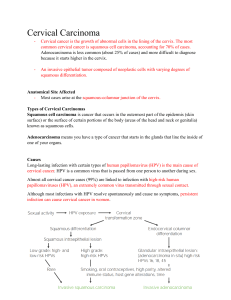
Anat Path - Cervical Carcinoma
Thursday, 19 October 2023
17:38
1. With regards to cervical carcinoma:
List the risk factors of cervical carcinoma
- Long interval between pap smears
- Immunodeficiency
- Smoking
Co-factors for cervical carcinoma
- Low SES
- Early sexual debut
- Multiple partners
- Parity (number of times a woman has given birth)
- STDs (Chlamydia, HSV)
a. Discuss the pathogenesis of cervical carcinoma with regards to HPV.
HPV is a dsDNA virus that infects cells of skin & squamous mucosa and infects basal epithelial cells of
the transformation zone of the cervix - needs to infect the basal cells in order for the HPV infection to
persist
Cells at the squamocolumnar junction (glandular cells of the endocervix transform into squamous cells)
interact with the HPV virus can come into contact with the basal cells of the squamous epithelium
Treatment of the HPV infection involves surgical removal of the transformation zone
Low risk HPV types 6, 11, 42, 53, 54, 62, 66 which exist as freelying episomes in the nucleus that do not
integrate and disrupt the host genome - form condylomata acuminata
Case 12 - Female Reproductive System Page 1
High-risk HPV types 16, 18, 31, 33 (35, 39, 45, 51, 52, 68, etc.) integrate and disrupt the human genome.
Viral E6 and E7 genes serve as oncogenes to reduce apoptosis and increase cellular proliferation.
E6 binds p53, inducing degradation, reducing apoptosis and upregulating telomerase
E7 binds Rb and induces its proteolysis, upregulates Cyclin E (cell cycle proteins) and p16
Outcome : unchecked cellular proliferation => dysplasia
Combination of these gene products and cofactors triggers development of cervical carcinoma
b. Discuss the classification systems used in grading cervical pre-neoplasia.
Dysplasia: non-invasive
Squamous intraepithelial lesions (SIL cytology)
Cervical intraepithelial neoplasia (CIN histology)
Case 12 - Female Reproductive System Page 2
Cervical intraepithelial neoplasia (CIN histology)
Invasive tumours (cervix is covered by both squamous and glandular epithelium)
Squamous cell carcinoma
Adenocarcinoma
Natural course of the HPV infection
- Majority of the HPV infection begins at 15 years, regresses by age 30 [HPV vaccine before age 15]
- Infection after 30 years will persist and can develop into dysplasia (pre-cancer) and cancer [screening after 30]
Biopsy includes the cervical epithelium and underlying stroma which is then examined histologically.
Dysplastic lesion is classified into cervical intraepithelial neoplasia I, II, III (according to British classification)
LSIL = CIN 1
HSIL = CIN II, CIN III
If precancer is identified and confirmed histologically, precancerous are is then excised under colposcopic guidance
- LLETZ (large loop excision of transformation zone)
Case 12 - Female Reproductive System Page 3
- Cone biopsy
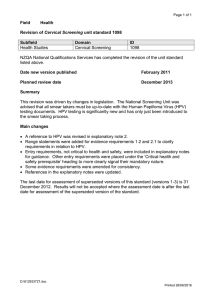
Prevention of cervical carcinoma:
Vaccination [Cervarix (16 & 18), Gardasil (6, 11, 16, 18) -> don't cover all risk types, still need
screening. 1-3 shots over 6 months, state schools > 9 years]
HPV typing [PCR testing for HPV DNA/RNA, >> sensitivity for CIN2 (90%), fair specificity (~
80%), 30+ yrs, every 5 years]
Cytology [pap smear uses exfoliative cytology (collect exfoliated cells from cervix with
brush/spatula), smear on a glass slide, stain and examine for abnormalities, >> specificity (95%),
not very high sensitivity (~50%), 3 pap smears in a 10 year cycle in public SA from age of 30]
Liquid cytology [head of brush in fluid medium, machine lays a mono-layer on slide, less
obscuring factors, better preservation, faster screening, automated screening and ancillary
techniques (HPV typing)
c. Explain how they affect management (such as referral for coloposcopy and what to do at colposcopy).
When patient has HSIL or persistent LSIL, refer for colposcopy (examination of the cervix using a
scope, between 6-40X magnification)
Case 12 - Female Reproductive System Page 4
Acetic acid is applied and based on cellular density, will turn white, more dense = more dense white
colour than normal "acetowhite" cervix
If SIL or CIL is high-grade, gynae will see abnormal vascular patterns, abnormal area is biopsied (punch
biopsy forceps) and then diagnosed
1. Discuss cervical carcinoma screening policy with reference to the benefits and the shortfalls. Anatomical
Pathology lectures and eReader
2. Describe the Bethesda system of reporting Pap smears. Anatomical Pathology lectures and eReader
Cervical squamous cells from pap smear classified based on this
Squamous Intraepithelial Lesion (SIL)
Normal
Normal superficial squamous cells have a small inactive nucleus, abundant cytoplasm right
in intermediate filaments and allowing cells to act as a hardy barrier to physical injury
LSIL (lowgrade SIL)
Patient may have a repeat pap smear or may be repeated after a year
HSIL (highgrade SIL)
Patient referred for colposcopy
3. Outline the Pap smear changes in the development of cervical carcinoma. Anatomical Pathology lectures and
eReader
HPV infection changes: genome dysregulation, dysregulation of the cell cycle and nuclei become enlarged cell loses ability to differentiate properly, hence reduced cytoplasmic content
4. Describe the pathological changes occurring with cervical carcinoma. (Staging and grading of cervical
carcinoma.) Anatomical Pathology lectures and eReader
Case 12 - Female Reproductive System Page 5
carcinoma.) Anatomical Pathology lectures and eReader
Invasive carcinomas breach the BM to infiltrate the underlying stroma, can then metastasise
Most common tumour is squamous cell carcinoma (HPV affects mainly squamous cells) in the ectocervix
/tranformation zone
85% of cervical cancers
Age 20-80
Arises a decade after patient develops HSIL
Adenocarcinoma in the endocervix with rising incidence
40-80% HPV-related
Maternal DES (diethylstilbestrol)
Peutz-Jeghers syndrome (minimum deviation adenocarcinoma
Case 12 - Female Reproductive System Page 6
Small cell carcinoma
Rare, highly aggressive
Associated with HPV 18
Case 12 - Female Reproductive System Page 7
Associated with HPV 18
1. Discuss the spread of cervical carcinoma: Anatomical Pathology lectures and eReader
a. List the routes of spread.
- Local {most common route of mets}
- Lymphatic [early invasion <3mm: minimal chance of LN mets]
- Haematogenous - vaginal plexus is porto-systemic connection
b. List the possible causes of death.
- Local extension (most common cause of death)
Case 12 - Female Reproductive System Page 8
Haemorrhage
Secondary infection
Renal failure (obstructive hydronephrosis)
- Mets (liver, lungs, bone and adnexae)
- Iatrogenic e.g. pulmonary embolus from DVT
c. Explain how the extent of spread affects the staging of cervical carcinoma.
Using the FIGO systems (International federation of Gynaecology and Obstetrics)
FIGO stage I (confined to cervix)
IA: visible only microscopically, <5mm deep beyond the BM
IB >/= 5mm deep beyond the BM
FIGO Stage II (beyond cervix)
Case 12 - Female Reproductive System Page 9
Diagnosis
Cervical squamous cell carcinoma
Cause
High risk HPV and co-factors
FIGO stage FIGO IIA
Treatment
Radical hysterectomy and bilateral pelvic lymphadenectomy
Prognosis
Fair
IIA - upper 2/3 of vagina, resectable with radical hysterectomy (uterus and cuff of the vagina is
removed, when it extends to lower 1/3 can't be removed
IIB - Involves parametrium
FIGO Stage III (irresectable)
IIIA - lower 1/3 of vagina
IIIB - pelvic sidewall/hydronephrosis/non-functioning kidney [indicative of pelvic wall
involvement with entrapment and obstruction of the ureter]
FIGO Stage IV (other organ systems
Case 12 - Female Reproductive System Page 10
IVA - Mucosa of bladder/rectum - causes rectovaginal or vesicovaginal fistula, patient becomes
incontinent with urine/faeces draining from vagina
IVB - Distant sites (e.g. liver/lung/supraclavicular LN mets)
d. Explain how staging affects the treatment of cervical carcinoma.
Treatment depends on the stage (extent of spread)
If resectable -> surgery (usually radical hysterectomy)
If irresectable -> radiation and chemotherapy
Stage IA -> 95% 5-year survival
Stage IB -> 80-90% 5-year survival
Stage II -> 75% 5-year survival
Stage III+ <50% 5-year survival
Case 12 - Female Reproductive System Page 11