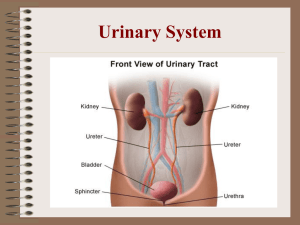
Excretion In Humans blood kidney urine renal The main excretory system in humans is the urinary system. The skin also acts as an organ of excretion by removing water and small amounts of urea and salts (as sweat). The urinary system includes a pair of bean-shaped kidneys located in the back of the abdominal cavity. Each day, the kidneys filter about 162 at (180 L) of blood, enough to fill a bathtub. They remove urea, toxins, medications, and excess ions and form urine. The kidneys also balance water and salts as well as acids and bases. At the same time, they return needed substances to the blood. Of the total liquid processed, about 1.3 qt (1.5 L) leaves the body as urine. The size of an adult kidney is approximately 4 in (10 cm) long and 2 in (5 cm) wide. Urine leaves the kidneys in tubes at the hilus, a notch that occurs at the center of the concave edge. Blood vessels, lymph vessels, and nerves enter and leave the kidneys at the hilus. If we cut into a kidney, we see that the hilus leads into a space known as the renal sinus. We also observe two distinct kidney layers. There is the renal cortex, an outer reddish layer, and the renal medulla, a reddish brown layer. Within the kidneys, nephrons clear the blood of wastes, create urine, and deliver urine to a tube called a ureter, which carries the urine to the bladder. The urinary bladder is a hollow muscular structure that is collapsed when empty and pear-shaped and distended when full. The urinary bladder then empties urine into the urethra, a duct leading to outside the body. A sphincter muscle controls the flow of urine between the urinary bladder and the urethra. Each kidney contains over one million nephrons, each of which consists of a tuft of capillaries surrounded by a capsule on top of a curving tube. The tuft of capillaries is called a glomerulus. Its capsule is cup-shaped and is known as Bowman's capsule. The glomerulus and Bowman's capsule form the top of a tube, the renal tubule. Blood vessels surround the renal tubule, and urine forms in it. The renal tubules of many nephrons join in collecting tubules, which in turn merge into larger tubes and empty their urine into the ureters in the renal sinus. The ureters exit the kidney at the hilus. The job of clearing the blood of wastes in the nephrons occurs in three stages. They are filtration, reabsorption, and tubular secretion: 1. The first stage in clearing the blood is filtration, the passage of a liquid through a filter to remove impurities. Filtration occurs in the glomeruli. Blood pressure forces plasma, the liquid portion of the blood, through the capillary walls in the glomerulus. The plasma contains water, glucose, amino acids, and urea. Blood cells and proteins are too large to pass through the wall, so they stay in the blood. The fluid, now called filtrate, collects in the capsule and enters the renal tubule. 2.During reabsorption, needed substances in the filtrate travel back into the bloodstream. Reabsorption occurs in the renal tubules. There, glucose and other nutrients, water, and essential ions materials pass out of the renal tubules and enter the surrounding capillaries. Normally 100% of glucose is reabsorbed. (Glucose detected in the urine is a sign of diabetes mellitus, which is characterized by too much sugar in the blood due to a lack of insulin.) Reabsorption involves both diffusion and active transport, which uses energy in the form of ATP. The waste-containing fluid that remains after reabsorption is urine. 3.Tubular secretion is the passage of certain substances out of the capillaries directly into the renal tubules. Tubular secretion is another way of getting waste materials into the urine. For example, drugs such as penicillin and phenobarbital are secreted into the renal tubules from the capillaries. Urea and uric acid that may have been reabsorbed are secreted. Excess potassium ions are also secreted into the urine. Tubular secretions also maintain the pH of the blood. The volume of the urine varies according to need. Antidiuretic hormone (ADH), released by the posterior pituitary gland, controls the volume of urine. The amount of ADH in the bloodstream varies inversely with the volume of urine produced. If we perspire a lot or fail to drink enough water, special nerve cells in the hypothalamus, called osmoreceptors, detect the low water concentration in the blood. They then signal neurosecretory cells in the hypothalamus to produce ADH, which is transmitted to the posterior pituitary gland and released into the blood, where it travels to the renal tubules. With ADH present, the kidney tubules reabsorb more water from the urine and return it to the blood, and the volume of urine is reduced. If we take in too much water, on the other hand, the osmoreceptors detect the overhydration and inhibit the production of ADH. Reabsorption of water is reduced, and the volume of urine is increased. Alcohol inhibits ADH production and therefore increases the output of urine. The liver also plays an important role in excretion. This organ removes the ammonia and converts it into the less toxic urea. The liver also chemically changes and filters out certain drugs such as penicillin and erythromycin. These substances are then picked up by the blood and transported to the kidneys, where they are put into the execretory system. The urinary system must function properly to ensure good health. During a physical examination, the physician frequently performs a urinalysis. Urine testing can reveal diseases such as diabetes mellitus, urinary tract infections, kidney stones, and renal disease. Urography, taking x rays of the urinary system, also helps diagnose urinary problems. In this procedure, an opaque dye is introduced into the urinary structures so that they show up in the x rays. Ultrasound scanning is another diagnostic tool. It uses high frequency sound waves to produce an image of the kidneys. Biopsies, samples of kidney tissue obtained in a hollow needle, are also useful in diagnosing kidney disease. Disorders of the urinary tract include urinary tract infections (UTI). An example is cystitis, a disease in which bacteria infect the urinary bladder, causing inflammation. Most UTIs are treated with antibiotics. Sometimes kidney stones, solid salt crystals, form in the urinary tract. Kidney stones can obstruct the urinary passages and cause severe pain, and bleeding. If they do not pass out of the body naturally, the physician may use shock wave treatment. In this treatment, a shock wave focused on the stone from outside the body disintegrates it. Physicians also use surgery to remove kidney stones. Renal failure is a condition in which the kidneys lose the ability to function. Nitrogenous wastes build up in the blood, the pH drops, and urine production slows down. If left unchecked, this condition can result in death. In chronic renal failure, the urinary system declines, causing permanent loss of kidney function. Hemodialysis and kidney transplant are two methods of helping chronic renal failure. In hemodialysis, an artificial kidney device cleans the blood of wastes and adjusts the composition of ions. During the procedure, blood is taken out of the radial artery in the patient's arm. It then passes through dialysis tubing, which is selectively permeable. The tubing is immersed in a solution. As the blood passes through the tubing, wastes pass out of the tubing and into the surrounding solution. The cleansed blood returns to the body. Kidney transplants also help chronic kidney failure. In this procedure, a surgeon replaces a diseased kidney with a closely matched donor kidney. Although about 23,000 people in the United States wait for donor kidneys each year, fewer than 8,000 receive kidney transplants. Current research aims to develop new drugs to help kidney failure better dialysis membranes for the artificial kidney.