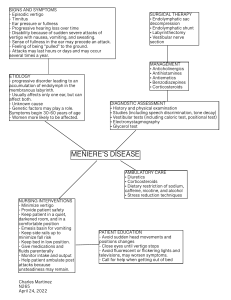
THERAPY IN PRACTICE CNS Drugs 2003; 17 (2): 85-100 1172-7047/03/0002-0085/$30.00/0 © Adis International Limited. All rights reserved. Pharmacological Treatment of Vertigo Timothy C. Hain and Mohammed Uddin Departments of Neurology, Otolaryngology and Physical Therapy and Human Movement Sciences, Northwestern University, Chicago, Illinois, USA Contents Abstract . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1. Physiology of Vertigo . . . . . . . . . . . . . . . . . . . . . . . . . . . 2. Neurochemistry of Vertigo . . . . . . . . . . . . . . . . . . . . . . . . 3. Drugs Used in the Treatment of Vertigo . . . . . . . . . . . . . . . . . 3.1 Vestibular Suppressants . . . . . . . . . . . . . . . . . . . . . . . 3.1.1 Anticholinergics . . . . . . . . . . . . . . . . . . . . . . . . . 3.1.2 Antihistamines . . . . . . . . . . . . . . . . . . . . . . . . . . 3.1.3 Benzodiazepines . . . . . . . . . . . . . . . . . . . . . . . . 3.1.4 Calcium Channel Antagonists . . . . . . . . . . . . . . . . 3.2 Antiemetics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3.3 Agents That Affect the Rate of Compensation . . . . . . . . . . 3.4 Agents of Uncertain Efficacy and Mechanism . . . . . . . . . . 4. Drug Treatment of Individual Conditions . . . . . . . . . . . . . . . . 4.1 Benign Paroxysmal Positional Vertigo . . . . . . . . . . . . . . . 4.2 Ménière’s Disease . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2.1 Episodic Treatment . . . . . . . . . . . . . . . . . . . . . . . 4.2.2 Prophylaxis . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.3 Vestibular Neuritis . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.4 Bilateral Vestibular Paresis . . . . . . . . . . . . . . . . . . . . . . 4.5 Central Vertigo . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.6 Psychogenic Vertigo . . . . . . . . . . . . . . . . . . . . . . . . . 4.7 Treatment of Undetermined and Ill-Defined Causes of Vertigo 5. Conclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Abstract . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 85 86 87 88 88 88 89 89 89 90 91 91 92 92 93 93 93 94 94 95 96 97 97 This review discusses the physiology and pharmacological treatment of vertigo and related disorders. Classes of medications useful in the treatment of vertigo include anticholinergics, antihistamines, benzodiazepines, calcium channel antagonists and dopamine receptor antagonists. These medications often have multiple actions. They may modify the intensity of symptoms (e.g. vestibular suppressants) or they may affect the underlying disease process (e.g. calcium channel antagonists in the case of vestibular migraine). Most of these agents, particularly those that are sedating, also have a potential to modulate the rate of compensation for vestibular damage. This consideration has become more relevant in recent years, as vestibular rehabilitation physical therapy is now often recommended in an attempt to promote compensation. Accordingly, therapy of vertigo is optimised when the prescriber has detailed knowledge of the pharma- 86 Hain & Uddin cology of medications being administered as well as the precise actions being sought. There are four broad causes of vertigo, for which specific regimens of drug therapy can be tailored. Otological vertigo includes disorders of the inner ear such as Ménière’s disease, vestibular neuritis, benign paroxysmal positional vertigo (BPPV) and bilateral vestibular paresis. In both Ménière’s disease and vestibular neuritis, vestibular suppressants such as anticholinergics and benzodiazepines are used. In Ménière’s disease, salt restriction and diuretics are used in an attempt to prevent flare-ups. In vestibular neuritis, only brief use of vestibular suppressants is now recommended. Drug treatments are not presently recommended for BPPV and bilateral vestibular paresis, but physical therapy treatment can be very useful in both. Central vertigo includes entities such as vertigo associated with migraine and certain strokes. Prophylactic agents (L-channel calcium channel antagonists, tricyclic antidepressants, β-blockers) are the mainstay of treatment for migraineassociated vertigo. In individuals with stroke or other structural lesions of the brainstem or cerebellum, an eclectic approach incorporating trials of vestibular suppressants and physical therapy is recommended. Psychogenic vertigo occurs in association with disorders such as panic disorder, anxiety disorder and agoraphobia. Benzodiazepines are the most useful agents here. Undetermined and illdefined causes of vertigo make up a large remainder of diagnoses. An empirical approach to these patients incorporating trials of medications of general utility, such as benzodiazepines, as well as trials of medication withdrawal when appropriate, physical therapy and psychiatric consultation is suggested. 1. Physiology of Vertigo Vertigo is the illusion of rotational motion. Most vertigo with definable cause is otological, caused by dysfunction of the rotational velocity sensors of the inner ear, the semicircular canals. For consideration of other types of vertigo, it is helpful to consider how the brain processes motion signals. In the normal situation, individuals continuously process three types of sensory input: vestibular (inner ear), visual and somatosensory. These three streams of information are combined in the central vestibular apparatus to form an estimate of orientation and motion of the head and body. Physiological and pathological vertigo is caused by asymmetrical input into the central vestibular apparatus or asymmetrical central processing.[1] Accordingly, possible sources of vertigo include all possible combinations of sensory disturbances related to motion as well as malfunction of the central vestibular apparatus. Practically, however, because the visual and somatosensory senses mainly produce position-coded signals, vertigo is © Adis International Limited. All rights reserved. only rarely a consequence of visual or somatosensory malfunction. An example of ‘visual vertigo’ might be vertigo associated with an oculomotor disturbance accompanied by nystagmus. Nevertheless, the common varieties of visual disturbance, diminished vision, double vision or disorders of the accommodation system usually do not create vertigo. Similarly, vertigo is only occasionally associated with somatosensory dysfunction, as in cervical vertigo. Central vertigo is more frequent than nonvestibular sensory vertigo but still uncommon compared with otological vertigo, as is discussed in more detail in section 4. When planning treatment, the symptom of vertigo should be differentiated from motion sickness, which is the malaise and nausea that may follow real or illusory sensations of motion. Motion sickness can be caused by a mismatch of sensory signals as well as malfunction of central structures involved in comparison between senses encoding motion. Vertigo and motion sickness are not synonymous. For example, carnival rides frequently CNS Drugs 2003; 17 (2) Treatment of Vertigo elicit illusory rotational sensations, but motion sickness can often be avoided. Also, the symptoms of motion sickness usually persist longer and tend to be more disturbing than the inciting vertigo. Again, although normal individuals experiencing similar sensory disturbances reliably experience vertigo, susceptibility to motion sickness varies remarkably. In addition, the pharmacological management of vertigo and motion sickness are clearly distinct.[2,3] Finally, when planning treatment, recovery and compensation must also be considered. Every vestibular stimulus, whether the result of natural motion or disease, has the potential to initiate a process of compensatory adaptation. The pharmacological management of compensation is distinct from that of vertigo and motion sickness and, in fact, agents that relieve vertigo or motion sickness often block compensation. There are two key concepts regarding compensation that need to be considered when planning therapy of vertigo. First, promotion of central compensation is desirable during the process of recovery from persistent vestibular imbalance, such as after a severe bout of vestibular neuritis (see section 4.3). Second, prevention of unneeded and counterproductive compensation may be desirable after a transient vestibular imbalance, such as might be caused by Ménière’s disease (see section 4.2). 2. Neurochemistry of Vertigo There are at least six neurotransmitters of the vestibular system involved in the three-neuron arc between the vestibular hair cells and oculomotor nuclei that drives the vestibulo-ocular reflex (see table I). There are also a host of other neurotransmitters that modulate function or are involved in a more minor way. Glutamate (and aspartate) is an excitatory transmitter at all three neurons in the arc.[4,5] Alphaamino-3-hydroxy-5-methylisoxazole-4-proprionic acid (AMPA)–type glutamate receptors are thought to mediate synaptic transmission, as they do in most regions of the CNS. N-methyl-D-aspartate (NMDA)– type glutamate receptors appear to contribute to © Adis International Limited. All rights reserved. 87 both maintenance of resting discharge of central vestibular neurons as well as possibly long-term modulation of synaptic transmission in the central vestibular structures.[5] Acetylcholine is both a peripheral and central agonist affecting muscarinic receptors. However, peripherally acetylcholine appears only to be involved in the brainstem efferent–hair cell synapse, which has an uncertain functional significance. Acetylcholine appears to function centrally as an excitatory neurotransmitter. Both nicotinic and muscarinic cholinergic receptors have been demonstrated in all vestibular nuclei with the highest density within the medial vestibular nuclei.[5] Local injection of cholinergic agonists into the vestibular nuclei induces a postural syndrome in intact animals that closely resembles the postural syndrome following hemilabyrinthectomy. Acetylcholine is involved with compensation. In animals that have compensated for vestibular deficits, systemic injection of cholinomimetics induces the reappearance of postural asymmetries.[6] Of five subtypes of acetylcholine receptors presently known, receptors found in the pons and medulla, presumably those involved with dizziness, are almost exclusively of the muscarinic M2 subtype.[7] γ-Aminobutyric acid (GABA) is thought to be the inhibitory neurotransmitter for the commissures in the medial vestibular nucleus as well as being the inhibitory neurotransmitter between the cerebellar Purkinje cells and lateral vestibular nucleus.[8] Stimulation of the two types of GABA receptors, GABAA and GABAB, have similar inhibitory effects on vestibular pathways.[9] Specific Table I. Neurotransmitters of the vestibular system Neurotransmitter Peripheral role Central role Glutamate Excitatory Excitatory Acetylcholine Excitatory for efferent synapse Excitatory GABA Unclear Inhibitory Dopamine Excitatory Noradrenaline (norepinephrine) Modulator Histamine Unclear GABA = γ-aminobutyric acid. CNS Drugs 2003; 17 (2) 88 GABAB agonists, such as baclofen, decrease the duration of vestibular responses in animal models.[10] GABA is also the inhibitory neurotransmitter for the vertical vestibulo-ocular system, whereas glycine serves for the horizontal vestibulo-ocular system.[11] The mechanisms of action of several other neurotransmitters known to be important targets in the pharmacological management of vertigo are less well understood. Histamine is found diffusely in central vestibular structures. Histamine does not appear to be a neurotransmitter in the peripheral vestibular system.[12] Centrally acting antihistamines modulate symptoms of motion sickness.[2] Stimulation of histamine H1 and H2 receptors excites central medial vestibular nucleus neurons.[4,5] H3 is an autoreceptor that inhibits histamine release. Noradrenaline (norepinephrine) modulates the intensity of central reactions to vestibular stimulation[13] and facilitates compensation. Centrally acting adrenergic drugs such as amphetamine and ephedrine have a prophylactic effect against motion sickness.[13] Dopamine may accelerate vestibular compensation to unilateral labyrinthectomy, and dopamine blockers may delay recovery.[14] The neurochemistry of emesis overlaps in part with the neurochemistry of vertigo and motion sickness. Acetylcholine and histamine are excitatory neurotransmitters involved in the central control of emesis.[3] GABA receptor agonists inhibit central emesis reflexes as well as cortical pathways involved in anticipatory vomiting. Dopamine is more important in emesis than vertigo as it is an excitatory central neurotransmitter in the chemoreceptor trigger zone and vomiting centre and is involved peripherally in modulating gut motility. Serotonin is also important in emesis but plays little or no role in vertigo and a minor role in motion sickness.[15,16] Selective agents that block the serotonin 5-HT3 receptor subtype reduce nausea and emesis through a combined action on central reflexes and peripheral receptors.[17] © Adis International Limited. All rights reserved. Hain & Uddin 3. Drugs Used in the Treatment of Vertigo Vestibular suppressant and antiemetic drugs are the mainstay of treatment of vertigo. 3.1 Vestibular Suppressants Vestibular suppressants are drugs that reduce nystagmus evoked by a vestibular imbalance. Conventional vestibular suppressants consist of three major drug groups: the anticholinergics, the antihistamines and the benzodiazepines (see table II). We will also discuss use of calcium channel antagonists for vestibular suppression, although their use for this purpose currently is not accepted universally. 3.1.1 Anticholinergics Anticholinergics are central vestibular suppressants that suppress firing in vestibular nucleus neurons of animals[18] and reduce the velocity of vestibular nystagmus in humans.[19-22] In spite of a study suggesting effectiveness of glycopyrrolonium bromide (glycopyrrolate) in Ménière’s disease,[23] as acetylcholine is not a peripheral neurotransmitter in vestibular afferents it seems unlikely that anticholinergics that have no central action are useful for vestibular suppression. Anticholinergics are also useful for managing motion sickness. Scopolamine, for example, increases motion tolerance.[13] Agents with central anticholinergic effects are most important, because anticholinergic drugs that do not cross the bloodbrain barrier are ineffective in controlling motion sickness.[2] Unlike antihistamines, which are discussed is section 3.1.2, pure anticholinergics are ineffective for motion sickness if administered after symptoms have already appeared. All anticholinergics conventionally used in the management of vertigo or motion sickness have prominent adverse effects, often including a dry mouth, dilated pupils and sedation. Scopolamine and atropine are nonspecific muscarinic receptor antagonists.[7] It is to be hoped that agents selective for vestibular subtypes of muscarinic receptors will eventually be developed or discovered among CNS Drugs 2003; 17 (2) Treatment of Vertigo 89 Table II. Vestibular suppressants, arranged in order of preference from most to least commonly used (oral doses unless otherwise stated) Drug Dosea Meclozine Oral tablets 12.5–50mg every 4-6h Antihistamine, anticholinergic or chewable tablets 25mg tid Sedating, precaution in prostatic enlargement Clonazepam 0.5mg bid Benzodiazepine Mildly sedating, drug dependency Scopolamine 0.5mg patch every 3 days Anticholinergic Topical allergy, precaution in glaucoma, tachyarrhythmia, prostatic enlargement Dimenhydrinate 50mg every 4–6h Antihistamine, anticholinergic Sedating, precaution in prostatic enlargement Diazepam 2–10mg (one dose) given acutely orally, IM or IV or 2mg orally bid Benzodiazepine Sedating, respiratory depressant, drug dependency, precaution in glaucoma Lorazepam 0.5mg bid Benzodiazepine Mildly sedating, drug dependency a Pharmacological class Adverse reactions Doses are all those used routinely for adults and generally will not be appropriate for children. bid = twice daily; IM = intramuscularly; IV = intravenously; tid = three times daily. our currently available pharmacopoeia, as these agents may provide vestibular suppression with fewer adverse effects. The transdermal preparation of scopolamine deserves some special comment. The transdermal delivery method has a great advantage in that it bypasses the stomach, making it effective in situations where gastric absorption may be erratic. The main problem is skin irritation, which usually precludes long-term usage. Anticholinergic adverse effects such as dry mouth and blurred vision also limit use. Occasional patients become dependent on scopolamine patches and develop withdrawal symptoms (usually nausea and vertigo) when it is discontinued.[24] 3.1.2 Antihistamines All the antihistamines in general use for control of vertigo also have substantial anticholinergic activity, and it seems likely that most or all of their vestibular suppressant effect derives from their anticholinergic action. It is well accepted, however, that centrally acting antihistamines can prevent motion sickness and reduce the severity of its symptoms even if taken after the onset of symptoms.[2] Antihistamines that do not cross the bloodbrain barrier are not used to treat vertigo. Little is known about the effect of drugs that affect histamine on vestibular compensation. In small doses, benzodiazepines are extremely useful for management of vertigo. They are also useful in prevention of motion sickness.[27] Habituation, impaired memory and increased risk of falling are the main problems. Although it has been suggested that benzodiazepine treatment might impair compensation for vestibular lesions, experimental data have not borne this out.[28] Lorazepam is a particularly useful agent because of its effectiveness and simple kinetics. Lorazepam has no active metabolites. Habituation, the biggest problem,[29] can be avoided by keeping the dose to 0.5mg twice a day or less. Lorazepam can also be taken sublingually (1mg) for an acute attack of vertigo. For brief bouts of vertigo, such as are typically found in Ménière’s disease, lorazepam usually can be discontinued after a few days. Low doses of diazepam (2mg twice a day) can be used similarly. Relatively little information is available about habituation potential and efficacy of clonazepam, but it appears as effective as a vestibular suppressant as lorazepam.[30] It is also usually prescribed in a dose of 0.5mg twice a day. The authors prefer to avoid use of alprazolam for vestibular suppression because of the potential for a difficult withdrawal syndrome. Long-acting benzodiazepines are usually not helpful for relief of vertigo. 3.1.4 Calcium Channel Antagonists 3.1.3 Benzodiazepines Benzodiazepine drugs are GABA modulators, acting centrally to suppress vestibular responses.[25,26] © Adis International Limited. All rights reserved. Calcium channel antagonists may have utility in the treatment of dizziness. Two examples of this group, flunarizine and cinnarizine, are popular CNS Drugs 2003; 17 (2) 90 Hain & Uddin antivertiginous agents outside of the USA.[31,32] Nimodipine has recently been reported as possibly effective in Ménière’s disease[33] as well as in alleviating peripheral vertigo.[34] There are several reasons why calcium channel antagonists might be of help in the management of vertigo. Some calcium channel antagonists have been shown to be vestibular suppressants.[31,35] Vestibular dark cells also contain calcium channels, suggesting the possibility that calcium channel antagonists might change ion concentration in endolymph.[36] Practically, some calcium channel antagonists, such as verapamil, have strong constipating effects, which may be helpful in managing diarrhoea caused by vestibular imbalance. Calcium channel antagonists also often have anticholinergic and/or antihistaminic activity.[37] Finally, calcium channel antagonists may be effective in ‘vestibular Ménière’s’, as individuals with this diagnosis have a high prevalence of migraine,[38] for which calcium channel antagonists are often effective.[39] positories are commonly used in outpatients who are unable to absorb oral agents because of gastric atony or vomiting. Sublingual administration is also useful. Injectables are used in the emergency room or inpatient settings. Some antihistamines commonly used as vestibular suppressants have significant antiemetic properties (e.g. meclozine). When an oral agent is appropriate, meclozine is generally the first to be used, because it rarely causes adverse effects any more severe than drowsiness. A combination of an antihistamine (doxylamine) and pyridoxine (vitamin B6) is presently marketed for nausea associated with pregnancy. Phenothiazines, such as prochlorperazine and promethazine, are effective antiemetics, probably because of their dopamine receptor antagonist activity, but they also act at other sites. For example, promethazine is also an H1 and muscarinic receptor antagonist. Because these drugs can induce significant adverse effects, such as dystonia, they are considered second-line drugs whose use should be brief and cautious. Dopamine antagonists such as the phenothiazines also have the potential to slow vestibular compensation.[14] Drugs that speed gastric emptying, such as metoclopramide, a dopamine antagonist, and powdered ginger root may be helpful in managing emesis.[40] Although metoclopramide is a potent cen- 3.2 Antiemetics Table III lists the drugs that are commonly used for control of nausea in patients with vertigo. The choice of agent depends on consideration of the route of administration and the adverse effect profile. The oral agents are used for mild nausea. SupTable III. Antiemetics for use in vertigo, arranged in alphabetical order Drug Usual adult dosea Pharmacological class Adverse reactions Granisetron 1mg orally or IV Serotonin 5-HT3 antagonist Headache Meclozine 12.5 or 25mg orally every 4–6h or tid; 25mg chewable tablet tid Antihistamine, anticholinergic Sedating, precautions in glaucoma, prostate enlargement Metoclopramide 10mg orally tid or 10mg IM Dopamine antagonist, stimulates upper gastrointestinal motility Restlessness or drowsiness, extrapyramidal Ondansetron 4mg orally or IV Serotonin 5-HT3 antagonist Headache, diarrhoea, fever Prochlorperazine 5 or 10mg IM or orally every 6–8h or 25mg rectally every 12h Phenothiazine Sedating, extrapyramidal Promethazine 25mg orally every 6–8h, 25mg rectally every 12h or 12.5mg IM every 6–8h Antihistamine Sedating, extrapyramidal Thiethylperazine 10mg orally or IM up to tid Phenothiazine Sedating, extrapyramidal Trimethobenzamide 250mg orally tid, 200mg IM tid or 200mg rectally tid Similar to phenothiazine Sedating, extrapyramidal a Doses are all those used routinely for adults and generally will not be appropriate for children. IM = intramuscularly; IV = intravenously; tid = three times daily. © Adis International Limited. All rights reserved. CNS Drugs 2003; 17 (2) Treatment of Vertigo tral antiemetic, it is ineffective in preventing motion sickness.[41] Domperidone, a peripherally acting dopamine D2 receptor antagonist, has antiemetic activity as a result of peripheral gastrokinetic action as well as central action on the chemoreceptor trigger zone. It has similar efficacy to metoclopramide combined with a more favourable safety profile.[42] It is not available in the USA. All of these medications, being dopamine antagonists, probably slow vestibular compensation. 5-HT3 antagonists such as ondansetron are highly effective antiemetics that are also sometimes effective in vestibular disorders that manifest with nausea, including some central disorders.[43] These agents do not appear to be helpful in preventing motion sickness.[15] The high cost of these agents currently limits their usefulness. 3.3 Agents That Affect the Rate of Compensation Although the manipulation of compensation ordinarily is not considered in clinical practice, it seems reasonable to do so in the interest of improving patient outcomes. If a patient has a permanent vestibular lesion, for instance an acoustic neuroma or a persistent vestibular neuritis, it may be desirable to accelerate central compensation. On the other hand, one might wish to retard compensation in individuals with a transient vestibular lesion, such as is often caused by Ménière’s syndrome, as ‘recovery’ nystagmus can be part of the clinical picture.[44,45] At this writing, there are few data regarding the effect on clinical outcomes of pharmacological agents that alter vestibular compensation.[46] Many drugs used to treat vertigo are reported to affect the rate of compensation to vestibular lesions in animal models.[46] Drugs that accelerate compensation are mainly stimulants, and drugs that retard compensation are mainly sedatives. Most, if not all, vestibular suppressants retard compensation. Dopamine agonists accelerate compensation, and antagonists slow compensation.[14] Adrenergic agonists such as ephedrine and amphetamines occasionally are used in combination with vestibular © Adis International Limited. All rights reserved. 91 suppressants.[13] Although they are most often used to counteract the sedative effects of vestibular suppressants, these stimulants may also help by promoting vestibular compensation. Amphetamines have been shown to speed recovery of motor function in stroke.[47] Calcium channel antagonists such as verapamil also may enhance compensation.[46] It seems likely that antihypertensive agents, which act through adrenergic blocking or depleting, may slow vestibular compensation. 3.4 Agents of Uncertain Efficacy and Mechanism Many substances, procedures and devices have been promoted as effective treatments of vertigo, and many of these have no clear proof of efficacy. The tendency to attribute curative properties to a bewildering number of medications and procedures has been particularly evident in the treatment of Ménière’s disease.[48,49] It seems likely that most of these agents have minor or no pharmacological efficacy, but they may function as placebos. An intriguing member of this group is betahistine. Whereas the antihistamines used in treating vertigo are usually centrally acting H1 receptor antagonists that are also muscarinic blockers (e.g. meclozine), betahistine is an H1 receptor agonist and H3 receptor antagonist.[50] It has been suggested that betahistine decouples the negative feedback loop controlling histamine release, resulting in central facilitation of histaminergic neurotransmission in the brain.[51] In therapeutic doses, administration of betahistine is associated with reduction in the gain of the vestibulo-ocular reflex.[51,52] In addition, betahistine increases blood flow to the inner ear.[53] It has also been suggested that betahistine may accelerate compensation.[54] In the USA, however, as of 2002, the US FDA does not recognise betahistine as an effective medication. A recent review concluded that there was insufficient evidence to say whether or not betahistine had an effect in Ménière’s disease.[55] Ginkgo biloba is promoted for the treatment of Alzheimer’s disease, sexual dysfunction, depresCNS Drugs 2003; 17 (2) 92 Hain & Uddin sion, headache, claudication, vertigo and tinnitus.[56] Ginkgo biloba may reduce the viscosity of the blood (literally blood thinning), and it also may be an antioxidant. A recent study suggests that Ginkgo biloba is similar in efficacy for vertigo as betahistine.[57] Like Ginkgo biloba, Vertigoheel, a homeopathic remedy, has recently been compared with betahistine and found to be equivalent.[58] Baclofen and amantadine, both centrally acting agents used generally in conditions unrelated to vertigo, are sometimes advocated for vertigo. Baclofen is most commonly used in patients in whom the diagnosis of microvascular compression of the eighth nerve is being considered. Amantadine is used in an attempt to promote compensation in individuals with brain injury.[59] As amantadine is a dopamine agonist, it seems possible that it might be useful. No formal studies of efficacy of these drugs for treatment of vertigo and related conditions are yet available. 4. Drug Treatment of Individual Conditions 4.1 Benign Paroxysmal Positional Vertigo Benign paroxysmal positional vertigo (BPPV) is the single most common type of vertigo, accounting for roughly 20% of all vertigo cases.[60] BPPV is diagnosed by combining a history of positional vertigo with a typical nystagmus pattern that appears on positional testing. It is currently thought that BPPV is caused by the presence of free otoconia or ‘canaliths’ within the semicircular canals, dislodged from the otolith organs by trauma, infection or degeneration (see figure 1). The debris moves to the lowest part of the posterior canal with changes in head position and causes vertigo and nystagmus as it tumbles. Symptoms can be very intense, but fortunately they are brief, since dizziness occurs only while the debris shifts position. Physical treatments based on manipulation of the head are the most effective treatment for BPPV.[61] Drugs are not nearly as helpful for BPPV as are physical treatments, but antiemetics can be helpful in patients whose vertiginous spells are fol© Adis International Limited. All rights reserved. lowed by nausea. Meclozine may also be an effective adjunct to the specific exercises for this condition. In this situation, meclozine is taken prior to the home exercise in an attempt to prevent motion sickness and nausea. Ondansetron can be very helpful in preventing emesis associated with diagnostic or therapeutic manoeuvres. In this situation, an oral or sublingual dose of 4–8mg is given 30 minutes prior to the manoeuvre. Vestibular suppressants that have little antiemetic activity (e.g. diazepam, lorazepam) are generally unable to reduce day-to-day symptoms of BPPV to acceptable levels. Some patients with BPPV are conditioned by the reliable appearance of vertigo with particular positions and develop a phobia related to sleeping on their back or on one side. The phobia can persist for years after the inner ear condition has resolved. This entity is called ‘phobic postural vertigo’. Phobic postural vertigo is best treated with exercises, such as the Brandt-Daroff exercises,[62] that are desensitising rather than with vestibular suppressant medications. Benzodiazepines can be helpful in individuals with phobic postural vertigo who Posterior semicircular canal Utricle Vestibule Cupulolithiasis, debris attached to cupula Canalithiasis, debris in posterior canal Fig. 1. Canalithiasis mechanism of benign paroxysmal positional vertigo (reproduced with permission from Dr T. Hain). CNS Drugs 2003; 17 (2) Treatment of Vertigo 93 otherwise might refuse to participate in the desensitisation procedures. Endolymphatic sac 4.2 Ménière’s Disease Ménière’s disease is the second most common cause of vertigo of otological origin. It is classically attributed to dilation and periodic rupture of the endolymphatic compartment of the inner ear (see figure 2). The pathognomonic symptoms include fluctuating hearing, roaring tinnitus, aural fullness and tinnitus.[63] Endolymphatic duct Utricle Saccule Stapes 4.2.1 Episodic Treatment For the episodic vertigo that is common in Ménière’s syndrome, vestibular suppressants with or without an antiemetic (table II and table III) are used to treat the acute attack, and no medications are used in the interim. These agents do nothing to correct the vestibular imbalance that causes the symptoms, but they suppress the manifestations of the imbalance (vertigo and nausea). Meclozine, diazepam, lorazepam and clonazepam are the most useful suppressant agents for mild attacks (see table II for doses). Intramuscular promethazine or prochlorperazine and intravenous diazepam are used in the emergency department or inpatient setting for treatment of severe attacks. Otherwise, nausea is managed with sublingual or suppository preparations. However, these are rarely required because most patients have some warning involving a change in hearing or aural sensation and can take meclozine or a similar preparation before the full-blown attack appears. 4.2.2 Prophylaxis There is no consensus on prophylaxis of Ménière’s syndrome,[62,64] and simply treating the symptoms is considered acceptable. No matter what prophylactic treatment is used, remission eventually occurs in 60–80% of cases.[48,49] Because of the great variability in the course of Ménière’s disease, to have adequate power a clinical trial requires very large numbers, and very few of these have been performed. However, it is common practice to advise dietary salt restriction (1–2g salt diet) and use of a mild © Adis International Limited. All rights reserved. Fig. 2. Engorged endolymphatic compartment of the inner ear in Ménière’s disease (reproduced with permission from Northwestern University, Chicago, IL, USA). diuretic such as hydrochlorothiazide/triamterene (Dyazide®1 or Maxide®), as it is felt that this regimen may reduce the frequency of attacks. It should be noted that Dyazide® may cause significant hyponatraemia, especially in the elderly and in those who are already salt restricted; in this situation, one may wish to use an every-other-day dose schedule and/or monitor serum electrolytes. The Maxide® form of the drug is scored and can be broken in half. In patients who cannot tolerate hydrochlorothiazide/ triamterene, diuretics that inhibit carbonic anhydrase, such as acetazolamide or methazolamide, are occasionally helpful. Spironolactone may be used in women with perimenstrual flare-ups. Calcium channel antagonists such as verapamil may also be helpful, although very few formal studies of efficacy are available.[33] Patients are also encouraged to avoid caffeine and stop smoking. Daily use of vestibular suppressants, as a prophylactic treatment, is generally discouraged out of concern that they may impair vestibular compensation. Some authors recommend a 1 Use of tradenames is for product identification only and does not imply endorsement. CNS Drugs 2003; 17 (2) 94 Hain & Uddin brief course of corticosteroids, especially if a surgical treatment is being considered.[65] 4.3 Vestibular Neuritis Vestibular neuritis is a monophasic, self-limited condition that presents with vertigo, nausea, ataxia and nystagmus.[66] These symptoms are brought about by an acute imbalance in vestibular tone combined with directionally asymmetrical response to head rotation. Vestibular neuritis is thought to be caused by a viral infection of the vestibular portion of the eighth cranial nerve. Mumps and various types of herpes viruses are possible infectious agents. A peculiar aspect of this condition is that hearing is not impaired; the viral infection is hypothesised to selectively affect vestibular fibres of the eighth nerve, sparing the neighbouring fibres carrying cochlear information. When hearing is also affected, the syndrome is termed ‘labyrinthitis’. Similar presentations can arise from noninfectious aetiologies, such as vascular compromise. Evidence suggests that almost all patients with vestibular neuritis have satisfactory resolution of their symptoms as a result of a combination of recovery of function and central compensation.[66] Severe distress associated with constant vertigo, nausea and malaise usually lasts 2 or 3 days. Many patients are ready to return to their regular activities after a week, and it is likely that in these instances there has been only a transient and incomplete vestibular lesion. However, a substantial proportion of patients may take as long as 2 months to improve. On subsequent testing, this group often is demonstrated to have a continued unilateral paralysis of vestibular function. Unfortunately, it is not possible to predict whether a patient will have a transient vestibular imbalance and recover quickly or a permanent loss of function associated with a poorer prognosis. The implication for treatment is that if a permanent vestibular imbalance is made more tolerable by a vestibular suppressant medication or if central compensation is partially blocked by a benzodiazepine or agent with dopamine receptor blocking activity, © Adis International Limited. All rights reserved. the patient may not recover as rapidly as otherwise. Even bedrest may be poorly conceived, since animal studies have shown that immobilisation delays recovery from experimental vestibular lesions.[67] Thus, the treatment strategy for vestibular neuritis involves use of as few medications as possible and encouraging activity as much as is practical. In the first few days of the illness, patients usually severely restrict their activities, as rapid head movements and activities such as sitting up or turning over in bed may cause increased vertigo. Vestibular suppressants and antiemetics are commonly used at this point, prescribed as suppositories if necessary. By the third day, it is usually possible to greatly reduce usage of vestibular suppressants, and the patient should be encouraged to increase activity as tolerated. Most patients recover completely within 2 months. Those that do not usually have a significant fixed vestibular paresis combined with central dysfunction that slows their compensation. For example, patients with alcoholic cerebellar degeneration or individuals of advanced age may recover much more slowly.[68,69] Such patients can benefit from a programme of physical therapy incorporating gait training and visual-vestibular exercises. Surgical treatment is not indicated for vestibular neuritis. 4.4 Bilateral Vestibular Paresis Bilateral vestibular paresis presents with oscillopsia, ataxia and mild vertigo.[70] Typically, patients have recently been treated for a serious infection, most often osteomyelitis or peritonitis. The infection is treated for several weeks with an ototoxic antibacterial (of which gentamicin is the most commonly encountered). The symptoms of bilateral vestibular paresis, ataxia and oscillopsia manifest themselves when the patient recovers from their infection and tries to walk. When examined, these patients can read the vision chart with their head still but lose at least four lines of acuity when their head is gently oscillated from side to side. They are unable to stand in the tandem Romberg position (heel to toe, arms crossed) CNS Drugs 2003; 17 (2) Treatment of Vertigo with eyes closed for 6 seconds. Hearing is generally little affected. Rotatory chair testing is the best way to confirm this diagnostic impression. The long-term prognosis of patients with ototoxicity is only fair. A lengthy exposure to an aminoglycoside antibacterial such as gentamicin can cause a loss of vestibular hair cells.[71] As there is no mechanism for hair cell regeneration in humans, the loss is permanent. Nevertheless, unless there is a superimposed cerebellar lesion, substantial recovery is the rule. Most patients return to productive work within 1–2 years of exposure, although they continue to have impaired balance in situations where other senses are not informative, such as in the dark or while walking on an uneven surface. Recovery is felt to be a result of a combination of CNS plasticity and sensory substitution.[72] It is important to note that medications that reduce symptoms of other forms of otological vertigo, such as the vestibular suppressants and most antiemetics, generally make symptoms worse in bilateral vestibular paresis. Vestibular suppressants must be eliminated in the management of this condition. It is also prudent to avoid medications with potential vestibular suppressant activity, such as calcium channel antagonists, and those that have central anticholinergic adverse effects (e.g. many of the tricyclic antidepressants). Patients should be warned to avoid subsequent exposure to ototoxic drugs, especially gentamicin and loop diuretics (e.g. furosemide, bumetanide and ethacrynic acid). If a loop diuretic is necessary, bumetanide is the least ototoxic.[73] These patients should also be advised to avoid loud noises, as they are likely to be more vulnerable to noise-induced hearing loss than the general population. Theoretically, in individuals with some remaining vestibular function, medications that promote central plasticity might be helpful in treating bilateral vestibular paresis, and those that retard compensation, such as dopamine antagonists, would slow or prevent recovery. Bilateral vestibular paresis often responds well to physical therapy. No surgical treatment is cur© Adis International Limited. All rights reserved. 95 rently available for bilateral vestibular loss. Prosthetic devices are presently being developed. 4.5 Central Vertigo Vertigo caused by CNS dysfunction, or ‘central vertigo’, is unusual. In the emergency room setting or otolaryngology clinic, a central cause of vertigo is identified in less than 5% of cases. Even in neurology settings, central vertigo typically accounts for only about 20% of diagnoses in patients complaining of vertigo.[74] Central vertigo is largely caused by vascular disorders. In the authors’ experience, vertigo associated with migraine, stroke or transient ischaemia accounts for the majority of cases of central vertigo. A large number of individual miscellaneous neurological disorders, such as seizures, multiple sclerosis, posterior fossa tumours and the Arnold-Chiari malformation, make up the remainder. In central vertigo, a prolonged duration of symptoms is common. Although patients with peripheral vestibular imbalance typically recover within days to months, patients with central vertigo may continue to be distressed by ataxia, nausea and the illusion of motion for years. Presumably, the persistence of symptoms in patients with central vertigo reflects a defect in the central mechanisms that usually compensate for vestibular lesions. A combination of headache and vertigo is a common presentation, particularly in women in their mid-30s. In most instances, these symptoms are caused by vertebrobasilar migraine, and a prophylactic drug should be tried. [75] A sustainedrelease preparation of verapamil 120mg is often effective.[39] If the patient does not tolerate verapamil (constipation is the most common problem), a trial of amitriptyline can be made. When treating vertigo, amitriptyline is favoured over the newer selective serotonin reuptake inhibitor (SSRI) family of antidepressant medications because of its anticholinergic and antihistamine activity. Pizotifen, an antihistamine with a chemical structure similar to the tricyclic antidepressants, can also be effective.[76] β-Blockers form the third line of treatment, CNS Drugs 2003; 17 (2) 96 Hain & Uddin but do not have the vestibular suppressant effects of verapamil and amitriptyline.[77] Valproic acid can be used for migraine prophylaxis, but adverse effects, including weight gain and hair loss, limits its usefulness.[77] Some authors have suggested that acetazolamide therapy may also be effective in this situation, but its significant adverse effects limit its usefulness.[78] Another common presentation of central vertigo is in patients with a known central lesion, for whom the goal is to reduce symptoms of vertigo or ataxia. Benzodiazepines such as lorazepam, clonazepam and diazepam are frequently helpful (see table II for doses), but one must be wary of habituation and physical dependence.[79] Meclozine taken in a dose of 25mg twice daily is occasionally successful. Dopamine blockers such as prochlorperazine can be tried. The antiemetic ondansetron may be helpful when central vertigo does not respond to the usual agents.[80] Similarly, occasional patients with oculomotor signs localising to the vestibulocerebellum are helped by acetazolamide therapy.[81] Carbamazepine or oxcarbazepine, in doses appropriate for neuralgia or epilepsy, can be tried in patients having vertigo combined with an abnormal EEG or brief episodic symptoms, ‘quick spins’, that have not responded to other medications. Gabapentin, a glutamate blocker, may also be used in this situation.[82] Baclofen is used similarly. In this situation, also called ‘vestibular paroxysmia’, one might be treating epilepsy, microvascular compression of the eighth nerve, irritation of the vestibular nerve caused by a neurotrophic virus, postsurgical vestibular neuralgia or intrinsic brainstem lesions.[83] Gabapentin is also generally useful as a suppressor of nystagmus.[82] Physical therapy emphasising effective use of appliances such as canes, walkers and footwear is often useful. 4.6 Psychogenic Vertigo Psychogenic vertigo is vertigo that is caused by an independently diagnosable psychiatric problem such as anxiety, depression, somatisation or malin© Adis International Limited. All rights reserved. gering. Psychiatric-associated vertigo is the coexistence of an organic vertigo with an independently diagnosable psychiatric condition, such as anxiety, which might be comorbid or reactive. Often ‘dizziness’ is a more appropriate term to use in this situation than ‘vertigo’, as these patients may not be able to define their symptoms in terms of an inappropriate movement of the environment, but rather use terms such as ‘light-headed’ or ‘woozy’. Because of inadequacies of our diagnostic methodology, it is difficult to determine the proportion of these patients in the ‘dizzy’ population as it presents to the clinician or at large in the population. Some authors indicate that as many as 50% of all patients with dizziness have a ‘functional’ source of complaints.[84] However, this large percentage results from an algorithm where patients with no findings on testing were assigned this diagnosis. This process is obviously fraught with peril, given that patients for whom the diagnostic process may have failed are placed in the same category as those who do indeed have a psychological origin of symptoms. In the first author’s practice, only about 5% of patients are assigned the ‘psychogenic’ diagnosis. A high proportion of patients with chronic (organic) vertigo develop secondary reactive psychiatric complications such as panic disorder and depression, which are important to treat on their own merits. Treatment is based on the psychiatric diagnosis. Anxiety and panic are the most common diagnoses, and benzodiazepines are the mainstay of treatment. As considerably larger doses of these medications are needed for anxiety than for vestibular suppression, and because it is likely that these patients will need long-term treatment, psychiatric referral can be very useful in these cases. SSRIs can also be used, but they are less useful. Although they have an advantage over the benzodiazepines in that they are not habituating, SSRIs are not as reliable as the benzodiazepines for management of anxiety, and they can also contribute to nausea and ataxia.[85,86] CNS Drugs 2003; 17 (2) Treatment of Vertigo Depression is an extremely unusual cause of vertigo. When it is very clear that depression is significant, one of the SSRI family, such as sertraline, may be used. These agents can result in some minor nausea as well as increase anxiety, and for this reason should be used with caution.[87,88] Almost all antidepressants increase ataxia.[89,90] Somatisation syndrome and malingering are also commonly encountered in patients with a potentially disabling but subjective symptom such as dizziness. No drug treatments are available for either diagnosis. In these situations, the clinician’s goal is to reduce inappropriate expense and use of healthcare resources. 4.7 Treatment of Undetermined and Ill-Defined Causes of Vertigo Regardless of whether one is practising in the emergency room, otolaryngology clinic, neurology clinic or a general medical setting, variants of unlocalisable diagnoses such as ‘unknown diagnosis’, ‘vasovagal’ syncope, ‘hyperventilation syndrome’, ‘post-traumatic vertigo’ and ‘nonspecific’ dizziness are the most common single ‘cause’ of dizziness reported. Between 38 and 52% of diagnoses fall in this category across many series.[74,84,91,92] The unifying feature of these diagnoses is the lack of abnormality on otological and neurological examinations. Treatment is necessarily empirical in vertigo of undetermined origin. In the first author’s practice, we ask the patient to log their symptoms on a calendar. Next, for patients already taking medication, we withdraw drugs that could affect the vestibular system, recording symptoms over 2 or more weeks. This strategy may identify individuals with ataxia caused by medication. One must be very careful in this situation not to eliminate a medication critical to the patient’s well being. For example, when one withdraws an antihypertensive such as a calcium channel antagonist that has vasodilator properties, angina may be precipitated. Several drugs are then tried. If the patient does not respond to daily meclozine, this may be replaced by a small dose of clonazepam or lorazepam. © Adis International Limited. All rights reserved. 97 It is generally difficult to exclude mild Ménière’s disease, and salt restriction and a diuretic such as hydrochlorothiazide/triamterene may be tried. A trial of migraine prophylaxis with sustained-release verapamil (120mg of a sustained-release preparation each morning) is sometimes helpful in patients with dizziness and headaches or patients with the diagnosis of ‘vestibular Ménière’s’. Carbamazepine or oxcarbazepine is tried for the symptom of ‘quick spins’ alluded to in section 4.5. Gabapentin is also a reasonable drug to try empirically for central vertigo. Patients who do not respond to the above regimens are followed at 3- to 6-month intervals and undergo yearly audiometric screenings. This is important, as occasionally the symptoms of individuals with small acoustic neuromas or early Ménière’s disease will evolve into an identifiable clinical presentation. It is often helpful to re-examine patients quickly when there is an acute flare of symptoms, as in this way one can sometimes diagnose intermittent conditions that can have normal intercurrent examinations, such as BPPV and Ménière’s disease. 5. Conclusion Vertigo is caused by several broad categories of illness. The most common forms of otological vertigo are BPPV, Ménière’s disease, vestibular neuritis and ototoxicity. Treatment of these disorders may be very effective but depends critically on attaining the correct diagnosis. Central vertigo has a poorer prognosis than otological vertigo, and the approach to treatment is largely empirical. Psychogenic vertigo is difficult to diagnose, and the treatment approach critically depends on the diagnosis. Psychiatric referral will be needed in many of these cases. The treatment of patients with dizziness of unknown cause is also empirical. An organised and methodical approach to management of these patients is essential to maximise patient satisfaction. CNS Drugs 2003; 17 (2) 98 Hain & Uddin Acknowledgements The authors have provided no information on sources of funding or on conflicts of interest directly relevant to the content of this review/study. 20. 21. References 1. Baloh RW, Honrubia V. Clinical neurophysiology of the vestibular system. Contemp Neurol Ser 1979; 18: 1-21 2. Takeda N, Morita M, Hasegawa S, et al. Neurochemical mechanisms of motion sickness. Am J Otolaryngol 1989; 10 (5): 351-9 3. Takeda N, Morita M, Hasegawa S, et al. Neuropharmacology of motion sickness and emesis: a review. Acta Otolaryngol Suppl 1993; 501: 10-5 4. Serafin M, Khateb A, Waele C, et al. In vitro properties of medial vestibular neurones. In: Shimazu H, Shinoda Y, editors. Vestibular and brain stem control of eye, head, and body movements. Basel: Karger AG, 1992: 111-21 5. de Waele C, Muhlethaler M, Vidal PP. Neurochemistry of the central vestibular pathways. Brain Res Brain Res Rev 1995; 20 (1): 24-46 6. Bienhold H, Flohr H. Role of cholinergic synapses in vestibular compensation. Brain Res 1980; 195 (2): 476-8 7. Barton JJ, Huaman AG, Sharpe JA. Muscarinic antagonists in the treatment of acquired pendular and downbeat nystagmus: a double-blind, randomized trial of three intravenous drugs. Ann Neurol 1994; 35 (3): 319-25 8. Smith PF, Darlington CL. Pharmacology of the vestibular system. Baillieres Clin Neurol 1994; 3 (3): 467-84 9. Van Neerven J, Pompeiano O, Collewijn H. Depression of the vestibulo-ocular and optokinetic responses by intrafloccular microinjection of GABA-A and GABA-B agonists in the rabbit. Arch Ital Biol 1989; 127 (4): 243-63 10. Cohen B, Helwig D, Raphan T. Baclofen and velocity storage: a model of the effects of the drug on the vestibulo-ocular reflex in the rhesus monkey. J Physiol 1987; 393: 703-25 11. Spencer RF, Wang SF, Baker R. The pathways and functions of GABA in the oculomotor system. Prog Brain Res 1992; 90: 307-31 12. Smith PF, Darlington CL. Recent advances in the pharmacology of the vestibulo-ocular reflex system. Trends Pharmacol Sci 1996; 17 (11): 421-7 13. Wood CD. Antimotion sickness and antiemetic drugs. Drugs 1979; 17 (6): 471-9 14. Petrosini L, Dell’Anna ME. Vestibular compensation is affected by treatment with dopamine active agents. Arch Ital Biol 1993; 131 (2-3): 159-71 15. Stott JR, Barnes GR, Wright RJ, et al. The effect on motion sickness and oculomotor function of GR 38032F, a 5-HT3receptor antagonist with anti-emetic properties. Br J Clin Pharmacol 1989; 27 (2): 147-57 16. Okada F, Torii Y, Saito H, et al. Antiemetic effects of serotonergic 5-HT1A-receptor agonists in Suncus murinus. Jpn J Pharmacol 1994; 64 (2): 109-14 17. Endo T, Minami M, Hirafuji M, et al. Neurochemistry and neuropharmacology of emesis: the role of serotonin. Toxicology 2000; 153 (1-3): 189-201 18. Kirsten EB, Schoener EP. Action of anticholinergic and related agents on single vestibular neurones. Neuropharmacology 1973; 12 (12): 1167-77 19. Pyykko I, Schalen L, Jantti V. Transdermally administered scopolamine vs. dimenhydrinate. I: effect on nausea and vertigo © Adis International Limited. All rights reserved. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. in experimentally induced motion sickness. Acta Otolaryngol 1985; 99 (5-6): 588-96 Pyykko I, Padoan S, Schalen L, et al. The effects of TTSscopolamine, dimenhydrinate, lidocaine, and tocainide on motion sickness, vertigo, and nystagmus. Aviat Space Environ Med 1985; 56 (8): 777-82 Pyykko I, Schalen L, Matsuoka I. Transdermally administered scopolamine vs. dimenhydrinate. II: effect on different types of nystagmus. Acta Otolaryngol 1985; 99 (5-6): 597-604 Shojaku H, Watanabe Y, Ito M, et al. Effect of transdermally administered scopolamine on the vestibular system in humans. Acta Otolaryngol Suppl 1993; 504: 41-5 Storper IS, Spitzer JB, Scanlan M. Use of glycopyrrolate in the treatment of Meniere’s disease. Laryngoscope 1998; 108 (10): 1442-5 Feder RE. Transdermal scopolamine withdrawal syndrome [letter]. Clin Neuropharmacol 1999; 22 (2): 120 Padoan S, Korttila K, Magnusson M, et al. Reduction of gain and time constant of vestibulo-ocular reflex in man induced by diazepam and thiopental. J Vestib Res 1990; 1 (1): 97-104 Blair SM, Gavin M. Modifications of vestibulo-ocular reflex induced by diazepam: experiments in the macaque. Arch Otolaryngol 1979; 105 (12): 698-701 McClure JA, Lycett P, Baskerville JC. Diazepam as an antimotion sickness drug. J Otolaryngol 1982; 11 (4): 253-9 Martin J, Gilchrist DP, Smith PF, et al. Early diazepam treatment following unilateral labyrinthectomy does not impair vestibular compensation of spontaneous nystagmus in guinea pig. J Vestib Res 1996; 6 (2): 135-9 Funderburk FR, Griffiths RR, McLeod DR, et al. Relative abuse liability of lorazepam and diazepam: an evaluation in ‘recreational’ drug users. Drug Alcohol Depend 1988; 22 (3): 215-22 Halmagyi M. Vertigo and vestibular disorders. In: Eadie MJ, editor. Drug therapy in neurology. Edinburgh: Churchill Livingstone, 1992: 375-85 Lee JA, Watson LA, Boothby G. Calcium antagonists in the prevention of motion sickness. Aviat Space Environ Med 1986; 57 (1): 45-8 Verspeelt J, De Locht P, Amery WK. Postmarketing study of the use of flunarizine in vestibular vertigo and in migraine. Eur J Clin Pharmacol 1996; 51 (1): 15-22 Lassen LF, Hirsch BE, Kamerer DB. Use of nimodipine in the medical treatment of Meniere’s disease: clinical experience. Am J Otol 1996; 17 (4): 577-80 Pianese CP, Hidalgo LO, Gonzales RH, et al. New approaches to the management of peripheral vertigo: efficacy and safety of two calcium antagonists in a 12-week, multinational, doubleblind study. Otol Neurotol 2002; 23 (3): 357-63 Aoki M, Ito Y, Miyata H. Prevention of vestibular deafferentationinduced spontaneous nystagmus with pretreatment of Ca2+ channel/N-methyl-D-aspartic acid receptor antagonists in guinea pigs. Acta Otolaryngol 1998; 118 (4): 554-6 Takeuchi S, Marcus DC, Wangemann P. Maxi K+ channel in apical membrane of vestibular dark cells. Am J Physiol 1992; 262 (6 Pt 1): C1430-6 Rascol O, Clanet M, Montastruc JL. Calcium antagonists and the vestibular system: a critical review of flunarizine as an antivertigo drug. Fundam Clin Pharmacol 1989; 3: 79s-87s Rassekh CH, Harker LA. The prevalence of migraine in Meniere’s disease. Laryngoscope 1992; 102 (2): 135-8 Solomon GD, Steel JG, Spaccavento LJ. Verapamil prophylaxis of migraine: a double-blind, placebo-controlled study. JAMA 1983; 250 (18): 2500-2 CNS Drugs 2003; 17 (2) Treatment of Vertigo 40. Grontved A, Brask T, Kambskard J, et al. Ginger root against seasickness: a controlled trial on the open sea. Acta Otolaryngol 1988; 105 (1-2): 45-9 41. Kohl RL. Failure of metoclopramide to control emesis or nausea due to stressful angular or linear acceleration. Aviat Space Environ Med 1987; 58 (2): 125-31 42. Barone JA. Domperidone: a peripherally acting dopamine2receptor antagonist. Ann Pharmacother 1999; 33 (4): 429-40 43. Macleod AD. Ondansetron in multiple sclerosis. J Pain Symptom Manage 2000; 20 (5): 388-91 44. Bance M, Mai M, Tomlinson D, et al. The changing direction of nystagmus in acute Meniere’s disease: pathophysiological implications. Laryngoscope 1991; 101 (2): 197-201 45. McClure JA, Copp JC, Lycett P. Recovery nystagmus in Meniere’s disease. Laryngoscope 1981; 91 (10): 1727-37 46. Smith PF, Darlington CL. Can vestibular compensation be enhanced by drug treatment? A review of recent evidence. J Vestib Res 1994; 4 (3): 169-79 47. Crisostomo EA, Duncan PW, Propst M, et al. Evidence that amphetamine with physical therapy promotes recovery of motor function in stroke patients. Ann Neurol 1988; 23 (1): 94-7 48. Torok N. Old and new in Meniere disease. Laryngoscope 1977; 87 (11): 1870-7 49. Ruckenstein MJ, Rutka JA, Hawke M. The treatment of Meniere’s disease: Torok revisited. Laryngoscope 1991; 101 (2): 211-8 50. Fischer AJ. Histamine in the treatment of vertigo. Acta Otolaryngol Suppl 1991; 479: 24-8 51. Kingma H, Bonink M, Meulenbroeks A, et al. Dose-dependent effect of betahistine on the vestibulo-ocular reflex: a doubleblind, placebo controlled study in patients with paroxysmal vertigo. Acta Otolaryngol 1997; 117 (5): 641-6 52. Botta L, Mira E, Valli S, et al. Effects of betahistine on vestibular receptors of the frog. Acta Otolaryngol 1998; 118 (4): 519-23 53. Dziadziola JK, Laurikainen EL, Rachel JD, et al. Betahistine increases vestibular blood flow. Otolaryngol Head Neck Surg 1999; 120 (3): 400-5 54. Colletti V. Medical treatment in Meniere’s disease: avoiding vestibular neurectomy and facilitating postoperative compensation. Acta Otolaryngol Suppl 2000; 544: 27-33 55. James AL, Burton MJ. Betahistine for Meniere’s disease or syndrome [CD001873]. The Cochrane Database Systematic Reviews. Available in the Cochrane Library [database on disk and CD ROM]. The Cochrane Collaboration; issue 1. Oxford: Oxford Update Software, 2001 56. Kanigel R. Why patients take Ginkgo. Hippocrates 1999 Oct: 11-3 57. Cesarani A, Meloni F, Alpini D, et al. Ginkgo biloba (EGb 761) in the treatment of equilibrium disorders. Adv Ther 1998; 15 (5): 291-304 58. Weiser M, Strosser W, Klein P. Homeopathic vs conventional treatment of vertigo: a randomized double-blind controlled clinical study. Arch Otolaryngol Head Neck Surg 1998; 124 (8): 879-85 59. Shiller AD, Burke DT, Kim HJ, et al. Treatment with amantadine potentiated motor learning in a patient with traumatic brain injury of 15 years’ duration. Brain Inj 1999; 13 (9): 715-21 60. Brandt T. Vertigo: its multisensory syndromes. London: Springer-Verlag, 1991: 17, 48-9 61. Brandt T. Benign paroxysmal positioning vertigo. Adv Otorhinolaryngol 1999; 55: 169-94 © Adis International Limited. All rights reserved. 99 62. Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol 1980; 106 (8): 484-5 63. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere’s disease: American Academy of Otolaryngology – Head and Neck Foundation, Inc. Otolaryngol Head Neck Surg 1995; 113: 181-5 64. Brandt T, Steddin S, Daroff RB. Therapy for benign paroxysmal positioning vertigo, revisited. Neurology 1994; 44 (5): 796-800 65. Shea Jr JJ. Classification of Meniere’s disease. Am J Otol 1993; 14 (3): 224-9 66. Bergenius J, Borg E. Audio-vestibular findings in patients with vestibular neuritis. Acta Otolaryngol 1983; 96 (5-6): 389-95 67. Lacour M, Roll JP, Appaix M. Modifications and development of spinal reflexes in the alert baboon (Papio papio) following an unilateral vestibular neurotomy. Brain Res 1976; 113 (2): 255-69 68. Furman JM, Balaban CD, Pollack IF. Vestibular compensation in a patient with a cerebellar infarction. Neurology 1997; 48 (4): 916-20 69. Barion U, Andretta M. Compensation mechanisms after acute peripheral disorders of the labyrinth as a function of age. Acta Otorhinolaryngol Belg 1988; 42 (1): 28-34 70. JC. Living without a balancing mechanism. N Engl J Med 1952; 246: 458-60 71. Hinojosa R, Nelson EG, Lerner SA, et al. Aminoglycoside ototoxicity: a human temporal bone study. Laryngoscope 2001; 111 (10): 1797-805 72. Minor LB. Gentamicin-induced bilateral vestibular hypofunction. JAMA 1998; 279 (7): 541-4 73. Oliveira J. Audiovestibular toxicity of drugs. Vol. II. Boca Raton (FL): CRC Press, 1989 74. Drachman DA, Hart CW. An approach to the dizzy patient. Neurology 1972; 22 (4): 323-34 75. Bikhazi P, Jackson C, Ruckenstein MJ. Efficacy of antimigrainous therapy in the treatment of migraine-associated dizziness. Am J Otol 1997; 18 (3): 350-4 76. Diener HC, Kaube H, Limmroth V. A practical guide to the management and prevention of migraine. Drugs 1998; 56 (5): 811-24 77. Diener HC, Limmroth V. Advances in pharmacological treatment of migraine. Expert Opin Investig Drugs 2001; 10 (10): 1831-45 78. Vahedi K, Taupin P, Djomby R, et al. Efficacy and tolerability of acetazolamide in migraine prophylaxis: a randomised placebo-controlled trial. J Neurol 2002; 249 (2): 206-11 79. Juergens S. Alprazolam and diazepam: addiction potential. J Subst Abuse Treat 1991; 8 (1-2): 43-51 80. Rice GP, Ebers GC. Ondansetron for intractable vertigo complicating acute brainstem disorders. Lancet 1995; 345 (8958): 1182-3 81. Baloh RW, Winder A. Acetazolamide-responsive vestibulocerebellar syndrome: clinical and oculographic features. Neurology 1991; 41 (3): 429-33 82. Averbuch-Heller L, Tusa RJ, Fuhry L, et al. A double-blind controlled study of gabapentin and baclofen as treatment for acquired nystagmus. Ann Neurol 1997; 41 (6): 818-25 83. Lawden MC, Bronstein AM, Kennard C. Repetitive paroxysmal nystagmus and vertigo. Neurology 1995; 45 (2): 276-80 84. Afzelius LE, Henriksson NG, Wahlgren L. Vertigo and dizziness of functional origin. Laryngoscope 1980; 90 (4): 649-56 CNS Drugs 2003; 17 (2) 100 85. Spigset O. Adverse reactions of selective serotonin reuptake inhibitors: reports from a spontaneous reporting system. Drug Saf 1999; 20 (3): 277-87 86. Trindade E, Menon D, Topfer LA, et al. Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. CMAJ 1998; 159 (10): 1245-52 87. Kyle CJ, Petersen HE, Overo KF. Comparison of the tolerability and efficacy of citalopram and amitriptyline in elderly depressed patients treated in general practice. Depress Anxiety 1998; 8 (4): 147-53 88. Brauer HR, Nowicki PW, Catalano G, et al. Panic attacks associated with citalopram. South Med J 2002; 95 (9): 1088-9 89. Ensrud KE, Blackwell TL, Mangione CM, et al. Central nervous system-active medications and risk for falls in older women. J Am Geriatr Soc 2002; 50 (10): 1629-37 © Adis International Limited. All rights reserved. Hain & Uddin 90. Cumming RG. Epidemiology of medication-related falls and fractures in the elderly. Drugs Aging 1998; 12 (1): 43-53 91. Herr RD, Zun L, Mathews JJ. A directed approach to the dizzy patient. Ann Emerg Med 1989; 18 (6): 664-72 92. Sloane PD. Dizziness in primary care: results from the National Ambulatory Medical Care Survey. J Fam Pract 1989; 29 (1): 33-8 Correspondence and offprints: Dr Timothy C. Hain, Departments of Neurology, Otolaryngology and Physical Therapy/ Human Movement Science, Northwestern University, 645 N. Michigan, Suite 1100, Chicago, IL 60611, USA. E-mail: t-hain@northwestern.edu CNS Drugs 2003; 17 (2)