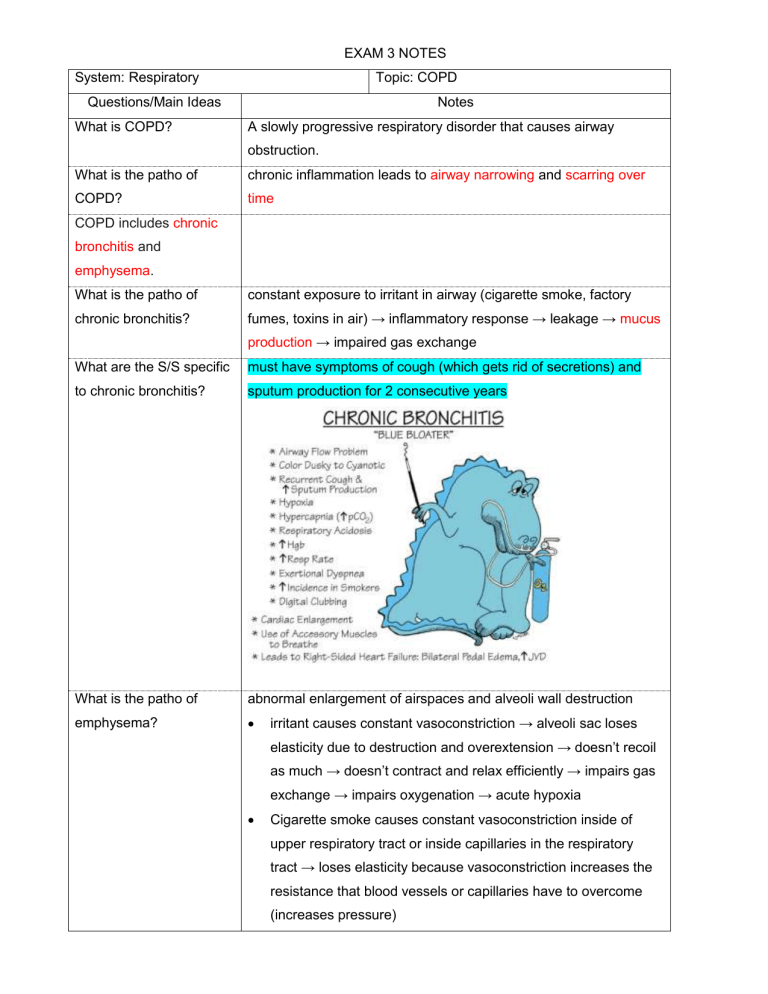
EXAM 3 NOTES System: Respiratory Topic: COPD Questions/Main Ideas What is COPD? Notes A slowly progressive respiratory disorder that causes airway obstruction. What is the patho of chronic inflammation leads to airway narrowing and scarring over COPD? time COPD includes chronic bronchitis and emphysema. What is the patho of constant exposure to irritant in airway (cigarette smoke, factory chronic bronchitis? fumes, toxins in air) → inflammatory response → leakage → mucus production → impaired gas exchange What are the S/S specific must have symptoms of cough (which gets rid of secretions) and to chronic bronchitis? sputum production for 2 consecutive years What is the patho of abnormal enlargement of airspaces and alveoli wall destruction emphysema? irritant causes constant vasoconstriction → alveoli sac loses elasticity due to destruction and overextension → doesn’t recoil as much → doesn’t contract and relax efficiently → impairs gas exchange → impairs oxygenation → acute hypoxia Cigarette smoke causes constant vasoconstriction inside of upper respiratory tract or inside capillaries in the respiratory tract → loses elasticity because vasoconstriction increases the resistance that blood vessels or capillaries have to overcome (increases pressure) What are the risk factors o for COPD? How is COPD classified? age (vasoconstriction and calcification of blood vessels → hypertension) o environmental exposures (smoking or secondhand smoking) o exposure to occupational chemicals (mine workers, contractors) o deficiency in alpha1 antitrypsin (protects lungs from injury) Different stages of COPD are classified based on severity: mild, moderate, severe What are the clinical o chronic cough (due to mucus production) manifestations of COPD? o sputum production o dyspnea (impaired gas exchange initiates stress response → SOB) o weight loss (stress response causes hypoperfusion of the gut) o barrel chest (CO2 building up → impaired gas exchange → hypoventilation → hypercapnia → air gets trapped → circumference of chest increases → chronic respiratory acidosis with chronic hypoxia) o AP diameter 1:1 (because of air trapping; normal is 2:1) o clubbing (chronically hypoxic, nail bed is greater than or equal to 180 degrees) Initially may be on BIPAP - gives patient pressure and keeps alveoli in lungs open; patient can get a certain amount of FiO2 to keep alveoli inflated and get them out of a hypoxic state SpO2: 88-92% is normal o Patient is acutely hypoxic and hyperventilating → increased retention of CO2 → increasing O2 increases CO2 → patient retains more CO2 → you don’t want to give more O2 since they don’t have the ability to remove CO2 What is the management o Smoking cessation - #1 way to treat COPD for COPD (not including o Administer supplemental oxygen in low doses to prevent oxygen meds)? toxicity because patient is acutely hypoxic and has loss of drive to breathe → continuous hyperventilation → increased CO2 → hypercapnia If you give too much oxygen → increased hypercapnia → becomes sleepy → can’t protect their airway o Don’t give non-rebreather mask Preventative measures to prevent exacerbations (ex. updated flu vaccine and pneumococcal vaccine) - already chronically inflamed and hypoxic, so you don’t want to worsen the problems o Pulmonary rehab to reduce symptoms o Chest PT can be utilized to move secretions - more common in chronic bronchitis than emphysema o Allocate extra time to complete activities and conserve energy do slow AM care and ADLs o A balanced diet helps to reverse weight loss - need adequate protein o Advanced disease → lung transplant or lobectomy/pneumonectomy to remove a piece of the lung Medications used for COPD depend on severity. What are the 3 main meds? Antibiotics, Bronchodilators, Corticosteroids Antibiotics: given to patients with chronic bronchitis (NOT emphysema) to help with mucus production o antibiotic of choice - respiratory fluoroquinolones (ex. Levaquin) causes Achilles tendon rupture and sun sensitivity In this case, patient doesn’t need to have elevated WBC Bronchodilators: dilates bronchioles → increases permeability → more O2 can get through membrane and into bronchioles o Rescue drug: Albuterol Complication is tachycardia → give ipratropium bromide → anticholinergic effects (dry mouth, constipation, paralytic ileus, urinary retention) → don’t give to BPH patients because it will cause more urinary retention o Xopenex (levalbuterol) for maintenance - combo of Albuterol and ipratropium at lower concentrations Corticosteroids: reduces inflammation in airway o Give IV: Methylprednisone (methylprednisolone) o Complications: delays wound healing, hyperglycemia, Cushing’s if too aggressive, Addison’s if abruptly stopped o Inhaled corticosteroids are also given, but short-term only Summary: COPD includes chronic bronchitis and emphysema. Both are commonly due to cigarette smoke that causes vasoconstriction of the airway, leading to impaired gas exchange. This is directly due to sputum production in chronic bronchitis. In emphysema, it is due to the abnormal enlargement of airspaces and alveolar wall destruction. COPD is medically treated with bronchodilators, corticosteroids, and antibiotics. System: Respiratory Topic: Asthma Questions/Main Ideas What is asthma? Notes Chronic airway inflammation due to exposure to airway irritants or allergens What are the S/S of Histamine is the problem - constricts smooth muscle in airway o Cough with or without sputum (different from chronic bronchitis - asthma? always with sputum) o Dyspnea o Wheezing - indicates air going through a tight airway and is not specific to asthma o Also associated with eczema from exposure to an allergen (ex. latex, tree nuts, bananas) due to eosinophil release during immune response o Chest tightness in acute asthma → respiratory alkalosis from hyperventilation → acute hypoxemia → hypercapnia → if sustained over time without treatment → respiratory acidosis How is Asthma diagnosed? H&P What labs are done for a Labs to assess for Eosinophilia and IgE patient with asthma? What is a Major respiratory failure – caused by hypoventilation complication of asthma? How is asthma managed? o Rescue meds: SABA (short-acting beta-agonists) - ex. Albuterol (causes tachycardia) Anticholinergics – ex. Ipratropium (not for BPH patients) o Long-term/daily meds: Corticosteroids – ex. Beclomethasone, Advair o For inhalers, educate patient on rinsing mouth after using to prevent oral thrush/candida Leukotriene modifiers – ex. Montelukast/Singulair (prevents asthma attacks) o All clients must have an asthma management plan – use peak flow and document levels daily, and know when to notify the provider o Peak flow: measures the highest airflow during forced expiration Must be documented in a journal daily to prevent status asthmaticus What do the different levels Green Zone (>80%): good mean on the peak flow Yellow Zone (60-80%): caution - something meter? may be going on and patient may be symptomatic → should call provider for treatment of symptoms (i.e. corticosteroid inhaler) and return for follow-up within 1-2 days Red Zone (<60%): GO TO ER! → goal is to prevent status asthmaticus - patient may need more medication to take long term to help manage their asthma Summary: Asthma is caused by exposure to irritants or allergens that lead to chronic airway inflammation. If it’s not treated appropriately, asthma can lead to respiratory failure. Therefore, asthma should be managed with rescue meds—such as albuterol and ipratropium—and daily meds—such as beclomethasone and montelukast. All asthma patients should have an asthma management plan with daily usage of a peak flow meter. System: Respiratory Topic: Laryngeal Cancer Questions/Main Ideas Notes Larynx cancer accounts for ½ of head and neck cancers. What are the risk factors for o Smoking - #1 risk factor laryngeal CA? o Alcohol - main risk factor along with smoking (both cause vasoconstriction) o Men o Adults older than 65 o Exposure to toxins (ex. asbestos) - causes inflammation which over time, causes cell differentiation → cancer What are the S/S of o laryngeal CA? hoarseness for more than 2 weeks (patient’s main complaint) - due to compression of vocal cords from the tumor growing o Raspy voice and low pitch o Persistent cough o Sore throat o Lump in neck and dysphagia – occurs as cancer progresses and becomes more advanced → tumor gets bigger and compresses vocal cords and makes it difficult for food to go down o Weight loss – nothing goes down when they eat What are the diagnostic o Definitive diagnosis - fine needle aspiration (FNA) biopsy tests for laryngeal CA? o Barium swallow study – for dysphagia o CT scan, MRI, and PET scan – for metastasis How is laryngeal CA Depends on the stage treated? o Chemotherapy and radiation o Surgery: o cordectomy (incision and removal of vocal cords) in mild cancer o [rare] laryngectomy in severe disease - partial or total removal of larynx depending on severity and complications What is the pre-op care for a o educate patient on loss of voice post-op and explore alternative laryngectomy? methods of communication (i.e. pen and paper) o What is the post-op care for Will be NPO post-op for about 1 week → enteral feeding or TPN o a laryngectomy? The airway is a priority post-op! Monitor for respiratory distress (ex. SOB, using accessory muscles, agitation, nasal flaring, JVD, increased respirations) and report any findings ASAP o Explain to the client with a complete laryngectomy that the natural voice will be gone. o NPO for 7 days, so will have enteral feeding or TPN. o Because smoking and alcoholism are main causes of laryngeal cancer: o Monitor for alcohol withdrawal (delirium tremens symptoms): tremors, sweating/diaphoresis, tachycardia, agitation, nausea, vomiting → treatment: Ativan (lorazepam), Librium (chlordiazepoxide) o Monitor for nicotine withdrawal: headache → treatment: nicotine patch o Psychosocial assessment: assess patient for disturbed body image, knowledge deficit, and anxiety → RN should address these issues and allow patient to discuss how they feel When is enteral feeding Enteral feeding (NGT, PEG) is used with a patient who still has the ability used vs. TPN feeds? to absorb in the gut. TPN (IV) feeding is utilized when a patient has issues with absorption inside of the gut. What must the RN monitor Electrolytes with enteral feeding? Blood sugar Risk for aspiration - Notify UAP/CNA to hold feeds when turning patient Dumping Syndrome – food goes quickly through GI tract → S/S: nausea, vomiting, diarrhea, bloating What must the RN monitor Blood sugar - TPN includes glucose and insulin with TPN? Don't abruptly stop – will cause rebound hypoglycemia o Instead put them on D10 and slowly taper them down How is speech managed Speech therapy: alternate methods to communicate. Utilize writing, lip- post-laryngectomy? reading, and electronic devices such as iPads or cell phones. Will work with speech pathologist during acute phase post-op. o Different types of speech: Esophageal speech – works with speech pathologist on using muscles to speak Artificial larynx – electrolarynx Tracheoesophageal puncture – valve placed in stoma → covering valve produces speech What education is showering (don’t cover too tightly) necessary for the client and family post-laryngectomy? Wear a loose-fitting bib or hold your hand over your stoma when AVOID swimming Humidification is needed in the house – dry air will dry out site Proper care and management of tracheostomy – nothing goes inside stoma because anything inside will cause systemic infection → sepsis Summary: Cancer of the larynx is due to a tumor compressing the vocal cords. Treatment may involve surgical removal of the vocal cords or larynx depending on severity. The patient will need speech therapy post-op and will require enteral or TPN feeds within the first 7 days. The nurse must monitor for complications of Dumping Syndrome that comes with enteral feeds and rebound hypoglycemia from TPN feeds. Proper care and of the stoma prevents sepsis. System: Cardiovascular Topic: Coronary Artery Disease (CAD) Questions/Main Ideas Why are the coronary arteries Notes/Answers They provide blood, oxygen, and nutrients to the myocardium. important? What are the 3 levels of 1. BEGINS with ischemia: insufficient oxygen supply to meet requirements of the damage caused by CAD? myocardium 2. Ischemia leads to injury. 3. Prolonged injury leads to infarction. What is the patho of CAD? o uncontrolled hypertension → vasoconstriction of blood vessels → changes structure of blood vessels and makes them more prone to inflammation o HLD (from high cholesterol, fatty foods) → plaque buildup → obstruction - lumen of artery gets smaller → not enough blood to meet oxygen demands → reduced blood flow to myocardium and reduced oxygen to blood vessels → ischemia (presents as headache, chest pain) → over time, this activates stress response → vasoconstriction as compensatory mechanism for decreased oxygenation in blood vessels (on top of plaque buildup) AND inflammation occurring at the same time → coronary arteries become more diseased and less oxygen is going through them → prolonged injury → acute coronary syndrome → complete occlusion from plaque → infarction: STEMI or NSTEMI o Long term: inflammation (since plaque is considered foreign) → clot from plaque breaks off → stroke or MI What are the modifiable risk Elevated serum cholesterol (normal is <200) factors for CAD? Cigarette smoking Hypertension - if vasoconstriction of blood vessels becomes chronic → left ventricle works harder→ increases afterload → left ventricular hypertrophy → heart failure Impaired glucose tolerance/DM - glucose molecules stick to capillaries → affe oxygenation - impairs gas exchange → teach patients to consistently take antidiabetic meds, exercise, and watch what they eat Obesity o Most likely has metabolic syndrome – patient has 5 risk factors for CV and will have an MI in 5-10 years 1. hypertension (normal BP should be <130/80) 2. elevated waist circumference >35.4 for males and >31.4 for females 3. elevated triglycerides ≥175 4. reduced HDL (normal should be >40 in males and >50 in females) 5. elevated fasting glucose >100 Excessive alcohol – causes vasoconstriction Limited physical activity – increased fat stores leads to increased risk for metabolic syndrome Stress – stress response causes vasoconstriction What are the non-modifiable Age (older adults) – can be middle-aged and at risk if they have other risk fac risk factors for CAD? Male gender Family history of CAD African American ethnic background When does someone with or Testing for CAD (lipid panel) occurs with every annual physical exam if you have without risk factors get a lipid factors or every 5 years if you don’t have risk factors panel test? What are the typical S/S of o CAD? Chest pain that radiates to left shoulder or jaw (due to decreased oxygenation heart) o Nausea and vomiting (stress response causes decreased blood flow to the gu o Diaphoresis (sympathetic nervous system/stress response) o How do men with CAD mainly Shortness of breath (stress response) chest pain (pressure on chest) that radiates to left shoulder, diaphoresis/sweating present? How do women and older 70% present with atypical (mostly GI) symptoms: indigestion, nausea and vomiting, adults with CAD mainly palpitations (increased blood flow to the heart), and numbness present? What are the labs and o CBC - to check WBC count, hemoglobin, hematocrit, platelet count diagnostics for CAD? o BMET (measures BUN and Creatinine) – to check kidney function (in addition to GFR) How would you educate a o CRP – inflammatory marker o Educate on importance of consuming plant foods and minimizing processed patient with CAD? foods and red meats - heart healthy foods include oatmeal, salmon, whole grains almonds, green vegetables, fruits o Connect them to social work to provide resources in the community for affordable food options o Encourage participation in regular, moderate physical activity - must break a sweat 3 times a week o Educate on the importance of smoking cessation o Educate on the importance of BP control and tight glycemic control and adhering to medications (to prevent chronic massive vasoconstriction → calcification of blood vessels → reduces oxygen supply to the myocardium) What are the 4 elements of fat Lipid panel: metabolism that can lead to 1. Total cholesterol CAD? 2. LDL 3. HDL o cardioprotective - gets rid of bad cholesterol through liver o The higher the HDL, the lower the risk for getting an MI 4. Triglycerides o From fatty foods, but oral contraceptives and steroids can also increas triglycerides What are the 2 types of meds HMG-CoA reductase inhibitors (statins) used for managing Fibric acids (fibrates) cholesterol? What do statins do? Inhibit enzymes involved in lipid synthesis Gets rid of bad cholesterol – given to patients with really high total cholesterol levels What are examples of statins? Creator, Lipitor, Mevacor, Lescol What are the side effects of statins? rhabdomyolysis (muscle pain and weakness) - indicates increased risk for ren failure and liver failure (statins are excreted by the liver) → notify provider, nee a liver function test (LFT) → AST and ALT levels will be high Monitor for S/S of liver failure and notify provider: 1. Tea-colored dark urine 2. Clay-colored stool 3. Jaundice What do fibrates do? Decrease synthesis of TGL and other lipids – given to patients with high TGL What are the side effects of Cholesterol is made in the liver → check liver function → monitor for rhabdo, S/S fibrates? liver failure, pancreatitis (pancreas has digestive enzymes to break down fats and lipids) Summary: Coronary artery disease begins with ischemia and can eventually lead to a myocardial infarction. It occ due to chronic massive vasoconstriction and HLD. The signs and symptoms differ between men and women, with women commonly experiencing GI symptoms. Lifestyle modifications are necessary on top of medication adheren to prevent a stroke or MI. Statins and fibrates are the main medications given to control cholesterol and prevent CA System: Cardiovascular Questions/Main Ideas What is hypertension? Summary: Topic: HTN Notes When the force of the blood against the artery walls (BP) is too high CRITICAL READING: CORNELL NOTES Chapter Section: Questions/Main Ideas/Vocabulary Summary: Name: Date: Period: Notes/Answers/Definitions/Examples/Sentences