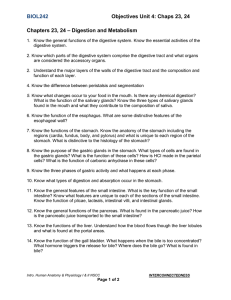
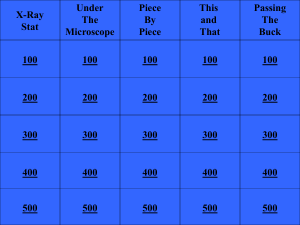
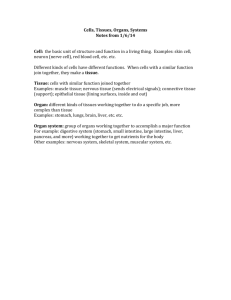
digestive system 100 level second semester work 2022 reg no
advertisement

1 INTRODUCTION Digestion is a process by which food is broken down into simple chemical substances that can be absorbed and used as nutrients by the body. Most of the substances in the diet cannot be utilized as such. These substances must be broken into smaller particles, so that they can be absorbed into blood and distributed to various parts of the body for utilization. Digestive system is responsible for these functions. Digestive process is accomplished by mechanical and enzymatic breakdown of food into simpler chemical compounds. A normal young healthy adult consumes about 1 kg of solid diet and about 1 to 2 liter of liquid diet every day. All these food materials are subjected to digestive process, before being absorbed into blood and distributed to the tissues of the body. NB: Digestive system plays the major role in the digestion and absorption of food substances. FUNCTIONS OF DIGESTIVE SYSTEM INCLUDE: 1. Ingestion or consumption of food substances 2. Breaking them into small particles 3. Transport of small particles to different areas of the digestive tract 4. Secretion of necessary enzymes and other substances for digestion 5. Digestion of the food particles 6. Absorption of the digestive products (nutrients) 7. Removal of unwanted substances from the body. The intake of food is necessary for life because the foods we eat provide essential nutrients. Nutrients are substances necessary for growth and repair of tissue and for maintenance of normal body functioning. A "nutritionally adequate" diet will contain all the essential nutritive substances in the amounts and proportions required to maintain life and health. ESSENTIAL NUTRIENTS OR SIX CLASSES OF FOOD These essential nutrients are carbohydrates, proteins, fats, minerals, vitamins, and water. NB: THE BASIC FUELS FOR CELLULAR ACTIVITY ARE Carbohydrates, proteins, and fats. MINERALS: Minerals are inorganic substances that help to regulate body processes. Some work with the enzymes, some act as catalysts, and Some work within the buffer systems. VITAMINS: Vitamins are organic nutrients that function to regulate physiological processes such as growth and metabolism. WATER: Water is an important nutrient with many functions. It acts as a coolant, It acts as a lubricant, It acts as a suspending medium, and It functions as a reactant in chemical processes. NB: Since the food we eat cannot be used for fuel in its consumed form, it must be broken down (digested) to the molecular level. In molecular form, the chemicals can be transported and absorbed through the cell membranes for utilization by the body cells. This process of digestion consists of both mechanical breakdown and chemical breakdown. MECHANICAL BREAKDOWN: This is a process by which the food items are being broken down into smaller particle by the help of chewing, swallowing, peristalsis and defecation. Mechanical digestion includes chewing, swallowing, peristalsis, and defecation. CHEMICAL DIGESTION: It’s a process that occurs by the enzymatic breakdown of the food- stuffs into chemically simple molecules that can be absorbed and utilized by the cells. CARBOHYDRATES: Carbohydrates, also known as sugars and starches, are organic compounds that provide the most ready source of energy to the body. Carbohydrates are broken down to their simplest form, called a monosaccharide, to be absorbed from the digestive tract. Carbohydrates consist of three major groups: Monosaccharides, Disaccharides, and By Mr. C. A. MBAH Page 1 2 Polysaccharides MONOSACCHARIDES: Monosaccharides are called the "simple sugars" because they cannot be further broken down into simpler molecules. The monosaccharide glucose is the major carbohydrate used for fuel by the cells. DISACCHARIDES: They are two monosaccharides that are joined chemically. POLYSACCHARIDES: They are a group of five or more monosaccharides that are joined chemically. PROTEINS: They are complex molecules of chemically linked chains of amino acids. Proteins are essential components of all cells in the body and have many functions within the human body. Some proteins function as enzymes, some as antibodies, and some are used for nutrition. The diet must contain sufficient protein to replace the protein broken down during normal body functions and growth. Proteins are broken down into their constituent amino acids to be absorbed from the digestive tract. These amino acids are transported to the body's cells, where they are recombined to form (synthesize) new protein molecules. NB: (1) All proteins are synthesized from combinations of the naturally occurring amino acids. (2) A great variety of proteins are made possible with only a limited number of amino acids because a different protein is created with each variation in the number and arrangement of the amino acids. This can be likened to the alphabet and words. The letters (amino acids) can be combined in a multitude of ways to form different words (proteins). (3) Ten of these amino acids are termed "essential" amino acids. This is due to the fact that these amino acids cannot be synthesized within the body, but must be consumed as food for growth and survival. (4) Other amino acids can be synthesized within the body from other molecules present within the cells. (5) A food protein that contains all the essential amino acids is referred to as a "complete" protein. FAT: Fat is primarily an energy source. In addition to its value as an energy source, fat serves as a carrier for the fat-soluble vitamins (A, D, E, and K) and adds flavor to the diet. Fats are emulsified in the intestine and split into fatty acids and glycerol for absorption. If not used as immediate energy sources, fatty acids are re-synthesized into body fat and stored in the many fat cells of the body for future use. METABOLISM: It refers to all the chemical activity within the body. All chemical reactions either release or require energy. PHASES OF METABOLISM: 1. An energy-generating process called catabolism and 2. An energy-requiring process called anabolism. NB: Both processes occur simultaneously within the cells, but they are regulated independently. For this reason, the body's metabolism can be thought of as energy balancing. CATABOLISM: It is a degenerative, energy-generating process. Complex molecules of proteins, carbohydrates, and fats are systematically broken down into simpler, smaller molecules by the body's cells. NB: The bonding energies that hold the atoms of a complex molecule together are released as the molecule is broken down. Much of this energy released by catabolism is captured and stored by the cells in the form of a chemical molecule known as ATP. Digestion is a catabolic process because the breakdown of the food releases energy. By Mr. C. A. MBAH Page 2 3 ANABOLISM: It is a building, energy-requiring process. New, more complex molecules are synthesized from simple molecules. These larger molecules form the body's structural and functional components. This synthesis requires the expenditure of the cellular energy generated by the cell's catabolic activities. ABSORPTION: This is the process by which digested food substances pass through the walls of some organs of the alimentary canal in to blood and lymph capillaries or circulation and use by body cells. ELIMINATION: Food substances that have been eaten but not be digested and absorbed are excreted from the alimentary canal as faces by the process of defecation. INGESTION: This is the taking of food into the alimentary tract i.e. eating and drinking. PROPULSION: This mixes and moves the contents along the alimentary tract THE DIGESTIVE SYSTEM The digestive system is made up of the alimentary canal (food passageway) and the accessory organs of digestion. The products of the accessory organs help to prepare food for its absorption and use by the tissues of the body. The main functions of the digestive system are: (1) To ingest and carry food so that digestion can occur. (2) To eliminate unused waste material. Gross anatomy of Gastrointestinal Tract (Alimentary Tract) Upper gastrointestinal tract The upper Gastrointestinal tract consists of the mouth, pharynx, esophagus, stomach, and duodenum proximal to the ligament o the buccal cavity, which contains the openings of the salivary glands; the tongue; and the teeth Lower gastrointestinal tract The lower gastrointestinal tract comprises the most of the intestines and anus. o Bowel or intestine, Small intestine, two of the three parts: o Duodenum o Jejunum o lleum o Large intestine, which has three parts: o Cecum (the vermiform appendix is attached to the cecum). o Colon (ascending colon, transverse colon, descending colon and sigmoid flexure) o Rectum o Anus NB: The alimentary canal is approximately 28 feet long in the adult and extends from the lips to the anus. It is composed of the organs listed below. (1) Mouth (and associated glands). (2) Pharynx. (3) Esophagus. (4) Stomach. (5) Small intestine (and associated glands). (6) Large intestine. (7) Rectum. (8) Anal canal and anus. Accessory Digestive Organs Accessory digestive organs are those which help primary digestive organs in the process of digestion. Various secretions are poured into the alimentary tract, some by glands on the lining membrane of the organs e.g. gastric juice secreted by glands in the lining of the stomach, and some glands situated outside the tract. 1. Teeth 2. Tongue 3. 3 pairs of salivary glands 4. The pancreas (Exocrine part of pancreas) 5. The liver and biliary tract, Gallbladder By Mr. C. A. MBAH Page 3 4 Fig. 1.1 Gastrointestinal tract BASIC STRUCTURE (HISTOLOGY) OF THE ALIMENTARY CANAL The gastrointestinal tract has a uniform general histology with some differences which reflect the specialization in functional anatomy. The GI tract can be divided into 4 concentric layers: • Mucosa • Submucosa • Muscularis externa (the external muscle layer) • Adventitia or serosa Mucosa: The mucosa is the innermost layer of the gastrointestinal tract that is surrounding the lumen, or space within the tube. This layer comes in direct contact with the food (or bolus), and is responsible for absorption and secretion, important processes in digestion. The mucosa can be divided into: Epithelium Lamina propria Muscularis mucosae The mucosa are highly specialized in each organ of the gastrointestinal tract, facing a low pH in the stomach, absorbing a multitude of different substances in the small intestine, and also absorbing specific quantities of water in the large intestine. Reflecting the varying needs of these organs, the structure of the mucosa can consist of invaginations of secretory glands (e.g., gastric pits), or it can be folded in order to increase surface area (examples include villi and plicae circulares). Submucosa: The submucosa consists of a dense irregular layer of connective tissue with large blood vessels, lymphatics and nerves branching into the mucosa and muscularis. It contains Meissner's plexus, an enteric nervous plexus, situated on the inner surface of the muscularis externa. Muscularis Externa: The muscularis externa consists of an inner circular layer and a longitudinal outer muscular layer. The circular muscle layer prevents the food from going backwards and the longitudinal layer shortens the tract. The coordinated contractions of these layers is called peristalsis and propels the bolus, or balled-up food, through the GI tract. Between the two muscle layers are the myenteric or Auerbach's plexus. By Mr. C. A. MBAH Page 4 5 Adventitia: The adventitia consists of several layers of epithelia. When the adventitia is facing the mesentery or peritoneal fold, the adventitia is covered by a mesothelium supported by a thin connective tissue layer, together forming a serosa, or serous membrane. Fig. 1.2 Basic Structure (Histology) of the Alimentary Canal GROSS ANATOMY OF GIT THE MOUTH The mouth, buccal cavity, or oral cavity is the first portion of the alimentary canal that receives food and begins digestion by mechanically breaking up the solid food particles into smaller pieces and mixing them with saliva. The oral mucosa is the mucous membrane epithelium lining the inside of the mouth. In addition to its primary role as the beginning of the digestive system, in humans the mouth also plays a significant role in communication. While primary aspects of the voice are produced in the throat, the tongue, lips, and jaw are also needed to produce the range of sounds included in human language. Another nondigestive function of the mouth is its role in secondary social and/or sexual activity such as kissing. The physical appearance of the mouth and lips play a part in defining sexual attractiveness. The mouth is normally moist, and is lined with a mucous membrane. The lips mark the transition from mucous membrane to skin, which covers most of the body. NB: Here food taken into the body is broken into small particles and mixed with saliva so that it can be swallowed. TEETH. (1) A person develops two sets of teeth during his life, a deciduous (or temporary) set and a permanent set. There are 20 deciduous teeth and these erupt during the first 3 years of life. They are replaced during the period between the 6th and 14th years by permanent teeth. There are 32 permanent teeth in the normal mouth: 4 incisors, 2 cuspids, 4 bicuspids, and 6 molars in each jaw. Each tooth is divided into two main parts: the crown, that part which is visible above the gums; and the root, that part which is not visible and which is embedded in the bony structure of the jaw. The crown of the tooth is protected by enamel. Tooth decay is from the outside in; once the protective enamel is broken, microorganisms attack the less resistant parts of the tooth. (2) The primary function of the teeth is to chew or masticate food. The teeth also help modify sound produced by the larynx to form words. SALIVARY GLANDS: These glands are the first accessory organs of digestion. There are three pairs of salivary glands. They secrete saliva into the mouth through small ducts. One pair, the parotid glands, is located at the side of the face below and in front of the ears. The second pair, the submandibular glands, lies on either side of the mandible. The third pair, the sublingual glands, lies just below the mucous membrane in the floor of the mouth. The flow of saliva is begun in several ways. Placing food in the mouth affects the nerve endings there. These nerve endings stimulate cells of the glands to excrete a small amount of thick fluid. The sight, thought, or smell of food also activates the brain and induces a large flow of saliva.. Salivary glands release their secretions into ductus that lead to the mouth. There are three main pairs By Mr. C. A. MBAH Page 5 6 a. The parotid glands: situated one on each side of the face. Each gland has parotid duct open into the mouth. b. Submandibular glands: these lie one on each side of the face under the angle of the jaw. The submandibular ducts open on the floor of the mouth. c. Sublingual glands: these glands lie under the mucous membrane of the floor of the mouth in front of the submandibular glands. They have numerous small ductus that open into the floor the mouth. Fig. 1.3: salivary gland Contribution by each major salivary gland is: i. Parotid glands : 25% ii. Submaxillary glands : 70% iii. Sublingual glands : 5%. By Mr. C. A. MBAH Page 6 7 Saliva: Saliva is combined secretions from the salivary glands and the small mucus secreting glands of the oral mucosa. About 1.5 liters of saliva is produced daily and it consist of Water Mineral salts An enzyme; salivary amylase Mucus Lysozyme Immunoglobulins Blood clotting factors Functions a. Chemical digestion of polysaccharides: saliva contains the enzyme amylase that begins the breakdown of complex sugars, including starches, reducing them to the disaccharide maltose. b. Lubrication of food: Dry food entering the mouth is moistened and lubricated by saliva before it can be made into a bolus ready for swallowing. c. Cleansing and lubricating: cleans the mouth and keep it soft, moist and pliable. It helps to prevent damage of mucous membrane by rough food. d. Non-specific defence: lysozyme, immunoglobulin and clotting factors combat invading microbes. e. Taste: the taste buds are stimulated only chemical substances in solution APPLIED PHYSIOLOGY a. HYPOSALIVATION It is the reduction in the secretion of saliva is called hyposalivation. It is of two types, namely temporary hyposalivation and permanent hyposalivation. 1. Temporary hyposalivation occurs in: i. Emotional conditions like fear. ii. Fever. iii. Dehydration. 2. Permanent hyposalivation occurs in: i. Sialolithiasis (obstruction of salivary duct). ii. Congenital absence or hypoplasia of salivary glands. iii. Bell palsy (paralysis of facial nerve). b. HYPERSALIVATION Excess secretion of saliva is known as hypersalivation. Physiological condition when hypersalivation occurs is pregnancy. Hypersalivation in pathological conditions is called ptyalism, sialorrhea, sialism or sialosis. Hypersalivation occurs in the following pathological conditions: 1. Decay of tooth or neoplasm (abnormal new growth or tumor) in mouth or tongue due to continuous irritation of nerve endings in the mouth. 2. Disease of esophagus, stomach and intestine. 3. Neurological disorders such as cerebral palsy, mental retardation, cerebral stroke and parkinsonism. 4. Some psychological and psychiatric conditions. 5. Nausea and vomiting In addition to hyposalivation and hypersalivation, salivary secretion is affected by other disorders also, which include: 1. Xerostomia 2. Drooling 3. Chorda tympani syndrome 4. Paralytic secretion of saliva 5. Augmented secretion of saliva 6. Mumps 7. Sjögren syndrome. By Mr. C. A. MBAH Page 7 8 TONGUE: The tongue is a muscular organ attached at the back of the mouth and projecting upward into the oral cavity. It is on the floor of the mouth that manipulates food for chewing and swallowing (deglutition). FUNCTIONS OF THE TONGUE: It is the primary organ of taste, as much of the upper surface of the tongue is covered in papillae and taste buds. It is utilized for taste, speech, mastication, salivation, and swallowing. A secondary function of the tongue is speech, in which the organ assists. It is sensitive and kept moist by saliva, and is richly supplied with nerves and blood vessels to help it move. Taste Buds: Located on the tongue and at the back of the mouth are special clumps of cells known as taste buds. Taste buds are sensitive to substances that are sweet, sour, bitter, and salty. PHARYNX The pharynx is a musculomembranous passage that leads from the nose and mouth to the esophagus. The passage of food from the pharynx into the esophagus is the second stage of swallowing. When food is being swallowed, the larynx is closed off from the pharynx to keep food from getting into the respiratory tract. The pharynx (plural: pharynges) is the part of the neck and throat situated immediately posterior to (behind) the mouth and nasal cavity, and cranial, or superior, to the esophagus, larynx, and trachea. Functions of the Pharynx The pharynx is part of the digestive system and respiratory system of many organisms. Because both food and air pass through the pharynx, a flap of connective tissue called the epiglottis closes over the trachea when food is swallowed to prevent choking or aspiration. In humans the pharynx is important in vocalization. The human pharynx is conventionally divided into three sections: 1. Oropharynx The oropharynx lies behind the oral cavity. The anterior wall consists of the base of the tongue and the epiglottic vallecula; the lateral wall is made up of the tonsil, tonsillar fossa, and tonsillar (faucial) pil-lars; the superior wall consists of the inferior surface of the soft palate and the vulva. 2. Nasopharynx The nasopharynx lies behind the nasal cavity. Postero-superiorly this extends from the level of the junction of the hard and soft palates to the base of skull. The inferior wall consists of the superior surface of the soft palate. 3. Laryngopharynx The laryngopharynx, also known as the hypopharynx, roughly corresponds to the levels between C4 to C6, it includes the pharyngo-esophageal junction (postericoid area), the piriform sinus, and the posterior pharyngeal wall. Like the oropharynx above it the hypopharynx serves as a passageway for food and air and is lined with a stratified squamous epithelium. It lies inferior to the upright epiglottis and extends to the larynx, where the respiratory and digestive pathway diverge. At that point the laryngopharynx is continuous with the esophagus posteriorly. The esophagus conducts food and fluid to the stomach; air enters the larynx anteriorly. During swallowing, food has the “right of way”, air passage temporarily stops. THE ESOPHAGUS The esophagus is a musculomembranous passage about 10 inches long, lined with a mucous membrane. It leads from the pharynx through the chest to the upper end of the stomach. Its function is to complete the act of swallowing. The involuntary movement of material down the esophagus is carried out by the process known as peristalsis, which is the wavelike action produced by contraction of the muscular wall. This is the method by which food is moved throughout the alimentary canal. By Mr. C. A. MBAH Page 8 9 The oesophagus is about 25 cm long and about 2 cm in diameter and lies in the median plane in the thorax in front of the vertebral column behind the trachea and the heart. It is continuous with the pharynx above and just below the diaphragm it joins the stomach. Functions of the mouth, pharynx and esophagus: a. Formation of bolus: when the food is taken into the mouth it is masticated chewed, by the teeth and move round the mouth by the tongue and muscles of cheeks. It is mixed with saliva and formed into a soft mass or bolus ready for swallowing. b. Swallowing: this occurs in three stages after mastication is complete and the bolus has been formed The mouth is closed and voluntary muscles of the tongue and cheeks push bolus backward into the pharynx The muscles of the pharynx are stimulated by reflex action initiated by the walls of the oropharynx and coordinated in the medulla and lower pons in brain stem. Involuntary con. traction of these muscles propels the bolus down into esophagus. the presence of the bolus in the pharynx stimulates a wave of peristalsis that propels the bolus through the esophagus to the stomach c. The walls of the oesophagus are lubricated by mucus which assists the passage of the bolus during the peristaltic contraction of the muscular wall. THE STOMACH The stomach is a J-shaped dilated portion of the alimentary tract situated in the epigastric, umbilical and left hypochondriac regions of the abdominal cavity. Structure of stomach The stomach is continuous with the esophagus at the cardiac sphincter and with the duodenum at the pyloric sphincter. The stomach lies between the esophagus (food and liquid throat tube) and the duodenum (the first part of the small intestine). It is on the left side of the abdominal cavity. The top of the stomach lies against the diaphragm. Lying beneath the stomach is the pancreas, and the greater omentum which hangs from the greater curvature. The stomach is divided into three regions 1. The fundus 2. The body 3. The antrum At the distal end of the pyloric antrum is the pyloric sphincter, guarding the opening between the stomach and duodenum. When the stomach is inactive the pyloric sphincter is relaxed and open, when stomach contains food the sphincter is closed. Walls of the stomach: The four layers of tissue that comprise the basic structure of the alimentary canal are found in the stomach but with some modifications. Muscle layer. This consists of three layers of smooth muscle fibres 1. An outer layer of longitudinal fibres 2. A middle layer of circular fibres 3. An inner layer of oblique fibres Mucosa By Mr. C. A. MBAH Page 9 10 When the stomach is empty the mucous membrane lining is thrown in to longitudinal folds or rugae and when fill the rugae are toned out and the surface has a smooth. Numerous gastric glands are situated below the surface in the mucous membrane. They consist of specialized cells that secrete gastric juice in to the stomach. Fig. 1.4: Structure of stomach Functions of Stomach: a. Temporary storage allowing time for the digestive enzymes, pepsins, to act. b. Chemical digestion-pepsin converts proteins to polypeptides. c. Mechanical breakdown. d. Limited absorption of water, alcohol and some lipid soluble drugs. e. Non-specific defence against microbes-provided by hydrochloric acid in gastric. juice. Vomiting occur in response to ingestion of gastric irritants. f. Preparation of iron for absorption further along the tract. g. Production and secretion of intrinsic factor needed for absorption of vitamin B12 in ileum h. Regulation of passage of gastric contents into the duodenum. i. Secretion of gastrin. Gastric Juice About 2 liters of gastric juice are secreted daily by specialized secretoy glands in the mucosa. It consists of Water Mineral salts Mucus Hydrochloric acid Intrinsic factor Inactive enzyme precursors: pepsinogens Functions of Gastric Juice: a. water further liquefies the food swallowed b. Hydrochloric acid: acididies the food ans stops the action of salivary amylase, kills the ingested microbes, provides the acid environment needed for effective digestion by pepsins. c. Pepsinogens: are activated to pepsins by hydrochloric acid and by pepsins then begins digestion of proteins d. intrinsic factor: is necessary of absorption of Vit B12 e. Mucus: prevents mechanical injury to the stomach wall by lubricating the contents, prevent chemical injury by acting as barrier between the stomach wall and the corrosive gastric juice. By Mr. C. A. MBAH Page 10 11 PHYSIOLOGICAL FUNCTIONS OF THE STOMACH Gastric acid is produced by parietal cells (also called oxyntic cells) in the stomach. Its secretion is a complex and relatively energetically expensive process. Parietal cells contain an extensive secretory network (called canaliculi) from which the gastric acid is secreted into the lumen of the stomach. These cells are part of epithelial fundic glands in the gastric mucosa. The pH of gastric acid is 2 to 3 in the human stomach lumen, the acidity being maintained by the proton pump HI* ATPase. The parish Cell releases bicarbonate into the blood stream in the process, which causes the temporary rise of pH, the blood, known as alkaline tide. The resulting highly acidic environment in the stomach lumen causes proteins from food to lose their characteristic folded structure (or denature). This exposes the protein's peptide bonds. The chief cells of the stomach secrete enzymes for protein breakdown (inactive pepsinogen and renin). Gastric acid activates pepsinogen into pepsin- this enzyme then helps digestion by breaking the bonds linking amino acids, a process known as proteolysis. In addition, many microorganisms have their growth inhibited by such an acidic environment which is helpful to prevent infection. Secretions: Gastric acid secretion happens in several steps. Chloride and hydrogen ions are secreted separately from the cytoplasm of parietal cells and mixed in the canaliculi. Gastric acid is then secreted into the lumen of the oxyntic gland and gradually reaches the main stomach lumen. Chloride and sodium ions are secreted actively from the cytoplasm of the parietal cell into the lumen of the canaliculus. This creates a negative potential of -40 mV to -70 mV across the parietal cell membrane that causes potassium ions and a small number of sodium ions to diffuse from the cytoplasm into the parietal cell canaliculi. The enzyme carbonic anhydrase catalyses the reaction between carbon dioxide and water to form carbonic acid. This acid immediately dissociates into hydrogen and bicarbonate ions. The hydrogen ions leave the cell through H*/K* ATPase antiporter pumps. At the same time sodium ions are actively reabsorbed. This means the majority of secreted K+ and Nations return to the cytoplasm. In the canaliculus, secreted hydrogen and chloride ions mix and are secreted into the lumen of the oxyntic gland. The highest concentration that gastric acid reaches in the stomach is 160 mM in the canaliculi. This is about 3 million times that of arterial blood, but almost exactly isotonic with other bodily fluids. The lowest pH of the secreted acid is 0.8, but the acid is diluted in the stomach lumen to a pH between 1 and? There are three phases in the secretion of gastric acid: 1. The cephalic phase: 30% of the total gastric acid to be produced is stimulated by anticipation of eating and the smell or taste of food. 2. The gastric phase: 60% of the acid secreted is stimulated by the distention of the stomach with food. Plus, digestion produces proteins, which causes even more gastrin production. 3. The intestinal phase: the remaining 10% of acid is secreted when chyme enters the smallines tine, and is stimulated by small intestine distention. Regulation of Secretion Gastric acid production is regulated by both the autonomic nervous system and several hormones. The parasympathetic nervous system, via the vagus nerve, and the hormone gastrin stimulate the parietal cell to produce gastric acid, both directly acting on parietal cells and indirectly, through the stimulation of the secretion of the hormone histamine from enterochromaffine-like cells (ECL). Vasoactive intestinal peptide, cholecystokinin, and secretin all inhibit production. By Mr. C. A. MBAH Page 11 12 The production of gastric acid in the stomach is tightly regulated by positive regulators and negative feedback mechanisms. Four types of cells are involved in this process: parietal cells, G cells, D cells and enterochromaffine-like cells. Besides this, the endings of the vagus nerve (X) and the intramural nervous plexus in the digestive tract influence the secretion significantly. Nerve endings in the stomach secrete two stimulatory neurotransmitters: acetylcholine and gastrin-releasing peptide. Their action is both direct on parietal cells and mediated through the secretion of gastrin from G cells and histamine from enterochromaffine-like cells. Gastrin acts on parietal cells directly and indirectly too, by stimulating the release of histamine. The release of histamine is the most important positive regulation mechanism of the secretion of gastric acid in the stomach. Its release is stimulated by gastrin and acetylcholine and inhibited by somatostatin. Neutralization In the duodenum, gastric acid is neutralized by sodium bicarbonate. This also blocks gastric enzymes that have their optima in the acid range of pH. The secretion of sodium bicarbonate from the pancreas is stimulated by secretin. This polypeptide hormone gets activated and secreted from so-called S cells in the mucosa of the duodenum and jejunum when the pH in duodenum falls below 4.5 to 5:0. The neutralization is described by the equation: • HCI + NaHCO3 --» NaCI + H2CO3 The carbonic acid instantly decomposes into carbon dioxide and water, then gets eliminated through urine. Fig. 1.5: Secretion of gastric juice MECHANICAL FUNCTION i. Storage Function Food is stored in the stomach for a long period, i.e. for 3 to 4 hours and emptied into the intestine slowly. The maximum capacity of stomach is up to 1.5 L. Slow emptying of stomach provides enough time for proper digestion and absorption of food substances in the small intestine. ii. Formation of Chyme Peristaltic movements of stomach mix the bolus with gastric juice and convert it into the semisolid material known as chyme. APPLIED PHYSIOLOGY Gastric secretion is affected by the following disorders: 1. GASTRITIS It Is an inflammation of the lining of the stomach, and has many possible causes. The main acute causes are excessive alcohol consumption or prolonged use of nonsteroidal anti-inflammatory drugs (also known as NSAIDs) such as aspirin or ibuprofen. Sometimes gastritis develops after major surgery, traumatic injury, burns, or severe infections. Gastritis may also occur in those who have had weight loss surgery resulting in the banding or reconstruction of the digestive tract. Chronic causes are infection with bacteria, primarily Helicobacter pylori. NB: Inflammation of gastric mucosa is called gastritis. It may be acute or chronic. Acute gastritis is characterized by inflammation of superficial layers of mucus membrane and infiltration with leukocytes, mostly neutrophils. By Mr. C. A. MBAH Page 12 13 Chronic gastritis involves inflammation of even the deeper layers and infiltration with more lymphocytes. It results in the atrophy of the gastric mucosa, with loss of chief cells and parietal cells of glands. Therefore, the secretion of gastric juice decreases. Causes of Acute Gastritis i. Infection with bacterium Helicobacter pylori ii. Excess consumption of alcohol iii. Excess administration of Aspirin and other nonsteroidal antiinflammatory drugs (NSAIDs) iv. Trauma by nasogastric tubes v. Repeated exposure to radiation (rare). Causes of Chronic Gastritis a. Chronic infection with Helicobacter pylori Longterm intake of excess alcohol b. Longterm use of NSAIDs c. Autoimmune disease. Features Features of gastritis are nonspecific. Common feature is abdominal upset or pain felt as a diffused burning sensation. It is often referred to epigastric pain. Other features are: i. Nausea ii. Vomiting iii. Anorexia (loss of appetite) iv. Indigestion v. Discomfort or feeling of fullness in the epigastric region vi. Belching (process to relieve swallowed air that is accumulated in stomach). 2. GASTRIC ATROPHY Gastric atrophy is the condition in which the muscles of the stomach shrink and become weak. Gastric glands also shrink, resulting in the deficiency of gastric juice. Causes of Gastric atrophy Gastric atrophy is caused by chronic gastritis called chronic atrophic gastritis. There is atrophy of gastric mucosa including loss of gastric glands. Autoimmune atrophic gastritis also causes gastric atrophy. Features of Gastric atrophy Generally, gastric atrophy does not cause any noticeable symptom. However, it may lead to achlorhydria (absence of hydrochloric acid in gastric juice) and pernicious anemia. Some patients develop gastric cancer. 3. PEPTIC ULCER A peptic ulcer, also known as ulcus pepticum, PUD or peptic ulcer disease, is an ulcer (defined as mucosal erosions equal to or greater than 0.5 cm) of an area of the gastrointestinal tract that is usually acidic and thus extremely painful. As many as 80% of ulcers are associated with Helicobacter pylori, a spiral-shaped bacterium that lives in the acidic environment of the stomach, ulcers can also be caused or worsened by drugs such as aspirin and other NSAIDs. NB: Ulcer means the erosion of the surface of any organ due to shedding or sloughing of inflamed necrotic tissue that lines the organ. Peptic ulcer means an ulcer in the wall of stomach or duodenum, caused by digestive action of gastric juice. If peptic ulcer is found in stomach, it is called gastric ulcer and if found in duodenum, it is called duodenal ulcer. Contrary to general belief, more peptic ulcers arise in the duodenum (first part of the small intestine, just after the stomach) than in the stomach. About 4% of stomach ulcers are caused by a malignant tumor, so multiple biopsies are needed to exclude cancer. Duodenal ulcers are generally benign. A peptic ulcer may arise at various locations: o Stomach (called gastric ulcer) o Duodenum (called duodenal ulcer) o Oesophagus (called Oesophageal ulcer) o Meckel's Diverticulum (called Meckel's Diverticulum ulcer) Types of peptic ulcers: Type I: Ulcer along the lesser curve of stomach Type II: Two ulcers present - one gastric, one duodenal Type III: Prepyloric ulcer Type IV: Proximal gastroesophageal ulcer Type V: Anywhere along gastric body, NSAID induced By Mr. C. A. MBAH Page 13 14 Signs and symptoms Abdominal pain, clasical epigastrio with severity relating to mealtimes, afer around 3 hours of taking a meal (duodenal ulcers are classically relieved by food, while gastric ulcers are exacerbated by it); Bloating and abdominal fullness; Waterbrash (rush of saliva after an episode of regurgitation to dilute the acid in esophagus); Nausea, and lots of vomiting; Loss of appetite and weight loss; Hematemesis (vomiting of blood); this can occur due to bleeding directly from a gastric ulcer, or from damage to the Oesophagus from severe/continuing vomiting Melena (tarry, foul-smelling feces due to oxidized iron from hemoglobin) Rarely, an ulcer can lead to a gastric or duodenal perforation. This is extremely painful and requires immediate surgery. Causes of peptic ulcer i. Increased peptic activity due to excessive secretion of pepsin in gastric juice ii. Hyperacidity of gastric juice iii. Reduced alkalinity of duodenal content iv. Decreased mucin content in gastric juice or decreased protective activity in stomach or duodenum v. Constant physical or emotional stress vi. Food with excess spices or smoking (classical causes of ulcers) vii. Longterm use of NSAIDs (see above) such as Aspirin, Ibuprofen and Naproxen viii. Chronic inflammation due to Helicobacter pylori. NB: A history of heartburn, gastroesophageal reflux disease (GERD) and use of certain forms of medi cation can raise the suspicion for peptic ulcer. Medicines associated with peptic ulcer include NSAID (non-steroid anti-inflammatory drugs) that inhibit cyclooxygenase, and most glucocorticoids (e.g. dexamethasone and prednisolone). Features of peptic ulcer Most common feature of peptic ulcer is severe burning pain in epigastric region. In gastric ulcer, pain occurs while eating or drinking. In duodenal ulcer, pain is felt 1 or 2 hours after food intake and during night. Other symptoms accompanying pain are: i. Nausea ii. Vomiting iii. Hematemesis (vomiting blood) iv. Heartburn (burning pain in chest due to regurgitation of acid from stomach into esophagus) v. Anorexia (loss of appetite) vi. Loss of weight. 4. DYSPEPSIA Popularly known as indigestion, meaning hard or difficult digestion, is a medical condition characterized by chronic or recurrent pain in the upper abdomen, upper abdominal fullness and feeling full earlier than expected when eating. It can be accompanied by bloating, belching, nausea or heartburn. Dyspepsia is a common problem, and is frequently due to gastroesophageal reflux disease (GERD) or gastritis. 5. PYLORIC STENOSIS (OR INFANTILE HYPERTROPHIC PYLORIC STENOSIS) Is a condition that causes severe vomiting in the first few months of life. There is narrowing (stenosis) of the opening from the stomach to the intestines, due to enlargement (hypertrophy) of the muscle surrounding this opening (the pylorus, meaning "gate"), which spasms when the stomach empties. Achlorhydria and Hypochlorhydria It refers to states where the production of gastric acid in the stomach is absent or low, respectively. It is associated with various other medical problems. Gastroparesis, (Delayed Gastric Emptying) Is a medical condition consisting of a paresis (partial paralysis) of the stomach ("gastro-"), resulting in food remaining in the stomach for a longer period of time than normal. Normally, the stomach contracts to move food down into the small intestine for digestion. The vagus nerve controls these contractions. Gastroparesis may occur when the vagus nerve is damaged and the muscles of the stomach and intestines do not work normally. Food then moves slowly or stops moving through the digestive tract. By Mr. C. A. MBAH Page 14 15 6. GASTROPTOSIS Is the abnormal downward displacementof the stomach. I is not a life threatening condition. The condition frequently causes digestive symptoms and constipation, and is much more prominent in women than men. 7. ULCERATIVE COLITIS Ulcerative colitis (Colitis ulcerosa, UC) is a form of inflammatory bowel disease (IBD). Ulceratin colts is a cotin Colts I disease of the intestine, specifically the large intestine or colon, that in. cludes character stealter, or open sores, in the colon. The main symptom of active disease is usuals constancharacteristieuicersibioen, or gradual onset. Ulcerative colitis is, however, believed to have a systemic etiology that leads to many symptoms outside the intestine. Because of the name, IBD Often conf sad weh iritable bowel syndrome ("IBS"), a troublesome, but much less serious, condition Ulcerative colitis has similarities to Crohn's disease, another form of IBD. Ulcerative colitis is an inter. mittent disease, with periods of exacerbated symptoms, and periods that are relatively symptom-free Although the symptoms of ulcerative colitis can sometimes diminish on their own, the disease usual requires treatment to go into remission. Ulcerative colitis has no known cause; there is a presumed genetic component to susceptibility. The disease may be triggered in a susceptible person by environmental factors. Although dietary modif-cation may reduce the discomfort of a person with the disease, ulcerative colitis is not thought to be caused by dietary factors. Although ulcerative colitis is treated as though it were an autoimmune dis-ease, there is no consensus that it is such. Treatment is with anti-inflammatory drugs, immunosuppres-sion, and biological therapy targeting specific components of the immune response. Colectomy (partial or total removal of the large bowel through surgery) is occasionally necessary, and is considered to be a cure for the disease. 8. HEPATIC DISORDERS Hepatitis Hepatitis (plural hepatitides) implies injury to the liver characterized by the presence of inflammatory cells in the tissue of the organ. The condition can be self-limiting, healing on its own, or can progress to scarring of the liver. Hepatitis is acute when it lasts less than six months and chronic when it persists longer. A group of viruses known as the hepatitis viruses cause most cases of liver damage worldwide. Hepatitis can also be due to toxins (notably alcohol), other infections or from autoimmune process. It may run a subclinical course when the affected person may not feel ill. The patient becomes unwell and symptomatic when the disease impairs liver functions that include, among other things, removal of harmful substances, regulation of blood composition, and production of bile to help digestion. Causes of Hepatitis Acute Hepatitis Viral hepatitis: Hepatitis A through E (more than 95% of viral cause), Herpes simplex, Cytomegalovirus, Epstein-Barr, yellow fever virus, adenoviruses. o Non viral infection: toxoplasma, Leptospira, O fever, rocky mountain spotted fever o Toxins: Amanita toxin in mushrooms, carbon tetrachloride, asafetida o Drugs: Paracetamol amoxycilin, antituberculosis medicihes, minocycline and many others (see longer list below). o Ischemic hepatitis (circulatory insufficiency) o Pregnancy o Auto immune conditions, e.g. Systemic Lupus Erythematosus (SLE) o Metabolic diseases, e.g. Wilson's disease Chronic Hepatitis o Viral hepatitis: Hepatitis B with or without hepatitis D, hepatitis C (neither hepatitis A nor hepatitis E causes chronic hepatitis) o Autoimmune: Autoimmune hepatitis o Alcohol o Drugs: methyldopa, nitrofurantoin, isoniazid, ketoconazole o Non-alcoholic steatohepatitis o Heredity: Wilson's disease, alpha 1-antitrypsin deficiency o Primary biliary cirrhosis and primary sclerosing cholangitis occasionally mimic chronic hepatitis Symptoms of Hepatitis Acute Clinically, the course of acute hepatitis varies widely from mild symptoms requiring no treatment to fulminant hepatic failure needing liver transplantation. Acute viral hepatitis is more likely to be asymptomatic in younger By Mr. C. A. MBAH Page 15 16 people. Symptomatic individuals may present after convalescent stage of 7 to 10 days, with the total illness lasting 2 to 6 weeks. Initial features are of nonspecific flu-like symptoms, common to almost all acute viral infections and may include malaise, muscle and joint aches, fever, nausea or vomiting, diarrhea, and headache. More specific symptoms, which can be present in acute hepatitis from any cause, are: profound loss of appetite, aversion to smoking among smokers, dark urine, yellowing of the eyes and skin (i.e., jaun-dice) and abdominal discomfort. Physical findings are usually minimal, apart from jaundice (33%) and tender hepatomegaly (10%). There can be occasional lymphadenopathy (5%) or splenomegaly (5%). Chronic Majority of patients will remain asymptomatic or mildly symptomatic, abnormal blood tests being the only manifestation. Features may be related to the extent of liver damage or the cause of hepatitis. Many experience return of symptoms related to acute hepatitis. Jaundice can be a late feature and may indicy exertensive damage. Other features include abdominal Fullness from enlarged liver or spleen, low grade fever and fluid retention (ascites). Extensive damage and scarring of liver (i.e., cirrhosis leads to weight loss, easy bruising and bleeding tendencies. Acne, abnormal menstruation, lung scarring, inflammation of the thyroid gland and kidneys may be present in women with autoimmune hepatitis. Cirrhosis Is a consequence of chronic liver disease characterized by replacement of liver tissue by fibrous scar tissue as well as regenerative nodules (lumps that occur as a result of a process in which damaged tissue is regenerated), leading to progressive loss of liver function. Cirhosis is most commonly caused by alcoholism, hepatitis B and C and fatty liver disease but has many other possible causes. Some cases are idiopathic, i.e., of unknown cause. Fatty liver (fatty liver disease (FL.D), steatorrhoeic hepatosis, or steatosis hepatitis) Is a reversible condition where large vacuoles of tristyceride fat accumulate in liver cells via the pro-Is as elstearosis. Despile havins multi a cool in take alive can be considered a single discase that o-curs world resistance). The condition is also associated with other diseases that inherencies metabolism. Liver abscess Is a pus-filled mass inside or attached to the liver. Common causes are an abdominal infection such as appendicitis or diverticulitis. With treatment, the death rate is 10-30%. Liver failure Is the inability of the liver to perform its normal synthetic and metabolic function as part of normal physiology. Two forms are recognised: o Acute liver failure - development of hepatic encephalopathy (confusion, stupor and coma) and decreased production of proteins (such as albumin and blood clotting proteins) within four weeks of the first symptoms (such as jaundice) of a liver problem. "Hyperacute" liver failure is said to be present if this interval is 7 days or less, while "subacute" liver failure is said to be present if the interval is 5-12 weeks. o Chronic liver failure usually occurs in the context of cirrhosis, itself potentially the result of many possible causes, such as excessive alcohol intake, hepatitis B or C, autoimmune, hereditary and metabolic causes (such as iron or copper overload or non-alcoholic fatty liver disease) 9. ZOLLINGER-ELLISON SYNDROME Zollinger Ellison syndrome is characterized by secretion of excess hydrochloric acid in the stomach. Cause of Zollinger Ellison syndrome This disorder is caused by tumor of pancreas. Pancreatic tumor produces a large quantity of gastrin. Gastrin increases the hydrochloric acid secretion in stomach by stimulating the parietal cells of gastric glands. Features of Zollinger Ellison syndrome i. Abdominal pain ii. Diarrhea (frequent and watery, loose bowel movements) iii. Difficulty in eating iv. Occasional hematemesis SMALL INTESTINE Small intestine is the part of gastrointestinal (GI) tract, extending between the pyloric sphincter of stomach and ileocecal valve, which opens into large intestine. It is called small intestine because of its small diameter, compared to that of the large intestine. It is 5 meters long and lies in the abdominal cavity surrounded by the large intestine. Although a simple tube the length and diameter of the small intestine would have a surface area By Mr. C. A. MBAH Page 16 17 of only about 0.5m2, the surface complexity of the inner lining of the small intestine increase its surface area by a factor of 500 to approximately 250m2 But it is longer than large intestine. Its length is about 6 meter. Important function of small intestine is absorption. Maximum absorption of digested food products takes place in small intestine. The small intestine comprises three main sections continuous with each other a. The duodenum is about 25cm long and corves around the head of the pancreas. b. The jejunum is the middle section of the small intestine and is about 2meters long c. The ileum, or terminal section, is about 3 meters long and ends at the ileocaecal valve, which controls the flow of material from the ileum to the caccum, the first part of the large intestine NB: Wall of the small intestine has all the four layers as in stomach. The intestine is divided into three continuous parts: duodenum, jejunum, and ileum. Most of the absorption of food takes place in the small intestine. Muscular contraction of the intestinal walls produces the wave-like motion called peristalsis, which propels the contents through the length of the intestines. The walls of the intestines are covered with small, fingerlike projections called villi, which provide a larger surface area for absorption. After food has been digested, it is absorbed into the capillaries of the villi and carried to all parts of the body via the circulatory system. The small intestine receives digestive juices from three accessory organs of digestion: the pancreas, liver, and gallbladder. INTESTINAL JUICE Intestinal juice (suceus entericus) refers to the clear to pale yellow watery secretions from the glands lining the small intestine walls. Secretion is stimulated by the mechanical pressure of partly digested food in the intestine. Its function is to complete the process begun by pancreatic juice; the enzyme trypsin exists in pancreatic juice in the inactive form trypsinogen, it is activated by the intestinal enterokinase in intestinal juice. Trypsin can then activate other protease enzymes and catalyze the reaction pro-colipase colipase. Colipase is necessary, along with Bile Salts, to enable Lipase function. Intestinal juice also contains hormones, digestive enzymes, mucus, substances to neutralize hydro. chloric acid coming from the stomach and erepsin which further digests polypeptides into amino acids, completing protein digestion. FUNCTIONS OF SUCCUS ENTERICUS 1. DIGESTIVE FUNCTION: Enzymes of succus entericus act on the partially digested food and convert them into final digestive products. Enzymes are produced and released into succus entericus by enterocytes of the villi 2. PROTECTIVE FUNCTION i. Mucus present in the succus entericus protects the intestinal wall from the acid chyme, which enters the intestine from stomach; thereby it prevents the intestinal ulcer. ii. Defensins secreted by paneth cells of intestinal glands are the antimicrobial peptides. These peptides are called natural peptide antibiotics because of their role in killing the phagocytosed bacteria. 3. Activator Function: Enterokinase present in intestinal juice activates trypsinogen into trypsin. Trypsin, in turn activates other enzymes 4. Hemopoietic Function: Intrinsic factor of Castle present in the intestine plays an important role in erythropoiesis. It is necessary for the absorption of vitamin B12. 5. Hydrolytic Process Intestinal juice helps in all the enzymatic reactions of digestion. FUNCTIONS OF SMALL INTESTINE 1. Mechanical Function: Mixing movements of small intestine help in the thorough mixing of chyme with the digestive juices like succus entericus, pancreatic juice and bile. 2. Secretory Function: Small intestine secretes succus entericus, enterokinase and the GI hormones. 3. Hormonal Function: Small intestine secretes many GI hormones such as secretin, cholecystokinin, etc. These hormones regulate the movement of GI tract and secretory activities of small intestine and pancreas By Mr. C. A. MBAH Page 17 18 4. Digestive function 5. Activator function 6. Hemopoietic function 7. Hydrolytic function 8. Absorptive functions: Presence of villi and microvilli in small intestinal mucosa increases the surface area of mucosa. This facilitates the absorptive function of intestine. MOVEMENTS OF SMALL INTESTINE The duodenum receives food from stomach in small quantities. This mixture of food and digestive juices, called "chyme" is passed along the length of the small intestine. The movements of small intestine are of two types. 1. Segmentation: these are rhythmical alternating contractions and relaxations. These shutting movements mix the chyme and bring it into contact with absorptive mucosa, i.e. digestion and absorption are promoted. 2. Peristalsis: entry of food into the small intestine stimulates the stretch receptors and the stretch receptors convey information to the CNS and according to the need, the parasympathetic nerves stimulates contraction of the intestine and sympathetic stimulation decreases the motility of the intestine. The segmentation is myogenic in nature, i.e. it is the property of the smooth muscles. It doesn't depend upon the nervous mechanism, where as peristaltic movements are neurogenic, i.e. it is carried out with help of sympathetic and parasympathetic nerves of the ANS (Autonomic Nervous System). INTESTINAL VILLI AND GLANDS OF SMALL INTESTINE a. INTESTINAL VILLI Mucous membrane of small intestine is covered by minute projections called villi. The height of villi is about 1 mm and the diameter is less than 1 mm. Villi are lined by columnar cells, which are called Enterocytes. Each enterocyte gives rise to hair-like projections called microvilli. Villi and microvilli increase the surface area of mucous membrane by many folds. Within each villus, there is a central channel called lacteal, which opens into lymphatic vessels. It contains blood vessels also. b. CRYPTS OF LIEBERKÜHN OR INTESTINAL GLANDS Crypts of Lieberkühn or intestinal glands are simple tubular glands of intestine. Intestinal glands do not penetrate the muscularis mucosa of the intestinal wall, but open into the lumen of intestine between the villi. Intestinal glands are lined by columnar cells. Lining of each gland is continuous with epithelial lining of the villi Epithelial cells lining the intestinal glands undergo division by mitosis at a faster rate. Newly formed cells push the older cells upward over the lining of villi. These cells which move to villi are called enterocytes. Enterocytes secrete the enzymes. Old enterocytes are continuously shed into lumen along with enzymes. Types of cells interposed between columnar cells of intestinal glands: 1. Argentaffin cells or enterochromaffin cells, which secrete intrinsic factor of Castle 2. Goblet cells, which secrete mucus 3. Paneth cells, which secrete the cytokines called defensins. (1) PANCREAS: By Mr. C. A. MBAH Page 18 19 The pancreas is a pale grey gland weighing about 60 grams. It is about 12 to 15 em long and is situated in the epigastric and left hypochondriac regions of the abdominal cavity. It consists of a broad head, a body, and a narrow tail. The head lies in the curve of the duodenum, the body behind the stomach and the tail lies in front of the left kidney. The pancreas is both an exocrine and endocrine gland. The exocrine pancreas: this consists of a large number of lobules made up of small alveoli, the walls of which consist of secretory cells. Each lobule is drained by a tiny duct and these unite eventually to form the pancreatic duct, which extends the whole length of gland and opens in to the duodenum. Just before entering the duodenum the pancreatic duct joins the common bile duct to form the hepatopan-creatic ampulla. The function of exocrine pancreas is to produce pancreatic juice containing enzymes that digest carbohydrates, proteins and fats. The endocrine pancreas: Distributed throughout the gland are groups of specialized cells called the pancreatic islets (of Langerhans). The islets have no ducts so the hormones diffuse directly into the blood. The endocrine pancreas secretes insulin, glucagons, somatostatin, and pancreatic polypeptide. Fig. 1.8: The pancreas Composition of Pancreatic Juice: Pancreatic juice is alkaline (pH 8) because it contains significant quantities of bicarbonate ions, which are alkaline in solution. o Water o Mineral salts o Enzymes: amylase, lipase o Inactive enzyme precursors: trypsinogen, chymotrypsingen, procarboxypeptidase. Functions of the Pancreas: a. Digestion of proteins: trypsinogen and chymotrypsinogen are inactive enzyme precursors activated by enterokinase (an enzyme in microvilli), which converts then in to the active proteo-lytic enzymes trypsin and chymotrypsin. These enzymes convert polypeptides to tripeptides. dipeptides and amino acids. b. Digestion of carbohydrates: pancreatic amylase converts all digestible polysaccharides (starch-es) not acted upon by salivary amylase to disaccharides. c. Digestion of fats: lipase converts fats to fatty acids and glycerol. REGULATION OF PANCREATIC SECRETION Secretion of pancreatic juice is regulated by both nervous and hormonal factors. a. STAGES OF PANCREATIC SECRETION Pancreatic juice is secreted in three stages like the gastric juice: 1. Cephalic phase 2. Gastric phase 3. Intestinal phase. These three phases of pancreatic secretion correspond with the three phases of gastric secretion. 1. CEPHALIC PHASE By Mr. C. A. MBAH Page 19 20 As in case of gastric secretion, cephalic phase is regulated by nervous mechanism through reflex action. Two types of reflexes occur: i. Unconditioned reflex ii Conditioned reflex Unconditioned Reflex Unconditioned reflex is the inborn reflex. When food is placed in the mouth, salivary secretion and gastric secretion are induced. Simultaneously, pancreatic secretion also occurs. Stages of reflex action: i. Presence of food in the mouth stimulates the taste buds and other receptors in the mouth ii. Sensory (afferent) impulses from mouth reach dorsal nucleus of vagus and efferent impulses reach pancreatic acini via vagal efferent nerve fibers iii. Vagal efferent nerve endings secrete acetylcholine, which stimulates pancreatic secretion. Conditioned Reflex Conditioned reflex is the reflex response acquired by previous experience. Presence of food in the mouth is not necessary to elicit this reflex. The sight, smell, hearing or thought of food, which induce salivary secretion and gastric secretion induce pancreatic secretion also. 2. GASTRIC PHASE Secretion of pancreatic juice when food enters the stomach is known as gastric phase. This phase of pancreatic secretion is under hormonal control. The hormone involved is gastrin. When food enters the stomach, gastrin is secreted from stomach. When gastrin is transported to pancreas through blood, it stimulates the pancreatic secretion. The pancreatic juice secreted during gastric phase is rich in enzymes. 3. INTESTINAL PHASE Intestinal phase is the secretion of pancreatic juice when the chyme enters the intestine. This phase is also under hormonal control. When chyme enters the intestine, many hormones are released. Some hormones stimulate the pancreatic secretion and some hormones inhibit the pancreatic secretion. APPLIED PHYSIOLOGY a. PANCREATITIS Pancreatitis is the inflammation of pancreatic acini. It is a rare but dangerous disease. Pancreatitis is of two types: 1. Acute pancreatitis 2. Chronic pancreatitis. 1. Acute Pancreatitis Acute pancreatitis is more severe and it occurs because of heavy alcohol intake or gallstones. Features of acute pancreatitis: i. Severe upper abdominal pain ii. Nausea and vomiting iii. Loss of appetite and weight iv. Fever v. Shock. By Mr. C. A. MBAH Page 20 21 2. Chronic Pancreatitis Chronic pancreatitis develops due to repeated acute inflammation or chronic damage to pancreas. Causes of chronic pancreatitis i. Longtime consumption of alcohol ii. Chronic obstruction of ampulla of Vater by gallstone iii. Hereditary cause (passed on genetically from one generation to another) iv. Congenital abnormalities of pancreatic duct v. Cystic fibrosis is a generalized disorder affecting the functions of many organs such as lungs (due to excessive mucus), exocrine glands like pancreas, biliary system and immune system vi. Malnutrition (poor nutrition; mal = bad) vii. Idiopathic pancreatitis (due to unknown cause). STEATORRHEA: Steatorrhea is the formation of bulky, foul smelling, frothy and clay colored stools with large quantity of undigested fat because of impaired digestion and absorption of fat. Causes of Steatorrhea Any condition that causes indigestion or malabsorption of fat leads to steatorrhea. Various causes of steatorrhea are: 1. Lack of pancreatic lipase: Since most of the fat is digested only by pancreatic lipase, its deficiency leads to steatorrhea 2. Liver disease affecting secretion of bile: Bile salts are essential for the digestion of fat by lipase and absorption of fat from intestine. Absence of bile salts results in excretion of fatty stool 3. Celiac disease: Atrophy of intestinal villi leads to malabsorption, resulting in steatorrhea 4. Cystic fibrosis (2) LIVER: The liver is the largest gland in the body, weighing between 1 and 2.3 kg. it is situated in the upper part of the abdominal cavity occupying the grater part of the right hypochondriac region. The liver is enclosed in a thin inelastic capsule and incompletely covered by a layer of peritoneum. The liver has four lobes. The two most are the large right lobe and the smaller, wedge-shaped, left lobe. The other two, the caudate and quadrate lobes, an areas on the posterior surface. THE PORTAL FISSURE. This is the name given to the region on the posterior surface of the liver where various structures enter and leave the gland. The portal vein enters, carrying blood from the stomach, spleen, pancreas and the small and the large intestine. The hepatic artery enters, carrying arterial blood. Nerve fibres (sympathetic and parasympathetic). The right and left hepatic ducts leave, carrying bile from the liver to the gall bladder. Lymph vessels leave the liver, draining some lymph to abdominal and some to thoracic nodes. Fig. 1.6: structure of the liver STRUCTURE OF THE LIVER The lobes of the liver are made up of tiny functional units, called lobules, which are just visible to the pasted eye. Liver lobules are hexagonal in outline and formed by cubical-shaped cells, the hepatocytes, arranged in pairs of columns radiating from a central vein. Between two pairs of columns of cells are sinusoids containing By Mr. C. A. MBAH Page 21 22 mixure of blood from the tiny branches of the portal vein and hepatic artery. This arrangement allows the arterial blood and portal venous blood to mix and come in to close contact with liver cells. Cells lining sinusoids are hepatic macrophages (Kupper cells). Blood drains from the sinusoids into central or centrilobular veins. These then join with veins from other lobules, forming larger veins, until eventually they become the hepatic veins, which leave the liver and empty into the inferior vena cava. Fig. 1.7: Histology of liver Functions of the liver The various functions of the liver are carried out by the liver cells or hepatocytes. Currently, there is no artificial organ or device capable of emulating all the factions of the liver. Some functions can be emulated by liver dialysis, an experimental treatment for liver failure. Synthesis Further information: Proteins produced and secreted by the liver o A large part of amino acid synthesis o The liver performs several roles in carbohydrate metabolism: o Gluconeogenesis (the synthesis of glucose from certain amino acids, lactate or glycerol) o Glycogenolysis (the breakdown of glycogen into glucose) o Glycogenesis (the formation of glycogen from glucose) (muscle tissues can also do this) o The liver is responsible for the mainstay of protein metabolism, synthesis as well as degradation o The liver also performs several roles in lipid metabolism: o Cholesterol synthesis o Lipogenesis, the production of triglycerides (fats). o The liver produces coagulation factors I (fibrinogen), II (prothrombin), V, VII, IX, X and XI, as well as protein C, protein Sand antithrombin. o In the first three months foetus, the liver is the main site of red blood cell production. By the 32nd week of gestation, the bone marrow has almost completely taken over that task. o The liver produces and excretes bile (a greenish liquid) required for emulsifying fats. Some of the bile drains directly into the duodenum, and some is stored in the gallbladder. o The liver also produces insulin-like growth factor 1 (IGF-1), a polypeptide protein hormone that plays an important role in childhood growth and continues to have anabolic effects in adults. o The liver is a major site of thrombopoietin production. Thrombopoietin is a glycoprotein hormone that regulates the production of platelets by the bone marrow. Breakdown o The breakdown of insulin and other hormones o The liver breaks down hemoglobin, creating metabolites that are added to bile as pigment (bili-rubin and biliverdin). o The liver breaks down toxic substances and most medicinal products in a process called drug metabolism. This sometimes results intoxication, when the metabolite is more toxic than its precursor. Preferably, the toxins are conjugated to avail excretion in bile or urine. By Mr. C. A. MBAH Page 22 23 o The liver converts ammonia to urea. Other Functions o The liver stores a multitude of substances, including glucose (in the form of glycogen), vitamin o A (1-2 years' supply), vitamin D (1-4 months' supply), vitamin B12, iron, and copper. o The liver is responsible for immunological effects- the reticuloendothelial system of the liver contains many immunologically active cells, acting as a 'sieve' for antigens carried to it via the portal system. The liver produces albumin, the major osmolar component of blood serum. (3) Gall Bladder: The gallbladder is a dark green sac, shaped like a blackjack and lodged in a hollow on the underside of the liver. Its ducts join with the duct of the liver to conduct bile to the upper end of the small intestine. The main function of the gallbladder is the storage and concentration of the bile when it is not needed for digestion. In adults, the gallbladder measures approximately 10 cm in length and 4 cm in diameter when fully distended. It is divided into three sections: fundus, body, and neck. The neck tapers and connects to the biliary tree via the cystic duct, which then joins the common hepatic duct to become the common bile duct. Fig.1.9: The Gall bladder Microscopic Anatomy of the Gallbladder The different layers of the gallbladder are as follows: The gallbladder has a simple columnar epithelial lining characterized by recesses called As. choff's recesses, which are pouches inside the lining. Under the epithelium there is a layer of connective tissue (lamina propria). Beneath the connective tissue is a wall of smooth muscle (muscularis externa) that contracts in response to cholecystokinin, a peptide hormone secreted by the duodenum. There is essentially no submucosa separating the connective tissue from serosa and adventitia, but there is a thin lining of muscular tissue to prevent infection. Functions of the Gallbladder a. The gallbladder stores about 50 ml. (1.7 US Aluid ounces / 1.8 Imperial fuid ounces) of bile, which is released when food containing fat enters the digestive tract, stimulating the secretion of cholecystokinin (CCK). The bile, produced in the liver, emulsifies fats and neutralizes acids in partly digested food. b. After being stored in the gallbladder the bile becomes more concentrated than when it lef the fiver, increasing its potency and intensifying its effect on fats. Most digestion occurs in the duodenum. c. Concentration of bile by upto 10-or15- fold, by absorbing water. Bile: Bile or gall is a bitter yellow, blue and green fluid secreted by hepatocytes from the liver of most ver. sales. In many species, bile is stored in the gallbladder between meals and upon eating is discharged so the duodenum where the bile aids the process of digestion of lipids by emulsification. About 500 ml of bile are secreted by the liver daily. Bile consists of Water Mineral salts By Mr. C. A. MBAH Page 23 24 Mucus Bile pigments (bilirubin) Bile salts (salts cholic acids and chenodoxycholic acid) Phospholipids (lecithin) Cholesterol Secretion Bile is produced by hepatocytes in the liver, draining through the many bile ducts that penetrate the Iver. During this process, the epithelial cells add a watery solution that is rich in bicarbonates that di-wes and increases alkalinity of the solution. Bile then flows into the common hepatic duct, which joins with the cystic duct from the gallbladder to form the common bile duct. The common bile duct in turn joins with the pancreatic duct to empty into the duodenum. If the sphincter of Oddi is closed, bile is prevented from draining into the intestine and instead flows into the gallbladder, where it is stored and concentrated to up to five times its original potency between meals. This concentration occurs through de absorption of water and small electrolytes, while retaining all the original organic molecules. Cho-listerol is also released with the bile, dissolved in the acids and fats found in the concentrated solution. When food is released by the stomach into the duodenum in the form of chyme, the duodenum releases cholecystokinin, which causes the gallbladder to release the concentrated bile to complete digestion. The human liver can produce close to one litre of bile per day (depending on body size). 95% of the salts secreted in bile are reabsorbed in the terminal ileum and re-used. Blood from the ileum flows Girectly to the hepatic portal vein and returns to the liver where the hepatocytes reabsorb the salts and refum them to the bile ducts to be re-used, sometimes two to three times with each meal. Functions of the Bile: a. The bile salts emulsify fats in the small intestine. b. Fatty acids are insoluble in water, which makes cholesterol and fatty acids soluble and also fat soluble vitamins for absorption. c. The bile pigment, bilirubin, is a waste product of the breakdown of erythrocytes and is excreted in the bile rather than in the urine because of its low solubility in water. d. Stercobilin colours and deodorizes the faces By Mr. C. A. MBAH Page 24 25 Digestive enzymes of different secretion from different glands Saliva (salivary glands) Salivary amylase Lingual lipase Gastric juice (gastric glands) Pepsin Gastric lipase Pancreatic juice (pancreas) Pancreatic amylase Trypsin Chymotrypsin Elastase Carbosypeptidaase Pancreatic lipase Nacleases (ribonucleases, deoxyribonuclease) Brush border enzymes (small intestine) Alpha-dextrinase Maltase Sucrase Lactase Enterokinase Peptidases (Aminopeptidase, dipeptidase) Nucleosidases(small intestine) Phosphatases (small intestine) LARGE INTESTINE (COLON) The large intestine is the last part of the digestive system--the final stage of the alimentary canal--in vertebrate animals. Its function is to absorb water from the remaining indigestible food matter, and then to pass useless waste material from the body. It consists of the caecum and colon. It starts in the right iliac region of the pelvis, just at or below the right waist, where it is joined to the bottom end of the small intestine. From here it continues up the abdomen, then across the width of the abdominal cavity, and then it turns down, continuing to its endpoint at the anus called the intestinal canal. The large intestine is about 1.5 metres (4.9 f) long, which is about one-fifth of the whole length of the intestinal canal. NB: a. The large intestine is about 5 feet long. b. The cecum, located on the lower right side of the abdomen, is the first portion of the large intestine into which food is emptied from the small intestine. c. The appendix extends from the lower portion of the cecum and is a blind sac. Although the appendix usually is found lying just below the cecum, by virtue of its free end it can extend in several different directions, depending upon its mobility. By Mr. C. A. MBAH Page 25 26 b. The colon extends along the right side of the abdomen from the cecum up to the region of the liver (ascending colon). There the colon bends (hepatic flexure) and is continued across the upper portion of the abdomen (transverse colon) to the spleen. The colon bends again (splenic flexure) and goes down the left side of the abdomen (descending colon). The last portion makes an S curve (sigmoid) toward the center and posterior of the abdomen and ends in the rectum. c. The main function of the large intestine is the recovery of water and electrolytes from the mass of undigested food it receives from the small intestine. As this mass passes through the colon, water is absorbed and returned to the tissues. Waste materials, or feces, become more solid as they are pushed along by peristaltic movements. Constipation is caused by delay in movement of intestinal contents and removal of too much water from them. Diarrhea results when movement of the intestinal contents is so rapid that not enough water is removed THE RECTUM AND ANUS The rectum is about 5 inches long and follows the curve of the sacrum and coccyx until it bends back into the short anal canal. The anus is the external opening at the lower end of the digestive system. It is kept closed by a strong sphincter muscle. The rectum receives feces and periodically expels this material through the anus. This elimination of refuse is called defecation. DIGESTION Digestion is the process whereby food is broken down into smaller parts, chemically changed, and moved through the gastrointestinal system. The gastrointestinal (GI) tract consists of the body structures that participate in digestion. Digestion begins in the mouth and ends at the anus. Along the entire GI tract secretions of mucus lubricate and protect the mucosal tissues. Digestion occurs through two types of action—mechanical and chemical. During mechanical digestion, food is broken into smaller pieces by the teeth. It is then moved along the gastrointestinal tract through the esophagus, stomach, and intestines. This movement is caused by a rhythmic contraction of the muscular walls of the tract called peristalsis. Mechanical digestion helps to prepare food for chemical digestion by breaking it into smaller pieces. Several small pieces collectively have more surface area than fewer large ones and thus are more readily broken down by digestive juices. Mechanical digestion is the part of digestion that requires certain mechanical movements such as chewing, swallowing, and peristalsis. During chemical digestion, the composition of carbohydrates, proteins, and fats is changed. Chemical changes occur through the addition of water and the resulting splitting, or breaking down, of the food molecules. This process is called hydrolysis. Food is broken down into nutrients that the tissues can absorb and use. Hydrolysis also involves digestive enzymes that act on food substances, causing them to break down into simple compounds. An enzyme can also act as a catalyst, which speeds up the chemical reactions without itself being changed in the process. Digestive enzymes are secreted by the mouth, stomach, pancreas, and small intestine. An enzyme is often named for the substance on which it acts. For example, the enzyme sucrase acts on sucrose, the enzyme maltase acts on maltose, and lactase acts on lactose. Digestion in the Mouth Digestion begins in the mouth, where the food is broken into smaller pieces by the teeth and mixed with saliva. At this point, each mouthful of food that is ready to be swallowed is called a bolus. Saliva is a secretion of the salivary glands that contains water, salts, and a digestive enzyme called salivary amylase (also called ptyalin), which acts on complex carbohydrates (starch). Food is normally held in the mouth for such a short time that only small amounts of carbohydrates are chemically changed there. The salivary glands also secrete a mucous material that lubricates and binds food particles to help in swallowing the bolus. The final chemical digestion of carbohydrates occurs in the small intestine. Digestion and Absorption In the mouth, salivary amylase converts starch (polysaccharide) to maltose (a disaccharide), maltotri-ose (a trisaccharide) and alpha-dextrins (short chain, branched, fragments of starch with 5 to 10 glucose units). In the stomach pepsin converts proteins to peptides (small fragments of proteins), and lingual and gastric lipases converts some triglycerides in to fatty acids, diglycerides and monoglycerides. Thus, chyme entering the small intestine contains partially digested carbohydrates, proteins and lipids By Mr. C. A. MBAH Page 26 27 Digestion of Carbohydrates The action of salivary amylase may continue in the stomach for a while, the acidic pH of the stomach destroys salivary amylase and ends its activity. Thus, only a few starches are broken down by the time chime leaves the stomach. Those starches not already broken down into maltose, maltotriose, and alpha-dextrins are cleaved by pancreatic amylase (an enzyme in pancreatic juice that acts in the small intestine). It acts on both glycogen and starches and not on polysaccharides (cellulose). After amylase, alpha-dextrinase (brush border enzyme) splits the alpha-dextrins. Ingested molecules of sucrose, lactose and maltose (three disaccharides) are not acted on until they reach the small in testine. Three brush border enzymes digest the disaccharides in to monosaccharides. Sucrase breaks sucrose into a molecule of glucose and a molecule of fructose, lactase digests lactose into a molecule of glucose and a molecule of galactose, and maltase splits maltose and maltotriose into two or three molecules of glucose, respectively. Digestion of carbohydrates ends with the production of monosac-charides, which the digestive system is able to absorb. Absorption of Carbohydrates: All carbohydrates are absorbed as monosaccharides. All dietary carbohydrates that are digested nor. mally are absorbed, leaving only indigestible cellulose and fibers in the feces. Monosaccharides pass from the lumen through the apical membrane via facilitated diffusion or active transport. Fructose (monosaccharide from fruits) is transported by facilitated diffusion. Glucose and galactose are transported by secondary active transport that is coupled to the active transport of Na* Monosaccarides then move out of the absorptive cells through their basolateral surfaces via facilitated diffusion and enters the capillaries of the villi. Digestion of Proteins: Digestion of proteins starts in the stomach, where proteins are fragmented into peptides by the action of pepsin. Enzymes in pancreatic juice -trypsin, chymotrypsin, carboxypeptidase, and elastase continue to break down proteins into peptides (all enzymes converts proteins into peptides) Trypsin, chymotrypsin, and elastase all cleave the peptide bond between a specific amino acid and its neighbour. Carboxypeptidase's splits off the amino acid at the carboxyl end of a peptide. Protein digestion is completed by two peptidases in brush border: aminopeptidase and dipeptidase. Aminopeptidase cleaves amino acid at the amino end of peptide. Dipeptidase splits dipeptides (two amino acids joined by a peptide bond) in to single amino acids. Absorption of Amino acids, Dipeptides and Tripeptides: Most proteins are absorbed as amino acids via active transport process that occur mainly in the duodenum and jejunum. About 95-98% of the protein present in the small intestine is digested and absorbed. Amino acids transported into the absorptive cells by active transport/secondary active transport with Na* and in to villi by diffusion. Dipeptides and tripeptides transported in to the absorptive cells by secondary active transport with H* (hydrolyzed to single amino acids) and into villus by diffusion. Digestion of Lipids The most abundant lipids in the diet are triglycerides, which consist of a molecule of glycerol bonded to three fatty acid molecules. Enzymes that split triglycerides and phospholipids are called lipases. Three types of lipase that can involve in lipid digestion. Lingual lipase (sublingual glands) Gastric lipase (stomach) Pancreatic lipase (pancreatic juice) Some of lipids digestion occurs in stomach through the action of lingual and gastric lipases, most occurs in the small intestine through the action of pancreatic lipase. Triglycerides are broken down by pancreatic lipase in to fatty acids and monoglycerides. The liberated fatty acids can be either short-chain fatty acids or long chain fatty acids. Large lipid globules containing triglycerides can be digested in the small intestine, it must undergo emulsification (process in which large lipid globule is broken down into several small lipid globules) by bile salts (Na* and K* salts of bile acids). Large lipid globule is broken in to several small lipid globules (each is about Ium in diameter) and increase larger surface of the globules that allows pancreatic lipase to act. By Mr. C. A. MBAH Page 27 28 Absorption of Lipids: All dietary lipids are absorbed via simple diffusion, Emulsification and digestion, triglycerides are mainly broken down in to monoglycerides and fatty acids, which can be either short/long, chain fatty acids. Short chain fatty acids: are hydrophobic, they are very small in size, because of their size they dissolve in the watery intestinal chyme; pass trouet tie absorplive cells via simple difusion. Long chain fatty acids and monoglycerides are large and hydrophobic and have difficulty in dissol. ing in watery environment. Bromoteeries writh bile salts help to make these long chain fatty acid, and monoglycerides more soluble. Bile salts surround the long chain fatty acids and monoglycerides forming tiny spheres called micelles (2-ihim in diameter). Then micelle transport to absorptive cells by simple diftusion. In absorptive cells, long chain fatty acids and monoglycerides are recombined to form triglycerides, which aggregate into globules along with phospholipids and cholesterol and be Come coated with proteins (80hm diameter) to form chylomicrons. Chylomicrons leave the absorptive cell via exocytosis and enters in to lacteal of villi: Absorption of the majority of nutrients takes place in the jejunum, with the following notable exceptions: o Iron is absorbed in the duodenum. o Vitamin B12 and bile salts are absorbed in the terminat ileum. o Water and lipids are absorbed by passive diffusion throughout the small intestine. o Sodium is absorbed by active transport and glucose and amino acid co-transport. o Fructose is absorbed by facilitated diffusion. The Esophagus The esophagus is a 10-inch muscular tube through which food travels from the mouth to the stomach. When swallowed, the bolus of food is moved down the esophagus by peristalsis and gravity. At the lower end of the esophagus, the cardiac sphincter opens to allow passage of the bolus into the stomach. The cardiac sphincter prevents the acidic content of the stomach from flowing back into the esophagus. When this sphincter malfunctions, it causes acid reflux disease. Digestion in the Stomach The stomach consists of an upper portion known as the fundus, a middle area known as the body of the stomach, and the end nearest the small intestine called the pylorus. Food enters the fundus and moves to the body of the stomach, where the muscles in the stomach wall gradually knead the food, tear it, and mix it with gastric juices, and with the intrinsic factor necessary for the absorption of vitamin B12, before it can be propelled forward in slow, controlled movements. The food becomes a semiliquid mass called chyme (pronounced “kime”). When the chyme enters the pylorus, it causes distention and the release of the hormone gastrin, which increases the release of gastric juices. Gastric juices are digestive secretions of the stomach. They contain hydrochloric acid, pepsin, and mucus. Hydrochloric acid activates the enzyme pepsin, prepares protein molecules for partial digestion by pepsin, destroys most bacteria in the food ingested, and makes iron and calcium more soluble. As the hydrochloric acid is released, thick mucus is also secreted to protect the stomach from this harsh acid. In children, there are two additional enzymes: rennin, which acts on milk protein and casein, and gastric lipase, which breaks the butterfat molecules of milk into smaller molecules. The functions of the stomach include the following: 1. Temporary storage of food 2. Mixing of food with gastric juices 3. Regulation of a slow, controlled emptying of food into the intestine 4. Secretion of the intrinsic factor for vitamin B12 5. Destruction of most bacteria inadvertently consumed THE PARIETAL CELL: MECHANISM OF ACID SECRETION The best-known component of gastric juice is hydrochloric acid, the secretory product of the parietal, or oxyntic cell. It is known that the capacity of the stomach to secrete HCl is almost linearly related to parietal cell numbers. When stimulated, parietal cells secrete HCl at a concentration of roughly 160 mM (equivalent to a pH of 0.8). The acid is secreted into large cannaliculi, deep invaginations of the plasma membrane which are continuous with the lumen of the stomach. By Mr. C. A. MBAH Page 28 29 When acid secretion is stimulated there is a dramatic change in the morphology of the membranes of the parietal cell. Cytoplasmic tubulovesicular membranes which are abundant in the resting cell virtually disappear in concert with a large increase in the cannalicular membrane. It appears that the proton pump as well as potassium and chloride conductance channels initially reside on intracellular membranes and are transported to and fused into the cannalicular membrane just prior to acid secretion. The epithelium of the stomach is intrinsically resistant to the damaging effects of gastric acid and other insults. Nonetheless, excessive secretion of gastric acid is a major problem in human and, to a lesser extent, animal populations, leading to gastritis, gastric ulcers and peptic acid disease. As a consequence, the parietal cell and the mechanisms it uses to secrete acid have been studied extensively, leading to development of several drugs useful for suppressing acid secretion. Mechanism of Acid Secretion The hydrogen ion concentration in parietal cell secretions is roughly 3 million fold higher than in blood, and chloride is secreted against both a concentration and electric gradient. Thus, the ability of the partietal cell to secrete acid is dependent on active transport. The key player in acid secretion is a H+/K+ ATPase or "proton pump" located in the cannalicular membrane. This ATPase is magnesium-dependent, and not inhibitable by ouabain. The current model for explaining acid secretion is as follows: Hydrogen ions are generated within the parietal cell from dissociation of water. The hydroxyl ions formed in this process rapidly combine with carbon dioxide to form bicarbonate ion, a reaction cataylzed by carbonic anhydrase. Bicarbonate is transported out of the basolateral membrane in exchange for chloride. The outflow of bicarbonate into blood results in a slight elevation of blood pH known as the "alkaline tide". This process serves to maintain intracellular pH in the parietal cell. Chloride and potassium ions are transported into the lumen of the cannaliculus by conductance channels, and such is necessary for secretion of acid. Hydrogen ion is pumped out of the cell, into the lumen, in exchange for potassium through the action of the proton pump; potassium is thus effectively recycled. Accumulation of osmotically-active hydrogen ion in the cannaliculus generates an osmotic gradient across the membrane that results in outward diffusion of water - the resulting gastric juice is 155 mM HCl and 15 mM KCl with a small amount of NaCl. A key substrate in the production of gastric acid is CO2, and diffusion of CO2 through the basal surface of the parietal appears to be the rate limiting step in acid synthesis. Interestingly, this biochemical principle has been validated by studying gastric function in alligators. These reptiles produce huge amounts of gastric acid after ingestion of a large carcass, and abundant acid seems to be important in speeding digestion of bone. Alligators have a vascular shunt that diverts CO2-rich venous blood to the stomach rather than directly back to the lungs, increasing the amount of CO2 that diffuses into parietal cells and thereby enhancing synthesis of acid. Control of Acid Secretion Parietal cells bear receptors for three stimulators of acid secretion, reflecting a triumverate of neural, paracrine and endocrine control: Acetylcholine (muscarinic type receptor) Gastrin Histamine (H2 type receptor) Histamine from enterochromaffin-like cells may well be the primary modulator, but the magnitude of the stimulus appears to result from a complex additive or multiplicative interaction of signals of each type. For example, the low amounts of histamine released constantly from mast cells in the gastric mucosa only weakly stimulate acid secretion, and similarly for low levels of gastrin or acetylcholine. However, when low levels of each are present, acid secretion is strongly forced. Additionally, pharmacologic antagonists of each of these molecules can block acid secretion. Histamine's effect on the parietal cell is to activate adenylate cyclase, leading to elevation of intracellular cyclic AMP concentrations and activation of protein kinase A (PKA). One effect of PKA activation is phosphorylation of cytoskeletal proteins involved in transport of the H+/K+ ATPase from cytoplasm to plasma membrane. Binding of acetylcholine and gastrin both result in elevation of intracellular calcium concentrations. By Mr. C. A. MBAH Page 29 30 Several additional mediators have been shown to result in gastric acid secretion when infused into animals and people, including calcium, enkephalin and bombesin. Calcium and bombesin both simulate gastrin release, while opiate receptors have been identified on parietal cells. It is unclear whether these molecules have a significant physiologic role in parietal cell function. A variety of substances are capable of reducing gastric acid secretion when infused intravenously, including prostaglandin E2 and several peptides hormones, including secretin, gastric inhibitory peptide, glucagon and somatostatin. PGE2, secretin and somatostatin may be physiologic regulators. Somatostatin inhibits secretion of gastrin and histamine, and appears to have a direct inhibitory effect on the parietal cell. Digestion in the Small Intestine Chyme moves through the pyloric sphincter into the duodenum, the first section of the small intestine. Chyme subsequently passes through the jejunum, the midsection of the small intestine, and the ileum, the last section of the small intestine. When food reaches the small intestine, the hormone secretin causes the pancreas to release sodium bicarbonate to neutralize the acidity of the chyme. The gallbladder is triggered by the hormone cholecystokinin (CCK), which is produced by intestinal mucosal glands when fat enters, to release bile. Bile is produced in the liver but stored in the gallbladder. Bile emulsifies fat after it is secreted into the small intestine. This action enables the enzymes to digest the fats more easily. Chyme also triggers the pancreas to secrete its juice into the small intestine. Pancreatic juice contains the following enzymes: 1. Trypsin, chymotrypsin, and carboxypeptidases split proteins into smaller substances. These are called pancreatic proteases because they are protein-splitting enzymes produced by the pancreas. 2. Pancreatic amylase converts starches (polysaccharides) to simple sugars. 3. Pancreatic lipase reduces fats to fatty acids and glycerol. The small intestine itself produces an intestinal juice that contains the enzymes lactase, maltase, and sucrase. These enzymes split lactose, maltose, and sucrose, respectively, into simple sugars. The small intestine also produces enzymes called peptidases that break down proteins into amino acids. THE LARGE INTESTINE The large intestine, or colon, consists of the cecum, colon, and rectum. The cecum is a blind pouch-like beginning of the colon in the right lower quadrant of the abdomen. The appendix is a diverticulum that extends off the cecum. The cecum is separated from the ileum by the ileocecal valve and is considered to be the beginning of the large intestine (colon). Its primary function is to absorb water and salts from undigested food. It has a muscular wall that can knead the contents to enhance absorption. One of the end products of fermentation in the cecum is volatile fatty acids. The major volatile fatty acids are acetate, propionate, and butyrate. These are absorbed from the large intestine and used as sources of energy. The digested food then enters the ascending colon and moves through the transverse colon and on to the descending colon, the sigmoid colon, the rectum, and, finally, the anal canal. ABSORPTION After digestion, the next major step in the body’s use of its food is absorption. Absorption is the passage of nutrients into the blood or lymphatic system (the lymphatic vessels carry fat-soluble particles and molecules that are too large to pass through the capillaries into the bloodstream). To be absorbed, nutrients must be in their simplest forms. Carbohydrates must be broken down to the simple sugars (glucose, fructose, and galactose), proteins to amino acids, and fats to fatty acids and glycerol. Most absorption of nutrients occurs in the small intestine, although some occurs in the large intestine. Water is absorbed in the stomach, small intestine, and large intestine. ABSORPTION IN THE SMALL INTESTINE The small intestine is approximately 22 feet long. Its inner surface has mucosal folds, villi, and microvilli to increase the surface area for maximum absorption. The fingerlike projections called villi have hundreds of microscopic, hair like projections called microvilli. The microvilli are very sensitive to the nutrient needs of our bodies. Each villus contains numerous blood capillaries (tiny blood vessels) and lacteals (lymphatic vessels). The villi absorb nutrients from the chyme by way of these blood capillaries and lacteals, which eventually transfer them to the bloodstream. Glucose, fructose, galactose, amino acids, minerals, and water-soluble vitamins are absorbed by the capillaries. Fructose and galactose are subsequently carried to the liver, where they By Mr. C. A. MBAH Page 30 31 are converted to glucose. Lacteals absorb glycerol and fatty acids (end products of fat digestion) in addition to the fat-soluble vitamins. ABSORPTION IN THE LARGE INTESTINE When the chyme reaches the large intestine, most digestion and absorption have already occurred. The colon walls secrete mucus as a protection from the acidic digestive juices in the chyme, which is coming from the small intestine through the ileocecal valve. The major tasks of the large intestine are to absorb water, to synthesize some B vitamins and vitamin K (essential for blood clotting), and to collect food residue. Food residue is the part of food that the body’s enzyme action cannot digest and consequently the body cannot absorb. Such residue is commonly called dietary fiber. Examples include the outer hulls of corn kernels and grains of wheat, celery strings, and apple skins. It is important that the diet contain adequate fiber because it promotes the health of the large intestine by helping to produce softer stools and more frequent bowel movements. Undigested food is excreted as feces by way of the rectum. In healthy people, 99% of carbohydrates, 95% of fat, and 92% of proteins are absorbed. PHYSIOLOGY OF DEFAECATION Propulsion of the Residue and Defecation: When presented with residue, the colon becomes mobile, but its contractions are sluggish or short-lived Haustral contractions: The movements most seen in the colon are haustral contractions, slow segmenting movements lasting about one minute that occur every 30 minutes or so. Propulsion: As the haustrum fills with food residue, the distension stimulates its muscle to contract, which propels the luminal contents into the next haustrum. Mass movements: Mass movements are long, slow-moving, but powerful contractile waves that move over large areas of the colon three or four times daily and force the contents toward the rectum. Rectum: The rectum is generally empty, but when feces are forced into it by mass movements and its wall is stretched, the defecation reflex is initiated. Defecation reflex: The defecation reflex is a spinal (sacral region) reflex that causes the walls of the sigmoid colon and the rectum to contract and anal sphincters to relax. Impulses: As the feces is forced into the anal canal, messages reach the brain giving us time to make a decision as to whether the external voluntary sphincter should remain open or be constricted to stop passage of feces. Relaxation: Within a few seconds, the reflex contractions end and rectal walls relax; with the next mass movement, the defecation reflex is initiated again. TIME REQUIRED FOR DIGESTION Within a few minutes after a meal reaches the stomach, it begins to pass through the lower valve of the stomach. After the first hour the stomach is half-empty, and at the end of the sixth hour none of the meal is present in the stomach. The meal goes through the small intestine, and the first part of it reaches the cecum in 20 minutes to 2 hours. At the end of the sixth hour, most of it should have passed into the colon; in 12 hours, all should be in the colon. Twenty-four hours from the time when food is eaten, the meal should reach the rectum. However, part of a meal may be defecated at one time and the rest at another. CLINICALS GASTROINTESTINAL DISORDERS GASTRITIS/GASTROENTERITIS a. Acute gastritis is the irritation and inflammation of the stomach's mucous lining. Gastritis may be caused by a chemical, thermal, or bacterial insult. For example, drugs such as alcohol, aspirin, and chemotherapeutic agents may cause an attack of gastritis. Likewise, hot, spicy, rough, or contaminated foods may bring about an attack. Management involves symptomatic treatment measures after removal of the causative agent. b. Gastroenteritis, or inflammation of the stomach and intestines, is generally caused by bacteria and viruses. Other causes include parasites, food allergens, drug reactions to antibiotics, and ingestion of toxic plants. Treatment is the same as for gastritis, with the addition of anti-microbial drugs for severe cases. By Mr. C. A. MBAH Page 31 32 1. c. Signs and symptoms of both include pain, cramping, belching, nausea, and vomiting. Severe cases may include hematemesis. Diarrhea may occur with gastroenteritis. GASTROINTESTINAL ULCERS a. A gastrointestinal ulcer is a break in the continuity of the mucous lining. Ulcers may occur in any part of the GI tract that comes in contact with the gastric juices. Ulcers commonly occur in the lower esophagus, the stomach, and the duodenum. b. In addition to mucosal deterioration by hydrochloric acid and pepsin secretion, other factors may be implicated in the development of ulcers. (1) Emotional stress. (2) Prolonged physical stress associated with trauma, surgery, burns, and so forth. (3) Hereditary factors. (4) Certain drugs and medications. For example: alcohol, caffeine, aspirin, corticosteroids, and chemotherapeutic agents. APPENDICITIS a. Definition. Appendicitis is the inflammation of the vermiform appendix. The appendix fills with food and empties regularly. Because its lumen is quite small, it empties irregularly and is prone to obstruction. The obstruction sets off an inflammatory process that may lead to infection, necrosis, and perforation. b. Signs and Symptoms. (1) Generalized abdominal pain that localizes in the right lower quadrant. (2) Anorexia. (3) Nausea and vomiting. (4) Abdominal rigidity or guarding. (5) Rebound tenderness. (6) Fever. (7) Elevated white blood cell count. Treatment. Treatment of choice is surgical removal of the appendix, especially if rupture is suspected or imminent. (1) If the appendix can be removed before it ruptures, the post-op course is generally uncomplicated. The wound is closed and the patient is usually discharged within a week. (2) If rupture has occurred, the wound is often left open to drain. The patient must be observed for signs and symptoms of obstruction, peritonitis, hemorrhage, or abscess. PERITONITIS a. The peritoneum is the serous membrane that lines the abdominal cavity and covers the visceral organs. Peritonitis is inflammation of the peritoneum. Inflammation may be generalized throughout the peritoneum, affecting the visceral and parietal surfaces of the abdominal cavity, or may be localized in one area as an abscess. b. Peritonitis occurs as a result of leakage of contents from an abdominal organ into the abdominal cavity. Generally, this disorder results from perforation of the GI tract, allowing bacterial contamination of the peritoneum. Peritonitis may also occur as a result of chemical irritation, and subsequent infection, caused by rupture of an organ. (For example, the ovaries, spleen, or urinary bladder.) c. Signs and symptoms. (1) Diffuse pain that eventually localizes in the area of the underlying process. (2) Abdominal tenderness. (3) Abdominal muscle rigidity. (4) Rebound tenderness. (5) Nausea and vomiting (6) Paralytic ileus. (7) Fever. (8) Rapid pulse rate. (9) Elevated WBC. By Mr. C. A. MBAH Page 32 33 INTESTINAL OBSTRUCTION a. Intestinal obstruction is defined as any hindrance to the passage of intestinal contents through the small and/or large bowel. Obstruction may be partial or complete. Severity depends upon the area of bowel affected, the degree of blockage, and the degree of vascular impairment. b. Intestinal obstruction is divided into two basic categories: mechanical and non-mechanical. (1) Mechanical obstruction results from obstruction within the lumen of the intestine or mural obstruction from pressure on the walls of the intestines. Causes include: (a) Foreign bodies such as fruit pits, parasitic worms, or gallstones. (b) Volvulus. (c) Intussusception. (d) Hernia. (e) Cancer. DIVERTICULAR DISEASE a. Definition. Diverticula are bulging dilatations or "out-pouchings" of the gastrointestinal walls. Common sites are the sigmoid colon, duodenum, and the distal ileum. However, diverticula can occur anywhere along the GI tract, from the esophagus to the anus. b. Diverticulosis. The presence of asymptomatic diverticula is called diverticulosis. Diverticulosis is sometimes the source of LLQ pain that is relieved by defecation or flatulence. Constipation or diarrhea may also occur. Diverticulosis generally requires no treatment other than dietary modification to prevent irritation of the bowel. c. Diverticulitis. When diverticula become inflamed or infected, the condition is referred to as diverticulitis. Food and bacteria lodge and harden in the diverticular sac. Inflammation results, followed by infection. Complications include abscess, obstruction, perforation, peritonitis, and hemorrhage. (1) Symptoms include low grade fever, nausea, gas, abdominal pain, and abdominal rigidity. DEFECATION The passage or Voiding of feces is called defecation. It is begun voluntarily by contraction of the abdominal muscles. At the same time, the sphincter muscles of the anus relax, and there is a peristaltic contraction wave of the colon and rectum. Feces are expelled as a result of all these actions. Feces consist of undigested food residue, secretions from the digestive glands, bile, mucus, and millions of bacteria. Mucus is derived from the many mucous glands that pour secretions into the intestine. Bacteria are especially numerous in the large intestine. They act upon food material, causing putrefaction of proteins and fermentation of carbohydrates. Although the bacteria normally in the large intestine serve a useful purpose internally, they are contaminants outside the intestine. NB: Feces is formed in the large intestine and stored in sigmoid colon. By the influence of an appropriate stimulus, it is expelled out through the anus. This is prevented by tonic constriction of anal sphincters, in the absence of the stimulus Mass movement drives the feces into sigmoid or pelvic colon. In the sigmoid colon, the feces is stored. The desire for defecation occurs when some feces enters rectum due to the mass movement. Usually, the desire for defecation is elicited by an increase in the intrarectal pressure to about 20 to 25 cm H2O. Usual stimulus for defecation is intake of liquid like coffee or tea or water. But it differs from person to person. MECHANISM OF DEFECATION Act of defecation is preceded by voluntary efforts like assuming an appropriate posture, voluntary relaxation of external sphincter and the compression of abdominal contents by voluntary contraction of abdominal muscles. Usually, the rectum is empty. During the development of mass movement, the feces is pushed into rectum and the defecation reflex is initiated. The process of defecation involves the contraction of rectum and relaxation of internal and external anal sphincters. Internal anal sphincter is made up of smooth muscle and it is innervated by parasympathetic nerve fibers via pelvic nerve. External anal sphincter is composed of skeletal muscle and it is controlled by somatic nerve fibers, which pass through pudendal nerve. Pudendal nerve always keeps the external sphincter constricted and the sphincter can relax only when the pudendal nerve is inhibited. By Mr. C. A. MBAH Page 33 34 Gastrocolic reflex is the contraction of rectum, followed by the desire for defecation caused by distention of stomach by food. It is mediated by intrinsic nerve fibers of GI tract. This reflex causes only a weak contraction of rectum. But, it initiates defecation reflex. PATHWAY FOR DEFECATION REFLEX By Mr. C. A. MBAH Page 34