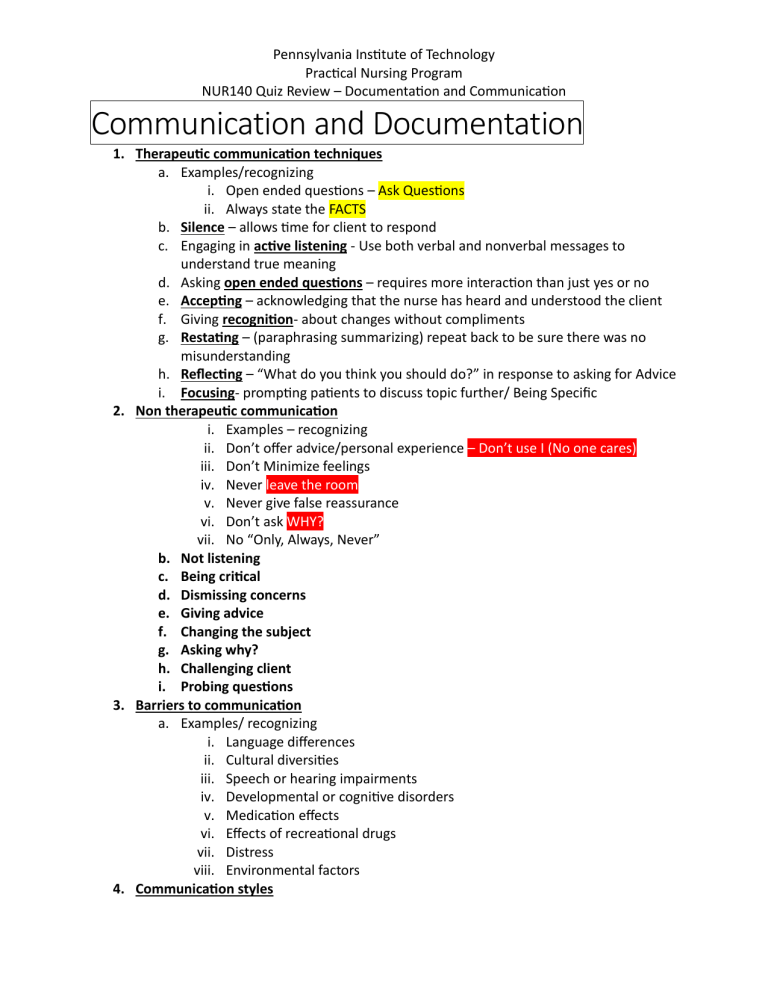
Pennsylvania Institute of Technology Practical Nursing Program NUR140 Quiz Review – Documentation and Communication Communication and Documentation 1. Therapeutic communication techniques a. Examples/recognizing i. Open ended questions – Ask Questions ii. Always state the FACTS b. Silence – allows time for client to respond c. Engaging in active listening - Use both verbal and nonverbal messages to understand true meaning d. Asking open ended questions – requires more interaction than just yes or no e. Accepting – acknowledging that the nurse has heard and understood the client f. Giving recognition- about changes without compliments g. Restating – (paraphrasing summarizing) repeat back to be sure there was no misunderstanding h. Reflecting – “What do you think you should do?” in response to asking for Advice i. Focusing- prompting patients to discuss topic further/ Being Specific 2. Non therapeutic communication i. Examples – recognizing ii. Don’t offer advice/personal experience – Don’t use I (No one cares) iii. Don’t Minimize feelings iv. Never leave the room v. Never give false reassurance vi. Don’t ask WHY? vii. No “Only, Always, Never” b. Not listening c. Being critical d. Dismissing concerns e. Giving advice f. Changing the subject g. Asking why? h. Challenging client i. Probing questions 3. Barriers to communication a. Examples/ recognizing i. Language differences ii. Cultural diversities iii. Speech or hearing impairments iv. Developmental or cognitive disorders v. Medication effects vi. Effects of recreational drugs vii. Distress viii. Environmental factors 4. Communication styles a. b. c. d. Pennsylvania Institute of Technology Practical Nursing Program NUR140 Quiz Review – Documentation and Communication Passive: want to avoid conflict, so individual says nothing or simply agrees. Assertive: honest and clear communication that does not violate the rights of others. Aggressive: communication that is verbally, and sometimes physically, abusive. Passive Aggressive: communication that appears passive on the surface, but often, the individual is demonstrating anger in a subtle, indirect, or secretive way. 5. Nurses role when there are Language differences a. Use a medical interpreter, instead of family members b. Develop cultural competence show respect and compassion c. Do not interrupt d. Be aware of body language e. Provide simple honest messages 6. Nurse’s role in maintaining confidentiality of client’s private information a. What is the nurse’s responsibility/ actions i. Protect privacy of consumer ii. Right to confidentiality iii. Do not share information to anyone not directly involved in care iv. Nurses must follow regulations 7. Focus notes – components a. Centers on specific health care problems and changes in condition, client events, and concerns b. Components (D.A.R) i. Data: Objective/Subjective Date Collected ii. Action: Action taken by nurse/ Intervention iii. Response: How the patient responded to action 8. SOAP notes – components a. Subjective, objective, assessment, and plan charting i. S: Subjective Data: What is said ii. O: Objective Data: What is observed/seen iii. A: Assessment: An analysis of the data that was collected iv. P: Plan: This section details interventions the nurse plans to implement. b. A characteristic of a problem-oriented medical record. 9. Recognizing a note that is factual, accurate, complete and timely (FACT) – not opinion, not personal a. FACT stands for i. Factual: Documentation should contain concrete, objective, and descriptive information. This objective description is obtained from direct observation and measurement. This is what the nurse sees, hears, smells, and feels Pennsylvania Institute of Technology Practical Nursing Program NUR140 Quiz Review – Documentation and Communication ii. Accurate: Documentation should establish accuracy by including exact descriptions and measurements. This provides concrete data for comparing a client’s condition over time. iii. Complete: Documentation must be complete; it must contain the what, when, where, why, and how. All information provided must be nonbiased. iv. Timely: All documentation should be put in chronological order. This gives a clear understanding of what has happened. Refrain from charting on clients until the end of the shift. 10. What information may be included in a medical record. a. Contains data about client b. Hospitalization and procedures c. Demographics d. Vital signs e. Medical history f. Medications g. Allergies h. Immunizations 11. Nurse’s role in receiving a verbal or telephone order a. Factors When Receiving Telephone Prescriptions i. Confirm the client’s information (identity; allergies; and age and weight when needed). ii. Make sure all prescriptions are complete (medication, dose, strength, route, time/frequency, indication, and special instructions). iii. Record the prescription on the designated area of the client’s chart. iv. Read the prescription back to the provider. v. Use clarifying techniques (spelling medications, reading numerals sequentially, distinguishing letters and terms that sound alike). vi. Ask additional questions as needed to ensure completeness and accuracy of the prescription.




