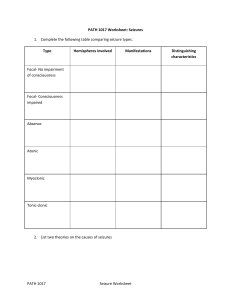
Anticonvulsants Epilepsy Seizure disorder o Abnormal electric discharges from cerebral neurons Characterized by two or more seizures o Loss of consciousness o Convulsive movements Unknown cause o Epileptic seizures often are symptoms of an underlying disorder o Secondary to trauma, anoxia (absence of oxygen), infection, stroke o Isolated seizures due to fever, electrolyte, or acid base balance International classification of seizures (See Table 19.1 in book) Generalized o Tonic clonic (grand mal) Most common Generalized alternating muscle spasms and jerkiness o Absence (petit mal) Brief loss of consciousness (10 seconds or less) Usually occurs in children Partial o Psychomotor Repetitive behavior Chewing or swallowing motions Behavioral changes Motor seizures Anticonvulsants/Antiepileptic Drugs (AEDS) Action – Suppress abnormal neuron firing – They DO NOT eliminate the cause Suppress sodium influx o Phenytoin (Dilantin), fosphenytoin, carbamazepine, oxcarbazepine, valproic acid, topiramate o Suppress calcium influx Valproic acid (Depakane) o Enhance action of GABA Barbiturates, benzodiazepines o Promote GABA release Gabapentin Choice of AED o Dependent on seizure type and characteristics o Highly individualized and dependent on many factors Patient medical history Type of seizure o Characteristics and length of seizure Results of electroencephalogram (EEG) Presence of comorbid conditions Dose of AED Treatment Begins at lowest effective dose Increased as necessary to prevent adverse drug effects. Serum drug levels may be obtained to determine drug efficacy Drug discontinuation or reductions must be extended over 6 to 12 weeks. Effective management may be obtained by a single AED However if seizure activity continues the initial drug is incrementally discontinued and replaced by a different class. Hydantoins: Phenytoin (Dilantin) Method of action o Reduces motor cortex activity by altering Na ion transport o Stabilizes against hyperexcitability that results from excessive stimulation or environmental changes o Prevent Tonic-clonic and Partial seizures and Status Epilepticus o Therapeutic serum level 10 – 20 mcg/mL Contraindications o Pregnancy (teratogenic) o Hypersensitivity o Heart block, bradycardia (Since drug alters Na ion transport) Caution o Hyponatremia, hypotension, hypoglycemia o Suicidal ideation, alcoholism o Myasthenia gravis, thyroid disease, diabetes mellitus o Renal and hepatic impairment Side effects o Headache o Confusion, dizziness, drowsiness, ataxia (impaired balance or coordination, tremor. o Insomnia, fatigue, diplopia, nystagmus o Rash, gingival hyperplasia, anorexia, nausea, vomiting o May cause harmless red/brown discoloration of urine Adverse Reactions o Leukopenia, hepatic impairment, depression, hyperglycemia (because of inhibition of insulin) o Bradycardia, peripheral neuropathy, purple glove syndrome o Life threatening Aplastic anemia, thrombocytopenia, agranulocytosis Steven johnson syndrome Hypotension, ventricular fibrillation, suicidal ideation. Drug interactions o Highly protein bound – compete with many drugs o o o Increased risk of bleeding: anticoagulants and aspirin Antacids/Calcium decrease absorption Antipsychotics and certain herbs can lower seizure threshold (Makes medication harder to dose) o Seizure Threshold – Level at which a seizure may be induced Nursing Process o Assessment Current meds/herbs/OTC Look for possible drug interactions Assess patients knowledge of therapy Hx of insomnia or anxiety? Check urinary output >1500 ml/day Renal and Liver function o Nursing diagnosis Risk of injurt r/t decreased coordination Impaired oral mucous membranes r/t gingival hyperplasia Imbalanced nutrition: less r/t decreased appetite Risk for falls r/t dizziness o Planning Patient will be free of seizures Patient will adhere to therapy Side effects will be minimal o Nursing Interventions Monitor serum drug level (10-20 mcg/mL) Ensure pt is received adequate nutrition due to appetite loss Safety Fall precautions Seizure Precautions (padding, suction, O2 Teaching Patients using oral contraceptives to use additional contraception. Discuss contemplating pregnancy with provider. Encourage patient to wear medical alert identification Warm patient of harmless pinkish red or brown urine Take drug at same time everyday Frequent oral and dental check ups Not to discontinue abruptly Report sore throat, bruising, nosebleeds Med should be taken with food Diabetic must monitor glucose levels Avoid certain herbs, alcohol, and other CNS depression Do not perform hazardous activities when initiating. o Evaluation Effectiveness of controlling seizures? Serum phenytoin levels maintained? Barbiturates Mechanism of Action o Decreases neuronal excitability by increasing fux of chloride ions into the neuron Indications o Partial seizures, Tonic-Clonic seizures o Acute episodes of Status Epilepticus Seizures Therapeutic serum range: 20 to 40 mcg/mL Risks o Sedation and patient tolerance to drug Discontinue gradually to avoid the recurrence of seizures. Succinimides: ethosuximide (Zarontin) Mechanism of Action o Decreasing calcium influx through T-type calcium channels o Depresses motor cortex o Increases CNS threshold to convulsive stimuli Indications o Absence seizures o May be used in combination with other AEDs Adverse effects o Bloody dyscrasia, renal/liver impairment, systemic lupus erythematosus. Benzodiazepines Clonazepam (Klonopin) o Indication Effective in controlling Absence and Myoclonic Seizures o Dosage Tolerance may occur 6 months after drug therapy starts Dosage must be adjusted Diazepam (Valium) o Indications Primarily prescribed for treating Acute Status Epilepticus o Administration Must be administered IV to achieve desired response Short-term effect Other AEDs need to be given during or immediately after Administer slowly: Avoids Respiratory depression and hypotension Chlorazepate o Benzodiazepine used to treat anxiety Iminostilbenes: Carbamazepine (Tegretol) Mechanism of action o Unknown appears to exert its anticonvulsant properties by reducing the polysynaptic response and blocking post tetanic potentiation Indications o Tonic-Clonic and Partial Seizures and a combination of these seizures o Psychiatric disorders, trigeminal neuralgia, and alcohol withdrawal o Effective in treating refractory seizure disorders that have not responded to other anticonvulsant therapies. o The therapeutic level is 5 to 12 mcg/mL. Interactions o May occur when taken with grapefruit juice, causing possible toxicity. Valproate: Valproic acid (Depakote) Indication o Used to treat Absence, Grand Mal, and Mixed types of seizures. Safety and efficacy o Has not been established for children younger than 2 years of age o Caution in patients with liver disorders Hepatotoxicity is one of the possible adverse reactions Liver enzymes should be monitored Therapeutic serum range o 50 to 150 mcg/mL Anticonvulsants and Pregnancy Seizure episodes increase 25% in women with epilepsy Hypoxia that may occur during seizures o Places both the pregnant patient and the fetus at risk. Tend to act as inhibitors of vitamin K o Contributing to hemorrhage in infants shortly after birth Increase the loss of folate (folic acid) in pregnant patients Anticonvulsants and Febrile Seizures Associated with fever usually occur 3 months – 5 years Epilepsy develops in ~2.5% who have had febrile seizures. Prophylactic anticonvulsant treatment such as phenobarbital or diazepam may be indicated for high risk patients. Anticonvulsants and Status Epilepticus First Line, either o Diazepam (Valium) o Lorazepam (Ativan)+Phenytoin (Dilantin) Continued Seizures, either o Midazolam (Versed) o Propofol (Diprivan)