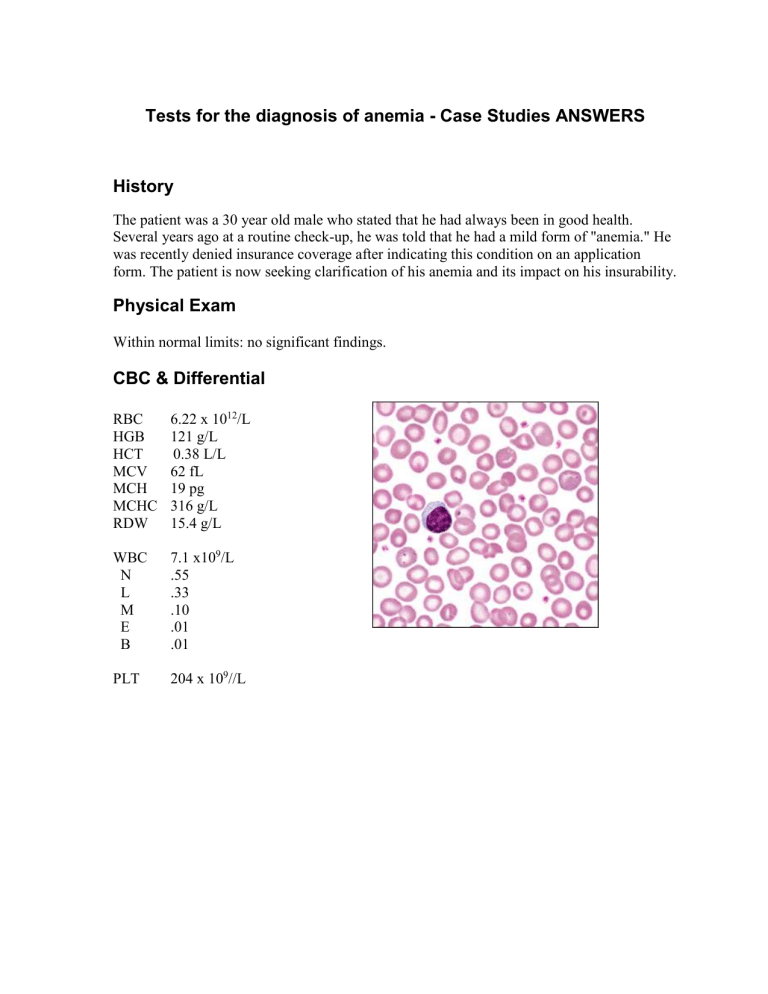
Tests for the diagnosis of anemia - Case Studies ANSWERS History The patient was a 30 year old male who stated that he had always been in good health. Several years ago at a routine check-up, he was told that he had a mild form of "anemia." He was recently denied insurance coverage after indicating this condition on an application form. The patient is now seeking clarification of his anemia and its impact on his insurability. Physical Exam Within normal limits: no significant findings. CBC & Differential RBC HGB HCT MCV MCH MCHC RDW 6.22 x 1012/L 121 g/L 0.38 L/L 62 fL 19 pg 316 g/L 15.4 g/L WBC N L M E B 7.1 x109/L .55 .33 .10 .01 .01 PLT 204 x 109//L Questions: 1. What further laboratory studies, if any, are indicated? Manual Blood Smear Hemoglobin electrophoresis 2. What are the expected results? Manual Blood Smear: Microcytic, normochromic Some targets (1+) Basophilic stippling present WBC morphology normal Platelet morphology normal Hemoglobin electrophoresis 3. Hemoglobin A 92.7% Hemoglobin A2 6.6% Hemoglobin F 0.7% What is the most likely diagnosis? Beta Thalassemia trait 4. What are the expected results? Tests for the diagnosis of anemia - Case Studies History A 23 year old male presented at the Emergency Room. Blood samples were drawn and transported to the acute care laboratory for stat analysis. No information on the patient’s condition or the reason for the ER admission was provided. CBC & Differential RBC HGB HCT MCV MCH MCHC 5.69 x 1012/L 155 g/L 0.45 L/L 80 fL 27 pg 344 g/L WBC N L M E B 12.4 x 109/L .70 .23 .07 .00 .00 PLT 184 x 109/L Questions: 1. What morphologic alterations are seen in this blood smear field? Normocytic, normochromic Many microspherocytes (3+) Many fragments (3+) Some targets (1+) WBC Morphology: reactive neutrophils with Dohle bodies present Platelet morphology normal 2. What is the most likely diagnosis? Acute hemolysis due to severe burns 3. What further laboratory studies, if any, are indicated? 4. What are the expected results? Sodium decreased Potassium normal Chloride normal Bicarbonate normal BUN normal Creatinine increased Serum was grossly hemolyzed. Urinalysis: Blood 3+ Protein 3+ The patient had been severely burned in a fire at his residence. He suffered 50% total burns with 35% third degree burns. He was immediately transferred to a specialized burn unit, but did not survive. Tests for the diagnosis of anemia - Case Studies History A 70 year old female patient visited her doctor complaining of shortness of breath on exertion, easy fatigability, and lassitude for past 2 to 3 months. The patient denied having bloody urine, gastrointestinal or vaginal bleeding. She claimed that her diet was good, but her appetite varied. Physical Exam: Other than pallor, no significant physical findings were noted. Occult blood was negative. CBC & Differential RBC HGB HCT MCV MCH MCHC RDW 3.71 x 1012/L 59 g/L 0.21 L/L 56 fL 16 pg 283 g/L 20.2 g/L WBC N L M E B 5.9 x 109/L .82 .13 .01 .04 .00 PLT 383 x 109/L Questions: 1. What morphologic alterations are seen in this blood smear field? Results of the blood smear exam were: Microcytic (marked – 3+), hypochromic (moderate – 2+) Moderate anisocytosis – 2+ Some pencil cells and targets – 2+ Occasional tear drops and fragments 2. What is the most likely diagnosis? Iron deficiency Anemia 3. 4. What further laboratory studies, if any, are indicated? What are the expected results? Serum ferritin decreased Serum iron decreased TIBC increased %Saturation (transferrin) decreased Tests for the diagnosis of anemia - Case Studies History The patient is a 34 year old male seen in the emergency room for treatment of superficial skin wounds resulting from a shotgun accident. He claimed that this happened while goose hunting. The patient had had his gall bladder removed five years prior to admission. At that time, he was told that he had Gilbert’s syndrome. He stated that he had always had “low blood”, and that his father and parental grandfather both had “liver ailments”. Physical Exam: He was somewhat pale with yellowish skin (slight pallor and jaundice). He also had scattered small surface wounds – mostly over his face, scalp and upper extremities. His spleen was palpable 3 cm below the left costal margin. CBC & Differential RBC HGB HCT MCV MCH MCHC RDW 3.93 x 1012/L 113 g/L 0.33 L/L 84 fL 29 pg 344 g/L 18.7 g/L WBC 5.0 x 109/L N L M E B PLT .53 .31 .08 .06 .02 362 x 109/L Questions: 1. What morphologic alterations are seen in this blood smear field? Normocytic, normochromic Moderate anisocytosis - 2+ Increased polychromasia – 2+ Some spherocytes – 2+ Occasional burr cells – 1+ WBC morphology normal Platelet morphology normal 2. What is the most likely diagnosis? Hereditary Spherocytosis 3. What further laboratory studies, if any, are indicated? 4. What are the expected results? Reticulocyte count 14.3% Absolute reticulocyte count 562 X 109/L Osmotic Fragility : Initial hemolysis 0.65% NaCL Complete hemolyis 0.40% NaCL Control: Initial hemolysis 0.45% NaCL Complete hemolysis 0.30% NaCL Bilirubin: Direct bilirubin slightly increased Total bilirubin increased The patient was referred to a hematologist to evaluate the possibility of a splenectomy Tests for the diagnosis of anemia - Case Studies History A 33 year old female immigrated to the United States from Laos four years prior to admission. Her history was obtained through an interpreter. She’s had multiple transfusions and splenectomy two years prior to admission. She doesn’t understand why she had this surgery. She is complaining of flu-like symptoms and general malaise. She has a fever, heartburn and a nonproductive cough. CBC & Differential RBC HGB HCT MCV MCH MCHC RDW 4.15 x 1012/L 81 g/L 0.29 L/L 69 fL 20 pg 282 g/L 22.3 g/L PLT 540 x 109/L WBC (corrected) 8.0 x 109/L N .51 L .36 M .07 E .04 B .02 83 NRBC/100 WBC Questions: 1. What morphologic alterations are seen in this blood smear field? Results of the blood smear exam were: Microcytic (moderate), hypochromic (marked – 3+) Moderate anisocytosis – 2+ Increased polychromasia – 1+ Marked target cells – 3+ Occassional sphereocytes, fragments and Howell-Jolly bodies 2. What is the most likely diagnosis? Hemoglobinopathy or Thalassemia 3. What further laboratory studies, if any, are indicated? 4. What are the expected results? Hemoglobin electrophoresis Hemoglobin E 80% Hemoglobin F 5% Other hemoglobins* 15% *Identified as hemoglobin A2, hemoglobin Bart’s and a hemoglobin H mutant Serum ferritin markedly increased Serum iron normal TIBC decreased %Saturation Increased Confirmed diagnosis – Homozygous hemoglobin E disease and alpha thalassemia. The patient’s flulike symptoms subsided; they were presumed to be viral in origin. She was referred to the Hematology Clinic and placed on iron chelation therapy. After 18 months, her serum ferritin had fallen to just slightly above normal. Her hemoglobin remained in the 70-90 g/L range. Chelation was discontinued, with plans to monitor the ferritin level every six months and resume treatment when needed. Tests for the diagnosis of anemia - Case Studies History This patient has a lifelong history of a seizure disorder, and has been receiving treatment since the age of two. At a routine check up with his neurologist, he complained of fatigue and lightheadedness upon exertion over the past 2-3 months. He appeared pale, but otherwise his physical exam was within normal limits. A CBC was ordered and he was found to have decreased hemoglobin. He was referred to the Hematology Clinic for a consultation. CBC & Differential Peripheral Blood RBC HGB HCT MCV MCH MCHC RDW 1.26 x 1012/L 57 g/L 0.16 L/L 130 fL 45 pg 349 g/L 18.1 g/L WBC N L M E B 3.2 x 109/L .73 .21 .01 .04 .01 PLT 219 x 109/L Bone Marrow History: 37 year old male. Lifelong history of a seizure disorder, treated since age two. At a routine check with his neurologist, he complained of fatigue, exertional dyspnea, and lightheadedness over the past 2-3 months. He appeared pale, but otherwise his physical exam was within normal limits. He was found to have a decreased hemoglobin, and was referred to Hematology Clinic. Questions: 1. What morphologic alterations are seen in this blood smear field? Results of the blood smear exam were: Marked oval macrocytes – 3+, normochromic Marked anisocytosis – 3+ Occasional tear drop cells and fragments Many neutrophils show nuclear hypersegmentation Platelet morphology normal 2. What is the most likely diagnosis? Megaloblastic anemia due to folate deficiency 3. What further laboratory studies, if any, are indicated? 4. What are the expected results? Serum folate decreased RBC folate decreased Bone Marrow Biopsy: Aspirate: Erythroid hyperplasia with megaloblastic maturation. Large polychromatic and orthochromatic megaloblasts show nuclear karyorrhexis and other dyserythropoietic changes. Multiple Howell Jolly bodies are seen in both megaloblasts and oval macrocytes. Neutrophils show premature nuclear segmentation, with metamyelocytes and band forms. Biopsy: Appears hypercellular The patient was given large doses of folic acid, and within 6 days his reticulocyte count was 15.2%. One month later, his hemoglobin was 127 g/L, MCV was 92 fL, and his blood smear morphology was normal. The anticonvulsant drug he had been taking is known to interfere with folate metabolism. In addition, the patient had been trying to lose weight, and over the past few months his diet had consisted mainly of TV dinners, with little or no fresh vegetables or fruits. A nutritional consult was arranged, and he was instructed to add folic acid to his daily medications. Note: Patients with folic acid deficiency occasionally show decreased levels of vitamin B12. Because of the patient’s history and lack of typical neurologic symptoms, concurrent pernicious anemia was considered very unlikely. Tests for the diagnosis of anemia - Case Studies History A 8 month old baby boy was brought to emergency room by his mother. The baby was in good health until 24 hours prior to admission, when his parents noted fever, progressive lethargy, and dark red urine. His mother had experienced a normal pregnancy and an uncomplicated delivery. His diet had consisted mainly of breast milk and formula, with some fruits and vegetables added recently. His parents are both Egyptian, and there is no family history of anemia, jaundice, gallstones, or splenectomy. Physical Exam: The baby appeared pale, lethargic, and had jaundiced skin. He had moderate splenomegaly and hepatomegaly. His temperature was 102 F. CBC & Differential RBC HGB HCT MCV MCH MCHC 1.28 x10 12/L 45 g/L 0.11 L/L 89 fL 35 pg 394 g/L PLT 425 x 109/L WBC N seg N myelo L M E B 27.8 x 109/L .65 .01 .31 .03 .00 .00 2 NRBC/100 WBC Questions: 1. What morphologic alterations are seen in this blood smear field? Results of the blood smear exam were: Normocytic, normochromic Increased polychromasia – 2+ Marked irregulary shaped spherocytes – 3+ Some fragments – 2+ Few burr cells – 1+ Many of the spherocytes have a clear “veil” or “blister” of membrane on the edge of the cell. RBC fragments include helmet and “bite” cell forms. Relative neutrophils with toxic granulation Platelet morphology is normal 2. What is the most likely diagnosis? Glucose-6-phosphate dehydrogenase (G6PD) deficiency 3. What further laboratory studies, if any, are indicated? 4. What are the expected results? Serum was grossly hemolyzed. Bilirubin: Direct increased Total increased Haptoglobin decreased Urinalysis: Urine was grossly red. Blood 3+ Protein 3+ Biochemical Genetics: RBC enzymes G6PD levels Pyruvate kinase levels decreased normal The patient was admitted and transfused with packed RBC’s. On the following day, his hemoglobin was 107 g/L. His condition stabilized and his hematuria cleared. He recovered rapidly. Other laboratory parameters returned to normal levels and there was no further evidence of hemolysis. Note: G6PD is an enzyme that protects erythrocyte hemoglobin from oxidation and subsequent denaturation. Individuals with a deficiency of this enzyme are susceptible to hemolytic episodes following oxidant stress to their red cells. In the Mediterranean type of G6PD deficiency, acute hemolysis can be initiated by the ingestion of fava beans. Questioning of the parents disclosed that one of the vegetables that had been added to the infant’s diet on the day before admission – was fava beans. The patient was discharged, and the parents were provided with a list of foods, medications, and other substances that should be avoided by persons with G6PD deficiency.