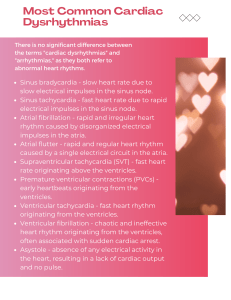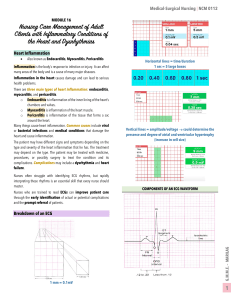
Disorders of Cardiac Conduction and Rhythm Pathophysiology Dr. Patti Landerfelt Chapter 28 Conduction System of the Heart • Sinoatrial (SA) node – pacemaker of the heart • Intrinsic rate 60-100 bpm • Atrioventricular (AV) node • Pauses electrical impulse to allow action potential to spread across atria for coordinated contraction • Intrinsic rate 45-50 bpm • Bundle of His • Bundle branches • Purkinje fibers • Intrinsic rate 15-40 bpm Action Potentials • Membrane potential: electrical potential (difference) across the cell membrane • During depolarization the membrane potential becomes less negatively charged as Na+ ions rapidly rush into the cell • During repolarization, K+ ions leave the cell to reestablish the resting membrane potential • The Na+/K+ ATPase pump functions to maintain resting membrane potential Action Potentials • Absolute refractory period – action potential cannot be initiated • Relative refractory period – action potential can be initiated with a “larger than normal” stimulus Assessment of Coronary Blood Flow and Perfusion: Electrocardiogram Electrocardiogram P-wave: atrial depolarization, QRS complex: ventricular depolarization; T wave: ventricular repolarization Why do we monitor the ECG? • Advantages of continuous cardiac monitoring • More sensitive to changes related to myocardial ischemia or arrhythmias than patient report • More accurate and timely detection of ischemic events that can predict early complications Normal Sinus Rhythm • Sinus node fires 60–100 beats/minute • Follows normal conduction pattern • Regular rhythm • R – R distance regular • P wave before each QRS complex • P wave normal shape and duration • P-R interval normal • QRS complex normal shape and duration Sinus Bradycardia • Sinus node fires < 60 beats/minute • Follows normal conduction pattern • Regular rhythm • R – R distance regular • P wave before each QRS complex • P wave normal shape and duration • P-R interval normal • QRS complex normal shape and duration Sinus Tachycardia • Sinus node fires > 100 beats/minute • Follows normal conduction pattern • Regular rhythm • R – R distance regular • P wave before each QRS complex • P wave normal shape and duration • P-R interval normal • QRS complex normal shape and duration Arrhythmias of Atrial Origin • Atrial flutter • Rapid atrial ectopic tachycardia • Atrial rate 240-340 bpm • QRS may be normal or abnormal • Occurs after corrective surgery for congenital heart disease Arrhythmias of Atrial Origin • Atrial fibrillation • Rapid, disorganized atrial activation • Atrial rate 400-600 bpm • Risks: CAD, mitral valve disease, MI, hypertension, pericarditis, HF, hyperthyroidism • Symptoms: palpitations, pulmonary edema, fatigue • ↑ risk for thrombus formation stroke • Supraventricular tachycardia (SVT) Arrhythmias of Atrial Origin • Paroxysmal Supraventricular tachycardia (PSVT) • Tachyarrhythmia that originates above Bundle of His • Sudden onset and termination • Rate: 140-240 bpm • Symptoms: sudden awareness of rapid heartbeat, brief shortness of breath • Can occur in otherwise healthy individuals Ventricular Arrhythmias – Medical Emergencies • Ventricular tachycardia (VT) • Cardiac rhythm originating after the bundle of His • Ventricular rate 70-250 bpm • + pulse or NO PULSE • Dangerous rhythm: Eliminates atrial filling, decreases diastolic filling time severely limited or no cardiac output Ventricular Arrhythmias – Medical Emergencies • Ventricular fibrillation (VF) • Severe derangements of cardiac rhythm • NO PULSE, no cardiac output • Ventricle quivers rather than contracts • Pulseless ventricular tachycardia and ventricular fibrillation require immediate defibrillation Treatment of Arrythmia Disorders • Pharmacologic therapy and electrical interventions • Cardiac pacemaker • Slow heart rate (bradycardia) • Delivers an electrical stimulus to the heart when normal pacemaker of heart is defective • Cardioversion • • • • Synchronized cardioversion: Atrial fibrillation Unsynchronized cardioversion or defibrillation: Pulseless VT or VF Completely depolarizes the heart allowing SA node to regain control on the heart Despite TV and movies – you cannot shock asystole • Ablation: Destroying or removing arrhythmogenic tissue • Surgery: Remove cause • CABG, aneurysm removal Thank you! Questions/Concerns? Please contact me: patti.e.landerfelt@emory.edu