivers in a variety of settings, from a fetal
demise (death of an unborn child), to the adolescent victim
of an accident, to the older client who finally succumbs to
a chronic illness. Nurses must recognize the influences
loss, 1085
mortician, 1101
mourning, 1086
mutual pretense, 1096
open awareness, 1096
palliative care, 1099
perceived loss, 1085
persistent vegetative state (PVS),
1094
rigor mortis, 1100
shroud, 1101
undertaker, 1101
on the dying process—legal, ethical, spiritual, biological, psychologic—and be prepared to provide sensitive,
skilled, and supportive care to all those affected.
Loss and Grief
Loss is an actual or potential situation in which something
that is valued is changed or no longer available. Individuals
can experience the loss of body image, a significant other, a
sense of well-being, a job, personal possessions, or beliefs.
Illness and hospitalization often produce losses.
Death is a loss both for the dying individual and for
those who survive. Although death is inevitable, it can
stimulate individuals to grow in their understanding of
themselves and others. Individuals experiencing loss often
search for the meaning of the event, and it is generally
accepted that finding meaning is needed in order for healing to occur. However, individuals can be well adjusted
without searching for meaning, and even those who find
meaning may not see it as an end point but rather as an
ongoing process.
Types and Sources of Loss
There are two general types of loss, actual and perceived.
An actual loss can be recognized by others. A perceived
loss is experienced by an individual but cannot be verified
by others. Psychologic losses are often perceived losses
1085
M43_BERM9793_11_GE_C43.indd 1085
03/02/2021 18:18
1086
Unit 9
●
Promoting Psychosocial Health
because they are not directly verifiable. For example, a
woman who leaves her employment to care for her children at home may perceive a loss of independence and
freedom. Both losses can be anticipatory. An anticipatory
loss is experienced before the loss actually occurs. For
example, a woman whose husband is dying may experience actual loss in anticipation of his death.
Loss can be viewed as situational or developmental.
Losing one’s job, the death of a child, and losing functional
ability because of acute illness or injury are situational
losses. Losses that occur in normal development—such
as the departure of grown children from the home, retirement from a career, and the death of aged parents—are
developmental losses that can, to some extent, be anticipated and prepared for.
There are many sources of loss: (a) loss of an aspect of
oneself—a body part, a physiologic function, or a psychologic attribute; (b) loss of an object external to oneself; (c)
separation from an accustomed environment; and (d) loss
of a loved or valued individual.
Aspect of Self
Losing an aspect of self changes an individual’s body
image, even though the loss may not be obvious. A face
scarred from a burn is generally obvious; loss of part of
the stomach or loss of the ability to feel emotion may not
be as obvious. The degree to which these losses affect an
individual largely depends on the integrity of the individual’s body image.
During old age, changes occur in physical and mental
capabilities. Again the self-image is vulnerable. Old age
is the stage when people may experience many losses:
of employment, of usual activities, of independence, of
health, of friends, and of family.
External Objects
Loss of external objects includes (a) loss of inanimate
objects that have importance to the individual, such as losing money or the burning down of a family’s house; and
(b) loss of animate (live) objects such as pets that provide
love and companionship.
Familiar Environment
Separation from an environment and individuals who provide security can cause a sense of loss. The 6-year-old is
likely to feel loss when first leaving the home environment
to attend school. Immigrants who leave their country to
settle down in another also experience loss and helplessness in the form of culture shock (Arredondo-Dowd, 1981;
Henry, Stiles & Biran, 2005).
Loved Ones
Losing a loved one or valued individual through illness,
divorce, separation, or death can be very disturbing. In
some illnesses (such as Alzheimer’s disease), an individual may undergo personality changes that make friends
and family feel they have lost that individual.
M43_BERM9793_11_GE_C43.indd 1086
Grief, Bereavement, and Mourning
Grief is the total response to the emotional experience
related to loss. Grief is manifested in thoughts, feelings,
and behaviors associated with overwhelming distress or
sorrow. Bereavement is the subjective response experienced by the surviving loved ones. Mourning is the behavioral process through which grief is eventually resolved or
altered; it is often influenced by culture, spiritual beliefs,
and custom. Grief and mourning are experienced not
only by the individual who faces the death of a loved
one but also by the individual who suffers other kinds of
losses. Grieving permits the individual to cope with the
loss gradually and to accept it as part of reality. Grief is a
social process; it is best shared and carried out with the
assistance of others.
Working through one’s grief is important because
bereavement may have potentially devastating effects on
health. Among the symptoms that can accompany grief
are anxiety, depression, weight loss, difficulties in swallowing, vomiting, fatigue, headaches, dizziness, fainting,
blurred vision, skin rashes, excessive sweating, menstrual
disturbances, palpitations, chest pain, and dyspnea. The
grieving and the bereaved may experience alterations in
libido, concentration, and patterns of eating, sleeping,
activity, and communication.
Although bereavement can threaten health, a positive
resolution of the grieving process can enrich the individual with new insights, values, challenges, openness, and
sensitivity. For some, the pain of loss, though diminished,
recurs for the rest of their lives.
Types of Grief Responses
A normal grief reaction may be abbreviated or anticipatory. Abbreviated grief is brief but genuinely felt. This can
occur when the lost object is not significantly important to
the grieving individual or may have been replaced immediately by another, equally esteemed object. Anticipatory
grief is experienced in advance of the event such as the
wife who grieves before her ailing husband dies. A young
individual may grieve before an operation that will leave
a scar. Because many of the normal symptoms of grief
will have already been expressed in anticipation, the
reaction when the loss actually occurs is sometimes quite
abbreviated.
Disenfranchised grief occurs when an individual is
unable to acknowledge the loss to others. Situations
in which this may occur often relate to a socially unacceptable loss that cannot be spoken about, such as suicide, abortion, or giving a child up for adoption. Other
examples include losses of relationships that are socially
unsanctioned and may not be known to others (such as
with extramarital relationships).
Unhealthy grief—that is, pathologic or complicated
grief—exists when the strategies to cope with the loss
are maladaptive and out of proportion or inconsistent with cultural, religious, or age-appropriate norms.
03/02/2021 18:18
Chapter 43
The disorder, referred to by physicians as persistent complex bereavement disorder, may be said to exist if the preoccupation lasts for more than 12 months and leads to
reduced ability to function normally (Boelen, Lenferink,
Nickerson, & Smid, 2018). Many factors can contribute to
complicated grief, including a prior traumatic loss, family
or cultural barriers to the emotional expression of grief,
sudden death, strained relationships between the survivor and the deceased, and lack of adequate support for
the survivor.
Complicated grief may take several forms. Unresolved
or chronic grief is extended in length and severity. The same
signs are expressed as with normal grief, but the bereaved
may also have difficulty expressing the grief, may deny
the loss, or may grieve beyond the expected time. With
inhibited grief, many of the normal symptoms of grief are
suppressed and other effects, including physiologic, are
experienced instead. Delayed grief occurs when feelings
are purposely or subconsciously suppressed until a much
later time. A survivor who appears to be using dangerous
activities as a method to lessen the pain of grieving may
experience exaggerated grief.
Complicated grief after a death may be inferred from
the following data or observations:
•
•
•
The client fails to grieve; for example, a husband does
not cry at, or absents himself from, his wife’s funeral.
The client avoids visiting the grave and refuses to participate in memorial services, even though these practices are a part of the client’s culture.
The client develops persistent guilt and lowered
self-esteem.
TABLE 43.1
•
•
•
●
Loss, Grieving, and Death
1087
Even after a prolonged period, the client continues to
search for the lost loved one. Some may consider suicide to affect reunion.
After the normal period of grief, the client experiences
physical symptoms similar to those of the individual
who died.
The client’s relationships with friends and relatives
worsen following the death.
Many factors contribute to unresolved grief after a death:
•
•
•
•
•
•
Ambivalence (intense feelings, both positive and negative) toward the lost individual
A perceived need to be brave and in control; fear of losing control in front of others
Endurance of multiple losses, such as losing an entire
family, which the bereaved finds too overwhelming to
contemplate
Extremely high emotional value invested in the dead
individual; failure to grieve in this instance helps the
bereaved avoid the reality of the loss
Uncertainty about the loss—for example, when a loved
one is “missing in action”
Lack of support systems.
Stages of Grieving
Many authors have described stages or phases of grieving,
perhaps the most well known of them being Kübler-Ross
(1969), who described five stages: denial, anger, bargaining, depression, and acceptance (Table 43.1). Engel (1964)
identified six stages of grieving: shock and disbelief,
Client Responses and Nursing Implications in Kübler-Ross’s Stages of Grieving
Stage
Behavioral Responses
Nursing Implications
Denial
Refuses to believe that loss is happening.
Is unready to deal with practical problems, such as prosthesis after the loss of a leg. May assume artificial cheerfulness
to prolong denial.
Verbally support client but do not reinforce denial.
Examine your own behavior to ensure that you do not share
in client’s denial.
Anger
Client or family may direct anger at nurse or staff about matters that normally would not bother them.
Help client understand that anger is a normal response to
feelings of loss and powerlessness.
Avoid withdrawal or retaliation; do not take anger personally.
Deal with needs underlying any angry reaction.
Provide structure and continuity to promote feelings of
security.
Allow clients as much control as possible over their lives.
Bargaining
Seeks to bargain to avoid loss (e.g., “let me just live until [a
certain time] and then I will be ready to die”).
Listen attentively, and encourage client to talk to relieve guilt
and irrational fear.
If appropriate, offer spiritual support.
Depression
Grieves over what has happened and what cannot be.
May talk freely (e.g., reviewing past losses such as money or
job), or may withdraw.
Allow client to express sadness.
Communicate nonverbally by sitting quietly without expecting conversation.
Convey caring by touch.
Acceptance
Comes to terms with loss.
May have decreased interest in surroundings and support
people.
May wish to begin making plans (e.g., will, prosthesis,
altered living arrangements).
Help family and friends understand client’s decreased need
to socialize.
Encourage client to participate as much as possible in the
treatment program.
M43_BERM9793_11_GE_C43.indd 1087
03/02/2021 18:18
1088
Unit 9
●
TABLE 43.2
Promoting Psychosocial Health
Engel’s Stages of Grieving
Stage
Behavioral Responses
Shock and disbelief
Refuses to accept loss.
Has stunned feelings.
Accepts the situation intellectually, but denies it emotionally.
Developing awareness
Reality of loss begins to penetrate consciousness.
Anger may be directed at agency, nurses, or others.
Restitution
Conducts rituals of mourning (e.g., funeral).
Resolving the loss
Attempts to deal with painful void.
Still unable to accept new love object to replace lost person or object.
May accept more dependent relationship with support person.
Thinks over and talks about memories of the lost object.
Idealization
Produces image of lost object that is almost devoid of undesirable features.
Represses all negative and hostile feelings toward lost object.
May feel guilty and remorseful about past inconsiderate or unkind acts to lost person.
Unconsciously internalizes admired qualities of lost object.
Reminders of lost object evoke fewer feelings of sadness.
Reinvests feelings in others.
Outcome
Behavior influenced by several factors: importance of lost object as source of support, degree of dependence
on relationship, degree of ambivalence toward lost object, number and nature of other relationships, and number
and nature of previous grief experiences (which tend to be cumulative).
From “Grief and Grieving,” by G. L. Engel, 1964, American Journal of Nursing, 64(9), pp. 93–98. Adapted with permission.
developing awareness, restitution, resolving the loss, idealization, and outcome (Table 43.2). Sanders (1998) described
five phases of bereavement: shock, awareness of loss, conservation/withdrawal, healing, and renewal (Table 43.3).
Whether an individual can integrate the loss and how
this is accomplished are related to that individual’s development, personality, and emotional preparedness. In addition, individuals responding to the very same loss cannot
be expected to follow the same pattern or schedule in
resolving their grief, even while they support each other.
Age
Manifestations of Grief
CHILDHOOD
The nurse assesses the grieving client or family members following a loss to determine the phase or stage
of grieving. Physiologically, the body responds to a
current or anticipated loss with a stress reaction. The
nurse can assess the clinical signs of this response (see
Chapter 42 ).
Manifestations of grief considered normal include verbalization of the loss, crying, sleep disturbance, loss of appetite, and difficulty concentrating. Complicated grieving
may be characterized by extended time of denial, depression, severe physiologic symptoms, or suicidal thoughts.
Factors Influencing the Loss and
Grief Responses
Several factors affect an individual’s response to a loss or
death. These factors include age, significance of the loss,
culture, spiritual beliefs, gender, socioeconomic status, support systems, and the cause of the loss or death. Nurses can
learn general concepts about the influence of these factors
on the grieving experience, but the constellation of these
factors and their significance will vary from client to client.
M43_BERM9793_11_GE_C43.indd 1088
Age affects an individual’s understanding of and reaction
to loss. With familiarity, individuals usually increase their
understanding and acceptance of life, loss, and death.
Individuals rarely experience the loss of loved ones at
regular intervals. As a result, preparation for these experiences is difficult. Other life losses, such as losing a pet, a
friend, youth, or a job, can help individuals anticipate the
more severe loss of death of loved ones by teaching them
successful coping strategies.
Children differ from adults not only in their understanding of loss and death but also in how they are affected by
losing others. Losing a parent or other significant individual can threaten the child’s ability to develop, and regression sometimes results. Assisting the child with the grief
experience includes helping the child regain the normal
continuity and pace of emotional development.
Some adults may assume that children do not have
the same need as an adult to grieve the loss of others.
In situations of crisis and loss, children are sometimes
pushed aside or protected from the pain. They can
feel afraid, abandoned, and lonely. Careful work with
bereaved children is especially necessary because experiencing a loss in childhood can have serious effects later
in life (Figure 43.1 ■).
EARLY AND MIDDLE ADULTHOOD
As individuals grow, they come to experience loss as part of
normal development. By middle age, for example, the loss
of a parent through death seems a more normal occurrence
compared to the death of a younger individual. Coping
with the death of an aged parent has even been viewed as
an essential developmental task of the middle-aged adult.
03/02/2021 18:18
Chapter 43
TABLE 43.3
●
Loss, Grieving, and Death
1089
Sander’s Phases of Bereavement
Phase
Description
Behavioral Responses
Shock
Survivors are left with feelings of confusion, unreality, and disbelief that the loss has occurred. They are
often unable to process normal thought sequences.
Phase may last from a few minutes to many days.
Disbelief
Confusion
Restlessness
Feelings of unreality
Regression and helplessness
State of alarm
Physical symptoms: dryness of mouth and throat,
sighing, weeping, loss of muscular control, uncontrolled trembling, sleep disturbance, loss of appetite
Psychologic symptoms: egocentric phenomenon,
preoccupation with thoughts of the deceased,
psychologic distancing
Awareness of loss
Friends and family resume normal activities. The
bereaved experience the full significance of their loss.
Separation anxiety
Conflicts
Acting out emotional expectations
Prolonged stress
Physical symptoms: yearning, anger, guilt, frustration,
shame, crying, sleep disturbance, fear of death
Psychologic symptoms: oversensitivity, disbelief and
denial, dreaming, sense of presence of the deceased
Conservation/withdrawal
During this phase, survivors feel a need to be alone
to conserve and replenish both physical and emotional energy. The social support available to the
bereaved has decreased, and they may experience
despair and helplessness.
Withdrawal
Despair
Diminished social support
Helplessness
Physical symptoms: weakness, fatigue, need for
more sleep, a weakened immune system
Psychologic symptoms: hibernation or holding pattern, obsessional review, grief work, turning point
Healing: the turning point
During this phase, the bereaved move from distress
about living without their loved one to learning to live
more independently.
Assuming control
Identity restructuring
Relinquishing roles, such as spouse, child, or parent
Physical symptoms: increased energy, sleep restoration, immune system restoration, physical healing
Psychologic symptoms: forgiving, forgetting, searching for meaning, closing of the circle, hope
Renewal
In this phase, survivors move on to a new selfawareness, an acceptance of responsibility for
self, and learning to live without the loved one.
New self-awareness
Acceptance of responsibility
Process of learning to live without
Physical symptoms: functional stability, revitalization,
caring for physical needs
Assumption of responsibility for self-care needs
Psychologic symptoms: living for oneself, loneliness,
anniversary reactions, reaching out to others, time for
the process of bereavement
From Grief: The Mourning After: Dealing with Adult Bereavement, 2nd ed., by Catherine M. Sanders, 1999, New York, NY: John Wiley & Sons, Inc.
The middle-aged adult can experience losses other
than death. For example, losses resulting from impaired
health or body function and losses of various role functions can be difficult for the middle-aged adult. How
the middle-aged adult responds to such losses is influenced by previous experiences with loss, the individual’s
sense of self-esteem, and the strength and availability of
support.
LATE ADULTHOOD
Figure 43.1 ■ Children experience the same emotions of
grief as adults.
Kzenon/123RF.
M43_BERM9793_11_GE_C43.indd 1089
Losses experienced by older adults include loss of health,
mobility, independence, and work role. Limited income
and the need to change one’s living accommodations can
also lead to feelings of loss and grieving.
03/02/2021 18:19
1090
Unit 9
●
Promoting Psychosocial Health
For older adults, the loss through death of a longtime
mate is profound. Although individuals differ in their ability
to deal with such a loss, some research suggests that health
problems for widows decrease and health problems of widowers increase following the death of the spouse (Trevisan
et al., 2016). This may be because the widows are relieved
of the stresses of caring for their spouse while the widowers
have lost the care provided by their spouse, although this
would vary depending on culture and gender norms.
Because the majority of deaths occur among older
adults, and because the number of older adults is increasing
in North America, nurses will need to be especially alert to
the potential problems of older grieving adults. These problems may intensify because the very old grieving individual
may have children who, themselves, are older and possibly
unwell. Some older adults no longer have living peer support people and the nurse may need to fill some of that role.
Significance of the Loss
The significance of a loss depends on the perceptions of
the individual experiencing the loss. One individual may
experience a great sense of loss over a divorce; another
may find it only mildly disrupting. Several factors affect
the significance of the loss:
•
•
•
Importance of the lost individual, object, or function
Degree of change required because of the loss
The individual’s beliefs and values.
For older adults who have already encountered many
losses, an anticipated loss such as their own death may not
be viewed as highly negative, and they may be apathetic
about it instead of reactive. More than fearing death, some
may fear loss of control or becoming a burden.
Culture
Culture influences an individual’s reaction to loss. How
grief is expressed is often determined by the customs of
the culture. Unless an extended family structure exists,
grief is handled by the nuclear family. The death of a family member in a typical nuclear family leaves a great void
because the same few individuals fill most of the roles. In
cultures where several generations and extended family
members either reside in the same household or are physically close, the impact of a family member’s death may
be softened because the roles of the deceased are quickly
filled by other relatives.
Some individuals believe that grief is a private matter to be endured internally. Therefore, feelings tend to
be repressed and may remain unidentified. Individuals
socialized to “be strong” and “make the best of the situation” may not express deep feelings or personal concerns
when they experience a serious loss.
Some cultural groups value social support and the
expression of loss. In some groups, expressions of grief
through wailing, crying, physical prostration, and other
outward demonstrations are acceptable and encouraged.
Other groups may frown on this demonstration as a loss
of control, favoring a more quiet and stoic expression of
grief. In cultural groups where strong kinship ties are
M43_BERM9793_11_GE_C43.indd 1090
maintained, physical and emotional support and assistance are provided by family members.
Spiritual Beliefs
Spiritual beliefs and practices greatly influence both an
individual’s reaction to loss and subsequent behavior.
Most religious groups have practices related to dying, and
these are often important to the client and support people. To provide support at a time of death, nurses need to
understand the client’s particular beliefs and practices (see
Chapter 41 ).
Gender
The gender roles into which many individuals are socialized in the United States affect their reactions at times of
loss. Males are frequently expected to “be strong” and
show very little emotion during grief, whereas it is acceptable for females to show grief by crying. When a wife dies,
the husband, who is the chief mourner, may be expected to
repress his own emotions and to comfort sons and daughters in their grieving.
Gender roles also affect the significance of body image
changes to clients. A man might consider his facial scar to be
“macho,” but a woman might consider hers ugly. Thus the
woman, but not the man, would see the change as a loss.
Socioeconomic Status
The socioeconomic status of an individual often affects the
support system available at the time of a loss. A pension
plan or insurance, for example, can offer an individual who
is widowed or disabled a choice of ways to deal with a loss;
an individual who is confronted with both severe loss and
economic hardship may not be able to cope with either.
Support System
The individuals closest to the grieving individual are often
the first to recognize and provide needed emotional, physical, and functional assistance. However, because many
individuals are uncomfortable or inexperienced in dealing
with losses, the usual support people may instead withdraw from the grieving individual. In addition, support
may be available when the loss is first recognized, but
as the support people return to their usual activities, the
need for ongoing support may be unmet. Sometimes, the
grieving individual is unable or unready to accept support
when offered.
Cause of Loss or Death
Individual and societal views on the cause of a loss or
death may significantly influence the grief response.
Some diseases are considered “clean,” such as cardiovascular disorders, and engender compassion, whereas others may be viewed as repulsive and less unfortunate. A
loss or death beyond the control of those involved may
be more acceptable than one that is preventable, such as a
drunk driving incident. Injuries or deaths that occur during respected activities, such as “in the line of duty,” are
considered honorable, whereas those occurring during
illicit activities may be considered the individual’s just
rewards.
03/02/2021 18:19
Chapter 43
NURSING MANAGEMENT
Assessing
Nursing assessment of the client experiencing a loss
includes three major components: (1) nursing history, (2)
assessment of personal coping resources, and (3) physical
assessment. During the routine health assessment of every
client, the nurse poses questions regarding previous and
current losses. The nature of the loss and the significance
of such losses to the client must be explored.
If there is a current or recent loss, greater detail is
needed in the assessment. Because clients do not always
associate physical ailments with emotional responses such
as grief, the nurse may need to probe to identify possible
loss-related stresses. If the client reports significant losses,
examine how the client usually copes with loss and what
resources are available to assist the client in coping. Data
regarding general health status; other personal stressors;
cultural and spiritual traditions, rituals, and beliefs related
to loss and grieving; and the client’s support network will
be needed to determine a plan of care (see the Assessment
Interview). In assessing the client’s response to a current
loss, the nurse may identify complicated grief, which is
best treated by a healthcare professional expert in assisting such clients. If the nursing assessment reveals severe
physical or psychologic signs and symptoms, the client
should be referred to an appropriate care provider.
Diagnosing
Examples of nursing diagnoses that may be appropriate
for clients who have problems related to death, loss, and
bereavement are grief and potential for complicated grief.
Planning
The overall goals for clients grieving the loss of body function or a body part are to adjust to the changed ability
and to redirect both physical and emotional energy into
●
Loss, Grieving, and Death
1091
rehabilitation. The goals for clients grieving the loss of a
loved one or thing are to remember them without feeling
intense pain and to redirect emotional energy into one’s
own life and adjust to the actual or impending loss.
Planning for Home Care
Clients who have sustained or anticipate a loss may
require ongoing nursing care to assist them in adapting
to the loss. Determining how much and what type of
home care follow-up is needed is based in great part on
the nurse’s knowledge of how the client and family have
coped with previous losses. To prepare for home care, the
nurse reassesses the client’s abilities and needs.
QSEN
Patient-Centered Care: Grieving
CLIENT AND FAMILY: ASSESS
•
•
•
•
•
•
Knowledge: understanding of the implications of the loss
Self-care abilities: skill in caring for self and the client, based on any physical abilities that may have been
altered by the loss
Current coping: stage in the grieving or bereavement
process
Current manifestations of the grief response: adaptive
or maladaptive signs and symptoms; cultural or spiritually based behaviors
Role expectations: perception of the need to return to
work or family roles
Support people’s availability and skills: sensitivity to
the client’s emotional and physical needs; ability to provide an accepting environment
COMMUNITY: ASSESS
•
Resources: availability and familiarity with possible
sources of assistance such as grief support groups, religious or spiritual centers, counseling services, physical
care providers
ASSESSMENT INTERVIEW Loss and Grieving
PREVIOUS LOSS
• Have you ever lost someone or something very important to
you?
• Have you or your family ever moved to a new home or location?
• What was it like for you when you first started school? Moved
away from home? Got a job? Retired?
• Are you physically able to do all the things you used to do?
• Has anyone important or close to you died?
• Do you think there will be any losses in your life in the near future?
If there has been previous grieving:
• Tell me about [the loss]. What was losing like for you?
• Did you have trouble sleeping? Eating? Concentrating?
• What kinds of things did you do to make yourself feel better
when something like that happened?
• Did you observe any spiritual or cultural practices when you had
a loss like that?
• Whom did you turn to if you were very upset about [the loss]?
• How long did it take you to feel more like yourself again and go
back to your usual activities?
M43_BERM9793_11_GE_C43.indd 1091
CURRENT LOSS
• What have you been told about [the loss]? Is there anything
else you would like to know or don’t understand?
• What changes do you think this [illness, surgery, problem] will
cause in your life? What do you think it will be like without [the
lost object]?
• Have you ever experienced a loss like this before?
• Can you think of anything good that might come out of this?
• What kind of help do you think you will need? Who is going to
be helping you with this loss?
• Are there any organizations in your community that might be
able to help?
If there is current grieving:
• Are you having trouble sleeping? Eating? Concentrating?
Breathing?
• Do you have any pain or other new physical problems?
• What are you doing to help you deal with this loss?
• Are you taking any drugs or medications to help you cope with
this loss?
03/02/2021 18:19
1092
Unit 9
●
Promoting Psychosocial Health
Implementing
Besides providing physical comfort, maintaining privacy
and dignity, and promoting independence, the skills
most relevant to situations of loss and grief are those
of effective communication: attentive listening, silence,
open and closed questioning, paraphrasing, clarifying
and reflecting feelings, and summarizing. Less helpful
to clients are responses that give advice and evaluation,
those that interpret and analyze, and those that give
unwarranted reassurance. Communication with grieving clients must relate to their stage of grief. Whether
the client is angry or depressed affects how the client
hears messages and how the nurse interprets the client’s
statements.
Besides using effective communication skills, the
nurse implements a plan to provide client and family
teaching and to help the client work through the stages
of grief.
Facilitating Grief Work
•
•
•
•
•
Explore and respect the client’s and family’s ethnic, cultural, religious, and personal values in their expressions
of grief.
Teach the client or family what to expect in the grief
process, such as that certain thoughts and feelings are
normal (acceptable) and that labile emotions, feelings
of sadness, guilt, anger, fear, and loneliness, will stabilize or lessen over time. Knowing what to expect may
lessen the intensity of some reactions.
Encourage the client to express and share grief with
support people. Sharing feelings reinforces relationships and facilitates the grief process.
Teach family members to encourage the client’s expression of grief, not to push the client to move on or enforce
his or her own expectations of appropriate reactions.
If the client is a child, encourage family members to
be truthful and to allow the child to participate in the
grieving activities of others.
Encourage the client to resume normal activities on
a schedule that promotes physical and psychologic
health. Some clients may try to return to normal activities too quickly. However, a prolonged delay in return
may indicate complicated grieving.
Providing Emotional Support
•
•
•
•
Use silence and personal presence along with techniques of therapeutic communication. These techniques
enhance exploration of feelings and let clients know
that the nurse acknowledges their feelings.
Acknowledge the grief of the client’s family and significant others. Family support persons are part of the
grieving client’s world.
Offer choices that promote client autonomy. Clients
need to have a sense of some control over their own
lives at a time when much control may not be possible.
Provide information regarding how to access community resources: clergy, support groups, and counseling
services.
M43_BERM9793_11_GE_C43.indd 1092
•
Suggest additional sources of information and help
such as:
a. Bereavement Network Europe
b. Hong Kong Family Welfare Society
c. Australian Centre for Grief and Bereavement
d. National Hospice and Palliative Care Organization.
Examples of nursing actions appropriate for clients in various stages of the grief process are shown in the Concept
Map on page 1102.
Evaluating
Evaluating the effectiveness of nursing care of the grieving
client is difficult because of the long-term nature of the life
transition. Criteria for evaluation must be based on goals
set by the client and family.
Client goals and related desired outcomes for a grieving client will depend on the characteristics of the loss and
the client. If outcomes are not achieved, the nurse needs to
explore why the plan was unsuccessful. Such exploration
begins with reassessing the client in case the nursing diagnoses were inappropriate. Examples of questions guiding
the exploration include these:
•
•
•
•
Do the client’s grieving behaviors indicate dysfunctional grieving or another nursing diagnosis?
Is the expected outcome unrealistic for the given time
frame?
Does the client have additional stressors previously not
considered that are affecting grief resolution?
Have nursing orders been implemented consistently,
compassionately, and genuinely?
Dying and Death
The concept of death is developed over time, as the individual grows, experiences various losses, and thinks about
concrete and abstract concepts. In general, humans move
from a childhood belief in death as a temporary state, to
adulthood in which death is accepted as very real but also
very frightening, to older adulthood in which death may
be viewed as more desirable than living with a poor quality of life. Table 43.4 describes some of the specific beliefs
common to different age groups. The nurse’s knowledge of
these developmental stages helps in understanding some
of the client’s responses to a life-threatening situation.
Responses to Dying and Death
The reaction of any individual to another individual’s
impending or real death, or to the potential reality of his
or her own death, depends on all the factors regarding loss
and the development of the concept of death. In spite of
the individual variations in clients’ views about the cause
of death, spiritual beliefs, availability of support systems,
or any other factor, responses tend to cluster in the phases
described by theorists (see Tables 43.1 to 43.3).
Both the client who is dying and the family members
grieve as they recognize the loss. Signs and symptoms for
the nursing diagnosis of grieving include denial, guilt,
03/02/2021 18:19
Chapter 43
TABLE 43.4
●
Loss, Grieving, and Death
Development of the Concept of Death
Age
Beliefs and Attitudes
Infancy–5 years
Does not understand the concept of death.
Infant’s sense of separation forms basis for later understanding of loss and death.
Believes death is reversible, a temporary departure, or sleep.
Emphasizes immobility and inactivity as attributes of death.
5–9 years
Understands that death is final.
Believes own death can be avoided.
Associates death with aggression or violence.
Believes wishes or unrelated actions can be responsible for death.
9–12 years
Understands death as the inevitable end of life.
Begins to understand own mortality, expressed as interest in afterlife or as fear of death.
12–18 years
Fears a lingering death. May fantasize that death can be defied, acting out defiance through reckless behaviors
(e.g., dangerous driving, substance abuse).
Seldom thinks about death, but views it in religious and philosophic terms.
May seem to reach “adult” perception of death but be emotionally unable to accept it.
May still hold concepts from previous developmental stages.
18–45 years
Has attitude toward death influenced by religious and cultural beliefs.
45–65 years
Accepts own mortality.
Encounters death of parents and some peers.
Experiences peaks of death anxiety.
Death anxiety diminishes with emotional well-being.
65+ years
Fears prolonged illness.
Encounters death of family members and peers.
Sees death as having multiple meanings (e.g., freedom from pain, reunion with already deceased family members).
Clinical Alert!
Individuals may use a variety of terms instead of the word died. Serious examples include passed away, gone to a better place, lost, or
free from suffering. Humorous examples include bought the farm,
kicked the bucket, or croaked.
anger, despair, feelings of worthlessness, crying, and inability to concentrate. They may extend to thoughts of suicide,
delusions, and hallucinations. Fear, the feeling of disruption related to an identifiable source (in this case someone’s
death), may also be present. Many of the characteristics
seen in a fearful individual are similar to those of grieving
and include crying, immobility, increased pulse and respirations, dry mouth, anorexia, difficulty sleeping, and nightmares. Hopelessness occurs when the individual perceives
no solutions to a problem—when the death becomes inevitable and the individual cannot see how to move beyond
the death. The nurse may observe apathy, pessimism, and
inability to decide. An individual who perceives a solution
to the problem but does not believe that it is possible to
implement the solution may be said to experience powerlessness. This loss of control may be manifested by anger,
violence, acting out, or depression and passive behavior.
Caregivers, both professionals and support people,
also respond to the impending death. The ongoing responsibilities for providing physical, economic, psychologic,
and social support to a dying client can create extreme
stress for the provider. Often, the time between a terminal diagnosis and when death will occur is unknown and
those supporting the dying client become fatigued and
depressed. There may be anger due to loss of time and
M43_BERM9793_11_GE_C43.indd 1093
1093
resources for personal activities or attention to others.
Within a family that usually functions effectively, death of
a member may cause alterations in usual family processes.
In this situation, the family may be unable to meet the
physical, emotional, or spiritual needs of the members and
may have difficulty communicating and problem-solving.
Professional caregivers, including nurses, may experience stress due to repeated interactions with dying clients and their families. Although most nurses who work
in oncology, hospice, intensive care, emergency, or other
areas where client deaths are common have chosen such
assignments, there can still be a sense of failure when clients die. Just as there must be support systems for grieving clients, there must also be support systems for grieving
healthcare professionals.
Some individuals may think of death as the worst
occurrence in life and do their best to avoid thinking or
talking about death—especially their own. Nurses are not
immune to such attitudes. Nurses who are uncomfortable
with dying clients tend to impede the clients’ attempts to
discuss dying and death in these ways:
•
•
•
•
•
Change the subject (e.g., “Let’s think of something
more cheerful” or “You shouldn’t say things like that”).
Offer false reassurance (e.g., “You are doing very well”).
Deny what is happening (e.g., “You don’t really mean
that” or “You’re going to live until you’re a hundred”).
Be fatalistic (e.g., “Everyone dies sooner or later” or
“What’s meant to be, will be”).
Block discussion (e.g., “I don’t think things are really
that bad”) and convey an attitude that stops further
discussion of the subject.
03/02/2021 18:19
1094
•
•
Unit 9
●
Promoting Psychosocial Health
Be aloof and distant or avoid the client.
“Manage” the client’s care and make the client feel
increasingly dependent and powerless.
Caring for the dying and the bereaved is one of the
nurse’s most complex and challenging responsibilities,
bringing into play all the skills needed for holistic physiologic and psychosocial care. The American Nurses Association position statement Nurses’ Roles and Responsibilities
in Providing Care and Support at the End of Life (2016) states
that the nurse must demonstrate competence and compassion, communication with families, and collaboration with
other members of the healthcare team to provide symptom management and support, and develop realistic plans
of decision-making and care that reflect the client and family wishes. To be effective, nurses must confront their own
attitudes toward loss, death, and dying, because these attitudes will directly affect their ability to provide care.
Definitions of Death
The traditional clinical signs of death were cessation of
the apical pulse, respirations, and blood pressure, also
referred to as heart-lung death. However, since the advent
of artificial means to maintain respirations and blood
circulation, identifying death is more difficult. Another
definition of death is cerebral death or higher brain death,
which occurs when the higher brain center, the cerebral
cortex, is irreversibly destroyed.
Responding to requests from a number of countries to
provide guidance on the formation of leading practices and
health policies that determine the definition of death, the
WHO and the Transplantation Society held a forum, the
focus of which was to discuss death as a biological event.
The legal, ethical, cultural, and religious aspects surrounding death were not considered by the members of the forum
as they strictly based the debate on those scientific and
medical aspects of death that could be observed and measured. After careful deliberation, the forum concluded that
for death to occur, a person must have a permanent loss of
the ability to use all brainstem function and a permanent
incapacity for consciousness. These events may arise from
the permanent ceasing of circulation or from major brain
injury. In their definition of death, the WHO (2012) used
the word permanent to describe a state in which the loss
of function cannot be reversed on its own or restored via
external intervention. This definition was not guided by
terms such as brain death or cardiac death, which could
incorrectly imply the death of that particular organ. Instead,
participants considered the cessation of neurological and
circulatory functions to determine the definition of death.
In cases where artificial life support is used, these
recommendations should guide doctors on when to withdraw treatment. However, the forum agreed that their
report should be the basis for further discussions in the
future about this topic.
These definitions of death are differentiated from a
persistant vegetative state (PVS) in which the client has lost
cognitive function and awareness but respiration and circulation remain. Clients in a PVS may have a variety of facial,
M43_BERM9793_11_GE_C43.indd 1094
eye, and limb movements but do not interact purposefully
with their environment. Depending on the cause of the PVS,
some clients may recover partially or completely.
Death-Related Religious and
Cultural Practices
Cultural and religious traditions and practices associated
with death, dying, and the grieving process help clients
cope with these experiences. Nurses are often present
through the dying process and at the moment of death.
Knowledge of the client’s religious and cultural heritage
helps nurses provide individualized care to clients and
their families, even though they may not participate in the
rituals associated with death.
Some individuals prefer a peaceful death at home
rather than in the hospital. Members of certain ethnic
groups may request that health professionals not reveal
the prognosis to dying clients. They believe the individual’s last days should be free of worry. Other cultures
prefer that a family member (preferably a male in some
cultures) be told the diagnosis so the client can be tactfully
informed by a family member in gradual stages or not be
told at all. Nurses also need to determine whom to call,
and when, as the impending death draws near.
Beliefs and attitudes about death, its cause, and the soul
also vary among cultures. Unnatural deaths, or “bad deaths,”
are sometimes distinguished from “good deaths.” In addition, the death of an individual who has behaved well in life
may be less threatening based on the belief that the individual will be reincarnated into a good life or go to heaven.
Beliefs about preparation of the body, autopsy, organ
donation, cremation, and prolonging life are closely allied
to the client’s religion. Autopsy, for example, may be prohibited, opposed, or discouraged by Eastern Orthodox
religions, Muslims, Jehovah’s Witnesses, and Orthodox
Jews. Some groups, such as Hindus, may oppose autopsy
based on not wanting non-Hindus to touch the body. Some
religions prohibit the removal of body parts or dictate that
all body parts be given appropriate burial. Organ donation
is prohibited by Jehovah’s Witnesses, whereas Buddhists
in America consider it an act of mercy and encourage it.
Cremation is discouraged, opposed, or prohibited by the
Baha’i, Mormon, Eastern Orthodox, Islamic, and Roman
Catholic faiths. Hindus, in contrast, prefer cremation and
cast the ashes in a holy river. Some religions, such as Christian Science, are unlikely to recommend medical means to
prolong life, and the Jewish faith generally opposes prolonging life after irreversible brain damage. In hopeless
illness, Buddhists may permit euthanasia.
Nurses also need to be knowledgeable about the client’s death-related rituals, such as last rites (Figure 43.2 ■),
chanting at the bedside, and other practices, such as
special procedures for washing, dressing, positioning,
shrouding, and attending the dead. Certain cultures retain
their native customs in which family members of the same
sex wash and prepare the body for burial and cremation.
Muslims also customarily turn the body toward Mecca.
In several religions, the body cannot be left unattended
03/02/2021 18:19
Chapter 43
●
Loss, Grieving, and Death
1095
an additional document known as the Physician Orders
for Life-Sustaining Treatment (POLST). The POLST is
signed by both the client or healthcare decision maker and
the primary care provider (physician, physician assistant,
or nurse practitioner), and specifies current preferences
for resuscitation; medical interventions such as comfort
measures, intravenous medications, and noninvasive airway support; and artificial nutrition and hydration. This
document remains with the client when transferred to different levels of care, including to the home, or is available
in an electronic registry. The advantage of the POLST over
an advance directive is that, because it is an order signed
by a healthcare provider, physicians, first responders, hospitals, emergency departments, and others are compelled
to follow it (Stuart, Volandes, & Moulton, 2017). However,
it does not allow for a proxy to be specified. Thus, clients
may wish to have both an advance directive and a POLST.
Do-Not-Resuscitate Orders
Figure 43.2 ■ Catholic clients may request last rites or the sacrament of anointing the sick.
Dennis MacDonald/Alamy Stock Photo.
while awaiting burial and individuals may be hired to sit
with the body if family members do not perform this duty.
Nurses need to ask family members about their preference
and verify who will carry out these activities if performed
at the healthcare facility. The nurse must ensure that any
ritual items present in the healthcare agency are returned
to the family or to the funeral home.
Death-Related Legal Issues
Laws that describe issues involving decisions about death
and dying are constantly changing. These include advance
directives, do not resuscitate, organ donation, and aid in
dying. Nurses must remain knowledgeable about the legal
issues and engage with the healthcare team to advocate
for clients.
Advance Healthcare Directives
In the United States, federal law requires healthcare providers to determine clients’ end-of-life care wishes by inquiring
if the individual has an advance healthcare directive (see
Chapter 3
). This document describes preferences for
future treatment, whether or not the client is currently
unwell. The client specifies one or more individuals who will
serve as their proxy (substitute) in making healthcare decisions should they be unable to do so. Although the majority
of Americans state that it is important to have their endof-life wishes written down, only about 27% have actually
done so, and only 11% have discussed their wishes with their
healthcare provider (Hamel, Wu, & Brodie, 2017b).
For individuals already diagnosed with serious, progressive, or chronic illnesses, almost every U.S. state has
M43_BERM9793_11_GE_C43.indd 1095
Do-not-resuscitate orders, also referred to as DNR, no
code blue, no code, allow natural death (AND), and similar terms, refer to the documentation of the decision to
refrain from cardiopulmonary resuscitation (CPR) should
the client’s heart or breathing cease from an irreversible
underlying condition (also see Chapter 3 ). The decision
should be made with the client and family, when possible,
and always reflect the competent client’s wishes. DNR is
not the same as “do nothing” and decisions to withhold
or withdraw treatment are separate from DNR decisions.
Organ Donation
Both in the U.S. and countries in the EU, the law allows
competent adults to pre-authorize the donation of their
organs for research, education, or transplantation. In the
case of brain death, most organs continue to function normally for some time, although the client may require a
ventilator to control respiratory function.
There are two main approaches to organ donation:
presumed consent and explicit consent. In countries that
follow the explicit consent system, such as the Netherlands, no one is considered a donor unless they voluntarily ‘opt-in’ to become one. However, in the presumed
consent system, everyone is considered a donor unless
they officially ‘opt-out’ of the system.
There have been debates on whether the opt-out
approach is a better method than the opt-in approach
(Willis & Quigley, 2014) since the former tends to yield a
higher percentage of organ donors. For example, Austria,
which follows the opt-out system, has a consent rate of
99.98% (Johnson & Goldstein, 2003; Thaler, 2009).
In countries such as India, organs and tissues of a
person declared legally dead can be donated after permission from the family is attained. The rate of deceased
organ donation is around 0.34 per million population,
which is very low. To mitigate this shortage, an opt-out
system for organ donation has been suggested by several
medical experts (Kaushik, 2009). Nevertheless, this may
not improve deceased organ donation rates because of the
lack of public awareness in India. (Nagar, 2019).
03/02/2021 18:19
1096
Unit 9
●
Promoting Psychosocial Health
Whichever approach a country decides to take, the nurse
should act as an educator. In countries, where there could be
resistance in consenting to organ donation, the nurse is duty
bound to explain the benefits of organ donation and transplantation, clearly state what happens to the organ donor in
case of death, and encourage the public to consider organ
donation after their death. The nurse should also be supportive in the case where relatives of a deceased person are
asked to give consent for organ donation. Here, the nurse
should take into consideration the devastation and grief that
the family is going through and guide them to make the best
decision without pushing them to give consent.
Euthanasia, Aid in Dying
Increasing numbers of U.S. states are implementing
regulations that allow for medical assistance in dying
(MAID), also known as physician-assisted death, end-oflife options, or death with dignity acts. These statutes are
very explicit in delineating who is eligible for this assistance and the process for applying, being approved, and
implementing. MAID, in which the individual self-administers a lethal dose of medications, is not the same as active
euthanasia, in which the lethal dose is administered to the
individual by a physician. In some countries, both MAID
and active euthanasia are illegal, while in others, one or
both may be legal (ProCon.org, 2016).
Each of these death-related legal issues is complex and
is best implemented by a team consisting of individuals
with substantial expertise and experience with the issue.
Nurses need to remain informed on changes in legislation
that may affect their practice but also engage in discussions regarding the ethical aspects of the issues.
NURSING MANAGEMENT
Assessing
To gather a complete database that allows accurate analysis and identification of appropriate nursing diagnoses for
dying clients and their families, the nurse first needs to
recognize the states of awareness manifested by the client
and family members.
In cases of terminal illness, the state of awareness
shared by the dying client and the family affects the
nurse’s ability to communicate freely with clients and
other healthcare team members and to assist in the grieving process. Three types of awareness that have been
described are closed awareness, mutual pretense, and
open awareness (Glaser & Strauss, 1965).
In closed awareness, the client is not made aware of
impending death. The family may choose this because they
do not completely understand why the client is ill or they
believe the client will recover. The primary care provider
may believe it is best not to communicate a diagnosis or
prognosis to the client. Nursing personnel may experience
an ethical problem in this situation. See Chapter 4
for
further information on ethical dilemmas.
With mutual pretense, the client, family, and healthcare personnel know that the prognosis is terminal but
do not talk about it and make an effort not to raise the
subject. Sometimes the client refrains from discussing
M43_BERM9793_11_GE_C43.indd 1096
death to protect the family from distress. The client may
also sense discomfort on the part of healthcare personnel
and therefore not bring up the subject. Mutual pretense
permits the client a degree of privacy and dignity, but it
places a heavy burden on the dying client, who then has
no one in whom to confide.
With open awareness, the client and others know
about the impending death and feel comfortable discussing it, even though it is difficult. This awareness provides
the client an opportunity to finalize affairs and even participate in planning funeral arrangements.
Not all individuals are comfortable with open awareness. Some believe that terminal clients acquire knowledge of
their condition even if they are not directly informed. Others
believe that clients remain unaware of their condition until
the end. It is difficult, however, to distinguish what clients
know from what they will accept or acknowledge.
Nursing care and support for the dying client and family include making an accurate assessment of the physiologic signs of approaching death. Besides signs related
to the client’s specific disease, certain other physical signs
indicate impending death. The four main characteristic
changes are loss of muscle tone, slowing of the circulation,
changes in respirations, and sensory impairment. Box 43.1
lists indications of impending clinical death.
BOX 43.1
Signs of Impending Clinical Death
LOSS OF MUSCLE TONE
• Relaxation of the facial muscles (e.g., the jaw may sag)
• Difficulty speaking
• Difficulty swallowing and gradual loss of the gag reflex
• Decreased activity of the gastrointestinal tract, with subsequent nausea, accumulation of flatus, abdominal distention,
and retention of feces, especially if narcotics or tranquilizers
are being administered
• Possible urinary and rectal incontinence due to decreased
sphincter control
• Diminished body movement
SLOWING OF THE CIRCULATION
• Diminished sensation
• Mottling and cyanosis of the extremities
• Cold skin, first in the feet and later in the hands, ears, and
nose (the client, however, may feel warm if there is a fever)
• Slower and weaker pulse
• Decreased blood pressure
CHANGES IN RESPIRATIONS
• Rapid, shallow, irregular, or abnormally slow respirations
• Noisy breathing, referred to as the death rattle, due to collecting of mucus in the throat
• Mouth breathing, dry oral mucous membranes
SENSORY IMPAIRMENT
• Blurred vision
• Impaired senses of taste and smell
Various levels of consciousness may exist just before
death. Some clients are alert, whereas others are drowsy,
stuporous, or comatose. Hearing is thought to be the last
sense lost.
03/02/2021 18:19
Chapter 43
●
Loss, Grieving, and Death
1097
As death approaches, the nurse assists the family and
other significant individuals to prepare. Depending in part
on knowledge of the client’s state of awareness, the nurse
asks questions that help identify ways to provide support
during the period before and after death. In particular, the
nurse needs to know what the family expects to happen
when the client dies so accurate information can be given
at the appropriate depth. See the Assessment Interview for
sample interview questions. When the family members
know what to expect, they may better support the dying
client and others who are grieving. In addition, they may
make certain decisions about events surrounding the death
such as whether they will want to view the body after death.
nurses will then conduct a full assessment of the home
and care providers’ skills.
Diagnosing
A range of nursing diagnoses, addressing both physiologic and psychosocial needs, can apply to the dying
client, depending on the assessment data. Diagnoses that
may be particularly appropriate for the dying client are
fear, hopelessness, and powerlessness. In addition, caregiver stress and alterations in family processes are common diagnoses for caregivers and family members.
Helping Clients Die with Dignity
Planning
Major goals for dying clients are (a) maintaining physiologic and psychologic comfort and (b) achieving a dignified
and peaceful death, which includes maintaining personal
control and accepting declining health status. Many clinical
agencies and organizations have created documents that
describe the dying client’s rights. When planning care for
dying clients, these guides can be useful guides.
Planning for Home Care
Clients facing death may need help accepting that they have
to depend on others. Some dying clients require only minimal care; others need continuous attention and services.
Clients need help, well in advance of death, in planning for
the period of dependence. They need to consider what will
happen and how and where they would like to die.
In a survey of 4000 Americans, Brazilians, Italians,
and Japanese, 55–71% of adults stated they wished to die
at home, although only about one-half of those believed
that they would die there (Hamel, Wu, & Brodie, 2017a).
A major factor in determining whether an individual will
die in a healthcare facility or at home is the availability
of willing and able caregivers. If the dying client wishes
to be at home, and family or others can provide care to
maintain symptom control, the nurse should facilitate a
referral to outpatient hospice services. Hospice staff and
Implementing
The major nursing responsibility for clients who are dying
is to assist the client to a peaceful death. More specific
responsibilities include the following:
•
•
•
•
To minimize loneliness, fear, and depression
To maintain the client’s sense of security, self-confidence,
dignity, and self-worth
To help the client accept losses
To provide physical comfort.
Nurses need to ensure that the client is treated with dignity,
that is, with honor and respect. Dying clients often feel they
have lost control over their lives and over life itself. Helping
clients die with dignity involves maintaining their humanity, consistent with their values, beliefs, and culture. By introducing options available to the client and significant others,
nurses can restore and support feelings of control. Some
choices that clients can make are the location of care (e.g.,
hospital, home, or hospice facility), times of appointments
with health professionals, activity schedule, use of health
resources, and times of visits from relatives and friends.
Clients want to manage the events preceding death so
they can die peacefully. Nurses can help clients to determine their own physical, psychologic, and social priorities.
Dying individuals often strive for self-fulfillment more
than for self-preservation, and may need to find meaning
in continuing to live if suffering. Part of the nurse’s challenge is to support the client’s will and hope.
Although it is natural for individuals to be uncomfortable discussing death, steps can be taken to make such
discussions easier for both the nurse and the client. Strategies include the following:
•
•
•
Identify your personal feelings about death and how
they may influence interactions with clients. Acknowledge personal fears about death, and discuss them with
a friend or colleague.
Focus on the client’s needs. The client’s fears and beliefs
may differ from the nurse’s. It is important for the nurse
to avoid imposing personal fears and beliefs on the
client or family.
Talk to the client or family members about how the client
usually copes with stress. Clients typically use their usual
coping strategies for dealing with impending death.
ASSESSMENT INTERVIEW The Family of the Dying Client
Ask the spouse, partner, or significant others:
• Have you ever been in a similar situation?
• Would you like to discuss what may happen if and when your
loved one passes away?
• Would you like to ask me anything about the situation?
M43_BERM9793_11_GE_C43.indd 1097
Would you like me to call someone who can stay with you at
this time to support you?
• Would you like to eat or drink something while waiting?
• Is there anything else I can do for you to help you at this time?
•
03/02/2021 18:19
1098
•
•
•
•
Unit 9
●
Promoting Psychosocial Health
For example, if they are usually quiet and reflective, they
may become more quiet and withdrawn when facing terminal illness.
Establish a communication relationship that shows
concern for and commitment to the client. Communication strategies that let the client know you are available
to talk about death include the following:
a. Describe what you see, for example, “You seem
sad. Would you like to talk about what’s happening
to you?”
b. Clarify your concern, for example, “I’d like to know
better how you feel and how I may help you.”
c. Acknowledge the client’s struggle, for example, “It
must be difficult to feel so uncomfortable. I would
like to help you be more comfortable.”
d. Provide a caring touch. Holding the client’s hand
or offering a comforting massage can encourage the
client to verbalize feelings.
Determine what the client knows about the illness and
prognosis.
Respond with honesty and directness to the client’s
questions about death.
Make time to be available to the client to provide
support, listen, and respond.
usually apparent, but emotional and behavioral signs are
often more subtle. A good assessment and ongoing evaluation can help indicate when modifications or changes are
needed.
The principles of hospice care can be carried out in a
variety of settings, the most common being the home, the
hospital, or a nursing home–based unit. Services focus on
symptom control and pain management. Commonly, clients are eligible for hospice care or hospice insurance benefits when certified by a physician to be likely to die within
6 months. Hospice care is always provided by a team of
both health professionals and nonprofessionals to ensure
a full range of care services. The National Hospice and
Palliative Care Organization (2018) reports that more than
1.43 million Medicare beneficiaries access hospice services
each year, representing approximately 48% of all Medicare
deaths. Contrary to popular belief, only about 28% of hospice clients are diagnosed with cancer. The top noncancer
primary diagnoses for those admitted to hospice are cardiac
and circulatory disease, dementia, and respiratory disease.
More than 18,000 nursing personnel in the United
States are nationally certified in one or more of the seven
hospice and palliative care programs (Hospice and Palliative Credentialing Center, 2019).
Hospice and Palliative Care
The hospice movement was founded by the physician
Cecily Saunders in London, England, in 1967. Hospice care
focuses on support and care of the dying client with a life
expectancy of 6 months or less and the family, with the
goal of facilitating a peaceful and dignified death. Hospice
care is based on holistic concepts and emphasizes teambased care to improve quality of life rather than cure, support the client and family through the dying process, and
support the family through bereavement. Assessing the
needs of the client’s family is just as important as caring
for the client who is receiving hospice care (Figure 43.3 ■).
The condition of the client usually deteriorates, and attention needs to be focused on the caregivers to ensure that
they are receiving support and resources as these changes
occur. If the hospice team meets regularly, these needs can
be discussed and interventions initiated. Physical needs are
Figure 43.3 ■ Family members may be closely involved in both
physical and psychologic support of the dying.
Katarzyna Białasiewicz/123RF.
EVIDENCE-BASED PRACTICE
Evidence-Based Practice
What Is the Impact of Palliative Care Consultation Services?
Evidence-Based Practice
In some geographical areas, inpatient hospice bed space is very
limited. One solution to this problem is to provide palliative care
consultative services (PCCS). In this study, PCCS from a team of
physicians, nurses, social workers, psychologists, and chaplains
was provided to 1369 hospital cancer patients in Taiwan over a
6-year period (Wu, Chu, Chen, Ho, & Pan, 2016). Of this number,
about half died in the hospital, one-fourth were discharged, and
one-fourth were transferred to a hospice unit. The group who died
were statistically older, male, and more likely to have lung or liver
cancer. Almost half of those who died already had a DNR order
M43_BERM9793_11_GE_C43.indd 1098
when PCCS began. The patients transferred to the hospice ward
tended to have greater pain, constipation, dyspnea, nausea, vomiting, and delirium.
IMPLICATIONS
The authors of this report state the limitations of the study but also
the benefits of heightened awareness of the characteristics of the
three groups of patients and the outcomes of their care. In order
to advocate for palliative and end-of-life support, nurses need to
establish which groups or characteristics of clients will benefit from
specific services. Studies such as these are needed because the
availability of resources is limited.
03/02/2021 18:19
Chapter 43
Palliative care is described by the World Health Orga-
nization (n.d.) as:
an approach that improves the quality of life of
patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early
identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual. Palliative care:
•
•
•
•
•
•
•
•
provides relief from pain and other distressing
symptoms;
affirms life and regards dying as a normal process;
intends neither to hasten nor postpone death;
integrates the psychological and spiritual aspects
of patient care;
offers a support system to help patients live as
actively as possible until death;
offers a support system to help the family cope
during the patient’s illness and in their own
bereavement;
uses a team approach to address the needs of
patients and their families, including bereavement counselling, if indicated;
will enhance quality of life, and may also positively influence the course of illness;
TABLE 43.5
•
●
Loss, Grieving, and Death
1099
is applicable early in the course of illness, in conjunction with other therapies that are intended to
prolong life, such as chemotherapy or radiation
therapy, and includes those investigations needed
to better understand and manage distressing clinical complications. (para. 1)
Palliative care “attends to the physical, functional, psychologic, practical, and spiritual consequences of a serious
illness. It is a person- and family-centered approach to care,
providing seriously ill people relief from the symptoms and
stress of an illness. Through early integration into the care
plan of seriously ill people, palliative care improves quality of life for both the patient and the family” (National
Consensus Project for Quality Palliative Care, 2018, p. i).
This care may differ from hospice because the client is not
necessarily believed to be imminently dying. Both hospice
and palliative care can include end-of-life care, that is, the
care provided in the final weeks before death.
Meeting the Physiologic Needs of the Dying Client
The physiologic needs of clients who are dying are related to
a slowing of body processes and to homeostatic imbalances.
Interventions include providing personal hygiene measures;
controlling pain; relieving respiratory difficulties; assisting
with movement, nutrition, hydration, and elimination; and
providing measures related to sensory changes (Table 43.5).
Physiologic Needs of Dying Clients
Problem
Nursing Care
Airway clearance
Fowler position: conscious clients
Throat suctioning: conscious clients
Lateral position: unconscious clients
Nasal oxygen for hypoxic clients
Anticholinergic medications may be indicated to help dry secretions
Air hunger
Open windows or use a fan to circulate air
Morphine may be indicated in an acute episode
Bathing and hygiene
Frequent baths and linen changes if diaphoretic
Mouth care as needed for dry mouth
Liberal use of moisturizing creams and lotions for dry skin
Moisture-barrier skin preparations for incontinent clients
Physical mobility
Assist client out of bed periodically, if able
Regularly change client’s position
Support client’s position with pillows, blanket rolls, or towels as needed
Elevate client’s legs when sitting up
Implement pressure injury prevention program and use pressure-relieving surfaces as indicated
Nutrition
Antiemetics or a small amount of an alcoholic beverage to stimulate appetite
Encourage liquid foods as tolerated
Constipation
Dietary fiber as tolerated
Stool softeners or laxatives as needed
Urinary elimination
Skin care in response to incontinence of urine or feces
Bedpan, urinal, or commode chair within easy reach
Call light within reach for assistance onto bedpan or commode
Absorbent pads placed under incontinent client; linen changed as often as needed
Catheterization, if necessary
Keep room as clean and odor free as possible
Sensory and perceptual changes
Check preference for light or dark room
Hearing is not diminished; speak clearly and do not whisper
Touch is diminished, but client will feel pressure of touch
Implement pain management protocol if indicated
M43_BERM9793_11_GE_C43.indd 1099
03/02/2021 18:19
1100
Unit 9
●
Promoting Psychosocial Health
Pain control is essential to enable clients to maintain some quality in their life and their daily activities,
including eating, moving, and sleeping. Many drugs
have been used to control the pain associated with terminal illness: morphine, heroin, methadone, and alcohol. Usually the primary care provider determines the
dosage, but the client’s opinion should be considered;
the client is the one ultimately aware of personal pain
tolerance and fluctuations of internal states. Because
primary care providers usually prescribe dosage ranges
for pain medication, nurses use their own judgment on
the amount and frequency of pain medication in providing client relief. Because of decreased blood circulation, if analgesics cannot be administered orally, they
are given topically, by intravenous infusion, sublingually, or rectally, rather than subcutaneously or intramuscularly. Clients on narcotic pain medications also
require implementation of a protocol to treat opioidinduced constipation. See Chapter 30
for more on
pain management.
Providing Spiritual Support
Spiritual support is of great importance in dealing with
death. Although not all clients identify with a specific
religious faith or belief, most have a need for meaning
in their lives, particularly as they experience a terminal
illness.
The nurse has a responsibility to ensure that the client’s spiritual needs are attended to, either through direct
intervention or by arranging access to individuals who
can provide spiritual care. Nurses need to be aware of
their own comfort with spiritual issues and be clear about
their own ability to interact supportively with the client.
Nurses have an ethical and moral responsibility to not
impose their own religious or spiritual beliefs on a client
but to respond to the client in relation to the client’s own
background and needs. Communication skills are most
important in helping the client articulate needs and in
developing a sense of caring and trust.
Interventions may include facilitating expressions of
feeling, prayer, meditation, reading, and discussion with
clergy or a spiritual adviser. It is important for nurses to
establish an effective interdisciplinary relationship with
spiritual support specialists. For a further discussion of
spiritual issues, see Chapter 41 .
Clinical Alert!
Individuals who have experienced the deaths of multiple individuals
in their lives, such as members of the AIDS community, those serving
in war zones, or victims of natural disasters, do not necessarily feel
the loss or grieve any more or less than those who have experienced
fewer deaths.
Family members should be encouraged to participate
in the physical care of the dying client as much as they
wish to and are able. The nurse can suggest they assist
with bathing, speak or read to the client, and hold hands.
The nurse must not, however, have specific expectations
for family members’ participation. The dying and the
family must be allowed as much privacy as they desire
in order to meet their needs for physical and emotional
intimacy. Those who feel unable to care for or be with the
dying client also require support from the nurse and from
other family members. They should be shown an appropriate waiting area if they wish to remain nearby.
Sometimes, it seems as if the client is “holding on,”
possibly out of concern for the family not being ready for
the client to die. It may be therapeutic for both the client
and the family for the family to verbally give permission
to the client to “let go,” to die when he or she is ready.
This is a painful process, and the nurse must be prepared
to encourage and support the family through saying their
last good-byes.
After the client dies, the family should be encouraged
to view the body (with or without a nurse present or after
preparation by the funeral home), because this has been
shown to facilitate the grieving process. They may wish to
clip a lock of hair as a remembrance. Children should be
included in the events surrounding the death if they wish
to. If the family was not present prior to the death, they may
have questions about events surrounding the final hours
that the nurse should answer sensitively and honestly.
Clinical Alert!
Even when the client appears unresponsive, the nurse must always
provide high-quality care. Though the client is dying, and actions may
seem futile, the client deserves respect and appropriate interventions. Nurses do not provide less care to dying clients, just different
care.
Supporting the Family
Postmortem Care
The most important aspects of providing support to the
family members of a dying client involve using therapeutic communication to facilitate their expression of feelings.
When nothing can reverse the inevitable dying process,
the nurse can provide an empathetic and caring presence.
The nurse also serves as a teacher, explaining what is happening and what the family can expect. Due to the stress
of moving through the grieving process, family members
may not absorb what they are told and may need to have
information provided repeatedly. The nurse must have a
calm and patient demeanor.
Rigor mortis is the stiffening of the body that occurs about
2 to 4 hours after death. Rigor mortis starts in the involuntary muscles (heart, bladder, and so on), then progresses
to the head, neck, and trunk, and finally reaches the
extremities.
Because the deceased’s family often wants to view the
body, and because it is important that the deceased appear
natural and comfortable, nurses need to place the body in
an anatomic position, place dentures in the mouth, and
close the eyes and mouth before rigor mortis sets in. Rigor
mortis usually leaves the body about 96 hours after death.
M43_BERM9793_11_GE_C43.indd 1100
03/02/2021 18:19
Chapter 43
Algor mortis is the gradual decrease of the body’s temperature after death. When blood circulation terminates and
the hypothalamus ceases to function, body temperature falls
about 1°C (1.8°F) per hour until it reaches room temperature. Simultaneously, the skin loses its elasticity and can easily be broken when removing dressings and adhesive tape.
After blood circulation has ceased, the red blood cells
break down, releasing hemoglobin, which discolors the
surrounding tissues. This discoloration, referred to as livor
mortis, appears in the lowermost or dependent areas of
the body.
Tissues after death become soft and eventually liquefied by bacterial fermentation. The hotter the temperature,
the more rapid the change. Therefore, bodies are often
stored in cool places to delay this process. Embalming
prevents the process through injection of chemicals into
the body to destroy the bacteria.
Nursing personnel may be responsible for care of a
body after death. Postmortem care should be carried out
according to the policy of the hospital or agency. Because
care of the body may be influenced by religious law, the
nurse should check the client’s religion and make every
attempt to comply. If the deceased’s family or friends
wish to view the body, make the environment clean and
pleasant and make the body appear natural and comfortable. All equipment, soiled linen, and supplies should be
removed from the bedside. Some agencies require that all
tubes in the body remain in place; in other agencies, tubes
may be cut to within 2.5 cm (1 in.) of the skin and taped in
place; in others, all tubes may be removed.
Normally the body is placed in a supine position
with the arms either at the sides, palms down, or across
the abdomen. One pillow is placed under the head and
shoulders to prevent blood from discoloring the face by
settling in it. The eyelids are closed and held in place for a
few seconds so they remain closed. Dentures are usually
inserted to help give the face a natural appearance. The
mouth is then closed.
Soiled areas of the body are washed; however, a
complete bath is not necessary, because the body will be
●
Loss, Grieving, and Death
1101
washed by the mortician (also referred to as an undertaker),
a professional trained in care of the dead. Absorbent pads
are placed under the buttocks to take up any feces and
urine released because of relaxation of the sphincter muscles. A clean gown is placed on the client, and the hair is
arranged. All jewelry is removed, except a wedding band
in some instances, which is taped to the finger. The top bed
linens are adjusted neatly to cover the client to the shoulders. Soft lighting and chairs are provided for the family.
In the hospital, after the body has been viewed by the
family, the deceased’s wrist identification tag is left on
and additional identification tags are applied. The body
is wrapped in a shroud, a large piece of plastic or cotton
material used to enclose a body after death. Identification
is then applied to the outside of the shroud. The body is
taken to the morgue if arrangements have not been made
to have a mortician pick it up from the client’s room.
Nurses have a duty to handle the deceased with dignity
and to label the corpse appropriately. Mishandling can
cause emotional distress to survivors. Mislabeling can create legal problems if the body is inappropriately identified
and prepared incorrectly for burial or a funeral.
Evaluating
To evaluate the achievement of client goals, the nurse collects data in accordance with the desired outcomes established in the planning phase. Evaluation activities may
include the following:
•
•
•
Listening to the client’s reports of feeling in control of
the environment surrounding death, such as control
over pain relief, visitation of family and support people, or treatment plans
Observing the client’s relationship with significant
others
Listening to the client’s thoughts and feelings related to
hopelessness or powerlessness.
Some of the special needs of older adults and their
families during death and dying are found in Lifespan
Considerations.
LIFESPAN CONSIDERATIONS Responses to Death
CHILDREN
• Children’s response to death or loss depends on the messages
they get from adults and others around them as well as their
understanding of death. When adults are able to cope effectively with a death, they are more likely to be able to support
children through the process.
• As children develop, they will “reprocess” their grieving around
a loss or death. Preschoolers who have lost a parent, for
example, often reconceptualize their understanding of that loss
when they reach school age and adolescence and have greater
cognitive and emotional skills. The same process occurs with
parents who have lost a child to death; as the years pass and
the child “would have been in first grade,” for example, parents
must cope with the added dimensions of the loss.
M43_BERM9793_11_GE_C43.indd 1101
OLDER ADULTS
Older adults who are dying often have a need to know that their lives
had meaning. An excellent way to assure them of this is to make recordings of them telling stories of their lives. This gives the client a sense of
value and worth and also lets him or her know that family members and
friends will also benefit from it. Doing this with children and grandchildren
often eases communication and support during this difficult time.
Caregivers need ongoing support and teaching as the dying client’s condition changes. Some of these needs are teaching:
• Ways to feed the client when swallowing becomes difficult
• Ways to transfer and reposition the client safely
• Ways to communicate if verbalization becomes more difficult
• Nonpharmacologic methods of pain control
• Comfort measures, such as frequent oral care and frequent
repositioning
• When and whom to call if the client’s condition changes.
03/02/2021 18:19
1102
Unit 9
●
Promoting Psychosocial Health
Critical Thinking Checkpoint
Mrs. Govinda, 75, was admitted to the hospital after repeated episodes
of pneumonia. Despite aggressive antibiotic therapy, her condition
rapidly deteriorated and she died unexpectedly 1 week after being
admitted to the hospital. Mrs. Govinda’s oldest son, who lived nearby
and frequently cared for his mother, arranged for the funeral and
visited with relatives. He misses his mother and cries occasionally
but managed to return to work the following week. The youngest son
had difficulty attending the funeral, has been unable to sleep or eat,
cannot concentrate at work, and cannot believe that his mother is
dead. The middle son did not weep at the funeral and had little to say
to his brothers or other relatives. He returned home to another state
but has remained distant. He is back to work but feels very fatigued
and apathetic.
1. From the data provided, describe the phase of bereavement
being experienced by each of the three surviving sons.
2. What factors may have affected how each of the sons reacted to
the death of their mother?
3. What cues, other than physical signs, might have indicated
that Mrs. Govinda was dying, even though her death was
unexpected?
4. With the diagnosis of pneumonia, a respiratory infection, what
physiologic (palliative) needs might she have had?
5. How might your own feelings about death affect the care you
provide to the dying client?
Answers to Critical Thinking Checkpoint questions are available on the faculty resources site. Please
consult with your instructor.
CONCEPT MAP
The Grieving Client
Denial Stage
Anger Stage
Example Behavior
Example Behavior
Wife of dying client states:
"Next year, we are going to
move to a warmer climate."
Teenage girl
with a spinal
cord injury
yells at all
caregivers.
Possible
nursing
intervention
Possible
nursing
intervention
Possible nursing
intervention
Ensure other
individuals
are available
to provide
support
to the wife
(clergy,
family).
Nurse; "Have
you thought
about what
might happen
if he does
not get well
again?"
Provide accurate explanation of
the client’s condition, e.g., "His
heart is no longer able to keep
his blood pressure up."
Shock Stage
Idealization Stage
Example Behavior
The son of an 89-year-old
mother who has just died
tells everyone he sees
about how wonderful she
always was and what
a terrible son he was to her.
Possible
nursing
intervention
Example Behavior
Parents of a stillborn
baby cry continuously,
cannot eat, experience
chest pains.
Possible nursing
intervention
Possible
nursing
intervention
Anticipate
her anger
and present
a calm
demeanor.
Reassure her that
her reactions are
part of the process
of learning to
accept her loss.
Remind him that
all individuals
have both good
and bad in them.
Possible nursing
intervention
Possible nursing
intervention
Use silence
and presence
to demonstrate
acceptance.
Possible
nursing
intervention
Encourage her
to talk about
her feelings:
"You are really
angry. Tell me
about it."
Consider
requesting
medical
treatment if
their own
health becomes
at risk.
Note: All nursing actions must be individualized to the client and the stage of the grieving process.
M43_BERM9793_11_GE_C43.indd 1102
03/02/2021 18:19
Chapter 43
●
Loss, Grieving, and Death
1103
Chapter 43 Review
CHAPTER HIGHLIGHTS
• Nurses help clients deal with many losses, including loss of body
•
•
•
•
image, a loved one, a sense of well-being, or a job.
Loss, especially loss of a loved one or a valued body part, can be
viewed as either a situational or a developmental loss and as either
an actual or a perceived loss (both of which can be anticipatory).
Grieving is a normal, subjective emotional response to loss; it is
essential for mental and physical health. Grieving allows the bereaved
individual to cope with loss gradually and to accept it as a reality.
Knowledge of different stages or phases of grieving and factors
that influence the loss reaction can help the nurse understand the
responses and needs of clients.
How an individual deals with loss is closely related to the individual’s
age, culture, spiritual beliefs, gender, socioeconomic status, support systems, and the significance and cause of the loss or death.
• Caring for the dying and the bereaved is one of the nurse’s most
complex and challenging responsibilities.
• Death-related legal issues include advance healthcare directives,
do-not-resuscitate orders, organ donation, and euthanasia, aid in
dying.
• Nurses’ attitudes about death and dying directly affect their ability
to provide care.
• Nurses must consider the entire family as requiring care in situations
involving loss, especially death.
• Dying clients require open communication, physical help, and emotional and spiritual support to ensure a peaceful and dignified death.
They need to maintain a sense of control in managing the events
preceding death.
TEST YOUR KNOWLEDGE
1. Which of the following may be considered normal or “healthy”
types of grief? Select all that apply.
1. Abbreviated grief
2. Anticipatory grief
3. Disenfranchised grief
4. Complicated grief
5. Unresolved grief
6. Inhibited grief
2. The family of a client who has just died wants to spend time with
the client. What should the nurse do to prepare the client for the
family? Select all that apply.
1. Check the client’s religion to make sure care is in compliance
with religious expectations.
2. Remove equipment from the room.
3. Permit the family to view the client before postmortem care
is done.
4. Change the linen.
5. Place the client in a natural body position.
3. The shift changed while the nursing staff was waiting for the
adult children of a deceased client to arrive. The oncoming
nurse has never met the family. Which initial greeting is most
appropriate?
1. “I’m very sorry for your loss.”
2. “I’ll take you in to view the body.”
3. “I didn’t know your father but I am sure he was a wonderful
person.”
4. “How long will you want to stay with your father?”
4. At which age does a child begin to accept that he or she will
someday die?
1. Less than 5 years old
2. 5–9 years old
3. 9–12 years old
4. 12–18 years old
M43_BERM9793_11_GE_C43.indd 1103
5. An 82-year-old man has been told by his primary care provider
that it is no longer safe for him to drive a car. Which statement
by the client would indicate beginning positive adaptation to this
loss?
1. “I told the doctor I would stop driving, but I am not going
to yet.”
2. “I always knew this day would come, but I hoped it wouldn’t
be now.”
3. “What does he know? I’m a better driver than he will
ever be.”
4. “Well, at least I have friends and family who can take
me places.”
6. When asked to sign the permission form for surgical removal of
a large but noncancerous lesion on her face, the client begins to
cry. Which is the most appropriate response?
1. “Tell me what it means to you to have this surgery.”
2. “You must be very glad to be having this lesion removed.”
3. “I cry when I am happy or relieved sometimes, too.”
4. “Isn’t it wonderful that the lesion is not cancer?”
7. A nurse receives an advance health care directive to include in
the medical record upon admitting a client to the hospital. The
directive is witnessed by two of the client’s three children. How
does the nurse interpret this information?
1. This advance directive may not be legal as children cannot
witness advance directives in some states.
2. Having the children’s signatures on the advance directive
is good because it indicates they agree with the client’s
wishes.
3. The advance directive cannot be honored unless it is
witnessed by all three children.
4. In order to be valid, the advance directive must be witnessed
by the client’s physician.
03/02/2021 18:19
1104
Unit 9
●
Promoting Psychosocial Health
8. The nurse is caring for a family in a shelter 2 days after the loss
of their home due to a fire. The fire caused minor burns to several members of the family but no life-threatening conditions.
Which is the most important assessment data for the nurse to
gather at this time?
1. Availability of insurance coverage for rebuilding the house
2. Family members’ understanding of the extent of their physical injuries
3. Psychologic support resources available from friends or
other sources
4. Family members’ grief responses and coping behaviors
9. A client who is in the terminal phases of a debilitating muscular
disease tells his wife that he believes the health care team has
“failed” and “given up” on him and “aren’t trying as hard.” What
does the nurse caring for this client realize?
1. This idea of abandonment is unfounded.
2. This is a common fear in the terminally ill client.
3. When clients become terminal, physician care is no longer
necessary.
4. Clients who feel this way are in denial of the facts of their care.
10. In working with a dying client, the nurse demonstrates assisting
the client to die with dignity when performing which action?
1. Allows the client to make as many decisions about care as
is possible
2. Shares with the client the nurse’s own views about life after
death
3. Avoids talking about dying and focuses on the present
4. Relieves the client of as much responsibility for self-care as
is possible
See Answers to Test Your Knowledge in Appendix A.
READINGS AND REFERENCES
Suggested Readings
The American Nurses Association publishes position statements on topics of critical importance to nurses related
to death and dying. Examples include Nurses’ roles
and responsibilities in providing care and support at
the end of life; euthanasia, assisted suicide, and aid in
dying; nursing care and do not resuscitate (DNR) and
allow natural death (AND) decisions; and nutrition and
hydration at the end of life. Retrieved from https://www
.nursingworld.org/practice-policy/nursing-excellence/
official-position-statements/
Related Research
Fuchs, L., Anstey, M., Feng, M., Toledano, R., Kogan, S.,
Howell, M. D. . . . Novack, V. (2017). Quantifying the
mortality impact of do-not-resuscitate orders in the ICU.
Critical Care Medicine, 45, 1019–1027. doi:10.1097/
CCM.0000000000002312
References
American Nurses Association. (2016). Nurses’ roles and
responsibilities in providing care and support at the end of
life. Retrieved from https://www.nursingworld.org/practicepolicy/nursing-excellence/official-position-statements/id/
nurses-roles-and-responsibilities-in-providing-care-andsupport-at-the-end-of-life
Arredondo-Dowd, P. M. (1981). Personal Loss and Grief as a
Result of Immigration. Personnel and Guidance Journal.
Retrieved from https://doi.org/10.1002/j.2164-4918.1981
.tb00573.x
Boelen, P. A., Lenferink, L. I. M., Nickerson, A., & Smid, G. E.
(2018). Evaluation of the factor structure, prevalence,
and validity of disturbed grief in DSM-5 and ICD-11.
Journal of Affective Disorders, 240, 79–87. doi:10.1016/j.
jad.2018.07.041
Citerio, G., & Murphy, P. G. (2015). Brain death the European
perspective. Seminars in Neurology, 35(02), 139–144.
Engel, G. L. (1964). Grief and grieving. American Journal of
Nursing, 64(9), 93–98.
European Council. (2020). More Donors and Transplantations
to Save Lives. Retrieved from https://www.coe.int/en/web/
human-rights-channel/organ-donation
Glaser, B., & Strauss, A. (1965). Awareness of dying. Chicago,
IL: Aldine.
Hamel, L., Wu, B., & Brodie, M. (2017a). Views and experiences with end-of-life medical care in Japan, Italy, the
United States, and Brazil: A cross-country survey.
Retrieved from http://www.kff.org/other/report/views-andexperiences-with-end-of-life-medical-care-in-japan-italythe-united-states-and-brazil-a-cross-country-survey
M43_BERM9793_11_GE_C43.indd 1104
Hamel, L., Wu, B., & Brodie, M. (2017b). Views and experiences with end-of-life medical care in the U.S. Retrieved
from http://files.kff.org/attachment/Report-Views-andExperiences-with-End-of-Life-Medical-Care-in-the-US
Henry, H. M., Stiles, W. B., & Biran, M. W. (2005). Loss and
mourning in immigration: Using the assimilation model to
assess continuing bonds with native culture. Counselling
Psychology Quarterly, 18(2): 109–119. Retrieved from
https://www.researchgate.net/deref/http%3A%2F%2Fdx
.doi.org%2F10.1080%2F09515070500136819
Hospice and Palliative Credentialing Center. (2019). CHPN®
candidate handbook. Retrieved from http://documents.
goamp.com/Publications/candidateHandbooks/HPCCCHPN-Handbook.pdf
Johnson, E. J. & Goldstein, D. (2003). Do defaults save lives?
Science, 302. doi:10.1126/science.1091721
Kaushik, J. (2009). Organ Transplant and Presumed Consent:
Towards an “Opting-out” System. Indian Journal of Medical
Ethics, 6(3), 149–152. Retrieved from https://doi.org/
10.20529/ijme.2009.047
Kübler-Ross, E. (1969). On death and dying. New York, NY:
Macmillan.
Nagar, D. (2019). An opt-out model for organ donation.
Deccan Herald. Retrieved from https://www.deccanherald
.com/opinion/panorama/an-opt-out-model-for-organdonation-763526.html
National Consensus Project for Quality Palliative Care.
(2018). Clinical practice guidelines for quality palliative
care (4th ed.). Retrieved from https://www.nationalcoalitionhpc.org/wp-content/uploads/2018/10/NCHPCNCPGuidelines_4thED_web_FINAL.pdf
National Hospice and Palliative Care Organization. (2018).
NHPCO facts and figures: Hospice care in America.
Retrieved from https://www.nhpco.org/sites/default/files/
public/Statistics_Research/2017_Facts_Figures.pdf
ProCon.org. (2016). Euthanasia & physician-assisted suicide
(PAS) around the world: Legal status in 28 countries from
Australia to Uruguay. Retrieved from http://euthanasia
.procon.org/view.resource.php?resourceID=000136
Sanders, C. M. (1998). Grief: The mourning after: Dealing with
adult bereavement (2nd ed.). New York, NY: John Wiley
& Sons.
Stuart, B., Volandes, A., & Moulton, B. W. (2017). Advance
care planning: Ensuring patients’ preferences govern the
care they receive. Generations, 41(1), 31–36.
Thaler, R. (2009). Opting in vs Opting Out. The New York
Times. September 26, 2009. Retrieved from https://www
.nytimes.com/2009/09/27/business/economy/27view.html
Trevisan, C., Veronese, N., Maggi, S., Baggio, G., De Rui, M.,
Bolzetta, F., . . . Sergi, G. (2016). Marital status and frailty
in older people: Gender differences in the Progetto Veneto
Anziani longitudinal study. Journal of Women’s Health,
25(6), 630–637. doi:10.1089/jwh.2015.5592
Willis, B. H., & Quigley, M. (2014). Opt-out Organ Donation:
On evidence and Public Policy. Journal of the Royal Society
of Public Medicine, 107(2), 56–60. Retrieved from https://
dx.doi.org/10.1177%2F0141076813507707
World Health Organization. (2012). International Guidelines for
the Determination of Death – Phase 1. May 30–31, 2012.
Montreal. Canadian Blood Services. Retrieved from https://
www.who.int/patientsafety/montreal-forum-report.pdf
World Health Organization. (n.d.). WHO definition of palliative
care. Retrieved from http://www.who.int/cancer/palliative/
definition/en
Wu, L., Chu, C., Chen, Y., Ho, C., & Pan, H. (2016). Relationship between palliative care consultation service and endof-life outcomes. Supportive Care in Cancer, 24, 53–60.
doi:10.1007/s00520-015-2741-6
Selected Bibliography
Annas, G. J., & Grodin, M. A. (2017). Frozen ethics: Melting
the boundaries between medical treatment and organ procurement. American Journal of Bioethics, 17(5), 22–24.
doi:10.1080/15265161.2017.1299252
Balch, B. (2017). Death by lethal prescription: A right for older
people—or their duty? Generations, 41(1), 42–46.
Barbus, A. J. (1975). The dying person’s bill of rights. Created at the Terminally Ill Patient and the Helping Person
Workshop, Lansing, MI, South Western Michigan Inservice
Education Council.
Carter, L. (2016). Understanding our role in bereavement. International Journal of Childbirth Education, 31(4), 28–30.
Chung, G., Yoon, J., Rasinski, K., & Curlin, F. (2016). US
Physicians’ opinions about distinctions between withdrawing and withholding life-sustaining treatment. Journal
of Religion & Health, 55, 1596–1606. doi:10.1007/
s10943-015-0171-x
Coombs Lee, B. (2017). Medical aid in dying: The cornerstone
of patient-centered care. Generations, 41(1), 39–41.
Corr, C. A., Corr, D. M., & Doka, K. J. (2019). Death & dying,
life & living (8th ed.). Boston, MA: Cengage.
Dalle Ave, A. L., & Bernat, J. L. (2018). Uncontrolled donation after circulatory determination of death: A systematic
ethical analysis. Journal of Intensive Care Medicine, 33,
624–634. doi:10.1177/0885066616682200
Dickinson, G., & Leming, M. (Eds.). (2017). Annual editions:
Dying, death, and bereavement (15th ed.). Boston, MA:
McGraw-Hill.
Fahlberg, B., Foronda, C., & Baptiste, D. (2016). Cultural
humility: The key to patient/family partnerships for making
difficult decisions. Nursing, 46(9), 14–16. doi:10.1097/01.
NURSE.0000490221.61685.e1
03/02/2021 18:19
Chapter 43
Harris, D. G., & Colombo, C. J. (2017). The road to unintended consequences is paved with good intentions.
Critical Care Medicine, 45, 1100–1101. doi:10.1097/
CCM.0000000000002394
Iocovozzi, D. D. S. (2010). Sooner or later: Restoring sanity to
your end-of-life care. Bloomington, IN: Pen and Publish.
Kübler-Ross, E. (1974). Questions and answers on death and
dying. New York, NY: Macmillan.
Kübler-Ross, E. (1975). Death: The final stage of growth.
Englewood Cliffs, NJ: Prentice Hall.
Kübler-Ross, E. (1978). To live until we say good-bye. Englewood Cliffs, NJ: Prentice Hall.
Malgaroli, M., Maccallum, F., & Bonanno, G. A. (2018).
Symptoms of persistent complex bereavement disorder,
depression, and PTSD in a conjugally bereaved sample:
A network analysis. Psychological Medicine, 48(14),
2439–2448. doi:10.1017/S0033291718001769
Milne, V., Doig, C., & Taylor, M. (2017). Combining
organ donation and medical assistance in death:
Considering the ethical questions. Retrieved
from http://healthydebate.ca/2017/05/topic/
organ-donation-medical-assistance-death
Moorlock, G., Ives, J., Bramhall, S., & Draper, H. (2016).
Should we reject donated organs on moral grounds
or permit allocation using non-medical criteria?
M43_BERM9793_11_GE_C43.indd 1105
A qualitative study. Bioethics, 30, 282–292. doi:10.1111/
bioe.12169
Murray, K. (2016). Essentials in hospice and palliative care: A
practical resource for every nurse. Victoria, Canada: Life
and Death Matters.
National Institute on Aging. (2016). End-of-life: Helping with
comfort and care. Retrieved from http://www.elderguru.
com/wp-content/uploads/2016/09/end-of-life-helpingwith-comfort-and-care.pdf
Palmer, M., Saviet, M., & Tourish, J. (2016). Understanding
and supporting grieving adolescents and young adults.
Pediatric Nursing, 42(6), 275–281.
Petrillo, L. A., Dzeng, E., Harrison, K. L., Forbes, L., Scribner,
B., & Koenig, B. A. (2017). How California prepared for
implementation of physician-assisted death: A primer.
American Journal of Public Health, 107(6), 883–888.
doi:10.2105/AJPH.2017.303755
Rando, T. A. (2000). Clinical dimensions of anticipatory mourning: Theory and practice in working with the dying, their
loved ones, and their caregivers. Champaign, IL: Research
Press.
Rodríguez-Arias, D., Wilkinson, D., & Youngner, S. (2017). How
can you be transparent about labeling the living as dead?
American Journal of Bioethics, 17(5), 24–25. doi:10.1080/1
5265161.2017.1299243
●
Loss, Grieving, and Death
1105
Sajid, M. I. (2016). Autopsy in Islam: Considerations for
deceased Muslims and their families currently and in the
future. American Journal of Forensic Medicine and Pathology, 37, 29–31. doi:10.1097/PAF.0000000000000207
Shimizu, K., Kikuchi, S., Kobayashi, T., & Kato, S. (2017). Persistent complex bereavement disorder: Clinical utility and
classification of the category proposed for Diagnostic and
Statistical Manual of Mental Disorders, 5th edition. Psychogeriatrics, 17(1), 17–24. doi:10.1111/psyg.12183
Squires, J. E., Coughlin, M., Dorrance, K., Linklater, S.,
Chassé, M., Grimshaw, J. M., . . . Knoll, G. A. (2018).
Criteria to identify a potential deceased organ donor: A
systematic review. Critical Care Medicine, 46, 1318–1327.
doi:10.1097/CCM.0000000000003200
Stroebe, M., Schut, H., & Boerner, K. (2017). Cautioning
health-care professionals: Bereaved persons are misguided
through the stages of grief. Omega: Journal of Death &
Dying, 74, 455–473. doi:10.1177/0030222817691870
Stroebe, M., Stroebe, W., Schut, H., & Boerner, K. (2017).
Grief is not a disease but bereavement merits medical
awareness. Lancet, 389(10067), 347–349. doi:10.1016/
S0140-6736(17)30189-7
Thomas, J., & Sabatino, C. (2017). Patient preferences, policy,
and POLST. Generations, 41(1), 102–109.
03/02/2021 18:19
UNIT
9
Meeting the Standards
In this unit, we learned about sensory perception, self-concept, sexuality, spirituality,
stress and coping, and loss, grieving, and death. All are essential concepts that a
nurse needs to consider to care properly for a client. Often, the nurse finds these
topics challenging because they are somewhat abstract and involve the intangible
core aspects of what makes us individuals. In the case below, you will explore how
two nursing standards guide the nurse in professional practice and in providing safe,
quality care.
CLIENT: Christina AGE: 72
CURRENT MEDICAL DIAGNOSIS: Breast Cancer
Medical History: Christina was diagnosed with an early-stage
common form of breast cancer 4 years ago. She had removal of
the lump, followed by radiation therapy and oral chemotherapy.
She has no current symptoms of her cancer and is tolerating the
chemotherapy without difficulty. She has no other significant health
conditions. The 5-year survival projection for women with similar
breast cancers is 95% and the 10-year survival rate is 82%.
Personal and Social History: Christina is retired from employment and lives with her retired husband and their cats. Their
socioeconomic status is middle class. They have Social Security,
Medicare, and sufficient retirement savings.
Questions
1. How might you respond to Christina? What have you learned
about stress, loss and grieving, spirituality, and other similar
concepts in this unit that can assist you in providing a helpful
response?
American Nurses Association Standard of Professional
Performance #11 is Leadership: The registered nurse leads
within the professional practice setting and the profession. One
of the many competencies is that the nurse contributes to the
establishment of an environment that supports and maintains
respect, trust, and dignity.
When you examine Christina’s breasts in preparing the biopsy
site, she avoids meeting your eyes. She says, quietly, “I know you
don’t want to hear about my troubles, but I don’t think my husband
finds me attractive anymore.”
2. What response might you make that exemplifies the competency above and your learning from this unit?
American Nurses Association Standard of Professional
Performance #17 is Environmental Health: The registered
nurse practices in an environmentally safe and healthy manner.
The competencies include that the registered nurse (a) participates in
Christina is your client in the same-day surgery unit, where she
is being seen for a biopsy of a new lump in her breast. During
your admission interview and assessment, you identify several
areas requiring nursing care planning. Christina is very anxious as
shown by her elevated blood pressure and pulse, perspiration, and
nervous movements. She says to you, “I just know this is cancer
again. It must be that deodorant I use. Or, maybe it’s the electrical
wires near our house. Or, just God punishing me for bad thoughts.
What do you think?”
developing strategies to promote healthy communities and practice
environments; and (b) communicates information about environmental health risks and exposure reduction strategies.
3. Considering the standard, what categories of possible interventions might you consider for a nursing diagnosis and goal
focused on Christina’s need for a healing environment?
A concept found throughout the ANA Standards is that the nurse
demonstrates commitment to continuous, lifelong learning and
education for self and others.
4. During your care of Christina, you realize that you are insufficiently knowledgeable about breast cancer treatment effects.
You wonder about the sensation in the breast after radiation
therapy (for both Christina and her husband) and the support
systems that would be in place for the many breast cancer
survivors who might be worrying about a recurrence. Describe
the various ways you might investigate answers to these
questions by interacting with your colleagues.
American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.).
Silver Spring, MD: Author.
Answers to Meeting the Standards questions are available on the faculty resources site.
Please consult with your instructor.
1106
M43_BERM9793_11_GE_C43.indd 1106
03/02/2021 18:19
UNIT
10
Promoting
Physiologic Health
44
Activity and Exercise 1108
45
Sleep 1165
46
Nutrition 1187
47
Urinary Elimination 1234
48
Fecal Elimination 1271
49
Oxygenation 1303
50
Circulation 1349
51
Fluid, Electrolyte, and Acid–Base Balance 1369
1107
M44A_BERM9793_11_GE_P10.indd 1107
27/01/2021 18:05
44
Activity and Exercise
LEA R NIN G OU TC OME S
After completing this chapter, you will be able to:
1. Describe four basic elements of normal movement.
2. Differentiate isotonic, isometric, isokinetic, aerobic, and anaerobic exercise.
3. Compare the effects of exercise and immobility on body
systems.
4. Identify factors influencing a client’s body alignment and activity.
5. Assess activity-exercise pattern, body alignment, gait, appearance and movement of joints, mobility capabilities and limitations, muscle mass and strength, activity tolerance, and
problems related to immobility.
6. Develop nursing diagnoses and outcomes related to activity,
exercise, and mobility problems.
7. Use safe practices when positioning, moving, transferring, and
ambulating clients.
8. Compare and contrast active, passive, and active-assistive
range-of-motion (ROM) exercises.
9. Describe client teaching for clients who use mechanical aids
for walking.
10. Verbalize the steps used in:
a. Moving a client up in bed
b. Turning a client to the lateral or prone position in bed
c. Logrolling a client
d. Assisting a client to sit on the side of the bed
e. Transferring between bed and chair
f. Transferring between bed and stretcher
g. Assisting a client to ambulate.
11. Recognize when it is appropriate to assign aspects of moving,
transferring, and ambulating a client to assistive personnel.
12. Demonstrate appropriate documentation and reporting of
moving, transferring, and ambulating a client.
K EY T ER M S
active ROM exercises, 1148
activity-exercise pattern, 1109
activity tolerance, 1115
aerobic exercise, 1116
ambulation, 1149
anabolism, 1121
anaerobic exercise, 1117
ankylosed, 1119
anorexia, 1121
atelectasis, 1121
atrophy, 1119
basal metabolic rate (BMR), 1121
base of support, 1109
bedrest, 1115
calculi, 1122
catabolism, 1121
center of gravity, 1109
contracture, 1119
crepitation, 1124
dorsal position, 1134
dorsal recumbent position,
1134
embolus, 1120
flaccid, 1119
foot drop, 1119
Fowler’s position, 1133
functional strength, 1115
gait, 1124
high-Fowler’s position, 1133
hypertrophy, 1117
isokinetic (resistive) exercises,
1116
Introduction
Our ability to move is an essential aspect of well-being and
our overall health is affected by our activities. The nursing diagnosis of inactive lifestyle emphasizes the role of
exercise and activity as an essential component of health.
In fact, too much sitting is emerging as a recognized health
risk for a variety of chronic illnesses (Eanes, 2018).
Many Healthy People 2020 (HealthyPeople.gov, 2019)
objectives pertain to exercise and activity. Moderate exercise is identified as significant to enhancing physical
isometric (static or setting)
exercises, 1116
isotonic (dynamic) exercises, 1116
lateral position, 1135
line of gravity, 1109
logrolling, 1140
lordosis, 1124
metabolism, 1121
mobility, 1109
orthopneic position, 1134
orthostatic hypotension, 1119
osteoporosis, 1115
pace, 1124
paresis, 1119
passive ROM exercises, 1148
prone position, 1134
proprioception, 1110
range of motion (ROM), 1110
relaxation response (RR), 1118
semi-Fowler’s position, 1133
Sims’ position, 1136
spastic, 1119
supine position, 1134
thrombophlebitis, 1120
thrombus, 1120
tripod (triangle) position, 1156
urinary incontinence, 1122
urinary reflux, 1122
urinary retention, 1122
urinary stasis, 1122
Valsalva maneuver, 1119
vital capacity, 1120
fitness. The Midcourse Progress Report (Centers for Disease Control and Prevention, 2016) provides information
as to the nation’s progress toward the Healthy People 2020
exercise and activity objectives. For example, the objectives
relating to adults engaging in regular physical activity and
meeting physical activity and muscle strengthening goals
have exceeded the target. Unfortunately, the objectives for
adolescents meeting the guidelines for aerobic physical
activity and muscle-strengthening activity have had little
or no change, as has the objective of school districts requiring regular elementary school recess for 20+ minutes.
1108
M44B_BERM9793_11_GE_C44.indd 1108
03/02/2021 18:19
Chapter 44
A strong, well-developed body of research evidence
supports the role of exercise in improving the health status of individuals with cardiovascular disease, pulmonary dysfunction, disabilities of aging, and depression.
Integrating well-researched exercise protocols with conventional nursing and medical approaches will result in
optimal treatment of these common disorders. Evidence
shows that regular exercise can prevent and even reverse
many of the chronic diseases experienced by aging adults.
An activity-exercise pattern refers to an individual’s
routine of exercise, activity, leisure, and recreation. It
includes (a) activities of daily living (ADLs) that require
energy expenditure such as hygiene, dressing, cooking,
shopping, eating, working, and home maintenance, and
(b) the type, quality, and quantity of exercise, including
sports.
Mobility, the ability to move freely, easily, rhythmically,
and purposefully in the environment, is an essential part
of living. Individuals must move to protect themselves
from trauma and to meet their basic needs. Mobility is
vital to independence; a fully immobilized individual is
as vulnerable and dependent as an infant.
Individuals often define their health and physical fitness by their activity because mental well-being and the
effectiveness of body functioning depend largely on their
mobility status. For example, when a client is upright, the
lungs expand more easily, intestinal activity (peristalsis)
is more effective, and the kidneys are able to empty completely. In addition, motion is essential for proper functioning of bones and muscles.
The ability to move without pain also influences
self-esteem and body image. For most individuals, selfesteem depends on a sense of independence and a feeling
of usefulness or being needed. Individuals with mobility
impairments may feel helpless and burdensome to others, and their ability to work and earn a living may be
compromised. Painful mobility makes coping even more
difficult. Body image can be altered by paralysis, amputations, or any motor impairment. The reaction of others
to impaired mobility can also alter self-esteem and body
image significantly.
For those with impaired mobility, movement must be
raised to the full potential to enable a satisfying life. For
example, many individuals who have impairments or use
wheelchairs participate in athletics to experience the joys
of competition and fitness. Many individuals with paralysis can use a hand control to enter and drive adapted vans
or use their mouth to manipulate a paintbrush and create
art. No matter what their level of mobility, they must be
encouraged to breathe fully, engage their abdominal muscles, and move as much as possible to prevent the physical
and psycho-emotional hazards of immobility.
M44B_BERM9793_11_GE_C44.indd 1109
Activity and Exercise
1109
Body movement involves four basic elements: body alignment (posture), joint mobility, balance, and coordinated
movement.
Alignment and Posture
Proper body alignment and posture bring body parts into
position in a manner that promotes optimal balance and
maximal body function whether the client is standing, sitting, or lying down. An individual maintains balance as
long as the line of gravity (an imaginary vertical line drawn
through the body’s center of gravity) passes through the
center of gravity (the point at which all of the body’s mass
is centered) and the base of support (the foundation on
which the body rests). In humans, the usual line of gravity
begins at the top of the head and falls between the shoulders, through the trunk, slightly anterior to the sacrum,
and between the weight-bearing joints and base of support (Figure 44.1 ■).
When the body is well aligned, strain on the joints,
muscles, tendons, or ligaments is minimized and internal
structures and organs are supported. Proper body alignment
enhances lung expansion and promotes efficient circulatory,
renal, and gastrointestinal functions. An individual’s posture
is one criterion for assessing general health, physical fitness,
and attractiveness. Posture reflects the mood, self-esteem,
and personality of an individual, and vice versa.
Abdominal and skeletal muscles function almost continuously, making tiny adjustments that enable an erect
or seated posture despite the endless downward pull of
gravity.
Line of
gravity
Center
of
gravity
Base of
support
Normal Movement
Normal movement and stability are the result of an intact
musculoskeletal system, an intact nervous system, and
intact inner ear structures responsible for equilibrium.
●
Figure 44.1 ■ The center of gravity and the line of gravity influence
standing alignment.
03/02/2021 18:19
1110
Unit 10
●
Promoting Physiologic Health
Joint Mobility
Joints are the functional units of the musculoskeletal system. The bones of the skeleton articulate at the joints, and
most of the skeletal muscles attach to the two bones at the
joint. These muscles are categorized according to the type
of joint movement they produce on contraction. Muscles
are therefore called flexors, extensors, internal rotators,
and the like. The flexor muscles are stronger than the
extensor muscles. Thus, when an individual is inactive,
the joints are pulled into a flexed (bent) position. If this
tendency is not reduced through exercise and position
changes, the muscles permanently shorten, and the joint
becomes fixed in a flexed position (contracture). Types of
joint movement are listed in Table 44.1.
The range of motion (ROM) of a joint is the maximum
movement that is possible for that joint. Joint range of motion
varies from individual to individual and is determined
by genetic makeup, developmental patterns, the presence
or absence of disease, and the amount of physical activity in which the individual normally engages. Table 44.2
shows the various joint movements and the usual ranges
of motion.
Balance
The mechanisms involved in maintaining balance and posture are complex and involve informational inputs from the
labyrinth (inner ear), from vision (vestibulo-ocular input),
and from stretch receptors of muscles and tendons (vestibulospinal input). Mechanisms of equilibrium (sense of
TABLE 44.1
Types of Joint Movements
Movement
Action
Flexion
Decreasing the angle of the joint (e.g., bending the elbow)
Extension
Increasing the angle of the joint (e.g.,
straightening the arm at the elbow)
Hyperextension
Further extension or straightening of a joint
(e.g., bending the head backward)
Abduction
Movement of the bone away from the midline
of the body
Adduction
Movement of the bone toward the midline of
the body
Rotation
Movement of the bone around its central axis
Circumduction
Movement of the distal part of the bone in a
circle while the proximal end remains fixed
Eversion
Turning the sole of the foot outward by moving the ankle joint
Inversion
Turning the sole of the foot inward by moving
the ankle joint
Pronation
Moving the bones of the forearm so that the
palm of the hand faces downward when held
in front of the body
Supination
Moving the bones of the forearm so that the
palm of the hand faces upward when held in
front of the body
M44B_BERM9793_11_GE_C44.indd 1110
balance) respond, frequently without our awareness, to
various head movements. Proprioception is the term used
to describe awareness of posture, movement, and changes
in equilibrium and the knowledge of position, weight, and
resistance of objects in relation to the body.
Coordinated Movement
Balanced, smooth, purposeful movement is the result
of proper functioning of the cerebral cortex, cerebellum,
and basal ganglia. The cerebral cortex initiates voluntary
motor activity, the cerebellum coordinates the motor activities of movement, and the basal ganglia maintain posture.
When a client’s cerebellum is injured, movements become
clumsy, unsure, and uncoordinated.
Factors Affecting Body
Alignment and Activity
A number of factors affect an individual’s body alignment,
mobility, and daily activity level. These include growth
and development, nutrition, personal values and attitudes, certain external factors, and prescribed limitations.
Growth and Development
An individual’s age and musculoskeletal and nervous
system development affect posture, body proportions,
body mass, body movements, and reflexes. Newborn
movements are reflexive and random. All extremities are
generally flexed but can be passively moved through a
full range of motion. As the neurologic system matures,
control over movement progresses during the first year.
Gross motor development precedes fine motor skills.
Gross motor development occurs in a head-to-toe fashion, that is, progression from head control, to crawling,
to pulling up to a standing position, to standing, and to
walking, usually after the first birthday. The contralateral
motion of crawling, however brief, is an important building block for walking. Initially, walking involves a wide
stance and unsteady gait, thus the term toddler. From ages
1 to 5 years, both gross and fine motor skills are refined.
For example, preschoolers master riding a tricycle, running, jumping, using crayons to draw, fastening or using
zippers, and brushing their teeth. Immobility can impair
the social and motor development of young children.
From 6 to 12 years of age, refinement of motor skills
continues and exercise patterns for later life are generally determined. Posture in school-age children is usually
excellent. In adolescence, growth spurts and behaviors
such as carrying heavy book bags on one shoulder and
extended computer use may result in postural changes
that often persist into adulthood.
Adults between 20 and 40 years of age generally have
few physical changes affecting mobility, with the exception of pregnant women. Pregnancy alters the body’s
center of gravity and affects balance. The most recent
03/02/2021 18:19
Chapter 44
TABLE 44.2
●
Activity and Exercise
1111
Selected Joint Movements and Example of Corresponding Activity of Daily Living (ADL)
Body Part—Type of Joint/Movement
NECK—PIVOT JOINT
Flexion. Move the head from the upright midline position forward,
so that the chin rests on the chest (Figure 44.2 ■).
Normal Range
and Example of
Corresponding ADL
45° from midline
Example: nodding head
“yes”
Illustration
Figure 44.2 ■
Extension. Move the head from the flexed position to the upright
position (Figure 44.2).
45° from midline
Example: nodding head
“yes”
Hyperextension. Move the head from the upright position back
as far as possible (Figure 44.2).
45° from midline
Lateral flexion. Move the head laterally to the right and left
shoulders (Figure 44.3 ■).
40° from midline
Rotation. Turn the face as far as possible to the right and left
(Figure 44.4 ■).
70° from midline
Example: shaking head
“no”
Figure 44.4 ■
180° from the side
Example: reaching to turn
on overhead light
Figure 44.5 ■
SHOULDER—BALL-AND-SOCKET JOINT
Flexion. Raise each arm from a position by the side forward and
upward to a position beside the head (Figure 44.5 ■).
Figure 44.3 ■
Extension. Move each arm from a vertical position beside the
head forward and down to a resting position at the side of the
body (Figure 44.5).
180° from vertical position beside the head
Hyperextension. Move each arm from a resting side position to
behind the body (Figure 44.5).
50° from side position
Abduction. Move each arm laterally from a resting position at the
sides to a side position above the head, palm of the hand either
toward or away from the head (Figure 44.6 ■).
180°
Example: reaching to
bedside stand on same
side of bed as arm
Adduction (anterior). Move each arm from a position at
the sides across the front of the body as far as possible
(Figure 44.6). The elbow may be straight or bent.
50°
Example: reaching across
body toward opposite
side of bed
Circumduction. Move each arm forward, up, back, and down in
a full circle (Figure 44.7 ■).
360°
Figure 44.7 ■
External rotation. With each arm held out to the side at
shoulder level and the elbow bent to a right angle, fingers
pointing down, move the arm upward so that the fingers point
up (Figure 44.8 ■).
90°
Example: reaching over
opposite shoulder to
scratch upper back
Figure 44.8 ■
Internal rotation. With each arm held out to the side at shoulder level
and the elbow bent to a right angle, fingers pointing up, bring the arm
forward and down so that the fingers point down (Figure 44.8).
90°
Example: reaching to
scratch same side lower
back
Figure 44.6 ■
Continued on page 1112
M44B_BERM9793_11_GE_C44.indd 1111
03/02/2021 18:19
1112
Unit 10
TABLE 44.2
●
Promoting Physiologic Health
Selected Joint Movements and Example of Corresponding Activity of Daily
Living (ADL)—continued
Body Part—Type of Joint/Movement
ELBOW—HINGE JOINT
Flexion. Bring each lower arm forward and upward so that the
hand is at the shoulder (Figure 44.9 ■).
Normal Range
and Example of
Corresponding ADL
150°
Example: eating, bathing,
shaving
Extension. Bring each lower arm forward and downward,
straightening the arm (Figure 44.9).
150°
Example: eating, bathing,
shaving
Rotation for supination. Turn each hand and forearm so that the
palm is facing upward (Figure 44.10 ■).
70° to 90°
Rotation for pronation. Turn each hand and forearm so that the
palm is facing downward (Figure 44.10).
70° to 90°
WRIST—CONDYLOID JOINT
Flexion. Bring the fingers of each hand toward the inner aspect of
the forearm (Figure 44.11 ■).
80° to 90°
Example: eating, bathing,
shaving, writing
Illustration
Figure 44.9 ■
Figure 44.10 ■
Figure 44.11 ■
Extension. Straighten each hand to the same plane as the arm
(Figure 44.11).
80° to 90°
Example: eating, bathing,
shaving
Hyperextension. Bend the fingers of each hand back as far as
possible (Figure 44.12 ■).
70° to 90°
Figure 44.12 ■
Radial flexion (abduction). Bend each wrist laterally toward the
thumb side with hand supinated (Figure 44.13 ■).
0° to 20°
Figure 44.13 ■
Ulnar flexion (adduction). Bend each wrist laterally toward the
fifth finger with the hand supinated (Figure 44.13).
30° to 50°
HAND AND FINGERS: METACARPOPHALANGEAL JOINTS—
CONDYLOID; INTERPHALANGEAL JOINTS—HINGE
Flexion. Make a fist with each hand (Figure 44.14 ■).
90°
Example: squeezing,
gripping, writing
Extension. Straighten the fingers of each hand (Figure 44.14).
90°
Hyperextension. Bend the fingers of each hand back as far as
possible (Figure 44.14).
30°
Abduction. Spread the fingers of each hand apart
(Figure 44.15 ■).
20°
Adduction. Bring the fingers of each hand together (Figure 44.15).
20°
Example: writing, gripping, eating, many hobbies involving fine motor
coordination (e.g., art,
music)
THUMB—SADDLE JOINT
Flexion. Move each thumb across the palmar surface of the hand
toward the fifth finger (Figure 44.16 ■).
Figure 44.15 ■
Figure 44.16 ■
90°
Extension. Move each thumb away from the hand
(Figure 44.16).
90°
Abduction. Extend each thumb laterally (Figure 44.17 ■).
30°
Adduction. Move each thumb back to the hand
(Figure 44.17).
30°
M44B_BERM9793_11_GE_C44.indd 1112
Figure 44.14 ■
Figure 44.17 ■
03/02/2021 18:19
Chapter 44
TABLE 44.2
●
Activity and Exercise
1113
Selected Joint Movements and Example of Corresponding Activity of Daily
Living (ADL)—continued
Body Part—Type of Joint/Movement
Normal Range
and Example of
Corresponding ADL
Figure 44.18 ■
Opposition. Touch each thumb to the top of each finger of the
same hand. The thumb joint movements involved are abduction,
rotation, and flexion (Figure 44.18 ■).
HIP—BALL-AND-SOCKET JOINT
Flexion. Move each leg forward and upward. The knee may be
extended or flexed (Figure 44.19 ■).
Illustration
Knee extended, 90°;
knee flexed, 120°
Example: walking, leg lifts
in front of the body
Figure 44.19 ■
Extension. Move each leg back beside the other
(Figure 44.20 ■).
90° to 120°
Example: walking, lining
the leg up with the body
Figure 44.20 ■
Hyperextension. Move each leg back behind the body
(Figure 44.20).
30° to 50°
Example: walking; lying
on side, reach the leg
behind the body
Abduction. Move each leg out to the side (Figure 44.21 ■).
45° to 50°
Example: moving leg
away from body
Adduction. Move each leg back to the other leg and beyond in
front of it (Figure 44.21).
20° to 30° beyond other
leg
Example: moving leg over
the other leg toward the
middle of the body
Circumduction. Move each leg backward, up, to the side, and
down in a circle (Figure 44.22 ■).
360°
Example: leg circles
clockwise and
counterclockwise
Figure 44.22 ■
Internal rotation. Flex knee and hip to 90°. Place the foot away
from the midline. Move the thigh and knee toward the midline
(Figure 44.23 ■).
40°
Figure 44.23 ■
External rotation. Flex knee and hip to 90°. Place the foot toward
the midline. Move the thigh and knee away from the midline
(Figure 44.23).
45°
KNEE—HINGE JOINT
Flexion. Bend each leg, bringing the heel toward the back of the
thigh (Figure 44.24 ■).
Extension. Straighten each leg, returning the foot to its position
beside the other foot (Figure 44.24).
Figure 44.21 ■
0°
45°
120° to 130°
Example: knee bends,
walking
40°
Internal
rotation
to 40°
External
rotation
to 45°
Figure 44.24 ■
120° to 130°
Example: straightening
leg from bent position,
walking
Continued on page 1114
M44B_BERM9793_11_GE_C44.indd 1113
03/02/2021 18:19
1114
Unit 10
TABLE 44.2
●
Promoting Physiologic Health
Selected Joint Movements and Example of Corresponding Activity of Daily
Living (ADL)—continued
Body Part—Type of Joint/Movement
ANKLE—HINGE JOINT
Extension (plantar flexion). Point the toes of each foot downward (Figure 44.25 ■).
Flexion (dorsiflexion). Point the toes of each foot upward
(Figure 44.25).
FOOT—GLIDING
Eversion. Turn the sole of each foot laterally (Figure 44.26 ■).
Inversion. Turn the sole of each foot medially (Figure 44.26).
TOES: INTERPHALANGEAL JOINTS—HINGE; METATARSOPHALANGEAL JOINTS—HINGE; INTERTARSAL
JOINTS—GLIDING
Flexion. Curl the toe joints of each foot downward
(Figure 44.27 ■).
Extension. Straighten the toes of each foot (Figure 44.27).
TRUNK—GLIDING JOINT
Flexion. Bend the trunk toward the toes (Figure 44.28 ■).
Normal Range
and Example of
Corresponding ADL
20°
Example: pressing toes
away from face, walking
Illustration
Figure 44.25 ■
45° to 50°
Example: pulling toes
toward face, walking
5°
Example: foot circles clockwise and
counterclockwise
Figure 44.26 ■
5°
Example: foot circles clockwise and
counterclockwise
Example: walking, wiggling toes
35° to 60°
Figure 44.27 ■
35° to 60°
70° to 90°
Example: touching toes
Figure 44.28 ■
Extension. Straighten the trunk from a flexed position
(Figure 44.28).
Hyperextension. Bend the trunk backward (Figure 44.28).
20° to 30°
Example: gentle supported back bend with
hands on buttocks
Lateral flexion. Bend the trunk to the right and to the left
(Figure 44.29 ■).
35° on each side
Example: gently allow
right hand to slide down
right side of thigh, repeat
on left side
Rotation. Turn the upper part of the body from side to side
(Figure 44.30 ■).
30° to 45°
Example: gently swing
torso right and left,
maintaining forward hip
alignment
M44B_BERM9793_11_GE_C44.indd 1114
Figure 44.29 ■
Figure 44.30 ■
03/02/2021 18:19
Chapter 44
recommendations from the American College of Obstetricians and Gynecologists (2017) suggest that healthy
pregnant women should exercise at least 150 minutes with
moderate intensity aerobic activity every week. Thorough
clinical evaluations of the client should be completed prior
to recommending any exercise regimen.
As age advances, muscle tone and bone density
decrease, joints lose flexibility, reaction time slows, and
bone mass decreases, particularly in women who have
osteoporosis. Osteoporosis is a condition in which the
bones become brittle and fragile due to calcium depletion.
Osteoporosis is common in older women and primarily
affects the weight-bearing joints of the lower extremities
and the anterior aspects of spinal bones, causing compression fractures of the vertebrae and hip fractures. All
of these changes affect older adults’ posture, gait, and
balance. Posture becomes forward leaning and stooped,
which shifts the center of gravity forward. To compensate for this shift, the knees flex slightly for support and
the base of support is widened. Gait becomes wide based,
short stepped, and shuffling.
A strong body of research supports the benefits of
regular activity for older adults to maintain and regain
strength, flexibility, cardiovascular fitness, and bone density. Other health benefits are well documented, including
reduction in falls, mood stabilization, reduction in obesity,
and diabetes management (Kraschnewski et al., 2016a).
Nutrition
Both undernutrition and overnutrition can influence body
alignment and mobility. Poorly nourished people may
have muscle weakness and fatigue. Vitamin D deficiency
causes bone deformity during growth. Inadequate calcium intake and vitamin D synthesis and intake increase
the risk of osteoporosis. Obesity can distort movement
and stress joints, adversely affecting posture, balance, and
joint health. See Chapter 46
for more information about
nutrition.
Personal Values and Attitudes
Whether individuals value regular exercise is often the
result of family influences. In families that incorporate
regular exercise into their daily routine or spend time
together in activities, children learn to value physical
activity. Sedentary families, on the other hand, participate
in sports only as spectators, and this lifestyle is often transmitted to their children. With the increase in TV, computer,
and video activities, youth are increasingly sedentary
with associated declines in health. Values about physical
appearance also influence some individuals’ participation in regular exercise. Individuals who value a muscular
build or physical attractiveness may participate in regular
exercise programs to produce the appearance they desire.
Choice of physical activity or type of exercise is also
influenced by values. Choices may be influenced by
M44B_BERM9793_11_GE_C44.indd 1115
●
Activity and Exercise
1115
geographic location and cultural role expectations. For
many, thinking of exercise more as “recreational movement,” “enhancement of well-being,” and “an essential part
of daily self-care” may help overcome perceptions that exercise is drudgery. Options include informal and fun activities
such as dancing to music. Motivational states influence our
behavior and choices, and vary widely from day to day.
External Factors
Many external factors affect an individual’s mobility.
Excessively high temperatures and high humidity discourage activity, whereas comfortable temperatures and low
humidity are conducive to activity. Proper hydration needs
vary according to the individual, health status, activity levels, and environment. Water is the best fluid to replace loss
incurred through metabolic processes and exercise.
The availability of recreational facilities also influences activity; for example, lack of money may prohibit
a client from joining an exercise club or gymnasium or
from purchasing needed equipment. Neighborhood safety
promotes outdoor activity, whereas an unsafe environment discourages individuals from going outdoors. Adolescents, in particular, may spend many hours sitting at
computers, watching television, or playing video games
rather than engaging in physical activities.
Prescribed Limitations
Limitations to movement may be medically prescribed
for some health problems. To promote healing, devices
such as casts, braces, splints, and traction are often used
to immobilize body parts. Clients who are short of breath
may be advised not to walk up stairs. Bedrest may be
the therapeutic choice for certain clients, for example, to
relieve edema, to reduce metabolic and oxygen needs, to
promote tissue repair, or to decrease pain.
The term bedrest varies in meaning to some extent.
In some agencies, bedrest means strict confinement to
bed or “complete” bedrest. Others may allow the client
to use a bedside commode or have bathroom privileges.
Nurses need to familiarize themselves with the meaning
of bedrest in their practice setting. In any case, the effects
of limiting activity are immediate, and therapeutic positioning is important to prevent further complications and
improve client outcomes. There is rarely a need for complete bedrest.
Exercise
Individuals participate in exercise programs to decrease
risk factors for chronic diseases and to increase their
health and well-being. Functional strength is another goal
of exercise, and is defined as the ability of the body to
perform work. Activity tolerance is the type and amount of
exercise or ADLs an individual is able to perform without
experiencing adverse effects.
03/02/2021 18:19
1116
Unit 10
●
Promoting Physiologic Health
Types of Exercise
Exercise involves the active contraction and relaxation
of muscles. Exercises can be classified according to the
type of muscle contraction (isotonic, isometric, or isokinetic) and according to the source of energy (aerobic or
anaerobic).
Isotonic (dynamic) exercises are those in which the
muscle shortens to produce muscle contraction and
active movement. Most physical conditioning exercises—
running, walking, swimming, cycling, and other such
activities—are isotonic, as are ADLs and active ROM
exercises (those initiated by the client). Examples of
isotonic bed exercises are pushing or pulling against a
stationary object, using a trapeze to lift the body off the
bed, lifting the buttocks off the bed by pushing with the
hands against the mattress, and pushing the body to a
sitting position.
Isotonic exercises increase muscle tone, mass, and
strength and maintain joint flexibility and circulation.
During isotonic exercise, both heart rate and cardiac output quicken to increase blood flow to all parts of the body.
Isometric (static or setting) exercises are those in
which muscle contraction occurs without moving the
joint (muscle length does not change). These exercises
involve exerting pressure against a solid object and
are useful for strengthening abdominal, gluteal, and
quadriceps muscles used in ambulation; for maintaining strength in immobilized muscles in casts or traction; and for endurance training. An example of an
isometric bed exercise would be squeezing a towel
or pillow between the knees while at the same time
tightening the muscles in the fronts of the thighs by
pressing the knees backwards (see Figure 44.31 ■),
and holding for several seconds. These are often called
“quad sets.” Isometric exercises produce a mild increase
in heart rate and cardiac output, but no appreciable
increase in blood flow to other parts of the body.
Isokinetic (resistive) exercises involve muscle contraction or tension against resistance. During isokinetic
exercises, the individual tenses (isometric) against resistance. Special machines or devices provide the resistance
Figure 44.31 ■ Example of an isometric exercise for the knees and
legs. The client sits or lies on a flat surface with the legs straight out.
Using a rolled towel between the knees, the client pushes the knees
together and tightens the muscles in the front of the thighs by forcing the
knees downward and holding for 10 seconds.
to the movement. These exercises are used in physical
conditioning and are often done to build up certain muscle groups.
Aerobic exercise is activity during which the amount
of oxygen taken into the body is greater than that used to
perform the activity. Aerobic exercises use large muscle
groups that move repetitively. Aerobic exercises improve
cardiovascular conditioning and physical fitness. Assessment of physical fitness is discussed in Chapter 19
.
The accompanying Client Teaching feature describes frequency, duration, and types of activity recommended for
healthy adults.
Intensity of exercise can be measured in three ways:
1. Target heart rate. The goal is to work up to and sustain
a target heart rate during exercise, based on the individual’s age. To determine target heart rate, first calculate the client’s maximum heart rate by subtracting
his or her current age in years from 220. Then obtain
the target heart rate by taking 60% to 85% of the maximum. Because heart rates vary among individuals, the
tests that follow are replacing this measure.
CLIENT TEACHING Guidelines and Minimal Requirements for Physical Activity
FREQUENCY AND DURATION
• Aerobic: Cumulative 30 minutes or more daily (can be divided
throughout the day) of “moderate intensity” movement as measured by talk test and perceived exertion scale.
• Stretching: Should be added onto that minimum requirement
so that all parts of the body are stretched each day.
• Strength training: Should be added onto these minimum
requirements so that all muscle groups are addressed at least
three times a week, with a day of rest after training.
TYPE OF EXERCISE
• Aerobic: Elliptical exercisers, walking, biking, gardening,
dancing, and swimming are recommended for all individuals,
including beginners and older adults. Activities that are more
M44B_BERM9793_11_GE_C44.indd 1116
strenuous include jogging, running, Spinning, power yoga, boxing, and jumping rope.
• Stretching: Yoga, Pilates, qigong, and many other flexibility programs are effective.
• Strength training: Resistance can be provided with weights,
bands, balls, and body weight.
SAFETY
• Stress the importance of balance and prevention of falls, proper
clothing to ensure thermal safety, checking equipment for
proper function, wearing a helmet and other protective gear,
using reflective devices at night, and carrying identification and
emergency information.
03/02/2021 18:19
Chapter 44
2. Talk test. This test is easier to implement and keeps
most people at 60% of maximum heart rate or more.
When exercising, the client should experience labored
breathing, yet still be able to carry on a conversation.
3. Borg scale of perceived exertion (Borg, 1998). This
scale measures “how difficult” the exercise feels to the
client in terms of heart and lung exertion. The scale
progresses from 1 to 20 with the following markers:
7 = very, very light; 9 = very light; 11 = fairly light;
13 = somewhat hard; 15 = hard; 17 = very hard;
and 19 = very, very hard.
“Very, very hard” corresponds closely to 100%
of maximum heart rate. “Very light” is close to 40%.
Most people need to strive for the “somewhat hard”
level (13/20), which corresponds to 75% of maximum heart rate.
Anaerobic exercise involves activity in which the
muscles cannot draw out enough oxygen from the bloodstream, and anaerobic pathways are used to provide additional energy for a short time. This type of exercise is used
in endurance training for athletes such as weight lifting
and sprinting.
QSEN
Patient-Centered Care: Therapeutic
Movement Modalities
Therapeutic movement modalities from Eastern cultures are
finding a place in evidence-based healthcare. In particular,
Hatha yoga, qigong, and t’ai chi are receiving wide attention for improving strength and balance as well as treating
a wide variety of health problems. Hatha yoga, developed
in ancient Hindu culture, is a series of physical exercises,
breath control, and meditation that tones and strengthens the
whole individual—body, mind, and spirit (Figure 44.32 ■).
The beauty of yoga is that it can be fully practiced by those
who must use a wheelchair or remain in bed.
●
Activity and Exercise
1117
Figure 44.33 ■ Men and women practicing t’ai chi outdoors.
Dinis Tolipov/123RF.
Qigong is a Chinese discipline that involves breathing and gentle movements of mostly arms and torso. The
regular practice of qigong is intended to generate as well
as conserve energy to maintain health or treat illness.
Although developed as a martial art, t’ai chi is practiced today mostly for health promotion. In China, it is
common to see individuals of all ages, including older
adults, practicing these movement disciplines outdoors
in public parks (Figure 44.33 ■).
Nurses can independently recommend that clients
who are able to do so consider initiating these movement modalities. Through appropriate referrals to group
classes in the community as well as the use of videotapes
in homes and long-term care facilities, clients can take
charge of their own health in ways that are empowering,
holistic, and free of negative side effects. Nurses should
assess each individual for readiness, safety issues, balance,
and ability to engage in any physical activity.
Benefits of Exercise
In general, regular exercise is essential for maintaining
mental and physical health.
Musculoskeletal System
Figure 44.32 ■ Woman in a yoga stretch.
Artur Bogacki/Shutterstock.
M44B_BERM9793_11_GE_C44.indd 1117
The size, shape, tone, and strength of muscles (including the heart muscle) are maintained with mild exercise
and increased with strenuous exercise. With strenuous
exercise, muscles hypertrophy (enlarge), and the efficiency of muscular contraction increases. Joints lack a
discrete blood supply. It is through activity that joints
receive nourishment. Exercise increases joint flexibility,
stability, and range of motion. Bone density and strength
are maintained through weight bearing. The stress of
weight-bearing and high-impact movement maintains
a balance between osteoblasts (bone-building cells)
and osteoclasts (bone-resorption and breakdown cells).
Examples of non–weight-bearing exercise include swimming and bicycling.
03/02/2021 18:19
1118
Unit 10
●
Promoting Physiologic Health
Cardiovascular System
The American Heart Association (2018) places great
emphasis on physical activity by recommending at least
150 minutes per week of moderate exercise or 75 minutes
per week of vigorous exercise, or a combination of moderate and vigorous activity. Adequate moderate-intensity
exercise increases the heart rate, the strength of heart
muscle contraction, and the blood supply to the heart and
muscles through increased cardiac output. Exercise also
promotes heart health by reducing the harmful effects of
stress. The types of exercise that will provide cardiac benefit vary. They include aerobic exercise such as walking
and cycling. Research evidence supports the benefits of
yoga practice on cardiovascular health.
Respiratory System
Ventilation (air circulating into and out of the lungs)
and oxygen intake increase during exercise, thereby
improving gas exchange. More toxins are eliminated
with deeper breathing, and problem-solving and emotional stability are enhanced due to increased oxygen
to the brain. Adequate exercise also prevents pooling
of secretions in the bronchi and bronchioles, decreasing breathing effort and risk of infection. Attention to
exercising muscles of respiration (by deep breathing)
throughout an activity as well as rest enhances oxygenation (improving stamina) and circulation of lymph
(improving immune function).
Gastrointestinal System
Exercise improves the appetite and increases gastrointestinal tract tone, facilitating peristalsis. Activities such as
rowing, swimming, walking, and sit-ups work the abdominal muscles and can help relieve constipation.
Endocrine System and Metabolism
Exercise elevates the metabolic rate, thus increasing the
production of body heat and waste products and calorie use.
During strenuous exercise, the metabolic rate can increase
to as much as 20 times the normal rate. This elevation lasts
after exercise is completed. Exercise increases the use of
triglycerides and fatty acids, resulting in a reduced level of
serum triglycerides, glycosylated hemoglobin A1C (HbA1C)
levels, and cholesterol. Weight loss and exercise stabilize
blood sugar and make cells more responsive to insulin.
Urinary System
With adequate exercise, which promotes efficient blood
flow, the body excretes wastes more effectively. In addition, stasis (stagnation) of urine in the bladder is usually
prevented, which in turn decreases the risk for urinary
tract infections (UTIs).
Immune System
As respiratory and musculoskeletal effort increase with
exercise and as gravity is enlisted with postural changes,
lymph fluid is more efficiently pumped from tissues
into lymph capillaries and vessels throughout the body.
Circulation through lymph nodes where destruction of
M44B_BERM9793_11_GE_C44.indd 1118
pathogens and removal of foreign antigens can occur is
also improved.
Psychoneurologic System
Mental or affective disorders such as depression or chronic
stress may affect an individual’s desire to move. The
depressed client may lack enthusiasm for taking part in
any activity and may even lack energy for usual hygiene
practices. Lack of visible energy is often seen in a slumped
posture with head bent down. Chronic stress can deplete
the body’s energy reserves to the point that fatigue discourages the desire to exercise, even though exercise can
energize the client and facilitate coping. By contrast, clients with eating disorders may exercise excessively in an
effort to prevent weight gain.
A growing body of evidence supports the role of exercise in elevating mood and relieving stress and anxiety
across the lifespan. Solid data examining relationships
between both aerobic and nonaerobic styles of exercise
support the use of this modality to relieve symptoms of
depression. The mechanism of action is thought to be a
result of one or more of the following: Exercise increases
levels of metabolites for neurotransmitters such as norepinephrine and serotonin; exercise releases endogenous
opioids, thus increasing levels of endorphins; exercise
increases levels of oxygen to the brain and other body
systems, inducing euphoria; and through muscular exertion (especially with movement modalities such as yoga
and t’ai chi) the body releases stored stress associated with
accumulated emotional demands. Regular exercise also
improves quality of sleep for most individuals.
Cognitive Function
Current research supports the positive effects of exercise
on cognitive functioning, in particular decision-making
and problem-solving processes, planning, and paying
attention. Physical exertion induces cells in the brain to
strengthen and build neuronal connections.
Spiritual Health
Yoga-style exercise improves the mind–body–spirit connection, relationship with God, and physical well-being by
establishing balance in the internal and external environment. The combination of mind, body, and breath awareness
is likely to have an impact on psychophysiologic functioning. The emphasis on breathing in is thought to soothe the
nervous and cardiorespiratory systems, promoting relaxation and preparedness for a contemplative experience.
The relaxation response (RR), first described by
Dr. Herbert Benson, is beneficial for counteracting some
of the harmful effects of stress on the body and mind. The
RR is a healthful physiologic relaxation that can be elicited
through recitation of a word or phrase or prayer while sitting quietly and relaxing your muscles.
Progressive muscle relaxation techniques involve
contracting and then releasing groups of muscles
throughout the body until all parts of the body feel
relaxed. These movements are subtle and, along with
03/02/2021 18:19
Chapter 44
relaxation breathing, can be done by almost anyone at
any time, regardless of mobility or fitness status, providing potent stress relief and neurocardiovascular
health benefits.
Effects of Immobility
Mobility and activity tolerance are affected by any disorder that impairs the ability of the nervous system, musculoskeletal system, cardiovascular system, respiratory
system, and vestibular apparatus. Congenital problems
such as hip dysplasia, spina bifida, cerebral palsy, and
the muscular dystrophies affect motor functioning. Disorders of the nervous system such as Parkinson’s disease,
multiple sclerosis, central nervous system tumors, strokes,
infectious processes (e.g., meningitis), and head and spinal
cord injuries can leave muscle groups weakened, paralyzed (paresis), spastic (with too much muscle tone), or
flaccid (without muscle tone). Musculoskeletal disorders
affecting mobility include strains, sprains, fractures, joint
dislocations, amputations, and joint replacements. Inner
ear infections and dizziness can impair balance. Many
other acute and chronic illnesses that limit the supply of
oxygen and nutrients needed for muscle contraction and
movement can seriously affect activity tolerance. Examples include chronic obstructive lung disease, anemia,
congestive heart failure, and angina.
Individuals who have inactive lifestyles or who are
faced with inactivity because of illness or injury are at risk
for many problems that can affect major body systems.
Whether immobility causes any problems often depends
on the duration of the inactivity, the client’s health status,
and the client’s sensory awareness. The most obvious
signs of prolonged immobility are often manifested in the
musculoskeletal system, and the deconditioning effects can
be observed even after a matter of days. Clients experience
a significant decrease in muscular strength and agility
whenever they do not maintain a moderate amount of
physical activity. In addition, immobility adversely affects
the cardiovascular, respiratory, metabolic, urinary, and
psychoneurologic systems. Nurses need to understand
these effects and encourage client movement as much as
possible. Early ambulation after illness or surgery is an
essential measure to prevent complications.
Clinical Alert!
A review of studies on effects of bedrest in clients with different
disorders revealed that bedrest for treatment of medical conditions is
associated with worse outcomes than early mobilization. In general,
there are few indications for bedrest, and bedrest may delay recovery
or actually harm clients.
•
•
•
●
Activity and Exercise
1119
strength and density. Regardless of the amount of calcium in an individual’s diet, the demineralization process, known as osteoporosis, continues with immobility.
The bones become spongy and may gradually deform
and fracture easily.
Disuse atrophy. Unused muscles atrophy (decrease in
size), losing most of their strength and normal function.
Contractures. When the muscle fibers are not able to
shorten and lengthen, eventually a contracture (permanent shortening of the muscle) forms, limiting joint
mobility. This process eventually involves the tendons,
ligaments, and joint capsules; it is irreversible except
by surgical intervention. Joint deformities such as
foot drop (Figure 44.34 ■), wrist drop, and external hip
rotation occur when a stronger muscle dominates the
opposite muscle.
Stiffness and pain in the joints. Without movement,
the collagen (connective) tissues at the joint become
ankylosed (permanently immobile). In addition, as the
bones demineralize, excess calcium may deposit in the
joints, contributing to stiffness and pain.
Cardiovascular System
•
•
•
Diminished cardiac reserve. Decreased mobility creates an imbalance in the autonomic nervous system,
resulting in a dominance of sympathetic activity that
increases heart rate. Rapid heart rate reduces diastolic
pressure, coronary blood flow, and the capacity of the
heart to respond to any metabolic demands above the
basal levels. Because of this diminished cardiac reserve,
the immobilized client may experience tachycardia
with even minimal exertion.
Increased use of the Valsalva maneuver. The Valsalva
maneuver refers to holding the breath and straining
against a closed glottis. For example, clients tend to
hold their breath when attempting to move up in a bed
or sit on a bedpan. This builds up sufficient pressure on
the large veins in the thorax to interfere with the return
blood flow to the heart and coronary arteries. When
the client exhales and the glottis again opens, pressure
is suddenly released, and a surge of blood flows to the
heart. Cardiac arrhythmias can result if the client has
preexisting cardiac disease.
Orthostatic (postural) hypotension. Orthostatic
hypotension is a common result of immobilization.
Under normal conditions, sympathetic nervous system
activity causes automatic vasoconstriction in the blood
vessels in the lower half of the body when a mobile
client changes from a horizontal to a vertical posture.
Musculoskeletal System
•
Disuse osteoporosis. Without the stress of weightbearing activity, the bones demineralize. They are
depleted chiefly of calcium, which gives the bones
M44B_BERM9793_11_GE_C44.indd 1119
Figure 44.34 ■ Plantar flexion contracture (foot drop).
03/02/2021 18:19
1120
•
•
Unit 10
●
Promoting Physiologic Health
Vasoconstriction prevents pooling of the blood in the
legs and effectively maintains central blood pressure
to ensure adequate perfusion of the heart and brain.
During any prolonged immobility, however, this reflex
becomes inactive. When the immobile client attempts to
sit or stand, this reconstricting mechanism fails to function properly in spite of increased adrenalin output.
The blood pools in the lower extremities, and central
blood pressure drops. Cerebral perfusion is seriously
compromised, and the client feels dizzy or light-headed
and may even faint. This sequence is usually accompanied by a sudden and marked increase in heart rate, the
body’s effort to protect the brain from an inadequate
blood supply.
Venous vasodilation and stasis. The skeletal muscles
of an active client contract with each movement, compressing the blood vessels in those muscles and helping
to pump the blood back to the heart against gravity. The
tiny valves in the leg veins aid in venous return to the
heart by preventing backward flow of blood and pooling. In an immobile client, the skeletal muscles do not
contract sufficiently, and the muscles atrophy. The skeletal muscles can no longer assist in pumping blood back
to the heart against gravity. Blood pools in the leg veins,
causing vasodilation and engorgement. The valves in
the veins can no longer work effectively to prevent
backward flow of blood and pooling (Figure 44.35 ■).
This phenomenon is known as incompetent valves.
As the blood continues to pool in the veins, its greater
volume increases venous blood pressure, which can
become much higher than that exerted by the tissues
surrounding the vessel.
Dependent edema. When the venous pressure is sufficiently great, some of the serous part of the blood is
forced out of the blood vessel into the interstitial spaces
surrounding the blood vessel, causing edema. Edema is
most common in parts of the body positioned below the
•
A thrombus (clot) is particularly dangerous if it breaks
loose from the vein wall to enter the general circulation
as an embolus (an object that has moved from its place
of origin, causing obstruction to circulation elsewhere).
Large emboli that enter the pulmonary circulation may
occlude the vessels that nourish the lungs to cause an
infarcted (dead) area of the lung. If the infarcted area
is large, pulmonary function may be seriously compromised, or death may ensue. Emboli traveling to the
coronary vessels or brain can produce a similarly dangerous outcome.
Clinical Alert!
Prolonged inactivity (such as bedrest or sleeping during a long plane
ride) in combination with oral contraceptive use can lead to dangerous clot formation in deep leg veins, even in otherwise healthy young
women. Smoking increases this risk. Regular movement, stretching,
and keeping legs uncrossed are recommended. Monitor for tenderness, redness or discoloration, warmth, and swelling in the legs.
Respiratory System
•
BP:
10–15 mmHg
BP:
20–30 mmHg
Vein valves
Interstitial
tissue pressure
10–20 mmHg
seeping into
interstitial
tissues
•
A
B
Figure 44.35 ■ Leg veins: A, in a mobile client; B, in an immobile
client.
M44B_BERM9793_11_GE_C44.indd 1120
heart. Dependent edema is most likely to occur around
the sacrum or heels of a client who sits up in bed or in
the feet and lower legs of a client who sits in a chair.
Edema further impedes venous return of blood to the
heart, causing more pooling and more edema. Edematous tissue is uncomfortable and more susceptible to
injury than normal tissue.
Thrombus formation. Three factors collectively predispose a client to the formation of a thrombophlebitis
(a clot that is loosely attached to an inflamed vein
wall): impaired venous return to the heart, hypercoagulability of the blood (sometimes caused by
medications such as oral contraceptives), and injury
to a vessel wall.
Decreased respiratory movement. In a recumbent,
immobile client, ventilation of the lungs is passively
altered. The body presses against the rigid bed and
decreases chest movement. The abdominal organs
push against the diaphragm, restricting lung movement and making it difficult to expand the lungs fully.
An immobile, recumbent client rarely sighs, partly
because overall muscle atrophy also affects the respiratory muscles and partly because there is no stimulus of
activity. Without these periodic stretching movements,
the cartilaginous intercostal joints may become fixed
in an expiratory phase of respiration, further limiting
the potential for maximal ventilation. These changes
produce shallow respirations and reduce vital capacity
(the maximum amount of air that can be exhaled after
a maximum inhalation).
Pooling of respiratory secretions. Secretions of the
respiratory tract are normally expelled by changing positions or posture and by coughing. Inactivity
allows secretions to pool by gravity (Figure 44.36 ■),
interfering with the normal diffusion of oxygen and
03/02/2021 18:19
Chapter 44
•
•
Figure 44.36 ■ Pooling of secretions in the lungs of an immobile client.
•
•
carbon dioxide in the alveoli. The ability to cough up
secretions may also be hindered by loss of respiratory
muscle tone, dehydration (which thickens secretions),
or sedatives that depress the cough reflex. Poor oxygenation and retention of carbon dioxide in the blood can,
if allowed to continue, predispose the client to respiratory acidosis, a potentially lethal disorder.
Atelectasis. When ventilation is decreased, pooled
secretions may accumulate in a dependent area of a
bronchiole and effectively block it. Because of changes
in regional blood flow, bedrest decreases the amount
of surfactant produced. (Surfactant enables the alveoli
to remain open.) The combination of decreased surfactant and blockage of a bronchiole with mucus can cause
atelectasis (the collapse of a lobe or of an entire lung)
distal to the mucous blockage. Immobile older, postoperative clients are at greatest risk of atelectasis.
Hypostatic pneumonia. Pooled secretions provide
excellent media for bacterial growth. Under these conditions, a minor upper respiratory infection can evolve
rapidly into a severe infection of the lower respiratory
tract. Pneumonia caused by static respiratory secretions
can severely impair oxygen–carbon dioxide exchange
in the alveoli and is a fairly common cause of death
among weakened, immobile clients, especially heavy
smokers.
Metabolism
•
Decreased metabolic rate. Metabolism refers to the sum
of all the physical and chemical processes by which
M44B_BERM9793_11_GE_C44.indd 1121
•
●
Activity and Exercise
1121
living substance is formed and maintained and by
which energy is made available for use by the body.
The basal metabolic rate (BMR) is the minimal energy
expended for the maintenance of these processes,
expressed in calories per hour per square meter of body
surface. In immobile clients, the basal metabolic rate
and gastrointestinal motility and secretions of various
digestive glands decrease as the energy requirements
of the body decrease.
Negative nitrogen balance. In an active client, a balance exists between protein synthesis (anabolism) and
protein breakdown (catabolism). Immobility creates a
marked imbalance, and the catabolic processes exceed
the anabolic processes. Catabolized muscle mass
releases nitrogen. Over time, more nitrogen is excreted
than is ingested, producing a negative nitrogen balance.
The negative nitrogen balance represents a depletion
of protein stores that are essential for building muscle
tissue and for wound healing.
Anorexia. Loss of appetite (anorexia) occurs because
of the decreased metabolic rate and the increased
catabolism that accompany immobility. Reduced
caloric intake is usually a response to the decreased
energy requirements of the inactive client. If protein intake is reduced, the nitrogen imbalance may
become more pronounced, sometimes so severely
that malnutrition ensues.
Negative calcium balance. A negative calcium balance occurs as a direct result of immobility. Greater
amounts of calcium are extracted from bone than can be
replaced. The absence of weight bearing and of stress
on the musculoskeletal structures is the direct cause of
the calcium loss from bones. Weight bearing and stress
are also required for calcium to be replaced in bone.
Urinary System
•
Urinary stasis. In a mobile client, gravity plays an
important role in the emptying of the kidneys and the
bladder. The shape and position of the kidneys and
active kidney contractions are important in completely
emptying the urine from the calyces, renal pelvis, and
ureters (Figure 44.37A ■). The shape and position of
A
B
Figure 44.37 ■ Pooling of urine in the kidney: A, The client is in an
upright position. B, The client is in a back-lying position.
03/02/2021 18:19
1122
•
•
•
•
•
Unit 10
●
Promoting Physiologic Health
the urinary bladder (the detrusor muscle) and active
bladder contractions are also important in achieving
complete emptying.
When the client remains in a horizontal position,
gravity impedes the emptying of urine from the kidneys and the urinary bladder. To urinate, the client
who is supine (in a back-lying position) must push
upward, against gravity (Figures 44.37B). The renal
pelvis may fill with urine before it is pushed into
the ureters. Emptying is not as complete, and urinary
stasis (stoppage or slowdown of flow) occurs after a
few days of bedrest. Because of the overall decrease
in muscle tone during immobilization, including the
tone of the detrusor muscle, bladder emptying is further compromised.
Renal calculi. In a mobile client, calcium in the
urine remains dissolved because calcium and citric
acid are balanced in appropriately acidic urine. With
immobility and the resulting excessive amounts of
calcium in the urine, this balance is no longer maintained. The urine becomes more alkaline, and the
calcium salts precipitate out as crystals to form renal
calculi (stones). In an immobile client in a horizontal position, the renal pelvis filled with stagnant,
alkaline urine is an ideal location for calculi to form.
The stones usually develop in the renal pelvis and
pass through the ureters into the bladder. As the
stones pass along the long, narrow ureters, they
cause extreme pain and bleeding and can sometimes
obstruct the urinary tract.
Urinary retention. The immobile client may suffer
from urinary retention (accumulation of urine in the
bladder), bladder distention, and occasionally urinary
incontinence (involuntary urination). The decreased
muscle tone of the urinary bladder inhibits its ability to
empty completely. In addition, the discomfort of using
a bedpan or urinal, the embarrassment and lack of privacy associated with this function, and the unnatural
position for urination combine to make it difficult for
the client to relax the perineal muscles sufficiently to
urinate while lying in bed.
When urination is not possible, the bladder gradually becomes distended with urine. The bladder may
stretch excessively, eventually inhibiting the urge to
void. When bladder distention is considerable, some
involuntary urinary “dribbling” may occur (retention
with overflow). This does not relieve the urinary distention, because most of the stagnant urine remains in
the bladder.
Urinary infection. Static urine provides an excellent
medium for bacterial growth. The flushing action of normal, frequent urination is absent, and urinary distention
often causes minute tears in the bladder mucosa, allowing infectious organisms to enter. The increased alkalinity of the urine caused by the hypercalcuria supports
bacterial growth. The organism most commonly causing
M44B_BERM9793_11_GE_C44.indd 1122
urinary tract infections is Escherichia coli, which normally
resides in the colon. The normally sterile urinary tract
may be contaminated by improper perineal care, the use
of an indwelling urinary catheter, or occasionally urinary
reflux (backward flow). During reflux, contaminated
urine from an overly distended bladder backs up into
the renal pelvis to contaminate the kidney pelvis as well.
Gastrointestinal System
Constipation is a frequent problem for immobilized clients
because of decreased peristalsis and colon motility. The
overall skeletal muscle weakness affects the abdominal
and perineal muscles used in defecation. When the stool
becomes very hard, more strength is required to expel it.
The immobile client may lack this strength. This can lead
to impaction.
A client’s unnatural and uncomfortable position on
a bedpan does not facilitate elimination. The backwardleaning posture does not promote effective use of the muscles used in defecation. Some clients are reluctant to use
the bedpan in the presence of others. The embarrassment,
lack of privacy, dependence on others to assist with the
bedpan, and disruption of normal bowel habits may cause
the client to postpone or ignore the urge for elimination.
Repeated postponement eventually suppresses the urge
and weakens the defecation reflex.
Some clients may make excessive use of the Valsalva
maneuver by straining at stool in an attempt to expel
the hard stool. This effort dangerously increases intraabdominal and intrathoracic pressures and places undue
stress on the heart and circulatory system.
Integumentary System
•
•
Reduced skin turgor. The skin can atrophy as a result
of prolonged immobility. Shifts in body fluids between
the fluid compartments can affect the consistency
and health of the dermis and subcutaneous tissues
in dependent parts of the body, eventually causing a
gradual loss in skin elasticity.
Skin breakdown. Normal blood circulation relies on
muscle activity. Immobility impedes circulation and
diminishes the supply of nutrients to specific areas.
As a result, skin breakdown and formation of pressure
injuries can occur.
Psychoneurologic System
Due to a decline in production of mood-elevating substances such as endorphins, individuals experience negative effects on mood when unable to engage in physical
activity. Clients who are unable to carry out the usual
activities related to their roles (e.g., as employee, husband, mother, or athlete) become aware of an increased
dependence on others. These factors lower the client’s
03/02/2021 18:20
Chapter 44
self-esteem. Frustration and the decrease in self-esteem
may in turn provoke exaggerated emotional reactions.
Emotional reactions vary considerably. Some clients
become apathetic and withdrawn, some regress, and some
become angry and aggressive.
Because the immobilized client’s participation in
life becomes much narrower and the variety of stimuli
decreases, the client’s perception of time intervals deteriorates. Problem-solving and decision-making abilities may
deteriorate as a result of lack of intellectual stimulation
and the stress of the illness and immobility. In addition,
the loss of control over events can cause anxiety.
NURSING MANAGEMENT
Assessing
Assessment of a client’s activity and exercise should
be routinely addressed and includes a nursing history
and a physical examination of body alignment, gait,
appearance and movement of joints, capabilities and
limitations for movement, muscle mass and strength,
activity tolerance, problems related to immobility, and
physical fitness.
The nurse collects information from the client, from
other nurses, and from the client’s records. The examination and history are important sources of information
about disabilities affecting the client’s mobility and activity status, such as contractures, edema, pain in the extremities, or generalized fatigue.
●
Activity and Exercise
1123
Assessment Interview. If the client indicates a recent pattern
change or difficulties with mobility, a more detailed history
is required. This detailed history should include the specific
nature of the problem, when it first began, its frequency, its
causes if known, how the problem affects daily living, what
the client is doing to cope with the problem, and whether
these methods have been effective.
Physical Examination
Conduct the physical examination focusing on activity
and exercise patterns. The exam includes assessment of
body alignment, gait, appearance and movement of joints,
capabilities and limitations for movement, muscle mass
and strength, activity tolerance, and problems related to
immobility.
Body Alignment
Assessment of body alignment includes an inspection of
the client while the client stands. The purpose of body
alignment assessment is to identify:
•
•
•
•
Normal developmental variations in posture
Posture and learning needs to maintain good posture
Factors contributing to poor posture, such as fatigue,
pain, compression fractures, or low self-esteem
Muscle weakness or other motor impairments.
Nursing History
To assess alignment, the nurse inspects the client from
lateral (Figure 44.38A ■), anterior, and posterior perspectives. From the anterior and posterior views, the nurse
should observe whether:
An activity and exercise history is usually part of the comprehensive nursing history. Examples of interview questions to elicit these data are shown in the accompanying
•
•
•
The shoulders and hips are level
The toes point forward
The spine is straight, not curved to either side.
•
Do you ever experience dizziness, shortness of breath, marked
increase in respiratory rate, or other problems following mild or
moderate activity?
ASSESSMENT INTERVIEW Activity and Exercise
DAILY ACTIVITY LEVEL
• What activities do you carry out during a routine day?
• Are you able to carry out the following tasks independently?
a. Eating
b. Dressing and grooming
c. Bathing
d. Toileting
e. Ambulating
f. Using a wheelchair
g. Transferring in and out of bed, bath, and car
h. Cooking
i. House cleaning
j. Shopping
• Where problems exist in your ability to carry out such tasks:
a. Would you rate yourself as partially or totally dependent?
b. How is the task achieved (by family, friend, agency, or use
of specialized equipment)?
ACTIVITY TOLERANCE
• What types of activities make you tired?
M44B_BERM9793_11_GE_C44.indd 1123
EXERCISE
• What type of exercise do you carry out to enhance your physical fitness?
• What is the frequency and length of this exercise session?
• Do you believe exercise is beneficial to your health? Explain.
FACTORS AFFECTING MOBILITY
• Environmental factors. Do stairs, lack of railings or other assistive devices, or an unsafe neighborhood impede your mobility
or exercise regimen?
• Health problems. Do any of the following health problems affect
your muscle strength or endurance: heart disease, lung disease, stroke, cancer, neuromuscular problems, musculoskeletal
problems, visual or mental impairments, trauma, or pain?
• Financial factors. Are your finances adequate to obtain equipment or other aids that you require to enhance your mobility?
03/02/2021 18:20
1124
Unit 10
●
Promoting Physiologic Health
A
Figure 44.38 ■ A standing person with A, good trunk alignment;
B, poor trunk alignment. The arrows indicate the direction in which the
pelvis is tilted.
The “slumped” posture (Figure 44.38B) is the most
common problem that occurs when people stand. The
neck is flexed far forward, the abdomen protrudes, the
pelvis is thrust forward to create lordosis (an exaggerated
anterior or inward curvature of the lumbar spine), and
the knees are hyperextended. Low back pain and fatigue
occur quickly in people with poor posture.
Gait
The characteristic pattern of a client’s gait (walk) is
assessed to determine the client’s mobility and risk for
injury due to falling. Two phases of normal gait are swing
and stance (Figure 44.39 ■). When one leg is in the swing
phase, the other is in the stance phase. In the stance phase,
(a) the heel of one foot strikes the ground, and (b) body
weight is spread over the ball of that foot while the other
heel pushes off and leaves the ground. In the swing phase,
the leg from behind moves in front of the body.
The nurse assesses gait as the client walks into the
room or asks the client to walk a distance of 10 feet down
a hallway and observes for the following:
•
•
•
•
•
Chin is level, gaze is straight ahead, sternum is lifted,
and shoulders are down and back, relaxed away from
the ears.
Heel strikes the ground before the toe. It is here, where
both feet are taking some body weight, that the spine
is most rotated.
Feet are dorsiflexed in the swing phase.
Arm opposite the swing-through foot moves forward
at the same time.
Gait is smooth, coordinated, and rhythmic, with even
weight borne on each foot. Hips gently sway with spinal rotation; the body moves forward smoothly, stopping and starting with ease.
M44B_BERM9793_11_GE_C44.indd 1124
Swing phase
begins
B
Stance phase
Swing phase
completed
Figure 44.39 ■ The swing and stance phases of a normal gait.
The nurse may also assess pace (the number of steps
taken per minute), which often slows with age and disability. A normal walking pace is 70 to 100 steps per minute.
The pace of an older adult may slow to about 40 steps per
minute.
The nurse should also note the client’s need for a prosthesis or assistive device, such as a cane or walker. For
a client who uses assistive aids, the nurse assesses gait
without the device and compares the assisted and unassisted gaits.
Appearance and Movement of Joints
Physical examination of the joints involves inspection,
palpation, assessment of range of active motion, and if
active motion is not possible, assessment of range of passive motion. The nurse should assess the following:
•
•
•
•
•
•
•
Any joint swelling or redness, which could indicate the
presence of an injury or an inflammation
Any deformity, such as a bony enlargement or contracture, and symmetry of involvement
The muscle development associated with each joint and
the relative size and symmetry of the muscles on each
side of the body
Any reported or palpable tenderness
Crepitation (palpable or audible crackling or grating
sensation produced by joint motion and frequently
experienced in joints that have suffered repeated
trauma over time)
Increased temperature over the joint; palpate the joint
using the backs of the fingers and compare the temperature with that of the symmetric joint
Degree of joint movement; ask the client to move
selected body parts as shown in Table 44.2.
Assessment of range of motion should not be unduly
fatiguing, and the joint movements need to be performed
03/02/2021 18:20
Chapter 44
smoothly, slowly, and rhythmically. No joint should be
forced. Uneven, jerky movement and forcing can injure
the joint and its surrounding muscles and ligaments.
Capabilities and Limitations for Movement
The nurse needs to obtain data that may indicate hindrances or restrictions to the client’s movement and the
need for assistance, including the following:
•
•
•
•
•
•
•
How the client’s illness influences the ability to move
and whether the client’s health contraindicates any
exertion, position, or movement
Limitations to movement, such as an IV line in place
or a heavy cast
Mental alertness and ability to follow directions; check
whether the client is receiving medications that hinder
the ability to walk safely. Narcotics, sedatives, tranquilizers, and some antihistamines cause drowsiness, dizziness, weakness, and orthostatic hypotension.
Balance and coordination
Presence of orthostatic hypotension before transfers;
specifically, assess for any increase in pulse rate, marked
fall in blood pressure, dizziness, light-headedness, and
dimming of vision when the client moves from a supine
to a vertical posture.
Degree of comfort (Clients who have pain may not
want to move and may require an analgesic before they
are moved.)
Vision: Is it adequate to prevent falls?
The nurse also assesses the amount of assistance the client
requires for the following:
•
•
•
•
Moving in the bed. In particular, observe for the amount
of assistance the client requires for turning:
a. From a supine position to a lateral position
b. From a lateral position on one side to a lateral position on the other
c. From a supine position to a sitting position in bed.
Rising from a lying position to a sitting position on the
edge of the bed. Healthy individuals can normally rise
without support from the arms.
Rising from a chair to a standing position. Normally
this can be done without pushing with the arms.
Coordination and balance. Determine the client’s abilities to hold the body erect, to bear weight and keep
balance in a standing position on both legs or only
one, to take steps, and to push off from a chair or bed.
Muscle Mass and Strength
Before the client undertakes a change in position or attempts
to ambulate, it is essential for the nurse to assess the client’s
strength and ability to move. Providing appropriate assistance decreases the risk of muscle strain and body injury to
both the client and nurse. Assessment of upper extremity
strength is especially important for clients who use ambulation aids, such as walkers and crutches. For information on
how to determine muscle mass and strength in lower and
upper extremities, see Chapter 29 .
M44B_BERM9793_11_GE_C44.indd 1125
●
Activity and Exercise
1125
Physical Energy for Activities
By determining an appropriate activity level for a client, the nurse can predict whether the client has the
strength and endurance to participate in activities that
require similar amounts of energy. This assessment is
useful in encouraging increasing independence in clients
who (a) have a cardiovascular or respiratory disability,
(b) have been completely immobilized for a prolonged
period, (c) have decreased muscle mass or a musculoskeletal disorder, (d) have experienced inadequate sleep,
(e) have experienced pain, or (f) are depressed, anxious,
or unmotivated.
The most useful measures in predicting activity tolerance are heart rate, strength, and rhythm; respiratory rate,
depth, and rhythm; and blood pressure. These data are
obtained at the following times:
•
•
•
•
Before the activity starts (baseline data), while the client is at rest
During the activity
Immediately after the activity stops
Three minutes after the activity has stopped and the
client has rested.
The activity should be stopped immediately in the
event of any physiologic change indicating the activity is
too strenuous or prolonged for the client. These changes
include the following:
•
•
•
•
•
•
•
•
Sudden facial paleness
Feelings of dizziness or weakness
Change in level of consciousness
Heart rate or respiratory rate that significantly exceeds
baseline or preestablished levels
Change in heart or respiratory rhythm from regular to
irregular
Weakening of the pulse
Dyspnea, shortness of breath, or chest pain
Diastolic blood pressure change of 10 mmHg or more.
If, however, the client tolerates the activity well, and
if the client’s heart rate returns to baseline levels within
5 minutes after the activity ceases, the activity is considered safe. This activity, then, can serve as a standard for
predicting the client’s tolerance for similar activities.
Problems Related to Immobility
When collecting data pertaining to the problems of
immobility, the nurse uses the assessment methods
of inspection, palpation, and auscultation; checks results of
laboratory tests; and takes measurements, including body
weight, fluid intake, and fluid output. Specific techniques
for assessing immobility problems and abnormal assessment findings related to the complications of immobility
are listed in Table 44.3.
It is extremely important to obtain and record baseline
assessment data soon after the client first becomes immobile. These baseline data serve as the standard against
which all data collected throughout the period of immobilization are compared.
03/02/2021 18:20
1126
Unit 10
●
Promoting Physiologic Health
ANATOMY & PHYSIOLOGY REVIEW
Upper and Lower Body Integration and the Spine’s Role in Locomotion
It is important to be aware of the connection between the
upper and lower body in terms of function, comfort, and
mobility. The iliopsoas muscles (hip flexors) allow us to stand
upright and are crucial for spinal alignment and locomotion.
Prolonged sitting and inactivity can shorten these muscles,
compromising mobility, function, and comfort in the back,
hips, and legs. The shoulder blades and surrounding muscles
are a major part of the shoulder girdle and allow the arms to
be in relationship with the back. Muscular imbalance in the
shoulder girdle will cause dysfunctional movement patterns
throughout the body, including the spine. Balanced strength
in the pelvic muscles enhances back stability and alignment
of the feet and legs. Muscular imbalance in the pelvis will
also cause dysfunctional movement patterns throughout the
body, including the cervical and thoracic spine. All of these
considerations affect total body alignment, comfort, and gait.
Proper alignment and function lead to greater efficiency of
movement and conservation of energy.
It is theorized that gait originates in the spine rather
than in the legs. This “spinal engine” theory (developed
by S. A. Gracovetsky) rejects the notion that locomotion is
a function of leg movement with the trunk being passively
carried along. Rather, motion in the spine and surrounding tissues precedes that of the legs, making the spine the
basic engine of locomotion. The contralateral swinging of
each leg with the opposite arm (e.g., the right arm swings
forward with the left leg and vice versa) constitutes the
rhythm of a normal gait with free motion in the shoulders
and hips. The coordinated and fluid connection between
upper and lower body motion indicates overall balance,
energy efficiency, and comfort in movement.
Nursing Implications: Nurses should keep upper–lower
body connection and spinal rotation in mind when evaluating gait, and encourage clients to walk with flowing
contralateral movement between upper and lower limbs
and a loose, rhythmic swing in the hips.
T1
T2
T3
T4
T5
T6
T7
T8
T9
T10
T11
T12
L1
L2
L3
L4
L5
-8 -4 0
Degrees
4
8
Psoas
Iliopsoas
muscles
Iliacus
Spinal rotation precedes locomotion.
The iliopsoas muscle is frequently regarded as a single muscle because it is
a blending of two muscles, the psoas and the iliacus. The psoas originates
on the lumbar vertebrae and attaches to the femur. The iliacus originates
on the pelvic crest and attaches to the femur. The connection between the
spine and legs is evident when visualizing the iliopsoas muscles.
M44B_BERM9793_11_GE_C44.indd 1126
QUESTIONS
1. Why might someone with a foot or knee problem
develop low back pain?
2. Why is contralateral movement of the upper and
lower limbs important in a fluid, balanced gait?
Answers to Anatomy & Physiology Review Questions are available on the faculty resources
site. Please consult with your instructor.
03/02/2021 18:20
Chapter 44
TABLE 44.3
●
Activity and Exercise
1127
Assessing Problems of Immobility
Assessment
Problem
MUSCULOSKELETAL SYSTEM
Measure arm and leg circumferences.
Palpate and observe body joints.
Take goniometric measurements of joint ROM.
Decreased circumference due to decreased muscle mass
Stiffness or pain in joints
Decreased joint ROM, joint contractures
CARDIOVASCULAR SYSTEM
Auscultate the heart.
Measure blood pressure.
Palpate and observe sacrum, legs, and feet.
Palpate peripheral pulses.
Measure calf muscle circumferences.
Observe calf muscles for redness, tenderness, and swelling.
RESPIRATORY SYSTEM
Observe chest movements.
Auscultate chest.
Increased heart rate
Orthostatic hypotension
Peripheral dependent edema, increased peripheral vein
engorgement
Weak peripheral pulses
Edema
Thrombophlebitis
Asymmetric chest movements, dyspnea
Diminished breath sounds, crackles, wheezes, and increased respiratory rate
METABOLIC SYSTEM
Measure height and weight.
Palpate skin.
Weight loss due to muscle atrophy and loss of subcutaneous fat
Generalized edema due to low blood protein levels
URINARY SYSTEM
Measure fluid intake and output.
Inspect urine.
Palpate urinary bladder.
Dehydration
Cloudy, dark urine; high specific gravity
Distended urinary bladder due to urinary retention
GASTROINTESTINAL SYSTEM
Observe stool.
Auscultate bowel sounds.
Hard, dry, small stool
Decreased bowel sounds due to decreased intestinal motility
INTEGUMENTARY SYSTEM
Inspect skin.
Break in skin integrity
PSYCHONEUROLOGIC SYSTEM
Observe behaviors, affect, and cognition. Monitor developmental
skills in children.
Because a major nursing responsibility is to prevent
the complications of immobility, the nurse needs to identify clients at risk of developing such complications before
problems arise. Clients at risk include those who (a) are
poorly nourished; (b) have decreased sensitivity to pain,
temperature, or pressure; (c) have existing cardiovascular,
pulmonary, or neuromuscular problems; and (d) have an
altered level of consciousness.
Diagnosing
Mobility problems may be appropriate as the diagnostic
label or as the etiology for other nursing diagnoses. Example
of nursing diagnoses for clients with mobility problems can
include inadequate physical energy for activities; potential
for inadequate physical energy for activities; altered physical
mobility (specify, such as with walking or transferring); inactive lifestyle; and decline in health (from inactivity).
Depending on the data obtained, problems with
mobility often affect other areas of human functioning and
indicate other diagnoses. In these instances, the mobility
problem becomes the etiology. The etiology needs to be
M44B_BERM9793_11_GE_C44.indd 1127
Anger, flat affect, crying, confusion, anxiety, decline in cognitive
function, or signs such as sleep and appetite disturbances warrant
further evaluation
described more clearly in terms such as reduced ROM,
neuromuscular impairment or musculoskeletal impairment of upper and lower extremities, or joint pain. Examples in which inadequate physical energy for activities is
the etiology can include fear (of falling), potential for falling, and impaired self-esteem.
When problems associated with prolonged immobility arise, many other nursing diagnoses may be necessary.
Examples include, but are not limited to the following:
altered respiratory status, if there is stasis of pulmonary
secretions; potential for infection, if there is stasis of urinary or pulmonary secretions; and potential for impaired
self-esteem, if there is functional impairment or role
disturbance.
Planning
When planning for desired outcomes, Nursing Outcomes
Classification (NOC) labels that pertain to exercise and
activity can be helpful and include the following: activity
tolerance; ambulation; balance; body positioning; coordinated movement; endurance; fall prevention behavior;
03/02/2021 18:20
1128
Unit 10
●
Promoting Physiologic Health
fatigue level; immobility consequences, both physiologic
and psycho-cognitive; joint movement; mobility; physical
fitness; play participation; and self-care (Moorhead, Swanson, Johnson, & Maas, 2018).
Positioning, transferring, and ambulating clients are
almost always independent nursing functions. The primary care provider usually orders specific body positions
only after surgery, anesthesia, or trauma involving the
nervous and musculoskeletal systems. All clients should
have an activity order written by their primary care provider when they are admitted to the agency for care.
As part of planning, the nurse is responsible for identifying those clients who need assistance with body alignment and determining the degree of assistance they need.
The nurse must be sensitive to the client’s need to function
as independently as possible yet provide assistance when
the client needs it.
Most clients require some nursing guidance and
assistance to learn about, achieve, and maintain proper
body mechanics. The nurse should also plan to teach clients applicable skills. For example, a client with a back
injury needs to learn how to get out of bed safely and
comfortably, a client with an injured leg needs to learn
how to transfer from bed to wheelchair safely, and a client with a newly acquired walker needs to learn how
to use it safely. Nurses often teach family members or
caregivers safe moving, lifting, and transfer techniques
in the home setting.
The goals established for clients will vary according
to the nursing diagnosis and signs and symptoms related
to each individual. Examples of overall goals for clients
with actual or potential problems related to mobility or
activity follow.
The client will have:
•
•
•
•
Increased tolerance for physical activity
Restored or improved capability to ambulate and participate in ADLs
Absence of injury from falling or improper use of body
mechanics
Absence of any complications associated with
immobility.
Examples of desired outcomes, interventions, and
activities are provided in the Nursing Care Plan and Concept Map on pages 1159–1161.
Planning for Home Care
Clients who have been hospitalized for activity or mobility
problems often need continued care in the home. In preparation for discharge, the nurse needs to determine the client’s actual and potential health problems, strengths, and
resources.
QSEN
Safety: Assessment Data for Discharge Plan
Following is the specific assessment data required for the
nurse to address before establishing a discharge plan for
clients with mobility or activity problems.
M44B_BERM9793_11_GE_C44.indd 1128
CLIENT AND ENVIRONMENT
•
•
•
•
•
Capabilities or tolerance for required and desired
activities: self-care (feeding, bathing, toileting, dressing, grooming, home maintenance, shopping, cooking);
recreational activities
Mobility aids required: cane, walker, crutches, wheelchair, transfer boards
Equipment required if immobilized: special bed, side rails,
pressure-reducing mattress, assistive lifting equipment
Current level of knowledge: body mechanics for use of
mobility aids; specific exercises prescribed
Home mobility hazard appraisal: adequacy of lighting;
presence of handrails; safety of pathways and stairs;
congested areas; unanchored rugs, mats, or electrical
cords, and any other obstacles to safe movement; structural adjustments needed for wheelchair access
FAMILY OR CAREGIVER
•
•
•
Caregiver availability, skills, and willingness to assist:
assess learning needs and develop appropriate teaching plan, primary people able to assist client with selfcare, movement, shopping, and so on; physical and
emotional status to assist with care
Family role changes and coping: effect on financial status, parenting and spousal roles, social roles
Availability of caregiver support: other support people
available for occasional duties such as shopping, transportation, housekeeping, cooking, budgeting; refer to
community agencies for respite care, where appropriate
COMMUNITY
•
Resources: availability and familiarity with sources of
medical equipment and assistive lifting equipment,
financial assistance, homemaker services, hygienic
care; Meals on Wheels; spiritual counselors and visitors; sources of respite for the caregiver
A major aspect of discharge planning involves instructional needs of the client and family. See Client Teaching
features throughout this chapter.
Implementing
Nurses can initiate and apply a wide variety of exercise
and activity interventions as needed to address a multitude of client concerns. Nursing Interventions Classification (NIC) labels that pertain to exercise and activity
include the following: activity therapy; cardiac care; rehabilitation; constipation management; exercise promotion
(strength and stretching); exercise therapy (ambulation,
balance, joint mobility, muscle control); fall prevention;
health education; mood management; pelvic muscle exercise; pressure ulcer prevention; progressive muscle relaxation; recreation therapy; self-care assistance; self-esteem
enhancement; simple relaxation therapy; sleep enhancement; sports-injury prevention; teaching: prescribed activity and exercise; therapeutic play; weight management;
and weight reduction (Butcher, Bulechek, Dochterman, &
Wagner, 2018).
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1129
CLIENT TEACHING Home Care Activity and Exercise
MAINTAINING MUSCULOSKELETAL FUNCTION
• Teach the systematic performance of passive or assistive ROM
exercises to maintain joint mobility.
• Demonstrate, as appropriate, the proper way to perform isotonic, isometric, or isokinetic exercises to maintain muscle
mass and tone (collaborate with the physical therapist about
these). Incorporate ADLs into exercise program if appropriate.
• Provide a written schedule for the type, frequency, and duration
of exercises; encourage the use of a progress graph or chart to
facilitate adherence with the therapy.
• Offer an ambulation schedule.
• Instruct in the availability of assistive ambulatory devices and
correct use of them.
• Discuss pain control measures required before exercise.
PREVENTING INJURY
• Provide assistive devices for moving and transferring, whenever
possible, and teach safe transfer and ambulation techniques.
• Discuss safety measures to avoid falls (e.g., locking wheelchairs, wearing appropriate footwear, using rubber tips on
crutches, keeping the environment safe, and using mechanical
aids such as raised toilet seat, grab bars, urinal, and bedpan or
commode to facilitate toileting).
Nursing strategies to maintain or promote body
alignment and mobility involve positioning clients
appropriately, moving and turning clients in bed, transferring clients, providing ROM exercises, ambulating
clients with or without mechanical aids, and strategies
to prevent the complications of immobility. Whenever
positioning, moving, and ambulating clients, nurses
must use assistive lifting or moving equipment and
proper body mechanics to avoid musculoskeletal strain
and injury.
Preventing Musculoskeletal Disorders (MSDs)
Nurses provide clients with the opportunity to change
positions, expand their lungs, or change their environments as appropriate. It is important, however, that nurses
not put their own health at risk while caring for clients.
Client positioning, lifting, and transferring are significant
risk factors for developing MSDs.
In the field of nursing, MSDs such as back and shoulder injuries persist as the leading and most costly U.S.
occupational health problem. Manually moving and lifting clients often cause MSDs. The term patient handling
injury (PHI) has become a recognized term for identifying
nurses’ injuries caused by direct client care. A literature
review (Fragala et al., 2016, p. 41) resulted in the identification of four major risk factors for PHIs in nurses:
1. Exertion. The amount of exertion or effort required to
lift, move, or handle a client depends on factors such
as the client’s size, need for assistance, cognitive status, and ability and willingness to actively participate
in the move.
2. Frequency. This refers to the number of times a
nurse performs client-handling tasks during a shift.
M44B_BERM9793_11_GE_C44.indd 1129
•
Teach ways to prevent postural hypotension.
MANAGING ENERGY TO PREVENT FATIGUE
• Discuss activity and rest patterns and develop a plan as indicated; intersperse rest periods with activity periods.
• Discuss ways to minimize fatigue such as performing activities
more slowly and for shorter periods, resting more often, and
using more assistance as required.
• Provide information about available resources to help with ADLs
and home maintenance management.
• Teach ways to increase energy (e.g., increasing intake of highenergy foods, ensuring adequate rest and sleep, controlling
pain, sharing feelings with a trusted listener).
• Teach techniques to monitor activity tolerance as appropriate.
REFERRALS
• Provide appropriate information about accessing community
resources: home care agencies, physical and occupational
therapy agencies, local YMCAs and other agencies that provide
structured exercise and movement programs, and sources of
adaptive equipment.
Examples include pulling a client up in bed, turning a
client, and performing a lateral transfer.
3. Posture or the nurse’s body position when performing client-handling activities. Reaching across beds
or other equipment with arms extended can lead to
undesirable postures. Working in a confined space,
causing nurses to assume awkward postures, and
twisting the back while bending are other examples
that affect posture and can increase PHI.
4. Duration of exposure or the cumulative effects of exertion, frequency, and position.
Increasingly, healthcare facilities are focusing on “no
lift” policies for their employees, and 35 pounds of client
weight should be the maximum a nurse should attempt.
If the weight to be lifted exceeds 35 pounds or the risk factors exist, assistive devices should be used. These devices
include floor-based and ceiling lifts; slings; sit-to-stand
assist devices; sliding boards; friction-reducing devices;
transfer sheets or power-assist, air-cushioned mattresses;
and lateral transfer and transport chairs.
The American Nurses Association (ANA) has been
involved in the effort to protect nurses from MSDs for
many years and has taken the official position of supporting actions and policies that result in the elimination
of manual handling of clients in order to establish a safe
environment for nurses and clients. Evidence has shown
that safe patient handling and mobility (SPHM) programs
greatly reduce healthcare worker injuries (Teeple et al.,
2017; Walker, Docherty, Hougendobler, Guanowsky, &
Rosenthal, 2017). In 2003, the ANA launched a national
Handle with Care campaign to prevent MSDs. As a result,
11 states have enacted “safe patient handling” laws or initiated rules and regulations related to the implementation
03/02/2021 18:20
1130
Unit 10
●
Promoting Physiologic Health
of SPHM programs (Weinmeyer, 2016). However, there is
not consistency among these 11 states. For example, one
state requires replacing manual lifting with lifting devices
and another state requires healthcare facilities to develop
a comprehensive safe patient handling plan.
In 2013, the Centers for Medicare and Medicaid
Services (CMS), the Institute of Medicine (IOM),
the World Health Organization (WHO), the National
Quality Foundation (NQF), and the ANA supported the
concepts of universal standards and an interdisciplinary
approach to SPHM. This resulted in the publication of
Safe Patient Handling and Mobility Interprofessional National
Standards Across the Care Continuum. These standards
are voluntary performance standards to help healthcare
facilities establish policies and procedures. It is the hope,
however, that similar to the requirement of standard
precautions, the Safe Patient Handling and Mobility
Standards will become required instead of optional.
To this end, the ANA worked with congressional bill
sponsors in support of national legislation, which
resulted in the Nurse and Health Care Worker Protection
Act of 2015. Future action on this bill, however, remains
to be seen (Weinmeyer, 2016).
Until all work settings provide safe environments
in which nurses have the equipment they need, content pertaining to body mechanics will be included
here. Readers are encouraged to support “no manual
lift” and “no solo lift” policies in their workplaces, and
to become involved in legislation and equipment purchase initiatives. Nurses must participate in this safety
awareness, and are encouraged to support the Safe
Patient Handling and Mobility Standards of the ANA
and to keep informed of congressional action on bills to
enforce safer client handling.
Recently, the VA produced a Safe Patient Handling
app for healthcare professionals. This app provides evidence-based SPHM techniques to prevent injury of both
healthcare workers and clients. The app includes comprehensive client assessments, scoring and other algorithms for specific client handling tasks, and pictures and
video clips of a variety of client handling and mobility
technologies.
Clinical Alert!
MSDs are caused by force, repetition, and awkward positions.
The most common injuries among healthcare workers are low back
pain, herniated disks, strained muscles, pulled or torn ligaments,
and disk degradation.
Using Body Mechanics
Body mechanics is the term used to describe the efficient,
coordinated, and safe use of the body to move objects
and carry out the ADLs. When an individual moves, the
center of gravity shifts continuously in the direction of
the moving body parts. Balance depends on the interrelationship of the center of gravity, the line of gravity,
and the base of support. The closer the line of gravity
is to the center of the base of support, the greater the
individual’s stability (Figure 44.40A ■). Conversely, the
closer the line of gravity is to the edge of the base of support, the more precarious the balance (Figure 44.40B). If
the line of gravity falls outside the base of support, the
individual falls (Figure 44.40C).
Body balance can be greatly enhanced by (a) widening
the base of support and (b) lowering the center of gravity,
bringing it closer to the base of support. Spreading the feet
farther apart widens the base of support. Flexing the hips
Center of
gravity
Line of
gravity
Base of
support
A
B
C
Figure 44.40 ■ A, Balance is maintained when the line of gravity falls close to the base of support. B, Balance is precarious when the line of gravity
falls at the edge of the base of support. C, Balance cannot be maintained when the line of gravity falls outside the base of support.
M44B_BERM9793_11_GE_C44.indd 1130
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1131
and knees until achieving a squatting position lowers the
center of gravity. The importance of these alterations cannot be overemphasized for nurses.
Historically, nurses believed that “correct” body
mechanics would assist in the safe and efficient use of
appropriate muscle groups to maintain balance, reduce
the energy required, reduce fatigue, and decrease the risk
of injury for both nurses and clients, especially during
transferring, lifting, and repositioning. In reality, more
than 30 years of evidence show that:
•
•
•
•
•
•
Educating nurses in body mechanics alone will not
prevent job-related injuries.
Back belts have not been shown to be effective in reducing back injury.
Nurses who are physically fit are at no less risk of
injury.
The formerly accepted National Institute for Occupational
Safety and Health (NIOSH) “lifting equation,” which recommended that workers observe a limit of 51 pounds of
lifting, cannot be safely applied to nursing practice.
The long-term benefits of using the proper equipment
(e.g., mechanical lifts) far outweigh the costs related to
injuries.
Staff will use equipment when they have participated
in the decision-making process for purchasing the
equipment
Figure 44.42 ■ A ceiling-mounted lift.
Shirlee Snyder.
Lifting
It is important to remember that nurses should not lift
more than 35 pounds without assistance from proper
equipment or other individuals. Types of assistive equipment include mobile-powered or mechanical lifts, ceilingmounted lifts, sit-to-stand powered lifts, friction-reducing
devices, and air transfer systems. See Figure 44.41 ■
through Figure 44.45 ■. There are also transfer chairs that
can transfer the client laterally from bed to stretcher without lifting and then convert to a sitting or reclining position to transport the client through the facility.
Figure 44.43 ■ A sit-to-stand power lift allows for client transfers
from bed to chair. The client must be cognitive and provide some muscle
tone in at least one leg and the trunk.
belushi/Shutterstock.
Figure 44.41 ■ A mobile electric lift functions to lift clients from bed,
chair, toilet, and floor.
M44B_BERM9793_11_GE_C44.indd 1131
Figure 44.44 ■ Friction-reducing transfer device with handles.
03/02/2021 18:20
1132
Unit 10
●
Promoting Physiologic Health
Figure 44.45 ■ An air transfer system. Once inflated, the client can
be transferred laterally or repositioned on a frictionless air surface.
Pulling and Pushing
When pulling or pushing an object, an individual maintains balance with the least effort when the base of support is increased in the direction in which the movement
is to be produced or opposed. For example, when pushing an object, an individual can enlarge the base of support by moving the front foot forward. When pulling
an object, an individual can enlarge the base of support
by (a) moving the rear leg back if facing the object or
(b) moving the front foot forward if facing away from the
object. It is easier and safer to pull an object toward your
own center of gravity than to push it away, because you
can exert more control of the object’s movement when
pulling it.
are essential aspects of nursing practice. Clients who can
move easily automatically reposition themselves for comfort. Such clients generally require minimal positioning
assistance from nurses, other than guidance about ways
to maintain body alignment and to exercise their joints.
However, clients who are weak, frail, in pain, paralyzed,
or unconscious rely on nurses to provide or assist with
position changes. For all clients, it is important to assess
the skin and provide skin care before and after a position
change.
Any position, correct or incorrect, can be harmful
if maintained for a prolonged period. Frequent change
of position helps to prevent muscle discomfort, undue
pressure resulting in pressure injuries, damage to superficial nerves and blood vessels, and contractures. Position changes also maintain muscle tone and stimulate
postural reflexes.
When the client is not able to move independently
or assist with moving, the preferred method is for two or
more nurses to move or turn the client and use assistive
equipment. Appropriate assistance reduces the risk of
muscle strain and body injury to both the client and
nurse, and is likely to protect the dignity and comfort
of the client.
When positioning clients in bed, the nurse can do a
number of things to ensure proper alignment and promote
client comfort and safety:
•
•
Clinical Alert!
Lateral-assist devices such as horizontal air transfer mattresses
and transfer chairs are essential equipment for most client care
areas. They help prevent acute and chronic back pain and disability. Observing principles of body mechanics is recommended even
when using assistive equipment, because any lifting and forceful movement is potentially injurious, especially when repeated
over time.
Pivoting
Pivoting is a technique in which the body is turned in a
way that avoids twisting of the spine. To pivot, place one
foot ahead of the other, raise the heels very slightly, and
put the body weight on the balls of the feet. When the
weight is off the heels, the frictional surface is decreased
and the knees are not twisted when turning. Keeping
the body aligned, turn (pivot) about 90 degrees in the
desired direction. The foot that was forward will now
be behind.
Positioning Clients
Positioning a client in good body alignment and changing
the position regularly (every 2 hours) and systematically
M44B_BERM9793_11_GE_C44.indd 1132
•
•
•
Make sure the mattress is firm and level yet has enough
give to fill in and support natural body curvatures.
Ensure that the bed is clean and dry. Wrinkled or damp
sheets increase the risk of pressure injury formation.
Make sure extremities can move freely whenever possible. For example, the top bedclothes need to be loose
enough for clients to move their feet.
Place support devices in specified areas according to
the client’s position. Box 44.1 lists commonly used support devices. Use only those support devices needed to
maintain alignment and to prevent stress on the client’s
muscles and joints. If the client is capable of movement,
too many devices limit mobility and increase the potential for muscle weakness and atrophy.
Avoid placing one body part, particularly one with
bony prominences, directly on top of another body part.
Excessive pressure can damage veins and predispose
the client to thrombus formation. Pressure against the
popliteal space may damage nerves and blood vessels
in this area. Pillows can provide needed cushioning.
Avoid friction and shearing. Friction is a force acting
parallel to the skin surface. For example, sheets rubbing against skin create friction. Friction can abrade the
skin (i.e., remove the superficial layers), making it more
prone to breakdown. Shearing force is a combination of
friction and pressure. It occurs commonly when a client
assumes a sitting position in bed. In this position, the
body tends to slide downward toward the foot of
the bed. This downward movement is transmitted to the
03/02/2021 18:20
Chapter 44
•
sacral bone and the deep tissues. At the same time,
the skin over the sacrum tends not to move because of
sticking to the bed linens. The skin and superficial tissues are thus relatively unmoving in relation to the bed
surface, whereas the deeper tissues are firmly attached
to the skeleton and move downward. This causes a
shearing force in the area where the deeper tissues and
the superficial tissues meet. The force damages the tissues in this area.
Plan a systematic 24-hour schedule for position changes.
Frequent position changes are essential to prevent pressure injuries in immobilized clients. Such clients should
be repositioned every 2 hours throughout the day and
night and more frequently when there is a risk for skin
breakdown. This schedule is usually outlined on the
client’s nursing care plan. The use of visual cues (e.g.,
BOX 44.1
•
•
•
•
•
•
Support Devices
Pillows. Different sizes are available. Used for support
or elevation of an arm or leg. Specially designed dense
pillows can be used to elevate the upper body. Pillows
can also be used as a trochanter roll by placing the
pillow from the client’s iliac crest to midthigh. This prevents external rotation of the leg when the client is in a
supine position.
Mattresses. There are two types of mattresses: ones that
fit on the bed frame (e.g., standard bed mattress) and mattresses that fit on the standard bed mattress (e.g., egg-crate
mattress). Mattresses should be evenly supportive.
Suspension or heel guard boot. These are made of a variety
of substances. They usually have a firm exterior and padding of foam to protect the skin. They prevent foot drop and
relieve pressure on heels.
Footboard. A flat panel often made of plastic or wood. It
keeps the feet in dorsiflexion to prevent plantar flexion.
Hand roll. Can be made by rolling a washcloth. Purpose
is to keep hand in a functional position and prevent finger
contractures.
Abduction pillow. A triangular-shaped foam pillow that maintains hip abduction to prevent hip dislocation following total
hip replacement.
•
●
Activity and Exercise
1133
clock sign with moveable arrows to indicate next turning time) can also serve as reminders.
Always obtain information from the client to determine which position is most comfortable and appropriate. Seeking information from the client about what
feels best is a useful guide when aligning clients and
is an essential aspect of evaluating the effectiveness
of an alignment intervention. Sometimes a client who
appears well aligned may be experiencing real discomfort. Both appearance, in relation to alignment criteria, and comfort are important in achieving effective
alignment.
Fowler’s Position
Fowler’s position, or a semisitting position, is a bed posi-
tion in which the head and trunk are raised 45° to 60°
relative to the bed (visualize a 90° right angle to orient
your thinking) and the knees may or may not be flexed.
Nurses may need to clarify the meaning of the term
Fowler’s position in their particular setting. Typically,
Fowler ’s position refers to a 45° angle of elevation of
the upper body.
Semi-Fowler’s position (Figure 44.46 ■) is when the
head and trunk are raised 15° to 45°. This position is
sometimes called low Fowler’s and typically means 30°
of elevation. In high-Fowler’s position, the head and trunk
are raised 60° to 90°, and most often the client is sitting
upright at a right angle to the bed (Table 44.4).
Fowler’s position is the position of choice for people
who have difficulty breathing and for some people with
heart problems. When the client is in this position, gravity
pulls the diaphragm downward, allowing greater chest
expansion and lung ventilation.
30
A
45-60
B
Maintaining postoperative abduction following total hip replacement.
M44B_BERM9793_11_GE_C44.indd 1133
Figure 44.46 ■ A, Semi-Fowler’s (low-Fowler’s) position (supported);
B, Fowler’s position (supported). The amount of support depends on the
needs of the individual client.
03/02/2021 18:20
1134
Unit 10
●
TABLE 44.4
Promoting Physiologic Health
Fowler’s Position
Unsupported Position
Problem to Be Prevented
Corrective Measure*
Bed-sitting position with upper
part of body elevated 30° to 90°
commencing at hips
Posterior flexion of lumbar
curvature
Pillow at lower back (lumbar
region) to support lumbar region
Head rests on bed surface
Hyperextension of neck
Pillows to support head, neck,
and upper back
Arms fall at sides
Shoulder muscle strain, possible dislocation of shoulders,
edema of hands and arms with
flaccid paralysis, flexion contracture of the wrist
Pillow under forearms to eliminate pull on shoulder and assist
venous blood flow from hands
and lower arms
Legs lie flat and straight on
lower bed surface
Hyperextension of knees
External rotation of hips
Small pillow under thighs to flex
knees
Trochanter roll lateral to femur
(Figure 44.47 ■)
Heels rest on bed surface
Pressure on heels
Pillow under lower legs
Feet are in plantar flexion
Plantar flexion of feet (foot drop)
Footboard to provide support
for dorsiflexion
Greater
trochanter
*The amount of correction depends on the needs of the individual client.
Figure 44.47 ■ Making a trochanter roll: (1) Fold the towel in half lengthwise. (2) Roll the towel tightly, starting at one narrow edge and rolling
within approximately 30 cm (1 ft) of the other edge. (3) Invert the roll. Then palpate the greater trochanter of the femur and place the roll with the
center at the level of the greater trochanter; place the flat part of the towel under the client; then roll the towel snugly against the hip. The amount of
support depends on the needs of the individual client.
A common error nurses make when aligning clients in
Fowler’s position is placing an overly large pillow or more
than one pillow behind the client’s head. This promotes
the development of neck flexion contractures. If a client
desires several head pillows, the nurse should encourage
the client to rest without a pillow for several hours each
day to extend the neck fully and counteract the effects of
poor neck alignment.
Orthopneic Position
In the orthopneic position, the client sits either in bed or
on the side of the bed with an overbed table across the
lap (Figure 44.48 ■). This position facilitates respiration
by allowing maximum chest expansion. It is particularly
helpful to clients who have problems exhaling, because
they can press the lower part of the chest against the edge
of the overbed table.
Dorsal Recumbent Position
In the dorsal recumbent (back-lying) position (Figure 44.49 ■),
the client’s head and shoulders are slightly elevated on
a small pillow. In some agencies, the terms dorsal recumbent and supine are used interchangeably; strictly speaking, however, in the supine or dorsal position the head
and shoulders are not elevated. In both positions, the
client’s forearms may be elevated on pillows or placed
at the client’s sides. Supports are similar in both positions, except for the head pillow (Table 44.5). The dorsal
recumbent position is used to provide comfort and to
facilitate healing following certain surgeries or anesthetics (e.g., spinal).
Prone Position
In the prone position, the client lies on the abdomen with
the head turned to one side (Figure 44.50 ■). The hips are
not flexed. Both children and adults often sleep in this
Figure 44.48 ■ Orthopneic position.
M44B_BERM9793_11_GE_C44.indd 1134
Figure 44.49 ■ Dorsal recumbent position (supported).
03/02/2021 18:20
Chapter 44
TABLE 44.5
●
Activity and Exercise
1135
Dorsal Recumbent Position
Unsupported Position
Problem to Be Prevented
Corrective Measure*
Head is flat on bed surface
Hyperextension of neck in thick-chested
client
Pillow of suitable thickness under head and
shoulders if necessary for alignment
Lumbar curvature of spine is apparent
Posterior flexion of lumbar curvature
Roll or small pillow under lumbar curvature
Legs may be externally rotated
External rotation of legs
Roll or sandbag placed laterally to trochanter of femur (optional)
Legs are extended
Hyperextension of knees
Small pillow under thigh to flex knee slightly
Feet assume plantar flexion position
Plantar flexion (foot drop)
Footboard or rolled pillow to support feet in
dorsiflexion
Heels on bed surface
Pressure on heels
Pillow under lower legs
*The amount of correction depends on the needs of the individual client.
suffocating because chest expansion is inhibited during
respirations. The prone position should be used only when the
client’s back is correctly aligned, only for short periods, and only
for clients with no evidence of spinal abnormalities. As a result,
this position is not often used.
Lateral Position
Figure 44.50 ■ Prone position (supported).
position, sometimes with one or both arms flexed over
their heads. It is the only bed position that allows full extension of the hip and knee joints. When used periodically,
the prone position helps to prevent flexion contractures
of the hips and knees, thereby counteracting a problem
caused by all other bed positions. The prone position also
promotes drainage from the mouth and is especially useful for unconscious clients or those clients recovering from
surgery of the mouth or throat (Table 44.6).
The prone position creates some distinct disadvantages. The pull of gravity on the trunk produces a marked
lordosis in most individuals, and the neck is rotated laterally to a significant degree. For this reason, the prone
position may not be recommended for clients with problems of the cervical or lumbar spine. This position also
causes plantar flexion. Some clients with cardiac or respiratory problems find the prone position confining and
TABLE 44.6
In the lateral (side-lying) position (Figure 44.51 ■), the
client lies on one side of the body. Flexing the top hip and
knee and placing this leg in front of the body creates a
wider, triangular base of support and achieves greater stability. The greater the flexion of the top hip and knee, the
greater the stability and balance in this position. This flexion reduces lordosis and promotes good back alignment.
For this reason, the lateral position is good for resting and
sleeping clients. The lateral position helps to relieve pressure on the sacrum and heels in clients who sit for much
Figure 44.51 ■ Lateral position (supported).
Prone Position
Unsupported Position
Problem to Be Prevented
Corrective Measure*
Head is turned to side and neck is slightly
flexed
Flexion or hyperextension of neck
Small pillow under head unless contraindicated because of promotion of mucous
drainage from mouth
Body lies flat on abdomen accentuating
lumbar curvature
Hyperextension of lumbar curvature; difficulty breathing; pressure on breasts
(women); pressure on genitals (men)
Small pillow or roll under abdomen just
below diaphragm
Toes rest on bed surface; feet are in plantar
flexion
Plantar flexion (foot drop)
Allow feet to fall naturally over end of mattress, or support lower legs on a pillow so
that toes do not touch the bed
*The amount of correction depends on the needs of the individual client.
M44B_BERM9793_11_GE_C44.indd 1135
03/02/2021 18:20
1136
Unit 10
●
Promoting Physiologic Health
of the day or who are confined to bed and rest in Fowler’s
or dorsal recumbent positions much of the time. In the
lateral position, most of the body’s weight is borne by the
lateral aspect of the lower scapula, the lateral aspect of
the ilium, and the greater trochanter of the femur. Individuals who have sensory or motor deficits on one side of
the body usually find that lying on the uninvolved side is
more comfortable (Table 44.7).
Sims’ Position
In Sims’ (semiprone) position (Figure 44.52 ■), the client
assumes a posture halfway between the lateral and the
prone positions. The lower arm is positioned behind
the client, and the upper arm is flexed at the shoulder and the
elbow. Both legs are flexed in front of the client. The upper
leg is more acutely flexed at both the hip and the knee than
is the lower one.
Sims’ position may be used for unconscious clients
because it facilitates drainage from the mouth and prevents aspiration of fluids. It is also used for paralyzed
clients because it reduces pressure over the sacrum and
greater trochanter of the hip. It is often used for clients
receiving enemas and occasionally for clients undergoing examinations or treatments of the perineal area.
Many clients, especially pregnant women, find Sims’
position comfortable for sleeping. Clients with sensory
or motor deficits on one side of the body usually find
TABLE 44.7
Figure 44.52 ■ Sims’ position (supported).
that lying on the uninvolved side is more comfortable
(Table 44.8).
Moving and Turning Clients in Bed
Although healthy clients usually take for granted that
they can change body position and go from one place to
another with little effort, ill clients may have difficulty
moving, even in bed. How much assistance clients require
depends on their own ability to move and their health
Lateral Position
Unsupported Position
Problem to Be Prevented
Corrective Measure*
Body is turned to side, both arms in front
of body, weight resting primarily on lateral
aspects of scapula and ilium
Lateral flexion and fatigue of sternocleidomastoid muscles
Pillow under head and neck to provide
good alignment
Upper arm and shoulder are rotated internally and adducted
Internal rotation and adduction of shoulder
and subsequent limited function; impaired
chest expansion
Pillow under upper arm to place it in good
alignment; lower arm should be flexed
comfortably
Upper thigh and leg are rotated internally
and adducted
Internal rotation and adduction of femur;
twisting of the spine
Pillow under leg and thigh to place them in
good alignment; shoulders and hips should
be aligned
*The amount of correction depends on the needs of the individual client.
TABLE 44.8
Sims’ (Semiprone) Position
Unsupported Position
Problem to Be Prevented
Corrective Measure*
Head rests on bed surface; weight is borne
by lateral aspects of cranial and facial
bones
Lateral flexion of neck
Pillow supports head, maintaining it in good
alignment unless drainage from the mouth
is required
Upper shoulder and arm are internally
rotated
Internal rotation of shoulder and arm; pressure on chest, restricting expansion during
breathing
Pillow under upper arm to prevent internal
rotation
Upper leg and thigh are adducted and internally rotated
Internal rotation and adduction of hip and
leg
Pillow under upper leg to support it in
alignment
Feet assume plantar flexion
Foot drop
Sandbags to support feet in dorsiflexion
*The amount of correction depends on the needs of the individual client.
M44B_BERM9793_11_GE_C44.indd 1136
03/02/2021 18:20
Chapter 44
status. Nurses should be sensitive to both the need of clients to function independently and their need for assistance to move. Correct body alignment for the client must
also be maintained so that undue stress is not placed on
the musculoskeletal system.
When assisting a client to move, the nurse needs to use
appropriate numbers of staff and assistive devices (such as
those shown in previous Figures 44.41 through 44.45) to
avoid injury to self and client. Having sufficient staff and
assistive devices also helps to ensure client comfort and
modesty. Hydraulic lifts are examples of assistive equipment that take the place of manual lifts and transfers. A lift
can be used to transfer clients between the bed and a wheelchair, the bed and the bathtub, and the bed and a stretcher.
A lift consists of a base on casters, a hydraulic mechanical
pump, a mast boom, and a sling. The sling may consist of
a one-piece or two-piece canvas seat. The one-piece seat
stretches from the client’s head to the knees. The two-piece
seat has one canvas strap to support the client’s buttocks
and thighs and a second strap extending up to the axillae
to support the back. It is important to be familiar with the
model used and the practices that accompany use. Before
using the lift, the nurse ensures that it is in working order
and that the hooks, chains, straps, and canvas seat are in
good repair. Most agencies recommend that two nurses
operate a lift. Check agency policy.
Actions and rationales applicable to moving and lifting clients include the following:
Clinical Alert!
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Studies confirm that repositioning clients in bed, specifically pulling
a client toward the head of the bed, is a significant cause of MSDs
among caregivers in the healthcare industry. This risk of injury can
be decreased by using friction-reducing devices.
●
Activity and Exercise
1137
Prepare any needed assistive devices and supportive
equipment (e.g., mechanical lifts, friction-reducing
slide sheet, pillows, trochanter roll).
Plan around limitations to movement such as an IV or
urinary catheter.
Be alert to the effects of any medications the client
takes that may impair alertness, balance, strength, or
mobility.
Obtain required assistance from other individuals.
Explain the procedure to the client and listen to any
suggestions the client or support people have.
Provide privacy.
Perform hand hygiene.
Raise the height of the bed to bring the client close to your
center of gravity.
Lock the wheels on the bed, and raise the rail on the
side of the bed opposite you to ensure client safety.
Face in the direction of the movement to prevent spinal
twisting.
Assume a broad stance to increase stability and provide
balance.
Lean your trunk forward, and flex your hips, knees,
and ankles to lower your center of gravity, increase stability,
and ensure use of large muscle groups during movements.
Tighten your gluteal, abdominal, leg, and arm muscles
to prepare them for action and prevent injury.
Rock from the front leg to the back leg when pulling or
from the back leg to the front leg when pushing to overcome inertia, counteract the client’s weight, and help attain
a balanced, smooth motion.
After moving the client, determine and document
the client’s comfort (presence of anxiety, dizziness, or
pain), body alignment, tolerance of the activity (e.g.,
check pulse rate, blood pressure), ability to assist, use
of support devices, and safety precautions required
(e.g., side rails).
QSEN
Patient-Centered Care: Positioning, Moving,
and Turning Clients
The nurse working in the home care setting needs to perform the following actions that relate to positioning, moving, and turning clients:
•
•
•
•
Before moving a client, assess the degree of exertion
permitted, the client’s physical abilities (e.g., muscle
strength, presence of paralysis) and ability to assist
with the move, ability to understand instructions,
degree of comfort or discomfort when moving, client’s
weight, presence of orthostatic hypotension (particularly important when client will be standing), and your
own strength and ability to move the client.
If indicated, use pain relief modalities or medication
prior to moving the client.
M44B_BERM9793_11_GE_C44.indd 1137
•
•
Assess the height of the bed and the client’s leg length
to ensure that self-movements in and out of the bed
are smooth.
Inspect the mattress for support. A sagging mattress, a
mattress that is too soft, or an underfilled waterbed used
over a prolonged period can contribute to the development of hip flexion contractures and low back strain and
pain. Bed boards made of plywood and placed beneath a
sagging mattress are recommended for clients who have
back problems or are prone to them.
Assess the caregivers’ knowledge and application of
body mechanics to prevent injury.
Demonstrate how to turn and position the client
in bed. Observe the caregiver performing a return
03/02/2021 18:20
1138
•
•
•
Unit 10
●
Promoting Physiologic Health
demonstration. Reevaluate this technique periodically
to reinforce correct application of body mechanics.
Teach caregivers the basic principles of body alignment
and how to check for proper alignment after the client
has been changed to a new position.
Warn caregivers of the dangers of lifting and repositioning and encourage the use of assistive devices and
a “no solo lift” policy.
Teach the caregiver to check the client’s skin for redness
and integrity after repositioning the client. Stress the
importance of informing the nurse about the length of
time skin redness remains over pressure areas after the
client has been repositioned. Emphasize that reddened
areas should not be massaged because doing so may lead
to tissue trauma. Teach the caregiver that open areas must
be inspected and treated by a healthcare professional.
Also see Skills 44.1 through 44.4 on moving and turning
clients in bed and helping them sit up on the edge of the
bed. Note: The Assessment, Planning, Assignment, and
Equipment sections as listed in Skill 44.1 are the same for
each of these four procedures and are not repeated. The
Evaluation section at the end of Skill 44.4 is also the same
for all four procedures and, thus, is not repeated.
Moving a Client Up in Bed
SKILL 44.1
PURPOSE
• To assist clients who have slid down in bed from the Fowler’s position to move up in bed
ASSESSMENT
Before moving a client, assess the following:
• Client’s ability to lie flat or contraindications to lie flat (e.g., respiratory status)
• Client’s physical abilities to assist with the move (e.g., muscle
strength, presence of paralysis)
• Client’s ability to understand instructions and willingness to
participate
PLANNING
Review the client record to determine if previous nurses have
recorded information about the client’s ability to move. Use proper
assistive equipment and additional personnel whenever needed.
Ensure that the client understands instructions, and provide an interpreter as needed. Determine the number of personnel and type of
equipment needed to safely perform the positional change to prevent
injury to staff and client.
Assignment
The skills of moving and turning clients in bed can be assigned
to assistive personnel (AP). The nurse should make sure that any
IMPLEMENTATION
Preparation
Determine:
• Assistive devices that will be required
• Limitations to movement such as an IV or an indwelling urinary
catheter
• Medications the client is receiving, because certain medications
may hamper movement or alertness of the client
• Assistance required from other healthcare personnel.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client what you are going to do, why it is necessary, and how to
participate. Listen to any suggestions made by the client or
support people.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
4. Adjust the bed and the client’s position.
M44B_BERM9793_11_GE_C44.indd 1138
Client’s degree of comfort or discomfort when moving; if
needed, administer analgesics or perform other pain relief measures prior to the move (see Chapter 30
)
• Client’s weight
• The availability of equipment and other personnel to assist you.
•
needed equipment and additional personnel are available to reduce
risk of injury to the healthcare personnel. Emphasize the need for the
AP to report changes in the client’s condition that require assessment
and intervention by the nurse.
Equipment
• Assistive devices such as an overhead trapeze, friction-reducing
device, or a mechanical lift
Adjust the head of the bed to a flat position or as low as
the client can tolerate. Rationale: Moving the client upward
against gravity requires more force and can cause back strain.
• Raise the bed to a height appropriate for personnel safety
(i.e., at the caregiver’s elbows).
• Lock the wheels on the bed and raise the rail on the side of
the bed opposite you.
• Remove all pillows, then place one against the head of the
bed. Rationale: This pillow protects the client’s head from
inadvertent injury against the top of the bed during the
upward move.
5. For the client who is able to reposition without assistance:
• Place the bed in flat or reverse Trendelenburg’s position (as
tolerated by the client). Stand by and instruct the client to
move self. Assess if the client is able to move without causing friction to the skin.
• Encourage the client to reach up and grasp the upper side
rails with both hands, bend knees, and push off with the
feet and pull up with the arms simultaneously.
• Ask if a positioning device is needed (e.g., pillow).
•
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1139
Moving a Client Up in Bed—continued
7. Position yourself appropriately, and move the client.
• Face the direction of the movement, and then assume a
broad stance with the foot nearest the bed behind the forward foot and weight on the forward foot. Lean your trunk
forward from the hips. Flex the hips, knees, and ankles.
• Tighten your gluteal, abdominal, leg, and arm muscles and
rock from the back leg to the front leg and back again.
Then, shift your weight to the front leg as the client pushes
with the heels so that the client moves toward the head of
the bed.
8. For the client who is unable to assist:
• Use the ceiling lift with supine sling or mobile floor-based
lift and two or more caregivers. Follow manufacturer’s
guidelines for using the lift. Rationale: Moving a client up
in bed is not a one-person task. During any client handling,
if the caregiver is required to lift more than 35 lb of a client’s weight, then the client should be considered to be
fully dependent, and assistive devices should be used. This
reduces risk of injury to the caregiver.
9. Ensure client comfort.
• Elevate the head of the bed and provide appropriate support devices for the client’s new position.
• See the sections on positioning clients earlier in this chapter.
10. Document all relevant information. Record:
• Time and change of position moved from and position
moved to
• Any signs of pressure areas
• Use of support devices
• Ability of client to assist in moving and turning
• Response of client to moving and turning (e.g., anxiety, discomfort, dizziness).
SKILL 44.1
6. For the client who is partially able to assist:
• For a client who weighs less than 200 pounds: Use a friction-reducing device and two assistants. Rationale: Moving
a client up in bed is not a one-person task. During any client
handling, if the caregiver is required to lift more than 35 lb
of a client’s weight, then the client should be considered
fully dependent and assistive devices should be used. This
reduces risk of injury to the caregiver.
• For a client who weighs between 201–300 pounds: Use a
friction-reducing slide sheet and four assistants OR an air
transfer system and two assistants. Rationale: Moving a
client up in bed is not a one-person task. During any client
handling, if the caregiver is required to lift more than 35 lb
of a client’s weight, then the client should be considered
fully dependent and assistive devices should be used. This
reduces risk of injury to the caregiver.
• For a client who weighs more than 300 pounds: Use an air
transfer system and two assistants OR a total transfer lift.
• Ask the client to flex the hips and knees and position the
feet so that they can be used effectively for pushing. Rationale: Flexing the hips and knees keeps the entire lower leg
off the bed surface, preventing friction during movement,
and ensures use of the large muscle groups in the client’s
legs when pushing, thus increasing the force of movement.
• Place the client’s arms across the chest. Ask the client to
flex the neck during the move and keep the head off the
bed surface. Rationale: This keeps the arms and head off
the bed surface and minimizes friction during movement.
• Use the friction-reducing device and assistants to move
the client up in bed. Ask the client to push on the count of
three.
Turning a Client to the Lateral or Prone Position in Bed
IMPLEMENTATION
Preparation
Determine:
• Assistive devices that will be required (e.g., friction-reducing
device or mechanical lift)
• Limitations to movement such as an IV or an indwelling urinary
catheter
• Medications the client is receiving, because certain medications
may hamper movement or alertness of the client
• Assistance required from other healthcare personnel. Rationale: Moving a client is not a one-person task. During any client
handling, if the caregiver is required to lift more than 35 lb of a
client’s weight, then the client should be considered to be fully
dependent and assistive devices should be used. This reduces
risk of injury to the caregiver.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client what you are going to do, why it is necessary, and how to
participate.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
4. Position yourself and the client appropriately before performing
the move. Other individual(s) stands on the opposite side of the
bed.
• Adjust the head of the bed to a flat position or as low as the
client can tolerate. Rationale: This provides a position of
comfort for the client.
• Raise the bed to a height appropriate for personnel safety
(i.e., at the caregiver’s elbows).
• Lock the wheels on the bed.
• Move the client closer to the side of the bed opposite
the side the client will face when turned. Rationale: This
ensures that the client will be positioned safely in the center of the bed after turning. Use a friction-reducing device
or mechanical lift (depending on level of client assistance
required) to pull the client to the side of the bed. Adjust the
client’s head and reposition the legs appropriately.
• While standing on the side of the bed nearest the client,
place the client’s near arm across the chest. Abduct the
client’s far shoulder slightly from the side of the body and
externally rotate the shoulder. ❶ Rationale: Pulling the
one arm forward facilitates the turning motion. Pulling the
other arm away from the body and externally rotating the
SKILL 44.2
PURPOSE
• Movement to the lateral (side-lying) position may be necessary when placing a bedpan beneath the client, when changing the client’s
bed linen, or when repositioning the client.
Continued on page 1140
M44B_BERM9793_11_GE_C44.indd 1139
03/02/2021 18:20
1140
Unit 10
●
Promoting Physiologic Health
SKILL 44.2
Turning a Client to the Lateral or Prone Position in Bed—continued
❶ External rotation of the shoulder prevents
the arm from being caught beneath the
client’s body when the client is turned.
shoulder prevents that arm from being caught beneath the
client’s body during the roll.
• Place the client’s near ankle and foot across the far ankle
and foot. Rationale: This facilitates the turning motion.
Making these preparations on the side of the bed closest to
the client helps prevent unnecessary reaching.
• The individual on the side of the bed toward which the client
will turn should be positioned directly in line with the client’s
waistline and as close to the bed as possible.
5. Roll the client to the lateral position. The second individual(s)
standing on the opposite side of the bed helps roll the client
from the other side.
• Place one hand on the client’s far hip and the other hand
on the client’s far shoulder. Rationale: This position of the
hands supports the client at the two heaviest parts of the
body, providing greater control in movement during the roll.
• Position the client on his or her side with arms and legs
positioned and supported properly. ❷
Variation: Turning the Client to a Prone Position
To turn a client to the prone position, follow the preceding steps, with
two exceptions:
❷ Lateral position with pillows in place.
Instead of abducting the far arm, keep the client’s arm alongside the body for the client to roll over. Rationale: Keeping the
arm alongside the body prevents it from being pinned under the
client when the client is rolled.
• Roll the client completely onto the abdomen. Rationale: It is
essential to move the client as close as possible to the edge
of the bed before the turn so that the client will be lying on the
center of the bed after rolling. Never pull a client across the bed
while the client is in the prone position. Rationale: Doing so can
injure a woman’s breasts or a man’s genitals.
•
6. Document all relevant information. Record:
• Time and change of position moved from and position
moved to
• Any signs of pressure areas
• Use of support devices
• Ability of client to assist in moving and turning
• Response of the client to moving and turning (e.g., anxiety,
discomfort, dizziness).
SKILL 44.3
Logrolling a Client
PURPOSE
• Logrolling is a technique used to turn a client whose body
must at all times be kept in straight alignment (like a log). An
example is the client with back surgery or a spinal injury.
Considerable care must be taken to prevent additional injury.
IMPLEMENTATION
Preparation
Determine:
• Assistive devices that will be required
• Limitations to movement such as an IV or a urinary catheter
• Medications the client is receiving, because certain medications
may hamper movement or alertness of the client
• Assistance required from other healthcare personnel. At least
2–3 additional people are needed to perform this skill safely.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client what you are going to do, why it is necessary, and how to
participate.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
M44B_BERM9793_11_GE_C44.indd 1140
This technique requires two nurses or, if the client is large, three
nurses. For the client who has a cervical injury, one nurse must
maintain the client’s head and neck alignment.
4. Position yourselves and the client appropriately before the
move.
• Place the client’s arms across the chest. Rationale: Doing
so ensures that they will not be injured or become trapped
under the body when the body is turned.
5. Pull the client to the side of the bed.
• Use a friction-reducing device to facilitate logrolling. First,
stand with another nurse on the same side of the bed.
Assume a broad stance with one foot forward, and grasp
the rolled edge of the friction-reducing device. On a signal,
pull the client toward both of you. ❶
• One nurse counts: “One, two, three, go.” Then, at the same
time, all staff members pull the client to the side of the bed
by shifting their weight to the back foot. Rationale: Moving
the client in unison maintains the client’s body alignment.
6. One nurse moves to the other side of the bed, and places supportive devices for the client when turned.
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1141
Logrolling a Client—continued
SKILL 44.3
❶ Using a friction-reducing slide sheet, the nurses pull the sheet with the
client on it to the edge of the bed.
Place a pillow where it will support the client’s head after
the turn. Rationale: The pillow prevents lateral flexion of the
neck and ensures alignment of the cervical spine.
• Place one or two pillows between the client’s legs to support the upper leg when the client is turned. Rationale: This
pillow prevents adduction of the upper leg and keeps the
legs parallel and aligned.
7. Roll and position the client in proper alignment.
• Go to the other side of the bed (farthest from the client),
and assume a stable stance.
• Reaching over the client, grasp the friction-reducing device,
and roll the client toward you. ❷
• One nurse counts: “One, two, three, go.” Then, at the same
time, all nurses roll the client to a lateral position.
• The second nurse (behind the client) helps turn the client
and provides pillow supports to ensure good alignment in
the lateral position.
• Support the client’s head, back, and upper and lower
extremities with pillows.
•
❷ The nurse on the right uses the far edge of the frictionreducing slide sheet to roll the client toward him; the nurse on
the left remains behind the client and assists with turning.
Raise the side rails and place the call bell within the client’s
reach.
8. Document all relevant information. Record:
• Time and change of position moved from and position
moved to
• Any signs of pressure areas
• Use of support devices
• Ability of client to assist in moving and turning
• Response of client to moving and turning (e.g., anxiety, discomfort, dizziness).
•
Assisting a Client to Sit on the Side of the Bed (Dangling)
IMPLEMENTATION
Preparation
Determine:
• Assistive devices that will be required
• Limitations to movement such as an IV or a urinary catheter
• Medications the client is receiving, because certain medications
may hamper movement or alertness of the client
• Assistance required from other healthcare personnel.
Performance
1. Prior to performing the procedure, introduce self and verify the client’s identity using agency protocol. Explain to the client what you
are going to do, why it is necessary, and how to participate.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
4. Position yourself and the client appropriately before performing
the move.
• Assist the client to a lateral position facing you, using an
assistive device depending on client assistance needs.
• Raise the head of the bed slowly to its highest position.
Rationale: This decreases the distance that the client
needs to move to sit up on the side of the bed.
• Position the client’s feet and lower legs at the edge of the
bed. Rationale: This enables the client’s feet to move easily
off the bed during the movement, and the client is aided by
gravity into a sitting position.
• Stand beside the client’s hips and face the far corner of the
bottom of the bed (the angle in which movement will occur).
Assume a broad stance, placing the foot nearest the client
and head of the bed forward. Lean your trunk forward from
the hips. Flex your hips, knees, and ankles.
SKILL 44.4
PURPOSE
• The client assumes a sitting position on the edge of the bed before walking, moving to a chair or wheelchair, eating, or performing other
activities.
Continued on page 1142
M44B_BERM9793_11_GE_C44.indd 1141
03/02/2021 18:20
1142
Unit 10
●
Promoting Physiologic Health
SKILL 44.4
Assisting a Client to Sit on the Side of the Bed (Dangling)—continued
5. Move the client to a sitting position, using an assistive device
depending on client assistance needs.
• Place the arm nearest to the head of the bed under the client’s shoulders and the other arm over both of the client’s
thighs near the knees. ❶ Rationale: Supporting the client’s
shoulders prevents the client from falling backward during
the movement. Supporting the client’s thighs reduces friction of the thighs against the bed surface during the move
and increases the force of the movement.
• Tighten your gluteal, abdominal, leg, and arm muscles.
• Pivot on the balls of your feet in the desired direction facing the foot of the bed while pulling the client’s feet and
legs off the bed. Rationale: Pivoting prevents twisting of
the nurse’s spine. The weight of the client’s legs swinging
downward increases downward movement of the lower
body and helps make the client’s upper body vertical.
• Keep supporting the client until the client is well balanced
and comfortable. ❷ Rationale: This movement may cause
some clients to become light-headed or dizzy.
• Assess vital signs (e.g., pulse, respirations, and blood pressure) as indicated by the client’s health status.
6. Document all relevant information. Record:
• Ability of the client to assist in moving and turning
• Type of assistive device, if one was used
• Response of the client to moving and turning (e.g., anxiety,
discomfort, dizziness).
❶ Moving the client to a sitting position.
❷ Support the client until the client is well balanced and comfortable.
EVALUATION
• Check the skin integrity of the pressure areas from the previous
position. Relate findings to previous assessment data if available. Conduct follow-up assessment for previous and new skin
breakdown areas.
• Check for proper alignment after the position change. Do a
visual check and ask the client for a comfort assessment.
• Determine that all required safety precautions (e.g., side rails)
are in place.
• Determine client’s tolerance of the activity (e.g., vital signs
before and after dangling), particularly the first time the client
changes position.
• Report significant changes to the primary care practitioner.
Note: This skill describes the process to use for a client who is able to
perform the task independently and only needs standby assistance
for steadying, or a client who requires minimum assistance in which
the client can perform the task with or without friction-reducing assistive devices and the healthcare worker provides 25% of the work.
For clients who require moderate assistance (requiring no more than
50% assistance by the caregiver) or maximum assistance (requiring
more than 50% assistance by the caregiver), a lateral chair or mobile
or ceiling-mounted transfer system is required.
LIFESPAN CONSIDERATIONS Positioning, Moving, and Turning Clients
INFANTS
• Position infants on their back for sleep, even after feeding.
There is little risk of regurgitation and choking, and the rate of
sudden infant death syndrome (SIDS) is significantly lower in
infants who sleep on their backs.
• The skin of newborns can be fragile and may be abraded or
torn (sheared) if the infant is pulled across a bed.
CHILDREN
• Carefully inspect the dependent skin surfaces of all infants and
children confined to bed at least three times in each 24-hour
period.
M44B_BERM9793_11_GE_C44.indd 1142
OLDER ADULTS
• In clients who have had strokes, there is a risk of shoulder
displacement on the paralyzed side from improper moving or
repositioning techniques. Use care when moving, positioning
in bed, and transferring. Pillows or foam devices are helpful to
support the affected arm and shoulder and prevent injury.
• Decreased subcutaneous fat and thinning of the skin place
older adults at risk for skin breakdown. Repositioning approximately every 2 hours (more or less, depending on the unique
needs of the individual client) helps reduce pressure on bony
prominences and avoid tissue trauma.
03/02/2021 18:20
Chapter 44
Figure 44.53 ■ Gait belt.
Noel V. Baebler/Shutterstock.
Transferring Clients
Many clients require some assistance in transferring
between bed and chair or wheelchair, between wheelchair
and toilet, and between bed and stretcher. Before transferring any client, however, the nurse must determine the
client’s physical and mental capabilities to participate in
the transfer technique. In addition, the nurse must analyze
and organize the activity.
A gait belt, sometimes called a transfer or walking belt,
has traditionally been used to transfer a client from one
position to another and for ambulation (Figure 44.53 ■).
A gait belt can have handles that allow the nurse to
control movement of the client during the transfer
or during ambulation. The long-held belief that the
use of gait belts improves safety for both clients and
caregivers is based on tradition and not on evidencebased research. The few studies that have been done
indicate that using a gait belt for transfer falls into
either a moderate- or high-risk category for low back
disorders. Gait belts are not appropriate for all clients
and it is important to assess clients before using one on
them. They are suitable for clients who can bear weight
and require only minimal assistance. The gait belt with
handles is easier to grasp. Gait belts should not be
used to lift a client off the floor or for bariatric clients.
In addition, they should not be relied on for use with
clients who are at high risk for falls (Miller, Rockefeller,
& Townsend, 2017).
A sliding board is another device that can be used to
transfer a client between a bed and chair. Boards are often
●
Activity and Exercise
1143
made of low-friction materials or with movable sliding
sections. Some clients may be able to transfer themselves
using a sliding transfer board. If a caregiver is needed, the
client is either pushed or pulled across the transfer board
using a slide sheet. Clients must have sitting balance. See
Skill 44.5 for transferring a client between a bed and a
chair, and Skill 44.6 for transferring a client between a bed
and a stretcher. Note: The Evaluation section at the end of
Skill 44.6 also applies to Skill 44.5.
General guidelines for transfer techniques include the
following:
•
•
•
•
•
•
•
•
Plan what to do and how to do it. Determine the space
in which the transfer will take place (bathrooms, for
instance, are usually cramped), the number of assistants (one or two) needed to accomplish the transfer
safely, and the client’s capabilities (e.g., size, weight,
cognition, balance, cooperation).
Obtain essential equipment before starting (e.g., gait or
transfer belt; friction-reducing device, such as a slide
sheet, slide board, or air transfer system; wheelchair;
stretcher; lift) and check that all equipment is functioning
correctly. The gait or transfer belt is meant only to increase
control of the client’s movements; if the client requires lifting, a mechanical lifting device should be used.
Remove obstacles from the area used for the transfer.
Explain the transfer to the client, including what the
client should do.
Explain the transfer to the nursing personnel who are
helping; specify who will give directions (one staff
member needs to be in charge).
Always support or hold the client rather than the equipment and ensure the client’s safety and dignity.
During the transfer, explain step by step what the client should do, for example, “Move your right foot
forward.”
Make a written plan of the transfer, including the
client’s tolerance (e.g., pulse and respiratory rates).
Because wheelchairs and stretchers are unstable, they
can predispose the client to falls and injury. Guidelines for
the safe use of wheelchairs and stretchers are shown in the
accompanying Practice Guidelines.
PRACTICE GUIDELINES Wheelchair Safety
•
•
•
•
•
•
Always lock the brakes on both wheels of the wheelchair when
the client transfers in or out of it.
Raise the footplates and move the leg rests out of the way
before transferring the client into the wheelchair.
Lower the footplates after the transfer, and place the client’s
feet on them.
Ensure the client is positioned well back in the seat of the
wheelchair.
Use seat belts that fasten behind the wheelchair to protect confused clients from falls. Note: Seat belts are a form of restraint
and must be used in accordance with policies and procedures
that apply to the use of restraints (see Chapter 32
).
Back the wheelchair into or out of an elevator, rear large wheels
first.
M44B_BERM9793_11_GE_C44.indd 1143
•
Place your body between the wheelchair and the bottom of an
incline.
Clinical Alert!
Air, foam, and gel cushions that distribute weight evenly (not doughnut-type cushions) are essential for clients confined to a wheelchair
and must be checked frequently to ensure they are intact. Strict
continence management is also important for preventing skin breakdown. Maintaining tire pressure will prevent added resistance and
energy expenditure. Periodically monitor the client’s upper extremities
for pain and overuse syndromes.
03/02/2021 18:20
1144
Unit 10
●
Promoting Physiologic Health
PRACTICE GUIDELINES Safe Use of Stretchers
Lock the wheels of the bed and stretcher before the client
transfers in or out of them.
• Fasten safety straps across the client on a stretcher, and raise
the side rails.
• Never leave a client unattended on a stretcher unless the
wheels are locked and the side rails are raised on both sides or
the safety straps are securely fastened across the client.
• Always push a stretcher from the end where the client’s head is
positioned. This position protects the client’s head in the event
of a collision.
•
If the stretcher has two swivel wheels and two stationary
wheels:
a. Always position the client’s head at the end with the stationary wheels and
b. Push the stretcher from the end with the stationary wheels.
The stretcher is maneuvered more easily when pushed from
this end.
• Maneuver the stretcher when entering the elevator so that the
client’s head goes in first.
•
SKILL 44.5
Transferring Between Bed and Chair
PURPOSE
• A client may need to be transferred between the bed and a
wheelchair or chair, the bed and the commode, or a wheelchair
and the toilet. There are numerous variations in the technique.
ASSESSMENT
Before transferring a client, assess the following:
• The client’s body size and weight
• Ability to follow instructions
• Ability to bear weight (full, partial, or none)
• Ability to position and reposition feet on floor
• Ability to push down with arms and lean forward
• Ability to grasp
• Ability to achieve independent balance (sitting, standing, or
none)
• Activity tolerance
PLANNING
Review the client record to determine if previous nurses have
recorded information about the client’s ability to transfer. Implement pain relief measures so that they are effective when the transfer begins. The decision must be made at this time regarding the
client’s ability to participate. If the client can safely participate in the
transfer, a gait or transfer belt or sliding board can be used; if not,
a powered standing assist lift or full-body lift would be safer for the
client and nurse.
Equipment
• Robe or appropriate clothing
• Slippers or shoes with nonskid soles
• Gait or transfer belt
IMPLEMENTATION
Preparation
• Plan what to do and how to do it.
• Obtain essential equipment before starting (e.g., gait or transfer
belt, wheelchair), and check that all equipment is functioning
correctly.
• Remove obstacles from the area so clients do not trip. Make
sure there are no spills or liquids on the floor on which clients
could slip.
• Note any devices attached to the client (e.g., IV, urinary
catheter).
M44B_BERM9793_11_GE_C44.indd 1144
Which variation the nurse selects depends on factors related to
the client and the environment that are assessed prior to beginning the transfer.
Muscle strength
Joint mobility
Presence of paralysis
Level of comfort
Presence of orthostatic hypotension
The technique with which the client is familiar
The space in which the transfer will need to be maneuvered
(bathrooms, for example, are usually cramped)
• The number of assistants (one or two) needed to accomplish
the transfer safely.
•
•
•
•
•
•
•
•
•
•
Chair, commode, wheelchair as appropriate to client need
Slide board, if appropriate
Lift, if appropriate
Assignment
The skill of transferring a client can be assigned to AP who have
demonstrated safe transfer technique for the involved client. It is
important for the nurse to assess the number of staff needed, assistive devices needed, and the client’s ability to assist and to communicate specific information about what the AP should report to
the nurse.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain the transfer
process to the client. During the transfer, explain step by step
what the client should do, for example, “Move your right foot
forward.”
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
4. Position the equipment appropriately.
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1145
Transferring Between Bed and Chair—continued
Wheelchair
Bed
x Client
Nurse's
feet
Client's
feet
❶ The wheelchair is placed parallel to the bed and as close to the bed
as possible. Note that placement of the nurse’s feet mirrors that of the
client’s feet.
the nearest hand; the other hand supports the back of
the client’s shoulder. Lean your trunk forward from the
hips. Flex your hips, knees, and ankles. Assume a broad
stance, placing one foot forward and one back. Brace
the client’s feet with your feet to prevent the client from
sliding forward or laterally. Mirror the placement of the
client’s feet, if possible. Rationale: This helps prevent loss
of balance during the transfer.
8. Assist the client to stand, and then move together toward
the wheelchair or sitting area to which you wish to transfer
the client.
• On the count of three or the verbal instructions of
“Ready–steady–stand” and on the count of three or
the word “Stand,” ask the client to push down against
the mattress or side of the bed while you transfer your
weight from one foot to the other (while keeping your
back straight) and stand upright moving the client
forward (directly toward your center of gravity) into a
standing position. (If the client requires more than a
very small degree of pulling, even with the assistance
of two nurses, a mechanical device should be obtained
and used.)
• Support the client in an upright standing position for a few
moments. Rationale: This allows the nurse and the client to
extend the joints and provides the nurse with an opportunity
to ensure that the client is stable before moving away from
the bed.
• Together, pivot on your foot farthest from the chair, or take a
few steps toward the wheelchair, bed, chair, commode, or
car seat.
9. Assist the client to sit.
• Move the wheelchair forward or have the client back up to
the wheelchair (or desired seating area) and place the legs
against the seat. Rationale: Having the client place the legs
against the wheelchair seat minimizes the risk of the client
falling when sitting down.
• Make sure the wheelchair brakes are on.
• Have the client reach back and feel or hold the arms of the
wheelchair.
• Stand directly in front of the client. Place one foot forward
and one back.
• Tighten your grasp on the gait or transfer belt, and tighten
your gluteal, abdominal, leg, and arm muscles.
• Have the client sit down while you bend your knees and
hips and lower the client onto the wheelchair seat.
10. Ensure client safety.
• Ask the client to push back into the wheelchair seat.
Rationale: Sitting well back on the seat provides a broader
base of support and greater stability and minimizes the risk
of falling from the wheelchair. A wheelchair or bedside commode can topple forward when the client sits on the edge
of the seat and leans far forward.
• Remove the gait or transfer belt.
• Lower the leg rests and footplates, and place the client’s
feet on them, if applicable.
Variation: Transferring with a Belt and Two Nurses
• Even if a client is able to partially bear weight and is cooperative, it still may be safer to transfer a client with the assistance of
two nurses. If so, you should position yourselves on both sides
of the client, facing the same direction as the client. Flex your
hips, knees, and ankles. Grasp the client’s transfer belt with the
hand closest to the client, and with the other hand support the
client’s elbows.
SKILL 44.5
Lower the bed to its lowest position so that the
client’s feet will rest flat on the floor. Lock the wheels
of the bed.
• Place the wheelchair parallel to the bed and as close
to the bed as possible. ❶ Put the wheelchair on the
side of the bed that allows the client to move toward his
or her stronger side. Lock the wheels of the wheelchair,
raise the footplates, and move the leg rests out of
the way.
5. Prepare and assess the client.
• Assist the client to a sitting position on the side of the bed
(see Skill 44.4).
• Assess the client for orthostatic hypotension before moving
the client from the bed.
• Assist the client in putting on a bathrobe and nonskid slippers or shoes.
• Place a gait or transfer belt snugly around the client’s
waist. Check to be certain that the belt is securely
fastened.
6. Give explicit instructions to the client. Ask the client to:
• Move forward and sit on the edge of the bed (or surface on
which the client is sitting) with feet placed flat on the floor.
Rationale: This brings the client’s center of gravity closer to
the nurse’s.
• Lean forward slightly from the hips. Rationale: This brings
the client’s center of gravity more directly over the base of
support and positions the head and trunk in the direction of
the movement.
• Place the foot of the stronger leg beneath the edge of the
bed (or sitting surface) and put the other foot forward.
Rationale: In this way, the client can use the stronger leg
muscles to stand and power the movement. A broader
base of support makes the client more stable during the
transfer.
• Place the client’s hands on the bed surface (or available
stable area) so that the client can push while standing.
Rationale: This provides additional force for the movement and reduces the potential for strain on the nurse’s
back. The client should not grasp your neck for support.
Rationale: Doing so can injure the nurse.
7. Position yourself correctly.
• Stand directly in front of the client and to the side requiring the most support. Hold the gait or transfer belt with
•
Continued on page 1146
M44B_BERM9793_11_GE_C44.indd 1145
03/02/2021 18:20
1146
Unit 10
●
Promoting Physiologic Health
Transferring Between Bed and Chair—continued
SKILL 44.5
•
Coordinating your efforts, all three of you stand
simultaneously, pivot, and move to the wheelchair.
Reverse the process to lower the client onto the
wheelchair seat.
Variation: Transferring a Client with an Injured Lower
Extremity
When the client has an injured lower extremity, movement should
always occur toward the client’s unaffected (strong) side. For example, if the client’s right leg is injured and the client is sitting on the
edge of the bed preparing to transfer to a wheelchair, position the
wheelchair on the client’s left side. Rationale: In this way, the client
can use the unaffected leg most effectively and safely.
Variation: Using a Slide Board
For clients who cannot stand but are able to cooperate and possess sufficient upper body strength, use a slide board to help them
move without nursing assistance. ❷ Rationale: This method not
only promotes the client’s sense of independence but also preserves
your energy.
11. Document relevant information:
• Client’s ability to bear weight and pivot
• Number of staff needed for transfer and the safety
measures and precautions used
• Length of time up in chair
• Client response to transfer and being up in chair or
wheelchair.
QSEN
Patient-Centered Care: Transferring in the
Home Setting
❷ Using a slide board.
Note: This skill describes the process to use for a client who is able
to perform the task independently and only needs standby assistance for steadying. For clients who require moderate or maximum
assistance, a lateral chair or a mobile or ceiling-mounted transfer
system is required.
•
The nurse in the home care setting needs to consider the
following:
•
The caregiver and client should practice transfer
technique(s), using appropriate equipment as needed,
in the hospital or long-term care setting before being
discharged.
•
Assess furniture in the home. Does the client’s favorite chair have arms for ease of using and sitting?
Examine the fabric—is it rough? Will it cause skin
abrasions? If the client will be using a wheelchair, is
there enough space in the bedroom and bathroom for
a safe transfer?
Observe client and caregiver transfer technique in the
home setting to reinforce prior teaching.
SKILL 44.6
Transferring Between Bed and Stretcher
PURPOSE
• The stretcher, or gurney, is used to transfer supine clients from
one location to another. Whenever the client is capable of
accomplishing the transfer from bed to stretcher independently,
either by lifting onto it or by rolling onto it, the client should be
encouraged to do so. If the client cannot move onto the stretcher
independently and weighs less than 200 pounds, a frictionreducing device (i.e., slide sheet) or a lateral transfer board ❶ or
an air transfer system should be used, and at least two caregivers are needed to assist with the transfer. Some friction-reducing
devices have handles or long straps to avoid awkward stretching
by the caregivers when pulling the client during the lateral transfer. For clients between 201 and 300 pounds, a slide sheet or
transfer board and four caregivers or an air transfer system and
two caregivers should be used. For clients who weigh more than
300 pounds, two caregivers and either an air transfer system or
a ceiling lift with supine sling should be used.
• Depending on the client’s condition (e.g., neck immobilizer,
IVs, drains, chest tube), additional assistants may be needed.
M44B_BERM9793_11_GE_C44.indd 1146
❶ A lateral transfer board. The friction-reducing material rolls when
transferring clients in a supine position.
Shirlee Snyder.
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1147
Transferring Between Bed and Stretcher—continued
PLANNING
Review the client record to determine if previous nurses have
recorded information about how the client tolerated similar transfers.
If indicated, implement pain relief measures so that they are effective
when the transfer begins.
Equipment
• Stretcher
• Transfer assistive devices (e.g., slide sheet, transfer board, air
transfer system, lift)
IMPLEMENTATION
Preparation
Obtain the necessary equipment and nursing personnel to assist in
the transfer.
• Note any devices attached to the client.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client
what you are going to do, why it is necessary, and how to participate. Explain the transfer to the nursing personnel who are
helping and specify who will give directions (one staff member
needs to be in charge).
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
4. Adjust the client’s bed in preparation for the transfer.
• Lower the head of the bed until it is flat or as low as the client can tolerate.
• Place the friction-reducing device under the client.
• Raise the bed so that it is slightly higher (i.e., 1/2 in.) than
the surface of the stretcher. Rationale: It is easier for the
client to move down a slant.
• Ensure that the wheels on the bed are locked.
• Place the stretcher parallel to the bed next to the client and
lock the stretcher wheels.
• Fill the gap that exists between the bed and the stretcher
loosely with the bath blankets (optional).
5. Transfer the client securely to the stretcher.
• If the client can transfer independently, encourage him or
her to do so and stand by for safety.
• If the client is partially able or not able to transfer:
• One caregiver needs to be at the side of the client’s bed,
between the client’s shoulder and hip.
• The second and third caregivers should be at the side
of the stretcher: one positioned between the client’s
EVALUATION
• Compare client capabilities such as weight bearing, pivoting
ability, and strength and control during previous transfers.
• Report any significant deviations from normal to the primary
care practitioner.
M44B_BERM9793_11_GE_C44.indd 1147
•
•
•
Level of comfort
The space in which the transfer is maneuvered
The number of assistants (one to four) needed to accomplish
the transfer safely.
SKILL 44.6
ASSESSMENT
Before transferring a client, assess the following:
• The client’s body size and weight
• Ability to follow instructions
• Activity tolerance
Assignment
The skill of transferring a client can be assigned to AP who have
demonstrated safe transfer technique for the involved client. It is
important for the nurse to assess the client’s capabilities and communicate specific information about what the AP should report back
to the nurse.
shoulder and hip and the other between the client’s hip
and lower legs.
• All caregivers should position their feet in a walking
stance.
• Ask the client to flex the neck during the move, if possible, and place the arms across the chest. Rationale:
This prevents injury to those body parts.
• On a planned command, the caregivers at the stretcher’s side pull (shifting weight to the rear foot), and the
caregiver at the bedside pushes the client toward the
stretcher (shifting weight to the front foot).
6. Ensure client comfort and safety.
• Make the client comfortable, unlock the stretcher wheels,
and move the stretcher away from the bed.
• Immediately raise the stretcher side rails or fasten the safety
straps across the client. Rationale: Because the stretcher
is high and narrow, the client is in danger of falling unless
these safety precautions are taken.
Variation: Using a Transfer Board
The transfer board is a lacquered or smooth polyethylene board
measuring 45 to 55 cm (18 to 22 in.) by 182 cm (72 in.) with handholds along its edges. Transfer mattresses are also available, as are
mechanical assistive devices. It is imperative to have enough staff
assisting with the transfer to prevent injury to staff as well as clients.
Turn the client to a lateral position away from you, position the board
close to the client’s back, and roll the client onto the board. Pull the
client and board across the bed to the stretcher. Safety belts may be
placed over the chest, abdomen, and legs.
7. Document relevant information:
• Equipment used
• Number of personnel needed for transfer and safety measures and precautions used
• Destination if reason for transfer is to transport from one
location to another.
•
Note use of appropriate safety measures (e.g., transfer belt,
locking wheels of bed and stretcher) by AP during transfer
process.
03/02/2021 18:20
1148
Unit 10
●
Promoting Physiologic Health
LIFESPAN CONSIDERATIONS Transferring Clients
INFANTS
• The infant who is lying down, on the side or supine, can be
placed in either a bassinet or crib for transport. If the bassinet
has a bottom shelf, it can be used for carrying the IV pump or
monitor.
CHILDREN
• The toddler should be transported in a high-top crib with the
side rails up and the protective top in place. Stretchers should
not be used because the mobile toddler may roll or fall off.
Use special caution with older clients to prevent skin tears or
bruising during a transfer or when using a hydraulic lift.
• Write the method used to transfer each client—equipment
used, best position, and number of personnel needed to assist
in transfer. This can be part of the care plan and also be available in the client’s room as a guide to all personnel caring for
the client.
• Avoid sudden position changes. They can cause orthostatic
hypotension and increase the risk of fainting and falls.
•
OLDER ADULTS
• Because conditions of older adults can change from day to day,
always assess the situation to ensure that you have the right
equipment and enough people to assist when transferring a
client.
Providing ROM Exercises
Clients who experience restrictions in activity are at risk
for impaired joint mobility. Promoting exercise to maintain
a client’s muscle tone and joint mobility is an essential
function of nursing personnel. When clients are ill, they
may need to perform ROM exercises until they can regain
their normal activity levels.
Active ROM exercises are isotonic exercises in which
the client moves each joint in the body through its complete range of movement, maximally stretching all muscle
groups within each plane over the joint. These exercises
maintain or increase muscle strength and endurance and
help to maintain cardiorespiratory function in an immobilized client. They also prevent deterioration of joint capsules, ankylosis, and contractures (permanent shortening
of the muscle).
Full ROM does not occur spontaneously in the immobilized individual who independently achieves ADLs,
moves about in bed, transfers between bed and wheelchair
or chair, or ambulates a short distance, because only a few
muscle groups are maximally stretched during these activities. Although the client may successfully achieve some
active ROM movements of the upper extremities while
combing the hair, bathing, and dressing, the immobilized
client is very unlikely to achieve any active ROM movements of the lower extremities when these are not used in
the normal functions of standing and walking about. For
this reason, most clients who use a wheelchair and many
ambulatory clients need active ROM exercises until they
regain their normal activity levels.
At first, the nurse may need to teach the client and
family to perform the needed ROM exercises; eventually,
the client may be able to accomplish these independently.
Instructions for the client performing active ROM exercises are shown in the accompanying Client Teaching.
During passive ROM exercises, another individual
moves each of the client’s joints through its complete
range of movement, maximally stretching all muscle
groups within each plane over each joint. Because the client does not contract the muscles, passive ROM exercises
M44B_BERM9793_11_GE_C44.indd 1148
CLIENT TEACHING Active ROM Exercises
Perform each ROM exercise as taught to the point of
slight resistance, but not beyond, and never to the point of
discomfort.
• Perform the movements systematically, using the same
sequence during each session.
• Perform each exercise three times.
• Perform each series of exercises twice daily.
•
OLDER ADULTS
• For older adults, it is not essential to achieve full range of
motion in all joints. Instead, emphasize achieving a sufficient
range of motion to carry out ADLs, such as walking, dressing,
combing hair, showering, and preparing a meal.
are of no value in maintaining muscle strength but are useful in maintaining joint flexibility. For this reason, passive
ROM exercises should be performed only when the client
is unable to accomplish the movements actively.
Passive ROM exercises should be accomplished for
each movement of the arms, legs, and neck that the client
is unable to achieve actively. As with active ROM exercises, passive ROM exercises should be accomplished to
the point of slight resistance, but not beyond, and never
to the point of discomfort. The movements should be systematic, and the same sequence should be followed during
each exercise session. Each exercise should be repeated, at
the client’s tolerance, from three to five times. The series
of exercises should be done twice daily. Performing one
series of exercises along with the bath is helpful. Passive
ROM exercises are accomplished most effectively when
the client lies supine in bed. General guidelines for providing passive exercises are shown in the accompanying
Practice Guidelines.
During active-assistive ROM exercises, the client uses
a stronger, opposite arm or leg to move each of the joints
of a limb incapable of active motion. The client learns to
support and move the weak arm or leg with the strong
arm or leg as far as possible. Then the nurse continues the
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1149
PRACTICE GUIDELINES Providing Passive ROM Exercises
•
•
•
•
•
•
•
•
•
•
•
Ensure that the client understands the reason for doing ROM
exercises.
If there is a possibility of hand swelling, make sure rings are
removed.
Clothe the client in a loose gown, and cover the body with a
bath blanket.
Use correct body mechanics when providing ROM exercises to
avoid muscle strain or injury to both yourself and the client.
Position the bed at an appropriate height.
Expose only the limb being exercised to avoid embarrassing the
client and to maintain warmth.
Support the client’s limbs above and below the joint as needed
to prevent muscle strain or injury (Figure 44.54 ■). This may
also be done by cupping joints in the palm of your hand or
cradling limbs along your forearm (Figure 44.55 ■). If a joint is
painful (e.g., arthritic), support the limb in the muscular areas
above and below the joint.
Use a firm, comfortable grip when handling the limb.
Move the body parts smoothly, slowly, and rhythmically. Jerky
movements cause discomfort and, possibly, injury. Fast movements can cause spasticity (sudden, prolonged involuntary
muscle contraction) or rigidity (stiffness or inflexibility).
Avoid moving or forcing a body part beyond the existing range
of motion. Muscle strain, pain, and injury can result. This is particularly important for clients with flaccid (limp) paralysis, whose
muscles can be stretched and joints dislocated without their
awareness.
If muscle spasticity occurs during movement, stop the movement temporarily, but continue to apply slow, gentle pressure
on the part until the muscle relaxes; then proceed with the
motion.
Figure 44.54 ■ Supporting a limb above and below the joint for
passive exercise.
movement passively to its maximal degree. This activity
increases active movement on the strong side of the client’s body and maintains joint flexibility on the weak side.
Such exercise is especially useful for clients who have had
a stroke and are hemiplegic (paralyzed on one half of the
body).
Clinical Alert!
Clients who require passive ROM exercises after a disability should
have a goal of progressing to active-assistive ROM exercises and,
finally, to active ROM exercises.
Ambulating Clients
Ambulation (the act of walking) is a function that most
people take for granted. However, when clients are ill
M44B_BERM9793_11_GE_C44.indd 1149
•
•
•
•
•
If a contracture is present, apply slow, firm pressure, without
causing pain, to stretch the muscle fibers.
If rigidity occurs, apply pressure against the rigidity, and
continue the exercise slowly.
Teach client’s caregiver the purposes and technique of
performing passive ROM at home if appropriate.
Avoid hypertension of joints in older adults if joints are arthritic.
Use the exercises as an opportunity to also assess skin
condition.
A
B
Figure 44.55 ■ Holding limbs for support during passive exercise:
A, cupping; B, cradling.
they are often confined to bed and are thus nonambulatory. The longer clients are in bed, the more difficulty
they have walking. In fact, evidence continues to support
that early, routine mobilization of critically ill clients is
safe, improves muscle strength and functional independence, reduces incidence of delirium, and decreases hospital length of stay (Denehy, Lanphere, & Needham, 2017;
Hashem, Nelliot, & Needham, 2016; Kappel et al., 2018).
Even 1 or 2 days of bedrest can make an individual
feel weak, unsteady, and shaky when first getting out of
bed. A client who has had surgery, is elderly, or has been
immobilized for a longer time will feel more noticeable
weakness. The potential problems of immobility are far
less likely to occur when clients become ambulatory as
soon as possible. The nurse can assist clients to prepare for
ambulation by helping them become as independent as
possible while in bed. Nurses should encourage clients to
03/02/2021 18:20
1150
Unit 10
●
Promoting Physiologic Health
perform ADLs, maintain good body alignment, and carry
out active ROM exercises to the maximum degree possible yet within the limitations imposed by their illness and
recovery program. Collaboration with physical therapy,
when ordered, can also be very useful in strengthening
the muscles needed for ambulation.
Preambulatory Exercises
Clients who have been in bed for long periods often
need to perform muscle tone exercises to strengthen the
muscles used for walking before attempting to walk. One
of the most important muscle groups is the quadriceps
femoris, which extends the knee and flexes the thigh. This
group is also important for elevating the legs, for example,
for walking upstairs. These exercises are frequently called
quadriceps drills or sets. To strengthen these muscles,
the client consciously tenses them, drawing the kneecap
upward and inward. The client pushes the popliteal space
of the knee against the bed surface, relaxing the heels on
the bed surface (Figure 44.56 ■). On the count of 1, the
muscles are tensed; they are held during the counts of 2,
3, 4; and they are relaxed at the count of 5. The exercise
should be done within the client’s tolerance, that is, without fatiguing the muscles. Carried out several times an
Figure 44.56 ■ Tensing the quadriceps femoris muscles before
ambulation.
hour during waking hours, this simple exercise significantly strengthens the muscles used for walking.
Assisting Clients to Ambulate
Clients who have been immobilized for even a few days
may require assistance with ambulation. The amount
EVIDENCE-BASED PRACTICE
Evidence-Based Practice
Can a Formalized Ambulation Program Improve Ambulation
in Hospitalized Clients?
Older adults, orthopedic clients, and clients who have had general
surgery are at highest risk for immobility complications. Research
clearly documents the benefits of mobilization; however, mobilization of hospitalized clients is the most commonly missed nursing
care activity. Lack of personnel and time are the two common reasons given for failure to perform ambulation. Studies focused on
improving ambulation in hospitalized clients have primarily focused
on interventions to ambulate surgical clients earlier using a dedicated team of personnel, which is often unrealistic for most institutions. Based on these findings, Teodoro et al. (2016) conducted
a pretest and posttest randomized experimental research design
to determine if a formalized ambulation program could improve
ambulation in hospitalized medical–surgical clients.
The research design compared a planned ambulation program
with usual care. The ambulation program included daily goals
for walking posted in the client’s room, an education videotape
about the importance of walking and what clients can do to meet
their goals, and walking reminders in the client’s room. The nurse
assigned to care for each client directed the ambulation in the
usual care group. The outcome variable was the amount of ambulation measured in steps per hour captured with a pedometer.
The study was conducted on a 30-bed medical-surgical unit
of a community-based hospital. A total of 48 clients were included
in the study, with 22 assigned to the ambulation program and
26 assigned to the usual care group. The study took place over
3 sequential days. On the first day (pretest period), all the clients
had a pedometer attached to their gowns at 11 A.M. with instructions to wear the pedometer through the day and no instructions
given about ambulation. The pedometer was removed at 6 P.M.
M44B_BERM9793_11_GE_C44.indd 1150
The number of steps for the pretest period was recorded and
transcribed as the average number of steps walked per hour.
This monitoring was done to ensure that baseline ambulation values were similar for the two groups. The participants were then
randomly assigned to either the ambulation program group or
the usual care group. Between 6 and 9 P.M., the members of the
ambulation program group watched a 2.5-minute video on the
importance of ambulation. On day 2, the clients in the ambulation
program determined their goals when a researcher asked each
to estimate the distance he or she could walk outside the room
on that day and then double the distance as a goal for day 3. On
both days 2 and 3, all participants had the pedometer attached to
their gowns at 7 A.M. and removed at 11 P.M. The researchers then
recorded the number of steps for the 16-hour posttest period.
No significant differences were found between the ambulation and usual care groups for age, sex, reason for admission, or
pretest amount of ambulation. However, the participants in the
ambulation program had significantly higher amounts of ambulation within 2 days, while the usual care group decreased from
pretest values. The ambulation intervention required little extra staff
time to implement.
Implications
The intervention in this study can be easily implemented in any
busy acute care setting with minimal time, effort, and cost. The
use of a pedometer is an easy objective method to determine
if ambulation goals for clients are being achieved and a way for
clients to self-assess their progress. The researchers suggest that
future research should evaluate different approaches to encouraging ambulation in hospitalized clients and consider longer evaluation periods (e.g., 3–5 days).
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1151
of assistance will depend on the client’s condition,
including age, health status, and length of inactivity.
Assistance may mean walking alongside the client
while providing standby support for safety (Skill 44.7);
reinforcing instruction provided by the physical therapist
to the client about the use of assistive devices such as a
cane, walker, or crutches; or using a sit-to-stand lift with
ambulation capability or a lift with an ambulation sling
(Figure 44.57 ■).
QSEN
Safety: Assisting the Client to Ambulate
When the nurse is assisting a client to
ambulate in the home setting, the following
should be considered:
When making a home visit, assess carefully for safety
issues concerning ambulation. Counsel the client and
family about inadequate lighting, unfastened rugs, slippery floors, and loose objects on the floors.
Check the surroundings for adequate supports such as
railings and grab bars.
Recommend that nonskid strips be placed on outside
steps and inside stairs that are not carpeted.
Ask to see the shoes the client intends to wear while
ambulating. They should be in good repair and should
support the foot.
•
•
•
•
Figure 44.57 ■ Promoting ambulation by using a lift with an
ambulation sling.
CLIENT TEACHING Controlling Orthostatic Hypotension
•
•
•
•
•
Rest with the head of the bed elevated 8 to 12 inches. This
position makes the position change on rising less severe.
Avoid sudden changes in position. Arise from bed in three stages:
a. Sit up in bed for 1 minute.
b. Sit on the side of the bed with legs dangling for 1 minute.
c. Stand with care, holding onto the edge of the bed or
another nonmovable object for 1 minute.
Never bend down all the way to the floor or stand up too
quickly after stooping.
Postpone activities such as shaving and hair grooming for at
least 1 hour after rising.
Wear elastic stockings at night to inhibit venous pooling in the legs.
Be aware that the symptoms of hypotension are most severe at
the following times:
a. 30 to 60 minutes after a heavy meal
b. 1 to 2 hours after taking an antihypertension medication.
• Get out of a hot bath very slowly, because high temperatures
can lead to venous pooling.
• Use a rocking chair to improve circulation in the lower extremities. Even mild leg conditioning can strengthen muscle tone and
enhance circulation.
• Refrain from any strenuous activity that results in holding the
breath and bearing down. This Valsalva maneuver slows the
heart rate, leading to subsequent lowering of blood pressure.
•
Assisting a Client to Ambulate
PURPOSE
• To provide a safe condition for the client to walk with whatever support is needed
•
•
•
•
•
Client’s intake of medications (e.g., opioids, sedatives, tranquilizers, and antihistamines) that may cause drowsiness, dizziness,
weakness, and orthostatic hypotension, seriously hindering the
client’s ability to walk safely
Presence of joint inflammation, fractures, muscle weakness, or
other conditions that impair physical mobility
Ability to understand directions
Level of comfort
Weight-bearing status
SKILL 44.7
ASSESSMENT
Assess
• Length of time in bed and the amount and type of activity the
client was last able to tolerate
• Baseline vital signs
• Range of motion of joints needed for ambulating (e.g., hips,
knees, ankles)
• Muscle strength of lower extremities
• Need for ambulation aids (e.g., cane, walker, crutches, lift with
ambulation sling)
Continued on page 1152
M44B_BERM9793_11_GE_C44.indd 1151
03/02/2021 18:20
1152
Unit 10
●
Promoting Physiologic Health
SKILL 44.7
Assisting a Client to Ambulat—continued
PLANNING
Implement pain relief measures so that they are effective. The amount
of assistance needed while ambulating will depend on the client’s
condition (e.g., age, health status, length of inactivity, and emotional
readiness). Review any previous experiences with ambulation and
ASSIGNMENT
Ambulation of clients is frequently assigned to AP. However, the nurse
should conduct an initial assessment of the client’s abilities in order
to direct other personnel in providing appropriate assistance. Any
unusual events that result from assisting the client in ambulation must
be validated and interpreted by the nurse.
IMPLEMENTATION
Preparation
Be certain that others are available to assist you if needed. Also, plan
the route of ambulation that has the fewest hazards and a clear path
for ambulation.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client how you are going to assist, why ambulation is necessary,
and how to participate. Discuss how this activity relates to
the overall plan of care. Stress that the client must keep the
nurse informed as to how the activity is being tolerated as it
progresses.
2. Perform hand hygiene and observe appropriate infection prevention procedures.
3. Ensure that the client is appropriately dressed to walk and has
shoes or slippers with nonskid soles.
4. Prepare the client for ambulation.
• Have the client sit up in bed for at least 1 minute prior to
preparing to dangle legs.
• Assist the client to sit on the edge of the bed and allow
dangling for at least 1 minute.
• Assess the client carefully for signs and symptoms of
orthostatic hypotension (dizziness, light-headedness, or a
sudden increase in heart rate) prior to leaving the bedside.
Rationale: Allowing for gradual adjustment can minimize
drops in blood pressure (and fainting) that occur with shifts
in position from lying to sitting, and sitting to standing.
• Assist the client to stand by the side of the bed for at least
1 minute until he or she feels secure.
• Carefully attend to any IV tubing, catheters, or drainage
bags. Keep urinary drainage bags below level of the client’s
bladder. Rationale: To prevent backflow of urine into bladder and risk of infection.
• If the client is a high safety risk (e.g., cannot follow commands, medical instability, lack of experience with assistive
device, neurologic deficits), use a lift with ambulation sling
and 1 to 2 caregivers.
• If the client is a high safety risk and has upper extremity
strength and is able to grasp with at least one hand, use a
lift with ambulation sling or a sit-to-stand lift with ambulation
capability and 1 to 2 caregivers.
• If the client is a low safety risk (e.g., able to follow commands, medically stable, and experienced with assistive
device), use a gait or transfer belt for standby assist as
needed and assistive devices as needed (e.g., crutches,
walker, cane) and 1 to 2 caregivers. Make sure the belt
is pulled snugly around the client’s waist and fastened
securely. Grasp the belt at the client’s back, and walk
behind and slightly to one side of the client. ❶
M44B_BERM9793_11_GE_C44.indd 1152
the success of such efforts. Plan the length of the walk with the client, considering the nursing or primary care practitioner’s orders and
the medical condition of the client. Be prepared to shorten the walk
according to the client’s activity tolerance.
Equipment
• Assistive devices required for safe ambulation of client (e.g., gait
or transfer belt, walker, cane, sit-to-stand assist device, lift with
ambulation sling)
• Wheelchair for following client, or chairs along the route if the
client needs to rest
• Portable oxygen tank if the client needs it
❶ Using a gait or transfer belt to support the client during ambulation.
5. Ensure client safety while assisting the client to ambulate.
• Encourage the client to ambulate independently if he or she
is able, but walk beside the client’s weak side, if appropriate. If the client has a lightweight IV pole because of infusing fluids, he or she may find that holding onto the pole
while ambulating helps with balance. If the pole or other
equipment is cumbersome in any way, the nurse must push
it to match the client’s pace, securing any assistance necessary in order to move smoothly with the client.
• Remain physically close to the client in case assistance is
needed at any point.
• If it is the client’s first time out of bed following surgery,
injury, or an extended period of immobility, or if the client
is weak or unstable, have an assistant follow you and the
client with a wheelchair in the event that it is needed quickly.
• Encourage the client to assume a normal walking stance
and gait as much as possible. Ask the client to straighten
the back and raise the head so that the eyes are looking
forward in a normal horizontal plane. Rationale: Clients
who are unsure of their ability to ambulate tend to look
down at their feet, which makes them more likely to fall.
6. Protect the client who begins to fall while ambulating.
• If a client begins to experience the signs and symptoms of
orthostatic hypotension or extreme weakness, quickly assist
the client into a nearby wheelchair or other chair, and help
the client to lower the head between the knees.
• Stay with the client. Rationale: A client who faints while in
this position could fall head first out of the chair.
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1153
Assisting a Client to Ambulat—continued
Walk in unison with the client, using a smooth, even gait, at
the same speed and with steps the same size as the client’s.
Rationale: This gives the client a greater feeling of security.
•
7. Document distance and duration of ambulation and assistive
devices, if used, in the client record using forms or checklists supplemented by narrative notes when appropriate. Include description of the client’s gait (including body alignment) when walking;
pace; activity tolerance when walking (e.g., pulse rate, facial color,
any shortness of breath, feelings of dizziness, or weakness);
degree of support required; and respiratory rate and blood pressure after initial ambulation to compare with baseline data.
SKILL 44.7
When the weakness subsides, assist the client back to bed.
Never catch a falling client. A caregiver probably cannot
stop a client from falling. Quickly remove obstacles out of
the way that may injure the client (Martin, Rogers, & Matz,
n.d.; VHA Center for Engineering & Occupational Safety and
Health, 2016). Do not manually lift a client from the floor;
use SPHM technology.
Variation: Two Nurses
• Place a gait or transfer belt around the client’s waist. Each nurse
grasps the side handle with the near hand and the lower aspect
of the client’s upper arm with the other hand.
•
•
EVALUATION
• Establish a plan for continued ambulation based on expected or normal ability for the client.
LIFESPAN CONSIDERATIONS Assisting a Client to Ambulate
CHILDREN
• Children and adolescents who have suffered a sports injury (e.g.,
sprained ankle) may want to be more active than they should be. A
cast, splint, or boot may be put in place to limit activity and assist
in healing. Teach the child the importance of appropriate activity,
and the use of assistive devices (e.g., crutches) if necessary. Help
children focus on what they can do rather than what they cannot
do (e.g., “You can stand at the free-throw line and shoot baskets”).
OLDER ADULTS
• Inquire how the client has ambulated previously and check any
available chart notes regarding the client’s abilities and modify
assistance accordingly.
• Take into account a decrease in speed, strength, resistance to
fatigue, reaction time, and coordination due to a decrease in
nerve conduction.
• Be cautious when using a gait belt with a client with osteoporosis.
Too much pressure from the belt can increase the risk of vertebral
compression fractures. If a client has had abdominal surgery, it
may be necessary to use a gait vest instead of a gait belt.
•
•
•
•
•
If assistive devices such as a walker or cane are used, make
sure clients are supervised in the beginning to learn the proper
method of using them. Crutches may be much more difficult for
older adults to use due to decreased upper body strength.
Be alert to signs of activity intolerance, especially in older adults
with cardiac and lung problems.
Set small goals and increase slowly to build endurance,
strength, and flexibility.
Be aware of any fall risks the older adult may have, such as the
following:
• Effects of medications
• Neurologic disorders
• Orthopedic problems
• Presence of equipment that must accompany the client
when ambulating
• Environmental hazards
• Orthostatic hypotension
In older adults, the body’s responses return to normal more
slowly. For instance, an increase in heart rate from exercise may
stay elevated for hours before returning to normal.
Some clients experience orthostatic (postural)
hypotension on assuming a vertical position from a lying
position and may need information about ways to control
this problem (see Client Teaching). The client may exhibit
some or all of the following symptoms: pallor, diaphoresis, nausea, tachycardia, and dizziness. If any of these are
present, the client should be assisted to a supine position
in bed and closely assessed.
Using Mechanical Aids for Walking
Mechanical aids for ambulation include canes, walkers,
and crutches.
Canes
Three types of canes are commonly used: the standard
straight-legged cane; the tripod cane, which has three
feet; and the quad cane, which has four feet and provides
the most support (Figure 44.58 ■). Cane tips should have
M44B_BERM9793_11_GE_C44.indd 1153
Figure 44.58 ■ A quad cane.
03/02/2021 18:20
1154
Unit 10
●
Promoting Physiologic Health
CLIENT TEACHING Using Canes
Hold the cane with the hand on the stronger side of the body
to provide maximum support and appropriate body alignment
when walking.
• Position the tip of a standard cane (and the nearest tip of other
canes) about 15 cm (6 in.) to the side and 15 cm (6 in.) in front
of the near foot, so that the elbow is slightly flexed.
•
WHEN MAXIMUM SUPPORT IS REQUIRED
• Move the cane forward about 30 cm (1 ft), or a distance that
is comfortable while the body weight is borne by both legs
(Figure 44.59A ■).
• Then move the affected (weak) leg forward to the cane
while the weight is borne by the cane and stronger leg
(Figure 44.59B).
Next, move the unaffected (stronger) leg forward ahead of the
cane and weak leg while the weight is borne by the cane and
weak leg (Figure 44.59C).
• Repeat the steps. This pattern of moving provides at least two
points of support on the floor at all times.
•
AS YOU BECOME STRONGER AND REQUIRE LESS
SUPPORT
• Move the cane and weak leg forward at the same time, while
the weight is borne by the stronger leg (Figure 44.60A ■).
• Move the stronger leg forward, while the weight is borne by the
cane and the weak leg (Figure 44.60B).
B
A
C
Figure 44.59 ■ Steps involved in using a cane to provide maximum
support.
rubber caps to improve traction and prevent slipping.
The standard cane is 91 cm (36 in.) long; some aluminum canes can be adjusted from 56 to 97 cm (22 to 38 in.).
The length should permit the elbow to be slightly flexed.
Clients may use either one or two canes, depending on
how much support they require.
Walkers
Walkers are mechanical devices for ambulatory clients
who need more support than a cane provides and lack
the strength and balance required for crutches. Walkers
come in many different shapes and sizes, with devices
suited to individual needs. The standard type is made of
polished aluminum. It has four legs with rubber tips and
plastic handgrips (Figure 44.61A ■). Many walkers have
adjustable legs.
The standard walker needs to be picked up to be used.
The client therefore requires partial strength in both hands
and wrists, strong elbow extensors, and strong shoulder
M44B_BERM9793_11_GE_C44.indd 1154
A
B
Figure 44.60 ■ Steps involved in using a cane when less than
maximum support is required.
depressors. The client also needs the ability to bear at least
partial weight on both legs.
While four-wheeled and two-wheeled models of
walkers (roller walkers) do not need to be picked up to
be moved, they are less stable than the standard walker.
Clients who are too weak or unstable to pick up and
move the walker with each step use the roller walkers.
Some roller walkers have a seat at the back so the client
can sit down to rest when desired. An adaptation of the
standard and four-wheeled walker is one that has two
tips and two wheels (Figure 44.61B). This type provides
more stability than the four-wheeled model yet still permits the client to keep the walker in contact with the
ground all the time. The legs with wheels allow the client
to easily push the walker forward, and the legs without
wheels prevent the walker from rolling away as the client
steps forward.
The nurse may need to adjust the height of a client’s
walker so that the hand bar is just below the client’s waist
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1155
In crutch walking, the client’s weight is borne by the
muscles of the shoulder girdle and the upper extremities.
Before beginning crutch walking, exercises that strengthen
the upper arms and hands are recommended.
Measuring Clients for Crutches
When nurses measure clients for axillary crutches, it is
most important to obtain the correct length for the crutches
and the correct placement of the handpiece. There are two
methods of measuring crutch length:
A
B
Figure 44.61 ■ A, Standard walker; B, two-wheeled walker.
1. The client lies in a supine position and the nurse measures from the anterior fold of the axilla to the heel of
the foot and adds 2.5 cm (1 in.).
2. The client stands erect and positions the crutch as
shown in Figure 44.62 ■. The nurse makes sure the
shoulder rest of the crutch is at least 3 fingerwidths,
that is, 2.5 to 5 cm (1 to 2 in.), below the axilla.
To determine the correct placement of the hand bar:
CLIENT TEACHING Using Walkers
WHEN MAXIMUM SUPPORT IS REQUIRED
• Move the walker ahead about 15 cm (6 in.) while your body
weight is borne by both legs.
• Then move the right foot up to the walker while your body
weight is borne by the left leg and both arms.
• Next, move the left foot up to the right foot while your body
weight is borne by the right leg and both arms.
IF ONE LEG IS WEAKER THAN THE OTHER
• Move the walker and the weak leg ahead together
about 15 cm (6 in.) while your weight is borne by the stronger leg.
• Then move the stronger leg ahead while your weight is borne
by the affected leg and both arms.
1. The client stands upright and supports the body
weight by the handgrips of the crutches.
2. The nurse measures the angle of elbow flexion. It
should be about 30 degrees.
Crutch Gaits
The crutch gait is the gait a client assumes on crutches
by alternating body weight on one or both legs and the
crutches. Five standard crutch gaits are the four-point gait,
three-point gait, two-point gait, swing-to gait, and swingthrough gait. The gait used depends on the following individual factors: (a) the ability to take steps, (b) the ability to
bear weight and keep balance in a standing position on both
legs or only one, and (c) the ability to hold the body erect.
and the client’s elbows are slightly flexed. This position
helps the client assume a more normal stance. A walker
that is too low causes the client to stoop; one that is too
high makes the client stretch and reach.
2.5–5 cm
(1–
Crutches
Crutches may be a temporary need for some clients and
a permanent one for others. Crutches should enable a client to ambulate independently; therefore, it is important
to learn to use them properly. The most frequently used
kinds of crutches are the underarm crutch, or axillary
crutch with hand bars, and the Lofstrand crutch, which
extends only to the forearm. On the Lofstrand crutch, the
metal cuff around the forearm and the metal bar stabilize
the wrists and thus make walking easier, especially on
stairs. The platform or elbow extensor crutch also has a
cuff for the upper arm to permit forearm weight bearing.
All crutches require suction tips, usually made of rubber,
which help to prevent slipping on a floor surface.
M44B_BERM9793_11_GE_C44.indd 1155
30
elbow
6"
6"
Figure 44.62 ■ The standing position for measuring the correct
length for crutches.
03/02/2021 18:20
1156
Unit 10
●
Promoting Physiologic Health
Clients also need instruction about how to get into
and out of chairs and go up and down stairs safely.
All of these crutch skills are best taught before the
client is discharged and preferably before the client has
surgery.
CLIENT TEACHING Using Crutches
•
•
Crutch Stance (Tripod Position)
Before crutch walking is attempted, the client needs
to learn facts about posture and balance. The proper
standing position with crutches is called the tripod
(triangle) position (Figure 44.63 ■ ). The crutches are
placed about 15 cm (6 in.) in front of the feet and out
laterally about 15 cm (6 in.), creating a wide base of
support. The feet are slightly apart. A tall client requires
a wider base than does a short client. Hips and knees
are extended, the back is straight, and the head is held
straight and high. There should be no hunch to the
shoulders and thus no weight borne by the axillae.
The elbows are extended sufficiently to allow weight
bearing on the hands. If the client is unsteady, the
nurse places a gait or transfer belt around the client’s
waist and grasps the belt from above, not from below.
A fall can be prevented more effectively if the belt is
held from above.
Four-Point Alternate Gait
This is the most elementary and safest gait, providing at
least three points of support at all times, but it requires
coordination. Clients can use it when walking in crowds
because it does not require much space. To use this gait,
the client needs to be able to bear weight on both legs
(Figure 44.64 ■, reading from bottom to top). The nurse
asks the client to:
1. Move the right crutch ahead a suitable distance, such
as 10 to 15 cm (4 to 6 in.).
2. Move the left front foot forward, preferably to the
level of the left crutch.
3. Move the left crutch forward.
4. Move the right foot forward.
Crutch
15 cm
(6 in.)
Figure 44.63 ■ The tripod position.
M44B_BERM9793_11_GE_C44.indd 1156
•
•
•
•
•
Three-Point Gait
To use this gait, the client must be able to bear the
entire body weight on the unaffected leg. The two
crutches and the unaffected leg bear weight alternately
(Figure 44.65 ■, reading from bottom to top). The nurse
asks the client to:
1. Move both crutches and the weaker leg forward.
2. Move the stronger leg forward.
Two-Point Alternate Gait
Crutch
15 cm
(6 in.)
Left foot
•
Follow the plan of exercises developed for you to strengthen
your arm muscles before beginning crutch walking.
Have a healthcare professional establish the correct length for
your crutches and the correct placement of the handpieces.
Crutches that are too long force your shoulders upward and
make it difficult for you to push your body off the ground.
Crutches that are too short will make you hunch over and
develop an improper body stance.
The weight of your body should be borne by the arms
rather than the axillae (armpits). Continual pressure on
the axillae can injure the radial nerve and eventually cause
crutch palsy, a weakness of the muscles of the forearm,
wrist, and hand.
Maintain an erect posture as much as possible to prevent
strain on muscles and joints and to maintain balance.
Each step taken with crutches should be a comfortable distance for you. It is wise to start with a small rather than large
step.
Inspect the crutch tips regularly, and replace them
if worn.
Keep the crutch tips dry and clean to maintain their
surface friction. If the tips become wet, dry them well
before use.
Wear a shoe with a low heel that grips the floor. Rubber
soles decrease the chances of slipping. Adjust shoelaces
so they cannot come untied or reach the floor where they
might catch on the crutches. Consider shoes with alternative forms of closure (e.g., Velcro), especially if you cannot
easily bend to tie laces. Slip-on shoes are acceptable only
if they are snug and the heel does not come loose when
the foot is bent.
Right foot
This gait is faster than the four-point gait. It requires more
balance because only two points support the body at one
time; it also requires at least partial weight bearing on
each foot. In this gait, arm movements with the crutches
are similar to the arm movements during normal walking
(Figure 44.66 ■, reading from bottom to top). The nurse
asks the client to:
1. Move the left crutch and the right foot forward
together.
2. Move the right crutch and the left foot ahead
together.
03/02/2021 18:20
Chapter 44
●
Activity and Exercise
1157
Step 2
Step 4
Right foot advances
Step 1
affected
Step 3
Left crutch advances
Figure 44.65 ■ The three-point crutch gait.
Step 2
Left foot advances
1. Move both crutches ahead together.
2. Lift body weight by the arms and swing to the crutches.
Swing-Through Gait
This gait requires considerable skill, strength, and coordination. The nurse asks the client to:
Step 1
Right crutch advances
1. Move both crutches forward together.
2. Lift body weight by the arms and swing through and
beyond the crutch.
Getting into a Chair
Chairs that have armrests and are secure or braced against
a wall are essential for clients using crutches. For this procedure, the nurse instructs the client to:
Tripod position
Figure 44.64 ■ The four-point alternate crutch gait.
Swing-to Gait
The swing gaits are used by clients with paralysis of the
legs and hips. Prolonged use of these gaits results in atrophy of the unused muscles. The swing-to gait is the easier
of these two gaits. The nurse asks the client to:
M44B_BERM9793_11_GE_C44.indd 1157
1. Stand with the back of the unaffected leg centered
against the chair. The chair helps support the client
during the next steps.
2. Transfer the crutches to the hand on the affected side and
hold the crutches by the hand bars. The client grasps the
arm of the chair with the hand on the unaffected side
(Figure 44.67 ■). This allows the client to support the
body weight on the arms and the unaffected leg.
3. Lean forward, flex the knees and hips, and lower into
the chair.
03/02/2021 18:20
1158
Unit 10
●
Promoting Physiologic Health
Getting Out of a Chair
For this procedure, the nurse instructs the client to:
Step 2
Right crutch
and left limb advance
Step 1
Left crutch and
right limb advance
Tripod position
Figure 44.66 ■ The two-point alternate crutch gait.
Figure 44.67 ■ A client using crutches getting into a chair.
M44B_BERM9793_11_GE_C44.indd 1158
1. Move forward to the edge of the chair and place
the unaffected leg slightly under or at the edge of
the chair. This position helps the client stand up
from the chair and achieve balance, because the
unaffected leg is supported against the edge of
the chair.
2. Grasp the crutches by the hand bars in the hand on
the affected side, and grasp the arm of the chair by the
hand on the unaffected side. The body weight is placed
on the crutches and the hand on the armrest to support
the unaffected leg when the client rises to stand.
3. Push down on the crutches and the chair armrest
while elevating the body out of the chair.
4. Assume the tripod position before moving.
Going Up Stairs
For this procedure, the nurse stands behind the client and
slightly to the affected side if needed. The nurse instructs
the client to:
1. Assume the tripod position at the bottom of the stairs.
2. Transfer the body weight to the crutches and move the
unaffected leg onto the step (Figure 44.68 ■).
3. Transfer the body weight to the unaffected leg on the
step and move the crutches and affected leg up to
the step. The affected leg is always supported by the
crutches.
4. Repeat steps 2 and 3 until the client reaches the top
of the stairs.
Figure 44.68 ■ Climbing stairs: placing weight on the crutches while
first moving the unaffected leg onto a step.
03/02/2021 18:20
Chapter 44
Going Down Stairs
For this procedure, the nurse stands one step below the
client on the affected side if needed. The nurse instructs
the client to:
1. Assume the tripod position at the top of the stairs.
2. Shift the body weight to the unaffected leg, and move
the crutches and affected leg down onto the next step
(Figure 44.69 ■).
●
Activity and Exercise
1159
3. Transfer the body weight to the crutches, and move
the unaffected leg to that step. The affected leg is
always supported by the crutches.
4. Repeat steps 2 and 3 until the client reaches the bottom
of the stairs.
Evaluating
The goals established during the planning phase are evaluated according to specific desired outcomes, also established in that phase. Examples of these are shown in the
accompanying Nursing Care Plan.
If outcomes are not achieved, the nurse, client, and
support person if appropriate need to explore the reasons before modifying the care plan. For example, the
following questions may be considered if an immobilized client fails to maintain muscle mass and tone and
joint mobility:
•
•
•
•
•
•
Has the client’s physical or mental condition changed
motivation to perform required exercise?
Were appropriate range-of-motion exercises
implemented?
Was the client encouraged to participate in self-care
activities as much as possible?
Was the client encouraged to make as many decisions
as possible when developing a daily activity plan and
to express concerns?
Did the nurse provide appropriate supervision and
monitoring?
Was the client’s diet adequate to provide appropriate
nourishment for energy requirements?
Figure 44.69 ■ Descending stairs: moving the crutches and affected
leg to the next step.
NURSING CARE PLAN Potential for Decline in Health
ASSESSMENT DATA
NURSING DIAGNOSIS
DESIRED OUTCOMES*
NURSING ASSESSMENT
Peter Chan, a 69-year-old, unmarried accountant being
treated for heart failure, states he has dyspnea with mild
activity. (“I cannot climb a flight of stairs without stopping
and resting and become breathless even when walking on
level ground.”) Prefers the orthopneic position. He works at
home and sits at a table for most of the day.
Potential for decline in health related
to decreased activity resulting from
inadequate balance between oxygen supply and demand associated
with decreased cardiac output and
obesity
Immobility Consequences:
Physiological [0204], as evidenced by
• No pressure injuries
• Muscle strength not
compromised
Immobility Consequences:
Psycho-cognitive [0205], as evidenced by no
• Apathy
• Sleep disturbances
• Negative body image
Mobility [0208], as evidenced by
mildly compromised
• Walking
• Balance
M44B_BERM9793_11_GE_C44.indd 1159
03/02/2021 18:21
1160
Unit 10
●
Promoting Physiologic Health
NURSING CARE PLAN Potential for Decline in Health—continued
Physical Examination
Diagnostic Data
Height: 178 cm (5′10″)
CBC, and urinalysis
within normal limits
CXR reveals an
enlarged heart
Weight: 102 kg (225 lb)
Temperature: 37.8°C (100.4°F)
Pulse rate: 94 beats/min
Respirations: 20/min
Blood pressure: 174/92 mmHg
Rales present in both lungs.
Respirations slightly labored.
Color pale.
3 + (5 mm) edema both feet
and ankles.
NURSING INTERVENTIONS*/SELECTED ACTIVITIES
POSITIONING [0840]
Position to alleviate dyspnea, e.g., high Fowler’s.
RATIONALE
Clients with increased pulmonary secretions are able to breathe better when
upright because abdominal organs are lower and there is greater room for
lung and diaphragmatic excursion.
Provide support to edematous areas, e.g., elevate feet on
footstool when sitting.
Elevating the dependent area assists with decreasing tissue pressure and
promoting fluid return to the venous system and the heart.
Encourage active range-of-motion exercises.
Active ROM helps maintain muscle strength and promote circulation. Mild
activity also helps burn unneeded calories.
EXERCISE THERAPY: MUSCLE CONTROL [0226]
Collaborate with physical, occupational, and recreational
therapists in developing and executing an individually tailored exercise program.
This client will need a multidisciplinary approach to his care. Each member
contributes from his or her area of expertise. Research supports efficacy of
individually tailored exercise plans. Factors such as having an exercise partner, using music, and type of activity can motivate client and enhance adherence to the plan over time.
Offer options, explain rationale for type of exercise and pro- If the client understands what the reasons are for activity, he can make good
choices.
tocol to client, and allow him to make choices that appeal
to him and that address his needs.
Provide step-by-step cuing for each motor activity during
exercise or ADLs.
As-needed reminders help the client recall what to do next.
Use visual aids to facilitate learning how to perform
exercises.
Some people have better visual memory than auditory memory.
EVALUATION
Outcomes met. Mr. Chan did not develop any skin breakdown or other evidence of the complications of immobility to date. However, since
the risk factors remain, the care plan will be ongoing.
*The NOC # for desired outcomes and the NIC # for nursing interventions are listed in brackets following the appropriate outcome or intervention. Outcomes, indicators,
interventions, and activities selected are only a sample of those suggested by NOC and NIC and should be further individualized for each client.
APPLYING CRITICAL THINKING
1. What assessment findings alert you that Mr. Chan is developing problems associated with his current state of decreased mobility?
2. Mr. Chan may benefit from using a walker to assist with ambulation at home. What teaching should be done in regard to use of a walker?
3. The care plan does not address one of Mr. Chan’s risk factors—obesity. Would you add this to the plan?
4. What assumptions has the nurse made in assigning the desired outcome of “Immobility Consequences: Psycho-cognitive”?
5. How are the choices of outcomes influenced by the cause of his nursing diagnosis (a chronic illness)?
Answers to Applying Critical Thinking questions are available on the faculty resources website. Please consult with your instructor.
M44B_BERM9793_11_GE_C44.indd 1160
03/02/2021 18:21
Chapter 44
●
Activity and Exercise
1161
CONCEPT MAP
Client with Potential for a Decline in Health
PC
69 y.o. male
HF
assess
• Unmarried accountant: works at home
c/o dyspnea on exertion
• Height: 178 cm (5'10")
• Weight: 102 kg (225 lb)
• Temperature: 37.8°C (100.4°F)
•
•
•
•
•
•
Pulse rate: 94 BPM
Respirations: 20/minute
Blood pressure: 174/92 mmHg
CBC and urinalysis within normal limits
CXR shows enlarged heart
Rales in both lungs and 3+ edema
in both feet and ankles.
generate nursing diagnosis
Potential for a decline in health r/t decreased activity resulting from inadequate
balance between oxygen supply & demand associated with decreased CO and obesity
Outcomes met:
• Did not develop
any skin
breakdown or
other evidence of
the complication
of immobility to
date
evaluation
outcome
outcome
Immobility Consequences:
Physiologic aeb no:
• Pressure injury
• Decreased muscle strength
Mobility aeb
mildly compromised:
• Walking
• Balance
nursing intervention
nursing intervention
Positioning
Position to alleviate
dyspnea (e.g., high
Fowler's)
Provide support to
edematous areas, e.g.,
elevate feet on footstool when sitting
M44B_BERM9793_11_GE_C44.indd 1161
Exercise Therapy-Muscle Control
activity
activity
activity
activity
activity
activity
Encourage active
range-of-motion
exercises
evaluation
Outcomes met:
• Did not develop
any compromised
muscle function
• However, since
the risk factors
remain, the care
plan will be
ongoing
Use visual aids
to facilitate
learning how to
perform exercises
Provide step-by-step
cuing for each motor
activity during exercise
or ADLs
activity
Collaborate with physical,
occupational, and recreational
therapists in developing and
executing exercise program
Explain rationale
for type of exercise
and protocol to client
03/02/2021 18:21
1162
Unit 10
●
Promoting Physiologic Health
Chapter 44 Review
CHAPTER HIGHLIGHTS
• Exercise and activity are essential components for maintaining and
• Nursing diagnoses that relate to activity and mobility problems
regaining health and wellness.
Research on exercise has demonstrated it to be an excellent strategy for preventing and treating some cardiovascular and pulmonary diseases, mood disorders, diseases of aging, diabetes, and
immune diseases.
The ability to move freely, easily, and purposefully in the environment
is essential for individuals to meet their basic needs.
Purposeful coordinated movement of the body relies on the integrated functioning of the musculoskeletal system, the nervous system, and the vestibular apparatus of the inner ear.
Body movement involves four basic elements: body alignment, joint
mobility, balance, and coordinated movement.
Individuals maintain alignment and balance when the line of gravity
passes through the center of gravity and the base of support.
Exercise is physical activity performed to improve health and maintain fitness. Activity tolerance is the type and amount of exercise or
daily living activities an individual is able to perform without experiencing adverse effects. Functional strength is the ability to do work.
Exercise is classified as either isotonic, isometric, or isokinetic and
as either aerobic or anaerobic.
Many factors influence body alignment and activity. These include
growth and development, nutrition, personal values and attitudes,
certain external factors, and prescribed limitations to movement.
Immobility affects almost every body organ and system adversely.
Problems include disuse osteoporosis and atrophy; contractures;
diminished cardiac reserve; orthostatic hypotension; venous stasis,
edema, and thrombus formation; decreased respiratory movement
and pooling of secretions; decreased metabolic rate and negative
nitrogen balance; urinary stasis, retention, infection, and calculi;
constipation; and varying emotional reactions.
Assessment relative to a client’s activity and exercise includes a
nursing history and physical examination of body alignment, gait,
joint appearance and movement, capabilities and limitations for
movement, muscle mass and strength, activity tolerance, and problems related to immobility.
An activity and exercise history includes daily activity level, activity tolerance, type and frequency of exercise, and factors affecting mobility.
can include actual and potential for inadequate physical energy for
activities, and inactive lifestyle. Other relevant diagnoses are fear (of
falling), impaired self-esteem, potential for falling, and, if the client is
immobilized, many other potential problems such as altered repiratory status and potential for infection.
Body mechanics is the efficient, coordinated, and safe use of the
body to move objects and carry out the ADLs.
Nurses must use good body mechanics in their daily work and
especially when moving and turning clients in bed and assisting
clients to make transfers. Proper body mechanics do not ensure
protection from injury, however, and nurses and caregivers are
encouraged to avoid solo manual lifting, repositioning, and transferring of clients.
Positioning a client in good body alignment and changing the position regularly and systematically are essential aspects of nursing
practice.
Before positioning dependent clients, the nurse should plan a
systematic 24-hour schedule for position changes, including
positions that provide for full extension of the neck, hips, and
knees. The nurse also uses appropriate supportive devices to
maintain alignment and prevent strain on the client’s muscles
and joints.
Before moving, turning, or transferring a client, the nurse must consider the client’s health status and degree of exertion permitted,
physical ability to assist, ability to comprehend instruction, degree
of discomfort, and weight, and whether to use assistive devices or
another caregiver to assist.
The nurse can assist clients to prepare for ambulation by helping
them become as independent as possible while in bed. Ambulating
techniques that facilitate normal walking gait yet provide needed
supports are most effective.
Preambulatory exercises that strengthen the muscles for walking
are essential for clients who have been immobilized for a prolonged
period.
Clients need specific instructions about appropriate use of canes,
walkers, and crutches.
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
TEST YOUR KNOWLEDGE
1. A nurse is working on a hospital committee focused on
preventing back injury in nurses. Which recommendation by this
committee is most likely to result in a decrease in back injuries
if followed?
1. Nurses must wear back belts when lifting clients.
2. All nursing personnel must attend annual body mechanics
education.
3. In order to prevent injury, nurses must strive to become
physically fit.
4. No solo lifting of clients is permitted in the facility.
M44B_BERM9793_11_GE_C44.indd 1162
2. A nurse is caring for a client diagnosed with early osteoporosis.
Which intervention is most applicable for this client?
1. Institute an exercise plan that includes weight-bearing
activities.
2. Increase the amount of calcium in the client’s diet.
3. Protect the client’s bones with strict bed rest.
4. Provide the client with assisted range-of-motion exercising
twice daily.
03/02/2021 18:21
Chapter 44
3. Five minutes after the client’s first postoperative exercise, the
client’s vital signs have not yet returned to baseline. Which is an
appropriate nursing diagnosis?
1. Inadequate physical energy for activities
2. Potential for inadequate physical energy for activities
3. Impaired self-esteem
4. Potential for falling
4. Which statement from a client with one weak leg regarding use
of crutches when using stairs indicates a need for increased
teaching?
1. “Going up, the strong leg goes first, then the weaker leg with
both crutches.”
2. “Going down, the weaker leg goes first with both crutches,
then the strong leg.”
3. “The weaker leg always goes first with both crutches.”
4. “A cane or single crutch may be used instead of both
crutches if held on the weaker side.”
5. A nurse is providing range-of-motion exercising to a client’s
elbow when the client complains of pain. What action should the
nurse take?
1. Stop immediately and report the pain to the client’s physician.
2. Discontinue the treatment and document the results in the
medical record.
3. Reduce the movement of the joint just until the point of slight
resistance.
4. Continue to exercise the joint as before to loosen the stiffness.
6. When assessing a client’s gait, which does the nurse look for
and encourage?
1. The spine rotates, initiating locomotion.
2. Gaze is slightly downward.
3. Toes strike the ground before the heel.
4. Arm on the same side as the swing-through foot moves
forward at the same time.
●
Activity and Exercise
1163
7. Performance of activities of daily living (ADLs) and active rangeof-motion (ROM) exercises can be accomplished simultaneously
as illustrated by which of the following? Select all that apply.
1. Elbow flexion with eating and bathing
2. Elbow extension with shaving and eating
3. Wrist hyperextension with writing
4. Thumb ROM with eating and writing
5. Hip flexion with walking
8. A client weighs 250 pounds and needs to be transferred from
the bed to a chair. Which instruction by the nurse to the assistive
personnel (AP) is most appropriate?
1. “Using proper body mechanics will prevent you from injuring
yourself.”
2. “You are physically fit and at lesser risk for injury when transferring the client.”
3. “Use the mechanical lift and another staff member to transfer
the client from the bed to the chair.”
4. “Use the back belt to avoid hurting your back.”
9. The client is ambulating for the first time after surgery. The
client tells the nurse, “I feel faint.” Which is the best action by
the nurse?
1. Find another nurse for help.
2. Return the client to her room as quickly as possible.
3. Tell the client to take rapid, shallow breaths.
4. Assist the client to a nearby chair.
10. The nurse is performing an assessment of an immobilized client.
Which assessment causes the nurse to take action?
1. Heart rate 86 beats/min
2. Reddened area on sacrum
3. Nonproductive cough
4. Urine output of 50 mL/h
See Answers to Test Your Knowledge in Appendix A.
READINGS AND REFERENCES
Suggested Readings
Andrews, V. D., & Southard, E. P. (2017). Safe patient handling: Keeping health care workers safe. Med-Surg Matters, 26(1), 4–7.
This article highlights the important role that safe patient
handling and mobility programs perform in preventing
employee injuries.
Crawford, A., & Harris, H. (2016). Caring for adults with
impaired physical mobility. Nursing, 46(12), 36–41.
doi:10.1097/01.NURSE.0000504674.19099.1d
This article describes who is at risk for impaired mobility, the hazards of immobility, and nursing assessments
and interventions, including client teaching, for mobility
issues.
Eanes, L. (2018). Too much sitting: A newly recognized
health risk. American Journal of Nursing, 118(9), 26–34.
doi:10.1097/01.NAJ.0000544948.27593.9b
Moderate to vigorous physical activity is an important focus
of health promotion and disease prevention. The author
discusses how more attention and public awareness
need to be given to total daily sitting time and the need for
research in the field of inactivity physiology.
Kowalski, S. L., & Anthony, M. (2017). Nursing’s evolving role in
patient safety. American Journal of Nursing, 117(2), 34–48.
doi:10.1097/01.NAJ.0000512274.79629.3c
A content analysis of AJN articles over 115 years provides
a historical perspective of how client safety increased as
client care became more complex.
Related Research
Choi, S. D., & Brings, K. (2016). Work-related musculoskeletal
risks associated with nurses and nursing assistants handling overweight and obese patients: A literature review.
Work, 53, 439–448. doi:10.3233/WOR-152222
Nievera, R. A., Fick, A., & Harris, H. K. (2017). Effects of ambulation and nondependent transfers on vital signs in patients
receiving norepinephrine. American Journal of Critical Care,
26, 31–36. doi:10.4037/ajcc2017384
M44B_BERM9793_11_GE_C44.indd 1163
Teeple, E., Collins, J. E., Shrestha, S., Dennerlein, J. T., Losina,
E., & Katz, J. N. (2017). Outcomes of safe patient handling
and mobilization programs: A meta-analysis. Work, 58(2),
173–184. doi:10.3233/WOR-172608
Wiggermann, N. (2016). Biomechanical evaluation of
a bed feature to assist in turning and laterally repositioning patients. Human Factors, 58, 748–757.
doi:10.1177/0018720815612625
References
American College of Obstetricians and Gynecologists. (2017).
FAQ: Exercise during pregnancy. Retrieved from http://
www.acog.org/-/media/For%20Patients/faq119.pdf?dmc=
1&ts=20130728T1630124999
American Heart Association. (2018). American Heart Association recommendations for physical activity in adults and
kids. Retrieved from http://www.heart.org/HEARTORG/
HealthyLiving/PhysicalActivity/FitnessBasics/American-HeartAssociation-Recommendations-for-Physical-Activity-inAdults_UCM_307976_Article.jsp#.WNLArxjMzwc
Borg, G. (1998). Borg’s perceived exertion and pain scales.
Champaign, IL: Human Kinetics.
Butcher, H. K., Bulechek, G. M., Dochterman, J. M., &
Wagner, C. M. (Eds.). (2018). Nursing interventions
classification (NIC) (7th ed.). St. Louis, MO: Elsevier.
Centers for Disease Control and Prevention. (2016). Healthy
People 2020 midcourse review: Physical activity. Retrieved
from https://www.cdc.gov/nchs/data/hpdata2020/
HP2020MCR-C33-PA.pdf
Denehy, L., Lanphere, J., & Needham, D. M. (2017). Ten
reasons why ICU patients should be mobilized early.
Intensive Care Medicine, 43(1), 86–90. doi:10.1007/
s00134-016-4513-2
Eanes, L. (2018). Too much sitting: A newly recognized
health risk. American Journal of Nursing, 118(9), 26–34.
doi:10.1097/01.NAJ.0000544948.27593.9b
Fragala, G., Boynton, T., Conti, M. T., Cyr, L., Enos, L., Kelly,
D., . . . Vollman, K. (2016). Patient-handling injuries: Risk
factors and risk-reduction strategies. American Nurse
Today, 11(5), 40–44.
Hashem, M. D., Nelliot, A., & Needham, D. M. (2016). Early
mobilization and rehabilitation in the ICU: Moving back to
the future. Respiratory Care, 61(7), 971–979. doi:10.4187/
respcare.04741
HealthyPeople.gov. (2019). Healthy people 2020 topics
& objectives: Physical activity. Retrieved from https://
www.healthypeople.gov/2020/topics-objectives/topic/
physical-activity
Kappel, S. E., Larsen-Engelkes, J. J., Barnett, R. T., Alexander,
J. W., Klinkhammer, N. L., Jones, M. J., . . . Ye, P. (2018).
Creating a culture of mobility: Using real-time assessment
to drive outcomes. American Journal of Nursing, 118(12),
44–50. doi:10.1097/01.NAJ.0000549690.33457.bb
Kraschnewski, J. L., Sciamanna, C. N., Poger, J. M., Rovniak,
L. S., Lehman, E. B., Cooper, A. B., . . . Ciccolo, J. T.
(2016). Is strength training associated with mortality benefits? A 15 year cohort study of US older adults. Preventive
Medicine, 87, 121–127. doi:10.1016/j.ypmed.2016.02.038
Martin, M., Rogers, K. A., & Matz, M. W. (n.d.). New and
improved VA algorithms/new SPHM app! Retrieved from
https://slideplayer.com/slide/14317268
Miller, H., Rockefeller, K., & Townsend, P. (2017). International
round table discussion: Do gait belts have a role in safe
patient handling programs? International Journal of Safe
Patient Handling & Mobility (SPHM), 7(3), 116–121.
Moorhead, S., Swanson, E., Johnson, M., & Maas, M. L.
(Eds.). (2018). Nursing outcomes classification (NOC)
(6th ed.). St. Louis, MO: Elsevier.
Teeple, E., Collins, J. E., Shrestha, S., Dennerlein, J. T., Losina,
E., & Katz, J. N. (2017). Outcomes of safe patient handling
and mobilization programs: A meta-analysis. Work, 58(2),
173–184. doi:10.3233/WOR-172608
Teodoro, C. R., Breault, K., Garvey, C., Klick, C., O’Brien, J.,
Purdue, T., . . . Matney, L. (2016). STEP-UP: Study of the
effectiveness of a patient ambulation protocol. MEDSURG
Nursing, 25(2), 111–116.
03/02/2021 18:21
1164
Unit 10
●
Promoting Physiologic Health
VHA Center for Engineering & Occupational Safety and Health.
(2016). Safe patient handling and mobility guidebook.
St. Louis, MO: Author.
Walker, L., Docherty, T., Hougendobler, D., Guanowsky, C.,
& Rosenthal, M. (2017). Sharing the lessons: The 10-year
journey of a safe patient movement program. International
Journal of SPHM (Safe Patient Handling & Mobility), 7(1),
20–28.
Weinmeyer, R. (2016). Safe patient handling laws and programs for health care workers. American Medical Association Journal of Ethics, 18, 416–421. doi:10.1001/journalofe
thics.2016.18.4.hlaw1-1604
Selected Bibliography
American Nurses Association. (n.d.). Nurse and Health Care
Worker Protection Act: H.R. 4266/S.2408. Retrieved
from https://www.nursingworld.org/~4af9f9/globalassets/
practiceandpolicy/work-environment/health--safety/
nursehealthcareworkerprotectionact-factsheet.pdf
M44B_BERM9793_11_GE_C44.indd 1164
Bruce, R., & Forry, C. (2018). Integrating a mobility
champion in the intensive care unit. Dimensions of
Critical Care Nursing, 37(4), 201–209. doi:10.1097/
DCC.0000000000000306
Francis, R., & Dawson, J. M. (2016). Special report: Preventing
patient-handling injuries in nurses. American Nurse Today,
11(5), 37–44.
Link, T. (2018). Guideline implementation: Safe patient handling and movement. AORN Journal, 108(6), 663–674.
doi:10.1002/aorn.12423
Occupational Safety and Health Administration. (n.d.). Safe
patient handling: Busting the myths. Retrieved from https://
www.osha.gov/dsg/hospitals/documents/3.1_Mythbusters_508.pdf
Parry, A. (2016). Importance of early mobilisation in critical
care patients. British Journal of Nursing, 25(9), 486–488.
doi:10.12968/bjon.2016.25.9.486
Powell-Cope, G., Pippins, K. M., & Young, H. M. (2017).
Teaching family caregivers to assist safely with
mobility. American Journal of Nursing, 117(12), 49–53.
doi:10.1097/01.NAJ.0000527485.94115.7e
Przybysz, L., & Levin, P. F. (2016). Initial results of an evidencebased safe patient handling and mobility program to
decrease hospital worker injuries. Workplace Health &
Safety, 65, 83–88. doi:10.1177/2165079916670162
Reames, C. D., Price, D. M., King, E. A., & Dickinson, S.
(2016). Mobilizing patients along the continuum of critical care. Dimensions of Critical Care Nursing, 35, 10–15.
doi:10.1097/DCC.0000000000000151
Rion, J. H. (2016). The walk to save: Benefits of inpatient cardiac rehabilitation. MEDSURG Nursing, 25(3), 159–162.
Spinlife. (n.d.). Wheelchair store: Manual wheelchairs.
Retrieved from http://www.spinlife.com/category
.cfm?categoryID=2
03/02/2021 18:21
Sleep
45
LEA R N IN G OU TC OME S
After completing this chapter, you will be able to:
1. Explain the physiology and the functions of sleep.
2. Identify the characteristics of the NREM and REM sleep states.
3. Describe variations in sleep patterns throughout the lifespan.
4. Identify factors that affect sleep.
5. Describe common sleep disorders.
6. Identify the components of a sleep pattern assessment.
7. Develop nursing diagnoses, outcomes, and nursing interventions related to sleep problems.
8. Describe interventions that promote sleep.
K EY T E RMS
biological rhythms, 1166
electroencephalogram (EEG), 1177
electromyogram (EMG), 1177
electro-oculogram (EOG), 1177
hypersomnia, 1174
insomnia, 1173
narcolepsy, 1174
nocturnal emissions, 1170
Introduction
Sleep is a basic human need; it is a universal biological
process common to all individuals. Humans spend about
one-third of their lives asleep. We require sleep for many
reasons: to cope with daily stresses, to prevent fatigue,
to conserve energy, to restore the mind and body, and
to enjoy life more fully. Sleep enhances daytime functioning and is vital for cognitive, physiologic, and psychosocial function. Sleeping allows the brain to restore
itself. During sleep the body clears itself of adenosine.
This action allows an individual to awaken feeling alert
and refreshed (Sleep.org, n.d.). Sleep is an important
factor in an individual’s quality of life, and sleep disorders and sleep deprivation are contributing factors
to the development of many chronic diseases, such as
type 2 diabetes, heart disease, depression, and obesity,
as reported by the Centers for Disease Control and Prevention (CDC, 2018). It is estimated that 50 million to
70 million Americans suffer from a chronic disorder of
sleep and wakefulness that hinders daily functioning
and adversely affects health. All ages are affected by
sleep disorders. According to the CDC, the prevalence
of short sleep duration, sleep-disordered breathing, and
behavioral sleep problems in children ages 3 to 5 years is
20% to 50%. Sleep-disordered breathing is characterized
by snoring or obstructive sleep apnea. As with adults,
sleep problems in children can adversely affect cognitive and social development (Bonuck, Blank, True-Felt, &
Chervin, 2016). Wheaton, Jones, Cooper, and Croft (2018)
state that children and adolescents who have sleep deprivation have an increased risk of attention and behavioral
NREM sleep, 1167
parasomnia, 1175
polysomnography, 1177
REM sleep, 1167
sleep, 1165
sleep apnea, 1174
sleep architecture, 1167
sleep hygiene, 1178
problems, experience poor mental health, and have a
greater likelihood of poor academic performance.
There are five health-related behaviors that lead to
the development of chronic disease. Smoking, alcohol
consumption, obesity, lack of exercise, and insufficient
amounts of sleep contribute to an increased risk of hypertension, diabetes, obesity, depression, heart attack, and
stroke (Liu et al., 2016).
Physiology of Sleep
Historically, sleep was considered a state of unconsciousness. More recently, sleep has come to be considered an
altered state of consciousness in which the individual’s perception of and reaction to the environment are decreased.
Sleep is characterized by minimal physical activity, variable
levels of consciousness, changes in the body’s physiologic
processes, and decreased responsiveness to external stimuli. Some environmental stimuli, such as a smoke detector
alarm, will usually awaken a sleeper, whereas many other
noises will not. It appears that individuals respond to meaningful stimuli while sleeping and selectively disregard nonmeaningful stimuli. For example, a mother may respond
to her baby’s crying but not to the crying of another baby.
The cyclic nature of sleep is thought to be controlled
by centers located in the lower part of the brain. Neurons
within the reticular formation, located in the brainstem,
integrate sensory information from the peripheral nervous
system and relay the information to the cerebral cortex
(see Anatomy & Physiology Review). The upper part of
the reticular formation consists of a network of ascending
nerve fibers called the reticular activating system (RAS),
1165
M45_BERM9793_11_GE_C45.indd 1165
27/01/2021 18:05
1166
Unit 10
●
Promoting Physiologic Health
which is involved with the sleep-wake cycle. An intact
cerebral cortex and reticular formation are necessary for
the regulation of sleep and waking states.
Neurotransmitters, located within neurons in the
brain, affect the sleep-wake cycle. For example, serotonin
is thought to lessen the response to sensory stimulation
and gamma-aminobutyric acid (GABA) to shut off the
activity in the neurons of the reticular activating system.
Another key factor to sleep is exposure to darkness. Darkness and preparing for sleep (e.g., lying down, decreasing
noise) cause a decrease in stimulation of the RAS. During
this time, the pineal gland in the brain begins to actively
secrete the natural hormone melatonin, and the individual feels less alert. During sleep, the growth hormone is
secreted and cortisol is inhibited.
With the beginning of daylight, melatonin is at its lowest level in the body and the stimulating hormone, cortisol,
is at its highest. Wakefulness is also associated with high
levels of acetylcholine, dopamine, and noradrenaline. Acetylcholine is released in the reticular formation, dopamine
in the midbrain, and noradrenaline in the pons. These neurotransmitters are localized within the reticular formation
and influence cerebral cortical arousal.
Circadian Rhythms
Biological rhythms exist in plants, animals, and humans.
In humans, these are controlled from within the body and
synchronized with environmental factors, such as light and
darkness. The most familiar biological rhythm is the circadian rhythm. It is a sort of 24-hour internal biological clock.
The term circadian is from the Latin circa dies, meaning “about
a day.” Although sleep and waking cycles are the best known
of the circadian rhythms, body temperature, blood pressure,
and many other physiologic functions also follow a circadian pattern and are affected by changes in sleep patterns.
ANATOMY & PHYSIOLOGY REVIEW
Reticular Activating System
Nerve impulses from the senses reach the reticular activating system (RAS), which is in the reticular formation (located in the brainstem) with projections to the
hypothalamus and cerebral cortex. The nerve fibers in the
RAS relay impulses to the cerebral cortex for perception
by the individual.
Cerebral
cortex
Hypothalamus
Midbrain
Pons
Reticular formation
Brainstem
Cerebellum
Sensory input
cutaneous
visual
auditory
visceral
The reticular formation in the brainstem.
QUESTIONS
1. How would you describe activity of the RAS in preparation for and during sleep?
2. What happens physiologically when your alarm clock
wakes you in the morning?
M45_BERM9793_11_GE_C45.indd 1166
3. What areas of the brain are affected by head trauma
or stroke and affect an individual’s level of alertness?
Answers to Anatomy & Physiology Review Questions are available on the faculty resources
site. Please consult with your instructor.
27/01/2021 18:05
Chapter 45
Chronic sleep loss can lead to cardiovascular morbidity, obesity, and metabolic dysfunction (Morgenthaler et al., 2016).
Sleep is a complex biological rhythm. When an individual’s biological clock coincides with the sleep-wake
cycles, the individual is said to be in circadian synchronization; that is, the individual is awake when the body
temperature is highest, and asleep when the body temperature is lowest. Circadian regularity begins to develop
by the 6th week of life, and by 3 to 6 months most infants
have a regular sleep-wake cycle.
Types of Sleep
Sleep architecture refers to the basic organization of normal sleep. The two types of sleep are NREM (non–rapideye-movement) sleep and REM (rapid-eye-movement)
sleep. During sleep, NREM and REM sleep alternate in
cycles. Changes in the architecture of one’s sleep can
be linked to physiologic or psychosocial changes. For
example, Williams syndrome is a genetic disorder of neurodevelopment that results in cognitive changes. Clients
diagnosed with Williams syndrome have alterations in
sleep patterns resulting in decreased sleep efficacy that
affects their ability to learn, attention span, and behavior
(Martens, Seyfer, Andridge, & Coury, 2017).
NREM Sleep
NREM sleep occurs when activity in the RAS is inhibited.
About 75% of sleep during a night is NREM sleep. NREM
sleep was previously divided into four stages. It is now
divided into three stages. Each of the stages is associated
with distinct brain activity and physiology. Stage 1 is the
stage of very light sleep and lasts only a few minutes. During this stage, the individual feels drowsy and relaxed, the
eyes roll from side to side, and the heart and respiratory rates
drop slightly. The sleeper can be readily awakened and may
deny that he or she was sleeping. Low-voltage brain waves
are noted in stage 1 (National Sleep Foundation, 2018).
Stage 2 is the stage of sleep during which body processes
continue to slow down. The eyes are generally still, the heart
and respiratory rates decrease slightly, and body temperature
falls. An individual in stage 2 requires more intense stimuli
than in stage 1 to awaken, such as touching or shaking.
Stage 3 is the deepest stage of sleep, differing only in
the percentage of delta waves recorded during a 30-second
period. During deep sleep or delta sleep, the sleeper’s heart
and respiratory rates drop 20% to 30% below those exhibited during waking hours. The sleeper is difficult to arouse.
The individual is not disturbed by sensory stimuli, the
skeletal muscles are very relaxed, reflexes are diminished,
and snoring is most likely to occur. This stage is essential
for restoring energy and releasing important growth hormones (Box 45.1).
REM Sleep
REM sleep usually recurs about every 90 minutes and lasts
5 to 30 minutes. Most dreams take place during REM sleep
but usually will not be remembered unless the individual
arouses briefly at the end of the REM period.
M45_BERM9793_11_GE_C45.indd 1167
BOX 45.1
•
•
•
•
•
•
•
•
●
Sleep
1167
Physiologic Changes During
NREM Sleep
Arterial blood pressure falls.
Pulse rate decreases.
Peripheral blood vessels dilate.
Cardiac output decreases.
Skeletal muscles relax.
Basal metabolic rate decreases 10% to 30%.
Growth hormone levels peak.
Intracranial pressure decreases.
Clinical Alert!
Sleep deprivation in hospitalized clients contributes to delirium. Delirium initially presents as agitation, confusion, or combative behavior.
Secondary delirium is hypoactive with inattention and disorganized
thoughts (Miller, 2015).
During REM sleep, the brain is highly active, and
brain metabolism may increase as much as 20%. For example, during REM sleep, levels of acetylcholine and dopamine increase, with the highest levels of acetylcholine
release occurring during REM sleep. Because both of these
neurotransmitters are associated with cortical activation, it
makes sense that their levels would be high during dreaming sleep. This type of sleep is also called paradoxical sleep
because electroencephalogram (EEG) activity resembles
that of wakefulness. Distinctive eye movements occur,
voluntary muscle tone is dramatically decreased, and
deep tendon reflexes are absent. In this phase, the sleeper
may be difficult to arouse or may wake spontaneously,
gastric secretions increase, and heart and respiratory rates
often are irregular. It is thought that the regions of the
brain that are used in learning, thinking, and organizing
information are stimulated during REM sleep.
Clinical Alert!
Clients who experience sleep deprivation will more commonly experience an increase in fatigue. Sleep deprivation results in a significant
increase in thyroid stimulating hormone, which increases tension,
anger, and hostility (Ozdemir & Atilla, 2017; Selvi, Kilic, Aydin, & Guzel
Oxdemir, 2015).
Sleep Cycles
During a sleep cycle, individuals typically pass through
NREM and REM sleep, the complete cycle usually lasting
about 90 to 110 minutes in adults. In the first sleep cycle,
a sleeper usually passes through the first two stages of
NREM sleep in a total of about 20 to 30 minutes. Stage 3
lasts about 50 to 60 minutes. After stage 3 NREM, the sleep
passes back through stages 2 and 1 over about 20 minutes.
Thereafter, the first REM stage occurs, lasting about
10 minutes, completing the first sleep cycle. It is not unusual
for the first REM period to be very brief or even skipped
entirely. The healthy adult sleeper usually experiences four
to six cycles of sleep during 7 to 8 hours (Figure 45.1 ■).
27/01/2021 18:05
1168
Unit 10
●
Promoting Physiologic Health
Wake
REM
NREM 1
NREM 2
NREM 3
Figure 45.1 ■ Time spent in REM and non-REM stages of sleep in
an adult.
The sleeper who is awakened during any stage must begin
anew at stage 1 NREM sleep and proceed through all stages
to REM sleep.
The duration of NREM stages and REM sleep varies
throughout the sleep period. During the early part of the
night, the deep sleep periods are longer. As the night progresses, the sleeper spends less time in stage 3 of NREM
sleep. REM sleep increases and dreams tend to lengthen.
Before sleep ends, periods of near wakefulness occur, and
stages 1 and 2 NREM and REM sleep dominate.
Functions of Sleep
The effects of sleep on the body are not completely understood. Sleep exerts physiologic effects on both the nervous
system and other body structures. Sleep in some way
restores normal levels of activity and normal balance among
parts of the nervous system. Sleep is also necessary for protein synthesis, which allows repair processes to occur.
The role of sleep in psychologic well-being is best
noticed by the deterioration in mental functioning related
to sleep loss. Individuals with inadequate amounts of
sleep tend to become emotionally irritable, have poor
concentration, and experience difficulty making decisions.
Normal Sleep Patterns
and Requirements
Although it used to be believed that maintaining a regular
sleep–wake rhythm is more important than the number of
hours actually slept, recent research has shown that sleep
deprivation is associated with significant cognitive and
health problems. Although reestablishing the sleep–wake
rhythm (e.g., after the disruption of surgery) is important,
it is appropriate to allow and encourage daytime napping
in hospitalized clients.
Newborns
Newborns sleep 12 to 18 hours a day, on an irregular schedule with periods of 1 to 3 hours spent awake. Unlike older
children and adults, newborns enter REM sleep (called
active sleep during the newborn period) immediately.
Rapid eye movements are observable through closed lids,
and the body movements and irregular respirations may
M45_BERM9793_11_GE_C45.indd 1168
be observed. NREM sleep (also called quiet sleep during
the newborn period) is characterized by regular respirations, closed eyes, and the absence of body and eye movements. Newborns spend nearly 50% of their time in each
of these states, and the sleep cycle is about 50 minutes.
It is best to put newborns to bed when they are sleepy
but not asleep. Newborns can be encouraged to sleep less
during the day by exposing them to light and by playing more with them during the day hours. As evening
approaches, the environment can be less bright and quieter with less activity. Babies will even need a winding
down time with no computer or tablet screen time and
exposure to phones (National Sleep Foundation, n.d.c).
Infants
At first, infants awaken every 3 or 4 hours, eat, and then go
back to sleep. Periods of wakefulness gradually increase
during the first months. By 6 months, most infants sleep
through the night (from midnight to 5 a.m.) and begin to
establish a pattern of daytime naps. At the end of the first
year, an infant usually takes two naps per day and should
get about 14 to 15 hours of sleep in 24 hours.
About half of the infant’s sleep time is spent in light
sleep. During light sleep, the infant exhibits a great deal
of activity, such as movement, gurgles, and coughing. Parents need to make sure that infants are truly awake before
picking them up for feeding and changing. Putting infants
to bed when they are drowsy but not asleep helps them to
become “self-soothers.” This means that they fall asleep
independently and if they do awake at night, they can
put themselves back to sleep. Infants who become used
to parental assistance at bedtime will experience shorter
sleep intervals with nighttime wakening (Cowie, Palmer,
Hussain, & Alfano, 2016).
Toddlers
Between 12 and 14 hours of sleep are recommended
for children 1 to 3 years of age. Most still need an afternoon nap, but the need for midmorning naps gradually
decreases. The toddler may exhibit a great deal of resistance to going to bed and may awaken during the night.
Nighttime fears and nightmares are also common. A
security object such as a blanket or stuffed animal may
help. Parents need assurance that if the child has had adequate attention from them during the day, maintaining a
daily sleep schedule and consistent bedtime routine will
promote good sleep habits for the entire family (National
Sleep Foundation, n.d.a).
Preschoolers
The preschool-age child (3 to 5 years of age) requires 11 to
13 hours of sleep per night, particularly if the child is in
preschool. Sleep needs fluctuate in relation to activity and
growth spurts. Many children of this age dislike bedtime
and resist by requesting another story, game, or television
27/01/2021 18:05
Chapter 45
●
Sleep
1169
program. The 4- to 5-year-old may become restless and
irritable if sleep requirements are not met (National Sleep
Foundation, n.d.c).
Parents can help children who resist bedtime by maintaining a regular and consistent sleep schedule. It also helps
to have a relaxing bedtime routine that ends in the child’s
room. Preschool children wake up frequently at night, and
they may be afraid of the dark or experience night terrors or
nightmares. Often limiting or eliminating TV will reduce the
number of nightmares (National Sleep Foundation, n.d.c).
School-Age Children
The school-age child (5 to 12 years of age) needs 10 to
11 hours of sleep per night, but most receive less because
of increasing demands (e.g., homework, sports, social
activities). They may also be spending more time at
the computer and watching TV. Some may be drinking
caffeinated beverages. All of these activities can lead to
difficulty falling asleep and fewer hours of sleep. Nurses
can teach parents and school-age children about healthy
sleep habits. A regular and consistent sleep schedule and
bedtime routine need to be continued.
Clinical Alert!
Children who have a TV or computer in their bedroom are more likely
to get less sleep.
Adolescents
Adolescents (12 to 18 years of age) require 8 to 10 hours
of sleep each night; however, few actually get that
much sleep (Figure 45.2 ■) (National Sleep Foundation,
n.d.g). Teens are sleepy at times and in places where
they should be fully awake—at school, at home, and
on the road. This can result in lower grades, negative
moods (e.g., unhappy, sad, tense), and increased potential for car crashes. Interestingly, the National Sleep
Foundation (n.d.d) found that although more than half
of adolescents knew they were not getting enough sleep,
90% of the parents believed their adolescent was getting enough sleep. Nurses can teach parents to recognize signs and symptoms that indicate their teen is sleep
deprived (Box 45.2).
Figure 45.2 ■ Many adolescents do not get enough sleep.
As children reach adolescence, their circadian
rhythms tend to shift. Research in the 1990s found that
later sleep and wake patterns among adolescents are biologically determined; the natural tendency for teenagers is to stay up late at night and wake up later in the
morning. A psychosocial factor affecting later bedtime in
the adolescent population is the desire for greater independence. Using the internet, watching television, and
cell phone usage disrupt the ability to fall asleep due to
BOX 45.2
Sleep Deprivation and Sleep Problems
in Teens
The teen:
• Has difficulty waking in the morning for school.
• Falls asleep in class or during quiet times of the day.
• Increases the use of caffeinated beverages like coffee, soda,
or energy drinks.
• Feels tired, making it difficult to initiate or persist in projects
such as a school assignment.
• Is irritable, anxious, and angers easily on days when he or she
gets less sleep.
• Is involved in many extracurricular activities, has a job, and
stays up late doing homework every night, cutting into
sleep time.
• Sleeps extra long periods of time on the weekend.
EVIDENCE-BASED PRACTICE
Evidence-Based Practice
Do Adolescents with Smartphones Sleep Less Than Those
Without Smartphones?
Schweizer, Berchtold, Barrense-Dias, Akre, and Suris (2017) conducted a longitudinal study assessing the effect adolescent use of
smartphones has on sleep duration. Five hundred and ninety-one
adolescents participated in the study. The mean age of the participants was 14.3 years. The participants were divided into owners
of a smartphone, new owners of a smartphone after 2 years, and
nonowners. Each adolescent was asked to indicate how much
M45_BERM9793_11_GE_C45.indd 1169
sleep he or she attained nightly during school days and on weekends. In conclusion, smartphone owners experienced greater
sleep problems. The disruption of sleep was most commonly
associated with shorter sleep duration.
Implications
Smartphones are just like computers. Parents and adolescents
should be instructed to leave the phone in another area of the
home to enhance sleep outcomes.
27/01/2021 18:05
1170
Unit 10
●
Promoting Physiologic Health
blue-spectrum light exposure. A blue-light screen protector can reduce exposure to blue light (Kreieger, 2017).
In 2014 the American Academy of Pediatrics, the
Adolescent Sleep Working Group, and the Committee on
Adolescence, led by Dr. Judith Owens, reported that adolescents who do not receive adequate sleep tend to be
overweight; do not engage in daily exercise; may smoke,
drink, or use illicit drugs; and perform poorly in school.
In 2014 the American Academy of Pediatrics released a
policy statement encouraging school districts to implement later start times for middle and high school students.
It is important for nurses and healthcare professionals to
educate private and public schools on adolescent sleep
and the importance of later start times.
During adolescence, boys begin to experience nocturnal
emissions (orgasm and emission of semen during sleep),
known as “wet dreams,” several times each month. Boys
need to be informed about this normal development to
prevent embarrassment and fear.
Most healthy adults get 7 to 9 hours of sleep per
night. This amount of sleep will assist in decreasing
daytime sleepiness and contribute to health (National
Sleep Foundation, n.d.b). However, individual needs
do vary—some adults may be able to function well
(e.g., without sleepiness or drowsiness) with 6 hours of
sleep, and others may need 10 hours to function optimally. Signs that may indicate that an individual is not
getting enough sleep include falling asleep or becoming drowsy during a task that is not fatiguing (e.g., listening to a presentation), not being able to concentrate
or remember information, and being unreasonably
irritable with others. Lack of sleep also contributes to
short-term memory loss and inadequate performance
on newly learned tasks. Taking a nap in the middle of
the day improves mood, increases memory, reduces
fatigue, and lowers blood pressure (National Sleep
Foundation, n.d.h).
Adults are particularly vulnerable to sleep deprivation. Factors that contribute to diminished sleep include
stress, depression, pain, shift work, travel, and lifestyle
roles, such as job, student, or parenting. Adults working long hours or multiple jobs may find their sleep less
refreshing. A study by Owens, Allen, and Moultrie (2017)
examined the impact shift work had on nurses’ quality
of sleep. The descriptive study revealed that nurses are
fatigued from working long consecutive shifts. Working
shifts also affects their quality of life. The sleep habits of
children also have an impact on the adults caring for them.
A woman’s sleep pattern is more commonly affected by
the birth of a child. However, both parents of infants and
young children experience fatigue related to interrupted
sleep or sleep deprivation. This lack of sleep is associated with lower parental competence and greater stress
(Corkin et al., 2017). Biological conditions such as pregnancy, menses, and the perimenopausal period can also
affect a woman’s sleep patterns.
Nurses need to teach adults the importance of
obtaining sufficient sleep and provide tips on how to
M45_BERM9793_11_GE_C45.indd 1170
promote sleep that results in the client waking up feeling restored or refreshed. See Client Teaching later in
this chapter.
Older Adults
A hallmark change with age is a tendency toward earlier
bedtime and wake times. Older adults (65 to 75 years) usually awaken 1.3 hours earlier and go to bed approximately
1 hour earlier than younger adults (ages 20 to 30). Older
adults may show an increase in disturbed sleep that can
create a negative impact on their quality of life, mood,
and alertness. They may awaken an average of six times
during the night. Although the ability to sleep becomes
more difficult, the need to sleep does not decrease with
age. During sleep, an older adult has a flattened circadian rhythm. This is noted by the earlier bedtime and
morning arousal. The circadian rhythm changes due to a
decreased responsiveness of the superchiasmatic nucleus.
This is what controls the internal clock to respond to cues
such as light (Richards, Demartini, & Xiong, 2018). Older
adults have difficulty falling back to sleep after awakening
and have a diminished amount of REM sleep. Many older
adults report daytime napping, which may contribute to
reduced nocturnal sleep.
Medical conditions and pain are factors that interrupt
sleep. Older adults who have several medical conditions
and complain of having sleeping problems should discuss
this with their primary care provider. The older individual may have a major sleep disorder that is complicating
treatment of other conditions. It is important for the nurse
to teach about the connection between sleep, health, and
aging. See Client Teaching about sleep promotion later in
this chapter.
Some older clients with dementia may experience sundown syndrome. Although not a sleep disorder
directly, it refers to a pattern of symptoms (e.g., agitation, anxiety, aggression, and sometimes delusions) that
occur in the late afternoon (thus the name). These symptoms can last through the night, further disrupting sleep
(Graff-Radford, 2017).
Factors Affecting Sleep
Both the quality and the quantity of sleep are affected by
a number of factors. Sleep quality is a subjective characteristic and is often determined by whether an individual
wakes up feeling energetic or not. Quantity of sleep is the
total time the individual sleeps.
Illness
Illness that causes pain or physical distress (e.g., arthritis,
back pain) can result in sleep problems. Individuals who
are ill require more sleep than normal, and the normal
rhythm of sleep and wakefulness is often disturbed. Individuals deprived of REM sleep subsequently spend more
sleep time than normal in this stage.
27/01/2021 18:05
Chapter 45
Respiratory conditions can disturb an individual’s
sleep. Shortness of breath often makes sleep difficult, and
individuals who have nasal congestion or sinus drainage
may have trouble breathing and hence may find it difficult
to sleep.
Individuals who have gastric or duodenal ulcers may
find their sleep disturbed because of pain, often a result of
the increased gastric secretions that occur during REM sleep.
Certain endocrine disturbances can also affect sleep.
Hyperthyroidism lengthens presleep time, making it difficult for a client to fall asleep. Hypothyroidism, conversely,
decreases stage 3 sleep. Women with low levels of estrogen often report excessive fatigue. In addition, they may
experience sleep disruptions due, in part, to the discomfort associated with hot flashes or night sweats that can
occur with reduced estrogen levels.
Elevated body temperatures can cause some reduction in delta sleep and REM sleep. The need to urinate
during the night also disrupts sleep, and individuals who
awaken at night to urinate sometimes have difficulty getting back to sleep.
●
Sleep
1171
Environment
Environment can promote or hinder sleep. The individual
must be able to achieve a state of relaxation prior to entering a period of sleep. Any change, such as noise in the environment, can inhibit sleep. The absence of usual stimuli or
the presence of unfamiliar stimuli can prevent individuals
from sleeping. Hospital environments can be quite noisy,
and special care needs to be taken to reduce noise in the
hallways and nursing care units. In fact, some hospitals
have instituted “quiet times” in the afternoon on nursing
units where the lights are lowered and activity and noise
are purposefully decreased so clients can rest or nap.
Discomfort from environmental temperature (e.g., too
hot or cold) and lack of ventilation can affect sleep. Light
levels can be another factor. An individual accustomed to
darkness while sleeping may find it difficult to sleep in the
light. Another influence includes the comfort and size of
the bed. An individual’s partner who has different sleep
habits, snores, or has other sleep difficulties may become
a problem for the individual also.
LIFESPAN CONSIDERATIONS Sleep Disturbances
CHILDREN
Learning to sleep alone without the parent’s help is a skill that all
children need to master. Regular bedtime routines and rituals such
as reading a book help children learn this skill and can prevent sleep
disturbance. Some sleep disturbances seen in children include the
following:
• Trained night feeder. Infants who are fed during the night,
who are fed until they fall asleep and then put into bed,
or who have a bottle left with them in their bed learn to
expect and demand middle-of-the-night feedings. Infants
who are growing well do not need night feeding after about
4 months of age. Infants should never be put to bed with
a bottle. This practice increases the risk of otitis media.
Infants who are diagnosed with failure to thrive may need
to be fed at night.
• Sleep refusal. Many toddlers and young children are resistant
to settling down to sleep. This sleep refusal may be due to not
being tired, anxiety about separation from the parent, stress
(e.g., a recent move), lack of a regular sleep routine, the child’s
temperament, or changes in sleep arrangements (e.g., move
from a crib to a “big” bed).
• Night terrors. Night terrors are partial awakenings from NREM
stage 3 sleep. They are usually seen in children 3 to 6 years of
age. The child may sleepwalk, or may sit up in bed screaming and thrashing about. They usually cannot be wakened,
but should be protected from injury, helped back to bed, and
soothed back to sleep. Babysitters should be alerted to the
possibility of a night terror occurring. Children do not remember
the incident the next day, and there is no indication of a neurologic or emotional problem. Excessive fatigue and a full bladder
may contribute to the problem. Having the child take an afternoon nap and empty the bladder before going to sleep at night
may be helpful.
ADULTS
• New jobs, pregnancy, and babies are common examples that
often disrupt the sleep of a young adult.
M45_BERM9793_11_GE_C45.indd 1171
The sleep patterns of middle-aged adults can be disrupted by
the need to take care of older parents or chronically ill partners
in the home.
• See Client Teaching later in this chapter for tips on promoting
sleep.
•
OLDER ADULTS
The quality of sleep is often diminished in older adults. Some of the
leading factors that often are influential in sleep disturbances include
the following:
• Side effects of medications
• Gastric reflux disease
• Respiratory and circulatory disorders, which may cause
breathing problems or discomfort
• Pain from arthritis, increased stiffness, or impaired mobility
• Nocturia
• Depression
• Loss of life partner or close friends
• Confusion related to delirium or dementia.
Interventions to promote sleep and rest can help enhance the rejuvenation and renewal that sleep provides. The following interventions
can help promote sleep:
• Reduce or eliminate the consumption of caffeine and nicotine.
• Be sure the environment is warm and safe, especially if clients
get out of bed during the night.
• Provide comfort measures, such as analgesics if indicated, and
proper positioning.
• Enhance the sense of safety and security by checking on
clients frequently and making sure that the call light is within
reach. Answer the call light promptly.
• If lack of sleep is caused by medications or certain health conditions, interventions should focus on resolving the underlying
problem.
• Evaluate the situation and find out what the rest and sleep
disturbances mean to the client. The client may not perceive
nighttime sleeplessness to be a serious problem, and will just
do other activities and sleep when tired.
27/01/2021 18:05
1172
Unit 10
●
Promoting Physiologic Health
Lifestyle
Smoking
Following an irregular morning and nighttime schedule can affect sleep. Moderate exercise in the morning
or early afternoon is usually conducive to sleep, but
exercise late in the day can delay sleep. The individual’s ability to relax before retiring is an important factor
affecting the ability to fall asleep. It is best, therefore,
to avoid doing homework or office work before or after
getting into bed.
Night shift workers frequently obtain less sleep than
other workers and have difficulty falling asleep after
getting off work. Wearing dark wraparound sunglasses
during the drive home and light-blocking shades in the
bedroom can minimize the alerting effects of exposure to
daylight, thus making it easier to fall asleep when body
temperature is rising.
Nicotine has a stimulating effect on the body, and smokers often have more difficulty falling asleep than nonsmokers. Smokers are usually easily aroused and often
describe themselves as light sleepers. By refraining
from smoking after the evening meal, the individual
usually sleeps better; moreover, many former smokers
report that their sleeping patterns improved once they
stopped smoking.
Emotional Stress
Stress is considered by most sleep experts to be the one
of the greatest causes of difficulties in falling asleep or
staying asleep. Clients who are consistently exposed to
stress will increase the activation of the hypothalamic–
pituitary–adrenal (HPA) axis leading to sleep disorders.
An individual who becomes preoccupied with personal problems (e.g., school- or job-related pressures,
family or marriage problems) may be unable to relax
sufficiently to get to sleep. Anxiety increases the norepinephrine blood levels through stimulation of the sympathetic nervous system. This chemical change results
in less deep and REM sleep and more stage changes and
awakenings.
Stimulants and Alcohol
Caffeine-containing beverages act as stimulants of the
central nervous system (CNS). Drinking beverages
containing caffeine in the afternoon or evening may
interfere with sleep. Individuals who drink an excessive amount of alcohol often find their sleep disturbed.
Alcohol disrupts REM sleep, although it may hasten the
onset of sleep. While making up for lost REM sleep after
some of the effects of the alcohol have worn off, individuals often experience nightmares. The alcohol-tolerant
individual may be unable to sleep well and become irritable as a result.
Diet
Weight gain has been associated with reduced total sleep
time as well as broken sleep and earlier awakening.
Weight loss, on the other hand, seems to be associated
with an increase in total sleep time and less broken sleep.
Dietary L-tryptophan—found, for example, in cheese and
milk—may induce sleep, a fact that might explain why
warm milk helps some individuals get to sleep.
M45_BERM9793_11_GE_C45.indd 1172
Motivation
Motivation can increase alertness in some situations (e.g.,
a tired individual can probably stay alert while attending
an interesting concert or surfing the web late at night).
Motivation alone, however, is usually not sufficient to
overcome the normal circadian drive to sleep during the
night. Nor is motivation sufficient to overcome sleepiness
due to insufficient sleep. A combination of boredom and
lack of sleep can contribute to feeling tired.
Medications
Some medications affect the quality of sleep. Most hypnotics can interfere with deep sleep and suppress REM
sleep. Beta blockers have been known to cause insomnia
and nightmares. Narcotics, such as morphine, are known
to suppress REM sleep and to cause frequent awakenings
and drowsiness. Tranquilizers interfere with REM sleep.
Although antidepressants suppress REM sleep, this effect
is considered a therapeutic action. In fact, selectively
depriving a depressed client of REM sleep will result in
an immediate but transient improvement in mood. Clients
accustomed to taking hypnotic medications and antidepressants may experience a REM rebound (increased REM
sleep) when these medications are discontinued. Warning
clients to expect a period of more intense dreams when
these medications are discontinued may reduce their
anxiety about this symptom. Boxes 45.3 and 45.4, respectively, list drugs that can disrupt sleep or cause excessive
daytime sleepiness.
BOX 45.3
Drugs That Disrupt Sleep
These drugs may disrupt REM sleep, delay onset of sleep, or
decrease sleep time:
• Alcohol
• Amphetamines
• Antidepressants
• Beta-blockers
• Bronchodilators
• Caffeine
• Decongestants
• Narcotics
• Steroids
27/01/2021 18:05
Chapter 45
BOX 45.4
Drugs That May Cause Excessive
Daytime Sleepiness
These drugs may be associated with excessive daytime sleepiness:
• Antidepressants
• Antihistamines
• Beta blockers
• Narcotics
Common Sleep Disorders
A knowledge of common sleep disorders can help nurses
assess the sleep complaints of their clients and, when
appropriate, make a referral to a specialist in sleep disorders medicine. Although sleep disorders are typically
categorized for the purpose of research as dyssomnias,
parasomnias, and disorders associated with medical or
psychiatric illness, it is usually more appropriate for clinicians to focus on the client’s symptoms (e.g., insomnia,
excessive sleepiness, and abnormal events) that occur during sleep (parasomnias).
Insomnia
Insomnia is described as the inability to fall asleep or
remain asleep. Individuals with insomnia do not awaken
feeling rested. Insomnia is the most common sleep complaint in America. Acute insomnia lasts one to several
nights and is often caused by personal stressors or worry.
If the insomnia persists for longer than a month, it is
considered chronic insomnia. More often, individuals
experience chronic-intermittent insomnia, which means
difficulty sleeping for a few nights, followed by a few
nights of adequate sleep before the problem returns
(National Sleep Foundation, n.d.i). See Box 45.5 for
●
Sleep
1173
symptoms of insomnia. The two main risk factors for
insomnia are older age and female gender (National
Sleep Foundation, n.d.e). Women suffer sleep loss in
connection with hormonal changes (e.g., menstruation,
pregnancy, and menopause). The incidence of insomnia
increases with age, but it is thought that this is caused by
some other medical condition.
Treatment for insomnia frequently requires the client
to develop new behavior patterns that induce sleep and
maintain it. Examples of behavioral treatments include the
following:
Stimulus control: creating a sleep environment that
promotes sleep
Cognitive therapy: learning to develop positive
thoughts and beliefs about sleep
Sleep restriction: limiting time in bed in order to get to
sleep and stay asleep throughout the night.
•
•
•
BOX 45.5
•
•
•
•
•
•
•
•
•
•
•
•
Insomnia
Difficulty falling asleep
Waking up too early or frequently during the night
Difficulty returning to sleep
Waking up too early in the morning
Unrefreshing sleep
Daytime sleepiness
Difficulty concentrating
Irritability
Non-restorative sleep
Fatigue and irritability
Difficulty at work or school
Difficulty with personal relationships
From Insomnia: Symptoms, National Sleep Foundation, n.d.f. Retrieved from https://
sleepfoundation.org/insomnia/content/symptoms
EVIDENCE-BASED PRACTICE
Evidence-Based Practice
What Are the Interventions to Promote Sleep and Rest
in Hospitalized Clients?
Vincensi et al. (2016) conducted research with a threefold
purpose. The first purpose of the study was to describe nursing interventions used to promote sleep. The second purpose
was to determine the interventions nurses and clients identified
as most effective. The study also sought to obtain feedback
on the noninvasive biomedical device called the Vital Sleep
headband. The Vital Sleep headband is a medical device that
eliminates noise to promote sleep. It also monitors the client’s
vital signs and transmits the results to the nurses’ station.
A cross-sectional survey design was implemented to determine
if nurses and clients perceived the same sleep disturbances.
The study included 87 nurses and 34 clients. Both the clients
and nurses perceived that the biggest interruptions to sleep
were the administration of medications, vital sign checks,
M45_BERM9793_11_GE_C45.indd 1173
and pain. The most effective nursing interventions to promote
sleep reported by the clients and nurses were the administration of pharmacologic interventions and the avoidance
of sleep interruptions such as the assessment of vital signs.
The administration of the Vital Sleep headband with music
enhanced clients’ sleep.
Implications
Nurses must recognize the impact of sleep on the client’s
recovery. The study revealed that nursing strategies to
promote sleep included the use of adequate sleep hygiene.
Items and interventions to promote sleep hygiene include
warm blankets, bedtime snacks, and maintaining a sleep
routine. Nurses also need to develop and participate
in research studies that investigate interventions to
promote sleep.
27/01/2021 18:05
1174
Unit 10
●
Promoting Physiologic Health
The long-term efficacy of hypnotic medications is
questionable. Such medications do not deal with the cause
of the problem, and their prolonged use can create drug
dependencies. Although antihistamines such as diphenhydramine (Benadryl) are thought to be safer for older
clients than hypnotics, their side effects (i.e., atropine-like
effects, dizziness, sedation, and hypotension) make them
extremely hazardous. In fact, antihistamines should not
be recommended for any client with a history of asthma,
increased intraocular pressure, hyperthyroidism, cardiovascular disease, or hypertension.
Excessive Daytime Sleepiness
Clients may experience excessive daytime sleepiness as a
result of hypersomnia, narcolepsy, sleep apnea, and insufficient sleep.
Hypersomnia
Hypersomnia refers to conditions where the affected indi-
vidual obtains sufficient sleep at night but still cannot
stay awake during the day. Hypersomnia can be caused
by medical conditions, for example, CNS damage and certain kidney, liver, or metabolic disorders, such as diabetic
acidosis and hypothyroidism. Rarely does hypersomnia
have a psychologic origin.
Narcolepsy
Narcolepsy is a disorder of excessive daytime sleepi-
ness caused by the lack of the chemical hypocretin in
the area of the CNS that regulates sleep. Clients with
narcolepsy have sleep attacks or excessive daytime
sleepiness, and their sleep at night usually begins with a
sleep-onset REM period (dreaming sleep occurs within
the first 15 minutes of falling asleep). The majority of
clients also have cataplexy or the sudden onset of muscle
weakness or paralysis in association with strong emotion, sleep paralysis (transient paralysis when falling
asleep or waking up), hypnagogic hallucinations (visual,
auditory, or tactile hallucinations at sleep onset or when
waking up), and/or fragmented nighttime sleep. Their
fragmented nocturnal sleep is not the cause of their
excessive daytime sleepiness; many clients, particularly
younger clients, have sound restorative nocturnal sleep
but still cannot stay awake during the daytime. Onset
of symptoms tends to occur between ages 15 and 30,
and symptom severity usually stabilizes within the first
5 years of onset.
CNS stimulants such as methylphenidate (Ritalin) or
amphetamines have been used to reduce excessive daytime sleepiness. Xanthines, such as caffeine, stimulate the
cerebral cortex to increase alertness. Antidepressants, both
older monoamine oxidase inhibitors (MAOIs) and the
newer serotonergic antidepressants, are usually quite effective for controlling cataplexy. Modafinil (Provigil) has psychoactive effects to alter mood, perception, and thinking to
control excessive daytime sleepiness in narcoleptic clients.
Although its exact mechanism of action is unknown, it has
M45_BERM9793_11_GE_C45.indd 1174
fewer side effects and a lower potential for abuse than other
drugs. Modafinil is also used for sleep apnea-hypopnea
syndrome (Frandsen & Pennington, 2018). Sodium oxybate (Xyrem) is approved for the treatment of cataplexy. It
has been shown to reduce excessive daytime sleepiness in
clients with narcolepsy, although the exact mechanism of
action is unknown. Because Xyrem is difficult to administer (it is only available as a liquid and taken at bedtime
and then again 2.5 to 4 hours after sleep onset) and its use
is tightly controlled by the U.S. Food and Drug Administration (FDA), only those clients whose symptoms are not
controlled by other medications are usually offered Xyrem.
Only one pharmacy in the United States is allowed to dispense Xyrem. As a result, clients need to allow adequate
time for obtaining their medications from the central pharmacy. The herbal supplement guarana can also be administered to increase mental alertness during the daytime.
Clinical Alert!
Sodium oxybate is also known as gamma hydroxybutyrate or GHB—
one of the drugs frequently associated with “date rapes.”
Sleep Apnea
Sleep apnea is characterized by frequent short breathing pauses during sleep. Although all individuals have
occasional periods of apnea during sleep, more than
five apneic episodes or five breathing pauses longer
than 10 seconds per hour is considered abnormal and
should be evaluated by a sleep medicine specialist.
Symptoms suggestive of sleep apnea include loud snoring, frequent nocturnal awakenings, excessive daytime
sleepiness, difficulties falling asleep at night, morning
headaches, memory and cognitive problems, and irritability. Although sleep apnea is most frequently diagnosed in men and postmenopausal women, it may occur
during childhood.
The periods of apnea, which last from 10 seconds to
2 minutes, occur during REM or NREM sleep. Frequency
of episodes ranges from 50 to 600 per night. Because these
apneic pauses are usually associated with an arousal, clients frequently report that their sleep is nonrestorative
and that they regularly fall asleep when engaging in sedentary activities during the day.
Three common types of sleep apnea are obstructive
apnea, central apnea, and mixed apnea. Obstructive apnea
occurs when the structures of the pharynx or oral cavity
block the flow of air. The individual continues to try to
breathe; that is, the chest and abdominal muscles move.
The movements of the diaphragm become stronger and
stronger until the obstruction is removed. Enlarged tonsils and adenoids, a deviated nasal septum, nasal polyps,
and obesity predispose the client to obstructive apnea. An
episode of obstructive sleep apnea usually begins with
snoring; thereafter, breathing ceases, followed by marked
snorting as breathing resumes. Toward the end of each
apneic episode, increased carbon dioxide levels in the
blood cause the client to wake.
27/01/2021 18:05
Chapter 45
Central apnea is thought to involve a defect in the
respiratory center of the brain. All actions involved in
breathing, such as chest movement and airflow, cease.
Clients who have brainstem injuries and muscular dystrophy, for example, often have central sleep apnea. At
this time, there is no available treatment. Mixed apnea is a
combination of central apnea and obstructive apnea.
Treatment for sleep apnea is directed at the cause of
the apnea. For example, enlarged tonsils may be removed.
Other surgical procedures, including laser removal of
excess tissue in the pharynx, reduce or eliminate snoring
and may be effective in relieving the apnea. In other cases,
the use of a nasal continuous positive airway pressure
(CPAP) device at night is effective in maintaining an open
airway. Weight loss may also help decrease the severity
of symptoms.
Sleep apnea profoundly affects an individual’s work
or school performance. In addition, prolonged sleep apnea
can cause a sharp rise in blood pressure and may lead
to cardiac arrest. Over time, apneic episodes can cause
cardiac arrhythmias, pulmonary hypertension, and subsequent left-sided heart failure.
Clinical Alert!
Partners of clients with sleep apnea may become aware of the problem because they hear snoring that stops during the apneic period
and then restarts. Surgical removal of tonsils or other tissue in the
pharynx, if not the cause of the sleep apnea, can actually worsen
the situation by removing the snoring and, thus, the warning that
apnea is occurring.
●
Sleep
1175
legally drunk (with a blood alcohol level of 0.1). Nurses
who report reduced hours of sleep are more likely to make
an error, to have difficulty staying awake on duty, and to
have difficulty staying awake while driving home from
work than those who obtained more sleep.
When clients report obtaining more sleep on weekends or days off, it usually indicates that they are not
obtaining sufficient sleep. Convincing clients to obtain
more sleep may be difficult, but it can result in the resolution of their daytime symptoms.
Parasomnias
A parasomnia is behavior that may interfere with sleep
and may even occur during sleep. It is characterized by
physical events such as movements or experiences that
are displayed as emotions, perceptions, or dreams. The
International Classification of Sleep Disorders subdivides
parasomnias into three classes: non–rapid eye movement, rapid eye movement, and miscellaneous with no
specific stage of sleep (Judd & Sateia, 2019). Parasomnias
with non–rapid eye movement are associated with confusion upon arousal, sleep tremors, and sleep walking.
Parasomnias with rapid eye movement are associated
with arousal disorders such as sleep paralysis. This may
be a nightmare disorder with exaggerated features of REM
sleep. Miscellaneous parasomnias are not associated with
any stage of sleep and may produce nocturnal enuresis or
hallucinations. The miscellaneous parasomnias are often
related to a medication, substance abuse, or a medical
disorder. Box 45.6 describes examples of parasomnias.
Insufficient Sleep
Healthy individuals who obtain less sleep than they need
will experience sleepiness and fatigue during the daytime hours. Depending on the severity and chronicity
of this voluntary, albeit unintentional sleep deprivation,
individuals may develop attention and concentration
deficits, reduced vigilance, distractibility, reduced motivation, fatigue, malaise, and occasionally diplopia and dry
mouth. The cause of these symptoms may or may not be
attributed to insufficient sleep, because many Americans
believe that 6.8 hours of sleep is sufficient to maintain
optimal daytime performance. In fact, the sleep times of
Americans have decreased dramatically during the past
decade, with adults averaging only 6.8 hours of sleep on
weekdays and 7.4 hours on weekends. All age groups,
not just adults and adolescents, are getting less than the
recommended amounts of sleep. Even 4- to 5-year-old
children now average less than 9.5 hours of sleep, approximately 1.5 to 2.5 hours less than recommended.
Although the effects of obtaining less than optimal
amounts of sleep are generally considered benign, there
is growing evidence that insufficient sleep can have significant deleterious effects. Staying awake 19 consecutive
hours produces the same impairments in reaction times
and cognitive function as a blood alcohol level of 0.05,
and staying awake for 24 consecutive hours has the same
effects on reaction times and cognitive function as being
M45_BERM9793_11_GE_C45.indd 1175
BOX 45.6
•
•
•
•
•
Parasomnias
Bruxism. Usually occurring during stage 2 NREM sleep, this
clenching and grinding of the teeth can eventually erode
dental crowns, cause teeth to come loose, and lead to deterioration of the temporomandibular (TMJ) joint, which is called
TMJ syndrome.
Enuresis. Bed-wetting during sleep can occur in children over
3 years old. More males than females are affected. It often
occurs 1 to 2 hours after falling asleep, when rousing from
NREM stage 3.
Periodic limb movement disorder (PLMD). In this condition,
the legs jerk twice or three times per minute during sleep.
It is most common among older adults. This kicking motion
can wake the client and result in poor sleep. PLMD differs
from restless leg syndrome (RLS), which occurs whenever the
individual is at rest, not just at night when sleeping. RLS may
occur during pregnancy or be due to other medical problems
that can be treated. Many clients with PLMD or RLS respond
well to medications such as levodopa, pramipexole, ropinirole,
and gabapentin (Frandsen & Pennington, 2018).
Sleeptalking. Talking during sleep occurs during NREM sleep
before REM sleep. It rarely presents a problem to the individual unless it becomes troublesome to others.
Sleepwalking. Sleepwalking (somnambulism) occurs during
stage 3 of NREM sleep. It is episodic and usually occurs
1 to 2 hours after falling asleep. Sleepwalkers tend not to
notice dangers (e.g., stairs) and often need to be protected
from injury.
27/01/2021 18:05
1176
Unit 10
●
Promoting Physiologic Health
NURSING MANAGEMENT
Assessing
A complete assessment of a client’s sleep difficulty
includes a sleep history, health history, physical exam,
and, if warranted, a sleep diary and diagnostic studies. All
nurses, however, can take a brief sleep history and educate
their clients about normal sleep.
Sleep History
A brief sleep history, which is usually part of the comprehensive nursing history, should be obtained for all clients entering a healthcare facility. It should, however, be
deferred or omitted if the client is critically ill. Key questions to ask include the following:
•
•
•
When do you usually go to sleep? And when do you
wake up? Do you nap? If so, when? If the client is a
child, it is also important to ask about bedtime rituals.
This information provides the nurse with information
about the client’s usual sleep duration and preferred
sleep times, and allows for the incorporation of the client’s preferences in the plan of care.
Do you have any problems with your sleep? Has anyone
ever told you that you snore loudly or thrash around a
lot at night? Are you able to stay awake at work, when
driving, or engaging in your usual activities?
These questions elicit information about sleep complaints including the possibility of excessive daytime
sleepiness. Loud snoring suggests the possibility of
obstructive sleep apnea, and any client replying yes to
this question should be referred to a specialist in sleep
disorders medicine. Referrals should also be made if
clients indicate they have difficulty staying awake during the day or that their movements disturb the sleep
of their bed partners.
Do you take any prescribed medications, over-thecounter (OTC) medications, or herbal remedies to help
you sleep? Or to stay awake?
•
This information alerts the nurse to the use of prescription hypnotics and stimulants as well as the use of
OTC sleep aids and herbal remedies.
Is there anything else I need to know about your sleep?
This allows the client to voice any concerns or bring up
topics that the nurse may not have asked about.
If the client is being admitted to a long-term care facility, it is also appropriate to ask about preferred room temperature, lighting (complete darkness versus using a night
light), and preferred bedtime routine.
A more detailed assessment is required if the client
indicates any difficulty sleeping, difficulty remaining
awake during the day, or recent changes in sleep pattern.
This detailed history should explore the exact nature of
the problem and its cause, when it first began and its
frequency, how it affects daily living, what the client is
doing to cope with the problem, and whether these methods have been effective. Questions the nurse might ask
the client with a sleeping disturbance are shown in the
accompanying Assessment Interview.
Health History
A health history is obtained to rule out medical or psychiatric causes of the client’s difficulty sleeping. It is important to note that the presence of a medical or psychiatric
illness (e.g., depression, Parkinson’s disease, Alzheimer’s
disease, or arthritis) does not preclude the possibility that
a second problem (e.g., obstructive sleep apnea) may be
contributing to the difficulty sleeping. Because medications can frequently cause or exacerbate sleep disturbances, information should be obtained about all of the
prescribed and nonprescription medications, including
herbal remedies, that a client consumes.
Physical Examination
Rarely are sleep abnormalities noted during the physical
examination unless the client has obstructive sleep apnea
or some other health problem. Common findings among
ASSESSMENT INTERVIEW Sleep Disturbances
•
•
•
•
•
•
•
•
How would you describe your sleeping problem? What
changes have occurred in your sleeping pattern? How often
does this happen?
How many cups of coffee, tea, or caffeinated beverages do you
drink per day? Do you drink alcohol? If so, how much?
Do you have difficulty falling asleep?
Do you wake up often during the night? If so, how often?
Do you wake up earlier in the morning than you would like and
have difficulty falling back to sleep?
How do you feel when you wake up in the morning?
Are you sleeping more than usual? If so, how often do you
sleep?
Do you have periods of overwhelming sleepiness? If so, when
does this happen?
M45_BERM9793_11_GE_C45.indd 1176
•
•
•
•
•
Have you ever suddenly fallen asleep in the middle of a daytime
activity? Does anything unusual happen when you laugh or get
angry?
Has anyone ever told you that you snore, walk in your sleep, or
stop breathing for a while when sleeping?
What have you been doing to deal with this sleeping problem?
Does it help?
What do you think might be causing this problem? Do you have
any medical condition that might be causing you to sleep more
(or less)? Are you receiving medications for an illness that might
alter your sleeping pattern? Are you experiencing any stressful or upsetting events or conflicts that may be affecting your
sleep?
How is your sleeping problem affecting you?
27/01/2021 18:05
Chapter 45
clients with sleep apnea include an enlarged and reddened
uvula and soft palate, enlarged tonsils and adenoids (in
children), obesity (in adults), and in male clients a neck
size greater than 17.5 inches. Occasionally a deviated septum may be noted, but it is rarely the cause of obstructive
sleep apnea.
Sleep Diary
A sleep specialist may ask clients to keep a sleep diary or
log for 1 to 2 weeks in order to get a more complete picture
of their sleep complaints. A sleep diary may include all or
selected aspects of the following information that pertain
to the client’s specific problem:
•
•
•
•
•
•
•
•
Time of (a) going to bed, (b) trying to fall asleep, (c) falling asleep (approximate time), (d) any instances of waking up and duration of these periods, (e) waking up in
the morning, and (f) any naps and their duration
Activities performed 2 to 3 hours before bedtime (type,
duration, and time)
Consumption of caffeinated beverages and alcohol and
amounts of those beverages
Any prescribed medications, OTC medications, and
herbal remedies taken during the day
Bedtime rituals before sleep
Any difficulties remaining awake during the day and
times when difficulties occurred
Any worries that the client believes may affect sleep
Factors that the client believes have a positive or negative effect on sleep.
If the client is a child, the sleep diary or log may be completed by a parent.
Diagnostic Studies
Sleep is measured objectively in a sleep disorder laboratory
by polysomnography in which an electroencephalogram
(EEG), electromyogram (EMG), and electro-oculogram (EOG)
are recorded simultaneously. Electrodes are placed on the
scalp to record brain waves (EEG), on the outer canthus of
each eye to record eye movement (EOG), and on the chin
muscles to record the structural electromyogram (EMG).
The electrodes transmit electric energy from the cerebral
cortex and muscles of the face to pens that record the brain
waves and muscle activity on graph paper. Respiratory
effort and airflow, ECG, leg movements, and oxygen saturation are also monitored. Oxygen saturation is determined
by monitoring with a pulse oximeter, a light-sensitive electric cell that attaches to the ear or a finger. Oxygen saturation and ECG assessments are of particular importance if
sleep apnea is suspected. Through polysomnography, the
client’s activity (movements, struggling, noisy respirations)
during sleep can be assessed. Such activity of which the
client is unaware may be the cause of arousal during sleep.
Diagnosing
Impaired sleep, the diagnosis given to clients with sleep
problems, is usually made more explicit with descriptions
such as “difficulty falling asleep” or “difficulty staying
M45_BERM9793_11_GE_C45.indd 1177
●
Sleep
1177
asleep”; for example, impaired sleep (delayed onset of
sleep) related to overstimulation prior to bedtime.
Various factors or etiologies may be involved and
must be specified for the individual. These include physical discomfort or pain; anxiety about actual or anticipated
loss of a loved one, loss of a job, loss of life due to serious
disease process, or worry about a family member’s behavior or illness; frequent changes in sleep time due to shift
work or overtime; and changes in sleep environment or
bedtime rituals (e.g., noisy environment, alcohol or other
drug dependency, drug withdrawal, misuse of sedatives
prescribed for insomnia, and effects of medications such
as steroids or stimulants).
QSEN
Patient-Centered Care: Sleep
When caring for a client in the home it is important to
assess the client and the caregiver about their knowledge
of sleep and wellness. Once the assessment is completed
the nurse will develop appropriate teaching to augment
the client and caregiver’s knowledge. The client’s sleep
area should be assessed for environmental factors that
can contribute to a lack of sleep. These factors include the
mattress firmness, noise levels, a room that is too warm or
too cold, or the use of electronics. When in the home care
setting, remember to assess for the possibility of sleep disruption and deprivation in the caregiver. A sleep-deprived
family member may be caring for a well-rested client.
Respite care, where someone relieves the caregiver and
cares for the client for a period of time, may be needed.
Sleep pattern disturbances may also be stated as the
etiology of another diagnosis, in which case the nursing
interventions are directed toward the sleep disturbance
itself. Examples include:
Altered ability to cope related to insufficient quality
and quantity of sleep, fatigue related to no restorative
sleep pattern, alteration in tissue perfusion related to sleep
apnea, insufficient knowledge (nonprescription remedies
for sleep) related to lack of information, anxiety related
to sleep apnea or the diagnosis of a sleep disorder, and
impaired activity related to sleep deprivation or excessive
daytime sleepiness.
Planning
The major goal for clients with sleep disturbances is to
maintain (or develop) a sleeping pattern that provides sufficient energy for daily activities. Other goals may relate to
enhancing the client’s feeling of well-being or improving
the quality and quantity of the client’s sleep. The nurse
plans specific nursing interventions to reach the goal
based on the etiology of each nursing diagnosis. These
interventions may include reducing environmental distractions, promoting bedtime rituals, providing comfort
measures, scheduling nursing care to provide for uninterrupted sleep periods, and teaching stress reduction, relaxation techniques, and good sleep hygiene. Specific nursing
activities associated with each of these interventions can
27/01/2021 18:05
1178
Unit 10
●
Promoting Physiologic Health
be selected to meet the individual needs of the client. See
the Nursing Care Plan and the Concept Map at the end of
the chapter.
Implementing
The term sleep hygiene refers to interventions used to promote sleep. Nursing interventions to enhance the quantity
and quality of clients’ sleep involve largely nonpharmacologic measures. These involve health teaching about sleep
habits, support of bedtime rituals, the provision of a restful
environment, specific measures to promote comfort and
relaxation, and appropriate use of hypnotic medications.
For hospitalized clients, sleep problems are often
related to the hospital environment or their illness. Assisting the client to sleep in such instances can be challenging
to a nurse, often involving scheduling activities, administering analgesics, and providing a supportive environment. Explanations and a supportive relationship are
essential for the fearful or anxious client. Different types
of hypnotics may be prescribed depending on the type of
sleep problem (e.g., difficulties falling asleep or difficulties
maintaining sleep). Drugs with longer half-lives are often
prescribed for difficulties maintaining sleep, but must be
used with caution in older adults.
medications, (c) effects of other prescribed medications
on sleep, (d) effects of their disease states on sleep, and
(e) importance of long periods of uninterrupted sleep. Tips
for promoting sleep are listed in Client Teaching.
Supporting Bedtime Rituals
Most individuals are accustomed to bedtime rituals or
presleep routines that are conducive to comfort and relaxation. Altering or eliminating such routines can affect a
client’s sleep. Common prebedtime activities of adults
include listening to music, reading, taking a soothing
bath, and praying. Children need to be socialized into a
presleep routine such as a bedtime story, holding onto a
favorite toy or blanket, and kissing everyone goodnight.
Sleep is also usually preceded by hygienic routines, such
as washing the face and hands (or bathing), brushing the
teeth, and voiding.
In institutional settings, nurses can provide similar
bedtime rituals—assisting with a hand and face wash,
providing a massage or hot drink, plumping pillows, and
providing extra blankets as needed. Conversing about
accomplishments of the day or enjoyable events such as
visits from friends can also help to relax clients and bring
peace of mind.
Client Teaching
Creating a Restful Environment
Healthy individuals need to learn the importance of
sleep in maintaining active and productive lifestyles.
They need to learn (a) the conditions that promote sleep
and those that interfere with sleep, (b) safe use of sleep
Everyone needs a sleeping environment with minimal
noise, a comfortable room temperature, appropriate ventilation, and appropriate lighting. Although most individuals prefer a darkened environment, a lowlight source may
CLIENT TEACHING Promoting Sleep
SLEEP PATTERN
• If you have difficulty falling asleep or staying asleep, it is important to establish a regular bedtime and wake-up time for all
days of the week to enhance your biological rhythm. A short
daytime nap (e.g., 15 to 30 minutes), particularly among older
adults, can be restorative and not interfere with nighttime sleep.
A younger client with insomnia should not nap.
• Establish a regular, relaxing bedtime routine before sleep such
as reading, listening to soft music, taking a warm bath, or doing
some other quiet activity you enjoy.
• Avoid dealing with office work or family problems before
bedtime.
• Get adequate exercise during the day to reduce stress, but
avoid excessive physical exertion at least 3 hours before
bedtime.
• Use the bed for sleep or sexual activity, so that you associate it
with sleep. Take work material, computers, and TVs out of the
bedroom. Lying awake, tossing and turning, will strengthen the
association between wakefulness and lying in bed (many clients
with insomnia report falling asleep in a chair or in front of the TV
but having trouble falling asleep in bed).
• When you are unable to sleep, get out of bed, go into another
room, and pursue some relaxing activity until you feel drowsy.
Keep noise to a minimum; block out extraneous noise as
necessary with white noise from a fan, air conditioner, or white
noise machine. Music is not recommended because studies
have shown that music will promote wakefulness (it is interesting and individuals will pay attention to it).
• Sleep on a comfortable mattress and pillows.
•
DIET
• Avoid heavy meals 2 to 3 hours before bedtime.
• Avoid alcohol and caffeine-containing foods and beverages
(e.g., coffee, tea, chocolate) at least 4 hours before bedtime.
Caffeine can interfere with sleep. Both caffeine and alcohol act
as diuretics, creating the need to void during sleep time.
• If a bedtime snack is necessary, consume only light carbohydrates or a milk drink. Heavy or spicy foods can cause gastrointestinal upsets that disturb sleep.
MEDICATIONS
• Use sleeping medications only as a last resort. Use OTC medications sparingly because many contain antihistamines that
cause daytime drowsiness.
• Take analgesics before bedtime to relieve aches and pains.
• Consult with your healthcare provider about adjusting other
medications that may cause insomnia.
ENVIRONMENT
• Create a sleep-conducive environment that is dark, quiet, comfortable, and cool.
M45_BERM9793_11_GE_C45.indd 1178
27/01/2021 18:05
Chapter 45
provide comfort for children or those in a strange environment. Infants and children need a quiet room usually
separate from the parents’ room, a light or warm blanket
as appropriate, and a location away from open windows
or drafts.
Environmental distractions such as environmental
noises and staff communication noise are particularly
troublesome for hospitalized clients. Environmental noises
include the sound of paging systems, telephones, and call
lights; monitors beeping; doors closing; elevator chimes;
furniture squeaking; and linen carts being wheeled
through corridors. Staff communication is a major factor
creating noise, particularly at staff change of shift.
To create a restful environment, the nurse needs to
reduce environmental distractions, reduce sleep interruptions, ensure a safe environment, and provide a room
temperature that is satisfactory to the client. Some interventions to reduce environmental distractions, especially
noise, are listed in Box 45.7.
BOX 45.7
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Reducing Environmental Distractions
in Hospitals
Close window curtains if street lights shine through.
Close curtains between clients in semiprivate and larger
rooms.
Reduce or eliminate overhead lighting; provide a night light at
the bedside or in the bathroom.
Use a flashlight to check drainage bags, the client’s identification, dressings, and IV infusions, without turning on the
overhead lights.
Ensure a clear pathway around the bed to avoid bumping the
bed and jarring the client during sleeping hours.
Close the door of the client’s room.
Adhere to agency policy about times to turn off communal
televisions or radios.
Lower the ringtone of nearby telephones.
Discontinue use of the paging system after a certain hour
(e.g., 2100 hours) or reduce its volume.
Keep required staff conversations at low levels; conduct nursing reports or other discussions in a separate area away from
client rooms.
Wear rubber-soled shoes.
Ensure that all cart wheels are well oiled.
Perform only essential noisy activities during sleeping hours.
Make sure the bed linen is smooth, clean, and dry.
Assist or encourage the client to void before bedtime.
Offer to provide a back massage before sleep.
Position dependent clients appropriately to aid muscle
relaxation, and provide supportive devices to protect
pressure areas.
Schedule medications, especially diuretics, to prevent
nocturnal awakenings.
For clients who have pain, administer analgesics 30 minutes
before sleep.
Listen to the client’s concerns and deal with problems as
they arise.
M45_BERM9793_11_GE_C45.indd 1179
●
Sleep
1179
The environment must also be safe so that the client
can relax. Clients who are unaccustomed to narrow hospital beds may feel more secure with side rails.
Additional safety measures include:
•
•
•
Placing beds in low positions.
Using night lights.
Placing call bells within easy reach.
Promoting Comfort and Relaxation
Comfort measures are essential to help the client fall asleep
and stay asleep, especially if the effects of the client’s illness interfere with sleep. A concerned, caring attitude,
along with the following interventions, can significantly
promote client comfort and sleep:
•
•
Provide loose-fitting nightwear.
Assist clients with hygienic routines.
Individuals of any age, but especially older adults, are
unable to sleep well if they feel cold. Changes in circulation, metabolism, and body tissue density reduce the older
adult’s ability to generate and conserve heat. To compound this problem, hospital gowns have short sleeves
and are made of thin polyester. Bed sheets also are often
made of polyester rather than a warm fabric, such as cotton flannel. The following interventions can be used to
keep older adults warm during sleep:
•
•
•
Before the client goes to bed, warm the bed with prewarmed bath blankets.
Use 100% cotton flannel sheets or apply thermal blankets between the sheet and bedspread.
Encourage the client to wear own clothing, such as
flannel nightgown or pajamas, socks, leg warmers,
long underwear, sleeping cap (if scalp hair is sparse),
or sweater, or use extra blankets.
Emotional stress obviously interferes with an
individual’s ability to relax, rest, and sleep, and inability to sleep further aggravates feelings of tension. Sleep
rarely occurs until an individual is relaxed. Relaxation
techniques can be encouraged as part of the nightly routine. Slow, deep breathing for a few minutes followed by
slow, rhythmic contraction and relaxation of muscles can
alleviate tension and induce calm. Imagery, meditation,
and yoga can also be taught. These techniques are discussed in Chapter 19 .
Enhancing Sleep with Medications
Sleep medications often prescribed on a prn (as-needed)
basis for clients include the sedative–hypnotics, which
induce sleep, and antianxiety drugs or tranquilizers, which
decrease anxiety and tension. When prn sleep medications
are ordered in institutional settings, the nurse is responsible for making decisions with the client about when to
administer them. These medications should be administered only with complete knowledge of their actions and
effects and only when indicated.
27/01/2021 18:05
1180
Unit 10
●
Promoting Physiologic Health
Both nurses and clients need to be aware of the
actions, effects, and risks of the specific medication prescribed. Although medications vary in their activity and
effects, considerations include the following:
•
•
•
•
•
•
•
Sedative-hypnotic medications produce a general CNS
depression and an unnatural sleep; REM or NREM
sleep is altered to some extent, and daytime drowsiness and a morning hangover effect may occur. Some of
the new hypnotics, such as zolpidem (Ambien), do not
alter REM sleep or produce rebound insomnia when
discontinued.
Antianxiety medications decrease levels of arousal by
facilitating the action of neurons in the CNS that suppress responsiveness to stimulation. These medications
are contraindicated in pregnant women because of their
associated risk of congenital anomalies, and in breastfeeding mothers because the medication is excreted in
breast milk.
Sleep medications vary in their onset and duration of
action and will impair waking function as long as they
are chemically active. Some medication effects can last
many hours beyond the time that the client’s perception of daytime drowsiness and impaired psychomotor
skills have disappeared. Clients need to be cautioned
about such effects and about driving or handling
machinery while the drug is in their system.
Sleep medications affect REM sleep more than NREM
sleep. Clients need to be informed that one or two
nights of increased dreaming (REM rebound) are usual
after the drug is discontinued after long-term use.
Initial doses of medications should be low and increases
added gradually, depending on the client’s response.
Older adults, in particular, are susceptible to side effects
because of their metabolic changes; they need to be
closely monitored for changes in mental alertness and
coordination. Clients need to be instructed to take the
smallest effective dose and then only for a few nights
or intermittently as required.
Regular use of any sleep medication can lead to tolerance over time (e.g., 4 to 6 weeks) and rebound insomnia. In some instances, this may lead clients to increase
the dosage. Clients must be cautioned about developing a pattern of drug dependency.
Abrupt cessation of barbiturate sedative-hypnotics
can create withdrawal symptoms such as restlessness,
tremors, weakness, insomnia, increased heart rate, seizures, convulsions, and even death. Long-term users
need to taper their medications under the supervision
of a specialist.
About half of the clients who seek medical intervention for sleep problems are treated with sedative–
hypnotics. Sometimes the prescription of hypnotics can be
appropriate. For example, women with chronic difficulties
M45_BERM9793_11_GE_C45.indd 1180
maintaining sleep or nonrestorative sleep associated with
menopausal symptoms often benefit by the prescription of
10 mg of zolpidem, a low dose that was documented to be
both safe and efficacious in this population. Hypnotics are
not appropriate if clients have any symptoms suggestive
of sleep-related breathing disorders or decreased renal or
hepatic function.
Table 45.1 presents some of the common medications
used for enhancing sleep and the half-life of these medications. The half-life represents how long it takes for half of
the medication to be metabolized and eliminated by the
body; hence, those with shorter half-lives are less likely to
cause residual drowsiness after administration, but may
be less effective for the treatment of sleep maintenance
insomnia.
Evaluating
Using data collected during care and the desired outcomes
developed during the planning stage as a guide, the nurse
judges whether client goals and outcomes have been
achieved. Data collection may include (a) observations of
the duration of the client’s sleep, (b) questions about how
the client feels on awakening, or (c) observations of the
client’s level of alertness during the day.
If the desired outcomes are not achieved, the nurse
and client should explore the reasons, which may include
answers to the following questions:
•
•
•
•
•
•
•
Were etiologic factors correctly identified?
Has the client’s physical condition or medication therapy changed?
Did the client comply with instructions about establishing a regular sleep–wake pattern?
Did the client avoid ingesting caffeine?
Did the client participate in stimulating daytime activities to avoid excessive daytime naps?
Were all possible measures taken to provide a restful
environment for the client?
Were the comfort and relaxation measures effective?
TABLE 45.1
Selected Sedative–Hypnotic
Medications Used for Insomnia
Medication
Half-Life (Hours)
Chloral hydrate (Noctec)
8–11
Eszopiclone (Lunesta)
5–6
Flurazepam (Dalmane)
47–100
Lorazepam (Ativan)
10–20
Melatonin
1
Temazepam (Restoril)
8–24
Triazolam (Halcion)
2–3
Zaleplon (Sonata)
1
Zolpidem (Ambien)
2.5
27/01/2021 18:05
Chapter 45
●
Sleep
1181
DRUG CAPSULE
Non-Benzodiazepine Sedative-Hypnotics: zolpidem (Ambien)
THE CLIENT WITH MEDICATIONS THAT AFFECT SLEEP OR
ALERTNESS
Zolpidem is used for the short-term (7- to 10-day) management of
insomnia. The medication is used to reduce sleep latency and awakenings, and to lengthen sleep durations. Unlike traditional benzodiazepine sedative-hypnotics, zolpidem does not reduce REM sleep
durations or cause rebound insomnia when it is discontinued. At
therapeutic doses, it causes little or no respiratory depression, and
it has a low potential for abuse. Clients using it for short periods have
not demonstrated tolerance, physical dependence, or withdrawal
symptoms. It has a rapid onset of action and a half-life of 2.5 hours.
NURSING RESPONSIBILITIES
• The drug has a rapid onset of action, so it should not be given
until just prior to bedtime in order to minimize sedation while
awake.
Clients should be monitored for side effects (e.g., daytime
drowsiness and dizziness). Older clients and those with hepatic
insufficiency should start with a lower dose (e.g., 5 mg).
• According to the American Geriatrics Society Beers Criteria
(2019), the administration of zolpidem to older adults can place
the client at risk for falls; avoid the administration of zolpidem
unless safer alternatives are not available.
•
CLIENT AND FAMILY TEACHING
• Clients should be cautioned that zolpidem can intensify the
actions of other CNS depressants and warned against combining zolpidem with alcohol and all other drugs that depress CNS
function.
• Clients should be cautioned not to take this medication until
they are ready to go to bed because of its rapid onset of action.
Some clients may engage in activities such as driving and eating with no memory of having participated in those activities.
Central Nervous System Stimulant modafinil (Provigil)
Modafinil has been approved by the FDA for the treatment of narcolepsy, excessive daytime sleepiness associated with obstructive
sleep apnea, and shift-work sleep disorder. Because the drug does
not alter the function of the dopamine neurotransmitter system,
modafinil lacks the addictive potential of traditional stimulants. The
drug alters mood, perception, and thinking. The onset of action is
rapid and reaches peak plasma levels in 2 to 4 hours. It has a long
half-life (approximately 15 hours) and thus can usually be administered only once a day (in the morning). It does not interfere with
sleep at night.
NURSING RESPONSIBILITIES
• Monitor the client for side effects, particularly if the client is
older or has hepatic dysfunction. Side effects are rare and
usually consist of headache, nausea, and nervousness.
• If the client has obstructive sleep apnea, ensure that the
client continues to use nasal CPAP.
CLIENT AND FAMILY TEACHING
• Explain that modafinil is not a substitute for obtaining adequate
amounts of sleep. Any client with the diagnosis of narcolepsy,
obstructive sleep apnea, or shift-work sleep disorder needs
to obtain adequate amounts of sleep in addition to taking
prescribed medications.
• Caution clients with obstructive sleep apnea that it is very
important to continue using nasal CPAP and that modafinil is
being prescribed only to reduce excessive daytime sleepiness
and will not reduce the number of apneic episodes during
sleep.
• Modafinil may accelerate the metabolism of oral contraceptives,
leading to lower plasma levels. Women using low-dose birth
control pills may want to consider switching birth control
methods or adding a second type of birth control.
Note: Prior to administering any medication, review all aspects with a current drug handbook
or other reliable source.
NURSING CARE PLAN Sleep
ASSESSMENT DATA
NURSING DIAGNOSIS
DESIRED OUTCOMES*
NURSING ASSESSMENT
Jack Harrison is a 36-year-old police officer assigned to
a high-crime police precinct. One week ago he received
a surface bullet wound to his arm. Today he arrives at
the outpatient clinic to have the wound redressed. While
speaking with the nurse, Mr. Harrison mentions that he
has recently been promoted to the rank of detective
and has assumed new responsibilities. He states that
since his promotion, he has experienced increasing difficulty falling asleep and sometimes staying asleep. He
expresses concern over the danger of his occupation
and his desire to do well in his new position. He complains of waking up feeling tired and irritable.
Impaired sleep related to anxiety (as evidenced by difficulty
falling and remaining asleep,
fatigue, and irritability)
Sleep [0004] as evidenced by:
• No compromise in sleeping through the
night consistently
• No compromise in feeling rejuvenated
after sleep
• No dependence on sleep aids
Continued on page 1182
M45_BERM9793_11_GE_C45.indd 1181
27/01/2021 18:05
1182
Unit 10
●
Promoting Physiologic Health
NURSING CARE PLAN Sleep—continued
ASSESSMENT DATA
NURSING DIAGNOSIS
Physical Examination
Diagnostic Data
Height: 185.4 cm (6´2˝ )
Weight: 85.7 kg (189 lb)
Temperature: 37.0°C (98.6°F)
Pulse: 80 beats/min
Respirations: 18/min
Blood pressure: 144/88 mmHg
CBC within normal
range, x-ray left
arm: evidence of
superficial soft tissue injury
NURSING INTERVENTIONS*/SELECTED ACTIVITIES
SLEEP ENHANCEMENT [1850]
Determine the client’s sleep and activity pattern.
Encourage Mr. Harrison to establish a bedtime routine
to facilitate transition from wakefulness to sleep.
Encourage him to eliminate stressful situations before
bedtime.
Instruct Mr. Harrison and significant others about factors
(e.g., physiologic, psychologic, lifestyle, frequent work
shift changes, excessively long work hours, and other
environmental factors) that contribute to sleep pattern
disturbances.
Discuss with Mr. Harrison and his family comfort
measures, sleep-promoting techniques, and lifestyle
changes that can contribute to optimal sleep.
Monitor bedtime food and beverage intake for items that
facilitate or interfere with sleep.
Discuss specific situations or individuals that threaten
Mr. Harrison or his family.
Assist him to use coping responses that have been
successful in the past.
ANXIETY REDUCTION [5820]
Create an atmosphere to facilitate trust.
Seek to understand Mr. Harrison’s perspective of a
stressful situation.
Encourage verbalization of feelings, perceptions, and
fears.
Determine the client’s decision-making ability.
DESIRED OUTCOMES*
RATIONALE
The amount of sleep an individual needs varies with lifestyle, health, and age.
Rituals and routines induce comfort, relaxation, and sleep.
Stress interferes with an individual’s ability to relax, rest, and sleep.
Knowledge of causative factors can enable the client to begin to control factors
that inhibit sleep.
Knowledge of factors that affect sleep enables the client to implement changes
in lifestyle and prebedtime activities.
Milk and protein foods contain tryptophan, a precursor of serotonin, which is
thought to induce and maintain sleep. Stimulants should be avoided because
they inhibit sleep.
Fear is reduced when the reality of a situation is confronted in a safe environment. Awareness of factors that cause intensification of fears enhances control.
Feelings of safety and security increase when a client identifies previously
successful ways of dealing with anxiety-provoking or fearful situations.
Trust is an essential first step in the therapeutic relationship.
Anxiety is a feeling aroused by a vague, nonspecific threat. Identifying the client’s
perspective will facilitate planning for the best approach to anxiety reduction.
Open expression of feelings facilitates identification of specific emotions such as
anger or helplessness, distorted perceptions, and unrealistic fears.
Maladaptive coping mechanisms are characterized by an inability to make
decisions and choices.
EVALUATION
Outcome met. Mr. Harrison acknowledges his insomnia is a somatic expression of his anxiety regarding job promotion and fear of failing.
He states that talking with the police department counselor has been helpful. He is practicing relaxation techniques each night and sleeps
an average of 7 hours a night. Mr. Harrison expresses a feeling of being rested on awakening.
*The NOC # for desired outcomes and the NIC # for nursing interventions are listed in brackets following the appropriate outcome or intervention. Outcomes,
interventions, and activities selected are only a sample of those suggested by NOC and NIC and should be further individualized for each client.
APPLYING CRITICAL THINKING
1. What further information would be helpful to obtain from Mr. Harrison about his sleep problem?
2. What suggestions can you make that may help him develop better sleep habits?
3. What are the most common problems that interfere with clients’ ability to sleep?
Answers to Applying Critical Thinking questions are available on the faculty resources site. Please consult with your instructor.
M45_BERM9793_11_GE_C45.indd 1182
27/01/2021 18:05
Chapter 45
●
Sleep
1183
CONCEPT MAP
Sleep
JH
36 y.o. male
• Police officer high-crime precinct.
Bullet wound to arm 1 week ago
Recently promoted to detective
c/o increasing difficulty falling asleep
and sometimes staying asleep.
Concern over danger of his occupation
and desire to do well in new position.
c/o waking up feeling tired and irritable.
assess
•
•
•
•
•
•
•
Height: 185.4 cm (6' 2")
Weight: 85.7 kg (189 lb)
Temperature: 37.0°C (98.6°F)
Pulse rate: 80 BPM
Respirations: 18/minute
Blood pressure: 144/88 mmHg
Pale, drawn, with dark circles
under eyes
• CBC normal
• X-ray LA: evidence
of superficial soft
tissue injury
generate nursing diagnosis
Inability to sleep r/t anxiety (aeb difficulty falling and remaining asleep, fatigue, irritability)
outcome
Sleep aeb
• Sleep through the night consistently
• Feels rejuvenated after sleep
• No dependence on sleep aids
nursing intervention
Evaluation
nursing intervention
Anxiety Reduction
Outcomes met:
• Acknowledges his insomnia is a somatic
expression of his anxiety regarding job
promotion and fear of failing
• States that talking with the police
department counselor has been helpful
• Practicing relaxation techniques each night
and sleeps an average of 7 hours a night
• Expresses a feeling of being rested upon
awakening
Sleep Enhancement
activity
activity
activity
activity
activity
Create
an atmosphere
to facilitate trust
activity
Seek to understand
his perspective of
a stressful situation
Encourage verbalization
of feelings, perceptions,
and fears
M45_BERM9793_11_GE_C45.indd 1183
activity
activity
Determine his
decision-making
ability
Determine the
client's sleep
and activity
pattern
activity
activity
Encourage to
establish a bedtime
routine to facilitate
transition from
wakefulness to sleep
Encourage to
eliminate stressful
situations before
bedtime
Monitor bedtime
food and beverage
intake for items that
facilitate or interfere
with sleep
Discuss with the client
and his family comfort
measures, sleep-promoting
techniques, and lifestyle
changes that can contribute
to optimal sleep
Instruct the client
and significant others
about factors (e.g.,
physiologic, psychologic,
lifestyle, frequent work
shift changes, excessively
long work hours, and other
environmental factors)
that contribute to sleep
pattern disturbances
27/01/2021 18:05
1184
Unit 10
●
Promoting Physiologic Health
Chapter 45 Review
CHAPTER HIGHLIGHTS
• Sleep is needed for optimal psychologic and physiologic functioning.
• Insufficient sleep is widespread among all age groups in this coun-
•
•
•
•
try. Approximately 50 million to 70 million Americans suffer from
a chronic disorder of sleep and wakefulness that hinders daily
functioning and adversely affects health. Reports from government
agencies have stated that sleep disorders and sleep deprivation are
an unmet public health problem.
Sleep is a naturally occurring altered state of consciousness in
which an individual’s perception and reaction to the environment
are decreased.
The sleep cycle is controlled by specialized areas in the brainstem
and is affected by the individual’s circadian rhythm.
NREM sleep consists of three stages, progressing from stage 1,
very light sleep, to stage 3, deep sleep. NREM sleep dominates
during naps and nocturnal sleep periods. NREM sleep is essential
for physiologic well-being.
REM sleep recurs about every 90 minutes and is often associated
with dreaming. REM sleep is essential for psychosocial and mental
equilibrium.
• During a normal night’s sleep, an adult has four to six sleep cycles,
•
•
•
•
•
each with NREM (quiet sleep) and REM (rapid-eye-movement)
sleep.
The ratio of NREM to REM sleep varies with age.
Many factors can affect sleep, including illness, environment, lifestyle, emotional stress, stimulants and alcohol, diet, smoking, motivation, and medications.
Common sleep disorders include insomnia, hypersomnia, narcolepsy, parasomnias (such as somnambulism, sleeptalking, and
bruxism), and sleep apnea.
Assessment of a client’s sleep includes a sleep history, a health history, and a physical examination to detect signs that may indicate
the presence of sleep apnea.
Nursing responsibilities to help clients sleep include (a) teaching
clients ways to enhance sleep, (b) supporting bedtime rituals,
(c) creating a restful environment, (d) promoting comfort and relaxation, and (e) enhancing sleep with medications.
TEST YOUR KNOWLEDGE
1. A client is admitted for a sleep disorder. The nurse knows that
the reticular activating system (RAS) is involved in the sleep–
wake cycle. In the accompanying illustration, which letter indicates the location of the RAS?
D
C
B
A
1. A
2. B
3. C
4. D
2. A nurse is admitting a critically ill client to the intensive care unit.
What questions should the nurse ask regarding this client’s sleep
history?
1. No questions should be asked.
2. When do you usually go to sleep?
3. Do you have any problems with sleeping?
4. What are your bedtime rituals?
M45_BERM9793_11_GE_C45.indd 1184
3. A nurse is working with a client to develop an expected outcome
for the nursing diagnosis Disturbed Sleep Pattern, difficulty
staying asleep related to anxiety secondary to multiple life
stressors. Which expected outcome would be most applicable
to this client’s situation?
1. The client will sleep at least 8 hours each night.
2. The client will list three positive coping mechanisms for
anxiety relief.
3. The client will report getting sufficient sleep to provide energy
for daily activities.
4. The client will manifest less anxiety after taking prescribed
medications.
4. A client reports to the nurse that she has been taking barbiturate
sleeping pills every night for several months and now wishes
to stop taking them. Which statement is the most appropriate
advice for the nurse to provide the client?
1. Take the last pill on a Friday night so disrupted sleep can be
compensated on the weekend.
2. Continue to take the pills since sleeping without them after
such a long time will be difficult and perhaps impossible.
3. Discontinue taking the pills.
4. Continue taking the pills and discuss tapering the dose with
the primary care provider.
27/01/2021 18:05
Chapter 45
5. During a well-child visit, a mother tells the nurse that her 4-yearold daughter typically goes to bed at 10:30 P.M. and awakens
each morning at 7 A.M. She does not take a nap in the afternoon. Which is the best response by the nurse?
1. Encourage the mother to consider putting her daughter to
bed between 8 and 9 P.M.
2. Reassure the mother that it is normal for 4-year-olds to resist
napping, but encourage her to insist that she rest quietly
each afternoon.
3. Recommend that her daughter be allowed to sleep later in
the morning.
4. Reassure her that her daughter’s sleep pattern is normal and
that she has outgrown her need for an afternoon nap.
6. A client complains of being unable to stay awake during the day
even after sleeping throughout the night. What should the nurse
suggest to this client?
1. Go to your physician for a physical examination.
2. Go to a mental health professional for evaluation of possible
depression.
3. Purchase an over-the-counter sleep aid to deepen nighttime
sleep.
4. Drink more caffeinated beverages in the daytime to stay
awake.
7. During a yearly physical, a 52-year-old male client mentions
that his wife frequently complains about his snoring. During the
physical exam, the nurse notes that his neck size is 18 inches,
his soft palate and uvula are reddened and swollen, and he is
overweight. What is the most appropriate nursing intervention
for the nurse to recommend to this client?
1. Recommend that he and his wife sleep in separate bedrooms so that his snoring does not disturb his wife.
2. Refer him to a dietitian for a weight-loss program.
3. Caution him not to drink or take sleeping pills since they may
make his snoring worse.
4. Refer him to a sleep disorders center for evaluation and
treatment of his symptoms.
8. A new nursing graduate’s first job requires 12-hour night shifts.
Which strategy will make it easier for the graduate to sleep during the day and remain awake at night?
●
Sleep
1185
1. Wear dark wraparound sunglasses when driving home in the
morning, and sleep in a darkened bedroom.
2. Exercise on the way home to avoid having to stand around
waiting for equipment at the gym.
3. Drink several cups of strong coffee or 16 oz of caffeinated
soda when beginning the shift.
4. Try to stay in a brightly lit area when working at night.
9. The nurse is answering questions after a presentation on sleep
at a local seniors’ center. A woman in her late 70s asks for an
opinion about the advisability of allowing her husband to nap
for 15 to 20 minutes each afternoon. Which is the nurse’s best
response?
1. “Taking an afternoon nap will interfere with his being able to
sleep at night. If he’s tired in the afternoon, see if you can
interest him in some type of stimulating activity to keep him
awake.”
2. “He shouldn’t need to take an afternoon nap if he’s getting
enough sleep at night.”
3. “Unless your husband has trouble falling asleep at night, a
brief afternoon nap is fine.”
4. “Encourage him to consume coffee or some other caffeinated beverage at lunch to prevent drowsiness in the
afternoon.”
10. During admission to a hospital unit, the client tells the nurse that
her sleep tends to be very light and that it is difficult for her to
get back to sleep if she’s awakened at night. Which interventions
should the nurse implement? Select all that apply.
1. Remind colleagues to keep their conversation to a minimum
at night.
2. Encourage the client’s family members to bring in a radio to
play soft music at night.
3. Deliver necessary medications and procedures at 1.5- or
3-hour intervals between 11 P.M. and 6 A.M.
4. Encourage the client to ask family members to bring in a fan
to provide white noise.
5. Increase the temperature in the room.
See Answers to Test Your Knowledge in Appendix A.
READINGS AND REFERENCES
Suggested Readings
References
Matre, D., Andersen, M. R., Knardahl, S., & Nilsen, K. B.
(2016). Conditioned pain modulation is not decreased
after partial sleep restriction. European Journal of Pain, 20,
408–416. doi:10.1002/ejp.741
Sleep difficulties contribute to chronic pain conditions.
The study determined if sleep restriction affects heat pain
perception and conditioned pain response. The results of
the study revealed that sleep restriction leads to increased
heat pain perception.
Pallesen, S., Gundersen, H. S., Kristoffersen, M., Bjorvatn, B.,
Thun, E., & Harris, A. (2017). The effects of sleep deprivation on soccer skills. Perceptual and Motor Skills, 124,
812–829. doi:10.1177/0031512517707412
The study examined the effects of sleep deprivation on an
athlete’s soccer skills. The study results revealed a negative
effect of sleep deprivation on the continuous kick test.
American Geriatrics Society. (2019). American Geriatics
Society 2019 updated AGS Beers Criteria for potentially
inappropriate medication use in older adults. Journal of
American Geriatrics Society, 67(4), 674–694. doi:10.1111/
jgs.15767
Bonuck, K. A., Blank, A., True-Felt, B., & Chervin, R. (2016).
Promoting sleep health among families of young children
in Head Start: Protocol for a social-ecological approach.
Preventing Chronic Disease, 13, 160144. doi.org/10.5888/
pcd13.160144
Butcher, H. K., Bulechek, G. M., Dochterman, J. M., &
Wagner, C. M. (Eds.). (2018). Nursing interventions
classification (NIC) (7th ed.). St. Louis, MO: Elsevier.
Centers for Disease Control and Prevention. (2018). Sleep
and sleep disorders. Retrieved from https://www.cdc.gov/
sleep/index.html
Corkin, M., Peterson, E., Andrejic, N., Waldie, K., Reese, E.,
& Morton, S. (2017). Predicators of mothers’ self-identified
challenges in parenting infants: Insights from a large,
nationally diverse cohort. Journal of Child and Family
Studies, 27, 653–670. doi:10.1007/s10826-017-0903-5
Cowie, J., Palmer, C., Hussain, H., & Alfano, C. (2016).
Parental involvement in infant sleep routines predicts differential sleep patterns in children with and without anxiety
disorders. Child Psychiatry & Human Development, 47,
636–646. doi:10.1007/s10578-015-0597-0
Related Research
Louis, J., & Street, L. (2018). Obstructive sleep apnea in
pregnancy—what you need to know: Sleep disordered
breathing has implications for both mother and fetus.
Contemporary OB/GYN, 63(2), 18–22.
Taheri, M., & Irandoust, K. (2018). The exercise induced weight
loss improves self-reported quality of sleep in obese elderly
women with sleep disorders. Sleep and Hypnosis, 20(1),
54–59. doi:10.5350/Sleep.Hypn.2017.19.0134
M45_BERM9793_11_GE_C45.indd 1185
Frandsen, G., & Pennington, S. (2018). Abrams’ clinical drug
therapy rationales for nursing practice (11th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Graff-Radford, J. (2017). Sundowning: Late day confusion. Retrieved from https://www.mayoclinic.org/
diseases-conditions/alzheimers-disease/expert-answers/
sundowning/faq-20058511
Judd, B. G., & Sateia, M. J. (2019). Classification of sleep
disorders. Retrieved from https://www.uptodate.com/
contents/classification-of-sleep-disorders
Krieger, L. (2017). Better sleep A to Z. Good Housekeeping,
264(3), 107–112.
Liu, Y., Croft, J. B., Wheaton, A. G., Kanny, D., Cunningham,
T. J., Lu, H., . . . Giles, W. H. (2016). Clustering of five
health-related behaviors for chronic disease prevention
among adults, United States, 2013. Preventing Chronic
Disease, 13, 160054. doi:10.5888/pcd13.160054
Martens, M. A., Seyfer, D. L., Andridge, R. R., & Coury, D. L.
(2017). Use and effectiveness of sleep medications by parent report in individuals with Williams syndrome. Journal
of Developmental & Behavioral Pediatrics, 38(9), 765–771.
doi:10.1097/DBP.0000000000000503
Miller, N. (2015). Sleep deprivation and delirium risk in hospitalized patients. Nursing Made Incredibly Easy, 13(1), 22–28.
doi:10.1097/01.NME.0000457284.31841.36
Morgenthaler, T. I., Hashmi, S., Croft, J. B., Dort, L., Heald,
J., & Mullington, J. (2016). High school start times and
27/01/2021 18:05
1186
Unit 10
●
Promoting Physiologic Health
the impact on high school students: What we know, and
what we hope to learn. Journal of Clinical Seep Medicine,
12(12), 1681–1689. doi:10.5664/jcsm.6358
National Sleep Foundation. (n.d.). Stages of human sleep.
Retrieved from http://sleepdisorders.sleepfoundation.org/
chapter-1-normal-sleep/stages-of-human-sleep
National Sleep Foundation. (n.d.a). Children and sleep.
Retrieved from https://www.sleepfoundation.org/articles/
children-and-sleep
National Sleep Foundation. (n.d.b). How much sleep do adults
really need? Retrieved from https://sleep.org/articles/
how-much-sleep-adults/
National Sleep Foundation. (n.d.c). How much sleep
do babies and kids need? Retrieved from https://
sleepfoundation.org/excessivesleepiness/content/
how-much-sleep-do-babies-and-kids-need
National Sleep Foundation. (n.d.d). Improve your memory
with a good night’s sleep. Retrieved from https://
sleepfoundation.org/excessivesleepiness/content/
improve-your-memory-good-nights-sleep
National Sleep Foundation. (n.d.e). Insomnia and women.
Retrieved from https://sleepfoundation.org/insomnia/
content/insomnia-women
National Sleep Foundation. (n.d.f). Insomnia: Symptoms.
Retrieved from https://sleepfoundation.org/insomnia/
content/symptoms
National Sleep Foundation. (n.d.g). Myths and facts about
sleep. Retrieved from https://sleepfoundation.org/
how-sleep-works/myths-and-facts-about-sleep/page/0/1
National Sleep Foundation. (n.d.h). Sleeping during the
day: Is it OK? Retrieved from http://sleep.org/articles/
sleeping-during-the-day/
M45_BERM9793_11_GE_C45.indd 1186
National Sleep Foundation. (n.d.i). What is insomnia? Retrieved
from https://sleepfoundation.org/insomnia/content/
what-is-insomnia
Owens, B., Allen, W., & Moultrie, D. (2017). The impact of
shift work on nurses’ quality of sleep. ABNF Journal, 28(3),
59–63.
Owens, J., Adolescent Sleep Working Group, & Committee
on Adolescence. (2014). Insufficient sleep in adolescents
and young adults: An update on causes and consequences. Pediatrics, 134( 3), e921–e932. doi:10.1542/
peds.2014-1696
Ozdemir, P. G., & Atilla, E. (2017). A supportive therapeutic and
diagnostic modality: sleep deprivation. Sleep and Hypnosis, 19(3), 78–79. doi:10.5350/Sleep.Hypn.2016.18.0121
Richards, K., Demartini, J., & Xiong, G. (2018). Understanding
sleep disorders in older adults. Psychiatric Times, 35(2),
17–20.
Schweizer, A., Berchtold, A., Barrense-Dias, Y., Akre, C., &
Suris, J. C. (2017). Adolescents with a smartphone sleep
less than their peers. European Journal of Pediatrics, 176,
131–136. doi:10.1007/s00431-016-2823-6
Selvi, Y., Kilic, S., Aydin, A., & Guzel Oxdemir, G. (2015). The
effects of sleep deprivation on dissociation and profiles
of mood, and its association with biochemical changes.
Archives of Neuropsychiatry, 52(1), 83–88. doi:10.5152/
npa.2015.7116
Sleep.org. (n.d.). What is the sleep/wake cycle? Retrieved from
https://sleep.org/articles/sleepwake-cycle/
Vincensi, B., Pearce, K., Redding, J., Brandonisio, S., Tzou,
S., & Meiusi, E. (2016). Sleep in the hospitalized patient:
Nurse and patient perceptions. MedSurg Nursing, 25(5),
351–356.
Wheaton, A. G., Jones, S. E., Cooper, A. C., & Croft, J. B.
(2018). Short sleep duration among middle school and
high school students—United States, 2015. Morbidity and
Mortality Weekly Report, 67(3), 85–90.
Selected Bibliography
Amyx, M., Xiong, X., Xie, Y., & Buekens, P. (2017). Racial/
ethnic differences in sleep disorders and reporting trouble
sleeping among women of childbearing age in the United
States. Maternal Child Health Journal, 21, 306–314.
doi:10.1007/s10995-016-2115-9
Boivin, D. B. (2017). Treating delayed sleep–wake phase disorder in young adults. Journal of Psychiatry & Neuroscience,
42(5), E9–E10. doi:10.1503/jpn.160243
Ozcan, E., Aydin, E. F., & Ozcan, H. (2017). Paroxysmal
nocturnal sleep disorder with atypic clinical appearance and therapy with sleep hygiene: A case report.
Sleep and Hypnosis, 19(1), 18–20. doi:10.5350/Sleep.
Hypn.2016.18.0114
Pruitt, B. (2015). PTSD’s effect on sleep and sleep disorders.
The Journal of Respiratory Care Practitioners, 28(5), 19–22.
Tokizawa, K., Sawada, S., Tetsuo, L., & Jian, L. (2015). Effects
of partial sleep restriction and subsequent daytime napping on prolonged exertional heat strain. Occupational and
Environmental Medicine, 72(7), 521–528. doi:10.1136/
oemed-2014-102548
27/01/2021 18:05
Nutrition
46
LEA R N IN G OU TC OME S
After completing this chapter, you will be able to:
1. Identify essential nutrients and their dietary sources.
2. Describe normal digestion, absorption, and metabolism of
carbohydrates, proteins, and lipids.
3. Identify factors influencing nutrition.
4. Identify nutritional variations throughout the lifecycle.
5. Evaluate a diet using a food guide.
6. Discuss essential components and purposes of nutritional
assessment and nutritional screening.
7. Identify risk factors for and clinical signs of malnutrition.
8. Describe nursing interventions to promote optimal nutrition.
9. Discuss nursing interventions to treat clients with nutritional
problems.
10. Verbalize the steps used in:
a. Inserting a nasogastric tube.
b. Removing a nasogastric tube.
c. Administering a tube feeding.
d. Administering a gastrostomy or jejunostomy tube feeding.
11. Recognize when it is appropriate to assign aspects of feeding
clients to assistive personnel.
12. Plan, implement, and evaluate nursing care associated with
nursing diagnoses related to nutritional problems.
13. Demonstrate appropriate documentation and reporting of
nutritional therapy.
K EY T E RMS
24-hour food recall, 1208
anabolism, 1189
anemia, 1195
anorexia nervosa, 1197
basal metabolic rate (BMR), 1191
body mass index (BMI), 1191
bottle mouth syndrome, 1196
bulimia, 1197
caloric value, 1191
calorie, 1191
catabolism, 1189
cholesterol, 1189
complete proteins, 1188
demand feeding, 1195
diet history, 1208
disaccharides, 1188
dysphagia, 1193
enteral, 1213
enzymes, 1188
essential amino acids, 1188
fad, 1192
fat-soluble vitamins, 1190
fats, 1189
fatty acids, 1189
food diary, 1208
food frequency record, 1208
gastrostomy, 1217
glycerides, 1189
glycogen, 1188
ideal body weight (IBW), 1191
incomplete proteins, 1189
iron deficiency anemia, 1195
jejunostomy, 1217
kilojoule (kJ), 1191
large calorie (Calorie, kilocalorie
[Kcal]), 1191
lipids, 1189
lipoproteins, 1190
macrominerals, 1190
macronutrients, 1188
malnutrition, 1202
metabolism, 1191
Introduction
Nutrition is the sum of all the interactions between an organism and the food it consumes. In other words, nutrition is
what an individual eats and how the body uses it. Nutrients
are organic and inorganic substances found in foods that are
required for body functioning. Adequate food intake consists of a balance of nutrients: water, carbohydrates, proteins,
fats, vitamins, and minerals. Foods differ greatly in their
nutritive value (the nutrient content of a specified amount
of food), and no one food provides all essential nutrients.
Nutrients have three major functions: providing energy for
microminerals, 1190
micronutrients, 1188
mid-arm circumference (MAC), 1205
mid-arm muscle area (MAMA), 1205
minerals, 1190
monosaccharides, 1188
monounsaturated fatty acids, 1189
nasoenteric (nasointestinal) tube,
1217
nasogastric tube, 1213
nitrogen balance, 1189
nonessential amino acids, 1188
nutrients, 1187
nutrition, 1187
nutritive value, 1187
obese, 1202
oils, 1189
overnutrition, 1202
overweight, 1202
percutaneous endoscopic
gastrostomy (PEG), 1217
percutaneous endoscopic
jejunostomy (PEJ), 1217
polysaccharides, 1188
polyunsaturated fatty acids, 1189
protein-calorie malnutrition (PCM),
1203
pureed diet, 1210
refeeding syndrome, 1219
regurgitation, 1195
resting energy expenditure (REE),
1191
saturated fatty acids, 1189
skinfold measurement, 1205
small calorie (c, cal), 1191
triglycerides, 1189
undernutrition, 1203
unsaturated fatty acid, 1189
urea, 1206
vitamin, 1190
water-soluble vitamins, 1190
body processes and movement, providing structural material for body tissues, and regulating body processes.
Essential Nutrients
The body’s most basic nutrient need is water. Because every
cell requires a continuous supply of fuel, the most important
nutritional need, after water, is for nutrients that provide
fuel, or energy. The energy-providing nutrients are carbohydrates, fats, and proteins. Hunger compels people to eat
enough energy-providing nutrients to satisfy their energy
needs. Carbohydrates, fats, protein, minerals, vitamins, and
1187
M46_BERM9793_11_GE_C46.indd 1187
03/02/2021 18:20
1188
Unit 10
●
Promoting Physiologic Health
water are referred to as macronutrients, because they are
needed in large amounts (e.g., hundreds of grams) to provide energy. Micronutrients are those vitamins and minerals that are required in small amounts (e.g., milligrams or
micrograms) to metabolize the energy-providing nutrients.
Carbohydrates
Carbohydrates are composed of the elements carbon (C),
hydrogen (H), and oxygen (O) and are of two basic types:
simple carbohydrates (sugars) and complex carbohydrates
(starches and fiber). Natural sources of carbohydrates also
supply vital nutrients, such as protein, vitamins, and minerals that are not found in processed foods. Processed carbohydrate foods are relatively low in nutrients in relation
to the large number of calories they contain. High-sugarcontent (and solid fat) foods are referred to as “empty
calories.” In addition, alcoholic beverages contain significant amounts of carbohydrate, but very few nutrients and,
thus, they are also empty calories.
Types of Carbohydrates
SUGARS
Sugars, the simplest of all carbohydrates, are water soluble
and are produced naturally by both plants and animals.
Sugars may be monosaccharides (single molecules) or
disaccharides (double molecules). Of the three monosaccharides (glucose, fructose, and galactose), glucose is by
far the most abundant simple sugar.
Most sugars are produced naturally by plants, especially fruits, sugar cane, and sugar beets. However, other
sugars come from animal sources. For example, lactose, a
combination of glucose and galactose, is found in animal
milk. Processed or refined sugars (e.g., table sugar, molasses, and corn syrup) have been extracted and concentrated
from natural sources.
Not all sugars have calories and not all sweeteners are
sugars. Sugar substitutes are available from both natural
and manufactured sources and have almost no calories.
Often referred to as “artificial” sugar, noncaloric sweeteners including saccharin and aspartame are much sweeter
than sugar by volume. Sugar alcohols such as erythritol
and sorbitol are low in calories, do not contain ethanol
(present in alcoholic beverages), and are often used in
chewing gums. Some sweeteners are not easily categorized, such as the extract from the leaf of the stevia plant.
STARCHES
Starches are the insoluble, nonsweet forms of carbohydrate. They are polysaccharides; that is, they are composed
of branched chains of dozens, sometimes hundreds, of
glucose molecules. Like sugars, nearly all starches exist
naturally in plants, such as grains, legumes, and potatoes.
Other foods, such as cereals, breads, flour, and puddings,
are processed from starches.
FIBER
Fiber, a complex carbohydrate derived from plants, supplies roughage, or bulk, to the diet. However, fiber cannot
M46_BERM9793_11_GE_C46.indd 1188
be digested by humans. This complex carbohydrate satisfies the appetite and helps the digestive tract to function effectively and eliminate waste. Fiber is present in
the outer layer of grains, bran, and in the skin, seeds, and
pulp of many vegetables and fruits.
Carbohydrate Digestion
Major enzymes of carbohydrate digestion include ptyalin (salivary amylase), pancreatic amylase, and the disaccharidases: maltase, sucrase, and lactase. Enzymes are
biological catalysts that speed up chemical reactions.
The desired end products of carbohydrate digestion
are monosaccharides. Some simple sugars are already
monosaccharides and require no digestion. Essentially,
all monosaccharides are absorbed by the small intestine
in healthy individuals.
Carbohydrate Metabolism
Carbohydrate metabolism is a major source of body
energy. After the body breaks carbohydrates down into
glucose, some glucose continues to circulate in the blood
to maintain blood levels and to provide a readily available source of energy. The remainder is used as energy
or stored. Insulin, a hormone secreted by the pancreas,
enhances the transport of glucose into cells.
Storage and Conversion
Carbohydrates are stored either as glycogen or as fat.
Glycogen is a large polymer (compound molecule) of glucose. Almost all body cells can store glycogen; however,
most is stored in the liver and skeletal muscles, where it is
available for conversion back into glucose. Glucose that cannot be stored as glycogen is converted to fat.
Proteins
Amino acids, organic molecules made up primarily of carbon, hydrogen, oxygen, and nitrogen, combine to form
proteins. Every cell in the body contains some protein, and
about three-quarters of body solids are proteins.
Amino acids are categorized as essential or nonessential. Essential amino acids are those that cannot be manufactured in the body and must be supplied as part of the
protein ingested in the diet. Nine essential amino acids—
histidine, isoleucine, leucine, lysine, methionine, phenylalanine, tryptophan, threonine, and valine—are necessary for
tissue growth and maintenance. A tenth, arginine, appears
to have a role in the immune system.
Nonessential amino acids are those that the body can
manufacture. The body takes amino acids derived from
the diet and reconstructs new ones from their basic elements. Nonessential amino acids include alanine, aspartic
acid, cystine, glutamic acid, glycine, hydroxyproline, proline, serine, and tyrosine.
Proteins may be complete or incomplete. Complete
proteins contain all of the essential amino acids plus many
nonessential ones. Most animal proteins, including meats,
poultry, fish, dairy products, and eggs, are complete proteins.
Some animal proteins, however, contain less than the required
amount of one or more essential amino acids and therefore
cannot alone support continued growth. These proteins are
03/02/2021 18:20
Chapter 46
sometimes referred to as partially complete proteins. Examples
are gelatin, which has small amounts of tryptophan, and the
milk protein casein, which has only a little arginine.
Incomplete proteins lack one or more essential amino
acids (most commonly lysine, methionine, or tryptophan)
and are usually derived from vegetables. If, however, an
appropriate mixture of plant proteins is provided in the diet,
a balanced ratio of essential amino acids can be achieved.
For example, a combination of corn (low in tryptophan and
lysine) and beans (low in methionine) is a complete protein. Such combinations of two or more vegetables are called
complementary proteins. Another way to take full advantage
of vegetable proteins is to eat them with a small amount of
animal protein. Spaghetti with cheese, rice with pork, noodles with tuna, and cereal with milk are just a few examples
of combining vegetable and animal proteins.
Protein Digestion
Digestion of protein foods begins in the stomach, where
the enzyme pepsin breaks protein down into smaller units.
However, most protein is digested in the small intestine.
The pancreas secretes the proteolytic enzymes trypsin,
chymotrypsin, and carboxypeptidase; glands in the intestinal wall secrete aminopeptidase and dipeptidase. These
enzymes break protein down into smaller molecules and
eventually into amino acids.
Storage
Amino acids are absorbed by active transport through
the small intestine into the portal blood circulation. The
liver uses amino acids to synthesize specific proteins (e.g.,
liver cells and the plasma proteins albumin, globulin, and
fibrinogen). Plasma proteins are a storage medium that
can rapidly be converted back into amino acids.
Other amino acids are transported to tissues and cells
throughout the body where they are used to make protein
for cell structures. In a sense, protein is stored as body
tissue. The body cannot actually store excess amino acids
for future use. However, a limited amount is available in
the “metabolic pool” that exists because of the constant
breakdown and buildup of the protein in body tissues.
Protein Metabolism
Protein metabolism includes three activities: anabolism
(building tissue), catabolism (breaking down tissue), and
maintaining nitrogen balance.
ANABOLISM
All body cells synthesize proteins from amino acids. The
types of proteins formed depend on the characteristics of
the cell and are controlled by its genes.
CATABOLISM
Because a cell can accumulate only a limited amount of protein, excess amino acids are degraded for energy or converted
to fat. Protein degradation occurs primarily in the liver.
NITROGEN BALANCE
Because nitrogen is the element that distinguishes protein
from lipids and carbohydrates, nitrogen balance reflects
the status of protein nutrition in the body. Nitrogen balance
M46_BERM9793_11_GE_C46.indd 1189
●
Nutrition
1189
is a measure of the degree of protein anabolism and catabolism; it is the net result of intake and loss of nitrogen.
When nitrogen intake equals nitrogen output, a state of
nitrogen balance exists.
Lipids
Lipids are organic substances that are greasy and insoluble
in water but soluble in alcohol or ether. Fats are lipids that
are solid at room temperature; oils are lipids that are liquid
at room temperature. In common use, the terms fats and
lipids are used interchangeably. Lipids have the same elements (carbon, hydrogen, and oxygen) as carbohydrates,
but they contain a higher proportion of hydrogen.
Fatty acids, made up of carbon chains and hydrogen,
are the basic structural units of most lipids. Fatty acids are
described as saturated or unsaturated, according to the relative number of hydrogen atoms they contain. Saturated
fatty acids are those in which all carbon atoms are filled
to capacity (i.e., saturated) with hydrogen; an example is
butyric acid, found in butter. An unsaturated fatty acid is
one that could accommodate more hydrogen atoms than
it currently does. It has at least two carbon atoms that are
not attached to a hydrogen atom; instead, there is a double bond between the two carbon atoms. Fatty acids with
one double bond are called monounsaturated fatty acids;
those with more than one double bond (or many carbons
not bonded to a hydrogen atom) are polyunsaturated fatty
acids. An example of a polyunsaturated fatty acid is linoleic acid, found in vegetable oil.
Based on their chemical structure, lipids are classified
as simple or compound. Glycerides, the simple lipids, are
the most common form of lipids. They consist of a glycerol
molecule with up to three fatty acids attached. Triglycerides
(which have three fatty acids) account for more than 90%
of the lipids in food and in the body. Triglycerides may
contain saturated or unsaturated fatty acids. Saturated
triglycerides are found in animal products, such as butter,
and are usually solid at room temperature. Unsaturated
triglycerides are usually liquid at room temperature and
are found in plant products, such as olive oil and corn oil.
Cholesterol is a fatlike substance that is both produced
by the body and found in foods of animal origin. Most
of the body’s cholesterol is synthesized in the liver; however, some is absorbed from the diet (e.g., from milk, egg
yolk, and organ meats). Cholesterol is needed to create
bile acids and to synthesize steroid hormones. Along with
phospholipids, large quantities of cholesterol are present
in cell membranes and other cell structures.
Lipid Digestion
Although chemical digestion of lipids begins in the stomach, they are digested mainly in the small intestine, primarily by bile, pancreatic lipase, and enteric lipase, an intestinal
enzyme. The end products of lipid digestion are glycerol,
fatty acids, and cholesterol. These are immediately reassembled inside the intestinal cells into triglycerides and cholesterol esters (cholesterol with a fatty acid attached to it), which
are not water soluble. For these reassembled products to be
transported and used, the small intestine and the liver must
03/02/2021 18:20
1190
Unit 10
●
Promoting Physiologic Health
convert them into soluble compounds called lipoproteins.
Lipoproteins are made up of various lipids and a protein.
Lipid Metabolism
Converting fat into usable energy occurs through the use
of the enzyme hormone-sensitive lipase, which breaks
down triglycerides in adipose cells, releasing glycerol
and fatty acids into the blood. A pound of fat provides
3500 kilocalories. Fasting individuals will obtain most of
their calories from fat metabolism, but some amount of
carbohydrate or protein must also be used because the
brain, nerves, and red blood cells require glucose. Only
the glycerol molecules in fat can be converted to glucose.
Micronutrients
A vitamin is an organic compound that cannot be manufactured by the body and is needed in small quantities
to catalyze metabolic processes. Thus, when vitamins
are lacking in the diet, metabolic deficits result. Vitamins
are generally classified as fat soluble or water soluble.
Water-soluble vitamins include C and the B-complex vitamins: B1 (thiamine), B2 (riboflavin), B3 (niacin or nicotinic acid), B6 (pyridoxine), B9 (folic acid, folate, folacin),
B12 (cobalamin), pantothenic acid, and biotin. The body
cannot store water-soluble vitamins; thus, people must get
a daily supply in the diet. Water-soluble vitamins can be
degraded by food processing, storage, and preparation.
Fat-soluble vitamins include A, D, E, and K. The body
can store these vitamins, although there is a limit to the
amounts of vitamins E and K the body can store. Therefore, a daily supply of fat-soluble vitamins is not absolutely necessary. Vitamin content is highest in fresh foods
consumed soon after harvest.
Minerals are found in organic compounds, as inorganic
compounds, and as free ions. Calcium and phosphorus
make up 80% of all mineral elements in the body. The two
categories of minerals are macrominerals and microminerals.
Macrominerals are those that people require daily in amounts
over 100 mg. They include calcium, phosphorus, sodium,
potassium, magnesium, chloride, and sulfur. Microminerals
are those that people require daily in amounts less than
100 mg. They include iron, zinc, manganese, iodine, fluoride,
copper, cobalt, chromium, and selenium.
Common problems associated with the mineral nutrients are iron deficiency resulting in anemia, and osteoporosis
resulting from loss of bone calcium. Additional information
about major minerals associated with the body’s fluid and
electrolyte balance is given in Chapter 51 .
ANATOMY & PHYSIOLOGY REVIEW
Digestive System
1 If the salivary glands
do not function or are
bypassed, which nutrients
would miss beginning
digestion?
Parotid gland
Tongue
Oral cavity
Pharynx
Salivary glands
2 The client has an
obstruction at the pyloric
sphincter. Where is this
and what result comes
from this obstruction?
Liver
Spleen
Gallbladder
Stomach
Pancreas
Small intestine
3 If storage of bile is
not possible because
the gallbladder has
been removed, what
on the client?
Esophagus
Cecum
Vermiform
appendix
4 All of the colon is
sometimes removed.
What digestive actions
would then not occur?
Transverse colon
Ascending colon
Decending colon
Sigmoid colon
Rectum
Anus
Answers to Anatomy & Physiology Review questions are available on the faculty resources site. Please consult with your instructor.
M46_BERM9793_11_GE_C46.indd 1190
03/02/2021 18:20
Chapter 46
Energy Balance
Energy balance is the relationship between the energy
derived from food and the energy used by the body. The
body obtains energy in the form of calories from carbohydrates, protein, fat, and alcohol. The body uses energy
for voluntary activities such as walking and talking and
for involuntary activities such as breathing and secreting
enzymes. An individual’s energy balance is determined by
comparing his or her energy intake with energy output.
Energy Intake
The amount of energy that nutrients or foods supply to the
body is their caloric value. A calorie is a unit of heat energy.
A small calorie (c, cal) is the amount of heat required to raise
the temperature of 1 gram of water 1 degree Celsius. This unit
of measure is used in chemistry and physics. A large calorie
(Calorie, kilocalorie [Kcal]) is the amount of heat energy
required to raise the temperature of 1 gram of water 15 to 16
degrees Celsius and is the unit used in nutrition (although it is
not universally capitalized). In the metric system, the measure
is the kilojoule (kJ). One Calorie (Kcal) equals 4.18 kilojoules.
The energy liberated from the metabolism of food has
been determined to be:
•
•
•
•
4 Calories/gram (17 kJ) of carbohydrates
4 Calories/gram (17 kJ) of protein
9 Calories/gram (38 kJ) of fat
7 Calories/gram (29 kJ) of alcohol.
Energy Output
Metabolism refers to all biochemical and physiologic
processes by which the body grows and maintains itself.
Metabolic rate is normally expressed in terms of the rate
of heat liberated during these chemical reactions. The
basal metabolic rate (BMR) is the rate at which the body
metabolizes food to maintain the energy requirements of
an individual who is awake and at rest. The energy in food
maintains the basal metabolic rate of the body and provides energy for activities such as running and walking.
Resting energy expenditure (REE) is the amount of energy
required to maintain basic body functions; in other words,
the calories required to maintain life. The REE of healthy
individuals is generally about 1 cal/kg of body weight/h
for men and 0.9 cal/kg/h for women although there is great
variation among individuals. BMR is calculated by measuring the REE in the early morning, 12 hours after eating.
The actual daily expenditure of energy depends on the
degree of activity of the individual. Some activities require
many times the REE. Examples of approximate real caloric
expenditures compared to the REE are as follows:
Studying: 150%
Heavy housework (e.g., vacuuming): 400%
Walking steadily at 3.5 mph: 450%
Gardening: 600%
Average jogging, cycling, energetic swimming: 800%
M46_BERM9793_11_GE_C46.indd 1191
●
Nutrition
1191
Body Weight and Body
Mass Standards
Maintaining a healthy or ideal body weight requires a balance between the expenditure of energy and the intake
of nutrients. Generally, when energy requirements of an
individual equate with the daily caloric intake, the body
weight remains stable. Ideal body weight (IBW) is the optimal weight recommended for optimal health. To determine an individual’s approximate IBW, the nurse can
consult standardized tables or can quickly calculate a
value using the Rule of 5 for females and the Rule of 6 for
males (Box 46.1). Many standardized tables and formulas
were developed many years ago and are based on limited
samples. The nurse should use great caution in suggesting
that these weights apply to all clients.
BOX 46.1
Approximating Ideal Body Weight
Rule of 5 for Females
Rule of 6 for Males
100 lb (45.5 kg) for 5 ft (152 cm) 106 lb (48.2 kg) for 5 ft (152 cm)
of height
of height
+5 lb (2.27 kg) for each inch
(2.54 cm) over 5 ft (152 cm)
+6 lb (2.73 kg) for each inch
(2.54 cm) over 5 ft (152 cm)
{ 10% for body-frame size*
{ 10% for body-frame size*
*Determine body-frame size by measuring the client’s wrist circumference and applying to the
table below. Add 10% for large body-frame size, and subtract 10% for small body-frame size.
Female Wrist Measurements
Height More
Height Less Height
Than 5′2″
5′2″95′5″ Than 5′5″
(Less Than (155–
(More Than
155 cm)
163 cm) 163 cm)
Small
Less than
Less than Less than
5.5″
6.0″
6.25″
(140 mm)
(152 mm) (159 mm)
Medium 5.5″95.75″ 6″96.25″ 6.25″96.5″
(140–
(152–
(159–
146 mm)
159 mm) 165 mm)
Large
More than More than More than
5.75″
6.25″
6.5″
(146 mm)
(159 mm) (165 mm)
Male Wrist
Measurements
Height More
Than 5′5″
(More Than
163 cm)
5.5″96.5″
(140–
165 mm)
6.5″97.5″
(165–
191 mm)
More than
7.5″
(191 mm)
Many health professionals consider the body mass
index to be a more reliable indicator of an individual’s
healthy weight. For people older than 18 years, the body
mass index (BMI) is an indicator of changes in body fat
stores and whether an individual’s weight is appropriate for height, and may provide a useful estimate of
malnutrition. However, the results must be used with
caution in people who have fluid retention (e.g., ascites
or edema), athletes, or older adults. To calculate the BMI:
Measure the individual’s height in meters, e.g., 1.7 m
(1 meter = 3.3 ft, or 39.6 in.)
Measure the weight in kilograms, e.g., 72 kg
(1 kg = 2.2 pounds)
03/02/2021 18:20
1192
Unit 10
●
Promoting Physiologic Health
Calculate the BMI using the following formula:
BMI =
weight in kilograms
(height in meters)2
Development
or
72 kilograms
1.7 * 1.7 meters
= 24.9
Box 46.2 provides an interpretation of the results.
BOX 46.2
Classification of Overweight and
Obesity by BMI, Waist Circumference,
and Associated Disease Risks*
BMI
(kg/m2)
Underweight
Normal+
Overweight
Obesity
Extreme
obesity
618.5
18.5–24.9
25.0–29.9
30.0–34.9
35.0–39.9
40.0+
Disease Risk* Relative to Normal
Weight and Waist Circumference
Obesity Men: 102 cm Men > 102 cm
Class (40 in.) or Less (40 in.)
I
II
III
Women: 88 cm
(35 in.) or Less
—
—
Increased
High
Very high
Extremely high
Women > 88 cm
(35 in.)
—
—
High
Very high
Very high
Extremely high
*Disease risk for type 2 diabetes, hypertension, and cardiovascular disease.
+
Increased waist circumference can also be a marker for increased risk even in individuals of
normal weight.
From Aim for a Healthy Weight, National Heart, Lung, and Blood Institute, n.d., Washington,
DC: U.S. Department of Health & Human Services. Retrieved from http://www.nhlbi.nih.gov/
health/public/heart/obesity/lose_wt/bmi_dis.htm
Another measure of body mass is percent body fat.
Because BMI uses only height and weight, it can give
misleading results for certain groups of clients such
as athletes, frail older adults, and children. The most
accurate percentage of body fat can be measured by
underwater (hydrostatic) weighing and dual-energy
x-ray absorptiometry (DEXA), but these methods
are time consuming and expensive. Air displacement plethysmography (commonly referred to as the
BOD POD system) is faster and much less expensive
(Nelms, Sucher, & Lacey, 2016). Other indirect but more
practical measures include waist circumference (see
Box 46.2), skinfold testing, and bioelectrical impedance
analysis.
Factors Affecting Nutrition
Although the nutritional content of food is an important consideration when planning a diet, an individual’s food preferences and habits are often a major
factor affecting actual food intake. Habits about eating
are influenced by developmental considerations, gender, ethnicity and culture, beliefs about food, personal
preferences, religious practices, lifestyle, economics,
M46_BERM9793_11_GE_C46.indd 1192
medications and therapy, health, alcohol consumption,
advertising, and psychologic factors.
People in rapid periods of growth (i.e., infancy and adolescence) have increased needs for nutrients. Older adults,
on the other hand, may need fewer calories and also need
some dietary changes in view of their risk for coronary
heart disease, osteoporosis, and hypertension.
Sex
Nutrient requirements are different for males and females
because of body composition and reproductive functions.
The larger muscle mass of males translates into a greater
need for calories and proteins. Because of menstruation,
females require more iron than males do prior to menopause. Pregnant and lactating females have increased
caloric and fluid needs.
Ethnicity and Culture
Ethnicity often determines food preferences. Traditional
foods (e.g., rice for Asians, pasta for Italians, curry for
Indians) are eaten long after other customs are abandoned.
Nurses should not use a “good food, bad food”
approach, but rather should realize that variations of
intake are acceptable under different circumstances. The
only “universally” accepted guidelines are (a) to eat a
wide variety of foods to furnish adequate nutrients and
(b) to eat moderately to maintain body weight. Food preference probably differs as much among individuals of the
same cultural background as it does between cultures. Not
all Italians like pizza, for example, and many undoubtedly
enjoy Mexican food.
Beliefs About Food
Beliefs about effects of foods on health and well-being
can affect food choices. Many people acquire their beliefs
about food from television, magazines, and other media.
Some people are reducing their intake of animal fats in
response to evidence that excessive consumption of animal fats is a major risk factor in vascular disease, including heart attack and stroke.
Food fads that involve nontraditional food practices
are relatively common. A fad is a widespread but shortlived interest or a practice followed with considerable
zeal. It may be based either on the belief that certain foods
have special powers or on the notion that certain foods
are harmful. Food fads appeal to the individual seeking
a miracle cure for a disease, the individual who desires
superior health, or someone who wants to delay aging.
Some fad diets are harmless, but others are potentially
dangerous. Determining the needs a fad diet fills for the
client enables the nurse both to support these needs and
to suggest a more nutritious diet.
03/02/2021 18:20
Chapter 46
Personal Preferences
People develop likes and dislikes based on associations
with a typical food. A child who loves to visit his grandparents may love pickled crabapples because they are
served in the grandparents’ home. Another child who
dislikes a very strict aunt grows up to dislike the chicken
casserole she often prepared. People often carry such preferences into adulthood.
Individual likes and dislikes can also be related to
familiarity. Children often say they dislike a food before
they sample it. Some adults are very adventuresome and
eager to try new foods. Others prefer to eat the same
foods repeatedly. Preferences in the tastes, smells, flavors
(blends of taste and smell), temperatures, colors, shapes,
and sizes of food influence an individual’s food choices.
Some people may prefer sweet and sour tastes to bitter or
salty tastes. Textures play a great role in food preferences.
Some people prefer crisp food to limp food, firm to soft,
tender to tough, smooth to lumpy, or dry to soggy.
Religious Practices
Religious practice also affects diet. Some Roman Catholics avoid meat on certain days, and some Protestant
faiths prohibit meat, tea, coffee, or alcohol. Both Orthodox Judaism and Islam prohibit pork. Orthodox Jews
observe kosher customs, eating certain foods only if they
are inspected by a rabbi and prepared according to dietary
laws. The nurse must plan care with consideration of such
religious dietary practices.
Lifestyle
Certain lifestyles are linked to food-related behaviors.
Individuals who are always in a hurry may buy convenience grocery items or eat restaurant meals. Those
who spend many hours at home may take time to prepare more meals “from scratch.” Individual differences
also influence lifestyle patterns (e.g., cooking skills,
concern about health). Some individuals work at different times, such as evening or night shifts. They might
need to adapt their eating habits to this and also make
changes in their medication schedules if they are related
to food intake.
Muscular activity affects metabolic rate more than any
other factor; the more strenuous the activity, the greater
the stimulation of the metabolism. Mental activity, which
requires only about 4 Kcal per hour, provides very little
metabolic stimulation.
Economics
What, how much, and how often an individual eats are
frequently affected by socioeconomic status. For example, people with limited income, including some older
adults, may not be able to afford meat and fresh vegetables. In contrast, individuals with higher incomes may
purchase more proteins and fats and fewer complex
M46_BERM9793_11_GE_C46.indd 1193
●
Nutrition
1193
carbohydrates. Not all individuals have the financial
resources for extensive food preparation and storage
facilities. The nurse should not assume that clients have
their own stove, refrigerator, or freezer. In some lowincome areas, food costs at small local grocery stores
can be significantly higher than at large chain stores
farther away.
Medications and Therapy
The effects of drugs on nutrition vary considerably.
They may alter appetite, disturb taste perception, or
interfere with nutrient absorption or excretion. Nurses
need to be aware of the nutritional effects of specific
drugs when evaluating a client for nutritional problems.
The nursing history interview should include questions
about the medications the client is taking. Conversely,
nutrients can affect drug utilization. Some nutrients can
decrease drug absorption; others enhance absorption.
For example, the calcium in milk hinders absorption of
the antibiotic tetracycline but enhances the absorption
of the antibiotic erythromycin. Older adults are at particular risk for drug–food interactions due to the number
of medications they may take, age-related physiologic
changes affecting medication actions (e.g., decrease in
lean-to-fat ratio, decrease in renal or hepatic function),
and disease-restricted diets. Selected drug and nutrient
interactions are shown in Table 46.1.
Therapies prescribed for certain diseases (e.g., chemotherapy and radiation for cancer) may also adversely
affect eating patterns and nutrition. Normal cells of the
bone marrow and the gastrointestinal (GI) mucosa are
naturally very active and particularly susceptible to
antineoplastic agents. Oral ulcers, intestinal bleeding, or
diarrhea resulting from the toxicity of the antineoplastic
agents used in chemotherapy can seriously diminish an
individual’s nutritional status.
The effects of radiotherapy depend on the area that
is treated. Radiotherapy of the head and neck may cause
decreased salivation, taste distortions, and swallowing
difficulties; radiotherapy of the abdomen and pelvis may
cause malabsorption, nausea, vomiting, and diarrhea.
Many clients undergoing radiotherapy feel profound
fatigue and anorexia (loss of appetite).
Health
An individual’s health status greatly affects eating habits
and nutritional status. Missing teeth, ill-fitting dentures,
or a sore mouth makes chewing food difficult. Difficulty
swallowing (dysphagia) due to a painfully inflamed throat
or a stricture of the esophagus can prevent an individual
from obtaining adequate nourishment. Disease processes
and surgery of the GI tract can affect digestion, absorption,
metabolism, and excretion of essential nutrients. GI and
other diseases also create nausea, vomiting, and diarrhea,
all of which can adversely affect an individual’s appetite
and nutritional status. Gallstones, which can block the
03/02/2021 18:20
1194
Unit 10
Promoting Physiologic Health
●
TABLE 46.1
Selected Drug–Nutrient Interactions
Drug
Effect on Nutrition
Acetylsalicylic acid (aspirin)
Decreases folic acid absorption when taken together orally.
Increases excretion of vitamin C, thiamine, potassium, amino acids, and glucose.
May cause nausea and gastritis.
Antacids containing aluminum or
magnesium hydroxide
Decrease absorption of phosphate and vitamin A.
Inactivate thiamine.
May cause deficiency of calcium and vitamin D.
Increase excretion of sodium, potassium, chloride, calcium, magnesium, zinc, and riboflavin.
Thiazide diuretics
May cause anorexia, nausea, vomiting, diarrhea, or constipation.
Decrease absorption of vitamin B12.
May cause diarrhea, nausea, or vomiting.
Potassium chloride
Increases excretion of potassium, magnesium, and calcium.
May cause anorexia, nausea, or vomiting.
Is incompatible with protein hydrolysates.
Laxatives
May cause calcium and potassium depletion.
Mineral oil and phenolphthalein (Ex-Lax) decrease absorption of vitamins A, D, E, and K.
Antihypertensives
Hydralazine may cause anorexia, vomiting, nausea, and constipation.
Methyldopa increases need for vitamin B12 and folate.
May cause dry mouth, nausea, vomiting, diarrhea, and constipation.
Anti-inflammatory agents
Colchicine decreases absorption of vitamin B12, carotene, fat, lactose, sodium, potassium, protein,
and cholesterol.
Prednisone decreases absorption of calcium and phosphorus.
Antidepressants
Amitriptyline increases food intake (large amounts may suppress intake).
Antineoplastics
Can cause nausea, vomiting, anorexia, malabsorption, and diarrhea.
Nutrient
Effect on Drugs
Grapefruit
Can cause toxicity when taken with a variety of medications including amiodarone, carbamazepine,
cisapride, cyclosporine, diazepam, nifedipine, saquinavir, statins, terfenadine, verapamil.
Vitamin K
Can decrease the effectiveness of warfarin (Coumadin).
Tyramine (found in aged cheeses,
tap beer, dried sausages, fermented
soy, sauerkraut)
In combination with monoamine oxidase inhibitor (MAOI) medications, e.g., isocarboxazid
(Marplan), isoniazid, linezolid, phenelzine, tranylcypromine, creates sudden increase in epinephrine
leading to headaches, increased pulse and blood pressure, and possible death.
Milk
Interferes with absorption of tetracycline antibiotics.
flow of bile, are a common cause of impaired lipid digestion. Metabolic processes can be impaired by diseases
of the liver. Diseases of the pancreas can affect glucose
metabolism or fat digestion. Autoimmune and genetic disorders such as celiac disease and irritable bowel syndrome
may be worsened when eating foods containing wheat or
gluten.
Between 30 million and 50 million Americans have
lactose intolerance (also called lactose maldigestion), a
shortage of the enzyme lactase, which is needed to break
down the sugar in milk. Certain populations are more
widely affected, especially African Americans, American Indians, Ashkenazi Jews, Asians, and Hispanics and
Latinos although they may not always show symptoms
(DeBruyne & Pinna, 2017).
Alcohol Consumption
The calories in alcoholic drinks include both those of the
alcohol itself and of the juices or other beverages added
to the drink. These can constitute large numbers of calories, for example, 150 calories for a regular 12-ounce beer,
and 160 calories for a “screwdriver” (1.5 ounces vodka
M46_BERM9793_11_GE_C46.indd 1194
plus 4 ounces orange juice). Drinking alcohol can lead
to weight gain by adding these calories to the regular
diet plus the effect of alcohol on fat metabolism. A small
amount of the alcohol is converted directly to fat. However, the greater effect is that the remainder of the alcohol
is converted into acetate by the liver. The acetate released
to the bloodstream is used for energy instead of fat and
the fat is then stored.
Excessive alcohol use contributes to nutritional
deficiencies in several ways. Alcohol may replace food
in an individual’s diet, and it can depress the appetite.
Excessive alcohol can have a toxic effect on the intestinal mucosa, thereby decreasing the absorption of
nutrients. The need for vitamin B increases, because it
is used in alcohol metabolism. Alcohol can impair the
storage of nutrients and increase nutrient catabolism
and excretion.
Several studies have shown health benefits of moderate alcohol consumption such as with red wine. Examples
include reduced risk of cardiovascular disease, strokes,
dementia, diabetes, and osteoporosis. However, any benefits of alcohol must be weighed against the many harmful
effects, and the possibility of alcohol abuse.
03/02/2021 18:20
Chapter 46
Advertising
Food producers try to persuade consumers to change from
the product they currently use to the brand of the producer.
Popular actors are often used in television, radio, Internet,
and print to influence consumers’ choices. Advertising is
thought to influence individuals’ food choices and eating patterns to a certain extent. Of note is that such products as alcoholic beverages, coffee, frozen foods, and soft
drinks are more heavily advertised than such products
as bread, vegetables, and fruits. Convenience foods (frozen or packaged and easy to prepare) and take-out (fast)
foods are heavily advertised. Children’s television show
commercials often promote snack foods, candy, soda, and
sugared cereals over fresh, healthy foods. Australia, Canada, Sweden, and Great Britain have adopted regulations
prohibiting food advertising on programs targeting audiences of young children.
There has been an increase in advertising that targets
older adults in particular and encourages use of herbs
and supplements. Some products are nutritionally safe,
whereas others are not and can cause interactions with
medications they might be taking or cause unexpected
side effects. The cost of some of these supplements is also
usually high, is generally not covered by health insurance,
and may take money that the individual could spend for
healthier food.
Psychologic Factors
Although some people overeat when stressed, depressed,
or lonely, others eat very little under the same conditions.
Anorexia and weight loss can indicate severe stress or
depression. Anorexia nervosa and bulimia are severe psychophysiologic conditions seen most frequently in female
adolescents.
Nutritional Variations
Throughout the Lifecycle
Nutritional requirements vary throughout the lifecycle.
Guidelines follow for the major developmental stages.
Neonate to 1 Year
The neonate’s fluid and nutritional needs are met by
breast milk or formula. Fluid needs of infants are proportionately greater than those of adults because of a higher
metabolic rate, immature kidneys, and greater water
losses through the skin and the lungs. Therefore, fluid
balance is a critical factor. Under normal environmental
conditions, infants do not need additional water beyond
that obtained from breast or bottle formula feedings; however, neonates in very warm environments may require
additional fluids.
The total daily nutritional requirement of the newborn is about 80 to 100 mL of breast milk or formula per
M46_BERM9793_11_GE_C46.indd 1195
●
Nutrition
1195
kilogram of body weight. The newborn infant’s stomach
capacity is about 90 mL, and feedings are required every
2 1/2 to 4 hours.
The newborn infant is usually fed “on demand.”
Demand feeding means that the child is fed when hungry rather than on a set time schedule. This method tends
to decrease the problem of overfeeding or underfeeding
the infant. The newborn who is hungry usually cries and
exhibits tension in the entire body. During feeding, the
infant sucks readily and needs burping after each ounce
of formula or after 5 minutes of breastfeeding.
Infants demonstrate satiety (fullness) by slowing their
sucking activity or by falling asleep. Infants should not
be coaxed into finishing the feeding. This could lead to
discomfort or overfeeding. When feeding is completed,
healthy infants can be placed in a supine position for sleep
during the first 6 months of life to reduce the risk of sudden infant death syndrome (SIDS).
Regurgitation, or spitting up, during or after a feeding
is a common occurrence during the first year. Although
this may concern parents, it does not usually result in
nutritional deficiency. Demonstration of adequate weight
gain should reassure parents that the infant is receiving
adequate nutrition.
Adding solid food to the diet usually takes place
between 4 and 6 months of age. Six-month-old infants can
consume solid food more readily because they can sit up,
can hold a spoon, and have decreased sucking and tongue
protrusion reflexes. Solid foods (strained or pureed) are
generally introduced in the following order: cereals (rice
before oat and wheat), fruits, vegetables (yellow before
green), and strained meats. Foods are introduced one at a
time, usually with only one new food introduced every 5
days to ensure that the infant tolerates the food and demonstrates no allergy to it. This sequence can vary according to cultural preferences. With the eruption of teeth at
about 7 to 9 months, the infant is ready to chew and can
experience different textures of food. At this time, the
infant enjoys finger foods, such as skinless fruit cut into
small pieces to prevent choking, dry cereal, or toast.
Because honey can contain spores of Clostridium botulinum and this has been a source of infection (and death)
for infants, children less than 12 months old should not be
fed honey. According to the Centers for Disease Control
and Prevention (CDC) (2017), honey is safe for children
1 year of age and older.
At about 6 months of age, infants require iron supplementation to prevent iron deficiency anemia. Iron deficiency anemia is a form of anemia (decrease in red blood
cells) caused by inadequate supply of iron for synthesis
of hemoglobin. Cow’s milk is low in iron and, thus, ironfortified cereals or formulas are usually recommended by
6 months of age and are continued until the child reaches
18 months.
Weaning from the breast or bottle to the cup takes
place gradually and is usually achieved by 12 to
24 months of age. It is recommended that infants be
breastfed exclusively for 6 months and then until 1 year
03/02/2021 18:20
1196
Unit 10
●
Promoting Physiologic Health
of age or longer as desired (Spatz, 2017). Some infants
have difficulty giving up the bottle, particularly at naptime or bedtime. Parents should be warned that having
the bottle in bed could lead to bottle mouth syndrome.
The term describes decay of the teeth caused by constant contact with sweet liquid from the bottle. Some
dentists advocate brushing or cleaning the infant’s teeth
to prevent bottle mouth syndrome, especially for the
infant who requires a bottle only at naptime or bedtime.
Weaning from the bottle can be facilitated by diluting
the formula with water increasingly until the infant is
drinking plain water. By the age of 1, most infants can
be completely fed on table food, and milk intake is about
20 ounces per day.
Toddler
Because of a maturing GI tract, toddlers can eat most
foods and adjust to three meals each day. Toddlers’ fine
motor skills are sufficiently well developed for them to
learn how to feed themselves. Before the age of 20 months,
most toddlers require help with glasses and cups because
their wrist control is limited. By age 3, when most of the
deciduous teeth have emerged, the toddler can bite and
chew adult table food.
Developing independence may be exhibited through
the toddler’s refusal of certain foods. Meals should be
short because of the toddler’s brief attention span and
environmental distractions. Often toddlers display their
liking of rituals by eating foods in a certain order, cutting
foods a specific way, or accompanying certain foods with
a particular drink.
The toddler is less likely to have fluid imbalances than
the infant. The toddler’s GI function is more mature, and
the percentage of fluid body weight is lower. A healthy
toddler weighing 15 kg (33 lb) needs about 1250 mL of
fluid per 24 hours.
During the toddler stage, the caloric requirement is
1000 to 1400 Kcal/day. From 1 to 2 years of age, the toddler may eat a combination of prepared toddler foods and
some table foods. Parents should be instructed to read
labels carefully and be aware that table foods offer more
variety and are less expensive and more nutritious than
prepared toddler foods. The need for adequate iron, calcium, and vitamins C and A, which are common toddler
deficiencies, should also be discussed.
The following suggestions may help parents meet
the child’s nutritional needs and promote effective
parent–child interactions: (a) Make mealtime a pleasant
time by avoiding tensions at the table and discussions
of bad behavior; (b) offer a variety of simple, attractive foods in small portions; (c) do not use food as a
reward or punish a child who does not eat; (d) schedule
meals, sleep, and snack times that will allow for optimal
appetite and behavior; and (e) avoid routinely serving
sweet desserts. Many children show dislike of particular foods. In some cases, this may be a natural mechanism to protect the child from food allergies. When in
M46_BERM9793_11_GE_C46.indd 1196
doubt, the child should be evaluated by a professional
for food allergies (DeBruyne & Pinna, 2017).
Preschooler
The preschooler eats adult foods. Parents should become
informed about the diet of their child in day care or preschool settings so that they can ensure that the child’s
total nutritional needs are being met. Children at this age
are very active and may rush through meals to return
to playing. Active children often require snacks between
meals. Cheese, fruit, yogurt, raw vegetables, and milk
are good choices. The 4-year-old still requires parents’
help in cutting meat and may spill milk when pouring
from a large container. Parents also need to teach the preschooler how to use utensils and should provide them
with the opportunity to practice (e.g., buttering bread).
However, 4- and 5-year-olds often use their fingers to
pick up food. Children at this age may enjoy helping in
the kitchen, and both girls and boys should be encouraged to do so.
The preschooler is even less at risk than the toddler
for fluid imbalances. The average 5-year-old weighing
20 kg (45 lb) requires at least 75 mL of liquid per kilogram
of body weight per day, or 1500 mL every 24 hours.
School-Age Child
School-age children require a balanced diet including
approximately 1600 to 2200 Kcal/day. They can eat three
meals a day and one or two nutritious snacks. Children
need a protein-rich food at breakfast to sustain the prolonged physical and mental effort required at school.
Children who skip breakfast become inattentive and restless by late morning and have decreased problem-solving
ability. Undernourished children become fatigued easily
and face a greater risk of infection, resulting in frequent
absences from school.
The average healthy 8-year-old weighing 30 kg
(66 lb) requires about 1750 mL of fluid per day. Many
school-age children have only one meal a day with
their family, at dinner. Mealtime should be a social time
enjoyed by all, and parents should encourage good eating habits. Parents should be aware that children learn
many of their food habits by observing their parents.
Eating a balanced diet should be the norm for both parent and child.
The school-age child generally eats lunch at school.
The child may bring lunch from home or get lunch at the
school. Many dietary problems stem from this independence in food choices. Children may trade their food,
not eat lunch at all, or buy sweets or junk food with their
lunch money. Parents should discuss with the child the
foods that they should eat and continue to provide a balanced diet in the home setting.
Poor eating habits may cause obesity. Childhood
obesity is an increasing problem. More than 23% of
American children ages 2 to 18 are at or above the
03/02/2021 18:20
Chapter 46
95% for BMI (Ogden et al., 2016). Obesity in schoolage children tends to result in adult obesity and all the
related health risks. It is both caused by and results in
decreased activity and psychosocial problems. Obese
children may be ridiculed and discriminated against
by peers. Such behavior reinforces low self-esteem.
The CDC’s Division of Adolescent and School Health
has established many programs to address both prevention and treatment of childhood obesity. The goal of
treatment for children who are overweight is to reduce
weight gain, allowing their weight to increase more
slowly than their height. Counseling and teaching for
parents should include the following:
•
•
•
•
Reviewing the child’s eating habits, including snacks
Altering meal content
Using rewards other than food
Promoting regular exercise.
Adolescent
The adolescent’s need for nutrients and calories increases,
particularly during the growth spurt. In particular, the
need for protein, calcium, vitamin D, iron, and B vitamins increases during adolescence. An adequate diet for
an adolescent is 1 quart of milk per day and appropriate
amounts of meat, vegetables, fruits, breads, and cereals.
Calcium intake during adolescent years (1200 to 1500 mg/
day) may help decrease osteoporosis (a decrease in bone
density) in later life. Peak bone mineralization occurs on
average at 12.5 years in girls and 14.0 years in boys when
40% of total adult bone mass is accumulated. The majority
of adolescent females do not get enough calcium in their
diets (Rolfes, Pinna, & Whitney, 2018).
Many parents observe that teenagers, particularly
boys, seem to eat all the time. Teenagers have active lifestyles and irregular eating patterns. They tend to diet or
snack frequently, often eating high-calorie foods such as
soft drinks, ice cream, and fast foods. Parents and nurses
can promote better lifelong eating habits by encouraging teenagers to eat healthy snacks. Parents can provide
healthy snacks such as fruits and cheese and limit the junk
food available in the home. The teenager’s food choices
relate to physical, social, and emotional factors and
impulses and may not be influenced by teaching. Nurses
need to advise parents to help adolescents take responsibility for their decisions in many areas of life, and to avoid
conflicts that relate to food.
Common problems related to nutrition and selfesteem among adolescents include obesity, anorexia
nervosa, and bulimia. Obesity continues to be a problem in the adolescent period. Depression is not unusual
among adolescents who are obese. Treatment of obesity
in this age group includes education on nutrition and
assessment of psychosocial problems that may produce
overeating.
Under social pressure to be slim, some adolescents
severely limit their food intake to a level significantly
M46_BERM9793_11_GE_C46.indd 1197
●
Nutrition
1197
below that required to meet the demands of normal
growth. Sometimes, the adolescent may develop an
eating disorder, such as anorexia or bulimia. These disorders are considered to be related to the need for control. Anorexia nervosa is characterized by a prolonged
inability or refusal to eat, rapid weight loss, and emaciation in individuals who continue to believe they are
fat. Individuals with anorexia may also induce vomiting
and use laxatives and diuretics to remain thin. Bulimia
is an uncontrollable compulsion to consume enormous
amounts of food (binge) and then expel it by selfinduced vomiting or by taking laxatives (purge). These
illnesses are most effectively treated in the early stages
by psychotherapy. Hospitalization may be necessary
when the effects of starvation become life threatening.
Young Adult
Many young adults are aware of food groups but may not
be knowledgeable about how many servings they need or
how much a serving constitutes. The nurse should provide the young adult client with resources such as a chart
or list that contains the foods and the amounts needed in
each group.
Young adult females need to maintain adequate
iron intake. Many do not ingest sufficient dietary iron
each day. To prevent iron deficiency anemia, menstruating females should ingest 18 mg of iron daily. The nurse
should instruct the female client to include iron-rich
foods, such as organ meats (liver and kidneys), eggs,
fish, poultry, leafy vegetables, and dried fruits, in her
daily diet. In addition, the World Health Organization
(WHO) recommends folate (folic acid) supplements
for all women of childbearing ability. Because folate
can prevent neural tube defects in the fetus but must
be taken prior to and during the early portion of the
pregnancy, the United States and more than 50 other
countries have mandated folic acid supplementation of
enriched grain products.
Calcium is needed in young adulthood to maintain
bones and help decrease the chances of developing osteoporosis in later life. Along with calcium, the individual
must have adequate vitamin D, necessary for the calcium
to enter the bloodstream. Vitamin D is made in the skin
on exposure to the sun. If the individual does not get sufficient sun exposure (15 minutes three times each week),
supplements may be indicated.
Obesity may occur during the young adult years as
the active teen becomes the sedentary adult but does not
decrease caloric intake. The young adult who is overweight or obese is at risk for hypertension, a major health
problem for this age group.
Hypertension and obesity are 2 of more than 40 risk
factors identified in the development of cardiovascular
(CV) disease. Preventing these risk factors and lowering
the risk of CV disease are critical. Low-fat and lowcholesterol diets play a significant role in both the
prevention and treatment of CV disease.
03/02/2021 18:20
1198
Unit 10
●
Promoting Physiologic Health
DRUG CAPSULE
Mineral: ferrous sulfate (Slow-Fe, Feosol), ferrous gluconate (Fergon)
CLIENT WITH IRON DEFICIENCY ANEMIA
Iron is required for the formation of red blood cells. When iron stores
are low, the body cannot produce enough red blood cells and
anemia can develop. Symptoms of iron deficiency anemia include
fatigue, listlessness, anorexia, and pallor. Although iron deficiency
anemia is not the only kind of anemia, it is possibly the most common and one of the easiest to treat. Immediate and timed-release
forms are available.
NURSING RESPONSIBILITIES
• Administer on an empty stomach, 1 hour before or 2 hours after
meals, with a full glass of water. If the client experiences gastric
upset, administer with or after food. The immediate-release
formulation is administered up to three times per day.
• Vitamin C increases absorption of iron from the stomach. Some
preparations contain both iron and vitamin C.
• Administer at least 2 hours apart from antacids, ciprofloxacin,
tetracycline, and several other medications. Consult a drug
handbook for possible drug interactions.
• Liquid forms should be diluted in a glass of water or juice and
sipped through a straw to prevent staining of the teeth.
• Shake suspension forms well before each use; take with a full
glass of water.
Middle-Aged Adult
The middle-aged adult should continue to eat a healthy
diet, following the recommended portions of the food
groups, with special attention to protein and calcium
intake, and limiting cholesterol and caloric intake. Two or
three liters of fluid should be included in the daily diet.
Postmenopausal females need to ingest sufficient calcium
and vitamin D to reduce osteoporosis, and antioxidants
such as vitamins A, C, and E may be helpful in reducing
the risks of heart disease in women. Although iron supplements are no longer needed, the amount in a multivitamin
is not harmful.
Middle-aged adults who gain weight may not be
aware of some common facts about this age period.
Decreased metabolic activity and decreased physical
activity mean a decrease in caloric need. The nurse’s role
in nutritional health promotion is to counsel clients to
prevent obesity by reducing caloric intake and participating in regular exercise. Clients should also be warned
that being overweight is a risk factor for many chronic
diseases, such as diabetes and hypertension, and for problems of mobility, such as arthritis.
For the client who requires additional resources, a
variety of programs is frequently available. Most programs use behavior modification techniques and group
support to assist clients in reaching their goals. Clients
should seek medical advice before considering any major
changes in their diets.
M46_BERM9793_11_GE_C46.indd 1198
•
Iron comes in different dose strengths and may require adjustment for optimal effect.
CLIENT AND FAMILY TEACHING
• Take the medication on an empty stomach, 1 hour before or
2 hours after meals, with a full glass of water. If upset stomach
occurs, take with or after food, but not with coffee, tea, eggs,
or milk because these decrease absorption. Do not lie down
for 30 minutes after taking the tablet or capsule.
• Sustained-release capsules and tablets must be swallowed
whole. Do not crush or chew them because side effects may
be increased.
• Common side effects may include nausea, stomach cramps,
vomiting, and constipation. These should decrease within a
few days even while continuing the iron.
• Stools will turn green-black, and this is normal.
• Do not stop taking the medication, even if you feel stronger.
• Do not take iron without consulting the primary care provider
if you have a history of intestinal problems.
• Store at room temperature, away from moisture and sunlight.
Keep away from children. Accidental overdose can be fatal.
Note: Prior to administering any medication, review all aspects with a current drug handbook
or other reliable source.
During late middle age, gastric juice secretions and
free acid gradually decline. Some individuals may complain of “heartburn” (acid indigestion) or an increase in
belching. They may determine that certain foods disagree
with them. Clients should be advised to develop sensible
eating habits and avoid fried or fatty foods.
Older Adults
The older adult requires the same basic nutrition as the
younger adult. However, fewer calories are needed by
older adults because of the lower metabolic rate and the
decrease in physical activity.
Some older adults may need more carbohydrates for
fiber and bulk, but most nutrient requirements remain
relatively unchanged. Such physical changes as tooth loss
and impaired sense of taste and smell may affect eating
habits. Decreased saliva and gastric juice secretion may
also affect the older adult’s nutrition.
Psychosocial factors may also contribute to nutritional
problems. Some older adults who live alone do not want
to cook for themselves or eat alone. They may adopt poor
dietary habits. Other factors, such as lack of transportation,
poor access to stores, and inability to prepare the food also
affect nutritional status. Loss of spouse, anxiety, depression,
dependence on others, and lowered income all affect eating
habits (Table 46.2). Guidelines to include high-nutrient foods
compatible with the nutritional needs of older adults are summarized in Client Teaching. Also see Lifespan Considerations.
03/02/2021 18:20
Chapter 46
TABLE 46.2
●
Nutrition
1199
Problems Associated with Nutrition in Older Adults
Problems
Nursing Interventions
Difficulty chewing
Encourage regular visits to the dentist to have dentures repaired, refitted, or replaced.
Chop fruits and vegetables; shred green, leafy vegetables; select ground meat, poultry, or fish.
Lowered glucose tolerance
Eat more complex carbohydrates (e.g., breads, cereals, rice, pasta, potatoes, and legumes) rather
than sugar-rich foods.
Decreased social interaction,
loneliness
Promote appropriate social interaction at meals, when possible.
Encourage the client and family to take an interest in food preparation and serving, perhaps as an
activity they can do together.
Encourage family or caregivers to present the food at a dining table with other people.
If food preparation is not possible, suggest community resources, such as Meals on Wheels.
Suggest inviting friends over for meals.
Loss of appetite and senses of
smell and taste
Eat essential, nutrient-dense foods first; follow with desserts and low-nutrient-density foods.
Review dietary restrictions, and find ways to make meals appealing within these guidelines.
Eat small meals frequently instead of three large meals a day.
Limited income
Suggest using generic brands and coupons.
Substitute milk, dairy products, and beans for meat.
Avoid convenience foods if able to cook. Buy foods that are on sale and store for future use.
Suggest community resources and nutrition programs.
Difficulty sleeping at night
Have the major meal at noon instead of in the evening.
Avoid tea, coffee, or other stimulants in the evening.
CLIENT TEACHING Nutrition for Older Adults
Include each food group on MyPlate. For example, a 65-yearold female of average height and weight who performs less
than 30 minutes of exercise per day requires 1600 Kcal consisting of the following:
Grains: 5 ounces
Vegetables: 2 cups
Fruits: 1.5 cups
Milk, yogurt, or cheese: 3 cups
Meat or beans: 5 ounces
• Reduce caloric intake. Caloric needs generally decrease in older
adults often because of decreased activity. Older adults need to
consume nutrient-dense foods and avoid foods that are high in
calories but have few nutrients.
• Reduce fat consumption. Use leaner cuts of meat, and limit
portions to 4 to 6 oz per day. (Be sure intake of protein is sufficient, because older adults often consume inadequate amounts
of these foods.) Broil, boil, or bake foods instead of frying them.
Use low-fat milk and cheese; limit intake of butter, margarine,
and salad dressings.
• Reduce consumption of empty calories. Substitute fruit or
puddings made with low-fat milk in place of pastry, cookies,
and rich desserts.
•
•
•
•
•
•
Reduce sodium consumption for clients who have hypertension or other cardiac problems. Avoid canned soups, ketchup,
and mustard that are high in sodium (not all are). Avoid salted,
smoked, cured, and pickled meats (e.g., ham and bacon), poultry, and fish. Do not add salt when cooking foods or at the table.
Ensure adequate calcium intake (at least 800 mg) to prevent
bone loss. Milk, cheese, yogurt, cream soups, puddings, and
frozen milk products are good sources.
Ensure adequate vitamin D intake. Vitamin D is essential to
maintain calcium homeostasis. Include some milk, because
other dairy products are not usually fortified with vitamin D.
If milk cannot be tolerated because of a lactose deficiency,
provide vitamin supplements.
Ensure adequate iron intake. Iron intake in older adults may
be compromised by such factors as increased incidence of GI
disturbance, chronic diarrhea, regular aspirin use, and possible
reduction in meat consumption.
Consume fiber-rich foods to prevent constipation and minimize
use of laxatives. Because fiber-rich foods provide bulk and a
feeling of fullness, they help clients control their appetites and
lose weight. Examples are bran and beans. Some clients may
also require fiber supplements such as insoluble bulk-forming
or soluble fiber products.
LIFESPAN CONSIDERATIONS Nutrition
CHILDREN
• Children learn eating habits from their parents. It is the parents’
responsibility to be good nutritional role models, both in terms of
what they eat and how they incorporate food into their lifestyle.
• During the preschool and early school-age years, children learn
lifelong eating habits. It is the parents’ responsibility to provide the child with adequate amounts of nutritious foods in an
environment that is relaxed and comfortable for eating. It is the
child’s responsibility to decide what and how much of the nutritious foods to eat. Parents should be counseled that eating can
become a source of conflict if the parent tries to tell the child what
and how much to eat, or if the child tries to tell the parent what
foods should be eaten. Children’s access to “junk food” should be
limited, but completely forbidding a food may also create conflict.
• Adolescents who are vegans or vegetarians are at risk for some
nutritional deficits.
Continued on page 1200
M46_BERM9793_11_GE_C46.indd 1199
03/02/2021 18:20
1200
Unit 10
●
Promoting Physiologic Health
LIFESPAN CONSIDERATIONS Nutrition—continued
OLDER ADULTS
Most older adults take several medications. Considerations for
potential problems include the following:
• Some foods interact adversely or decrease the effectiveness
of certain medications, such as foods high in vitamin K and
the anticoagulant warfarin (Coumadin). Older adults should not
change their diet significantly without consulting the healthcare
provider since drug dosage may have been based on the older
adult’s previous dietary intake.
• Some medications increase appetite, such as glucocorticoids.
• Some medications decrease appetite by their actions or by
causing an unpleasant taste.
• Certain tablets should not be crushed to be given by mouth
or by gastric tubes, such as enteric-coated or slow-release
medications.
Conditions such as neuromuscular disorders and dementia
can make it difficult for older adults to eat or to be fed. Safety
should always be a priority concern with attention paid to prevent
Standards for a Healthy Diet
Various daily food guides have been developed to help
healthy individuals meet the daily requirements of essential nutrients and to facilitate meal planning. Food group
plans emphasize the general types or groups of foods
rather than the specific foods, because related foods are
similar in composition and often have similar nutrient
values. For example, all grains, whether wheat or oats,
are significant sources of carbohydrate, iron, and the
B vitamin thiamine. Food guides currently used include
2015–2020 Dietary Guidelines for Americans (2015) and the
U.S. Department of Agriculture’s (USDA’s) MyPlate.
Dietary Guidelines for Americans
This guide is published by the USDA every 5 years, and
the 2015–2020 edition contains recommendations for the
total diet that allows food choices that result in a nutrientrich and calorie-balanced intake. Key points of the latest
dietary guidelines follow:
•
•
•
•
•
•
•
Shift to more plant-based foods such as vegetables,
fruits, grains, beans, and nuts.
Significantly reduce foods with added sugars and solid
fats.
Engage in regular physical activity.
Consume foods, including milk products, each day that
increase commonly insufficient nutrients: vitamin D,
calcium, potassium, and fiber.
Keep daily total fat intake within 20% to 35% of total
calories, less than 10% from saturated fatty acids and
less than 300 mg cholesterol. (See also Client Teaching
for ways to reduce fat intake.)
Consume less than 2300 mg of sodium per day.
If you drink alcohol, do so in moderation (one drink
per day for women and two drinks per day for men).
These dietary recommendations are intended to help
achieve the nutritional goals stated in Healthy People 2020
M46_BERM9793_11_GE_C46.indd 1200
aspiration. All healthcare personnel and family caregivers should be
taught proper techniques to reduce this risk. Effective techniques
include:
• Use the chin-tuck method when feeding clients with dysphagia.
Have them flex the head toward the chest when swallowing to
decrease the risk of aspiration into the lungs.
• Use foods of prescribed consistency. Many older adults can
swallow foods with thicker consistency more easily than thin
liquids.
• Try to focus on food preferences—the family can help provide
this information.
• Try to maintain mealtime as a positive social occasion with conversations and extra attention to having a pleasant environment.
Economic factors may influence older adults’ nutritional status if they
cannot afford food, especially if a prescribed diet requires expensive
supplements. Inexpensive or convenience foods such as canned
soups are often high in fat and sodium.
(U.S. Department of Health and Human Services, 2019).
Those goals include 22 specific nutritional objectives, such
as the following:
Reduce the incidence of obese adults (target = 30.5%)
and children ages 2 to 19 (target = 14.5%).
Increase the proportion of individuals ages 2 years and
older who consume no more than 2300 mg of sodium
daily.
Prevent inappropriate weight gain in youth and adults.
Reduce consumption of calories from solid fats
(target = 14.2%) and added sugars in the population
ages 2 years and older (target = 9.7%).
•
•
•
•
MyPlate
In May 2011, First Lady Michelle Obama introduced the
MyPlate icon as a simple reminder of how to implement
the dietary guidelines. This depiction and the website that
CLIENT TEACHING Reducing Dietary Fat
•
•
•
•
•
•
•
•
•
•
•
•
Cook meat by grilling, baking, broiling, or microwaving rather
than frying.
Substitute popcorn or pretzels for such snacks as potato
chips, cheese puffs, and corn chips.
Read labels. Some crackers, for example, are high in fat;
others are not.
Limit desserts high in fat, such as ice cream, cake, and
cookies.
Substitute hard candies for chocolate bars.
Use skim or reduced-fat milk instead of whole milk, for drinking
as well as in recipes.
Use less butter or margarine on breads.
Remove fat from meat and skin from chicken before cooking.
Eat less meat; eat more fish.
Use less dressing, or use low-fat dressings, on salads.
Eat plant sources of protein (e.g., kidney, lima, and navy beans).
Use nuts as a source of protein, but since they are high in fat,
use to replace meat rather than in addition.
03/02/2021 18:20
Chapter 46
accompanies it promote getting more fruits and vegetables, whole grains, and low-fat dairy foods into the diet
(Figure 46.1 ■).
Using and following the guide does not guarantee
that an individual will consume the necessary levels of all
essential nutrients. For example, someone who chooses
cooked and low-fiber fruits and vegetables might not have
an adequate intake of dietary fiber even though the recommended number of servings is eaten. However, the food
guide is easy to follow, and individuals who eat a variety
of foods from each group, in the suggested amounts, are
likely to come close to recommended nutrient levels.
Recommended Dietary Intake
The Committee on the Scientific Evaluation of Dietary
Reference Intakes of the Institute of Medicine publishes
dietary reference intakes (DRIs) tables, which contain
four sets of reference values: estimated average requirements (EARs), recommended dietary allowances (RDAs),
adequate intakes (AIs), and tolerable upper intake levels
(ULs). Definitions of these terms are found in Box 46.3.
The values for RDAs and AIs in the tables are modified for
different age groups and according to gender. The effect of
illness or injury (increasing the need for nutrients) and the
variability among individuals within any given subgroup
are not taken into account in the DRIs.
Consumers most commonly learn recommended
dietary intake information from the U.S. Food and Drug
Administration (FDA) nutrition labels. Food labeling is
required for most prepared foods, such as breads, cereals, canned and frozen foods, snacks, desserts, and drinks.
Nutrition labeling for raw produce (fruits and vegetables)
and fish is voluntary. Everyone must learn how to read
and interpret these labels.
In Figure 46.2 ■, the section at the top of the label ❶
indicates serving size and number of servings in the container. The remaining information on the label indicates
the values for each serving. Serving sizes were updated
●
Nutrition
1201
to be more realistic in 2018. If the individual consumes
a container that has more than one serving, he or she
must multiply the values to determine the real nutrient
content. The next section ❷ indicates the number of total
BOX 46.3
Definitions for Dietary Reference
Value Tables
Dietary reference intakes (DRIs) are the standards for nutrient
recommendations that include the following values:
Recommended dietary allowance (RDA): the average daily
nutrient intake level sufficient to meet the nutrient requirement
of nearly all (97% to 98%) healthy individuals in a particular life
stage and gender group
• Adequate intake (AI): used when RDA cannot be determined;
a recommended average daily nutrient intake level based on
observed or experimentally determined approximations or
estimates of nutrient intake for a group (or groups) of healthy
individuals that are assumed to be adequate
• Tolerable upper intake level (UL): the highest average daily
nutrient intake level likely to pose no risk of adverse health
effects to almost all individuals in a particular life stage and
gender group. As intake increases above the UL, the potential
risk of adverse health effects increases.
•
Source: Nutrient Recommendations: Dietary Reference Intakes, National Institutes of
Health Office of Dietary Supplements, n.d. Retrieved from https://ods.od.nih.gov/Health_
Information/Dietary_Reference_Intakes.aspx
Nutrition Facts
1 8 servings per container
Serving size
2/3 cup (55g)
2 Amount per serving
Calories
230
% Daily Value*
3 Total Fat 8g
Saturated Fat 1g
Trans Fat 0g
Cholesterol 0mg
Sodium 160mg
Total carbohydrate 37g
Dietary Fiber 4g
Total Sugars 12g
4
Includes 10g Added Sugars
10%
5%
0%
7%
13%
14%
20%
Protein 3g
5 Vitamin D 2mcg
10%
Calcium 200mg
15%
Iron 8mg
45%
Potassium 235mg
6
Figure 46.1 ■ MyPlate illustrates the five food groups using a familiar
mealtime visual, a place setting.
From U.S. Department of Agriculture, 2013.
M46_BERM9793_11_GE_C46.indd 1201
6%
* The % Daily Value (DV) tells you how much a
nutrient in a serving of food contributes to a daily diet.
2,000 calories a day is used for general nutrition advice.
Figure 46.2 ■ The Nutrition Facts label.
From The New and Improved Nutrition Facts Label—Key Changes, by the U.S. Food and Drug
Administration, 2018. Retrieved from https://www.fda.gov/files/food/published/The-New-andImproved-Nutrition-Facts-Label-%E2%80%93-Key-Changes.pdf
03/02/2021 18:20
1202
Unit 10
●
Promoting Physiologic Health
calories per serving. Based on a 2000-calorie diet, a serving
with 100 calories is considered moderate and 400 calories
high. Section ❸ has nutrients that should be minimized:
both saturated and trans fats. Trans fats are created when
unsaturated oils are hydrogenated to create a solid form
and are used in frying foods, margarine, and many snack
products. They are also present in meat and dairy fats.
Trans fats have been shown to increase cholesterol and
contribute to heart disease. In section ❹, the manufacturer
must list added sugar in addition to the total carbohydrates, fiber, and total sugars. It is considered difficult to
stay within calorie limits consuming more than 10 percent
of total daily calories from added sugar. The next section
❺ includes the actual values of the vitamins and minerals
most commonly insufficient in American diets. In 2018,
vitamins A and C were removed from the label, potassium
and vitamin D were added, and the daily value (DV) of
calcium and iron were updated. The footnote ❻ indicates
that the DV shows the percent of a typical individual’s
daily requirement of that component contained in each
serving. When adding the percent values from all foods
eaten in one day, the goal is for the total DV of each of
these to be at least 100%.
Vegetarian Diets
Individuals may become vegetarians for economic, health,
religious, ethical, or ecologic reasons. There are two basic
vegetarian diets: those that use only plant foods (vegan)
and those that include milk, eggs, or dairy products. Some
individuals eat fish and poultry but not beef, lamb, or
pork; others eat only fresh fruit, juices, and nuts; and still
others eat plant foods and dairy products but not eggs.
Vegetarian diets can be nutritionally sound if they
include a wide variety of foods and if proper protein
and vitamin and mineral supplementation are provided.
Because the proteins found in plant foods are incomplete
proteins, vegetarians must eat complementary protein
foods to obtain all of the essential amino acids. A plant
protein can be complemented by combining it with a different plant protein. The combination produces a complete protein (Box 46.4). Obtaining complete proteins is
especially important for growing children and pregnant
and lactating women, whose protein needs are high.
Generally, legumes (starchy beans, peas, lentils) have
complementary relationships with grains, nuts, and
seeds. Complementary foods must be eaten in the same
meal. Diets such as the fruitarian diet do not provide
sufficient amounts of essential nutrients and are not recommended for long-term use.
Foods of animal origin are the best source of vitamin B12. Therefore, vegans need to obtain this vitamin
from other sources: brewer’s yeast, foods fortified with
vitamin B12, or a vitamin supplement. Because iron from
plant sources is not absorbed as efficiently as iron from
meat, vegans should eat iron-rich foods (e.g., green
leafy vegetables, whole grains, raisins, and molasses)
M46_BERM9793_11_GE_C46.indd 1202
BOX 46.4
Combinations of Plant Proteins That
Provide Complete Proteins
Grains plus legumes = complete protein.
Legumes plus nuts or seeds = complete protein.
Grains, legumes, nuts, or seeds plus milk or milk products
1e.g., cheese2 = complete protein.
Grains
Legumes
Nuts and Seeds
Brown rice
Black beans
Almonds
Barley
Kidney beans
Brazil nuts
Corn meal
Lima beans
Cashews
Millet
Soybeans
Pecans
Oats/oatmeal
Lentils
Walnuts
Rye
Tofu
Pumpkin seeds
Whole wheat
Black-eyed peas
Sesame seeds
Split peas
Sunflower seeds
Examples
Black-eyed peas and rice
Lentil soup and whole-wheat bread
Beans and tortillas
Lima beans and sesame seeds
Cereal with milk
Macaroni with cheese
and iron-enriched foods. They should eat a food rich in
vitamin C at each meal to enhance iron absorption. Calcium deficiency is a concern only for strict vegetarians.
It can be prevented by including in the diet soybean milk
and tofu (soybean curd) fortified with calcium and leafy
green vegetables.
Altered Nutrition
Malnutrition is commonly defined as the lack of neces-
sary or appropriate food substances, but in practice
includes both undernutrition and overnutrition.
Overnutrition refers to a caloric intake in excess of daily
energy requirements, resulting in storage of energy in
the form of adipose tissue. As the amount of stored
fat increases, the individual becomes overweight or
obese. An individual is said to be overweight when the
BMI is between 25 and 29.9 kg>m2 and obese when
the BMI is greater than 30 kg>m2 (National Heart, Lung,
and Blood Institute, n.d.).
Excess body weight increases the stress on body
organs and predisposes individuals to chronic health
problems such as hypertension and diabetes mellitus.
Obesity that interferes with mobility or breathing is
referred to as morbid obesity. Obese individuals may also
manifest undernourishment in important nutrients (e.g.,
essential vitamins or minerals) even though excess calories are ingested.
03/02/2021 18:20
Chapter 46
Undernutrition refers to an intake of nutrients insufficient to meet daily energy requirements because of
inadequate food intake or improper digestion and
absorption of food. An inadequate food intake may be
caused by the inability to acquire and prepare food,
inadequate knowledge about essential nutrients and a
balanced diet, discomfort during or after eating, dysphagia, anorexia, nausea, vomiting, and so on. Improper
digestion and absorption of nutrients may be caused
by an inadequate production of hormones or enzymes
or by medical conditions resulting in inflammation or
obstruction of the GI tract.
Inadequate nutrition is associated with marked
weight loss, generalized weakness, altered functional
abilities, delayed wound healing, increased susceptibility to infection, decreased immunocompetence, impaired
pulmonary function, and prolonged length of hospitalization. In response to undernutrition, carbohydrate reserves,
stored as liver and muscle glycogen, are mobilized. However, these reserves can only meet energy requirements
for a short time (e.g., 24 hours) and then body protein is
mobilized.
Protein-calorie malnutrition (PCM), seen in starving
children of underdeveloped countries, is now also recognized as a significant problem of clients with long-term
deficiencies in caloric intake (e.g., those with cancer and
chronic disease). Characteristics of PCM are depressed
visceral proteins (e.g., albumin), weight loss, and visible
muscle and fat wasting.
Protein stores in the body are generally divided into
two compartments: somatic and visceral. Somatic protein
consists largely of skeletal muscle mass; it is assessed most
commonly by conducting anthropometric measurements
such as the mid-arm circumference (MAC) and the midarm muscle area (MAMA). (See the Anthropometric Measurements section on page 1205.) Visceral protein includes
plasma protein, hemoglobin, several clotting factors,
TABLE 46.3
●
1203
hormones, and antibodies. It is usually assessed by measuring serum protein levels such as albumin and transferrin, discussed in the Biochemical (Laboratory) Data section
of Assessing, which follows.
NURSING MANAGEMENT
Assessing
A nutritional assessment identifies clients at risk for malnutrition and those with poor nutritional status. In most
healthcare facilities, the responsibility for nutritional
assessment and support is shared by the primary care
provider, the dietitian, and the nurse. A comprehensive
nutritional assessment is often performed by a nutritionist
or a dietitian, and the primary care provider. Components
of a nutritional assessment are shown in Table 46.3 and
may be remembered as ABCD data: anthropometric, biochemical, clinical, and dietary.
Nutritional Screening
Because a comprehensive nutritional assessment is time
consuming and expensive, various levels and types of
assessment are available. Nurses perform a nutritional
screen. A nutritional screen is an assessment performed
to identify clients at risk for malnutrition or those who are
malnourished. For clients who are found to be at moderate or high risk for malnutrition (Box 46.5), follow-up is
provided in the form of a comprehensive assessment by a
dietitian. Medicare standards for nursing homes require
that any resident who experiences unplanned or undesired weight loss of 5% or more in 1 month, 7.5% or more
in 3 months, or 10% or more in 6 months receive a full
nutritional assessment by a nurse.
Nurses carry out nutritional screens through routine
nursing histories and physical examinations. Customdesigned screens for a particular population (e.g., older
adults and pregnant women) and specific disorders (e.g.,
cardiac disease) are available.
Components of a Nutritional Assessment
Screening Data
Additional In-Depth Data
Anthropometric data
•
•
•
•
•
• Triceps skinfold (TSF)
• Mid-arm circumference (MAC)
• Mid-arm muscle area (MAMA)
Biochemical data
• Hemoglobin
• Serum albumin
• Total lymphocyte count
• Serum transferrin level
• Urinary urea nitrogen
• Urinary creatinine excretion
Clinical data
•
•
•
•
• Hair analysis
• Neurologic testing
Dietary data
• 24-hour food recall
• Food frequency record
M46_BERM9793_11_GE_C46.indd 1203
Nutrition
Height
Weight
Ideal body weight
Usual body weight
Body mass index
Skin
Hair and nails
Mucous membranes
Activity level
• Selective food frequency record
• Food diary
• Diet history
03/02/2021 18:20
1204
Unit 10
BOX 46.5
●
Promoting Physiologic Health
Summary of Risk Factors for Nutritional Problems
DIET HISTORY
• Chewing or swallowing difficulties (including ill-fitting dentures,
dental caries, and missing teeth)
• Inadequate food budget
• Inadequate food intake
• Inadequate food preparation facilities
• Inadequate food storage facilities
• Intravenous fluids (other than total parenteral nutrition for 10 or
more days)
• Living and eating alone
• Physical disabilities
• Restricted or fad diets
MEDICAL HISTORY
• Alcohol or substance abuse
• Catabolic or hypermetabolic condition: burns, trauma
• Chronic illness: end-stage renal disease, liver disease, AIDS,
pulmonary disease (e.g., chronic obstructive pulmonary disease
[COPD]), cancer
• Fluid and electrolyte imbalance
Screening tools such as the Patient-Generated Subjective Global Assessment (PG-SGA) and the one created by
the Nutrition Screening Initiative (NSI) can be incorporated into the nursing history. The PG-SGA is a method
of classifying clients as either well nourished, moderately malnourished, or severely malnourished based on
a dietary history and physical examination. It was established primarily for use with cancer clients, but has been
widely tested and is appropriate for both inpatient and
outpatient clients with various diagnoses.
The NSI tool is consistent with the U.S. Older Americans Act (authorized through 2018) Nutrition Programs
goals. The NSI screens older adults using a nutrition
checklist that contains nine warning signs of conditions
that can interfere with good nutrition (Box 46.6).
BOX 46.6
GI problems: anorexia, dysphagia, nausea, vomiting, diarrhea,
constipation
• Neurologic or cognitive impairment
• Oral and GI surgery
• Unintentional weight loss or gain of 10% within 6 months
•
MEDICATION HISTORY*
• Antacids
• Antidepressants
• Antihypertensives
• Anti-inflammatory agents
• Antineoplastic agents
• Aspirin
• Digitalis
• Diuretics (thiazides)
• Laxatives
• Potassium chloride
*The potential effects of some medications on nutrition are shown in Table 46.1 on
page 1194.
Nursing History
As mentioned earlier, nurses obtain considerable nutrition-related data in the routine admission nursing history.
Data include but are not limited to the following:
• Age, sex, and activity level
• Difficulty eating (e.g., impaired chewing or swallowing)
• Condition of the mouth, teeth, and presence of dentures
• Changes in appetite
• Changes in weight
• Physical disabilities that affect purchasing, preparing,
and eating
• Cultural and religious beliefs that affect food choices
• Living arrangements (e.g., living alone) and economic
status
Nutritional Screening Tool
Read the statement. Circle the number in the Yes column for those
that apply to you. Total your nutritional assessment.
If you scored 0–2: Good! Recheck your nutritional score in
6 months.
If you scored 3–5: You are at moderate nutritional risk. See what
can be done to improve your eating habits and lifestyle.
Recheck your score in 3 months.
If you scored 6 or above: You are at high nutritional risk. Take this
checklist to your doctor, nurse practitioner, or home health
nurse. Ask for help to improve your nutritional health.
Nutritional Assessment Statements
Yes
I have an illness or condition that made me
change the kind or amount of food I eat.
I eat fewer than two meals per day.
I eat few fruits, vegetables, or milk products.
I have three or more drinks of beer, liquor, or
wine almost every day.
M46_BERM9793_11_GE_C46.indd 1204
2
3
2
2
I have tooth or mouth problems that make it
hard for me to eat.
I do not always have enough money to buy the
food I need.
I eat alone most of the time.
I take three or more different prescribed or overthe-counter drugs a day.
Without wanting to, I have lost or gained
10 pounds in the last 6 months.
I am not always physically able to shop, cook, or
feed myself.
Total
2
4
1
1
2
2
From “Determine Your Nutritional Health,” by the Nutrition Screening Initiative, 2008,
Washington, DC: National Council on Aging. Reprinted with permission by the Nutrition
Screening Initiative, a project of the American Dietetic Association, funded in part by a grant
from Ross Products Division, Abbott Laboratories, Inc.
03/02/2021 18:20
Chapter 46
•
•
General health status and medical condition
Medication history.
Anthropometric Measurements
Anthropometric measurements are noninvasive techniques that aim to quantify body composition. A skinfold
measurement is performed to determine fat stores. The
most common site for measurement is the triceps skinfold (TSF). The fold of skin measured includes subcutaneous tissue but not the underlying muscle. It is measured
in millimeters using special calipers. To measure the TSF,
locate the midpoint of the upper arm (halfway between
the acromion process and the olecranon process), then
grasp the skin on the back of the upper arm along the long
axis of the humerus (Figure 46.3 ■). Placing the calipers
1 cm (0.4 in.) below the nurse’s fingers, measure the thickness of the fold to the nearest millimeter.
The mid-arm circumference (MAC) is a measure of fat,
muscle, and skeleton. To measure the MAC, ask the client to sit or stand with the arm hanging freely and the
forearm flexed to horizontal. Measure the circumference
at the midpoint of the arm, recording the measurement
in centimeters, to the nearest millimeter (e.g., 24.6 cm)
(Figure 46.4 ■).
●
Nutrition
1205
The mid-arm muscle area (MAMA) is then calculated
by using reference tables or by using a formula that incorporates the TSF and the MAC. The MAMA is an estimate
of lean body mass, or skeletal muscle reserves. If tables
are not available, the nurse uses the following formula to
calculate the MAMA from the triceps skinfold and MAC
direct measurements:
MAMA 1cm2 2 =
3midarm circumference 1cm2 - 13.14 * TSF cm24 2
4p
-101 males2or - 6.51 females2
Values for anthropometric measurements for adults
vary by ethnicity. Examples of variations in MAC are
shown in Table 46.4.
Changes in anthropometric measurements occur
slowly and reflect chronic rather than acute changes in
nutritional status. They are used, therefore, to monitor the client’s progress for months to years rather than
days to weeks. Ideally, initial and subsequent measurements need to be taken by the same clinician. In addition, measurements obtained need to be interpreted
with caution. Fluctuations in hydration status that
often occur during illness can influence the accuracy
of results. In addition, normal standards often do not
account for normal changes in body composition such
as those that occur with aging.
Biochemical (Laboratory) Data
Laboratory tests provide objective data to the nutritional
assessment, but because many factors can influence these
tests, no single test specifically predicts nutritional risk or
measures the presence or degree of a nutritional problem.
The tests most commonly used are serum proteins, urinary
urea nitrogen and creatinine, and total lymphocyte count.
Serum Proteins
Figure 46.3 ■ Measuring the triceps skinfold.
Serum protein levels provide an estimate of visceral protein stores. Tests commonly include hemoglobin, albumin,
transferrin, and total iron-binding capacity. A low hemoglobin level may be evidence of iron deficiency anemia.
However, abnormal blood loss or a pathologic process
TABLE 46.4
Figure 46.4 ■ Measuring the mid-arm circumference.
M46_BERM9793_11_GE_C46.indd 1205
MAC Values for Adults
Ethnicity
Male
Female
ALL
34.3 cm
32.2 cm
Non-Hispanic White
34.3 cm
32 cm
Non-Hispanic Black
35.2 cm
34.8 cm
Non-Hispanic Asian
31.3
28.4 cm
Hispanic
34.4
32.6 cm
From “Anthropometric Reference Data for Children and Adults: United States, 2011–2014,”
in Vital and Health Statistics, 3(39), 2016, by C. D. Fryar, Q. Gu, C. L. Ogden, and
K. M. Flegal, National Center for Health Statistics.
03/02/2021 18:20
1206
Unit 10
●
Promoting Physiologic Health
such as GI cancer must be ruled out before iron deficiency
related to diet is confirmed.
Albumin, which accounts for over 50% of the total
serum proteins, is one of the most common visceral proteins evaluated as part of the nutritional assessment.
Because there is so much albumin in the body and because
it is not broken down very quickly (i.e., it has a half-life of
18 to 20 days), albumin concentrations change slowly. A
low serum albumin level is a useful indicator of prolonged
protein depletion rather than acute or short-term changes
in nutritional status. However, many conditions besides
malnutrition can depress albumin concentration, such as
altered liver function, hydration status, and losses from
open wounds and burns.
Transferrin binds and carries iron from the intestine through the serum. Because it has a shorter half-life
than albumin (8 to 9 days), transferrin responds more
quickly to protein depletion than albumin. Serum transferrin can be measured directly or by a total iron-binding capacity (TIBC) test, which indicates the amount of
iron in the blood to which transferrin can bind. Transferrin levels below normal are found with protein loss,
iron deficiency anemia, pregnancy, hepatitis, or liver
dysfunction.
Prealbumin, also referred to as thyroxine-binding
albumin or transthyretin, has the shortest half-life and
smallest body pool and is, therefore, the most responsive
serum protein to rapid changes in nutritional status. Prealbumin levels of 15 to 35 mg/dL are normal, below 15 indicates clients at risk, and below 11 indicates that aggressive
nutritional intervention is needed.
Urinary Tests
Urinary urea nitrogen and urinary creatinine are measures
of protein catabolism and the state of nitrogen balance.
Urea, the chief end product of amino acid metabolism, is
formed from ammonia detoxified by the liver, circulated
in the blood, and transported to the kidneys for excretion
in urine. Urea concentrations in the blood and urine, therefore, directly reflect the intake and breakdown of dietary
protein, the rate of urea production in the liver, and the
rate of urea removal by the kidneys.
The state of nitrogen balance is determined by comparing the nitrogen intake (grams of protein) to the nitrogen
output over a 24-hour period. A positive nitrogen balance
exists when intake exceeds nitrogen output; a negative
nitrogen balance occurs when output exceeds nitrogen
intake. Protein intake must be accurately recorded and
kidney function must be normal to ensure the validity of
a urinary urea nitrogen test.
Urinary creatinine reflects an individual’s total muscle
mass because creatinine is the chief end product of the
creatine produced when energy is released during skeletal muscle metabolism. The rate of creatinine formation
is directly proportional to the total muscle mass. Creatinine is removed from the bloodstream by the kidneys
and excreted in the urine at a rate that closely parallels its
formation. The greater the muscle mass, the greater the
M46_BERM9793_11_GE_C46.indd 1206
excretion of creatinine. As skeletal muscle atrophies during malnutrition, creatinine excretion decreases. Urinary
creatinine is influenced by protein intake, exercise, age,
sex, height, renal function, and thyroid function.
Total Lymphocyte Count
Certain nutrient deficiencies and forms of PCM can
depress the immune system. The total number of lymphocyte white blood cells decreases as protein depletion
occurs.
Clinical Data (Physical Examination)
Physical examination reveals some nutritional deficiencies
and excesses besides obvious weight changes. Assessment
focuses on rapidly proliferating tissues such as skin, hair,
nails, eyes, and mucosa but also includes a systematic
review comparable to any routine physical examination.
See Box 46.7 and Figure 46.5 ■ for signs associated with
malnutrition. These signs must be viewed as suggestive of
malnutrition because the signs are nonspecific. For example, red conjunctiva may indicate an infection rather than
a nutritional deficit, and dry, dull hair may be related to
excessive exposure to the sun rather than severe proteinenergy malnutrition. To confirm malnutrition, clinical
findings need to be substantiated with laboratory tests
and dietary data.
BOX 46.7
Malnutrition
Area of Examination Signs Associated
(Possible Cause)
with Malnutrition
General appearance
and vitality
Apathetic, listless, looks tired, easily
fatigued
Weight
Overweight or underweight
Skin
Dry, flaky, or scaly; pale or pigmented;
presence of petechiae or bruises; lack of
subcutaneous fat; edema
Nails
Brittle, pale, ridged, or spoon shaped
(iron deficiency)
Hair
Dry, dull, sparse, loss of color, brittle
(Figure 46.6A)
Eyes
Pale or red conjunctiva, dryness, soft
cornea, dull cornea, night blindness
(vitamin A deficiency)
Lips
Swollen, red cracks at side of
mouth, vertical fissures (B vitamins deficiency) (Figure 46.6C)
Tongue
Swollen, beefy red or magenta colored,
smooth appearance (B vitamins deficiency); decrease or increase in size
Gums
Spongy, swollen, inflamed; bleed easily
(vitamin C deficiency)
Muscles
Underdeveloped, flaccid, wasted, soft
GI system
Anorexia, indigestion, diarrhea, constipation, enlarged liver, protruding abdomen
Nervous system
Decreased reflexes, sensory loss, burning
and tingling of hands and feet (B vitamins
deficiency), mental confusion or irritability
03/02/2021 18:20
Chapter 46
●
Nutrition
1207
B
A
C
Figure 46.5 ■ Examples of nutritional deficiencies: A, dull, sparse hair and inflammation of the corners of the mouth from protein deficiency;
B, rickets from vitamin D or calcium deficiency; C, pellagra, caused by a chronic lack of niacin (vitamin B).
A, from Centers for Disease Control and Prevention; B, Biophoto Associates/Science Source; C, Clinical Photography, Central Manchester University Hospitals NHS Foundation Trust, UK/Science Source.
Calculating Percentage of Weight Loss
Accurate assessment of the client’s height, current body
weight (CBW), and usual body weight (UBW) is essential. Although the client’s CBW can be compared with
an ideal body weight discussed earlier, the IBW is based
on healthy individuals and does not account for changes
in the client’s body composition that accompany illness or reflect any changes in weight. The client’s UBW
better indicates weight change and the possibility of
BOX 46.8
malnutrition. Calculation and interpretation of the percentage of deviation from UBW and the percentage of
weight loss are shown in Box 46.8. An important aspect
of weight assessment, obtained during the nursing history, is a description of weight change. The nurse should
document any weight loss or gain, the duration of the
change, and whether the weight change was intentional
or unintentional.
Calculating and Interpreting the Percentage of Deviation from Usual Body Weight
and the Percentage of Weight Loss
CALCULATING PERCENTAGE OF USUAL BODY WEIGHT
% Usual body weight =
current weight
usual body weight
* 100
CALCULATING PERCENTAGE OF WEIGHT LOSS
% Weight loss =
usual weight-current weight
usual weight
* 100
Mild malnutrition
85–90%
Significant Weight Loss
Severe Weight Loss
Moderate malnutrition
75–84%
5% over 1 mo
Greater than 5% over 1 mo
Severe malnutrition
Less than 74%
7.5% over 3 mo
Greater than 7.5% over 3 mo
10% over 6 mo
Greater than 10% over 6 mo
M46_BERM9793_11_GE_C46.indd 1207
03/02/2021 18:20
1208
Unit 10
●
Promoting Physiologic Health
Dietary Data
Dietary data include the client’s usual eating patterns
and habits; food preferences, allergies, and intolerances;
frequency, types, and quantities of foods consumed; and
social, economic, ethnic, or religious factors influencing
nutrition. Factors may include, but are not limited to,
living and eating companions, ability to purchase and
prepare food, availability of refrigeration and cooking
facilities, income, and effect of religion and ethnicity on
food choices.
Four possible methods for collecting dietary data are a
24-hour food recall, a food frequency record, a food diary,
and a diet history.
For a 24-hour food recall, the nurse asks the client to
recall all of the food and beverages the client consumes
during a typical 24-hour period when at home. The data
obtained are then generally evaluated according to the
Food Guide to judge overall adequacy.
A food frequency record is a checklist that indicates
how often general food groups or specific foods are eaten.
Frequency may be categorized as times/day, times/week,
times/month, or frequently, seldom, never. This record provides information about the types of foods eaten but not the
quantities. When specific foods or nutrients are suspected of
being deficient or excessive, the healthcare professional may
use a selective food frequency that focuses, for example, on
fat, fruit, vegetable, or fiber intake.
A food diary is a detailed record of measured amounts
(portion sizes) of all food and fluids a client consumes
during a specified period, usually 3 to 7 days.
A diet history is a comprehensive time-consuming
assessment of a client’s food intake that involves an extensive interview by a nutritionist or dietitian. It includes characteristics of foods usually eaten and the frequency and
amount of food consumed. It may include a 24-hour recall,
a food frequency record, and a food diary. Medical and psychosocial factors are also assessed to evaluate their impact
on nutritional requirements, food habits, and choices. Data
obtained are analyzed by computer and translated into
caloric and nutrient intake. Results are compared with the
DRIs appropriate for the client’s age, sex, and condition.
Diagnosing
Some nursing diagnoses for clients with nutritional problems are: obesity, excess dietary intake, insufficient dietary
intake, and overweight. Many other nursing diagnoses
may apply to certain individuals, because nutritional
problems often affect other areas of human functioning.
Examples include constipation related to inadequate fluid
intake and fiber intake, and altered self-esteem related
to obesity.
Planning
Major goals for clients with or at risk for nutritional problems include the following:
•
•
•
•
•
Maintain or restore optimal nutritional status.
Promote healthy nutritional practices.
Prevent complications associated with malnutrition.
Decrease weight.
Regain specified weight.
Specific nursing activities associated with each of these
goals can be selected to meet the individual needs of the
client. See the Nursing Care Plan and Concept Map at the
end of this chapter.
Planning for Home Care
To provide for continuity of care, the nurse must consider
the client’s need for assistance with nutrition. Some clients
will need help with eating, purchasing food, and preparing meals; others will need instructions about nutrition
therapy.
Home care planning incorporates an assessment of
the client’s and family’s abilities for self-care, financial
resources, and the need for referrals and home health
services. A major aspect of discharge planning involves
the instructional needs of the client and family (see Client
Teaching).
CLIENT TEACHING Healthy Nutrition
•
•
•
•
•
•
Instruct clients about the content of a healthy diet based on the
MyPlate and Dietary Guidelines for Americans
Encourage clients, particularly older clients, to reduce dietary fat
(see Client Teaching on reducing dietary fat, page 1200).
Instruct strict vegetarians about proper protein complementation and additional vitamin and mineral supplementation.
Discuss foods high in specific nutrients required such as
protein, iron, calcium, vitamin C, and fiber.
Discuss importance of properly fitted dentures and dental care.
Discuss safe food preparation and preservation techniques as
appropriate.
DIETARY ALTERATIONS
• Explain the purpose of the diet.
• Discuss allowed and excluded foods.
M46_BERM9793_11_GE_C46.indd 1208
Explain the importance of reading food labels when selecting
packaged foods.
• Include family or significant others.
• Reinforce information provided by the dietitian or nutritionist as
appropriate.
• Discuss herbs and spices as alternatives to salt and substitutes
for sugar.
•
FOR CLIENTS WHO ARE OVERWEIGHT
• Discuss physiologic, psychologic, and lifestyle factors that
predispose to weight gain.
• Provide information about desired weight range and recommended calorie intake.
• Discuss principles of a well-balanced diet and high- and
low-calorie foods.
03/02/2021 18:20
Chapter 46
●
Nutrition
1209
CLIENT TEACHING Healthy Nutrition—continued
•
•
•
•
•
•
Encourage intake of low-calorie, caffeine-free beverages, and
plenty of water.
Discuss ways to adapt eating practices by using smaller plates,
taking smaller servings, chewing each bite a specified number
of times, and putting fork down between bites.
Discuss ways to control the desire to eat by taking a walk, drinking a glass of water, or doing slow deep-breathing exercises.
Discuss the importance of exercise and help the client plan an
exercise program.
Discuss stress reduction techniques.
Provide information about available community resources (e.g.,
weight-loss groups, dietary counseling, exercise programs, selfhelp groups).
FOR CLIENTS WHO ARE UNDERWEIGHT
• Discuss factors contributing to inadequate nutrition and weight
loss.
• Discuss recommended calorie intake and desired weight range.
• Provide information about the content of a balanced diet.
• Provide information about ways to increase calorie intake (e.g.,
high-protein or high-calorie foods and supplements).
• Discuss ways to manage, minimize, or alter the factors contributing to malnourishment.
Implementing
Nursing interventions to promote optimal nutrition for
hospitalized clients are often provided in collaboration
with the primary care provider who writes the diet orders
and the dietitian who informs clients about special diets.
The nurse reinforces this instruction and, in addition,
creates an atmosphere that encourages eating, provides
assistance with eating, monitors the client’s appetite and
food intake, administers enteral and parenteral feedings,
and consults with the primary care provider and dietitian
about nutritional problems that arise.
In the community setting, the nurse’s role is largely
educational. Nurses promote optimal nutrition at health
fairs, in schools, at prenatal classes, and with well or ill
clients and support people in their homes. In the home setting, nurses also initiate nutritional screens, refer clients at
risk to appropriate resources, instruct clients about enteral
and parenteral feedings, and offer nutrition counseling as
needed. Nutrition counseling involves more than providing information. The nurse must help clients integrate diet
changes into their lifestyle and provide strategies to motivate them to change their eating habits.
All dietary instructions must be individually designed
to meet the client’s intellectual ability, motivation level,
lifestyle, culture, and economic status. Both nutritionists
and dietitians help to adapt a diet to suit the client. Simple
verbal instructions need to be given and reinforced with
written material. Family and support persons must be
included in the dietary instruction.
Assisting with Special Diets
Alterations in the client’s diet are often needed to treat a
disease process such as diabetes mellitus, to prepare for
M46_BERM9793_11_GE_C46.indd 1209
•
•
If appropriate, discuss ways to purchase low-cost nutritious foods.
Provide information about community agencies that can assist
in providing food (e.g., Meals on Wheels).
PREVENTING FOODBORNE ILLNESS
• Reinforce hygienic handling of food and dishes:
• Wash hands before preparing foods.
• Wash hands and all dishes, utensils, and cutting boards with
hot water and soap after contact with raw meats.
• Defrost frozen foods in the refrigerator.
• Cook beef, poultry, and eggs thoroughly. Use a cooking
thermometer.
• Refrigerate leftovers promptly (at 40°F [5°C] or less) and
keep no more than 3 to 5 days.
• Wash or peel raw fruits and vegetables.
• Do not use foods from containers that have been damaged
or have opened seals.
• Follow the rules “keep hot foods hot and cold foods cold”
and “when in doubt, throw it out.”
• Recommend the client consider a preventive vaccination for
hepatitis A.
• Instruct clients to seek medical attention for prolonged vomiting, fever, abdominal pain, or severe diarrhea following a meal.
a special examination or surgery, to increase or decrease
weight, to restore nutritional deficits, or to allow an organ
to rest and promote healing. Diets are modified in one or
more of the following aspects: texture, kilocalories, specific nutrients, seasonings, or consistency.
Hospitalized clients who do not have special needs
eat the regular (standard or house) diet, a balanced diet
that supplies the metabolic requirements of a sedentary
individual (about 2000 Kcal). Most agencies offer clients a
daily menu from which to select their meals for the next
day; others provide standard meals to each client on the
general diet.
A variation of the regular diet is the light diet, designed
for postoperative and other clients who are not ready for
the regular diet. Foods in the light diet are plainly cooked
and fat is usually minimized, as are bran and foods containing a great deal of fiber.
Diets modified in consistency are often given to clients
before and after surgery or procedures or to promote healing in clients with GI distress. These diets include clear
liquid, full liquid, soft, and diet as tolerated. In some agencies, GI surgery clients are not permitted red-colored liquids or candy since, if vomited, the color may be confused
with blood.
Clear Liquid Diet
This diet is limited to water, tea, coffee, clear broths,
ginger ale or other carbonated beverages, strained and
clear juices, and plain gelatin. Note that “clear” does not
necessarily mean “colorless.” This diet provides the client with fluid and carbohydrate (in the form of sugar),
but does not supply adequate protein, fat, vitamins,
minerals, or calories. It is a short-term diet (24 to
03/02/2021 18:20
1210
Unit 10
●
Promoting Physiologic Health
36 hours) provided for clients after certain surgeries or
in the acute stages of infection, particularly of the GI
tract. The major objectives of this diet are to relieve thirst,
prevent dehydration, and minimize stimulation of the GI
tract. Examples of foods allowed in clear liquid diets are
shown in Box 46.9.
Full Liquid Diet
This diet contains only liquids or foods that turn to liquid
at body temperature, such as ice cream (see Box 46.9). Full
liquid diets are often eaten by clients who have GI disturbances or cannot tolerate solid or semisolid foods. This
diet is not recommended for long-term use because it is
low in iron, protein, and calories. In addition, its cholesterol content may be high because of the amount of cow’s
milk offered. Clients who must receive only liquids for
long periods are usually given a nutritionally balanced
oral supplement, such as Boost, Ensure, or Sustacal. The
full liquid diet is monotonous and difficult for clients to
accept. Planning six or more feedings per day may encourage a more adequate intake.
Soft Diet
The soft diet is easily chewed and digested. It is often
ordered for clients who have difficulty chewing and
swallowing. It is a low-residue (low-fiber) diet containing very few uncooked foods; however, restrictions
vary among agencies and according to individual tolerance. Examples of foods that can be included in a soft or
semisoft diet are shown in Box 46.9. The pureed diet is a
modification of the soft diet. Liquid may be added to the
food, which is then blended to a semisolid consistency.
Diet as Tolerated
“Diet as tolerated” is ordered when the client’s appetite,
ability to eat, and tolerance for certain foods may change.
For example, on the first postoperative day a client may
BOX 46.9
be given a clear liquid diet. If no nausea occurs, normal
intestinal motility has returned as evidenced by active
bowel sounds and client reports passing gas, and the client feels like eating, the diet may be advanced to a full
liquid, light, or regular diet.
Modification for Disease
Many special diets may be prescribed to meet requirements for disease processes or altered metabolism. For
example, a client with diabetes mellitus may need a diet
recommended by the American Diabetes Association, an
obese client may need a calorie-restricted diet, a cardiac
client may need sodium and cholesterol restrictions, and
a client with allergies will need a hypoallergenic diet.
Some clients must follow certain diets (e.g., the diabetic diet) for a lifetime. If the diet is long term, the client
must understand the diet and also develop a healthy, positive attitude toward it. Assisting clients and support persons with special diets is a function shared by the dietitian
or nutritionist and the nurse. The dietitian informs the client and support persons about the specific foods allowed
and not allowed and assists the client with meal planning.
The nurse reinforces this instruction, assists the client to
make changes, and evaluates the client’s responses.
Dysphagia
Some clients may have no difficulty with choosing a
healthy diet, but be at risk for nutritional problems due
to dysphagia. These clients may have inadequate solid
or fluid intake, be unable to swallow their medications,
or aspirate food or fluids into the lungs—causing pneumonia. Clients at risk for dysphagia include older adults,
those who have experienced a stroke, clients with cancer
who have had radiation therapy to the head and neck, and
others with cranial nerve dysfunction. Consider dysphagia if the client exhibits the following behaviors: coughs,
Examples of Foods for Clear Liquid, Full Liquid, and Soft Diets
Clear Liquid
Full Liquid
Soft
Coffee, regular and
decaffeinated
All foods on clear liquid diet
plus:
All foods on clear and full liquid diets, plus:
Tea
Milk and milk drinks
Carbonated beverages
Puddings, custards
Bouillon, fat-free broth
Ice cream, sherbet
Clear fruit juices (apple,
cranberry, grape)
Vegetable juices
Meat: all lean, tender meat, fish, or poultry (chopped, shredded); spaghetti sauce with ground meat over pasta
Meat alternatives: scrambled eggs, omelet, poached eggs; cottage
cheese and other mild cheese
Vegetables: mashed potatoes, sweet potatoes, or squash; vegetables in
cream or cheese sauce; other cooked vegetables as tolerated (e.g., spinach, cauliflower, asparagus tips), chopped and mashed as needed; avocado
Other fruit juices, strained
Refined or strained cereals
(e.g., cream of rice)
Popsicles
Cream, butter, margarine
Gelatin
Eggs (in custard and pudding)
Sugar, honey
Smooth peanut butter
Breads and cereals: enriched rice, barley, pasta; all breads; cooked cereals (e.g., oatmeal)
Hard candy
Yogurt
Desserts: soft cake, bread pudding
M46_BERM9793_11_GE_C46.indd 1210
Fruits: cooked or canned fruits; bananas, grapefruit and orange sections
without membranes, applesauce
03/02/2021 18:20
Chapter 46
chokes, or gags while eating; complains of pain when
swallowing; has a gurgling voice; requires frequent oral
suctioning.
Nurses may be the first individuals to detect dysphagia and are in an excellent position to recommend further
evaluation; implement specialized feeding techniques
and diets; and work with clients, family members, and
other healthcare professionals to develop a plan to assist
the client with difficulties. If the client condition suggests
dysphagia, the nurse should review the history in detail;
interview the client or family; assess the mouth, throat, and
chest; and observe the client swallowing. Although absence
of or a reduced gag reflex indicates the client will have difficulty swallowing, the presence of the gag reflex should
not be interpreted to indicate that swallowing will not be
impaired.
A multidisciplinary group developed the National
Dysphagia Diet (NDD), which delineates standards of
food textures (American Dietetic Association, 2002). The
four levels of liquid foods are thin, nectar-like, honeylike, and spoon-thick liquids. The four levels of semisolid or solid foods are pureed, mechanically altered,
mechanically soft, and regular. In consultation with
●
Nutrition
1211
the dietitian, occupational therapist, swallowing specialist, speech-language pathologist, and primary care
provider, these levels can be used to determine a consistent approach to a particular client’s dysphagia. For
example, a mechanically soft diet may result in lower
pneumonia rates than a pureed diet in clients who have
had a stroke and a history of aspiration pneumonia.
Due to confusion regarding the terminology used to
describe varying levels of food thickness, the International Dysphagia Diet Standardisation Initiative (IDDSI)
developed standardized terminology and definitions to
describe texture-modified foods and thickened liquids
used for individuals with dysphagia of all ages, in all
care settings, and all cultures (Cichero et al., 2017). See
the IDDSI Framework in Figure 46.6 ■. Early detection
and intervention can prevent the adverse outcomes of
dysphagia in most clients.
Stimulating the Appetite
Physical illness, unfamiliar or unpalatable food, environmental and psychologic factors, and physical discomfort
or pain may depress the appetites of many clients. A shortterm decrease in food intake usually is not a problem
FOODS
REGULAR
TR
7
AN
EASY TO CHEW
IO
SIT
6
DS
OO
LF
NA
SOFT & BITE-SIZED
MINCED & MOIST
5
PUREED
4
3
LIQUIDISED
2
1
0
EXTREMELY THICK
MODERATELY THICK
MILDLY THICK
SLIGHTLY THICK
THIN
DRINKS
Figure 46.6 ■ The IDDSI Framework
© The International Dysphagia Diet Standardisation Initiative, 2019. @http://iddsi.org/resources/framework/
M46_BERM9793_11_GE_C46.indd 1211
03/02/2021 18:20
1212
Unit 10
●
Promoting Physiologic Health
for adults; over time, however, it leads to weight loss,
decreased strength and stamina, and other nutritional
problems. Decreased food intake is often accompanied by
a decrease in fluid intake, which may cause fluid and electrolyte problems. Stimulating a client’s appetite requires
the nurse to determine the reason for the lack of appetite
and then deal with the problem. Some general interventions for improving the client’s appetite are summarized
in Box 46.10.
BOX 46.10
•
•
•
•
•
•
•
Improving Appetite
Provide familiar food that the client likes. Often the family and
friends of clients are pleased to bring food from home but
may need some guidance about special diet requirements.
Select small portions so as not to discourage the client.
Avoid unpleasant or uncomfortable treatments immediately
before or after a meal.
Provide a tidy, clean environment that is free of unpleasant sights and odors. A soiled dressing, a used bedpan, an
uncovered irrigation set, or even used dishes can negatively
affect the appetite.
Encourage or provide oral hygiene before mealtime. This
improves the client’s ability to taste.
Relieve illness symptoms that depress appetite before mealtime; for example, give an analgesic for pain or an antipyretic
for a fever or allow rest for fatigue.
Reduce psychologic stress. A lack of understanding of therapy, the anticipation of an operation, and fear of the unknown
can cause anorexia. Often, the nurse can help by discussing
feelings with the client, giving information and assistance, and
allaying fears.
BOX 46.11
•
•
•
•
•
•
•
Assisting Clients with Meals
Because clients in healthcare agencies are frequently confined to their beds, meals are brought to the client. The
client receives a tray that has been assembled in a central
kitchen. Nursing personnel may be responsible for giving
out and collecting the trays; however, in most settings this
is done by dietary personnel. Long-term care facilities and
some hospitals serve meals to mobile clients in a special
dining area. Guidelines for providing meals to clients are
summarized in Box 46.11.
Individuals who frequently require help with their
meals include older adults who are weakened, individuals with disabilities such as visual impairment, those who
must remain in a back-lying position, or those who cannot
use their hands. The client’s nursing care plan will indicate that assistance is required with meals.
The nurse must be sensitive to clients’ feelings of
embarrassment, resentment, and loss of autonomy.
Whenever possible, the nurse should help clients feed
themselves rather than feed them. Some clients become
depressed because they require help and because they
believe they are burdensome to busy nursing personnel. Although feeding a client is time consuming, nurses
should try to appear unhurried and convey that they have
ample time. Sitting at the bedside is one way to convey
this impression. If the client is to be fed by assistive personnel, the nurse must ensure that the same standards
are met.
When feeding a client, ask in which order the client
would like to eat the food. If the client cannot see, tell
Providing Client Meals
Offer the client assistance with hand washing and oral hygiene
before a meal.
If it is permitted, assist the client to a comfortable position in
bed or in a chair, whichever is appropriate.
Clear the overbed table so there is space for the tray. If the client must remain in a lying position in bed, arrange the overbed
table close to the bedside so the client can see and reach the
food.
Check each tray for the client’s name, the type of diet,
and completeness. Do not leave an incorrect diet for a client
to eat.
Assist the client as required (e.g., remove the food covers, butter the bread, pour the tea, and cut the meat).
For a client with a visual impairment, identify the placement of the
food as you would describe the time on a clock (Figure 46.7 ■).
For instance, the nurse might say, “The potatoes are at eight
o’clock, the chicken at 12 o’clock, and the green beans at
4 o’clock.”
After the client has completed the meal, observe how much
and what the client has eaten and the amount of fluid taken.
Use a standard tool to estimate the amount eaten in relation
to a typical meal. For example, if served a donut and coffee
for breakfast, although the client may have consumed both
of these, they certainly do not represent 100% of a nutritious
breakfast.
M46_BERM9793_11_GE_C46.indd 1212
If the client is on a special diet or is having problems eating,
record the amount of food eaten and any pain, fatigue, or nausea experienced.
• If the client is not eating, document this so that changes can be
made, such as rescheduling the meals, providing smaller, more
frequent meals, or obtaining special self-feeding aids.
•
12 o’clock
9
3
8 o’clock
4 o’clock
6
Figure 46.7 ■ For a client who is visually impaired, the nurse can
use the clock system to describe the location of food on the plate.
03/02/2021 18:20
Chapter 46
the client which food is being given. Always allow ample
time for the client to chew and swallow the food before
offering more. Also, provide fluids as requested or, if the
client cannot communicate, offer fluids after every three
or four mouthfuls of solid food. Make the time a pleasant
one, choosing topics of conversation that are of interest to
clients who want to talk.
Although normal utensils should be used whenever
possible, special utensils may be needed to assist a client to eat. For clients who have difficulty drinking from a
cup or glass, a straw often permits them to obtain liquids
with less effort and less spillage. Special drinking cups are
also available. One model has a spout; another is specially
designed to permit drinking with less tipping of the cup
than is normally required.
Many adaptive feeding aids are available to help clients maintain independence. A standard eating utensil
with a built-up or widened handle helps clients who cannot grasp objects easily. Utensils with wide handles can
be purchased, or a regular eating utensil can be modified
by taping foam around the handle. The foam increases
friction and steadies the client’s grasp. Handles may be
bent or angled to compensate for limited motion. Collars
or bands that prevent the utensil from being dropped can
be attached to the end of the handle and fit over the client’s hand. Clients requiring pureed or liquid diets are
sometimes fed with a feeding syringe.
Plates with rims and plastic or metal plate guards
enable the client to pick up the food by first pushing it
against this raised edge. A suction cup or damp sponge
or cloth may be placed under the dish to keep it from
moving while the client is eating. No-spill mugs and twohandled drinking cups are especially useful for individuals with impaired hand coordination. Stretch terry cloth
and knitted or crocheted glass covers enable the client to
keep a secure grasp on a glass. Lidded tip-proof glasses
are also available. Figures 46.8 ■ and 46.9 ■ show some
of these aids.
●
Nutrition
1213
Figure 46.9 ■ Dinner plate with guard attached and lipped plate
facilitates scooping; angled spoon and padded knife facilitate grip.
Special Community Nutritional Services
In many places, community programs have been developed to help special groups meet nutritional needs. For
older adults who cannot prepare meals or leave their
homes, ready-to-eat meals or frozen dinners are delivered
to the home by local organizations. Meals on Wheels is one
such well-known organization. For individuals who can
prepare meals but have physical disabilities and cannot
shop for groceries, grocery delivery services are available.
For low-income individuals in the United States,
the USDA funds the Supplemental Nutrition Assistance
Program (SNAP). Through this program, individuals
and families can use an electronic benefit card (similar
to a debit card) to purchase food at any approved store.
The value of the benefit provided depends on the size and
income of the family.
Enteral Nutrition
Alternative feeding methods that ensure adequate nutrition include enteral (through the GI system) methods.
Enteral nutrition (EN), also referred to as total enteral
nutrition (TEN), is provided when the client cannot ingest
foods or the upper GI tract is impaired and the transport of
food to the small intestine is interrupted. Enteral feedings
are administered through nasogastric and small-bore feeding tubes, or through gastrostomy or jejunostomy tubes.
Enteral Access Devices
Figure 46.8 ■ Left to right: glass holder, cup with hole for nose,
two-handled cup holder.
M46_BERM9793_11_GE_C46.indd 1213
Enteral access is achieved by means of nasogastric or
nasointestinal (nasoenteric) tubes, or gastrostomy or jejunostomy tubes.
A nasogastric tube is inserted through one of the
nostrils, down the nasopharynx, and into the alimentary tract. Traditional firm, large-bore nasogastric tubes
03/02/2021 18:20
1214
Unit 10
●
Promoting Physiologic Health
Figure 46.11 ■ A polyurethane feeding tube designed for nasogastric
and nasoduodenal feeding with a weighted tip for easier insertion. The feeding port is incompatible with Luer-Lok or IV connections, reducing the risk of
accidental connection or infusion. Tubes can be 8Fr–12Fr and 36”–55” long.
Cardinal Health.
Figure 46.10 ■ Left, Single-lumen Levin tube. Right, Double-lumen
Salem sump tube with filter on air vent port.
(i.e., those larger than 12 Fr in diameter) are placed
into the stomach. Examples are the Levin tube, a flexible rubber or plastic, single-lumen tube with holes near
the tip, and the Salem sump tube, with a double lumen
(Figure 46.10 ■). The larger lumens allow delivery of
liquids to the stomach or removal of gastric contents.
When the Salem tube is used for suction of gastric contents, the smaller vent lumen (the proximal port is often
referred to as the blue pigtail) allows for an inflow of
atmospheric air, which prevents a vacuum if the gastric
tube adheres to the wall of the stomach. Irritation of
the gastric mucosa is thereby avoided. Softer, more flexible and less irritating small-bore feeding tubes (SBFTs),
smaller than 12 Fr in diameter, are frequently used for
enteral nutrition (Figure 46.11 ■).
Nasogastric tubes are used for feeding clients who
have adequate gastric emptying, and who require shortterm feedings. They are not advised for feeding clients
without intact gag and cough reflexes since the risk of
accidental placement of the tube into the lungs is much
higher in those clients. Skill 46.1 provides guidelines for
inserting a nasogastric tube. If the nurse is unsuccessful in
placing the tube using the standard methods or the client
has a particularly challenging anatomic condition, the tube
may be placed by a physician endoscopically or by specially trained nurses using electromagnetic-guided bedside
placement (Gerritsen et al., 2016). Skill 46.4 later in this
chapter outlines the steps for removing a nasogastric tube.
SKILL 46.1
Inserting a Nasogastric Tube
PURPOSES
• To administer tube feedings and medications to clients unable
to eat by mouth or swallow a sufficient diet without aspirating
food or fluids into the lungs
• To establish a means for suctioning stomach contents to prevent gastric distention, nausea, and vomiting
ASSESSMENT
• Check for history of nasal surgery or deviated septum. Assess
patency of nares.
PLANNING
Before inserting a nasogastric tube, determine the size of tube to be
inserted and whether the tube is to be attached to suction.
Assignment
Insertion of a nasogastric tube is an invasive procedure requiring
application of knowledge (e.g., anatomy and physiology, risk factors)
and problem-solving. In some agencies, only healthcare providers
with advanced training are permitted to insert nasogastric tubes that
require use of a stylet. Assignment or delegation of this skill to assistive personnel (AP) is not appropriate. The AP, however, can assist
with the oral hygiene needs of a client with a nasogastric tube.
Equipment
• Large- or small-bore tube (nonlatex preferred)
• Nonallergenic adhesive tape, 2.5 cm (1 in.) wide
• Commercial securement device, if available
• Clean gloves
M46_BERM9793_11_GE_C46.indd 1214
•
•
To remove stomach contents for laboratory analysis
To lavage (wash) the stomach in case of poisoning or overdose
of medications
•
•
Determine presence of gag reflex.
Assess mental status or ability to participate in the procedure.
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Water-soluble lubricant
Topical lidocaine (optional)
Facial tissues
Glass of water and drinking straw
20- to 50-mL catheter-tip syringe
Basin
pH test strip or meter (optional)
Bilirubin dipstick (optional)
Stethoscope
Disposable pad or towel
Antireflux valve for air vent if Salem sump tube is used
Suction apparatus
Safety pin and elastic band
Clamp or plug (optional)
CO2 detector (optional)
03/02/2021 18:21
Chapter 46
●
Nutrition
1215
Inserting a Nasogastric Tube—continued
Performance
1. Prior to performing the insertion, introduce self and verify the client’s identity using agency protocol. Explain to the client what you
are going to do, why it is necessary, and how to participate. The
passage of a gastric tube is unpleasant because the gag reflex is
activated during insertion. Establish a method for the client to indicate distress and a desire for you to pause the insertion. Raising a
finger or hand is often used for this.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures (e.g., clean gloves).
3. Provide for client privacy.
4. Assess the client’s nares.
• Apply clean gloves.
• Ask the client to hyperextend the head, and, using a flashlight, observe the intactness of the tissues of the nostrils,
including any irritations or abrasions.
• Examine the nares for any obstructions or deformities by asking the client to breathe through one nostril while occluding
the other.
• Select the nostril that has the greater airflow.
5. Prepare the tube.
• If a small-bore tube is being used, ensure stylet or guidewire
is secured in position. Rationale: An improperly positioned
stylet or guidewire can traumatize the nasopharynx, esophagus, and stomach.
• If a large-bore tube is being used, place the tube in a basin of
warm water while preparing the client. Rationale: This allows
the tubing to become more pliable and flexible. However,
if the softened tube becomes difficult to control, it may be
helpful to place the distal end in a basin of ice water to help it
hold its shape.
6. Determine how far to insert the tube.
• Use the tube to mark off the distance from the tip of the client’s nose to the tip of the earlobe and then from the tip of
the earlobe to the tip of the xiphoid. ❶ Rationale: This length
approximates the distance from the nares to the stomach. This distance varies among individuals.
• Mark this length with adhesive tape if the tube does not
have markings.
7. Insert the tube.
• Lubricate the tip of the tube well with water-soluble lubricant or water to ease insertion. Rationale: A water-soluble
lubricant dissolves if the tube accidentally enters the lungs.
An oil-based lubricant, such as petroleum jelly, will not dissolve and could cause respiratory complications if it enters
the lungs. Agency policy should permit topical lidocaine
anesthetic to be used on the tube or in the client’s nose to
numb the area (Solomon & Jurica, 2017).
• Insert the tube, with its natural curve downward, into the
selected nostril. Ask the client to hyperextend the neck,
and gently advance the tube toward the nasopharynx.
Rationale: Hyperextension of the neck reduces the curvature of the nasopharyngeal junction.
• Direct the tube along the floor of the nostril and toward
the midline. Rationale: Directing the tube along the floor
avoids the projections (turbinates) along the lateral wall.
• Slight pressure and a twisting motion are sometimes
required to pass the tube into the nasopharynx, and
some clients’ eyes may water at this point. Rationale:
Tears are a natural body response. Provide the client with
tissues as needed.
• If the tube meets resistance, withdraw it, relubricate it,
and insert it in the other nostril. Rationale: The tube
should never be forced against resistance because of the
danger of injury.
• Once the tube reaches the oropharynx (throat), the client
will feel the tube in the throat and may gag and retch.
Ask the client to tilt the head forward, and encourage the
client to drink and swallow. Rationale: Tilting the head
forward facilitates passage of the tube into the posterior pharynx and esophagus rather than into the larynx;
swallowing moves the epiglottis over the opening to the
larynx. ❷
• If the client gags, stop passing the tube momentarily.
Have the client rest, take a few breaths, and take sips of
water to calm the gag reflex.
SKILL 46.1
IMPLEMENTATION
Preparation
• Assist the client to a high-Fowler’s position if the client’s health
condition permits, and support the head on a pillow. Rationale:
It is often easier to swallow in this position and gravity helps the
passage of the tube.
• Place a towel or disposable pad across the chest.
Pharynx
Epiglottis
(open)
Larynx
Esophagus
Trachea
Epiglottis
(closed)
Esophagus
Trachea
❶ Measuring the appropriate length to insert a nasogastric tube.
❷ Swallowing closes the epiglottis.
Continued on page 1216
M46_BERM9793_11_GE_C46.indd 1215
03/02/2021 18:21
1216
Unit 10
●
Promoting Physiologic Health
Inserting a Nasogastric Tube—continued
In cooperation with the client, pass the tube 5 to 10 cm
(2 to 4 in.) with each swallow, until the indicated length is
inserted.
• If the client continues to gag and the tube does not
advance with each swallow, withdraw it slightly, and inspect
the throat by looking through the mouth. Rationale: The
tube may be coiled in the throat. If so, withdraw it until it is
straight, and try again to insert it.
• If a CO2 detector is used, after the tube has been advanced
approximately 30 cm (12 in.), draw air through the detector.
Any change in color of the detector indicates placement of
the tube in the respiratory tract. Immediately withdraw the
tube and reinsert.
8. Ascertain correct placement of the tube.
• Nasogastric tubes are radiopaque, and position can be
confirmed by x-ray. If an SBFT is used, leave the stylet or
guidewire in place until correct position is verified by x-ray.
This is the only definitive method of verifying feeding tube tip
placement. If an x-ray is not feasible, at least two of the following methods should be used.
• Aspirate stomach contents, and check the pH, which
should be acidic. Rationale: Testing pH is a reliable way to
determine location of a feeding tube. Gastric contents are
commonly pH 1 to 5; 6 or greater would indicate the contents are from lower in the intestinal tract or in the respiratory
tract. However, pH may not discriminate between gastric and
esophageal placement (Morton & Fontaine, 2018).
SKILL 46.1
•
Safety Alert!
❸ Taping a nasogastric tube to the bridge of the nose.
10.
11.
SAFETY
If the stylet has been removed, never reinsert it while the tube is in
place. Rationale: The stylet is sharp and could pierce the tube and
injure the client or cut off the tube end.
Because small-bore tubes offer more resistance during
aspirations than large-bore tubes and are more likely to
collapse when negative pressure is applied, it may not
be possible to obtain an aspirate from an SBFT. Aspirate
can also be tested for bilirubin. Bilirubin levels in the lungs
should be almost zero, while levels in the stomach will be
approximately 1.5 mg/dL and in the intestine more than
10 mg/dL.
• Historically, nurses placed a stethoscope over the client’s
epigastrium and injected 10 to 30 mL of air into the tube
while listening for a whooshing sound. This method does
not guarantee tube position. Even if the sound is heard, the
tube could be in the stomach or the lungs (Lyman, Peyton,
& Healey, 2018).
• If the signs indicate placement in the lungs, remove the
tube and begin again.
• If the signs do not indicate placement in the lungs or stomach, advance the tube 5 cm (2 in.), and repeat the tests.
9. Secure the tube by taping it to the bridge of the client’s nose.
• If the client has oily skin, wipe the nose first with alcohol to
defat the skin.
• Apply a commercial securement device
or
• Cut 7.5 cm (3 in.) of tape, and split it lengthwise at one end,
leaving a 2.5-cm (1-in.) tab at the end.
• Place the tape over the bridge of the client’s nose, and
bring the split ends either under and around the tubing,
or under the tubing and back up over the nose. ❸
•
M46_BERM9793_11_GE_C46.indd 1216
12.
13.
14.
15.
Ensure that the tube is centrally located prior to securing with tape to maximize airflow and prevent irritation to
the side of the nares. Rationale: Taping in this manner
prevents the tube from pressing against and irritating the
edge of the nostril.
Once correct position has been determined, attach the tube to
a suction source or feeding apparatus as ordered, or clamp the
end of the tubing.
Secure the tube to the client’s gown.
• Loop an elastic band around the end of the tubing, and
attach the elastic band to the gown with a safety pin.
or
• Attach a piece of adhesive tape to the tube, and pin the
tape to the gown. Rationale: The tube is attached to prevent it from dangling and pulling.
• If a Salem sump tube is used, attach the antireflux valve to
the vent port (if used) and position the port above the client’s waist. Rationale: This prevents gastric contents from
flowing into the vent lumen.
• Remove and discard gloves.
• Perform hand hygiene.
Document relevant information: the insertion of the tube, the
means by which correct placement was determined, and client
responses (e.g., discomfort or abdominal distention).
Establish a plan for providing daily nasogastric tube care.
• Inspect the nostril for discharge and irritation.
• Clean the nostril and tube with moistened, cotton-tipped
applicators.
• Apply water-soluble lubricant to the nostril if it appears dry
or encrusted.
• Change the adhesive as required.
• Give frequent mouth care. Due to the presence of the tube,
the client may breathe through the mouth.
If suction is applied, ensure that the patency of both the nasogastric and suction tubes is maintained.
• Irrigation of the tube may be required at regular intervals.
In some agencies, irrigations must be ordered by the primary care provider. Prior to each irrigation, recheck tube
placement.
• If a Salem sump tube is used, follow agency policies for
irrigating the vent lumen with air to maintain patency of the
suctioning lumen. Often, a sucking sound can be heard
from the vent port if it is patent.
• Keep accurate records of the client’s fluid intake and output, and record the amount and characteristics of the
drainage.
Document the type of tube inserted, date and time of tube
insertion, type of suction used, color and amount of gastric
contents, and the client’s tolerance of the procedure.
03/02/2021 18:21
Chapter 46
●
Nutrition
1217
Inserting a Nasogastric Tube—continued
SAMPLE DOCUMENTATION
secured to nose. Pt. verbalizes understanding of need to not pull on
tube. L. Traynor, RN
EVALUATION
Conduct appropriate follow-up, such as degree of client comfort, client tolerance of the nasogastric tube, correct placement of
nasogastric tube in stomach, client understanding of restrictions,
color and amount of gastric contents if attached to suction, or stomach contents aspirated.
SKILL 46.1
11/5/2020 1030 #8 Fr feeding tube inserted without difficulty through
R nare with stylet in place. To x-ray to check placement. Radiologist
reports tube tip in stomach. Stylet removed. Aspirate pH 4. Tube
LIFESPAN CONSIDERATIONS Inserting a Nasogastric Tube
INFANTS AND YOUNG CHILDREN
• Restraints may be necessary during tube insertion and throughout therapy. Rationale: Restraints will prevent accidental dislodging of the tube.
• Place the infant in an infant seat or position the infant with a
rolled towel or pillow under the head and shoulders.
• When assessing the nares, obstruct one of the infant’s nares
and feel for air passage from the other. If the nasal passageway
is very small or is obstructed, an orogastric tube may be more
appropriate.
Measure appropriate nasogastric tube length from the nose to
the tip of the earlobe and then to the point midway between the
umbilicus and the xiphoid process.
• If an orogastric tube is used, measure from the tip of the earlobe to the corner of the mouth to the xiphoid process.
• Do not hyperextend or hyperflex an infant’s neck. Rationale:
Hyperextension or hyperflexion of the neck could occlude the
airway.
• Tape the tube to the area between the end of the nares and the
upper lip as well as to the cheek.
•
Although the focus of this chapter is nutrition, nasogastric tubes may be inserted for reasons other than to
provide a route for feeding the client, including these:
•
•
•
To prevent nausea, vomiting, and gastric distention following surgery. In this case, the tube is attached to a
suction source.
To remove stomach contents for laboratory analysis.
To lavage (wash) the stomach in cases of poisoning or
overdose of medications.
A nasoenteric (nasointestinal) tube , a longer tube
than the nasogastric tube (at least 40 cm [15.75 in.] for
an adult), is inserted through one nostril down into the
upper small intestine. See Figure 46.12A ■. Some agencies require specially trained nurses or primary care
providers to perform this procedure. Nasoenteric tubes
are used for clients who are at risk for aspiration. Clients at risk for aspiration are those who manifest the
following:
•
•
•
•
Decreased level of consciousness
Poor cough or gag reflexes
Inability to participate in the procedure
Restlessness or agitation.
Gastrostomy and jejunostomy devices are used for
long-term nutritional support, generally more than 6
to 8 weeks. Tubes are placed surgically or by laparoscopy through the abdominal wall into the stomach
(gastrostomy) or into the jejunum (jejunostomy). See
Figure 46.12B. A percutaneous endoscopic gastrostomy
(PEG) (Figure 46.13 ■) or percutaneous endoscopic
jejunostomy (PEJ) (Figure 46.14 ■) is created by using an
endoscope to visualize the inside of the stomach, making
M46_BERM9793_11_GE_C46.indd 1217
A
Nasogastric
Nasoduodenal
Nasojejunal
B
Gastrostomy
(placed surgically,
endoscopically,
or laparoscopically)
Jejunostomy
(placed surgically,
endoscopically,
or laparoscopically)
Figure 46.12 ■ Placements for enteral access: A, for nasoenteric
and nasointestinal tubes; B, for gastrostomy and jejunostomy tubes.
03/02/2021 18:21
1218
Unit 10
●
Promoting Physiologic Health
Figure 46.15 ■ Low-profile gastrostomy feeding tubes.
Cardinal Health.
A
tube can be used that remains in place (Figure 46.15 ■).
A feeding set is attached when needed.
Testing Feeding Tube Placement
B
Figure 46.13 ■ Percutaneous endoscopic gastrostomy (PEG) tube.
A, Cardinal Health.
Before feedings are introduced, tube placement is confirmed by radiography, particularly when a small-bore
tube has been inserted or when the client is at risk for
aspiration. After placement is confirmed, the nurse
marks the tube with indelible ink or tape at its exit point
from the nose and documents the length of visible tubing for baseline data. The nurse is responsible, however,
for verifying tube placement (i.e., GI placement versus
respiratory placement) before each intermittent feeding and at regular intervals (e.g., at least once per shift)
when continuous feedings are being administered. See
Skill 46.1, step 8.
Methods nurses use to check tube placement include
the following:
1. Aspirate GI secretions. Gastric secretions tend to be a
grassy-green, off-white, or tan color; intestinal fluid is
stained with bile and has a golden yellow or brownish
green color.
2. Measure the pH of aspirated fluid. Testing the pH of
aspirates can help distinguish gastric from respiratory
and intestinal placement as follows:
Gastric aspirates tend to have a pH of 1 to 5 but
may be as high as 6 if the client is receiving medications that control gastric acid.
• Small intestine aspirates generally have a pH equal
to or higher than 6.
• Respiratory secretions are more alkaline with values of 7 or higher. However, there is a slight possibility of respiratory placement when the pH
reading is as low as 5.
Therefore, when pH readings are 5 or higher,
radiographic confirmation of tube location needs to
be considered, especially in clients with diminished
cough and gag reflexes.
3. Confirm length of tube insertion with the insertion
mark. If more of the tube is now exposed, the position
of the tip should be questioned.
•
Figure 46.14 ■ Percutaneous endoscopic jejunostomy (PEJ) tube.
a puncture through the skin and subcutaneous tissues of
the abdomen into the stomach, and inserting the PEG or
PEJ catheter through the puncture.
The surgical opening is sutured tightly around the
tube or catheter to prevent leakage. Care of this opening
before it heals requires sterile technique. The catheter has
an external bumper and an internal inflatable retention balloon to maintain placement. When the tract is established
(about 1 month), the tube or catheter can be removed and
reinserted for each feeding. Alternatively, a skin-level
M46_BERM9793_11_GE_C46.indd 1218
03/02/2021 18:21
Chapter 46
●
Nutrition
1219
Currently, the most effective method is radiographic
verification of tube placement. Repeated x-ray studies,
however, are not feasible in terms of cost. More research
is required to devise effective alternatives, especially for
placement of small-bore tubes. In the meantime, nurses
should (a) ensure initial radiographic verification of smallbore tubes, (b) aspirate contents when possible and check
their acidity, (c) closely observe the client for signs of obvious distress, and (d) consider tube dislodgment after episodes of coughing, sneezing, and vomiting.
Enteral Feedings
The type and frequency of feedings and amounts to be
administered are ordered by the primary care provider.
Liquid feeding mixtures are available commercially or
may be prepared by the dietary department in accordance
with the primary care provider’s orders. A standard formula provides 1 Kcal per milliliter of solution with protein, fat, carbohydrate, minerals, and vitamins in specified
proportions.
Enteral feedings can be given intermittently or continuously. Intermittent feedings are the administration
of 300 to 500 mL of enteral formula several times per
day. The stomach is the preferred site for these feedings,
which are usually administered over at least 30 minutes. Initial intermittent feedings should be no more
than 120 mL. If tolerated, increase by 120 mL each feeding until the goal is reached (Morton & Fontaine, 2018).
Bolus intermittent feedings are those that use a syringe
to deliver the formula into the stomach. Because the
formula is delivered rapidly by this method, it is not
usually recommended but may be used in long-term
situations if the client tolerates it. These feedings must
be given only into the stomach; the client must be monitored closely for distention and aspiration.
Continuous feedings are generally administered
over a 24-hour period using an infusion pump (often
referred to as a kangaroo pump) that guarantees a
constant flow rate (Figure 46.16 ■). Initial continuous
feedings should be no more than 40 mL per hour. If
tolerated, increase by 20 mL each feeding until the goal
is reached (Morton & Fontaine, 2018). Continuous feedings are essential when feedings are administered in the
small bowel. Pumps are also used when smaller bore
gastric tubes are in place or when gravity flow is insufficient to instill the feeding.
Cyclic feedings are continuous feedings that are
administered in less than 24 hours (e.g., 12 to 16 hours).
These feedings, often administered at night, allow the
client to attempt to eat regular meals through the day.
Because nocturnal feedings may use higher nutrient densities and higher infusion rates than the standard continuous feeding, particular attention needs to be given to
monitoring fluid status and circulating volume.
Enteral feedings are administered to clients through
open or closed systems. Open systems use an open-top
container or a syringe for administration. Enteral feedings
for use with open systems are provided in flip-top cans
M46_BERM9793_11_GE_C46.indd 1219
Figure 46.16 ■ An enteric feeding pump.
or powdered formulas that are reconstituted with sterile
water. Sterile water, rather than tap water, reduces the risk
of microbial contamination. Open systems should have
no more than 8 hours of premixed formula or 4 hours
of reconstituted formula poured at one time (DeBruyne,
Pinna, & Whitney, 2016). At the completion of this time,
remaining formula should be discarded and the container
rinsed before new formula is poured. The bag and tubing should be replaced every 24 hours. Closed systems
consist of a prefilled container that is spiked with enteral
tubing and attached to the enteral access device. Prefilled
containers can hang safely for 48 hours if sterile technique
is used. Closed system materials are more expensive than
open system materials, but if nursing care costs and the
potential cost of infections resulting from contamination
are included, closed systems are less expensive (DeBruyne
et al., 2016).
A somewhat rare but potentially fatal complication
of tube feeding is refeeding syndrome—a combination of
fluid and electrolyte shifts that can occur after a lengthy
period of malnutrition or starvation. This syndrome can
occur when the starving body converts from creating
glucose from carbohydrates to creating it from protein
stores since carbohydrate was unavailable. The body’s
03/02/2021 18:21
1220
Unit 10
●
Promoting Physiologic Health
reaction to the sudden presence of glucose and synthesis of protein leads to the shifts. People at high risk for
developing refeeding syndrome are those with chronic
alcoholism, anorexia nervosa, massive weight loss,
cancer clients receiving chemotherapy, or anyone who
has gone 7 to 10 days without food. The nurse takes a
detailed history and examines laboratory data that can
indicate malnutrition, such as albumin and prealbumin
levels. Serum potassium, calcium, phosphate, and magnesium levels must be checked and supplemented until
within normal levels before feeding. Experts suggest
beginning feeding for at-risk clients with less than the
desired amount and increasing to the full desired daily
feeding slowly (Mullins, 2016).
Skill 46.2 provides the essential steps involved in
administering a tube feeding, and Skill 46.3 indicates the
steps involved in administering a gastrostomy or jejunostomy tube feeding.
Clinical Alert!
Enteral feedings should be started postoperatively in surgical clients without the need to wait for flatus or a bowel movement (Baird,
2016).
SKILL 46.2
Administering a Tube Feeding
PURPOSES
• To restore or maintain nutritional status
• To administer medications
ASSESSMENT
Assess
• For any clinical signs of malnutrition or dehydration.
• For allergies to any food in the feeding. If the client is lactose
intolerant, check the tube feeding formula. Notify the primary
care provider if any incompatibilities exist.
•
•
PLANNING
Before commencing a tube feeding, determine the type, amount, and
frequency of feedings and tolerance of previous feedings.
Assignment
Administering a tube feeding requires application of knowledge and
problem-solving and is not usually assigned to AP. Some agencies,
however, may allow a trained AP to administer a feeding if allowed
by law (for example, in California, APs are prohibited from performing tube feedings by the Nursing Practice Act). In any case, it is the
responsibility of the nurse to assess tube placement and determine
that the tube is patent; reinforce major points, such as making sure
the client is sitting upright; and instruct the AP to report any difficulty
administering the feeding or any complaints voiced by the client.
Equipment
• Correct type and amount of feeding solution
• 60-mL catheter-tip syringe
• Emesis basin
• Clean gloves
• pH test strip or meter
• Large syringe or calibrated plastic feeding bag with label and
tubing that can be attached to the feeding tube or prefilled
bottle with a drip chamber, tubing, and a flow-regulator clamp
• Measuring container from which to pour the feeding (if using
open system)
• Water (60 mL unless otherwise specified) at room temperature
• Feeding pump as required
For the presence of bowel sounds.
For any problems that suggest lack of tolerance of previous
feedings (e.g., delayed gastric emptying, abdominal distention,
diarrhea, cramping, or constipation).
Safety Alert!
SAFETY
Do not add colored food dye to tube feedings. Previously, blue dye
was often added to assist in recognition of aspiration. However, the
FDA reports cases of many adverse reactions to the dye, including
toxicity and death.
IMPLEMENTATION
Preparation
Assist the client to a Fowler’s position (at least 30° elevation) in
bed or a sitting position in a chair, the normal position for eating.
If a sitting position is contraindicated, a slightly elevated right sidelying position is acceptable. Rationale: These positions enhance
the gravitational flow of the solution and prevent aspiration of fluid
into the lungs.
Performance
1. Prior to performing the feeding, introduce self and verify the client’s identity using agency protocol. Explain to the client what
you are going to do, why it is necessary, and how to participate.
M46_BERM9793_11_GE_C46.indd 1220
Inform the client that the feeding should not cause any discomfort but may cause a feeling of fullness.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide privacy for this procedure if the client desires it. Tube
feedings are embarrassing to some clients.
4. Assess tube placement.
• Apply clean gloves.
• Attach the syringe to the open end of the tube and aspirate.
Check the pH.
03/02/2021 18:21
Chapter 46
●
Nutrition
1221
Administering a Tube Feeding—continued
Allow 1 hour to elapse before testing the pH if the client has
received a medication.
• Use a pH meter rather than pH paper if the client is receiving a continuous feeding. Follow agency policy if the pH is
equal to or greater than 6.
5. Assess residual feeding contents.
• If the tube is placed in the stomach, aspirate all contents
and measure the amount before administering the feeding.
Rationale: This is done to evaluate absorption of the last
feeding; that is, whether undigested formula from a previous feeding remains. If the tube is in the small intestine,
residual contents cannot be aspirated.
• If 100 mL (or more than half the last feeding) is withdrawn,
check with the primary care provider or refer to agency
policy before proceeding. The precise amount is usually determined by the primary care provider’s order or by
agency policy. Rationale: At some agencies, a feeding is
delayed when the specified amount or more of formula
remains in the stomach. Some guidelines allow for up to
500 mL residual before holding the next feeding (Houston &
Fuldauer, 2017).
or
• Reinstill the gastric contents into the stomach if this is the
agency policy or primary care provider’s order. Rationale:
Discarding the contents could disturb the client’s electrolyte
balance.
• If the client is on a continuous feeding, check the gastric
residual every 4 to 6 hours or according to agency protocol.
6. Administer the feeding.
• Before administering feeding:
a. Check the expiration date of the feeding.
b. Warm the feeding to room temperature. Rationale:
An excessively cold feeding may cause abdominal
cramps.
• When an open system is used, clean the top of the feeding
container with alcohol before opening it. Rationale: This
minimizes the risk of contaminants entering the feeding
syringe or feeding bag.
Feeding Bag (Open System)
• Apply a label that indicates the date, time of starting the feeding, and nurse’s initials on the feeding bag. Hang the labeled
bag from an infusion pole about 30 cm (12 in.) above the tube’s
point of insertion into the client.
• Clamp the tubing and add the formula to the bag.
• Open the clamp, run the formula through the tubing, and reclamp the tube. Rationale: The formula will displace the air in
the tubing, thus preventing the instillation of excess air into the
client’s stomach or intestine.
• Attach the bag to the feeding tube ❶ and regulate the drip
by adjusting the clamp to the drop factor on the bag (e.g.,
20 drops/mL) if not placed on a pump.
•
SKILL 46.2
Syringe (Open System)
• Remove the plunger from the syringe and connect the syringe
to a pinched or clamped nasogastric tube. Rationale: Pinching or clamping the tube prevents excess air from entering the
stomach and causing distention.
• Add the feeding to the syringe barrel. ❷
• Permit the feeding to flow in slowly at the prescribed rate.
Raise or lower the syringe to adjust the flow as needed. Pinch
or clamp the tubing to stop the flow for a minute if the client
❶ Using a calibrated plastic bag to administer a tube feeding.
❷ Using the barrel of a syringe to administer a tube feeding.
experiences discomfort. Rationale: Quickly administered feedings can cause flatus, cramps, or vomiting.
Prefilled Bottle with Drip Chamber (Closed System)
• Remove the screw-on cap from the container and attach the
administration set with tubing. ❸
• Close the clamp on the tubing.
• Hang the container on an IV pole about 30 cm (12 in.) above
the tube’s insertion point into the client.
❸ Feeding set with spike and tubing. Note, the special safety screw
spike and graduated connector prevent accidental connection to
intravenous tubing.
Cardinal Health.
Continued on page 1222
M46_BERM9793_11_GE_C46.indd 1221
03/02/2021 18:21
1222
Unit 10
●
Promoting Physiologic Health
Administering a Tube Feeding—continued
Squeeze the drip chamber to fill it to one-third to one-half of its
capacity.
• Open the tubing clamp, run the formula through the tubing, and
reclamp the tube. Rationale: The formula will displace the air in
the tubing, thus preventing the instillation of excess air.
• Attach the feeding set tubing to the feeding tube and regulate
the drip rate to deliver the feeding over the desired length of
time or attach to a feeding pump.
SKILL 46.2
•
7. If another bottle is not to be immediately hung, flush the
feeding tube before all of the formula has run through the
tubing.
• Instill 50 to 100 mL of water through the feeding tube or
medication port. Rationale: Water flushes the lumen of the
tube, preventing future blockage by formula.
• Be sure to add the water before the feeding solution has
drained from the neck of a syringe or from the tubing of an
administration set. Rationale: Adding the water before the
syringe or tubing is empty prevents the instillation of air into
the stomach or intestine and thus prevents unnecessary
distention.
8. Clamp the feeding tube.
• Clamp the feeding tube before all of the water is instilled.
Rationale: Clamping prevents air from entering the tube.
9. Ensure client comfort and safety.
• Secure the tubing to the client’s gown. Rationale: This
minimizes pulling of the tube, thus preventing discomfort
and dislodgment.
• Ask the client to remain sitting upright in Fowler’s position
or in a slightly elevated right lateral position for at least 30
minutes. Rationale: These positions facilitate digestion
and movement of the feeding from the stomach along the
alimentary tract, and prevent the potential aspiration of the
feeding into the lungs.
• Check the agency’s policy on the frequency of changing
the nasogastric tube and the use of smaller lumen tubes if a
large-bore tube is in place. Rationale: These measures prevent irritation and erosion of the pharyngeal and esophageal
mucous membranes.
10. Dispose of equipment appropriately.
• If the equipment is to be reused, wash it thoroughly with
soap and water so that it is ready for reuse.
• Change the equipment every 24 hours or according to
agency policy.
• Remove and discard gloves.
• Perform hand hygiene.
EVALUATION
Perform a follow-up examination of the following:
• Tolerance of feeding (e.g., nausea, cramping)
• Bowel sounds
• Regurgitation and feelings of fullness after feedings
• Weight gain or loss
• Fecal elimination pattern (e.g., diarrhea, flatulence, constipation)
• Skin turgor
M46_BERM9793_11_GE_C46.indd 1222
11. Document all relevant information.
• Document the feeding, including amount and kinds of
fluids administered (feeding plus any water used to flush
the tubing), duration of the feeding, and assessments of
the client.
• Record the volume of the feeding and water administered
on the client’s intake and output record.
12. Monitor the client for possible problems.
• Carefully assess clients receiving tube feedings for
problems.
• To prevent dehydration, give the client supplemental water
in addition to the prescribed tube feeding as ordered.
Variation: Continuous-Drip Feeding
• Clamp the tubing at least every 4 to 6 hours, or as indicated
by agency protocol or the manufacturer, and aspirate and
measure the gastric contents. Then flush the tubing with
30 to 50 mL of water. Rationale: This determines adequate
absorption and verifies correct placement of the tube. If
placement of a small-bore tube is questionable, a repeat
x-ray should be done.
• Determine agency protocol regarding withholding a feeding.
Many agencies withhold the feeding if more than 75 to 100 mL
of feeding is aspirated.
• To prevent spoilage or bacterial contamination, do not allow the
feeding solution to hang longer than 12 hours for an open system and 48 hours for a closed system. Check agency policy or
manufacturer’s recommendations regarding time limits.
• Follow agency policy regarding how frequently to change the
feeding bag and tubing. Changing the feeding bag and tubing
every 24 hours reduces the risk of contamination.
SAMPLE DOCUMENTATION
11/5/2020 1330 Aspirated 20 mL pale yellow fluid from NG tube,
pH 4.5. Client in Fowler’s position. 1 L room-temperature ordered
formula begun @ 60 mL/hour on pump. No nausea reported.
L. Traynor, RN
Urine output and specific gravity
Glucose and acetone in urine.
Relate findings to previous assessment data if available. Report
significant deviations from normal to the primary care provider.
•
•
03/02/2021 18:21
Chapter 46
●
Nutrition
1223
Administering an Intermittent Gastrostomy or Jejunostomy Feeding
PURPOSES
See Skill 46.2.
•
•
•
•
SKILL 46.3
ASSESSMENT
See Skill 46.2.
Planning
Before beginning a gastrostomy or jejunostomy feeding, determine
the type and amount of feeding to be instilled, frequency of feedings,
and any pertinent information about previous feedings (e.g., the positioning in which the client best tolerates the feeding).
Assignment
See Skill 46.2.
Equipment
• Correct amount of feeding solution
• Graduated container
• 60-mL catheter-tip syringe
Precut 4 *4 gauze squares
Uncut 4 *4 gauze squares
Paper tape
Extension tube with clamp for low-profile gastrostomy tube or
very short tube in place
For Tube Insertion
• Clean gloves
• Moisture-proof bag
• Water-soluble lubricant
• Feeding tube
For a Tube That Remains in Place
• Mild soap and water
• Clean gloves
• Petrolatum, zinc oxide ointment, or other skin protectant
IMPLEMENTATION
Preparation
See Skill 46.2.
Performance
1. Prior to performing the feeding, introduce self and verify the client’s identity using agency protocol. Explain to the client what
you are going to do, why it is necessary, and how to participate. Discuss how the results will be used in planning further
care or treatments.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures (e.g., clean gloves).
3. Provide for client privacy.
4. Insert a feeding tube, if one is not already in place.
• Wearing gloves, remove the dressing. Then discard the
dressing and gloves in the moisture-proof bag.
• Perform hand hygiene.
• Apply new clean gloves.
• Lubricate the end of the tube, and insert it into the ostomy
opening 10 to 15 cm (4 to 6 in.).
• For a low-profile gastrostomy, attach extension tubing.
5. Check the location and patency of the tube.
• Determine correct placement of the tube by aspirating
secretions and checking the pH.
• Follow agency policy for amount of residual formula. This
may include withholding the feeding, rechecking in 3 to
4 hours, or notifying the primary care provider if a large
residual remains.
• For continuous feedings, check the residual every 4 to 6
hours and hold feedings according to agency policy.
• Clamp the feeding tube. Remove the syringe plunger. Insert
the syringe barrel into the tube. Pour 15 to 30 mL of water
into the barrel, open the tube clamp, and allow the water to
flow into the tube. Rationale: This determines the patency
of the tube. If water flows freely, the tube is patent. Clamp
the tubing.
• If the water does not flow freely, notify the nurse in charge
or the primary care provider.
6. Administer the feeding.
• Hold the barrel of the syringe 7 to 15 cm (3 to 6 in.) above
the ostomy opening.
• Slowly pour the solution into the barrel, open the clamp,
and allow the solution to flow through the tube by gravity.
• Just before the syringe is empty, add 30 mL of water.
Rationale: Water flushes the tube and preserves its
patency.
• If the tube is to remain in place, hold it upright, remove
the syringe, and then clamp or plug the tube to prevent
leakage.
• If a tube was inserted for the feeding, remove it.
• Remove and discard gloves.
• Perform hand hygiene.
7. Ensure client comfort and safety.
• After the feeding, ask the client to remain in the sitting
position or a slightly elevated right lateral position for at
least 30 minutes. Rationale: This minimizes the risk of
aspiration.
• Assess status of peristomal skin. Rationale: Gastric or jejunal drainage contains digestive enzymes that can irritate the
skin. Document any redness and broken skin areas.
• Check orders about cleaning the peristomal skin, applying a skin protectant, and applying appropriate dressings.
Generally, the peristomal skin is washed with mild soap
and water at least once daily. The tube may be rotated
between thumb and forefinger to release any sticking and
promote tract formation. Petrolatum, zinc oxide ointment,
or other skin protectant may be applied around the stoma,
and precut 4 *4 gauze squares may be placed around the
tube. The precut squares are then covered with regular 4 *4
gauze squares, and the tube is coiled over them and taped
in place.
• Observe for common complications of enteral feedings:
aspiration, hyperglycemia, abdominal distention, diarrhea, and fecal impaction. Report findings to primary care
Continued on page 1224
M46_BERM9793_11_GE_C46.indd 1223
03/02/2021 18:21
1224
Unit 10
●
Promoting Physiologic Health
SKILL 46.3
Administering an Intermittent Gastrostomy or Jejunostomy Feeding—continued
provider. Often, a change in formula or rate of administration can correct problems.
• When appropriate, teach the client how to administer feedings and when to notify the healthcare provider concerning
problems.
8. Document all assessments and interventions.
SAMPLE DOCUMENTATION
1/24/2020 2045 No fluid aspirated from gastrostomy tube. Client in
Fowler’s position. 30 mL water flowed freely by gravity through tube.
250 mL room-temperature Ensure formula given over 20 minutes. No
complaints of discomfort. L. Traynor, RN
EVALUATION
See Skill 46.2.
LIFESPAN CONSIDERATIONS Administering a Tube Feeding
INFANTS AND YOUNG CHILDREN
• Feeding tubes may be removed after each feeding and reinserted at the next feeding to prevent irritation of the mucous
membrane, nasal airway obstruction, and stomach perforation
that may occur if the tube is left in place continuously. Check
agency practice.
• Orogastric feeding tubes may be preferred since infants are
nose-breathers (Rolfes et al., 2018).
• Formula should not be allowed to hang more than 4 hours
(DeBruyne & Pinna, 2017).
• Position a small child or infant in your lap, provide a pacifier,
and hold and cuddle the child during feedings. This promotes
comfort, supports the normal sucking instinct of the infant, and
facilitates digestion.
feedings. Decreased gastric emptying may necessitate checking frequently for gastric residual. Diarrhea from administering
the feeding too fast or at too high a concentration may cause
dehydration. If the feeding has a high concentration of glucose,
assess for hyperglycemia because with aging, the body has a
decreased ability to handle increased glucose levels.
• Conditions such as hiatal hernia and diabetes mellitus may
cause the stomach to empty more slowly. This increases the
risk of aspiration in a client receiving a tube feeding. Checking
for gastric residual more frequently can help document this if
it is an ongoing problem. Changing the formula or the rate of
administration, repositioning the client, or obtaining a primary
care provider’s order for a medication to increase stomach
emptying may resolve this problem.
OLDER ADULTS
• Physiologic changes associated with aging may make the older
adult more vulnerable to complications associated with enteral
EVIDENCE-BASED PRACTICE
Evidence-Based Practice
Will Increasing Nurses’ Knowledge Decrease the Need for
Long-Term Feeding Tube Reinsertions?
The authors of this study wanted to know if increasing nursing
home nurses’ knowledge of long-term gastrostomy or gastrojejunostomy feeding tube practices would decrease the frequency
of the need for tube reinsertion in their hospital interventional
radiology unit (Shipley, Gallo, & Fields, 2016). A 10-item pre- and
posttest method was used with the 1-hour educational in-service
between the tests. The in-service was based on numerous evidence-based reports of best practices in tube care. Although the
number of nurses who completed both tests was small (n = 16),
Before administering a tube feeding, the nurse must
determine any food allergies of the client and assess tolerance to previous feedings. Table 46.5 lists essential assessments to conduct before administering tube feedings. The
nurse must also check the expiration date on a commercially prepared formula or the preparation date and time
of agency-prepared solution, discarding any formula that
M46_BERM9793_11_GE_C46.indd 1224
there was a statistically significant increase in their knowledge
as measured on the posttest. Importantly, the number of tube
replacements after the intervention was half of those prior to
the study.
Implications
This was a small study using only two nursing homes and requires
replication with varied and larger samples. However, the nurses’
receptivity to the intervention and the significant decrease in the
need for tube reinsertion suggest an effective intervention. Nurses
are always learning, and techniques for preventing feeding tube
clogs and displacements are relevant learning topics.
has passed the expiration date or that was prepared more
than 24 hours previously.
Feedings are usually administered at room temperature unless the order specifies otherwise. The nurse warms
the specified amount of solution in a basin of warm water
or leaves it to stand for a while until it reaches room temperature. Because a formula that is warmed can grow
03/02/2021 18:21
Chapter 46
TABLE 46.5
●
Nutrition
1225
Assessing Clients Receiving Tube Feedings
Assessments
Rationale
Allergies to any food in the feeding
Common allergenic foods include milk, sugar, water, eggs, and
vegetable oil.
Bowel sounds before each feeding or, for continuous feedings,
every 4 to 8 hours
To determine intestinal activity.
Correct placement of tube before feedings
To prevent aspiration of feedings.
Presence of regurgitation and feelings of fullness after feedings
May indicate delayed gastric emptying, need to decrease quantity
or rate of the feeding, or high fat content of the formula.
Dumping syndrome: nausea, vomiting, diarrhea, cramps, pallor,
sweating, heart palpitations, increased pulse rate, and fainting after
a feeding
Clients with a jejunostomy may experience these symptoms, which
result when hypertonic foods and liquids suddenly distend the
jejunum. To make the intestinal contents isotonic, body fluids shift
rapidly from the client’s vascular system.
Abdominal distention, at least daily (Measure abdominal girth at the
umbilicus.)
Abdominal distention may indicate intolerance to a previous
feeding.
Diarrhea, constipation, or flatulence
The lack of bulk in liquid feedings may cause constipation. The
presence of hypertonic or concentrated ingredients may cause
diarrhea and flatulence.
Urine for sugar and acetone
Hyperglycemia may occur if the sugar content of the feeding is
too high.
Hematocrit and urine specific gravity
Both hematocrit and urine specific gravity increase as a result of
dehydration.
Serum BUN and sodium levels
Feeding formula may have a high protein content. If a high protein
intake is combined with an inadequate fluid intake, the kidneys may
not be able to excrete nitrogenous wastes adequately.
microorganisms, it should not hang longer than the manufacturer recommends. Excessively cold feedings can
reduce the flow of digestive juices by causing vasoconstriction and may cause cramps. Guidelines for teaching
clients and families regarding administration of tube feedings in the home are found in Client Teaching.
Managing Clogged Feeding Tubes
Even if feeding tubes are flushed with water before and
after feedings and medications, tubes still may become
clogged—especially SBFTs. This can occur when the feeding container runs dry, solid medication is not adequately
crushed, or medications are mixed with formula. Even the
important practice of aspirating to check residual volume
increases the incidence of clogging. To avoid the necessity
of removing the tube and reinserting a new tube, both prevention and intervention strategies must be used.
To prevent clogged feeding tubes, flush liberally (at
least 30 mL water) before, between, and after each separate
medication is instilled, using a 60-mL piston syringe. Too
great a pressure can rupture the tube—especially smallbore feeding tubes. Do not add medications to formula
or to each other because the combination could create a
precipitate that clogs the tube.
CLIENT TEACHING Tube Feedings
Clients and caregivers need the following instructions to manage
these feedings:
• Preparation of the formula. Include name of the formula and
how much and how often it is to be given; the need to inspect
the formula for expiration date and leaks and cracks in bags or
cans; how to mix or prepare the formula, if needed; and aseptic
techniques such as cleansing the container’s top with alcohol
before opening it, and changing the syringe administration set
every 24 hours.
• Proper storage of the formula. Include the need to refrigerate diluted or reconstituted formula and formula that contains
additives.
• Administration of the feeding. Include proper hand cleansing
technique, how to fill and hang the feeding bag, operation of an
infusion pump if indicated, the feeding rate, and client positioning during and after the feeding.
• Discuss strategies for hanging formula containers if an IV pole is
unavailable or inconvenient.
M46_BERM9793_11_GE_C46.indd 1225
•
•
•
•
•
Plan for optimal timing of feedings to allow for daily activities.
Many clients can tolerate having the majority of their feedings
run during sleep so they are free from the equipment during
the day.
Management of the enteral or parenteral access device. Include
site care; aseptic precautions; dressing change, as indicated;
how the site should look normally; and flushing protocols (e.g.,
type of irrigant and schedule).
Daily monitoring needs. Include temperature, weight, and intake
and output.
Signs and symptoms of complications to report. Include fever,
increased respiratory rate, decrease in urine output, increased
stool frequency or diarrhea, and altered level of consciousness.
Whom to contact about questions or problems. Include
emergency telephone numbers of home care agency, nursing
clinician, primary care provider, or 24-hour on-call emergency
service.
03/02/2021 18:21
1226
Unit 10
●
Promoting Physiologic Health
Many strategies have been used to try to unclog
feeding tubes. The first strategy that should be tried is to
reposition the client (this may allow a kink to straighten).
Alternately flush and aspirate the tube with water using
a 60-mL syringe. If the clog is in the external portion of
the tube, rolling it between the thumb and fingers may
help dislodge the block (Thompson, 2017). Do not flush
with juice or carbonated beverages (Shipley et al., 2016).
A combination of pancreatic enzymes and sodium
bicarbonate has been shown to be effective at unclogging
(Schallom, 2016).
If efforts to unclog a feeding tube are unsuccessful,
the tube may need to be removed. Skill 46.4 describes the
steps in removing a nasogastric tube.
SKILL 46.4
Removing a Nasogastric Tube
ASSESSMENT
Assess
• For the presence of bowel sounds
• For the absence of nausea or vomiting when tube is clamped
PLANNING
Assignment
Due to the need for assessment of client status, the skill of removing
a nasogastric tube is not assigned to AP.
IMPLEMENTATION
Preparation
• Confirm the primary care provider’s order to remove the tube.
• Assist the client to a sitting position if health permits.
• Place the disposable pad or towel across the client’s chest to
collect any spillage of secretions from the tube.
PERFORMANCE
1. Prior to performing the removal, introduce self and verify the
client’s identity using agency protocol. Explain to the client
what you are going to do, why it is necessary, and how to participate. Discuss how the results will be used in planning further
care or treatments.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures (e.g., clean gloves).
3. Provide for client privacy.
4. Detach the tube.
• Apply clean gloves.
• Disconnect the nasogastric tube from the suction apparatus, if present.
• Unpin the tube from the client’s gown.
• Remove the adhesive securing the tube to the nose.
5. Remove the nasogastric tube.
• Optional: Instill 50 mL of air or water into the tube.
Rationale: This clears the tube of any contents such as
feeding or gastric drainage.
• Ask the client to take a deep breath and to hold it.
Rationale: This closes the glottis, thereby preventing
accidental aspiration of any gastric contents.
• Pinch the tube with the gloved hand. Rationale: Pinching
the tube prevents any contents inside the tube from
draining into the client’s throat.
• Smoothly, withdraw the tube.
• Place the tube in the trash bag. Rationale: Placing the
tube immediately into the bag prevents the transference
EVALUATION
• Perform a follow-up examination, such as presence of bowel
sounds, absence of nausea or vomiting when tube is removed,
and intactness of tissues of the nares.
M46_BERM9793_11_GE_C46.indd 1226
Equipment
• Disposable pad or towel
• Tissues
• Clean gloves
• 60-mL syringe (optional)
• Moisture-proof trash bag
•
Provide tissues to the client to wipe the nose and mouth after
tube removal.
of microorganisms from the tube to other articles or
individuals.
• Observe the intactness of the tube. Rationale: This ensures
that no portion of the tube has broken off in the client.
6. Ensure client comfort.
• Provide mouth care.
• Assist the client as required to blow the nose. Rationale:
Excessive secretions may have accumulated in the nasal
passages.
7. Dispose of the equipment appropriately.
• Place the pad, bag with tube, and gloves in the biohazard
receptacle designated by the agency. Rationale: Correct
disposal prevents the transmission of microorganisms.
• Remove and discard gloves.
• Perform hand hygiene.
8. Document all relevant information.
• Record the removal of the tube, the amount and appearance of any drainage if connected to suction, and any relevant assessments of the client.
SAMPLE DOCUMENTATION
11/8/2020 1500 Complete NG tube removed intact without difficulty.
Oral & nasal care given. No bleeding or excoriation noted. Client
states is hungry & thirsty. 60 mL apple juice given. No c/o nausea.
L. Traynor, RN
•
•
Relate findings to previous assessment data if available.
Report significant deviations from normal to the primary care
provider.
03/02/2021 18:21
Chapter 46
Parenteral Nutrition
Parenteral nutrition, also referred to as total parenteral
nutrition (TPN) or intravenous hyperalimentation, is the
IV infusion of dextrose, water, fat, proteins, electrolytes,
vitamins, and trace elements. Because TPN solutions are
hypertonic (highly concentrated in comparison to the solute concentration of blood), they are injected only into
high-flow central veins, where they are diluted by the client’s blood.
TPN is a means of achieving an anabolic state in clients
who are unable to maintain a normal nitrogen balance.
Such clients may include those with severe malnutrition,
severe burns, bowel disease disorders (e.g., ulcerative colitis or enteric fistula), acute renal failure, hepatic failure,
metastatic cancer, or major surgeries where nothing may
be taken by mouth for more than 5 days.
TPN is not risk free. Infection prevention is of
utmost importance during TPN therapy. The nurse
must always observe aseptic technique when changing
solutions, tubing, dressings, and filters. Clients are at
increased risk of fluid, electrolyte, and glucose imbalances and require frequent evaluation and modification
of the TPN mixture.
TPN solutions are 10% to 50% dextrose in water, plus
a mixture of amino acids and special additives such as
vitamins (e.g., B complex, C, D, K), minerals (e.g., potassium,
sodium, chloride, calcium, phosphate, magnesium), and
trace elements (e.g., cobalt, zinc, manganese). Additives are
modified to each client’s nutritional needs. Fat emulsions
may be given to provide essential fatty acids to correct or
prevent essential fatty acid deficiency or to supplement
the calories for clients who, for example, have high calorie
needs or cannot tolerate glucose as the only calorie source.
Note that 1000 mL of 5% glucose or dextrose contains
50 grams of sugar. Thus, a liter of this solution provides
less than 200 calories!
Because TPN solutions are high in glucose, infusions
are started gradually to prevent hyperglycemia. The client
needs to adapt to TPN therapy by increasing insulin output from the pancreas. For example, an adult client may
be given 1 liter (40 mL/h) of TPN solution the first day; if
the infusion is tolerated, the amount may be increased to
M46_BERM9793_11_GE_C46.indd 1227
●
Nutrition
1227
2 liters (80 mL/h) for 24 to 48 hours, and then to 3 liters
(120 mL/h) within 3 to 5 days. Glucose levels are monitored during the infusion.
When TPN therapy is to be discontinued, the TPN
infusion rates are decreased slowly to prevent hyperinsulinemia and hypoglycemia. Weaning a client from TPN
may take up to 48 hours but can occur in 6 hours as long
as the client receives adequate carbohydrates either orally
or intravenously.
Peripheral parenteral nutrition (PPN) is delivered
into the smaller peripheral veins. PPN cannot handle as
concentrated a solution as central lines, but can accommodate lipids. For example, a 20% lipid emulsion can
provide nearly 2000 Kcal/day through a peripheral vein.
PPN is considered to be a safe and convenient form of
therapy. One major disadvantage, however, is the frequent
incidence of phlebitis (vein inflammation) associated with
PPN. Peripheral parenteral nutrition is administered to
clients whose needs for IV nutrition will last only a short
time or in whom placement of a central IV catheter is contraindicated. It is a form of therapy used more frequently
to prevent nutritional deficits than to correct them.
Enteral or parenteral feedings may be continued
beyond hospital care in the client’s home or may be initiated in the home.
Evaluating
The goals established in the planning phase are evaluated
according to specific desired outcomes, also established
in that phase. If the outcomes are not achieved, the nurse
should explore the reasons. The nurse might consider the
following questions:
•
•
•
•
•
•
Was the cause of the problem correctly identified?
Was the family included in the teaching plan? Are family members supportive?
Is the client experiencing symptoms that cause loss of
appetite (e.g., pain, nausea, fatigue)?
Were the outcomes unrealistic for this client?
Were the client’s food preferences considered?
Is anything interfering with digestion or absorption of
nutrients (e.g., diarrhea)?
03/02/2021 18:21
1228
Unit 10
●
Promoting Physiologic Health
NURSING CARE PLAN Nutrition
ASSESSMENT DATA
NURSING DIAGNOSIS
DESIRED OUTCOMES*
NURSING ASSESSMENT
Mrs. Rose Santini, a 59-year-old homemaker, attends a community hospital–sponsored health fair. She approaches the
nutrition information booth, and the clinical specialist in nutritional support gathers a nutritional history. Mrs. Santini is very
upset about her 9-kg (20-lb) weight gain. She relates to the
nurse clinician that since the death of her husband 1 month ago
she has lost interest in many of her usual physical and social
activities. She no longer attends YMCA exercise and swimming
sessions and has lost contact with her couple’s bridge group.
Mrs. Santini states she is bored, depressed, and very unhappy
about her appearance. She has a small frame and has always
prided herself on her petite figure. She says her eating habits
have changed considerably. She snacks while watching TV and
rarely prepares a complete meal.
Overweight related to excess
intake and decreased activity
expenditure (as evidenced by
weight gain of 9 kg [20 lb], triceps
skinfold greater than normal, undesirable eating patterns)
Weight-Loss Behavior [1627] as
evidenced by demonstrating:
• Eats three meals each day that
result in a 500-calorie reduction
in intake.
• Establishes a physical exercise
plan that engages her in 15 to
20 minutes of exercise daily by
day 5.
• Identifies eating habits that contribute to weight gain by day 2.
Physical Examination
Diagnostic Data
Height: 162.6 cm (5′4″)
CBC normal, urinalysis
Weight: 66 kg (145 lb)
negative, chest x-ray
Temperature: 37°C (98.6°F)
negative, thyroid profile
Pulse: 76 beats/min
within normal limits
Respirations: 16/min
Blood pressure: 144/84 mmHg
Triceps skinfold: 21 mm
Small frame, weight in excess
of 10% over ideal for height and
frame
NURSING INTERVENTIONS*/SELECTED ACTIVITIES
RATIONALE
WEIGHT REDUCTION ASSISTANCE [1280]
Determine current eating patterns by having Mrs. Santini keep a
diary of what, when, and where she eats.
Increases awareness of activities and foods that contribute to excessive
intake.
Set a weekly goal for weight loss.
The desirable weight-loss rate is 1/2–1 kg (1–2 lb) per week.
Encourage use of internal reward systems when goals are
accomplished.
Goal setting provides motivation, which is essential for a successful
weight-loss program.
Set a realistic plan with Mrs. Santini to include reduced food
intake and increased energy expenditure.
A combined plan of calorie reduction and exercise can enhance weight
loss since exercise increases caloric utilization.
Assist client to identify motivation for eating and internal and
external cues associated with eating.
Awareness of factors that contribute to overeating will assist the individual in planning behavior modification techniques to avoid situations that
prompt excess food consumption.
Encourage attendance at support groups for weight loss or
refer to a community weight-control program.
Membership in a support group can enhance clients’ continuation of
weight-loss efforts.
Develop a daily meal plan with a well-balanced diet, reduced
calories, and reduced fat.
Snack foods tend to be high in calories and fat and low in nutritional
values.
NURSING INTERVENTIONS*/SELECTED ACTIVITIES
RATIONALE
NUTRITIONAL COUNSELING [5246]
Facilitate identification of eating behaviors to be changed.
Increases individual’s awareness of those actions that contribute to
excessive intake.
Use accepted nutritional standards to assist Mrs. Santini in
evaluating adequacy of dietary intake.
Comparing the individual’s dietary history with nutritional standards will
facilitate identification of nutritional deficiencies or excesses.
Help Mrs. Santini to consider factors of age, past eating experi- Social, economic, physical, and psychologic factors play a role in nutriences, culture, and finances in planning ways to meet nutritional tion and malnutrition.
requirements.
M46_BERM9793_11_GE_C46.indd 1228
03/02/2021 18:21
Chapter 46
●
Nutrition
1229
NURSING CARE PLAN Nutrition—continued
Discuss Mrs. Santini’s knowledge of the basic food groups, as
well as perceptions of the needed diet modification.
Helps to determine the client’s knowledge base and identify misconceptions and gaps in understanding.
Discuss food likes and dislikes.
Incorporating Mrs. Santini’s food preferences into the dietary plan will
promote adherence to the weight-loss program.
Assist Mrs. Santini in stating her feelings and concerns about
goal achievement.
Fear of success, failure, or other concerns may block goal achievement.
BEHAVIOR MODIFICATION [4360]
Assist Mrs. Santini to identify strengths and reinforce these.
Reinforcing strengths enhances self-esteem and encourages the individual to draw on these assets during the weight-loss program.
Encourage her to examine her own behavior.
Involving Mrs. Santini in self-appraisal will promote identification of
behaviors that may be contributing to excessive caloric intake.
Identify the behavior to be changed in specific, concrete terms
(e.g., stop snacking in front of the TV).
Identification of specific behaviors is essential for planning behavior
modification.
Consider that it is easier to increase a behavior than to
decrease a behavior (e.g., increase activities or hobbies that
involve the hands such as sewing versus decreasing TV
snacking).
Habitual behaviors are difficult to change. Breaking old habits may be
easier if viewed from the standpoint of increasing an enjoyable, healthy
activity.
Choose reinforcers that are meaningful to Mrs. Santini.
Positive reinforcement is not likely to be an effective part of behavior
modification if the reinforcer is meaningless to the individual.
EVALUATION
Outcome met. Mrs. Santini kept a dietary log for 5 days and has eaten balanced meals each day, resulting in a daily deficit of 400 to 500
calories. She is aware that she eats excessively because she is bored and depressed. She has reestablished her former social contacts
including her church bridge club. Mrs. Santini has purchased a stationary bicycle and exercises 20 minutes daily. She enrolled in a knitting
class that meets two nights per week. She has lost 2/3 kg (1 1/2 lb) in the past week. As a reward, Mrs. Santini renewed her membership
to the YMCA.
*The NOC # for desired outcomes and the NIC # for nursing interventions are listed in brackets following the appropriate outcome or intervention. Outcomes, interventions,
and activities selected are only a sample of those suggested by NOC and NIC and should be further individualized for each client.
APPLYING CRITICAL THINKING
1. How do Mrs. Santini’s personal characteristics influence her nutritional needs?
2. What further information do you need regarding Mrs. Santini’s present diet?
3. Offer suggestions for ways to modify Mrs. Santini’s tendency to snack.
4. Mrs. Santini asks what her weight should be. How do you respond?
Answers to Applying Critical Thinking questions are available on the student resources site. Please consult with your instructor.
M46_BERM9793_11_GE_C46.indd 1229
03/02/2021 18:21
1230
Unit 10
●
Promoting Physiologic Health
CONCEPT MAP
Nutrition
RS
outcome
Outcome met:
c
c
to T
c
T TV
M46_BERM9793_11_GE_C46.indd 1230
03/02/2021 18:21
Chapter 46
●
Nutrition
1231
Chapter 46 Review
CHAPTER HIGHLIGHTS
• Essential nutrients are grouped into categories: carbohydrates, pro-
• Assessment of nutritional status may involve all or some of the fol-
teins, lipids, vitamins, and minerals.
Nutrients serve three basic purposes: forming body structures
(such as bones and blood), providing energy, and helping to regulate the body’s biochemical reactions.
The amount of energy that nutrients or foods supply to the body
is their caloric value. The basal metabolic rate (BMR) is the rate
at which the body metabolizes food to maintain the energy and
requirements of an individual who is awake and at rest. The amount
of energy required to maintain basic body functions is referred to as
the resting energy expenditure (REE).
An individual’s state of energy balance can be determined by comparing caloric intake with caloric expenditure.
Ideal body weight (IBW) is the optimal weight recommended for
optimal health.
Body mass index (BMI) and percentage of body fat are indicators
of changes in body fat stores. They indicate whether an individual’s
weight is appropriate for height and may provide a useful estimate
of nutrition.
Factors influencing an individual’s nutrition include development, gender, ethnicity and culture, beliefs about foods, personal preferences,
religious practices, lifestyle, economics, medications and therapy,
health, alcohol consumption, advertising, and psychologic factors.
Nutritional needs vary considerably according to age, growth, and
energy requirements. Adolescents have high energy requirements
due to their rapid growth; a diet plentiful in milk, meats, green and
yellow vegetables, and fresh fruits is required. Middle-aged adults
and older adults often need to reduce their caloric intake because
of decreases in metabolic rate and activity levels.
Various daily food guides have been developed to help healthy
individuals meet the daily requirements of essential nutrients and
to facilitate meal planning. These include the Dietary Guidelines for
Americans and MyPlate.
Both inadequate and excessive intakes of nutrients result in malnutrition. The effects of malnutrition can be general or specific,
depending on which nutrients and what level of deficiency or
excess are involved.
lowing: nutritional screening, nursing history data, anthropometric
measurements, biochemical (laboratory) data, clinical data (physical
examination), calculation of the percentage of weight loss, and a
dietary history.
Nursing diagnoses for clients with nutritional problems may be
broadly stated as insufficient dietary intake or overweight. Because
nutritional problems may affect many other areas of human functioning, a nutritional problem may be the etiology of other diagnoses, such as constipation and low self-esteem.
Major goals for clients with or at risk for nutritional problems
include the following: Maintain or restore optimal nutritional status,
decrease or regain specified weight, promote healthy nutritional
practices, and prevent complications associated with malnutrition.
Assisting clients and support persons with therapeutic diets is a
function shared by the nurse and the dietitian. The nurse reinforces
the dietitian’s instructions, assists the client to make beneficial
changes, and evaluates the client’s response to planned changes.
Because many hospitalized clients have poor appetites, a major
responsibility of the nurse is to provide nursing interventions that
stimulate their appetites.
Whenever possible, the nurse should help incapacitated clients to
feed themselves; a number of self-feeding aids help clients who
have difficulty handling regular utensils.
The nurse can refer clients to various community programs that help
special subgroups of the population meet their nutritional needs.
Enteral feedings, administered through nasogastric, nasointestinal,
gastrostomy, or jejunostomy tubes, are provided when the client is
unable to ingest foods or the upper GI tract is impaired.
A nasogastric or nasointestinal tube is used to provide enteral nutrition for short-term use. A gastrostomy or jejunostomy tube can be
used to supply nutrients via the enteral route for long-term use.
The two most accurate methods of confirming GI tube placement
are radiographs and pH testing of aspirate.
Parenteral nutrition, provided when oral intake is insufficient or
unadvisable, is given intravenously into a large central vein (e.g.,
the superior vena cava).
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
TEST YOUR KNOWLEDGE
1. A client receives several tube feedings each day. After
documenting the client’s tolerance of the feedings and
assessments in the medical record, on which of the following
should a nurse also document the amount fed?
1. Graphic sheet
2. Dietary consultation notes
3. Vital signs record
4. Intake and output record
2. An adult reports usually eating 3 cups dairy, 2 cups fruit, 2 cups
vegetables, 5 ounces grains, and 5 ounces meat each day. The
nurse would counsel the client to:
M46_BERM9793_11_GE_C46.indd 1231
1. Maintain the diet; the servings are adequate.
2. Increase the number of servings of dairy.
3. Decrease the number of servings of vegetables.
4. Increase the number of servings of grains.
3. A nurse completes measuring the triceps skinfold of a client. In
order to obtain the most meaningful data, how soon should the
nurse repeat this measurement?
1. Two days
2. Ten days to two weeks
3. One month
4. One year
03/02/2021 18:21
1232
Unit 10
●
Promoting Physiologic Health
4. A client begins to gag and cough as a nasogastric tube is
passed into his oropharynx. What is the correct nursing action?
1. Remove the tube and attempt reinsertion.
2. Give the client a few sips of water.
3. Use firm pressure to pass the tube through the glottis.
4. Have the client tilt the head back to open the passage.
5. What is the proper technique with gravity tube feeding?
1. Hang the feeding bag 1 foot higher than the tube’s insertion
point into the client.
2. Administer the next feeding only if there is less than 25 mL of
residual volume from the previous feeding.
3. Place client in the left lateral position.
4. Administer feeding directly from the refrigerator.
6. A 55-year-old female is about 9 kg (20 lb) over her desired
weight. She has been on a “low-calorie” diet with no improvement. Which statement reflects a healthy approach to the
desired weight loss? “I need to:
1. Increase my exercise to at least 30 minutes every day.”
2. Switch to a low-carbohydrate diet.”
3. Keep a list of my forbidden foods on hand at all times.”
4. Buy more organic and less processed foods.”
7. An older Asian client has mild dysphagia from a recent stroke.
The nurse plans the client’s meals based on the need to:
1. Have at least one serving of thick dairy (e.g., pudding, ice
cream) per meal.
2. Eliminate the beer usually ingested every evening.
3. Include as many of the client’s favorite foods as possible.
4. Increase the calories from lipids to 40%.
8. Two months ago a client weighed 195 pounds. The current
weight is 182 pounds. Calculate the client’s percentage of
weight loss and determine its significance.
______ % weight loss
1. Not significant
2. Significant weight loss
3. Severe weight loss
4. Unable to determine significance
9. Which of the sites on the diagram below indicates the correct
location for the tip of a small-bore nasally placed feeding tube?
1
2
3
4
Gastrointestinal tract
10. Which meal would the nurse recommend to the client as highest
in calcium, iron, and fiber?
1. 3 ounces cottage cheese with 1/3 cup raisins and 1 banana
2. 1/2 cup broccoli with 3 ounces chicken and 1/2 cup
peanuts
3. 1/2 cup spaghetti with 2 ounces ground beef and 1/2 cup
lima beans plus 1/2 cup ice cream
4. 3 ounces tuna plus 1 ounce cheese sandwich on wholewheat bread plus a pear
See Answers to Test Your Knowledge in Appendix A.
READINGS AND REFERENCES
Suggested Reading
Ojo, O. (2017). Providing optimal enteral nutrition support in
the community. British Journal of Community Nursing,
22(5), 218–221. doi:10.12968/bjcn.2017.22.5.218
There are increasing numbers of clients receiving tubebased nutrition in the home. This article describes the role
of the nurse in screening for dysphagia and malnutrition
and managing feeding tubes.
Related Research
Gerritsen, A., de Rooij, T., Dijkgraaf, M. G., Busch, O. R.,
Bergman, J. J., Ubbink, D. T., . . . Besselink, M. G. (2016).
Electromagnetic-guided bedside placement of nasoenteral
feeding tubes by nurses is non-inferior to endoscopic
placement by gastroenterologists: A multicenter randomized controlled trial. American Journal of Gastroenterology,
111, 1123–1132. doi:10.1038/ajg.2016.224
References
American Dietetic Association. (2002). National dysphagia diet:
Standardization for optimal care. Chicago, IL: Author.
Baird, M. S. (2016). Manual of critical care nursing: Nursing
interventions and collaborative management (7th ed.).
St. Louis, MO: Elsevier.
Butcher, H. K., Bulechek, G. M., Dochterman, J. M., &
Wagner, C. M. (Eds.). (2018). Nursing interventions classification (NIC) (7th ed.). St. Louis, MO: Elsevier.
Centers for Disease Control and Prevention. (2017). Botulism:
Prevention. Retrieved from https://www.cdc.gov/botulism/
prevention.html
M46_BERM9793_11_GE_C46.indd 1232
Cichero, J. A. Y., Lam, P., Steele, C. M., Hanson, B., Chen, J.,
Dantas, R. O., . . . Stanschus, S. (2017). Development of
international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: The IDDSI Framework. Dysphagia, 32, 293–314.
doi:10.1007/s00455-016-9758-y
DeBruyne, L. K., & Pinna, K. (2017). Nutrition for health and
healthcare (6th ed.). Boston, MA: Cengage.
DeBruyne, L. K., Pinna, K., & Whitney, E. (2016). Nutrition and
diet therapy (9th ed.). Boston, MA: Cengage.
Fryar, C. D., Gu, Q., Ogden, C. L., & Flegal, K. M. (2016).
Anthropometric reference data for children and adults:
United States, 2011–2014. National Center for Health
Statistics. Vital and Health Statistics, 3(39). Retrieved from
https://www.cdc.gov/nchs/data/series/sr_03/sr03_039.pdf
Gerritsen, A., de Rooji, T., Mijkgraaf, M. C., Busch, O. R.,
Bergman, J. J., Ubbink, D. T., . . . . Besselink, M. J. (2016).
Electromagnetic-guided bedside placement of nasoenteral
feeding tubes by nurses is non-inferior to endoscopic
placement by gastroenterologists: A multicenter randomized controlled trial. American Journal of Gastroenterology,
111, 1123–1132. doi:10.1038/ajg.2016.224
Houston, A., & Fuldauer, P. (2017). Enteral feeding: Indications,
complications, and nursing care. American Nurse Today,
12(1), 20–25.
Lyman, B., Peyton, C., & Healey, F. (2018). Reducing nasogastric tube misplacement through evidence-based practice:
Is your practice up-to-date? American Nurse Today,
13(11), 6–11.
Moorhead, S., Johnson, M., Maas, M. L., & Swanson, E.
(Eds.). (2019). Nursing outcomes classification (NOC) (6th
ed.). St. Louis, MO: Mosby Elsevier.
Morton, P. G., & Fontaine, D. K. (2018). Critical care nursing: A
holistic approach (11th ed.). Philadelphia, PA: Wolters Kluwer.
Mullins, A. (2016). Refeeding syndrome: Clinical guidelines for
safe prevention and treatment. Support Line, 38(1), 10–13.
National Heart, Lung, and Blood Institute. (n.d.). Aim for a
healthy weight: Classification of overweight and obesity by
BMI, waist circumference, and associated disease risks.
Washington, DC: U.S. Department of Health & Human
Services. Retrieved from http://www.nhlbi.nih.gov/health/
public/heart/obesity/lose_wt/bmi_dis.htm
National Institutes of Health Office of Dietary Supplements.
(n.d.). Nutrient recommendations: Dietary reference
intakes. Retrieved from https://ods.od.nih.gov/Health_Information/Dietary_Reference_Intakes.aspx
Nelms, M. N., Sucher, K. P., & Lacey, K. (2016). Nutrition therapy and pathophysiology (3rd ed.). Boston, MA: Cengage.
Nutrition Screening Initiative. (2008). Determine your nutritional
health. Washington, DC: National Council on Aging.
Ogden, C. L., Carroll, M. D., Lawman, H. G., Fryar, C. D.,
Kruszon-Moran, D., Kit, B. K., & Flegal, K. M. (2016). Trends
in obesity prevalence among children and adolescents in the
United States, 1988–1994 through 2013–2014. JAMA, 315,
2292–2299. doi:10.1001/jama.2016.6361
Rolfes, S. R., Pinna, K., & Whitney, E. (2018). Understanding normal and clinical nutrition (11th ed.). Stamford, CT:
Cengage.
03/02/2021 18:21
Chapter 46
Schallom, M. (2016). How to recognize, prevent, and troubleshoot mechanical complications of enteral feeding tubes.
American Nurse Today, 11(2), 1–7.
Shipley, K., Gallo, A.-M., & Fields, W. (2016). Is your feeding
tube clogged? Maintenance of gastrostomy and gastrojejunostomy tubes. MEDSURG Nursing, 25(4), 224–228.
Solomon, R., & Jurica, K. (2017). Closing the research-practice
gap: Increasing evidence-based practice for nasogastric tube insertion using education and an electronic
order set. Journal of Emergency Nursing, 43, 133–137.
doi:10.1016/j.jen.2016.09.001
Spatz, D. L. (2017). SPN position statement: The role of
pediatric nurses in the promotion and protection of human
milk and breastfeeding. Journal of Pediatric Nursing, 37,
136–139. doi:10.1016/j.pedn.2017.08.031
Thompson, R. (2017). Troubleshooting PEG feeding tubes in
the community setting. Journal of Community Nursing,
31(2), 61–66.
M46_BERM9793_11_GE_C46.indd 1233
U.S. Department of Health and Human Services & U.S.
Department of Agriculture. (2015). 2015–2020 dietary
guidelines for Americans (8th ed.). Retrieved from http://
health.gov/dietaryguidelines/2015/guidelines/
U.S. Department of Health and Human Services. (2019).
Healthy People 2020 nutrition and weight status: Objectives. Retrieved from http://www.healthypeople.gov/2020/
topics-objectives/topic/nutrition-and-weight-status
U.S. Food and Drug Administration. (2018). New and improved
nutrition facts label—key changes. Retrieved from https://
www.fda.gov/files/food/published/The-New-and-ImprovedNutrition-Facts-Label-%E2%80%93-Key-Changes.pdf
Selected Bibliography
Lyman, B. (2019). Challenge 15: Nasogastric feeding and drainage tube placement and verification.
Retrieved from https://patientsafetymovement.
●
Nutrition
1233
org/actionable-solutions/challenge-solutions/
nasogastric-tube-ngt-placement-and-verification
National Academies of Sciences, Engineering, and Medicine.
(2017). Nutrition across the lifespan for healthy aging:
Proceedings of a workshop. Washington, DC: National
Academies Press. doi:10.17226/24735
Peterson, C. M., Thomas, D. M., Blackburn, G. L., & Heymsfield, S. B. (2016). Universal equation for estimating ideal
body weight and body weight at any BMI. American
Journal of Clinical Nutrition, 103, 1197–1203. doi:10.3945/
ajcn.115.121178
Roth, R. A. (2018). Nutrition and diet therapy (12th ed.).
Clifton Park, NY: Cengage. doi:10.12968/bjcn.2015.20.
Sup6a.S24
Wyer, N. (2017). Parenteral nutrition: Indications and safe management. British Journal of Community Nursing, 22(Suppl. 7),
S22–S28. doi:10.12968/bjcn.2017.22.Sup7.S22
03/02/2021 18:21
47
Urinary Elimination
LEA R NIN G OU TC OME S
After completing this chapter, you will be able to:
1. Describe the process of urination, from urine formation through
micturition.
2. Identify factors that influence urinary elimination.
3. Identify common causes of selected urinary problems.
4. Describe nursing assessment of urinary function, including
subjective and objective data.
5. Identify normal and abnormal characteristics and constituents
of urine.
6. Develop nursing diagnoses and desired outcomes related to
urinary elimination.
7. Describe nursing interventions to maintain normal urinary
elimination, prevent urinary tract infection, and manage urinary incontinence.
8. Delineate ways to prevent urinary infection.
9. Explain the care of clients with indwelling catheters or urinary
diversions.
10. Verbalize the steps used in:
a. Applying an external urinary device
b. Performing urinary catheterization
c. Performing bladder irrigation.
11. Recognize when it is appropriate to assign aspects of urinary
elimination to assistive personnel.
12. Demonstrate appropriate documentation and reporting of
applying an external catheter, performing urethral urinary catheterization, and performing bladder irrigation.
K EY T ER M S
anuria, 1239
bladder retraining, 1247
blood urea nitrogen (BUN), 1243
CAUTI, 1250
creatinine clearance, 1243
Credé’s maneuver, 1250
detrusor muscle, 1235
diuresis, 1238
diuretics, 1238
dysuria, 1240
enuresis, 1240
flaccid, 1250
habit training, 1247
ileal conduit, 1264
irrigation, 1259
meatus, 1235
micturition, 1236
nephrostomy, 1263
neurogenic bladder, 1240
Introduction
Elimination from the urinary tract is usually taken for
granted. Only when a problem arises do most individuals
become aware of their urinary habits and any associated
symptoms.
An individual’s urinary habits depend on social
culture, personal habits, and physical abilities. In North
America, most individuals are accustomed to privacy
and clean (even decorative) surroundings while they
urinate.
Personal habits regarding urination are affected by the
social politeness of leaving to urinate, the availability of a
private clean facility, and initial bladder training. Urinary
elimination is essential to health, and voiding can be postponed for only so long before the urge normally becomes
too great to control.
nocturia, 1239
nocturnal enuresis, 1240
oliguria, 1239
polydipsia, 1239
polyuria, 1238
postvoid residual (PVR), 1243
reflux, 1235
suprapubic catheter, 1262
trigone, 1235
ureterostomy, 1263
urgency, 1239
urinary frequency, 1239
urinary hesitancy, 1240
urinary incontinence (UI), 1240
urinary retention, 1240
urination, 1236
vesicostomy, 1263
voiding, 1236
Physiology of Urinary
Elimination
Urinary elimination depends on the effective functioning
of the upper urinary tract’s kidneys and ureters and the
lower urinary tract’s urinary bladder, urethra, and pelvic
floor (Figure 47.1 ■).
Kidneys
The paired kidneys are situated on either side of the spinal
column, behind the peritoneal cavity. The right kidney is
slightly lower than the left due to the position of the liver.
They are the primary regulators of fluid and acid–base balance in the body. The functional units of the kidneys, the
nephrons, filter the blood and remove metabolic wastes.
1234
M47_BERM9793_11_GE_C47.indd 1234
27/01/2021 18:07
Chapter 47
Cavernous (penile) urethra
Adrenal gland
●
Urinary Elimination
1235
Bladder
Diaphragm
10th rib
11th rib
Prostate
12th rib
Hilum
Abdominal aorta
Testis
Epididymis
Vena cava
Ureter
urethra
Glans
Membranous
urethra
Figure 47.2 ■ The male urogenital system.
Rectum
Uterus
Trigone
Urinary
bladder
Internal
Bladder detrusor
muscle
Urethra
Figure 47.1 ■ Anatomic structures of the urinary tract.
Symphysis
pubis
Urethra
Pelvic muscles
Vagina
Figure 47.3 ■ The female urogenital system.
In the average adult 1200 mL of blood, or about 21% of the
cardiac output, passes through the kidneys every minute.
Each kidney contains approximately 1 million nephrons.
Ureters
Once the urine is formed in the kidneys, it moves through
the collecting ducts into the calyces of the renal pelvis and
from there into the ureters. In adults the ureters are from
25 to 30 cm (10 to 12 in.) long and about 1.25 cm (0.5 in.) in
diameter. The upper end of each ureter is funnel shaped as
it enters the kidney. The lower ends of the ureters enter the
bladder at the posterior corners of the floor of the bladder
(see Figure 47.1). At the junction between the ureter and
the bladder, a flaplike fold of mucous membrane acts as a
valve to prevent reflux (backflow) of urine up the ureters.
Bladder
The urinary bladder is a hollow, muscular organ that
serves as a reservoir for urine and as the organ of excretion. When empty, it lies behind the symphysis pubis. In
men, the bladder lies in front of the rectum and above the
prostate gland (Figure 47.2 ■); in women it lies in front of
the uterus and vagina (Figure 47.3 ■).
The wall of the bladder is made up of smooth muscle
layers called the detrusor muscle. The detrusor muscle
allows the bladder to expand as it fills with urine, and to
contract to release urine to the outside of the body during
voiding. The trigone at the base of the bladder is a triangular area marked by the ureter openings at the posterior corners and the opening of the urethra at the anterior
inferior corner (see Figure 47.1).
M47_BERM9793_11_GE_C47.indd 1235
The bladder is capable of considerable distention
because of rugae (folds) in the mucous membrane lining and
because of the elasticity of its walls. When full, the dome
of the bladder may extend above the symphysis pubis; in
extreme situations, it may extend as high as the umbilicus.
Normal bladder capacity is between 300 and 600 mL of urine.
Urethra
The urethra extends from the bladder to the urinary
meatus (opening). The male urethra is approximately
20 cm (8 in.) long and serves as a passageway for semen as
well as urine (see Figure 47.2). The meatus is located at the
distal end of the penis. In the adult woman, the urethra lies
directly behind the symphysis pubis, anterior to the vagina,
and is between 3 and 4 cm (1.5 in.) long (see Figure 47.3).
The urethra serves only as a passageway for the elimination
of urine. The urinary meatus is located between the labia
minora, in front of the vagina and below the clitoris.
In both men and women, the urethra has a mucous
membrane lining that is continuous with the bladder and
the ureters. Thus, an infection of the urethra can extend
through the urinary tract to the kidneys. Women are particularly prone to urinary tract infections (UTIs) because
of their short urethra and the proximity of the urinary
meatus to the vagina and anus.
Pelvic Floor
The vagina, urethra, and rectum pass through the pelvic
floor, which consists of sheets of muscles and ligaments that
27/01/2021 18:07
1236
Unit 10
●
Promoting Physiologic Health
ANATOMY & PHYSIOLOGY REVIEW
Female and Male Urinary Bladders and Urethras
The pelvic floor muscles (PFM) are under voluntary
control and are important in controlling urination
(continence). These muscles can become weakened by
pregnancy and childbirth, chronic constipation, a decrease
in estrogen (menopause), being overweight, aging, and
lack of general fitness.
Review the figures and find the pelvic floor muscles.
Kidney
Ureter
Detrusor muscle
Opening of ureters
Trigone
Internal urethral sphincter
Prostate gland
Urethra
External urethral sphincter
QUESTIONS
1. Do you think pelvic floor muscles can be strengthened?
Provide your rationale.
provide support to the viscera of the pelvis (see Figures 47.2
and 47.3). These muscles and ligaments extend from the
symphysis pubis to the coccyx forming a sling. Specific
sphincter muscles contribute to the continence mechanism
(see the Anatomy & Physiology Review). The internal
sphincter muscle situated in the proximal urethra and the
bladder neck is composed of smooth muscle under involuntary control. It provides active tension designed to close
the urethral lumen. The external sphincter muscle is composed of skeletal muscle under voluntary control, allowing
the individual to choose when urine is eliminated.
Urination
Micturition, voiding, and urination all refer to the process of
emptying the urinary bladder. Urine collects in the bladder until pressure stimulates special sensory nerve endings in the bladder wall called stretch receptors. This occurs
when the adult bladder contains between 250 and 450 mL
of urine. In children, a considerably smaller volume, 50 to
200 mL, stimulates these nerves.
M47_BERM9793_11_GE_C47.indd 1236
2. Explain how exercising the pelvic floor muscles helps
to control urination.
Answers to Anatomy & Physiology Review questions are available on the faculty resources
site. Please consult with your instructor.
The stretch receptors transmit impulses to the spinal
cord, specifically to the voiding reflex center located at
the level of the second to fourth sacral vertebrae, causing
the internal sphincter to relax and stimulating the urge
to void. If the time and place are appropriate for urination, the conscious portion of the brain relaxes the external
urethral sphincter muscle and urination takes place. If the
time and place are inappropriate, the micturition reflex
usually subsides until the bladder becomes more filled
and the reflex is stimulated again.
Voluntary control of urination is possible only if the
nerves supplying the bladder and urethra, the neural
tracts of the cord and brain, and the motor area of the cerebrum are all intact. The individual must be able to sense
that the bladder is full. Injury to any of these parts of the
nervous system—for example, by a cerebral hemorrhage
or spinal cord injury above the level of the sacral region—
results in intermittent involuntary emptying of the bladder. Older adults whose cognition is impaired may not be
aware of the need to urinate or able to respond to this urge
by seeking toilet facilities.
27/01/2021 18:07
Chapter 47
Factors Affecting Voiding
Numerous factors affect the volume and characteristics of
the urine produced and the manner in which it is excreted.
Developmental Factors
See Table 47.1 and the Lifespan Considerations feature
for summaries of the developmental changes affecting
urinary output.
●
Urinary Elimination
1237
Psychosocial Factors
For many individuals, a set of conditions helps stimulate the
micturition reflex. These conditions include privacy, normal
position, sufficient time, and, occasionally, running water.
Circumstances that do not allow for the client’s accustomed
conditions may produce anxiety and muscle tension. As a
result, the client is unable to relax abdominal and perineal
muscles and the external urethral sphincter; thus, voiding is
inhibited. Clients also may voluntarily suppress urination
Changes in Urinary Elimination Throughout the Lifespan
TABLE 47.1
Stage
Variations
Fetuses
The fetal kidney begins to excrete urine between the 11th and 12th week of development.
Infants
Ability to concentrate urine is minimal because of immature kidneys; therefore, urine is colorless and odorless and has
a specific gravity of 1.008.
Because of neuromuscular immaturity, voluntary urinary control is absent and an infant may urinate as often as 20 times a day.
Children
Most renal growth occurs during the first 5 years of life.
The kidneys’ efficiency (i.e., regulation of electrolyte and acid–base balance) greatly increases after age 2.
At approximately 2 1/2 to 3 years of age, the child can perceive bladder fullness, hold urine after the urge to void, and
communicate the need to urinate.
Full urinary control usually occurs at age 4 or 5 years; daytime control is usually achieved by age 3 years.
Adults
The kidneys reach maximum size between 35 and 40 years of age.
After 50 years, the kidneys begin to diminish in size and function. Most shrinkage occurs in the cortex of the kidney as
individual nephrons are lost.
Older Adults
An estimated 30% of nephrons are lost by age 80.
Renal blood flow decreases because of vascular changes and a decrease in cardiac output.
The ability to concentrate urine declines.
Bladder muscle tone diminishes, causing increased frequency of urination and nocturia (awakening to urinate at night).
Diminished bladder muscle tone and contractibility may lead to residual urine in the bladder after voiding, increasing
the risk of bacterial growth and infection.
Urinary incontinence may occur due to mobility problems or neurologic impairments.
LIFESPAN CONSIDERATIONS Factors Affecting Voiding
INFANTS AND CHILDREN
• UTIs are the second most common infection in children, after
respiratory infections. They are seen more frequently in newborn
and young infant boys than girls and are most often due to
obstructions or malformations of the urinary system (Ball, Bindler,
Cowen, & Shaw, 2017). In older infants and children, girls have
more UTIs than boys, usually due to contamination of the urethra
with stool.
• Children often forget to wash their hands. Teaching proper
perineal hygiene can reduce infection. Girls should learn to wipe
from front to back and wear cotton underwear.
• Teach children and parents that they should go to the bathroom
as soon as the sensation to void is felt and not try to hold the
urine in.
OLDER ADULTS
Many changes of aging cause specific problems in urinary elimination. Many conditions can be treated to lessen symptoms. Some of
the following conditions are etiologic factors in problems with urinary
elimination:
• Many older men have enlarged prostate glands, which can
inhibit complete emptying of the bladder, resulting in urinary
retention and urgency that can cause incontinence.
M47_BERM9793_11_GE_C47.indd 1237
After menopause women have decreased estrogen levels,
which results in a decrease in perineal tone and support of
bladder, vagina, and supporting tissues. This often results in
urgency and stress incontinence and can even increase the
incidence of UTIs.
• Increased stiffness and joint pain, previous joint surgery, and
neuromuscular problems can impair mobility, making it difficult
to get to the bathroom.
• Cognitive impairment, such as in dementia, often prevents
the individual from understanding the need to urinate and the
actions needed to perform the activity.
Interventions that may improve these conditions include:
• Medications or surgery to relieve obstructions in men and
strengthen support in the urogenital area in women.
• Behavioral training for better bladder control.
• Providing safe, easy access to the bathroom or bedside
commode, whether at home or in an institution. Make sure the
room is well lit, the environment is safe, and the proper assistive
devices are within reach (such as walkers, canes).
• Habit training, such as taking the client to the bathroom at a
regular, scheduled time. This can often work very well with
clients who have cognitive impairments.
•
27/01/2021 18:07
1238
Unit 10
●
Promoting Physiologic Health
because of perceived time pressures; for example, nurses
often ignore the urge to void until they are able to take a
break. This behavior can increase the risk of UTIs.
Fluid and Food Intake
The healthy body maintains a balance between the
amount of fluid ingested and the amount of fluid eliminated. When the amount of fluid intake increases, therefore, the output normally increases. Certain fluids, such
as alcohol, increase fluid output by inhibiting the production of antidiuretic hormone. Fluids that contain caffeine
(e.g., coffee, tea, and cola drinks) also increase urine production. By contrast, food and fluids high in sodium can
cause fluid retention because water is retained to maintain
the normal concentration of electrolytes.
Medications
Many medications, particularly those affecting the autonomic nervous system, interfere with the normal urination
process and may cause retention (Box 47.1). Diuretics (e.g.,
chlorothiazide and furosemide) increase urine formation
by preventing the reabsorption of water and electrolytes
from the tubules of the kidney into the bloodstream. Some
medications may alter the color of the urine.
Muscle Tone
Good muscle tone is important to maintain the stretch and
contractility of the detrusor muscle so the bladder can fill
adequately and empty completely. Clients who require a
retention catheter for a long period may have poor bladder muscle tone because continuous drainage of urine
prevents the bladder from filling and emptying normally.
Pelvic floor muscle tone also contributes to the ability to
store and empty urine.
Pathologic Conditions
Some diseases and pathologies can affect the formation
and excretion of urine. Diseases of the kidneys may affect
the ability of the nephrons to produce urine. Abnormal
amounts of protein or blood cells may be present in the
BOX 47.1
•
•
•
•
•
•
•
Medications That May Cause Urinary
Retention
Anticholinergic medications, such as Atropine, Robinul, and
Pro-Banthine
Antidepressant and antipsychotic agents, such as tricyclic
antidepressants and monoamine oxidase inhibitors (MAOIs)
Antihistamine preparations, such as pseudoephedrine (Actifed
and Sudafed)
Antihypertensives, such as hydralazine (Apresoline) and
methyldopa (Aldomet)
Antiparkinsonism drugs, such as levodopa, trihexyphenidyl
(Artane), and benztropine mesylate (Cogentin)
Beta-adrenergic blockers, such as propranolol (Inderal)
Opioids, such as hydrocodone (Vicodin)
M47_BERM9793_11_GE_C47.indd 1238
urine, or the kidneys may virtually stop producing urine
altogether, a condition known as renal failure. Heart and
circulatory disorders such as heart failure, shock, or hypertension can affect blood flow to the kidneys, interfering
with urine production. If abnormal amounts of fluid are
lost through another route (e.g., vomiting or high fever),
the kidneys retain water and urinary output falls.
Processes that interfere with the flow of urine from the
kidneys to the urethra affect urinary excretion. A urinary
stone (calculus) may obstruct a ureter, blocking urine flow
from the kidney to the bladder. Hyperplasia (enlargement)
of the prostate gland, a common condition affecting older
men, may obstruct the urethra, impairing urination and
bladder emptying.
Surgical and Diagnostic Procedures
Some surgical and diagnostic procedures affect the passage
of urine and the urine itself. The urethra may swell following a cystoscopy, and surgical procedures on any part of the
urinary tract may result in some postoperative bleeding;
as a result, the urine may be red or pink tinged for a time.
Spinal anesthetics can affect the passage of urine
because they decrease the client’s awareness of the need
to void. Surgery on structures adjacent to the urinary tract
(e.g., the uterus) can also affect voiding because of swelling in the lower abdomen.
Altered Urine Production
Although patterns of urination are highly individual, most
individuals void about 5 to 6 times a day. Individuals usually void when they first awaken in the morning, before
they go to bed, and around mealtimes. Table 47.2 shows
the average urinary output per day at different ages.
Polyuria
Polyuria (or diuresis) refers to the production of abnor-
mally large amounts of urine by the kidneys, often several
liters more than the client’s usual daily output. Polyuria
can follow excessive fluid intake, a condition known as
TABLE 47.2
Average Daily Urine Output by Age
Age
Amount (mL)
1–2 days
15–60
3–10 days
100–300
10 days–2 months
250–450
2 months–1 year
400–500
1–3 years
500–600
3–5 years
600–700
5–8 years
700–1000
8–14 years
800–1400
14 years through adulthood
1500
Older adulthood
1500 or less
27/01/2021 18:07
Chapter 47
polydipsia, or may be associated with diseases such as diabetes mellitus, diabetes insipidus, and chronic nephritis.
Polyuria can cause excessive fluid loss, leading to intense
thirst, dehydration, and weight loss.
Oliguria and Anuria
The terms oliguria and anuria are used to describe decreased
urinary output. Oliguria is low urine output, usually less
than 500 mL a day or 30 mL an hour for an adult. Although
oliguria may occur because of abnormal fluid losses or a
lack of fluid intake, it often indicates impaired blood flow
to the kidneys or impending renal failure and should be
promptly reported to the primary care provider. Restoring
renal blood flow and urinary output promptly can prevent
renal failure and its complications. Anuria refers to a lack
of urine production.
Altered Urinary Elimination
Despite normal urine production, a number of factors
or conditions can affect urinary elimination. Frequency,
nocturia, urgency, and dysuria often are manifestations of underlying conditions such as a UTI. Enuresis,
incontinence, retention, and neurogenic bladder may be
either a manifestation or the primary problem affecting
TABLE 47.3
●
Urinary Elimination
1239
urinary elimination. Selected factors associated with
altered patterns of urine elimination are identified in
Table 47.3.
Frequency and Nocturia
Urinary frequency is voiding at frequent intervals, that is,
more than 4 to 6 times per day. An increased intake of fluid
causes some increase in the frequency of voiding. Conditions such as UTI, stress, and pregnancy can cause frequent voiding of small quantities (50 to 100 mL) of urine.
Total fluid intake and output may be normal.
Nocturia is voiding 2 or more times at night. Like
frequency, it is usually expressed in terms of the number
of times the individual gets out of bed to void, for example, “nocturia * 4.”
Urgency
Urgency is the sudden, strong desire to void. There may
or may not be a great deal of urine in the bladder, but
the individual feels a need to void immediately. Urgency
accompanies psychologic stress and irritation of the trigone and urethra. It is also common in individuals who
have poor external sphincter control and unstable bladder
contractions. It is not a normal finding.
Selected Factors Associated with Altered Urinary Elimination
Pattern
Selected Associated Factors
Polyuria
Ingestion of fluids containing caffeine or alcohol
Prescribed diuretic
Presence of thirst, dehydration, and weight loss
History of diabetes mellitus, diabetes insipidus, or kidney disease
Oliguria, anuria
Decrease in fluid intake
Signs of dehydration
Presence of hypotension, shock, or heart failure
History of kidney disease
Signs of renal failure such as elevated blood urea nitrogen (BUN) and serum creatinine, edema, hypertension
Frequency or nocturia
Pregnancy
Increase in fluid intake
UTI
Urgency
Presence of psychologic stress
UTI
Dysuria
Urinary tract inflammation, infection, or injury
Hesitancy, hematuria, pyuria (pus in the urine), and frequency
Enuresis
Family history of enuresis
Difficult access to toilet facilities
Home stresses
Incontinence
Bladder inflammation, stroke (cerebrovascular accident [CVA]), spinal cord injury, or other disease
Difficulties in independent toileting (mobility impairment)
Leakage when coughing, laughing, sneezing
Cognitive impairment
Retention
Distended bladder on palpation and percussion
Associated signs, such as pubic discomfort, restlessness, frequency, and small urine volume
Recent anesthesia
Recent perineal surgery
Presence of perineal swelling
Medications prescribed
Lack of privacy or other factors inhibiting micturition
M47_BERM9793_11_GE_C47.indd 1239
27/01/2021 18:07
1240
Unit 10
●
Promoting Physiologic Health
Dysuria
Dysuria means voiding that is either painful or difficult.
It can accompany a stricture (decrease in diameter) of
the urethra, urinary infections, and injury to the bladder
and urethra. Often clients will say they have to push to
void or that burning accompanies or follows voiding. The
burning may be described as severe, like a hot poker, or
more subdued, like a sunburn. Often, urinary hesitancy
(a delay and difficulty in initiating voiding) is associated
with dysuria.
Enuresis
Enuresis is involuntary urination in children beyond the
age when voluntary bladder control is normally acquired,
usually 4 or 5 years of age. Nocturnal enuresis often is
irregular in occurrence and affects boys more often than
girls. Diurnal (daytime) enuresis may be persistent and
pathologic in origin. It affects women and girls more
frequently.
Urinary Incontinence
Urinary incontinence (UI), is any involuntary urine leakage.
UI is a widespread problem internationally, peaking in the
geriatric population (Searcy, 2017, p. 447). About 16% to
18% of postmenopausal women develop UI (Tso & Lee,
2018). UI can lead to depression, feelings of shame and
embarrassment, and isolation, and can prevent individuals from traveling far from home (Kehinde, 2016; Nazarko,
2017). Kehinde (2016) reports that UI increases admission
to long-term care facilities. Older adults have the highest
incidence of UI, which puts them at risk for skin breakdown, recurrent UTIs, and falls related to symptoms of
urgency. In spite of the high numbers of adults with UI,
it is underreported and undertreated and can lead to a
decreased quality of life. Many individuals do not seek
help because they think nothing can be done or they think
they are too old for treatment (Leaver, 2017). It is important to remember that UI is not a normal part of aging and
often is treatable.
The types of UI can be classified based on symptoms: stress, urgency, mixed, overflow, and transient and
functional.
Stress Urinary Incontinence
Stress urinary incontinence (SUI), the most common
type of UI, occurs because of weak pelvic floor muscles
or urethral hypermobility, causing urine leakage with
such activities as laughing, coughing, sneezing, or any
body movement that puts pressure on the bladder. Facts
that make women more likely to experience SUI include
shorter urethras, the trauma to the pelvic floor associated
with childbirth, and changes related to menopause. For
men, SUI may result after a prostatectomy. It is important
for clients to understand that SUI is not related to emotional stress but is caused by increased intra-abdominal
pressure on the bladder, as well as anatomic changes to
the urethra and pelvic floor muscle weakness.
M47_BERM9793_11_GE_C47.indd 1240
Urgency Urinary Incontinence
Urgency urinary incontinence (UUI) is also called
overactive bladder (Palmer & Willis-Gray, 2017; Tso & Lee,
2018). It is described as an urgent need to void and the
inability to stop urine leakage, which can range from a few
drops to soaking of undergarments. Normally the bladder
contracts on urination. Individuals with an overactive
bladder experience contractions while the bladder is
filling, leading to an urgency to void, which can lead to
UI (Nazarko, 2017).
Mixed Urinary Incontinence
Mixed incontinence is diagnosed when symptoms of both
SUI and UUI are present. The SUI and UUI symptoms do
not occur at the same time; usually the individual experiences episodes of isolated SUI and isolated UUI. It is very
common among older women (Searcy, 2017). Treatment is
usually based on which type of UI is the most bothersome
to the client.
Overflow Urinary Incontinence
This is when the bladder overfills and urine leaks out
due to pressure on the urinary sphincter. It occurs in
men with an enlarged prostate and clients with a neurologic disorder (e.g., multiple sclerosis, Parkinson’s
disease, spinal cord injury). An impaired neurologic
function can interfere with the normal mechanisms of
urine elimination, resulting in a neurogenic bladder .
The client with a neurogenic bladder does not perceive
bladder fullness and is therefore unable to control the
urinary sphincters.
Transient and Functional Urinary
Incontinence
Transient urinary incontinence results from factors outside of the urinary tract (e.g., medications, delirium, infection, constipation). Functional urinary incontinence (FUI)
is a subcategory of transient urinary incontinence. FUI is
connected with a cognitive or physical impairment, for
example, unavailable toileting facilities or the inability to
reach a toilet due to physical limitations. An individual
with cognitive impairment may recognize the need to
void but be unable to communicate the need.
Urinary Retention
When emptying of the bladder is impaired, urine accumulates and the bladder becomes overdistended, a condition
known as urinary retention. Overdistention of the bladder
causes poor contractility of the detrusor muscle, further
impairing urination. Common causes of urinary retention
include benign prostatic hyperplasia (BPH), surgery, and
some medications (see Box 47.1). Acute urinary retention
is the most common complication postoperatively (Hoke
& Bradway, 2016). Clients with urinary retention may
experience overflow incontinence, eliminating 25 to 50 mL
of urine at frequent intervals. The bladder is firm and distended on palpation and may be displaced to one side of
the midline.
27/01/2021 18:07
Chapter 47
●
Urinary Elimination
1241
EVIDENCE-BASED PRACTICE
Evidence-Based Practice
What Are the Outcomes of the Application of
Nonpharmacologic and Nonsurgical Resources
to Treat Female Urinary Incontinence?
Women are at greater risk for UI than men and the risk increases
with age. UI affects the quality of life as well as the social, physical,
psychologic, occupational, and sexual aspects of women’s lives.
Unfortunately, most women never seek or receive UI treatments.
Believing that healthcare providers should use evidence-based
practice in UI health services, Mendes, Rodolpho, and Hoga
(2016) conducted an integrative review (IR) of literature to answer
the question posed in the title. The IR resulted in an initial 1592
empirical studies with 198 potentially relevant papers identified.
Further analysis resulted in 14 studies that met the eligibility criteria
of the IR. Studies were conducted in 10 countries, indicating the
international relevance of UI.
The types of treatments used in the studies included electrical
stimulation, transvaginal electrical stimulation, vaginal cone, global
NURSING MANAGEMENT
Assessing
A complete assessment of a client’s urinary function
includes the following:
•
•
•
Nursing history
Physical assessment of the genitourinary system,
hydration status, and examination of the urine
Relating the data obtained to the results of any diagnostic
tests and procedures.
Nursing History
The nurse determines the client’s normal voiding pattern
and frequency, appearance of the urine and any recent
changes, any past or current problems with urination, the
postural reeducation, biofeedback for pelvic floor muscle (PFM)
training, cognitive behavioral therapy, extracorporeal magnetic
stimulation therapy, multidimensional exercise treatment, interferential therapy, interpersonal support, and digital vaginal palpation.
PFM training was the main resource used to treat UI. All the UI
treatments focused on improving the skills required to perform
PFM exercises. The researchers found that all the treatments and
equipment that were used resulted in the improvement of UI or
its cure. The effectiveness of adding PFM training to other active
treatments as compared with the same active treatment alone
increased the effectiveness in reducing all types of UI.
Implications
UI treatment requires multiprofessional involvement and close relationships among healthcare providers. For example, the studies
that included interpersonal support and nurse monitoring in addition to PFM exercises improved the effectiveness of UI treatment.
presence of an ostomy, and factors influencing the elimination pattern.
Examples of interview questions to elicit this information are shown in the Assessment Interview. The number
of questions asked depends on the individual and the
responses to the first three categories.
Physical Assessment
Complete physical assessment of the urinary tract usually includes percussion of the kidneys to detect areas of
tenderness. Palpation and percussion of the bladder are
also performed. If the client’s history or current problems
indicate a need for it, the urethral meatus of both male
and female clients is inspected for swelling, discharge, and
inflammation.
ASSESSMENT INTERVIEW Urinary Elimination
VOIDING PATTERN
• How many times do you urinate during a 24-hour period?
• Has this pattern changed recently?
• Do you need to get out of bed to void at night? How often?
•
DESCRIPTION OF URINE AND ANY CHANGES
• How would you describe your urine in terms of color, clarity
(clear, transparent, or cloudy), and odor (faint or strong)?
FACTORS INFLUENCING URINARY ELIMINATION
• Medications. What medications are you taking? Do you know if
any of your medications increase urinary output or cause retention of urine? Note specific medication and dosage.
• Fluid intake. How much and what kind of fluid do you drink
each day (e.g., six glasses of water, two cups of coffee, three
cola drinks with or without caffeine)?
• Environmental factors. Do you have any problems with toileting
(mobility, removing clothing, toilet seat too low, facility without
grab bar)?
• Stress. Are you experiencing any major stress? If so, what are
the stressors? Do you think these affect your urinary pattern?
• Disease. Have you had or do you have any illnesses that may
affect urinary function, such as hypertension, heart disease,
neurologic disease, cancer, prostatic enlargement, or diabetes?
• Diagnostic procedures and surgery. Have you recently had a
cystoscopy or anesthetic?
URINARY ELIMINATION PROBLEMS
• What problems have you had or do you now have with passing
your urine?
• Passage of small amounts of urine?
• Voiding at more frequent intervals?
• Trouble getting to the bathroom in time, or feeling an urgent
need to void?
• Painful voiding?
• Difficulty starting urine stream?
• Frequent dribbling of urine or feeling of bladder fullness
associated with voiding small amounts of urine?
• Reduced force of stream?
M47_BERM9793_11_GE_C47.indd 1241
Accidental leakage of urine? If so, when does this occur (e.g.,
when coughing, laughing, or sneezing; at night; during the day)?
• Past urinary tract illness such as infection of the kidney, bladder,
or urethra? History of renal, ureteral, or bladder surgery?
27/01/2021 18:07
1242
Unit 10
TABLE 47.4
Promoting Physiologic Health
●
Characteristics of Normal and Abnormal Urine
Characteristic
Normal
Abnormal
Nursing Considerations
Amount in 24 hours
(adult)
1200–1500 mL
Under 1200 mL
A large amount over
intake
Urinary output normally is approximately equal to fluid intake. Output
of less than 30 mL/h may indicate decreased blood flow to the kidneys
and should be immediately reported.
Color, clarity
Straw, amber
Transparent
Dark amber
Cloudy
Dark orange
Red or dark brown
Mucous plugs,
viscid, thick
Concentrated urine is darker in color. Dilute urine may appear almost clear,
or very pale yellow. Some foods and drugs may color urine. Red blood
cells in the urine (hematuria) may be evident as pink, bright red, or rusty
brown urine. Menstrual bleeding can also color urine but should not be
confused with hematuria. White blood cells, bacteria, pus, or contaminants
such as prostatic fluid, sperm, or vaginal drainage may cause cloudy urine.
Odor
Faint aromatic
Offensive
Some foods (e.g., asparagus) cause a musty odor; infected urine can
have a fetid odor; urine high in glucose has a sweet odor.
Sterility
No microorganisms present
Microorganisms
present
Urine in the bladder is sterile. Urine specimens, however, may be
contaminated by bacteria from the perineum during collection.
pH
4.5–8
Over 8
Under 4.5
Freshly voided urine is normally somewhat acidic. Alkaline urine may
indicate a state of alkalosis, UTI, or a diet high in fruits and vegetables.
More acidic urine (low pH) is found in starvation, with diarrhea, or with a
diet high in protein foods or cranberries.
Specific gravity
1.010–1.025
Over 1.025
Under 1.010
Concentrated urine has a higher specific gravity; diluted urine has a
lower specific gravity.
Glucose
Not present
Present
Glucose in the urine indicates high blood glucose levels (greater than
180 mg/dL) and may be indicative of undiagnosed or uncontrolled
diabetes mellitus.
Ketone bodies
(acetone)
Not present
Present
Ketones, the end product of the breakdown of fatty acids, are not
normally present in urine. They may be present in the urine of clients
who have uncontrolled diabetes mellitus, who are in a state of
starvation, or who have ingested excessive amounts of aspirin.
Blood
Not present
Occult (microscopic)
Bright red
Blood may be present in the urine of clients who have UTI, kidney
disease, or bleeding from the urinary tract.
Because problems with urination can affect the elimination of wastes from the body, it is important for the nurse
to assess the skin for color, texture, and tissue turgor as
well as the presence of edema. If incontinence, dribbling,
or dysuria is noted in the history, the skin of the perineum
should be inspected for irritation because contact with
urine can excoriate the skin.
•
•
•
•
Assessing Urine
Normal urine consists of 96% water and 4% solutes.
Organic solutes include urea, ammonia, creatinine, and
uric acid. Variations in color can occur. Characteristics of
normal and abnormal urine are shown in Table 47.4.
•
Instruct the client to keep urine separate from feces and to
avoid putting toilet paper in the urine collection container.
Pour the voided urine into a calibrated container.
Hold the container at eye level and read the amount
in the container. Containers usually have a measuring
scale on the inside.
Record the amount on the fluid intake and output
(I&O) sheet, which may be at the bedside or in the
bathroom.
Rinse the urine collection and measuring containers
with cool water and store appropriately.
Measuring Urinary Output
Normally, the kidneys produce urine at a rate of approximately 60 mL/h or about 1500 mL/day. Urine output is
affected by many factors, including fluid intake, body
fluid losses through other routes such as perspiration and
breathing or diarrhea, and the cardiovascular and renal
status of the individual.
Urine outputs below 30 mL/h may indicate low blood
volume or kidney malfunction and must be reported. To
measure fluid output the nurse follows these steps:
•
•
Wear clean gloves to prevent contact with microorganisms or blood in urine.
Ask the client to void in a clean urinal, bedpan, commode, or toilet collection device (“hat”) (Figure 47.4 ■).
M47_BERM9793_11_GE_C47.indd 1242
Figure 47.4 ■ A urine “hat”—a urine collection device for the toilet.
27/01/2021 18:07
Chapter 47
Figure 47.5 ■ Urine being measured from a urine collection bag.
•
•
Remove gloves and perform hand hygiene.
Calculate and document the total output at the end of
each shift and at the end of 24 h on the client’s chart.
Many clients can measure and record their own urine output when the procedure is explained to them.
When measuring urine from a client who has a urinary catheter, the nurse follows these steps:
•
•
•
•
•
Apply clean gloves.
Take the calibrated container to the bedside.
Place the container under the urine collection bag so
that the spout of the bag is above the container but not
touching it. The calibrated container is not sterile, but
the inside of the collection bag is sterile (Figure 47.5 ■).
Open the spout and permit the urine to flow into the
container.
Close the spout, then proceed as described in the previous list.
Measuring Residual Urine
Postvoid residual (PVR) (urine remaining in the bladder fol-
lowing voiding) is normally 50 to 100 mL. However, a bladder outlet obstruction (e.g., enlargement of the prostate gland)
or loss of bladder muscle tone may interfere with complete
emptying of the bladder during urination. Manifestations
of urine retention may include frequent voiding of small
amounts (e.g., less than 100 mL in an adult), urinary stasis,
and UTI. PVR is measured to assess the amount of retained
urine after voiding and determine the need for interventions
(e.g., medications to promote detrusor muscle contraction).
To measure PVR, the nurse catheterizes or bladder scans
the client after voiding (Figure 47.6 ■). The amount of urine
voided and the amount obtained by catheterization or bladder scan are measured and recorded. An indwelling catheter
may be inserted if the PVR exceeds a specified amount.
Diagnostic Tests
Blood levels of two metabolically produced substances,
urea and creatinine, are routinely used to evaluate renal
function. The kidneys through filtration and tubular secretion normally eliminate both urea and creatinine. Urea,
the end product of protein metabolism, is measured as
blood urea nitrogen (BUN). Creatinine is produced in
M47_BERM9793_11_GE_C47.indd 1243
●
Urinary Elimination
1243
Figure 47.6 ■ A handheld, portable ultrasound device can measure
bladder urine volume noninvasively. It is placed 1–1.5 inch above the
symphysis pubis and tilted toward the bladder.
relatively constant quantities by the muscles. The creatinine clearance test uses 24-hour urine and serum creatinine levels to determine the glomerular filtration rate, a
sensitive indicator of renal function. Other tests related
to urinary functions such as collecting urine specimens,
measuring specific gravity, and visualization procedures
are described in Chapter 34 .
Diagnosing
An example of a nursing diagnosis for clients with urinary
elimination problems is altered urinary elimination, and
to help make it more specific, identify the problem. An
example is altered urinary elimination (urinary retention).
Another example of a nursing diagnosis is urinary incontinence and specifying the type (i.e., functional, overflow,
reflex, stress, or urge). Other examples of nursing diagnoses include potential for incontinence (specify type) and
potential altered urinary elimination (urinary retention).
Clinical examples of assessment data clusters and
related nursing diagnoses, outcomes, and interventions
are shown in the Nursing Care Plan and Concept Map at
the end of this chapter.
Problems of urinary elimination also may become
the etiology for other problems experienced by the client.
Examples include the following:
•
•
•
•
Potential for infection if the client has urinary retention
or undergoes an invasive procedure such as catheterization or cystoscopic examination.
Impaired self-esteem or social seclusion if the client is
incontinent. Incontinence can be physically and emotionally distressing to clients because it is considered
socially unacceptable. Often the client is embarrassed
about dribbling or having an accident and may restrict
normal activities for this reason.
Potential for developing altered skin integrity if the
client is incontinent. Bed linens and clothes saturated
with urine irritate and macerate the skin. Prolonged
skin dampness leads to dermatitis (inflammation of
the skin) and subsequent formation of dermal ulcers.
Lack of knowledge if the client requires self-care skills
to manage (e.g., a new urinary diversion ostomy).
27/01/2021 18:07
1244
Unit 10
●
Promoting Physiologic Health
Planning
The goals established will vary according to the diagnosis
and signs and symptoms. Examples of overall goals for
clients with urinary elimination problems may include the
following:
•
•
•
•
•
Maintain or restore a normal voiding pattern.
Regain normal urine output.
Prevent associated risks such as infection, skin breakdown, fluid and electrolyte imbalance, and lowered
self-esteem.
Perform toileting activities independently with or without assistive devices.
Contain urine with the appropriate device, catheter,
ostomy appliance, or absorbent product.
Appropriate preventive and corrective nursing interventions that relate to these must be identified. Specific nursing activities associated with each of these interventions can
be selected to meet the client’s individual needs. Examples
of clinical applications of these using nursing diagnoses,
NIC, and NOC designations are shown in the Nursing Care
Plan and Concept Map at the end of the chapter.
•
•
•
•
•
Planning for Home Care
To provide for continuity of care, the nurse needs to consider the client’s needs for teaching and assistance with care
in the home. Discharge planning includes assessment of
the client and family’s resources and abilities for self-care,
available financial resources, and the need for referrals and
home health services.
QSEN
FAMILY
•
Patient-Centered Care: Urinary Elimination
The nurse needs to complete an assessment of the following home care capabilities related to urinary elimination
problems and needs:
CLIENT AND ENVIRONMENT
•
toilet, to manipulate clothing for toileting, and to perform hygiene measures after toileting
Current level of knowledge: fluid and dietary intake
modifications to promote normal patterns of urinary
elimination, bladder training methods, and specific
techniques to promote voiding care for indwelling catheter or ostomy (if appropriate)
Assistive devices required: ambulatory aids such as
walker, cane, or wheelchair; safety devices such as
grab bars; toileting aids such as raised toilet seat,
urinal, commode, or bedpan; presence of a urinary
catheter
Physical layout of the toileting facilities: presence of
mobility aids; toilet at correct height to enable older
clients to get up after voiding
Home environment factors that interfere with toileting:
distance to the bathroom from living areas or bedrooms;
barriers such as stairways, scatter rugs, clutter, or
narrow doorways that interfere with bathroom access;
lighting (including night lighting)
Urinary elimination problems: type of incontinence
and precipitating factors; manifestations of UTI such
as dysuria, frequency, urgency; evidence of benign
prostatic hyperplasia and effect on urination; ability to
perform self-catheterization and care for other urinary
elimination devices such as indwelling catheter, urinary diversion ostomy, or condom drainage.
•
Self-care abilities: ability to consume adequate fluids,
to perceive bladder fullness, to ambulate and get to the
Caregiver availability, skills, and responses: ability
and willingness to assume responsibilities for care,
including assisting with toileting, intermittent catheterization, indwelling catheter care, urinary drainage devices or ostomy care; ready access to laundry
facilities; access to and willingness to use respite or
relief caregivers
Family role changes and coping: effect on spousal and
family roles, sleep and rest patterns, sexuality, and
social interactions
DRUG CAPSULE
Anticholinergic Agent: oxybutynin ER (Ditropan XL)
THE CLIENT WITH MEDICATIONS FOR URGENCY URINARY
INCONTINENCE
Anticholinergic agents reduce urgency and frequency by blocking
muscarinic receptors in the detrusor muscle of the bladder, thereby
inhibiting contractions and increasing storage capacity. They are useful in relieving symptoms associated with voiding problems in clients
with neurogenic bladder and reflex neurogenic bladder, and UUI.
NURSING RESPONSIBILITIES
• Monitor for constipation, dry mouth, urinary retention, blurred
vision, and mental confusion in older adults; symptoms may be
dose related.
• Keep primary care provider informed of expected responses
to therapy (e.g., effect on urinary frequency, urge incontinence,
nocturia, and bladder emptying).
• Start with small doses in clients over the age of 75.
M47_BERM9793_11_GE_C47.indd 1244
•
•
Try using intermittently.
Oxybutynin is contraindicated in clients with urinary retention, GI
motility problems (partial or complete GI obstruction, paralytic
ileus), or uncontrolled narrow-angle glaucoma.
CLIENT AND FAMILY TEACHING
• Explain the reason for taking oxybutynin.
• Explain the side effects and the importance of reporting them to
the healthcare provider.
• Exercise caution in hot environments. By suppressing sweating,
oxybutynin can cause fever and heat stroke.
• Provide strategies for managing dry mouth.
• Instruct and advise regarding behavioral therapies for urge
suppression.
Note: Prior to administering any medication, review all aspects with a current drug handbook or
other reliable source.
27/01/2021 18:07
Chapter 47
•
Financial resources: ability to purchase protective
pads and garments, supplies for catheterization or
ostomy care.
•
COMMUNITY
•
Environment: access to public restrooms and sanitary
facilities
●
Urinary Elimination
1245
Current knowledge of and experience with community
resources: medical and assistive equipment and supply companies, home health agencies, local pharmacies,
available financial assistance, support and educational
organizations
Client Teaching addresses the learning needs of the client
and family.
CLIENT TEACHING Urinary Elimination in the Home Setting
FACILITATING URINARY ELIMINATION SELF-CARE
• Teach the client and family to maintain easy access to toilet
facilities, including removing scatter rugs and ensuring that halls
and doorways are free of clutter.
• Suggest graduated lighting for night-time voiding: a dim night
light in the bedroom and low-wattage hallway lighting.
• Advise the client and family to install grab bars and elevated
toilet seats as needed.
• Provide for instruction in safe transfer techniques. Contact
physical therapy to provide training as needed.
• Suggest clothing that is easily removed for toileting, such
as elastic waist pants or Velcro closures.
PROMOTING URINARY ELIMINATION
• Instruct the client to respond to the urge to void as soon as
possible; avoid voluntary urinary retention.
• Teach the client to empty the bladder completely at each
voiding.
• Emphasize the importance of drinking eight to ten 8-ounce
glasses of water daily.
• Teach female clients about PFM exercises to strengthen
perineal muscles.
• Inform the client about the relationship between tobacco use
and bladder cancer and provide information about smoking
cessation programs as indicated.
• Teach the client to promptly report any of the following to the
primary care provider: pain or burning on urination, changes in
urine color or clarity, foul-smelling urine, or changes in voiding
patterns (e.g., nocturia, frequency, dribbling).
ASEPSIS
• Teach the client to maintain perineal-genital cleanliness,
washing with soap and water daily and cleansing the anal and
perineal area after defecating.
• Instruct female clients to wipe from front to back (from the
urinary meatus toward the anus) after voiding, and to discard
toilet paper after each swipe.
• Provide information about products to protect the skin, clothing,
and furniture for clients who are incontinent. Emphasize the
importance of cleaning and drying the perineal area after
incontinence episodes. Instruct in the use of protective skin
barrier products as needed.
• Teach clients with an indwelling catheter and their family about
care measures such as cleaning the urinary meatus, managing
and emptying the collection device, maintaining a closed system, and bladder irrigation or flushing if ordered.
• For clients with a urinary diversion, teach about care of the stoma,
drainage devices, and surrounding skin. For continent diversions,
teach the client how to catheterize the stoma to drain urine.
• For clients with an indwelling catheter or urinary diversion,
emphasize the importance of maintaining a generous fluid
intake (2.5 to 3 quarts daily) and of promptly reporting changes
in urinary output, signs of urinary retention such as abdominal
pain, and manifestations of UTI such as malodorous urine,
abdominal discomfort, fever, or confusion.
M47_BERM9793_11_GE_C47.indd 1245
MEDICATIONS
• Emphasize the importance of taking medications as prescribed.
Instruct the client to take the full course of antibiotics ordered to
treat a UTI, even though symptoms are relieved.
• Inform the client and family about any expected changes in
urine color or odor associated with prescribed medications.
• For clients with urinary retention, emphasize the need to contact the primary care provider before taking any medication
(even over-the-counter medications such as antihistamines) that
may exacerbate symptoms.
• For clients taking medications that may damage the kidneys
(e.g., aminoglycoside antibiotics), stress the importance
of maintaining a generous fluid intake while taking the
medication.
• Suggest measures to reduce anticipated side effects of prescribed medications, such as increasing intake of potassiumrich foods when taking a potassium-depleting diuretic such as
furosemide.
DIETARY ALTERATIONS
• Teach the client about dietary changes to promote urinary
function, such as consuming cranberry juice and foods that
acidify the urine to reduce the risk of repeated UTIs or forming
calcium-based urinary stones. See the Dietary Measures section on page 1259.
• Instruct clients with stress or urge incontinence to limit their
intake of caffeine, alcohol, citrus juices, and artificial sweeteners
because these are bladder irritants that may increase incontinence. Also, teach clients to limit their evening fluid intake to
reduce the risk of night-time incontinence episodes.
MEASURES SPECIFIC TO URINARY PROBLEMS
• Provide instructions for clients with specific urinary problems or
treatments such as these:
a. Timed urine specimens (see Chapter 34
)
b. Urinary incontinence
c. Urinary retention
d. Retention catheters.
REFERRALS
Make appropriate referrals to home health agencies, community agencies, or social services for assistance with resources
such as installing grab bars and raised toilet seats; providing
wheelchair access to bathrooms; obtaining toileting aids such
as commodes, urinals, or bedpans; and services such as
home health aides for assistance with activities of daily living
(ADLs).
•
COMMUNITY AGENCIES AND OTHER RESOURCES
• Provide information about resources for durable medical
equipment such as commodes or raised toilet seats, possible
financial assistance, and medical supplies such as drainage
bags, incontinence briefs, or protective pads.
• Suggest additional sources of information and help such as
the National Council of Independent Living, United Ostomy
Association, National Association for Continence, and Simon
Foundation for Continence.
27/01/2021 18:07
1246
Unit 10
●
Promoting Physiologic Health
Implementing
Assisting with Toileting
Maintaining Normal Urinary Elimination
Clients who are weakened by a disease process or
impaired physically may require assistance with toileting. The nurse should assist these clients to the bathroom
and remain with them if they are at risk for falling. The
bathroom should contain an easily accessible call signal to
summon help if needed. Clients also need to be encouraged to use handrails placed near the toilet.
For clients unable to use bathroom facilities, the nurse
provides urinary equipment close to the bedside (e.g.,
urinal, bedpan, commode) and provides the necessary
assistance to use them.
Most interventions to maintain normal urinary elimination are independent nursing functions. These include
promoting adequate fluid intake, maintaining normal
voiding habits, and assisting with toileting.
Promoting Fluid Intake
Increasing fluid intake increases urine production, which
in turn stimulates the voiding reflex. A normal daily intake
averaging 1500 mL of measurable fluids is adequate for
most adult clients.
Many clients have increased fluid requirements,
necessitating a higher daily fluid intake. For example, clients who are perspiring excessively (have diaphoresis) or
who are experiencing abnormal fluid losses through vomiting, gastric suction, diarrhea, or wound drainage require
fluid to replace these losses in addition to their normal
daily intake requirements.
Clients who are at risk for UTI or urinary calculi
(stones) should consume 2000 to 3000 mL of fluid daily.
Dilute urine and frequent urination reduce the risk of UTI
as well as stone formation.
Increased fluid intake may be contraindicated for
some clients such as individuals with kidney failure or
heart failure. For these clients, a fluid restriction may be
necessary to prevent fluid overload and edema.
Preventing Urinary Tract Infections
The rate of UTI is greater in women than men because of
the short urethra and its proximity to the anal and vaginal
areas. Most UTIs are caused by bacteria common to the
intestinal environment (e.g., Escherichia coli). These gastrointestinal (GI) bacteria can colonize the perineal area and
move into the urethra, especially when there is urethral
trauma, irritation, or manipulation.
For women who have experienced a UTI, nurses need
to provide instructions about ways to prevent a recurrence. The following guidelines are useful for anyone:
•
•
Maintaining Normal Voiding Habits
Prescribed medical therapies often interfere with a client’s
normal voiding habits. When a client’s urinary elimination pattern is adequate, the nurse helps the client adhere
to normal voiding habits as much as possible (see Practice
Guidelines).
•
Drink eight 8-ounce glasses of water per day to flush
bacteria out of the urinary system.
Practice frequent voiding (every 2 to 4 hours) to flush
bacteria out of the urethra and prevent organisms from
ascending into the bladder. Void immediately after
intercourse.
Avoid use of harsh soaps, bubble bath, powder, or
sprays in the perineal area. These substances can be
irritating to the urethra and encourage inflammation
and bacterial infection.
PRACTICE GUIDELINES Maintaining Normal Voiding Habits
POSITIONING
• Assist the client to a normal position for voiding: standing for
male clients; for female clients, squatting or leaning slightly forward when sitting. These positions enhance movement of urine
through the tract by gravity.
• If the client is unable to ambulate to the lavatory, use a bedside
commode for females and a urinal for males standing at the
bedside.
• If necessary, encourage the client to push over the pubic area
with the hands or to lean forward to increase intra-abdominal
pressure and external pressure on the bladder.
RELAXATION
• Provide privacy for the client. Many clients cannot void in the
presence of another individual.
• Allow the client sufficient time to void.
• Suggest the client read or listen to music.
• Provide sensory stimuli that may help the client relax. Pour
warm water over the perineum of a female or have the client sit
in a warm bath to promote muscle relaxation. Applying a hot
water bottle to the lower abdomen of both men and women
may also foster muscle relaxation.
M47_BERM9793_11_GE_C47.indd 1246
Turn on running water within hearing distance of the client to
stimulate the voiding reflex and to mask the sound of voiding
for clients who find this embarrassing.
• Provide ordered analgesics and emotional support to relieve
physical and emotional discomfort to decrease muscle tension.
•
TIMING
• Assist clients who have the urge to void immediately. Delays
only increase the difficulty in starting to void, and the desire to
void may pass.
• Offer toileting assistance to the client at usual times of voiding, for example, on awakening, before or after meals, and at
bedtime.
FOR CLIENTS WHO ARE CONFINED TO BED
• Warm the bedpan. A cold bedpan may prompt contraction of
the perineal muscles and inhibit voiding.
• Elevate the head of the client’s bed to Fowler’s position, place a
small pillow or rolled towel at the small of the back to increase
physical support and comfort, and have the client flex the hips
and knees. This position simulates the normal voiding position
as closely as possible.
27/01/2021 18:07
Chapter 47
Avoid tight-fitting pants or other clothing that creates
irritation to the urethra and prevents ventilation of the
perineal area.
Wear cotton rather than nylon underclothes. Accumulation of perineal moisture facilitates bacterial growth.
Cotton enhances ventilation of the perineal area.
Girls and women should always wipe the perineal area
from front to back following urination or defecation in
order to prevent introduction of GI bacteria into the
urethra.
If recurrent urinary infections are a problem, take showers rather than baths. Bacteria present in bath water can
readily enter the urethra.
•
•
•
•
Urinary Elimination
1247
Continence (Bladder) Retraining
A continence retraining program requires the involvement
of the nurse, the client, and support people. Clients must be
alert and physically able to participate in the training protocol. A bladder retraining program may include the following:
• Education of the client and support people.
• Bladder retraining promotes complete bladder contraction
Managing Urinary Incontinence
It is important to remember that UI is not a normal part of
aging and often is treatable. The preliminary assessment
and identification of the symptoms of UI are truly within the
scope of nursing practice. All clients should be asked about
their voiding patterns. Older adults who are incontinent
while in their home or who manage to contain or conceal
their incontinence from others do not consider themselves
incontinent. Therefore, if asked if they are incontinent, they
may deny it. However, asking if they lose urine when they
cough, sneeze, or laugh or if they need to use some type
of incontinence product may provide more accurate information. Independent nursing interventions for clients with
UI include (a) a behavior-oriented continence training program that may consist of bladder retraining, habit training,
and pelvic floor muscle exercises; (b) meticulous skin care;
and (c) for males, application of an external drainage device
(condom-type catheter device).
●
•
•
Clinical Alert!
If the client has any type of incontinence, recommend the use of
incontinence pads because they are designed to absorb urine as
opposed to feminine hygiene pads.
and emptying and requires that the client postpone voiding, resist or inhibit the sensation of urgency, and void
according to a timetable rather than according to the urge
to void. The goals are to gradually lengthen the intervals
between urination to correct the client’s frequent urination, to stabilize the bladder, and to diminish urgency. This
form of training may be used for clients who have bladder
instability and urge incontinence. Delayed voiding provides larger voided volumes and longer intervals between
voiding. Initially, voiding may be encouraged every 2 to
3 hours except during sleep and then every 4 to 6 hours.
A vital component of bladder training is inhibiting the
urge-to-void sensation. To do this, the nurse instructs
the client to practice deep, slow breathing until the urge
diminishes or disappears. This is performed every time
the client has a premature urge to void. Guidelines for
bladder retraining are in the Practice Guidelines.
Habit training, also referred to as timed or prompted
voiding and scheduled toileting, attempts to keep clients dry by having them void at regular intervals, such
as every 2 to 4 hours. The goal is to keep the client dry
and is a common therapy for frail older clients and clients with dementia.
Lifestyle modification can greatly influence the incidence of UI. For example, weight loss in overweight
clients can reduce UI because the abdominal weight
places extra force on the bladder. Eliminating beverages
containing caffeine, citrus drinks, and alcohol and balancing fluid intake where there is sufficient fluid intake
during the day and limited fluids before bedtime can
decrease UI (Stewart, 2018).
PRACTICE GUIDELINES Bladder Retraining
Determine the client’s voiding pattern and encourage voiding
at those times, or establish a regular voiding schedule and
help the client to maintain it, whether the client feels the urge
or not (e.g., on awakening, every 1 or 2 hours during the day
and evening, before retiring at night, every 4 hours at night).
The stretching–relaxing sequence of such a schedule tends to
increase bladder muscle tone and promote more voluntary control. Consider a double-voiding technique to promote complete
bladder contraction and emptying. This technique promotes
urinary drainage through position changes or a brief period of
standing prior to a second void (Stewart, 2018). Encourage the
client to inhibit the urge-to-void sensation when a premature
urge to void is experienced. Instruct the client to practice slow,
deep breathing until the urge diminishes or disappears.
• When the client finds that voiding can be controlled, the intervals between voiding can be lengthened slightly without loss of
continence.
• Regulate fluid intake, particularly during evening hours, to help
reduce the need to void during the night.
•
M47_BERM9793_11_GE_C47.indd 1247
•
•
•
•
•
•
•
Encourage fluids between the hours of 0600 and 1800.
Avoid excessive consumption of citrus juices, carbonated beverages (especially those containing artificial sweeteners), alcohol, and drinks containing caffeine because these irritate the
bladder, increasing the risk of incontinence.
Schedule diuretics early in the morning.
Explain to clients that adequate fluid intake is required to ensure
adequate urine production that stimulates the micturition reflex.
Apply protector pads to keep the bed linen dry and provide
specially made waterproof underwear to contain the urine and
decrease the client’s embarrassment. Avoid using diapers, which
are demeaning and also suggest that incontinence is permissible.
Assist the client with a PFM exercise program to increase the
general muscle tone and a program aimed at strengthening the
pelvic floor muscles.
Provide positive reinforcements to encourage continence.
Praise clients for attempting to toilet and for maintaining
continence.
27/01/2021 18:07
1248
Unit 10
●
Promoting Physiologic Health
Pelvic Floor Muscle Exercises
Pelvic floor muscle (PFM), or Kegel, exercises help to
strengthen pelvic floor muscles (see Figures 47.2 and 47.3)
and can reduce or eliminate episodes of incontinence. The
client can identify the perineal muscles by tightening the anal
sphincter as if to control the passing of gas, around the vagina
and the urethra as if trying to stop urine mid flow. When the
exercise is properly performed, contraction of the muscles
of the buttocks and thighs is avoided. PFM exercises can be
performed anytime, anywhere, sitting or standing. Specific
client instructions are summarized in Client Teaching.
Maintaining Skin Integrity
Skin that is continually moist becomes macerated (softened).
Urine that accumulates on the skin is converted to ammonia,
which is very irritating to the skin. Because both skin irritation and maceration can cause skin breakdown and ulceration, the incontinent client requires meticulous skin care. To
maintain skin integrity, the nurse gently cleanses the client’s
perineal area with mild soap and water or a commercially
prepared no-rinse cleanser after episodes of incontinence.
The nurse then rinses the area thoroughly if soap and water
were used, and dries it gently and thoroughly. Clean, dry
clothing or bed linen should be provided. The nurse applies
barrier ointments or creams to protect the skin from contact
with urine. If it is necessary to pad the client’s clothes for protection, the nurse should use products that absorb wetness
and leave a dry surface in contact with the skin.
Specially designed incontinence drawsheets provide
significant advantages over standard drawsheets for
incontinent clients confined to bed. These sheets are like
a drawsheet but are double layered, with a quilted upper
nylon or polyester surface and an absorbent viscose rayon
layer below. The rayon soaker layer generally has a waterproof backing on its underside. Fluid (i.e., urine) passes
through the upper quilted layer and is absorbed and dispersed by the viscose rayon, leaving the quilted surface
dry to the touch. This absorbent sheet helps maintain skin
integrity; it does not stick to the skin when wet, decreases
the risk of bedsores, and reduces odor.
Applying External Urinary Devices
To prevent the complications and inconveniences associated with incontinence in males, an external urinary
device, also referred to as a penile sheath or condom catheter, attached to a urinary drainage system may be used.
External urinary devices may be more comfortable than
an indwelling catheter and cause fewer UTIs. Latex or silicone devices are available. The silicone penile sheath has
two advantages in that it allows the client or his caregivers
to assess the skin without removing the sheath and it has
oxygen and water vapor transmission properties, allowing the skin to breathe (Nazarko, 2018, p. 112).
Methods of applying external urinary devices vary.
The nurse needs to follow the manufacturer’s instructions when applying a condom. First the nurse determines
when the client experiences incontinence. Some clients
may require an external urinary device at night only, others continuously with daily changes. Skill 47.1 describes
how to apply and remove an external device.
CLIENT TEACHING Pelvic Floor Muscle Exercises (Kegel Exercises)
Contract your PFMs where you pull your rectum, urethra, and
vagina up inside, followed by relaxation. Do not hold your
breath or tighten your thighs, buttocks, or abdomen while doing
PFM exercises.
• Hold each contraction for several seconds. It is suggested that
at least eight contractions should be performed three times a
day (Ostle, 2016; Stewart, 2018).
•
Make the exercises part of your daily life, for example, before
getting out of bed in the morning, when working at the kitchen
sink, or on your way to the bathroom. The exercises can be
done anywhere, anytime, and in any position.
• To control episodes of stress incontinence, perform a pelvic
floor muscle contraction when initiating any activity that
increases intra-abdominal pressure, such as coughing, laughing, sneezing, or lifting.
•
SKILL 47.1
Applying an External Urinary Device
PURPOSES
• To collect urine and control urinary incontinence
• To permit the client physical activity while controlling UI
• To prevent skin irritation as a result of UI
ASSESSMENT
• Review the client record to determine a voiding pattern and
other pertinent data, such as latex sensitivity or allergy.
PLANNING
• Discuss the use of external urinary devices with the client and
family or caregiver.
• Determine if the client has had an external catheter previously
and any difficulties with it.
M47_BERM9793_11_GE_C47.indd 1248
•
Apply clean gloves to examine the client’s penis for swelling or
excoriation that would contraindicate use of the condom catheter.
•
Perform any procedures that are best completed without the
catheter in place; for example, weighing the client would be
easier without the tubing and bag.
27/01/2021 18:07
Chapter 47
●
Urinary Elimination
1249
Applying an External Urinary Device—continued
SKILL 47.1
Assignment
Applying an external urinary device may be assigned to assistive personnel (AP). However, the nurse must determine if the specific client
has unique conditions such as impaired circulation or latex allergy
that would require special training of the AP in the use of the device.
Abnormal findings must be validated and interpreted by the nurse.
Equipment
• Penile sheath of appropriate size. Use the manufacturer’s size
guide as indicated. Use latex-free silicone for clients with latex
allergies. Use self-adhering condom devices, or those with
Velcro, tape, or other external securing device. ❶
• Leg drainage bag if ambulatory or urinary drainage bag with
tubing
• Clean gloves
• Basin of warm water and soap
• Washcloth and towel
• External fixation device (e.g., flexible, self-adhesive tape or
Velcro strap, if needed)
❶ An external urinary device.
IMPLEMENTATION
Preparation
• Assemble the leg drainage bag or urinary drainage bag for
attachment to the condom sheath.
• If the condom supplied is not rolled onto itself, roll the condom
outward onto itself to facilitate easier application.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client what you are going to do, why it is necessary, and how to
participate.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Position the client in either a supine or a sitting position. Provide for client privacy.
• Drape the client appropriately with the bath blanket, exposing only the penis.
4. Apply clean gloves.
5. Inspect and clean the penis.
• Clean the genital area and dry it thoroughly. Rationale: This
minimizes skin irritation and excoriation after the condom is
applied.
6. Apply and secure the condom.
• Roll the condom smoothly over the penis, leaving 2.5 cm
(1 in.) between the end of the penis and the rubber or
plastic connecting tube. ❷ Rationale: This space prevents
irritation of the tip of the penis and provides for full drainage
of urine.
• Secure the condom firmly, but not too tightly, to the penis.
Some condoms have an adhesive inside the proximal end
that adheres to the skin of the base of the penis. Many condoms are packaged with special tape. If neither is present,
use a strip of elastic tape or Velcro around the base of the
penis over the condom. Ordinary tape is contraindicated
because it is not flexible and can stop blood flow.
7. Securely attach the urinary drainage system.
• Make sure that the tip of the penis is not touching the condom and that the condom is not twisted, which can occur
if there is too much space between the tip of the penis and
the funnel of the sheath. Rationale: A twisted condom
could obstruct the flow of urine.
• Attach the urinary drainage system to the condom device.
• Remove and discard gloves.
• Perform hand hygiene.
❷ A self-adhering external urinary device rolled over the penis.
If the client is to remain in bed, attach the urinary drainage
bag to the bed frame.
• If the client is ambulatory, attach the bag to the client’s leg
using both straps. ❸ Rationale: Attaching the drainage
bag to the leg using both straps helps control the movement of the tubing and reduces traction on the sheath and
the risk of it becoming dislodged.
8. Teach the client about the drainage system.
• Instruct the client to keep the drainage bag below the level
of the condom device and to avoid loops or kinks in the
tubing. Instruct the client to report pain, irritation, swelling,
wetness, or leaking around the penis to the primary care
provider.
•
❸ Urinary drainage leg bag.
Continued on page 1250
M47_BERM9793_11_GE_C47.indd 1249
27/01/2021 18:07
1250
Unit 10
●
Promoting Physiologic Health
SKILL 47.1
Applying an External Urinary Device—continued
9. Inspect the penis 30 minutes following device application and
at least every 4 hours. Check urine flow. Document these
findings.
• Assess the penis for swelling and discoloration. Rationale:
This indicates that the condom is too tight.
• Assess urine flow if the client has voided. Normally, some
urine is present in the tube if the flow is not obstructed.
• Assess for redness or skin blistering the first few days.
Rationale: This could indicate a latex allergy.
10. Change the external urinary device as indicated and provide
skin care. In most settings, the condom is changed daily.
• Remove the elastic or Velcro strip, apply clean gloves, and
roll off the condom.
• Wash the penis with soapy water, rinse, and dry it thoroughly.
• Assess the foreskin for signs of irritation, swelling, and
discoloration.
EVALUATION
• Perform a detailed follow-up based on findings that deviated
from expected or normal for the client. Relate findings to previous assessment data if available.
Reapply a new external urinary device.
Remove and discard gloves.
Perform hand hygiene.
11. Document in the client record using forms or checklists supplemented by narrative notes when appropriate. Record the application of the external urinary device, the time, and pertinent
observations, such as irritated areas on the penis.
•
•
•
SAMPLE DOCUMENTATION
4/22/2020 2145 Condom catheter applied for the night per client
request. Glans clean, skin intact. Catheter attached to bedside collection bag. Instructed to notify staff if pain, irritation, swelling, wetness, or leaking occurs. Verbalized that he would. L. Chan, RN
Report significant deviations from normal to the primary care
provider.
•
Managing Urinary Retention
Interventions that assist the client to maintain a normal
voiding pattern, discussed earlier, also apply when dealing
with urinary retention. If these actions are unsuccessful, the
primary care provider may order a cholinergic drug such as
bethanechol chloride (Urecholine) to stimulate bladder contraction and help voiding. Clients who have a flaccid bladder (weak, soft, and lax bladder muscles) may use manual
pressure on the bladder to promote bladder emptying. This
is known as Credé’s maneuver or Credé’s method. It is not
advised without a primary care provider or nurse practitioner’s order and is used only for clients who have lost and
are not expected to regain voluntary bladder control. When
all measures fail to initiate voiding, urinary catheterization
may be necessary to empty the bladder completely. An
indwelling Foley catheter may be inserted until the underlying cause is treated. Alternatively, intermittent straight catheterization (every 3 to 4 hours) may be performed because
the risk of UTI may be less than with an indwelling catheter.
Urinary Catheterization
Urinary catheterization is the introduction of a catheter
through the urethra into the urinary bladder. This is usually performed only when absolutely necessary, because
the danger exists of introducing microorganisms into the
bladder. The Centers for Disease Control and Prevention
[CDC] developed criteria for indwelling urinary catheter
(IUC) insertion as listed in Box 47.2.
The most frequent healthcare-associated infection (HAI)
is a UTI, and IUCs cause 80% of these UTIs (Institute for
Healthcare Improvement [IHI], n.d.). A catheter-associated
urinary tract infection (CAUTI) is a UTI associated with an
IUC that has been in place for more than 2 calendar days
when the day of placement was day one (CDC, 2019). Clients with a CAUTI remain in the hospital longer and need
to be placed on antibiotic therapy, which increases healthcare
costs. The high incidence and high costs related to CAUTI,
M47_BERM9793_11_GE_C47.indd 1250
BOX 47.2
•
•
•
•
•
•
CDC Criteria for IUC Insertion
Acute urinary retention or bladder outlet obstruction
Critically ill and needs accurate measurements of urine output
Selected surgical procedures (e.g., urologic surgery)
Assist in healing of open sacral or perineal wounds in incontinent clients.
Client requires prolonged immobilization (e.g., multiple trauma
injuries)
To improve comfort for end-of-life care if needed.
From Guidelines for Prevention of Catheter-Associated Urinary Tract Infections (2009)
by CDC, 2017, p. 11. Retrieved from https://www.cdc.gov/hicpac/pdf/CAUTI/
CAUTIguideline2009final.pdf
in addition to the fact that most are preventable, resulted in
the Centers for Medicare and Medicaid Services (CMS) not
reimbursing hospitals unless the CAUTI was documented as
present on admission (McNeill, 2017). It is well known that
the risk to the client of developing a CAUTI correlates to the
length of time the catheter is in place. According to the IHI
(n.d.), the risk of infection increases by 3% to 7% for each day
that a catheter remains in place. Best practice is to remove a
urinary catheter that is not necessary.
Although most HAIs are decreasing, the rates for
CAUTI are rising. The American Nurses Association
(ANA, n.d.) states that there is no universally accepted
evidence-based tool to reduce CAUTI as there are for other
HAIs. The ANA, together with the CMS Partnership for
Patients (PfP), made CAUTI reduction a priority. Their
actions resulted in an evidence-based, user-friendly tool
to help nurses prevent CAUTI in hospitals. Box 47.3 provides evidence-based guidelines for preventing CAUTIs.
Another hazard is trauma with urethral catheterization, particularly in the male client, whose urethra
is longer and more tortuous. It is important to insert a
catheter along the normal contour of the urethra. Damage
to the urethra can occur if the catheter is forced through
27/01/2021 18:07
BOX 47.3
Preventing or Reducing the Risk of CAUTI
AVOID UNNECESSARY USE OF AN INDWELLING URINARY
CATHETER (IUC)
• Develop criteria for appropriate catheter insertion (see Box 47.2).
• Consider alternatives to an IUC (e.g., external condom catheter,
toileting protocols).
• Use a bladder scanner to assess for urinary retention.
NURSE PREPARATION FOR INSERTION OF IUC
• Perform hand hygiene.
• Perform pericare, then re-perform hand hygiene.
INSERT IUC USING ASEPTIC TECHNIQUE
• Catheter kit should include a catheter and all necessary items.
• Use the smallest catheter possible that allows for proper drainage and decreases urethral trauma.
• Catheters should only be inserted by trained individuals.
• Use aseptic technique and sterile equipment.
• Obtain assistance prn (e.g., two-person insertion) to help position the client, improve visualization, and help prevent breaks in
aseptic technique.
• Insert the IUC to appropriate length and check urine flow before
inflating the balloon.
• Inflate the IUC balloon per manufacturer’s instructions.
• Secure the IUC.
MAINTAIN THE IUC
• Use hand hygiene and standard precautions during any manipulation of the catheter or collecting system.
Safety Alert!
SAFETY
2019 The Joint Commission National Patient
Safety Goals
Goal 7: Reduce the Risk of Healthcare-Associated Infections
NPSG.07.06.01 Implement evidence-based practices
to prevent indwelling catheter-associated urinary tract
infections (CAUTI).
• Educate staff and licensed independent practitioners
involved in the use of indwelling urinary catheters about
CAUTI and the importance of infection prevention.
• Educate patients who will have an indwelling catheter,
and their families as needed, on CAUTI prevention and
the symptoms of a urinary tract infection.
• Develop written criteria, using established evidencebased guidelines, for placement of an indwelling
urinary catheter.
• Follow written procedures based on established
evidence-based guidelines for inserting and
maintaining an indwelling urinary catheter.
• Measure and monitor CAUTI-prevention processes
and outcomes in high-volume areas.
© Joint Commission Resources: Comprehensive Accreditation Manual for Hospitals, National
Patient Safety Goals. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations, 2019, NPSG-1-23. Reprinted with permission and © Joint Commission
Resources: Comprehensive Accreditation Manual for Nursing Care Centers, National Patient
Safety Goals. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations, 2019, NPSG-1-20. Reprinted with permission.
strictures or at an incorrect angle. In males, the urethra is
normally curved, but it can be straightened by elevating
the penis to a position perpendicular to the body.
Catheters are commonly made of rubber or plastics
although they may be made from latex, silicone, or Teflon.
Latex catheters are inexpensive and the most commonly
Maintain a sterile, closed drainage system.
Maintain unobstructed urine flow; keep catheter and tubing
from kinking.
• Keep the collection bag below the level of the bladder at all
times, but do not rest the bag on the floor.
• Empty the collection bag regularly with a separate, clean collecting container for each client; and prevent contact of the
drainage spigot with the nonsterile collecting container.
•
•
PRACTICES TO AVOID
• Irrigation of catheters, except in cases of catheter obstruction
• Disconnecting the catheter from the drainage tubing
• Replacing catheters routinely
• Cleaning the periurethral area with antiseptics. Routine hygiene
(cleaning the meatus during daily bathing) is appropriate.
REVIEW URINARY CATHETER NECESSITY DAILY
AND REMOVE PROMPTLY
• Assess the need for catheter in daily nursing assessments;
contact the primary care provider if criteria not met.
• Develop nursing protocols that allow nurses to remove urinary
catheters if criteria for necessity are not met and there are no
contraindications for removal.
From “Back to Basics: How Evidence-Based Nursing Practice Can Prevent Catheter-Associated
Urinary Tract Infections,” by L. McNeill, 2017, Urologic Nursing, 37(4), pp. 204–206; Streamlined
Evidence-Based RN Tool: Catheter Associated Urinary Tract Infection (CAUTI) Prevention, by
American Nurses Association, n.d. Retrieved from http://nursingworld.org/CAUTI-Tool; and
“Improving Outcomes with the ANA CAUTI Prevention Tool,” by T. L. Panchisin, 2016,
Nursing, 46(3), pp. 55–59.
used. Silicone catheters may be used if the client has a latex
allergy or prolonged catheterization is required (Schaeffer,
2017). There are also antimicrobial catheters, coated with
an antimicrobial agent; however, they are more expensive
and studies have been inconsistent as to whether they
reduce the occurrence of CAUTI. Catheters are sized by
the diameter of the lumen using the French (Fr) scale:
the larger the number, the larger the lumen. Box 47.4
provides guidelines for catheter selection.
The straight catheter is a single-lumen tube with a
small eye or opening about 1.25 cm (0.5 in.) from the insertion tip (Figure 47.7 ■).
The indwelling, or Foley, catheter is a double-lumen
catheter. The outside end of this two-way indwelling catheter
BOX 47.4
Selecting a Urinary Catheter
Check if client has a latex allergy.
Determine the appropriate catheter length by the client’s gender. For adult female clients use a 22-cm catheter; for adult
male clients, a 40-cm catheter.
• Determine appropriate catheter size by the size of the urethral
canal. Use sizes such as #8 or #10 for children, #14 or #16
for adults. Men frequently require a larger size than women,
for example, #18. The lumen of a silicone catheter is slightly
larger than that of a same-sized latex catheter.
• Select the appropriate balloon size. For adults, use a 5-mL
balloon to facilitate optimal urine drainage. The smaller balloons allow more complete bladder emptying because the
catheter tip is closer to the urethral opening in the bladder.
However, a 30-mL balloon is commonly used to achieve
hemostasis of the prostatic area following a prostatectomy.
Use 3-mL balloons for children.
•
•
1251
M47_BERM9793_11_GE_C47.indd 1251
27/01/2021 18:07
1252
Unit 10
●
Promoting Physiologic Health
Figure 47.9 ■ A coudé catheter.
Figure 47.7 ■ Red-rubber or plastic Robinson straight catheters.
Cardinal Health.
Clients who require continuous or intermittent
bladder irrigation may have a three-way Foley catheter (Figure 47.10 ■). The three-way catheter has a third
lumen through which sterile irrigating fluid can flow into
the bladder. The fluid then exits the bladder through the
drainage lumen, along with the urine.
The size of the indwelling catheter balloon is indicated
on the catheter along with the diameter, for example, “#16
Fr—5 mL balloon.” The purpose of the catheter balloon is
to secure the catheter in the bladder. Historically, nurses
pretested the catheter balloon to prevent insertion of a
defective catheter. Panchisin (2016) states that manufacturers no longer recommend inflating the IUC balloon before
insertion as it may cause microtears, increasing the risk of
infection (p. 56). Pretesting of silicone balloons is not recommended because the silicone can form a cuff or crease
at the balloon area that can cause trauma to the urethra
Figure 47.8 ■ An indwelling (Foley) catheter with the balloon inflated.
is bifurcated; that is, it has two openings, one to drain the
urine, the other to inflate the balloon (Figure 47.8 ■). The
larger lumen drains urine from the bladder and the second
smaller lumen is used to inflate the balloon near the tip of
the catheter to hold the catheter in place within the bladder.
A variation of the indwelling catheter is the coudé
(elbowed) catheter, which has a curved tip (Figure 47.9
■). This is sometimes used for men who have an enlarged
prostate (benign prostatic hyperplasia), because its tip is
somewhat stiffer than a regular catheter and thus it can
be better controlled during insertion, and passage is often
less traumatic.
M47_BERM9793_11_GE_C47.indd 1252
Figure 47.10 ■ A three-way Foley catheter often used for continuous
bladder irrigation.
Cardinal Health.
27/01/2021 18:07
Chapter 47
during catheter insertion. It is important to follow the
manufacturer’s instructions for the proper volume to use
for balloon inflation. Improperly inflated catheter balloons may cause drainage and deflation difficulties.
Indwelling catheters are usually connected to a closed
gravity drainage system. This system consists of the catheter, drainage tubing, and a collecting bag for the urine. A
closed system cannot be opened anywhere along the system, from catheter to collecting bag. It is the standard of
care because it reduces the risk of microorganisms entering
the system and infecting the urinary tract. Urinary drainage
●
Urinary Elimination
1253
systems typically depend on the force of gravity to drain
urine from the bladder to the collecting bag.
Skill 47.2 describes catheterization of females and
males, using straight and indwelling catheters.
Nursing Interventions for Clients with Indwelling Catheters
Nursing care of the client with an indwelling catheter and
continuous drainage is mostly directed toward preventing infection of the urinary tract and encouraging urinary
flow through the drainage system. It includes encouraging large amounts of fluid intake, accurately recording
Performing Indwelling Urinary Catheterization
ASSESSMENT
• Determine the most appropriate method of catheterization based
on the purpose and any criteria specified in the order such as total
amount of urine to be removed or size of catheter to be used.
• Use a straight catheter if only a one-time urine specimen is
needed, if amount of residual urine is being measured, or if temporary emptying of the bladder is required.
• Use an indwelling catheter if the bladder must remain empty,
intermittent catheterization is contraindicated, or continuous
urine measurement or collection is needed.
• Assess the client’s overall condition. Determine if the client is able
to participate and hold still during the procedure and if the client
PLANNING
• Allow adequate time to perform the catheterization. Although
the entire procedure can require as little as 15 minutes, several
sources of difficulty could result in a much longer period of time.
If possible, it should not be performed just prior to or after a meal.
• Some agencies require two nurses to be present for the procedure: one to perform the catheterization and the other to assist
with positioning and ensure there is no break in aseptic technique.
• Some clients may feel uncomfortable being catheterized by
nurses of the opposite gender. If this is the case, obtain the client’s permission. Also consider whether agency policy requires
or encourages having an individual of the client’s same gender
present for the procedure.
Assignment
Due to the need for sterile technique and detailed knowledge of
anatomy, insertion of a urinary catheter is not assigned to AP.
Equipment
For a straight catheterization:
• Straight catheterization kit:
• Sterile straight catheter of appropriate size
• Sterile gloves
• Waterproof drape(s)
• Antiseptic solution
• Cleansing balls
• Forceps
• Water-soluble lubricant
•
•
•
•
•
To facilitate accurate measurement of urinary output for critically
ill clients whose output needs to be monitored hourly
To provide for intermittent or continuous bladder drainage and/
or irrigation
To prevent urine from contacting an incision after perineal surgery if needed
To assist in healing of open sacral or perineal wounds in incontinent clients
To improve comfort for end-of-life care if needed.
SKILL 47.2
PURPOSES
Straight catheter:
• To relieve discomfort due to bladder distention
• To assess the amount of residual urine if the bladder empties
incompletely
• To obtain a sterile urine specimen
• To empty the bladder completely prior to surgery.
Indwelling catheter:
• To relieve urinary retention or bladder outlet obstruction
• For selected surgical procedures
can be positioned supine with head relatively flat. For female clients, determine if she can have knees bent and hips externally
rotated.
• Determine when the client last voided or was last catheterized.
• If catheterization is being performed because the client has
been unable to void, when possible, complete a bladder scan
to assess the amount of urine present in the bladder. Rationale:
This prevents catheterizing the bladder when insufficient urine is
present. Often, a minimum of 500 to 800 mL of urine indicates
urinary retention and the client should be reassessed until that
amount is present.
Urine receptacle
Specimen container.
(An extra catheter should also be at hand in case of a break in
aseptic technique.)
For an indwelling catheter:
• Closed catheterization kit ❶:
• Sterile indwelling catheter of appropriate size
•
•
❶ A closed indwelling urinary catheter insertion kit.
Continued on page 1254
M47_BERM9793_11_GE_C47.indd 1253
27/01/2021 18:07
1254
Unit 10
●
Promoting Physiologic Health
Performing Indwelling Urinary Catheterization—continued
Sterile gloves
Waterproof drape(s)
Antiseptic solution
Cleansing balls
Forceps
Water-soluble lubricant
Syringe prefilled with sterile water in amount specified by
catheter manufacturer
• Collection bag and tubing
SKILL 47.2
•
•
•
•
•
•
•
5–10 mL 2% Xylocaine gel or water-soluble lubricant for male
urethral injection (if agency permits)
• Clean gloves
• Supplies for performing perineal cleansing
• Bath blanket or sheet for draping the client
• Adequate lighting (Obtain a flashlight or lamp if necessary.)
(An extra catheter should also be at hand in case of a break in
aseptic technique.)
•
IMPLEMENTATION
Preparation
• If using a catheterization kit, read the label carefully to ensure
that all necessary items are included.
• Apply clean gloves and perform routine perineal care to cleanse
the meatus from gross contamination. ❷ For women, use
this time to locate the urinary meatus relative to surrounding
structures. ❸
• Remove and discard gloves.
• Perform hand hygiene.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client
what you are going to do, why it is necessary, and how to
participate.
Labia majora
Clitoris
Urinary meatus
Vagina
Labia minora
Anus
❸ To expose the urinary meatus, separate the labia minora and retract
the tissue upward.
A
B
❷ A, Male and B, female pericare in preparation for catheterization.
M47_BERM9793_11_GE_C47.indd 1254
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
4. Place the client in the appropriate position and drape all areas
except the perineum.
• Female: supine with knees flexed, feet about 2 feet apart,
and hips slightly externally rotated, if possible
• Male: supine, thighs slightly abducted or apart
5. Establish adequate lighting. Stand on the client’s right if
you are right-handed, on the client’s left if you are left-handed.
6. If using a collecting bag and it is not contained within the catheterization kit, open the drainage package and place the end
of the tubing within reach. Rationale: Because one hand is
needed to hold the catheter once it is in place, open the package while two hands are still available.
7. If agency policy permits, apply clean gloves and inject 10 to
15 mL Xylocaine gel into the urethra of the male client. Wipe
the underside of the penile shaft to distribute the gel up the
urethra. Wait at least 5 minutes for the gel to take effect before
inserting the catheter.
8. Remove and discard gloves.
• Perform hand hygiene.
9. Open the catheterization kit. Place a waterproof drape under
the buttocks (female) or penis (male) without contaminating the
center of the drape with your hands.
10. Apply sterile gloves.
11. Organize the remaining supplies:
• Saturate the cleansing balls with the antiseptic solution. ❹
• Open the lubricant package. ❺
• Remove the specimen container and place it nearby with
the lid loosely on top.
• Remove plastic covering of indwelling catheter. ❻
27/01/2021 18:07
Chapter 47
●
Urinary Elimination
1255
Performing Indwelling Urinary Catheterization—continued
SKILL 47.2
❹ Saturating the cleansing balls with the antiseptic solution.
❼ Lubricating the catheter.
❽ Attaching the prefilled syringe to the IUC.
❺ Putting lubricant on the tray.
❻ Removing the wrapping of the IUC.
12. Lubricate the catheter 2.5 to 5 cm (1 to 2 in.) for females, 15
to 17.5 cm (6 to 7 in.) for males, and place it with the drainage
end inside the collection container. ❼
13. Attach the prefilled syringe to the indwelling catheter inflation
hub. ❽ Do not pre-inflate the balloon. Rationale: Pre-inflation
is no longer recommended and may cause microtears, risking
infection.
14. If desired, place the fenestrated drape over the perineum,
exposing the urinary meatus. ❾
15. Cleanse the meatus. Note: The nondominant hand is
considered contaminated once it touches the client’s skin.
• Females: Use your nondominant hand to spread the
labia so that the meatus is visible. Establish firm but
gentle pressure on the labia. The antiseptic may make
the tissues slippery but the labia must not be allowed
to return over the cleaned meatus. Note: Location of
the urethral meatus is best identified during the cleansing process. Pick up a cleansing ball with the forceps
in your dominant hand and wipe one side of the labia
majora in an anteroposterior direction. ❿ Use great
care that wiping the client does not contaminate this
Continued on page 1256
M47_BERM9793_11_GE_C47.indd 1255
27/01/2021 18:08
1256
Unit 10
●
Promoting Physiologic Health
SKILL 47.2
Performing Indwelling Urinary Catheterization—continued
❿ When cleaning the urinary meatus, move the swab downward.
⓫ Cleanse center of male meatus in a circular motion around the glans.
❾ Drape over the perineum of male and female.
sterile hand. Use a new ball for the opposite side.
Repeat for the labia minora. Use the last ball to cleanse
directly over the meatus.
• Males: Use your nondominant hand to grasp the
penis just below the glans. If necessary, retract the
foreskin. Hold the penis firmly upright, with slight tension. Rationale: Lifting the penis in this manner helps
straighten the urethra. Pick up a cleansing ball with
the forceps in your dominant hand and wipe from the
center of the meatus in a circular motion around the
glans. ⓫ Use great care that wiping the client does
not contaminate the sterile hand. Use a new ball and
repeat 3 more times. The antiseptic may make the tissues
slippery but the foreskin must not be allowed to return
over the cleaned meatus nor the penis be dropped.
16. Insert the catheter.
• Grasp the catheter firmly 5 to 7.5 cm (2 to 3 in.) from the
tip. Ask the client to take a slow deep breath and insert
the catheter as the client exhales. ⓬ Slight resistance is
expected as the catheter passes through the sphincter. If
necessary, twist the catheter or hold pressure on the catheter until the sphincter relaxes.
• Advance the catheter 5 cm (2 in.) farther after the urine
begins to flow through it. Rationale: This is to be sure
it is fully in the bladder, will not easily fall out, and the
M47_BERM9793_11_GE_C47.indd 1256
balloon is in the bladder completely. For male clients,
advance the catheter to the “Y” bifurcation of the
catheter.
• If the catheter accidentally contacts the labia or slips into
the vagina, it is considered contaminated and a new, sterile
catheter must be used. The contaminated catheter may be
left in the vagina until the new catheter is inserted to help
avoid mistaking the vaginal opening for the urethral meatus.
17. Hold the catheter with the nondominant hand.
18. For an indwelling catheter, inflate the IUC balloon with the designated volume. ⓭
• Without releasing the catheter (and, for females,
without releasing the labia), hold the inflation valve
between two fingers of your nondominant hand while
you attach the syringe (if not left attached earlier) and
inflate with your dominant hand. If the client complains
of discomfort, immediately withdraw the instilled fluid,
advance the catheter farther, and attempt to inflate the
balloon again.
• Pull gently on the catheter until resistance is felt to ensure
that the balloon has inflated and to place it in the trigone of
the bladder.
19. Collect a urine specimen if needed. For a straight catheter,
allow 20 to 30 mL to flow into the bottle without touching the
catheter to the bottle. For an indwelling catheter preattached
to a drainage bag, a specimen may be taken from the bag this
initial time only.
27/01/2021 18:08
Chapter 47
●
Urinary Elimination
1257
Performing Indwelling Urinary Catheterization—continued
⓬ Insert the catheter.
SKILL 47.2
20. Allow the straight catheter to continue draining into the urine
receptacle. If necessary (e.g., open system), attach the drainage end of an indwelling catheter to the collecting tubing
and bag.
21. Examine and measure the urine. In some cases, only 750
to 1000 mL of urine are to be drained from the bladder at
one time. Check agency policy for further instructions if this
should occur.
22. Remove the straight catheter when urine flow stops. For an
indwelling catheter, secure the catheter tubing to the thigh
for female clients or the upper thigh or lower abdomen for male
clients to prevent movement on the urethra or excessive tension or pulling on the indwelling balloon. Adhesive and nonadhesive catheter-securing devices are available and should be
used to secure the catheter tubing to the client. ⓮ Rationale:
This prevents unnecessary trauma to the urethra.
A
B
⓮ Catheter securement devices: A, nonadhesive device (Velcro
⓭ Inflating the IUC balloon.
strap); B, adhesive device.
Continued on page 1258
M47_BERM9793_11_GE_C47.indd 1257
27/01/2021 18:08
1258
Unit 10
●
Promoting Physiologic Health
SKILL 47.2
Performing Indwelling Urinary Catheterization—continued
23. Next, hang the bag below the level of the bladder. No tubing
should fall below the top of the bag. ⓯
24. Wipe any remaining antiseptic or lubricant from the perineal
area. Replace the foreskin if retracted earlier. Return the client
to a comfortable position. Instruct the client on positioning
and moving with the catheter in place.
25. Discard all used supplies in appropriate receptacles.
26. Remove and discard gloves.
• Perform hand hygiene.
27. Document the catheterization procedure including
catheter size and results in the client record using forms
or checklists supplemented by narrative notes when
appropriate.
SAMPLE DOCUMENTATION
2/24/2020 0530 Client agreed to insertion of pre-op catheter as
per order. #16 Fr Foley with 5-mL balloon inserted without difficulty,
secured to thigh, connected to continuous drainage. Immediate
return of 300 mL pale, clear, yellow urine. G. Hampton, RN
⓯ Correct position for urine drainage bag and tubing.
EVALUATION
• Notify the primary care provider of the catheterization results.
• Perform a detailed follow-up based on findings that deviated
from expected or normal for the client. Compare findings to
previous assessment data if available.
•
Teach the client how to care for the indwelling catheter, to drink
more fluids, and provide other appropriate instructions.
LIFESPAN CONSIDERATIONS Urinary Catheterization
INFANTS AND CHILDREN
• Adapt the size of the catheter for pediatric clients.
• Ask a family member to assist in holding the child during catheterization, if appropriate.
OLDER ADULTS
When catheterizing older clients, be very attentive to problems of
limited movement, especially in the hips. Arthritis, or previous hip
or knee surgery, may limit their movement and cause discomfort.
Modify the position (e.g., side-lying) as needed to perform the procedure safely and comfortably. For women, obtain the assistance of
another nurse to flex and hold the client’s knees and hips as necessary or place her in a modified Sims’ position.
the fluid I&O, maintaining the patency of the drainage
system, preventing contamination of the drainage system,
and teaching these measures to the client.
the acidity of urine. Conversely, most fruits and vegetables,
legumes, and milk and milk products result in alkaline urine.
Fluids
No special cleaning other than routine daily hygienic care
with soap and water is necessary for clients with an indwelling catheter, nor is special meatal care recommended. The
nurse should check agency practice in this regard.
The client with an indwelling catheter should drink up to
3000 mL/day if permitted. Large amounts of fluid ensure a
large urine output, which keeps the bladder flushed out and
decreases the likelihood of urinary stasis and subsequent
infection. Large volumes of urine also minimize the risk of
sediment or other particles obstructing the drainage tubing.
Dietary Measures
Acidifying the urine of clients with an indwelling catheter
may reduce the risk of UTI and calculus formation. Foods
such as eggs, cheese, meat and poultry, whole grains, cranberries, plums and prunes, and tomatoes tend to increase
M47_BERM9793_11_GE_C47.indd 1258
Perin eal Care
Changing the Catheter and Tubing
Routine changing of catheter and tubing is not recommended. Collection of sediment in the catheter or tubing
and impaired urine drainage are indicators for changing
the catheter and drainage system. When this occurs the
catheter and drainage system are removed and discarded,
and a new sterile catheter with a closed drainage system
is inserted using aseptic technique.
27/01/2021 18:08
Chapter 47
Removing Indwelling Catheters
Indwelling catheters are removed after their purpose has
been achieved, usually on the order of the primary care
provider. Unfortunately, not all primary care providers
know which of their clients has an indwelling catheter.
As a result, some facilities have incorporated an alert
system that requires the provider to take an action after
a specified time frame. Increasingly, healthcare facilities
are allowing the nurse to remove an indwelling catheter
through the use of a nurse-driven protocol with specific
criteria.
If the catheter has been in place for a short time (e.g.,
48 to 72 hours), the client usually has little difficulty
regaining normal urinary elimination patterns. Swelling
of the urethra, however, may initially interfere with voiding, so the nurse should regularly assess the client for urinary retention until voiding is reestablished.
Clients who have had an indwelling catheter for a
prolonged period may require bladder retraining to
regain bladder muscle tone. With an indwelling catheter
in place, the bladder muscle does not stretch and contract regularly as it does when the bladder fills and empties by voiding. A few days before removal, the catheter
may be clamped for specified periods of time (e.g., 2 to 4
hours), then released to allow the bladder to empty. This
allows the bladder to distend and stimulates its musculature. Check agency policy regarding bladder training
procedures.
To remove an indwelling catheter the nurse follows
these steps:
•
•
•
•
•
•
•
•
Obtain a receptacle for the catheter (e.g., a disposable
basin); a clean, disposable towel; clean gloves; and
a sterile syringe to deflate the balloon. The syringe
should be large enough to withdraw all the solution in
the catheter balloon. The size of the balloon is indicated
on the label at the end of the catheter.
Ask the client to assume a supine position as for a
catheterization.
Optional: Obtain a sterile specimen before removing the
catheter. Check agency protocol.
Remove the catheter-securing device attaching the
catheter to the client, apply gloves, and then place the
towel between the legs of the female client or over the
thighs of the male.
Insert the syringe into the injection port of the catheter,
and withdraw the fluid from the balloon. After the fluid
has been aspirated, the walls of the balloon do not deflate
to their original shape but collapse into uneven ridges,
forming a “cuff” around the catheter. This cuff is more
pronounced with a silicone catheter. This cuff may cause
discomfort to the client as the catheter is removed.
Do not pull the catheter while the balloon is inflated;
doing so will injure the urethra.
After all of the fluid is removed from the balloon, gently
withdraw the catheter and place it in the waste receptacle.
Dry the perineal area with a towel.
• Measure the urine in the drainage bag.
M47_BERM9793_11_GE_C47.indd 1259
•
•
•
•
•
●
Urinary Elimination
1259
Remove and discard gloves.
• Perform hand hygiene.
Record the removal of the catheter. Include in the
recording (a) the time the catheter was removed; (b) the
amount, color, and clarity of the urine; (c) the intactness
of the catheter; and (d) instructions given to the client.
Provide the client with either a urinal (men), bedpan,
commode, or toilet collection device (“hat”) to be used
with each subsequent unassisted void.
Following removal of the catheter, determine the time
of the first voiding and the amount voided during the
first 8 hours. Compare this output to the client’s intake.
Observe for dysfunctional voiding behaviors (i.e.,
6 100 mL per void), which might indicate urinary retention. If this occurs, perform an assessment of PVR using a
bladder scanner if available. Generally a PVR greater than
200 mL will require straight catheterization as needed.
Clean Intermittent Catheterization
Clean intermittent catheterization (CIC) is performed by
many clients who have some form of neurogenic bladder
dysfunction such as that caused by spinal cord injury and
multiple sclerosis. Clean or medical aseptic technique is
used. CIC has these benefits:
•
•
•
•
•
•
Enables the client to retain independence and gain control of the bladder
Reduces incidence of UTI
Protects the upper urinary tract from reflux
Allows normal sexual relations without incontinence
Reduces the use of aids and appliances
Frees the client from embarrassing dribbling.
The procedure for self-catheterization is similar to
that used by the nurse to catheterize a client. Essential
steps are outlined in the accompanying Client Teaching. Because the procedure requires physical and mental
preparation, client assessment is important. The client
should have:
•
•
•
•
•
Sufficient manual dexterity to manipulate a catheter
Sufficient mental ability
Motivation and acceptance of the procedure
For women, reasonable agility to access the urethra
Bladder capacity greater than 100 mL.
Before teaching CIC, the nurse should establish the
client’s voiding patterns, the volume voided, fluid intake,
and residual amounts. CIC is easier for males to learn
because of the visibility of the urinary meatus. Females
need to learn initially with the aid of a mirror but eventually should perform the procedure by using only the sense
of touch (as described in Client Teaching).
Urinary Irrigations
An irrigation is a flushing or washing-out with a specified
solution. Bladder irrigation is carried out on a primary care
provider’s order, usually to wash out the bladder and sometimes to apply a medication to the bladder lining. Catheter
irrigations may also be performed to maintain or restore the
27/01/2021 18:08
1260
Unit 10
●
Promoting Physiologic Health
CLIENT TEACHING Clean Intermittent Catheterization (CIC)
•
•
•
•
•
•
•
•
Catheterize as often as needed to maintain. At first, catheterization may be necessary every 2 to 3 hours, increasing to 4 to 6
hours.
Attempt to void before catheterization; insert the catheter to
remove residual urine if unable to void or if amount voided is
insufficient (e.g., less than 100 mL).
Assemble all needed supplies ahead of time. Good lighting is
essential, especially for women.
Wash your hands.
Clean the urinary meatus with either a towelette or soapy washcloth, then rinse with a wet washcloth. Women should clean the
area from front to back.
Assume a position that is comfortable and that facilitates passage of the catheter, such as a semireclining position in bed or
sitting on a chair or the toilet. Men may prefer to stand over the
toilet; women may prefer to stand with one foot on the side of
the toilet.
Apply lubricant to the catheter tip (1 in. [2.5 cm] for women; 2
to 6 in. [5 to 15 cm] for men). Some catheters are coated with a
slippery surface that may require activation of a wetting solution
and eliminating the need for a lubricant.
Insert the catheter until urine flows through.
patency of a catheter, for example, to remove pus or blood
clots blocking the catheter. Sterile technique is used.
The closed method is the preferred technique for
catheter or bladder irrigation because it is associated
with a lower risk of UTI. Closed catheter irrigations
may be either continuous or intermittent. This method
is most often used for clients who have had genitourinary surgery. The continuous irrigation helps prevent
blood clots from occluding the catheter. A three-way,
or triple lumen, catheter (see Figure 47.10) is generally used for closed irrigations. The irrigating solution
flows into the bladder through the irrigation port of the
catheter and out through the urinary drainage lumen of
the catheter.
•
•
•
•
•
a. If a woman, locate the meatus using a mirror or other aid, or
use the “touch” technique as follows:
• Place the index finger of your nondominant hand on
your clitoris.
• Place the third and fourth fingers at the vagina.
• Locate the meatus between the index and third fingers.
• Direct the catheter through the meatus and then upward
and forward.
b. If a man, hold the penis with a slight upward tension at a
60° to 90° angle to insert the catheter. Return the penis to
its natural position when urine starts to flow.
Hold the catheter in place until all urine is drained.
Withdraw the catheter slowly to ensure complete drainage
of urine.
Discard the catheter. Evidence does not endorse catheter reuse
(Beauchemin, Newman, LeDanseur, Jackson, & Ritmiller, 2018).
Contact your care provider if your urine becomes cloudy or
contains sediment; if you have bleeding, difficulty, or pain when
passing the catheter; or if you have a fever.
Drink at least 2000 to 2500 mL of fluid a day to ensure adequate
bladder filling and flushing. To keep your urine acidic and reduce
the risk of bladder infections, drink cranberry and prune juices.
Occasionally an open irrigation may be necessary to
restore catheter patency. The risk of injecting microorganisms into the urinary tract is greater with open irrigations, because the connection between the indwelling
catheter and the drainage tubing is broken. Strict precautions must be taken to maintain the sterility of both
the drainage tubing connector and the interior of the
indwelling catheter.
The open method of catheter or bladder irrigation is
performed with double-lumen indwelling catheters. It
may be necessary for clients who develop blood clots and
mucous fragments that occlude the catheter or when it is
undesirable to change the catheter. Techniques for bladder
irrigation are outlined in Skill 47.3.
SKILL 47.3
Performing Bladder Irrigation
PURPOSES
• To maintain the patency of a urinary catheter and tubing (closed
continuous irrigation)
ASSESSMENT
• Determine the client’s current urinary drainage system. Review
the client record for recent I&O and any difficulties the client has
been experiencing with the system. Review the results of previous irrigations.
PLANNING
Before irrigating a catheter or bladder, check (a) the reason for the
irrigation; (b) the order authorizing the continuous or intermittent irrigation (in most agencies, a primary care provider’s order is required);
(c) the type of sterile solution, the amount and strength to be used,
and the rate (if continuous); and (d) the type of catheter in place. If
these are not specified on the client’s chart, check agency protocol.
M47_BERM9793_11_GE_C47.indd 1260
•
To free a blockage in a urinary catheter or tubing (open intermittent irrigation)
•
Assess the client for any discomfort, bladder spasms, or distended bladder.
Assignment
Due to the need for sterile technique, urinary irrigation is generally
not assigned to AP. If the client has continuous irrigation, the AP
may care for the client and note abnormal findings. These must be
validated and interpreted by the nurse.
27/01/2021 18:08
Chapter 47
●
Urinary Elimination
1261
Performing Bladder Irrigation—continued
IMPLEMENTATION
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client
what you are going to do, why it is necessary, and how to participate. The irrigation should not be painful or uncomfortable.
Discuss how the results will be used in planning further care or
treatments.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Provide for client privacy.
4. Apply clean gloves.
5. Empty, measure, and record the amount and appearance of
urine present in the drainage bag. Rationale: Emptying the
drainage bag allows more accurate measurement of urinary
output after the irrigation is in place or completed. Assessing the character of the urine provides baseline data for later
comparison.
6. Discard urine and gloves.
7. Prepare the equipment.
• Perform hand hygiene.
• Connect the irrigation infusion tubing to the irrigating solution and flush the tubing with solution, keeping the tip sterile. Rationale: Flushing the tubing removes air and prevents
it from being instilled into the bladder.
• Apply clean gloves and cleanse the port with antiseptic
swabs.
• Connect the irrigation tubing to the input port of the threeway indwelling catheter.
• Connect the drainage bag and tubing to the urinary drainage port if not already in place.
• Remove and discard gloves.
• Perform hand hygiene.
8. Irrigate the bladder.
• For closed continuous irrigation using a three-way catheter,
open the clamp on the urinary drainage tubing (if present).
❶ Rationale: This allows the irrigating solution to flow out
of the bladder continuously.
a. Apply clean gloves.
b. Open the regulating clamp on the irrigating fluid infusion
tubing and adjust the flow rate as prescribed by the
primary care provider or to 40 to 60 drops per minute if
not specified.
c. Assess the drainage for amount, color, and clarity.
The amount of drainage should equal the amount
of irrigant entering the bladder plus expected urine
output. Empty the bag frequently so that it does not
exceed half full.
• For closed intermittent irrigation, determine whether the
solution is to remain in the bladder for a specified time.
a. If the solution is to remain in the bladder (a bladder
irrigation or instillation), close the clamp to the urinary
drainage tubing. Rationale: Closing the flow clamp
allows the solution to be retained in the bladder and in
contact with bladder walls.
Sterile irrigating solution warmed or at room temperature (Label
the irrigant clearly with the words Bladder Irrigation, including
the information about any medications that have been added
to the original solution, and the date, time, and nurse’s initials.)
• Infusion tubing
• IV pole
•
SKILL 47.3
Equipment
• Clean gloves (two pairs)
• Indwelling catheter in place
• Drainage tubing and bag (if not in place)
• Drainage tubing clamp
• Antiseptic swabs
• Sterile receptacle
Irrigation bag
Drip chamber
Clamp
Bladder
Tubing
to irrigation
port
of catheter balloon
Tubing
from
bladder
Drainage
bag
❶ A continuous bladder irrigation (CBI) setup.
b. If the solution is being instilled to irrigate the catheter,
open the flow clamp on the urinary drainage tubing.
Rationale: Irrigating solution will flow through the urinary
drainage port and tubing, removing mucous shreds
or clots.
c. If a three-way catheter is used, open the flow clamp to
the irrigating fluid infusion tubing, allowing the specified
amount of solution to infuse. Then close the clamp on
the infusion tubing.
or
d. If a two-way catheter is used, connect an irrigating syringe with a needleless adapter to the injection port on the drainage tubing and instill the
solution.
e. After the specified period the solution is to be retained
has passed, open the drainage tubing flow clamp and
allow the bladder to empty.
f. Assess the drainage for amount, color, and clarity.
The amount of drainage should equal the amount
of irrigant entering the bladder plus expected urine
output.
g. Remove and discard gloves.
• Perform hand hygiene.
9. Assess the client and the urinary output.
• Assess the client’s comfort.
• Apply clean gloves.
Continued on page 1262
M47_BERM9793_11_GE_C47.indd 1261
27/01/2021 18:08
1262
Unit 10
●
Promoting Physiologic Health
Performing Bladder Irrigation—continued
3. Prepare the equipment.
• Perform hand hygiene.
• Using aseptic technique, open supplies and pour the irrigating
solution into the sterile basin or receptacle. Rationale: Aseptic
technique is vital to reduce the risk of instilling microorganisms into the urinary tract during the irrigation.
• Place the disposable water-resistant towel under the
catheter.
• Apply clean gloves.
• Disconnect catheter from drainage tubing and place the
catheter end in the sterile basin. Place sterile protective
cap over end of drainage tubing. Rationale: The end of
the drainage tubing will be considered contaminated if it
touches bed linens or skin surfaces.
• Draw the prescribed amount of irrigating solution into the
syringe, maintaining the sterility of the syringe and solution.
4. Irrigate the bladder.
• Insert the tip of the syringe into the catheter opening.
• Gently and slowly inject the solution into the catheter at
approximately 3 mL per second. In adults, about 30 to
40 mL generally is instilled for catheter irrigations; 100 to
200 mL may be instilled for bladder irrigation or instillation.
Rationale: Gentle instillation reduces the risks of injury to
bladder mucosa and of bladder spasms.
• Remove the syringe and allow the solution to drain back
into the basin.
• Continue to irrigate the client’s bladder until the total
amount to be instilled has been injected or when fluid
returns are clear and clots are removed.
• Remove the protective cap from the drainage tube and
wipe with antiseptic swab.
• Reconnect the catheter to drainage tubing.
• Remove and discard gloves.
• Perform hand hygiene.
• Assess the drainage for amount, color, and clarity. The
amount of drainage should equal the amount of irrigant
entering the bladder plus any urine that may have been
dwelling in the bladder. Determine the amount of fluid used
for the irrigation and subtract from total output on the client’s I&O record.
5. Assess the client and the urinary output and document the
procedure as in steps 8 and 9.
Empty the drainage bag and measure the contents. Subtract the amount of irrigant instilled from the total volume of
drainage to obtain the volume of urine output.
• Remove and discard gloves.
• Perform hand hygiene.
10. Document findings in the client record using forms or checklists supplemented by narrative notes when appropriate.
• Note any abnormal constituents such as blood clots, pus,
or mucous shreds.
Variation: Open Irrigation Using a Two-Way Indwelling Catheter
1. Assemble the equipment. Use an irrigation tray ❷ or assemble
individual items, including:
• Clean gloves
• Disposable water-resistant towel
• Sterile irrigating solution
• Sterile irrigation set
• Sterile basin
• Sterile 30- to 50-mL irrigating syringe
• Antiseptic swabs
• Sterile protective cap for catheter drainage tubing.
2. Prepare the client (see steps 1–5 of main procedure for
catheter irrigation).
SKILL 47.3
•
❷ An irrigation set.
EVALUATION
• Perform detailed follow-up based on findings that deviated from
expected or normal for the client. Relate findings to previous
assessment data if available.
Suprapubic Catheter Care
A suprapubic catheter is inserted surgically through the
abdominal wall above the symphysis pubis into the urinary
bladder. The suprapubic catheter may have a balloon or
pigtail that holds it in the bladder depending on the manufacturer (Figure 47.11 ■). The healthcare provider inserts the
catheter using local anesthesia or during bladder or vaginal
surgery. The catheter may be secured in place with sutures
to reinforce the security of the catheter and is then attached
to a closed drainage system. The suprapubic catheter may
be placed for temporary bladder drainage until the client is
able to resume normal voiding (e.g., after urethral, bladder,
or vaginal surgery) or it may become a permanent device
(e.g., urethral or pelvic trauma).
M47_BERM9793_11_GE_C47.indd 1262
•
Report significant deviations from normal to the primary care
provider.
Care of clients with a suprapubic catheter includes
regular assessments of the client’s urine, fluid intake, and
comfort; maintenance of a patent drainage system; skin
care around the insertion site; and periodic clamping of
the catheter prior to removing it if it is not a permanent
appliance. If the catheter is temporary, orders generally
include leaving the catheter open to drainage for 48 to
72 hours, then clamping the catheter for 3- to 4-hour periods during the day until the client can void satisfactory
amounts. Satisfactory voiding is determined by measuring the client’s residual urine after voiding.
Care of the catheter insertion site involves sterile
technique. Dressings around the newly placed suprapubic catheter are changed whenever they are soiled with
27/01/2021 18:08
Chapter 47
Urinary Elimination
1263
be needed and the healed insertion tract enables removal
and replacement of the catheter as needed. Formation,
however, of a healed insertion tract takes approximately
6 weeks to 6 months to develop. Before that time, the
catheter needs to be replaced within 30 minutes if it falls
out to prevent the opening from closing over. The nurse
assesses the insertion area at regular intervals. If pubic
hair invades the insertion site, it may be carefully trimmed
with scissors. Any redness or discharge at the skin around
the insertion site must be reported.
To collection bag
Symphysis pubis
Removable
trocar cannula
Urinary
bladder
Suprapubic
catheter
●
Urinary Diversions
A urinary diversion is the surgical rerouting of urine from
the kidneys to a site other than the bladder. Clients with
bladder cancer often need a urinary diversion when the
bladder must be removed or bypassed. There are two categories of diversions: incontinent and continent.
A
Bladder
Inflated
balloon
Prostate
Catheter
Incontinent
Pubic
bone
Urethra
B
Figure 47.11 ■ A suprapubic catheter in place: A, using a pigtail
loop; B, using a balloon to keep the catheter in place.
drainage to prevent bacterial growth around the insertion
site and reduce the potential for infection. Cleanse with
4*4s with chlorhexidine gluconate and warm water. The
area is dressed with a 4*4 and taped in an occlusive fashion. Securing the catheter tube to the abdomen helps to
reduce tension at the insertion site. For catheters that have
been in place for an extended period, no dressing may
With incontinent diversions clients have no control over
the passage of urine and require the use of an external
ostomy appliance to contain the urine. Urinary diversions may or may not involve the removal of the bladder
(cystectomy). Examples of incontinent diversions include
ureterostomy, nephrostomy, vesicostomy, and ileal conduits.
A ureterostomy is when one or both of the ureters may be
brought directly to the side of the abdomen to form small
stomas. This procedure, however, has some disadvantages
in that the stomas provide direct access for microorganisms
from the skin to the kidneys, the small stomas are difficult to
fit with an appliance to collect the urine, and they may narrow, impairing urine drainage. A nephrostomy diverts urine
from the kidney via a catheter inserted into the renal pelvis
to a nephrostomy tube and bag (Figure 47.12 ■).
A vesicostomy may be formed when the bladder is left
intact but voiding through the urethra is not possible (e.g.,
due to an obstruction or a neurogenic bladder). The ureters
Rib cage
Kidney
Kidney
Nephrostomy
catheter
Nephrostomy
catheter
Nephrostomy
tube and bag
Ureter
Ureter
Bladder
Pigtail loop locks nephrostomy
tube in place
Urethra
Figure 47.12 ■ A nephrostomy.
M47_BERM9793_11_GE_C47.indd 1263
27/01/2021 18:08
1264
Unit 10
●
Promoting Physiologic Health
Kidney
Ureter
Ileal
conduit
Stoma
Bladder
removed
Reattachment
or
Anastomosis
of ileum
Figure 47.13 ■ An incontinent urinary diversion (ileal conduit).
remain connected to the bladder, and the bladder wall is
surgically attached to an opening in the skin below the
navel, forming an opening (stoma) for urinary drainage.
The most common incontinent urinary diversion is the
ileal conduit or ileal loop (Figure 47.13 ■). In this procedure,
a segment of the ileum is removed and the intestinal ends
are reattached. One end of the portion removed is closed
with sutures to create a pouch, and the other end is brought
out through the abdominal wall to create a stoma. The ureters are implanted into the ileal pouch. The ileal stoma is
more readily fitted with an appliance than ureterostomies
because of its larger size. The mucous membrane lining of
the ileum also provides some protection from ascending
infection. Urine drains continuously from the ileal pouch.
Continent
Continent urinary diversion involves creation of a mechanism that allows the client to control the passage of urine,
either by intermittent catheterization of the internal reservoir (e.g., Kock pouch) or by creating a neobladder or
internal pouch.
The Kock (pronounced “coke”) pouch, or continent
ileal bladder conduit, also uses a portion of the ileum to
form a reservoir for urine (Figure 47.14 ■). In this procedure, nipple valves are formed by doubling the tissue
backward into the reservoir where the pouch connects to
the skin and the ureters connect to the pouch. These valves
close as the pouch fills with urine, preventing leakage and
reflux of urine back toward the kidneys. The client empties
the pouch by inserting a clean catheter approximately every
2 to 3 hours at first and increases to every 5 to 6 hours as the
pouch expands. Between catheterizations, a small dressing
is worn to protect the stoma and clothing.
A continent diversion with a neobladder involves replacing a diseased or damaged bladder with a piece of ileum and
colon that is located in the same location as the bladder that
was removed. A pouch or new bladder is created. The ureters are sutured to one end of the new pouch or bladder and
this new bladder is then sutured to the functional urethra to
facilitate client voiding control (Figure 47.15 ■). The client
will need to relearn how to void. Voiding occurs when the
urethral sphincter muscle relaxes and abdominal straining
occurs to put pressure on the pouch.
When caring for clients with a urinary diversion, the
nurse must accurately assess I&O; note any changes in
urine color, odor, or clarity (mucous shreds are commonly
seen in the urine of clients with an ileal diversion); and
frequently assess the condition of the stoma and surrounding skin. Clients who must wear a urine collection
appliance are at risk for impaired skin integrity because
of irritation by urine. Well-fitting appliances are vital. The
nurse should consult with the wound ostomy continence
nurse (WOCN) to identify strategies for management of
stoma and peristomal problems when selecting the most
appropriate appliance for the client’s needs. The steps
of changing a urostomy appliance are similar to those
described in the procedure for changing a bowel diversion appliance (see Chapter 48
). However, there are
some differences, including the following: Incontinent
urinary diversions drain continually. As a result, some
type of wicking material (e.g., rolled dry gauze pad or
tampon) can be placed over the stoma to absorb the urine
and keep the skin dry throughout the measurement and
change of the ostomy appliance. Immediately following
surgery, ureteral stents may be present and protruding
from the stoma. These remain in place for 10 to 14 days
postop and are removed by either the surgeon or the
WOCN, depending on institutional protocol. Ureteral
Kidney
Stoma
Ureters
Kock
pouch
New bladder
joined to urethra
Urethra
carrying urine from new
bladder down the penis
Figure 47.14 ■ The Kock pouch—a continent urinary diversion.
M47_BERM9793_11_GE_C47.indd 1264
Figure 47.15 ■ A neobladder.
27/01/2021 18:08
Chapter 47
stents are used to maintain the patency of ureters at the
anastomotic sites.
Clients with urinary diversions may experience body
image and sexuality problems and may require assistance
in coping with these changes and managing the stoma.
Most clients are able to resume their normal activities and
lifestyle.
Evaluating
Using the overall goals and desired outcomes identified in
the planning stage, the nurse collects data to evaluate the
effectiveness of nursing activities. If the desired outcomes
are not achieved, explore the reasons before modifying
the care plan. For example, if the outcome “Remains dry
between voidings and at night” is not met, examples of
questions that need to be considered include:
•
•
•
What is the client’s perception of the problem?
Does the client understand and comply with the healthcare instructions provided?
Is access to toilet facilities a problem?
•
•
•
•
•
•
•
•
•
●
Urinary Elimination
1265
Can the client manipulate clothing for toileting? Can
adjustments be made to allow easier disrobing?
Are scheduled toileting times appropriate?
Is there adequate transition lighting for night-time
toileting?
Are mobility aids such as a walker, elevated toilet seat,
or grab bar needed? If currently used, are they appropriate or adequate?
Is the client performing PFM exercises appropriately
as scheduled?
Is the client’s fluid intake adequate? Does the timing
of fluid intake need to be adjusted (e.g., restricted after
dinner)?
Is the client restricting caffeine, citrus juice, carbonated
beverages, and artificial sweetener intake?
Is the client taking a diuretic? If so, when is the medication taken? Do the times need to be adjusted (e.g.,
taking second dose no later than 4 p.m.)?
Should continence aids such as a condom catheter or
absorbent pads be used?
NURSING CARE PLAN Urinary Elimination
ASSESSMENT DATA
NURSING DIAGNOSIS
DESIRED OUTCOMES*
NURSING ASSESSMENT
Mr. John Baker, 68 years old, was admitted to the hospital
with urinary retention, hematuria, and fever. The admitting
nurse gathers the following information when taking a nursing history. Mr. Baker states he has noticed urinary frequency
during the day for the past 2 weeks, and that he doesn’t feel
he has emptied his bladder after urinating. He also has to
get up two or three times during the night to urinate. During
the past few days, he has had difficulty starting urination and
dribbles afterward. He verbalizes the embarrassment his
urinary problems cause in his interactions with others. Mr.
Baker is concerned about the cause of this urinary problem.
He is diagnosed with benign prostatic hyperplasia (BPH) and
referred to a urologist who suggests a transurethral resection
of the prostate (TURP). He is placed on antibiotic therapy.
Altered urinary elimination (urinary
retention) related to bladder neck
obstruction by enlarged prostate
gland (as evidenced by dysuria,
frequency, nocturia, dribbling, hesitancy, and bladder distention)
Urinary Continence [0502] sometimes demonstrated as evidenced
by:
• Able to start and stop stream
• Empties bladder completely
Knowledge: Treatment Regimen
[1813] as evidenced by substantial
knowledge of:
• Self-care responsibilities for
ongoing treatment
• Self-monitoring techniques
Physical Examination
Diagnostic Data
Height: 185.4 cm (6′2″)
Weight: 85.7 kg (189 lb)
Temperature: 38.1°C (100.6°F)
Pulse: 88 beats/min
Respirations: 20/min
Blood pressure: 146/86 mmHg
Bladder scan for urinary
retention indicated 400 mL
urine. Straight catheterization
performed.
CBC normal; urinalysis:
amber,
clear, pH 6.5, specific
gravity
1.025, negative for
glucose,
protein, ketone, RBCs,
and
bacteria; IVP: evidence of
enlarged prostate gland
NURSING INTERVENTIONS*/SELECTED ACTIVITIES
RATIONALE
URINARY INCONTINENCE CARE [0610]
Monitor urinary elimination, including consistency, odor, volume, and color.
These parameters help determine adequacy of urinary tract function.
Help the client select appropriate incontinence garment or
pad for short-term management while more definitive treatment is designed.
M47_BERM9793_11_GE_C47.indd 1265
Appropriate undergarments can help diminish the embarrassing aspects
of urinary incontinence.
27/01/2021 18:08
1266
Unit 10
●
Promoting Physiologic Health
NURSING CARE PLAN Urinary Elimination—continued
URINARY INCONTINENCE CARE [0610]
Instruct Mr. Baker to limit fluids for 2 to 3 hours before
bedtime.
Decreased fluid intake several hours before bedtime will decrease the incidence of urinary retention and overflow incontinence, and promote rest.
Instruct him to drink a minimum of 1500 mL (six 8-ounce
glasses) of fluids per day.
Increased fluids during the day will increase urinary output and discourage
bacterial growth.
Limit ingestion of bladder irritants (e.g., colas, coffee, tea,
alcohol, and chocolate).
Alcohol, coffee, and tea have a natural diuretic effect and are bladder
irritants.
URINARY RETENTION CARE [0620]
Instruct Mr. Baker or a family member to record urinary
output.
Serves as an indicator of urinary tract and renal function and of fluid
balance.
Monitor degree of bladder distention by palpation and percussion or bladder scanner.
An enlarged prostate compresses the urethra so that urine is retained.
Checking for bladder distention provides information about bladder emptying and potential residual urine.
Implement intermittent catheterization, as appropriate.
Helps maintain tonicity of the bladder muscle by preventing overdistention
and providing for complete emptying.
Provide enough time for bladder emptying (10 minutes).
In addition to the effect of an enlarged prostate on the bladder, stress or
anxiety can inhibit relaxation of the urinary sphincter. Sufficient time should
be allowed for micturition.
Instruct the client in ways to avoid constipation or stool
impaction.
Impacted stool may place pressure on the bladder outlet, causing urinary
retention.
TEACHING: DISEASE PROCESS [5602]
Appraise Mr. Baker’s current level of knowledge about
benign prostatic hyperplasia.
Assessing the client’s knowledge will provide a foundation for building a
teaching plan based on his present understanding of his condition.
Explain the pathophysiology of the disease and how it
relates to urinary anatomy and function.
In this case, urinary retention and overflow incontinence are caused by
obstruction of the bladder neck by an enlarged prostate gland.
Describe the rationale behind management, therapy, and
treatment recommendations.
Adequate information about treatment options is important to diminish
anxiety, promote compliance, and enhance decision-making.
Instruct Mr. Baker on which signs and symptoms to report to
the healthcare provider (e.g., burning on urination, hematuria, oliguria).
In the individual with prostatic hyperplasia, urinary retention and an overdistended bladder reduce blood flow to the bladder wall, making it more
susceptible to infection from bacterial growth. Monitoring for these manifestations of UTI is essential to prevent urosepsis.
EVALUATION
Outcomes partially met. Following straight catheterization, Mr. Baker reported continued difficulty initiating a urinary stream but experienced
less dribbling and nocturia. He and his wife selected an undergarment that was acceptable to Mr. Baker and he reports that he feels more
confident. Intermittent catheterization not indicated. Intake is approximately 200 mL in excess of output. He is able to discuss the correlation between his enlarged prostate and urinary difficulties. A transurethral resection of the prostate is scheduled in 2 weeks.
*The NOC # for desired outcomes and the NIC # for nursing interventions are listed in brackets following the appropriate outcome or intervention. Outcomes, interventions, and activities selected are only a sample of those suggested by NOC and NIC and should be further individualized for each client.
APPLYING CRITICAL THINKING
1. Considering Mr. Baker’s history and assessment data, what other physical conditions could explain his symptoms?
2. The primary care provider has recommended surgery. What assumptions will the nurse need to validate in helping prepare Mr. and Mrs.
Baker for this surgery?
3. It does not appear that other alternatives have been considered. Why might this be so?
4. Incontinence can lead to client decisions to limit social interactions. What would be an appropriate response if Mr. Baker states that he
will just stay home until he has his surgery?
Answers to Applying Critical Thinking questions are available on the faculty resources site. Please consult with your instructor.
M47_BERM9793_11_GE_C47.indd 1266
27/01/2021 18:08
Chapter 47
●
Urinary Elimination
1267
CONCEPT MAP
Urinary Elimination
JB
outcome
outcome
Outcomes met:
hours
output
report to the
short-term
M47_BERM9793_11_GE_C47.indd 1267
27/01/2021 18:08
1268
Unit 10
●
Promoting Physiologic Health
Chapter 47 Review
CHAPTER HIGHLIGHTS
• Urinary elimination depends on normal functioning of the upper uri-
•
•
•
•
•
•
•
•
nary tract’s kidneys and ureters and the lower urinary tract’s urinary
bladder, urethra, and pelvic floor.
Urine is formed in the nephron, the functional unit of the kidney,
through a process of filtration, reabsorption, and secretion.
The normal process of urination is stimulated when sufficient urine
collects in the bladder to stimulate stretch receptors. Impulses from
stretch receptors are transmitted to the spinal cord and the brain,
causing relaxation of the internal sphincter (unconscious control)
and, if appropriate, relaxation of the external sphincter (conscious
control).
In the adult, urination generally occurs after 250 to 450 mL of urine
has collected in the bladder.
Many factors influence an individual’s urinary elimination, including
growth and development, psychosocial factors, fluid intake, medications, muscle tone, various diseases and conditions, and surgical
and diagnostic procedures.
Alterations in urine production and elimination include polyuria,
oliguria, anuria, frequency, nocturia, urgency, dysuria, enuresis,
incontinence, and retention. Each may have various influencing
and associated factors that need to be identified.
Millions of Americans, mostly women, suffer from urinary incontinence (UI). UI can have a significant impact on the client’s quality of
life, creating physical problems, such as skin breakdown, and also
psychosocial problems, such as social isolation and withdrawal,
less positive relationships with others, poorer perceived health,
negative effect on sexual function and intimacy, depression, and a
barrier to physical and everyday activities.
The five main types of UI are stress, urge, mixed, overflow, and
transient and functional incontinence.
Nurses, as part of their clinical practice, should assess all clients
for UI. Assessment of a client’s urinary function includes (a) a nursing history that identifies voiding patterns, recent changes, past
and current problems with urination, and factors influencing the
•
•
•
•
•
•
•
•
•
•
•
elimination pattern; (b) a physical assessment of the genitourinary
system; (c) inspection of the urine for amount, color, clarity, and
odor; and, if indicated, (d) testing of urine for specific gravity, pH,
and the presence of glucose, ketone bodies, protein, and occult
blood.
Examples of nursing diagnoses that may apply to clients with urinary
elimination problems can include altered urinary elimination (specify
specific problem, e.g., urinary retention), urinary incontinence (specify
type) and related diagnoses such as potential for infection.
Goals for the client with problems with urinary elimination include
maintaining or restoring normal voiding patterns and preventing
associated risks such as skin breakdown.
In planning for home care, the nurse considers the client’s needs
for teaching and assistance in the home.
Interventions include assisting the client to maintain adequate fluid
intake and normal voiding patterns, and assisting with toileting.
The most common cause of UTI is bacteria. Women in particular
are prone to UTIs because of their short urethras.
Urinary catheterization may be needed for clients with urinary retention but is only performed when all other measures to facilitate voiding fail. Sterile technique is essential to prevent urinary infections.
It is well documented that the risk to the client of developing a
CAUTI correlates to the length of time the catheter is kept in place.
Care of clients with indwelling catheters is directed toward assessing the necessity for the catheter, preventing infection of the urinary
tract, and encouraging urinary flow through the drainage system.
Clients with urinary retention may be taught to perform clean intermittent catheterization to enhance their independence, reduce the
risk of infection, and eliminate incontinence.
Bladder or catheter irrigations may be used to apply medication to
bladder walls or maintain catheter patency.
A urinary diversion is the surgical rerouting of urine from the kidneys
to a site other than the bladder. There are two categories of diversions: incontinent and continent.
TEST YOUR KNOWLEDGE
1. A client is diagnosed with an elevated aldosterone level. Which
aspect of urinary elimination will this finding affect?
1. Increased urine output
2. Urinary incontinence
3. Decreased urine output
4. Urinary retention
2. A client needs a test to determine the amount of residual urine.
Which of the following would the nurse use this assessment for?
Select all that apply.
1. To evaluate glomerular filtration rate
2. To determine the extent of renal failure
3. To determine the amount of retained urine after voiding
4. To determine the need for medications
5. To evaluate fluid volume status
M47_BERM9793_11_GE_C47.indd 1268
3. A nurse is applying an external urinary device to a client. Before
attaching the device to the drainage bag, what should the
nurse do?
1. Wash her hands.
2. Document the client’s tolerance of the procedure.
3. Instruct the client about the drainage system.
4. Ensure that the condom is not twisted.
4. The catheter slips into the vagina during a straight catheterization of a female client. The nurse does which action?
1. Leaves the catheter in place and gets a new sterile catheter.
2. Leaves the catheter in place and asks another nurse to
attempt the procedure.
3. Removes the catheter and redirects it to the urinary meatus.
4. Removes the catheter, wipes it with a sterile gauze, and redirects it to the urinary meatus.
27/01/2021 18:08
Chapter 47
5. You have explained to the client the reason for and steps
involved for insertion of an indwelling urinary catheter. List the
following actions in the correct sequence:
1. Apply sterile gloves
2. Attach prefilled syringe
3. Secure IUC appropriately to prevent urethural irritation
4. Perform pericare
5. Insert catheter to appropriate length and check urine flow
6. Lubricate catheter
7. Inflate balloon
8. Perform hand hygiene
9. Clean urinary meatus with antiseptic solution
10. Open catheter kit
1. 8, 10, 4, 1, 2, 6, 9, 5, 7, 3
2. 2, 4, 8, 10, 1, 6, 2, 9, 5, 7, 3
3. 4, 8, 1, 10, 6, 2, 9, 5, 7, 3
4. 10, 4, 8, 1, 7, 2, 6, 9, 5, 3
6. During shift report, the nurse learns that an older female client is
unable to maintain continence after she senses the urge to void
and becomes incontinent on the way to the bathroom. Which
specific type of urinary incontinence is the most appropriate for
the nursing diagnosis?
1. Stress
2. Reflex
3. Functional
4. Urge
7. A female client has a urinary tract infection (UTI). Which teaching
points by the nurse would be helpful to the client? Select all that
apply.
1. Limit fluids to avoid the burning sensation on urination.
2. Review symptoms of UTI with the client.
3. Wipe the perineal area from back to front.
4. Wear cotton underclothes.
5. Take baths rather than showers.
●
Urinary Elimination
1269
8. The nurse will need to assess the client’s performance of clean
intermittent catheterization (CIC) for a client with which urinary
diversion?
1. Ileal conduit
2. Kock pouch
3. Neobladder
4. Vesicostomy
9. Which focus is the nurse most likely to teach for a client with a
flaccid bladder?
1. Habit training: Attempt voiding at specific time periods.
2. Bladder retraining: Delay voiding according to a preschedule
timetable.
3. Credé’s maneuver: Apply gentle manual pressure to the
lower abdomen.
4. Kegel exercises: Contract the pelvic floor muscles.
10. Which of the following behaviors indicates that the client on a
bladder retraining program has met the expected outcomes?
Select all that apply.
1. Voids each time there is an urge.
2. Practices slow, deep breathing until the urge decreases.
3. Uses adult diapers, for “just in case.”
4. Drinks citrus juices and carbonated beverages.
5. Performs pelvic floor muscle exercises.
See Answers to Test Your Knowledge in Appendix A.
READINGS AND REFERENCES
Suggested Readings
References
Beauchemin, L., Newman, D. K., LeDanseur, M., Jackson, A.,
& Ritmiller, M. (2018). Best practices for clean intermittent
catheterization. Nursing, 48(9), 49–54. doi:10.1097/01.
NURSE.0000544216.23783.bc
CIC is not taught in many undergraduate nursing programs. This article provides a synopsis of best practices
for CIC.
Francis, K. (2018). Damage control: Differentiating
incontinence-associated dermatitis from pressure injury. Nursing, 48(6), 18–25. doi:10.1097/01.
NURSE.0000532739.93967.20
The author discusses how to differentiate, classify, and
document incontinence-associated dermatitis and pressure injuries with an emphasis on assessing clients with
dark skin.
American Nurses Association. (n.d.). Streamlined evidencebased RN tool: Catheter associated urinary tract infection
(CAUTI) prevention. Retrieved from https://www.nursingworld.org/~4aede8/globalassets/practiceandpolicy/
innovation--evidence/clinical-practice-material/cauti-prevention-tool/anacautipreventiontool-final-19dec2014.pdf
Ball, J., Bindler, R., Cowen, K., & Shaw, M. (2017). Principles
of pediatric nursing (7th ed.). Hoboken, NJ: Pearson.
Beauchemin, L., Newman, D. K., LeDanseur, M., Jackson, A.,
& Ritmiller, M. (2018). Best practices for clean intermittent
catheterization. Nursing, 48(9), 49–54. doi:10.1097/01.
NURSE.0000544216.23783.bc
Butcher, H. K., Bulechek, G. M., Dochterman, J. M., &
Wagner, C. M. (Eds.). (2018). Nursing interventions
classification (NIC) (7th ed.). St. Louis, MO: Elsevier.
Centers for Disease Control and Prevention. (2017). Guidelines
for prevention of catheter-associated urinary tract infections (2009). Retrieved from https://www.cdc.gov/hicpac/
pdf/CAUTI/CAUTIguideline2009final.pdf
Centers for Disease Control and Prevention. (2019). Urinary
tract infection (catheter-associated urinary tract infection (CAUTI) and non-catheter-associated urinary tract
infection (UTI) and other urinary system infection (USI)
events. Retrieved from https://www.cdc.gov/nhsn/
pdfs/pscmanual/7psccauticurrent.pdf
Hoke, N., & Bradway, C. (2016). A clinical nurse
specialist-directed initiative to reduce postoperative
urinary retention in spinal surgery patients. American
Journal of Nursing, 116(8), 47–52. doi:10.1097/01.
NAJ.0000490176.22393.69
Related Research
Ferguson, A. (2018). Implementing a CAUTI prevention
program in an acute care hospital setting. Urologic
Nursing, 38(6), 273–302.
doi:10.7257/1053-816X.2018.38.6.273
Rhone, C., Breiter, Y., Benson, L., Petri, H., Thompson, P., &
Murphy, C. (2017). The impact of two-person indwelling
urinary catheter insertion in the emergency department
using technical and socioadaptive interventions. Journal of
Clinical Outcomes Management, 24(10), 451–456.
Schlittenhardt, M., Smith, S. C., & Ward-Smith, P.
(2016). Tele-continence care: A novel approach
for providers. Urologic Nursing, 36(5), 217–223.
doi:10.7257/1053-816X.2016.36.5.217
M47_BERM9793_11_GE_C47.indd 1269
Institute for Healthcare Improvement. (n.d.). Catheter-associated
urinary tract infection. Retrieved from http://www.ihi.org/
Topics/CAUTI/Pages/default.aspx
The Joint Commission. (2019). National Patient Safety
Goals effective January 2019—hospital accreditation
program. Retrieved from https://www.jointcommission.
org/assets/1/6/NPSG_Chapter_HAP_Jan2019.pdf
Kehinde, O. (2016). Common incontinence problems seen by
community nurses. Journal of Community Nursing, 30(4),
46–55.
Leaver, R. (2017). Assessing patients with urinary incontinence: The basics. Journal of Community Nursing, 31(1),
40–46.
McNeill, L. (2017). Back to basics: How evidence-based
nursing practice can prevent catheter-associated urinary tract infections. Urologic Nursing, 37(4), 204–206.
doi:10.7257/1053-816X.2017.37.4.204
Mendes, A., Rodolpho, J. R. C., & Hoga, L. A. (2016). Nonpharmacological and non-surgical treatments for female
urinary incontinence: An integrative review. Applied Nursing
Research, 31, 146–153. doi:10.1016/j.apnr.2016.02.005
Moorhead, S., Swanson, E., Johnson, M., & Maas, M. L.
(Eds.). (2018). Nursing outcomes classification (NOC)
(6th ed.). St. Louis, MO: Elsevier.
Nazarko, L. (2017). Beyond the bladder: Holistic care
when urinary incontinence develops. British Journal of
Community Nursing, 22(1), 662–666. doi:10.12968/b
jcn.2017.22.1.662
Nazarko, L. (2018). Male urinary incontinence management:
Penile sheaths. British Journal of Community Nursing,
23(3), 110–116. doi:10.12968/bjcn.2018.23.3.110
27/01/2021 18:08
1270
Unit 10
●
Promoting Physiologic Health
Ostle, Z. (2016). Assessment, diagnosis and treatment of
urinary incontinence in women. British Journal of Nursing,
25(2), 84–91. doi:10.12968/bjon.2016.25.2.84
Palmer, M. H., & Willis-Gray, M. (2017). Overactive bladder
in women. American Journal of Nursing, 117(4), 34–41.
doi:10.1097/01.NAJ.0000515207.69721.94
Panchisin, T. L. (2016). Improving outcomes with the
ANA CAUTI prevention tool. Nursing, 46(3), 55–59.
doi:10.1097/01.NURSE.0000480603.14769.d6
Schaeffer, A. J. (2017). Placement and management of urinary
bladder catheters in adults. Retrieved from https://www
.uptodate.com/contents/placement-and-management-ofurinary-bladder-catheters-in-adults
Searcy, J. A. R. (2017). Geriatric urinary incontinence. Nursing
Clinics of North America, 52(3), 447–455. doi:10.1016/j.
cnur.2017.04.002
M47_BERM9793_11_GE_C47.indd 1270
Stewart, E. (2018). Assessment and management of urinary
incontinence in women. Nursing Standard, 33(2), 75–81.
doi:10.7748/ns.2018.e11148
Tso, C., & Lee, W. (2018). Postmenopausal women and urinary
incontinence. American Nurse Today, 13(1), 18–21.
Selected Bibliography
Ballard, J. P., Parsons, S., Rodgers, J., Mosack, V., &
Starks, B. (2018). HOUDINI impacts on utilization
and infection rates—A retrospective quality improvement initiative. Urologic Nursing, 38(4), 184–191.
doi:10.7257/1053-816X.2018.38.4.184
Cadet, M. J. (2018). Diagnosis, treatment, and prevention of
cystitis. American Nurse Today, 13(7), 24–27.
Collins, L. (2019). Diagnosis and management of a urinary
tract infection. British Journal of Nursing, 28(2), 84–88.
doi:10.12968/bjon.2019.28.2.84
Culbertson, S., & Davis, A. M. (2017). Nonsurgical management of urinary incontinence in women. JAMA, 317(1),
79–80. doi:10.1001/jama.2016.18433
Davis, C. (2019). Catheter-associated urinary tract infection:
Signs, diagnosis, prevention. British Journal of Nursing,
28(2), 96–100. doi:10.12968/bjon.2019.28.2.96
Hill, B., & Mitchell, M. (2018). Urinary catheters PART 1. British Journal of Nursing, 27(21), 1234–1236. doi:10.12968/
bjon.2018.27.21.1234
Knill, L., Maduro, R., & Payne, J. E. (2018). Targeting zero
CAUTIs. American Nurse Today, 13(11), 54–57.
Schreiber, M. L. (2016). Ostomies: Nursing care and management. MEDSURG Nursing, 25(2), 127–130.
Yates, A. (2016). The risks and benefits of suprapubic catheters. Nursing Times 11(6/7), 19–22.
27/01/2021 18:08
Fecal Elimination
48
LEA R N IN G OU TC OME S
After completing this chapter, you will be able to:
1. Describe the physiology of defecation.
2. Distinguish normal from abnormal characteristics and constituents of feces.
3. Identify factors that influence fecal elimination and patterns of
defecation.
4. Identify common causes and effects of selected fecal elimination problems.
5. Describe methods used to assess fecal elimination.
6. Identify examples of nursing diagnoses, outcomes, and interventions for clients with elimination problems.
7. Identify measures that maintain normal fecal elimination patterns.
8. Describe the purpose and action of commonly used enema
solutions.
9. Describe essentials of fecal stoma care for clients with an
ostomy.
10. Recognize when it is appropriate to assign assistance with
fecal elimination to assistive personnel.
11. Verbalize the steps used in:
a. Administering an enema
b. Changing a bowel diversion ostomy appliance.
12. Demonstrate appropriate documentation and reporting related
to fecal elimination.
K EY T E RMS
bedpan, 1282
bowel incontinence, 1277
carminatives, 1283
cathartics, 1283
chyme, 1271
colostomy, 1290
commode, 1282
constipation, 1275
defecation, 1272
diarrhea, 1277
enema, 1284
fecal impaction, 1276
fecal incontinence, 1277
feces, 1271
Introduction
Nurses frequently are consulted or involved in assisting
clients with elimination problems. These problems can
be embarrassing to clients and can cause considerable
discomfort. The elimination of feces is a recognizable public topic in North America. For example, laxative advertisements, describing such feelings as tiredness due to
irregularity, keep the subject in the public consciousness.
Some older adults are preoccupied with their bowels. Individuals who have had a bowel movement once a day for
many years can view missing one day as a serious problem.
Physiology of Defecation
Elimination of the waste products of digestion from the
body is essential to health. The excreted waste products
are referred to as feces or stool.
Large Intestine
The large intestine extends from the ileocecal (ileocolic)
valve, which lies between the small and large intestines, to
the anus. The colon (large intestine) in the adult is generally
flatulence, 1278
flatus, 1272
gastrocolic reflex, 1274
gastrostomy, 1290
hemorrhoids, 1272
ileostomy, 1290
jejunostomy, 1290
laxatives, 1275
meconium, 1274
ostomy, 1290
peristalsis, 1272
stoma, 1290
stool, 1271
suppositories, 1283
about 125 to 150 cm (50 to 60 in.) long. It has seven parts:
the cecum; ascending, transverse, and descending colons;
sigmoid colon; rectum; and anus (Figure 48.1 ■).
The large intestine is a muscular tube lined with
mucous membrane. The muscle fibers are both circular
and longitudinal, permitting the intestine to enlarge and
contract in both width and length.
The colon’s main functions are the absorption of water
and nutrients, the mucoid protection of the intestinal wall,
and fecal elimination. The waste products leaving the stomach through the small intestine and then passing through
the ileocecal valve are called chyme. The ileocecal valve
regulates the flow of chyme into the large intestine and
prevents backflow into the ileum. As much as 1500 mL of
chyme passes into the large intestine daily, and all but about
100 mL is reabsorbed in the proximal half of the colon. The
100 mL of fluid is excreted in the feces.
The colon also serves a protective function in that it
secretes mucus. This mucus contains large amounts of
bicarbonate ions. The mucous secretion is stimulated by
excitation of parasympathetic nerves. During extreme
stimulation—for example, as a result of emotions—large
amounts of mucus are secreted, resulting in the passage
of stringy mucus with little or no feces. Mucus serves to
1271
M48_BERM9793_11_GE_C48.indd 1271
27/01/2021 18:03
1272
Unit 10
●
Promoting Physiologic Health
Rectum
Transverse
colon
Descending
colon
Ascending colon
Cecum
Appendix
Rectum
Sigmoid
colon
Anus
Anal-rectal ridge
Internal
anal sphincter
External
anal sphincter
Anal columns
Anal valve
Anal canal
Figure 48.1 ■ The large intestine.
B. F. FREMGEN, and S. S. FRUCHT, MEDICAL TERMINOLOGY: A LIVING LANGUAGE,
6th Ed.,© 2016. Reprinted and Electronically reproduced by permission of Pearson Education,
Inc., New York, NY.
protect the wall of the large intestine from trauma by the
acids formed in the feces, and it serves as an adherent for
holding the fecal material together. Mucus also protects
the intestinal wall from bacterial activity.
The colon acts to transport along its lumen the products of digestion, which are eventually eliminated through
the anal canal. These products are flatus and feces. Flatus
is largely air and the by-products of the digestion of carbohydrates. Peristalsis is wavelike movement produced by
the circular and longitudinal muscle fibers of the intestinal
walls; it propels the intestinal contents forward.
Rectum and Anal Canal
The rectum in the adult is usually 10 to 15 cm (4 to 6 in.)
long; the most distal portion, 2.5 to 5 cm (1 to 2 in.) long, is
the anal canal. The rectum has folds that extend vertically.
Each of the vertical folds contains a vein and an artery. It
is believed that these folds help retain feces within the
rectum. When the veins become distended, as can occur
with repeated pressure, a condition known as hemorrhoids
occurs (Figure 48.2 ■).
The anal canal is bounded by an internal and an external
sphincter muscle (Figure 48.3 ■). The internal sphincter is
A
Rectum
External
anal sphincter
Anal canal
B
Figure 48.3 ■ The rectum, anal canal, and anal
sphincters: A, open; B, closed.
under involuntary control, and the external sphincter normally is voluntarily controlled. The internal sphincter muscle
is innervated by the autonomic nervous system; the external
sphincter is innervated by the somatic nervous system.
Defecation
Defecation is the expulsion of feces from the anus and
rectum. It is also called a bowel movement. The frequency
of defecation is highly individual, varying from several
times per day to two or three times per week. The amount
defecated also varies among individuals. When peristaltic waves move the feces into the sigmoid colon and the
rectum, the sensory nerves in the rectum are stimulated
and the individual becomes aware of the need to defecate.
Clinical Alert!
Individuals (especially children) may use very different terms for a
bowel movement. The nurse may need to try several different common words before finding one the client understands.
External
hemorrhoid
Internal
hemorrhoid
Figure 48.2 ■ Internal and external hemorrhoids.
M48_BERM9793_11_GE_C48.indd 1272
When the internal anal sphincter relaxes, feces move
into the anal canal. After the individual is seated on a
toilet or bedpan, the external anal sphincter is relaxed
voluntarily. Expulsion of the feces is assisted by contraction of the abdominal muscles and the diaphragm, which
increases abdominal pressure, and by contraction of the
muscles of the pelvic floor, which moves the feces through
27/01/2021 18:03
Chapter 48
TABLE 48.1
●
Fecal Elimination
1273
Characteristics of Normal and Abnormal Feces
Characteristic Normal
Abnormal
Possible Cause
Color
Adult: brown
Clay or white
Absence of bile pigment (bile obstruction);
diagnostic study using barium
Infant: yellow
Black or tarry
Drug (e.g., iron); bleeding from upper gastrointestinal tract (e.g., stomach, small intestine); diet high in
red meat and dark green vegetables (e.g., spinach)
Red
Bleeding from lower gastrointestinal tract
(e.g., rectum); some foods (e.g., beets)
Pale
Malabsorption of fats; diet high in milk and milk
products and low in meat
Consistency
Formed, soft, semisolid, moist
Orange or green
Intestinal infection
Hard, dry
Dehydration; decreased intestinal motility resulting
from lack of fiber in diet, lack of exercise, emotional
upset, laxative abuse
Diarrhea
Increased intestinal motility (e.g., due to irritation of
the colon by bacteria)
Narrow, pencil-shaped,
or stringlike stool
Obstructive condition of the rectum
Shape
Cylindrical (contour of rectum) about
2.5 cm (1 in.) in diameter in adults
Amount
Varies with diet (about 100–400 g/day)
Odor
Aromatic: affected by ingested food
and individual’s own bacterial flora
Pungent
Infection, blood
Constituents
Small amounts of undigested
roughage, sloughed dead bacteria
and epithelial cells, fat, protein, dried
constituents of digestive juices (e.g.,
bile pigments, inorganic matter)
Pus
Parasites
Blood
Large quantities of fat
Foreign objects
Mucus
Bacterial infection
Inflammatory condition
Gastrointestinal bleeding
Malabsorption
Accidental ingestion
the anal canal. Normal defecation is facilitated by (a) thigh
flexion, which increases the pressure within the abdomen,
and (b) a sitting position, which increases the downward
pressure on the rectum.
If the defecation reflex is ignored, or if defecation is
consciously inhibited by contracting the external sphincter
muscle, the urge to defecate normally disappears for a few
hours before occurring again. Repeated inhibition of the urge
to defecate can result in expansion of the rectum to accommodate accumulated feces and eventual loss of sensitivity to
the need to defecate. Constipation can be the ultimate result.
Feces
Normal feces are made of about 75% water and 25%
solid materials. They are soft but formed. If the feces are
propelled very quickly along the large intestine, there
is not time for most of the water in the chyme to be
reabsorbed and the feces will be more fluid, containing
perhaps 95% water. Normal feces require a normal fluid
intake; feces that contain less water may be hard and
difficult to expel.
Feces are normally brown, chiefly due to the presence
of stercobilin and urobilin, which are derived from bilirubin (a red pigment in bile). Another factor that affects
fecal color is the action of bacteria such as Escherichia coli
or staphylococci, which are normally present in the large
intestine. The action of microorganisms on the chyme is
M48_BERM9793_11_GE_C48.indd 1273
also responsible for the odor of feces. Table 48.1 lists the
characteristics of normal and abnormal feces.
Factors That Affect Defecation
Defecation patterns vary at different stages of life. Circumstances of diet, fluid intake and output, activity, psychologic factors, defecation habits, medications, diagnostic
and medical procedures, pathologic conditions, and pain
also affect defecation.
Development
See Table 48.2 for a summary of the developmental
changes affecting defecation.
Diet
Sufficient bulk (cellulose, fiber) in the diet is necessary to
provide fecal volume. Inadequate intake of dietary fiber
contributes to the risk of developing obesity, type 2 diabetes, coronary artery disease, and colon cancer. Fiber is classified into two categories: insoluble fiber and soluble fiber.
Insoluble fiber promotes the movement of material through
the digestive system and increases stool bulk. Sources of
insoluble fiber include whole-wheat flour, wheat bran, nuts,
and many vegetables. Soluble fiber dissolves in water to
form a gel-like material. It can help lower blood cholesterol
27/01/2021 18:03
1274
Unit 10
TABLE 48.2
Promoting Physiologic Health
●
Changes in Defecation Throughout the Lifespan
Stage
Variations
Newborns and
Infants
• Meconium is the first fecal material passed by the newborn, normally up to 24 hours after birth. It is dark green,
tarry, odorless, and sticky. Transitional stools, which follow for about a week, are generally greenish yellow; they
contain mucus and are loose.
• Infants pass stool frequently, often after each feeding. The intestine is immature, causing water to not be well
absorbed and frequent soft, liquid stools. Stool becomes less frequent and firmer after solid foods are started.
• Breastfed infants have light yellow to golden feces. Infants who take formula have dark yellow or tan, more formed stool.
Toddlers
• Some control of defecation starts at 11⁄2 to 2 years of age. Daytime control is typically achieved by
age 21⁄2, after toilet training.
School-Age Children
and Adolescents
• Bowel habits are similar to those of adults. Patterns of defecation vary in frequency, quantity, and consistency.
• Some school-age children may delay defecation because of an activity such as play.
Older Adults
• Many suffer from constipation because of reduced activity levels, inadequate fluid and fiber intake, and muscle
weakness.
• Many believe that “regularity” means a bowel movement every day and may use over-the-counter (OTC) medications to relieve what they consider constipation. May need to be advised that normal patterns of bowel elimination
vary considerably.
and glucose levels (Mayo Clinic, 2018). Sources of soluble
fiber include oats, peas, beans, apples, citrus fruits, carrots,
barley, and psyllium. The Mayo Clinic recommends the following daily amount of fiber:
•
•
•
•
Men ages 50 and younger: 38 grams
Men ages 51 and older: 30 grams
Women ages 50 and younger: 25 grams
Women ages 51 and older: 21 grams.
It is important to drink plenty of water because fiber
works best when it absorbs water.
Bland diets and low-fiber diets are lacking in bulk and
therefore create insufficient residue of waste products to
stimulate the reflex for defecation. Low-residue foods,
such as rice, eggs, and lean meats, move more slowly
through the intestinal tract. Increasing fluid intake with
such foods increases their rate of movement.
Certain foods are difficult or impossible for some individuals to digest. This inability results in digestive upsets
and, in some instances, the passage of watery stools. Irregular eating can also impair regular defecation. Individuals
who eat at the same times every day usually have a regularly timed, physiologic response to the food intake and a
regular pattern of peristaltic activity in the colon.
Spicy foods can produce diarrhea and flatus in some
individuals. Excessive sugar can also cause diarrhea.
Other foods that may influence bowel elimination include
the following:
•
•
•
Gas-producing foods, such as cabbage, onions, cauliflower, bananas, and apples
Laxative-producing foods, such as bran, prunes, figs,
chocolate, and alcohol
Constipation-producing foods, such as cheese, pasta,
eggs, and lean meat.
Fluid Intake and Output
Even when fluid intake is inadequate or output (e.g., urine
or vomitus) is excessive for some reason, the body continues
to reabsorb fluid from the chyme as it passes along the colon.
The chyme becomes drier than normal, resulting in hard
M48_BERM9793_11_GE_C48.indd 1274
feces. In addition, reduced fluid intake slows the chyme’s
passage along the intestines, further increasing the reabsorption of fluid from the chyme. Healthy fecal elimination usually requires a daily fluid intake of 2000 to 3000 mL. If chyme
moves abnormally quickly through the large intestine, however, there is less time for fluid to be absorbed into the blood;
as a result, the feces are soft or even watery.
Activity
Activity stimulates peristalsis, thus facilitating the movement of chyme along the colon. Weak abdominal and
pelvic muscles are often ineffective in increasing the intraabdominal pressure during defecation or in controlling
defecation. Weak muscles can result from lack of exercise,
immobility, or impaired neurologic functioning. Clients
confined to bed are often constipated.
Psychologic Factors
Some individuals who are anxious or angry experience
increased peristaltic activity and subsequent nausea or
diarrhea. In contrast, individuals who are depressed may
experience slowed intestinal motility, resulting in constipation. How someone responds to these emotional states is
the result of individual differences in the response of the
enteric nervous system to vagal stimulation from the brain.
Defecation Habits
Early bowel training may establish the habit of defecating
at a regular time. Many individuals defecate after breakfast
due to the gastrocolic reflex (increased peristalsis of the
colon after food has entered the stomach). If an individual
ignores this urge to defecate, water continues to be reabsorbed, making the feces hard and difficult to expel. When
the normal defecation reflexes are inhibited or ignored,
these conditioned reflexes tend to be progressively weakened. When habitually ignored, the urge to defecate is
ultimately lost. Adults may ignore these reflexes because
of the pressures of time or work. Hospitalized clients may
27/01/2021 18:03
Chapter 48
suppress the urge because of embarrassment about using
a bedpan, because of lack of privacy, or because defecation
is too uncomfortable.
Medications
Some drugs have side effects that can interfere with normal elimination. Some cause diarrhea; others, such as large
doses of certain tranquilizers and repeated administration
of opioids, cause constipation because they decrease gastrointestinal activity through their action on the central
nervous system. Iron supplements act more locally on the
bowel mucosa and can cause constipation or diarrhea.
Some medications directly affect elimination.
Laxatives are medications that stimulate bowel activity
and so assist fecal elimination. Other medications soften
stool, facilitating defecation. Certain medications suppress
peristaltic activity and may be used to treat diarrhea.
Medications can also affect the appearance of the feces.
Any drug that causes gastrointestinal bleeding (e.g., aspirin
products) can cause the stool to be red or black. Iron salts lead
to black stool because of the oxidation of the iron; antibiotics
may cause a gray-green discoloration; and antacids can cause
a whitish discoloration or white specks in the stool. PeptoBismol, a common OTC drug, causes stools to be black.
Diagnostic Procedures
Before certain diagnostic procedures, such as visualization
of the colon (colonoscopy or sigmoidoscopy), the client is
restricted from ingesting food or fluid. The client may also
be given a cleansing enema prior to the examination. In
these instances normal defecation usually will not occur
until eating resumes.
Pathologic Conditions
Spinal cord injuries and head injuries can decrease the
sensory stimulation for defecation. Impaired mobility may
limit the client’s ability to respond to the urge to defecate
and the client may experience constipation. Or, a client
may experience fecal incontinence because of poorly functioning anal sphincters.
Pain
Clients who experience discomfort when defecating (e.g.,
following hemorrhoid surgery) often suppress the urge to
M48_BERM9793_11_GE_C48.indd 1275
Fecal Elimination
1275
defecate to avoid the pain. Such clients can experience constipation as a result. Clients taking opioid analgesics for
pain may also experience constipation as a side effect of the
medication.
Fecal Elimination Problems
Four common problems are related to fecal elimination:
constipation, diarrhea, bowel incontinence, and flatulence.
Constipation
Constipation may be defined as fewer than three bowel
movements per week. This infers the passage of dry, hard
stool or the passage of no stool. It occurs when the movement of feces through the large intestine is slow, thus
allowing time for additional reabsorption of fluid from
the large intestine. Associated with constipation are difficult evacuation of stool and increased effort or straining
of the voluntary muscles of defecation. The individual
may also have a feeling of incomplete stool evacuation
after defecation. However, it is important to define constipation in relation to the individual’s regular elimination
pattern. Some individuals normally defecate only a few
times a week; others defecate more than once a day. Careful assessment of the client’s habits is necessary before a
diagnosis of constipation is made. Box 48.1 lists the common characteristics of constipation.
BOX 48.1
•
•
•
Anesthesia and Surgery
General anesthetics cause the normal colonic movements
to cease or slow by blocking parasympathetic stimulation
to the muscles of the colon. Clients who have regional or
spinal anesthesia are less likely to experience this problem.
Surgery that involves direct handling of the intestines
can cause temporary stoppage of intestinal movement.
This condition, called ileus, usually lasts 24 to 48 hours.
Listening for bowel sounds that reflect intestinal motility
is an important nursing assessment following surgery.
●
•
•
•
•
Common Characteristics of
Constipation
Decreased frequency of defecation
Hard, formed stools
Straining at stool; painful defecation
Reports of rectal fullness or pressure or incomplete bowel
evacuation
Abdominal pain, cramps, or distention
Anorexia, nausea
Headache
Many causes and factors contribute to constipation.
Among them are the following:
•
•
•
•
•
•
•
•
•
•
•
•
Insufficient fiber intake
Insufficient fluid intake
Insufficient activity or immobility
Irregular defecation habits
Change in daily routine
Lack of privacy
Chronic use of laxatives or enemas
Irritable bowel syndrome (IBS)
Pelvic floor dysfunction or muscle damage
Poor motility or slow transit
Neurologic conditions (e.g., Parkinson’s disease),
stroke, or paralysis
Emotional disturbances such as depression or mental
confusion
27/01/2021 18:03
1276
•
•
Unit 10
●
Promoting Physiologic Health
Medications such as opioids, iron supplements, antihistamines, antacids, and antidepressants
Habitual denial and ignoring the urge to defecate.
BOX 48.2
Colorectal Cancer
RISK FACTORS
Nonmodifiable
• Age (risk increases after age 50; leading cause of death in
women aged 75 and older)
• Race (incidence and mortality rates are highest in
non-Hispanic Black individuals)
• Personal or family history of colorectal polyps
• Personal history of inflammatory bowel disease
Constipation can cause health problems for some
clients. In children constipation is often associated with
changes in activity, diet, and toileting habits (Ball, Bindler,
Cowen, & Shaw, 2017). Straining associated with constipation is often accompanied by holding the breath. This
Valsalva maneuver can present serious problems to people
with heart disease, brain injuries, or respiratory disease.
Holding the breath while bearing down increases intrathoracic pressure and vagal tone, slowing the pulse rate.
The reasons for constipation can range from lifestyle
habits (e.g., lack of exercise) to serious malignant disorders
(e.g., colorectal cancer). The nurse should evaluate any
complaints of constipation carefully for each individual.
A change in bowel habits over several weeks with or without weight loss, pain, or fever should be referred to a primary care provider for a complete medical evaluation. See
Box 48.2 for risk factors and symptoms of colorectal cancer.
Modifiable
• Cigarette smoking
• Poor diet (e.g., low in fiber and high in fat; high amounts of
red or processed meats)
• Lack of physical activity
• Obesity
• Heavy consumption of alcohol
SYMPTOMS
Early colorectal cancer often has no symptoms. Screening is
important and includes using high-sensitivity fecal occult blood
testing, sigmoidoscopy, or colonoscopy beginning at age 45 and
continuing until age 75.
Inform clients to see their primary care provider if they have any
of the following:
• A change in bowel habits such as diarrhea, constipation, or
narrowing of the stool that lasts for more than a few days
• A feeling of needing to have a bowel movement that is not
relieved by doing so
• Rectal bleeding or blood in the stool (often, though, the stool
will look normal)
• Cramping or steady abdominal pain
• Weakness and fatigue
• Unexpected weight loss
Fecal Impaction
Fecal impaction is a mass or collection of hardened feces in
the folds of the rectum. Impaction results from prolonged
retention and accumulation of fecal material. In severe
impactions the feces accumulate and extend well up into
the sigmoid colon and beyond. A client who has a fecal
impaction will experience the passage of liquid fecal seepage (diarrhea) and no normal stool. The liquid portion of
the feces seeps out around the impacted mass. Impaction
can also be assessed by digital examination of the rectum,
during which the hardened mass can often be palpated.
Along with fecal seepage and constipation, symptoms
include frequent but nonproductive desire to defecate and
rectal pain. A generalized feeling of illness results; the client becomes anorexic, the abdomen becomes distended,
and nausea and vomiting may occur.
The causes of fecal impaction are usually poor defecation habits and constipation. Also, the administration of
medications such as anticholinergics and antihistamines will
From Colorectal Cancer Facts & Figures 2017–2019, by American Cancer Society,
2017. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancerfacts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-andfigures-2017-2019.pdf; Colorectal Cancer Risk Factors, by American Cancer Society, 2018.
Retrieved from https://www.cancer.org/cancer/colon-rectal-cancer/causes-risks-prevention/
risk-factors.html; and “The Big 3: An Updated Overview of Colorectal, Breast, and Prostate
Cancers,” by J. Gordon, E. Fischer-Cartlidge, and M. Barton-Burke, 2017, Nursing Clinics of
North America, 52, 27–52.
DRUG CAPSULE
Emollient or Surfactant: docusate calcium (Surfak), docusate sodium (Colace)
CLIENT WITH DRUGS FOR TREATING THE LOWER
GASTROINTESTINAL TRACT
Docusates lower the surface tension of fecal material, which allows
water and lipids to penetrate the stool, resulting in a softer fecal
mass. They do not stimulate peristalsis.
Docusates are commonly used for prevention of constipation and
to decrease the strain of defecation in individuals who should avoid
straining during bowel movements (e.g., cardiac disease [prevent
Valsalva maneuver], eye surgery, rectal surgery).
NURSING RESPONSIBILITIES
• Assess the client for abdominal distention, bowel sounds, and
usual bowel movement frequency.
• Evaluate the effectiveness of the medication.
M48_BERM9793_11_GE_C48.indd 1276
CLIENT AND FAMILY TEACHING
Advise the client to drink a glass of fluid (e.g., water, juice, milk)
with each dose.
• Explain that it may take 1 to 3 days to soften fecal material.
• Advise the client not to take docusate within 2 hours of other
laxatives, especially mineral oil, because it may cause increased
absorption of the mineral oil.
• Discuss other forms of bowel regulation (e.g., increasing fiber
intake, fluid intake, and activity).
•
Note: Prior to administering any medication, review all aspects with a current drug handbook or
other reliable source.
27/01/2021 18:03
Chapter 48
increase the client’s risk in the development of a fecal impaction. The barium used in radiologic examinations of the
upper and lower gastrointestinal tracts can also be a causative factor. Therefore, after these examinations, laxatives or
enemas are usually given to ensure removal of the barium.
Clinical Alert!
An older adult with a fecal impaction may show symptoms of delirium. Assess for fecal impaction if the client with constipation problems has a sudden change in mental status.
Digital examination of the impaction through the rectum should be done gently and carefully. Although digital
rectal examination is within the scope of nursing practice,
some agency policies require a primary care provider’s order
for digital manipulation and removal of a fecal impaction.
Although fecal impaction can generally be prevented,
treatment of impacted feces is sometimes necessary. When
fecal impaction is suspected, the client is often given an
oil retention enema, a cleansing enema 2 to 4 hours later,
and daily additional cleansing enemas, suppositories, or
stool softeners. If these measures fail, manual removal is
often necessary.
Diarrhea
Diarrhea refers to the passage of liquid feces and an
increased frequency of defecation. It is the opposite of constipation and results from rapid movement of fecal contents through the large intestine. Rapid passage of chyme
reduces the time available for the large intestine to reabsorb
water and electrolytes. Some individuals pass stool with
increased frequency, but diarrhea is not present unless the
stool is relatively unformed and excessively liquid. The
individual with diarrhea finds it difficult or impossible
to control the urge to defecate. Diarrhea and the threat of
incontinence are sources of concern and embarrassment.
Often, spasmodic cramps are associated with diarrhea.
Bowel sounds are increased. With persistent diarrhea, irritation of the anal region extending to the perineum and
buttocks generally results. Fatigue, weakness, malaise, and
emaciation are the results of prolonged diarrhea.
When the cause of diarrhea is irritants in the intestinal
tract, diarrhea is thought to be a protective flushing mechanism. It can create serious fluid and electrolyte losses in
TABLE 48.3
●
Fecal Elimination
1277
the body, however, that can develop within frighteningly
short periods of time, particularly in infants, small children, and older adults.
The prevalence of Clostridium difficile infection (CDI),
which produces mucoid and foul-smelling diarrhea, has
been increasing in recent years. Clients at the highest risk
for the development of CDI include immunosuppressed
individuals, clients of advanced age, and those who have
recently used antimicrobial agents, usually fluoroquinolones (Sams & Kennedy-Malone, 2017). Older adults are at
the greatest risk due to underlying disease(s) and greater
exposure in hospitals and extended care facilities. Infection control against CDI includes hand hygiene, contact
precautions, and cleaning of surfaces with a bleach solution. All individuals involved in the care of the client need
to be reminded to wash their hands with soap and water
because alcohol-based hand gels are not effective against
C. difficile. Also, wearing gloves when coming into contact with soiled linens is needed to prevent the spread of
the bacteria and spores that exist with C. difficile (Smith &
Taylor, 2016). Table 48.3 lists some of the major causes of
diarrhea and the physiologic responses of the body.
The irritating effects of diarrhea stool increase the risk
for skin breakdown. Therefore, the area around the anal
region should be kept clean and dry and be protected with
zinc oxide or other ointment. In addition, a fecal collector
can be used (see page 1289).
Bowel Incontinence
Bowel incontinence, also called fecal incontinence, refers to
the loss of voluntary ability to control fecal and gaseous discharges through the anal sphincter. The incontinence may
occur at specific times, such as after meals, or it may occur
irregularly. Fecal incontinence is generally associated with
impaired functioning of the anal sphincter or its nerve supply, such as in some neuromuscular diseases, spinal cord
trauma, and tumors of the external anal sphincter muscle.
The prevalence of bowel incontinence increases with
age. Bowel incontinence is an emotionally distressing problem that can ultimately lead to social isolation. Afflicted
individuals withdraw into their homes or, if in the hospital,
the confines of their room, to minimize the embarrassment
associated with soiling. Treatment depends on the cause of
the fecal incontinence. Many help manage their situation
Major Causes of Diarrhea
Cause
Physiologic Effect
Psychologic stress (e.g., anxiety)
Increased intestinal motility and mucous secretion
Medications
Inflammation and infection of mucosa due to overgrowth of pathogenic intestinal microorganisms
Antibiotics
Irritation of intestinal mucosa
Iron
Irritation of intestinal mucosa
Cathartics
Incomplete digestion of food or fluid
Allergy to food, fluid, drugs
Increased intestinal motility and mucous secretion
Intolerance of food or fluid
Reduced absorption of fluids
Diseases of the colon (e.g., malabsorption
syndrome, Crohn’s disease)
Inflammation of the mucosa often leading to ulcer formation
M48_BERM9793_11_GE_C48.indd 1277
27/01/2021 18:03
1278
Unit 10
●
Promoting Physiologic Health
by modifying their diet (e.g., decreasing alcohol, caffeine,
greasy or spicy food, gas-producing vegetables). Weight
loss improves continence by removing weight on the pelvic
muscles. Pelvic muscle function is also enhanced by exercises. A regular defecation schedule can also help (Gump &
Schmelzer, 2016). Several surgical procedures are used for
the treatment of fecal incontinence. These include repair of
the sphincter and bowel diversion or colostomy.
Flatulence
The three primary sources of flatus are (1) action of bacteria on the chyme in the large intestine, (2) swallowed
air, and (3) gas that diffuses between the bloodstream
and the intestine.
Most gases that are swallowed are expelled through
the mouth by eructation (belching). However, large
amounts of gas can accumulate in the stomach, resulting
in gastric distention. The gases formed in the large intestine are chiefly absorbed through the intestinal capillaries
into the circulation. Flatulence is the presence of excessive
flatus in the intestines and leads to stretching and inflation of the intestines (intestinal distention). Flatulence can
occur in the colon from a variety of causes, such as foods
(e.g., cabbage, onions), abdominal surgery, or opioids. If
the gas is propelled by increased colon activity before it
can be absorbed, it may be expelled through the anus. If
excessive gas cannot be expelled through the anus, it may
be necessary to insert a rectal tube to remove it.
LIFESPAN CONSIDERATIONS Factors in Potential Bowel Elimination Problems
CHILDREN
• Successful toilet training can prevent many problems with elimination. The family should be assessed for “readiness to train.”
Assess the child’s physical, cognitive, and interpersonal skills,
and parental readiness. Does the child have sphincter control
(usually by 18 to 24 months)? Does the child understand the
meaning of toileting? Is the child able to express him- or herself
and does the child demonstrate interest in learning? Are parents ready to work with the child?
• Encourage a regular toileting routine for children. When toilet
training, ensure that toddlers can rest their feet comfortably
on the floor or a footstool, and are not frightened or pressured
while toileting.
• An acute episode of dehydration and constipation (often related
to an illness) can lead to chronic stool problems. Constipation
can cause painful defecation, which causes the child to withhold
stool, leading to more severe constipation, more pain on defecation, more withholding, and so on. Breaking the cycle by helping
ease defecation is important to prevent long-term problems.
OLDER ADULTS
• Poor fluid intake and inability to eat a high-fiber diet, due to swallowing or chewing difficulties, are often causes of constipation.
• Medications that are commonly taken by older adults such as
antacids, many antihypertensives, antidepressants, diuretics,
and narcotics for pain also contribute to constipation.
• Clients receiving tube feedings can experience diarrhea. To alleviate
it, they require a change of formula, a change in its strength, or a
change in the speed or temperature of tube feeding administration.
• Clients receiving laxative preparation for x-rays or other procedures
may experience fluid and electrolyte imbalances due to diarrhea.
• Clients with cognitive impairment, such as Alzheimer’s disease,
may be unaware of what and when they eat or drink or of their
bowel habits. It is important that caregivers monitor the client’s
bowel elimination patterns.
• Individuals with impaired mobility may have difficulty getting to the
bathroom or using a regular toilet. A raised toilet seat and other
devices, such as bars to assist in ambulation, may be very helpful.
The decrease in activity may also contribute to constipation.
ANATOMY & PHYSIOLOGY REVIEW
Small and Large Intestines
Review the figure and reflect back on your anatomy and
physiology courses.
Pyloric sphincter
Duodenum
Transverse
colon
Ascending colon
Descending
colon
Small intestine
(jejunum and ileum)
Sigmoid
colon
Cecum
Appendix
QUESTIONS
1. What are the primary functions of the small intestine?
2. What are the primary functions of the large intestine?
3. What part of the small intestine connects to the colon?
4. What consistency would the stool be in a client with
an ileostomy and why?
5. Compare and contrast the consistency of stool in a
transverse colostomy and a descending colostomy.
6. How would you describe the stool discharged from a
sigmoidostomy?
Answers to Anatomy & Physiology Review questions are available on the faculty resources
site. Please consult with your instructor.
Rectum
Small and large intestines.
B. F. FREMGEN, and S. S. FRUCHT, MEDICAL TERMINOLOGY: A LIVING LANGUAGE,
6th Ed.,© 2016. Reprinted and Electronically reproduced by permission of Pearson Education,
Inc., New York, NY.
M48_BERM9793_11_GE_C48.indd 1278
27/01/2021 18:03
Chapter 48
NURSING MANAGEMENT
Assessing
Assessment of fecal elimination includes taking a nursing
history; performing a physical examination of the abdomen, rectum, and anus; and inspecting the feces. The
nurse also should review any data obtained from relevant
diagnostic tests.
Nursing History
A nursing history for fecal elimination helps the nurse
learn the client’s normal pattern. The nurse obtains a
description of usual feces and any recent changes and
collects information about any past or current problems
with elimination, the presence of an ostomy, and factors
influencing the elimination pattern.
Examples of questions to obtain this information are
shown in the Assessment Interview. The number of questions to ask is adapted to the individual client, according
to the client’s responses in the first three categories. For
example, questions about factors influencing elimination
might be addressed only to clients who are experiencing
problems.
When obtaining data about the client’s defecation
pattern, the nurse needs to understand that the time of
defecation and the amount of feces expelled are as individual as the frequency of defecation. Often, the patterns
individuals follow depend largely on early training and
on convenience.
Physical Examination
Physical examination of the abdomen in relation to fecal
elimination problems includes inspection, auscultation,
percussion, and palpation with specific reference to the
●
Fecal Elimination
1279
intestinal tract. Auscultation precedes palpation because
palpation can alter peristalsis. Examination of the rectum
and anus includes inspection and palpation. Physical
examination of the abdomen, rectum, and anus is discussed in Chapter 29 .
Inspecting the Feces
Observe the client’s stool for color, consistency, shape,
amount, odor, and the presence of abnormal constituents.
Table 48.1, earlier in this chapter, summarizes normal and
abnormal characteristics of stool and possible causes.
Diagnostic Studies
Diagnostic studies of the gastrointestinal tract include
direct visualization techniques, indirect visualization techniques, and laboratory tests for abnormal constituents (see
Chapter 34 ).
Diagnosing
Examples of nursing diagnoses for clients with fecal
eliminal problems can include bowel incontinence, constipation, and diarrhea. Clinical application of selected
diagnoses is shown at the end of the chapter in the Nursing Care Plan and Concept Map.
Fecal elimination problems may affect many other
areas of human functioning and as a consequence may
be the etiology of other nursing diagnoses. Examples
include: Potential for decreased fluid volume or potential for altered electrolytes related to prolonged diarrhea,
potential for developing altered skin integrity related to
prolonged diarrhea or bowel incontinence, impaired selfesteem related to fecal incontinence, lack of knowledge
(bowel training, ostomy management) related to lack of
previous experience.
ASSESSMENT INTERVIEW Fecal Elimination
DEFECATION PATTERN
• When do you usually have a bowel movement?
• Has this pattern changed recently?
DESCRIPTION OF FECES AND ANY CHANGES
• Have you noticed any changes in the color, texture (hard, soft,
watery), shape, or odor of your stool recently?
FECAL ELIMINATION PROBLEMS
• What problems have you had or do you now have with your
bowel movements (constipation, diarrhea, excessive flatulence,
seepage, or incontinence)?
• When and how often does it occur?
• What do you think causes it (food, fluids, exercise, emotions,
medications, disease, surgery)?
• What have you tried to solve the problem, and how effective
was it?
FACTORS INFLUENCING ELIMINATION
• Use of elimination aids. What routines do you follow to maintain
your usual defecation pattern? Do you use natural aids such as
specific foods or fluids (e.g., a glass of hot lemon juice before
breakfast), laxatives, or enemas to maintain elimination?
M48_BERM9793_11_GE_C48.indd 1279
•
•
•
•
•
Diet. What foods do you believe affect defecation? What foods
do you typically eat? What foods do you avoid? Do you take
meals at regular times?
Fluid. What amount and kind of fluid do you take each day
(e.g., 6 glasses of water, 2 cups of coffee)?
Exercise. What is your usual daily exercise pattern? (Obtain
specifics about exercise rather than asking whether it is sufficient; ideas of what is sufficient vary among individuals.)
Medications. Have you taken any medications that could affect
the intestinal tract (e.g., iron, antibiotics)?
Stress. Are you experiencing any stress? Do you think this
affects your defecation pattern? How?
PRESENCE AND MANAGEMENT OF OSTOMY
• What is your usual routine with your colostomy or ileostomy?
• What type of appliance do you wear and did you bring a spare
with you?
• What problems, if any, do you have with it?
• How can the nurses help you manage your colostomy or
ileostomy?
27/01/2021 18:03
1280
Unit 10
●
Promoting Physiologic Health
Planning
The major goals for clients with fecal elimination problems
are to:
•
•
•
Maintain or restore normal bowel elimination pattern.
Maintain or regain normal stool consistency.
Prevent associated risks such as fluid and electrolyte
imbalance, skin breakdown, abdominal distention, and
pain.
Appropriate preventive and corrective nursing interventions that relate to these must be identified. Specific
nursing activities associated with each of these interventions can be selected to meet the client’s individual needs.
Examples of clinical applications of these using nursing
diagnoses, Nursing Interventions Classifications (NIC),
and Nursing Outcomes Classifications (NOC) designations are shown in the Nursing Care Plan at the end of
the chapter.
Planning for Home Care
Clients who have ongoing elimination problems will need
continuing care in the home setting. In preparation for discharge, the nurse needs to assess the client’s and family’s
ability to meet specific care needs.
QSEN
CLIENT AND ENVIRONMENT
•
•
•
•
Self-care abilities for toileting: ability to get to the toilet, to adjust clothing for toileting, to perform toileting
hygiene, and to flush the toilet
Mechanical aids required: walker, cane, wheelchair,
raised toilet seat, grab bars, bedpan, commode
Mechanical barriers that limit access to the toilet or
are unsafe: poor lighting, cluttered pathway to bathroom, narrow doorway for wheelchair, and so on
Bowel elimination problem: alterations in characteristics of feces, diarrhea, constipation, incontinence, presence of ostomy, and methods of handling these
Level of knowledge: planned bowel management or
training program, prescribed medications, ostomy care,
dietary alterations, and fluid and exercise requirements
or restrictions
Facilities: adequacy of bathroom facilities to assist toileting hygiene and ostomy care and to contain potentially infectious fecal effluent or stool
FAMILY
•
•
•
Patient-Centered Care Fecal Elimination
The following specific home care assessment data are
required before developing a home care plan.
•
•
Caregiver availability and skills: caregivers able to
assist with toileting, medications, ostomy care, or other
prescribed therapeutic measures
Family role changes and coping: effect on financial
status, parenting and spousal roles, sexuality, social
roles
Alternate potential primary or respite caregivers: for
example, other family members, volunteers, church
members, paid caregivers or housekeeping services;
available community respite care (adult day care,
seniors’ centers)
COMMUNITY
•
Availability of and familiarity with possible sources of
assistance: equipment and supply companies, financial
assistance, home health agencies
Using the assessment data, the nurse designs a teaching plan for the client and family (see Client Teaching).
CLIENT TEACHING Fecal Elimination
FACILITATING TOILETING
• Ensure safe and easy access to the toilet. Make sure lighting is
appropriate, scatter rugs are removed or securely fastened, and
so on.
• Facilitate instruction as needed about transfer techniques.
• Suggest ways that garments can be adjusted to make disrobing easier for toileting (e.g., Velcro closing on clothing).
MONITORING BOWEL ELIMINATION PATTERN
• Instruct the client, if appropriate, to keep a record of time and
frequency of stool passage, any associated pain, and color and
consistency of the stool.
DIETARY ALTERATIONS
• Provide information about required food and fluid alterations to
promote defecation or to manage diarrhea.
MEDICATIONS
• Discuss problems associated with overuse of laxatives, if
appropriate, and the use of alternatives to laxatives, suppositories, and enemas.
• Discuss the addition of a fiber supplement if the client is taking
a constipating medication.
M48_BERM9793_11_GE_C48.indd 1280
MEASURES SPECIFIC TO ELIMINATION PROBLEM
• Provide instructions associated with specific elimination problems and treatment, such as constipation, diarrhea, and ostomy
care.
COMMUNITY AGENCIES AND OTHER SOURCES OF HELP
• Make appropriate referrals to home care or community care
for assistance with resources such as installation of grab
bars and raised toilet seats, structural alterations for wheelchair access, homemaker or home health aide services
to assist with activities of daily living, and an enterostomal
therapy nurse for assistance with stoma care and selection
of ostomy appliances.
• Provide information about companies where durable medical equipment (e.g., raised toilet seats, commodes, bedpans, urinals) can be purchased, rented, or obtained free of
charge, and where medical supplies such as incontinence
pads or ostomy irrigating supplies and appliances can be
obtained.
• Suggest additional sources of information and help such as
ostomy self-help and support groups or clubs.
27/01/2021 18:03
Chapter 48
Implementing
Promoting Regular Defecation
The nurse can help clients achieve regular defecation
by attending to (a) the provision of privacy, (b) timing,
(c) nutrition and fluids, (d) exercise, and (e) positioning.
See Client Teaching for healthy habits related to bowel
elimination.
Privacy
Privacy during defecation is extremely important to many
clients. The nurse should therefore provide as much privacy as possible for such clients but may need to stay with
those who are too weak to be left alone. Some clients also
prefer to wipe, wash, and dry themselves after defecating.
A nurse may need to provide water, washcloth, and towel
or wipes for this purpose.
Timing
A client should be encouraged to defecate when the urge
is recognized. To establish regular bowel elimination, the
client and nurse can discuss when peristalsis normally
occurs and provide time for defecation. Many clients have
well-established routines. Other activities, such as bathing
and ambulating, should not interfere with the defecation
time.
Nutrition and Fluids
The diet a client needs for regular normal elimination varies, depending on the kind of feces the client currently has,
the frequency of defecation, and the types of foods that the
client finds assist with normal defecation.
CLIENT TEACHING Healthy Defecation
•
•
•
•
•
•
Establish a regular exercise regimen.
Include high-fiber foods, such as vegetables, fruits, and whole
grains, in the diet.
Maintain fluid intake of 2000 to 3000 mL/day.
Do not ignore the urge to defecate.
Allow time to defecate, preferably at the same time each day.
Avoid OTC medications to treat constipation and diarrhea.
●
Fecal Elimination
1281
For Constipation
Increase daily fluid intake, and instruct the client to drink
hot liquids, warm water with a squirt of fresh lemon, and
fruit juices, especially prune juice. Include fiber in the diet,
that is, foods such as raw fruit, bran products, and wholegrain cereals and bread.
For Diarrhea
Encourage oral intake of fluids and bland food. Eating
small amounts can be helpful because small amounts
are more easily absorbed. Excessively hot or cold fluids
should be avoided because they stimulate peristalsis. In
addition, highly spiced foods and high-fiber foods can
aggravate diarrhea. See Client Teaching for details about
managing diarrhea.
For Flatulence
Limit carbonated beverages, the use of drinking straws,
and chewing gum—all of which increase the ingestion of
air. Gas-forming foods, such as cabbage, beans, onions,
and cauliflower, should also be avoided.
Exercise
Regular exercise helps clients develop a regular defecation pattern. A client with weak abdominal and pelvic
muscles (which delay normal defecation) may be able to
strengthen them with the following isometric exercises:
•
•
In a supine position, the client tightens the abdominal muscles as though pulling them inward, holding
them for about 10 seconds and then relaxing them.
This should be repeated 5 to 10 times, four times a day,
depending on the client’s health.
Again in a supine position, the client can contract the
thigh muscles and hold them contracted for about 10 seconds, repeating the exercise 5 to 10 times, four times a day.
This helps the client confined to bed gain strength in the
thigh muscles, thereby making it easier to use a bedpan.
Positioning
Although the squatting position best facilitates defecation, on a toilet seat the best position for most individuals
seems to be leaning forward.
CLIENT TEACHING Managing Diarrhea
•
•
•
•
•
Drink at least 8 glasses of water per day to prevent dehydration. Consider drinking a few glasses of electrolyte replacement
fluids a day.
Eat foods with sodium and potassium. Most foods contain
sodium. Potassium is found in meats and many vegetables
and fruits, especially purple grape juice, tomatoes, potatoes,
bananas, cooked peaches, and apricots.
Increase foods containing soluble fiber, such as rice, oatmeal,
and skinless fruits and potatoes.
Avoid alcohol and beverages with caffeine, which aggravate the
problem.
Limit foods containing insoluble fiber, such as high-fiber wholewheat and whole-grain breads and cereals, and raw fruits and
vegetables.
M48_BERM9793_11_GE_C48.indd 1281
Limit fatty foods.
Thoroughly clean and dry the perianal area after passing stool
to prevent skin irritation and breakdown. Use soft toilet tissue
to clean and dry the area. Apply a dimethicone-based cream or
alcohol-free barrier film as needed.
• If possible, discontinue medications that cause diarrhea.
• When diarrhea has stopped, reestablish normal bowel flora by
eating fermented dairy products, such as yogurt or buttermilk.
• Seek a primary care provider consultation right away if weakness, dizziness, or loose stools persist more than 48 hours.
•
•
27/01/2021 18:03
1282
Unit 10
●
Promoting Physiologic Health
For clients who have difficulty sitting down and
getting up from the toilet, an elevated toilet seat can be
attached to a regular toilet. Clients then do not have to
lower themselves as far onto the seat and do not have
to lift as far off the seat. Elevated toilet seats can be purchased for use in the home.
A bedside commode, a portable chair with a toilet seat
and a receptacle beneath that can be emptied, is often used
for the adult client who can get out of bed but is unable to
walk to the bathroom (Figure 48.4 ■). Some commodes have
wheels and can slide over the base of a regular toilet when
the waste receptacle is removed, thus providing clients the
privacy of a bathroom. Potty chairs are available for children.
Clients restricted to bed may need to use a bedpan, a
receptacle for urine and feces. Female clients use a bedpan for both urine and feces; male clients use a bedpan
for feces and a urinal for urine. The two main types of
bedpans are the regular high-back pan and the slipper, or
fracture, pan (Figure 48.5 ■). The slipper pan has a low
back and is used for clients unable to raise their buttocks
because of physical problems or therapy that contraindicates such movement. Many older adults benefit from the
use of a slipper pan. See Practice Guidelines for the techniques of giving and removing a bedpan.
Figure 48.4 ■ A commode with overlying seat.
Figure 48.5 ■ Left, The high-back or regular bedpan; right, the slipper or fracture pan.
PRACTICE GUIDELINES Giving and Removing a Bedpan
•
•
•
•
•
•
•
•
•
Provide privacy.
Wear clean gloves.
If the bedpan is metal, warm it by rinsing it with warm water.
Adjust the bed to a height appropriate to prevent back strain.
Elevate the side rail on the opposite side to prevent the client
from falling out of bed.
Ask the client to assist by flexing the knees, resting the weight
on the back and heels, and raising the buttocks, or by using a
trapeze bar, if present.
Help lift the client as needed by placing one hand under the
lower back, resting your elbow on the mattress, and using your
forearm as a lever.
Lubricate the back of the bedpan with a small amount of hand
lotion or liquid soap to reduce tissue friction and shearing.
Place a regular bedpan so that the client’s buttocks rest on the
smooth, rounded rim. Place a slipper pan with the flat, low end
under the client’s buttocks (Figure 48.6 ■).
M48_BERM9793_11_GE_C48.indd 1282
Figure 48.6 ■ Placing a slipper pan under the buttocks.
27/01/2021 18:03
Chapter 48
●
Fecal Elimination
1283
PRACTICE GUIDELINES Giving and Removing a Bedpan—continued
For the client who cannot assist, obtain the assistance of
another nurse to help lift the client onto the bedpan or place
the client on his or her side, place the bedpan against the
buttocks (Figure 48.7 ■), and roll the client back onto the
bedpan.
• Provide a more normal position for the client’s lower back by
elevating the client’s bed to a semi-Fowler’s position, if permitted. If elevation is contraindicated, support the client’s back
with pillows as needed to prevent hyperextension of the back.
• Cover the client with bed linen to maintain comfort and dignity.
•
•
•
•
•
•
•
•
•
•
•
•
Figure 48.7 ■ Placing a regular bedpan against the client’s buttocks.
Teaching About Medications
The most common categories of medications affecting
fecal elimination are cathartics and laxatives, antidiarrheals, and antiflatulents.
Cathartics and Laxatives
Cathartics are drugs that induce defecation. They can have
a strong, emptying effect. A laxative is mild in comparison
to a cathartic, and it produces soft or liquid stools that are
sometimes accompanied by abdominal cramps. Examples of
cathartics are castor oil, cascara, phenolphthalein, and bisacodyl. Table 48.4 describes the different types of laxatives.
Laxatives are contraindicated in the client who has
nausea, cramps, colic, vomiting, or undiagnosed abdominal pain. Clients need to be informed about the dangers
of laxative use. Continual use of laxatives to encourage
bowel evacuation weakens the bowel’s natural responses
to fecal distention, resulting in chronic constipation. To
eliminate chronic laxative use, it is usually necessary to
teach the client about dietary fiber, regular exercise, taking sufficient fluids, and establishing regular defecation
habits. In addition, any medication regimen should be
examined to see whether it could cause constipation.
Some laxatives are given in the form of suppositories.
These act in various ways: by softening the feces, by releasing gases such as carbon dioxide to distend the rectum, or
by stimulating the nerve endings in the rectal mucosa. The
best results can be obtained by inserting the suppository
M48_BERM9793_11_GE_C48.indd 1283
Provide toilet tissue, place the call light within reach, lower the
bed to the low position, elevate the side rail if indicated, and
leave the client alone.
Answer the call light promptly.
Do not leave clients on a bedpan longer than 15 minutes unless
they are able to remove the pan themselves. Lengthy stays on
a bedpan can cause skin breakdown.
When removing the bedpan, return the bed to the position used
when giving the bedpan, hold the bedpan steady to prevent
spillage of its contents, cover the bedpan, and place it on the
adjacent chair.
If the client needs assistance, apply gloves and wipe the client’s
perineal area with several layers of toilet tissue. If a specimen is
to be collected, discard the soiled tissue into a moisture-proof
receptacle other than the bedpan. For female clients, clean
from the urethra toward the anus to prevent transferring rectal
microorganisms into the urinary meatus.
Wash the perineal area of dependent clients with soap and
water as indicated and thoroughly dry the area.
For all clients, offer warm water, soap, a washcloth, and a towel
to wash the hands.
Assist the client to a comfortable position, empty and clean the
bedpan, and return it to the bedside.
Remove and discard your gloves and wash your hands.
Spray the room with air freshener as needed to control odor unless
contraindicated because of respiratory problems or allergies.
Document color, odor, amount, and consistency of urine and
feces, and the condition of the perineal area.
30 minutes before the client’s usual defecation time or when
the peristaltic action is greatest, such as after breakfast.
Antidiarrheal Medications
These medications slow the motility of the intestine or
absorb excess fluid in the intestine. Guidelines for using
antidiarrheals are shown in Box 48.3.
Antiflatulent Medications
Antiflatulent agents such as simethicone do not
decrease the formation of flatus but they do coalesce
the gas bubbles and facilitate their passage by belching
through the mouth or expulsion through the anus. A
combination of simethicone and loperamide (Imodium
Advanced) is effective in relieving abdominal bloating and gas associated with acute diarrhea; however,
no convincing evidence has been shown for common
flatulence. Carminatives are herbal oils known to act as
agents that help expel gas from the stomach and intestines. Suppositories can also be given to relieve flatus
by increasing intestinal motility.
Decreasing Flatulence
There are a number of ways to reduce or expel flatus,
including exercise, moving in bed, ambulation, and
avoiding gas-producing foods. Movement stimulates
peristalsis and the escape of flatus and reabsorption
of gases in the intestinal capillaries. Certain medications can decrease flatulence. Bismuth subsalicylate
27/01/2021 18:03
1284
Unit 10
●
Promoting Physiologic Health
Types of Laxatives
TABLE 48.4
Type
Action
Examples
Pertinent Teaching Information
Bulk forming
Increases the fluid,
gaseous, or solid bulk in
the intestines.
Psyllium hydrophilic mucilloid
(Metamucil), methylcellulose
(Citrucel)
May take 12 or more hours to act. Sufficient fluid
must be taken. Safe for long-term use.
Osmotic
Draws water into the
intestine by osmosis, and
works by holding water in
the stool to soften the stool.
The active ingredient is
polyethylene glycol (PEG).
MiraLax,
GoLYTELY, NuLYTELY
A laxative that is helpful in the treatment of
constipation. It is a powder that is tasteless when
mixed in a flavored liquid such as juice.
Used for cleaning of the colon before colonoscopy.
Requires drinking a large volume (4 L), which
may be difficult for clients to tolerate. Has an
unpleasant taste.
Saline
The active ingredients are
usually magnesium, sulfate,
citrate, and phosphate
ions, which draw water
into the intestines. The
additional water softens
the stool and stimulates
peristalsis.
Fleet Phospho-Soda,
milk of magnesia, and
magnesium citrate
Should be taken with one to two 8-ounce glasses
of water.
May be rapid acting.
Can cause fluid and electrolyte imbalance,
particularly in older people and children with
cardiac and renal disease.
Use caution when giving to older adults.
Stimulant or irritant
Irritates the intestinal
mucosa or stimulates
nerve endings in the wall of
the intestine, causing rapid
propulsion of the contents.
Bisacodyl (Dulcolax,
Correctol), senna (Senokot,
Ex-Lax), cascara, castor oil
Acts more quickly than bulk-forming agents.
Fluid is passed with the feces.
May cause cramps.
Use only for short periods of time. Prolonged use
may cause fluid and electrolyte imbalance.
Stool softener or
surfactant
Softens and delays the
drying of the stool; causes
more water and fat to be
absorbed into the stool.
Docusate sodium (Colace)
Docusate calcium (Surfak)
Slow-acting; may take several days.
Lubricant
Lubricates the stool and
colon mucosa.
Mineral oil (Haley’s M-O)
Prolonged use inhibits the absorption of some
fat-soluble vitamins.
BOX 48.3
•
•
•
•
•
•
Guidelines for Using Antidiarrheal
Medications
If the diarrhea persists for more than 3 or 4 days, determine
the underlying cause. Using a medication such as an opiate
when the cause is an infection, toxin, or poison may prolong
diarrhea.
Long-term use of OTC medications (e.g., loperamide hydrochloride [Imodium]) can produce dependence.
Some antidiarrheal agents can cause drowsiness (e.g.,
diphenoxylate hydrochloride [Lomotil]) and should not be used
when driving an automobile or running machinery.
Kaolin-pectin preparations (e.g., Kaopectate) may absorb
nutrients.
Bulk laxatives and other absorbents may be used to help bind
toxins and absorb excess bowel liquid.
Bismuth preparations (e.g., Pepto-Bismol), often used to treat
“traveler’s diarrhea,” may contain aspirin and should not be
given to children and teenagers with chickenpox, influenza,
and other viral infections.
Administering Enemas
An enema is a solution introduced into the rectum and
large intestine. The action of an enema is to distend the
intestine and sometimes to irritate the intestinal mucosa,
thereby increasing peristalsis and the excretion of feces
and flatus. The enema solution should be at 37.7°C (100°F)
because a solution that is too cold or too hot is uncomfortable and causes cramping. Enemas are classified into
groups: cleansing, retention, and distention reduction,
which includes carminative and return-flow enemas.
Cleansing Enema
Cleansing enemas are intended to remove feces. They are
given chiefly to:
•
•
•
(Pepto-Bismol) can be effective; however, it should
not be used as a continuous treatment because it contains aspirin and could cause salicylate toxicity. Alphagalactosidase (Beano) is effective for reducing flatulence
caused by eating fermentable carbohydrates (e.g.,
beans, bran, fruit).
M48_BERM9793_11_GE_C48.indd 1284
Prevent the escape of feces during surgery.
Prepare the intestine for certain diagnostic tests such as
x-ray or visualization tests (e.g., colonoscopy).
Remove feces in instances of constipation or impaction.
Cleansing enemas use a variety of solutions. Table 48.5
lists commonly used solutions.
Hypertonic solutions exert osmotic pressure, which
draws fluid from the interstitial space into the colon. The
increased volume in the colon stimulates peristalsis and
thus defecation. A commonly used hypertonic enema is the
commercially prepared Fleet phosphate enema. Hypotonic
27/01/2021 18:03
Chapter 48
TABLE 48.5
●
Fecal Elimination
1285
Commonly Used Enema Solutions
Solution
Constituents
Action
Time to Take Effect
Adverse Effects
Hypertonic
90–120 mL of solution (e.g.,
sodium phosphate [Fleet])
Draws water into the colon.
5–10 min
Retention of sodium
Hypotonic
500–1000 mL of tap water
Distends colon, stimulates
peristalsis, and softens
feces.
15–20 min
Fluid and electrolyte imbalance;
water intoxication
Isotonic
500–1000 mL of normal
saline
Distends colon, stimulates
peristalsis, and softens
feces.
15–20 min
Possible sodium retention
Soapsuds
500–1000 mL (3–5 mL soap
to 1000 mL water)
Irritates mucosa, distends
colon.
10–15 min
Irritates and may damage
mucosa
Oil (mineral, olive,
cottonseed)
90–120 mL
Lubricates the feces and
the colonic mucosa.
0.5–3 h
solutions (e.g., tap water) exert a lower osmotic pressure
than the surrounding interstitial fluid, causing water to
move from the colon into the interstitial space. Before the
water moves from the colon, it stimulates peristalsis and
defecation. Because the water moves out of the colon, the
tap water enema should not be repeated because of the danger of circulatory overload when the water moves from the
interstitial space into the circulatory system.
Safety Alert!
SAFETY
Special precautions must be used to alert nurses to possible contraindications when Fleet enemas are prescribed
for clients with renal failure. The label on the Fleet enema
warns that using more than one enema every 24 hours
can be harmful. Clients and family may underestimate the
risks for a client with decreased renal function because a
Fleet enema can be obtained over the counter in stores.
Isotonic solutions, such as physiologic (normal) saline,
are considered the safest enema solutions to use. They exert
the same osmotic pressure as the interstitial fluid surrounding the colon. Therefore, there is no fluid movement into or
out of the colon. The instilled volume of saline in the colon
stimulates peristalsis. Soapsuds enemas stimulate peristalsis by increasing the volume in the colon and irritating the
mucosa. Only pure soap (i.e., Castile soap) should be used
in order to minimize mucosa irritation.
Some enemas are large volume (i.e., 500 to 1000 mL)
for an adult and others are small volume (90 to 120 mL),
including hypertonic solutions. The amount of solution
administered for a high-volume enema will depend on
the age and medical condition of the individual. For example, clients with certain cardiac or renal diseases would be
adversely affected by significant fluid retention that might
result from large-volume hypotonic enemas.
Cleansing enemas may also be described as high or
low. A high enema is given to cleanse as much of the colon
as possible. The client changes from the left lateral position to the dorsal recumbent position and then to the right
lateral position during administration so that the solution
M48_BERM9793_11_GE_C48.indd 1285
can follow the large intestine. The low enema is used to
clean the rectum and sigmoid colon only. The client maintains a left lateral position during administration.
The force of flow of the solution is governed by (a) the
height of the solution container, (b) size of the tubing, (c)
viscosity of the fluid, and (d) resistance of the rectum. The
higher the solution container is held above the rectum,
the faster the flow and the greater the force (pressure) in the
rectum. During most adult enemas, the solution container
should be no higher than 30 cm (12 in.) above the rectum.
During a high cleansing enema, the solution container is usually held 30 to 48 cm (12 to 18 in.) above the rectum because
the fluid is instilled farther to clean the entire bowel.
Retention Enema
A retention enema introduces oil or medication into the
rectum and sigmoid colon. The liquid is retained for a
relatively long period (e.g., 1 to 3 hours). An oil retention enema acts to soften the feces and to lubricate the
rectum and anal canal, thus facilitating passage of the
feces. Antibiotic enemas are used to treat infections locally,
anthelmintic enemas to kill helminths such as worms and
intestinal parasites, and nutritive enemas to administer
fluids and nutrients to the rectum.
Carminative Enema
A carminative enema is given primarily to expel flatus.
The solution instilled into the rectum releases gas, which
in turn distends the rectum and the colon, thus stimulating
peristalsis. For an adult, 60 to 80 mL of fluid is instilled.
Return-Flow Enema
A return-flow enema, also called a Harris flush, is occasionally used to expel flatus. Alternating flow of 100 to 200 mL of
fluid into and out of the rectum and sigmoid colon stimulates
peristalsis. This process is repeated five or six times until the
flatus is expelled and abdominal distention is relieved.
From a holistic perspective, it is important for the
nurse to remember that clients may perceive this type
of procedure as a significant violation of personal space.
The nurse needs to consider personal space, gender of the
27/01/2021 18:03
1286
Unit 10
●
Promoting Physiologic Health
caregiver, and the potential meaning of the structures and
fluids found in this private area of the body. Keep in mind
the client’s potential discomfort with the gender of the
caregiver and try to accommodate the client’s preferences
whenever possible. When it is not possible to honor the
client’s wishes, respectfully explain the circumstances.
A gentle, matter-of-fact approach is often most helpful.
Also, insertion of anything foreign into an orifice of a client’s body may trigger memories of past abuse. Monitor
the client for emotional responses to the procedure (both
subtle and extreme) because this could indicate a history
of trauma and require appropriate referral for counseling.
Simply asking the client to describe the experience will
give the nurse more information for possible referral.
Skill 48.1 describes how to administer an enema.
Clinical Alert!
Some clients may wish to administer their own enemas. If this is
appropriate, the nurse validates the client’s knowledge of correct
technique and assists as needed.
Administering an Enema
SKILL 48.1
PURPOSE
• To achieve one or more of the following actions: cleansing, retention, carminative, or return-flow
ASSESSMENT
Assess
• When the client last had a bowel movement and the amount,
color, and consistency of the feces
• Presence of abdominal distention
PLANNING
Before administering an enema, determine that there is a primary
care provider’s order. At some agencies, a primary care provider must
order the type of enema and the time to give it, for example, the
morning of an examination. At other agencies, enemas are given at
the nurse’s discretion (i.e., as necessary on a prn order). In addition,
determine the presence of kidney or cardiac disease that contraindicates the use of a hypotonic or hypertonic solution.
Assignment
Administration of some enemas may be assigned to assistive personnel (AP). However, the nurse must ensure the personnel are competent in the use of standard precautions. Abnormal findings such as
inability to insert the rectal tip, client inability to retain the solution, or
unusual return from the enema must be validated and interpreted
by the nurse.
IMPLEMENTATION
Preparation
• Lubricate about 5 cm (2 in.) of the rectal tube (some commercially prepared enema sets already have lubricated nozzles).
Rationale: Lubrication facilitates insertion through the sphincter
and minimizes trauma.
• Run some solution through the connecting tubing of a largevolume enema set and the rectal tube to expel any air in the
tubing, then close the clamp. Rationale: Air instilled into the
rectum, although not harmful, causes unnecessary distention.
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client
what you are going to do, why it is necessary, and how to participate. Discuss how the results will be used in planning further
care or treatment. Indicate that the client may experience a
feeling of fullness while the solution is being administered.
Explain the need to hold the solution as long as possible.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Apply clean gloves.
4. Provide for client privacy.
M48_BERM9793_11_GE_C48.indd 1286
•
•
Whether the client has sphincter control
Whether the client can use a toilet or commode or must remain
in bed and use a bedpan
Equipment
• Disposable linen-saver pad
• Bath blanket
• Bedpan or commode
• Clean gloves
• Water-soluble lubricant if tubing not prelubricated
• Paper towel
Large-Volume Enema
• Solution container with tubing of correct size and tubing clamp
• Correct solution, amount, and temperature
Small-Volume Enema
• Prepackaged container of enema solution with lubricated tip
5. Assist the adult client to a left lateral position, with the right
leg as acutely flexed as possible ❶, with the linen-saver pad
under the buttocks. Rationale: This position facilitates the flow
of solution by gravity into the sigmoid and descending colon,
which are on the left side. Having the right leg acutely flexed
provides for adequate exposure of the anus.
6. Insert the enema tube.
• For clients in the left lateral position, lift the upper buttock.
❷ Rationale: This ensures good visualization of the anus.
❶ Assuming a left lateral position for an enema. Note the commercially
prepared enema.
27/01/2021 18:03
Chapter 48
●
Fecal Elimination
1287
Administering an Enema—continued
SKILL 48.1
❷ Inserting the enema tube.
Insert the tube smoothly and slowly into the rectum, directing it toward the umbilicus. ❸ Rationale: The angle follows
the normal contour of the rectum. Slow insertion prevents
spasm of the sphincter.
• Insert the tube 7 to 10 cm (3 to 4 in.). Rationale: Because
the anal canal is about 2.5 to 5 cm (1 to 2 in.) long in
the adult, insertion to this point places the tip of the tube
beyond the anal sphincter into the rectum.
• If resistance is encountered at the internal sphincter, ask
the client to take a deep breath, then run a small amount of
solution through the tube. Rationale: This relaxes the internal anal sphincter.
• Never force tube or solution entry. If instilling a small amount
of solution does not permit the tube to be advanced or
the solution to freely flow, withdraw the tube. Check for
any stool that may have blocked the tube during insertion.
If present, flush it and retry the procedure. You may also
perform a digital rectal examination to determine if there is
an impaction or other mechanical blockage. If resistance
persists, end the procedure and report the resistance to the
primary care provider and nurse in charge.
7. Slowly administer the enema solution.
• Raise the solution container, and open the clamp to allow
fluid flow.
or
• Compress a pliable container by hand.
• During most low enemas, hold or hang the solution container no higher than 30 cm (12 in.) above the rectum.
Rationale: The higher the solution container is held above
the rectum, the faster the flow and the greater the force
(pressure) in the rectum. During a high enema, hang the
solution container about 30 to 49 cm (12 to18 in.).
Rationale: Fluid must be instilled farther for a high enema to
clean the entire bowel. See agency protocol.
• Administer the fluid slowly. If the client complains of fullness
or pain, lower the container or use the clamp to stop the
•
❹ Rolling up a commercial enema container.
flow for 30 seconds, and then restart the flow at a slower
rate. Rationale: Administering the enema slowly and stopping the flow momentarily decreases the likelihood of intestinal spasm and premature ejection of the solution.
• If you are using a plastic commercial container, roll it up as
the fluid is instilled. This prevents subsequent suctioning of
the solution. ❹
• After all the solution has been instilled or when the client
cannot hold any more and feels the desire to defecate
(the urge to defecate usually indicates that sufficient fluid
has been administered), close the clamp, and remove the
enema tube from the anus.
• Place the enema tube in a disposable towel as you withdraw it.
8. Encourage the client to retain the enema.
• Ask the client to remain lying down. Rationale: It is easier
for the client to retain the enema when lying down than
when sitting or standing, because gravity promotes drainage and peristalsis.
• Request that the client retain the solution for the appropriate
amount of time, for example, 5 to 10 minutes for a cleansing enema or at least 30 minutes for a retention enema.
9. Assist the client to defecate.
• Assist the client to a sitting position on the bedpan, commode,
or toilet. A sitting position facilitates the act of defecation.
• Ask the client who is using the toilet not to flush it. The
nurse needs to observe the feces.
• If a specimen of feces is required, ask the client to use a
bedpan or commode.
• Remove and discard gloves.
• Perform hand hygiene.
10. Document the type and volume, if appropriate, of enema given.
Describe the results.
SAMPLE DOCUMENTATION
8/2/2020 1000. States last BM five days ago. Abdomen distended and
firm. Bowel sounds hypoactive. Fleet enema, given per order, resulted in
large amount of firm brown stool. States he “feels better.” M. Lopez, RN
❸ Inserting the enema tube following the direction of the rectum.
VARIATION: ADMINISTERING AN ENEMA TO AN INCONTINENT CLIENT
Occasionally a nurse needs to administer an enema to a client who is
unable to control the external sphincter muscle and thus cannot retain
the enema solution for even a few minutes. In that case, after the enema
Continued on page 1288
M48_BERM9793_11_GE_C48.indd 1287
27/01/2021 18:03
1288
Unit 10
●
Promoting Physiologic Health
SKILL 48.1
Administering an Enema—continued
tube is inserted, the client assumes a supine position on a bedpan. The
head of the bed can be elevated slightly, to 30 degrees if necessary for
easier breathing, and pillows used to support the client’s head and back.
VARIATION: ADMINISTERING A RETURN-FLOW ENEMA
For a return-flow enema, the solution (100 to 200 mL for an adult)
is instilled into the client’s rectum and sigmoid colon. Then the
solution container is lowered so that the fluid flows back out
through the rectal tube into the container, pulling the flatus with
it. The inflow–outflow process is repeated five or six times (to
stimulate peristalsis and the expulsion of flatus), and the solution
is replaced several times during the procedure if it becomes thick
with feces.
Document the type of solution; length of time the solution was
retained; the amount, color, and consistency of the returns; and
the relief of flatus and abdominal distention in the client record
using forms or checklists supplemented by narrative notes when
appropriate.
EVALUATION
• Perform a detailed follow-up based on findings that deviated
from expected or normal for the client. Compare findings to
previous assessment data if available. Report significant deviations from expected to the primary care provider.
LIFESPAN CONSIDERATIONS Administering an Enema
INFANTS AND CHILDREN
• Provide a careful explanation to the parents and child before the
procedure. An enema is an intrusive procedure and therefore
threatening to the child.
• The enema solution should be isotonic (usually normal saline).
Some hypertonic commercial solutions (e.g., Fleet phosphate
enema) can lead to hypovolemia and electrolyte imbalances. In
addition, the osmotic effect of the enema may produce diarrhea
and subsequent metabolic acidosis.
• Infants and small children who do not have sphincter control need
to be assisted in retaining the enema. The nurse administers the
enema while the infant or child is lying with the buttocks over the
bedpan, and the nurse firmly presses the buttocks together to
prevent the immediate expulsion of the solution. Older children
can usually hold the solution if they understand what to do and
are not required to hold it for too long a period. It may be necessary to ensure that the bathroom is available for an ambulatory
child before starting the procedure or to have a bedpan ready.
• Enema temperature should be 37.7°C (100°F) unless otherwise
ordered.
• Large-volume enemas consist of 50 to 200 mL in children less
than 18 months old; 200 to 300 mL in children 18 months to 5
years; and 300 to 500 mL in children 5 to 12 years old.
Digital Removal of a Fecal Impaction
Digital removal involves breaking up the fecal mass
digitally and removing it in portions. Because the bowel
mucosa can be injured during this procedure, some agencies restrict and specify the personnel permitted to conduct
digital disimpactions. Rectal stimulation is also contraindicated for some clients because it may cause an excessive
vagal response resulting in cardiac arrhythmia. Before disimpaction it is suggested an oil retention enema be given
and held for 30 minutes. After a disimpaction, the nurse
can use various interventions to remove remaining feces,
such as a cleansing enema or the insertion of a suppository.
Clinical Alert!
Clients with a history of cardiac disease or dysrhythmias may be at
risk with digital stimulation to remove an impaction. Digital examination of the rectum can cause stimulation of the vagal nerve, which
can slow the heart rate. If in doubt, the nurse should check with the
primary care provider before performing the procedure.
M48_BERM9793_11_GE_C48.indd 1288
For infants and small children, the dorsal recumbent position is
frequently used. Position them on a small padded bedpan with
support for the back and head. Secure the legs by placing a
diaper under the bedpan and then over and around the thighs.
Place the underpad under the client’s buttocks to protect the
bed linen, and drape the client with the bath blanket.
• Insert the tube 5 to 7.5 cm (2 to 3 in.) in the child and only 2.5
to 3.75 cm (1 to 1.5 in.) in the infant.
• For children, lower the height of the solution container appropriately for the age of the child. See agency protocol.
• To assist a small child in retaining the solution, apply firm pressure over the anus with tissue wipes, or firmly press the buttocks together.
•
OLDER ADULTS
• Older adults may fatigue easily.
• Older adults may be more susceptible to fluid and electrolyte
imbalances. Use tap water enemas with great caution.
• Monitor the client’s tolerance during the procedure, watching
for vagal episodes (e.g., slow pulse) and dysrhythmias.
• Protect older adults’ skin from prolonged exposure to moisture.
• Assist older clients with perineal care as indicated.
Because manual removal of an impaction can be painful, the nurse may use, if the agency permits, 1 to 2 mL of
lidocaine (Xylocaine) gel on a gloved finger inserted into
the anal canal as far as the nurse can reach. The lidocaine
will anesthetize the anal canal and rectum and should be
inserted 5 minutes before the disimpaction.
Disimpacting the client requires great sensitivity and
a caring, yet matter-of-fact, approach. Be aware of personal facial expressions or anything that may convey
distaste or disgust to the client. When dealing with fecal
matter, many clients feel a sense of shame that relates to
childhood experiences that may have been traumatic in
some way. Control issues may also be triggered, and can
manifest in many ways. Confusion and negative feelings
are easily triggered in both client and nurse. Awareness
and an ability to discuss these issues with a client, when
appropriate, are important to providing appropriate care.
Self-awareness will help the nurse be more therapeutically
present to the client.
27/01/2021 18:03
Chapter 48
For digital removal of a fecal impaction:
1. If indicated, obtain assistance from a second individual who can comfort the client during the procedure.
2. Ask the client to assume a right or left side-lying
position, with the knees flexed and the back toward
the nurse. When the client lies on the right side, the
sigmoid colon is uppermost; thus, gravity can aid
removal of the feces. Positioning on the left side allows
easier access to the sigmoid colon.
3. Place a disposable absorbent pad under the client’s
buttocks and a bedpan nearby to receive stool.
4. Drape the client for comfort and to avoid unnecessary
exposure of the body.
5. Apply clean gloves and liberally lubricate the gloved
index finger.
6. Gently insert the index finger into the rectum and
move the finger along the length of the rectum.
7. Loosen and dislodge stool by gently massaging
around it. Break up stool by working the finger into
the hardened mass, taking care to avoid injury to the
mucosa of the rectum.
8. Carefully work stool downward to the end of the rectum and remove it in small pieces. Continue to remove
as much fecal material as possible. Periodically assess
the client for signs of fatigue, such as facial pallor, diaphoresis, or change in pulse rate. Manual stimulation
should be minimal.
9. Following disimpaction, assist the client to clean the
anal area and buttocks. Then assist the client onto a bedpan or commode for a short time because digital stimulation of the rectum often induces the urge to defecate.
Bowel Training Programs
For clients who have chronic constipation, frequent impactions, or fecal incontinence, bowel training programs may be
helpful. The program is based on factors within the client’s
control and is designed to help the client establish normal
defecation. Such matters as food and fluid intake, exercise,
and defecation habits are all considered. Before beginning
such a program, clients must understand it and want to be
involved. The major phases of the program are as follows:
•
•
•
Determine the client’s usual bowel habits and factors
that help and hinder normal defecation.
Design a plan with the client that includes the following:
a. Fluid intake of about 2500 to 3000 mL/day
b. Increase in fiber in the diet
c. Intake of hot drinks, especially just before the usual
defecation time
d. Increase in exercise.
Maintain the following daily routine for 2 to 3 weeks:
a. Administer a cathartic suppository (e.g., Dulcolax)
30 minutes before the client’s defecation time to
stimulate peristalsis.
b. When the client experiences the urge to defecate,
assist the client to the toilet or commode or onto a
bedpan. Note the length of time between the insertion of the suppository and the urge to defecate.
M48_BERM9793_11_GE_C48.indd 1289
•
•
●
Fecal Elimination
1289
c. Provide the client with privacy for defecation and
a time limit; 30 to 40 minutes is usually sufficient.
d. Teach the client to lean forward at the hips, to apply
pressure on the abdomen with the hands, and to
bear down for defecation. These measures increase
pressure on the colon. Straining should be avoided
because it can cause hemorrhoids.
Provide positive feedback when the client successfully
defecates. Refrain from negative feedback if the client
fails to defecate.
Offer encouragement to the client and convey that
patience is often required. Many clients require weeks
or months of training to achieve success.
Fecal Incontinence Pouch
To collect and contain large volumes of liquid feces, the nurse
may place a fecal incontinence collector pouch around the
anal area (Figure 48.8 ■). The purpose of the pouch is to prevent progressive perianal skin irritation and breakdown and
frequent linen changes necessitated by incontinence. In many
agencies, the pouch is replacing the traditional approach to
this problem; that is, inserting a large Foley catheter into the
client’s rectum and inflating the balloon to keep it in place—
a practice that may damage the rectal sphincter and rectal
mucosa. A rectal catheter also increases peristalsis and incontinence by stimulating sensory nerve fibers in the rectum.
A fecal collector is secured around the anal opening
and may or may not be attached to drainage. Pouches are
best applied before the perianal skin becomes excoriated.
If perianal skin excoriation is present, the nurse either (a)
applies a dimethicone-based moisture-barrier cream or
alcohol-free barrier film to the skin to protect it from feces
until it heals and then applies the pouch, or (b) applies a
skin barrier or hydrocolloid barrier underneath the pouch
to achieve the best possible seal.
Nursing responsibilities for clients with a rectal pouch
include (a) regular assessment and documentation of the
perianal skin status, (b) changing the bag every 72 hours
or sooner if there is leakage, (c) maintaining the drainage
Figure 48.8 ■ A drainable fecal collector pouch.
27/01/2021 18:03
1290
Unit 10
●
Promoting Physiologic Health
Pump
Balloon
reservoir
through the abdominal wall into the jejunum, an ileostomy
opens into the ileum (small bowel), and a colostomy opens
into the colon (large bowel). Gastrostomies and jejunostomies are generally performed to provide an alternate feeding route. The purpose of bowel ostomies is to divert and
drain fecal material. Bowel diversion ostomies are often
classified according to (a) their status as permanent or temporary, (b) their anatomic location, and (c) the construction
of the stoma, the opening created in the abdominal wall by
the ostomy. A stoma is generally red in color and moist. Initially, slight bleeding may occur when the stoma is touched
and this is considered normal. The client does not feel the
stoma because there are no nerve endings in the stoma.
Permanence
Figure 48.9 ■ Inflatable artificial sphincter.
system, and (d) providing explanations and support to the
client and support people.
Some clients (e.g., post-stroke, post-trauma, quadriplegia, or paraplegia) may be treated for fecal incontinence
with surgical repair of a damaged sphincter or an artificial
bowel sphincter. The artificial sphincter consists of three
parts: a cuff around the anal canal, a pressure-regulating
balloon, and a pump that inflates the cuff (Figure 48.9 ■).
The cuff is inflated to close the sphincter, maintaining continence. To have a bowel movement, the client deflates the
cuff. The cuff automatically reinflates in 10 minutes. Management of this device is usually specific to the device;
contact the manufacturing company for details.
Administering enemas and rectal medications may be
harmful with this device in place. Ensure safety of these
practices with the device instruction guide provided by
the device manufacturer.
Evaluating
The goals established during the planning phase are
evaluated according to specific desired outcomes, also
established in that phase. If outcomes are not achieved,
the nurse should explore the reasons. The nurse might
consider some or all of the following questions:
•
•
•
•
•
Were the client’s fluid intake and diet appropriate?
Was the client’s activity level appropriate?
Are prescribed medications or other factors affecting
the gastrointestinal function?
Do the client and family understand the provided instructions well enough to comply with the required therapy?
Were sufficient physical and emotional support provided?
Colostomies can be either temporary or permanent. Temporary colostomies are generally performed for traumatic
injuries or inflammatory conditions of the bowel. They
allow the distal diseased portion of the bowel to rest and
heal. Permanent colostomies are performed to provide
a means of elimination when the rectum or anus is nonfunctional as a result of a birth defect or a disease such as
cancer of the bowel.
Clinical Alert!
Surgery to reconnect the ends of the bowel of a temporary ostomy
may be called a take-down.
Anatomic Location
An ileostomy generally empties from the distal end of the
small intestine. A cecostomy empties from the cecum (the
first part of the ascending colon). An ascending colostomy
empties from the ascending colon, a transverse colostomy
from the transverse colon, a descending colostomy from
the descending colon, and a sigmoidostomy from the sigmoid colon (Figure 48.10 ■).
The location of the ostomy influences the character
and management of the fecal drainage. The farther along
the bowel, the more formed the stool (because the large
bowel reabsorbs water from the fecal mass) and the more
Transverse colostomy
Ascending colostomy
Descending colostomy
Ileostomy
Cecostomy
Bowel Diversion Ostomies
An ostomy is an opening for the gastrointestinal, urinary,
or respiratory tract onto the skin. There are many types of
intestinal ostomies. A gastrostomy is an opening through
the abdominal wall into the stomach. A jejunostomy opens
M48_BERM9793_11_GE_C48.indd 1290
Sigmoidostomy
Figure 48.10 ■ The locations of bowel diversion ostomies.
27/01/2021 18:03
Chapter 48
control over the frequency of stomal discharge can be
established. For example:
•
•
•
•
An ileostomy produces liquid fecal drainage. Drainage
is constant and cannot be regulated. Ileostomy drainage
contains some digestive enzymes, which are damaging to
the skin. For this reason, ileostomy clients must wear an
appliance continuously and take special precautions to
prevent skin breakdown. Compared to colostomies, however, odor is minimal because fewer bacteria are present.
An ascending colostomy is similar to an ileostomy in
that the drainage is liquid and cannot be regulated,
and digestive enzymes are present. Odor, however, is a
problem requiring control.
A transverse colostomy produces a malodorous, mushy
drainage because some of the liquid has been reabsorbed. There is usually no control.
A descending colostomy produces increasingly solid
fecal drainage. Stools from a sigmoidostomy are of normal or formed consistency, and the frequency of discharge can be regulated. Clients with a sigmoidostomy
may not have to wear an appliance at all times, and
odors can usually be controlled.
●
Fecal Elimination
1291
or by a piece of rubber tubing (Figure 48.12 ■). A loop
stoma has two openings: the proximal or afferent end,
which is active, and the distal or efferent end, which is
inactive. The loop colostomy is usually performed in an
emergency procedure and is often situated on the right
transverse colon. It is a bulky stoma that is more difficult
to manage than a single stoma.
The divided colostomy consists of two edges of bowel
brought out onto the abdomen but separated from each
other (Figure 48.13 ■). The opening from the digestive
or proximal end is the colostomy. The distal end in this
situation is often referred to as a mucous fistula, since this
section of bowel continues to secrete mucus. The divided
colostomy is often used in situations where spillage of
feces into the distal end of the bowel needs to be avoided.
The double-barreled colostomy resembles a doublebarreled shotgun (Figure 48.14 ■). In this type of colostomy, the proximal and distal loops of bowel are sutured
The length of time that an ostomy is in place also
helps to determine the consistency of the stool, particularly with transverse and descending colostomies. Over
time, the stool becomes more formed because the remaining functioning portions of the colon tend to compensate
by increasing water reabsorption.
Surgical Construction of the Stoma
Stoma constructions are described as single, loop, divided,
or double-barreled colostomies. The single stoma is created
when one end of bowel is brought out through an opening
onto the anterior abdominal wall. This is referred to as an end
or terminal colostomy; the stoma is permanent (Figure 48.11 ■).
In the loop colostomy, a loop of bowel is brought out
onto the abdominal wall and supported by a plastic bridge
Figure 48.12 ■ Loop colostomy.
Cory patrick Hartley RN. WCC, OMS.
Rectal stump
Figure 48.11 ■ End colostomy. The diseased portion of bowel is
removed and a rectal pouch remains.
M48_BERM9793_11_GE_C48.indd 1291
Figure 48.13 ■ Divided colostomy with two separated stomas.
27/01/2021 18:03
1292
Unit 10
●
Promoting Physiologic Health
Stoma and Skin Care
Figure 48.14 ■ Double-barreled colostomy.
together for about 10 cm (4 in.) and both ends are brought
up onto the abdominal wall.
Ostomy Management
Clients with fecal diversions need considerable psychologic
support, instruction, and physical care. This section is limited
to the nurse’s physical interventions of stoma assessment,
application of an appliance to collect feces and protect skin,
and promotion of self-care. Many agencies have access to
a wound ostomy continence nurse (WOCN) to assist these
clients. If possible, clients should meet with the WOCN prior
to the surgery to assist in marking the stoma site, also termed
siting. Burch (2018) states that “preoperative stoma siting is
likely to result in a well-placed stoma, in a position that best
suits the client’s lifestyle, resulting in fewer problems with
the appliance, including leakage, and a better quality of life
for the client” (p. S10). Additionally, national organizations
(e.g., United Ostomy Associations of America) have support
groups whose mission is to improve the quality of life of individuals who have, or will have, an ostomy. Members of local
chapters of such an organization have been known to meet
and visit with a client who has a new ostomy. It is common
for a client with a new ostomy to feel frightened and alone.
Talking with another individual who has gone through a
similar experience may help the client realize that he or she
is not alone and others are willing to listen and help.
Dietary Considerations
An ileostomy or colostomy usually begins functioning by
the 4th or 5th postoperative day. Clients with an ileostomy
or colostomy have few dietary restrictions. Nutritional
deficiencies, however, can result from ileostomies. In addition to poor absorption of vitamin B12, iron, magnesium,
fat, and folic acid, excess water and sodium can be lost
through the ileostomy’s liquid waste (Schreiber, 2016,
p. 129). Over time, the bowel can compensate for some of
the absorption losses, but it is important to monitor the
client and provide supplements as needed.
Stomal blockages can be avoided by informing clients to chew well and increase their hydration. The usual
changes in diet are focused on minimizing gas and odor.
Foods that produce gas include broccoli, cruciferous vegetables, carbonated liquids, and alcohol. Odor-producing
foods include onions, asparagus, cruciferous vegetables,
eggs, and fish. Foods that provide a natural deodorizer
include yogurt, parsley, and buttermilk (Hollister, 2017;
Schreiber, 2016, p. 129).
M48_BERM9793_11_GE_C48.indd 1292
Care of the stoma and skin is important for all clients who
have ostomies. The fecal material (effluent) from a colostomy or ileostomy is irritating to the peristomal skin, with
the resulting moisture-associated skin damage being the
most common cause of peristomal skin problems. This
is particularly true of stool from an ileostomy, which
contains digestive enzymes. In addition to pain and discomfort, the peristomal skin damage can cause difficulty
in obtaining an adequate seal from the appliance, which
causes the client embarrassment and stress from the leakage. It is important to assess the peristomal skin for irritation each time the appliance is changed. Any irritation
or skin breakdown needs to be treated immediately. The
skin is kept clean by washing off any excretion with water
and drying thoroughly. If soap is used, it should not contain cream or lotion that may leave a residue, which can
interfere with the skin barrier adhesive (Hollister, 2017).
Different materials can be used to treat and manage
moisture-associated skin damage. Metcalf (2018) suggests
the proactive approach of using the materials to anticipate
and manage the causes of skin damage to prevent peristomal skin breakdown from occurring in the first place.
Examples of materials include stoma powder, which
absorbs moisture and also creates a dry coating, increasing
adhesion of the stoma appliance. Protective films, available as wipes or spray, act as a barrier against the fecal
material and are applied prior to attaching the appliance.
Sealant pastes can be applied directly onto unbroken skin
or to the opening of the appliance to provide a better seal.
Because the paste can be difficult to remove, it should be
used primarily in the area(s) that have been assessed to be
at risk for potential leakage.
An ostomy appliance should protect the skin, collect
stool, and control odor. The appliance consists of a skin
barrier and a pouch. Some clients may prefer to also wear
an adjustable ostomy belt, which attaches to an ostomy
pouch to hold the pouch firmly in place (Figure 48.15 ■).
Skin barriers are important because they protect the
peristomal skin. They come in two shapes: flat or convex.
The flat barrier is used when the skin around the stoma is
smooth with no wrinkles, creases, folds, or gullies. A convex
ostomy skin barrier has some degree of protrusion (curved
or rounded shape) on the adhesive side, which can better
adapt to skin around the stoma that is not smooth (Hoeflok
& Purnell, 2017; Metcalf, 2018). In addition, skin barriers can
have either a cut-to-fit opening or a stretch-back opening to
accommodate the stoma. A stretch-back opening eliminates
Figure 48.15 ■ Adjustable ostomy belt.
27/01/2021 18:03
Chapter 48
the need to measure, cut, or rely on a pattern. No matter
how much or how little the opening is stretched, it conforms
snugly around the stoma (Zeigler & Min, 2017, p. 8).
Appliances can be one piece where the skin barrier
is already attached to the pouch (Figure 48.16A ■), or an
appliance can consist of two pieces: a separate pouch with
a flange and a separate skin barrier with a flange where the
pouch fastens to the barrier at the flange (Figure 48.16B).
The pouch can be removed without removing the skin
barrier when using a two-piece appliance. Pouches can be
closed or drainable (Figure 48.17 ■). A drainable pouch
usually has a clip where the end of the pouch is folded
over the clamp and clipped (Figure 48.18 ■). Newer drainable pouches have an integrated closure system instead
of a clamp. With the integrated closure system, the client
folds up the end of the pouch three times and presses
firmly to seal the pouch.
Drainable pouches are usually used by clients who
need to empty the pouch more than twice a day. Closed
pouches are often used by clients who have a regular
stoma discharge (e.g., sigmoid colostomy) and only have
to empty the pouch one or two times a day. Some clients
A
B
Figure 48.16 ■ A, A one-piece ostomy appliance or pouching system; B, a two-piece ostomy appliance or pouching system.
Shirlee Snyder.
●
Fecal Elimination
1293
Figure 48.18 ■ Applying a pouch clamp.
Shirlee Snyder.
find it easier to change a closed pouch than emptying a
drainable pouch, which requires some dexterity.
Odor control is essential to clients’ self-esteem. As soon
as clients are ambulatory, they can learn to work with the
ostomy in the bathroom to avoid odors at the bedside. Selecting the appropriate kind of appliance promotes odor control.
An intact appliance contains odors. Most pouches contain
odor-barrier material. Some pouches also have a pouch filter
that allows gas out of the pouch but not the odor.
The pouch should be changed on a routine basis,
before leakage occurs. The most common routine for
changing the appliance is every 2 to 3 days (Hollister,
2017). Some manufacturers recommend removing the
pouch and skin barrier twice a week to clean and inspect
the peristomal skin unless stool leaks onto the peristomal
skin, necessitating a change. If the skin is erythematous,
eroded, or ulcerated, the pouch should be changed every
24 to 48 hours to allow appropriate treatment of the skin.
More frequent changes are recommended if the client
complains of pain or discomfort.
The type of ostomy and amount of output influence
how often the pouch is emptied. The pouch is emptied
when it is one-third to one-half full of discharge or gas.
If the pouch overfills, it can cause separation of the skin
barrier from the skin and allow stool to come in contact
with the skin. This results in the entire appliance needing
to be removed and a new one applied.
QSEN
Patient-Centered Care Ostomy Care
When providing nursing care for the client with an ostomy,
the nurse should consider the following:
•
•
A
B
Figure 48.17 ■ A, A closed pouch; B, a drainable pouch.
M48_BERM9793_11_GE_C48.indd 1293
•
Provide the client with the names and phone numbers
of a WOCN, supply vendor, and other resource people
to contact when needed. Provide pertinent internet
resources for information and support.
Inform the client of signs to report to a healthcare provider (e.g., peristomal redness, skin breakdown, and
changes in stomal color).
Provide client and family education regarding care of
the ostomy and appliance when traveling.
27/01/2021 18:03
1294
•
•
Unit 10
●
Promoting Physiologic Health
Educate the client and family regarding infection control precautions, including proper disposal of used
pouches since these cannot be flushed down a toilet.
Younger clients may have special concerns about odor
and appearance. Provide information about community
support groups. A visit from someone who has had an
ostomy under similar circumstances may be helpful.
Skill 48.2 explains how to change a bowel diversion
ostomy appliance.
EVIDENCE-BASED PRACTICE
Evidence-Based Practice
Can Nursing Students Develop Empathy for Clients with an
Ostomy?
Approximately 750,000 people in the United States are living with
an ostomy. In addition to providing and teaching ostomy care,
nurses need to be able to empathize with their clients. Empathy
communicates appreciation and comprehension of the client’s
experience and is a major part of the therapeutic nurse–client relationship. Literature shows that empathy can be developed through
education. Hood, Haskins, and Roberson (2018) developed
and implemented an ostomy simulation for 30 first-year nursing
students enrolled in their second clinical course in an associate degree program within a university setting. The experience
included a guided reflection booklet for the students to record
their reflections before, during, and after the wearing of an ostomy
appliance. Participation in the study was voluntary.
The students were provided brief ostomy education about placement, purpose, and nursing care in the traditional classroom setting
in preparation for the following day. Students were told to complete
the preactivity reflection questions. On the following day, students
were assigned a partner and a “My Ostomy Story” card, which
presented a simulated client identity, including medical and social
history relevant to the client’s ostomy journey. During this laboratory
experience, students were asked to take on both a nurse and a client role. Using the “My Ostomy Story” card, students determined
the anatomical placement of the ostomy and fitted their partner with
an ostomy appliance. Students were informed to go about with their
usual routines with the appliance in place for 24 hours. They were
asked to complete the reflection-in-action portion of the reflection
booklet before returning the next day. The next morning the students were encouraged to create a simulated stool appropriate to
their ostomy and place the simulated stool in the ostomy bag. The
student pairs worked together to empty and remove the appliance
under faculty direction. Students were asked to complete the final
reflection-on-action and return the booklet the following day.
The researchers conducted an analysis of the student reflections, which resulted in the identification of three distinct themes.
“Encountering emotions” was the first theme. The students
expressed a range of emotions before beginning the project, with
apprehension and hesitation being the strongest. They considered the potential implications and inconvenience on their physical comfort and their social life. The impact on their body image
began before the ostomy bag was first applied. The second theme,
“becoming aware,” occurred as a result of the students placing,
wearing, and removing an ostomy appliance. The students became
aware of the physical challenges faced by their future clients. Again,
the students became aware of body image issues brought on by
wearing an ostomy bag. They also became mindful of the need for
their clients to be treated with dignity and respect. The third theme,
“impacting personal practice,” came about through the hands-on
experiences of placing and removing the bag with a student partner.
Students also recognized the need to provide clients with nonjudgmental, emotional support.
Implications
The analysis of the themes of the student reflections before, during, and after the ostomy experience demonstrated the ability of
students to become self-aware of their emotions. As the authors
stated, the experience of accepting another individual and helping
him or her feel understood is an important part of empathy. This
ostomy learning experience was an effective strategy that helped
nursing students identify with the feelings and reality of others as
well as acquire needed nursing skills. This study can provide helpful information for nurse educators to provide similar learning activities for students to learn about other types of client experiences.
SKILL 48.2
Changing a Bowel Diversion Ostomy Appliance
PURPOSES
• To assess and care for the peristomal skin
• To collect stool for assessment of the amount and type of output
• To minimize odors for the client’s comfort and self-esteem
ASSESSMENT
Determine the following:
• The type of ostomy and its placement on the abdomen. Surgeons often draw diagrams when there are two stomas. If there
is more than one stoma, it is important to confirm which is the
functioning stoma.
• The type and size of appliance currently used and the special
barrier substance applied to the skin, according to the nursing
care plan.
M48_BERM9793_11_GE_C48.indd 1294
Assess
• Stoma color: The stoma should appear red, similar in color to
the mucosal lining of the inner cheek, and slightly moist. Very
pale or darker-colored stomas with a dusky bluish or purplish
hue indicate impaired blood circulation to the area. Notify the
surgeon immediately.
• Stoma size and shape: Most stomas protrude slightly from
the abdomen. New stomas normally appear swollen, but
swelling generally decreases over 2 or 3 weeks or for as
27/01/2021 18:03
Chapter 48
●
Fecal Elimination
1295
Changing a Bowel Diversion Ostomy Appliance—continued
•
•
•
•
•
PLANNING
Review features of the appliance to ensure that all parts are present
and functioning correctly.
IMPLEMENTATION
Preparation
1. Determine the need for an appliance change.
• Assess the used appliance for leakage of stool. Rationale:
Stool can irritate the peristomal skin.
• Ask the client about any discomfort at or around the stoma.
Rationale: A burning sensation may indicate breakdown
beneath the faceplate of the pouch.
• Assess the fullness of the pouch. Rationale: The weight of
an overly full bag may loosen the skin barrier and separate
it from the skin, causing the stool to leak and irritate the
peristomal skin.
2. If there is pouch leakage or discomfort at or around the stoma,
change the appliance.
3. Select an appropriate time to change the appliance.
• Avoid times close to meal or visiting hours. Rationale: Ostomy
odor and stool may reduce appetite or embarrass the client.
• Avoid times immediately after meals or the administration
of any medications that may stimulate bowel evacuation.
Rationale: It is best to change the pouch when drainage is
least likely to occur.
• The best time to change a pouching system is first thing in
the morning when the bowel is least active (Hollister, 2017).
Performance
1. Prior to performing the procedure, introduce self and verify
the client’s identity using agency protocol. Explain to the client
what you are going to do, why it is necessary, and how to participate. Discuss how the results will be used in planning further
care or treatments. Changing an ostomy appliance should not
cause discomfort, but it may be distasteful to the client. Communicate acceptance and support to the client. It is important
to change the appliance competently and quickly. Include support people as appropriate.
2. Perform hand hygiene and observe other appropriate infection
prevention procedures.
3. Apply clean gloves.
4. Provide for client privacy preferably in the bathroom, where clients can learn to deal with the ostomy as they would at home.
5. Assist the client to a comfortable sitting or lying position in bed
or preferably a sitting or standing position in the bathroom.
Rationale: Lying or standing positions may facilitate smoother
pouch application, that is, avoid wrinkles.
6. Unfasten the belt if the client is wearing one.
Assignment
Care of a new ostomy is not assigned to AP. However, aspects of
ostomy function are observed during usual care and may be recorded
by a WOCN in addition to the unit nurse. Abnormal findings must be
validated and interpreted by the nurse. In some agencies, AP may be
assigned to remove and replace well-established ostomy appliances.
Equipment
• Clean gloves
• Bedpan
• Moisture-proof bag (for disposable pouches)
• Cleaning materials, including warm water, mild soap (optional),
washcloth, towel
• Tissue or gauze pad
• Skin barrier (optional)
• Stoma measuring guide
• Pen or pencil and scissors
• New ostomy pouch with optional belt
• Tail closure clamp
• Deodorant for pouch (optional)
SKILL 48.2
•
long as 6 weeks. Failure of swelling to recede may indicate a
problem, for example, blockage.
Stomal bleeding: Slight bleeding initially when the stoma is
touched is normal, but other bleeding should be reported.
Status of peristomal skin: Any redness and irritation of the peristomal skin—the 5 to 13 cm (2 to 5 in.) of skin surrounding the
stoma—should be noted. Temporary redness after removal of
adhesive is normal.
Amount and type of feces: Assess the amount, color, odor, and
consistency. Inspect for abnormalities, such as pus or blood.
Complaints: Complaints of burning sensation under the skin
barrier may indicate skin breakdown. The presence of abdominal discomfort or distention also needs to be determined.
Learning needs of the client and family members regarding the
ostomy and self-care.
The client’s emotional status, especially strategies used to cope
with the body image changes and the ostomy.
7. Empty the pouch and remove the ostomy skin barrier.
• Empty the contents of a drainable pouch through the bottom opening into a bedpan or toilet. Rationale: Emptying
before removing the pouch prevents spillage of stool onto
the client’s skin.
• If the pouch uses a clamp, do not throw it away because it
can be reused.
• Assess the consistency, color, and amount of stool.
• Peel the skin barrier off slowly, beginning at the top and
working downward, while holding the client’s skin taut.
Rationale: Holding the skin taut minimizes client discomfort
and prevents abrasion of the skin.
• Discard the disposable pouch in a moisture-proof bag.
8. Clean and dry the peristomal skin and stoma.
• Use toilet tissue to remove excess stool.
• Use warm water and a washcloth to clean the skin and
stoma. ❶ Check agency practice on the use of soap.
Rationale: Soap is sometimes not advised because it
can be irritating to the skin. If soap is allowed, do not use
deodorant or moisturizing soaps. Rationale: They may
interfere with the adhesives in the skin barrier.
• Dry the area thoroughly by patting with a towel. Rationale:
Excess rubbing can abrade the skin.
❶ Cleaning the skin.
Cory patrick Hartley RN. WCC, OMS.
Continued on page 1296
M48_BERM9793_11_GE_C48.indd 1295
27/01/2021 18:03
1296
Unit 10
●
Promoting Physiologic Health
SKILL 48.2
Changing a Bowel Diversion Ostomy Appliance—continued
❷ A guide for measuring the stoma.
Cory patrick Hartley RN. WCC, OMS.
❹ Centering the skin barrier over the stoma.
Cory patrick Hartley RN. WCC, OMS.
❺ Pressing the skin barrier of a disposable one-piece pouch for
30 seconds to activate the adhesives in the skin barrier.
❸ The nurse is making a stoma opening on a disposable one-piece pouch.
9. Assess the stoma and peristomal skin.
• Inspect the stoma for color, size, shape, and bleeding.
• Inspect the peristomal skin for any redness, ulceration, or irritation. Transient redness after the removal of adhesive is normal.
10. Place a piece of tissue or gauze over the stoma, and change
it as needed. Rationale: This absorbs any seepage from the
stoma while the ostomy appliance is being changed.
11. Prepare and apply the skin barrier (peristomal seal).
• Use the guide ❷ to measure the size of the stoma.
• On the backing of the skin barrier, trace a circle the same
size as the stomal opening.
• Cut out the traced stoma pattern to make an opening in
the skin barrier. ❸ Make the opening no more than 1/8 inch
(2–3 mm) larger than the stoma. Rationale: This allows
space for the stoma to expand slightly when functioning
and minimizes the risk of stool contacting peristomal skin.
• Remove the backing to expose the sticky adhesive side.
The backing can be saved and used as a pattern when
making an opening for future skin barriers.
M48_BERM9793_11_GE_C48.indd 1296
For a One-Piece Pouching System
Center the one-piece skin barrier and pouch over the stoma,
and gently press it onto the client’s skin for 30 seconds. ❹, ❺
Rationale: The heat and pressure help activate the adhesives in
the skin barrier.
For a Two-Piece Pouching System
• Center the skin barrier over the stoma and gently press it onto
the client’s skin for 30 seconds.
• Remove the tissue over the stoma before applying the pouch.
• Snap the pouch onto the flange or skin barrier wafer.
• For drainable pouches, close the pouch according to the manufacturer’s directions.
• Remove and discard gloves. Perform hand hygiene.
•
12. Document the procedure in the client record using forms or
checklists supplemented by narrative notes when appropriate. Record pertinent assessments and interventions. Report
any increase in stoma size, change in color indicative of
circulatory impairment, and presence of skin irritation or erosion. Record on the client’s chart discoloration of the stoma,
the appearance of the peristomal skin, the amount and type
of drainage, the client’s reaction to the procedure, the client’s
experience with the ostomy, and skills learned by the client.
27/01/2021 18:03
Chapter 48
●
Fecal Elimination
1297
Changing a Bowel Diversion Ostomy Appliance—continued
SAMPLE DOCUMENTATION
VARIATION: EMPTYING A DRAINABLE POUCH
• Empty the pouch when it is one-third to one-half full of stool or
gas. Rationale: Emptying before it is overfull helps avoid breaking the seal with the skin and stool then coming in contact with
the skin.
EVALUATION
Relate findings to previous data if available. Adjust the teaching
plan and nursing care plan as needed. Reinforce the teaching each time the care is performed. Encourage and support
self-care as soon as possible because clients should be able
to perform self-care by discharge. Rationale: Client learning is
facilitated by consistent nursing interventions.
•
Colostomy Irrigation
A colostomy irrigation (CI), similar to an enema, is a form
of stoma management used only for clients who have a
sigmoid or descending colostomy. The purpose of irrigation is to distend the bowel sufficiently to stimulate
peristalsis, which stimulates evacuation. CI has many
potential benefits. For example, CI makes the wearing of a
colostomy pouch unnecessary; decreases odor and flatus;
facilitates sleeping, eating, and traveling; and has been
shown to improve quality of life (Bauer, Arnold-Long, &
Kent, 2016, p. 69). Currently, colostomy irrigations are not
routinely taught to most clients; however, best evidence
indicates clients with a descending or sigmoid colostomy
should be given the option to learn CI (Bauer et al., 2016).
CI may be taught in the home or the ostomy clinic.
Routine irrigations (e.g., every 24 to 48 hours) for control of elimination is the client’s decision. Some clients prefer to control the time of elimination through rigid dietary
While wearing gloves, hold the pouch outlet over a bedpan or
toilet. Lift the lower edge up.
Unclamp or unseal the pouch.
Drain the pouch. Loosen feces from sides by moving fingers
down the pouch.
Clean the inside of the tail of the pouch with a tissue or a
premoistened towelette.
Apply the clamp or seal the pouch.
Dispose of used supplies.
Remove and discard gloves.
Perform hand hygiene.
Document the amount, consistency, and color of stool.
•
•
•
•
•
•
•
•
•
•
SKILL 48.2
8/3/2020 0900 Colostomy bag changed. Moderate to large amount
of semi-formed brown stool. Stoma reddish color. No redness or
irritation around stoma. Client looked at stoma today and started
asking questions as to how she will be able to change the pouch
when she is home. Asked if she would like to do the next changing
of the pouch. Stated “yes.” G. Hsu, RN
Perform detailed follow-up based on findings that deviated from
expected or normal for the client. Report significant deviations
from normal to the primary care provider.
regulation and not be bothered with CI, which can take up
30to 90 minutes to complete. When CI is chosen, it should
be done at the same time each day.
Bauer, Arnold-Long, and Kent (2016) explain the following process for CI: The client fills the irrigation bag
with usually 500 to 750 mL of lukewarm tap water. An
irrigation cone is attached to the irrigation tubing. After
priming the irrigation tubing, the client attaches the irrigation sleeve to the ostomy wafer or the client’s body.
The client lubricates the stoma cone and gently places it
into the stoma and opens the clamp on the tubing. After
the volume is infused, the cone is held in place for about
5 minutes or when cramping begins. The cone is removed
and the client waits for the initial return of the irrigation
fluid and stool. A secondary return of fluid and stool
occurs and can take 30 to 90 minutes to complete. After
stool evacuation is complete, the pouch is replaced or the
stoma is covered.
NURSING CARE PLAN Altered Bowel Elimination
ASSESSMENT DATA
NURSING DIAGNOSIS
DESIRED OUTCOMES
NURSING ASSESSMENT
Mrs. Emma Brown is a 78-year-old widow of 9 months. She lives
alone in a low-income housing complex for older adults. Her two children live with their families in a city approximately 150 miles away. She
has always enjoyed cooking for her family; however, now that she is
alone, she does not cook for herself. As a result, she has developed
irregular eating patterns and tends to prepare soup-and-toast meals.
She gets little exercise and has had bouts of insomnia since her
husband’s death. For the past month, Mrs. Brown has been having
a problem with constipation. She states she has a bowel movement
about every 3 to 4 days and her stools are hard and painful to excrete.
Mrs. Brown decides to attend the health fair sponsored by the housing
complex and seeks assistance from the county public health nurse.
Constipation related to low-fiber
diet and inactivity (as evidenced
by infrequent, hard stools; painful
defecation; abdominal distention)
Bowel Elimination [0501], not
compromised as evidenced by:
• Ease of stool passage
• Stool soft and formed
• Passage of stool without aids
Continued on page 1298
M48_BERM9793_11_GE_C48.indd 1297
27/01/2021 18:03
1298
Unit 10
●
Promoting Physiologic Health
NURSING CARE PLAN Altered Bowel Elimination—continued
Physical Examination
Diagnostic Data
Height: 162 cm (5′4″)
Weight: 65 kg (143 lb)
Temperature: 36.2°C (97.2°F)
Pulse: 82 beats/min
Respirations: 20/min
Blood pressure: 128/74 mmHg
Active bowel sounds, abdomen
slightly distended
CBC: Hgb 10.8
Urinalysis negative
NURSING INTERVENTIONS*/SELECTED ACTIVITIES
RATIONALE
CONSTIPATION/IMPACTION MANAGEMENT [0450]
Identify factors (e.g., medications, bedrest, diet) that may cause or
contribute to constipation.
Assessing causative factors is an essential first step in teaching and
planning for improved bowel elimination.
Encourage increased fluid intake, unless contraindicated.
Sufficient fluid intake is necessary for the bowel to absorb sufficient
amounts of liquid to promote proper stool consistency.
Evaluate medication profile for gastrointestinal side effects.
Constipation is a common side effect of many drugs including narcotics and antacids.
Teach Mrs. Brown how to keep a food diary.
An appraisal of food intake will help identify if Mrs. Brown is eating a
well-balanced diet and consuming adequate amounts of fluid and fiber.
Excessive meat or refined food intake will produce small, hard stools.
Instruct Mrs. Brown on a high-fiber diet, as appropriate.
Fiber absorbs water, which adds bulk and softness to the stool and
speeds up passage through the intestines.
Instruct her on the relationship of diet, exercise, and fluid intake to
constipation and impaction.
Fiber without adequate fluid can aggravate, not facilitate, bowel
function.
Exercise Promotion [0200]
Encourage verbalization of feelings about exercise or need for
exercise.
Perceptions of the need for exercise may be influenced by misconceptions, cultural and social beliefs, fears, or age.
Determine Mrs. Brown’s motivation to begin or continue an exercise
program.
Individuals who have been successful in an exercise program can
assist Mrs. Brown by providing incentive and enhancing motivation.
For example, a walking partner may be beneficial.
Inform Mrs. Brown about the health benefits and physiologic effects
of exercise.
Activity influences bowel elimination by improving muscle tone and
stimulating peristalsis.
Instruct her about appropriate types of exercise for her level of
health, in collaboration with a primary care provider.
Any individual beginning an exercise program should consult a primary
care provider primarily for a cardiac evaluation. Mrs. Brown’s age and
lack of activity should be considered in planning the level of activity.
Assist Mrs. Brown to set short-term and long-term goals for the
exercise program.
Realistic goal setting provides direction and motivation.
Evaluation
Outcome not met. Mrs. Brown has kept a food diary and is able to identify the need for more fluid and fiber, but has not consistently
included fiber in her diet. She has started a walking program with a neighbor but is only able to walk for 10 minutes at a time twice a week.
She states her last bowel movement was 3 days ago.
*The NOC # for desired outcomes and the NIC # for nursing interventions are listed in brackets following the appropriate outcome or intervention. Outcomes, interventions, and activities selected
are only a sample of those suggested by NOC and NIC and should be further individualized for each client.
APPLYING CRITICAL THINKING
1. You learn that Mrs. Brown’s stools have been liquid, in very small amounts, and at infrequent intervals, generally occurring when she
feels the urge to defecate. What additional data are important to obtain from her?
2. What nursing intervention is most appropriate before making suggestions to correct or prevent the problem she is experiencing?
3. What suggestions can you give her about maintaining a regular bowel pattern?
4. Explain why cathartics and laxatives are generally contraindicated for individuals in Mrs. Brown’s situation.
Answers to Applying Critical Thinking questions are available on the faculty resources site. Please consult with your instructor.
M48_BERM9793_11_GE_C48.indd 1298
27/01/2021 18:03
Chapter 48
●
Fecal Elimination
1299
CONCEPT MAP
Altered Bowel Elimination
outcome
M48_BERM9793_11_GE_C48.indd 1299
Outcome not met
27/01/2021 18:03
1300
Unit 10
●
Promoting Physiologic Health
Chapter 48 Review
CHAPTER HIGHLIGHTS
• Primary functions of the large intestine are the absorption of water
• A function of the nurse is to assist clients with diet and bowel prep-
and nutrients, the mucoid protection of the intestinal wall, and fecal
elimination.
Patterns of fecal elimination vary greatly among individuals, but a
regular pattern of fecal elimination with formed, soft stools is essential to health and a sense of well-being.
Various factors affect defecation: developmental level, diet, fluid
intake, activity and exercise, psychologic factors, defecation habits, medications, diagnostic and medical procedures, pathologic
conditions, and pain.
Common fecal elimination problems include constipation, diarrhea,
bowel incontinence, and flatulence. Each has specific defining characteristics and contributing causes that often relate to or are identical to the factors that affect defecation.
Lack of exercise, irregular defecation habits, and overuse of laxatives are all thought to contribute to constipation. Sufficient fluid and
fiber intake are required to keep feces soft.
An adverse effect of constipation is straining during defecation, during which the Valsalva maneuver may be used. Cardiac problems
may ensue.
An adverse effect of prolonged diarrhea is fluid and electrolyte
imbalance.
Assessment relative to fecal elimination includes a nursing history;
physical examination of the abdomen, rectum, and anus; and in
some situations, visualization studies and inspection and analysis
of stool for abnormal constituents such as blood.
A nursing history includes data about the client’s defecating pattern,
description of feces and any changes, problems associated with elimination, and data about possible factors altering bowel elimination.
When inspecting the client’s stool, the nurse must observe its color,
consistency, shape, amount, and odor, and the presence of abnormal constituents.
aration before endoscopic and radiographic studies of the large
intestine.
Nursing diagnoses that relate specifically to altered bowel elimination can include bowel incontinence. However, because altered
elimination patterns affect several areas of human functioning, diagnoses such as potential for decreased fluid volume, potential for
altered electrolytes, potential for developing altered skin integrity,
impaired self-esteem, and lack of knowledge may also apply.
Normal defecation is often facilitated in both well and ill clients by
providing privacy, teaching clients to attend to defecation urges
promptly, assisting clients to normal sitting positions whenever possible, encouraging appropriate food and fluid intake, and scheduling regular exercise.
Nursing strategies include administering cathartics and antidiarrheals; administering cleansing, carminative, retention, or return-flow
enemas; applying protective skin agents; monitoring fluid and electrolyte balance; and instructing clients in ways to promote normal
defecation.
The purpose of an enema is to increase peristalsis and the excretion of feces and flatus. Enemas are classified into groups: cleansing, retention, and distention reduction, which includes carminative
and return-flow enemas.
Digital removal of an impaction should be carried out gently because
of vagal nerve stimulation and subsequent depressed cardiac rate.
A primary care provider’s order is often necessary.
Clients who have bowel diversion ostomies require special care,
with attention to psychologic adjustment, diet, and stoma and skin
care. A variety of stoma management methods is available to these
clients, depending on the type and position of the ostomy.
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
TEST YOUR KNOWLEDGE
1. A client asks an RN why it is more difficult to use a bedpan than a
toilet for defecating. Which of the following is the best response?
1. The sitting position decreases the contractions of the muscles of the pelvic floor.
2. The sitting position increases the downward pressure on the
rectum, making it easier to pass stool.
3. The sitting position increases the pressure within the abdomen.
4. The sitting position inhibits the urge to urinate, allowing one
to defecate.
2. An older client tells a nurse that in order to achieve a daily bowel
movement, the client uses laxatives most days of the week.
What should the nurse tell this client? Select all that apply.
1. Normal patterns of elimination are different for everyone.
2. Increase fiber intake to 20–35 grams a day.
3. Engage in enjoyable exercise.
4. Ignore the urge to have a bowel movement.
5. Have 6–8 glasses of fluid daily.
M48_BERM9793_11_GE_C48.indd 1300
3. A client has received an oil retention enema. What time frame
should the nurse provide the client for the enema to take effect?
1. 1–3 hours
2. 10–20 minutes
3. 5–10 minutes
4. 10–15 minutes
4. The nurse is most likely to report which finding to the primary
care provider for a client who has an established colostomy?
1. The stoma extends 1/2 in. above the abdomen.
2. The skin under the appliance looks red briefly after removing
the appliance.
3. The stoma color is a deep red-purple.
4. The ascending colostomy delivers liquid feces.
27/01/2021 18:03
Chapter 48
5. Which goal is the most appropriate for clients with diarrhea
related to ingestion of an antibiotic for an upper respiratory
infection?
1. The client will wear a medical alert bracelet for antibiotic
allergy.
2. The client will return to his or her previous fecal elimination
pattern.
3. The client will verbalize the need to take an antidiarrheal
medication prn.
4. The client will increase intake of insoluble fiber such as
grains, rice, and cereals.
6. A client with a new stoma who has not had a bowel movement
since surgery last week reports feeling nauseous. What is the
appropriate nursing action?
1. Prepare to irrigate the colostomy.
2. After assessing the stoma and surrounding skin, notify the
surgeon.
3. Assess bowel sounds and administer antiemetic.
4. Administer a bulk-forming laxative, and encourage increased
fluids and exercise.
7. The nurse assesses a client’s abdomen several days after
abdominal surgery. It is firm, distended, and painful to palpate.
The client reports feeling “bloated.” The nurse consults with the
surgeon, who orders an enema. The nurse prepares to give
what kind of enema?
1. Soapsuds
2. Retention
3. Return flow
4. Oil retention
●
Fecal Elimination
1301
8. Which of the following is most likely to validate that a client is
experiencing intestinal bleeding?
1. Large quantities of fat mixed with pale yellow liquid stool
2. Brown, formed stools
3. Semisoft black-colored stools
4. Narrow, pencil-shaped stool
9. Which nursing diagnoses is/are most applicable to a client with
fecal incontinence? Select all that apply.
1. Bowel incontinence
2. Potential for decreased fluid volume
3. Altered body image
4. Social seclusion
5. Potential for developing altered skin integrity
10. A student nurse is assigned to care for a client with a sigmoidostomy. The student will assess which ostomy site?
3
2
4
1
5
See Answers to Test Your Knowledge in Appendix A.
READINGS AND REFERENCES
Suggested Readings
References
Hoeflok, J., & Purnell, P. (2017). Understanding the role of
convex skin barriers in ostomy care. Nursing, 47(9), 51–56.
doi:10.1097/01.NURSE.0000516224.24273.88
This article reviews the advantages of convex skin barriers
and their role in ostomy care.
Metcalf, C. (2018). Managing moisture-associated skin damage in stoma care. British Journal of Nursing, 27(22),
S6–S14. doi:10.12968/bjon.2018.27.22.S6
This article provides helpful information about the different types of appliances and accessories that can
be used to treat moisture-associated skin damage in
stoma care.
American Cancer Society. (2017). Colorectal cancer facts &
figures 2017–2019. Retrieved from https://www.cancer
.org/content/dam/cancer-org/research/cancer-facts-andstatistics/colorectal-cancer-facts-and-figures/colorectalcancer-facts-and-figures-2017-2019.pdf
American Cancer Society. (2018). Colorectal cancer risk
factors. Retrieved from https://www.cancer.org/cancer/
colon-rectal-cancer/causes-risks-prevention/riskfactors.html
Ball, J. W., Bindler, R., Cowen, K., & Shaw, M. (2017).
Principles of pediatric nursing (7th ed.). Hoboken, NJ:
Pearson.
Bauer, C., Arnold-Long, M., & Kent, D. J. (2016). Colostomy irrigation to maintain continence: An old method
revived. Nursing, 46(8), 59–62. doi:10.1097/01.
NURSE.0000484963.00982.b5
Burch, J. (2018). Research and expert opinion on siting a stoma: A review of the literature. British
Journal of Nursing, 27(16), S4–S12. doi:10.12968/
bjon.2018.27.16.S4
Fremgen, B. F., & Frucht, S. S. (2016). Medical terminology
(6th ed.). Hoboken, NJ: Pearson.
Gordon, J., Fischer-Cartlidge, E., & Barton-Burke, M. (2017).
The big 3: An updated overview of colorectal, breast, and
prostate cancers. Nursing Clinics of North America, 52,
27–52. doi:10.1016/j.cnur.2016.11.004
Gump, K., & Schmelzer, M. (2016). Gaining control over fecal
incontinence. MEDSURG Nursing, 25(2), 97–102.
Hollister. (2017). Understanding your colostomy. Retrieved
from http://www.hollister.com/~/media/files/pdfs%E2%80
Related Research
Cutting, K. (2016). Comparing ostomates’ perceptions of
hydrocolloid and silicone seals: A survey. British Journal of
Nursing, 25(22), S24–S29. doi:10.12968/bjon.2016.25.22.
S30
Oliver, J. S., Ewell, P., Nicholls, K., Chapman, K., & Ford, S.
(2016). Differences in colorectal cancer risk knowledge among Alabamians: Screening implications.
Oncology Nursing Forum, 43(1), 77–85. doi:10.1188/16.
ONF.77-85
Saraiva de Aguiar, F. A., Pinheiro de Jesus, B., Cardoso Rocha, F., Barbosa Cruz, I., de Andrade
Neto, G. R., Meira Rios, B. R., . . . Batista Andrade,
D. L. (2019). Colostomy and self-care: Meanings
for ostomized patients. Journal of Nursing UFPE
Online, 13(1), 105–110. doi:10.5205/1981-8963v13i01a236771p105-110-2019
M48_BERM9793_11_GE_C48.indd 1301
%93for%E2%80%93download/ostomy%E2%80%93care/
understanding%E2%80%93your%E2%80%93colost
omy_923054-0917.pdf
Hood, D. G., Haskins, T. L., & Roberson, S. C. (2018).
Stepping into their shoes: The ostomy experience. Journal of Nursing Education, 57(4), 233–236.
doi:10.3928/01484834-20180322-08
Mayo Clinic. (2018). Dietary fiber: Essential for a healthy
diet. Retrieved from http://www.mayoclinic.org/healthylifestyle/nutrition-and-healthy-eating/in-depth/fiber/
art-20043983
Moorhead, S., Swanson, E., Johnson, M., & Maas, M. L.
(Eds.). (2018). Nursing outcomes classification (NOC)
(6th ed.). St. Louis, MO: Elsevier.
Sams, A. W., & Kennedy-Malone, L. (2017). Recognition
and management of Clostridium difficile in older adults.
The Nurse Practitioner, 42(5), 50–55. doi:10.1097/01.
NPR.0000512254.47992.8e
Schreiber, M. L. (2016). Evidence-based practice. Ostomies:
Nursing care and management. MEDSURG Nursing, 25(2),
127–130.
Smith, S., & Taylor, J. (2016). Best practices in caring for
patients infected with Clostridium difficile. Critical Care
Nurse, 36(3), 71–72. doi:10.4037/ccn2016696
Zeigler, M. H., & Min, A. (2017). Ostomy management: Nuts
and bolts for every nurse’s toolbox. American Nurse Today,
12(9), 6–11.
27/01/2021 18:03
1302
Unit 10
●
Promoting Physiologic Health
Selected Bibliography
Burch, J. (2016). Making maintaining dignity a top priority:
Caring for older people with a stoma in the community.
British Journal of Community Nursing, 21(6), 280–282.
doi:10.12968/bjcn.2016.21.6.280
Burch, J. (2017). Stoma care: An update on current
guidelines for community nurses. British Journal of
M48_BERM9793_11_GE_C48.indd 1302
Community Nursing, 22(4), 162–166. doi:10.12968/
bjcn.2017.22.4.162
Peate, I. (2016). How to perform digital removal of faeces. Nursing Standard, 30(40), 36–39. doi:10.7748/
ns.30.40.36.s43
Perrin, A. (2016). Convex stoma appliances: An audit of stoma
care nurses. British Journal of Nursing, 25(22), S10–S15.
doi:10.12968/bjon.2016.25.22.S10
Walls, P. (2018). Seeking a consensus for a glossary of terms
for peristomal skin complications. Journal of Stomal
Therapy Australia, 38(4), 8–12.
Williams, J. (2017). The importance of choosing the correct
stoma appliance to meet patient needs. British Journal
of Community Nursing, 22(2), 58–60. doi:10.12968/
bjcn.2017.22.2.58
27/01/2021 18:03
Oxygenation
49
LEA R N IN G OU TC OME S
After completing this chapter, you will be able to:
1. Outline the structure and function of the respiratory system.
2. Describe the processes of breathing (ventilation) and gas
exchange (respiration).
3. Explain the role and function of the respiratory system in transporting oxygen and carbon dioxide to and from body tissues.
4. Describe the mechanisms for respiratory regulation.
5. Identify factors influencing respiratory function.
6. Identify four major types of conditions that can alter respiratory function.
7. Describe nursing assessments for oxygenation status.
8. Describe nursing measures to promote respiratory function
and oxygenation.
9. Explain the use of therapeutic measures such as medications,
inhalation therapy, oxygen therapy, artificial airways, airway
suctioning, and chest tubes to promote respiratory function.
10. State outcome criteria for evaluating client responses to
measures that promote adequate oxygenation.
11. Verbalize the steps used in:
a. Administering oxygen by cannula, face mask, or face tent
b. Oropharyngeal, nasopharyngeal, and nasotracheal
suctioning
c. Suctioning a tracheostomy or endotracheal tube
d. Providing tracheostomy care.
12. Recognize when it is appropriate to assign aspects of oxygen therapy, suctioning, and tracheostomy care to assistive
personnel.
13. Demonstrate appropriate documentation and reporting of
oxygen therapy, suctioning, and tracheostomy care.
K EY T E RMS
adventitious breath sounds, 1309
apnea, 1309
atelectasis, 1305
bradypnea, 1309
cyanosis, 1309
diffusion, 1307
dyspnea, 1309
emphysema, 1307
erythrocytes, 1307
eupnea, 1309
expectorate, 1314
hematocrit, 1307
hemoglobin, 1307
hemothorax, 1341
humidifiers, 1315
hypercapnia, 1309
hypercarbia, 1309
hyperinflation, 1333
hyperoxygenation, 1333
hyperventilation, 1333
hypoxemia, 1309
hypoxia, 1309
Introduction
Oxygen, a clear, odorless gas that constitutes approximately 21% of the air we breathe, is necessary for proper
functioning of all living cells. The absence of oxygen
can lead to cellular, tissue, and organism death. Cellular
metabolism produces carbon dioxide, which must be eliminated from the body to maintain normal acid–base balance. Delivery of oxygen and removal of carbon dioxide
require the integration of several systems including the
hematologic, cardiovascular, and respiratory systems. The
respiratory system provides the movement and transfer of
gases between the atmosphere and the blood. Impaired
function of the system can significantly affect our ability
to breathe, transport gases, and participate in everyday
activities.
lung compliance, 1305
lung recoil, 1305
mucus clearance device (MCD),
1317
noninvasive positive pressure
ventilation (NPPV), 1324
orthopnea, 1309
oxyhemoglobin, 1307
pleural effusion, 1341
pneumothorax, 1341
postural drainage, 1317
respiratory membrane, 1305
sputum, 1309
stridor, 1309
suctioning, 1329
surfactant, 1305
tachypnea, 1309
tidal volume, 1305
vibration, 1317
Respiration is the process of gas exchange between
the individual and the environment and involves four
components:
1. Ventilation or breathing, the movement of air in and
out of the lungs as we inhale and exhale
2. Alveolar-capillary gas exchange, which involves
the diffusion of oxygen and carbon dioxide between the
alveoli and the pulmonary capillaries
3. Transport of oxygen and carbon dioxide between
the tissues and the lungs
4. Movement of oxygen and carbon dioxide between
the systemic capillaries and the tissues.
1303
M49_BERM9793_11_GE_C49.indd 1303
27/01/2021 18:05
1304
Unit 10
●
Promoting Physiologic Health
Structure and Processes of
the Respiratory System
The structure of the respiratory system facilitates gas
exchange and protects the body from foreign matter such
as particulates and pathogens. The four processes of the
respiratory system include pulmonary ventilation, alveolar gas exchange, transport of oxygen and carbon dioxide,
and systemic diffusion.
Structure of the Respiratory System
The respiratory system (Figure 49.1 ■) is divided structurally into the upper respiratory system and the lower
respiratory system. The mouth, nose, pharynx, and larynx
compose the upper respiratory system. The lower respiratory system includes the trachea and lungs, with the bronchi, bronchioles, alveoli, pulmonary capillary network,
and pleural membranes.
Air enters through the nose, where it is warmed,
humidified, and filtered. Hairs at the entrance of the
nares trap large particles in the air, and smaller particles
are filtered and trapped as air changes direction on contact
with the nasal turbinates and septum. Irritants in the nasal
passages initiate the sneeze reflex. A large volume of air
rapidly exits through the nose and mouth during a sneeze,
helping to clear nasal passages.
Inspired air passes from the nose through the pharynx. The pharynx is a shared pathway for air and food. It
includes both the nasopharynx and the oropharynx, which
are richly supplied with lymphoid tissue that traps and
destroys pathogens entering with the air.
The larynx is important for maintaining airway
patency and protecting the lower airways from swallowed
food and fluids. During swallowing, the inlet to the larynx
(the epiglottis) closes, routing food to the esophagus. The
epiglottis is open during breathing, allowing air to move
freely into the lower airways. Below the larynx, the trachea
Nasopharynx
Nasal cavity
Oropharynx
Laryngeal pharynx
Epiglottis
Larynx
Right lung
Esophagus
Right
bronchus
Trachea
Left lung
Left bronchus
Mediastinum
Terminal
bronchiole
Terminal
bronchiole
Respiratory
bronchioles
Diaphragm
Pleura
A
Alveolar
duct
Alveoli
B
Figure 49.1 ■ A, Organs of the respiratory tract; B, respiratory bronchioles, alveolar ducts, and alveoli.
M49_BERM9793_11_GE_C49.indd 1304
27/01/2021 18:05
Chapter 49
leads to the right and left main bronchi (primary bronchi)
and the other conducting airways of the lungs. Within the
lungs, the primary bronchi divide repeatedly into smaller
and smaller bronchi, ending with the terminal bronchioles. Together these airways are known as the bronchial
tree. The trachea and bronchi are lined with mucosal epithelium. These cells produce a thin layer of mucus, the
“mucous blanket,” that traps pathogens and microscopic
particulate matter. These foreign particles are then swept
upward toward the larynx and throat by cilia, tiny hairlike
projections on the epithelial cells. The cough reflex is triggered by irritants in the larynx, trachea, or bronchi.
After air passes through the trachea and bronchi, it
enters the respiratory bronchioles and alveoli where all gas
exchange occurs. This gas exchange or respiratory zone of
the lungs includes the respiratory bronchioles (which have
scattered air sacs in their walls), the alveolar ducts, and
the alveoli (see Figure 49.1). Alveoli have very thin walls,
composed of a single layer of epithelial cells covered by
a thick mesh of pulmonary capillaries. The alveolar and
capillary walls form the respiratory membrane (also known
as the alveolar–capillary membrane), where gas exchange
occurs between the air on the alveolar side and the blood
on the capillary side. The airways move air to and from
the alveoli; the right ventricle and pulmonary vascular
system transport blood to the capillary side of the membrane. For example, deoxygenated blood leaves the right
heart through the pulmonary artery and enters the lungs
and capillaries. Oxygenated blood returns via capillaries to
the pulmonary vein to the heart (Figure 49.2 ■). The thin,
highly permeable membrane of the respiratory membrane
(estimated to be not more than 0.0004 mm thick) is essential
to normal gas exchange. Thus, fluid or other materials in
the alveoli interfere with the respiratory process.
The outer surface of the lungs is covered by a thin,
double layer of tissue known as the pleura. The parietal
pleura lines the thorax and surface of the diaphragm. It
doubles back to form the visceral pleura, covering the
Inspired air
Expired air
Pulmonary
vein
Pulmonary
artery
From heart
and systemic
circulation
Alveoli
(lungs)
To heart and
systemic
circulation
CO2
O2
Tissues
Figure 49.2 ■ Gas exchange occurs between the air on the alveolar
side and the blood on the capillary side.
M49_BERM9793_11_GE_C49.indd 1305
●
Oxygenation
1305
external surface of the lungs. Between these pleural layers
is a potential space that contains a small amount of pleural fluid, a serous lubricating solution. This fluid prevents
friction during the movements of breathing and serves
to keep the layers adherent through its surface tension.
Pulmonary Ventilation
The first process of the respiratory system, ventilation of
the lungs, is accomplished through the act of breathing:
inspiration (inhalation) as air flows into the lungs, and
expiration (exhalation) as air moves out of the lungs. Adequate ventilation depends on several factors:
•
•
•
•
Clear airways
An intact central nervous system (CNS) and respiratory
center (medulla and pons in the brainstem)
An intact thoracic cavity capable of expanding and
contracting
Adequate pulmonary compliance and recoil.
A number of mechanisms, including ciliary action and
the cough reflex, work to keep airways open and clear.
In some cases, however, these defenses may be overwhelmed. The inflammation, edema, and excess mucous
production that occur with some types of pneumonia may
clog small airways, impairing ventilation of distal alveoli.
The degree of chest expansion during normal breathing is minimal, requiring little energy expenditure. In
adults, approximately 500 mL of air is inspired and
expired with each breath. This is known as tidal volume.
Breathing during strenuous exercise or some types of
heart disease requires greater chest expansion and effort.
At this time, more than 1500 mL of air may be moved with
each breath. Accessory muscles of respiration, including
the anterior neck muscles, intercostal muscles, and muscles of the abdomen, are used. Active use of these muscles
and noticeable effort in breathing are seen in clients with
obstructive pulmonary disease.
Lung compliance, the expansibility or stretchability of
lung tissue, plays a significant role in the ease of ventilation. At birth, the fluid-filled lungs are stiff and resistant
to expansion, much as a new balloon is difficult to inflate.
With each subsequent breath, the alveoli become more
compliant and easier to inflate, just as a balloon becomes
easier to inflate after several tries. Lung compliance tends
to decrease with aging, making it more difficult to expand
alveoli and increasing the risk for atelectasis, or collapse
of a portion of the lung.
In contrast to lung compliance is lung recoil, the continual tendency of the lungs to collapse away from the
chest wall. Just as lung compliance is necessary for normal
inspiration, lung recoil is necessary for normal expiration.
The surface tension of fluid lining the alveoli has the greatest effect on recoil. Surfactant, a lipoprotein produced by
specialized alveolar cells, reduces the surface tension of
alveolar fluid. Without surfactant, lung expansion is exceedingly difficult and the lungs collapse. Premature infants
whose lungs are not yet capable of producing adequate
surfactant often develop respiratory distress syndrome.
27/01/2021 18:05
1306
Unit 10
●
Promoting Physiologic Health
ANATOMY & PHYSIOLOGY REVIEW
The Respiratory System
Larynx
Trachea
Right lung
Left lung
Right upper
lobe (RUL)
Left bronchus
Right
bronchus
Left upper
lobe (LUL)
Right
middle
lobe
(RML)
Indentation
for the
normal
placement
of the
heart
Left lower
lobe (LLL)
Right
lower
lobe
(RLL)
Alveolar sacs
Pulmonary vein
Pulmonary artery
Capillaries
Alveolus
The larynx, trachea, bronchi, and lungs with an expanded view showing the structures of an alveolus and the pulmonary blood vessels.
JANE RICE, MEDICAL TERMINOLOGY FOR HEALTH CARE PROFESSIONALS, 9th Ed.,©2018. Reprinted and Electronically reproduced by permission of Pearson Education, Inc., New York, NY.
QUESTIONS
1. Pneumonia occurs when microorganisms get into the
lower respiratory tract and overwhelm the body’s
defenses. Name at least two normal defense mechanisms present in the upper airway that help prevent
microorganisms getting into the lower respiratory tract.
2. Microorganisms can travel past the upper respiratory
tract defense mechanisms. What defense mechanisms
M49_BERM9793_11_GE_C49.indd 1306
are present in the lower respiratory tract that may help
the client?
3. The microorganisms have quickly multiplied and
overpowered the client’s defense mechanisms. The
client has pneumonia and the alveoli are filled with
infectious fluid. How will this affect gas exchange at
the respiratory or alveolar–capillary membrane?
Answers to Anatomy & Physiology Review questions are available on the faculty resources
site. Please consult with your instructor.
27/01/2021 18:05
Chapter 49
Alveolar Gas Exchange
After the alveoli are ventilated, the second phase of the
respiratory process—the diffusion of oxygen from the
alveoli and into the pulmonary blood vessels—begins.
Diffusion is the movement of gases or other particles from
an area of greater pressure or concentration to an area of
lower pressure or concentration. Pressure differences in
the gases on each side of the respiratory membrane affect
diffusion. Carbon dioxide diffuses from the blood into the
alveoli, where it can be eliminated with expired air.
Transport of Oxygen and
Carbon Dioxide
The third part of the respiratory process involves the transport of respiratory gases. Oxygen needs to be transported
from the lungs to the tissues, and carbon dioxide must be
transported from the tissues back to the lungs. Normally
most of the oxygen (97%) combines loosely with hemoglobin
(oxygen-carrying red pigment) in the red blood cells
(RBCs) and is carried to the tissues as oxyhemoglobin (the
compound of oxygen and hemoglobin).
Several factors affect the rate of oxygen transport from
the lungs to the tissues:
1. Cardiac output
2. Number of erythrocytes and blood hematocrit
3. Exercise.
Any pathologic condition that decreases cardiac
output (e.g., damage to the heart muscle, blood loss, or
pooling of blood in the peripheral blood vessels) diminishes the amount of oxygen delivered to the tissues. The
heart compensates for inadequate output by increasing
its pumping rate or heart rate; however, with severe damage or blood loss, this compensatory mechanism may not
restore adequate blood flow and oxygen to the tissues.
The second factor influencing oxygen transport is the
number of erythrocytes or red blood cells (RBCs) and the
hematocrit. The hematocrit is the percentage of the blood
that is erythrocytes. Normally the hematocrit is about
40% to 54% in men and 37% to 50% in women. Excessive
increases in the blood hematocrit raise the blood viscosity, reducing the cardiac output and therefore reducing
oxygen transport. Excessive reductions in the blood hematocrit, such as occur in anemia, reduce oxygen transport.
Exercise also has a direct influence on oxygen transport.
In well-trained athletes, oxygen transport can be increased
up to 20 times the normal rate, due in part to an increased
cardiac output and to increased use of oxygen by the cells.
Systemic Diffusion
The fourth process of respiration is diffusion of oxygen and
carbon dioxide between the capillaries and the tissues and
cells down to a concentration gradient similar to diffusion
at the alveolar–capillary level. As cells consume oxygen, the
partial pressure of oxygen in the tissues decreases, causing
the oxygen at the arterial end of the capillary to diffuse into
the cells. When cells consume more oxygen during exercise
M49_BERM9793_11_GE_C49.indd 1307
●
Oxygenation
1307
or stress, the pressure gradient increases and diffusion is
enhanced, allowing the cells to regulate their own flow of
oxygen. Carbon dioxide from metabolic processes accumulates in the tissues and diffuses into the capillaries where
the partial pressure of carbon dioxide is lower. In reduced
blood flow states such as shock, capillary blood flow may
decrease, interfering with tissue oxygen delivery.
Respiratory Regulation
Respiratory regulation includes both neural and chemical
controls to maintain the correct concentrations of oxygen,
carbon dioxide, and hydrogen ions in body fluids. The
nervous system of the body adjusts the rate of alveolar
ventilations to meet the needs of the body so that PO2 and
PCO2 remain relatively constant. The body’s “respiratory
center” is actually a number of groups of neurons located
in the medulla oblongata and pons of the brain.
A chemosensitive center in the medulla oblongata is
highly responsive to increases in blood CO2 or hydrogen
ion concentration. By influencing other respiratory centers, this center can increase the activity of the inspiratory
center and the rate and depth of respirations. In addition
to this direct chemical stimulation of the respiratory center
in the brain, special neural receptors sensitive to decreases
in oxygen (O2) concentration are located outside the central nervous system in the carotid bodies (just above the
bifurcation of the common carotid arteries) and aortic bodies located above and below the aortic arch. Decreases in
arterial oxygen concentrations stimulate these chemoreceptors, and they in turn stimulate the respiratory center
to increase ventilation. Of the three blood gases (hydrogen,
oxygen, and carbon dioxide) that can trigger chemoreceptors, increased carbon dioxide concentration normally has
the strongest effect on stimulating respiration.
However, in clients with certain chronic lung ailments
such as emphysema, oxygen concentrations, not carbon
dioxide concentrations, play a major role in regulating
respiration. For some clients, decreased oxygen concentrations are the main stimuli for respiration because the
chronically elevated carbon dioxide levels that occur with
emphysema “desensitize” the central chemoreceptors.
This is sometimes called the hypoxic drive. Increasing the
concentration of oxygen depresses the respiratory rate.
Thus, oxygen must be administered cautiously to these
clients and often at low flow rates.
Clinical Alert!
Oxygen is considered a drug and must be carefully prescribed based
on individual client conditions.
Factors Affecting
Respiratory Function
Factors that influence oxygenation affect the cardiovascular system as well as the respiratory system. These factors
include age, environment, lifestyle, health status, medications, and stress.
27/01/2021 18:05
1308
Unit 10
●
Promoting Physiologic Health
Age
Health Status
Developmental factors have important influences on
respiratory function. At birth, profound changes occur in
the respiratory systems. The fluid-filled lungs drain, the
PCO2 rises, and the neonate takes a first breath. The lungs
gradually expand with each subsequent breath, reaching
full inflation by 2 weeks of age.
Changes of aging that affect the respiratory system
of older adults become especially important if the system
is compromised by changes such as infection, physical or
emotional stress, surgery, anesthesia, or other procedures.
These types of changes are seen:
In the healthy individual, the respiratory system can provide sufficient oxygen to meet the body’s needs. Diseases
of the respiratory system, however, can adversely affect
the oxygenation of the blood.
•
•
•
•
•
•
•
•
Chest wall and airways become more rigid and less
elastic.
The amount of exchanged air is decreased.
The cough reflex and cilia action are decreased.
Mucous membranes become drier and more fragile.
Decreases in muscle strength and endurance occur.
If osteoporosis is present, adequate lung expansion
may be compromised.
A decrease in efficiency of the immune system occurs.
Gastroesophageal reflux disease is more common in
older adults and increases the risk of aspiration. The
aspiration of stomach contents into the lungs often
causes bronchospasm by setting up an inflammatory
response.
Environment
Altitude, heat, cold, and air pollution affect oxygenation.
The higher the altitude, the lower the PO2 an individual
breathes. As a result, the individual at high altitudes has
increased respiratory and cardiac rates and increased
respiratory depth, which usually become most apparent
when the individual exercises.
Healthy individuals exposed to air pollution, such
as smog or secondhand tobacco smoke, may experience
stinging of the eyes, headache, dizziness, and coughing. Individuals who have a history of existing lung disease and altered respiratory function experience varying
degrees of respiratory difficulty in a polluted environment. Some are unable to perform self-care in such an
environment.
Lifestyle
Physical exercise or activity increases the rate and depth
of respirations and hence the supply of oxygen in the
body. Sedentary individuals, by contrast, lack the alveolar expansion and deep-breathing patterns of individuals
with regular activity and are less able to respond effectively to respiratory stressors.
Certain occupations predispose an individual to lung
disease. For example, silicosis is seen more often in sandstone blasters and potters than in the rest of the population;
anthracosis in coal miners; and organic dust disease in farmers and agricultural employees who work with moldy hay.
M49_BERM9793_11_GE_C49.indd 1308
Medications
A variety of medications can decrease the rate and depth
of respirations. The most common medications having
this effect are the benzodiazepine sedative–hypnotics and
antianxiety drugs (e.g., diazepam [Valium], lorazepam
[Ativan], midazolam [Versed]), barbiturates (e.g., phenobarbital), and opioids such as morphine. When administering these, the nurse must carefully monitor respiratory
status, especially when the medication is begun or when
the dose is increased. Older clients are at high risk of respiratory depression and usually require reduced dosages.
Stress
When stress and stressors are encountered, both psychologic
and physiologic responses can affect oxygenation. Some individuals may hyperventilate in response to stress. When this
occurs, arterial PO2 rises and PCO2 falls. The individual may
experience light-headedness and numbness and tingling of
the fingers, toes, and around the mouth as a result.
Physiologically, the sympathetic nervous system is
stimulated and epinephrine is released during stress. Epinephrine causes the bronchioles to dilate, increasing blood
flow and oxygen delivery to active muscles. Although
these responses are adaptive in the short term, when stress
continues they can be destructive, increasing the risk of
cardiovascular disease.
Alterations in Respiratory
Function
Respiratory function can be altered by conditions that
affect:
•
•
•
•
Patency (open airway)
The movement of air into or out of the lungs
The diffusion of oxygen and carbon dioxide between
the alveoli and the pulmonary capillaries
The transport of oxygen and carbon dioxide via the
blood to and from the tissue cells.
Conditions Affecting the Airway
A completely or partially obstructed airway can occur
anywhere along the upper or lower respiratory passageways. An upper airway obstruction—that is, in the nose,
pharynx, or larynx—can occur when a foreign object
such as food is present, when the tongue falls back into
the oropharynx when an individual is unconscious, or
when secretions collect in the passageways. Lower airway
27/01/2021 18:05
Chapter 49
obstruction involves partial or complete occlusion of the
passageways in the bronchi and lungs most often due
to increased accumulation of mucus or inflammatory
exudate.
Assessing for and maintaining a patent airway is a
nursing responsibility, one that often requires immediate action. Partial obstruction of the upper airway passages is indicated by a low-pitched snoring sound during
inhalation. Complete obstruction is indicated by extreme
inspiratory effort that produces no chest movement and
an inability to cough or speak. Such a client, in an effort
to obtain air, may also exhibit marked sternal and intercostal retractions. Lower airway obstruction is not always
as easy to observe. Stridor, a harsh, high-pitched sound,
may be heard during inspiration. The client may have
altered arterial blood gas levels, restlessness, dyspnea, and
adventitious breath sounds (abnormal breath sounds).
See Table 29.8, page 610.
BOX 49.1
•
Conditions Affecting Movement of Air
•
The term breathing patterns refers to the rate, volume,
rhythm, and relative ease or effort of respiration. Normal respiration (eupnea) is quiet, rhythmic, and effortless. Tachypnea (rapid respirations) is seen with fevers,
metabolic acidosis, pain, and hypoxemia. Bradypnea is an
abnormally slow respiratory rate, which may be seen in
clients who have taken drugs such as morphine or sedatives, who have metabolic alkalosis, or who have increased
intracranial pressure (e.g., from brain injuries). Apnea is
the absence of any breathing.
Hypoventilation, that is, inadequate alveolar ventilation, may be caused by either slow or shallow breathing,
or both. Hypoventilation may occur because of diseases
of the respiratory muscles, drugs, or anesthesia. Hypoventilation may lead to increased levels of carbon dioxide
(hypercarbia or hypercapnia) or low levels of oxygen
(hypoxemia).
Hyperventilation is the increased movement of air
into and out of the lungs. During hyperventilation, the
rate and depth of respirations increase and more CO2 is
eliminated than is produced. Hyperventilation can also
occur in response to stress or anxiety.
Orthopnea is the inability to breathe easily unless
sitting upright or standing. Difficulty breathing or
the feeling of being short of breath (SOB) is called
dyspnea . Dyspnea may occur with varying levels of
exertion or at rest. The client with dyspnea will generally have observable (objective) signs such as flaring
of the nostrils, labored-appearing breathing, increased
heart rate, cyanosis, and diaphoresis. Dyspnea has
many causes, most of which stem from cardiac or respiratory disorders.
•
Impaired diffusion may affect levels of gases in the blood,
particularly oxygen, which does not diffuse as readily as
M49_BERM9793_11_GE_C49.indd 1309
Oxygenation
1309
carbon dioxide. Hypoxemia, or reduced oxygen levels in the
blood, may be caused by conditions that impair diffusion
at the alveolar–capillary level such as pulmonary edema or
atelectasis (collapsed alveoli) or by low hemoglobin levels.
The cardiovascular system compensates for hypoxemia by
increasing the heart rate and cardiac output, to attempt to
move adequate oxygen to the tissues. If the cardiovascular
system is unable to compensate or hypoxemia is severe,
tissue hypoxia (insufficient oxygen anywhere in the body)
results, potentially causing cellular injury or death. Box 49.1
lists signs of hypoxia. Cyanosis (bluish discoloration of the
skin, nail beds, and mucous membranes due to reduced
hemoglobin and decreased oxygen saturation) may be present with hypoxemia or hypoxia.
•
Conditions Affecting Diffusion
●
•
•
Hypoxia
Rapid pulse
Rapid, shallow respirations and dyspnea
Increased restlessness or light-headedness
Flaring of the nares
Substernal or intercostal retractions
Cyanosis
Adequate oxygenation is essential for cerebral functioning. The cerebral cortex can tolerate hypoxia for only
3 to 5 minutes before permanent damage occurs. The face
of the acutely hypoxic individual usually appears anxious,
tired, and drawn. The individual usually assumes a sitting
position, often leaning forward slightly to permit greater
expansion of the thoracic cavity.
Conditions Affecting Transport
Once oxygen moves into the lungs and diffuses into the
capillaries, the cardiovascular system carries the oxygen
to all body tissues, and moves CO2 from the cells back to
the lungs where it can be exhaled from the body. Conditions that decrease cardiac output, such as heart failure
or hypovolemia, affect tissue oxygenation and also the
body’s ability to compensate for hypoxemia.
NURSING MANAGEMENT
Assessing
Nursing assessment of oxygenation status includes a
history, physical examination, and review of relevant
diagnostic data.
Nursing History
A comprehensive nursing history relevant to oxygenation status should include data about current and past
respiratory problems; lifestyle; presence of cough, sputum
(coughed-up material), or pain; medications for breathing;
and presence of risk factors for impaired oxygenation status. Examples of interview questions to elicit this information are shown in the Assessment Interview.
27/01/2021 18:05
1310
Unit 10
●
Promoting Physiologic Health
LIFESPAN CONSIDERATIONS Respiratory Development
INFANTS
• Respiratory rates are highest and most variable in newborns. The
respiratory rate of a neonate is 40 to 80 breaths per minute.
• Infant respiratory rates average about 30 per minute.
• Because of rib cage structure, infants rely almost exclusively on
diaphragmatic movement for breathing. This is seen as abdominal breathing, as the abdomen rises and falls with each breath.
CHILDREN
• The respiratory rate gradually decreases, averaging around 25
per minute in the preschooler and reaching the adult rate of 12
to 18 per minute by late adolescence.
• During infancy and childhood, viral upper respiratory infections
(e.g., colds) are common and, fortunately, usually not serious.
Infants and preschoolers also are at risk for airway obstruction
by foreign objects such as coins and small toys. Cystic fibrosis
is a congenital disorder that affects the lungs, causing them to
become congested with thick, tenacious (sticky) mucus. Asthma
is another chronic disease often identified in childhood. The
airways of the asthmatic child react to stimuli such as allergens,
exercise, or cold air by constricting, becoming edematous, and
producing excessive mucus. Airflow is impaired, and the child
may wheeze as air moves through narrowed air passages.
OLDER ADULTS
• Older adults are at increased risk for acute respiratory diseases
such as pneumonia and chronic diseases such as emphysema
and chronic bronchitis. Chronic obstructive pulmonary disease
(COPD) may affect older adults, particularly after years of exposure to cigarette smoke or industrial pollutants. Obstructive
airway changes are accelerated with the genetic deficiency of
the enzyme alpha1-antitrypsin.
• Pneumonia may not present with the usual symptoms of a fever,
but will present with atypical symptoms, such as confusion, weakness, loss of appetite, and increase in heart rate and respirations.
Nursing interventions should be directed toward achieving optimal
respiratory effort, gas exchange, self-care habits, and wellness. Additionally, nurses play an important role in chronic disease management by assisting clients to cope with and minimize the effects of
illnesses such as COPD.
• Always encourage wellness and prevention of disease by reinforcing the need for good nutrition, exercise, and immunizations, such as for influenza and pneumonia.
• Increase fluid intake, if not contraindicated by other problems,
such as cardiac or renal impairment.
• In hospitalized and immobile clients, encourage ambulation and
frequent changing of positions to allow for better lung expansion and air and fluid movement.
• Teach the client to use deep-breathing and coughing techniques for better lung expansion and airway clearance. (See
Client Teaching throughout this chapter.)
• Pace activities to conserve energy.
• Encourage the client to eat more frequent, smaller meals to
decrease gastric distention, which can cause pressure on the
diaphragm.
• Teach the client to avoid extreme hot or cold temperatures,
which can further tax the respiratory system.
• Teach actions and side effects of drugs, inhalers, and treatments.
ASSESSMENT INTERVIEW Oxygenation
CURRENT RESPIRATORY PROBLEMS
• Have you noticed any changes in your breathing pattern (e.g.,
shortness of breath, difficulty breathing, need to be in upright
position to breathe, or rapid and shallow breathing)?
• If so, which of your activities might cause these symptom(s)
to occur?
• How many pillows do you use to sleep at night?
HISTORY OF RESPIRATORY DISEASE
• Have you had colds, allergies, asthma, tuberculosis, bronchitis,
pneumonia, or emphysema?
• How frequently have these occurred? How long did they last?
And how were they treated?
• Have you been exposed to any pollutants?
LIFESTYLE
• Do you smoke? If so, how much? If not, did you smoke previously, and when did you stop?
• Does any member of your family smoke?
• Is there cigarette smoke or other pollutants (e.g., fumes, dust,
coal, asbestos) in your workplace?
• Do you use alcohol? If so, how many drinks (mixed drinks, glasses
of wine, or beers) do you usually have per day or per week?
• Describe your exercise patterns. How often do you exercise
and for how long?
PRESENCE OF COUGH
• How often and how much do you cough?
• Is it productive, that is, accompanied by sputum, or nonproductive, that is, dry?
• Does the cough occur during certain activity or at certain times
of the day?
M49_BERM9793_11_GE_C49.indd 1310
DESCRIPTION OF SPUTUM
• When is the sputum produced?
• What is the amount, color, thickness, odor?
• Is it ever tinged with blood?
PRESENCE OF CHEST PAIN
• How does going outside in the heat or the cold affect you?
• Do you experience any pain with breathing or activity?
• If so, where is the pain located?
• Describe the pain. How does it feel?
• Does it occur when you breathe in or out?
• How long does it last, and how does it affect your breathing?
• Do you experience any other symptoms when the pain occurs
(e.g., nausea, shortness of breath or difficulty breathing, lightheadedness, palpitations)?
• What activities precede your pain?
• What do you do to relieve the pain?
PRESENCE OF RISK FACTORS
• Do you have a family history of lung cancer, cardiovascular
disease (including strokes), or tuberculosis?
• The nurse should also note the client’s weight, activity pattern,
and dietary assessment. Risk factors include obesity, sedentary
lifestyle, and diet high in saturated fats.
MEDICATION HISTORY
• Have you taken or do you take any over-the-counter or
prescription medications for breathing (e.g., bronchodilator,
inhalant, narcotic)?
• If so, which ones? What are the dosages, times taken, and
results, including side effects?
27/01/2021 18:05
Chapter 49
●
Oxygenation
1311
Physical Examination
Pulmonary Function Tests
In assessing a client’s oxygenation status, the nurse uses
all four physical examination techniques: inspection,
palpation, percussion, and auscultation. The nurse first
observes the rate, depth, rhythm, and quality of respirations, noting the position the client assumes for breathing.
The nurse also inspects for variations in the shape of the
thorax that may indicate adaptation to chronic respiratory conditions. For example, clients with emphysema
frequently develop a barrel chest.
The nurse palpates the thorax for bulges, tenderness, or
abnormal movements. Palpation is also used to detect vocal
(tactile) fremitus. The thorax can be percussed for diaphragmatic excursion (the movement of the diaphragm during
maximal inspiration and expiration). However, this is not
commonly done in acute care and long-term care settings. The
nurse frequently auscultates the chest to assess if the client’s
breath sounds are normal or abnormal. See Chapter 29 ,
Skill 29.11 on page 611 for more information.
Pulmonary function tests measure lung volume and
capacity. Clients undergoing pulmonary function tests,
which are usually carried out by a respiratory therapist, do not require an anesthetic. The client breathes
into a machine. The tests are painless, but the client’s
cooperation is essential. It requires the ability to follow
directions and some hand–eye coordination. Nurses
need to explain the tests to clients beforehand and help
them to rest afterward because the tests are often tiring. Table 49.1 describes the measurements taken, and
Figure 49.3 ■ shows their relationships and normal
adult values.
Diagnostic Studies
The primary care provider may order various diagnostic
tests to assess respiratory status, function, and oxygenation. Included are sputum specimens, throat cultures,
visualization procedures (see Chapter 34 ), venous and
arterial blood specimens, and pulmonary function tests.
Measurement of arterial blood gases is an important
diagnostic procedure (see Chapter 51
). Specimens of
arterial blood are normally taken by specialty nurses,
respiratory therapists, or medical technicians. Blood for
these tests is taken directly from the radial, brachial, or
femoral arteries or from catheters placed in these arteries. Because of the relatively high pressure of the blood in
these arteries, it is important to prevent hemorrhaging by
applying pressure to the puncture site for about 5 minutes
after removing the needle. Frequently the noninvasive
measurement of oxygen saturation (using a device placed
on the fingertip) is sufficient for attaining a measurement
of oxygenation of the arterial blood.
TABLE 49.1
Diagnosing
Examples of nursing diagnoses for clients with oxygenation problems can include altered respiratory status,
altered breathing pattern, altered gas exchange, and
inadequate physical energy for activities. The preceding nursing diagnoses may also be the etiology of several other nursing diagnoses, such as fatigue related to
altered breathing pattern, insomnia related to orthopnea
and required oxygen therapy, and social seclusion related
to inadequate physical energy for activities and inability
to travel to usual social activities.
Planning
The overall outcomes or goals for a client with oxygenation problems are to:
•
•
•
•
•
Maintain a patent airway.
Improve comfort and ease of breathing.
Maintain or improve pulmonary ventilation and
oxygenation.
Improve the ability to participate in physical activities.
Prevent risks associated with oxygenation problems
such as skin and tissue breakdown, syncope, acid–base
imbalances, and feelings of hopelessness and social
isolation.
Pulmonary Volumes and Capacities
Measurement
Description
Tidal volume (VT)
Volume inhaled and exhaled during normal quiet breathing
Inspiratory reserve volume (IRV)
Maximum amount of air that can be inhaled over and above a normal breath
Expiratory reserve volume (ERV)
Maximum amount of air that can be exhaled following a normal exhalation
Residual volume (RV)
The amount of air remaining in the lungs after maximal exhalation
Total lung capacity (TLC)
The total volume of the lungs at maximum inflation; calculated by adding the VT, IRV, ERV,
and RV
Vital capacity (VC)
Total amount of air that can be exhaled after a maximal inspiration; calculated by adding the
VT, IRV, and ERV
Inspiratory capacity
Total amount of air that can be inhaled following normal quiet exhalation; calculated by adding
the VT and IRV
Functional residual capacity (FRC)
The volume left in the lungs after normal exhalation; calculated by adding the ERV and RV
Minute volume (MV)
The total volume or amount of air breathed in 1 minute
M49_BERM9793_11_GE_C49.indd 1311
27/01/2021 18:05
1312
Unit 10
●
Promoting Physiologic Health
mL
6000
5000
Inspiratory
reserve volume
3100 mL
4000
Inspiratory capacity
3600 mL
Vital capacity
4800 mL
3000
Tidal volume 500 mL
Expiratory
reserve volume
1200 mL
2000
Total
lung
capacity
6000 mL
Functional
residual capacity
2400 mL
1000
Residual volume
1200 mL
0
Figure 49.3 ■ The relationship of lung volumes and capacities. Volumes (mL) shown are for an average adult male; female volumes are
20% to 25% smaller.
These outcomes provide direction for planning interventions and as criteria for evaluating client progress.
A clinical example of desired outcomes, interventions,
and activities is provided in the Nursing Care Plan and
Concept Map at the end of the chapter.
•
•
Planning for Home Care
To provide for continuity of care, the nurse needs to consider the client’s learning needs and needs for assistance
with care in the home. Client Teaching: Home Care Oxygenation addresses the learning needs of the client and family.
Planning incorporates an assessment of the client’s and
family’s knowledge and abilities for self-care, financial
resources, and evaluation of the need for referrals and for
home health services.
QSEN
Patient-Centered Care: Oxygenation
When conducting a home care assessment for a client with
oxygenation problems and needs, the nurse includes the
following assessments:
FAMILY
•
•
•
CLIENT
•
•
•
Self-care abilities: ability to ambulate and perform activities of daily living (ADLs) independently
Exercise and activity pattern: type and regularity of usual
exercise, perceived and actual energy for desired and
required leisure activities
Assistive devices required: supplemental oxygen,
humidifier, nebulizer treatments, or inhalers; walker,
cane, or wheelchair; grab bars, shower chair, and
other devices to promote safety and minimize energy
expenditure; scale to monitor weight on a regular
basis
M49_BERM9793_11_GE_C49.indd 1312
Home environment for factors that impair airway clearance,
gas exchange, or activity tolerance: indoor pollutants such as
cigarette smoke, dust, and allergens such as pets; lack of
humidity in the air; and barriers such as stairs
Current level of knowledge: importance of avoiding
smoking and other pollutants; dietary salt and other
restrictions (if appropriate); recommended activities;
medications; need to limit exposure to respiratory infections; use of prescribed nebulizer, multidose inhaler,
powdered dose inhaler, or home oxygen; activity level
Caregiver availability, skills, and responses: ability and
willingness to provide care as needed (help with
ADLs, providing meals, assisting with transportation
and shopping, caring for dependents; performing treatments such as percussion and postural drainage)
Family role changes and coping: effect on financial status,
parenting and spousal roles, sexuality, social roles
Alternate potential primary or respite caregivers: for example, other family members, volunteers, church members,
paid caregivers, or housekeeping services; available community respite care (e.g., adult day care, senior centers)
COMMUNITY
•
•
Environment: usual temperature and humidity; presence
of air pollutants such as automobile exhaust, industrial
smoke and pollutants, smoke from field burning
Current knowledge of and experience with community resources:
medical and assistive equipment and supply companies,
respiratory and physical therapy services, home health
agencies, local pharmacies, available financial assistance,
support and educational organizations such as the local
lung association, COPD support groups
27/01/2021 18:05
Chapter 49
●
Oxygenation
1313
CLIENT TEACHING Home Care Oxygenation
MAINTAINING AIRWAY CLEARANCE AND EFFECTIVE
GAS EXCHANGE
• Emphasize to the client and family the importance of not smoking or lighting any flammable materials (e.g., candles) in the
same room. Refer them to smoking cessation programs as
needed. For family members resistant to not smoking, emphasize the need to avoid smoking inside the home.
• Instruct the client in effective coughing techniques such as
controlled coughing or “huff” coughing (see Client Teaching:
Forced Expiratory Technique (Huff Coughing) in the Implementing section).
• Discuss the significance of changes in sputum, including the
amount and characteristics such as color, viscosity, and odor.
Instruct the client when to contact a healthcare provider.
• Teach the client to maintain a fluid intake of 2500 to 3000 mL
(2.5 to 3 qt) per day if not contraindicated due to other health
conditions such as heart failure or renal disease.
• Instruct the client of the rationale for using and how to use
nebulizers or inhalers if prescribed; see Chapter 35
,
pages 908–911.
• Teach the client and family how to use home oxygen delivery
systems, emphasizing safety considerations.
PROMOTING EFFECTIVE BREATHING
• Teach relaxation techniques such as progressive muscle relaxation, meditation, and visualization. Use DVDs or phone apps
as needed.
• Help the client identify specific factors that affect breathing such
as stress, exposure to allergens or air pollution, and exposure
to cold. Assist with identifying possible interventions and measures to avoid these factors.
MEDICATIONS
• Teach the client about prescribed medications, including the
rationale for the medications, the dose, the desired and possible adverse effects, and any precautions about using a medication with food, beverages, or other medications.
SPECIFIC MEASURES FOR OXYGENATION PROBLEMS
• Provide instructions and rationale for specific procedures and
problems such as:
a. Suctioning oropharyngeal and nasopharyngeal cavities
b. Caring for a temporary or permanent tracheostomy
c. Preventing the spread of tuberculosis and other respiratory
infections to family members and others.
REFERRALS
• Make appropriate referrals to home health agencies or community social services for assistance in obtaining medical and
assistive equipment such as grab bars, respiratory and physical
therapy services, and home health or housekeeping services to
assist with ADLs.
COMMUNITY AGENCIES AND OTHER SOURCES OF HELP
• Provide information about where durable medical equipment
can be purchased, rented, or obtained free of charge; how to
access home oxygen equipment and support services and
physical and occupational therapy services; and where to
obtain supplies such as tracheostomy supplies or nutritional
supplements.
• Suggest additional sources of information such as the American
Lung Association and the Asthma and Allergy Foundation of
America.
Implementing
Examples of nursing interventions to facilitate pulmonary
ventilation may include ensuring a patent airway, positioning, encouraging deep breathing and coughing, and
ensuring adequate hydration. Other nursing interventions
helpful to ventilation are suctioning, lung inflation techniques, administration of analgesics before deep breathing and coughing, postural drainage, and percussion and
vibration. Nursing strategies to facilitate the diffusion of
gases through the alveolar membrane include encouraging coughing, deep breathing, and suitable activity. A client’s nursing care plan should also include appropriate
dependent nursing interventions such as oxygen therapy,
tracheostomy care, and maintenance of a chest tube.
CLIENT TEACHING Promoting Healthy Breathing
•
•
•
•
•
•
•
•
•
•
•
Sit straight and stand erect to permit full lung expansion.
Exercise regularly.
Breathe through the nose.
Breathe in to expand the chest fully.
Do not smoke cigarettes, cigars, or pipes.
Eliminate or reduce the use of household pesticides and irritating chemical substances.
Do not incinerate garbage in the house.
Avoid exposure to secondhand smoke.
Use building materials that do not emit vapors.
Make sure furnaces, ovens, and wood stoves are correctly
ventilated.
Support a pollution-free environment.
Promoting Oxygenation
Most individuals in good health give little thought to their
respiratory function. Changing position frequently, ambulating, and exercising usually maintain adequate ventilation and gas exchange.
Client Teaching lists other ways to promote healthy
breathing.
When individuals become ill, however, their respiratory functions may be inhibited for such reasons as pain
and immobility. Shallow respirations inhibit both diaphragmatic excursion and lung distensibility. The result
of inadequate chest expansion is pooling of respiratory
M49_BERM9793_11_GE_C49.indd 1313
secretions, which ultimately harbor microorganisms and
promote infection. Additionally, shallow respirations may
potentiate alveolar collapse, which may cause decreased
diffusion of gases and subsequent hypoxemia.
Interventions by the nurse to maintain the normal respirations of clients include:
•
•
•
Positioning the client to allow for maximum chest
expansion
Encouraging or providing frequent changes in position
Encouraging deep breathing and coughing
27/01/2021 18:05
1314
•
•
Unit 10
●
Promoting Physiologic Health
Encouraging ambulation
Implementing measures that promote comfort, such as
giving pain medications.
The semi-Fowler’s or high-Fowler’s position allows
maximum chest expansion in clients who are confined
to bed, particularly those with dyspnea. The nurse also
encourages clients to turn from side to side frequently, so
that alternate sides of the chest are permitted maximum
expansion. Clients with severe pneumonia or other pulmonary disease in one lung, if positioned laterally, should
be generally positioned with the “good lung down” to
improve diffusion of oxygen to the blood from functioning alveoli. Dyspneic clients often sit in bed and lean over
their overbed tables (which are raised to a suitable height),
usually with a pillow for support. This orthopneic position is an adaptation of the high-Fowler’s position. Some
clients also sit upright and lean on their arms or elbows,
which is called the tripod position. The advantage to these
positions is that each one forces the diaphragm down and
forward and stabilizes the chest, which reduces the work
of breathing. Also, a client in the orthopneic position can
press the lower part of the chest against the table to help
in exhaling (Figure 49.4 ■).
Deep Breathing and Coughing
The nurse can facilitate respiratory functioning by encouraging deep-breathing exercises and coughing to remove
secretions from the airways. When coughing raises secretions high enough, the client may either expectorate (spit
out) or swallow them. Swallowing the secretions is not
harmful but does not allow the nurse to view the secretions for documentation purposes or to obtain a specimen
for testing.
Clients with conditions that increase secretions or
impair mobilization of secretions such as chest surgery,
COPD, or cystic fibrosis often require encouragement
to cough and breathe deeply. Specialized breathing
exercises may be prescribed for clients with chronic
obstructive diseases as part of their pulmonary rehabilitation. These generally require collaboration with
other healthcare providers. One technique, pursedlip breathing, may help alleviate dyspnea. The client
is taught to breathe in normally through the nose and
exhale through pursed lips as if about to whistle, and
blow slowly and purposefully, tightening the abdominal muscles to assist with exhalation. Clients may practice by slowly blowing a ping-pong ball across a table or
visualizing that they are trying to make a candle flame
waver.
Normal forceful coughing is highly effective, but some
clients may lack the strength or ability to cough normally.
Normal forceful coughing involves the client inhaling
deeply and then coughing twice while exhaling. Alternative cough techniques such as forced expiratory technique, or huff coughing, may be taught as alternatives for
those clients who are unable to perform a normal forceful
cough. A client with a pulmonary condition (e.g., COPD)
M49_BERM9793_11_GE_C49.indd 1314
Figure 49.4 ■ Two sitting tripod positions that help assist with
breathing.
is instructed to exhale through pursed lips and to exhale
with a “huff” sound in mid-exhalation. The huff cough
helps prevent the high expiratory pressures that collapse
diseased airways. This cough technique is described in
Client Teaching.
Hydration
Adequate hydration maintains the moisture of the respiratory mucous membranes. Normally, respiratory tract secretions are thin and are therefore moved readily by ciliary
action. However, when the client is dehydrated or when
the environment has a low humidity, the respiratory secretions can become thick and tenacious. Fluid intake should
be as great as the client can tolerate. See Chapter 51
for normal daily fluid intake.
27/01/2021 18:05
Chapter 49
●
Oxygenation
1315
CLIENT TEACHING Forced Expiratory Technique (Huff Coughing)
After using a bronchodilator treatment (if prescribed), inhale
deeply and hold your breath for a few seconds.
• Cough twice while exhaling. The first cough loosens the mucus;
the second expels secretions.
• For huff coughing, lean forward and exhale sharply with a “huff”
sound mid-exhalation. This technique helps keep your airways
open while moving secretions up and out of the lungs.
•
Humidifiers are devices that add water vapor to
inspired air. Room humidifiers provide cool mist to room
air. Nebulizers are used to deliver humidity and medications. They may be used with oxygen delivery systems
to provide moistened air directly to the client. Their purposes are to prevent mucous membranes from drying
and becoming irritated and to loosen secretions for easier
expectoration.
Medications
A number of types of medications can be used for clients
with oxygenation problems.
Bronchodilators, anti-inflammatory drugs, leukotriene modifiers, expectorants, and cough suppressants are
some medications that may be used to treat respiratory
problems. Bronchodilators, including sympathomimetic
drugs and xanthines, reduce bronchospasm, opening tight
or congested airways and facilitating ventilation. These
drugs may be administered orally or intravenously, but
the preferred route is by inhalation to prevent many systemic side effects.
Because drugs used to dilate the bronchioles and
improve breathing are usually drugs that enhance the
sympathetic nervous system, clients must be monitored
for side effects of increased heart rate, blood pressure,
anxiety, and restlessness. This is especially important
in older adults, who may also have cardiac problems.
Some over-the-counter drugs for respiratory problems
have these same effects, so clients should be cautioned
about taking them without checking with their primary
care provider.
Another class of drugs used is the anti-inflammatory
drugs, such as glucocorticoids. They can be given orally,
intravenously, or by inhaler. They work by decreasing the
edema and inflammation in the airways and allowing
a better air exchange. If both bronchodilators and antiinflammatory drugs are ordered by inhaler, the client
should be instructed to use the bronchodilator inhaler first
and then the anti-inflammatory inhaler. If the bronchioles
are dilated first, more tissue is exposed on which the antiinflammatory drugs can act. Newer formulations may
combine a long-acting bronchodilator with an inhaled
corticosteroid to improve client compliance with therapy
because they require less time and less frequent dosing.
Another class of drugs is the leukotriene modifiers.
These medications decrease the effects of leukotrienes on
the smooth muscle of the respiratory tract. Leukotrienes
M49_BERM9793_11_GE_C49.indd 1315
Inhale by taking rapid short breaths in succession (“sniffing”) to
prevent mucus from moving back into smaller airways.
• Rest and breathe slowly between coughs.
• Try to avoid prolonged episodes of coughing because these
may cause fatigue and hypoxia.
•
cause bronchoconstriction, mucous production, and
edema of the respiratory tract.
Expectorants help “break up” mucus, making it more
liquid and easier to expectorate. Guaifenesin is a common
expectorant found in many prescription and nonprescription cough syrups. When frequent or prolonged coughing
interrupts sleep, cough suppressants such as codeine may
be prescribed.
Other medications can be used to improve oxygenation by improving cardiovascular function. The digitalis
glycosides act directly on the heart to improve the strength
of contraction and slow the heart rate. Beta-adrenergic
stimulating agents such as dobutamine similarly increase
cardiac output, thus improving oxygen transport. Betaadrenergic blocking agents such as propranolol affect the
sympathetic nervous system to reduce the workload of the
heart. These drugs, however, can negatively affect people
with asthma or COPD because they may constrict airways
by blocking beta-2 adrenergic receptors.
Percussion, Vibration, and Postural Drainage
Percussion, vibration, and postural drainage (PVD) are
performed according to a primary care provider’s order
by nurses, respiratory therapists, physical therapists, or an
interdisciplinary team of these healthcare team members.
Percussion, sometimes called clapping, is forceful striking
of the skin with cupped hands. Mechanical percussion
cups and vibrators are also available. When the hands are
used, the fingers and thumb are held together and flexed
slightly to form a cup, as one would to scoop up water.
Percussion over congested lung areas can mechanically
dislodge tenacious secretions from the bronchial walls.
Cupped hands trap the air against the chest. The trapped
air then sets up vibrations through the chest wall to the
secretions.
To percuss a client’s chest, follow these steps:
•
•
•
•
Cover the area with a towel or gown to reduce
discomfort.
Ask the client to breathe slowly and deeply to promote
relaxation.
Alternately flex and extend the wrists rapidly to slap
the chest (Figure 49.5 ■).
Percuss each affected lung segment for 1 to 2 minutes.
When done correctly, the percussion action should
produce a hollow, popping sound. Percussion is avoided
over the breasts, sternum, spinal column, and kidneys.
27/01/2021 18:05
1316
Unit 10
●
Promoting Physiologic Health
CLIENT TEACHING Using Cough Medications
Do not take cough medications in excessive amounts because
of adverse side effects.
• If you have diabetes mellitus, avoid cough syrups that contain
sugar or alcohol; these can disturb metabolism.
•
When a cough medicine does not act as expected, consult a
healthcare professional.
• Be aware of side effects (e.g., drowsiness) that can make the
operation of machinery dangerous.
•
DRUG CAPSULE
Sympathomimetics: albuterol (Proventil, Ventolin)
CLIENT WITH RESPIRATORY MEDICATIONS THAT CAUSE
BRONCHODILATION BY STIMULATING BETA-2 ADRENERGIC RECEPTORS IN THE LUNG
The beta-2 adrenergic agonists are called sympathomimetic drugs
because they “mimic” the action of sympathetic stimulation to the
beta-2 receptors in the smooth muscle of the lung. At therapeutic levels these drugs promote bronchodilation and so relieve bronchospasm.
Sympathomimetic agents are useful in the treatment of bronchospasm in reversible obstructive airway diseases such as asthma
and bronchitis. They are also useful in preventing exercise-induced
bronchospasm.
Drugs that block the parasympathetic nervous system (anticholinergics) such as ipratropium (Atrovent) may be used alone or in
combination (Combivent) with sympathomimetic agents to provide
additional bronchodilation.
NURSING RESPONSIBILITIES
• Most inhaled sympathomimetics have a very rapid onset and
short duration of action, so they are useful for relief of acute
attacks but not for prophylaxis.
• Monitor the client’s respiratory status while administering sympathomimetics. This includes respiratory rate, lung sounds,
oxygen saturation, and subjective symptoms.
These medications should be used with caution in clients with
conditions such as cardiac disease, vascular disease, hypertension, hyperthyroidism, and pregnancy.
• Monitor the client for common side effects including increased
heart rate (due to sympathetic stimulation of the heart) and
tremors.
• Monitor for other side effects that occur with excessive dosing, which may include CNS stimulation, gastrointestinal upset,
hypertension, and sweating.
•
CLIENT AND FAMILY TEACHING
• Caution the client to use the least amount of medication
needed to get relief for the shortest time period necessary. This
will help prevent adverse effects.
• Counsel the client to report immediately any chest pain or
changes in heart rate or rhythm.
• Teach the client and family how to use the delivery system. This
will most often be a metered-dose inhaler (MDI) or dry powder
inhaler (DPI) or nebulizer.
• Teach the client to record the frequency and intensity of
symptoms.
Note: Prior to administering any medication, review all aspects with a current drug handbook or
other reliable source.
DRUG CAPSULE
Glucocorticosteroids Inhaled: fluticasone (Flovent)
CLIENT WITH RESPIRATORY MEDICATIONS THAT
SUPPRESS INFLAMMATION
Glucocorticosteroids are administered to clients with oxygenation
problems to suppress inflammation. They can be administered
either by inhalation, orally, or intravenously. The route of administration depends on the severity of the client’s disorder and the
individual’s response. Glucocorticosteroids (steroids) are well
absorbed from the respiratory tract so giving them by inhalation
is often effective. Steroids suppress the inflammatory response in
the airways by decreasing synthesis and release of inflammatory
mediators, decreasing activity of inflammatory cells, and decreasing edema.
NURSING RESPONSIBILITIES
• Glucocorticosteroids are intended for preventive therapy. They
will not be useful in an acute attack.
• If the client is also taking a sympathomimetic medication,
delivery of inhaled corticosteroids to the respiratory tract may
be enhanced by administering the sympathomimetic first (and
waiting 3 to 5 minutes).
• It is important to monitor the client’s respiratory status while
administering steroids. This includes respiratory rate, lung
sounds, oxygen saturation, and subjective symptoms.
• These medications should be used with caution or not at all in
clients with conditions such as allergy, pregnancy, lactation, and
systemic infections.
M49_BERM9793_11_GE_C49.indd 1316
Monitor the client for side effects of the medications. Most
commonly this could be an increase in heart rate (due to sympathetic stimulation of the heart) and tremors.
• The client should be monitored for other side effects, which will
usually only occur with excessive dosing and may include CNS
stimulation, gastrointestinal upset, hypertension, and sweating.
•
CLIENT AND FAMILY TEACHING
• Caution the client to use the least amount needed to get relief
for the shortest time period necessary. This will help prevent
adverse effects. Alternate-day therapy may be recommended
to decrease adrenal suppression.
• Make sure the client understands that these drugs are not for
acute attacks. They are intended to be preventive therapy.
• Teach the client and family how to use the delivery system. This
will most often be a metered-dose inhaler (MDI) or dry powder
inhaler (DPI) or nebulizer.
• Counsel the client to rinse the mouth after using inhaled corticosteroids to decrease the risk of oropharyngeal or esophageal
fungal infections (thrush).
• Counsel the client to report adverse effects such as sore throat,
hoarseness, and pharyngeal and laryngeal fungal infections.
• Teach the client to record the frequency and intensity of
symptoms.
Note: Prior to administering any medication, review all aspects with a current drug handbook or
other reliable source.
27/01/2021 18:05
Chapter 49
Figure 49.5 ■ Percussing the upper posterior chest.
Vibration is a series of vigorous quiverings produced
by hands that are placed flat against the client’s chest wall.
Vibration is used after percussion to increase the turbulence of the exhaled air and thus loosen thick secretions.
It is often done alternately with percussion.
To vibrate the client’s chest, the nurse follows these
steps:
•
•
•
•
•
Place hands, palms down, on the chest area to be
drained, one hand over the other with the fingers
together and extended (Figure 49.6 ■). Alternatively,
the hands may be placed side by side.
Ask the client to inhale deeply and exhale slowly
through the nose or pursed lips.
During the exhalation, tense all the hand and arm
muscles, and using mostly the heel of the hand, vibrate
(shake) the hands, moving them downward. Stop the
vibrating when the client inhales.
Vibrate during five exhalations over one affected lung
segment.
After each vibration, encourage the client to cough and
expectorate secretions into the sputum container.
Postural drainage is the drainage by gravity of secretions from various lung segments. Secretions that remain
in the lungs or respiratory airways promote bacterial
●
Oxygenation
1317
growth and subsequent infection. They also can obstruct
the smaller airways and cause atelectasis. Secretions in
the major airways, such as the trachea and the right and
left main bronchi, are usually coughed into the pharynx,
where they can be expectorated, swallowed, or effectively
removed by suctioning.
A wide variety of positions is necessary to drain all
segments of the lungs, but not all positions are required
for every client. Only those positions that drain specific
affected areas are used. The lower lobes require drainage
most frequently because the upper lobes drain by gravity.
Before postural drainage, the client may be given a bronchodilator medication or nebulization therapy to loosen
secretions. Postural drainage treatments are scheduled
two or three times daily, depending on the degree of lung
congestion. The best times include before breakfast, before
lunch, in the late afternoon, and before bedtime. It is best
to avoid hours shortly after meals because postural drainage at these times can be tiring and can induce vomiting.
The nurse needs to evaluate the client’s tolerance of
postural drainage by assessing the stability of the client’s
vital signs, particularly the pulse and respiratory rates,
and by noting signs of intolerance, such as pallor, diaphoresis, dyspnea, nausea, and fatigue. Some clients do
not react well to certain drainage positions, and the nurse
must make appropriate adjustments. For example, some
become dyspneic in Trendelenburg’s position and require
only a moderate tilt or a shorter time in that position.
The sequence for PVD is usually as follows: positioning, percussion, vibration, and removal of secretions by
coughing or suction. Each position is usually assumed for
10 to 15 minutes, although beginning treatments may start
with shorter times and gradually increase.
Following PVD, the nurse should auscultate the client’s lungs, compare the findings to the baseline data,
and document the amount, color, and character of expectorated secretions.
Today, kinetic therapy beds with modalities such as
vibration and percussion therapy are available. These
beds provide continuous lateral rotational therapy (CLRT)
along with vibration and percussion modules that are programmed to perform for a specific amount of time.
Mucus Clearance Devices
A mucus clearance device (MCD) is used for clients with
excessive secretions such as with cystic fibrosis, COPD, and
bronchiectasis. The Flutter MCD is an example of one of
these devices. It is a small, handheld device with a hard plastic mouthpiece at one end and a perforated cover at the other
end. Inside the device is a steel ball that sits in a circular cone
shape (Figure 49.7 ■). The client inhales slowly and then,
keeping the cheeks firm, exhales fast through the device,
causing the steel ball to move up and