lOMoARcPSD|8263507
Pharm-100-full-notes
Introductory Pharmacology (Queen's University)
StuDocu is not sponsored or endorsed by any college or university
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Lesson A1: History of Drug Use and Development
Objectives:
1. Describe how many of our important drugs arose through a study of poisons
2. Describe how some drugs arose from a study of plant materials that had medicinal uses
3. Describe development of antibacterial and anaesthetic agents
DRUGS INFLUENCE OF RELIGION
- Intoxicating substances from plants were used by medicine men (physician and priest)
to alter state of consciousness and facilitate communication with god
- Psilocybe mushroom contains psilocybin and psilocin – alter conciousness (Mexico)
- Peyote Cactus contains mescaline (North America) – causes hallucinations and
distorts perception
DRUGS INFLUENCE OF POISONS
- “All substances are poisons…. The right dose differentiates a poison and a remedy”
- Calabar Bean – used in ordeal trials in west/central Africa to identify sorcerers. The
drug physostigmine is derived from the Calabar bean. It is used to treat glaucoma
- Curare – used on spears to paralyze and kill animals. Combines with muscle receptors
usually reserved for acetylcholine which causes muscles to contract: prevents the
muscle from contraction. Used as an anaesthetic to keep muscle in relaxed state
- Ergot - fungus that grows on ears of rye and is poisonous to people (killed 20 000 in
Russia when found on the bread)
- Ergot Poisoning Symptoms
1. Burning in limbs “St. Anthony’s Fire”
2. Constriction of blood vessels: fingers, toes, limbs became starved of
blood and die
3. Mental Frenzy, hallucinations, convulsions: resemble LSD in structure
4. Abortion: violent contractions of uterus
- Ergotamine: used in treatment of migraine – migraine are caused by
pulpatation of blood vessels which carry blood to head. Ergotamine constricts
these blood vessesls and reduces the amplitude of the pulsation
- Ergonovine No longer used to hasten birth too risky. Used in obstetrics after
the baby is born to arrest the bleeding that occurs after the placenta has been
separated from the uteran wall. Arrest bleeding after childbirth
DRUGS AND ANCIENT CIVILIZATIONS
Early Chinese Medicine
- Ma Huang: “medium drug” used for coughs, influenza, and fevers. Now ephedrineused for asthma and other conditions
Early Egypt Medicine
- Pugatives: drugs used to cause bowel movements that were recommended were
castor oil, figs and senna - products with senna still available today
- Ebers Papyrus: Papyrus that was intended to be a textbook of drug use for medical
students
Early Greek Medicine
- Opium Poppy: contains OPIUM contains 10% morphine and 0.5% codeine
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Morphine: gold standard for analgesic (pain-relief) – can be chemically converted to
heroin. Morphine acts by combinging with receptors in the nervous system normally
utilized by pain-relieving chemicals enkephalins and endorphins
- Codiene – widely used for pain relief – in Tylenol 1
Spain, Persia, Mesopotamia (Iraq)
- Colchicum plant: used to treat gout. Colchicine has been extracted and used for
treatment of gout still
DRUG DISCOVERY (18TH 19TH 20TH CENTURY)
Digitalis Purpurea (foxglove) plant used to treat patients with heart disease. Helps improve
the work of the heart muscle (able to pump blood out) digoxin (Lanoxin) is the major pure
component that is now used to treat patients.
Nitroglycerin:
- initially, amyl nitrate was used in the treatment of angina pectoris (choking in chest),
however the effects were short lived.
- Nitroglycerin is a chemically related compound to amyl nitrate but has greater
duration and similar effect. The pain occurs because of insufficient oxygen to the heart
muscle. Nitroglycerin dilates blood vessels in the heart and elsewhere which brings
more oxygen in
Quinine – bark of the Cinchona Tree in south America Used therapeutically. Now used to
treat malaria. Quinidine (relative of Quinine) used to treat disorders of heart rhythms
(arrythmia)
DRUG ACTING ON THE BRAIN
Rauwolfia plant: used in Indian medicine to reduce tension, anxiety, and blood pressure.
Isolated Reserpine and used to treat excitable mental patients to change their behavior.
Proble – difficult to find the correct dose. Still the valuable for treating hypertension
Chlorpromazine: preferred for the management of mentally ill patients compared to
chlorpromazine. Synthetic substance makes people become tranquil. Helped drop the number
of mentally ill patients in special homes because they can go home.
Lysergic Acid Diethylamide (LSD):synthesized substance based on the components of ergot.
Albert Hoffmann accidently ingested some during his research on it’s hallucinogenic effect.
CHEMOTHERAPEUTIC AGENTS TIMELINE
1854 Paul Ehrlich: “father of chemotherapy”. Designed complexes of arsenic and
organoarsenicals (organic molecules) which selectively bind to parasites. Lead to a cure of
syphilis
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1930s Gerhard Domagk introduced sulfa drugsb – the first successful synthetic drug
for treatment of bacterial diseases
1929 -` (40s) Alexander Fleming discovered the first antibiotic penicillin (during WW2)
major use was in therapy of disease caused by gram-positive bacteria
1943 Selman Waksman discovered streptomycin – turning point for chemotherapy of
tuberculosis and diseases caused by gram-negative bacteria
ANAESTHESIA
1800 Humphrey Davy showed that nitrous oxide could prevent pain and suggested it be
tried in surgery – did not try for 42 years (!842)
1842 Colton gave public demonstrations of nitric oxides effect on people’s behaviors
(laughing gas) and a dentist Wells noticed that a participant at the demonstration gashed
his leg and did not feel the pain = wanted to use for his patients – “ A new era of tooth pulling”
1818 Faraday notied that Ether had similar properties to Nitric Oxide – medical students
used it at parties for ether parties or jags
Morton was associated with Wells in dentristry and retained an interest in anaesthesia –
practiced on himself and animals. Requested to try it during a surgical procedure First
operation with anaesthetic at Massechusetts General Hospital
Summary: Summarize drugs that have been covered
Hallucinogens: psilocybin, psilocin, mescaline, LSD
Analgesics: morphine, codeine, heroin, aspirin, acetaminophen (Tylenol)
Cardiovascular: digoxin, nitroglycerin, amyl nitrite, quinidine, reserpine
Antimicrobal: organoarsenicals, sulfa, penicillin, streptomycin
Anaesthetics: nitrous oxide, ether
Psychiatric Drugs: chlorpromazine, reserpine
Other: Physostigmine – Glaucoma
Curare – Muscle relaxation (modified to be safer)
Ergotamine – Migrane (replaced with better drugs)
Ergonovine – Obstetrics (stop bleeding after give birth)
Senna – Purgative
Ephedrine – Asthma (now replaced mostly)
Colchicine – Gout
Quinine - Malaria
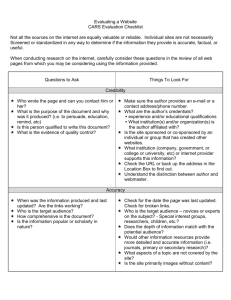
A.2 Drug Advertising, Drug Trials, and Placebo Effects
Objectives:
1. List techniques used in drug advertising
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
2. Explain/describe the placebo effect
3. Distinguish between a valid and invalid drug trial
DRUG ADVERTISING
19th century – pharmacies would pay artists to paint pictures to advertise drug use. One of
which was a nineteeth century poster of an anti-nicotine drug used to kick smoking –
nicotine patch is one of the best selling medications to date
Advertising Techniques
1. Catch the Audience Attentino
2. Use of Celebrities/ Authorities
3. Fear
4. Offering Easy Solution to Problems
5. Before/After Techniques
6. Discredits drugs produced by other manufacturers and praise your own
DRUG TRIALS
1938 – regulations for introducing drugs became more defined after sulfonamide
antibacterial drug dissolved in a solvent that turned toxic and killed about 100 people. After
this, requirement for new drugs to show that the new drug was non-toxic or had acceptale
toxicity profile
1962 – sleeping tablet thalidomide was introduced and then later was shown to have fetal
malformations in pregnancy, because of this the government further strengthened
regulations that pharmaceutical companies must show evidence of safety and efficacy for a
drug.
Steps of Drug Trials
1. Submit proof of safety and efficacy of the drug in animal species
- The proof must go to a government agency (Health Protection Branch in Canada and
Food and Drug Administration in USA (FDA)
2. Provide detailed methodology for clinical trials in humans
3. Get permission from scientists in regulatory agency
- Submission is carefully evaluated, if permission is given, they must then initiate
careful investigation on drugs in humans. Animal studies will nto always predict drug
behavior in humans
3 Phases of Clinical Trials
Phase 1: Small study of healthy volunteers – look at:
- Absorption
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Distribution
Elimination
Adverse Effects
Phase 2: Proof of Concept
- Determine whether drug is effective in treating the condition for which it’s
recommended.
- Test on limited number of people, careful attention paid to safety
Phase 3: Test on larger scale (1000+ people) to carefully study safety and efficacy
Phase 4: Postmarketing Surveillance
- Risks that are delayed or that are less frequent than 1 in 1000 may not appear in
Phase 3. Surveillance of drugs is required after it is released for general use.
Full risks may not be known at first –“Neither be the first to use a new drug, Nor the last to
discard the old” ** it is not advisable to demand that your physician change your drug
therapy ever time you read the introduction of a new drug
THE PLACEBO EFFECT
Placebo Effect: effects, which occur as a result of drug administration, that have nothing to
do with the pharmalogical effect of the drug
1955 Beecher conducted comprehensive study on placebo effects – collected data from 1000
patients with variety of conditions and found satisfactory relief in 33%
- Angina pectoris
- Common Cold
- Anxiety/Tension
- Cough
- Mood Swings
- Headache
- Seasickness
- Post-operative Pain
- Asthma
- Hypertension
- Depression
Someitmes patients report adverse effects (which are real) that are unrelated to
pharmalogical effect of drug.
The likelihood of placebo effects is greater in sick/anxious/stressed patients than normal.
We must compare a new drug to a placebo or older drug of proven value. It is not ethical to
compare a new drug to a placebo if there is an older drug in place (because it may not be as
effectve as the old drug, but more effective than placebo) – individuals may be depried of
effective therapy when conducting trial = unethical
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
DESIGN OF A PHASE 3 STUDY - COMPARATIVE EFFICACY TRIAL
The method of comparing a New drug with an Older Drug/Placebo
Design Options
1. Cross-Over Design (flawed) – give everyone a new drug and study the effect, then
administer old drug (or placebo) and study effects. Can be used in diseases states which are
chronic/stable
2. Parallel Design: divide into two groups, one receives new drug, other receives old drug and
compare **most Phase 3 are parallel designs
Randomization
- Assign subjects in a random manner in order to prevent flaws
Double Blind Design
1. Subjects are unaware of what drug they are receiving (new/old/placebo)
2. Cinical investigator is unaware of whether subject is receiving new or old
- helps eliminate bias on part of subject and experimenter
Design Elements of Phase 3 Trial
Study Population: Participants are selected according to strict set of requirements and
then assigned to groups
Overall: Valid vs. non-valid
1. Comparator: Placebo or best standard treatment?
2. Random Assignment of preselected subjects
3. Outcome: What’s being measured? Is it valid? Is it objective?
4. Blinding: double blind?
5. Control: are you controlling all other elements other than IV?
Good Questions to Ask When Assessing Clinical Trial
1. What question is the study designed to answer?
2. How were the patients assigned to test/control groups?
3. How were they selected?
4. How was the study designed to minimize patient/observer bas?
5. Who makes the observations?
6. Is there a clear definition of the desired therapeutic response?
7. Is the therapeutic response to be measured by objective or subjective criteria?
8. Have the data been subjected to statistical analysis?
9. Has the study answered the question that was initially posed?
10. Were the patients selected for the trial typical for those whom the drug is now
recommended? If a drug has been tested in male population only, is it recommended for both
men and women or for men only?
A.3 Dose-Response Curves and Selective Toxicity
Objectives
1. Distinguish potency and efficacy of a drug
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
2. Define “selective toxicity”
3. Describe how organoarsenicals were designed to achieve selective toxicity
4. State reason for selective toxicity of sulfonamide (sulfa) antimicrobal agents
DOSE-RESPONSE RELATIONSHIPS
In order to compare drugs, the dose used must be the same. For example, the pharmalogical
effects produced by marijuana increase in proportion to the dose and large doses of
marijuana impair performance of motor vehicle handling. In order to compare this to alcohol
you must ask:
1. How much alcohol compard to how much marijuana?
2. Used how often?
3. By what people?
4. Under what circumstances?
Potency and Efficacy of Drugs
Potency – the amount of drug that must be given to obtain a particular response. More potent
= need less for that effect
Efficacy – what the maximum effect is that is obtainable with a given drug. E.g. Morphine has
greater efficacy than aspirin ** a more important characteristic than potency
Dose-response Cruve: the effect of the drug on the y-axis, and the amount (log-dose) of the
drug on the x-axis
SELECTIVE TOXICITY
Selective Toxicity: the injury of one kind of living matter without harming some other kind.
E.g. we need agents that will destroy parasites and insect pests but not harm the person
taking the drug or the plant being given pesticides
- E.g. in New Brunswick – aerial spraying of forests with insecticide has led to damage to
birds and fish which is not what we want.
Selective Toxicity by Accumulation: A way of achieving selective toxicity by having an
agent that will be selectively accumulated by the species to be destroyed. Example: 10%
sulphuric acid used for a weed spray. The exterior of weeds is rough and wax free and acid is
accumated by the weeds, however cereal grass has smooth waxy exterior which does not
absorb the acid. Therefore, the weeds are attacked by the grass is fine.
In Cancer: Sensitive cancer ells accumulate the anticancer drugs and are killed. Some cancer
cells are resistant to the action of these drugs. P-glycoprotein and multidrug resistance
protein (MRP) are multidrug resitant proteins. They have normal function in the body but if
overproduced by a tumour they can result in drug resitance
Chemotherapy – Selective toxicity
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Paul Ehrlich discovered and coined the term. Means the use of drugs to injure invading
organisms without injury to the host. There were always thoughts that you had to get rid of
“evil spirits” from the body to get better
- burned sulphur so it smelled bad and they would leave
- Blood letting
- Administer agents that promote urination
It was only after the demonstration that many diseases are caused by microbes that any
attempt could be made to attack these diseases. (Ehrlich did this demonstration). Before this
there was little belief that a cure for microbial diseases would be found. People also thought
that substances that would kill microbes would kill the host.
Ehrlich noticed that some dyes stained certain body tissues and not others – decided to find
chemicals that would specifically stain parasites – realized if he could attach a toxic grouping
to the chemical, he could design a substance that would specifically kill the parasite and not
the human cells. He believed “bodies do not act unless fixed” meaning, the drug would not
act on a parasite unless it was attached. This was not believed by many scientists, they
believed that chemicals stimulate body’s defence system (argued this by saying that chemicals
don’t attack parasites in testtubes). Ehrlich refuted this by showing that Atoxl is converted in
the body to an ctive form which attaches to the parasite.
He used Arsenic compounds – organoarsenicals were created to try and cure syphilis in
rabbits – finally (after many failures) the successful compound was called Salvarsan – to save
health - and cured syphilis
Ehrlich argued four requirements for success in scientific research:
1. Geld (money)
2. Geduld (patience)
3. Geshick (cleverness)
4. Gluck (luck)
Sulfonamides – Domagk
1935 Domagk studied the effect of chemical compounds against bacterium streptococcus in
mice. Mice would die in a few days when injected. He looked to see if a combination of
chemicals could prevent this. He discovered the drug Prontosil which harmed streptococcus
without harming the mice.
In 1932-1935 71% f people with streptococcus in their blood died, after 1935, very few died.
Prontosil is split in the liver to give sulfianilamide which is the active principle (so it is
inactive in a test tube)
This is selective toxicity because microbes and host cells require folic acid. The body makes
folic acid and it can enter human cells but NOT microbes. Microbes make their own folic acid
by taking up para-aminobenzoic acid (PABA) which is then used to manufactor folic acid.
Sulfanilamide resembles PABA in structure and the microbe takes this up instead. Because
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
sulfanilamide is at the receptors for PABA, folic acid cannot be made and the microbes cannot
grow the body’s defece mechanism then can overpower the bacteria
Sulfanilamide owes it’s selective toxicity to the fact that it interferes with a chemical reaction
which is vital for the bacterium but not required for the host. Substances like this are referred
to as antimetabolites
Antimetabolites
Once the mechanism of action for sulfanilamide was understood, scientists wonderd whether
they could extend this idea to other antibacterial agents
- HIV treatment was discovered from this
Design of Anti-Cancer Drugs
Used the antimetabolite principle to see if it could treat cancer. Unfortunately, cancer cells are
very similar to normal cells but some differenes have been found
- Certain cancer cells cannot synthesize asparagine which is required for protein
synthesis and they must obtain asparagine from the blood. Asparaginase can reduce
asparagine levels in blood and inhibit protein synthesis of cancer cells. This is used to
treat childhood leukaemia
- The most important difference is that cancer cells divide continuously while most
normal cells are in a non-dividing state (except for bone marrow cells, intestinal tract
lining cells and hair root cells do not). This process of cell division DNA synthesis is
required so two resulting daughter cells contain sufficient DNA. Chemicls have been
designed that are closely related to building blocks of DNA and therefore inhibit the
division of cancer cells. However, because not all human cells are in a non-dividing
state, toxicity is inevitable (that’s why you lose hair/get sick)
Selective toxicity takes advantage of biochemical difference between mammalian and
bacterial cell for antibacterial agents. This is also true for anti-cancer drugs where
we take advantage of the difference between cancer and normal cell. The closer the
cells are to each other biochemically, the less there are differences.
A.4 Drug Toxicity and Routes of Drug Administration
Obectives:
1. List major substances involved in accidental child poisoning
2. List steps to be taken to minimize accidental child poisoning
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
3. Distinguish between four categories of adverse effects
4. List reasons why drug toxicity in humans is difficult to predict from animal studies
5. Define LD50, ED50 and therapeutic index
6. Explain why dosage of drugs must be adjusted in individual patients
7. List the advantages and disadvantages of administering drugs by different routes
DRUG TOXICITY
With the widespread distribution of drugs there is the problem of accidental poisoning and
suicide. The majority of cases of accidental poisoning occur in children under 5 and
acetaminophen or aspirin is often implicated.
Items accidently swallowed by young children
- Aspirin
- Acetaminophen
- Bleach
- Diaper-pail deodorizer
- Chocolate flavoured laxatives
- Children’s fever drops
- Cough Syrups
- Tranquilizers
- Birth Control Pills
- Cigarette butts
Preventing Accidental Child Poisoning
- Safety enclosures for bottles containing medicine
- Don’t present children with aspirin/medicine as candy
- Make sure toxic material (cleaners) are out of reach from children
Suicide by Overdose/Lethal mixtures
Barbiturates and similar drugs are the major drug group implicated in suicide. It is important
that depressed people are not allowed a large amount of sedatives/sleeping tablets
(barbiturates) at a time. Benzodiazepines are preferred to barbiturates becaue they have
enhanced safety.
TYPES OF ADVERSE EFFECTS TO DRUGS
*on exam
1. Extension of Therapeutic Effect - overdose of benzodiazepine (For example) will
produce over-sedation. An overdose of an anticoagulant (clot prevention) will cause bleeding.
Reduce dose of drug
2. Unrelated Effect to Main Drug Action – Example – digitalis is used to strengthen heart
muscle, but can produce nausea, vomiting and abnormal colour vision (unrelated to main
action)
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
3. Idiosyncrasy - unusual behavior. Example succinylcholine is used for muscle relaxation,
normally it’s inactivated by enzyme present in drug, but 1 in 3000 patients lack this enzyme
and therefore the effect of the drug will act for excessively long periods.
4. Drug Allergy – allergic reaction to drugs in some patients
1. First time administered it combines with a protein for form a complex known
antigen
2. The antigen provokes the body to make an antibody
3. The next time the drug is administered – antigen will combine with the antibodies
4. The antigen-antibody combo provokes and adverse reaction (mild to severe)
WHY IS TOXICITY DIFFICULT TO PREDICT?
Drugs are introduced through 3 stages – The 3 P’s
1. Pancea – thought of as a major new advance
2. Poison – after in use, adverse effects become apparent and drug sales drop, thought to be a
poison
3. Pedestrian – further passage of time, benefit/risk ratio is easier to assess, usually seen as
just an average drug
Toxicity That Appears Later – Why?
1. Toxic = Rare event: Chloramphenicol was an antibiotic used until it was realized that
death of cells in bone marrow (that leads to death of patient) occurs in 1 in 50 000. This was
very rare and obviously not detected initial testing. Now it’s used less but still used in cases
where benefits > costs
2. The Toxic Reaction is only For Prolonged Use: when Streptomycin was first used for
turberculosis but later was realized that it causes deafnes if used for extensive period of time.
A long period of time had to pass in order to realize the toxicity
3. Toxic Effect Not Detectable in Animals: Things like headache, insomnia, nausea, mental
disturbances cannot be picked up in animal testing
4. Toxic Effect may be unique to particular period: Thalidomide produced adverse effects
on the fetus, but this adverse effect is obviously only confined to pregnant patients. All new
drugs must be used with great caution in pregnant women.
THERAPEUTIC INDEX
Some people and animals are very sensitive while others are quire resistant to the effect of
drug. Drug toxicity must be tested in several animal species. A common measure for toxicity
of drugs animals is median toxic dose (TD50) – this is the dose that is toxic to 50% of the
population of animals. For effect of a drug, the dose which is effective in 50% of the
population is called the median effective dose ED50.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
The therapeutic index = TD50/ED50 the higher the figure, the greater the safety of
the drug and wider the safety margin. Drugs with low therapeutic index (anticoagulants,
anticancer agents etc.) must be used with caution.
RELATION OF DOSE OF DRUG, CONCENTRATION IN BLOOD, AND PHARMALOGICAL
EFFECT
The ‘usual dose’ of some of our most effective drugs will accomplish little in some persons, and
cause serious toxicity in others, and full satisfaction in some.
When drug is administered, it must be (1) absorbed into blood (2) carried to site of action (3)
exert its effect. A good relationship exists between the concentration of a drug in the blood
and the intensity of it’s pharcologica/therapeutic effect. But for some drugs there is a very
poor relationship beweteen the amount of drug administered and concentration in the blood.
Blood concentration also differs between people by as much as a factor of 10. Why? – There
are differences in the rate which the drug is absorbed and eliminated:
2. Environmental
1. Genetic
3. Disease
4. Presence of Other Drugs
If we are to use certain classes of drugs in the most effective way possible we should monitor
the blood concentration of these drugs in patients. This is especially important for:
1. drugs with low therapeutic index
2. where change in blood concentration is of major significance.
3. When drugs are given for long periods of time (e.g. phenytoin (Dilantin) for
epilepsy
Also the concentration in blood for lithium in bipolar (manic-depressive
illness) optimal efficacy and safety requires [lithium] to be maintained within
specific limits.
ROUTES OF ADMININISTRATION
Drugs may enter the body either enteral or parenteral route
- Enteral = directly into the gastrointestinal tract
- Parenteral = bypasses the gastrointestinal tract
Enteral Routes:
1. Oral administration
2. Rectal administration
3. Under the tongue
Parenteral Routes:
1. Intramuscular
2. Subcutaneous
3. Intravenous
4. Inhalation (less common)
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
5. Spinal canal (less common)
1853 hypodermic syringe was invented to inject morphine subcutaneously
Intravenous Administration
Pros:
- Drug is put directly into circulation
- Rate of drug infusion can be held constant using an apparatus
- Avoids the pain of administering certain drugs subcutaneously/intramuscular
Cons:
- Drugs injected into vein cannot be retrieved (given by mouth, for example, can puke)
- If drug is given to rapidly it can cause disaster (over one second high concentration
reaches heart) can lead to arrhythmia and death) usually done very slowly
- Danger of infection if sterile technique is not used (narcotics)
Intramuscular Administration
Pros:
- Slower dissolving into blood stream (10-30 minutes) can allow for drug to be more
long-acting
- Several penicillin preparations, hormones and antipsychotic drugs are given this way
Cons:
- some can be very painful
Subcutaneous Administration
- slightly slower than intramuscular; used for insulin
Transdermal Administration (through the skin)
- Poisonous materials can be readily absorbed through the skin
- People have been poisoned by insecticides: parathion and malathion as well as
nicotine (also used as insecticide)
- Parathion and malathion: inhibits enzyme acetylcholinesterase leading to a build up
of acetylcholine. Antidote: atropine (block acetylcholine receptors) and pralidoxime
(regenerate acetylcholinesterase). Often used in nerve gases for gas warfare
- Current drugs:
- Nitroglycerin for angina
- Fentanyl anaelgesic
- Hormonal contraceptive patch
- Nicotine patch
- All drugs are effective at small doses as only a small amount of a drug can be
transferred across the skin
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
A.5 Drug Absorption, Distribution, Metabolism, and Excretion
Objectives
1. Describe mechanisms whereby drugs are absorbed by inhalation and by mouth
2. Define the term bioavailabiity
3. Describe the procedure involved in providing a name for a new drg and provide an
explanation of the terms generic and brand names
4. List 3 major problems leading to the description of the drug field as thereapeutic jungle
and list ways of overcoming these problems
5. Describe the mechanisms available for termination of drug action
6. Describe and give examples of drug interactions
DRUG ABSORPTION
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Inhalation
Drugs in the form of gas can be inhaled and absorbed by the bloodstream through the lungs
and distributed throughout the body.
- Anaesthetics work this way: when the concentration of anaesthetic reache a critical
level in the brain, the patient become anaesthetized
- Bronchodilator and anti-inflammatory drugs fro asthma/respiratory diseaes are
administered by inhalation to produce a direct effect on respiratory system and
minimize the effect of the drugs on other organs
Rectal Administration
Often used for patients who are nauseous/vomiting and cannot take drug by mouth. The drug
is absorbed from the rectum into the blood stream.
- Drugs sometimes administered rectally for a local effect: hemorrhouds
- Systemic absorption is not as favourable from the rectal mucosa s from the intestine
Oral Administration
Most convenent route of administration and 90% of drus are oral. Only practical route for
self-administration.
Mechanism of Absorption
1. Tablet must disintegrate into small particles in stomach fluids/intestinal fluids
2. Small particiles must dissolve in the fluid of stomach/intestine
3. Dissolved, the drug must be absorbed through the walls of the stomach/intestine into blood
vessels (better on an empty stomach; intestine is major site of drug absorption because of
surface area)
4. Blood vessels carry the drug to the site of action
- Tablets must be made so that it will disintegrate and dissolve well so it can be absorbed, or
else it will be eliminated
Making a Tablet
1. Must have adequate amounts of the chemical responsible for the activity of the drug
2. Must disintegrate in a test tube
These don’t ensure it will be effective
1. disintegration time in a test-tube may not correspond to body fluids
2. Tablets are made in different ways by different companies and contain different
additives but must produce same blood levels of the active ingredient
3. What we need to know really is the blood level of the drug at different time intervals after
administration – this tells how much of a drug gets into the blood and can exert a therapeutic
effect
Bioavailability - the percentage of a drug contained in a drug that enters the systemic
(general) circulation in an unchanged form after the administration of the product. Also the
rate at which this entry occurs.
GENERIC AND BRAND NAMES
Formal Chemical Name: Every potential drug has a complex, chemical name. But this is not
satisfactory for general use
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Non-Proprietary/Generic Name: special name given to drugs b a organization such as the
American Medical Association. Any drug of this chemical name will be called this
Brand Name: The proprietary name of a drug, if more than one company markets it, a drug
could have several brand names.
Drug Benefit Forumulary/Comparative Drug Index: lists only drug products of good
quality
Drug products made by different companies can have very different levels of blood
concentraton. Example Digoxin is used for congestive heart failure – very efficacious but has a
considerable toxic potential, it was alarming when different companies had very different
blood levels. The bioavailability of products was different (different additives). But now
there are regulations about the additives used.
It’s important for physicians to hve reliable information when it comes to prescribing an
effective drug at reasonable cost. But Health Canada monitors bioavailablity so there is less of
a difference now.
THREADING ONE’S WAY THROUGH THE “THERAPEUTIC JUNGLE”
Therapeutic Jungle: the fact that there are so many drugs and drug combinations
The problems:
1. While there is only one generic name, different companies brand names
Solution: use generic name of drugs rather than brand name
2. There is an overwhelming number of drugs being introduced (often new drugs are
similar drugs with minor changes (economical for pharmaceuticals). New drugs are
often seen as panceas, but then realize years later they are no better than old ones
Solution:
3. Large amount of advertising directed to marketing new and old drugs. Quality of
drugs should be
Solution: consult unbiased, critical assessments of drugs by experts
MECHANISMS FOR TERMINATION OF DRUG ACTION
Process of Therapeutic Response:
1. Absoprtion
2. Distribution
3. Biotransformation (metabolism)
4. Excretion
Drug Absorption:
-
For a drug administered orally (or for all routes) it must be able to cross biological
membranes. Biological membranes have a lipid bilayer and drugs must be able to
dissolve in this lipid bilayer and move across the cell. Drugs do this to move across the
intestinal cells into the blood for effects throughout the body.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Once a drug is absorbed into the blood, it will produce effects on the body and the body
will begin to alter the drug for elimination
- When we administer drugs we are attempting to maintain the drug concentration at a
certain level / within therapeutic range
Ineffective plasma concentration {
Therapeutic Range } toxic concentration
(p. 37)
Termination of Drug Action
There are 3 mechanisms for termination of drug action:
1. Redistribution – the concentration of the drug is redistributed to other parts of the body
E.g. Thiopental initially has high concentration in the blood but after 15-30 minutes
the concentration increases in muscles/fat and decreases in the blood (reducing the
effect on the brain
2. Excretion – water soluble drugs are excreted through the kidney
This is the route most drugs take however, most are poorly water soluble and cannot
be excreted However, the body converts them…
3. Liver – converts lipid soluble into water-soluble products and they become inactive
Some chemicals are converted very slowly and accumulate in the body (PCBs and
insecticide DDT
DRUG INTERACTIONS
Drug Interaction: when one drug changes the pharmalogical effect of a second drug
1. Absorption
- A drug may combine with a second drug to form a complex that cannot be absorbed
- Example – tetracycline antibiotics and antacids (calcium, magnesium,
aluminum). Tetracyclines will not be absorbed if taken with antacids
- A drug that increases the movement of intestine may speed passage of second drug
through the intestine and the absorption may become hindered
- One drug may retard the absorption of the second by hindering the movement of the
intestine and the contents don’t mix as they usually do, minimizing contact of the drug
with the intestinal wall
2. Displacement
- Drugs can be found in blood in two forms: bound to blood protein or in a free form
- Free drugs are the only one that can move out of blood into tissues and exert their
effect.
- A second drug may displace the first drug from it’s binding site on the blood protein
causing more free drugs to be present in the blood and will exert more pharmalogical
effect (may overwhelm livers job of converting to inactive form)
3. Changes in Liver Handling of Drug
- Drug B may block mechanisms in the liver responsible for inactivation of Drug A –
causing greater amounts of Drug A in the body and greater pharmacological effect.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Example: combined use of antiulcer drug Cimetidine and the antiasthmatic
drug Theophylline. Cimetidine blocks mechanism of liver for inactivation of
Theophylline causing blood levels to rise to almost toxic
Drug B may speed up the inactivation of Drug A in the liver, causing less of Drug A in
the body than anticipated
- Example: antiepileptic drug Phenobarbital and anticoagulant Warfarin –
Phenobarbital causes liver to speed up inactivation of warfarin causing in a
drop in warfarin levels and diminished effect
-
-
4. Changes in Excretion
- Drug B may hinder the excretions of Drug A by the kidney, prolonging the effects of
Drug A in the body
- Example: Probenecid hinders the excretion of Penicillin G by the kdney
- Drug B may facilitate excertion by the kidney resulting in decreased levels of Drug A
- Example: Sodium bicarbonate facilitates the excretion of Aspirin when it is
taken in overdose
5. Interactions of Drugs with Potentially Toxic Substances in Food
- Well Matured Cheese: contain Tyramine (related to adrenaline) which is
brokendown by MAO. When taken with MAO inhibitors for depression, they will have
less MAO enzyme and therefore the tyramine can be poisonous by raising blood
pressure intensely
B.1 Physiological and Pharmalogical Aspects of The Central and Peripheral Nervous
Systems
Objectives
1. Describe the Components of a Neuron
2. Describe the Process of Synaptic Transmission
3. Describe the organization of the nervous system
4. List some of the common transmitters in the brain
5. Describe the organization of the peripheral nervous system (PNS)
6. List the transmitters in the autonomic nervous system, including their location and receptor
which mediates their response
INTRODUCTION
The nervous system is divided into two main components (1) Central Nervous System brain and spinal cord - and (2) Peripheral Nervous System - afferent/sensory nerves and
efferent nerve fibers
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Efferent system: motor nerves (innervate skeletal muscles) and autonomic nervous sytem
**p43
CENTRAL NERVOUS SYSTEM
Controls all bodily functions – consists of a central part (brain and spinal cord) and
peripheral part (nerve fibers)
- Sensory nerve fibers: carry message from tissues to the brain/spinal cord
- Motor nerve fibers: carry messages from brain/spinal to tissues
Parts of the Brain
3 Main Parts:
1. Forebrain
2. Midbrain
3. Hind Brain
The Forebrain
1. Cerebral Cortex: rich in nerve cells; made up of grey matter on the outside and white
matter on the inside. Divided into 4 lobe and 2 hemispheres
Main functions: sensory/motor coordination, mental processes, intelligence, memory,
vision, judgment, thought, speech, emotions, consciousness. Can be stimulated
(excited) or depressed (inhibited) by drugs
2. Thalamus: relay center – impulses are relayed to cerebral cortex. Thalamus coordinates
and filters incoming info/signals. Involved in pain sensation
3. Hypothalamus: specialized regions of nuclei used to control involuntary functions of the
body (heart regulation, blood pressure, body temp, metabolism).
Also controls feeding, drinking, sexual and emotional responses. Important part of
limbic system. Neurons in the hypothalamus produce releasing factors that go to
pituitary gland and modify it
4. Pituitary: gland behind base of brain that secretes hormones that control growth,
behavior and metabolism (e.g. FSH for maturation of ovaries) Thyroid stimulating hormone
synthesizes release of thyroid hormone
The Midbrain
Links the forebrain and hindbrain – relay center for visual and auditory stimuli
The Hindbrain
The hindbrain has many components: we describe the medulla and cerebellum
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1. Medulla (the bulb): site of origin for many cranial nerves. Where regulation of respiration,
regulation of heart, and blood pressure occur. Exercise control over some involuntary activity
(ANS). Drugs that depress respiration do so by acting on medulla
2. Cerebellum: large, structure connected to brain stem. Responsible for coordination and
posture. Does not initiate movement but organizes voluntary activity that has already been
initiated. Drugs that affect the cerebellum wil cause ataxia (drunkenness) – i.e. alcohol
The Brain Nerve Cell (The Neuron)
Functional unit of the brain; 3 parts
1. Cell Body – contains nucleus, cytoplasm and rough endoplasmic reticulum, smooth
endoplasmic reticulum and many vesicles that can be excreted – characteristics of cells active
in protein synthesis and secretion of substances
2. Dendrites – receiving antennae for incoming information with receptors. Electric current
is generated and transmitted to axon (many dendritic branches)
3. Axons – single fibre that extends from cell body to synapse. Carries signals away from cell
body to dendrites of another neuron
Organization**p. 46
The Synapse and Ceoncept of Synaptic Transmission
Nerve cells communicate with one another by sending electric signals to one another through
a junction between two neurons – synapse (axon of one neuron, dendrite/cell body of
another)
- The passage of this signal is called synaptic transmission
- Synaptic Transmitters – substances that mediate the synaptic transmission
- Chemical transmission – release of a transmitter substance is required to activate
the other cell/pass along the message
Process of Synaptic Transmission
1. Nerve impulse passes down axon of neuron
2. Impulse causes a release of a chemicl substance into the synaptic clefy
3. The post synaptic membrane contains binding sites (receptors) for the chemical
transmitter
4. Binding of chemical transmitter and receptor provokes change in permeability of the
membrane
5. Ions (calcium) move across the membrane changing electrical activity of the membrane
6. This electrical activity is passed to next cell
Continuous presence of a transmitter in cleft would prevent other impulses from getting
through to prevent synapses from being non-functional the chemical transmitter is
removed by 1 of 2 mechanisms
1. Broken down by enzymes
2. Taken back up into presynaptic cleft
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Some drugs can interrupt synaptic transmission while others can enhance or facilitate it
Concept of Receptors
Receptors are proteins synthesized in rough endoplasmic reticulum and transported to
different part sof the cell/inserted in cell membrane of cell body, dendrites, axon
- Receptors have specificity for endogenous transmitters and this specificity is exploited
in drug development
- Each endogenous transmitter has it’s own receptor – when a transmitter binds to
a receptor, it elicits a response
- Drugs can either stimulate a receptor (agonist) or inhibit the action (antagonist)
Types of Receptors and Neurotransmitters
- There are many Different Types of Receptors for a large number of transmitter
substances
1. Cholinergic Receptors 2 broad classifications (ACETYLCHOLINE)
- Nicotinic Receptors - stimulated by nicotine (found in autonomic ganglia,
neuromuscular junction and some regions of the brain)
- Muscarinic Receptors – stimulated by the alkaloid muscarine (found in many
regions of the brain) – involved in learning, memory, and cognitive function
- Transmitter: is Acetylcholine
- Drugs that block/antagonize action of acetylcholine at these rceptors produce
amnesia – loss of cholinergic neurons may be associated with Alzheimer’s
- Drugs that excite/activate action (agonist) is associated with excitatory response
2. Serotonin Receptors and Serotonin
- Serotonin and it’s receptors are found in the upper brain stem with many in the pons
and medulla, hypothalamus, hippocampus and cerebral cortex
- Hyperactivity of serotonergic system is involved with anxiety
- Hypoactivity of serotonergic system is involved with depression
3. Catecholamines – dopamine and norepinephrine
- Dopaminergic pathways: 1. Hypothalamus 2. Basal ganglia/brain stem 3. Midbrain
- Involved in
- control of hormonal systems (hypothalamus)
- Motor coordination (Basal ganglia)
- Motivation and reward
- Disturbances lead to Parkinson’s and schizophrenia
- D1 (excitatory) and D2 (inhibitory) are most important receptors
- Norepinephrine Pathways 1. Brain stem and project to 2. cerebral cortex, 3.
Hypothalamus, 4. Limbic system and 5. Cerebellum
-
Receptor types: Alpha α and Beta β activation of these receptors usually
cases excitation of the cell but one sublass is inhibitory
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Some antidepressants will enhance the norepinephrine system
4. Glutamate or Glutamic Acid
- Important amino acid neurotransmitter
- Primariily excitatory and found in almost all neurons
- Acts on glutamatergic receptors
- Involved in learning
5. Gamma Aminobutyric Acid (GABA)
- Main inhibitory neutrotransmitter in CNS
- GABAnergic receptors and neurons are in high concentrations in cerebral cortex,
hippocampus and cerebellum
- CNS depressants (benzodiazepines and barbiturates) bind to GABA receptor
6. Opioid Peptides
3 Main classes
1. Enkephalins
2. Endorphins
3. Dynorphins
Opioid Receptors
Mu μ
– pain regulation
- most abundant in cerebral cortex, hypothalamus, brain stem and spinal
Delta δ - Olfaction, motor integratio, reward, cognitive functions
- concentrated in olfactory system and various limbic
Kappa κ – regulation of food intake, water balance, pain perception, control endocrine
system
- caudate-putamen and hypothalamic sites
There are several types of a particular receptor, with different functions, and a specificity in
the distribution of receptors, allowing for integratin of functions. Narcotic
analgesics and opiates interact with these receptors
THE PERIPHERAL NERVOUS SYSTEM
The efferent compound of peripheral nervous system consist of motor nerves and ANS
Motor Neurons: innervate skeletal muscles/body parts that are under voluntary control
- Acetylcholine is the transmitter that is released by motor neurons as they innervate
- Receptor is nicotinic
- Synapsse is neuromuscular junction
Autonomic Nervous System: involved in maintaining stable internal environment and
governs vital bodily functions that are involuntary – BP, HR, bowel movement, urinary output,
sweating vegetative functions (visceral functions) ANS = involuntary nervous system
Two Parts of the ANS – act in a balanced and opposite fashion
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1. Sympathetic Nervous System (SNS) – mobilize resources for emergencies (increase HR,
BP, Blood supply to tissues stress reaction or alarm reaction
2. Parasympathetic Nervous System (PNS) - increases vegetative functions
General Organization p. 51 PNS nerve – Organ – SNS nerve
- Acetylcholine is the neurotransmitter at all autonomic ganglia and recepters are
nicotinic
- The postganglionic parasympathetic nerve is acetylcholine and the synapse is
cholinergic with muscarinic receptors stimulated by the alkaline muscarine
- The postganglionic sympathetic nerve is norepinephrine with adrenergic
receptors
- 1. Alpha – on smooth muscle
- 2. Beta-1 - heart
- 3. Beta -2 – in lungs, blood vessels, gastrointesetinal muscle, uterus
- **diagram p. 52
AUTONOMIC NERVOUS SYSTEM
PARA SYMPATHETIC
Constricts pupil
Decrease HR
Decrease force of ehaart
contraction
Constricts bronchi
Increases digestion movement
in gut
Contracts/Excites bladder
ORGAN
Eye
Heart
Heart
Lung (Bronchi
Gut
None
Dilates
Constricts
Urinary Bladder
Blood Vessels
In Skeletal Muscle
In skin
In heart
None
Adrenal Gland
SYMPATHETIC
Dilation of Pupil
Increase HR
Increase force of heart
contraction
Dilates bronchi
Decreases digestive
movement in gut
Relaxes/Inhibits bladder
Dilates
Constricts
Dilates
Discharge of epinephrine
The synaptic junctions in the ANS can be targets of drug action and modify function of SNS
and PNS
1. DRUGS THAT MIMIC EFFECT OF SNS
- Norepinephrine
2. DRUGS THAT BLOCK EFFECT OF SNS
- Propranolol (Beta receptors in heart)
- Prazosin (alpha receptors in blood vessels)
3. DRUGS THAT MIMIC EFFECT OF PNS
- Acetylcholine
4. DRUGS THAT BLOCK EFFECT OF PNS
- Atropine (belladonna)
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Drugs that block the activity of one system can often unmask the activity of the other
Drugs that Effect ANS through their Action on the Brain
ANS can also be modified by drugs acting on the brain.
Central Stimulants – can increase SNS and PNS activity (excitation)
Central Depressants – can decrease SNS and PNS activity (inhibition)
B.2 Drug Dependence and Drug Abuse
Objectives
1. State the definition for tolerance, psychic dependence, and physical dependence
2. State or list clinical features of substance dependence
3. State the difference between the medical perspective and social aspects of drug abuse
4. State the contributing factors and their role in determining the abuse potential of a
subtance
5. State the influence of societal values on determining what constitutes drug abuse
INTRODUCTION
-
-
-
People do drugs because they gain something from their use (good feelings, reduced
pain, escape problems). Some users rarely use psychoactive drugs when alone, but use
it to reduce social inhibitions.
Dopamine Hypothesis of Dependence: Some argue drugs that cause dependence
increase dopamine levels in the mesolimbic system – and this increase leads to
maladaptive behavior.
Reinforcement - The greater the good feelings, the more likely the drug will be
repeated.
Society has complex rules for acceptable use of substances – the use of morphine and
opiods for pain relief is ok. But not for the use of pleasure. Alcohol is accepted at
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
social gatherings, but drinking and driving is not. Some North American socieities
don’t approve of the use of hallucinogens but some socieities have used these agents in
ceremonies, rigious as well as for others.
DRUG DEPENDENCE
Drug Dependence = physical dependence
Addiction = denotes psychological dependence
Drug Addiction: often used to describe an intense pattern of drug use that is detrimental to
the individual and society.
Drug Habituation: Less intense form of drug use that produces detrimental effects on the
individual only.
Drug Dependence is a state of periodic or chronic intoxication produced by repeated
consumption of a drug (natural or synthetic):
1. Overpowering desire or need (compulsion) to continue taking the drug/obtain it by any
means
2. Tendency to increase dose
3. Psychic (psychological) “addiction” and sometimes a physical dependence on the
effects of the drug
Drug dependence includes all degrees of intensity of desire for the drug, all degrees of damage
to both individual and society and all degress of both physical and psychological need to
continue using the drug
3 important Aspects to Dependence
1. Drug Tolerance: repeated administration of a given dose has progressively less of an effect
so increased dose must be used to obtain the same pharmacological effect.
2. Physical Dependence (DEPENDENCE): abnormal physiological state produced by
repeated administration ofa drug that leads to appearance of characteristic and specific
group of symptoms (withdrawal) when drug administration is discontinued
3. Psychological Dependence (ADDICTION): state in which stopping abruptly/reducing a a
dose has non-physical symptoms. Emotional and mental preoccupation with a drug’s effects
and persistent craving.
There is a cluster of cognitive, behavioral, and physiological symptoms.
Cilnical Diagnosis:
Compulsive Use: takes substance in larger doses and for longer period of time than intended.
Harmful Use: psychoactive substance use pattern that is causing damage to health. Damage
may be physical or mental. Actual damage must be caused for it to be considered harmful.
Drug Abuse: Medical Perspecive
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Must have:
1. Maladaptive pattern of substance abuse – recurrent and significant adverse consequences
related to repeated use of substances. There may be repeated failure to fulfil major role
obligations, repeated use in hazardous situations, legal problems, social problems
2. Symptoms that have never met criteria for substance dependence for the class of substance
Impairment of function and inappropriate behavior without characteristics of substance
depdnence and without damage to physical/mental health.
Drug Abuse: Social Perspective
Judgments change as societal values change. Drug abuse refers to use of any drug in a manner
that deviates from approved medical or social patterns in a given culture. Social
disapproval but doesn’t necessarily include potential adverse effects
1. Use of prohibited drugs
2. Use of therapeutic drugs for other than intended use
3. Intentional ingestion of therapeutic drugs in amounts greater than prescribed or other
routes
4. Taking drugs in combination to obtain greater pleasurable effect
5. The excessive use of licit (legal) social drugs (alcohol, caffeine, tobacco)
-
this definition does not include all substances of abuse (e.g. glue, gasoline)
The list of do’s and don’ts is set becaue drug abuse is costly to society
Abuse Potential
The abuse potential of drugs is depdnent on 3 contributers
1. Intrinsic Dependence Liability of the Drug
2. Availability of the drug
3. Drug’s inherent harmfulness to cause physical and psychological effects
Dependence Liability - tendency of the drug to produce physical and psychological
depdnence.
1. Nature of the Drug – The more immediate the response coupled with an intense
response will lead to dependence and continued abuse. The level of Reinforcement a
drug has
2. Route of Administration – routes that give rapid absorption and therefore rapid
effects have greater potential for abuse than drugs which produce the effect more slowly
3. Amount Used – greater the dose and frequency of use = greater potential for
dependence to develop. I.e. occasional alcohol use will not lead to dependence but
frequent, high-dose will
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Availability of a Drug - More widespread a drug, the more likely it’s abused. For example,
alcohol has moderate intrinsic dependence liability but Is very available and therefore the
most highly abused psychoactive substance.
Inherent Harmfulness – the drugs potential to cause harm. E.g. Methyl alcohol in small
doses can cause blindness and death, where ethyl (drink) alcohol does not.
*Hallucinogens do not cause physical dependence **all other drugs mentioned do.
B.3 Sedative-Hypnotics and Anxiolytics
Objecives
1. State mechanism of action of benzodiazepines and barbiturates
2. List therapeutic use and rationale for clinical use of benzodiazepines nad barbiturates
3. Describe response to barbiturates and benzodiazepines at various doses and duration of use
4. Describe dependence liability for benzodiazepines and barbiturates
5. Describe withdrawal syndrome associated with barbiturate dependence
INTRODUCTION
Sedative-Hypnotic agents are CNS depressants. They produce CNS depression ranging rom
antianxiety sedation hypnosis (sleep) general anaesthesia
The magnitude of CNS depression produced by a drug at a particular dose determines
whether that agent is considered antianxiety agent, sedative, or hypnotic at that dose
Interactions of sedative-hypnotic agents with other CNS depressants (alcohol) are
clinically important and can be dangerous
HISTORY
19th century Bromides were first agents for clinical use of sedatives/hypnotics. Before it was
only ethyl alcohol and herbal preparations. But bromides eliminate slowly from the body and
accumulation occurs causing Bromism – mental and neurological aberrations, rash, and
gastrointestinal disturbances. Then chloral hydrate was introduced short afte.
1912 phenobarbital began the “age of the barbiturates”
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1950 meprobamate and glutehimide were introduced
1961 chlordiazepoxide was first benzodiazepine – this type is now widely used today
THERAPEUTIC USE
1. Anti-anxiety – benzodiazepines
2. Sedative (reduce sensory motor function, reduce tension) – benzodiazepines
3. Hypnotic (sleep) – short acting benzodiazepines
4. Anticonvulsant – Phenobarbital and some benzodiazepines
5. Skeletal Muscle Spasms – Benzodiaepines
6. Alcohol Withdrawal Syndrome – Benzodiazepines (diazepam)
CLASSIFICATION
Benzodiazepines (e.g. Diazepam, flurazepam)
Barbiturates (e.g. Phenobarbital)
Other Agents (E.g. chloral hydrate)
BENZODIAZEPINES
Mechanism of Action
1. Activate benzodiazepine receptor
2. Enhance action of GABA
3. Inhibitory processes occur
Site of Action: cerebellum, cerebral cortex, limbic system, reticular activating system, spinal
cord. All act on same structure as GABA but not on GABA receptor.
Pharmalogical Properties
1. HIGH therapeutic index
2. Produce relief from anxiety
3. Decrease aggression
4. Produce sedation and amnesia
5. Some are effective hypnotics
6. Minimal suppression of REM sleep aat normal doses
7. Skeletal muscle relaxation (diazepam)
8. Anticonvulsant action – epileptic seizures
Pharmacokinetics – there are appreciable differences among various benzodiazepines
1. Duration of action can be different
2. Different purposes (diazepam: anxiolyticand anticonvulsant flurazepam:
hypnotic)
Route of Administration – mostly oral tablet sometimes intravenous
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Effect of Benzodiazepines:
Effects Short Term Low/Moderate Dose:
CNS: - relief from anxiety/tension, calmness
- Moderate impairment of motor coordination, drowsiness, lethargy, fatigue, impair
thinking
- **impairment of driving can occur
Respiratory Depression
Gastrointestinal Symptoms
- constipation
- Nausea
- Dry mouth
Effect Short Term High Doses
- drowsiness, over-sedation, sleep
Effect of Long Term Use
- depends on the user, some can have no problems of intoxication while others
demonstrate chronic sedative-hypnotic intoxication symptoms
- Impaired thinking, poor memory and judgment, disorientation, slurred spee
Lethality
- Benzodiazepines are among the drugs most commonly involved in overdose. But
deaths are very rare.
Tolerance
- develops to sedative and impairment of coordination effect. Tolerance to anxiolytic
effect is less common. Tolerance is not a problem in clinical use
- Tolerance may develop to the desired effects of euphoria
Physical dependence/Withdrawal
- Short term = low risk
- Chronic/Long term 1year+ = may hae withdrawal and depends on which
benzodiazepine is used.
- Symptoms: agitation, paranoia, seizures, and delirium but not frequent
Psychological Dependence
- may develop but not in all users. Persistent cravings can occur even if drug no longer
produces an effect
Patterns of Use:
- Most widely prescribed drugs
- 10% of Canadians use them at least once a year for medical reasons. Some use in
combination with alcohol to increase effect (30-76% of alcohol abusers use)
Potential for Abuse
- low abuse liability – weak reinforcing properties, inherent harmfulness is low, margin
of safety is high
BARBITURATES
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Potent CNS depressants
Low dose: relaxation/tranquility
Moderate doses: induce sleep and impair motor function/cognitive if not sleeping
High doses: induce anesthesia – death can result from respiratory failure
Use: mostly replaced by newer/safer drugs – short acting ones are used to induce anesthesia
and Phenobarbital is used as an antiepilieptic
Mechanism of Action:
1. Modulate chloride channel
2. Potentiate effect of GABA at GABA receptor
3. Enhance inhibitory effect of GABA
Pharmacological Properties
1. LOW therapeutic index
2. Full spectrum of CNS depression antianxiety sedation hypnosis general anesthesia
death
3. Can supporess REM sleep (don’t feel rested)
4. Long-acting barbs are effecting in suppressing epileptic seizures
5. Thioprental – ultra short acting – induce general anesthesia
6. Respiratory Depression – major problem, dose-dependent
7. Cardiovascular system is depressed by high doses
Classification
Classified by duration of action:
1. Long-Acting (1-2 days) – Phenobarbital
2. Short-Acting (2-8 hours) – secobarbital (seconal)
3. Ultrashort-Acting (20 minuts) – thiopental
Route of Administration – usually oral, anesthesia = intravenous
Lethality
- is common, especially in combination with alcohol
- No specific antidotes for barbiturate poisoning
- Death can also occur from barbiturate withdrawal
Tolerance - develops rapidly to sleep induction, slower to motor coordination impairment
and slowed reaction, slower in anticonvulsant
Psychological Addiction – can result from regular use irrespective of dose
Physical Dpeendence/Withdrawal
- usually occurs with abrupt discontinuance
- Syndrome for Low Dose: sleep disturbances
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Syndrome for Chronic Use: severe withdrawal; tremors, anxiety, weakness,
insomnia, rapid drop in blood pressure when go from sitting to standing, hyperactive
blink peaking between 24-72 hours
- Eventuall may have seizures, fever, delirium, hallucinations – may not survive
- MUST WITHDRAW BARBITURATES SLOWLY
Patterns of Use
- Prescrcibed much less, illicit use is a problem. Sometimes combined with heroin.
Potential for Abuse
- Abuse liability is equal or greater to alcohol. High intrinsic dependence liability,
inherent harmfulness is high. THESE drugs SHOULD BE AVOIDED
-
OTHER AGENTS
Flumazenil – GABAa receptor antagonist – blocks effet of benzodiazepines (antidote for
benzo poisoning)
Zolpidem – new GABA receptor agonist – may have advantages over benzo as hypnotic
Buspirone does not act on GABA recepor but 5-HT receptor – used for general anxiety
Chloral Hydrate – old drug, was used as hypnotic – used sometimes in geriatric patient –
causes epigatric distress (heart burn) limited rationale for use
B.4 Narcotic Analgesics (Opiates, Opioids)
Objectives:
1. Define term opioid, endorphins and opiate
2. State the role of opioid receptors in mediating opioid-induced analgesia
3. List the classification of opiates and give examples in each class
4. State the therapeutic uses of opioid drugs
5. State the pharmacological effects of the opioids
6. Describe dependence to morphine and heroin
7. Describe opioid abuse
8. State the accepted treatment for opioid abuse
INTRODUCTION
Opium comes from the cut capsule of opium poppy and was used for thousands of years for
social and medical purposes – euphoria, analgesia, sleep, and relief from diarrhea. Opium
contains morphine (10%)and codeine (0.5%)– analgesics. Purification of morphine
revolutionized use of opiates
TERMINOLOGY
Opiod- any natural or synthetic sbstance which exerts actions on body that are similar to
those induced by morphine and that are antagonized by naloxone. Opioids include:
1. Opiate narcotics (analgesic agents obtained from opium poppy)
2. Substances structurally similar to morphine
3. Synthetic drugs with structures different from morphine
4. Endogenous brain peptides opioid peptides: enkephalins and endorphins
OPIOID RECEPTORS
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
There are specific receptor sites for opioid molecules in the brain. Endogenous substances that
interact with these receptors are endorphins there are 3 families: enkephalins,
dynorphins and beta-endorphins.
Endorphins act as neurotransmitters and neuromodulators. They affect percepion of pain
and emotional response to pain. Also associated with mood and rward pathways in brain.
Opioid Receptors:
Mu – in brain and spinal cord; mediate analgesia and depression of respiration
Delta –Endogenous ligands are Enkephalins; involved in analgesia at spinal cord level and
brain; modulate emotional response to opioids
Kappa – involved in analgesia, dysphoria, and miosis. Mixed agonist/antagonists
(pentazocine) act predominately on these receptors. The endogenous ligans are
dynorphins and sometimes endorphins
Opioid receptors are also located in peripheral – gastrointestinal tract and responsible for
constipation
Classification of Opiates/Opioids
Agonists
- Illicit a full response
- Natural – morphine and codeine
- Semi-synthetic – heroin
- Synthetic – meperidine and methadone
Mixed Agonists/Antagonists
- Can illicit a response when given alone, but block part of response to morphine when
given with morphine
- Pentazocine
Antagonists
- Block response to morphine, heroin and other opiates
- Giving this to an addict with precipitate withdrawal
- Naloxone used to
- 1. Reverse opioid overdose
- 2. Treat opioid dependence
- 3. Diagnosis of opioid physical dependence
- 4. Naltrexone – opioid antagonist to treat alcohol dependence
THERAPEUTIC USE OF OPIOID DRUGS
1. Relief of sever pain
2. Treat Diarrhea – receptors in gastrointestinal tract mediate motility
PHARMACOLOGICAL EFFECT OF OPIOID AGONISTS
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1. Analgesia
2. Euphoria
3. Sedation
4. Hypnosis/Sleep
5. Relief or Prevention of Cough
6. Respiratory Depression respiratory arrest
7. Decreased gastrointestinal motility constipation
8. Constriction of pupils of eyes miosis – pin-point pupils is a sign of a user
9. Nausea/Vomitting
10. Drug Dependence – develops to all opiate analgesics
MECHANISM OF ACTION For INFLUENCING PAIN
Opioids (including morphine) all act on opioid receptors. Naloxone does NOT activate
receptors but blocks them (antagonist)
1. Reduced presynaptic release of chemical transmitters that are mobilized by pain impulse
2. Block postsynaptic effect of these transmitters
3. Activation of descending inhibitory pathway to block pain input
4. Reduce emotional reaction to pain by acting on limbic brain
NARCOTIC (OPIOID) DRUG DEPENDENCE
1. Tolerance: to most pharalogical effects occurs. Exception: constriction of pupils and
constipating effect. Reversible in a few days after opioid is discontinued
Cross Tolerance between all narcotic opioid analgesics occurs providing they act on the
same receptor.
2. Physical Dependence: Develops after repeated administration. Pronounced withdrawal
syndrome can occur. NOT life threatening:
1. restelessness, anxiety, insomnia
2. Sweating, fever, chills
3. Increased respiratory rate
4. Retching and vomiting
5. Cramping
6. Explosive diarrhea
3. Psychologiacl Dependence (Addiction) pronounce craving and compulsion for narctotic
analgesics (opioid) can develop. The use of narcotic analgesics with other psychoactive drugs
can occur. The basis for psychic dependence is euphoric action
Neonatal Drug Dependnence
If a mother is physically dpeendnet on opioid analgesics during pregnancy, there’s an
increased risk of premature delivery and low birth weight infant. At birth the infant undergoes
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
abrupt termination of drug supply and goes through withdrawal (irritable, sleep
disturbances, poor feeding, sometimes seizures)
Opioid Overdose
Medical emergency. Can cause respiratory depression leading to death. Treatment with
Naxolone as an antidote
Opioid Abuse
The euphoria produced by opioid analgesics is main reason for their abuse
1. Properites of compound – how much eurphoria/reinforcment
2. Size of dose: greater dose = greater euphorias
3. Route of Administration: if euphoria is rapid in onset and intense following
intravenous
4. Use of opioids in combo with other drugs: euphoria of two drugs is greater than
one drug
Effect of Opioid Abuse
- Effects of chronic needle use
- Abscesses and infectios at site of administration – spread of disease through
contaminated needles
- Lifestyle of the user is often aberrant (spend all money on drugs, enter crime)
Treatment of Opioid Dependence
In some countries Europe, morphine and heroin are given to people with these addictions but
NOT IN CANADA
1. Cessation of Drug Use – Oral methadone replaces drug of dependence and dose of
methadone is reduced over time. Other pharmacological agents may be added to program
plus counseling and rehabilitation
2. Methadone Maintenance - method where the methadone is not reduced. Substitutes
methadone dependence in place of street heroin etc. This occurs because methadone is readily
available, oral tablets and they don’t need crime to afford it. This is a risk-reduction
method
MORPHINE
Street name: “M”, Morph, Miss Emma. Usually used alone but can be combined with
methamphetamine and cocaine. Tablet, smoked, sniffed, injected
Low Dose Effect: suppresses pain, emotional arousal to pain, euphoria, drowsiness,
relaxation can cause gastrointestinal problems like vomiting, nausea, constipation, loss of
appetite, decerased gastric motility
High Dose Effect: intensification of low dose effect and increased duration of effects. CNS
Depression can result in coma at very high doses – body temp low, skin is cold and
clammy, pupils are constricted
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Long Term Use: no marked physiological deterioration/psychological impairment. Mood
instability, pupilllary constriction (impairs night vision), constipation, reduced libido,
menstrual irregularity, and respiratory impairment
Potential for Abuse:
1. dependence liability exceeds all other opioids except heroin. Powerful euphoric and
analgesic effect
2. Inherent harmfulness is not high with low to moderate doses but lethal with high dose
3. Morphine is available by prescription – strict control reduces potential for abuse
HEROIN
Heroin is Diacetylmorphine which is synthetically produced from morphine. Used in 1900s
as analgesic but high dependence liability lead to abandonment
1980s people lobbied for it to be availale for medical use and this was allowed but legitimate
medical use is extremely low.
Heroin is more potent than morphine but NOT more efficacious (Heroin is rapidly
convered to morphine in the body)
Street names: Dust, “H”, Horse, Junk, Smack, Scag, Black Tar – sometimes combined with
amphetamines (bombitas) or cocain (dynamite, speed ball, whiz bang). Street heroin
concentration ranges from 3% to 20% and rare cases 90%
Inected subcutaneously (skin popping), intramuscularly, or intravenously (mainlining).
Sometimes snorted or smoked (chasing the dragon)
Low Dose: suppress sensation of pain, euphoria, mental clouding, feelings of relaxation and
drowsiness/talkativeness in others.
Respiratory: decreased respiratory rate – major cause of death at high dose
Gastrointestinal: nausea, vomiting, reduced appetite, decreased gastric motility
High Dose: magnitude and duration of response increase as dose increases. Response to
painful stimuli is blunted firther. Decerased concentration, wish to sleep.
Respiratory depression – can cause death
HR and BP decrease
Extremely high dose: induce sleep, lower bp, slow and irregular heart rate,
shallow/depressed respiration, body temp lower and skin is cold and clammy
Long Term Use: Under medical supervision no long term physical/psychological impairment.
Street heroin is associated with dangerous lifestyle (needles, impure drugs)
Heroin and Pregnancy
- high neonatal mortality rate – infant born low birth weight and premature
Tolerance and Dependence
- Tolerance develops with heroin like all opiates – powerful physical and psychological
dependence develops rapidly at regular high dose
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Potential For Abuse
1. HIGHEST Dependence Liability of all opiates
- Extremely powerful euphoric and analgesic effects and solubility (enters brain quick)
2. Inherent Harmfulness in low to moderate is low but HIGH doses are life-threatening
3. Availabiltiy: controlled by law but widely available on streets
OTHER DRUGS
1. Oxycodone
2. Hydrocodone
- Produce drug dependence when clinically used (over used)
- Recently, oxycodone has been made to be tamper resitant – when mixed with water the
resulting mixture forms a gel and cannot be drawn into a syringe for injection
B.5 Classification of Major Psychoactive Drugs
Objectives:
1. Describe Mechanismo of Action of the psychomotor stimulants, cocaine, amphetamine,
caffeine, and nicotine
2. List the six categories of CN
S depressant drugs
3. Describe how increasing doses of CNS depressant drugs effect an individual
4. Explain the terms “cross tolerance” and “cross dependence”
Psychoactive Drugs: agents that act on CNS and alter sensation, perception, mood, behavior
or consciousness
Ways to Classify Psychoactive Drugs
1. Mechanism of Action – but there’s insufficient information
2. Chemical Structure – does not work since some with similar structure have different
pharmacohological activities
3. Major Behavior Effect or Major Clinical or Non-Clinical Use: classification of agents
based on either of these is the MOST practiced method
Psychoactive drugs do not create new behavioral problems or physiologival
responses but act by modifying ongoing physiological and biochemical responses –
must understand the limitations of drugs. “The psychopharmacologist cannot add to the
faculties of the brain but he can eliminate obstructions” – Koestler
Behavioral effects of psychoactive drugs are secondary to their effects on physiological and
biochemical processes
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Psychoactive drugs can
1. Stimulate CNS
2. Depress CNS
Stimulants
1. Cocaine – blocks dopamine reuptake into presynaptic nerve terminals
2. Amphetamin and derivatives - acts by releasing dopamine from presynaptic nerve
terminals
3. Caffeine: Caffeine is a blocker of adenosine at it’s receptors in cell membranes in CNS and
PNS. It’s action as a stimulant results from antagonism of adenosine-induced neuronal
inhibition
4. Nicotine: stimulates selective subgroup of acetylcholine receptors in CNS (nicotinic
receptors which are excitatory)
Depressants
1. Barbiturates
2. Non-barbiturate hypnotics
3. General anesthetics
4. Ethyl alcohol
5. Benzodiazepines
6. Inhalants of abuse
The effect of depressants on CNS depend on dose
Barbiturates: small dose may cause relief of anxiety, while larger dose may cause sedation
by hypnosis and further general anesthesia, then coma, then death.
The medical use of CNS depressnat drug is usually a function of dose and the above terms
(tranquilizers, major tranquilizers, anxiolytic, sedatives) are merely used for marketing.
Four Principles of CNS Depressnat Use
1. Effect of CNS depressants are additive: Severe CNS depression occurs if more and more
depressants are taken
2. Use of a behavioral stimulant in combination with a CNS depressant may cause
arousal of the depressed individual. But when this stimulant effect ends, the individual may be
left even more depressed
3. Large doses of CNS depressents for long periods leads to physiolgocial and
psychological dependence
4. Cross Tolerance may be observed
Classification of Mood Altering Drugs or Used to Treat CNS Disorders
1. CNS Depressant – barbiturates, ethyl alcohol
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
2. CNS Stimulants – cocaine, amphetamine
3. Antidepressants – tricyclic antidepressants
4. Mood stabilizers – lithium
5. Antipsychotic drugs – phenothiazines
6. Narcotic analgesics – morphine
7. Psychedelics and hallucinogens – LSD
8. Cannabis
9. Neurlogical drugs – antiepileptic drugs – phenytoin
Amphetamines – immediate effet
Antidepressent – Slow evolving (can take weeks to develop fully)
Ameliorate
B.6 Classification of Mental Disorders, Antipsychotic and Antidepressant Drugs
Objectives
1. Differentiate between psychoses, affective disorders, and neuroses
2. Describe the evidence that excessive dopaminergic activity underlies schizophrenia
3. Describe mechanism of action of antipsychotic agents
4. Describe adverse effects of phenothiazines and mechanisms responsible for these adverse
effect
5. Differentiate between the averse effect of phenothiazines, butyrophenones and clozapine
6. Describe the mechanism of action of lithium as a therapeutic agent in manic depressie
illness
7. List adverse effects of lithium and one mens of trying to minimize the adverse effect
8. Classify the various types of depression
9. Describe amine hypothesis of depression
10. Describe the types of depressants and their mechanism of action
11. Describe the adverse effects of different types of antidepressants
PSYCHOSES
Psychoses: are among the most severe psychiatric diordres. Suffer from impairments in
behavior. Inability to think coherently, comprehend reality, or gain insight into these
abnromalities. May have hallucinations
1. Organic
2. Functional (of unknown cause)
Organic Psychoses: cause that are understood and definable – e.g. toxic metabolic changes
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
characterized by confusion, disorientation, memory disturbances, behavioral
disorganzation
Functional Psychoses – retain orientation and memory but have severely disorderd thought,
reasoning, emotion, behavior – schizophrenia
-
AFFECTIVE (MOOD) DISORDERS
Characterized primarily by a change in emotion or mood
Mania – elation, hyperactivity, uncontrollable thought/speech
Depression – feelings of intense sadness, self-disapproval, and physical and mental slowing
Manic-Depressive – alternating period of mania and depression
NEUROSES
Able to comprehend reality but suffering and disability may be severe. Often mood changes
such as anxiety, panic, restlessness – may have limited abnormalities of thought
(obsessions) or irrational fears, or behavior (rituals/compulsions)
ANTIPSYCHOTIC DRUGS (Schizophrenia)
1 in 100 people wil develop schizophrenia in their lifetime
Positive Symptoms: Delusions and hallucinations, bizaare behavior, lack of logic,
incoherence
Negative Symptoms: social withdrawal, loss of motivation
Dopamine Hypothesis: most fully developed theory for schizophrenia but other
neurotransmittesr have been found to be involved (serotonin, GABA, glutamate). Evidence for
the theory is circumstantial and suggests that:
Excessive dopaminergic activity explains the disorder
New antipsychotics have been shown to exacerbate symptoms of schizophrenia
- 5-HT antagonists (Serotonin)
- Glutamate Agonists (Glutamate)
Circumstantial Evidence for Dopamine Hypthesis
1. Most “typical” antipsychotic drugs block postsynaptic dopamine receptors
2. Drugs that increase dopaminergic activity (levodopa, amphetamines, or
apomorphine) either aggravate schizophrenia or induce it in some
3. Dopamine receptor density is increased in post-partem schizophrenics brains
4. PET scans show higher dopamine receptor density in schizophrenics (living)
Mechanism of Aciton in Antipsychotic Drugs
1. Phenothiazine antipsychotics are antagonists at dopamine receptors (block them)
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Adverse/Therapeutic Effects of Drugs (explained by dopamine antagosim):
1. Antipsychotic Action: can be explained by antagonism of dopamine receptors in
mesolimbic and mesofrontal systems because limbic system controls emotion and behavior
2. Extrapyramidal Movement Disordres: Parkinson-like symptoms are observed when
dopamine receptors are antagonized. Tardive dykenisia is a movement disorder that can
occur
3. Endocrine Effects: dopamine in hypothalamus exerts tonic inhibitory effect on prolactin
release. When dopamine receptors are antagonized, excess prolactin will be released milk
flow in women, sexual dysfunction in men.
Other receptors blocked by Phenothiazine Antipsychotics
1. Cholinergic (Muscarine -Acetylcholine) Receptors
- Therapeutic Effect: reduction in extrapyramidal adverse effects
- Adverse Effects: blurred vision, dry mouth, constipation, difficulty urinating
2. Serotonin Receptors
- Therapeutic Effect: reduce extrapyramidal; reduce negative symptoms
- Adverse Effect: unknown
3. Histamine Recepotrs
- Adverse: sedation, drowsiness, weigh gain
4. a-adrenoceptors (norepinephrine)
- Adverse: postural hypotension, dizziness, reflex tachycardia
Other Antipsychotic Drugs
Haloperidol
Chemical structure different to chlorpromazine (phenothiazine). Still blocks dopamine
recepotrs but its sedative and hypotensive action is less. Useful alternative to those
that don’t respond well to phenothiazines
Second Generation Antipsychotics (Atypical Antipsychotics)
Relieve both positive and negative symptoms of schizophrenia. Lower propensity for
extrapyramidal side effects
Clozapine, risperidone, olanzapine
Clozapine: relieves positive and negative symptoms; fewer extrapyramidal side effects
- can cause granulocytopenia –decrease in white blood cells in 1-2% which is a big
problem
- must test blood count at frequent intervals
LITHIUM CARBONATE
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Mood stabilizing agent used to prevent mood swings in manic depressive disorder and
mania
Mechanism of Action:
3 Possibilities
1. Effect on electrolyte and ion transport
2. Effect on neurotransmitters and release of neurotransmitters
3. Effect on second messengers that mediate transmitter action
- Phsphatidylinositol-4, 5-biphosphate (P1P2) is the cell membrane precursor of inositol1, 4, 5-triphosphate (IP3) and diacylglyceral (DAG).
- The enzymic reaction is catalyzed by phospholipase C. (PLC)
- IP3 and DAG are second messengers for alpha-adrenergic and muscarinic
transmission
- P1P2 gets converted to the second messengers then IP3 + DAG are reconstituted
- Lithium blocks two steps in the reconstitution processes of Ip2 - Ip1 I which
leads to the deletion of P1P2. The effects on transmitter on the receptor and the cell
will diminish.
-
Clinical Pharmacology of Lithium
- long term maintenance of manic and depressive episodes of patients with manicdepressive disorder
- Often need treatment temporarily of an antipsychotic drug for acute patients
- During depressive episodes, antidepressant is often needed in addition temporaitily
Monitoring Serium Concentration in Lithium
- taken 12 hours after last dose
- Should be 0.6 to 0.7mEqu/L to be effective and tolerated
Adverse Effects
- Nausea and fatigue after first treatment
- Tremor, thirst, excessive urination, edema, weight gain may persist
- Confusion and loss of muscle coordination
- Toxic kidney effects (chronic treatment, rare)
- Mild hypothyroidism
- Acne and skin reactions
- Malformations in fetus
Alternatives: anticonvulsants valproic acid, carbamazepine and clonazepam
ANTIDEPRESSANT AGENTS
1. Reactive (secondary) Depression: 60% of all accounts; occurs fater a real stimuli
(grief/illness) – can resolve spontaneously or two many different treatments
2. Major Depression (Endogenous): Disturbances in body rhythms of sleep, hunger and
appetite. Loss of pleasure, interest in activities, sexual drive, mental slowing. Genetically
determined biochemical disorder which causes inability to cope with ordinary stress.
Usually response to antidepressant therapy
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
3. Depression in Manic-Depressive Diorder - lithium and antidepressants
Theory of Causes of Major Depression - AMINE HYPOTHESIS
- 1950’s Resperpine was used for treatment of psychosis and hypertension but it also
induced depression
- Reserpine inhibited reuptake and storage of serotoninc and norepinephrine which
caused a depletion of amine stores in these vesicles and amine-dependent
neurotransmission would be diminished.
- Figured, it may be amine dependent neurotransmission that is associatied with
depression
All antidepressants have primary actions on the storage, metabolism or reuptake of
serotonin and norepinephrine
BUT amine hypothesis does not explain all effects of antidepressants in depression
- Neurotrophic hypothesis – depression is associated with reduced neurotriphic
(growth and inter connectivity of neurons) support and that antidepressants stimulate
neurogenesis and synaptic connectivity in cortical areas.
Types of Antidepressants
1. Tricyclic Antidepressants: Imipramine – three-ring nucleus
2. Second-Generation (Atypical) Antidepressants) Bupropion, Amoxapine – less adverse
effects than tricyclics
3. Selective Serotonin Reuptake Inhibitors (SSRIs) – Less effect on ANS and therefore less
toxicity (compared to tricyclics)
4. Drugs that Block Serotonin and Norephinephrine uptake: venlafaxine – better safety
than tricyclics
5. Monoamid Oxide Inhibiotrs (MAO) : two monoamine oxidase (MAO) enzymes – MAO-A
and MAO-B. MAO-A is the enzyme responsible for metabolism of norepinephrine, serotonin
and tyramine. MAO-B is selective for dopamine metabolism. Blockade of MAO-A is useful for
therapy of depression
6. Phenelzine and tranylcypromine – non-selectie inhibotrs of MAO-A and MAO-B.
7. Moclobemide – Selective MAO-A inhbibitor
Action of Antidepressants on Biogenic Amine Neurotransmitters
Amine Hypothesis has been strengthened by studies of mechanism of action of antidepressant
drugs.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Tricyclic: block the amine presynaptic transprter proteins which are the “off” switches of
amine neurotransmission. This allows for longer neurotransmitter time at receptor sites and
greater stimulation of postsynaptic neuron
MAO inhibitors block major degradative pathway for amine neurotransmitters – permitting
more amines to accumulate at presynaptic stores and more to be released when nerve
impulses reach presynaptic neuron
SSRIs selective for blockade of serotonin transporter protein in presynaptic terminal – less on
norephinatphine
Bottom line: antidepressant drugs remedy a deficiency in amine neurotransmission through
different mechanisms
Choice of Antidepressants
SSRI’s - preferred, especially for major depressive disorder and anxiety disorder
MAO – helpful for those who can’t handle tricyclics or SSRIs
TCAs and MAOs are second line drugs
Adverse Effects
Tricyclic Antidepressants (TCAs):
- Anticholinergic effect – dry mouth, uriary retention, constipation, blurred visio,
sedation, weight gain, sexual dysfunction and hypotension
- Disturb electric rhythm of heart
- Over dose is lethal
SSRI’s
- nausea
- headache
- nervousness
- insomnia
- high sexual dysfunction
- MUCH SAFER THAN TCAs in overdose
MAO
- Interact poorly with many drugs (prescription, over the counter, and tyramine
contaiing food)
- Must maintain caution for several weeks
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
B.7 Stimulant Drugs
Objectives:
1. Describe Mechanism of Action of Cocaine, Amphetamines and Caffeine
2. Describe responses to various doses of cocaine, amphetamines and caffeine
3. Describe methods used to adminster illicit cocaine and amphetamines
4. Describe dependence liability of cocaine, amphetamines and caeffiene
5. State the differences in response to cocaine and amphetamines
AMPHETAMINES
Class of CNS stimulants that enhance th acitivty of the brain
Dextroamphetamine, Methamphetamine and designer drugs
methylenedioxyamphetamine
History
1887 first synthesis of amphetamine
1933 Discovery of CNS stimulant action of amphetamine
1939-45 Use of amphetamines as anti-fatigue agents during ww2
1945 First marketing fo amphetamine as an appetite suppressent - lead to many dependent
1945-1958 Epidemic of abuse of amphetamines in Japan –
1960s Outbreaks of abuse of amphetamines in Sweden, US and Canada
1973 Clssification of amphetamines as controlled drugs in Canada restriction of legal use to
medical problems
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Chemistry
Amphetamines are synthetic organic compunds structurally similar to norepinephrine,
epinephrine and dopamine
3 common amphetamines: amphetamine, detroamphetamine, methamphetamine
- Amphetamines can be synthesized easily, especially methamphetamine
Pharmacology
Amphetamines stimulate the CNS and SNS
- Methamphetamine has more central stimulation and less SNS
- In CNS amphetamines act by releasing neurotransmitters: norepinephrine and
dopamine
- Dopamine released is responsible for the pleasurable respones produced by
amphetamine
Cardiovascular System effects of amphetmaines – due to displacement of norepinephrine
from adrenergic nerve terminals which acts on alpha and beta receptors (vasculature and
heart respectiveyly
1. flight response
2. Incerased BP
3. Increased HR
CNS Effects of Amphetamines- mediated y action of catecholamines in CNS
- Amphetamine increase release oand inhibit acive reuptake of dopamine and
norephinephrine
- Dopamine is primarily in many of the CNS effects
1. Behavioral and psychomotor stimulation (alterness, hyperactivity insomnia)
2. Anorexia (reduce appetite)
3. Hyperthermia (increase in body temp)
4. Respiratory center stimulation
5. Neurotransmission in spinal cord
6. Convulsions with high doses
Amphetamines on Brain Aras
- Reticular Activating System – decrease threshold for transmitting sensory input to
cerebral cortex
- Medial Forebrain Bundle (MFB) is stimulated – mediates reward
- Hypothalamus – temperature regulating, feeing centers are modified
- Limbic System – emotion (amphetamines may lead to aggression)
Methamphetamine > Dextroamphetamine >Amphetamine
- for magnitude of CNS effect
Therapeutic Uses of Amphetamine-Like Drugs
1. Narcolepsy – amphetamine and methylphenidate are effective but methylphenidate is
drug of choice because less cardiovasucalr effects. No tolerance to therapeutic effect
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
2. ADHD – D-amphetmine and methylphenidate helps increase attention/concentration
3. Parkinson’s Disease – amphetaimes
Amphetamine Abuse
- produce euphoria and are effective CNS stimulants therefore, widely abused.
- Usually orally, inected or smoked
Low Dose: CNS overstimulation, restlessness, dizziness, insomnia, euphoria, dysphoria, mild
confusion, tremor
Cardiovascular: irregular heart beat, headache, increased BP
Respiratory: increased respiratory rate
Other: increased OR decreased libido
High Dose: increased exhiaration and euphoria, flowing ideas, talkative, excitation, agitation,
irritability, paranoid thinking, confusion, distortion of events seizure, highfever, stroke
Amphetamine Rushb – can be accompanied with violent behavior
Cardiovascular: heart attack, angina pain, dysrhythmias, changes in BP and fainting
Long Term Use: chronic sleepin gprolem, anxious/tense, poor appetite, BP elevated,
suscpicious, paranoid, repetitive behavior
Lifestyle problems (needles, poor nutrition)
Amphetamine Run
The attempt to mainain initial effects of exhilaration and enhanced awarness and self
confidence by repeatedly administer the drug for several days – speeders or speed freaks
Tolerance – develops to some by not all effects euphoria and mood elevating tolerance
develops rapidly but not drug-induced psychosis. Tolerance develops to lethal effects,
anorectic effects and cardiovascular and respiratory stimulatory effects
Physical Dependence – cessation of administration may result in mood depression that may
be profound, prolonged sleep, huge appetite, lassitude and fatigue. Mood depression may be
the main withdrawal symptom
Psychological dependence – will crave the reward so intensily that if it’s not available they
will panic
Potential For Abuse:
1. Dependence Liability is extremely high (powerful euphoria)
2. Route of Administration – esasily dissolvable for injection
3. Inherent harmfulness in long-term toxicities but this does not deter abusers
COCAINE
- naturally occurring alkaoid form cocoa bush in south America
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1884 – Freu studied CNS effects of cocaine and used it to withdraw a colleague from morphine
which lead to dependence on cocaine third scourge of humanity
1884 Koller introduced cocaine as local anesthetic
1970s -90s – Incerase of non-medical use in north America – cocaine replaced amphetamines
as major stimulant to abuse.
Currently one of the most popular recreational drugs next to alcohol, nicotine,
caffeine and marijuana
Pharmacology
CNS Effects: due to generalized CNS stimulatio and is dose-dependent. Similar behavioral
effects to amphetamines. Duration is BRIEF (less than one hour)
Mechanism of Action:
1. Cocaine inhibits active reuptake of released dopamine and norepinephrine into
presynaptic terminal
2. Increases activation at postsynaptic receptors
3. Causes excitation of dopamine receptors and norepinephrine receptors
The local Anesthetic Effect: blockade of nerve impulse in sensory nerve fibres –
Main Differences Between Cocaine and Amphetamine
1. Shorter duration of action for cocaine
2. Lower incidence of complications with intravenous use as cocaine is usually snorted
3. Tolerance does not develop as readily to the hallucinatory and behavioral effects of cocaine
as compared to amphetamines
Therapeutic Uses of Cocaine
- ONLY legit use is as a local anesthetic for mouth and throat but rarely used
Cocaine Metabolism – metabolized into inactive metabolite benzoylecgonine which is
excreted – detected upt o 48 hours after single dose, 2 weeks in chronic user
Cocaine Abuse
Very powerful stimulate with intense euphoric feelings and is widely abused
Low Dose – dilate pupils, exaggerated reflexes, euphoria and sense of well-being and
postponement of physical and mental fatigue, reduced appetite or need for sleep, increased
talkativeness OR quiet contemplation, increased self-confidence and feelings of superiority
Cardiovascular: vasoconstriction, increased HR, increased BP
Respiratory: increased respiratory rate
High Dose: intensitifaction of low dose plus
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Behavioral: euphoria then severe agitation. Rapid flight of ideas, feelings of
grandiosity, paranoid thinking and bouts of repeated/meaningless behavior
(stereotypy)
Neurological: tremor and muscle twiches, seizures, headaches, hemorrhagic stroke and
cerebral infarction
Cardiovsacular: high BP, headache, pallor, rapid weak pulse, heart attack
Gastrointestinal: nausea and vomiting
Respiratory: shallow beathing and pulmonary edema and hemorrhage
Renal: acute renal failure, secondary to the detioratio of muscle tisse
Other: elevated body temp and cold sweat
Long Term Use: nervous, agitated and excitable with mood swings. Psychosis including
paranoia, hallucinations, sensations of insects crawling under skin. Sleep and eating disorders.
Sexual function is impaired. Changes in nasal mucosa from snorting. Social problems
Cocaine Binge: heavy users take it repeatedly over several hours to days to maintain
euphoria
Cocaine Dependence
Tolerance – develops to mood-elecvating effect but not to psychotic effect
Physical Dependence – withdrawal symptoms similar to amphetamines
Psychological Dependene - the pharmacodynamic characteristics of smoking crack are
almost ideal for development of compulsive drug use. Behavioral effect of cocaine usually
perceived as pleasurable and rewarding – reinforcement. Other psychoactive durgs are
usually concurrently used
Potential For Abuse
1. Dependence Liability - one of the HIGHEST of all drugs of abuse
Route of Administration – injection or inhalation causes rapid effect
2 Availability 3 Inherent Harmfulness – among the HIGHEST among drugs of abuse. But do not deter user
CAFFEINE
Most widely used drug in the world. Affects the CNS and the cardiovascular system
PHARMACOLOGY
Cerebral Cortex – increases mental performance and decreases drowsinesss/fatigue. Enhances
motor activity
Medulla – respiratory and vasomotor centers are stimulated increasing respiration and HR
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Cardiovascular System - low does increase HR and BP; high dose disturb heart rhythm
Mechanism of Action
1. Block adenosine receptors in brain
- Adenosine exerts inhibitory effect on neurons/transmitter systems
2. Blockage causes these neurons to be released from adenosine inhibition
3. Neuronal activity is increased
Low Dose
CNS – mood elevation, reduced fatigue, small increase of performance
Cardiovascular – constricts cerebral blood vessels (useful in headache) and peripheral blood
flow is increased stimulates cardiac muscle
Respiration – mild stimulation of respiratory rate and relaxation of bronchial smooth muscle
High Dose
CNS – irritability, restlessness, nervousness, insomnia, rampling of thoughts/speecn, agitated
movement of involuntary muscles
Cardiovascular – rapid and irregular heartbeat
Long Term Use: excess caffeine wil lead to restelessness, nervousness, insomnia, increased
urinary output, gastric upset and rampling speech/thought
Tolerance and Dependence
- Some evidence that tolerance does develop
- Dependence does develop. Headache, fatigue, and drowsiness can result if abrupt
cessation occurs. These symptoms are alleviated with caffeine. Psychological
dependence does occur.
Potential for Abuse
1. Dependence Liability – low, low reinforcer
2. Availability
3. Inherent Harmfulness – very low
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
B.8 Alcohol (Ethanol)
Objectives: p. 109
Ethanol is one of the three most used non-medical drugs in Canada (other = caffeine and
tobacco). Alcohol and ethanol are used interchangeably
Consumption has been reducing but health care costs remain enormous and more health
problems and deaths than all illicit deaths combined. It’s readily available and permissivie
attitudes of society
Historically alcohol was used as a sedative-hypnotic drug in ancient times. Traditionally it has
3 major purposes
1. Medical: sedative-hypnotic
2. Religious: sacramental use
3. Recreational
Ethanol Content of Alcoholic Beverages
1 drink = 341 ml (12oz) of beer 5%v/v = 43ml (1.5oz) spirit 40%v/v
= 170 ml (6oz) wine 10%v/v = 17 ml absolute ethanol = 13g absolute ethanol
10-13 ml of absolute alcohol is metabolized / hour by the liver
Absorption of Ethanol
Absorbed rapidly from stomach and uppr small intestine. Influenced by:
1. Stomach-emptying time OR time required for alcohol to reach the small intestine
2. Ethanol concentration in the G.I. Tract
The time from last drink to maximal blood alcohol concentration ranges from 30 to 90
minutes
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Distribution of Ethanol
Ethanol distributes throughout the total body water and distributes across blood-brain
barrier. For pregnant women, it distributes across the placenta and throughout total body
water of the fetus
Metabolism and Excretion
95% is eliminated by biotransformation in liver; 5% is excreted by breath, urine and sweat
Aldehyde dehydrogenase (ADH) converts alcohol to acetaldehyde. Then ADH converts
acetaldehyde (ALDH) into acetic acid. Acetic acid then is metabolized by tissues.
- Disulfiram and calcium carbimide (drugs to treat alcohol abuse) inhibit ADH and
then acetaldehyde accumulates and the indidividual will feel ill and stop abusing
alcohol
Metabolism of alcohol is constant rate regardless of blood alcohol concentration. This is
because ADH becomes rate-limiting/saturated at 20mg of alcohol per 100ml of blood
The normal body rate of ethanol metabolism is 120mg ethanol/kg body weight/hour. For
a 70kg person, the rate is 8.4g ethanol/hour or 10.6ml ethanol/hour
With this rate, blood ethanol concentration decreases at a rate of 15mg ethanol/100ml blood
per hour
Pharmacology and Toxicology of Alcohol
Ethanol is a CNS Depressant
Acute Use: more obviously affects the CNS than chronic, hight dose which affects organ sytems:
CNS, cardiovascular, gastrointestinal and liver. Chronic maternal use of high dose can lead to
fetal alcohol syndrome or fetal alcohol effects
Medical Uses of Ethyl Alcohol (Ethanol)
Few medical uses but some are:
- alcohol sponges applied to treat fever
- Skin disinfectant
- Low dose used as aperitif to improve appetite and digestion
- Antidote in the treatment of methanol poisoning
- Hand sanitizer
Central Nervous System
Ethanol produces dose-dependent depression of CNS function
Disinhibition sedation hypnosis general anesthesia coma
Low Dose: disinhibition, increased talkativeness and social interaction
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
High Dose: sedation hypnosis general anesthesia coma
CNS effects are proportional to BAC:
50mg/100ml (~2 drinks) – euphoria, minor motor disturbances
60mg/100ml – nystagmus, errors in math tets, increased motor incoordination
80mg/100ml – impaired driving ability, changes in electroencephalographic patterns
100-150mg/100ml – Gross motor incoordination
200-300mg/100ml – amnesia for the drinking experience
300-350mg/100ml – coma
350-600mg/100ml – may cause/lead to death
there is an appreciable interindividual variability in this relationship
Mechanism of Action – not understood.
- At high concentrations it was believed the drug depressed excitable cells in a nonselective manner
- At low concentrations it was believed that alcohol binds to GABA receptors to augment
GABA-mediated neuronal transmissions (inhibitory)
Effects of Alcohol
Low dose: disinhibition, feel jovial, relaxed, confident. Sometimes sleepy or irriated. Impaired
motor functions and more risk taking
High Dose: exaggerated emotional responses, thinking/memory/judgment and motor is
impaired
Adverse Short Term Use:
Blackouts: drinker does not remember events under the influence of alcohol
Psychiatric Effects – heavy drinking can lead to depression, irritability and over-sedation.
Drinking and Driving - 43% of fatally-injured drivers have consumed alcohol, 35% were
over 0.08. 20% of drivers report having drank and driven (25-45 greatest risk). The risk
increases exponentially as blood alcohol increases
Violence: those who drink heavily are more prone to violence
Respiratory Depression, Coma and Death – comatose drinkers aspirae their vomit and die
DOES NOT ENHANCE SEXUAL PERFORMANCE
Adverse Effect of Long Term Use;
Central nervous system : neurological and mental disorders – alcohol damages axons in brain
which leads to fewer connections between neurons
Dementia – reduced cognitive functioning, memory, judgment, thinking
Wernicke’s Encephalopathy – drowsy, confused, can’t walk (Vitamin B1 metabolism
is increased which results in thiamine deficiency
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Korsakoff’s Psychosis – severe form of dementia (thiamine deficiency)
Peripheral Nervou System
- Damages axons here too; cause burning pain and difficulty in walking
Ethanol Dependence
Chronic use in high doses can lead to dependene = alcoholism
Tolerance
Chronic use of ethanol causes a decreased intensity of ethanol action or shorterned duration
of action larger dose is needed. Some individuals can develop tolerance more rapidly to the
ethanol-induced impairment of performance of a task when they perform that task repeatedly
Mechanism
1. Metabolic tolerance due to increased ethanol metabolic rate same dose produces lower
blood-ethanol concentration or maintains the blood ethanol concentration above a certain
level for a shorter time
2. Cellular (functional, pharmocodynamic) tolerance: CNS adapts to effects of ethanol
MINIMAL TOLERANCE DEVELOPS TO THE LETHAL DOSE OF ETHANOL
Cross-Tolerance
1. Ethanol and sedative-hypnotics
2. Ethanol and general anesthetic
Physical Dependence – primarily involves CNS. Withdrawal produces excitability of CNS –
hyperexcitabiliy, leads to tremors, irritability, restelessness, anxiety, sweating, sleeplessness,
agitation, nausea, muscle tension, hyperthermia, increased HR – can lead to convulsions, coma
and death.
Severe case: Delirium Termens – tremulousness, auditory, visual and tactile
hallucinations, confusion, psychomotor agitation, disorientation and sleep disorders
Treatment: oral administration of diazepam (benzodiazepine-type sedative) – working on the
idea of cross dependence e
Psychological Dependence
There is an compulsive desire to seek,obtain and drink ethanol. May be the most powerful
factor in chronic use of ethanol. Naltrexone is effective treatment for psychological
depenence on alcohol.
Potential for Abuse
1. Dependence Liability – moderate
2. Availability – verrrry available and legal
3. Inherent Harmfulness
Cardio Vascular Effects: acute: vasodilation, alter normal rhythm of heart
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Chronic; low – reduced risk of heart disease/stroke high – destruction of
heart muscle and increased incidence of hypertension and stroke
Gastrointestinal Tract; low – gastric secretion and enhance appetite; high – irriatete
stomach lining causing ulcers
Liver low: no adverse effects; high – can lead to hypoglycemia (low blood sugar)
Chronic: alcoholic liver disease – major cause of death
1. Fatty liver
2. Alcoholic hepatitis
3. Cirrhosis – not reversible – damaged liver cells are now scar tissue
Embryo/Fetus
- Ethanol is a teratogen
- Fetal Alcohol Syndrome: facial abnormalities, CNS dysfunction, growth deficiency
- Fetal Alcohol Effect: have some of the symptoms of FAS but not all
Drugs to Treat Alcoholism
- used as pharmacological adjuncts to psychotherapy
- Drugs inhibit ADH and produce increased acetaldehyde making patients feel ill
Alcohol Drug Interactions
1. Acute Ethanol Use during Drug Therapy
1. Ingestion of Ethanol and CNS depressant has additive effect
2. Ethanol inhibits biotransformation/metabolism of certain drugs (sedativehypnotics)
2. Chronic ethanol use followed by drug therapy – not ethanol in body
Caues proliferaion of smooth endoplasmic reticulum of liver cell causing increased
activity of the liver drug-metabolizing system. There will be increased biotransformation of
certain drugs if there is no co-existing ethanol induced liver injury
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
B.9 Cannibis
Cannibis: drug containing forms of the hemp plant “cannabis sativa” – 2 types
1. Resin-producing
2. Fibre-producing
There are 420 chemical compounds in cannabis that are common to other plants and 60
unique – including THC
The 60 unique compounds are cannabinoids
THC is most potent and causes hallucinations
HISTORY
2700BC-1800 – Cannibis was manufactured as rope
1920-1930 – legislation outlawed use of marijuana
1960-70 - increased use of cannabis in form of marijuana
1978 – USA sponsored project herbicide to destrey cannabis crops in Mexico * found toxic
substane paraquat that is toxic to lungs
1980 – 42% of HS sctudents used weed in USA
1990 – Weed was the third most popular psychoactive drug (alcohol and dobacco, 4 th if you
include caffeine)
1996 – Arizone approved legal use of weed for medical purposes
1997 Ontario dismissed charges for possession for those with epilepsy
2002-2005 – health Canada supported trials for medical use of weed – program is suspended
CLASSIFICATION
Legal Classification: Marijuana - a narcotic controlled under the Narcotic Control Act
Pharmacological Classification: CNS depressant, euphoriant and hallucinogen
(hallucinations only at high doses)
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Mechanism of Action – not fully understood
1. THC binds to receptors in cerebral cortex, cerebellum, hippocampus etc.
2. Recptors called CB1 receptors
3. Endogenous ligand anandamide binds to CB1 receptors. When anandamide or THC
activates CB1 receptors, it inhibits the release of excitatory neurotransmittors
4. In periphery THC bninds to CB2 receptors on lymphocytes
THC is absorbed though smoke or oral administration but smoke effect is almost immediate
Drug Test: metabolized slowly and half life is 30 hours. Elimination from adipose tissue is
longer. Drug tests measure metabolites of THC - chronic users will be positive for metabolites
for several weeks
Medical Use of Marijuana
- Sedatives and hypnotics but not anymore
- Nausea and vomiting from anticancer drugs
- Anorexia (increases appetite)
- Epilepsy
- Glaucoma
- Spasticity
- Migraine
Anticancer drugs and THC synthetic derivaties: dronabinal and nabilone are more
selective than THC
Neuropathic Pain: dose inhaler has been approved – probably more effective than a
tablet
Non Medical use: street drug
Marijuana – dried flowering tops and leaves of plants
Hashish – dried resin
Effect of Cannabis
Low-Moderate Dose:
CNS: relaxation, drowsiness, disinhibition and talkativeness
- euphoria, exhilaration
- distortions in perception of time, body image and distance
- Enhanced senses of touch smell and taste
- Spontaneous laugher
- Motor coordination is impaired
Cardioascular: increased heart rate and blood flow
Respiratory: smoke irritates membranes lining respiratory system – bronchodilation
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Gastrointestinal: increased appetite and dryness of mouth/throat
Sexual; may reduce testosterone levels in men, and disrupt ovarian cycle in females
High Dose: increase effect and hallucinations
Long Term Use:
- psychological dependence
- Amotivation syndrome – mental slowing, loss of memory, can’t think abstractly, loss
of drive, emotional flatness
- Bronchitis
- Asthma
- Sore throat, irritation
- Cancer
- Can effect fertility
Tolerance
- psychoactive tolerance occurs
- Physical depdencen can occur withdrawal symptoms
Risk of Abuse
1. Dependence Liability - is low to moderate – high euphoria but not the highest
2. Availability
3. Inherent Harmfulness is LOW
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
B.10 Nicotine
Nicotine is found in tobacco.
Nicotine, caffeine and alcohol are 3 most used psychoactive drugs in society
Nicotine has no therapeutic value other than in smoking cessation programs
Tobacco results in large number of health problems and 100 deaths each day –
increase in use from 1940s to 1970s because it was “cool”. Steady decline however
recently(61% down to 27%)
Nicotine is NOT responsible for long term effects of smoking
PHARMACOLOGY OF NICOTINE
Nicotine stimulates CNS – increased psychomotor activity, cognitive function, attention and
enhanced memory
Large doses can produce tremors, seizures, and agitation.
Nicotinic receptors mediate the release of dopamine and serotonin mediates CNS effects
PNS – nicotine stimulates sympathetic ganglia and drives SNS --< increase in HR and BP
Powerful reinforcing Properties
20% of the nicotine in cigaraettes is absorbed during normal smoking and nicotine dropblets
are also absorbed through the gastrointestinal tract, oral mucosa and transdermally
Nicotine is rapidly metabolized and excreted through urine. Half-life = 2 hours
MEDICAL USE – only cessation of smoking
EFFECTS OF NICOTINE USE
Short Term: dizziness, headache, nausea, vomiting, abdominal cramps. Mild euphoria,
enhanced arousal, concentration, relaxation
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Long Term: premature death;
cardiovascular disease (atherosclerosis) 1/3 all CVD deaths
Lung disease – increased by smoking - wheezing, chest pain, congested lung
- emphezema
- lung cancer; oral cavity cancer, throat, bladder, uterus cancer risk
Passive Smoke (Second-hand Smoke) - 300 Canadaians
Tolerance – does not appear to be great
Physical and Pychological dependence – withdrawal: irritable, anxiety, insomnia, fatigue,
can’t concentrate
Abuse
1. Dependence Liability – high degree
2. Availability – legal
3. Inherent Harmfulness
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
C.1 Drugs for Tratment of Angina Pectoris and Congestive Heart Failure
TRETAMENT OF ANGINA PECTORIS
Angina Pectoris: choking pain in chest due to lipid deposits in coronary arteries hindering
blood flow. Sudden severe pressing pain in chesst. TO reduce pain, one must increase oxygen
requirement of the heart/ increase oxygen supply to deficient areas of heart muscle
Precipitated by FOUR E’s
1. Eating
2. Exercise
3. Excitement
4. Exposure
1768 William Heberden first described angina pectoris - “painful disagreeable sensation in
the breast which seems as if it would extinguish life if it were to increase or continue”
Treatment Options
1. Organic Nitrates
1857 - Amyl Nitrite was first agent introduced by Brunton – anginal pain would be
relieved in 30 to 60 seconds but the effect was short lasting and dosage was difficult to
adjust
1879 William Murrel introduced sublingual nitrogrlycerin (glycerol trinitrate) –
the effect lasted 20 to 30 minutes
Mechanism of Action
1. Relaxatino of large veins leading to vasodilation – decrease in energy expenditure,
decrease in heart sie, deceras in blood pressure
2. Dilates large coronary arteries – enhanced oxygen supply to heart
Nitroglycerin was made stable by Alfred Nobel was made when he learned to
stabilize nitroglycern by absorbing it on the absorbent Kieselguhr
1. Endothelial lining of cells in blood essels are Nitric Oxide (NO) that is made
by amino acid arginine
2. NO passess from endothelial cell into smooth muscle cell of blood vessel to
catalyze reactions
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
3. Nitric Oxide activates enzyme guanylyl
4. causing relaxation of blood vessel
5. Nitroglycerin enters blood vessels and is converted to NO --
2. Organic Nitrate Preparations
Nitroglycerin (Glyceryl Trinitrate, GTN) Sublingual
- much more intense effect when given sublingually
- peak levels within 5 minutes but only lasts 20-30 minutes
- fast onset shorter duration
Nitroglycern (GTN) Ointment – 2%
- Absorbed into blood vessels under the skin
- Takes approx 1 hour for peak levels but lasts 3 hours
- Slow onset longer duration
Transdermal GTN Systems (GTN Patch)
- oinment wrecked people’s cloths
- GTN impregnated into a polymer bonded to a membrane to control GTN
movement across skin
- Long lasting – 24 hours but as tolerance develops – 12-16
Tolerance
- GTN given sublingually no tolerance
- GTN tolerance is seen in explosive industry (first feel dizzy/headaches, then
don’t)
- Transdermal GTN – apply for 12 hours, then remove for 12 to allow patient to
recover sensitivity
Therapeutic Uses of GTN
1. Termination for an individual attack given sublingually
2. Prevention of individual attack sublingual and increases sthe exertion tolerated
by a patient before the amount of oxygen in heart muscle drosp to level of that pain is
experienced (e.g. taking exercise that would normally precipitate angina
3. Chronic prophylaxis several attacks a day; transdermal GTN or isosorbide
dinitrate
3. β –Adrenergic Blocking Agents (Propranolol)
Mechanism of Action – angina is precipitated by factors that increase SNS activity
(stress and exercise). Increased SNS results in increase HR and myocardial
contractility which leads to increased cardiac output and increased myocardial
oxygen requirement leading to angina pain
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
β-Adrenergic Blocking Agents such as proponal will block β receptors in the heart
, drecreasing heart rate and myocardial contractility
E.5 Drugs In Sport
Used for centuries, started more and more beginning in 1950s
Rationale for Banning: use of performance-enhacing substances is unethical. All athletes
should compete on their own abilities. Competition should compare the athletes not the team
of doctors, biochemists and pharmacologists behind then.
Random doping is used to enforce the ban
Main Drugs Uses
1. Reduce Pain/Inflammation – local anesthetics, narcotics, and anti-inflammatory steroids
(cortisone)
2. Increase Endurance and Speed – amphetamine and it’s derivatives. Blood doping
3. Increase strength – anabolic steroids and growth hormone
4. Alter heart – beta adrenoceptor blocking drugs propranolol used for precision sports
5. Reduce Body Weight – diuretics
6. Sedatives – benzodiazepines are used
Terms
Stacking: using several different drugs in the same class (e.g. 3 anabolic steroids). The body
may eliminate each drug at a rate independent of the other so using smaller doses of three
separate drugs, the athlete can use drugs closer to competition and it will be removed from
the body prior to the competition
Pyramiding – starting with small doses and building to large dose for maximal effect then
tapering to small doses and stoping the drug just before competition to have lower dose
eliminated quickly and athlete will be drug free
Doping Control – process of measuring the drug in urine
Masking – process of taking a second drug to mask the detection of the banned drug in urine
AMPHETAMINES
Powerful stimulants that produce alertness and feelings of power. Amphetamines increase
endurance and speed.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Toxicities
increase activity of CNS and PNS which result in excitation and euphoria – as the drug wears
off you experience a crash significant increases in HR and BP; large doses can lead to fatal
increases in blood pressur
Toxicities and Dependence develop quickly
ANABOLIC STEROIDS
Reduced androgenic effect but maintain anabolic effect – build muscle mass. Used for
muscle mass and strength as well as to enhance physical appearance
Previous research has all used low doses of anabolic steroids and shown that there was no
significant enhance in performance. Plus, the studies did not use conditioned athletes and
trained athletes may respond differently. The sports world knew there was a benefit –
especially for weigh lifters in a signle rep event
Recovery period between training sessions is reduced so you can train harder longer
Anabolic steroids increase size, and strength of athlete but not aerobic performance.
Mechanism of Action: (3 potential)
1. Produce anti-catabolic response – action of plateau point being reached where
more muscle fuel is used than produced is blocked by anabolic steroids
2. Anabolic effects produce new protein
3. Produce “Roid Rage” – aggressive behavior/motivation that may be beneficial
Summary
1. Low to moderate doses have modest effects on average adult
2. Effect on inexperienced weight lifters is less than a good exercise program
3. Large doses yield significant inceraes in lean body mass and strength
4. Aggressive behavior induced by steroids contributes to performance effects
5. High diet in protein is required to be fully effective
Toxicity – reduced testosterone levels; altered liver function; mood swings; CVD
Females – less use; enlarge clitoris, low voice, course skin, facial/body hair, amenhorrea
Designer Steroids
- Tetrahydrogetrinone – circumvent detection;
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Beta-Blockers (propranolol) – used when precision is needed to calm heart beat
Benzodiazepines – reduce anxiety in ski jumpers to calm nerves
Growth Hormone - increase muscle mass and therefore strength – clears body rapidly
Blood Doping – collect athletes own blood which is infused just before competition
enhanced hemoglobin concentrations and oxygen carrying capacity of the blood
Erythropoietin – protein hormone that stimulates red blood cell formation – enhanced
oxygen carrying capacity
Darbepoietin - stimulant of choice during salt lake city Olympics
Diuretics – reduce body water to compete in lower weight class
OTHER DRUGS
Probenecid – block urinary excretion of other drugs and reduce their levels in urine so they
won’t be detected
Caffeine – can’t be found in levels that exceed those expected from ingestion of a couple of
cups of coffee. All mild stimulates are banned – including ephedrine
Food Supplements may contain banned substances: Dehydroepiandrosterone (DHEA) is
precursor to testosterone and testosterone is a performance enhancer – DHEA is banned for
athletic use in Canda
Creatine: protein supplement used in body building. Efficacy is not established.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
E.6 Regulation of Fertility
CYCLE
Beginning: estrogen and progesterone are LOW
hypothalamus secretes gonadotropin releasing factor (GRF) which stimulates anterior
pituitary to release of FSH and LH
FSH causes ovarian follicles to enlarge ONE Follicle develops and others regress
Maturing follicle secretes etrogen in small amounts until peak at DAY 14 (ovulation)
Near Day 15 – LH secretion peaks – stimulating maturing ovarian follicle to grow more
rapidly
HORMONAL CONTRACEPTIVESU
1. Fixed Combinations: Estrogen and Progestin – Taken from 5th to 25th day of cycle (day 1
being onset of menses) – first was Enovid-E
2. Multiphasic (biphasic and triphasic) – fixed amount of estrogen and variable amounts
of progestin increasing from week to week. Advantage: hormone dose kept to a minimum
and mimics the pattern of hormone release in ovarian cycle
3. Continuous Estrogen progestin preparations – estrogen-progestin combo for 28 days
with no drug free period
4. Transdermal Contraceptive Patch – ethinyl estradiol and progestin (norelgestromin)
applied to patch on skin. Drug is delivered constantly for 7 days then use another patch (3
weeks) – same mechanism as oral estrogen-progestin contractevipves
5. Low Dose Progestin/Mini-pill – synthetic progestin – daily dose is taken as long as drug
is needed. Breakthrough bleeding is often a problem – less effective at preventing pregnancy
6. Norplant – silicone tubes filled with L-norgestrel (progestin) implanted under the skin –
drug is released over a period of five years. $700 but htat’s 3 years of a combo pill.
7. Depoprovera – injectable progestin every 3 months
Mechanism of Action
Estrogen Progestin Combinations:
1. Estrogen inhibits release of GnRH from hypothalamus – FSH and LH are not released,
follicles don’t mature
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
2. Progesterone results in thick secretions (usually thin) for whole cycle, not good for sperm
migration
3. Preparation of endometrium is not optimal (estrogen and progestin)
Low-Dose Progestin and Norplant and DepoProvera
1. Progestin inhibits the release of GnRH and ovulation is then inhibited
2. Endometrium is not fully developed
3. Thick secretions are not optimal
Progestin-alone is less effective (98% vs. 100%) but better for those who shouldn’t
have estrogen
Adverse Effects with Hormonal Contraceptives
Low-Dose Progestin: Mini Pill –
-
Breakthrough bleeding occurs
Sometimes plasma lipids are altered increase in LDL and decrease HDL causing an
increase risk of coronary vascular disease
Norplant
-
Breakthrough bleeding and duration of menstrual bleeding
Weight gain
Headache, nervousness, anxiety
Acne
Muscular pain, breast discharge, abdominal discomfort
Estrogen-Progestin Combinations
Mild – Nausea, Edema (water retention), headache, libido increase/decerase, menstrual flow
reduced, weight gain, increased skin pigmentation – estrogen causes, acne and hirsutism
(progestin), vaginal/uterine infection more common, post-drug amenhorrea, cholestatic
jaundice, less folate absorption
Serious – Thromboembolic disease: increased tendency for clotting
- Myocardial Infarction – increase risk
- Cerebrovascular disease (stroke) – increased risk
- Hypertension – more prevalent
- Cancer – reduces risk of endometrial and ovarian; no effect on breast cancer. Hepatic
adenomas have been reported
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Most of the toxicities were thought to be associated with estrogen but could be
progestin
Antiprogestins (Mifepristone)
-
-
Maintains endometrium in the last half of the cycle and during pregnancy.
Mifepristone blocks effect of progesterone on endometrium and endometrium lacks
support = lining is sloughed. This drug can be taken after a “missed period” to bring on
menstruation not approved as contraception (more like a Plan B)
Post Coital Contraceptives
-
Large doses of estrogen taken after coitus delays/inhibits ovulation. Nausea is caused.
Intrauterine Device
- IUD – hormone or copper placed into uterus
- Problems: heavy flow, discomfort, 10-15% expel spontaneiously, increase in uterine
infections
Diaphragm and Spermicidal Jelly
- must be fitted properly, must be inserted before coitus, must remain in for 6-8 hours
- not a great rate
Condoms – effective, interfere with sex act (15/100 women) because of error or breaks
Female Condoms – prevent STDs and pregnancy but not easy to use and not popular
Rhythm Method - body team and calendar
Coitus Interruptus – “pull out” (25/100)
Vaginal Douche - not effective.
Tubal Ligation – permanent conception – tying tubes
Vasectomy – sperm ducts ied off
Drug Contraceptvies for Men – not reached candian market yet. At bet 80% infertility rate.
Some promise in gonadotripin releasing hormone antagonist
1. Control of Spermatogenesis - GnRH stimulates sperm production but altering in males
can upset the libido because it’s closely connected to testosterone
2. Gossypol – phenolic from cottonseed that destroy elements of seminiferous tubulesdecreasing sperm production but doesn’t alter sex drive.
- Low potassium is a problem and this has resulted in transient paralysis
3. Estrogens – to suppress GnRH but this tends to decrease testosterone too and lose sex drive
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
- added small amounts of androgens but only 60% were infertile
4. Androgen based contraceptives – androgens can inhibit GnRH and spermatogenesis.
Inject intramuscularly but only 90% lower sperm count and enhanced secondary sex
characteristics s(aggression)
5. Progestin combined with androgen – inhibit GnRH but also loses testosterone.
Androgen added replaces testosteone promising but appropriate does of androgen is
challenge.
Efficacy of Contraceptives:
Oral Combo
Oral progestin only
Depo Provera
IUD
Diaphragm w/spermicide
Condom
Spermicides
Rhythm
No contraception
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
E.2 Over-The-Counter DRUGS
Don’t need physician prescription because mild symptoms should be able to diagnose easily
and select treatment. Mostly true but self-medication has serious consequences
OTC should be used when:
1. Symptoms are mild
2. Illness/ Symptoms don’t get worse (if they do – go to physician)
3. Self-medication should not exceed 2 weeks
4. If adverse effects occur – stop taking immediately
OTC Definition: any drug that can be purchased without a prescription. Some agents aren’t
considerd drugs by general public but they are drugs and can cause toxicities and drug
interactions.
Examples: internal analgesics, cough and cold medicines, vitamins, laxatives, antacids,
antihistamines, topical creams, ointments, sleeping aids, sunscreens, anti-acne agents.
Government – Sale of OTC is controlled by Food and Drug Act – safety, efficacy, advertising
and sale is controlled
INTERNAL ANALGESICS
1. Acetylsalicyclic Acid (ASA) - reduce pain (analgesic), reduce fever (antipyretic), and antiinflammatory inhibits synthesis of prostaglandins – enhance mediation of pain, fever, and
role in inflammation
- Gastric irritation in 2% of population
- Tinnitus can occur
- Acetaminophen is drug of choice for children with fever (ASA can cause Reyes
syndrome)
- ASA poisoning in children and adults is common – keep out of reach
- Buffered ASA is no better than ASA alone
- Effervesceent analgesics – Alka Seltzer – contain ASA and sodium and should be
used infrequently.
- ASA is also used to prevent stroke and myocardial infarctions
2. Acetominophen - NOT anti-infllammatory. Mechanism: inihibits prostaglandin
synthetase so prostaglandins don’t form.
- At therapeutic doses it’s well tolerated, but overdose can lead to fatal liver injury
(20 tablets or more)
- Liver injury can occur if taken for prolonged period of time
3. Ibuprofen
- non-steroidal anti-inflammatory agent – analgesic, antipyretic
- more effective than ASA for dental pain and menstrual pain
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
- one the most efficacious - reversible inhibition of synthesis of prostaglandins
- Gastric irritation, skin rash, dizziness, blurred vision, fluid retention
**Special care for elderly and alllll analgesics
4. Naproxen
- May be the most effectie OTC anti-inflammatory agent
All four above drugs inhibit COX I or II - reducing amount of prostaglandins available to
sensitize nerve endings to mediators of pain
5. Combination Products – ASA, acetaminophen, and ibuprofin use din combo with other
ingredients
- ASA with codeine and caffeine try to have analgesics acting on different
mechanisms
- ASA and acetominophen act on peripheral system while codeiene acts on CNS
6. Topical Analgesic
- not as good as internal
- e.g. absorbine jr. Deept heat rub, Ben Gay, Capsicum
- Contain, camphor, menthol, methylsalicylate, capsicum, and turpentine oils
- Local warmth may be an analgesic (but a heating pad will do fine)
- do not use on broken skin
7. Generic vs. Name Brand
- Generic is just as good now.
DRUGS FOR COMMON COLD
- NO CURE: some include: decongestants, antitussives, antihistamines, expectorants and
analgesics
- Cold preparations have been called “SHOTGUN” preparations
- Cold preparations are not recommended for children under 6 – death
1. Antihistamines:
- Drugs that block histimine receptor prevent vasodilation and inflammation – this can
alleviate cold symptoms
- May aid in reduction of nasal and salivary secretions
- Limited role in alleviating symptoms of a cold
2. Decongestants – nose drops
- alpha-adrenergic receptor stimulans (agonists) causing
vasoconstriction and reduction in congestion
- Phenylephrine and pseudoephedrine sympathomimetic alpha
receptors are agents most commonly used.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
- Phenylpropanolamine was withdrawn from market because it
caused strokes in yong women
Can also alter blood pressure and redistribute blood flow – problem
for hypertensive subjects
**BEST APPLIED LOCALLY – nose drops
Shuld not exceed 7 days and long-term use should be avoided
Rebound congestion: is a problem
Can have local irritation and chronic rhinitis
3. Cough Suppressants
- Cough is due to bronchial and/or throat irritation signals to medulla
- Centrally acting suppressants block the processing of the information in the meduall
and reduce the frequency of cough
- Codeine and Dextromethorphan HBr are widely used
- Codeine -30 mg can suppress cough center most OTC contain 8mg which is
ineffective (because it’s a narcotic opiate cant have too much)
- Dextromethorphan HBr- 30 mg is effective but most are 7.5
- ^^ preferred over codeine because not dependence causing
- Should we suppress coughs? Depends if it’s productive or not.
- Non-productive = dry cough
- Productive cough = clearing airways
- Menthol, camphor can be rubbed as vaporizors onto throat but efficacy is
questionable (likely placebo)
4. Expectorants
- Stimulate secretions in bronchial tree and loosen phlegm in airway
- OTC preparations are way too low a dose
5. Analgesics
- reduce fever and achy feelings
6. Cold Therapy
- Rest
- Fluids
- Analgesics and antipyretics (acetaminophen)
Antiussives
- Intended to suppress cough – contain a large number of ingredients (alcohol, sugar,
codeiene, dextromethrophan)
- OTC usually don’t have enough active ingredients
- Best would be ne with therapeutic dose of dextromethorphan HBr
Mouth Washes and Lozenges
-
Bad breath. Contain antiseptic (phenols, benzoic acid, cetylpryridinium chloride)
Contact time is way too short to kill the germs.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Good oral hygiene prevents bad breath and need for mouth wash
Lozenges – relieve pain of sore throat –contain local anesthetic and antiseptic
- Hard candy is just as effective b
Sleeping Preparations
- main ingredient is antihistamine which hs sedative properties
- little value in treating insomnia
- try nonpharmalogical first
Hay Fever
- Antibody mediated inflammatory disease of nasal mucous membranes
- runny nose and congestion
- Drug of choice: antihistmines
- First generation: cause sedation and drowsiness and dry mouth
- Second generation: do not and are preferred
- Dristan: antihistamine, decongestant and analgesics SHOULD NOT BE USED
- Long term use of sprays for hay fever may result in chronic rhinitis
Poison Ivy
- Poison Ivy, Poison Oak and Poison Sumac are responsible for allergic dermatitis resin
found in leaves cause inflammatory response
- Avoid but if contact wash area with tide detergent
- Calamine Lotion gives temporary relief for mild exposure
- 0.5% hydrocortisone ointment is effective and prevents inflamattion preferred
Insect Bite
- Calamine and 0.5%hydrocortisone cream
- Cold compress
- For people allergic to bees - epinephrine
Sunscreens
- UVB – sunburn and tanning UVA photosensitivity – pigment darkenting and sunburn
- 75% skin cancer from UV raditiaton
- Sunsceren is absorbed into stratum corneum and absorb/scatter UV energy and
prevent it from reaching the dermis
- Para-aminobenzoic acid derivaties, benzophenone, and cinamic acids
- Sun Protection Factor: minimum erythema dose (UV) of sunscreen-protected skin /
minimum erythema dose (UV) of unprotected skin
- Minimum erythema dose is time of expsore to UV that will cause a burn
- Choosing sunscreen
- 1. Skin type
- 2. Acitvity (e.g. higher elevation = more UV)
- 3. Site of application – lips and nose have thin stratum corneum
- 4. Condition of skin – dry (cream) oily – gel
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Antacid
Systemic: s
- Sodium bicarbonate is absorbed by GI tract and cause systemic alkalosis
- Rapidly neutralizes
- BUT causes systemic alkalosis, liberates CO2 causing gastric distention and may
perforate ulcers, if sodium is retained = hypertension
- Calcium carbonate is absorbed and can increase Ca load and is used as source of
calcium
NonSystemic: NOT absorbed and does not cause systemic alkalosis
- Aluminm hydroxide – very little absorbed
- Slow onset
- Coats mucosal lining of stomach and protects from acid
- Popular
- Cons: can decrease phostphate absorption leading to loss of bone calcium,
causees constipation
- Magnesium Hydroxide (Milk of Magnesium) – 5% absorbed
- Widely used antacid and cathartic
- Rapid onset
- Cathartic action, excreted quickly
- Magnesium Trisilicate
- Slow onset of action
- Large doses can raise gastric pH and cause diarrhea
- Can lead to toxic effects if absorbed
Antacid mixtures: to overcome constipating effect of aluminum hydroxide and the cathartic
action of magnesium combine
Antacid Therapy
- Goal is to hold pH contents at 4
Antacids are useful for epigastric distress or excess acid but should be limited in use
H2 Antagonists
- Famotidine and ranitidine are drugs that block H2 receptors in the stomach,
reducing the amount of acid secreted
- MORE effective than antacid in reducing acid and more convientent
- Only need to be taken once a day (Famotidine) where antacids re 3 x
- Free of major adverse effects
Cathartics and Laxatives
- Laxative Effect: Excretion of a soft formed stool – may have increased peristalsis or
increased hydration of the stool
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Cathartic Effect – more fluid evacuation – increased motor activity of GI tract
Stimulant Cathartics (contact cathartics)
- increase motor activity of intestine and cause intestinal cramps
- increase mucus secretion and increase secretion of water and electrolytes into lumen of
GI tract
- Castor Oil
- Phenolphthalein – site of action is colon NOT RECOMMENDED – 15% is absorbed
- Bisacodyl – acts on colon very effective – 5% is absorbed however can have excessive
cathartic action
- Anthroquinone Cathartics – cascara sagrada and senna but not recommended
Saline Cathartics
- Magnesium suflate (Epson salt)
- Mechanism of Action
- Salts are slowly/incompletely absorbed from digestive tract and retain water
by osmotic forces
- Intestinal transit is indirectly increased
- Enhance secretion of cholecystokinin (enhances intestinal mobility)
- Causes dehydration and magnesium ion may cause toxicity
Bulk-Forming Laxatives
- Polysaccharides – methylcellulose, dietary fiber and bran
- Mechanism of Action
- 1. Polysaccharides swell in water to become gelly – soften stool
- 2. Intestinal microflora metabolize the polysaccharides and this contributes to
osmotic effect in the gut
- May indirectly stimulate peristalsis
- Efffect is seen in 12-24 hours but full effect is 2-3 days
- THESE ARE THE PREFERRED LAXATIVES
Emollient Laxatives
- Soften stool without stimulation of peristalsis
- 1. Surface Active Agents (dioctyl sodium sulfosuccinate)
- Mechanism of Action: act by lowering surface tension and allowing water to
penetrate fecal matter
- Large doses cause nausea
- 2. Mineral Oil
- Mechanism of Action: softens stools by retarding absorption of water
- Toxicity: decreases absorption of fat soluble vitamins ( ADEK)
Uses of cathartics and laxatives:
1. constipation
2. In conjuction with anthelmintics to remove helminthes
3. Prior to radiological examination
4. Prior to bowel surgery
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
5. Soften stool in patients suffering from CV disease/hemorrouds
Dangers of Abuse – it’s readily available so a large number of people abuse
1. Spastic colitis can result from long term use
2. water and electroly disturbances
Antidiarrheal Agents
- major problem is dehydration
1. Absorbents – used for acute/mild diarrhea
- Kaolin and pectin – absorb water, toxins, and add bulk to GI track
- Loperamide – synthetic opioid that does not penetrate CNS but inhibits peristalstic
activity by acting on GI tract muscles and reduces cramps – should be carried by
travelers DRUG OF CHOICE
- DO NOT USE: antibiotics, atropine containing preparations
DRUG INTERACTIONS WITH OTC PREPARATIONS
1. Antihistamines are depressants and have additive CNS depression
2. Decongestants-sympathomimetics should not be used with monoamine oxidase
inhibitors- prevent metabolism of decongestant and hence increase its concentration in the
body
3. ASA given with oral anticoagulants may produce bleeding
4. Antacids will interfere with absorption of some drugs (tetracyclines) antacids will bind to
tetracycline preventing absorption
5. Mineral oil used as a laxative will retard the absorption of a number of drugs. Mineral oil is
not absorbed and any drug that is dissolved in the mineral oil will not be absorbed.
Selecting an OTC Product
Select the Product That:
1. Simplest formulation (single ingredient)
2. Therapeutically effective dose
3 Lists all ingredients and amounts
4. Good generic, if available
5. Be wary of gimmicks – fancy preparations have no added benefits
6. Appropriate dosage form (e.g. liquid for children) – must be palatable
What OTC drugs should be readily available
1. Ibuprofen as anti-inflammatory
2. Acetaminophen as an analgesic and antipyretic
3. 0.5% hydrocortisone cream
4. A second generation antihistamine
5. Famotidine or an antacid
6 Kaolin and pectin
7. Pseudoephedrine
8. Rubbing alcohol (cleanse wound)
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
9. Dextromethorphan HBr
10. Loperamide
E.3 Herbal Remedies
Increase in availability of HERBAL REMEDIES
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1. Desire of general public to be “natural” (think it’s safer)
2. Manufacturers promote this for financial gain
Before 1940s – much of medicine was natural products (opium, cascara, digitalis leaf)
Herbam medicine more popular in Europe – 40% of doctors prescribe plant-derived
pharmeceuticals/herbal medicine
2/3 of worlds population rely on herbal products. Total sales in Canada = 1-2 billion
Definitions
Allopathic Medicine: Drugs used by mainstream medicine – have a drug identification
number (DIN) and undergone safety and efficacy testing by Health Canada
Herbal medicine (homeopathic): plant products sold sa medicine (no DIN)
Allopathic phytopharaceuticals: They have a DIN – full status as a drug and meet
requirements – full safety and efficacy eval
Phytopharmeceuticals: drugs obtained frm plants, purified and used at therapeutic doses
ith scientific efficacy and documented toxicity (digitalis (digoxin) quinine, cocaine, atropine)
Food Supplement: herbal product used at one-quarted the proposed therapeutic dose
Why Move to Herbal?
1. Concern about side effects of allopathic medicine
2. Cost of allopathic medicine is high
3. Lack of faith in allopathic medicine in their effectiveness – think “what’s natural is best”
4. Hope that herbal/nature product will cure chronic/terminal disease
5. Belief that herbal is not toxic – while in reality some of the most toxic substances are
herbal/natural botulinum toxin
Value of Plants for Pharmaceuticals
- Source of direct therapeutic agents (digoxin – digitalis, or taxol)
- Source of raw material to manufacture more complex semisynthetic compounds
- Structure of plant substances can be used to model new compounds
Problems With Herbals?
1. Lack efficacy data
2. Lack safety data
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
3. Lack standardization - poor quality control
4. Undeclared ingredients
5. Intentional adulteration adding substances that aren’t herbal (e.g. adding
hydrocortisone)
6. The source is questionable foreign companies, no inspection at facilities
7. Confusing literature unsure what to believe
8. Toxicities – some can be lethal (herbal teas that can cause liver damage)
9. Drug interactions with allopathic medicine – people who take both. Important to tell
physician what other drugs (including herbal) that you’re on
Scale of Effectiveness
MILD ACTING
MEDIUM ACTING
POTENT
Hawthorn
Lilly of the Vally
Digitalis
Chamomile
Liquirice
Atropine
Valerian
Hypericim
Opium
Azulene
Salicin
Cortisone
CARDIOVASCULAR
ANTISPASMODIC
SEDATIVE
ANTIINFLAMMATORY
Valerian: Valeriana Officinalis
- Main use is sedative and hypnotic – drug of choiceb for herbalists in tretment of panic
attack. Depress CNS activity but less effective than allopathic benzodiazepines
but less adverse effects.
- No change in REM sleep but increase in slow wave sleep, no difference in
onset/duration of sleep and no difference in quality vs. placebo
- Other studies have shown small increases in quality of sleep
- Hepatotoxicity may be a significant problem
Feverfew
- Antipyretic, antispasmodic, emmemnogogue, carminative, and antithelmintic
- Treat migraines mostly. May be useful due to good study.
- Some batches contiain little active ingredient while others lots
- Toxicity in 20% mouth ulcerations and dermatitis
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Comfrey
- Used for wound healing – efficiacy is questionable.
- Cream or ointment base will have an effect – should NOT be used internally (used to
be)
- AVOID
Devil’s Claw
- extrat of harpogophytum procumbens treat inflammatory conditions (arthritis)
- Active ingredient is believed to be glucoiridoids plant steroid
- Lack biochemical effects expected of anti-inflammatory non-steroidal
(ibuprofen)
- Even doses 100 x the recommended for humans were ineffective in animals
- Likely become inactivated in acid of stomach
Echinacea
- one of most used herbal medicines treatment of common cold
- Echinacein is active ingredient. Mechanism of Action:
- 1. Stimulates cells involved in immune process (T-lymphocytes)
- May be a small benefit but nneed better studies
- Toxicity – rare, some may be allergic and those with autoimmune disease should not
take
Aloe
- topical aid in healing of wounds and burns
- Conflicting results from studies (probably due to variability in products)
- Some skin allergies occur; should NOT be injected
Ginseng
- Active Ingredient – ginsenasides or panaxosides
- Use to enhance endurance and stamina – also aphrodisiac, enhance learning,
memory, productivity etc.
- Adaptogen – restores normal balance (if BP is low, it raises it; if BP is high, it lowers
it) pharmacologits struggle with this claim….
- Tesets on small animals show slight increase in endurance but no trials on humans
- Adverse effects: headache, high BP, bleeding - may affect platlet aggregation and will
increase effect of anticoagulants. Raise insulin levels in plasma – don’t take if diabetic
- Often products are adulterated – caffeine, stimulants, etc.
St. John’s Wort
- Contains hypericin – used to traet mild to moderate depression and to heal wounds
- Modifies neuronal pathways in CNS – dopamine, serotonin, norepinephrine
- Similar process to antidepressants
- Hass been shown to have true antidepressant activity but less than antidepressants
- Government agencies in USA are doing large scale trials of St. John’s Wort in
depression.
- Also has been shown to increase rate of healing burns – stimulates growth of skin cells
- Adverse Effect: confusion, agitation, shivering, fever, sweating, diarrha, muscle
spasms, tremor; phototoxicity
- Addicitive – should not be taken with other antidepressants.
- Some products of ST. Johns wort contain ephedra – avoid.
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Solution to Herbal Product Use:
1. Regulate Standards
2. Determine efficacy of products in controlled trials
3. Need for Valid toxicity testing
E.4 Food Additives
Food Additives; substances added to food to improve appearance, texture and storage
- Broader definition: additives to improve nutritional value (vitamin/minerals
2 Classes of food additives
1. INTENTIONAL – vitamins/minerals, flavours, colours, preservatives, texture agents
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
2. UNINTENTIONAL – fertilizers, pesticides, heavy metals, rodent hairs,
microorganisms
- AKA Contaminents – amount present in food is regulated
Additives are convenience substances – not required. Criteria for safety is very stringent
because could expose whole population. Most additives could be eliminated – but this
would cause drastic change of our lifestyle
Efficacy – easily determined.
Toxicity – problems with determining risk/benefit ratio must be determined. Animal
studies must be used.. limitations:
1. Most food additives don’t have toxicity at low concentration – toxicity is
difficult to dtect at concentrations added to food, but humans may be exposed their
entire lifetime
2. Tested in animals – then have to extrapolate the results to humans (usually taking
1/100 or 1/100 of the highest no-effect dose - usually overestimate actual risk
which is good
3.What is the carcinogenic (cancer) and mutagenic potential? If a positive
response is observed it’s not allowed.
WHO Principles on Food Additives
1. Justified if they maintain quality/acceptability of food
- doesn’t address risk/benefit assessment
2. Additives should be used in only quantities suffiencent to obtain ends
3. Additives should be pure – additives often contain impurities and toxicity associated with
these impurities – toxciolocial evluation f impurities should be done
4. Toxicological evaluation of additives should happen
- Should additives used for 200 years be assessed? Is it at risk?
5. Special groups should be considered – those wh eat a large amount of one substance
E.g. 1970s – cobalt chloride added to beer to reduce foam – inhibited heart muscle
and caused death.
CLASS OF FOOD ADDITIVESU
Flavouring
- spices, flavouring agents, essence of smoke, synthetic flavours
- Pose large risk since there’s so many (5000) that have not been tested but are
approved
- Few demonstrate toxicity – excessive use may lead to it
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Monosodium glutamate (MSG) – tighten of muscles in face and neck, cause
headache, nausea and giddiness
Colours
- organic dye stuffs – most are well evaluated but unsure of carcinogenic potential
- used in small amounts – good because highest toxicity potential
- Can be derived from coal tar carcinogen? But maybe not.
- Colours are added to enhance appearance – acceptable appearance is necessary to eat
- Some people aer allergic – tartrazine – yellow food colour is most common (if you’re
allergic to aspirin, you’re allergic to this)
- Canada - 10 food colours, USA – 11, Denmark – 33. Red dye No. 2 is banned due to
cnacers in experimental animals at high doses (still used in USA)
Texture Agents
- Silicates – added to flower to keep them free flowing
- Emulsifying agents added to frozen foods
- Thickening Agent – added to milk shakes
- Relatively high concentrations in food – 1-3% of the product
Preservatives
- Preserve quality of food (one of more rational uses)
- Allows for delivery, ensure appropriate quality Usually benefits outweigh risks
- Antibacterials;
- Sodium Chloride – first preservative used; but high in sodium.. obvs
- Smoke – age old method for preserving meat. Also flavours. High incidence of
tumours in rats fed charbroiled steak (carcinogenic risk)
- Sodium benzoate – antibacterial and fungistatic – prevents spoilage usually
small amounts
- Parabens – derivative of sodium benzoate, anti-bacterial and fungistatic
- Propionic acid and salts – more active at lower pH – function as free acid.
Non-toxic
- Antibiotics – most effective but banned. Cause resistant strains of organisms
and sensitization of individuals to antibiotics.
- Sugar – early method. Syrups – very few survive. Toxicity is not a problem.
- Nitrites – controversy in adding sodium nitrite
1. Colour use (red in bacon and ham)
2. Inhibits growth of clostridium botulinum – preserves meats
without them becoming toxic
Adverse:b decerase BP, formation of methemoglobin (blood that can’t
carry oxygen) and nitrosamine formation (carcinogen)
- Sulphur Dioxide – prevent mold formation in wine. GOOD wine should not
have sulphur dioxide
- Antioxidants
- Prevent oxidation (thus rancidity) of foods
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Water-soluble – added to reduce oxidation of carbohydrates (browning of
fruit) ascorbic and citric acid – diarrhea can occur if excessive intake and
kidney stones
- Lipid Solubles – antioxidants prevent fats from becoming rancid – oxidizing
High level can cause fatty liver, impair growth and other biochemical
changes
Sequestrants
- Purpose is to bind metals (iron) that initiate the oxidation of fats (causing
rancidity)
- No known toxicity
-
-
Sweeteners
- Sugar, cyclamates, saccharin, and aspartame
- Saccharin – rats developed bladder tumours. Potential carcinogenic – restricted use
- Aspartame – has replaced saccharin and cyclamates - dipeptide and only toxicity is in
individuals with phenylketouria
- 200 times sweeter than sugar so used in smaller amounts
Conclusions
- part of our way of life – convenience substances that could be eliminated but would
change things.
- Must limit intake
E.1 Vitamins
Vitamin – substance essential for maintenance of normal metabolic functions but is not made
in the body so we must get it from an outside source
- discovered when studying deficiency diseases (scurvy – vitamin C, rickets – vitamin D,
Berberi – Bitamin B1 (thiamin), anemia – Vitamin B12, Pellagra – vitamin B3 (niacin)
Water Soluble – Vitamin C and B vitamins
Fat Soluble – ADEK
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
When vitamins are taken in chemically pure form they are considered DRUGS
DRI – Diatery recommended intakes intened to keep people healthy
EAR – Estimated Average Requirement (for 50% of the people)
RDA – recommended daily allowance (sufficient intake for 97-98%)
AI – Adequate Intake (no scientific data)
UL – Upper Limit (highest recommended intake)
Need For Vitamin Supplements
1. Inadequate Intake
Consume inadequate diet (poverty, geography)
Consume diet of one major food
Eccentric diet due to psychiatric disturbance
Particular ideas leading to idiosyncratic diet
Religious diets (that are inadequate)
Alcohol-dependent individuals who have inadequate food intake since large number of
claories is from alcohol
- Restricitve diets
- Retricted diets for disease management
2. Disturbances in Absorption
-
-
Prolonged diarrhea
Liver disease
Antibiotics for intestinal bacterial Vitamin K and Biotin (B vitamin) are derived from
intestinal bacterial
3. Incerased Tissue Requirement
1. In healthy individuals
- During growth
- During periods of hard physical work
- During pregnanc, lactation, menstruation
- Stress
2. In Illness
- Hyperthyroidism
- Fever
- Tissue wasting
Consequences of Excessive Vitamin Intake
1. Nutritional Approach
- One selects a diet aimed at supplying RDA for each vitamin or multivitamin
preparation whch supplies the RDA
2. Megavitamin Approach
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Based on delusion that if a small dose is good, a large dose is better
Can lead to toxic effects – millions ingest vitamins in excess of RDA
Water-soluble = readily excreted (“mst expensive urine in the world”)
Excess vitamin B6 can cuase nerve injuryb
ADE accumulation can cause severe toxic effects
VITAMIN C – ASCORBIC ACID
- RDA = 60 mg , and 100mg for smokers
- 200mg/day maintains maximum body pools (from fruits and veggies)
- Mechanism of Action: Vitamin C is reuiwred to hold cells together in organs
- Defet/Deficiency
- blood vessel cells not holding together and bleeding
- Gum cells become spongy and loosening of teeth (scurvy)
- Scurvy – british realized if they gave citrus fruit to the sailors, scurvy was cured
rationed lime juice = limies (nickname of british navy)
Therapeutic uses:
- Prevent scurvy
- Common cold? – Controversial
Adverse Effects:
- well above RDA = diarrhea and kidney stones
- benefits of megadose do NOT outwieigh risks
VITAMIN B
- 11 members
Folate
- 200 micrograms; 400 micrograms for childbearing aged women
- Impact on neural tube defects (spinabifida)
Vitamin B6 – high intake = decreased serum concentrations of homocysteine and low risk
of heart disease
Vitamin B12 – 10-30% of Americans over 60 years have difficulty aborbing b12 – need
supplement (absorption decreases with age)
VITAMIN A
- RDA = 1000 micrograms retinol or retinol equivalent
Deficiency
- Growth development will be retarded
- Vitamin A – is constituent of rhodopsin in the rods of the eye. Deficiency leads to
night blindness and drying of surface of eye
- Changes in lining of bronchioles – enhanced risk of respiratory infection
- Dry, thick and horny skin
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Toxicity
- results from excessive intake; dry itchy skin, vomting, headache, pressure in head, and
enlarged liver and spleen
Therapeutic Uses
- Serious nutritional deficiency disease in poor countries. Irriversable blindness
occurs in 250 000 children each year
- Increased requirements during infancy, pregnancy and lactation
- Used to treat acne and other skin diseases
VITAMIN D
RDA = 10 microgramsof cholecalciferol = 400 I.U. Vitamin D
Prevents RICKETS
Convertied in liver to active form
Milk in some countries is fortified with Vitamin D
Elderly people often require supplements
Actions of Vitamin D:
- Increases absorption of Calcium and phosphate form intestine (new bone formation
- Blood calcium leel must be maintained for health and vitamin D is involved in this
regulation
- Vitamin D is involved in removal of calcium from older bone
Deficiency
- Decreased absorption of calcium and phosphate
- Decreased blood calcium level
- Calcium is removed from bone to maintain blood level = bowleggedness = rickets
Excessive Intake
- When 50 000 units or more = toxicity
- Calcium depisits
- Excess removal of calcium from bone occurs (paradoxical!!!)
- Fatigue, nausea, vomiting, darrhea, impaired kidney functon
Vitamin D and osteoporosis
- All women over 55 recommended 1000 IU of vitamin D and 15000 elemental calcium
to prevent /slow osteoporosis
Vitamin D and Cancer – vitamin D may have protective effect against breast cancer in
premenopausal women. All women take 1000 IU (cancer society)
- not prostate cancer
VITAMIN E
RDA = 10 mg; stays in body for quite a long time (takes months to deplete)
Actions on Reproductive System
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Essential for normal reproduction in mammals. Termination occurs if vitamin E is
deficient in rats.
- Treatment for sterility in humans but NO BENEFITS
Actions on Muscular System
- Vitamin E deficiency was found to lead to muscular dystrophy – but not in humans – no
benefits for muscular dystrophy sufferers.
Treatment of Anemia – associaeted with anemia and useful for premature babies with
hemolytic anemia
-
Actions on Cardiovascular system
- Deficiency leads to dgeneration fo heart muscle in animal species. NO difference
between vitamin E and placebo therapy in humans.
- Lower incidence of coronary artery disease in those with vitamin E supplements, but
this is controverisla
- Dose dependent, but high doses can have harmful effects
- Usefulness is in question
Summary
1. effective in premature babies with hemolytic anemia
2. Controversial findings on benefit of high dietary vitamin E intake for cardiovascular disease
3. Ineffective in muscular dystrophy, habitual abortion, and sterility
4. Claims of effectiveness in minor skin ailments and schizophrenia have NOT been
substantiated
F.1 CANCER
1775 Percival Pott - describd cancer of scrotum in chimney sweeps relationship between
exposure to soot and chimney sweeps – called cancer “soot-wart”
1910 Clunet demonstrated x-rays to rats caused cancer
1915 – Yamagiwa and Ichikawa produced cancer of skin by applying prolonged coal tar to
rabbits ears
1930 Kennaway – highly carcinogenic polycyclic hydrocarbons from coal tar – found
hydrocarbon is an organic chemical made up of hydrogen and carbon and termed polycyclic
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
1895 – bladder cancer described by Rehm in dye workers, 2-Naphthylamine in dye
1938 Hueper showed that 2-Naphthylamine caused cancer in dog bladders
1961 epidemic in death of poultry by liver cancer traced to peanut meal used as feed.
Peanuts contained Aspergillus flavus which produced aflatoin – potent liver cancerinducing agent.
DEVELOPED VS. DEVELOPING COUNTRIES
Developing = liver cancer is most frequent (due to Hepatitis B infection and aflatoxin)
Developedb = colon-rectal cancer = high saturated fat and low fiber diet
CAUSES OF CANCER DEATHS
PERCENT
Tobacco = 30
Nutrition = 30
Sedentary Lifestyle = 5
Occupational Factors = 5
Chronic Infections = 5
Genetic factors = 5
Perinatal factors/growth = 5
Reproductive factors = 3
Alcohol Drinking = 3
SES = 3
Environmental Polution = 2
Solar and ionizing radiation = 2
Medicinal drugs/procedures = 1
Food Additives (salt) = 1
Tobacco Smoke = 30% of cancer deaths
- Lung cancer
- Upper respiratory tract cancer
- Esophagus cancer
- Bladder Cancer
- Pancreas cancer
Depends on the tar content of the cigarettes smoked, frequency of smoking and
duration of habit
- smokers are 8 x more likely to deelop cancer of the lung than non-smokers
- Latent period of 20 years between smoking and lung cancer
- Passive smoke will cause less lung cancer but still thousands die in the USA due to this
Diet – 30%
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Saturated animal fat and red meat are strongly linked to cancer of the colon and
rectum; as well as prostate
Salt- stomach and other cancers
Not eating fresh vegetables and fruit can lead to cancer
Infections
Viruses – DNA viruses cause cancer e.g. Hepatitis B and Hepatitis C cause liver cancer
(80% of liver cancer globally is caused by hepitits)
- HPV can cause cancer of the cervix
- Epstein-Barr virus – variety of cancers
- HIV - Kaposi’s sarcoma
Bacteria Helicobacter Pylori – stomach ulcer bacteria is associated with stomach cancer
Carcinogens in the Work Place
Arsenic – lung and skin cancer
Asbestos – lung
Benzene – leukemia
Diesel exhause – lung
Formaldehyde – nose
Man-made mineral fibers – lung
Hair dyes – bladder
Ionizing Radiation – bone marrow
Mineral Oils - skin (metal machinig)
Non-arsenical pesticides – lung
Painting Materials - lung
Polychlorinated biphenyls – liver skin (heat-transfer and hydraulic fluids/lubricants)
Randon – lung (mines, underground structures)
Soot – skin (chimney sweeps, cleaners, brick layers, firefighters, heating-unit service workers)
-
In the developed world control measures cut down cancers caued byoccupational
exposure, but in developing countries, it is a major hazard
HOW DO CHEMICAL CARCINOGENS INITIATE THE CANCER PROCESS
1. Carcinogens are inactive but undergo metabolic activation by enzymes in the body and
become highly chemically reactive forms = ultimate carcinogens
2. Ultimate Carcingens react irreversibly with a DNA molecule causing the change in the
chemistry of the gene.
3. The change is perpetuated in subsequent divisions of the cell a mutation is induced
4. Genes affected are oncogenes or tumor suppressor genes
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
5. Cancer occurs when a single cell accumulates a number of mutatinos and escapes
restraints on cell division
There are 3 categories of carcinogens
1. Initiatiors – described above; damage genes involved in cell division and facilitate the
proliferation/division of cells
2. Promotors – do not damage genes but selectively enhance growth of cancer cells or
precursor cancer cells
3. Progressors – allow rapid growth of tumours once they are established
TESTING CHEMICALS FOR CARCINOGENICITY
1958 Delaney Amendment to Food and Drug Act – prohibits the use in foodstuffs of any
substance that hs been shown to produce cancer in animal studies
The only official way to test for carcinogenicity is by animal studies – take years, expensive
New ways:
1. Ames Test – employ a mutant of Salmonella typhimrium and if carcinogens caused
mutations in this bacterial mutant deduced: if a chemical causes a mutation in the
bacterial sytem, there is a high likely hood that it’s a carcinogen (not officially recognized)
DRUGS USED TO TREAT CANCER
1. Surgery
2. Chemotherapy
3. Radiation
4. Biological therapies
5. Hormone Blocking and Hormone-supplementing
6. Bone Marrow Transplantation
CHEMOTHERAPY
Goals of Chemotherapy
1. CURE CANCER – only a few: childhood leukemia, Hodgkin’s disease, testicular
2. Prolong survival
3. Relief symptoms
4. Clinical research for future
Principles of Cancer Chemotherapy
- Benefit-Risk Assessment: mst weigh pros and cons. Re-evaluate prior to each
treatment. Are the goals being achieved? Are the adverse effets too severe?
- Mechanism of Action: Drugs in chemotherapy kill tumour cells by inhibiting protein
synthesis, DNA synthesis or cell division
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
Adverse Effects: rapidly dividing cells are also harmed (gastrointestinal, hair, bone
marrow)
Dosage and schedule: maximize anticancer effect while minimize toxicity
Combination chemotherapy: drugs are frequently used in combinaton. Cancer cells
are les likely to defend themselves when attacked by a variety of drugs. Plus can have
higher therapeutic effect without toxicity if combining drugs
Classification of drugs used in Cancer Chemotherapy
1. Alkylating Agents – Damages DNA – mechlorethamine aklylates DNA and q
nitrogen mustard
- 2. Antimetabolites – Disrupts cellular metabolism – methotrexate – folic acid
antagonist
- 3. Natural Products – E.g. vincristine isolated from Periwinkle Plant – arrests cell
division (ovarian cancer, breast cancer )
- 4. Antibiotics – damages DNA – doxorubicin
- 5. Hormones – - prednisone – suppresses cell division
- Tamoxifen – suppresses effect of female hormone estrogen
- 6. Biological - inhibit cell replication by blocking cytokines
- 7. Miscellaneous – procarbazine – damages DNA
D.1 Antibacterial, Antifungal, Antiviral, and Antimalarial Agents
Ehrlich – father of chemotherapy designed organoarsenicals – cured syphilis
Gerhard Domagk – Sulfonamide (Sulfa) used to treat bacterial diseases
Alexander Fleming – discovered penicillin – inhbited growth of Staphylococcus aureus
Selman Waksman – streptomycin treats tuberculosis
Antibiotic – chemical substance produced by microorganisms that suppress the growth of
other microorganisms and may eventually destroy them. Synthetic chemicals such as
sulfonamides are not antibiotics but antimicrobial compounds
Gram-Positive Bacteria – classified by colour after treatment of Gram’s stain – if they’ve
taken up colour they are gram-positive
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Gram-Negative Bacteria – if they do NOT take up colour after Gram’s stain they are gramnegative
Current Issues in Antibiotic Use
Resistant Strains: microorganisms mutate to have different properties and become resistant
- Due to over the counter inappropriate use (not in Canada)
- Antibiotics take advantage of differences between human and bacterial cells, now we
must find new differences
Classification of Antibiotics:
1. Narrow Spectrum – E.g. penicillin which acts primarily on gram-positive bacteria
Broad Spectrum – E.g. tetracyclines and chloramphenicol which act on BOTH grampositive and gram-negative bacteria
2. Bactericidal – antibiotics that destroy microorganisms
Bacteriostatic – antibiotics that prevent multiplication of microorganisms – factilitating
the ability of the body’s natural defence mechanisms to destroy the bacteria
PENICILLIN - narrow spectrum antibiotic
Mechanism of Action
1. Interior of bacteria is under high internal pressure – rigid cell walls which protect the
bacteria from this pressure
2. Penicilin is related to D-lanyl-Dalanine which is needed for new bacterial cell walls
3. Penicillin is taken in because of this resemblance and prevents new bacterial cell wall from
forming
4. resulting cells (protoplasts) are formed without cell walls and they are fragile and bursts
- Human cells don’t have cell walls so they aer unaffected selective toxicity
Classification of Penecillin
1. Penicillin G – extracted/purified from Penicillium mold – narrow spectrum – mainly
gram-positive bacteria – pneumococcus and streptococcus which cause: pneumoniae
meningitis, ear infection, also in treatment of syphilis
2. Penicilin V (semisynthetic)
- More acid stable than Peniciliin G less is destroyed by stomach acid s o higher blood levels
are achieved (this is used for oral administration)
3. Cloxacillin (semisynthetic)
-
Bacteria become resistant to penicillin G and others by producing penicillinase which
breaks it down
Cloxacillin is RESISTANT to penicillinase so it’s used against penicillinase-producing
staphylococcus aureus
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
4. Ampicillin and Amoxacillin (semisynthetic)
-
Broader Spectrum of antibacterial activity – active against several gram-negative
bacteria
Useful against Escherichia coli (E. Coli) - useful for infections such as UTI
5. Carbenicillin (semisynthetic)
-
Even BROADERb than ampicillin and amoxicillin – severe infections caused by
gram-negative bacterium, pseudomonas aeruginosa –
6. Aumentin
- Combinations of semisynthetic penicillins plus inhibitor of penicillinase
- Effective against penicillinase-producing straing of bacteria
Adverse Effects of Penicillins
- Most common is allergic reaction 1-10% of population
- Rare cases: fatal drop in blood pressure and difficulty breathing wear medic alert
tag if allergic to penicillin
Cephalosporins
- Antibiotic similar to penicilins but more resistant to penicilinase
- Selective inhibitors of bacterial cell wall synthesis
- 4 generations
First Generation – Cephalothin – good activity against gram-positive and moderate
against gram-negative
Second Generation – Cefamandole – increased agains gram-negative
Third Generation –Ceftriaxone (gonorrhea) less active than fist against gram-positive but
more active against gram-negative active against pseudomonas aeruginosa
Fourth Generation – Cefepine – increased stability to penicilinase and broader spectrum
than third
Vancomycin – antibiotic effective against staphylococci organism – inhibits cell wall
formation
Fluoroquinolones – synthetic antimicrobial ciprofloxacin – used for therapy of infections
by gram positive and negative bacteria can be taken orally
Erythromycin
- Antibiotic active against several bacterial infections of gram-positive
- Effective alternative if allergic to penicillin
- Can treat some gram-negative
- Selectively inhibits bacterial protein synthesis
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Azithromycin and Calrithromycin
- New. Chemically modified erythromycin
- Less frequent oral administration, less gastrointestinal problems, penetrate tissues
well
- Mor expensive
Tetracylcines
- Antibiotics with broad spectrum – exerts bacteriostatic effects by selectively
inhibiting bacterial protein synthesis – taken orally
- Bacteria are largely resistant now because use was so widespread. Less useful now
than they were before.
- Not used during pregnancy or before age 12
- Important to discard outdated supplies because they degredate into toxic products
Chloramphenicol
- Broad spectrum bacteriostatic antibiotic popular in 1950s until it was show to
cause fatal bone marrow failure
- Recommended for only serious infections caused by bacterial susceptible to it’s action
that can’t be treated with less dangerous drugs
Aminoglycosides
- Gentamicin – treatment for gram-negative bacterial infections. Can be toxic: kidney
damage, deafness, loss of balance, vertigo
- Streptomycin – aminoglycoside antibiotic gram-negative bacteria and first
effective drug against tuberculosis
- Toxic effects of genatmicin so safer drugs now used
Treating Tuberculosis
1. Test microorganism Myobacterium tuberculosis to see if it’s susceptible to first-line
antitubercular drugs.
- if it is: isoniazid plus rifampin daily for 6 months and pyrazinamideb for first
two months
2. If resistant – second-line drugsb
Co-Trimoxazole
- sulfamethoxazole and trimethoprim sulfonamide drug
- Traets bacterial disesases
- Use two similar compounds produces a constancy of blood concentrations of the two
agents
Mechanism of Action for Co-Trimoxazole
- similar for many
- Tetrahydrofolic acid is necessary for bacteria to prouce one-carbon units for DNA
synthesis
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
-
If tetrahydrofolic acid is not formed, growth will slow
-
1. Sulfamethoxazole competitively inhibits para-aminobenzoic incorporation into
dihydrofolic acid ( THIS IS SELECTIVE TOXICITY AT WORK)
ANTIFUNGAL DRUGS
Serious fungal inections are increasing, especially in those with AIDS – only a few highly
effective drugs are available
Amphotericin B
- Drug of choice for therapy of severe fungal infections
- 1. Binds to a steroid in outer membrane of susceptible fungi
- 2. This results in pore formation in the membrane and leakage across it
- Amphotericin B is poorly absorbed from gastrointestinal tract and must be intered
intravenously
- Adverse effects: kidney toxicity
Imidazoles (Or Azoles)
- Ketoconazole, fluconazole, itraconazole are effective when taken orally – greater
absorption for SYSTEMIC fungal infections
- Inhibit ergosterol (Steroid) synthesis which is needed for fungal cell membrane
formation
- Used for Yeast infections
ANTIVIRAL DRUGS
- HIV and AIDS
Amantidine – prevention of influenza due to influenza A virus 70-90% effective
Oseltamivir (Tamiflu)
- Neurominidase inhibitor the enzyme that allows the spread of the virus from cell to
cell
- Prevent neighbouring cells from being infected
- Resistance problem
Acyclovir
- Treat serious infections caused by herpes simplex virus
- Long term oral use decreases frequency of recurrance of genital herpes
- Useful in combating infections due to varicella-zoster virus (VSV) cause chicken pox
and shingles
Antiviral Agents for Treatment of HIV Infection
1987 Zidovudine (AZT) – nucleoside analoue which is a reverse transcriptase inhibitor
1996 – 5 new drugs for HIV
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
2 nucleoside: lamivudine and savudine
3 protease inhibitors: saquinavir, ritonavir and indinavir
Now new classes of drugs that inhibit entry of HIV virus into cells that inhibit the replication
of the virus
Optimal Therapy – multiple drug therapy (drug cocktail)
- New agents include entry inhibitors that block entry of virus into cells, and integrrase
inhibitors that block replication of the virus
Antibiotic Combinations
Disadvantages:
1. Unnescssary cost if one can be effective
2. INcreaesd chance of toxicity also won’t know what’s causing the toxicity
3. Enhances opportunity for resistant bacteria to arise and take over
4. Combination of antibiotics will decerase number of normal populations of different bacteria
and remove inhibitory influence on potentially dangerous bacteria --. Superinfection may
arise
Usefulness of Combinations
1. If you don’t know what microorganism is responsible and cannot wait
2. Treatment of mixed bacterial infection where no single antibiotic could eliminate all
different bacteria responsible
3. When treating tuberculosis prevents resistant bacteria
4. Two drugs may be effective where a single one may not E.G. inner lining of heart
infection – penicillin and aminoglycoside
GENERAL PRINCIPLES OF ANTIMICROBAL AGENTS
1 in 5 prescriptions are for antibiotics overprescribing
1. What are reasons for overprescribing by physicians
1. Greart deal of pressure by patients to prescribe
2. May be tmpted to prescribe broad-spectrum as a substitude for diagnostic
jdugement if it’s a virus, antibiotics will do NOTHING
3. Phamaceutical visits “educating” doctors on their drugs -influences
4. Remote areas – physicans wont hve laboratory help in determining the bacteria
2. Formulating a Specific Diagnosis – make the most intelligent guesss
3 Specimens taken and sent to Laboratories for Examination
- Take blood, urine, or saliva and have it sent for diagnostics
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Important to have these before antibiotics taken because presence of the antibiotics
will increase difficulty experienced by lab personnel in growing and identifying the
bacteria
4. Selection of Antibiotic Most likely to be Effective
- Heavy onus placed on physician must keep up to date with latest information on
newer antibiotics / changes in susceptibility of bacteria
-
5. Antimicrobial Susceptibility Tests
- Lab workers can help physicians select most effective antibiotic once microorganism is
identified
6. Prophylaxis (prevention) of infection with Antibiotics
- 30-50% of antibiotics are administrered to prevent infection
- In some situations this is highly effective – sometimes valueless
1. To prevent recurrent UTI caused by gram negative E. Coli – co-trimoxazole is used
2. To prevent wounds after surgeries
3. To prevent infections when dental procedures are carried out in patients with
valvular heart disease don’t want bacteria from mouth getting into blood stream
MALARIAU
200 million people are affected and 2 million deaths. Caused by four species of Plasmodium
genus
1. Plasmodium falciparum
2. Plasmodium vivax
3. Plasmodium ovale
4. Plasmodium Malariae
Life-Cycle of Malaria parasite Plasmodium
1. Infected anopheles mosquito bites an individual and injects malaria parasite into the
bloodstream
2. Sporozoites are carried by blood stream to liver and enter liver cells
3. In liver – become schizonts
4. Parasites emerge from the liver into the bloodstrem and enter red-blood cells, multiply and
rupture red blood cells repeat
Antimalarial Drugs
Chloroquine – prevention of malaria in areas where plasmodia are susceptible
- treats malaria due to all species except the chloroquine resistant plasmodium
falciparum
Mefloquine – DRUG OF CHOICE in areas where plasmodia are resistant to chloroquine
(Guyana, South America)
- Adverse Side Effects (rare) vertigo, seizures, psychosis
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)
lOMoARcPSD|8263507
Contraindications to use of mefloquine pregnancy (don’t get pregnant 3 mos
after) 2. Seizure disorder, depression or psychosis 3. Aactivities where vertigo
may become important
Quinine
- More toxic and less effective
- Value for therapy of severe illness due to chloroquine and multidrug-resistant strains of
plasmodium falciparum
- Oral or injection
- Adverse effects: tinnitus, headache, nausea, disturbed vision “cinchonism” --<
quinone comes from Cinchona bark
- Recommended you have a second drug for drug-resistant malaria
-
Doxycycline
- member of tetracycline group – contraindicated during pregnancy and in children less
that 12 years of age and breastfeeding women
Primaquine
- When infected with Plasmodium vivax or Plasmodium ovale
- Persistent liver phase occurs relapse happens
- After chloroquine therapy primaquine is agent of choice to prevent relapse
- Test for glucose-6phosphate dehydrogenase deficiency before prescribing because can
cause hemylosis (destruction of red blood cells) with enzyme deficiency
Inhibitors of Folate Synthesis
- Pyrimethamine is related to trimethoprime and is used to prevent malaria
Downloaded by Crystal O'Dea (13cnlo@queensu.ca)