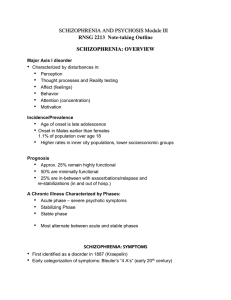
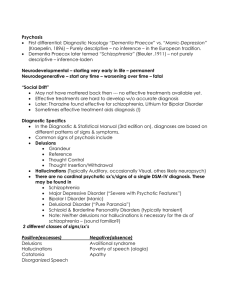
Schizophrenia Major disturbances in thought, emotion, and behavior Disordered thinking Ideas not logically related Faulty perception and attention Lack of emotional expressiveness Inappropriate or flat emotions Disturbances in movement or behavior Disheveled appearance Can disrupt interpersonal relationships, diminish capacity to work or live independently Significantly increased rates of suicide and death Lifetime prevalence ~1% Affects men slightly more often than women Onset typically late adolescence or early adulthood Men diagnosed at a slightly earlier age Diagnosed more frequently in African Americans May reflect diagnostic bias DSM-5 Criteria for Schizophrenia Two or more of the following symptoms for at least 1 month; one symptom should be either 1, 2, or 3: (1) delusions (2) hallucinations (3) disorganized speech (4) disorganized (catatonic) behavior (5) negative symptoms (diminished motivation or emotional expression) Functioning in work, relationships, or self-care has declined since onset Signs of disorder for at least 6 months; if during a prodromal or residual phase, negative symptoms or two or more of symptoms 1-4 in less severe form Clinical Description of Schizophrenia Three major clusters of symptoms: 1. Positive 2. Negative 3. Disorganized Positive Symptoms: Behavioral Excesses and Distortions Delusions Firmly held beliefs Contrary to reality Resistant to disconfirming evidence Types of delusions: Persecutory delusions “The CIA planted a listening device in my head” 65% have these Thought insertion Thought broadcasting Outside control Grandiose delusions Ideas of reference Hallucinations Sensory experiences in the absence of sensory stimulation Types of hallucinations: Auditory 74% have this symptom Visual Hearing voices Increased levels of activity in Broca’s area during hallucinations Negative Symptoms: Behavioral Deficits Avolition - lack of interest; apathy Asociality - inability to form close personal relationships Anhedonia - inability to experience pleasure Consummatory pleasure Anticipatory pleasure Blunted affect - exhibits little or no affect in face or voice Alogia - reduction in speech Can be grouped into 2 domains: 1. Experience domain Motivation Emotional experience Sociality 2. Expression domain • Outward expression of emotion • Vocalization Disorganized Symptoms Disorganized speech (formal thought disorder) Incoherence - inability to organize ideas Loose associations (derailment) - rambles, difficulty sticking to one topic Disorganized behavior Odd or peculiar behavior - silliness, agitation, unusual dress (e.g., wearing several heavy coats in hot weather) Movement Symptoms Catatonia Motor abnormalities Repetitive, complex gestures - usually of the fingers or hands Excitable, wild flailing of limbs Catatonic immobility Maintain unusual posture for long periods of time (e.g., stand on one leg) Waxy flexibility Limbs can be manipulated and posed by another Other Psychotic Disorders 1. Schizophreniform Disorder Same symptoms as schizophrenia Symptom duration greater than 1 month but less than 6 months Symptoms must include either hallucinations, delusions, or disorganized speech 2. Brief Psychotic Disorder Symptom duration of 1 day to 1 month Often triggered by extreme stress, such as bereavement Symptoms must include either hallucinations, delusions, or disorganized speech 3. Schizoaffective Disorder Symptoms of both schizophrenia and either a depressive or manic episode Symptoms of a major mood episode are present for a majority of the duration of illness 4. Delusional Disorder Delusions may include: Persecution; Jealousy; Being followed and; Erotomania (loved by a famous person); and Somatic delusions. No other symptoms of schizophrenia Etiology of Schizophrenia: Genetic Factors Genetically heterogeneous Not likely that disorder caused by single gene Family studies Relatives at increased risk Negative symptoms have stronger genetic component Twin studies 44% risk for MZ twins vs. 12% risk for DZ twins Children of non-schizophrenic MZ twin were more likely to develop schizophrenia (9.4% vs. 1% in general population) Adoption studies Increased likelihood of developing psychotic disorders Familial high-risk studies Differing negative vs. positive symptomatology Association studies Two genes associated with schizophrenia DTNGP1 (dystrobrevin-binding protein 1) NGR1 (growth factor neuregulin; risk factor for schizotypal traits) Two genes associated with cognitive deficits COMT (Catechol-O-Methyltransferase) BDNF (brain-derived neurotrophic factor) Genome-wide scans Identification of gene mutations Several identified but results need to be replicated Etiology of Schizophrenia: Neurotransmitters Dopamine Theory Disorder due to excess levels of dopamine Drugs that alleviate symptoms reduce dopamine activity Amphetamines, which increase dopamine levels, can induce a psychosis Theory revised Excess numbers of dopamine receptors or oversensitive dopamine receptors Localized mainly in the mesolimbic pathway Mesolimbic dopamine abnormalities mainly related to positive symptoms Underactive dopamine activity in the mesocortical pathway mainly related to negative symptoms Etiology of Schizophrenia: Evaluation of Dopamine Theory Dopamine theory doesn’t completely explain disorder Antipsychotics block dopamine rapidly but symptom relief takes several weeks To be effective, antipsychotics must reduce dopamine activity to below normal levels Other neurotransmitters involved: Serotonin GABA Glutamate Medication that targets glutamate shows promise Etiology of Schizophrenia: Brain Structure and Function Enlarged ventricles Implies loss of brain cells Correlate with Poor performance on cognitive tests Poor premorbid adjustment Poor response to treatment Etiology of Schizophrenia: Brain Structure and Function Prefrontal Cortex Many behaviors disrupted by schizophrenia (e.g., speech, decision making) are governed by prefrontal cortex Individuals with schizophrenia show impairments on neuropsychological tests of prefrontal cortex (e.g., memory) Individuals with schizophrenia show low metabolic rates in prefrontal cortex Failure to show frontal activity related to negative symptoms Disrupted communication among neurons due to loss of dendritic spines Disconnection Syndrome Structural and functional abnormalities in temporal cortex Temporal gyrus; Hippocampus; Amygdala; Anterior cingulate Reduced gray matter and volume evident - disrupted connectivity in the brain Environmental Factors Damage during gestation or birth Obstetrical complications rate high in patients with schizophrenia - Reduced supply of oxygen during delivery may result in loss of cortical matter Viral damage to fetal brain Presence of parasite, toxoplasma gondii, associated with 2.5x greater risk of developing schizophrenia In Finnish study, schizophrenia rates higher when mother had flu in second trimester of pregnancy Developmental factors Prefrontal cortex matures in adolescence or early adulthood Dopamine activity also peaks in adolescence Stress activates HPA system, which triggers cortisol secretion Cortisol increases dopamine activity Excessive pruning of synaptic connections Use of cannabis during adolescence associated with increased risk May explain why symptoms appear in late adolescence but brain damage occurs early in life Etiology of Schizophrenia: Psychological Stress Reaction to stress Individuals with schizophrenia and their first-degree relatives more reactive to stress Greater decreases in positive mood and increases in negative mood Socioeconomic status Highest rates of schizophrenia among urban poor Sociogenic hypothesis - stress of poverty causes disorder Social selection theory - downward drift in socioeconomic status Research supports social selection Etiology of Schizophrenia: Family Factors Schizophrenogenic mother Cold, domineering, conflict-inducing No support for this theory Communication deviance (CD) Hostility and poor communication Inconclusive at this time Etiology of Schizophrenia: Families and Relapse Family environment impacts relapse Expressed Emotion (EE) Hostility, critical comments, emotional overinvolvement Bidirectional association Unusual patient thoughts → increased critical comments Increased critical comments → unusual patient thoughts Etiology of Schizophrenia: Developmental Studies Use of retrospective or “follow-back” studies Developmental histories of children who later developed schizophrenia Lower IQ More often delinquent (boys) and withdrawn (girls) Coding of home movies Poorer motor skills More expression of negative emotion Treatment of Schizophrenia: Medications First-generation antipsychotic medications (neuroleptics; 1950s) Phenothiazines (Thorazine), butyrophenone (Haldol), thioxanthenes (Navane) Reduce agitation, violent behavior Block dopamine receptors Little effect on negative symptoms Extrapyramidal side effects Tardive dyskinesia Neuroleptic malignant syndrome Maintenance dosages to prevent relapse Second-generation antipsychotics Clozapine (Clozaril) - Impacts serotonin receptors Fewer motor side effects Less treatment noncompliance Reduces relapse Side effects Can impair immune symptom functioning Seizures, dizziness, fatigue, drooling, weight gain Newer medications may improve cognitive function: Olanzapine (Zyprexa) Risperidone (Risperdal) Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study Second-generation drugs were not more effective than the older, firstgeneration drug Second-generation drugs did not produce fewer unpleasant side effects Nearly three-quarters stopped taking the medications before study ended Second-generation antipsychotics have serious side effects Weight gain, diabetes, pancreatitis Psychological Treatments Patient Outcomes Research Team (PORT) treatment recommendation: Medication PLUS psychosocial intervention Social skills training Teach skills for managing interpersonal situations Completing a job application Reading bus schedules Make appointments Involves role-playing and other practice exercises, both in group and in vivo Family therapy to reduce expressed emotion Educate family about causes, symptoms, and signs of relapse Stress importance of medication Help family to avoid blaming patient Improve family communication and problem- solving Encourage expanded support networks Instill hope Cognitive behavioral therapy Recognize and challenge delusional beliefs Recognize and challenge expectations associated with negative symptoms e.g., “Nothing will make me feel better so why bother?” Cognitive remediation training or cognitive enhancement therapy (CET) Improve attention, memory, problem solving and other cognitive-based symptoms Case management Multidisciplinary team to provide comprehensive services Residential treatment Vocational rehabilitation