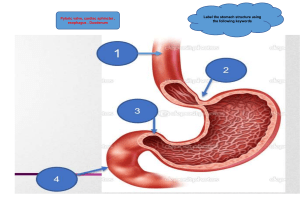
Dr / Hanaa Mabrouk Ahmed Identify the definition of common diseases of the gastro-intestinal tract. List predisposing factors, manifestations and treatment of gastro-intestinal disorders. Differentiate between clinical signs & symptoms for common diseases of the gastro-intestinal tract . Evaluate different child condition in diseases of the gastro-intestinal tract Analyze any complication, and implement proper intervention. Distinguish between different diseases of the gastro-intestinal tract. Appreciate parent roles in management of gastrointestinal diseases Carry out nursing care plan for different diseases of the gastro-intestinal tract Be responsible about the management of gastrointestinal diseases with cooperation of medical team. Design nursing care plans and case studies for different diagnosis Participate in giving and counseling about emergency care Reassure caregivers about condition of their children 1-Lecture 2-Group-Discussion 3-Class participation 4-Brain storming 5-Audiovisual with computer assisted 6-Case Study 1-Introduction 2-Causes 3- Functions of the Gastrointestinal System 4-The most common anomalies a- Congenital Hypertrophic Pyloric Stenosis b- Hirschsprung’s (congenital aganglionicmegacolon). c- Intussusception. 5- Follow up activities 6- References Birth defects are also called "congenital anomalies" or "congenital abnormalities." The word "congenital" means "present at birth." The words "anomalies" and "abnormalities" mean that there is a problem present in an infant. Unknown Inheritance Chromosome Abnormalities: A congenital metabolic disease Teratogens: A teratogen is an agent, that can cause a birth defect. It is usually something in the environment that the mother is exposed to during her pregnancy. It could be a prescribed medication, a street drug, alcohol use or a disease that the mother has, which can increase the chance for the baby to be born with a birth defect. Hypertrophic Pyloric stenosis (HPS) Hirschsprung's disease Intussusception Pyloric stenosis is an unusually narrow opening (stenosis) between your child’s stomach and small intestine (pylorus). Normally, food moves easily from the stomach into the small intestine through the pylorus. If the muscles of the pylorus are thicker than normal (hypertrophy), this makes the opening narrow and prevents food from passing easily out of the stomach. Pyloric stenosis can cause almost complete blockage of this opening. Pyloric stenosis usually develops in the first few weeks after birth. The most common sign is very forceful (projectile) vomiting soon after a feeding. It is a congenital hypertrophy of circular muscle layer of pyloric canal leading to stenosis of its lumen. The symptoms of this condition usually start at the age of 2-6 weeks of life resulting in partial or complete obstruction of the stomach outlet. The exact cause is unknown. Incidence 2: 1000 live births Male: female 4:1 (particularly first-born males). Risk The risk of pyloric stenosis may be greater if: Age: is between 3–6 weeks old. Gender: is male. There is a family history of pyloric stenosis. The mother uses tobacco during pregnancy. The circular muscle of the Pylorus as a result of the hypertrophy produces severe narrowing of the pyloric canal between the stomach and the duodenum. -Hypertrophy of circular muscle layer of pyloric canal. -Narrowing of pyloric canal. Elongated pyloric canal. Dilated stomach. Multiple superficial gastric ulcerations. The symptoms of pyloric stenosis are most frequently observed between the age of 3 and 6 weeks, but may well appear earlier. Vomiting Is Often Described As Non-Bile Stained ("Non Bilious") And "Projectile Vomiting", Poor Feeding Weight Loss Dehydration Constant Hunger, Belching, and colic Visible gastric peristalsis in the upper left abdominal quadrant from left to right (from the left subcostal margin to the umbilicus). Palpable pyloric mass (Olive like mass felt just beneath the outer border of the right rectus muscle at the level of the umbilicus). Initial treatment Rehydrate and correct electrolytes Correct alkalosis Surgical pyloromyotomy (Ramstedt procedure) Preoperative Care Nothing per mouth, and naso-gastric intubation for suction and repeated washing using warm saline Intravenous fluid therapy to correct dehydration and electrolyte disturbances. Intravenous broad-spectrum antibiotics and vitamin K. Operation: Pyloromyotomy operation) (Ramestedt’s Measuring vital signs Observe for postoperative complication Monitor parenteral fluids to maintain hydration Oral feeding resumed 2-8 hours after surgery (slowly) if the mother was breast feeding, she should resume this as soon as possible. Report any vomiting Removal of the naso-gastric tube after 12 hours post-operatively. Very gradual oral feeding starting by 5 ml of dextrose 5%, if tolerated the amount is increased in the next feed. Gradual Shifting to ½ strength milk formula, if tolerated well full strength milk formula is given gradually also 36-48 hours, and then the baby can be discharged with his mother with breast feeding. Pyloric stenosis can lead to: Failure to grow and develop. Dehydration. Frequent vomiting can cause dehydration and a mineral (electrolyte) imbalance. Electrolytes help regulate many vital functions. Stomach irritation. Repeated vomiting can irritate your baby's stomach and may cause mild bleeding. Jaundice. Rarely, a substance secreted by the liver (bilirubin) can build up, causing a yellowish discoloration of the skin and eyes It is a rare condition in which nerve cells that control squeezing movements (contractions) are missing from part of the large intestine (colon). The colon absorbs fluids and holds stool so that it can be passed out of the body with contractions. In Hirschsprung disease, the colon has trouble moving stool out through the rectum. This leads to constipation. Hirschsprung disease (HD) is a congenital absence of the parasympathetic ganglion nerve cells from within the muscle wall of the intestinal tract usually at the distal end of the colon resulting in a functional obstruction. Hirschsprung's disease occur in 1 every 5000 live births The basic pathological finding in Hirschsprung's disease is the absence of ganglion cells from the distal part of the rectum and extending proximally for a varying distance. This a ganglionic segment is nonpropulsive and fails to relax resulting in functional intestinal obstruction. The proximal colon is grossly dilated due retained stool, its wall is hypertrophied, and its mucosa is edematous and inflamed (Entero- colitis). The cause of this condition is not known, but it may be related to changes (mutations) in genes. It may run in families or be passed from parent to child (inherited) through genes. In children who have the disease, it is present from birth (congenital). It happens when nerve cells in the colon stop growing while the colon is developing before birth. Hirschsprung's disease is usually diagnosed shortly after birth, but in some milder cases, symptoms don't develop until later in life. Symptoms in older children include the following: Constipation or gas, which may make your baby fussy Poor appetite Vomiting bile (a green liquid) after eating Diarrhea Chronic constipation Lack of weight gain or growth Swollen abdomen Ribbon-like, foul-smelling stools Anemia (which is a low number of red blood cells) Frequent colon infections Abdominal distension Thin abdominal wall (superficial veins are visible) Visible peristalsis Constipation Foul-smelling stools Failure to growth This condition is diagnosed based on: child's symptoms. A physical exam. An X-ray of: child's colon after dye has been put into the colon (barium enema). Removal of a colon tissue sample to be examined under a microscope (biopsy). Measuring pressure in the rectum by inserting a balloon and inflating it (anal manometry). Goals Manage acute bowel obstruction Correct volume deficits and restore electrolyte balance Decompress gastrointestinal tract Recognize and eradicate any coexisting infections (eg, enterocolitis) Initial surgical goal is to eliminate functional obstruction caused by aganglionic bowel Ultimate surgical goal is to reconstruct the intestine, connecting normally innervated bowel to the anal opening Surgery is required for definitive treatment Antibiotics are given for any cases of suspected enterocolitis IV fluids Total parenteral nutrition for nutrient and calorie support if necessary Gastrointestinal decompression intestinal obstruction is present if A. Preoperative care If the operation is scheduled (elective), a bath or shower is recommended the night before or the morning prior to surgery. The child will not eat anything for 6-8 hrs before surgery. Intravenous antibiotics will be given in the operating room. 1- Skin Care After the operation for Hirschsprung's disease, children who do not have a stoma will have a lot of diarrhea. It is important to protect the skin around the anus at all times to prevent irritation, using a cream called "butt balm." child's nurse will teach you how to mix and apply the cream. 2-Dressings If the child has an incision on the abdomen, there will be a gauze pad and clear plastic dressing in place. You should remove this dressing two days after the operation. There may be a small amount of blood on pieces of tape, called Steri-strips, under the dressing. This is normal. You can remove the Steri-strips one week after the operation. Child can bathe with the Steri-strips in place. 3-Medications Most children don't need prescription pain medication after they're discharged from the hospital. Acetaminophen (Tylenol) or ibuprofen (Motrin) is usually sufficient. Administer the medication according to the dosage directions on the label. If the child is still uncomfortable, call our office and we may prescribe something stronger. 4-Activities The child can return to his or her usual activities without any special restrictions, unless the pediatric surgeon tells you otherwise. School-age children can resume their school activities as soon as they feel well enough Diet: child may eat a normal diet after surgery. Activity: child should avoid strenuous activity and heavy lifting for the first week after laparoscopic surgery, 4-6 weeks after open surgery. Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe. . Medicines: Medicines for pain such as acetaminophen or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain. What to call the doctor for: Call doctor for worsening belly pain, fever, vomiting, diarrhea, problems with urination or if the wounds are red or draining fluid. Follow-up care: the child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing Definition Intussusception is the invagination or telescoping of a portion of the intestine into an adjacent, more distal section of the intestine. Etiology Not usually known May be due to increased mobility of intestine and hyper peristalsis possible contributing factors include: ◦ Meckel's diverticulum ◦ Malrotation of intestine ◦ Acute gastroenteritis ◦ Abdominal injury Incidence Intussusception usually occurs in 6 months – 2 years infants. Boys :girls is 2:1. Pathophysiology It occurs when a segment of small bowel "telescopes" on itself, thus causing swelling, obstruction, gangrene. and eventually intestinal Intussusception preventing the passage of food that is being digested through the intestine. The walls of the two "telescoped" sections of intestine press on each other, causing irritation and swelling. Eventually, the blood supply to that area is cut off, which can cause damage to the intestine. Clinical manifestation Early signs/symptoms: (1) intermittent episodes of sudden onset of severe abdominal pain that lasts only a few minutes. Infants may pull up their legs during episodes of pain; (2) vomiting; (3) abdominal mass in the right upper side of the abdomen; suzage shaped mass (4) lethargy due to dehydration. Later signs/symptoms: (1) bloody stools with a mucus-like texture that resemble currant jelly; (2) bilious (green) vomiting from intestinal obstruction; (3) fever, low blood pressure, and fast heart rate can be signs of bowel perforation Investigations Plain X-ray Ultra sound Barium enema Hydrostatic reduction of telescoped bowel with a barium enema during the 1st 48 hours after onset. Surgical reduction of Intussusception, resection if bowel is gangrenous. Baseline observations include heart rate, respiratory rate, temperature and pain score. Blood pressure, oxygen saturations and neurological observations if clinically indicated. Minimum of 1 hourly observations Any significant changes should be reported immediately to the medical team Ensure appropriate medication, monitoring, oxygen and emergency equipment is available for transfer and reduction procedure Fluid input/output is to be monitored and documented. Enema Gastric suction Antibiotics Symptomatic Fluids intravenously until bowel function returns; he or she may then be allowed to resume a normal diet. Follow-up care may be indicated if the intussusception occurred as a result of a specific condition (e.g., cancerous tumors). Perforation of bowel, with peritonitis Necrosis of bowel requiring bowel resection Shock and sepsis Re-intussusception after spontaneous or active reduction.