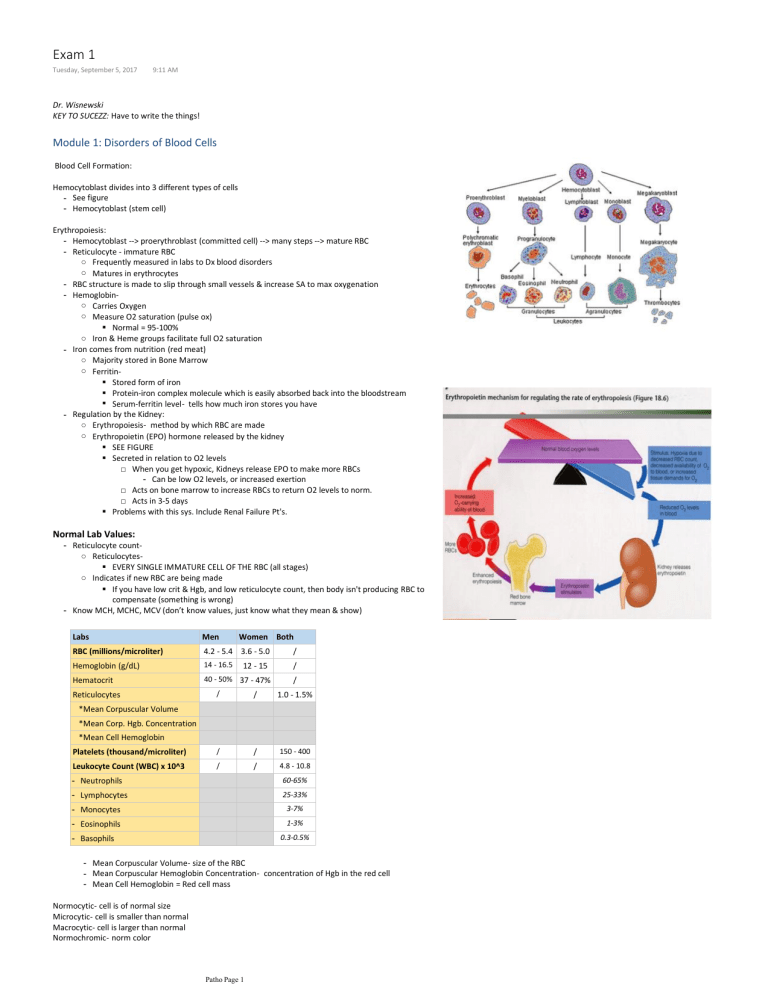
Exam 1 Tuesday, September 5, 2017 9:11 AM Dr. Wisnewski KEY TO SUCEZZ: Have to write the things! Module 1: Disorders of Blood Cells Blood Cell Formation: Hemocytoblast divides into 3 different types of cells - See figure - Hemocytoblast (stem cell) Erythropoiesis: - Hemocytoblast --> proerythroblast (committed cell) --> many steps --> mature RBC - Reticulocyte - immature RBC ○ Frequently measured in labs to Dx blood disorders ○ Matures in erythrocytes - RBC structure is made to slip through small vessels & increase SA to max oxygenation - Hemoglobin○ Carries Oxygen ○ Measure O2 saturation (pulse ox) ▪ Normal = 95-100% ○ Iron & Heme groups facilitate full O2 saturation - Iron comes from nutrition (red meat) ○ Majority stored in Bone Marrow ○ Ferritin▪ Stored form of iron ▪ Protein-iron complex molecule which is easily absorbed back into the bloodstream ▪ Serum-ferritin level- tells how much iron stores you have - Regulation by the Kidney: ○ Erythropoiesis- method by which RBC are made ○ Erythropoietin (EPO) hormone released by the kidney ▪ SEE FIGURE ▪ Secreted in relation to O2 levels □ When you get hypoxic, Kidneys release EPO to make more RBCs - Can be low O2 levels, or increased exertion □ Acts on bone marrow to increase RBCs to return O2 levels to norm. □ Acts in 3-5 days ▪ Problems with this sys. Include Renal Failure Pt's. Normal Lab Values: - Reticulocyte count○ Reticulocytes▪ EVERY SINGLE IMMATURE CELL OF THE RBC (all stages) ○ Indicates if new RBC are being made ▪ If you have low crit & Hgb, and low reticulocyte count, then body isn't producing RBC to compensate (something is wrong) - Know MCH, MCHC, MCV (don’t know values, just know what they mean & show) Labs Men RBC (millions/microliter) 4.2 - 5.4 3.6 - 5.0 Women Both / Hemoglobin (g/dL) 14 - 16.5 / Hematocrit 40 - 50% 37 - 47% 12 - 15 / / / 1.0 - 1.5% Platelets (thousand/microliter) / / 150 - 400 Leukocyte Count (WBC) x 10^3 / / 4.8 - 10.8 Reticulocytes *Mean Corpuscular Volume *Mean Corp. Hgb. Concentration *Mean Cell Hemoglobin - Neutrophils 60-65% - Lymphocytes 25-33% - Monocytes 3-7% - Eosinophils 1-3% - Basophils 0.3-0.5% - Mean Corpuscular Volume- size of the RBC - Mean Corpuscular Hemoglobin Concentration- concentration of Hgb in the red cell - Mean Cell Hemoglobin = Red cell mass Normocytic- cell is of normal size Microcytic- cell is smaller than normal Macrocytic- cell is larger than normal Normochromic- norm color Megaloblastic- large, irregular shape Patho Page 1 Megaloblastic- large, irregular shape Anemia- Anemia is indicated by: - Low numbers of RBC - Low percentage of Hgb (below 14 in men & 12 in females) - Low Hct (below 40% in men & 37% in women) - Etiologies: ○ Autoimmune- own body is destroying itself ▪ Lupus ▪ Erythematosus ▪ Rheumatoid Arthritis ○ Blood loss ○ Bone marrow failure ▪ Usually from infection, radiation, or cancer ▪ Inhibits hematopoiesis and thus low reticulocyte count ○ Erythropoietin Deficiency due to renal failure/disease ○ Hemolysis ▪ Destruction of the RBC in circulation □ Think of rattlesnake venom that causes hemolysis ○ Leukemia ▪ WBC are multiplying so much they crowd out RBCs and drop crit level ○ Malnutrition (iron, folate, vitamin B12 & B6) - Signs and Sxs.○ SEE FIGURE ON SYSTEMIC SYMPTOMATOLOGY -------------------------------------> ○ Fatigue▪ Most common symptom due to poor oxygenation ▪ Oxygen needed to metabolize fuel molecules for energy □ Cannot meet energy demands ○ Increased heart rate ▪ Compensating for the hypoxia, trying to move more blood to the tissues ▪ Self-defeating, can lead to decreased Cardiac Output ○ SOB ▪ Tend to breathe faster to alleviate sensation of hypoxia ▪ Dyspnea- labored breathing □ Different from SOB - SOB means looking at Resp. rate (fast) and intercostal retractions ○ Low BP ▪ Results from lower hematocrit levels, and thus lower viscosity of blood ○ Pale Skin▪ Low oxygenated blood is less red, thus resulting in pale skin Iron-Deficiency Anemia- Most common type of anemia - Also called "blood loss anemia" - Etiology○ Dietary deficiency ▪ Red meats, & organ meats = HIGH IN IRON ▪ Green, leafy vegetables ▪ Iron-Fortified foods ○ Acute or Chronic Blood Loss ▪ Chronic blood loss is the most common etiology of Iron -Deficiency Anemia ○ Increased Demands▪ Pregnancy ▪ Adolescents- due to growth spurts ▪ Diet deficiency □ Red meats, & organ meats = HIGH IN IRON ▪ Menstrual loss ▪ Increased iron requirements in children & elderly - Pathophysiology○ There is an IMPAIRED O2 Transport!! Due to: ▪ Lack of hemoglobin ▪ Tissue hypoxia ▪ Microcytic-hypochromic anemia □ Small cells with less coloring due to reduced amount of Hgb - Labs○ Hemoglobin & hematocrit are going to be low ○ Decreased iron stores: ▪ Low serum iron (in the blood) ▪ Low Ferritin levels (stored iron) - Signs and Sxs○ Sxs depend on how severe the anemia is ○ Fatigue, dyspnea, tachycardia, decreased BP ○ Pallor, smooth tongue, pica (eating weird things) ○ Occult blood▪ Hidden blood in feces ▪ Dark stools showing residual blood in fecal matter ▪ This is a sign of CHRONIC ABDOMINAL bleeding - Treatment○ Increase dietary intake of IRON Ferrous sulfate (oral supplement) Patho Page 2 ○ Ferrous sulfate (oral supplement) ○ Iron Dextran▪ Giving this iron IV can cause fatal dysrhythmias Hemolytic Anemias- Characterized by: ○ Premature destruction of RBC's (before 120 days) ○ Retention of iron & billirubin ▪ Remembers these are byproducts of Hgb destruction ○ Increase in erythropoiesis ▪ Bone marrow is hyperactive to compensate for the decreasing numbers of RBC's, thus an increase in the amount of RETICS - Sickle cell disease - Thalassemias○ Beware of this… just review and know it ○ Genetic hemolytic anemia ▪ Usually found in Mediterranean Peoples - Etiology: ○ Results of an inherited Enzyme Defect ▪ Sex linked X chromosome ○ Can be also caused by: ▪ Various drugs, diseases such as malaria, disseminated -intravascular-coagulation/clotting (DIC), severe burns, venoms, etc. □ DIC- you start bleeding and clotting simultaneously (sign of organ failure) Sickle Cell Anemia- Recessive disorder (must have both recessive genes) ○ Inherited HbS gene ▪ Abnormal Hgb, shaped like an S - Signs and Sxs○ Decreased RBC lifespan (20 days) ○ Chronic hemolytic anemia ○ Vessel Occlusion▪ Irregular shape of RBC can get stuck together or stuck in capillaries/smaller vessels ▪ Get caught and clump together, causing clots □ Causes extreme pain, ischemia - Risk factors for developing a Sickle Cell CRISIS: ○ Cold weather, stress, exertion, infection, other reasons for hypoxia, dehydration, acidosis - Other major complications○ Depending on where occlusion is, that organ will show sxs. ▪ MI, stroke (CVA), infection, pneumonia, bone crises (fx), splenic ischemia, other infarctions to the eyes/kidneys/etc. - Diagnoses○ Analysis of DNA (amniocentesis) ○ Hemoglobin electrophoresis ▪ DNA test to determine the genotype of the hemoglobin (if the HbS gene is present ○ Screening for all ethnicities done in all states - Treatment○ Supportive care given: no specific treatment, but can treat the associated problems! ▪ Antibiotics (infxn), fully immunized against flu, HepB, pneumonia ○ Hydroxyurea (drug), blood transfusion (packed RBCs), bone marrow transplant, stem cell transplant, etc. Megaloblastic Anemias: - Etiology: ○ Impaired DNA synthesis resulting in enlarged RBC ▪ MCV >100 - Main causes: ○ Vitamin B12 deficiency (pernicious anemia) ▪ Found in animal foods including dairy □ Deficiency in vegan/veggie eaters ▪ Essential for DNA synthesis & maturation of RBC ▪ Intrinsic Factor is produced in the ileum □ Need IF to absorb B12 □ Surgery to ileum can cause lack of IF □ Omeprazole (GERD) causes deficiency in B12 & folic acid ▪ Pernicious Anemia = autoimmune □ Often in older adults ▪ Must take large doses of B12 to supplement ○ Folic Acid deficiency ▪ Needed in DNA Synthesis and RBC maturation ▪ Folic Acid is found in: □ Leafy greens, fruits ▪ Associated with alcoholism (most common), celiac disease and some anti-seizure drugs - Pernicious Anemia: ○ VITAMIN B12 DEFICIENCY ▪ B12 COMES FROM ANIMAL PRODUCTS ○ Caused by lack of Intrinsic Factor ○ Pernicious Anemia is an autoimmune disorder: ▪ The gastric mucosa is damaged causing inhibited release of Intrinsic Factor ▪ Intrinsic Factor is required to absorb Vitamin B12 ▪ Thus a B12 deficiency ▪ Pernicious Anemia can also be caused by gastrectomy or surgeries on the ileum □ Results in lack of Intrinsic Factor and digestion of B12 (rather than absorption) Patho Page 3 □ Results in lack of Intrinsic Factor and digestion of B12 (rather than absorption) ○ Signs & Sxs▪ First sxs to appear = gait issues (ataxia) □ B12 deficiency causes demyelination of neurons □ Lack of B12 causes paresthesias which then lead to mobility/gait issues ▪ Severe anemia, mild jaundice, pallor, fatigue ○ Treatment▪ Lifelong IM injections of B12 or very large PO doses Aplastic Anemia: - Reduction of all types of cells (WBC, RBC, platelets) ○ Fatal - no blood cell production - Either insidious or acute onset - Etiology○ Exposure to radiation ▪ Radiation/chemotherapy suppress bone marrow ▪ Cancer treatment = purposeful aplastic anemia ○ Chemicals, toxins that reduce hematopoiesis ○ Benzene, chloramphenicol, AIDS ○ Most are unknown etiology - Signs & Sxs ○ Initial symptoms include that of Anemia: ▪ Fatigue, weakness, pallor ○ Petechieae (punctate skin bruising) and Ecchymosis (bruises) due to decreased platelets ▪ Also prone to bleeding from body cavities ○ Increased susceptibility to infxn (decreased WBC's) - Treatment○ Blood transfusions ○ Bone Marrow transplants ○ Immunosuppressive Therapy▪ Prevents the suppression of the hematopoietic stem cells in the bone marrow ○ Antibiotics for possible infxn. ○ Removal of the causative agent (chemotherapy, radiation, etc.) Polycythemia: - Characterized by High number of RBC & Elevated hematocrit- THIS IS A SYMPTOM (aka "Secondary Polycythemia") ○ Polycythemia Vera ("Primary Polycythemia") ▪ This is a TRUE DISEASE ▪ True disease in the bone marrow of the pluripotent stem cells ▪ Results in an increased production of RBC □ Also can result in: - Increased Blood volume, increased viscosity, HTN, Venous Stasis - Splenomegaly - Caused by: ○ Dehydration ▪ Results in an elevated Hct. % due to the proportion of RBC to plasma ○ Kidney disease (high erythropoietin production) ○ Low O2 levels in the blood caused by: ▪ Congenital Ht. disease ▪ Cor Pulmonale - failure of the R side of the Heart = less blood flow to pulmonary system ▪ Pulmonary fibrosis **This is backwards thinking… due to the hypoxia, erythropoiesis is increased to compensate ○ Smoking - Need to treat the cause of the increased RBC count ○ Some cases need to have blood removed (blood-letting) - Dangerous disease b/c increased risk of clotting Leukopenia: - Low WBC count due to: ○ Bone marrow failure (mainly) ▪ Can be due to infxn, tumor, radiation ○ Infectious diseases- viral diseases ○ Inflammatory disease (RA or allergies) ○ Leukemia ▪ Leukopenia will occur in specific cell lines (monophils, neutrophils, etc.) ○ Severe emotional or physical stress ▪ Remember excess Cortisol release decreases immune function ○ Tissue damage (burns) = related to above statement ○ Low Hgb levels can indicate: ▪ Anemia ▪ Blood loss - Types of WBC: ○ WBC are mediators in inflammation & immune response: ○ Different types of WBC: ▪ Neutrophils- Most prevalent □ Band cells- immature neutrophils ▪ Lymphocytes □ T, B cells ▪ Monocytes ▪ Eosinophils ▪ Basophils - GranulocytesGranulocytes are phagocytic cells that contain cytoplasmic granules Patho Page 4 ○ Granulocytes are phagocytic cells that contain cytoplasmic granules ○ Types of Granulocytes: ▪ Eosinophils- increases with allergic reactions and parasitic infxn ▪ Basophils- increase with allergic reactions (release heparin & histamines) ▪ Neutrophils- increase with infectious diseases □ Shift to the Left or Right…. ○ Shifting to the R & L▪ "we read L to R" ▪ Think of the process of BLOOD CELL MATURATION as a linear figure you're reading □ If there are more immature cells = Shift to the Left □ More mature and less immature = Shift to the Right ▪ Clinical Significance□ If pt. has infxn, there is a L Shift, due to increased production of WBC's □ If administering an Abx, and the pt. has high mature cells (Shift to R), this signals an inability to fight infxn. Due to the body not producing more immature WBC's to keep up - Agranulocytes○ Lymphocytes▪ Play a major role in the immune response ▪ T cells & B cells ○ Monocytes▪ Largest WBC's ▪ Play a huge role in chronic inflammation ▪ Also called Macrophages (phagocytic immune function) Neutropenia: - Neutrophil count less than 1500 cells/uL (norm = 4500-6500) - Agranulocytosis (count <200 u/L) ○ Very severe form of Neutropenia (almost zero neutrophils) - Etiology○ Aplastic Anemia ▪ Remember this is a complete deficiency of all cell types ○ Most cases are caused by DRUGS▪ Chemotherapy (bone marrow suppression) ▪ Drug interactions that cause bone marrow suppression □ Idiosyncratic expression- drug reaction that cannot be explained by a typical Allergy - Drug or its metabolites act as antigens that ruin bone marrow function - Treatment○ Stop the Drug! ○ Give WBC infusions to elevate levels back to normal Leukemias: - Patho: ○ Malignant proliferation of WBC ○ Diffuse replacement of bone marrow with unregulated proliferation of immature neoplastic cells. - Leading COD in children - Causes unknown, but has risks: ○ Radiation, benzene, antitumor drugs, ○ Known as a secondary cancer after chemo for other cancers ○ Can be genetic link (Down Syndrome = high incidence) and can run in families - Acute = kids ○ Overwhelming, quick onset - Chronic = adults ○ Insidious onset - Signs and Sxs: ○ Fatigue, low fever (below 101) ○ Wt. loss ○ Bleeding (due to thrombocytopenia and other forms of anemia) ○ Bone pain, tenderness ○ Lymphadenopathy ○ Splenomegaly, hepatomegaly ○ CNS involvement, HA, N&V, paralysis in Cranial Nerves (palsies), papilledema (enlargement of pupils), seizures, coma - Diagnosed by Increased WBC count (30,000-100,000) - Treatment○ Chemo ▪ CNS irradiation- chemo cannot cross blood-brain barrier ○ Bone marrow transplantation ○ Leukemia is one of the only cancers that can be cured ▪ Cure = 20 yrs free Hodgkin's Lymphoma- Presence of abnormal Reed-Sternberg cells - Cause unknown ○ Carcinogens, viruses, and genetics can play a factor in development - Pathophysiology○ Painless, progressive enlargement of a single node or group of nodes ○ Then spreads throughout the lymphatic system ▪ Usually spread through the liver and spleen - Dx through presence of Reed-Sternberg Cells Hemostasis Disorders- Characterized by 2 Things: Patho Page 5 - Characterized by 2 Things: ○ Inappropriate blood clotting (thrombocytic events) ○ Inappropriate bleeding 5 stages of Hemostasis: 1. Vessel Spasm- Thromboxane A2 released from platelets to induce vasoconstriction ▪ Reduces blood loss □ Aspirin acts specifically to stop thromboxane A2 □ Thus preventing vasoconstriction □ Must apply pressure for longer time to induce vasoconstriction 2. Formation of Platelet Plug - Immediately after injury, Von Willebrand factor released from endothelium released causing platelets to bind to exposed collagen fibers. 3. Blood Coagulation SEE FIGURE -------------------------------------------------------------------------------------------------------> - 2 pathways ▪ Intrinsic pathway: □ Begins in circulation and is initiated by Factor XII ▪ Extrinsic pathway: □ Activated by Tissue Factor - Both pathways activate Factor X ▪ Factor X activates Prothrombin to Thrombin (warfarin) □ Thrombin activates Fibrinogen to Fibrin (heparin) - Fibrin holds the clot together 4. Clot Retraction - Fibrin strands pull the serum out of the clot - This dries it out and cause it to shrink 5. Clot Dissolution - Large amounts of plasminogen are trapped in the clot - TPA (tissue plasminogen activator) is released from the injured tissues and the endothelium converts plasminogen to plasmin - Plasmin digests the fibrin strands and the clot dissolves **KNOW WHERE IN THE PROCESS OF HEMOSTASIS THAT DRUGS WORK** Thrombocytes & Bleeding Disorders: Thrombocytopenia- Reduction in platelets (<100,000) - Etiology: • Decrease in production • Excess pooling in spleen • Reduced lifespan of platelets in the blood - Risk Factors: • Radiation, cancer drugs, HIV - Signs and Symptoms: • Petechieae (think of the Idiopathic thrombocytopenia purpura pt. at Beutel) • Bleeding in body cavities ▪ Nose, eyes, stool, bruising - Treatment: • Platelet transfusions (can only last 1 day in body) • Corticosteroids • IV immune globin • Splenectomy • Immunosuppressant Von Willebrand Disease- Genetic autosomal dominant - Etiology = low level of Von Willebrand factor - Patho• There's a compound defect in platelet function and the coagulation pathway - Symptoms • Severe bleeding in Type 3 (Autosomal Negative - super rare) • Mild to moderate bleeding in Types 1 & 2 - Treatment• Avoid aspirin • Vasopressin (ADH drug) given to induce vasoconstriction ▪ Also causes endothelium to release stored VW factor and plasminogen activator ▪ Desmopressin acetate (drug) Hemophilia A- Sex linked (X linked) recessive (mostly males) • Can either be genetic (FHx) • Or due to Factor VIII gene mutation - Expression of the effects vary with some pts. producing no Factor VIII and others have only mild sxs. - Spontaneous bleeding (internally) • Hemophilia A = HIGH RISK for internal bleeding ▪ Can occur in the joints --> results in swelling --> results in decreased ROM - Treatment• Give them what's missing (Factor VIII) • Avoid aspirin, NSAIDS ▪ Aspirin (antiplatelet aggregator) = inhibits platelets from forming the platelet plug □ Acts directly on Thromboxane A Module 6 GENETICS: 09/07/2017 Patho Page 6 DRUGS!!!! - Step 1 - Vessel Spasm ○ Aspirin acts to inhibit release of Thromboxane A2 - Step 2 - Platelet Plug ○ Aspirin & Plavix also prevents platelets from aggregating - Step 3 - Blood Coagulation ○ Warfarin- Decrease amounts of prothrombin and other coagulation factors ○ Heparin- Prevents the activation of Fibrinogen to FIBRIN ▪ Naturally released by MAST Cells - Step 5 - Clot Dissolution ○ TPA- Can be given as a drug to instantly dissolve clots everywhere in the body! Module 6 GENETICS: 09/07/2017 EXPLOSION! Genome- total DNA in organism - Required to make the org. & for the org. to fxn properly Genetics- the study of the science of heredity! SEE TERMS TO KNOW FROM THE PWRPOINT! TERMS: DEFINITION: Gene Mutation Biochemical event leading to the change of DNA sequence Polymorphism More than one normal allele (alternate forms) at the same locus… - EX: Blood Type (AB, AO, BO, O, etc.) Congenital Deformity acquired in-utero (not developed later on) Genotype Genetic composition Phenotype Expressed character trait Polygenic inheritance Multiple genes at different loci, affecting 1 trait (hair color) Multifactorial inheritance Same as Polygenic Inheritance, but also includes environmental factors Karyotype Numeric classification system of autosomes and sex-chromosomes Homozygous Same allele Heterozygous Mixture of dominant and recessive alleles Gene penetrance The ability of a gene to express its function Gene expression The degree to which the phenotype of the gene is expressed Basic genetic info stored in chromosomes - 46 = 22 autosomes & 1 pair of Sex chromos - ** remember importance of X-linked genetic disorders (males impacted, etc.) DNA molecule- Double stranded helix - Info stored in nucleus - DNA Carried by 4 Nitrogenous Bases • Guanine, adenine, cytosine, thymine ▪ Cytosine -> Guanine ▪ Adenine -> Thymine • Pyrimidine & purines ▪ Pyrimidine = Thymine & Cytosine ▪ Purines = Adenine & Guanine - Almost every organism on earth uses this same genetic coding system Regulation of Gene Expression: - There are factors that allow genes and characteristics to be expressed individualistic to each person • Think of: **no two individuals with Downs are the same** - Induction• Process by which gene expression is increased ▪ (usually promoted by an external influence) - Gene repression• Process by which a regulatory gene reduces or prevents expression of a gene Gene Mutations: - Mutations can occur from substituting bases, adding/deleting bases or rearranging - Mutations often are corrected by DNA repair mechanisms in the cell - Inheritance of mutations: - Mutations that occur in the germ cells (ovum/sperm) can be inherited - Those occurring in somatic cells cannot be inherited - Mutations in the early embryonic can cause malformation & death • Ex: Cleft Pallet, Club Foot?, - Mutations form cancer later on in life • Radiation treatments per cancer usually cause another form of cancer • RADIATION is an ex. Of mutagenic agents that can cause cancer ▪ Also: viruses, chemicals, UV light, Role of RNA vs. DNA: - SERIOUSLY DUDE, GO BACK AND REVIEW ALL OF THIS JUNK - DNA determines the type of biochemical product that the cell will form - RNA• M-RNA- recognizes the start and end of Gene sequence, creating M-RNA from DNA (transcription) • T-RNA- Delivers AAcid to the ribosomes (protein synthesis) • R-RNA- Responsible for protein synthesis Genotype vs. Phenotype: - Genotype- genetic info stored in the basic triplet code on the chromosome - Phenotype- outward expression • Don't know genotype, because it can be either homozygous dom. Or heterozygous Expressivity/Penetrance- Transcription factors bind to DNA to regulate time or transcript that activate or repress gene expression • Ex: in down's some genes express mildly or severely Patho Page 7 • Ex: in down's some genes express mildly or severely ▪ Depends on the transcription factors and how they tell the DNA to express/repress the gene - Penetrance• Specific gene's ability to express itself in a pop that everyone has the genotype • Ex: entire pop. Has genotype for 6 fingers ▪ Not everyone in the room will express the phenotype for 6 fingers ▪ 75% penetrance = 75% of population with the genotype will express the phenotype Types of Inheritance: - Polygenic• There are multiple genes at different Loci ▪ Each gene on the loci exerts and additive effect on the expression of the trait ▪ THIS HAS NO ENVIRONMENTAL INFLUENCE • Ex: eye color, skin color, etc. ▪ Many genes are acting on this trait ▪ Very complex to guess the phenotype - Multifactorial• Multiple alleles at different loci affect the outcome • THIS INCLUDE ENVIRONMENTAL INFLUENCE • Ex: height, diabetes, alcoholism, etc. ▪ Height is multifactorial, because yes it includes genetics, but also environmental (maybe you weren't nourished properly, etc.) Mendel's Laws: - Locus- position of a gene on a chromosome (loci = plural) - Allele- Alternate forms of the same gene on the same locus • Dominant/recessive Singe-Gene Disorder: - Single gene is affected @ a single locus Abraham - Marfan's Syndrome ○ Autosomal Dominant Lincolon Disorder ▪ Need 1 gene from 1 parent ▪ There are a lack of certain proteins that regulate DNA to grow/develop properly ○ Affects: ▪ Ocular system ▪ Cardiovascular ▪ Skeletal system ○ Signs and Sxs: ▪ Mitral valve prolapse ▪ Weak aorta (risk of aneurysm) ▪ Arachnodactyly □ Long arms, face, etc. (JACKSON FUCKING MYERS) ▪ Pectus Excavatum = irregular sternum curvature (in or outward) ▪ Hyper-extendible joints ▪ Vertebral issues (scoliosis, kyphosis/outward curve) ○ Treatment▪ No true treatment for the syndrome, but you can repair weaknesses □ Repair the aorta, surgical repair of the sternum, etc. Sex-Linked Diseases: - Remember X-linked allow females to be "carriers" but not express• Thus males will AUTOMATICALLY express the gene (if they get that particular X chromosome from the mommy) ▪ There are 2 dummy, don't forget! One affected one is fine! ▪ Some people have boys that don’t get that X chromosome (lucky bastards) - Hemophilia○ Group of diseases in which blood doesn't clot properly ○ They lack the normal Factor VIII ▪ Lacking factor VIII prevents pt. from clotting normally ○ Can be treated by supplementing Factor VIII (drug), but biotech has allowed us to derive FVIII from bacteria (lessens health risk of the pt.) Multifactorial Inheritance Disorders- See definition above! - Examples of Congenital Disorders: ○ Cleft palate, congenital heart disease, Urinary tract malformation - Environmental Factors: • Think of it this way: you have the genetic predisposition, but your environmental factors can influence/heighten you risk (HTN, cancer, DM, CAD, etc.) - Environmental Influences on Fetal Devo: • Period of Vulnerability ▪ Ex: 2 weeks, the CNS is EXTREMELY vulnerable □ Vulnerability of CNS lasts until the 20-22 wks up to 2 yrs. ▪ Each system has a period of vulnerability • Teratogenic Agents: ▪ Alcohol, drugs, radiation, chemicals, infectious agents • Exposure to teratogens during period of vulnerability can alter genetic expression of the fetus… damn. • Fetal Alcohol Syndrome: ▪ Combo of physical, cognitive, & behavioral abnormalities ▪ Caused by alcohols during the pregnant □ Usually due to inability to know if pregnant within 2 weeks. ▪ Results in: □ Prenatal/postnatal growth retardation Patho Page 8 □ Prenatal/postnatal growth retardation □ Permanent effects on CNS □ Characteristic facial features - Flat nose bridge - Microcephaly - Etc. Autosomal Examples: - Human Allelic Disorders (dominant) • All you need is 1 gene from 1 parent - Conditions are very rare but commonly expressed - Examples: • Achondroplastic Dwarfism • Polydactyly • Huntington's Disease▪ Autosomal Dominant ▪ Progressive destruction of brain cells ▪ If parent has the disease, 50% of the children will have it □ Unless the parent was HOMOZYGOUS dominant ▪ Disease doesn’t usually manifest until after the age of 30 ▪ Dyskinesia- extremities/body parts don't move together/work together □ Cannot talk, cannot move properly, etc. FAT HOARDER IN THE • Nieman-Pick Disease BRAIN ▪ Autosomal Recessive □ Both parents must contribute **Review the statistics of autosomal recessive and the chances of acquiring** ▪ Lipid Storage Disorder: □ Subgroup of diseases known as "sphingolipidases" □ Harmful amounts of fat accumulate in the spleen, liver, brain, lungs, & bone marrow ▪ Missense Mutation causes a complete deficiency of Sphingomyelinase □ Deficiency of this enzyme results in fat buildup within the lysosomes □ Lipids cannot be destroyed so cells become enlarged ▪ Most are Polish, Jewish, Russian background **YOOO…. SHE'S SPENDING A LOT OF TIME COVERING THIS….*** • Color Blindness: ▪ Sex-linked traits □ More males are affected than females ▪ Color perception depends on three genes, each producing chemicals sensitive to different parts of the light spectrum (colors) ▪ Red & green detecting genes are on the X chromosome (most common) □ Blue detection is autosomal trait Genetic Technology- Gene mapping - Cloning (Dolly) - Recombinant DNA Technology (insulin) • Combining DNA molecules not found together in nature • Allows us to ID DNA sequence and produce the protein product - Gene Therapy• Cancer txt's, inserting genes into genome of an individual to treat disease - DNA Fingerprinting? Blood type is inherited - ABO is inherited separately from the Rh +/- factor Obesity & Heredity: - Two ID twins, genetic expression of obesity shows high heritability Module 8: Fluid Balance/Imbalances: Remember where the fluids are: - Intracellular (remember that body cells AND BLOOD CELLS have water) - Extracellular (plasma & interstitial spaces) Electrolytes- Substances that dissociates in solution to form a charged particle (Na+, CL-, K+) • Ions are these charged particles Nonelectrolytes- Substances that don't dissociate into charged particles • Ex: glucose KNOW THE NORMAL LAB VALUES - Normal Lab values will vary between organizations • Know the ones in the book/power point Electrolyte Sodium Normal Value 135 - 145 Potassium 3.5 - 5.0 Calcium 8.5 - 10.5 Magnesium 1.3 - 2.1 Chloride? 98 - 106 Patho Page 9 TaySachs Chloride? 98 - 106 Sodium Bicarbonate? 24 - 31 Interstitial Fluid Exchange: - SEE THE FIGURE & LOOK UP IN THE BOOK TO UNDERSTAND THIS - Capillary filtration pressure pushing fluid out • Acting against in the interstitial space is "Tissue Hydrostatic Pressure" • If you have a lot of water in the IS space, it will push into the vascular space - Capillary colloidal (protein typically albumin) Osmotic Pressure pushing fluid back into the blood stream • Pulls water from IS space back into the capillary - Interstitial Pressure opposes the movement of water out of the capillary ** remember pressure dynamics** • Arterial end higher pressure than venous end of capillaries • Know the exact numbers and how that relates to electrolytes/fluid balance in the capillaries • 120 mmHg in the LV and pushes the blood all the way to the caps. ▪ It is at its lowest point the Rt. Atrium 30 mmHg 10 mmHg Fluid Compartments or Spaces: - Intracellular - Extracellular - And a THIRD = Potential Space Third Spacing- Fluid trapped in one of the several possible transcellular spaces - Fluid that cannot be used for normal function within the body • Need to relieve the fluid through letting (cardiocentesis) • EX: ▪ Ascites (abdominal fluid buildup, trapped in abdomen) □ Associated with R-sided Ht. failure ▪ Pleural Effusion □ Fluid (bleeding) and air collecting in the pleural space - Normal value is 4 mL (just enough to separate membranes) □ Expect SOB, cyanosis, etc. □ Can be caused by trauma, cancer, etc. ▪ Cardio Effusion OsmosisSEE FIGURE ON OSMOSIS AND ITS EFFECT ON THE CELLS (ISOTONIC, ETC.) - Movement of water from higher concentration to lower concentration Osmolarity of Fluids: - Osmolarity is the amount of sodium and other solutes in the blood • KNOW THE NORMAL OSMOLARITY • The majority is sodium Main source of fluid intake is water Main source of fluid output is urine - Homeostatic mechanisms maintain proper balance • Secretion of ADH to retain water, or reduced secretion of ADH to let out water • Increased/decreased urine output ▪ Small amount & highly concentrated ▪ High amount & dilute • Thirst Water losses: - Obligatory Urine Output = must have 300-500 cc's per 24 hrs • Thus an hourly urine output assessment to ……. Remember that we’re focusing on the serum/fluid outside the cell cause you can’t measure inside the cell. So in a hypotonic solution you have not a lot of concentration, etc 1. increase blood flow ADH in POSTERIOR pituitary -by increasing water reabsorption in kidney tubules See image for normal feedback mechanisms Abnormal states of hydration: 2. increases systemic vascular resistance -vasocontriction of blood vessels - Fluid volume deficit- proper terminology for dehydrated • Types: • Isotonic- equal loss of water & sodium ▪ Ex: vomiting, diarrhea, misuse of diuretics/lasics ▪ Rx Tx- IV fluid replacement using NS (0.9%) • Hypertonic- more water loss than sodium ▪ Osmotic diuresis, excessive sweating, loss of thirst, unable to obtain drink fluids ▪ Usually occurs in diabetes--- large glucose molecules are drawing out fluids, while Na+ ions are maintaining normal filtration levels (thus relatively more sodium) ▪ Rx Tx- drinking plain water or IV of Dextrose 5% in water (D -5-W) • Hypotonic- more Na+ lost than water (serum Na+ is low) ▪ Excess renal losses of Na, aldosterone deficiency (aldosterone saves/retains Na) ▪ Tx w/ Iv of NS, or a 3% solution of Na IV • Sxs: ▪ Dry skin, mucous membranes (tongue) ▪ Poor skin turgor ▪ Decrease Urine output (concentrated) ▪ Babies have a decreased fontanel □ Eyes also appear sunken ▪ B.P. may be decreased with increased HR □ (orthostatic hypotension) • Physiological consequences: Patho Page 10 • Physiological consequences: ▪ Inadequate renal perfusion (blood flow) - Fluid Volume Excess• Causes: heart failure, kidney issues • Signs and Sxs ▪ Acute weight gain ▪ Increased BP ▪ BOUNDING pulse ▪ Possible SOB (dyspnea) ▪ Poss. Jugular venous distension (JVD) □ Visible jugular vain ▪ Edema Lab Tests: - Hematocrit (Hct) • Normal Values: ▪ Males = 40-50% ▪ Females = 37-47% • % of RBC to the amount of fluid in the blood • In dehydrated pt. the Hct is increased ▪ # of RBC didn't change, but the amount of water did!! □ The proportion changes, thus increased the Crit - Urine Specific Gravity• Measures the weight of urine compared to the density of water • Normal range = 1.010-1.025 • Low specific gravity is seen in dilute while concentrated shows high sp. Gravity ▪ Dehydration results in HIGH specific gravity! (Hypertonic urine) • Specific Gravity Conditions; ▪ Increased SG can be caused by glucose or proteins in the urine. □ Make the urine more dense! ▪ SG doesn't change in pt. where the kidneys are unable to concentrate the urine adequately ▪ If the SG is low, it indicates an adequately hydrated pt. due to it being dilute and not containing solutes. - Osmolality• Reflects the kidneys ability to produce concentrated/dilute urine • Measured by serum osmolality and the need for water conservation/excretion • If the urine is concentrated, that means the kidneys are conserving water due to an increased serum osmolality. Drugs to Decrease fluid volume- Diuretics• Lasix (Furosemide)▪ Loop diuretic = works in the loop of Henle • Hydrochlorothiazide (HCTZ) ▪ Thiazide diuretic ▪ They give to AA • Spironolactone (aldactone)▪ Aldosterone receptor antagonist ▪ This is a potassium sparing diuretic - Diuretics induces the excretion of sodium • WATER FOLLOWS SODIUM, therefore, there is a loss of water • This is why DIURETICS usually cause some forms of "hypo" electrolyte imbalances Edema = sign of excess IS fluid - Most common in the feet and legs - Anaphylaxis = edema in the face, throat, eyes, etc. - Etiologies: - Increased Hydrostatic pressure - Lowered plasma oncotic pressures ▪ Due to decreased amounts of plasma proteins - albumin ▪ DECREASED CAPILLARY COLLOIDAL OSMOTIC PRESSURE REDUCES THE ABILITY TO SUCK FLUID FROM IS BACK INTO CAPILLARY - Increased capillary permeability ▪ Causes solutes to leave the capillary, increase the interstitial osmolality and draw more water in the interstitial spaces; thus causing edema - Lymphatic Channel Obstruction ▪ Can be caused by cancer or surgery Electrolyte Disturbances: - Regulating Na & Water when Na is low • Serum sodium level decreases (decreased serum osmolality = less than 280) • Thirst response goes away and Intake is reduced • ADH release is slowed to induce more frequent diuresis • More diuresis = serum osmolality normalizes Everything is low and slow Hyponatremiawith hypo is low and slow • More common Everything than hypernatremia with hypo • Etiologies○ Excess ADH ○ Vomiting ○ Hypotonic irrigations (enemas) ○ Excessive water intake ○ Near drowning (freshwater) • Signs and SymptomsPatho Page 11 • Signs and Symptoms○ Muscle/abdominal cramping ○ N/V ○ Suppression of thirst reflex ○ HA, confusion, lethargy, seizures, coma, death **most sxs. Are manifestations from the brain!!!*** Neuro sxs • Drugs can cause hyponatremia: ○ Diuretics!! ▪ Induces sodium loss to reduce water concentrations • Diagnosis: ○ Serum sodium level = below 135 ○ Serum osmolality below 280 ○ Urine Specific Gravity below 1.010 ○ Elevated Hct & plasma proteins • Tx: ○ Treat the underlying cause! ○ Fluid restriction ○ Oral or IV of saline solution (NS) ○ Eat high sodium foods ○ Severe: ▪ Neurological symptoms such as seizures (serum sodium <110) ▪ Treated with hypertonic solution (3-5%) to increase sodium levels and return to normal □ Too much treatment with hypertonic solution can cause a rapid shift of water out of the brain cells and cause permanent brain damage (Karev) Hypernatremia- Sodium levels above 145 mEq/L ○ Serum osmolality above 295 - Etiologies: ○ Tube feedings ▪ Some of the canned foods for tube feedings are high in sodium (need to dilute them) ○ Watery diarrhea ○ IV infusion of hypertonic solution ○ Near drowning (salt water) ○ Inability to respond to thirst ▪ They are relatively hypernatremic due to low fluid levels - Signs and Symptoms○ Thirst ○ Oliguria (inability to form urine) ○ Decrease in skin turgor, salivation ○ Neuro sxs: ▪ HA, agitation, poor reflexes, seizures, coma, death - Assessment: ○ Drugs that cause: ▪ Antibiotics, anything with sodium bicarb, IV NaCl ○ Nursing functions: ▪ Monitor neuro status, seizures, etc. I&O, Vitals, Instruct to avoid high Na+ foods - Diagnoses: ○ Serum sodium above 145 ○ Serum osmolality above 295/300 ○ Urine specific gravity will be high (dehydrated) = 1.025+ - Treatment○ Treat the underlying CAUSE ○ Replace fluids, slowly and carefully ▪ Can be done orally or IV but gradually to avoid Cerebral Edema Potassium: - Normal value = 3.5-5.0 - Dietary Sources of K+ • Fruits (think bananas, oranges, etc.) • Meats • Vegetables Hypokalemia- K+ level below 3.5 - Etiologies: ○ Inadequate Dietary Intake: ▪ Anything that causes poor eating habits □ Anorexia □ NPO □ Unbalanced diet ○ Excess Renal, GI, Skin losses ▪ Potassium wasting diuretics (Lasix & thiazides) ▪ Diarrhea/emesis □ GI secretions are high in K+, therefore unusual wasting can cause hypokalemia - Signs and Symptoms○ Decreased urine specific gravity ▪ Less concentrated urine = lower Specific Gravity ○ GI, Neuromuscular, renal, & Cardiovascular systems are mostly effected ▪ Due to K+ acting on the electrical activity of excitable tissues □ HEART DYSRHYTHMIAS!! Decreased T-wave ▪ Abdominal distention, constipation, diminished bowel sounds (abnormal peristalsis) □ Due to the K+ deficiency acting on the bowels' contractility ▪ Muscle weakness, paralysis Patho Page 12 ▪ Muscle weakness, paralysis - Diagnoses: ○ Lab results ▪ Urine specific gravity ▪ K+ serum level ▪ Serum osmolality ○ Presence of sxs. (T-wave depression) - Treatment: Give them foods high in potasium ○ High K+ foods, oral supplements, or IV ▪ K+ must be diluted when given IV (or it will stop the heart) and also needs to be infused not pushed ○ Meds to help treat hypokalemia = K-Dur & IV Potassium Chloride Hyperkalemia- Serum potassium greater than 5.0 - Etiologies: ○ MOST COMMON CAUSE IS DECREASED RENAL FUNCTION ▪ The Kidney is unable to excrete potassium into urine like normal ○ Excess IV administration of K+ or excessive oral ingestion of supplements ○ K+ sparing diuretics (spironolactone) ○ Shift of K+ from intracellular to extracellular (ICF -> ECF) ▪ Crushing injuries, burns, etc. ▪ These types of injuries cause cell death and thus release of K+ into the ECF - Signs and Symptoms○ First symptom is paresthesia (numbness/tingling) ○ HEART DYSRHYTHMIAS ▪ Cardiac conduction is inhibited ▪ Shown through PEAKED/ELEVATED T-WAVES ○ Also GI sxs like in hypokalemia (N/V, intestinal cramping, diarrhea) ○ Muscle weakness, and decreased neuromuscular excitability ▪ Remember that K+ messes up the electrical activity of the systems ▪ Dyspnea due to respiratory muscle weakness - Diagnosed by looking at lab values, medical history (renal failure, etc.), & EKG findings - Treatment: • Limit K+ foods, & sparing meds (spironolactone) • Needs something that will remove K from body ▪ Sodium polystyrene (Kaexalate) □ Resin drug that exchanges potassium for sodium, lowering the K+ level ▪ Calcium gluconate□ Calcium antagonizes the reduced membrane excitability caused by excess K+, and returns excitability/membrane potential to normal Short-lived solution and thus combined with something that can reduce the ECF concentrations of K+ (insulin) □ Need to monito EKG for hypokalemia (flattened T-wave, etc.) • In severe cases, hemodialysis can be used for pt. with renal failure Calcium: 8.5 - 10.5 mg/dl Hypocalcemia- Serum calcium level less than 8.5 mg/dl - Etiology: ○ Most common cause is Renal Failure ▪ Results in decreased production of activated Vitamin D and hyperphosphatemia □ Vitamin D is activated in the Kidneys… □ Without active Vitamin D, calcium cannot be absorbed from the GIT □ Phosphate and Calcium have an inverse relationship □ Increased phosphate (hyperphosphatemia) results in hypocalcemia ○ Hypoparathyroidism! ▪ Decreased production of parathyroid hormone, thus less release of calcium from bone and less absorption from the GI tract (See figure on Pg. 182) ○ Pancreatitis which causes fat necrosis ○ Chronic diarrhea (inhibits ability to absorb Ca++ from the GIT) - Signs & Symptoms○ First, it will most likely cause NEURO/MUSCLE PROBLEMS (Increased Neuromuscular Excitability) ▪ Neuromuscular irritability ▪ Cramping!!! ▪ Hyperactive reflexes!!! ▪ Paresthesia ▪ Tetany (spasms in face, hands, feet)!!! ○ Heart dysrhythmias - Diagnoses: ○ Chvostek Sign ▪ Stimulating facial nerve by tapping and observing for tetany ○ Trousseau Sign ▪ Inflating BP cuff to 10 mm above systolic and watching for tetany in hands/fingers - Treatment using medications: ○ Calcium chloride ○ Calcium gluconate - restores functional integrity of the neuromuscular sys. ▪ Remember this from Hyperkalemia Hypercalcemia- Serum calcium above 10.5 mg/dl - Etiology○ Overconsumption of Vitamin D ▪ Results in excessive absorption of Calcium and increased serum Ca++ levels ○ Hyperparathyroidism▪ Excess release of PTH, thus excessive Ca++ release from bones Patho Page 13 ▪ Excess release of PTH, thus excessive Ca++ release from bones ○ Bone tumors can also cause increased Ca++ release from bones - Signs & Symptoms: ○ Decreased neural excitability & impaired cardiac and smooth muscle fxn ○ Muscle weakness ○ Neuromuscular▪ Headache, stupor, fatigue ○ Anorexia, constipation, N/V ▪ Think of the decreased smooth muscle ability ○ Cardiac dysrhythmias (ventricular) ▪ Ca++ is the primary ion responsible for cardiac conduction… too much causes deadly Ventricular Arrhythmias - Treatment: ○ Correct the underlying cause of the serum Ca++ excess ○ Promote urinary excretion of Ca++ ▪ The excretion of Na+ is accompanied by Ca++ ▪ Diuretics!! ○ Calcitonin- decrease osteoclast activity/calcium release from bone Magnesium: Normal serum magnesium is 1.3 - 2.1 mg/dl Hypomagnesemia • Serum Magnesium less than 1.3 mg/dl • Etiology○ Most common causes are malnutrition and chronic alcoholism ○ Diabetic Ketoacidosis, Diuretic therapy, & hyperparathyroidism ▪ Result in increased urine losses of magnesium • Signs & Symptoms○ Hyperactive NEUROMUSCULAR activity ▪ Tetany ▪ Nystagmus- following the finger back and forth with pupil (tracking without fluttering) ▪ Choreiform movements (dyskinesia) ▪ Trousseau signs ▪ + Babinski test- reflex and the bottom of the foot • Treatment○ Magnesium replacement ▪ Magnesium hydroxide (Milk of Magnesia) ▪ Magnesium sulfate ○ Route of administration depends on the severity of the hypomagnesemia Hypermagnesemia• Serum magnesium above 2.1 mg/dl • Etiology○ Renal Disease/failure ○ Excessive intake of drugs containing magnesium ▪ IV administration ▪ P.O. meds- antacids, supplements, laxatives • NEUROMUSCULAR & cardiac SXS ○ Muscle weakness / hyporeflexia ▪ Due to magnesium decreasing the acetylcholine release at the neuromuscular junction ○ Lethargy, confusion, coma ○ Cardiac arrest, arrhythmias, hypotension ▪ Due to the Calcium channel blocking effect of magnesium ○ Respiratory arrest, complete heart block, and cardiac arrest (think of the lack of muscular excitability) • Treatment○ Stop administration of magnesium ○ Administer calcium (direct antagonist of magnesium) Electrolyte Normal Lab Values: Electrolyte Levels Serum Sodium (Na+) Normal Lab Values 135-145 mEq/L Serum Potassium (K+) 3.5-5.0 mEq/L Serum Calcium (Ca++) 8.0-10.5 mg/dL Plasma Protein albumin Hematocrit (Hct) Urine Specific Gravity 3.4-4.7 g/dL Men 40-50% | Women 37-47% 1.010 - 1.025 Module 12: Diabetes****************************************** She fckin loves DM dude… study it. Don't play. Review- Insulin is produced in the BETA Islet cells of the Pancreas ○ Alpha Islet cells produce glucagon ○ Insulin released form the B cells is not the true form used by the cells ▪ There's a process of activation ○ The insulin then attaches to many cells ▪ Mainly muscle, fat, and tissue cells ▪ There are certain cells that don't use insulin ○ Without insulin attaching to the cell, glucose CANNOT enter the cell - Diabetes is a disease where the body doesn't produce or use insulin properly Patho Page 14 - Diabetes is a disease where the body doesn't produce or use insulin properly ○ There are other hormones that are affected! DM is a GROUP of metabolic disorders - Impaired metabolic functioning affecting fat, carbs, and protein metabolism - Characterized by HYPERglycemia (in all types) Significance of DM- Diabetes is a chronic disease - Affects ALL age groups (infant to elders) ○ More prevalent in minority populations (Am. Indian, Hispanic, Blacks) 1. American Indian/Alaskan Natives 2. Black 3. Hispanic 4. Asian 5. White ○ More prevalent in older adults (65+) - 7th leading COD in the US ○ Number 1 cause of blindness ○ Number 1 cause of END-stage Renal Disease (ESRD) ▪ Number 2 = HTN ○ Number 1 cause of lower extremity of amputations - Diabetes is a major risk factors for MI & CVA (heart attack and stroke) - Huge contributor of medical expenses and diminished QOL ○ 1/3 of the Medicare budget - Risks factors are all circulatory related: ○ That much glucose is not supposed to be in the blood ○ The glucose causes damage to all of these vital places where good, pure blood flow is needed: ▪ MI, CVA, blindness, ESRD, amputations, etc. Time Toward Complications = when you have hyperglycemia, each minute you have that, is time toward serious complications (MI, CVA, etc.) - Refers to a great 1/3 of people with DM are undiagnosed Diabetes & Death- 7th leading COD - Large amount of DM deaths go unreported ○ Report as MI, even though DM was the causing factor Historical Perspective- Egyptians found urine to be sweet - Greeks described polydipsia (excess thirst) and polyuria of sweet urine - Research in the US (1921) Banting & Best discovered the hormone insulin in dogs Diabetes: - Type I develops as a child ○ MUST inject insulin… you will die without - Type II usually develops as an adult ○ Can be managed w/ diet ○ Others take oral meds that stimulate the pancreas and the insulin process ○ Progressive disease ▪ After about 10 yrs, they are likely to need to have insulin supplements ▪ Due to exhaustion of cells - No major difference, except the LONGER you have the disease, the more complications can arise ○ Complications include: ▪ Heart disease, stroke, blindness, etc. Contributing Factors to Hyperglycemia- Hyperglycemia is in NO WAY @ ANY TIME normal - Pancreas○ Impaired insulin secretion/production - GI○ Absorption of glucose from diet - Liver○ Inappropriate glucose production ▪ Breaks down glycogen stores even if there is BG from GIT absorption - Muscle○ Decreased insulin-stimulated glucose uptake ▪ Glucose sparing for the brain and other vital organs Pancreatic Hormones: - Insulin○ Secreted by B cells in pancreas ○ Lowers the blood glucose by attaching to cells' insulin receptors, allowing glucose to enter the cell ▪ If there is excess glucose, it is stored as glycogen ○ Prevents the breakdown of fat and glycogen stores in the liver and lipid tissues ▪ Works to build fat to reduce the blood sugar levels ▪ Also inhibits gluconeogenesis ○ Increases protein synthesis, fatty acid transport into ADIPOSE tissues ▪ Increases transport of AA into protein cells ○ Inhibits the lipase in adipose- preventing breakdown of fats ○ Target Cells▪ Some cells don't require insulin for glucose uptake □ Liver, brain, RBC Patho Page 15 Unmanaged Type II can lead to Beta cell exhaustion and lack of insulin production and require insulin injections ▪ Increases transport of AA into protein cells ○ Inhibits the lipase in adipose- preventing breakdown of fats ○ Target Cells▪ Some cells don't require insulin for glucose uptake □ Liver, brain, RBC ▪ All other cells require insulin to uptake glucose into the cells ○ Normal Hormonal Control: ▪ 3 things control glucose levels □ Insulin secretion □ Uptake of glucose by peripheral tissues □ Glucose production in the liver - Can either store glucose as glycogen or through gluconeogenesis -> breakdown glycogen stores to increase blood glucose levels - Liver can inappropriately increase blood glucose levels in diabetics ○ Pathogenic Process▪ Autoimmune destruction of B cells (type I) ▪ Insulin resistance (type II) □ Obesity is a risk factor for type II ▪ Diminished tissue responsiveness to insulin □ Leads to hyperglycemia, then eventually overt diabetes - Glucagon○ Increases blood glucose levels ▪ Coverts stored glycogen in liver to glucose ▪ Released of glucagon stimulated by low blood sugar levels ○ Used for children with HYPOglycemia to induce the liver to break down glycogen stores to increase blood glucose levels - Amylin○ Islet amyloid polypeptide ○ Co-secreted from the B cells of the pancreas (along with insulin) ○ Released in response to nutritional stimuli ▪ Slows the movement of food through the stomach to lower the postprandial blood glucose (2 hours after meals) □ Blood sugar should be normal at this time (below 140) □ Persons with diabetes, manage the level between 140-180 ▪ This is the clinical significance (lowers postprandial glucose) - Somatostatin○ Released by the Delta pancreatic cells ○ Inhibits the release of insulin & glucagon ○ Decreases GI activity after ingestion of food ▪ Thus increasing the amount of time it takes for the food to absorbed into the bloodstream ** these 4 hormones control the regulation/absorption of glucose, AA, & fatty acids** - Incretin Hormones○ Incretin- Intestinal hormones in response to ingestion of food ▪ Increases the insulin response to get glucose in the cells ▪ Responses to incretin in T2DM is decreased (not as effective) ○ 2 main types of Incretins: GIP, GLP-1 ▪ GIP and GLP-1 are rapidly degraded by the DPP-4 Enzyme ○ Exenatide- synthetic GLP-1 ▪ Exenatide is resistant to the DPP-4 enzyme, and thus lasts longer in the bloodstream □ Since the synthetic GLP-1 is in the bloodstream longer, it potentiates the insulin release ▪ Given by injection to potentiate insulin release ▪ A synthetic DPP-4 agent (Januvia) has been developed to decrease hyperglycemia □ DPP-4 AGENT used to deactivate DPP-4 ENZYME □ Is that why the DPP-4 agent is used to decrease hyperglycemia??? Types of DM- Type I ○ ABSOLUTE INSULIN DEFICIENCY ▪ Caused by either: □ Type 1A- Immune mediated response (autoimmune destruction of B cells) □ Type 1B - Idiopathic (unknown etiology) - Type II○ Combination of decreased insulin production and cellular resistance to insulin ○ Most common - Other specific types○ Most of the times these are genetic in nature ○ Endocrine disorders (Cushing's) ○ Diseases of the Pancreas (pseudocysts) ▪ Pancreatic cancer, etc. - Gestational DM○ Develops during pregnancy (may or may not end after pregnancy) Dx Criteria: - Fasting Blood Glucose (FBG)- (Traditional Method) ○ 126 mg/dl or higher ▪ Diagnostic of DM ▪ Normal = 70-100 ○ This is the blood glucose after 8 hrs of fasting - Hgb A1C○ 6.5% or higher to Dx ▪ Normal is about 4-6% ▪ Diabetic want to keep it below 7% Patho Page 16 Prolonged cortisol release, causes increased/prolonged gluconeogenesis The study guide tutors send has the "goal" for DM pts. And then the normal ranges ▪ Diabetic want to keep it below 7% ○ Shows how long the RBC has been in circulation and being glycosylated (coated) with glucose ▪ Hgb is saturated with glucose over time ▪ If you have high blood glucose levels for a long time, the A1C level will be higher □ Like in poorly managed diabetes, there is circulating glucose in the blood and it glycosylates the RBC - 2 hours Plasma Glucose○ 200 mg or higher to Dx ▪ This is postprandial (2 hours after meals) ○ This test is done by giving an oral dose of glucose ▪ Oral Glucose Tolerance Test (OGTT) of 75 grams of glucose - With signs of HYPERglycemia, do a random glucose screening ○ Anything over 200 mg = DM Gestational Diabetes- ANY FORM/DEGREE OF HYPERGLYCEMIA is teratogenic and can cause abnormalities - Diagnostic Criteria: ○ FBG = 92+ ○ 1 hr = 180 mg/dl or higher ○ 2 hr = 153 - Treatment○ Preferably treated with INSULIN supplements ○ Or can use glyburide or Metformin Type I DM- IT IS A MULTIFACTORIAL DISEASE ○ 3 things cause Islet cell destruction○ Genetic predisposition ▪ Genetics□ Diabetes can aggregate in families □ Concordance rate for twins is 50% □ Exact mode of inheritance is unknown The reason someone has Type I DM, the CD4 & CD8 (T-cells) are attacking the ○ Autoimmunity --------------------------------------------------------------------------------------> pancreas and causing a total inability to produce insulin ▪ 90% pts have circulating islet cell antibodies within a year of Dx ▪ Approximately 10% have other autoimmune disorders include: □ Grave's Disease, & Addison's Disease ○ Environmental insult/effects ▪ Viruses are suspected as initiators the insult and causes Type I diabetes ▪ There has probably been a long latency period of the virus in the body with subsequent beta cell loss ▪ Chemical toxins - Signs and Sxs○ SIGNS ANS SXS DUE TO AN ABSOLUTE ZERO AMOUNT OF INSULIN ○ Classic Signs & Sxs = polydipsia, polyuria, polyphagia, & weight loss ▪ Increase the eating but losing weight ▪ Glucose is a very large molecule □ As it move through renal tubule, it filters out as urine and it draws water through osmosis. □ Some weight loss is due to the loss of water weight - And also due to the glucose being excreted as urine and not going into the cells for use/storage □ GLUCOSE IS AN OSMOTIC DIURETIC (polyuria) - Causing the thirst, hunger, and weight loss ○ Most common in younger population (under 30) ○ Leaving untreated can progress to Diabetic Ketoacidosis (DKA) ▪ Can lead to coma & death - Treated through INSULIN (primary), Medical Nutrition Therapy (MNT), and physical activity ○ YOU MUST BE TREATED WITH INSULIN No if's and's or but's ○ Physical activity is very important to any Dx/Treatment plan with DM - Blood Glucose Monitoring○ Fasting Blood Glucose as needed to monitor Diagnoses ○ Need blood glucose monitors when injecting insulin ▪ Type I check a minimum of 4 times per day before meals ○ A1C- check this 3-4 times annually for T1 & T2 ○ Medicare/Medicaid will cover most of these costs Type II Diabetes- Risk factors○ Need a FHx of Type II in a 1st or 2nd degree relative ○ Minority races/ethnicity ○ Signs of insulin resistance (metabolic syndrome)▪ HTN, dyslipidemia, PCOS, acanthosis nigricans (dark streak across the neck) ○ Low birth weight; Maternal Hx of gestational DM during pregnancy ○ Hx of GDM ○ DM related complications▪ Neuropathy, nephropathy, retinopathy (damage to the retina), gastroparesis (extremely bad diarrhea and damage to GI nerves) - Prevention/Delay of Type II○ Target the pt to lose 7% total body wt. loss and increase physical activity to at least 150 min/wk ▪ May prevent diabetes or delay the onset ○ Metformin can be used for prevention of Type II ▪ Used in those with impaired glucose tolerance, impaired fasting glucose or an A1C of 5.7 -6.5% ▪ Especially used in those with high BMI, below the age of 60, and prior to onset of GDM ○ Individualized MNT (med. Nutritional therapy)Patho Page 17 ○ Individualized MNT (med. Nutritional therapy)▪ Registered dietician used to change nutritional behaviors ○ Diabetes Testing for Asymptomatic Adults▪ If they are asymptomatic, of any age, are overweight/obese, or who have at least 1 risk factor = get tested annual ▪ If no risk factors = annual testing at 45 ▪ Repeat every 3 if first test was normal - Etiology○ The presence of insulin resistance ▪ Decreased number of insulin receptors (associated with obesity) ▪ Person is usually producing insulin but there is still hyperglycemia Unmanaged Type II can lead to Beta cell exhaustion and lack □ BUT EVENTUALLY BE….. of insulin production and require insulin injections ○ Beta Cell Failure in the future ▪ Due to exhaustion ▪ Then they will REQUIRE INSULIN INJECTIONS ○ Genetics▪ Concordance rate b/w twins is 90% ▪ No evidence of autoimmunity (like in Type I) - Pathophysiology○ Insulin resistance SEE FIGURE ------------------------------------------------------------------------------------------------------- > ▪ Insulin resistance is the MAIN etiology of Type II DM ▪ Impaired attachment of insulin to the target cell ▪ Results in elevated blood glucose levels ○ Inappropriate liver glucose production (especially at night) ○ Dyslipidemia▪ LDL's & triglycerides are high (HDL's are low!) ▪ Free floating Fatty Acids and Triglycerides will accumulate in the liver… This causes the liver to be less responsive to insulin and results in INAPPROPRIATE GLUCOSE PRODUCTION BY THE LIVER ▪ Dyslipidemia In Type II DM□ There's an eventual decrease in insulin release by the Beta Cells, resulting in abnormal lipid values - Increased LDL's - Increased Triglycerides - Decreased HDL's - The increased Triglycerides & decreased HDL's are indicators of Metabolic Syndrome - Signs and Sxs ○ Hyperglycemia ○ Most common over the age of 40 ▪ Between the age of 30-40, is the grey/unknown zone (Type I most prevalent in under 30) ○ Acute classical signs like in Type I ○ Usually present with signs of complications▪ Vision blurring, fatigue, paresthesias, skin infxn, foot ulcers, vulvovaginitis (yeast infxn) □ Vision Blurring- glucose is chunky causing vessels in the eye to burst.. - Eye starves with no O2 causing death and vision blurring/blindness See FIGUREON SLIDES 54-55 - Treatment○ Dietary management▪ Individualized diet plan to focus on mild-moderate weight loss ▪ Limit fat intake to less than 30% calories from fat ▪ Count your carbs -- should be eating the same number of carbs throughout the day every day ▪ Maintain normal protein levels □ Can be contraindicated with those with kidney disease ○ Exercise!!! ▪ 150 min/wk ▪ Exercise is shown to decrease blood sugar and also promotes weight loss ○ Oral meds▪ Lower blood glucose ▪ Usually start with 1 med, and then can increase number of meds □ Usually start with Metformin then add another if needed ▪ Insulin injections may be needed Prediabetes▪ ▪ ▪ ▪ Diabetes = 126+ Prediabetes = 100-125.9 Normal is 70-100 Significance□ Only applies to Type II DM □ Diagnostic Criteria = - Impaired glucose tolerance- post prandial (140-180) - Impaired Fasting Blood Glucose = 100-125 - HbA1C = 5.7-6.4% □ Diabetes Prevention Study- maintaining good glucose control, is heavily significant in preventing serious complications SEE INSERTS FOR PREDIABETES & TYPE II IN CHILDREN Tests to Monitor and Manage Diabetes: - Glycosylated (HbA1c)○ Goals for diabetics = LESS THAN 7% ▪ If there are other medical issues, the goal is held to below 8% Patho Page 18 Type II in Children○ The obesity epidemic in children has caused a rise in Type II in children Risk Factors- Tests to Monitor and Manage Diabetes: - Glycosylated (HbA1c)○ Goals for diabetics = LESS THAN 7% ▪ If there are other medical issues, the goal is held to below 8% □ More loose with the guidelines due to other health issues ○ Normal = 4-6% - Self-Monitoring of Blood Glucose○ Finger stick Type II in Children○ The obesity epidemic in children has caused a rise in Type II in children ○ Risk Factors▪ Low levels of exercise (no PE in school) ▪ High fat levels in food in school lunches ▪ Coke/Soda/Vending machines in schools ○ Metformin is used to treat/prevent Effects of Catecholamines on Blood Glucose- Epi, and Norepi raise BG levels during times of stress ○ Released by the Adrenal Gland ○ Usually in trauma situations, post-op, and other times of severe stress (bodily stress), they will have hyperglycemia even though they may NOT have Dx DM. - Catecholamines inhibits the release of insulin, and promotes glycogenolysis by converting stored glycogen to glucose Glucocorticoid Hormones and Effects on BG- Raise BG by stimulating the liver to break down glycogen stores - Can actually cause DM in "borderline" persons - CORTISOL drugs (prednisone, etc.) can make it difficult to maintain normal BG levels ○ These drugs are typically given to transplant pts. Which causes them to become Diabetic Acute Complications of Diabetes- ************ Diabetic Ketoacidosis- ***************** ○ Occurs when diabetes is out of control ▪ More common in Type I ○ 3 major metabolic problems▪ Hyperglycemia!!!!! Dangerously high levels of glucose ▪ Ketosis (presence of ketones in the blood) ▪ Metabolic acidosis (ketones are acid bodies) □ Body tries to normalize the acidosis caused by ketones and depletes the stores of NaCO3 ○ Onset▪ Risk Factors: □ Newly diagnosed □ Not taking sufficient insulin (you will die) □ Too little exercise, too much food, Stress, infxn - All of these cause an increase in BG levels ▪ Slow onset over several days…… unlike hypoglycemia ○ Clinical Signs and Sxs: ▪ Classical Signs of DM □ Polyuria, polydipsia, polyphagia ▪ Abdominal pain/tenderness ▪ Fruity Breath (due to ketones in the blood) ▪ Kussmaul's Respirations ▪ Hypotension/hypovolemic (due to polyuria) ▪ Decreased Level of Consciousness □ Will progress to coma if no intervention (INTERVENTION MUST BE INSULIN) ▪ Death can result from metabolic acidosis and hypovolemic shock ○ Pathogenesis▪ See figure -------------------------------------------------------------------------- > ▪ Body switches from carb metabolism to fat metabolism ▪ Ketones are intermediate products from incomplete metabolism of fat □ Will be able to measure ketones in the blood and urine ▪ Ketones are acid bodies, causing acidosis □ Normal pH is 7.35-7.45 ▪ Kussmaul's Respirations: Body will try to compensate with increasing respirations (very rapid deep respirations) □ Body is trying to blow off CO2, to balance the acid levels in the body ○ Lab Findings: ▪ Hyperglycemia (Blood Glucose above 250 mg/dL) ▪ Low Bicarbonate (less than 15) ▪ Decreased pH/acidic (less than 7.3) ▪ Ketonemia & Ketonuria □ Ketones are present in the blood and the urine ▪ Sodium levels are low & Potassium levels are elevated □ DKA causes hyperosmolality of extracellular fluid □ Thus Intracellular Water & K+ shifts to the extracellular component □ This causes a "pseudo-hyponatremia" due to the intracellular-extracellular fluid shift - AKA sodium levels are relatively low ○ Treatment▪ GIVE IV INSULIN ▪ Replace low electrolytes and monitor them every hour ▪ Usually admitted to the ICU ▪ Need to identify the underlying cause then treat the cause - Hypoglycemia○ Blood glucose lower than 53 or 70 mg/dl ○ Acute complication of DM ▪ Requires VERY FAST INTERVENTION to prevent coma and death ○ Etiology▪ Too much insulin or oral agents (metformin), ▪ Too much exercise, ▪ Too little food Signs and SxsPatho Page 19 You're literally starving your cells, and they NEED energy ○ Signs and Sxs▪ Confusion, HA, slurred speech, hunger, hypotension, diaphoretic, pale, tachy □ Hypoglycemia in children are usually denoted by changes in physical behavior ▪ Sweaty, pale, cool, clammy & increased HR due to the stress of the situation ▪ Each personal responds differently ▪ Sometimes, the person can be unable to feel the effects of low BG □ Called Hypoglycemia Unawareness □ Very dangerous… will go straight into coma if unaware of sxs ○ Pathophysiology▪ Low BG means that the cells are starving and unable to conduct proper cell functions □ i.e. the BRAIN MUST HAVE GLUCOSE ▪ The sympathetic nervous system is activated □ Note the signs and sxs ○ Treatment▪ Administer 15 g of glucose (15 x 15) □ Candy, orange juice, etc. ▪ Then follow with complex carb □ Milk, bread, etc. ▪ If unconscious, give IV 50% glucose □ Glucagon can be given to Type I pt. - Hyperglycemic Hyperosmolar State (HHS)○ Hyperglycemia above 600 mg/dl ▪ Higher than in DKA ○ Plasma osmolarity above 320 mOsm/L ○ Dehydrated due to increased osmolality (review) ▪ This is NOT ketoacidosis (there is not collection of ketone bodies) ○ Depressed sensorium▪ Limited ability to respond cognitively to situation ▪ Different from clinical depression ○ Can cause cerebral edema due to hyperosmolality! ▪ Includes severe potassium loss and severe dehydration □ Potassium loss results from the diuretic actions of the hyperosmolar state ○ Main focus is HYDRATION….. Not insulin ○ Seen most frequently in elderly people with Type II due to the insidious onset ○ Complications▪ Severe K+ loss ▪ Cerebral edema (and its effects) ▪ Severe Dehydration QUESTIONS: - Hypoglycemia blood glucose is below 53 mg/dL - DKA blood glucose is above 250 mg/dL - Normal FBG = less than 100 mg/dL - Hypoglycemia is usually felt with a glucose level of Less than 50-60 mg/dL - Treat hypoglycemia with GLUCOSE IV ○ Rule of 15: Give 15 g of glucose every 15 min for x3 doses - Treat DKA with IV INSULIN ○ Also need to replenish electrolytes (Na, K, PO4, Mg) Chronic Complications of DM- Occurs in both Type I & II DM ○ DM complications are a major cause of blindness, amputations, and the need for dialysis - DM is a major risk factor for development of CAD resulting in MI ○ The most common COD in DM pt.'s is CARDIAC COMPLICATIONS - Types of Chronic Complications: ○ Peripheral Neuropathy (nerve damage… think of foot ulcers, etc.) ○ Nephropathy ○ Retinopathy ○ Skin lesions & foot ulcers - Pathophysiology of Chronic Conditions○ Polyol Pathway▪ Hydroxyl Groups (OH-) on the glucose are converted to Sorbitol & Fructose □ Sorbitol causes swelling and clouding in the lens of the eye (NOT retinopathy) ▪ Polyol Pathway affects the eye lens, kidneys, nerves, & blood vessels ○ Formation of Glycoproteins▪ Glycoproteins are usually found in the basement membranes of capillaries ▪ Increased levels of blood glucose favors the formation of even more of the Glycoproteins □ Causes a disruption of capillary exchange due to narrowing of the vessel ▪ Affects the Eye, Kidney, & Vascular System ○ Tissue oxygenation ▪ RBC dysfunction that interferes with the release of O2 from the hemoglobin ○ Protein Kinase C▪ Protein Kinase C is an intracellular signaling molecule □ Regulates vascular functions: - Permeability, vasodilation, endothelial activation, & growth factor signaling ▪ DM causes an increase in Protein Kinase C □ Activation of PKC in the retina, kidney, & nerves can cause vascular damage □ Also causes disorders in mitochondrial function - Blindness/RetinopathyDon't know statistics, but know the ADA recommendation ▪ Annual dilated pupillary exam ○ Diabetes is the leading cause of new blindness ▪ Review why Retinopathy occurs Patho Page 20 Sympathetic Response to Hypoglycemia- The brain is spazzing out due to no Glucose Fuel - Initiates panic mode (sympathetic responses) ○ Increased HR, diaphoresis, etc. - Lack of glucose fuel also causes the brain to act funny.. ○ HA, confusion, slurred speech, etc. ▪ Review why Retinopathy occurs - Kidney Disease○ Diabetes leading cause of kidney failure (ESRD) ▪ Need an annual microalbumenuria exam □ There should be absolutely no protein in the urine □ Kidneys cannot filter proteins… if there are proteins, then there is a sign of renal failure/disease - Neuropathy○ Majority of DM population has some form of nerve damage ○ Recommendation is to check their feet without shoes/socks at every provider visit ▪ Looking for hair loss, thickened nails, check their sensation ○ Foot and Leg▪ Thickening of the basement membrane of the capillaries supplying the nerve □ Decreased blood flow can lead to necrosis ▪ Demyelination occurs causing a slowing in nerve conduction ▪ Sensory neuropathy = loss of pain/pressure sensation □ Injuries go unnoticed ○ Foot Care**SEE SLIDE** ----------------------------------------------------------------- > ○ Preventing Peripheral Neuropathy▪ Control blood sugar!!!!!! ▪ Daily inspection of feet ▪ Always wear shoes inside and outside ▪ Don't use heating pads ▪ Break in new shoes gradually ▪ Trim nails carefully DCCT Research Conclusions- Intensive therapy with insulin-dependent DM, delays the onset and slows the progression of retinopathy - Intensive therapy reduces the risk of albuminuria (protein in the urine) and thus slows the progression of End Stage Renal Disease (ESRD) - Intensive Insulin Therapy reduces the risk of long term complications!!! ○ But there is a 3x risk of HYPOGLYCEMIA Management of Diabetes in Adults: (includes both Type 1 & Type 2) 1. Dietary Management 2. Rx for exercise (150 min/week) 3. Hyperglycemic Control ○ Control through insulin administration or oral agents (except Type I) or both 4. Monitor Blood Glucose levels 5. Monitor Blood Pressure ○ Must be lower than 130/80 ○ Achieved through ACE Inhibitors or ARB ▪ Usually need to use 2+ agents to keep BP down 6. Manage Dyslipidemia○ LDL's between 70-100 ○ HDL above 50 ○ Triglycerides below 150 - Change their lifestyle! ○ Increase activity, promote weight loss, and smoking cessation Understand insulin from the perspective she has taught us… don't worry about the specifics that are on the slides - Specific insulin drugs and patterns don't worry about it - JUST KNOW HOW TO TREAT WHAT DISEASE PROCESS: by either using insulin, glucose, other, etc. Module 2 | Stress & Adaptation: FOCUS- Definitions on the slides - Know all of the factors that affect the ability to adapt to stressors ○ Psycho & physiology - Know the individual neuro hormones and their effects ○ Individuals may respond differently to the same stressor if they’ve had it repetitively? ○ May be interpreted differently b/w individuals - Understand the process in F/F - PSNS & SNS - Stages in the GASystem ○ Alarm and what happens ○ Etc. - Terminology, hormones, REVIEW THE POWERPOINT!!!! DON'T ADD TO CONTENT OR GO TOO DEEP - SERIOUSLY… READ THE FUCKING POWERPOINT DUDE - Ms. Glaze said this word for word. STRESS- Defined as the body's nonspecific response to a demand placed on it ○ Nonspecific response = increased HR, etc. ○ Also specific responses… know the difference - 3 tiers of stress: ○ Homeostasis ▪ State of constancy in which stress & stressors cause disruptions in the steady state ▪ Ability of a system to remain stable by regulating variables affecting the system ○ Stress Response ○ Adaptation - Stressors = event or environmental agent responsible for initiating the stress response ○ Can be environmental stressors or physiological (trauma, s/p, temp changes, etc.) ○ Endogenous or exogenous ▪ Endogenous- dehydration, chronic illnesses, etc. ▪ Exogenous- debt, relationships, social activities, etc. Homeostasis: - See definitions from slide - Dynamic balance b/w the autonomic balance ○ Balance b/w the Sympathetic NS & Parasympathetic NS Patho Page 21 Terms to Know Definition Stress The body's nonspecific response to a demand placed on it Stressor Event or environmental agent responsible for initiating the stress response Homeostasis A state of constancy (stress and stressors lead to on it Homeostasis: - See definitions from slide - Dynamic balance b/w the autonomic balance ○ Balance b/w the Sympathetic NS & Parasympathetic NS - Control Systems: ○ Acts to maintain homeostasis **SEE FIGURE** ○ The figure is an example of a negative control system ▪ Most of the body has negative feedback/control systems ○ Negative Feedback Loops▪ Insulin/glucose regulations ▪ Once the needs have been met, secretion is stopped ○ Positive Feedback Loops▪ Keeps giving more and more and keeps increasing ▪ Ex: L&D- release of oxytocin during labor, and it continues to release oxytocin until delivery is complete Internal & External Factors in Stress- External○ Adverse physical conditions (pain, hot/cold, etc.) ○ Stressful psychological environment (bad relationships, poor working environment, etc.) - Internal○ Physical (infxns, illness, inflammation) ○ Psychological (anxiety, intense worry about an event that may or may not occur) - Stressors: ○ Stressors change the internal environment of the body ▪ This yields signs & sxs ○ Then the general adaptation response helps maintain homeostasis ▪ This yields the signs & sxs of the General Adaptation Syndrome General Adaptation Syndrome- General stress response 1. Alarm stage - Immediate response to the stress 2. Resistance stage - Body begins to cope with the stress 3. Exhaustion stage - Resources completed out and signs of "wear and tear" or systemic damage appear Interactions of Integrative Systems in the Stress Response: - SEE FIGURE - Cerebral Cortex○ Responsible for focused attention, cognition, being vigilant, - Thalamus○ Relay center (very important) ○ Sorts the message coming in and distributes sensory information - Limbic system○ Associated with emotional components of the stress response ▪ Fear, excitement, rage, anger, ○ Also acts on the hypothalamus - Hypothalamus○ Coordinates response of the endocrine and the ANS ○ Releases CRF which acts on the Anterior Pituitary to release ACTH ○ ACTH acts on the Adrenal Cortex to release Cortisol ▪ Cortisol alters glucose/fat/protein metabolism and suppresses the immune & inflammatory responses Hormones and the Stress Response (neuroendocrine response)- All of the responses of stress are strongly influenced by the neuroendocrine system ○ These responses result in increased energy for the body to use in the Fight/Flight response - Cortisol = INCREASED RISK OF INFXN Norepinephrine & Epinephrine: - Origin: Locus ceruleus, adrenal medulla - These are the catecholamines - Function○ Decrease insulin release ○ Increase in glucagon release ▪ Results in elevated blood sugar levels ○ Increase HR, cardiac contractions, ○ Relaxes bronchial smooth muscles (bronchodilation) Corticotropin Releasing Factor- In the hypothalamus - CRF essential in the endocrine component of the neuroendocrine response - Stimulates ACTH to release from the anterior pituitary - Increases ANS activity in the locus ceruleus - CRF acts on the anterior pituitary therefore reproductive processes are affected by this ACTH- Anterior pituitary - Stims the synthesis and release of cortisol from Adrenal Cortex Patho Page 22 Stressor Event or environmental agent responsible for initiating the stress response Homeostasis A state of constancy (stress and stressors lead to disruptions in the steady state). - It is the ability of a system to remain stable by regulating variables that affect the system Coping The process (coping strategies) of creating a new balance/homeostasis as result of a stressor Adaptation Person has developed a new balance with the stressor and the ability to deal with that stressor - Also that person will not respond the same way as previously done so with a same stressor… they've learned to cope - CRF acts on the anterior pituitary therefore reproductive processes are affected by this ACTH- Anterior pituitary - Stims the synthesis and release of cortisol from Adrenal Cortex Cortisol- Adrenal cortex - Known as the stress hormone ○ Regulates the stress response - Potentiates the actions of epi and glucagon - Inhibits the release and actions of reproductive hormones and TSH's ○ These are not necessary in times of stress - Produces increased risk of infxn (Decreased immune activity) and decreased inflammation - Increases blood glucose for energy for the body ○ Can help maintain glucose levels and enhances the effects of the catecholamines Aldosterone- Adrenal cortex - Increases sodium reabsorption in the kidneys ○ Water follows salt = increased BP/Blood volume etc. **Remember: - Epinephrine results in decreased insulin release and increased glucagon release to increase the amount of serum blood glucose (gluconeogenesis/glycogenolysis) ADH- Also called vasopressin - Hypothalamus, posterior pituitary - Actions○ Increases water reabsorb in kidneys ○ Causes vasoconstriction ○ Stimulates the release of ACTH ▪ Particularly in response to stress/hypotension/fluid volume loss/hemorrhage □ Extreme stress!!! Responses to Stress- Physiological Responses○ Increased HR, BP, O2 intake (bronchodilation, increased ventilation) , ▪ Epi works as vasoconstriction to direct blood to tissues that need it (vital organs) □ Skin becomes pale, urine production/GIT decrease ▪ Increases HR, increases BP, inhibits GI activity, etc. ○ Increased serum glucose ○ Decreased inflammatory response & immune responses - cortisol ○ Pupil dilation (epi) ○ Reduced peristaltic action (reduced GIT) ○ Increased alertness - Psychological Responses: ○ Anger, rage, fear, ▪ Anxiety- dread, uneasiness, not related to any identifiable form of danger ○ Psychological Responses can result in obvious Somatic Symptoms▪ Anorexia, nausea, vomiting, ab cramps, diarrhea, flushed skin, diaphoresis ▪ Chest pain Autonomic Nervous System- Regulates BP, GIT responses to food, focusing eye, thermoreg., etc. - Know the difference b/w sympathetic (fight or flight responses - prepares the body for strenuous physical activity) & parasympathetic (rest & digest - person sitting quietly, resting) Sympathetic Response Parasympathetic Response Dilation pupil Decreased salivation Increased HR & BP Vasoconstriction Pupil constriction Increase salivation Decreased HR Arterial vasodilation Bronchodilation Decrease GIT motility Bladder relaxation Increased GIT motility Bladder constriction Immune system responses to stress- DUE TO CORTISOL - Various effects○ Decreased immune cell production ○ Decreased activity in the thymus ▪ Atrophies and few Tcells being produced ○ Changes in the type of immune cells are produced - Stress of individual's immune system is different from person to person Coping and Adaptation- Adaptation- person has created a new balance amidst the homeostasis imbalance - Factors Affecting Adaptation○ Physiologic and anatomical reserves▪ Greatly influences how people adapt ▪ Elderly people have depleted reserves of their body (especially with chronic illness) and they get run down quickly due to stress □ Increased R/o infxn Time Patho Page 23 ○ Time ▪ Adaptation most efficient when changes occur gradually ▪ Slow chronic blood loss = no signs of shock / rapid hemorrhage = shock ○ Genetic Environment ▪ Genes affect coping (alcoholism) ▪ Susceptible to depression, anxiety, etc. ○ Age ▪ Infants have impaired kidney fxn, older people are more susceptible to disease, etc. ▪ Infants and elderly are both affected in their ability to cope with stress ○ Gender ▪ Sex hormones result in the different ability to cope □ Males hypothalamus produce more CRF & ACTH than the premenopausal female □ Premenopausal women have lower activation of the Sympathetic NS in response to stressors ○ Health status- effects the reserves discussed above ▪ Mental and physical health status impact ability to cope ○ Nutrition ▪ Essential nutrient deficiencies impact health status and thus the ability to cope □ Alcoholics & obesity can lead to malnutrition ○ Sleep/wake cycles ▪ Sleep is the restoration period! ▪ Alteration in the cycle affect immune fxn ○ Hardiness ▪ Personality trait Sense of control over the environment ▪ Sense of having a purpose in life ▪ Sees the stressor as a challenge rather than a threat ○ Psychosocial factors▪ Social environment are a resource. People who can mobilize strong social resources are better able to strand negative effects of stress of their health ▪ Can have positive & negative resources □ Helpful people or degrading people/no people at all □ Can impact the person's ability to cope with stress Stress related health problems- Stress response is supposed to be acute and controlled by negative feedback - If its' chronic, it can lead to long term health problems - Example: ○ SEE FIGURE ○ PTSD!! ▪ Example of chronic activation of the stress response as a result of experiencing a significant traumatic event □ Traumatic events have the ability to provoke fear, horror with the threat of injury or death ▪ Experience of traumatic events can lead to HTN, asthma flares, etc. ▪ Psychological events can lead to stress responses ▪ Sxs□ State of intrusion, avoidance, hyperarousal (startle reflex, paranoid, etc.) - See Figure of the whole body and effects of stress Treatment of Stress- Relaxation techniques ○ Guided imagery ○ Music therapy ○ Massage therapy ○ Biofeedback ▪ Allows the person to learn to control physiologic fxn - These are used to relieve stress in a healthy manner instead of drinking LOL Patho Page 24 Exam 2 Thursday, September 21, 2017 8:54 AM Module 3 | PainPain- Definition- multidimensional experience - Unpleasant sensory/emotional experience associated with actual or potential tissues damage - Pain is subjective ○ It is whatever the pt. says it is ○ THE PATIENT IS TH-….. HOLY FUCK NOT AGAIN ▪ Pain means different things to different people based on experiences Somatosensory System- Provides the CNS with info related to deep and superficial body structures - Awareness of those deep and superficial parts in terms of temp, position, pain & pressure/touch ○ Each of these sensations is innervated by a specific type of nerve fiber… - 3 TYPES OF FIBERS○ A Fibers▪ Myelinated, and has the fastest rate of conduction ▪ Conduct, pressure, hot/cold, touch information ▪ RELAY ACUTE PAIN ○ B Fibers▪ Myelinated ▪ Transmit information from cutaneous and sub q receptors ○ C Fibers▪ Unmyelinated ▪ Smallest diameter = slowest conduction ▪ Conduct warm/hot, mechanical & chemical sensation, and heat/cold induced pain ▪ RELAY CHRONIC PAIN - 3 levels of neurons○ First order▪ Detect sensation and transmit sensory info from periphery to the CNS (spinal cord) ○ Second Order▪ Communicates with reflex responses and sensory pathways in the spinal cord and travels directly to the brain ▪ The impulses travel from spinal cord to the brain □ Into the thalamus & cerebellum ○ Third order▪ Relay from thalamus brain to the sensory cerebral cortex ▪ Sensation is process and….. ▪ Results in the feeling/interpretation of pain ○ *** "PAIN IMPULSES go from the periphery to the spinal cord to the brain" *** - Pain Pathways○ Both parallel pathways that carry info from the spinal cord to the thalamic region in the brain ▪ They take different routes, but all end up at the thalamus ○ Discriminative Pathways▪ Used for rapid transmission of sensory info □ Discriminative touch sensations (fine touch, feeling vibrations, etc.) ▪ Consists of large, myelinated fibers ○ Anterolateral Pathways▪ Ascending pathway conveying pain, temperature & crude sense of touch □ Damage to the anterolateral pathway results in difficulty sensing pain & temperature ▪ Neospinothalamic Tract□ Rapid transmission of sensory sensation using myelinated type A fibers to the thalamus □ Transmission of sharp, fast pain □ Allows pt to localization & identify of the pain ▪ Paleospinothalamic Tract□ Slow pain through unmyelinated type c fibers!!! - Slower conducting, mostly made of type C fibers, to the thalamus □ Concerned with diffuse/dull-aching unpleasant sensations - Doesn't require localization of signal source □ Commonly associated with chronic pain & visceral pain □ Activates part of the sleep/wake cycles (Reticular Activating System) Pain Theory- Pain warns of impending tissue injury, and forces the person to go seek help to fix the injury/pain ○ Functions as an alarm system - Acute and Chronic Pain are the MOST COMMON REASON pt.'s seek healthcare ○ Acute pain results from injury, surgery, infxn, etc. ○ Chronic pain = arthritis, cancer, etc. - Specificity Theory○ Regards pain as a separate sense ○ Evoked by the activity of receptors (nociceptors) that transmit special sense to pain centers in the CNS where the pain is interpreted - Pattern Theory○ Pain signals are sent to the brain when stimuli come together in a specific pattern Patho Page 25 ○ Pain signals are sent to the brain when stimuli come together in a specific pattern ▪ i.e. "light touch" is sensed as "touch", whereas "intense pressure" is sensed as "pain" - Gate Control Theory○ Pain impulses are felt when the gate (threshold) is opened at the spinal cord, in response to an excess of nociceptive impulses ▪ Pain threshold - the point at which the pain is felt □ Each pt has a different threshold □ Each pt has different things that can work/not work to keep the gate closed ○ Closing the gate occur with interventions of nonpharm controls ▪ Closing the gate = the pain is not felt ○ Can be hindered by stress or increased by exercise (increase of endorphins = increasing threshold) - Neuromatrix theory○ Brain contains widely distributed neural network (thalamus, limbic system, somatosensory) ▪ This network involves the interpretation of multiple sensory inputs ○ Can result in the feeling of pain even when it's not there ▪ PHANTOM LIMB PAIN Nerve Fibers- See figure --------------------------------------------------------------------------------------------------- > - A Fibers○ Large, myelinated, Fast, sharp pain ○ Release of glutamate at the synapse with the spinal neurons ○ ASSOCIATED WITH ACUTE PAIN - C Fiber○ Small, nonmyelinated = chronic, slow pain ○ Release glutamate and substance P Pain Mechanisms- Nociceptive Pain○ Initiated by nociceptors in peripheral tissues when there is damage - Neuropathic Pain○ Direct injury or dysfunction of the sensory axons or peripheral/central nerves - Pain threshold○ The amount of stimulus required to elicit a pain response ○ The point at which the nociceptive stimulus is perceived as painful - Pain tolerance○ Maximum intensity/duration of pain that a person is willing to endure before seeking intervention ○ Can't take it anymore! Types of Pain- Cutaneous pain ○ Skin, or sub q tissues (papercuts) ○ Sharp pain with burning qualities ▪ Can be abrupt or slow onset ○ Easily localized pain - Deep somatic ○ Bones, muscles, tendons, joints ○ More diffuse/radiating pain - Visceral ○ Visceral organs ○ One of the most common pains from disease (upset stomach, etc.) - Referred ○ Originates in another place then diffuses to another place where it is perceived Acute Pain vs. Chronic Pain- Acute Pain○ Short-lived, and is resolved when the underlying cause is resolved ("self-limiting") ▪ Initiated by trauma, injury, surgery by activation of nociceptors ○ Initial injury causes nociceptive firing (hyperalgesia), and then a secondary wave of intense acute pain results from secondary responses (inflammation, edema, etc.) ▪ This secondary hyperalgesia can result in the development of chronic pain if not treated properly ○ Treat acute pain preemptively (before it gets too severe) ▪ Increases comfort of the pt and also prevents hypersensitivity of pain centers in the periphery and CNS ▪ Also requires the use of less drugs if treated preemptively - Chronic Pain○ Pain that lasts longer than what is reasonably expected ▪ Pain is sustained by factors that are remote from the initial cause of the pain ○ Most common cause of chronic pain = cancer ○ Highly variable b/w pts▪ Can be unrelenting extreme pain (metastatic bone pain) ▪ Or… continuous w/ periods of escalation (back pain) ○ Serves no protective purpose and interferes w/ QOL & ADL's ▪ Nociceptors are persistently stimulated serving no useful protective purpose ○ Causes psychological, physiological, familial, and economical stress ○ Different Levels of Chronic Pain Sensations▪ Peripheral- (Peripheral Sensitization) □ Persistent stimulation of the peripheral nociceptors □ Inflammatory response increases the sensitivity of the C -Fibers ▪ Peripheral-Central□ Abnormal function of the peripheral and central systems Patho Page 26 □ Abnormal function of the peripheral and central systems □ Results from destruction of descending-inhibitory pathways (endogenous opioids) and the hyperexcitability/continuous firing of new nociceptors □ Ex: PHANTOM LIMB PAIN ▪ Central□ Due to a disease, injury, lesion of the CNS □ Ex: Multiple Sclerosis ○ Management of chronic pain is a COMPLEX PROCESS: ▪ Depends on a lot of factors□ Cause of the pain □ Underlying health problem □ Life expectancy of the individual ○ Best managed by a multidisciplinary team ▪ Anesthesiology, physicians, nurses, PT, surgeons, case management, etc. Altered Pain Sensitivity- Hyperpathia- continued stimulus that is causing the pain ○ Hypersensitive Reaction - Paresthesias- spontaneous, unpleasant sensation ○ Tingling/burning sensation of pins/needles - Dysesthesia- distorted/abnormal sensations ○ Dysfunction in the sense of touch ▪ Ex: Diabetic Neuropathy… can't feel sensations and can't feel pain ○ Most common in skin, scalp, mouth - Hypalgesia- reduced pain sensation - Analgesia- absence of pain - Allodynia- pain after non-noxious stimulus ○ Normal/non-painful stimulus causes stabbing/burning/sharp pain) ○ Ex: fibromyalgia, neuropathies, etc. Morphine- Opioid, CNS depressant, used to relieve the sensation of pain - Serves as an analgesic Neurogenic Inflammation- See figure ----------------------------------------------------------------------------------------------------- > - Inflammation of neurological tissue results in the release of inflammatory mediators ○ Substance P - Once released, these Neuropeptides cause the release of Histamine from the Mast Cells ○ Histamine from Mast Cells = inflammatory response ○ Antihistamines reduce the release of histamines - Results in increase of substance P which starts the process over again ○ Ex: Migraine- Trigeminal Nerve stimulation results in inflammation… inflammation causes the severe pain Causes of neuropathic pain- Pressure on the nerves (tumors) - Physical/chemical injury to neuron - Infxn of neuron - Ischemia (lack of O2 in the tissues) - Inflammation Neuropathic pain syndromes- Pain the originates from peripheral nerves injured or in diseases - Includes widespread, unexplainable pain - Examples: ○ Trigeminal neuralgia ○ Postherpetic neuralgia ○ Phantom limb pain ▪ Neuropathic pain following amputation of body ▪ 70% of amputees experience phantom limb pain ▪ Begins as tingling, cramping, shooting pain □ Can go away, or continue to chronic pain ▪ They can experience pain sxs that are present before the amputation □ They had an ulcer before, and can still feel the pain from the pressure ulcer even when the limb is gone…. ▪ Regenerating nerves get trapped in scar tissue Check what is in the book/ lecture Pain in children- Pain can be felt from neo-natal on.. - Children remember pain & can report pain at 3 yrs. - Use numeric & picture scales ○ Also look at physiological responses to pain in younger children ▪ Crying ▪ Lack of playing ▪ Lack of eating, etc. - Treat using nonpharmacologic and pharmacologic pain ○ Requires ongoing assessments to manage the pain properly ▪ Look at their behavior, functioning, playing, etc. Pain in older adults- Pain increases with age ○ Unrelieved pain can affect cognitive, emotion, and functional ability - Decreased QOL Patho Page 27 - Decreased QOL ○ Decreased appetite, decreased sleep quality, etc. - Pain is easier to assess if the pt. is lucid - Use nonpharmacologic methods FIRST because drug metabolism is impaired in adults ASSESSMENT- Pain is subjective and cannot be measured objectively ○ Some things can be measured objectively (pulse, BP, etc.) - Eliminate the cause of pain instead of treating the sxs - Get a complete health history ○ COLDSPA - Use numeric pain rating scales INTERVENTION- Nonpharmacological Interventions○ Cognitive behavioral interventions ▪ Relaxation techniques ○ Biofeedback ○ Distraction ○ Heat/cold therapy ○ TENS- electrical stimulation (STEM) - Pharmacological Interventions○ Use of narcotic & nonnarcotic analgesics to manage pain ▪ Adjuvant meds- increase the effect of other meds ○ Analgesics eliminate pain w/o effecting LOC ▪ They DO NOT cure the underlying cause ○ USE ANALGESICS ONLY WHEN THEY ARE NEEDED!!! ▪ This prevents the development of addiction/dependencies ○ May need to increase dosages of long term meds… ▪ Body becomes used to the effects and results in hyperalgesia… ○ Non-Narcotic Analgesics▪ Aspirin & NSAID's□ Antipyretic & anti-inflammatory effects □ Work by inhibiting the COX-enzymes ▪ Acetaminophenonly fever is □ Equal to NSAID's WITHOUT an anti-inflammatory effect only fever is ○ Opioid Analgesics▪ Morphine & Codeine ▪ Group of meds w/ Narcotic effects □ Work on the opioid receptors in the CNS □ Provides analgesia, BUT also causes DEPRESSES THE RESPIRATORY EFFORT - Always assess the pt respirations before and after administration - Also can lead to constipation due to decreased GIT motility ▪ Used to treat acute & chronic pain ▪ Increase the analgesic effects if you give routinely & preemptively before pain gets too severe reduced and pain is reduced and pain helped is helped Module 7 | Immunology- **She writes her test questions about learning objectives ○ LOOK AT THEM & ANSWER THEM ---------------------------------------------------------------- > Immunology- the study of the protection of disease by a coordinated response of the immune system cells Two types of Immunology- Innate○ This is the first line of defense ○ Early and rapid and lacks an organized attack (irrational jealous girlfriend) ○ Recognizes Self vs. Nonself Cells ○ This includes the▪ Skin, mucous membranes, phagocytic leukocytes, specialized lymphocytes (NK cells) ▪ Phagocytes and NK cells just blindly rush to the intruder ▪ Some cells eat the intruder, and PRESENT THE ANTIGEN (antigen presenting cells) to the other immune cells - Adaptive○ Specific/acquired ○ Slower to respond, more effective approach (rational jealous girlfriend) ○ Recognizes the threat, plans, and attacks ▪ Specialized cells attack the intruder ○ 2 types of responses▪ Humoral- B-cells create antibodies to fight the intruder ▪ Cell-Mediated- T cells activate phagocytes or kill Host cells which holds the intruder SEE THE IMMUNE SYSTEM FLOW CHART - Complement cascade- helps out by getting rid of debris ○ Complement are a group of proteins that rid the blood of the debris from phagocytized cells ○ Enhances the antibody response - Antibodies○ Created in response to a specific foreign substance in the body ▪ Antibodies are unique to that specific antigen ▪ Last forever in the body ○ IGM & IGG ▪ Immunoglobin-M & Immunoglobin-G Patho Page 28 Objectives- Describe the differences between cell-mediated (T lymphocyte) and humoralmediated (B lymphocyte) immune responses, and the major functions of each. ○ Adaptive/Acquired Immune System - Explain the effects of factors such as age, nutritional status, and emotional stress on immune system function. ○ Factors affecting immune response - Describe etiologies, pathophysiology, and clinical consequences of primary and secondary immunodeficiencies. ○ Immunodeficiency - Define hypersensitivity and the difference between immediate and delayed hypersensitivity. ○ Hypersensitivity - Describe the mechanisms producing Type I, Type II, Type III, and Type IV hypersensitivity reactions, and cite an example of each. ○ Four Types of Hypersensitivity - Cite common agents which can cause systemic anaphylaxis. ○ Common antigens - Describe the pathophysiology and signs and symptoms of systemic anaphylaxis or anaphylactic shock. ○ Signs & Symptoms - Discuss the concept of autoimmunity and cite at least one example of an autoimmune disorder. ○ AUTOIMMUNE DISORDERS - State the virus responsible for acquired immunodeficiency syndrome (AIDS) and explain how it infects body cells. ○ HIV is the virus that causes AIDS - Describe the transmission methods of the human immunodeficiency virus (HIV). ○ Transmission - Relate the pathophysiology of AIDS to the development of opportunistic infections, such as pneumocystis carinii, pneumonia, and malignancies. ○ Opportunistic Infxn - Describe the difference between HIV infection and AIDS. ○ Stages of HIV - Describe the role and actions of antihistamines in allergic responses. ○ Antihistamines ○ Created in response to a specific foreign substance in the body ▪ Antibodies are unique to that specific antigen ▪ Last forever in the body ○ IGM & IGG ▪ Immunoglobin-M & Immunoglobin-G ▪ IGM's indicate initial exposure to an antigen □ "M" = meet… you can only meet someone one time ▪ IGG's are the established antibodies that continue circulating □ "G" = greet… you can greet someone infinite times, but only meet someone one time □ IGG's indicate if someone has immunity over something (titers) ○ Some antibodies can be received from Mother (IGG) or through vaccination (passive immunity) ▪ IGG's cross the placenta and give the baby immunity Adaptive (Acquired) Immune System- Objectives - Humoral○ Defend in the blood and mucous (humorous) ○ B cells produce antibodies ○ B cells recognize the antigen differentiate into plasma cells and then secrete specific antibodies ○ Antibodies connect to antigens floating in the blood or the SURFACE of cells - Cell-Mediated○ T-cells are located INSIDE the cell (B cells cannot get here) ○ Recognize antigen-presenting cells by receiving the signal from the B-cells ○ Helper T-cells- (CD4) ▪ Helps regulate almost all other immune cells ▪ Release cytokines to help signal antigens for further destruction/help from other immune system cells ○ Cytotoxic T-cells- (CD8) ▪ Kill the intracellular antigens ▪ Inject enzymes into the cell where viruses/cancers/bacteria are and induce apoptosis Factors affecting immune response- Objectives - Age○ Newborns ▪ Thymus is fully functional and full sized at birth □ Thymus = produces Tcells ▪ Don't have a lot of antibodies unless they have IGG's from the mother ▪ Produce IGM's through environmental exposure after birth □ Takes about a year for them to get to adult level immune responses (IGG) ○ Elderly▪ Decreased immune fxn ▪ Possibly due to atrophy of the thymus (affects Tcells) □ Decreased amount of Tcells and thus the lymphocytes become unresponsive - Nutritional Status○ Malnutrition = decrease in immune cells ▪ (think of this as chronic stress on the body) ○ Obesity = chronic inflammatory response ▪ If the body is chronically dealing with an immune response, then there is a decreased response when an actual intruder enters the body ▪ "Boy who cried wolf" - Stress = Suppresses immune response (herpes/cold sores flare during stress) Hypersensitivity- Objectives - Whole group of disorders of the immune system being too responsive to a NONPATHOGENIC SUBSTANCE/ANTIGEN - Immediate Response- Type 1 Response ○ Rapid rxn to the antigen ○ Within minutes ○ Range in severity from itching, hives, to anaphylaxis - Delayed Response- Type 4 response ○ 24-72 hrs to respond ○ Ex: TB skin test - Body produces IGE for each allergen ○ IGE communicates to the MAST CELLS and the Mast Cells produce HISTAMINE ▪ Histamine causes the allergic rxn that we know □ Rhinitis, SOB, edema, anaphylaxis, etc. - Hypersensitivity can be delayed/manifest later in life… ○ Exposure can occur during an time of weakened immune system… causing the body to create antibodies ○ Exposure to high enough levels to reach the threshold of an allergic response ▪ Can accumulate enough exposure of an antigen/allergen to develop a true hypersensitivity ○ Moving to a new area (outdoor/seasonal allergies) - Four Types of Hypersensitivity- Objectives SEE FIGURE -------------------------------------------------------------------------------------------------- > **know the difference b/w immediate and delayed and the signs/sxs of what those responses are! ○ Type 1 = immediate responses ▪ IGE acts on the mast cells to release histamine ○ Type 2 = drug allergies ○ Type 3 = Serum sickness (blood stuff…. Don't worry about it…) ○ Type 4 = delayed rxn Patho Page 29 ○ Opportunistic Infxn - Describe the difference between HIV infection and AIDS. ○ Stages of HIV - Describe the role and actions of antihistamines in allergic responses. ○ Antihistamines - Describe the applications for immunosuppressive drugs. ○ Treatments - Explain the use of glucocorticoids in immune system disorders. ○ Treatments - Describe the major types of antiretroviral drugs used in the treatment of HIV/AIDS and their mechanism of action ○ Antiretrovirals Basophils & eosinophils = fungal infxn ○ Type 1 = immediate responses ▪ IGE acts on the mast cells to release histamine ○ Type 2 = drug allergies ○ Type 3 = Serum sickness (blood stuff…. Don't worry about it…) ○ Type 4 = delayed rxn ▪ Tend to be less serious (contact dermatitis, chronic asthma/allergies) - Anaphylaxis○ Life threatening allergic response characterized by: ▪ Widespread edema ▪ Bronchospasms ▪ Vascular shock (vasodilation) due to Histamine release ○ Previous exposure to antigen creates IGE antibodies ▪ The level of the allergic response depends on the number of IGE antibodies produced (aka.. The level of sensitivity) ○ Exposure Methods▪ Ingestion- food/medication ▪ Injected- bee venom/medication ▪ Absorbed- through skin or GIT ○ Signs & Symptoms- Objectives ▪ Hives, itching, erythema ▪ Dyspnea ▪ Vomiting, diarrhea, cramping ▪ Edema & angioedema (swelling of the face) ▪ Airway obstruction- caused by laryngeal spasms and laryngeal edema □ Can impair intubation procedures ○ Common antigens- Objectives ▪ Food, insects, drugs, latex □ Most common drug allergy = Beta-Lactam Abx (Penicillin) - Also Aspirin, NSAIDS, ▪ Exercise & temperature -- aka.. The body can get a hypersensitivity to literally anything Antihistamines- Objectives - Histamines are potent vasodilators ○ Respond to the antigen exposure within 5-30 min ○ Increase capillary permeability, smooth muscle contraction, and bronchoconstriction - Antihistamines block histamine release and treat the symptoms such as edema, rhinitis, hives, etc. - Examples: ○ Diphenhydramine (Benadryl) ○ Loratadine (Claritin) ○ Cetirizine (Zyrtec) ○ ALL CAUSE DROWSINESS AUTOIMMUNE DISORDERS- Objectives - Body is unable to recognize self vs. nonself - Cause unknown: ○ Can be genetic, and/or environmental, or caused by infectious agents (viruses) - Can effect almost any type of cell or tissue ○ Systemic Autoimmune Disorder▪ Can cause painful/swollen joints, fever, fatigue, swollen lymph nodes ▪ Examples: □ Systemic lupus erythematosus (SLE) - Hereditary and more common in women - Rash on the face - Swollen lymph nodes □ Rheumatoid arthritis ○ Blood Autoimmune Disorder▪ Autoimmune hemolytic anemia □ Body attacks RBC and lysis them ▪ Idiopathic thrombocytopenia purpura □ Body attacks platelets and leads to petechieae and bleeding ○ Other▪ Hashimoto Thyroiditis □ Severe atrophy of thyroid = hypothyroidism ▪ Type 1 DM □ Destruction of the pancreatic beta cells = lack of insulin production ▪ Crohn's Disease □ Issue w/ innate immunity and the body can't tolerate specific forms of natural bacteria (flora) in the GIT - Treatments- Objectives ○ Treat the mechanism that is underlying the disorder ○ Corticosteroids and immunosuppressives can stop, slow down or reverse symptoms ○ Immunosuppressive▪ Prevents DNA synthesis of WBC and prevents replication of the cells causing immune cell death ▪ Drugs don't work on specific cells, they suppress all types of WBC ▪ Educate pt on the importance of hygiene and preventing exposure w/ sick people ○ Steroids▪ Suppressing inflammatory response for disorders like RA & lupus □ i.e. swollen joints, lymph nodes, etc. ▪ Severe side effects can occur depending on dosage and length of schedule □ Wt gain □ Cushing's disease (buildup of cortisol = buffalo hump, moon face, etc.) Patho Page 30 Antibodies attack the thyroid causing atrophy □ □ □ □ Cushing's disease (buildup of cortisol = buffalo hump, moon face, etc.) Osteoporosis Pregnancy complications Glaucoma Immunodeficiency- Primary Immunodeficiency○ Congenital or inherited (rare but there are a lot of these) ▪ Genetic mutations, recessive genes, X-linked disorders, etc. ○ Pathophysiology▪ Mutations cause a lack of development of immune system cells ▪ Mimic the symptoms of autoimmune disorders ○ Early detection is critical because the primary deficiencies are FATAL in Children ▪ Family Hx is important because remember this is GENETIC ○ Notice primary immunodeficiencies by recurrent, persistent, or unusual infxn ▪ They will get the same type of infxn over and over and over ▪ The type of infections can help diagnose the immunodeficiency - Secondary Immunodeficiency○ Secondary is acquired ▪ AIDS most common secondary immunodeficiency ○ Much more common than primary ○ Caused by a pathogen, aging process, malignancies, malnutrition, drugs, etc. ○ Pathophysiology▪ WBC dysfunction □ There is an overall loss in the amount of IGG's - Makes you more susceptible to secondary infection □ Deficit in T-cell numbers and function ○ No cure for these disorders ○ Congenital transmission is possible (HIV+ mother) ○ Remember…. They are IMMUNOSUPPRESED and susceptible to secondary infxn T-cell deficits leave you more vulnerable to viral & fungal infections & Opportunistic infections B-cell deficits increased bacterial susceptibility - HIV/AIDS○ HIV is the virus that causes AIDS ▪ CD4 (Type of T-cell) count below 200 and/or an opportunistic infxn ○ Transmission▪ Can be transmitted through semen, blood, vaginal fluid, breastmilk □ Sexual contact is the most common transmission method ○ Pathophysiology▪ HIV is a retrovirus that kills immune cells □ CD4 Tcells □ Macrophages □ Dendritic cells ▪ Immune Cell Death results in decreased immune response □ EVEN if the person is ASYMPTOMATIC they will have a decreased immune response ▪ Results in increased susceptibility to many secondary illnesses/infections □ (TB, flu, literally anything…) ○ Stages of HIV1. Primary infection□ Can be asymptomatic or have flu-like symptoms 2. Latency period□ Chronic, asymptomatic period □ Can last for years and years and managed well with correct medical treatment 3. AIDS□ Diagnosed by presence of HIV, AND a CD4 Count below 200 and/or an opportunistic infxn ○ Treated w/ Antiretrovirals- Objectives ▪ Medications to treat HIV ▪ Works to decrease the amount of the virus in the body (HIV) □ Goal is to get an undetectable amount of HIV (viral load) in the body and to increase CD4 Count ▪ 5 Classes of Antiretrovirals- ------------------------------------------------------------------- > □ Each class of the drugs try to interrupt the life cycle of the HIV at different points □ Usually combine different types of these drugs to target the HIV replication process at multiple points - HAART (Highly Active Antiretroviral Therapy) = combination of multiple antiretrovirals - Opportunistic Infections- Objectives ○ Decreased levels of the CD4 cells creates susceptible to various conditions that wouldn't be pathogenic in a healthy person ○ Examples▪ Respiratory□ TB, bacterial pneumonia - Higher rate of TB in HIV+ population ▪ GIT□ Oral thrush (esophageal candidiasis) - yeast infxn of mouth/esophagus □ Gastroenteritis □ C.Diff., E.coli, etc. ▪ Nervous□ HANDS - HIV Associated Neurocognitive Disorders Patho Page 31 □ HANDS - HIV Associated Neurocognitive Disorders - Cognitive impairment w/ motor dysfunction - Behavioral issues - Psychosocial issues - Hallucinations □ Toxoplasmosis □ PML - Progressive Multifocal Leukoencephalopathy - Demyelinates white matter in the CNS ▪ Malignancies□ Some forms of cancer are more common in the HIV+ population □ Kaposi sarcoma □ Non-Hodgkin's Lymphoma ▪ Metabolic□ Wasting syndrome - Involuntary loss of 10% of baseline weight - Think of the stereotypical HIV+ pt that is small, skinny, frail □ Lipodystrophy (body is unable to produce fat) □ Insulin resistance Leuko = WBC Encephalopathy = Brain disorder - WBC's are attacking the brain and demyelinating the White Matter Module 4- InflammationCell injury- Cell injury is continually occurring - Reversible/Irreversible○ Reversible allows recovery ▪ Depends on the cell's condition and the level of trauma □ Severe injury can be irreversible ▪ Depends on the blood supply & pt nutritional status ○ Irreversible = apoptosis/necrosis - Etiology of Cell injury○ Physical- mechanical, trauma, electric, etc. ○ Radioactive- Xrays, Sunburns, lasers, ○ Chemical- drugs, toxicity (lead/mercury) ○ Biological- microbes ○ Nutritional imbalances▪ Deficits = decreased protein levels = decreased healing ▪ Excesses = atherosclerosis/obesity/hyperlipidemia Mechanisms of Cell injury- Direct/indirect○ Direct harm comes from a direct source (heat) ○ Indirect- mutation, metabolic disorders, decreased immune response - Main mechanisms○ FREE RADICAL FORMATION ▪ Free radicals- unpaired electron that results in a highly reactive, unstable molecule that react nonspecifically □ Unpaired electron causes Free Radicals to be highly unstable and highly reactive molecules ▪ Free Radicals can produce harmful chain reactions which yield MORE free radicals ▪ Free radicals will react with protein, lipids, & carbs □ Inactivate enzymes □ Damages the cell membrane □ Damage nucleic acids causing DNA damage ○ Hypoxia & ATP depletion ▪ Deprives the cell from O2 and interrupts the oxidative metabolism and effects the production of ATP □ Results in conversion to anaerobic respiration - Results in decreased pH and cell shrinking (buildup of lactic acid) □ Aka… it's a power down of the cell due to lack of ATP ▪ Heat, kidney, brain require large amounts of O2 to perform their normal fxn □ Brain can only last without oxygen for 4-6 min before permanent damage is done ▪ Hypoxia can result from decreased blood flow, anemia, respiratory disease ▪ Cells switch to anaerobic respiration in which there is a buildup of lactic acid □ Decreased pH and decreased cell size ○ Intracellular Calcium Accumulation▪ Impaired Calcium homeostasis ▪ Ca++ fxn as an important messenger & signaling molecule □ Increased intracellular Ca++ activates enzymes that can damage the cells **There is a glitch in the message and enzymes are activated inappropriately Outcomes of Cell Injury- Reversible injury results in swelling and fatty changes - Irreversible (death) results in apoptosis &/or necrosis ○ Apoptosis- controlled cell destruction ▪ The mechanisms the body uses to remove and replace cells if the cells were made in excess, developed improperly, or are worn out ○ Necrosis- cell death ▪ The cell will swell w/ lots of fluid and junk ▪ The cell membrane will rupture ▪ This will cause inflammation Cell Injury Process- Cell will adapt to stressors to keep fxn normal - Cell injury results when the stresses are too much to handle Patho Page 32 VERY EFFING IMPORTANT Adaptation- Cells adapt to stressors and/or injury by altering○ Size of the cells ○ Number of cells ○ Formation of the cells - Normal adaptation occurs in response to an appropriate stimulus (injury, stress, etc.) and stops once the need for adaptation has stopped (injury is healed, stress is resolved, etc.) - Changes in Cell Size○ Atrophy- decrease in cell size ○ Hypertrophy- increased in cell size ▪ Commonly occurs in the heart muscle/valves ○ Hyperplasia- increase in the number of cells (BPH) ○ Metaplasia- reversible change in which the adult cell is replaced by a different type of adult cell ▪ Chronic smokers- stratified squamous epithelium replaces the ciliated epithelium (smoker's cough) ○ Dysplasia- deranged cell growth.. Changes vary in size, shape, organization ▪ Checking for dysplasia on the cervix when doing a PAP smear Necrosis- Refers to cell death in an organ or tissue that is still part of a living person - The Process: (remember this from above…) ○ Unregulated enzyme digestion of cell components ○ Loss of the cell membrane integrity ○ Uncontrolled release of byproducts into the intracellular space ○ Initiates an inflammatory response - Liquefaction○ Cells die but the catalytic enzymes aren't destroyed ▪ i.e. cells are breaking down even when they are already dead ○ Abscesses soften in the center and discharge the contents - Coagulation○ Acidosis develops ▪ This denatures the enzymes/structural proteins of the cell ○ Usually found in infarcted areas… ▪ THINK…. □ There is a coagulation/clot that is keeping blood from reach the cells □ They are hypoxic and have to switch to anaerobic respiration… □ This leads to acidosis and denaturing of the cell proteins = death - Infarction○ Artery becomes occluded and no other source of blood flow is available ○ Hypoxic injury to the tissues - Caseous○ Form of coagulation necrosis ○ Dead cells persist and are not removed ▪ Looks like round nodules with soft-cheese-like debris ○ Commonly found in TB - Gangrene○ Large mass of tissue has undergone necrosis ○ Gas Gangrene▪ Gangrene that results from bacterial infection ▪ Clostridium- anaerobic-spore forming organisms (in soil!!) □ Prone to occurring w/ trauma or Fx when dirt gets into the wound ▪ Bacteria produce toxins that destroy cell membranes and cause: □ Death of muscle tissue □ Massive spreading edema □ Hemolysis of RBC = anemia - Hematuria & Hemoglobinuria □ Renal failure ▪ Treat with strong Abx and Amputation to stop the infection from spreading Apoptosis- Removal of cells so new healthy cells can replace them (programmed cell death) - Thought to be responsible for normal physiological processes: ○ Embryonic development (cells are destroyed and rebuilt and so on…) ○ Cell death when marked by Cytotoxic T-cells (cell-mediated immunity) ○ Recycling of RBC, WBC w/ new cells - Results in changes in the appearance of cytoplasm contents and nucleus - Extrinsic vs. Intrinsic pathways○ Extrinsic Apoptosis▪ Death Receptor Dependent ▪ Apoptosis under cellular control ▪ The death receptor has to bind to the cells to tell the cells to die ○ Intrinsic Apoptosis▪ Death Receptor Independent ▪ Typically results from an injury ** When a cell is injured it doesn't need the police (death receptors) to give them permission to die…. - BOTH PATHWAYS result in the activation of proteolytic enzymes called CASPACES ○ These enzymes break down proteins and other cell components into smaller components ▪ Thus… this is the apoptosis taking place Inflammation- Reaction of vascularized tissue in response to cell injury/death Patho Page 33 - Reaction of vascularized tissue in response to cell injury/death - Results in○ Increase in inflammatory mediators ○ Movement of fluid and leukocytes from the vascular system to the extravascular tissue ▪ Results in swelling - Inflammatory conditions (-itis) ○ Appendicitis ○ Neuritis - of the nerves ▪ Indicates the body response to an injury/damage/or ischemia Acute Inflammation- Two Stages of Acute Inflammation ○ Vascular stage▪ Increased blood flow (vasodilation, decreased venous return) ▪ Increased vascular permeability □ There is more plasma entering the tissues and leads to edema □ Plasma contains substances that help the tissue heal - Clotting factors help stop bleed and prevent the spread of infection - Antibodies are help to fight infection - Nutrients help feed tissue cells and proteins ○ Cellular Responses▪ Movement of phagocytic leukocytes (mainly neutrophils) from the blood to the injured area □ Margination- slowing of the blood leads to accumulation of WBC □ Transmigration- WBC leave the vessels through the endothelium □ Chemotaxis- WBC follow the chemical trail to get to the site of injury/infection □ Phagocytosis- neutrophils, monocytes, and macrophages are activated and engulf/destroy the microbe/tissues/etc. CARDINAL SIGNS OF INFLAMMATION○ All occurs during acute inflammation ▪ Happens w/in minutes-hours ▪ Acute inflammation is self-limited… □ When the cause of inflammation goes away, so does the inflammation ○ Rubor (redness)- due to vasodilation in the vascular phase ○ Heat- occurs due to vasodilation in the vascular phase ○ Swelling- increased fluid in IS space in the vascular phase ○ Pain- increased fluid in IS space in vascular phase ○ Loss/Alteration of Function- increased fluid in IS space in the vascular phase Chronic Inflammation- Can last from weeks to years - Etiology○ Low grade inflammation conditions ▪ Obesity ▪ Type II Diabetes ○ Inappropriate activation of immune system (autoimmune disorders) ▪ RA, IBS, Lupus, etc. ○ Persistent infxn - Chronic inflammation results in an increased risk of developing cancer ○ Due to the long term damage to DNA - Usually begins gradually as a low grade fever, etc. that is ASYMPTOMATIC ○ Over time the effects will start to manifest ▪ You may not even know you have chronic inflammation for a long -long time ○ Ex: Lupus, RA, IBS, etc. Know the differences b/w chronic & acute ------------------------------------------------------------------- > Chemical Mediators- Can be derived from the plasma or endogenous from the endothelium - Histamine & Serotonin○ Derived from Amino Acids ○ First mediators to be released in acute inflammation ○ Produce changes in blood vessel tone (vasoactive) - Platelet Activating Factor○ Derived from phospholipids ○ Broad inflammatory effect ▪ Stims neutrophils, monocytes, and endothelial cells ▪ Enhances serotonin release ▪ Enhances leukocyte adhesion ▪ Stimulates the production of prostaglandins - Omega-3 Polyunsaturated Fatty Acids○ Omega-3 can be found naturally in fatty fish (salmon, macerole) ○ Anti-inflammatory effects DIRECTLY on the cell membrane - Nitric Oxide & Oxygen Derived Free Radicals○ Regulate & amplify the inflammatory process Inflammatory Exudates**KNOW WHAT'S IN THEM AND THEIR CHARACTERISTICS** - Serous○ Watery and low in protein ○ Plasma entering an inflamed site Patho Page 34 Inflammatory Exudates**KNOW WHAT'S IN THEM AND THEIR CHARACTERISTICS** - Serous○ Watery and low in protein ○ Plasma entering an inflamed site - Fibrinous○ Contain large amounts of fibrinogen ○ Bloody meshwork - Membranous○ Develop on mucous surfaces ○ Composed of necrotic cells enmeshed in a fibro-purulent exudate ▪ It's going to look infected and maybe have some fibrous exudate as well - Purulent○ Yellow/greenish ○ Composed of degraded WBC, proteins, & tissue debris = PUS!! - Sanguineous○ Red exudate = ITS JUST BLOOD!!!! ○ Due to leaking RBC from the capillaries - Sero-Sanguineous○ Pink! ○ Due to a combination of serous and sanguineous exudate Systemic Manifestations of Inflammation- Fever○ Most prominent sign of inflammation ○ Systemic symptom caused by PYROGENS (released from the WBC) ▪ Promotes a hostile environment for pathogens ○ Four Types▪ SEE FIGURE ------------------------------------------------------------------------------ > ▪ Intermittent Fever□ Fever spikes and return to normal at least once per 24 hrs ▪ Remittent Fever□ Doesn't return to normal level □ Varies just a few degrees in either direction (up/down) □ Ex: UTI ▪ Sustained Fever□ Temp stays above normal w/ very little variation - (usually sustained with <1 degree variability) □ Ex: Drug Rxns, hypermetabolic fever ▪ Relapsing Fever□ Episodes of fever that occur days apart from each other □ Ex: malaria, Lyme Disease, TB - Leukocytosis○ Increased leukocyte count (15,000-20,000) ○ Allows efficient fighting of the inflammation/infection ▪ WBC's release pyrogenic mediators!!! ^^^^^^^^^^^^^^^^^^^^^ ▪ Aka… they really help themselves to eat/destroy the bacteria by increasing the temp & increasing their numbers - Lethargy/Fatigue○ Metabolism changes from energy making to heat making ▪ Heat making metabolism promotes a hostile environment for the pathogen □ Also helps sustain the fever ○ Results in lethargy/fatigue Lab Tests for Inflammation- Erythrocyte Sedimentation Rate (ESR) ○ Measures the rate RBC settle in plasma/saline over a period of time ○ Inflammation results in increased Sed Rate ▪ Caused by a rise in fibrinogen that allows the RBC to stack ○ Normal▪ Male = up to 15 mm/hr ▪ Female = up to 20 mm/hr - C-reactive Protein (CRP)○ During acute phase of inflammation, liver produces more fibrinogen ▪ Thus…. CRP level will increase ○ Normal is <1.0 mg/dL ○ Level will rise in acute inflammatory response Antinflammatory- --------------------------------------------------------------------------------------------------- > - Don't memorize drug interactions - Acetaminophen = analgesic/antipyretic ○ NO ANTIINFLAMMATORY ACTIONS ○ Route- PO, PR (rectal), IV - ASA (aspirin) = analgesic/antipyretic/AND ANTIINFLAMMATORY - NSAIDS○ Aspirin, Ibuprofen, Motrin, etc. Tissue Healing- Restoration of injured parts and replacing dead tissue - Types of tissues○ Labile▪ Continuously dividing and replicate through life ▪ Replace destroyed/dead cells ▪ Epithelial, oral cavity, vagina, cervix, GIT, uterus, etc. ○ StablePatho Page 35 Types of tissues○ Labile▪ Continuously dividing and replicate through life ▪ Replace destroyed/dead cells ▪ Epithelial, oral cavity, vagina, cervix, GIT, uterus, etc. ○ Stable▪ Cells stop dividing when growth stops ▪ Can undergo regeneration w/ appropriate stim ▪ Liver, Kidneys, Bones, (functional part of organs) ○ Fixed▪ Do not regenerate □ Replaced with scar tissue ▪ Neurons & myocardial cells Local & Systemic Factors Affecting Wound Healing- Blood Flow / Oxygen Delivery○ Blood supplies the tissues w/ nutrients and oxygen ○ Also aids in the removal of debris from the site of injury - Infection / Wound Separation / Foreign Bodies○ Delay the process of healing **Think… they healing process has to work around the fat, slobby company man that keeps getting in the way** - Inflammation and Immune System○ Prevent the formation of infection (remember this would slow the healing process) - Nutrition- increases the healing process ○ Increase protein intake - Aging- slower wound healing Healing Tissue - Intention - Primary intention○ Occurs when an incision/wound is sutured or stapled together ○ Well-approximated - means the 2 edges are touching each other completely - Secondary intention○ Larger wounds ▪ You have greater loss of tissue and high contamination ▪ Slower to heal and more scarring ○ Ex: Burn pt & pressure ulcers ▪ You can't suture that together… you have to cover and let it heal from the inside -out ○ Primary intentions can become infected and result in secondary intention to facilitate healing from within - Healing phases○ Inflammatory▪ Begins at time of injury ▪ Prepares the wound for healing ▪ Form clot, migration of blood cells to the wound ○ Proliferative▪ Build new tissues to fill the wound space ▪ Microblast synthesis ▪ Secrete collagen ▪ Epithelial cells gather at the edges of the wound gather to form new layer ○ Remodeling▪ 3 wks after injury ▪ Fibrous scar develops can last up to 6 mos+ Module 5- InfectionsTerms to know- Infection- the presence and multiplication of a microbe in a host that causes injury - Colonization- act of establishing a presence - Infectious disease- the process of sustained injury or damage from an infection ○ Can vary from mild to life-threatening based on… ▪ Health of the host ▪ Virulence of pathogen ▪ Effectiveness of the pathogen of producing a disease Infectious Agents- Prions are small modified infectious host proteins ○ No hereditary info ○ Can alter shape of normal proteins to make new prions ○ Clump together and damage cells ○ Can cause CNS degeneration (bovine spongiform encephalopathy) - Viruses○ Smallest of all pathogens ○ Contain no organized cellular structure ○ Contain protein coat, surrounding nucleic acid core ○ No metabolic enzymes of their own ○ Insert their genome into host cell DNA and rely on the host cell to live!!!!!!! ▪ Use the host cell to create more viruses - Bacteria○ No membrane bound organelle ○ Live independently w/o host cell ○ Use host for food/shelter ○ Produce toxins ▪ Exotoxins = proteins released by the bacteria to damage or kill host ▪ Endotoxin = part of the bacteria cell wall and initiate immune rxn in the host Patho Page 36 - - - - - ○ ○ Live independently w/o host cell ○ Use host for food/shelter ○ Produce toxins ▪ Exotoxins = proteins released by the bacteria to damage or kill host ▪ Endotoxin = part of the bacteria cell wall and initiate immune rxn in the host Mycoplasmas○ No cell wall ○ Can cause mycoplasma pneumonia Chlamydiae NO CELL WALL ○ No cell wall ○ Must live in cell to metabolize (like virus) MUST LIVE IN A HOST CELL TO SURVIVE ○ Chlamydia Rickettsia○ Must live in cell to metabolize (like virus) ○ Rocky Mountain Spotted Fever Fungi○ Require low body temp to survive ▪ You'll see them on the body surface (feet, ears, etc.) ○ Ringworm, athlete's foot, etc. Parasites (protozoa) ○ West Nile, malaria Helminths○ Roundworms, tapeworms The Risk of Infection | Influencing Factors- The presence of infection is based on the ability of the pathogen to breach the host's barriers and then to colonize to cause damage to the host ○ Body has multiple forms of barriers to prevent pathogens from invading the body…. - Risk for infection is determined by: ○ Type of pathogen (who, what, where, when) ○ Portal of entry▪ Penetration, contact, ingestion, or inhalation ▪ Method of transmission is based on the QUANTITY of the pathogen ○ Strength/status of the immune system and its ability to fight off pathogens (immunocompetence = intact immune system) - Chain of Infection**NEED ALL OF THESE COMPONENTS TO HAVE AN INFXN ○ Reservoir▪ Natural habitat of the pathogen (humans, food, environment, etc.) ▪ Humans can be reservoirs and be asymptomatic (HIV) □ Can still spread the disease ○ Portal of Entry▪ Where the org enters a new host ▪ Must find a portal of entry or the org will die ▪ Entry route can be the same as the exit route ▪ Respiratory, GIT, UT, skin = most common portals of entry ○ Portal of Exit▪ Point of escape from the reservoir ▪ Respiratory tract, GIT, UT, skin ○ Means of Transmission▪ Transmitting from reservoir to new host ▪ Direct contact, droplet, aerosol □ Proper hand hygiene/gloving can interrupt the means of transmission ○ Host Susceptibility▪ Host must be susceptible and the org must be able to overcome host defenses Bacterial Growth- Growth of bacteria varies amongst bacterial species and depends on factors to grow ○ Humidity- bacteria like humid environments ○ Biofilm▪ Bacteria stick to environmental surfaces and produce biofilm ▪ Biofilm permits access to nutrients and excrete wastes ○ Some require oxygenation & some don't (aerobic vs. anaerobic) - Endotoxins○ Bacterial toxin composed of lipids within a cell (lipids = cell membrane) ○ Endotoxins can be beneficial in low levels ▪ Induce cytokines and enhance T-cell activation (trigger an immune response) ○ Too high of levels can lead to sepsis - Exotoxins○ Proteins released from microorganisms ○ Inactivate/modify cell elements and cause cell death ○ Botulism (neurotoxin = paralysis) Transmission Methods- Direct ○ Close contact (sex, kissing, etc.) ○ Congenital = mom to baby - Indirect = ingestion/inhalation Protective Mechanisms- Skin/mucosa provide physical barrier to invading microbes ○ Epithelium defends the body surfaces by acting as a barrier ○ Tissue Macrophages▪ Second level of defense Patho Page 37 ▪ Second level of defense ▪ Pathogens that get through the skin/mucosa are immediately met by these phagocytes - Acid pH of the GIT = chemical barrier to infxn ○ Peptides produced in the intestines also help to kill off pathogens (fungi, bacteria, etc.) - Respiratory Tract○ Nasal hair, cilia = filter ○ Humidification ○ Coughing = expectorate pathogens/foreign substances Stages of infectious disease- Incubation○ Pathogen begins replication ○ No recognizable symptoms in the host ○ Can vary in length (hours to months) - Prodromal○ Initial appearance of NONSPECIFIC symptoms ▪ Mild fever, muscle aches, HA, fatigue ○ Person is most contagious in this phase - Acute○ When the host experiences the max impact of infxn ○ Symptoms very specific, pronounced, ▪ Blisters/rash/itching/etc. in Chickenpox - Convalescent○ Containment of the infxn ○ Elimination of the pathogen ○ Repair damaged tissue ○ Symptoms resolve ○ Time varies on the pathogen and the pt immune response - Resolution○ Totally eliminate the pathogen ○ No residual sxs Clinical Manifestations- Symptoms- outward expression of the immune response and the invading organism Specific Reflect the site of infection Nonspecific Shared w/ number of disease (fever, HA) Obvious Chicken pox symptoms are obvious Covert Discrete.. Requires further testing (LAB WORK) to determine infection (Increased WBC count) - Labs○ Complete Blood Count (CBC)▪ Determine if viral/bacterial infection & determines how to treat the infxn ○ Urinalysis (UA)▪ Look for blood, presence of WBC, culture, proteins, etc. ▪ Visually assess for□ Clarity- Cloudy/sediment = infection □ Odor □ Blood ○ Blood▪ In a suspected infxn you need to ID the pathogen (culture & sensitivity) ▪ Specimen collection□ Will culture the sample, and assess the susceptibility of the pathogen and thus to decide what Rx to use - Need to collect cultures prior to Rx/treatment - Before Abx admin, send the culture down for testing Antibiotic Resistant Organisms- Vancomycin Resistant Enterococci (VRE) - MRSA○ Methicillin Resistant Staphylococcus Aureus ○ Methicillin▪ Inhibits the manufacturing of the bacterial cell wall □ Enzymes link peptides together to form the cell wall □ Methicillin will attach to these enzymes and stops the cell wall formation □ Causes death of the bacterial cell bacteria produce enzymes that inactivate Abx - Inactivationaltered binding sites on the cell membrane - Mutationmetabolic pathways bypass Abx activity - Alternate MetabolismAbx cannot permeate through the cell membrane - Altered PermeabilityAntimicrobials - Includes antibiotics, antivirals, & antifungals - Abx cannot treat ALL types of bacteria ○ Some Abx are targeted to treat Gram-Negative Bacteria or Gram-Positive Bacteria ○ May start w/ a Broad-spectrum Antibiotic and then switch to one that is specific for that TYPE of bacteria - Four Mechanisms of Antibiotics○ Interfere w/ cell wall synthesis ▪ Penicillin ○ Inhibit bacterial protein synthesis Patho Page 38 ○ Inhibit bacterial protein synthesis ▪ Aminoglycosides ○ Interfere w/ normal metabolism ▪ Sulfa Drugs ○ Interrupt nucleic acid synthesis - Antivirals○ Interrupting replication of virus - Antifungals○ Target the cytoplasmic membranes in yeasts and molds Module 9 | RenalPresented by: Ms. Bruno… Anatomy Review- Kidney○ Structural form of the kidney = renal pelvis ▪ Nephron = functional part of the kidney ○ R kidney = lower than the L kidney ▪ Because of the liver…. ▪ Each kidney extends from the T12 - L3 ○ Blood enters the kidney from the Renal Artery - UT- Nephron- ---------------------------------------------------------------------------------------- > ○ Glomeruli▪ Sits in the Bowman's Capsule… ▪ Cluster of capillaries where the filtration takes place ▪ High capillary pressure forces plasma and ions through the cell membrane of the capillaries and into the Bowman's Capsule (step 1 called absorption) ▪ Filtration happens continuously 24/7 ▪ Volume of the blood is filtered about Q 30 min ○ Filtrate comes out of the Bowman's Capsule and then travels through the tubules ▪ This stage is called Reabsorption ▪ Allows the removal of waste and reabsorb of anything needed in the body ○ Final concentration of urine occurs in the Collecting Tubule!!! ○ Whatever is leftover is excreted as Filtrate (step 3 = excretion) The Renal System- The Kidney○ Urine formation occurs in the glomerulus ▪ GFR- rate at which glomeruli are able to filtrate waste from the blood (125 ml/min) ○ Primary fxn of kidney = filter wastes and maintain body homeostasis (fluid/electrolyte, acid-base balance, etc.) ○ Once the final wastes have been excreted into the filtrate, the filtrate is sent into the ureters ▪ The movement of urine is moved via peristalsis - The Bladder○ Bladder can hold about 400 mL ○ Urinary storage and emptying of urine (voiding/micturition) ▪ Peristalsis moves the urine through ureters and into the bladder ○ Voiding occurs when the micturition reflex acts on the detrusor muscle ▪ When the bladder is full/distended (about 250 ml) and (500 ml = critically full) ▪ Reflex sends that impulse to the micturition center of the brain (voluntary control) and the CNS tells the sphincter muscles to constrict to prevent voiding/incontinence ▪ Trauma (paralyzed, diabetic, etc.) cannot sense that the bladder is full, and/or they cannot effectively prevent contraction of the detrusor/constriction of the sphincter - Differences b/w Male & Female○ Females more likely to have UTI = shorter urethra and closer proximity to anus ▪ Higher chance of E.coli infxn (ascending bacteria) - ascends from external opening and goes up to the bladder Functions of the Renal System- Renal system has many other fxn other than urine formation…. ○ AKA… if there's Renal Disease, there are systemic effects that will occur - Regulation and excretion of: ○ Extracellular fluid ○ Serum osmolarity ▪ Regulates the concentration of key ions (Na, Ca++, K, etc.) ○ pH of the blood ○ Excretes waste/toxins (urea) - Production of: ○ Renin▪ Made and stored in the Juxtaglomerular Cells of the Kidney ▪ These cells detect a change in the blood flow to the glomerulus - Renin increases blood pressure & produces vasoconstriction to increase Glomerular Filtration Pressure ▪ Sympathetic NS releases Renin ▪ Converts Angiotensin to Angiotensin 1 ▪ An enzyme converts Angiotensin 1 to Angiotensin 2 ▪ Angiotensin 2 stimulates aldosterone release from the Adrenal Gland to conserve Na - Water follows salt, and increases BP ▪ Can be released due to Sepsis, Hypovolemia, Diminished Perfusion, etc. ▪ Look for low BP Patho Page 39 ▪ Look for low BP ▪ This will trigger the release of Renin ○ EPO▪ Increases RBC production in the bone marrow ▪ EPO release is triggered by hypoxia, to increase RBC, to increase O2 sats ▪ Look for increased HR (as seen in anemia), SOB, weakness, cyanosis, etc. ▪ When kidney damage occurs, the kidney's ability to make EPO is impaired ▪ Blood cells are immature, and takes longer for them to form, and they live a shorter life in circulation ▪ Give these pts synthetic form of EPO IV, Sub q, to help the body manufacture, normal, healthy RBC - Epogen, Procrit, Aranesp ○ Vitamin D▪ Helps activate Vitamin D after it's absorbed from the GIT ▪ Vitamin D is obtained via the diet - Also can be made by UV radiation on cholesterol on the skin ▪ Then has to be activated in the liver & then again in the kidney ▪ Kidney disease results in low Vitamin D levels ▪ Requires supplements or injections to maintain Vit. D levels - Remember how Vit D effects calcium in the bones…. Etc. ▪ Eventually low Ca++ levels will cause PTH to stim osteoclast activity in the bones (osteoporosis) ▪ Need to give meds to keep the Parathyroid in check - If meds don't work, then you have to remove the PT (must have constant Ca++ monitoring and PTH supplements) ▪ Calcium and phosphorus are opposite (one is high one is low) Labs and Tests- Blood serum studies: Potassium 3.5 - 5.0 Calcium VERY low calcium (<6) can result in tetany/muscle cramping/seizures/death etc…….. 8.5 - 10.5 Phosphate 2.5 - 4.5 Bicarb 24 - 31 BUN 8 - 20 Uric acid 2.4 - 7.4 (M) & 1.4 - 5.8 (F) Sodium 135 - 145 Renal creatinine clearance and GFR is the ability of the kidney to filter and reabsorb/secrete substances in the blood Creatinine 0.6 - 1.2 - Urinalysis (UA)○ General exam to determine if further testing is necessary ▪ Mid-stream, clean catch urine sample □ Clean meatus, begin urination, place specimen container as they are midstream…… ○ Normal urine is clear, amber-colored, with NO PROTEIN!!!! ▪ Checks for infxn (blood), glucose, WBC (infxn) ▪ Cloudy = UTI ▪ Foul smell - Urine Culture & Sensitivity○ Additional to UA ○ Determines ▪ What the org is that's growing (culture) ▪ What Abx are going to kill that org (sensitivity) - Specific gravity○ Varies w/ concentration of solutes ○ Higher SG = more concentrated - Presence of Protein ○ Needs to be negative or trace ○ If there is proteins, then this is a sign of Kidney Failure and/or damage to the Glomerulus ▪ Heavy exercise can lead to SOME protein in the urine Urine is normally acidic (ability to fight infxn) ------------------------------------------------------------- > Dx & Radiological Procedures- Intravenous pyelogram (IVP) ○ Visualize the UT after injecting Contrast (iodine) ○ Determine the size/position/shape of kidneys/bladder ○ Look for lesions, masses, etc. - Magnetic Resonance Imaging (MRI) ○ May require the use of IV Contrast (Iodine can be toxic to the kidneys) ▪ Pt w/ poor renal fxn can result in serious renal failure/damage ○ Educate the pt on not wearing anything metal, have any metal medical devices (plates, screws, clips, etc.) - Renal Biopsy ○ Use to Dx acute kidney disease or ESRD ○ Take a chunk of kidney tissue and monitor the pt afterwards ▪ Look for bleeding, vitals, bedrest - Computed Tomography (CT) scan - Cystoscopy ○ Insert scope into the urethra and inject fluid to look into the bladder - Kidneys, ureter, bladder (KUB) Xray ○ Xray looking at these structures to determine the size, shape, position of organs Can detect the presence of calculi in the kidneys Patho Page 40 ○ Can detect the presence of calculi in the kidneys - Urine Collection Renal Disorders- Neurogenic Bladder○ Flaccid/Spastic bladder dysfunction ▪ Disconnect in the ability of the brain/spine to tell the bladder to contract for urination (Urinary Retention) ▪ Spastic = cannot store urine (incontinence) ○ Bladder stretches to hold urine, but the pt is unable to voluntarily void (urinary retention / urinary stasis) ▪ May develop overflow incontinence (urine leaks because bladder is so full) ○ Cause of spinal injury, nerve damage, CNS issues ▪ Side note: males have trouble voiding when undergone anesthesia ○ May have to insert catheter ▪ Presents risk of CAUTI - Obstruction/Stasis○ Static urine can form kidney stones, or serve as a growth medium for bacteria ○ Urinary obstruction w/ retention/stasis of urine ▪ High risk of developing stones and/or UTI ○ Can be congenital or acquired through: ▪ BPH ▪ Neurogenic Bladder □ Spinal cord injury ▪ Calculi ▪ Tumors ▪ Scar tissue ▪ Pregnancy - lots of pressure that prevents the bladder from constricting properly ○ Major sites and causes▪ SEE FIGURE ------------------------------------------------------------------------------------------ > - Benign Prostatic Hypertrophy (BPH)○ Age related and benign ○ Urinary retention due to the prostate being enlarged ▪ Can cause urinary stasis and cause a r/o developing calculi and UTI ○ Signs and Symptoms▪ Hesitancy (dribbling, weak stream) ▪ Frequency, urgency ▪ Dysuria & Nocturia ▪ Hematuria ○ DIFFERENT THAN PROSTATITIS! ▪ BPH is not due to an infxn …. And it is NOT Curable (can be treated, but not cured) ▪ BPH can be asymptomatic ▪ BPH is age related ▪ But NOT ALL enlarged prostates are due to BPH…. - Renal & Urinary Calculi (stones)- ---------------------------------------------------------------------------- > ○ More frequent in whites and in SE USA and more likely in males ○ Crystals that come together to form prickly, hard, sharp stones that cause pain… omg. ○ Nephrolithiasis▪ Kidney Stones ▪ Crystalline structure that form from components of the urine ○ Urolithiasis▪ Urinary stones ▪ Any stones in the Urinary Tract (ureter, bladder, urethra) ○ Etiology▪ Obstruction/Urinary Stasis □ Assess for Signs of Stasis… - Bladder distention - Hesitancy - Dribbling - Straining when initiating urination - Small, weak urinary stream - Frequency - Feeling of incomplete bladder emptying - Overflow incontinence ▪ Hypercalcemia ▪ Dehydration ▪ Immobility ○ Clinical Manifestations▪ Severe pain (depending on the location of the stone) ▪ Diaphoresis ▪ N/V ▪ Fever ▪ Chills ▪ Hematuria & WBC's in the urine ○ Types of Calculi Pain▪ Renal Colic□ Pain associated with kidney stones (nephrolithiasis) □ Acute, extreme pain □ Flank pain ▪ Ureteral Colic□ Pain w/ urolithiasis □ Acute, intermittent pain □ Pain in lower-outer abdomen and radiating to pelvic area & scrotum (males) - Incontinence- Patho Page 41 ***Notice a lot of these disorders are "symptoms" or "associated problems" that can be caused by one another….. i.e. Neurogenic Bladder can result in Obstruction/Stasis, and so forth….*** Unrelenting pain due to it being hung up in the Renal Pelvis Intermittent pain elicited by peristalsis of the ureters, bladder, etc. - Incontinence○ Stress Incontinence▪ Cough, laugh, sneeze = leak urine ▪ Women can do Kegel Exercises to strengthen sphincter after birth ○ Overflow Incontinence- bladder so full that the pressure of the urine leaks out of sphincter ○ Urge Incontinence- some external stimuli triggers the need to pee (hearing water, seeing the bathroom) DIAPPERS: ○ Common in the Elderly PopulationD- Dementia ▪ Smaller Bladder I- Infection ▪ Difficulty moving to the toilet (Functional Incontinence) ▪ Strength of sphincter is reduced A- Atrophy of bladder ▪ BPH P- Pharmaceutics ▪ Poor detrusor muscle fxn P- Psychological ▪ Medications ▪ DIAPPERs- reasons for incontinence in elderly E- Endocrine disorders (diabetes) □ … See Acronym R- Restricted mobility - Urinary retentionS- Stool Impaction (pressure) ○ Signs of obstruction/retention ▪ Distended bladder ▪ Hesitancy (dribbling, weak stream, etc.) ▪ Straining when trying to urinate ▪ Frequency ▪ Feeling of incomplete emptying the bladder ▪ Overflow incontinence - UTI's○ Cystitis (bladder)▪ UTI of the lower UT ▪ Common one…. Women most effected…. Etc. ○ Pyelonephritis▪ UTI of the upper UT □ Women most effected ▪ Effects the renal pelvis □ Can result from sepsis or infected blood and then infect the kidney □ Or result from reflux of urine into the renal pelvis ▪ This is an acute infxn that can become chronic if left un- Rx ○ CAUTI's!!! ▪ Catheter in too long ▪ Break in sterile technique ○ Natural Protection Against UTI's▪ Males□ Urine acts as antiseptic (acidic) □ Urethra enclosed in penis (longer) □ Protective prostate ▪ Females□ Urine = antiseptic (acidic) □ Lactobacilli in vagina (acidic) □ Acidic environment ○ Special Considerations▪ Sexually active women are more likely to develop UTI □ Anus proximal distance to urethra □ Birth control methods (diaphragms) introduced bacteria to the urethral meatus Also pressure in the abdomen creates pressure on the Urinary ▪ Pregnant women-- anatomical changes makes urethra closer to anus ----------------> Tract causing STASIS!! ▪ Diabetic- Bacteria LOVE SUGAR!!!!!!! ▪ Age related□ Infants - sitting in spoiled diaper = increased risk □ Prepubescent women = poor acidic environment… □ Elderly- Functional reasons why they don't go the bathroom = stasis CONFUSION = common sign/symptom in the ELDERLY ○ Most Common Organisms▪ E.coli - THIS IS THE MAIN HERO!!! ▪ Staphylococcus Aureus ▪ Enterobacter - Urinary Reflux ○ Backward flow of urinary in the urinary tract ▪ Reflux from the bladder up the ureter and into the renal pelvis ○ Urethrovesicular Reflux- reflux of urine from the URETHRA into the BLADDER ○ Vesicoureteral Reflux- reflux from BLADDER to the URETERS - Cystitis○ Inflammation of the bladder ○ More common in females ▪ Also cause from CAUTI's ○ Signs & Symptoms▪ Urgency, frequency ▪ DYSURIA!! ▪ Lower abdominal pain ▪ Cloudy & foul smelling urine ○ Treatment▪ Increase fluid intake (water & cranberry juice = acidic) ▪ Collect specimen for UA ▪ Rx Abx ▪ Females need to urinate after sex to prevent UTI's ▪ Wipe properly - Pyelonephritis▪ Effects the renal pelvis Patho Page 42 ▪ Rx Abx ▪ Females need to urinate after sex to prevent UTI's ▪ Wipe properly - Pyelonephritis▪ Effects the renal pelvis ▪ Can result from sepsis or infected blood and then infect the kidney ▪ Or result from reflux of urine into the renal pelvis ▪ This is an acute infxn that can become chronic if left un- Rx ▪ Acute Pyelonephritis▪ Upper urinary tract ▪ Inflammation of kidney medulla, parenchyma, & renal pelvis, affecting tubules ▪ WBC formation and swelling of the renal pelvis ▪ Responds well to 2 weeks of organism-specific antibiotic therapy ▪ Chronic Pyelonephritis▪ Persistent or recurrent infection of the kidney by the same organism resulting □ Inflammation and scarring of the kidney - Structural abnormalities ▪ Can lead to Chronic Kidney Disease if left untreated ▪ Clinical Manifestations▪ Shaking, chills, fever, etc. □ WBC in the urine (test w/ UA) ▪ Dysuria, frequency, urgency ▪ N/v due to intense, prolonged abdominal pain ▪ Chronic Infection can lead to: □ Azotemia (nitrogenous waste in blood) □ Hypertension (due to renal failure) □ Acidosis □ Proteinuria Congenital Disorders- Polycystic Kidney Disease○ Autosomal Dominant Disorder ○ Enlarged cysts on the kidneys and causes kidney failure ○ Requires dialysis - Renal Agenesis○ Complete failure of renal development ○ Bilateral agenesis (both don't develop) ▪ This is INCOMPATIBLE W/ LIFE ○ Unilateral agenesis- they can survive barring any other complications - Renal Hypoplasia○ Small kidneys ○ Less number of nephrons ○ Can be unilateral or bilateral ▪ Bilateral hypoplasia results in kidney failure - Renal Dysplasia○ Primarily effects the renal tubules ○ Just a bunch of jacked up anatomy (dys-plasia) ▪ At r/o developing neoplasm (cancer) Renal Tumors- "In Cito"? ○ If the tumor is contained, then the pt has a good 5 yrs survival rate ○ If the tumor metastasizes, than the survival rate is way less - Renal cell carcinoma- Most common Bladder Cancer- 6th most common malignancy ○ Affects males over 60 yrs - Usually manifests as blood in the urine - Can metastasize into the blood and affect lymph nodes, liver, bones, lungs - Transitional Cell Carcinoma = MOST COMMON bladder cancer Glomerular Function Disorders- Glomerular Disorders○ Most common form of kidney disease - Results in decreased GFR ○ Normal GFR = 125 mL / min - Causes of Glomerular Injury○ Infectious microbes (prolonged UTI's) ○ Autoimmune disorders (antibodies attack the antigens in the glomerulus) ○ Environmental agents/abuse ○ Drugs (drugs are metabolized in the kidneys and can cause damage) Nephrotic Syndrome- ------------------------------------------------------------------------------------------ > - Signs & Symptoms○ Lots of protein in the urine ▪ Proteinuria = 3.5 g/day ▪ Hypoalbuminemia = <3 mg/dl ○ Fats in the urine (lipiduria) ○ Generalized Edema / ascites ▪ Results from decreased colloidal pressure due to the hypoalbuminemia - Protein in the urine is ABSOLUTELY NOT NORMAL ○ Indicates extensive damage to the glomeruli ○ They are super leaky and are allowing proteins to seep out - Caused by systemic diseases (diabetes, lupus, etc.) - ComplicationsPatho Page 43 Antigen-Antibody complexes clog up the glomerulus - Protein in the urine is ABSOLUTELY NOT NORMAL ○ Indicates extensive damage to the glomeruli ○ They are super leaky and are allowing proteins to seep out - Caused by systemic diseases (diabetes, lupus, etc.) - Complications○ Loss of immunoglobulins (proteins) = increase r/o infxn ○ Increased r/o blood clots, CAD, HTN = loss of clotting factors ○ Anemia (loss of RBC) ○ AKI ---> CKD - Assess the 24 hours urine specimen ○ Pt uses restroom in the morning and the clock starts ▪ Flush… you don't want first sample ○ For the next 24 hrs, every urine sample needs to be collected and refrigerated ▪ Leaving urine out, it will culture and grow bacteria (not accurate) ○ Keep and collect the last urine specimen Chronic Glomerulonephritis- Progressive disease that can lead to CKD - Usually secondary condition caused by diabetes, and lupus - Results in renal insufficiency which can lead to Nephrotic Syndrome and finally ESRD Post-streptal Glomerulonephritis- Associated w/ Strep infxn ○ Untreated strep can colonize in the blood and infect the glomeruli ▪ DESCENDING infxn ○ Also results from the accumulation of WBC and swelling of the endothelial cells - Left untreated can result in renal failure Acute Kidney Injury & CKDAcute Kidney Injury- Rapid onset ○ Oliguria ○ Azotemia (increased creatinine and BUN) ▪ BUN = amount of urea in the blood - Impaired kidney fxn ○ Inability to filter waste, fluid from the blood - Can result from meds, dehydration, toxins/poison, repeat UTI - Often times AKI is REVERSIBLE!! - High mortality rate with AKI…. The kidneys are super important ---------------------------------------> - Classification○ Pre-Renal ○ Intra-Renal ○ Post-Renal Pre-Renal AKI- Above the kidney - Caused by reduction of blood flow to the kidney - hypoperfusion ○ Ischemia of the Nephrons leads to Decreased GFR & urine output ▪ Drop in BP (shock) ▪ Sepsis □ THESE ARE TWO MAIN VILLAINS TO THE KIDNEYS - Associated Disorders○ Shock, CHF, MI ○ Burns ○ Trauma ○ Obstruction of the Renal Artery - Symptoms○ Oliguria▪ Low urine output ▪ Hypoperfusion in the glomerulus results in decreased urine output ○ Elevated BUN▪ Hypoperfusion results in slowed movement of urine through the kidney ▪ Allows more time for urea to be reabsorbed into the blood Intra-Renal AKI- Damage inside the kidney ○ Acute Tubular Necrosis (death) ▪ Most common Intra-Renal AKI ▪ Destruction of the epithelial cells in the renal tubules ▪ Due to nephrotoxic meds, ischemia, sepsis, or obstruction ○ Glomerulonephritis (see above) - Etiology○ Reduced blood supply (ischemia) ▪ Secondary to the Pre-Renal injury ○ Drugs/Toxins ○ Urinary reflux into the Renal Pelvis ▪ Obstruction in the tubules ○ Sepsis ○ Infections Post-Renal AKI- Below kidney (ureters, bladder, urethra) - Due to obstruction, Calculi & Strictures = Ureter Patho Page 44 INFECTION is the most common COD w/ AKI ○ Calculi & Strictures = Ureter ○ Tumors & Neurogenic Bladder = Bladder ○ BPH/pregnancy & Calculi = Urethra - Symptoms○ Distention ○ Tenderness w/ palpation ○ Symptoms reflect the level of the obstruction ▪ Pain may occur in flank w/ high obstruction - Need to treat the underlying cause of the obstruction ○ Restore urine flow before there is permanent damage to the kidneys !!! Stages of Acute Tubular Necrosis- Initiating Phase○ Onset of initial injury or event that causes the AKI ▪ Ischemia, obstruction, etc. ○ May take about 1 week for to cause tubular injury - Maintenance Phase○ Lasts 1-8 weeks ○ Oliguric/Anuric or Non-Oliguric manifestations ▪ Oliguria = urine output less than 30 mL per hour □ Less than 400 mL / day ▪ Produce little or no urine □ Due to decreased GFR which results in increased creatinine & BUN □ Water retention results in edema, fluid volume excess (water intoxication), and pulmonary congestion ○ May require dialysis to keep the stress off the kidneys ▪ Allows the kidneys to heal the problem w/o worrying about urine formation - Diuretic Phase○ Diuresis returns…. ○ CAN BE DEADLY ▪ Diuresis returns before renal function has been restored to normal □ Therefore, BUN & Creatinine levels remain elevated ▪ The diuresis w/ poor renal function can lead to excess water & electrolyte loss - Recovery Phase○ Eventually the renal tubular function is restored… ▪ Decrease in creatinine and BUN □ Indicates the tissue has been repaired and the nephrons have recovered ○ Moderate to Severe damage that has already been done remains permanent AKI & The Elderly- Risk factors for developing AKI○ Hypoperfusion ▪ Decreased GFR ▪ Hypotension ▪ Dehydration ▪ Diuretics ○ Diabetes ○ Infections ○ Obstructions to the urinary tract ○ Medications▪ Elderly use multiple numbers of medications that can be nephrotoxic Management of AKI- Assessment○ Monitor VS, labs, weight (water), mental status ○ Skin▪ Edema ▪ JVD ▪ Dialysis port for infection ○ Auscultate for crackles in the respiratory sounds ○ Urine▪ Look for output amount ▪ Color ▪ Sediment ▪ Protein - Diagnostic Studies○ UA ○ Ultrasound of the kidney ○ CT - Nursing Care○ Eliminate the cause of the AKI ○ Treat the symptoms ○ Nutritional Concerns▪ Provide adequate calories to promote healing □ Protein to prevent muscle wasting □ Carbs and fats for energy & to prevent ketosis ▪ Manage K & Na levels ○ May need dialysis to remove excess wastes and fluids Chronic Kidney Disease (CKD)- AKI can transition into CKD ○ Asymptomatic and undiagnosed …. Usually Dx when they come to the doctor for Patho Page 45 - - - - - ○ Asymptomatic and undiagnosed …. Usually Dx when they come to the doctor for something else CKD is progressive & Irreversible ○ High mortality rate --------------------------------------------------------------------------------------- > ○ More common than AKI Different stages○ Normal GFR = 125 mL / min ▪ The Stage of CKD is determined by their current GFR ▪ Below 15 = Stage 5 (ESRD) □ TERMINAL!!! □ Require dialysis or transplant to remain alive Creatinine – byproduct of muscle metabolism Etiology1. Diabetes 2. Hypertension CKD = very strict diet control ○ Watch salt for HTN ○ Watch carbs for DM ○ Watch fluid intake and foods that are high in fluid concentrations ○ Very difficult to create a balance between the DM & HTN and Diet Central Line is that fastest access to a pt blood ○ High r/o infxn due to line being inside the heart Transplant and dialysis are the only treatments for ESRD…. If not, they will DIE!!! Stages of CKD- Stage 1○ GFR 90+ ○ Usually asymptomatic ○ Elevated creatinine and BUN ○ Hematuria & proteinuria - Stage 2○ GFR 60-89 ○ Same sxs as Stage 1 ○ You just have a lower GFR - Stage 3- (moderate kidney disease) ○ GFR 30-59 ○ Fatigue ○ Fluid retention, edema, SOB ○ Flank pain ▪ Result in sleeping disturbances - Stage 4○ GFR 15-29 ○ Begin making dietary changes▪ Fluid restriction ▪ Decrease protein consumption - Stage 5- (ESRD) ○ GFR below 15 ○ Dietary restriction are different from Stage 4 ▪ Increase protein intake to prevent muscle wasting and to prevent edema ○ Treatment▪ MUST HAVE either transplant or dialysis ▪ Transplant□ Immunosuppressive agents = increased r/o cancer, infxn - Avoid situations in which infxns are imminent □ Take lifelong meds □ Requires extensive consultation to ensure the pt is ready for the potential complications of the treatment and the transplant □ Nonfunctioning kidneys are NOT removed - The new kidney is just placed in the abdominal cavity (3 kidneys) ▪ Dialysis□ Very tasking process & pt can become depressed □ Psychologically tasking to undergo dialysis, travel there, and get treated - Tasking process can lead them to stop dialysis - This requires extensive consultation and intervention to ensure they are of sound mind ○ Clinical Manifestations of ESRD- Patho Page 46 Most common COD for CKD = CARDIOVASCULAR!! - MI, CVA, etc. Peritoneal Dialysis- Catheter into peritoneal cavity ○ Pushes fluid into PC and through osmosis, the wastes are pushed into this spare fluid ○ Then the machine sucks out the fluid and pumps in new fluid to start over again - Big r/o developing peritonitis/infxn ○ Monitor the pt for constipation ▪ Bacteria can migrate from bowel to the site and cause peritonitis ESRD & Bone Disease- Calcium and Phosphorus are inversely proportional - Dietary phosphorus is restricted in ESRD pts (dark sodas) ○ High phosphorus causes low calcium levels ○ Low calcium stimulates PTH release resulting in secondary (or tertiary) hyperparathyroidism ▪ May need to Rx w/ parathyroidectomy - Pts can take phosphorus binders to excrete phosphorus in the stool ESRD & Anemia- Anemia occurs secondary to decreased EPO production - Need to treat with exogenous EPO (Epogen, Procrit, Aranesp) ○ Need to Rx the lowest dose possible ○ Too high of Hgb can cause clotting events (MI, CVA) - The goal of treating anemia w/ EPO is to reduce the amount of blood transfusions!!! ○ Blood transfusion introduce new antibodies into the body ○ This decreases the chance the pt will find a perfect transplant match Patho Page 47 Tutoring Junk Stuff Monday, October 16, 2017 4:59 PM Renal SystemUrine- Urea = 2% of the urine concentration and is a nitrogenous waste product - Creatinine = product of protein metabolism - pH typically acidic (6.0) - diet and disease change the acidity of the urine Kidney fxn- Eliminate waste - Regulate pH (normal = 7.35-7.45) - Regulation of fluid volume - Activates vitamin D (important to maintain bone health by absorbing calcium) - Produces EPO (kidney failure results in anemia!!) - Renin-angiotensin aldosterone system○ Regulates BP The functional unit (nephron) of the kidney- Bowman's capsule = holds the glomerulus - Proximal tubule - Loop of Henle - Distal tubule - Collecting duct ADH- "vasopressin" Released from the posterior pituitary Works at the nephron to retain water Too much ADH - SIADH (symptom of inappropriate ADH) Too little ADH - diabetes insipidus (urinating nonstop) Renal Labs- Creatinine (0.6-1.2) gold standard ○ Byproduct of protein metabolism - BUN (8-20) ○ Hot dog buns (come in packages of 8 & 20) - GFR (125 ml/min) - Specific Gravity (1.101 - 1.025) UTI- Cystitis involves the bladder ○ Can hold around 400 mL of fluid before you get the urge to pee ○ Sxs▪ Dysuria, frequency, ○ Rx▪ Abx (Bactrim), increase fluids, - Pyelonephritis○ Involves the kidney (bigger deal = worse sxs) ○ Sxs▪ Flank pain (kidney pain) ▪ Fever, chills, N/v ○ Rx▪ Abx - Test w/ UA Patho Page 48 - Test w/ UA - More suceptible population○ Pregnant women▪ Urethra descends to the anus ▪ Ureters compressed ▪ Causes urinary stasis and cultures bacteria ○ DM- bacteria love sugar ○ Children▪ Urinary stasis!!! (they don't want/don't have to use the restroom) ▪ Incorrect wiping Elderly○ ▪ Functional issues ▪ CONFUSION is a significant symptom for a UTI in elderly - Causes of UTI○ Urinary reflux- refluxes out of bladder and into the ureters ○ CAUTI ○ Anatomy that causes UTI ▪ Stones - cause stasis ▪ BPH - causes stasis ▪ Congenital defects in the anatomy of the urinary system ▪ Pregnancy (see above) ○ Infrequent Voiding (stasis) ○ Constipation (compressing the urinary tract and leads to stasis) - Treat UTI aggressively to prevent systemic infxn ○ Sepsis = death ○ Chronic pyelonephritis can lead to Kidney Failure and CKD - CHRONIC Pyelonephritis typically manifests as HTN ○ Secondary complication due to the infxn inhibiting the RAAS system of the kidneys !!!! Glomerulonephritis- Immune response in the glomerulus where antigens and antibodies collect in the glomerulus and cause inflammation over and over - Secondary to Strep throat - Sxs○ Decreased GFR ○ Flank pain ○ Coke colored urine (RBC and protein in urine) ○ HA, increase BP, edema (retain fluid), lethargy ○ Fever ○ Weight gain (fluid retention) ○ Proteinuria (leaking glomerulus), hematuria (leaking glomerulus = RBC getting through) , oliguria, dysuria, ○ Azotemia = buildup of waste products in the blood ▪ (creatinine above 1.2 and BUN above 20 measure the degree of azotemia) Nephrotic Syndrome- Massive protein loss ○ Leads to low albumin levels and thus EDEMA (fat black boy picture) Obstructions of the UT- BPH○ Enlarged prostate ○ High risk in Age 50+ ○ Sxs▪ Hesitancy (dribbling) - Nephrolithiasis & Urolithiasis○ Stones in the kidney Stones in the Ureters Patho Page 49 ○ Stones in the Ureters ○ Etiology▪ Hypercalcemia ▪ Dehydration ▪ Immobility ○ Sxs▪ Colic type pain (use location of pain to locate the stone) , diaphoresis, sxs of UT infections ○ Rx▪ Increase fluid intake, move around, and decrease Ca intake ○ Nursing interventions▪ Assess strained urine ▪ Educate pt on dietary changes based on the cause of the stone ▪ Lithotripsy = breaks stones to allow for easy passage - Major complication of obstruction = hydronephrosis??? ○ Water refluxes into the kidney … can lead to kidney failure AKI & chronic kidney disease - Both can be caused by anything we talked about already!!!!! AKI- Sudden onset - Reversible (intervene early and stop the problem) - Kidneys can't remove waste = azotemia (high creatinine and high BUN) ○ Dx criteria = sudden drop of urine output and high creatinine - Types of AKI○ Pre renal AKI ▪ Hypoperfusion = ischemia of the kidney (lack of blood & O2 in the kidney) ▪ Caused by trauma (hemorrhagic shock), dehydration, ▪ Remember the kidneys are healthy!!!! The lack of blood is causing the issues ○ Intra renal AKI ▪ Tissue damage to the kidney (tubular necrosis = kidneys dying) ▪ Medications can be toxic to the kidneys ▪ Infections mentioned above can damage kidneys ○ Post renal failure▪ Below the kidneys ▪ Buildup of fluid in the renal pelvis (hydronephritis) □ i.e. caused by obstructions/reflux - Phases of AKI1. Onset (initiation of injury) i. Ex = trauma that causes hypoperfusion in pre renal failure 2. Oliguria i. Producing less than 400 ml per day ii. Results in fluid volume excess, increased K+ (not excreted in the urine), elevated creatinine and BUN 3. Diuretic phasei. High urine output when diuretics are Rx-ed ii. Results in fluid volume deficit, electrolyte loss 4. Recoveryi. GFR increases slowly (will return to normal after a long time…. Weeks to years) ○ NURSES FOCUS ON BALANCING FLUID AND ELECTROLYTE ISSUES Most common fatal complication of AKI = infection Short term issue!!! Therefore, infxn will be the most common COD Chronic Kidney Disease- Permanent loss of nephrons = irreversible damage to kidneys - Most common COD = cardiovascular related (MI, CVA, etc.) - HTN & DM and other diseases can cause CKD Patho Page 50 - HTN & DM and other diseases can cause CKD - Associated sxs○ Azotemia ○ Hyperkalemia ○ Anemia ○ Weakness (decreased RBC/O2) ○ Decreased appetite (due to backed up of junk and waste = poor appetite) ○ Neuropathy w/ unsteady gait ○ Bone demineralization (lack of vitamin D activation) - Treatment○ Dialysis ○ Epogen (EPO) ○ K+ restriction ○ Fluid intake restriction (match the output) ○ Vitamin D & C supplements - Prevention○ Manage DM & HTN aggressively ▪ Diet ▪ Blood sugar ▪ Cholesterol levels ▪ Smoking ○ Once Dx w/ CKD = preventing MI & CVA ○ Low protein diet ○ Fluid intake Patho Page 51 Exam 3 Thursday, October 19, 2017 8:33 AM Module 10 | RespiratoryFunctions of the Airway and Lungs- Gas exchange - Inactivates vasoactive substances (bradykinins) - Converts Angiotensin I to Angiotensin II ○ ACE enzymes - Reservoir for blood storage - Type II alveoli secrete surfactant ○ Increased efficiency of lung inflation (lubricates) - Type II alveoli also protects against pathogens entering the airway - Nursing Implications○ Premies lungs aren't fully formed ○ Therefore functions (especially surfactant production) are impaired ▪ Results in severe consequences Respiration involves ventilation and gas exchange - These are independent fxn-s (can have ventilation w/o gas exchange) - Ventilation○ Movement of O2, Nitrogen, CO2 & gasses w/ pressure gradient from atmosphere and inside the body ○ Diaphragm & accessory muscles (ribs, shoulders, abs, etc.) contracts and decreases the pressure ▪ These muscles also relax/hyper-relax to increase pressure in the chest to exhale ○ Assess accessory muscles for signs of respiratory difficulty ▪ Physical activity/Exercise/exertion = main cause of respiratory difficulty □ Think of seeing the shoulders heaving, etc. ○ Lungs are very elastic when healthy and w/o disease ▪ Many diseases cause the lungs to stiffen and become non-compliant ▪ Compliance = elasticity of the lungs □ After surgery you need to assess the lungs carefully due to the anesthesia (general anesthesia) □ This depresses lung fxn for hours on end, and you need to make sure they are working properly ▪ Smoking = increased r/o lung dysfunction - Inspiration○ Intrapulmonary pressure decreases ○ Intrapleural Pressure becomes negative ▪ Decreased pressure in the pleural space between the lungs and the chest cavity □ Pleural space contains 4 mL of Serous Fluid ▪ Allows air to flow into the lungs ▪ Pleurisy□ Lack of pleural space causing lungs to stick to the chest wall ▪ Pleural space can have positive pressure (BAD) □ Pneumothorax ○ Alveoli rupture (bleb) or Trauma ○ Air escapes and enters pleural space ○ Pressure become negative and air flows into the lungs - Expiration○ Elastic components of the chest wall/lungs/diaphragm relax & recoil ○ Chest cavity decreases in size ○ Intra-thoracic pressure increases and air flows out Gas Exchange- Atmospheric pressure is 760 mmHg ○ This value is considered baseline and give 0 as a value - Concentration of O2 at elevation is less than the concentration of O2 at sea level - Partial Pressure of O2 (SPO2 = 95-100) ○ Partial pressure of CO2 = 35-45 mmHg - Gasses dissolve across the alveoli and into the capillaries ○ Alveoli are 1 cell thick and the Capillary is 1 cell thick ▪ Allows very efficient gas exchange ○ Arterial end of capillary facilitates O2 transport ○ Venous end exchanges CO2 and is expired through lungs ○ Capillary Diffusion is effected w/ lung disease ▪ Stiffened lungs, low O2 sats, poor muscle fxn that inhibits ventilation, etc. Valsalva Maneuver- Causes strong increase in intrathoracic pressure which slows venous return to the right atrium - Ex: holding breath when in pain / pooping - This stims the Vagus Nerve ○ Causes hypotension and pt will "Vagal Down" Perfusion- Movement of blood to the alveoli for gas exchange - Perfusion w/o Ventilation results in Atelectasis ○ Part of the alveoli isn’t contributing to gas exchange ▪ Usually occurs after surgery!! Patho Page 52 ▪ Usually occurs after surgery!! □ Use incentive spirometry, cough, deep breathe, etc. ○ The part of the lung not being aeriated is going to be bypassed by blood flow - Ventilation w/o Perfusion is dead air space ○ There's air in the lungs, but gas exchange isn't happening ○ Ex: Pulmonary Emboli - Ventilation Perfusion Mismatch○ Caused by diseases that affect EITHER ventilation or perfusion ○ Should be evenly matched ▪ Perfusion disorders (emboli) results in decreased perfusion but normal ventilation ▪ Ventilation disorders (COPD) results in decreased ventilation but normal perfusion Oxygen Transport- O2 is transported via hemoglobin/oxyhemoglobin ○ Results in O2 sats = 95-100% ▪ The amount of O2 Saturation depends on the amount of O2 bound to Hgb □ If 3/4 Hgb molecules are bound w/ O2 = 75% O2 sats ○ Diseases such as Anemia result in decreased Hgb & decrease O2% - O2 can also be dissolved (2-4%) and diffuse directly into tissue cells ○ This is measured as Partial Pressure of O2 (PO2) - Oxygen-Hemoglobin Dissociation CurveSEE FIGURE -------------------------------------------------------------------------------------- > ○ Hypoxemia = low amounts of dissolved O2 in the blood (whether on Hgb or dissolved) ○ Normal O2% = 95-100% ▪ This is the amount dissolved on the Hgb ○ PO2 is only measured through Arterial Blood draws (ABG's) ▪ Normal PO2 = 80-100 □ PO2 of less than 50 requires the Pt to be on a Ventilator ▪ Notice that dropping in PO2 doesn't result in a sharp decrease in O2%! ○ Need to measure BOTH pulse ox% and PO2 (ABG) to get an accurate O2 level analysis ○ Things that Effect the Curve▪ Temperature ▪ Acidotic ▪ Alkalotic Hypoxemia- Low blood O2 levels - Etiology ○ Respiratory disease ○ Dysfunction of the neuro system ○ Alterations in circulation ▪ Results in ventilation-perfusion mismatch - Patho○ Low PO2 levels cause the body to switch to ANAEROBIC METABOLISM ○ Causes a buildup of Lactic Acid ○ Results in metabolic acidosis - Signs & Symptoms○ **Changes in Mental Status & Hyperventilation (RR 20+) ▪ Restlessness, mood changes, increased respirations, etc. ▪ The KEY is to detect EARLY!!! □ Prevent them from developing from Mild to SEVERE!!!!! ○ Mild▪ Increase HR & BP (compensate) ▪ Changes in mental status ▪ Hyperventilation (compensate) ○ Severe▪ HR & BP will continue to increase ▪ Delirium, Stupor, Coma ▪ Cyanosis ○ Chronic- (conditions like COPD) ▪ Need to have the underlying disease for 6+ mos to Dx w/ chronic hypoxemia ▪ Polycythemia = increased RBC to compensate - Diagnosis○ ABG's to determine PO2 ○ SPO2 % - Rx○ Treat the underlying cause of the hypoxemia ○ Administer supplemental O2 as ordered ▪ Or 2L via nasal cannula w/o M.D. order Hypercapnia- Increased PCO2 in the blood (ABG's) ○ Normal PCO2 = 35-45 - Results in decreased pH (acidosis) & increased HR & RR (compensate) ○ Normal pH = 7.35-7.45 - Etiology○ Ventilation-Perfusion Mismatch ▪ Hypoventilation ▪ Poor CO2 exchange at the alveoli ○ Increased metabolic rate ▪ Fever ○ High carb intake ▪ Tube Feedings & TPN contain high amounts of Carbs Patho Page 53 ▪ Tube Feedings & TPN contain high amounts of Carbs □ End product of Carb metabolism = CO2!!! ▪ EN or TPN can cause hypercapnia or make existing hypercapnia worse!!! Respiratory Symptoms- Cyanosis○ Blue color of the skin d/t decreased amounts of oxygenated Hgb ○ Late sign of respiratory failure ▪ PO2 will decrease to about 50 & PCO2 increase to 50 before O2% decreases □ The low O2% results in cyanosis ▪ AKA…. Since O2% is slower to drop, cyanosis is a late sign of low O2 in the blood ○ Central Cyanosis- evident in the tongue and lips (MORE SERIOUS) ○ Peripheral Cyanosis- extremities, nose, ears - Dyspnea○ Subjective symptom of difficulty breathing ○ Etiologies▪ Stimulation of Lung Receptors ▪ Reduction in ventilatory capacity (decreased muscle function) ▪ Stimulation of muscle receptors ▪ Excessive chemoreceptors innervating the CNS ○ Nursing is subjective and needs to be measured w/ a scale (like pain) ○ Treat the underlying cause ▪ Decrease anxiety ▪ Conserve energy ▪ Breathing training/breathing exercises (slow, methodical breaths) - Cough Reflex○ Protective mechanism to prevent foreign bodies in the lungs ○ Chronic cough can damage lungs/trachea and tear muscles ▪ Bronchitis = cough x8 weeks ○ Nursing Implication▪ Bed rest (post-op or immobile) inhibits chest expansion □ Limited amount of air in/out during ventilation ○ Also results in weak cough reflex □ Need to have pt sit upright and cough/deep breathe ○ Splint surgical site ▪ NG tubes interfere w/ cough reflex □ Upper airway cannot close Pulmonary Diseases- Obstructive diseases ○ Limit inspiratory and expiratory AIRFLOW ○ COPD, asthma, emphysema, etc. - Respiratory Tract Infections - Lung Inflation Disorders ○ Decrease EXPANSION of the lungs ○ Atelectasis & pneumothorax Asthma- Obstructive disease that is reversible ○ d/t INFLAMMATION d/t hypersensitivity to allergens - Inflammation = Increased Airway Responsiveness ○ Increased cough reflex and hypersensitivity to foreign bodies ▪ Perpetuates and causes more inflammation & obstruction - Bronchial Asthma○ Chronic inflammation of bronchi ▪ Causes hyper-responsiveness & airflow obstruction - Patho○ Hypersensitivity (allergens, drugs, cold, exercise, etc.) ▪ Level of the reaction depends on the level of hypersensitivity ○ Inflammatory mediators released by: ▪ MAST CELLS!!!! ▪ T-cells ▪ Macrophages ▪ Eosinophils ▪ Basophils ○ Inflammation results in BRONCHO-CONSTRICTION (obstruction) - Extrinsic Asthma (Atopic)○ Induced by Type I Hypersensitivity (exposure to antigen/allergen) ○ Begins in childhood ○ 2 phases▪ Acute (10-20 minutes) □ Release of chemical mediators □ Bronchospasm □ Edema ▪ Late-Phase (4-8 hours) □ Inflammation □ Hyper-responsiveness (vicious cycle of exacerbation) - Intrinsic Asthma (Non-Atopic)○ Triggered by: ▪ Respiratory Tract Infections □ Infection creates IgE antibodies = hyper-responsiveness that lasts for weeks after infection is gone ▪ Exercise Patho Page 54 - - - - ▪ Exercise □ Exercise asthma worsened w/ cold air ▪ Pollutants □ Irritants/pollutants (tobacco smoke) can cause bronchospasm ▪ Hyperventilation ▪ Cold air ▪ GERD Signs & Symptoms of Asthma○ Wheezing ○ Chest tightness ○ Dyspnea (subjective SOB) ○ Cough ○ Increased sputum ○ Tachycardia & Tachypnea Asthma in Children○ Leading cause of chronic illness (80% symptomatic by 6 y/o) ▪ More common in Blacks ○ Exposure to smoke in-utero = huge risk factor ○ 1st sxs are mild but then rapidly progress….. Rx○ Prevention & Controlling exposure to triggers ○ Medications ▪ Allergen Immunotherapy ▪ Rx w/ epinephrine or inhalers w/ bronchodilators (albuterol) □ Medications are the primary method of treatment for symptomatic asthma Diagnose w/ spirometry tests to observe signs of obstruction COPD- Blanket term for both Emphysema & Chronic Bronchitis - 4th leading COD ○ Women > Men - Smoking is the most common cause ○ 2nd most common = Antitrypsin Deficiency (decreased elasticity in the lungs) - Patho○ Inflammation & Fibrosis of bronchial wall (decreased elasticity) & Excess mucus secretion ○ Cause a Ventilation-Perfusion Mismatch ▪ Decreased ventilation d/t obstructions (mucus) ▪ Decreased area for gas exchange ○ Results in destruction of Alveoli ▪ Alveoli cannot expel air normally = INCREASED AIR TRAPPING! □ Results in Atelectasis & CO2 retention ○ AKA…. COPD can breathe in normally, but cannot breathe out normally ▪ Results in retention of CO2 - Symptoms○ Presents no early symptoms ▪ COPD is usually far advanced when it's finally diagnosed ○ Fatigue / Exercise (ADL's) intolerance ○ Productive AM cough ○ SOB ○ Recurrent respiratory infections ▪ Stasis of excessive mucus results in bacterial growth ○ Chronic respiratory failure (PO2 & PCO2 levels) - Diagnosis○ CHEST XRAY!!! ○ Pulmonary Function tests (spirometry) - Treatment○ #1 treatment method = smoking cessation ○ Education, proper nutrition, ○ Medications▪ Bronchodilators ▪ Theophylline ▪ Oxygen therapy ○ Oxygen Therapy▪ Low flow O2 (1-2 L) prevents reduction of ventilatory drive □ Normal lungs respond to Increased CO2 levels to breathe ▪ LOW FLOW is KEY in COPD!!!! □ Pts are already retaining CO2… this isn't their ventilatory drive… □ Their drive is decreased O2 levels ○ AKA… if you admin too much O2, you're increasing their O2 levels and their ventilatory drive goes away ○ They will not breathe and will DIE!!! - PP vs. BB: ○ Most patients have sxs of both classes ○ BLUE BLOATERS▪ Chronic Bronchitis ▪ Cyanosis ▪ Fluid retention d/t R-sided heart failure ▪ Hypoxemia (blue) can result in polycythemia ○ PINK PUFFERS▪ Emphysema ▪ PO2 <65 & PCO2 55+ ▪ No cyanosis but they do have Air Trapping (CO2 retention) ▪ Barrel Chest Patho Page 55 ▪ Barrel Chest - CHRONIC BRONCHITIS○ Airway obstruction d/t inflammation ▪ Obstruction is persistent & irreversible ○ Hypersecretion of mucus and Chronic Cough x3 mos for 2 years ○ Etiology▪ 80-85% caused by SMOKING ▪ Males > Females ▪ Repeated airway infxn & chronic cough ○ Patho▪ Chronic inflammation results in scaring & fibrosis of mucous membranes □ Compensatory increase in mucous glands ○ Results in Mucous Plugs that clog small bronchioles ▪ Increased wall thickness in bronchi □ Results in obstruction of airflow ▪ Inflammation & Fibrosis can extend to alveoli ○ Symptoms▪ BLUE BLOATERS ▪ Hypersecretion of mucous = chronic productive cough ▪ Congested lung fields (crackles, rhonchi, etc.) □ Fluid retention w/ R-sided Heart failure ▪ Decreased PO2 (less than 65) □ Increased PCO2 ▪ Polycythemia (compensation) - EMPHYSEMA○ Destruction of alveoli WITHOUT FIBROSIS ▪ Abnormal enlargement of air sacs (hyperinflation) ○ Etiology▪ SMOKING □ Teen smokers have higher r/o developing at 50 y/o ▪ Weight Loss □ They are fatigued!!!! □ Results in loss of appetite d/t increased energy needed to even fckin breathe ▪ Genetic predisposition ▪ Results from bacterial infxn ○ Patho▪ Smoking damages alveoli 2 different ways: □ Inflammation of lung tissue □ Inactivates protective chemicals in the lung tissue ▪ Alveoli destroyed by enzymatic action of neutrophils & macrophages ▪ Results in: □ Loss of alveolar walls □ Decreased elasticity in lungs □ Increased airway pressure □ Decreased outflow of air ○ CO2 becomes trapped in the alveoli - Air Trapping results in formation of BULLAE!!! - BULLAE can RUPTURE… (pneumothorax) ○ Symptoms▪ PINK PUFFERS □ Pink represents adequate O2% in periphery WITHOUT CYANOSIS ▪ Dyspnea / fatigue ▪ Pursed lip breathing & use of accessory muscles ▪ Decreased PO2 (60-80) □ Progressively increasing PCO2 (air trapping) ▪ Barrel Chest (hyperinflation d/t air trapping) Atelectasis- Incomplete expansion of the lung or portion of the lung - Etiology○ Airway obstruction ○ Compression of lung tissue ▪ Trauma (pneumothorax) ▪ Tumor- erodes pleural wall and results in fluid buildup.. .places pressure on pleura inhibiting expansion ○ Lack of Surfactant - Signs & Symptoms○ Tachypnea & Tachycardia (compensation) ○ Dyspnea ○ Cyanosis / Hypoxemia ○ Decreased chest expansion (part of lung isn't inflating) ▪ Absent breath sounds Pneumothorax- Presence of air within the pleural space (partial or complete collapse of the lung) - 3 Types: ○ Spontaneous▪ Rupture of a bleb/bullae ▪ Cause unknown, but associated w/ males & heavy smoking ○ Traumatic▪ OPEN pneumothorax□ Severe trauma allows atmosphere air to enter cavity □ Need to insert Chest Tube to drain blood/air that's entering the pleural cavity □ Less emergent than a CLOSED Pneumothorax… - You're able to apply dressing to wound to control airflow in/out Patho Page 56 ○ Traumatic▪ OPEN pneumothorax□ Severe trauma allows atmosphere air to enter cavity □ Need to insert Chest Tube to drain blood/air that's entering the pleural cavity □ Less emergent than a CLOSED Pneumothorax… - You're able to apply dressing to wound to control airflow in/out ○ Tension Pneumothorax▪ Intrapleural pressure exceeds atmospheric pressure and prevents airflow into lung ▪ Closed = Tension Pneumothorax□ Some form of trauma that closes instantly (bullet wound) □ Tension builds in pleural space d/t air inside lungs escaping □ THIS IS A SURGICAL EMERGENCY - Signs & Symptoms○ Increased RR & HR ○ Dyspnea ○ Hypoxemia ○ Decreased/Absent breath sounds ○ Asymmetrical Chest Expansion ○ Mediastinal Shift▪ Trachea & vessels will be shifted to one side ▪ Direction of shift dependent on pressure differential Infections of Respiratory Tract- Common Cold○ Viral infection ○ Highly contagious the first 3 days when symptoms BEGIN! ○ Sxs▪ Watery, clear secretions ▪ Erythematous mucous membranes ▪ Swollen, sore throat ▪ Hoarseness ○ Rx▪ NO ANTIBIOTICS ▪ Encourage rest ▪ Symptomatic treatment w/ OTC meds - Influenza○ Viral Infxn ○ Common COD in the elderly ○ Highly contagious 24 hrs BEFORE SXS START ▪ Continue to be contagious for 5-10 days ▪ Transmitted via droplets (cough) □ NOT BY CONTACT/touch - Remember… this is a VIRUS… it CANNOT survive w/o a HOST ○ Sxs▪ MALAISE ▪ NON-PRODUCTIVE Cough ▪ Fever, chills, muscle aches ▪ HA ○ Rx▪ Rest, fluids, & aspirin □ DO NOT GIVE ASA TO CHILDREN under 12 (develop Reye's Disease) ▪ Antivirals (Amantadine) prevent replication of DNA □ Must be used in first 30 hrs of infxn ○ Prevention is the Primary Treatment/Focus▪ Everyone over 6 y/o needs to vaccinated yearly ▪ 3 strains of Influenza (A,B,C) □ A & B cause the flu epidemics □ 16 different variations divided into Hemogglutinin & Neuraminidase - H1N1, H2N3, etc. □ Tamiflu is a drug that acts against the Neuraminidase □ These different variations can infect all types of animals (swine, birds, chickies, etc.) ○ If left untreated it can develop into Viral Pneumonia - Pneumonia○ Inflammatory rxn in the alveoli & interstitial tissue of the lung from a pathogen ○ 6th leading COD (mostly in elderly) ○ Frequent complication of Flu & Immunocompromised ○ Categories of Pneumonia▪ Type of Agent□ Typical = bacteria □ Atypical = mycoplasmas or viruses d/t disease condition of lungs (stasis of mucous) ▪ Distribution w/in lungs□ Lobular Pneumonia □ Broncho-pneumonia ▪ Setting□ HAI - Pseudomonas aeruginosa, S. aureus, E. coli - Medicare doesn't cover health care costs of HAI's □ Community Acquired- Influenza, S. aureus, Mycoplasma pneumoniae, Chlamydia - Must be Dx w/in 48 hrs of admission - Pt must not have lived in long-term facility w/in 14 days prior to admit ○ Patho- Patho Page 57 Tension Pneumothorax- Air can enter but CANNOT LEAVE - Increases intrathoracic pressure ○ Results in heart & vessel shifting to unaffected side ○ Unaffected lung is compressed ○ Patho▪ Microbial agents multiply & cause inflammation ▪ Alveolar spaces fill w/ exudate/mucous ▪ Results in poor oxygenation d/t less surface area for gas exchange (hypoxemia) ▪ Exudate can solidify and become difficult to expectorate ○ Dx▪ Sputum culture & sensitivity ▪ Symptomatology ▪ CHEST XR - Pneumococcal Pneumonia○ S. pneumoniae = most common cause of bacterial pneumonia ○ 4 stages of the disease ○ Signs & Symptoms▪ Fever, chills, malaise □ Elderly rarely run fevers!!! - If they present w/ fever, the infxn is very severe - Watch for signs of rapid mental deterioration ▪ Productive cough ▪ Bloody sputum ○ Rx with ANTIBIOTICS ▪ Levofloxacin ▪ Piperacillin ▪ Cefotaxime ▪ Vancomycin ▪ Gentamycin ○ Primarily focus on PREVENTION □ Pneumococcal vaccination (65+ y/o & immunocompromised) □ 2 vaccines: both vaccines recommended for elderly 65+ - Tuberculosis- #1 COD from a SINGLE organism worldwide ○ Incidence has rapidly declined w/ vaccines but increased again with increase of HIV rates ○ HIV is most associated w/ TB ○ Increased d/t immigration from countries w/ high incidence/prevalence - Mycobacterium tuberculosis ○ Spread by airborne droplets ▪ Aka… living in close-confined quarters - TB mostly effect lungs but can affect all organs ○ Best survives in oxygen rich environment - Patho○ Macrophages initiated a cell-mediated immune response ▪ Contains the infxn and calls on T-cells ▪ T-cells "approve" the macrophages to initiate cell-mediated response □ Release lytic enzymes and cells undergo apoptosis ▪ This results in the cheese-like appearance of lung tissue in Chest XR ▪ Lasts 3-6 weeks □ Indicates the pt is EXPOSED but they DON'T have ACTIVE TB □ Aka… the TB is walled off and not actively infecting more tissue ○ TB can be latent for a long period of time ▪ Becomes active when the immune mechanisms fail and the TB is released from the walled off protection - Symptoms○ Insidious & Non-specific symptoms ○ Cardinal Signs of TB: ▪ Wt loss ▪ Night Sweats ▪ Fever ▪ Cough □ Once TB spreads to the sputum, it can be transmitted to another person - Diagnosis○ PPD, Chest XR ○ Sputum Tests!!!! - Rx○ Multiple drug combinations are MANDATORY ▪ INH (isoniazid), Rifampin, Pyrazinamide, Ethambutol, Streptomycin for 6+ mos ○ Drug resistant TB is rare… Arterial Blood Gasses- Normal values: ○ pH = 7.35 - 7.45 ○ HCO2 = 24 - 31 22-26 (arterial) ○ PCO2 = 35 - 45 mmHg (indicative of ventilation) ▪ Decrease in ventilation = increase in PCO2 ○ PO2 = 80 - 100 mmHg (indicative of perfusion) - Acid-Base Balance○ First determine Acid/Alkaline per pH level ○ Then determine if PCO2 or HCO3 is altered ▪ PCO2 off = respiratory ▪ HCO3 off = metabolic ▪ Whatever is normal = cause is opposite Module 15 | NeoplasmsPatho Page 58 Module 15 | NeoplasmsNew, unregulated growth = neoplasia - Uncoordinated growth due to lack of regulatory mechanisms Cancer Stats!!! - #1 cancer = skin cancer ○ Lung Cancer = #1 Cancer COD for MEN & WOMEN - 76% cases are diagnosis after age 55 - Cancer 5 year survival rate = 65% - 2nd COD in USA - Cancer rates higher in males - Incidence & mortality rates are highest in Blacks - Survival of Cancer dependent on○ Poverty ○ Access to care ○ Poor health when diagnosed ○ Comorbidities ○ Differences in cell/tumor biology ○ Later staging of the cancer Invasive Growth- Cancer cells are able to grow into different/adjacent tissues ○ Normal cells cannot do this (bladder cells can't extend into the pelvic wall) Cell Growth- Cell Proliferation○ Tissues acquire new cells through mitosis ○ Increase in the number of cells as a result of cell division - Differentiation○ Proliferating cells are transformed to specialized cells ○ Have a specific function ○ Hepatic cells, muscle cells, etc. - Apoptosis○ Normal programmed cell death ○ Used to eliminate old, damaged, excess cells - Neoplasm○ Increase in neoplastic cells due to uncontrolled proliferation w/ invasion into surround tissues ○ They avoid the apoptosis process and continue to grow, divide, and live. Stem Cells- Remain incompletely differentiated throughout their lifetime - "reserve cells" ○ Remain dormant until an appropriate stimuli causes them to proliferate - 2 Important Features of Stem Cells○ Self-renewal▪ Stem cell can undergo various mitotic division while remaining undifferentiated ○ Potency▪ This is the differentiating potential - Can treat health problems like Cancer ○ Typically used in Spinal Cord Injuries to help the neurons regenerate ○ Can use stem cells to treat Diabetes, Parkinson's, Muscular Dystrophy Chemotherapy drugs act on different parts of the cell cycle - The Cell Cycle -----------------------------------------------------------------------------> - Cell Cycle Specific ○ Action of the drug is exerted in a specific phase of the cell cycle ▪ Methotrexate interferes w/ DNA synthesis (G1) - Cell Cycle Nonspecific○ Exert drug effect on all phases of the cell cycle ○ Can act in the Resting State, DNA synthesis, or during mitosis - Combination Chemo○ Combination of the Cell Cycle Specific & Nonspecific ○ Ex: ABVD used to treat Hodgkin's Lymphomas Benign vs. Malignant- Benign can grow by expansion w/o invading other tissue and is encapsulated - Malignant grows by invasion and infiltrates surrounding tissue - Cell Characteristics○ Benign▪ Well differentiated cells and represent normal cells of that organ ○ Malignant▪ Poorly differentiated - Rate of Growth○ Benign▪ Progressive/slow ▪ Can regress and stop growing altogether ○ Malignant▪ Depends on the level of differentiating ▪ The more undifferentiated the cells are, the quicker it grows - Modes of growthBenignPatho Page 59 **Differentiation is the development of SPECIALIZED cells - Undifferentiated requires less time to grow…. - AKA… the more undifferentiated, the faster the growth ○ Benign▪ Don't invade. ▪ Grow by expansion ▪ Usually encapsulated or contained ○ Malignant▪ Invade other tissues, lymph & blood - Metastasis○ BENIGN DOESN'T METASTASIZE! ○ Malignant▪ Access the blood, lymph, etc. to spread to other parts of the body ▪ Malignant metastasizing neoplasms retain the characteristics of the original cell site □ Originating in the ovaries and metastasizes to the lungs…. Tumors in the lungs will have ovarian cell characteristics Metaplasia- Chronic irritation or injury there is a change in the type of adult cells in that tissue - Ex: smoker's squamous cell epithelium results in changes in the types of cells of the esophagus ○ Barret's Esophagus = increased r/o developing cancer Dysplasia- Alteration in the adult cell size, shape, organization, and number of cells - Ex: cervical dysplasia (PAP smears) The Cancer Development Process- See figure ----------------------------------------------------------------------------> - Dysplasia - IN SITU STAGE ○ Neoplasm confined to the original site and hasn't spread to surrounding tissue/organs ○ Early stage cancer ○ Malignant cells haven't crossed basement membrane ○ Usually can be surgically removed or treated ▪ It's in one location so it's easy to pluck out ▪ Very low chance of reoccurring □ "Cervical In Situ Cancer = 100% survival rate" - Invasive neoplasm Carcinogenesis- Process by which carcinogens cause normal cells to become cancer cells ○ Carcinogens- (chemical, physical, biological) ▪ Colon cancer can be caused by diets high in fats ▪ Diets high in nitrates = high incidence of cancer - Phases of Carcinogenesis-- understand them but don't go crazy -○ Initiation▪ Carcinogen is introduced to the tissues ▪ Produces change in the genome of the normal cell ○ Promotion▪ Induction of unregulated/accelerated growth in cells that have already been initiated by growth factors or chemicals ▪ Reversible if you remove the carcinogens ○ Transformation▪ Cell changes to a non-normal cell ▪ Escapes normal control mechanisms ▪ Increase in growth ▪ Changes in the cell membrane/surface ○ Progression▪ Cells acquire malignant phenotypes ▪ Can promote cell proliferation ▪ i.e. can lead to metastasis Angiogenesis- Tumor is causing new vessels to be produced to allow tumor to grow Control of Cell Replication- Cancer cells have to ability to grow indefinitely 6 Hallmarks of Cancer- Self-Sufficiency in emitting growth signals - Limitless replication potential - Insensitivity to regulatory signals - Evading apoptosis - Sustained angiogenesis - Tissue invasion / metastasis ○ Normal cells stop growing when they come into contact with other cells ○ Cancer cells continue to grow and "crowd out" normal cells Cancer Genes- Proto-Oncogenes○ Normal genes that become cancerous if they are MUTATED ○ These cells encode for growth factors ○ Can be MUTATED BY: ▪ Chromosomal Translocations□ Genes move from one chromosome to another □ Burkitt Lymphoma □ Chronic Myelogenous Leukemia Patho Page 60 □ Chronic Myelogenous Leukemia ▪ Gene Amplifications□ Multiple copies of genes enhance gene expression which can increase cell proliferation □ AKA genes in breast cancer Cancer Patho- Genetic damages causes cells to mutate - Cell's revert from a differentiated state to an undifferentiated state - Proliferation of cells is continuous ○ Proliferation = time it takes for the tumor to double in size Classifying Cancer- Anatomic Classifications○ Carcinomas▪ Originate in epithelial or mucosal tissues ▪ Basal Cell Carcinoma (skin cancer) ○ Sarcomas▪ Originate in bone, muscle, or nerve ▪ Osteogenic sarcoma (bone cancer) ○ Adenocarcinomas▪ Adeno = Glands ▪ Lymphoma, melanoma, etc. - Histologic Class○ Requires MICROSCOPIC EXAM to class this ○ Grades 1, 2, 3, & 4 ▪ Looking at the level of differentiation, rate of mitosis, number of normal cells, etc. ○ Grade 1▪ Mild dysplasia ▪ Differ very little from normal cells ○ Grade 4▪ Immature cells □ Immature cells indicate rapid, unregulated growth ▪ Cell origin is difficult to determine Incidence & Mortality- Most Common Incidences: ○ SKIN = most common site OVERALL ○ Prostate, Lung, Colorectal = most common site for MALES ○ Breast, Lung, Colorectal = most common site for FEMALES - Most Common Mortalities: ○ #1 COD in both sexes = LUNG CANCER ▪ Males = Lung, prostate, colorectal ▪ Females = Lung, breast, colorectal Lung cancer- One of the most common malignancies - 25% of the time Lung Cancer is ASYMPTOMATIC - Signs & Symptoms○ Difficulty breathing ○ Wheezing breath sounds ○ Hoarseness ○ Chest pain, back pain, shoulder radiating pain ▪ "Cancer" Pain usually occurs in the later stages of cancer Early Warning Signs- Unusual bleeding/discharge - Un-healing lesions - Change in bowel habits - Nagging cough / hoarseness - Lumps - Changes in moles/lesions - Dysphagia Staging Cancer- Purpose of Staging○ Gives them a method to determine how far it's spread ▪ Helps them determine their prognosis and treatment plan (surgery, further tests, etc.) - The earlier the stage = the better the prognosis ○ The very earliest stage = Carcinoma In Situ ▪ Completely curable if removed at this stage - TNM Method (tumor, lymph nodes, metastases) ▪ This is one method… some companies may use different staging methods ○ Tumor (T)▪ Staging on the size of the tumor ▪ 0-3 (3 is the worst) ○ Nodes (N)▪ Regional lymph node involvement ▪ Metastasizes into the nearest lymph nodes (same region/compartment) □ Breast cancer = Axillary Lymphs ▪ N = 0 … 0 lymph nodes involved ▪ N 1 = few N 2 = systemic Patho Page 61 Incidence: - Skin = Overall - Males○ Prostate ○ Lung ○ CR - Female○ Breast ○ Lung ○ CR Mortality: - Lung = Both - Males○ Lung ○ Prostate ○ CR - Female○ Lung ○ Breast ○ CR ▪ Regional lymph node involvement ▪ Metastasizes into the nearest lymph nodes (same region/compartment) □ Breast cancer = Axillary Lymphs ▪ N = 0 … 0 lymph nodes involved ▪ N 1 = few ▪ N 2 = systemic ○ Metastasis (M)▪ Absent or present ▪ M 0 = no metastasis ▪ M 1 = metastasis ▪ Can have a higher M number if the metastases are everywhere…. ○ Examples: ▪ Non-Small Cell Lung Cancer □ T2 = Tumor measures 2 cm □ N1 = Lymph involved □ M0 = No metastases Staging and Grading- Staging○ How big is the tumor ○ Has it spread ○ See above!!! - Grading○ Microscopic exam via microbiologist ○ How abnormal are the cells (Grades 1-4) ▪ Low grade = slow, progressive, less aggressive ▪ High grade = rapid growth, poorly differentiated - Nursing implications○ Nurses need to know the stage and grade bc…. ▪ To know their pain per pt subjective data ▪ Stage and Grade affects the Rx plan □ Rx plans can be VERY RIGID and SPECIFIC and INDIVIDUALIZED per pt ▪ Need to have psychological implementations to comfort them Risk Factors- Heredity - Hormonal Factors (estrogen / androgens) - Immunologic factors (AIDS related = Kaposi's Sarcoma) - Environmental/Chemical Carcinogens○ Oncogenic Viruses (HPV = cervical cancer) ○ Smoking and secondhand smoke ○ Lifestyle factors- obesity, diet, tobacco, alcohol, etc. ▪ Foods fried in used oil ▪ Nitrates in smoked/cured meats ▪ Fatty red meats ▪ Low fiber intake ▪ High fat diets ○ UV radiation ○ Occupational carcinogens TOBACCO- Contains both pro-carcinogens (interfere w/ cell regulatory controls) and promoters (change the genetic expression) - Lung, laryngeal, head/neck cancer, pancreas, uterine, cervical, bladder, etc. - 30% of ALL cancer deaths - 87% of LUNG cancer deaths Symptoms of Most Solid Tumors- Anemia○ Decreased RBC level ○ Tumors is drawing up normal amount of blood and making the body anemic ○ Bone marrow suppression - Anorexia & Cachexia (muscle wasting) - Fatigue and sleep disorders - Compression/obstruction of tissues/organs - Pain (not usually an early symptom) ○ SEVERE PAIN is associated with LATE STAGES of Cancer - Psychosocial integrity & QOL Diagnostics- Biopsy, XR, CT, endoscopies - Determine the stage and grade - Tumor Markers○ Sampled via blood test ○ Antigens expressed on the surface of tumor cells ○ Or the substances released from normal cells when tumor cells are present ▪ "HEEELLLLPPPP USSSS!!!!!" ○ Clinical Significance- use these for… ▪ Screening ▪ Establishing prognosis ▪ Monitor/evaluating treatment plan effectiveness ▪ Detecting recurrent disease ○ Carcinoembryonic Antigen ▪ CEA- Patho Page 62 ▪ CEA▪ Source of embryonic tissue of the gut and pancreas □ Used in suspected Colorectal, Pancreas, Stomach, etc. ○ CA-125 ▪ Marker for Ovarian cancer ▪ Produced by ovarian cells ○ PSA ▪ Prostate Specific Antigen □ Produced by epithelial cells of prostate ▪ Marker for Prostate Cancer Treatment- Surgery○ Oldest Rx for cancer ○ Can use surgery to Dx, stage, remove tumors, or palliative ○ First choice of treatment for SOLID TUMORS ○ Ex: Cryosurgery, chemosurgery, laser, laparoscopic - Radiation○ Rapidly proliferating and poorly differentiated cells are killed off by radiation ▪ AKA… it doesn't affect normal tissues as much ○ Can be used alone or as an adjuvant treatment (w/ surgery or chemo) ○ This can be a palliative form of treatment ○ Method▪ External beam ▪ Insertion of radioactive seeds/beads ○ Side Effects▪ Primary side effect of radiation = FATIGUE □ Bone marrow is suppressed causing ANEMIA ▪ Bone marrow is suppressed □ Neutrophils are decreased and they are at EXTREME RISK OF INFECTION = NEUTROPENIA - WBC are HIGHLY MITOTIC □ Also will have anemia ▪ Xerostomia = dry mouth ▪ Hair loss ▪ Skin burns □ DON'T USE LOTION ON THESE AREAS - Can cause severe damage to the skin when combined w/ radiation ○ DO NOT WASH OFF RADIATION LINES - Chemotherapy○ Most effective against rapid proliferating cells ○ Some are specific/nonspecific/combo therapy ○ Side effects▪ Anorexia, N/V, alopecia, □ Since chemo targets rapidly dividing cells, the hair is prevented from growing - Hair is RAPIDLY DIVIDING - N/V = GI cells are rapid dividing cells ▪ Bone marrow suppression□ Bone marrow produces WBC, RBC, & platelets □ Suppression makes you more susceptible to infection, anemia, and hemorrhage ▪ These types of cells replicate V V V V QUICKLY which causes the chemo to kill these cells ○ Pregnant people cannot enter pt room w/ chemo therapy Anti-Cancer Drugs- Chemotherapy only applies to cytotoxic agents - Four Major Classes of Drugs○ Cytotoxic agents- kill cells directly ○ Hormones & Hormone antagonists ▪ (breast & prostate cancers) ○ Biological response modifiers ○ Targeted drugs▪ Bind to specific molecules ▪ Breast cancer Rx… Chemotherapeutic Drugs- They kill cancerous cells or reduce the number of cells ○ Slay bish - Combination Therapy = 2-3 different drugs ○ More effective than just one drug - Protocols○ Predesigned schedule of treatment plans ○ Very strict and individualized schedule of treatments Stomatitis = sores in the mouth Module 11 | Cardiovascular- Patho Page 63 Organization of the Circulatory System - Pulmonary Circulation ( blood in the heart and lungs) - Systemic Circulation (the rest of the body) - Central Circulation (Heart and lungs) - Peripheral Circulation (outside of the heart and lungs) - Coronary Circulation- circulation in the coronary arteries and veins supplying the heart itself with blood Volume and Pressure Distribution- Blood flow depends on a blood volume to fill vessels and pressure push the blood ○ Blood flow begins in the LV - Moves from high pressure arterial system to low pressure ○ LV pressure = systolic pressure and maintains that pressure throughout the arterial system ○ RA pressure is usually 4 mm/Hg (VERY FCKIN LOW) - Venous system carries about 2/3 of the blood supply ○ Can stretch and expand to hold heavy volumes of static blood ○ Contain valves to prevent backflow of the low pressure blood Anatomy of the Heart - Pericardium○ Protection for the heart from infections ○ Consists of parietal and visceral layers ○ Pericarditis - Myocardium○ Muscle of the heart ○ Myocardial infarction- muscle layer of the heart was affected ○ Myocarditis - Endocardium○ Consists of three layers which include the heart valves ▪ Endocarditis = has infected the valves Myocardium - Cardiac muscle contraction is involuntary - Duration of contraction is much longer than skeletal muscle - Contraction dependent on calcium, potassium and sodium movement ○ Primary Electrons = Sodium & Potassium ○ Electrical conduction starts in the RA @ the SA node and then travels to the AV node then to Bundle of His ○ This conduction involves the exchange of Na & K b/w the cell membranes ▪ This movement is DEPOLARIZATION □ Without Na, K, Ca, Mg, depolarization cannot occur AND THIS IS V BAD - Muscle cells are arranged as intercalated disks ○ Serves as pathways for ions and electrical impulses ○ Allows the heart to contract as a SINGLE UNIT Heart Valves - Aortic, Pulmonic, Tricuspid, Mitral - AV valves are the mitral (bicuspid) and tricuspid ○ Supported by the chordae tendineae - Semilunar valves are the pulmonic and aortic and are shaped like half-moons - Valves must open and close properly or stenosis or regurgitation will occur Heart Sounds - Murmurs are abnormal heart sounds caused by the flow of blood across a diseased valve. ○ The narrowing ( stenosis) of the valve produces turbulence and rapid blood flow. ○ Also, a decreased viscosity of blood increases blood flow ▪ Ex: severe anemia - Clicks are sounds emitted by the valves when opening is impaired - S1 is the sound of the AV valves closing ○ Best heard at the apex of the heart - S2 sound of the SL valves closing ○ Best heard at the base of the heart Infective Endocarditis- Relatively rare but with significant mortality - May evolve over years/months or very quickly - Risk Factors○ Strep throat- Under- treated as a child ▪ AKA the abx therapy is unfinished ○ Drug abuse ○ Congenital heart defects ○ Mitral valve prolapse - Etiology○ Streptococcal with childhood strep ○ Congenital disorders ○ Staph infections in drug abusers ○ Other bacterial, fungal infxn - Patho○ Vegetative lesions form on the valves ▪ Release bacteria into bloodstream Patho Page 64 ▪ Release bacteria into bloodstream ▪ Lesions break off and form an obstruction ○ The lesions grow larger, weigh down the valves and cause: ▪ Regurgitation ▪ Stenosis - Signs and Symptoms○ Fever, cough, dyspnea ○ New heart murmur develops when they're older adults ○ Petechieae, splinter hemorrhage (due to obstruction in small vessels) - Treatment○ Must diagnose with blood cultures ○ IV antibiotics for six weeks (a million units of penicillin Q2H intradermal) ▪ High doses of Abx lead to other microbes growing □ Primarily vaginal FUNGAL INFXN □ C. diff, etc. ○ Prophylaxis with certain procedures ○ Valvular replacement may be necessary Cardiac Flow - See Figure --------------------------------------------------------------------------------------> Cardiac Cycle- 1st heart sound- closure of AV valves - Systole- ejection of blood (high ventricular pressure); ventricular depolarization - 2nd Heart sound- closure of semilunar valves - Diastole- ventricular repolarization, (T wave) ○ Heart is resting and ventricles are filling ○ Ends with atrial contraction ▪ 30% more blood volume into ventricles for systole Mechanical and Electrical - Electrical activity DOES NOT = pumping activity ○ Called Pulseless Electrical Activity (PEA) ▪ Pumping activity of the heart fails but electrical activity continues ○ PEA DO NOT SHOCK W/ defibrillator….. (need V-tach/V-fib to shock) Cardiac Conduction - If there are any blockages in the conduction (MI) in the muscle, than the EKG will show error in the conduction pathways - P wave = atrial depolarization - QRS = V depolarization & A repolarization - T = V repolarization Cardiac Cycle and Electrical Activity - Electrical Activity PRECEDES mechanical activity ○ P wave = atrial depolarization…. Atrial contraction soon to follow - SA node○ Innervated by the sympathetic and parasympathetic nervous System ▪ PSNS is innervated by the Vagus, located in the Medulla □ i.e. head trauma to the back of the head can lead to damaged medulla and cause the heart to stop beating ○ SA automatically fires and the electrical impulse travels to the…….. - AV node○ Impulse is slightly delayed. - Bundle of His- The impulse travels the left and right Bundle branches to the…….. - Purkinge fibers- innervates and depolarizes the myocardial cells. EKG- See figure ------------------------------------------------------------------------------------> - Measure the electrical activity of the cardiac conduction The Heart as a PUMP - Hemodynamics and Pressure ○ Low right atrial pressure allows for cardiac filling ▪ V V V LOW PRESSURE (about 4 mm/Hg) to allow the blood to make the complete circuit - Venous return is affected by amount of blood available to come into the heart, ○ e.g. shock, not enough fluid or too much fluid; RAP increases if lung pressure increases - Atria contract just before systole and add 30% to volume in ventricles Hemodynamics and pressure - If the Ventricular pressure increases then Atrial pressure increases - Preload is the volume of blood coming into the left ventricle causing muscle stretch. ○ Amount of blood the Right Ventricle will have to push into the pulmonary circuit during systole ○ The more you stretch the fibers in systole, the stronger the cardiac output ○ It represents workload for the heart. ○ There are medications such as nitroglycerin which can be given to decrease preload so the heart doesn’t have to work so hard. Pressure - Frank-Starling Law: ○ The more muscles are stretched in diastole the greater the contraction in systole. i.e. like a spring!!!! Patho Page 65 ○ ▪ i.e. like a spring!!!! ▪ V are filling in diastole (you want as much time for diastole to increase V filling) □ Any HR above 100 = reduced filling time (the faster the HR the worse it gets) - The stretch is about 2 1/2 times resting length ○ This results in a Normal Stroke Volume of 70 mL in Adults Cardiac Output (CO) - CO = (SV X HR) ○ Normal for adults = 4-6 L/min - Cardiac output increases with physical activity and decreases with rest - CO varies with body size and metabolic needs - FYI: Cardiac output can be clinically measured with the pulmonary artery catheter using the Fick temperature method Afterload- Afterload = "Systemic vascular resistance" - Afterload directly affects pumping - Afterload can also be considered the pressure the ventricles works against. - ANYTHING THAT INCREASES SYSTEMIC VASCULAR RESISTANCE INCREASES AFTERLOAD ○ Arterial blood pressure = main source of afterload LV ○ Pulmonary pressure = main source of afterload RV ○ Increase in serum lipids ○ Aortic stenosis Cardiac Contractility - The ability of the heart to change the force of its contraction without changing the length of diastole ○ Heart is working more efficiently - Contractility is based on the number of calcium ions available ○ Calcium affects actin/myosin interactions in the myocardial cells. Automaticity - Ability of certain cells in the conduction system to repeatedly beat or conduct - Classic Experiment Regulation of Cardiac Performance - Preload - Afterload - End-diastolic ventricular volume ○ This is the amount of blood in the ventricles that can be ejected out ○ Ejection fraction- amount of residual blood left in the ventricle after systole ▪ Normal = 70% ejection fraction ▪ Lower ejection fraction indicates poor pumping ability (CHF, MI, etc.) - Cardiac Contractility ○ Calcium channel ions & interaction of actin/myosin filaments - Heart rate ○ Both tachycardia & bradycardia will decrease cardiac output. ▪ In tachycardia there is not enough time to fill ▪ Bradycardia, the heart doesn’t beat enough ○ CO = HR X SV ▪ The amount of blood the ventricles are pushing out of the heart ▪ If HR increases and SV stays the same CO increases □ Tachy can result in decreased SV and Decreased CO - Heart can't fill properly □ Brady can result in decreased CO Blood Pressure- BP = CO x total peripheral resistance (TPR) ○ CO = SV X HR - BP is the amount of pressure exerted against the walls of the blood vessels ○ Think of diastole as constant pressure - Arterial Blood pressure results from contraction of the left ventricle during systole ○ This sends a pressure wave through the arteries & arterioles ○ This is what you're palpating - The Blood pressure in the aorta = 120 during systole & 80 during diastole ○ Mean arterial pressure is about 90 ○ Pressure in the venous system and vena cava is very low approaching zero and in the right atrium can be as low as negative 3-5 mm ▪ Can be negative d/t hypovolemia, shock, etc. - Blood pressure cuff indirectly measures ○ DIRECT measurements include Arterial Line's and Swan-Gantz line (Pulmonary Artery) Regulation of Blood Pressure - Short-term regulation○ Control BP over seconds/minutes/hours ○ Maintain life and function. ▪ Neural mechanisms ▪ Humoral mechanisms - Long-term regulation ○ Control over days and involve ▪ Renal / Fluid body system. ▪ Endothelial control - Neural Mechanisms (short term) Patho Page 66 - Neural Mechanisms (short term) ○ Mediated by Autonomic Nervous System via baroreceptors, chemoreceptors, and blood pressure responses to heat and cold. ▪ Emotions and changes in mood can also alter BP ○ Baroreceptors and chemoreceptors are located in the circulatory system ▪ Ex: Aorta and carotids ○ Baroreceptors respond to pressure changes ▪ Induce vasoconstriction & Increase HR to prevent orthostatic hypotension ○ Chemoreceptors▪ Detect changes in O2, CO2, and H+ content of the blood ▪ Induce vasoconstriction and regulate ventilation due to a buildup of CO2 and H+ ions - Humoral Mechanisms- (short term) ○ Renin-Angiotensin-Aldosterone system (RAAS)▪ Do this on the dry erase board ▪ Renin is made and stored in the juxtaglomerular cells of the kidneys in response to a fall in B/P or sympathetic stimulation or decreased extracellular sodium concentration. ▪ Renin then converts angiotensinogen (plasma protein) to angiotensin I ▪ Angiotensin I is converted to Angiotensin II □ ACE (angiotensin converting enzyme) - ACE Inhibitor (Lisinopril & drugs ending in "pril") - Blocks the production of ACE and causes a decrease in blood pressure ▪ Angiotensin II is a strong vasoconstrictor and stimulates aldosterone (from the adrenal glands) by increasing salt and water retention □ Angiotensin Receptor Two Blockers = ARB/ART (Losartan) blocks this process ○ Vasopressin (ADH)▪ Released from the posterior pituitary…… due to….. □ Decreases in blood pressure □ Increase in serum osmolality ▪ Direct vasoconstriction of blood vessels □ INCREASES BLOOD PRESSURE in critical situations (shock, hemorrhage, etc.) ▪ Relative short-term action since it does not produce volume expansion □ It simply prevents the excretion of MORE volume (urination) - Renal Body Fluid System- (long term) ○ Regulates fluid volume and sodium level ○ Increase in fluid volume causes a rise in arterial blood pressure by: ▪ Increasing cardiac output which causes systemic vasoconstriction (increased systemic vascular constriction) ○ Patho▪ When Cardiac Output increases Tissues are Exposed to Increased Blood Flow ▪ Tissues respond to this increase in blood flow with Vasoconstriction *** They are saying "Hey we have enough blood…. Go somewhere else ▪ Autoregulation = tissues regulate their own blood flow ▪ Systemic vasoconstriction in response to increased cardiac output results in systemic increase of Blood Pressure - Endothelial Control of Vasodilation and Vasoconstriction- (long term) ○ Endothelium produces substances to regulate blood pressure ○ Nitric oxide▪ Causes vasodilation ▪ Inhibits platelet aggregation ▪ Ex: Nitroglycerin promotes release of Nitric Oxide from the endothelium ○ Prostaglandins▪ Prostacyclin □ Causes vasodilation □ Inhibits platelet aggregation ▪ Thromboxane A2 □ Causes vasoconstriction □ Increases aggregation of the platelets □ Low Dose Aspirin (81 mg) blocks this response ▪ Prostacyclin vs. TXA□ Counteract each other - TXA wing man for the Platelets tryna get them to link up but Prostacyclin is all like nah bruh □ Whatever is being produced more is going to happen ○ Angiotensin II▪ Local vasoconstriction ▪ Stims aldosterone secretion from adrenal glands Primary (Essential) Hypertension- Etiology Unknown ○ Family History▪ V large component of acquiring HTN ▪ Risk increases 1st degree relatives with HTN before age 55 ○ Age- BP increases with age ○ Hyperinsulinemia and insulin resistance (T2DM)▪ Insulin activates the sympathetic system □ Increases systemic vascular resistance ▪ High triglycerides and low HDL’s □ Can result in HTN - Risk Factors○ Race▪ More prevalent and more severe in Blacks ▪ Blacks increased incidence of CVD and renal disease High salt intake (more in blacks)Patho Page 67 ○ High salt intake (more in blacks)▪ “Salt thrifty gene” ▪ More sensitive to salt increasing their BP ○ Obesity▪ CENTRAL obesity (located around the abdomen) is associated w/ HTN □ W 35+ % of body fat or something □ M 40+ % ○ Sodium & potassium intake ▪ A high sodium diet is low in K ▪ Increased K intake causes increased secretion of Na ○ Excess Alcohol consumption▪ Regular intake of 3 drinks or more daily increases B/P; ▪ Limit is 2 drinks in men and one drink daily in women. ○ Stress ○ OCP's ▪ Usually over 35 and smoking ▪ Causes mild hypertension and mortality in about 5% High Blood Pressure (HTN)- HTN is a CHRONIC DISEASE - See figure ------------------------------------------------------------------------------------> - Diabetes patients should have a BP below 130/80 - Signs and Symptoms of Hypertension○ Typically asymptomatic ○ Headache▪ Usually a late symptom ○ Latent symptoms relate to target organ damage **You've had HTN a long time and finally causing damage to other organs** ▪ Brain = CVA □ #1 organ affected ▪ Kidneys- loss of ability to concentrate urine ▪ Heart- Heart failure, CAD, sudden death ▪ Circulatory- peripheral vascular disease - Treatment○ Lifestyle modifications ▪ Diet, physical activity, smoking cessation, etc. ○ Pharmacologic treatment ▪ Begins with a single drug (Step-Wise Therapy) ▪ Usually a beta blocker or calcium channel blocker □ In DIABETES an ACE Inhibitor is used bc they're non-nephrotoxic ▪ Then add other HTN drugs PRN □ Diuretics (i.e. furosemide/Lasix) - Thiazide diuretic = best for blacks □ Beta-blockers (Metopr-olol) □ ACE inhibitors (Lisin-opril) □ Alpha1 blockers (Praz-osin) □ Calcium channel blockers (Nifed-ipine) □ ARB's (Angiotensin II receptor blockers) = (Los-artan) HTN and blood vessels - HTN damages blood vessels….. Damaged blood vessels increase HTN ○ Injury to vessels results in an inflammatory response ▪ This can increase vessel wall thickness and increase HTN ○ Double-whammy - Atherosclerosis ○ Formation of plaque buildup on the inside of blood vessel walls ▪ Makes the inner lining rough ▪ Easy for cholesterol stick to it ▪ Causes the formation of plaque ○ THIS IS DIFFERENT FROM Arteriosclerosis - Arteriosclerosis○ Chronic disease of the arteries ○ Abnormal thickening & hardening of artery walls ○ Can worsen blood pressure ▪ May develop with age, diabetes, & high fat diets - Hypertension: Summary ○ UNKNOWN ETIOLOGY for primary hypertension ○ Multiple mechanisms controlling blood pressure ○ No symptoms (silent killer) ○ Main complication is a CVA ○ Treatment focuses on lifelong drug therapy, maintaining normal weight, and reduced sodium and fat in diet are helpful Coronary Artery Disease (CAD) / Coronary heart disease (CHD) - Impaired coronary blood vessels○ Includes: angina, MI, cardiac dysrhythmias, conduction defects, congestive heart failure, and sudden death. ▪ This is a continuum - CAD is #1 COD in U.S. in both males and females - Etiology = Atherosclerosis - Coronary Circulation Left and right coronary arteries supply the cardiac muscle and heart with oxygen Patho Page 68 Classification Normal Systolic Diastolic < 120 < 80 Pre-hypertension 120-139 80-89 Stage 1 hypertension 140-159 90-99 Stage 2 hypertension > 160 > 100 ○ Left and right coronary arteries supply the cardiac muscle and heart with oxygen ▪ Left coronary arteries are more important than R side (block in L > block in R) ○ RCA ▪ Posterior portion of the heart ▪ SA Node ▪ Right side of the heart ○ Left main coronary artery --- > LAD (left anterior descending) -- > circumflex ▪ L heart ▪ Septum ▪ AV node - Coronary Arteries○ Buildup of plaque results in slowed blood flow to the cardiac cells ○ CAD asymptomatic until 70% occlusion of the artery ○ Rapid atherosclerosis = no time to build collateral circulation (angiogenesis) - Diagnosis of CAD○ Need to Dx EARLY!!! ○ EKG▪ Pathological Q wave shows zone of necrosis ▪ ST depression in lead II shows zone of injury □ Tells you that some form of necrosis has happened ▪ T wave inversion □ Results in ischemia (injury but not yet death) ○ Treadmill exercise testing with EKG▪ Try to induce chest pain and heart changes to DEFINITIVELY dx CAD ▪ This is the primary Dx test ○ Treadmill with medication e.g. thallium▪ Myocardial perfusion imaging = find “cold spots” = ischemic areas ○ Cardiac Catheterization Hyperlipidemia- High serum levels of lipids ○ Normal = Total cholesterol under 200 - 5 Classes of Lipoproteins○ VLDL’s - triglycerides ▪ 150 + is high ○ LDL’s - main carrier of cholesterol ▪ Below 100 ○ HDL’s - between 40-60 ○ VLDL’s ▪ Contain large amounts of triglycerides ▪ VLDL’s carry their fats to tissue capillaries of fat and muscle ○ LDL’s ▪ Main carrier of cholesterol ▪ Cholesterol used in the synthesis of steroid hormones □ e.g. estrogen, cortisol, testosterone ▪ Cholesterol is deposited in the intima layer of the epithelium arteries □ “fatty streak”. □ Begins developing at an early age □ Fatty Streak can progress and regress w/ lifestyle behaviors ○ Triglycerides▪ Genetic and Diet related ▪ Excess CARBS is converted to triglyceride and carried by the lipoproteins to adipose tissue for storage ○ HDL’s▪ “Good Guys” ▪ Inhibits cellular uptake of LDL’s ▪ HDL levels are increased with exercise - Etiology○ Genetic basis : there are several mutations in genes controlling lipase and apoproteins that have been identified. ○ Lack of LDL receptors ○ Increased dietary sensitivity to cholesterol = increase absorb and increased serum levels - Risk Factors for Hyperlipidemia ○ Metabolic Syndrome: ▪ Need 3/5 of these conditions for it to be Dx as Metabolic Syndrome: □ Abdominal Obesity (refer to the numbers she gave us earlier) □ HTN □ Low HDL □ Insulin resistance □ Hyperglycemia (and prediabetes = 100+) ○ Smoking ○ Increased Age ○ C-Reactive Protein (CRP) ▪ Rise in response to inflammation ○ Increased Homocysteine levels ▪ Homocysteine ▪ Homocysteine is biosynthesized from methionine ▪ It inhibits clotting cascade and is associated with endothelial damage. - How to treat high cholesterol○ Limit saturated fat ○ Limit daily intake of cholesterol ○ Lower caloric intake = lower LDL's Drugs to lower cholesterol ("statins") Patho Page 69 ○ Drugs to lower cholesterol ("statins") ○ Get tested annually for lipid levels (begin at age 20) - Statins ○ Atorvastatin (Lipitor); fluvastatin; lovastatin; pravastatin; rosuvastatin; simvastatin; ○ Inhibits enzyme for production of cholesterol ○ Increases number of LDL receptors = increasing LDL uptake and catabolism ▪ Lowers cholesterol level (LDL) Atherosclerosis○ Fatty plaques buildup in the coronary arteries, aorta, cerebral arteries, etc. ○ Atherosclerosis leads to CAD = #1 COD ○ Begins at an early age (young adults) and does not cause symptoms for 20-40 years - Risk factors○ Hyperlipidemia - Cholesterol > 200 ○ Low HDL’s <40 ▪ Men usually have low HDL's than women ○ Increasing age: ▪ Men 45+ & Women after menopause (55+) ○ FHx of MI/Sudden Death before 55 in men and 65 in women ▪ Strong hereditary link/predisposition ○ HTN▪ Smaller vessels = increased resistance ○ Smoking ○ Diabetes Mellitus = sugar is sharp and causes damage ○ Obesity - Non Traditional Risk Factors ○ Increased CRP○ Increased homocysteine○ Infectious agents ▪ e.g. chlamydia pneumoniae, herpes virus, cytomegalovirus- Patho1. Development of fatty streak ▪ Occurs at a young age 2. Injury to the intima▪ Smoking, high LDL, immune factors, HTN ▪ Inner layer of the artery is damaged and WBC and platelets attach 3. Accumulation of platelets, lipids, WBC's, growth factors. ▪ Remember the prostacyclin/ TXA fight ▪ TXA promotes the plaques building up □ #1 prevention strategy = take 1 aspirin 4. Weakening, and rupture of the unstable plaque ▪ Vessel becomes bogged down w/ heavy weight of the plaque and causes hemorrhage (small) 5. More clotting ▪ Larger blockage d/t the platelets forming a clot over the hemorrhage ▪ Results in partial or complete occlusion - Signs and Symptoms○ Pain or angina ▪ Symptoms ONLY appear after the blood vessel narrows too much!!! ▪ D/t Ischemia = lack of O2 to the tissues □ Causes a switch to anaerobic respiration and the lactic acid stims the nociceptors and causes the pain Angina Pectoris - Stable Angina○ Substernal/radiating chest pain to the left arm ▪ Pain is burning, squeezing, and usually doesn’t increase in intensity. ○ Predictable pattern & predictable duration ○ Precipitated by emotion, exercise, or cold. ▪ These stressors lead to constriction of vessels!!!!! ○ It lasts for a short time <5 minutes and stops with rest ▪ STABLE ANGINA STOPS W/ REST ▪ Lasting longer than 5 minutes can lead to necrosis (MI) ○ Treatment▪ Rest ▪ Nitroglycerine - Unstable Angina (Pre-infarction Angina)○ Symptoms of chest pain occurring at rest; ▪ Prolonged chest pain >15-20 minutes and non-predictable ▪ Pain is persistent in UNSTABLE ANGINA even w/ Nitro ○ Patho: ▪ Probably triggered by changes to the unstable Plaque ▪ Plaque is changing in nature/shape/form ○ Treatment of Unstable Angina ▪ THIS IS A MEDICAL EMERGENCY ▪ Cardiac Catheterization ▪ 12 lead (direction) EKG □ ST depression Pathological Q wave □ T wave inversion ▪ Rx: □ IV nitroglycerine to relieve pain - This is the only Med that might stop the pain □ Antiplatelet drugs (aspirin, Plavix) Patho Page 70 □ Antiplatelet drugs (aspirin, Plavix) □ Calcium channel blockers (-edepines) □ TPA instantly dissolves the clots ▪ Percutaneous Transluminal Coronary Angioplasty (PTCA or PCI) ▪ Stents to keep vessel open ▪ CABG will have to be done if stents are ineffective Myocardial Infarction- Death (necrosis) of cardiac tissue due to prolonged ischemia lasting about 20-40 minutes ○ Necrosis = death ○ Ischemia = lack of O2 - Number one killer of Americans - Patho○ Atherosclerotic plaque disrupts circulation and….. ▪ Blood vessel ruptures …or… ▪ Acute coronary thrombosis occurs ○ Three zones of myocardial damage▪ Necrosis□ Inner zone of dead tissue that was ISCHEMIC for 20-40 min □ Cannot be regenerated - Will become scar tissue and won't contract □ Pathological Q wave (more pronounced than in the QRS complex) ▪ Area of Injury□ Cells will die if the ischemia is not stopped IMMEDIATELY - Cells can be saved but won't be strong as before □ Elevated S wave from baseline - The higher the S wave, the worse the injury ▪ Ischemia□ Cells usually doesn't die… □ Can recover fully and work like normal ○ Necrotic areas are cleaned out by macrophages over the next 48 hours ▪ Results in increased Temperature d/t inflammatory process ▪ In about 10 days scar tissue begins forming and is complete in 7 weeks ▪ Scar areas cannot contract or conduct action potentials □ Seen as "bundle branch blockage" as seen via changes in EKG - Signs and Symptoms ○ Acute chest pain ▪ Classically radiates to the left arm ▪ Not relieved by Rest or Nitroglycerin (unstable angina) ○ EKG changes ▪ ST elevation ▪ Pathological Q wave ▪ Dysrhythmias (PVC’s) ○ Nausea and vomiting (d/t chest pain) ○ Weakness ○ Pale, cool skin ○ Fever and leukocytosis ○ ESR rises ○ Dyspnea, ○ Symptoms of cardiogenic shock with renal shutdown ▪ HIGH % of cardiogenic shock pt will die - Diagnosis of MI ○ 12 lead EKG-▪ Pathologic Q wave ▪ ST elevation ○ Enzymes (Bio-Markers)▪ These enzymes are released from dead cells due to necrosis □ You can measure these markers to assess the extent of the necrosis □ The higher the enzyme levels the greater the damage ▪ Elevated Troponin levels □ Troponin > 1 is positive in 1-2 hours - Less than 1 is normal ▪ CKMB rises □ Sign of muscle metabolism □ CK-MB- heart, 6-8 hrs - CK-MM- skeletal muscle - CK-BB-Brain - CK-MB - cardiac □ CK-MB begins rising in 6-8 hours - Location of Myocardial Infarction ○ Depends on which arteries are occluded, ▪ e.g. posterior MI, anterior MI, anterolateral ○ LAD occlusion- is the worst prognosis for immediate death - Treatment○ TPA = dissolves the clot ○ Aspirin and other anti-platelet aggregator ○ Heparin - anticoagulant… ▪ Doesn't dissolve current clots but prevents new one ○ Anti-dysrhythmics ○ Beta blockers (decrease HTN) ▪ Works on the ACE enzyme in the RAAS Calcium channel blockers Patho Page 71 ○ Calcium channel blockers ▪ Decrease BP ○ Nitroglycerine IV ▪ Chest pain and vasodilation (decrease BP) ○ Morphine = chest pain ○ Valium = anxiety ○ Stent to keep artery open ○ PTCA ○ CABG ○ Lifestyle modification education Congestive Heart Failure- CHF occurs when the heart is unable to compensate for the demands placed on it. - Pumping action of the heart is impaired ○ Decreased ability to contract…. PUMP PROBLEM ○ Results in fluid buildup (edema) - Chronic, progressive disease - Most common in the elderly - No cure & prognosis is generally poor ▪ 99-100% will die w/in 9 years of Dx - Etiology: ○ #1 Cause = MI ○ Hypertension, volume overload ▪ (Rx w/ diuretic) ○ Cardiomyopathies also cause CHF ○ Valvular disorders - Pathophysiology○ Reduced ejection fraction, decreased CO and decreased renal blood flow ▪ Results in increased sodium and water retention & increased venous return / blood volume ○ Poor renal perfusion leads to RENIN secretion ▪ RAAS cascade results in Aldosterone secretion from Adrenal Gland ▪ Propagates the problem ○ Inappropriate myocardial hypertrophy and remodeling ▪ Increase in muscle mass of the Left Ventricle & Chamber dilation ▪ Heart tries to compensate, but this further leads to poor pumping function □ Eventually will lead to systemic overload - Right Sided v. Left Sided Heart Failure ○ Right sided failure ▪ Think of failure w/ the venous return system of the heart ▪ R side is failing to pump blood to the lungs and the blood is refluxing into the vena cava □ Congestion in the liver □ JVD □ Dependent edema (legs) □ Ascites □ Fatigue ○ Left sided failure ▪ Now the failure is affecting the lungs ▪ Blood cannot be pumped out of the L side and is refluxing into the lungs!!!!! □ Crackles □ Dyspnea □ Cyanosis □ Tachycardia = compensation □ Fatigue - Diagnosis○ Chest X-ray ▪ Gold standard to show cardiomegaly ○ BNP- lab test ▪ When atrium and ventricles dilate, they release BNP ▪ 100+ is indicative of CHF ○ Echocardiogram used to monitor treatment ○ EKG- will show changes such as atrial and/or ventricular hypertrophy ○ Angiography ○ Cardiac Catheterization - Treatment ○ Require continuous monitoring ○ Diuretics- Lasix ○ Digoxin- Increases cardiac contractility ○ Vasodilators▪ Reduce BP (nitroglycerine) ○ Other drugs also used ○ Mechanical support- used for end-stage heart failure (LVAD) ○ Patient Teaching▪ Restrict Sodium Intake ▪ Increase Potassium Intake Arterial Diseases of the Extremities - Peripheral vascular disease (PVD) - Assessment ○ Monitoring capillary refill time ○ Peripheral pulses (strength) Auscultation to hear a bruit Patho Page 72 ○ Auscultation to hear a bruit ○ Doppler ultrasound Arteriosclerotic Occlusive Disease- also called arteriosclerosis obliterans - Most commonly called (arterial insufficiency) - Symptoms○ Intermittent claudication with walking (gastrocnemius muscle has highest O2 consumption) ○ Cool temperature ○ Limb color blanches with elevation and becomes deep red when leg is in dependent position ▪ Due to autoregulatory increases in blood flow and Increase in gravitational pressure ○ Pain becomes more severe at rest (rest pain) and leg must be lowered to gain relief. ▪ This action increases peripheral perfusion to the area. ○ Diminished or absent peripheral pulses ○ Loss of hair on toes, feet, nails thickened and ridged ○ Arterial ulcers ▪ Very painful, deep, and circular ▪ Tend to be on tips of toes, heel or other pressure areas ▪ Arterial ulcers are CLEAN - but deep and painful ▪ Venous ulcers = gross, jagged edges, purulent ○ Edema is minimal unless kept in dependent position to minimize pain - Treatment ○ Femoropopiteal (Fem-Pop) Bypass graft surgery▪ Use saphenous vein to bypass the occluded area ○ Walking to point of claudication to develop collateral circulation ○ Stop smoking▪ Absolutely necessary!!!!!! THIS IS FOUNDATIONAL TO TREATING ○ Control diabetes mellitus ▪ DM is the #1 CAUSE OF ARTERIAL INSUFFICIENCY Reynaud’s Disease - Vasospasm of the hands - Triggered by old Cold & Strong emotional responses - Women > Men - Rx: ○ Avoid exposure to cold ○ Vasodilators (Nitro) ○ Calcium channel blockers, - Can cause gangrene d/t intense vasospasm if left untreated Aneurysms- Abnormal dilation of a blood vessel ○ Usually in the aorta and the brain ○ Area is weakened and grows larger from BP on vessel - Weakness is due to congenital defects, infection, atherosclerosis - Symptoms depend on location: ○ Abdominal aneurysms are asymptomatic ▪ Can palpate the aneurysm ○ Pain = thoracic aneurysms - HTN is a risk factor for DISECTION of the ANEURYSM ○ This is life threatening - Treatment: ○ Surgery & resection of area ▪ Prosthetic graft Diseases of the Venous Circulation- Chronic Venous Insufficiency○ Usually a result of DVT or valvular incompetence (varicose veins) ▪ Valves of the legs are unable to close properly and blood refluxes in the legs ○ Muscle pumps are also ineffective ○ Signs and Symptoms▪ No ischemia as in arterial insufficiency ▪ Tissue congestion, edema, ▪ Varicose veins ▪ Brown discoloration ▪ Lymphatic Insufficiency ▪ Development of venous ulcers □ Weeping, nasty motherfuckers □ Minimal pain □ Irregular borders ○ Patient Teaching for Venous Insufficiency: ▪ Stop and Walk Every Several Hours When Traveling ▪ Long term immobility = worsening symptoms - Deep Vein ThrombosisThrombophlebitis, venous thrombosis ○ Presence of a thrombus in the vein ▪ Venous stasis ▪ Increased blood viscosity ▪ Vessel wall injury ○ Risk Factors: ▪ Bedrest (i.e. after surgery) ▪ Prolonged immobility (traveling) ▪ MI, CHF ▪ Pregnancy, childbirth, oral contractives ▪ Dehydration Patho Page 73 ▪ Dehydration ○ Complication = Pulmonary embolism ○ Signs and Symptoms▪ Asymptomatic if vessel not 100% occluded ▪ Sxs depend on site of DVT ▪ Signs for DVT in legs: □ Calf pain, deep muscle tenderness □ Swelling □ Dorsiflexion causes pain (Homan’s sign) □ Fever □ General Malaise □ Redness □ Increased WBC, ESR ○ Prevention, Diagnosis and Treatment ▪ Prevention is always best □ Active leg exercises when immobile □ Keep entire leg elevated at 15-20 to prevent stasis □ Early Ambulation □ Support stockings when on bedrest □ Use of SCD’s □ Prophylactic anticoagulants - Heparin - Lovenox - Coumadin (warfarin) □ Heat to relieve vasospasm Arterial vs Venous Insufficiency • Both may commonly occur simultaneously • Arterial pain is intermittent claudication while venous pain is aching • Arterial -pulses absent; Venous- present • Arterial ulcers are painful while venous ones aren’t if superficial • Arterial ulcers have a black base while venous are beefy red to yellow • Arterial- edema is minimal while in venous edema is moderate to severe (non-pitting) Module 17 | Neurological System**Ms. Morris = KNOW THE LEARNING OBJECTIVES** Headaches- 25% of adults c/o recurrent HA - Types of HA○ Primary▪ MAJORITY OF HA ▪ No organic cause ▪ Migraine ▪ Cluster ▪ Tension ○ Secondary▪ Due to underlying medical condition □ Meningitis □ Tumor □ Aneurysm ○ Cranial neuralgias & face pain - Migraine○ Men > women ○ Incidence decrease by Age 50 ○ Symptoms▪ Can have aura or no aura □ Majority of migraines DO NOT have aura ▪ SEVERE, pulsatile, throbbing UNILATERAL pain ▪ Last about 4-72 hours □ Migraines lasting longer than 72 hours = STATUS MIGRANOSIS □ This is a MEDICAL EMERGENCY ▪ Aggravated by physical activity ▪ N/V ▪ Sensitivity to light/sound/smell ▪ Visual disturbances ○ Aura▪ Can last from 5 min to 1 hour & develop over 5-20 minutes ▪ Precedes migraine □ Can have prodromal symptoms days before: - Fatigue - Irritability ▪ Speech disturbances ○ Patho▪ Hyper-activation of the Trigeminal V □ d/t hypersensitivity to environmental stimuli - Allergies, light, caffeine, etc. ▪ Release prostaglandins & other substances that results in vasodilation □ Results in Neurogenic Inflammation □ Stims the nociceptors and manifests as throbbing pain ▪ NSAIDS can prevent prostaglandins and prevent migraines from progressing ○ Triggers- Patho Page 74 FAMILY HX Genetic predisposition > w/ aura than w/o aura ○ Triggers▪ Stress ▪ Sleep deprivation ▪ Alcohol ▪ Foods (MSG, cheese, chocolate) ▪ Visual stimulation ▪ Estrogen □ Migraines coincide w/ menstrual cycle □ Most migraines (75-80%) go away after pregnancy ○ Phases▪ Prodromal□ Hrs to days before □ Energetic/excitable or depressed/ irritable □ Thirsty, cravings □ Tired, increased urination ▪ Aura□ Not always present □ Flickering lights □ Tingling □ Speech disturbances ▪ Attack□ Acute phase of the migraine lasting from 4-72 hours □ Varies in location □ Throbbing pain - Worsened w/ PA □ Sensitivity to light, sound, smells □ N/V, syncope, light-headedness ▪ Post-dromal□ Extreme tiredness/Sluggish □ Confusion □ Head pain exacerbated w/ bending over ○ Treatment▪ Acute (during)□ Aim to alleviate symptoms ▪ Acute Non-responder Care□ For those that don't respond w/ first treatment □ 10 mg IV Reglan (metoclopramide) - Relieves nausea & helps w/ absorption of other meds ▪ Prophylactic Treatment□ Use if migraines occur 2-3x per month or migraines are debilitating □ Taken daily for months/years □ Beta-blockers (propranolol) & anti-seizure meds & anti-depressants ▪ Pharmacologic Treatment□ Non narcotics used for mild-mod pain (best taken early) - NSAIDS - prevent prostaglandin synthesis □ Triptans- (Maxalt = Rizatriptan) - 1st line defense - Increase serotonin and promote vasoconstriction □ Narcotics- For severe HA - Ex: Norco/Vicodin □ Other- Midrin (isometheptene) = vasoconstriction - Ergotamines w/ caffeine = vasoconstriction ▪ Non Pharmacologic Treatment□ Control risk factors & triggers □ Behavior interventions- Stress manage - Relaxation therapy - Biofeedback - Cognitive therapy ○ Nursing considerations▪ Non-oral meds useful for sudden onset HA and N/V (IV Reglan/metoclopramide) ▪ Frequent use of acute therapies can cause rebound HA ▪ Triptans should be avoided in pt w/ CAD □ Causes coronary spasm ▪ Ergotamines CONTRAINDICATED in pregnants (uterine contractions) - Cluster HA○ Severe, unilateral pain ○ 15 min - 3 hrs ○ Hereditary - Tension HA○ Dull, aching, diffuse pain ○ Usually not severe enough to limit activity - Chronic Daily HA○ Must occur for 15+ days in 1 month ○ Can be from med overuse or caffeine Seizures- Result from abnormal/excessive firing from a group of neurons in the brain ○ Results from alteration of permeability and redistribution of ions and neurotransmitters ▪ AKA… there's an imbalance in the brain - Signs & Symptoms○ Depend on the type of neurons that are hyperactive Sensory, motor, autonomic, psychic (De Ja Vu, anxiety) Patho Page 75 ○ Sensory, motor, autonomic, psychic (De Ja Vu, anxiety) - Types○ Provoked▪ Secondary seizures caused by something else □ Infection □ Brain injury □ Drug abuse ○ Unprovoked ▪ Primary/epileptic seizures ▪ Idiopathic ▪ Focal seizures or Generalized Seizures - Provoked Seizures○ Most common = Febrile Seizures ▪ Seizures in children □ 6 mos & 5 yrs ▪ Temp above 104 not related to another metabolic disorder ○ Etiologies▪ Electrolyte imbalances (hyponatremia) ▪ Eclampsia ▪ Hypoxia ▪ Hypoglycemia ▪ Tumors ▪ Meningitis - Unprovoked (Epileptic Seizures)○ Focal Seizure WITHOUT Impairment of Consciousness▪ Begin in 1 part of the brain (localized) ▪ Symptoms□ Aura □ Involuntary muscle movements □ Sensory disturbances □ ANS stimulation (tachycardic, diaphoretic, pupillary changes, etc.) ○ Focal Seizure WITH Impairment of Consciousness▪ Occur in temporal lobe □ Begins UNILATERALLY and can spread to both ▪ Psychomotor symptoms- automatisms/repetitive activities ---------------------------> □ Lip smacking □ Patting □ Rubbing clothing □ déjà vu, hallucinations, etc. - Can be confused w/ psychiatric disorders ▪ Postictal Confusion is common ○ Generalized Seizures▪ Generalized = includes both hemispheres of brain at onset ▪ Tonic- stiffening of extremities w/ contractions ▪ Clonic- contractures and relaxations w/ hyperventilation ▪ Tonic Clonic (grand mal) = MOST COMMON □ Generalized seizure w/ extension of extremities w/ LOC □ Loss of bladder/bowel control □ Clonic rhythmic contractions & relaxation of extremities ▪ Absence (Petit mal) □ Only in children □ Non-convulsive □ Unresponsive □ Blank stare ▪ Myoclonic□ Brief, involuntary muscle contractions w/o strong extension (tonic) □ Limited to the face, trunk, or extremities ▪ Atonic- "drop attacks" = Caroline = sudden loss of muscle tone ▪ All generalized seizures can be followed by Todd's Paralysis□ Temporary paresis (weakness), aphasia, or hemianopia □ Lasts up to 24 hours - Status Epilepticus○ THIS IS A MEDICAL EMERGENCY ○ When seizures don't stop after 5 minutes or happen back-to-back w/ no recovery ○ Can occur w/ all generalized seizures ▪ Tonic-Clonic Seizures w/ SE can lead to respiratory failure & death ○ Most common in Elderly & Children ○ Treat the underlying cause ▪ Abrupt withdrawal of anti-epileptic drugs ▪ Alcohol withdrawal ▪ Acute neurological illness (meningitis) ▪ Metabolic disorders (hypernatremia, etc.) ▪ Stroke ○ Life support measures & admin meds ▪ Secure an airway!!! ▪ Ativan, Cerebyx, Keppra, Phenobarbital, Propofol, Versed, Ketamine - Treatment○ Pharmacological▪ Suppress the hyperactive neurons or inhibit transmission of electrical impulses ▪ Benzodiazepines ▪ More than 20 different types of drugs □ Important to limit number of drugs to 1!!! □ These drugs can interact w/ OCP's, affect fertility, and cause birth defects ▪ 65% of pt don't fully respond to anti-epileptic drugs Patho Page 76 Focal = effect 1 part of the brain AT ONSET - They can generalize…. Generalized = include BOTH hemispheres AT ONSET!!!! First ever Seizure pt in EMU Suppress the hyperactive neurons or inhibit transmission of electrical impulses ▪ Benzodiazepines ▪ More than 20 different types of drugs □ Important to limit number of drugs to 1!!! □ These drugs can interact w/ OCP's, affect fertility, and cause birth defects ▪ 65% of pt don't fully respond to anti-epileptic drugs ○ Non-Pharmacological▪ MRI's & EEG's to diagnose □ EEG's are the GOLD STANDARD ▪ Surgery if medications continue to fail ▪ Neurostimulation of Vagal Nerve ▪ Diet modification□ Ketogenic diet = induce ketosis to help prevent seizures Stroke- Vascular event that injures brain tissue causing acute-FOCAL neuro deficit ○ Deficits match the territory effected - 4th leading cause of morbidity & mortality - Hemorrhagic Strokes○ Least common but most frequently fatal ○ Spontaneous rupture of cerebral vessel causing hematoma ○ AGE & HTN are MOST COMMON risk factors ○ Etiology▪ Arteriovenous Malformations□ Development in utero of anomalies in vascular bundles of AV unions □ These can rupture ▪ Trauma ▪ Aneurysm ▪ Drugs (cocaine abuse) ▪ Coagulation disorders ○ Symptoms▪ Sudden SEVERE SEVERE HA at onset □ "worst HA of my life" □ Due to the subarachnoid hemorrhage ▪ Vomiting ○ Treatment▪ Limit the spread of hematoma ▪ Manage Intracranial Pressure ▪ Surgery□ Resect AVM □ Clip aneurysms ▪ Interventional Radiology- endovascular coiling walls off aneurysm - Ischemic Strokes○ Most common type of CVA ○ Results from obstruction of blood flow d/t thrombosis or emboli ▪ Thrombotic stroke□ Atherosclerotic plaques develop near cerebral vessel bifurcations □ Damage to the vessel wall results in buildup of a clot □ DM & HTN are huge risk factors ▪ Embolic□ Moving clot that migrates to cerebral vessels (most common MCA) □ Cardiac risk factors are most common (A-fib, MI, endocarditis, etc.) ○ Risk Factors▪ FHx ▪ HTN ▪ Obesity ▪ Smoking ▪ A-fib ▪ CKD ○ Transient Ischemic Attacks- -------------------------------------------------------------> ▪ "Mini-Strokes" ▪ Brief episodes of ischemia w/o infarction ▪ Same causes of ischemic stroke but w/ partial blockage ▪ Serve as a warning sign of future stroke □ Most people have stroke w/in 3 mos of TIA - Diagnosis of CVA○ EARLY DETECTION!!!! ▪ FAST □ Face droop □ Arms drop □ Speech slurred □ Time = 3 hour TPA window ○ Confirm neurological deficits by: ▪ Head CT w/o contrast ▪ Neurological exam - Treatment○ Administer TPA (tissue plasminogen activator)▪ MUST R/O HEMORRHAGIC STROKE FIRST ▪ Need to be given w/in 3 hours of onset of symptoms ○ Salvage brain tissue ○ Prevent secondary strokes ▪ ID risk factors, educate, etc. ○ Minimize long-term disability ▪ Rehab, etc. Impact of Stroke LocationPatho Page 77 ○ Salvage brain tissue ○ Prevent secondary strokes ▪ ID risk factors, educate, etc. ○ Minimize long-term disability ▪ Rehab, etc. - Impact of Stroke Location○ Effects are obvious on the OPPOSITE side of the brain ▪ R side CVA = L sided weakness ○ Deficits manifest based on the location of the CVA ----------------------------------------------> - Nursing Considerations Post CVA○ Get them mobile w/in 24 hours to prevent further blood clots ○ Assess ADL's ▪ Consult w/ rehab ○ Orient yourself to the non-affected side ▪ Ensures they can hear/see/interact with you ○ Include the family/caregivers in the education - Post Stroke Care○ Risk of recurrence is highest in the first week ○ Admin antiplatelets ○ Reduce modifiable risk factors ▪ HTN, DM management, smoking cessation, etc. ○ Treat underlying medical conditions ○ Consult w/ rehab to build on deficits▪ Motor, language, sensory, cognitive ▪ Dysarthria ▪ Dysphagia ▪ Fine motor skill deficits ▪ Inability to perform ADL's Dementia- Umbrella term that includes: ○ Alzheimer's ○ Lewy body dementia ○ Parkinson's ○ Vascular ○ Etc. - Incidence is increasing as the population ages - Cognitive decline in areas of the brain w/ cognition and memory - Diagnosis○ Based on presenting problem ○ History ○ Neuro exam ○ Brain imaging ○ Behavioral/cognitive functioning - Need to r/o reversible causes of memory loss & cognitive decline -----------------------> ○ Acute infection, trauma, drugs, emotional, etc. - Diagnosing○ Requires 2 components▪ Decline in memory ▪ Decline in at least 1/4 cognitive functions□ Language comprehension / speech □ Process & interpret visual information □ Planning, sound judgements, abstract thought □ Motor functioning - Treating○ Treat underlying causes that can reverse it ▪ B12 deficiency ▪ Hypothyroidism ▪ Drug toxicity ▪ Tumors ○ Treat problematic behaviors▪ Agitation ▪ Sleep disorders ▪ Wandering ▪ Sundowner's Syndrome- in the evening = higher incidence of agitation, confusion, etc. Alzheimer's Disease- Risk increases w/ age - Slow, progressive dementia w/ subtle onset of memory loss - Patho○ Caused by accumulation of amyloid beta peptides ▪ Cause a chain reaction of physical changes to the brain tissue ▪ Axons become entangled ▪ Prevents communication of these cells and causes cell death ○ MRI shows atrophy of cerebral cortex & ventricle enlargement -----------------------------> ○ Microscopic exam shows Neuritic Plaques, degenerated & tangled axons - Stages of Alzheimer's○ Early▪ Lasts 2-4 years ▪ Short term memory loss ▪ Random detail loss ▪ Personality changes ○ Moderate- Patho Page 78 ▪ Lasts 2-4 years ▪ Short term memory loss ▪ Random detail loss ▪ Personality changes ○ Moderate▪ Lasts 2-10 years ▪ More cognitive impairment ▪ Language deficits ▪ Depression ▪ Unable to perform self-care ○ Severe▪ Lasts 1-3 years ▪ Loss of ability to respond to their environment ▪ Total dependent care needed ▪ Bed ridden ▪ Death - Treatment○ Many medications for Alzheimer's ▪ Aim to decrease Acetylcholine breakdown and preventing the formation of those plaques ○ Can cause N/V, loss of appetite, weakness, etc. - Nursing Considerations○ Biopsychosocial disorder ▪ Affects every aspect of them and their family's life ○ Focus on the things they CAN DO! ○ Support the caregivers ○ Utilize community resources for pt and caregivers Multiple Sclerosis- Autoimmune disorder○ Inflammation and destruction of myelin in the CNS - Progressive, degenerative disorder - Genetic and environmental (smoking, low vitamin D) risk factors ○ Women 2x > Men - Symptoms dependent on location of lesions/plaques formed by broken down myelin ○ Visual changes ○ Speech deficits ○ Muscle weakness ○ Gait issues ○ Depression = 30-50% ▪ d/t impaired fxn - Diagnose ○ MRI ○ Neuro exam ○ Charcot's Neurologic Triad▪ Nystagmus ▪ Intentional tremors ▪ Staccato speech - Treatment○ Treat acute attacks w/ corticosteroids ○ Modify the course of the disease ▪ Interferon B□ Immune booster ▪ Glatiramer Acetate□ Mimics myelin so the body destroys it instead of the actual myelin ○ Treat symptoms ▪ Pain ▪ Fatigue ▪ Depression ▪ Bowel/Bladder dysfunction ▪ Constipation ▪ Tremors Patho Page 79 RELAPSE W/ PREGO - D/t it being a stress on the body…… . Tutoring Junk Stuff Monday, October 30, 2017 5:09 PM Ventilation-Perfusion Mismatch- Both processes are working properly just not in synch Hypoxemia = overall, systemic disease state Vs. Hypoxia = inadequate oxygenation of the tissues Polycythemia- Compensation of hypoxemia - Found in smokers and old men??? Lung fxn- Gas exchange at the alveoli - Inactivation of bradykinins - Secretes ACE (angiotensin converting enzyme) ○ Very important for controlling BP - Blood storage - Surfactant ○ Allows for proper lung expansion ○ This is the last system to develop in utero ▪ Premies don't have surfactant and will have collapsed lungs - Innate immune protection (nonspecific defenses) Obstructive disorders- Asthma○ Reversible & trigger-induced ○ Inflammatory response that recruits all immune cells to the airway ○ Extrinsic = type 1 hypersensitivity to an allergen ○ Intrinsic = exercise, cold, pollution, URTI ○ Signs & Symptoms▪ Cold sxs ▪ Wheezing ▪ Dyspnea ▪ Tachycardia & tachypnea to compensate ○ Rx- eliminate the cause and educate pt about triggers ▪ Reduce sxs w/ corticosteroids - COPD○ Chronic bronchitis ○ Emphysema - Chronic Bronchitis○ Blue bloaters ○ Hx of smoking ○ Productive cough w/ muco-purulent drainage ○ Overweight and cyanotic and peripheral edema Increased Hgb to compensate Patho Page 80 ○ Increased Hgb to compensate ○ Auscultate rhonchi - Emphysema○ Pink puffers ○ Pursed lips to compensate ○ Cachectic = muscle wasting thin ○ Tripod position ○ Lungs are hyper-inflated ○ Old and thin, severe dyspnea Disorders of Inflation- Atelectasis○ Alveoli collapse and don't expand ▪ No gas exchange occurs ○ Caused by obstruction, compression, no surfactant ○ Sxs- tachypnea, tachycardia, absent breath sounds - Pneumothorax○ Air in the pleural space leading to one or more lobes of the lung collapse ○ Spontaneous = rupture of the lung cyst word ○ Traumatic = knife wound ○ Tension = pressure from tumor, etc. Pregnant smoking = increased r/o developing asthma for the baby Infections- Common Cold○ Viral = no Abx ○ Clear and watery secretions - Influenza○ Abrupt onset w/ fever, chills, and malaise - Pneumonia○ Inflammatory rxn to unwelcome pathogen in the alveoli ▪ Can be bacterial or viral… bacterial can be resistant ○ Community Acquired▪ Pneumonia that the pt comes into the hospital with it ○ Hospital Acquired▪ 48 hrs pass and then they test + for pneumonia Arterial Blood Gasses- pH = 7.35-7.45 - CO2 = .35-.45 - HCO3 = 24-31 - Kidneys are responsible for monitoring pH by excreting/retaining H+ and/or HCO3 Neoplasms: Patho Page 81 Cell-proliferation = generating new somatic cells via mitosis Differentiation = cells specialize Apoptosis = natural/normal programmed cell death Stem Cells- Undifferentiated cells that can self-renew and can become any type of cell Chemotherapy Agents- Use multiple agents to target different areas of the cell cycle Benign- Well differentiated cells - Do not invade - No metastasis Malignant- Poorly differentiated - Grow into lymph and blood stream - Metastasis Barrett's Esophagus- Normal epithelium of the respiratory tract begins to change cell types to reflect different types of epithelium - Dysplasia of the normal esophageal cells… begin to look like cells in the GIT In situ- Tumor that hasn't spread and is stable Angiogenesis- formation of new blood vessels via the tumor Fried food in reused oil, red meat, lunch meat, = increased r/o cancer CardioBlood moves from high pressure to low pressure - This pressure gradient and the pumping via the heart is what causes blood to flow through the CV system High pressures are found in the beginning of the cycle - It takes more effort (pressure) to push the blood from your heart - It takes little effort for blood to passively flow in the veins to return to the heart Coronary Circulation- Right coronary artery - Left Coronary Artery ○ Most common area to get a MI Nitroglycerin- Vasodilator Patho Page 82 - Vasodilator Relaxes smooth muscle Reduces preload, afterload, & O2 consumption Side effects○ HA, Orthostatic Hypotension, facial flushing, circulatory collapse - Take BP before & 1 hr after administering nitro - Swimming and bathing is okay with the nitro patch Varicose Veins- Dilated veins - Lead to venous insufficiency - Most commonly caused by DVT - Cause by increased pressure for standing for long periods of time ○ Prevent w/ compression stockings Patho Page 83 FINALE!!!!!!!!! Thursday, November 9, 2017 Les go boiiii 10:27 AM Module 13 | GI, Biliary, Pancreatic, & HepaticCommon GI Signs and Symptoms- Anorexia○ Lack of appetite ○ Associated with nausea, emotional factors, smells, drugs, and disease states - Abdominal pain○ Determine location of pain ○ Observe for rebound tenderness - Nausea & Vomiting- ----------------------------------------------------------------------------> ○ Vomiting Center is located in the medulla ▪ Activated in response to stimuli □ Ingestion of harmful substances □ Smells, etc. ○ Chemoreceptor center on the floor of the fourth ventricle ▪ Mediates emetic effects of blood-borne drugs and toxins Oral lesions- Oral leukoplakia ○ White plaque ○ A precancerous lesion - Tongue○ Most common site for oral cancer ○ Lift tongue and check with finger for lesions - Ulcerations○ Occur d/t chemotherapy ▪ Chemo targets rapidly dividing cells….. Duh Oral, head and neck cancer- Risk Factors○ Tobacco ▪ #1 cause ○ Heavy alcohol (ETOH = ethanol) intake ▪ #1 cause ○ Other chronic irritants ****GERD- Etiology○ Weak/incompetent lower esophageal sphincter ○ Delayed gastric emptying ○ Overweight, tight clothing, laying down after eating, large meals, etc. ▪ Increased pressure in gut and forces contents upward - Signs and Symptoms○ Heartburn, most severe at night ○ Reflux into mouth (can be severe) ○ Pain and hoarseness after reflux ▪ Pain can be mistaken for cardiac pain ○ Respiratory symptoms▪ Wheezing ▪ Chronic cough ▪ Hoarseness ▪ Asthma and GERD are linked….. - Patho○ Reflux asthma and chronic cough due to…… ▪ Aspiration ▪ Laryngeal injury ▪ Vagal-mediated bronchospasm - Treatment○ Lose weight ○ Sit upright after eating ○ Sleep with head elevated ○ Small meals ○ Avoid foods that lower esophageal sphincter tone ▪ Alcohol and smoking ▪ Caffeine ▪ Chocolate ▪ Fats ○ Rx▪ H2 blockers = Tagamet (cimetidine) (inhibit gastric acid secretion) ▪ Proton Pump Inhibitors = Prilosec (omeprazole) (proton pumps secrete gastric acid) - Diagnose GERD w/ Esophageal-Gastro-Duodenal Endoscopy - Complications ○ Scarring ○ Strictures ○ Barrett’s esophagus (highly linked to GERD d/t prolonged irritation) Esophageal Cancer- Squamous Cell Cancers = MOST COMMON Patho Page 84 - Squamous Cell Cancers = MOST COMMON - Risk factors ○ Smoking & alcohol abuse ○ Old age (60+) ○ Male gender - Barrett’s esophagus○ Adenocarcinoma of the esophagus ○ Very very malignant - Signs & Symptoms○ Dysphagia ○ Weight loss - Prognosis poor due to late dx Gastritis- Inflammation of the gastric lining ○ Acute gastritis & Chronic gastritis ARE 2 TOTALLY DIFFERENT DISEASE PROCESSES!!!!!! ▪ THE ETIOLOGIES ARE TOTALLY DIFFERENT ○ #1 cause = H. pylori ○ #2 cause = NSAIDS - Common factors○ Helicobacter pylori ○ NSAIDS / Aspirin ○ Alcohol ○ Corticosteroids - Patho○ Aspirin and NSAIDS inhibit prostaglandin secretion ▪ Prostaglandins protect the stomach lining!!!! □ Improve gastric mucosal blood flow □ Decrease acid secretion □ Increase bicarbonate secretion □ Enhance mucous production Acute Gastritis- Sudden inflammation of the gastric mucosa - Etiology○ H. pylori ○ NSAIDS / Aspirin ○ Alcohol ○ Serious illnesses - Symptoms○ Hemorrhage ▪ Life threatening hemorrhage can occur from NSAIDS (ibuprofen) ○ Heartburn ○ Hematemesis ○ Violent vomiting ▪ Five hours after ingestion of contaminated food □ Don't try to stop the vomiting!! □ This is a good compensatory mechanism that's trying to rid the body of the toxin - Treatment○ IV fluid replacement d/t vomiting ○ Removal of irritant Chronic Gastritis- Different from Acute Gastritis… ○ There are ANATOMICAL changes to the gastric mucosa - Absence of grossly visible erosions with chronic inflammatory changes ○ Leads to atrophy of the gastric epithelium - Three types○ Helicobacter pylori ○ Autoimmune (associated w/ T1DM = autoimmune disorder) ○ Chemical gastropathy - Treatment of H pylori○ Difficult due to drug resistant strains ○ Simultaneous two or more antibiotics plus Prilosec (omeprazole) for 10-14 days ▪ Proton pumps produce HCl▪ PPI's (omeprazole) inhibit HCl- production and reduce irritation of gastric mucosa - Chronic gastritis = long term complication of T2DM… ○ Results in diarrhea ○ Requires extensive dietary modifications to fix gastritis and prevent glycemic fluctuations ****Peptic Ulcer Disease- Location in stomach or duodenum ○ Ulcerative disorder affecting stomach layers and proximal duodenum - Risk Factors○ Elderly ○ NSAID use ○ Concurrent corticosteroid use. - Patho ○ H. pylori stimulates release of cytokines which increase mucosal damage - Signs and Symptoms○ Burning, gnawing, cramping stomach pain ▪ Especially when empty = [between meals & Early AM (0100-0200)] ○ Epigastric Pain ▪ Radiates to costal margins and the back Patho Page 85 Drugs to treat PUD (anti-ulcer drugs) - Antibiotics- eradicate H. pylori ○ Combination of the following - Signs and Symptoms○ Burning, gnawing, cramping stomach pain ▪ Especially when empty = [between meals & Early AM (0100-0200)] ○ Epigastric Pain ▪ Radiates to costal margins and the back ○ Pain relieved by food / antacids - Complications○ Sudden severe hemorrhage (life threatening) ▪ Melena (occult blood) □ Loose tarry stools ▪ Coffee ground emesis, - Treatment○ Antacids ○ PPI's ○ Sulfacrate- Mucous lines the ulcer and serves as barrier to acids ○ Misoprostol- Stimulates mucous production and bicarbonate secretion. ****Stress Ulcers (physiologic stress)- Curling’s Ulcer - GI ulcerations that develop in response to a major physiologic illness - Risk Factors○ Major burns / trauma ○ Sepsis ○ Severe liver failure ○ Major surgical procedures ○ MODS (multi system organ disease syndrome) ○ Pts admitted to ICU’s - Cushing Ulcer ○ Similar type of ulcer occurring with intracranial tumors, surgery, trauma ○ Result from hypersecretion of HCl- d/t increased ICP stimulating the Vagus Nerve - Treatment ○ Preventative with H2 Receptor Blockers and PPI's (IV Protonix) Drugs to treat PUD (anti-ulcer drugs) - Antibiotics- eradicate H. pylori ○ Combination of the following ▪ Amoxicillin ▪ Clarithromycin (Biaxin) ▪ Tetracycline ▪ Metronidazole (Flagyl) ▪ Bismuth (Pepto-Bismol) ○ Use at least 2, preferably 3 antibiotics for 14 days ▪ Heavy use of Abx can lead to 2nd infxn (C. diff.) - PPI's○ Omeprazole (Prilosec) = (the first PPI) ○ Esomeprazole (Nexium) = “the purple pill” ○ Pantoprazole (Protonix) - Antacids and mucosal protector drugs○ Antacids are alkaline drugs that neutralize stomach acid. Main uses: GERD & PUD ▪ Antacids = Maalox, Amphojel, Milk of Magnesia ▪ Many people self-prescribe and take ○ Mucosal protectors = Sulfacrate (Carafate) Protects ulcer w/ mucous secretions ○ Misoprostol (Cytotec) = Antiinflammatory ****Cholecystitis- Diffuse inflammation of the GB ○ Usually associated with stones - Risk factors○ Women ○ Overweight - Symptoms○ Acute onset of RUQ / epigastric pain ▪ Episodes of colicky pain. ○ Mild fever, anorexia, N&V. ○ Intolerance to fatty foods - Labs ○ Increased WBC’s ○ Elevations in AST, ALT, SGOT, SGPT, and bilirubin ▪ LIVER FUNCTION TESTS - Dx by Ultrasound - Treatment = laparoscopic surgery Cholelithiasis- Gallstones - Risk factors ○ Obesity ○ Female ○ Multiple pregnancies ○ Oral contraceptives - Large stones block duct and cause: ○ Jaundice ○ Epigastric and RUQ pain ▪ May radiate to upper back, R shoulder Choledocholithiasis- Stone in common bile duct - RUQ pain, fever, chills, jaundice - Bilirubinuria & elevated serum bilirubin levels Biliary system & pancreas **Note the locations of the pancreatic duct and the common bile duct** ---------------------------------> - Pancreas ○ Endocrine fxn = insulin, glucagon, etc. ○ Exocrine fxn = amylase for digestion in the small intestine ○ Cannot palpate pancreas ▪ Makes pancreatic tumors difficult to ID and makes pancreatic cancer v v bad Pancreatitis caused by gallstone in duct- Patho Page 86 ****Acute Pancreatitis- Inflammatory process of the pancreatic acini - Etiology○ Choledocholithiasis blocks the common bile duct and causes STASIS of pancreatic exocrine fluid ○ Alcohol abuse ○ Hyperlipidemia above 1000 ▪ Know the normal triglyceride, LDL, HDL levels ○ Viral infections ○ Hypercalcemia ○ Surgical and abdominal trauma ○ Drugs: ▪ Thiazide diuretics ▪ T2DM Drugs = Byetta (Exenatide) - Patho○ Premature activation of trypsin causes autodigestion of the pancreas ▪ Eventually causes multisystem organ failure and SIRS (systemic inflammatory response syndrome) □ MODS = organs dying one after the other - Signs and Symptoms ○ Epigastric or periumbilical pain ▪ Radiate to back, chest or flank ○ Severe abdominal tenderness & distention ○ Fever - Labs ○ Increased Serum amylase and lipase ("pancreatic function tests") ○ Increased CRP (inflammatory marker) - Treatment ○ Demerol (meperidine) for pain ▪ Morphine increases spasm of the sphincter of the pancreatic duct ○ NPO to give the pancreas a rest ○ IV fluids Pancreatic Cancer- Fourth leading cause of cancer death ○ Cancer has usually metastasized before diagnosis ○ d/t not being able to palpate the pancreas - Symptoms○ Jaundice ○ Pain ○ Pruritus ○ Multiple thrombi d/t activation of clotting factors by tumor cells. Colonoscopy - NUMBER ONE method to detecting colorectal cancer!!! - Every five years after age 50 ○ Begin at age 40 if FHx - Inspection of the large intestines for polyps ○ Polyps are precancerous ○ They will clip and remove the polyp ▪ Need to get colonoscopy every year after Colon cancer- Third most common cancer - 2nd leading cause of cancer deaths ○ #1 = lung - Risk Factors: ○ Older age (>50) ○ Family Hx ○ Chron's ○ Ulcerative Colitis ○ Polyps ○ High fat, low fiber diet - Aspirin seems protective - Symptoms ○ Symptoms manifest late and cancer has spread ○ Bleeding ○ Change in bowel habits ○ Pain = v v v late sxs - Treatment = Surgical removal ****Crohn’s vs. Ulcerative Colitis- Crohn’s disease- Patho Page 87 - Crohn’s disease○ Can occur in the small or large intestine ○ Unknown etiology - Ulcerative colitis○ Mainly effects LARGE intestine ○ Ulcers are graded by pathologists Ulcerative colitis: Grades I - IV - Both are inflammatory, but lesions are different - Crohn’s ○ Recurrent granulomatous type of inflammatory response ○ Affects any area of GI tract (mainly ileum and cecum) ○ Slowly progressive ○ Bowel becomes fibrotic - Severity of both vary with remissions and exacerbations. ○ Just bc sxs go away, doesn’t mean the disease is cured. ○ Disease is INCURABLE ****Crohn’s- Recurrent type of inflammation that is slowly progressive ○ Exacerbations and remissions. - Affect both large intestines and small (mainly Ileum & Cecum) - Usually affects women > men - Genetic Link - Symptoms○ Diarrhea ▪ Wt. loss and electrolyte disorders due to the diarrhea ○ Malaise and low grade fever - Complications○ Fistula formation ▪ Abnormal tube where feces enters the body □ Causes infxn/peritonitis ○ Intestinal obstruction - Treatment○ Medications▪ Corticosteroids (prednisone) □ High anti-inflammatory action = drug of choice □ Side effect = diarrhea ▪ Methotrexate (immunosuppressant) ▪ Abx = Can cause diarrhea by acting on intestinal flora ○ Surgical resection of damaged GI tract ○ Diet high in calories, vitamins and protein ▪ Avoidance of fats = worsen diarrhea. ****Ulcerative Colitis- Most common in 30 yrs old - Confined to the rectum and colon (large intestine) ○ Affected area tends to be continuous ▪ Unlike Crohn’s where affected area is in patches. - Disease can be mild, moderate or severe (six or more bloody stools per day) - Symptoms○ Relapsing disorder (remission w/ exacerbation) ○ Diarrhea containing blood and pus for weeks. ○ Mild abdominal cramping ○ Fecal incontinence ○ Anorexia ○ Fatigue - Complications○ Colon cancer ○ Perforation ▪ GIT contents are in the peritoneal cavity - Treatment○ Avoid triggers (caffeine, lactose, spicy foods, gas forming foods) ○ Corticosteroids (prednisone) ○ Immune suppressants (methotrexate) ○ Probiotic therapy ****Clostridium difficile- Bacterial infection associated with antibiotic therapy - Gram positive spore forming bacillus - Etiology○ Broad spectrum antibiotics disrupt normal flora allowing for colonization (via oral-fecal route) - Symptoms○ Abd. cramping, diarrhea, hemorrhage (d/t perforation of the bowel….. TREAT ASAP!!!) - Treatment○ Stop current antibiotic ○ Treatment with metronidazole (Flagyl) or vancomycin ○ Contact Isolation until three clear cultures obtained DIVERTICULA DEVELOP due to INCREASED LUMINAL PRESSURE IN COLON ****Diverticula, Diverticulosis, Diverticulitis- Diverticula = outpouching of colon - Diverticulosis = presence of diverticula w/o infxn - Diverticulitis = infxn of diverticula (can have perforation) ○ Slow moving stool festers in the pouches Patho Page 88 ****Diverticulitis- Symptoms○ Pain in LLQ ****Diverticula, Diverticulosis, Diverticulitis- Diverticula = outpouching of colon - Diverticulosis = presence of diverticula w/o infxn - Diverticulitis = infxn of diverticula (can have perforation) ○ Slow moving stool festers in the pouches ▪ Presence of high residue foods (nuts, seeds, etc.) = increased risk ○ Increase fiber intake ○ Bland diet restrictions Appendicitis- RLQ pain ○ DO NOT PALPATE…. You can rupture it - Rebound tenderness - Elevated WBC - Treat w/ surgery Peritonitis- Due to inflamed adhesions and infection - Perforation of the intestines or an ulcer is the usual cause - Treat w/ Antibiotics and manage electrolyte imbalance ****Diverticulitis- Symptoms○ Pain in LLQ ○ N/V ○ Fever & elevated WBC - Complications○ Perforation --> peritonitis ○ Hemorrhage ○ Bowel obstruction - Treatment○ Increase bulk (fiber) ▪ Promotes regular defecation which prevents increases in intraluminal pressure ○ Withhold solid foods ○ Broad Spectrum Antibiotic therapy Bowel (intestinal) obstruction- Strangulation leads to necrosis, perforation, and sepsis. ○ Volvulus = twisting of the bowel ○ Intussception = telescoping of the bowel (frequent in babies) - Adhesions: may cause bowel obstruction ○ Adhesions = scar tissues on the outside of the intestine ▪ Inhibits normal peristalsis ○ Usually occur after Abdominal Surgery Intestinal (bowel) obstruction- Mechanical or Paralytic - Paralytic ileus occur with general anesthesia ○ DO NOT give oral fluids until return of bowel sounds ○ Signs & Symptoms ▪ Abdominal pain & distention & rigidity ▪ Absolute constipation ▪ Vomiting ▪ No bowel sounds present. ○ Gases and fluids accumulate in the gut ▪ Causes more fluid and electrolyte imbalances ▪ Need Immediate medical attention! ○ NPO; IV fluids, NGT Hepatitis- Etiology○ Viruses ▪ Hepatitis A ▪ Hepatitis B ▪ Hepatitis C ○ Chronic alcoholism ○ Drug Toxicities ○ Autoimmune Disorders ****Viral Hepatitis - Direct cellular injury = inflammation ----> immune responses ○ The more prevalent the sxs, the greater chance of seeking treatment and not becoming a carrier - Phases○ Prodromal phase▪ Symptoms are vague ▪ Fatigued, myalgia, malaise ▪ Severe anorexia ▪ N&V ▪ Dark urine ○ Icterus Phase▪ About 5-10 days after prodromal phase ▪ Prodromal symptoms worsen ▪ Jaundice appears ▪ Severe pruritus and liver tenderness ○ Convalescent Phase▪ Improving symptoms after 2-3 weeks --------------------> - Return of appetite ▪ Complete recovery - Disappearance of Jaundice □ Hep A = 9 weeks □ Hep B = 16 weeks □ Hep C and other strains = years - Hepatitis A○ Contracted through fecal-oral route ▪ Common sources = day care & cafeteria ○ Symptoms▪ Jaundice ▪ Mild fever ▪ Malaise ▪ Nausea ▪ Anorexia Patho Page 89 ▪ Anorexia ▪ Dark urine. ○ Children younger than 6 may be asymptomatic ○ DOES NOT cause chronic hepatitis or induce a carrier state ▪ Rarely causes Acute Fulminant Hepatitis (LIVER FAILURE) □ AFH causes systemic symptoms ○ Hep A vaccine for people traveling to areas of poor sanitation. ▪ CDC recommended vaccination of at risk children & after exposure - Hepatitis B○ Contracted mainly through blood, semen ▪ IV drug use and unprotected sexual intercourse ▪ Not common in transfusions thanks to Hep B screening ○ Vaccine widely given and numbers have decreased - Hepatitis C ○ Most common cause of cirrhosis and liver cancer worldwide ○ Blood transmission ▪ Recreational drug use and semen are the most common routes ▪ Tattooing, acupuncture and body piercing may also be a source of transmission. ○ Interferon has been used as a treatment - Hep B and C lead to chronic liver disease and a state of being a carrier of the disease. Cirrhosis- Most common is alcohol abuse - Cirrhosis impairs all functions of the liver - Portal hypertension ○ Caused by liver cirrhosis ○ Venous blood (via portal vein) cannot flow through the liver normally ○ Leads to EV ▪ Varicose veins in the esophagus ▪ As blood pressure increases, the pumping effects is getting worse (vessels are enlarging more and more) ▪ These can rupture and causing hemorrhage into stomach and vomiting blood - EV is expected in severe cirrhosis ○ If they start to have prodromal sxs (chest pain) they’ll band the EV to prevent rupturing - Symptoms○ Jaundice is one of the earliest symptoms ○ Severe ascites ○ Peripheral edema ○ Signs of malnutrition ○ Bleeding ○ Portal hypertension ○ Hepatic encephalopathy ○ Clay colored stools = lack of bile in stool ○ Pruritus ○ Esophageal varices - Labs○ Elevated ammonia levels ○ Elevated liver enzymes▪ SGOT, SGPT, ALT, AST ○ High bilirubin ○ Decreased Hgb, Hct, blood clotting factors (liver produces clotting factors) ○ Leukopenia ○ Low vitamin K ○ Hypoalbuminemia Drugs to treat PUD (anti-ulcer drugs) - Antibiotics- eradicate H. pylori ○ Combination of the following ▪ Amoxicillin ▪ Clarithromycin (Biaxin) ▪ Tetracycline ▪ Metronidazole (Flagyl) ▪ Bismuth (Pepto-Bismol) ○ Use at least 2, preferably 3 antibiotics for 14 days ▪ Heavy use of Abx can lead to 2nd infxn (C. diff.) - PPI's○ Omeprazole (Prilosec) = (the first PPI) ○ Esomeprazole (Nexium) = “the purple pill” ○ Pantoprazole (Protonix) - Antacids and mucosal protector drugs○ Antacids are alkaline drugs that neutralize stomach acid. Main uses: GERD & PUD ▪ Antacids = Maalox, Amphojel, Milk of Magnesia ▪ Many people self-prescribe and take ○ Mucosal protectors = Sucralfate (Carafate) Protects ulcer w/ mucous secretions - Misoprostol (Cytotec) = Antiinflammatory Constipation and treatment- Non drug approaches – increase fiber, fluids, activity, routines - Laxatives○ DO NOT USE until ABSOLUTELY NECESSARY ▪ Stop use x2-3 days (to prevent dependence) Bulk forming Patho Page 90 ○ Bulk forming ▪ Psyllium (Metamucil) □ Nursing implications = take with full 8 oz glass of fluid. ○ Surfactant (stool softener) ▪ Docusate sodium (Colace) ○ Stimulants (irritate the bowel & promote peristalsis) ▪ Bisacodyl (Dulcolax) ○ Osmotic – pull water into the lumen of the bowel ▪ Magnesium hydroxide (Milk of Magnesia) ▪ Sodium phosphate (Fleet Phospho-Soda) Diarrhea- A symptom, not a disease - Stools of excessive volume and fluidity, & increased frequency - Etiologies○ Infection (example, Traveler's diarrhea) ○ IBS ○ Some medical treatments (some cancer chemos d/t GIT cells being rapidly dividing) ○ Preps for Dx tests - Antidiarrheal agents ○ Non-specific agents – opioids – decreases intestinal motility by activating opioid receptors in the GI tract ○ Loperamide (Imodium) – can be purchased OTC or obtained by Rx ○ Diphenoxylate (plus Atropine) ▪ Atropine is an anti-cholinergic drug ▪ (Lomotil) ○ Paregoric (contains 0.4mg morphine/mL) - Infectious Diarrhea ○ Treat if infection is serious ▪ Diarrhea is mostly self-limiting (resolve with symptomatic treatment) ○ Treat w/ Abx▪ Salmonella, Shigella, Campylobacter or C. Diff. ○ Traveler’s diarrhea – usually caused by Escherichia coli ▪ Most cases self-limiting. Module 16 | Musculoskeletal SystemOA & RA are 2 of the most common MSK disorders… Osteoarthritis (OA)Compare & Contrast OA & RA on Whiteboard!!! - MOST COMMON FORM OF ARTHRITIS - Caused by “wear and tear” on the body ○ Aging mechanical stress on the joints - Less severe than RA - Generally affects people over age 40 ○ MOST COMMON OVER 60 - Usually only affects the joints (not systemic) - Commonly found in both men and women Rheumatoid arthritis (RA)- More severe than OA - Affects women > men - Most commonly affects between age 20 - 50 years - Immune system attacking the body ○ Autoimmune disorder characterized by inflammation - Symptoms can be felt throughout the entire body (systemic) - Genetic link (HLA DR alleles)○ Specific to the X-chromosome which highlights the higher prevalence in females Osteoarthritis- Signs and Symptoms○ Joint pain▪ Aching pain d/t synovial inflammation and fibrosis of the joint ▪ Usually worsens with activity □ Relieved by rest ○ “Gelling”▪ Pt has difficulty initiating the joint movement after a period of inactivity ▪ Stiffness of the joints (knees) when initiating movement □ "Getting joints warmed/oiled up…… " ○ Limitations in joint motion and stability ○ Crepitus ○ Joint locking upon movement ○ Joint enlargement - Most Common Joints○ Hips, knees, lumbar & cervical vertebrae, PIP & DIP in hands, first carpometacarpal joint (base of thumb), and the first metatarsophalangeal joints of the feet (Great Toe) ○ Development of Nodes▪ Bouchard's Nodules occur at the proximal IP joint ▪ Hebreden's Nodules occur at the distal IP joint ▪ Occur d/t repeated trauma of the joint - Diagnosis○ Pt Hx Patho Page 91 ^^^^ WHITEBOARD THIS!!!!!! Cartilage protects the bones from rubbing together - OA results in injury to the chondrocytes and release of cytokines (interleukin I, TNF) - Cytokines stim the release of Proteases (enzymes) that destroy the joint structure - Chondrocytes are more susceptible to more injury and the cycle goes on and on ○ Inhibits their ability to repair itself - Chondrocytes become enlarged and disorganized ○ Trying to compensate for the quickly deteriorating cartilage - Results in Inflammation of the cartilage and the cartilage loses its smooth/cushioning effect ○ Develops surface cracks and synovial fluid seeps in the cracks and causes widening of the cracks - Eventually completely wears through to the bone ○ Bone rubbing on bone ○ Fragments of cartilage and bone become dislodged and float in the joint cavity ▪ Bouchard's Nodules occur at the proximal IP joint ▪ Hebreden's Nodules occur at the distal IP joint ▪ Occur d/t repeated trauma of the joint - Diagnosis○ Pt Hx ○ XR, labs ○ Trying to exclude the presence of other diseases - Treatment○ No cure ○ Symptomatic treatment ○ Oral meds▪ Aimed at reducing inflammation & pain relief ▪ NSAIDs, ASA, Corticosteroids injection, Prednisone, etc. □ Have to take the meds frequently = increases r/o GI bleeding w/ NSAIDS & ASA □ Corticosteroid injections are given sparsely apart and w/ a small dose - d/t the long term effects of corticosteroids - 1x injection Q3mos ▪ Tylenol can help w/ pain but NOT INFLAMMATION Patho of Rheumatoid Arthritis- Immunologic process○ Autoimmune disorder ○ Abnormal immune response = synovial inflammation and joint destruction ▪ Destruction of the joint is irreversible □ Disease progresses and is v v v v debilitating ○ Rheumatoid Factors- (80% of people) ▪ RF reacts w/ IGG and forms immune complexes ▪ High serum RF Titer = more severe sxs & unremitting disease ○ INFLAMMATORY RESPONSE = Increased blood flow & capillary permeability ▪ Synovial cells and sub-synovial tissues undergo reactive hyperplasia □ Abnormal numerical increase of cell numbers ▪ PANNUS (destructive vascular granulation tissue) forms b/w cartilage and subchondral bone - Articular manifestations○ Joint involvement is symmetric and poly-articular = multiple joints involved ▪ Bilateral joints are effected at the same time ▪ THIS IS DIFFERENT FROM OA (OA depends on WHERE the wear/tear occurred) ○ Pain and stiffness (lasting for 30 minutes – several hours) ○ Progresses to larger joints ▪ Ankles, knees, shoulders, etc. ▪ Spinal involvement is limited to the cervical vertebrae ○ Progressive joint destruction leads to subluxation ▪ Subluxation = dislocation of the joint and bone ends are misaligned □ Leads to instability and limited ROM of the joint / loss of fxn ○ Stretching of joint capsule and ligaments leading to joint deformities resulting in loss of function ▪ Opening jars, buttoning shirts, etc. ○ Swan Neck Deformity- ------------------------------------------------------------------------------> ▪ Hyperextension of PIP and partial flexion of DIP ▪ Fairly common in long term RA pts ▪ Results in loss of fxn in hands - Extra articular (systemic) manifestations○ Fatigue / Weakness ▪ Fatigue related to systemic inflammation (immune response!!!!!) ○ Anorexia and weight loss (d/t inflammation like above) ○ Elevated ESR and CRP (inflammatory response) ▪ The more elevated, the higher the severity of the RA ○ Rheumatic nodules ▪ Granulomatous lesion that can have a central core filled w/ fibrin and proteins ▪ Usually occur on the bony surfaces (edge of forearm) ▪ May or may not occur, and may be tender… or not ▪ Vary in size ○ Dryness of the eyes, mouth and mucous membranes ▪ More advanced sxs ○ Episcleritis, scleritis, scleromalacia ▪ All eye problems ○ Pulmonary fibrosis, pericarditis ○ Splenomegaly and lymph node enlargement ▪ D/t inflammatory process ○ Vasculitis (as in ischemic areas in the nail folds) Diagnosis and Treatment of Rheumatoid Arthritis- Diagnosis○ Based on findings of patient history & physical examination ○ XR & blood tests ○ At least 4 criteria (from ARA) must be present for diagnosis ▪ Morning stiffness lasting x1 hr for 6 wks ▪ Simultaneous swelling of 3+ joints x6 wks ▪ Swelling of the wrist, PIP joints x6 wks ▪ Symmetric joint swelling x6 wks ▪ Presence of bone nodules - Treatment○ Goals ▪ EDUCATE ▪ Reduce pain ▪ Minimize stiffness and swelling Patho Page 92 ○ Develops surface cracks and synovial fluid seeps in the cracks and causes widening of the cracks - Eventually completely wears through to the bone ○ Bone rubbing on bone ○ Fragments of cartilage and bone become dislodged and float in the joint cavity - Synovial fluid leaks through these defects into the bone ○ Can lead to development of cysts inside the bone & osteophytes (bone spurs) RA- Autoimmune, inflammatory w/ systemic effects - Disease can be launched w/ CD4 T-cell mediated response d/t immunologic triggers (infxn, stress, bacterial, viral, etc.) ○ Person is already predisposed and is kicked into gear ▪ Genetic- First degree relative FHx ○ Release of inflammatory mediators (cytokines, TNF, Interleukin) and start the process of destruction like above - Destruction of the joint = hypertrophy ○ Leads to development of pannus ▪ Formation of abnormal granulation tissue in the joint ▪ Vascular tissue that grows and invades the space b/w bones ○ Pannus limits ROM and can lead to complete joint fusion ○ PANNUS ONLY OCCURS IN RA - Treatment○ Goals ▪ EDUCATE ▪ Reduce pain ▪ Minimize stiffness and swelling ▪ Maintain mobility ○ Physical rest ▪ Balance w/ mobility to prevent permanent loss of ROM ▪ Reduces stress on the joints ○ Therapeutic exercises ▪ Help to maintain ROM of the joint and improve muscle strength to prevent atrophy ○ Safe use of heat and cold = nonpharm pain relief ○ Relaxation techniques ○ Rx▪ Salicylates (ASA) □ Can cause GI issues w/ overuse ▪ NSAIDs ▪ COX-2 inhibitors □ Celebrex □ Salicylates □ Blocks prostaglandin synthesis which decreases inflammatory response - Less tendency for GI bleeds than ASA ▪ DMARDs □ Disease Modifying Anti-Rheumatic Drugs □ Work to reduce the sxs of RA - Prevent permanent tissue damage of the joints □ Methotrexate - Rx of CHOICE!!!!!! □ DMARDs can be toxic and require close monitoring for adverse effects - Ex: bone marrow suppression (methotrexate) ▪ Corticosteroids □ Help w/ pain, but don't modify disease and don’t protect against joint destruction □ Simply symptomatic treatment ▪ Biologic agents (Remicade, Enbrel, Humira, & drugs ending in "-umab") □ Block TNF (inflammatory mediator) Gout- Alcohol, and dieting can lead to gout - Acute attack is usually mono-articular ○ Most common joint = great toe ○ Attacks usually occur at night and follow a pattern (activity during the day and pain at night) - Pathophysiology○ Elevation of serum uric acid ▪ End product of PURINE metabolism ▪ Can be from overproduction of Purines, Uric Acid, or inadequate elimination of uric acid through urine □ Treat based on the underlying problem ○ Monosodium urate crystals precipitate in joints resulting in inflammation ○ Repeated attacks lead to chronic arthritis and tophi (large, hard nodules) ▪ Tophi don't appear until after about 10 years w/ gouty flare-ups - Signs & Symptoms○ Pain ▪ Onset of pain is abrupt ▪ Can be VVV severe (weight of bedsheets on toes cause severe pain!) ○ Redness, swelling, may begin at night - Diagnosis○ Synovial fluid analysis ▪ Look for monosodium urate crystals, tophi, etc. ○ Serum uric acid levels ○ 24 hours urine sample - Treatment○ Reduce inflammation▪ Allopurinol (reduces uric acid levels) ▪ NSAIDs ▪ Colchicine □ Anti-inflammatory □ Given PO & IV (IV acts rapidly to decrease acute attack) ▪ Steroids ○ Nonpharm▪ Alcohol cessation ▪ Maintain ideal body weight (obesity = predisposing) ▪ Avoid foods high in purines □ Red meat □ Organ meat (liver, kidney) □ Sardines, anchovies Rheumatic Disease in the Elderly- Very common cause of complaints in elderly ○ Pain, weakness, muscle stiffness ○ Rheumatic disease is VVVV debilitating and can lead to decreased QOL, life-span, and depression - Mobility○ Weakness & pain = Gait Disturbance = increased r/o falls and fractures ▪ Decreased independence - Pain, Stiffness and Muscle Weakness affect daily life, threaten independence, and quality of life. Patho Page 93 - Pain, Stiffness and Muscle Weakness affect daily life, threaten independence, and quality of life. ○ May threaten duration of life **she mentioned this like 3 times** ***All of the sxs can lead to a decreased QOL and a decreased life-span*** - Non-Pharmacological Treatment○ Aimed at reducing load on joints & maintaining mobility ▪ Lose weight & use walking aids to reduce load ▪ Muscle-building exercise ▪ Muscle-strength & stretch particularly effective with early start ▪ Local heat ○ Caution: excess rest provides PAIN RELIEF BUT causes lost muscle strength & immobility - Drug Therapies○ NSAIDS & Analgesics ▪ NSAIDs not tolerated as well & side effects more serious □ GI bleed, renal insufficiency, cognitive impairment ○ Elderly have decreased renal and liver fxn = decreased drug metabolism Osteomyelitis- Very difficult to treat!!! - Can be acute or chronic infection of the bone and marrow ○ Potential sources of infection▪ Many different types of microorganisms (fungal, viral, etc.) ▪ (most common is S. Aureus and MRSA) ○ Introduction of Microorganisms ▪ During injury ▪ Operative procedures ▪ From the blood stream□ Systemic infxn that travels to the bone and cultures ○ Acute Osteomyelitis usually occurs from a foreign object being introduced into the bone ▪ Surgery, trauma, etc. - Symptoms○ Severe Pain (exacerbated w/ movement) ○ Warmth, swelling, redness, etc. ○ Fever, chills, malaise ○ Nausea ○ Drainage of pus through the skin if infxn is severe enough ○ Post-Op Osteomyelitis sxs▪ Persistent and recurrent fever ▪ Severe pain at the operative site/trauma site ▪ Poor incision healing - Treatment○ Identification of causative organism (culture and sensitivity) ▪ Have to treat w/ the right Abx since it is so serious ○ Antimicrobials (Abx, antivirals, etc.) ○ Debridement and/or surgical intervention may be used 3 basic categories- MUST TREAT OSTEOMYELITIS w/ LONG TERM IV Abx THERAPY - Hematogenous Osteomyelitis○ Comes from bacterial source in blood stream ○ Rapid onset (few days) after primary infxn ▪ Resolves in 6-8 wks ○ CHILDREN = more common d/t immature bone tissue / rapidly dividing cells / high vascularity ▪ Affects long bones near the growth plates (terminal ends of arteries allow bacteria to sequester ▪ Purulent exudate collects inside the bone □ Not much room for expansion/swelling □ Exudate has to escape the bone and begins to seep out behind the periosteum which damages the arteries that feed the bone - Results in necrosis ▪ May penetrate skin and involve joints ○ Adults▪ More common in males > females (males = increased risky behavior = increased r/o trauma) ▪ Seen in debilitated pts□ Chronic UTI's □ Chronic/recurring Skin Infections □ Diabetes Mellitus □ IV DRUG USERS (S. aureus & pseudomonas) □ Immunosuppressed ▪ In vertebrae, sternoclavicular, & sacroiliac joints/pubic symphysis ▪ Tends to affect joint space - Chronic Osteomyelitis○ More common in adults ○ Infxn continues past expected course (6-8 wks) and can last for years ▪ Usually results from inadequate or delayed treatment of Acute Hematogenous Osteomyelitis ○ Sequestrum = HALLMARK SIGN/SX ▪ Areas of dead bone separated from healthy bone ○ Treat w/ IV Abx and surgery to remove necrotic bone & surgical devices that may have caused the infxn Module 14 | Endocrine- Patho Page 94 infxn Module 14 | EndocrineALL HORMONES IN THE BODY CAUSE ELEVATED GLUCOSE LEVELS - Defined as glucose intolerance ○ Prediabetes/glucose intolerance = 100-126 ○ Diabetes = 126+ **know the difference in definition** Hypothalamus is the OVERALL CONTROL CENTER of endocrine fxn via its own hormones - Hypothalamic hormones effect pituitary and then the target organ - Target organ acts on the hypothalamus ○ NEGATIVE FEEDBACK LOOOP!!!! Primary, secondary, and tertiary endocrine disorders - Primary○ Problem originates in the TARGET ORGAN - Secondary○ Problem originates in the pituitary ▪ Pituitary effects the target organ - Tertiary○ Problem originates in the hypothalamus ADH (vasopressin)- Can be given synthetically when pt is in cardiac arrest to increase BP - Released in response to: ○ Decrease in blood volume ○ Decrease in BP ○ Increase in osmolality of serum - Actions○ Increases arterial pressure ▪ Water reabsorb by kidney ▪ Direct vasoconstriction ○ ACTIONS ARE SHORTLIVED ▪ Vasopressin is used as a quick-fix! - SIADH's○ Syndrome of Inappropriate ADH ▪ Too much ADH is released ○ Failure of the negative feedback mechanism ○ Etiology▪ Usually originates in the lungs ▪ Lung tumors (produce their own ADH) ▪ Stress conditions (surgery, pain, temp extremes, TB, pneumonia) ○ Signs & Symptoms▪ Increased water retention ▪ Dilutional hyponatremia ○ Patho▪ Activation of baroreceptors in the carotid and pulmonary vessels □ Respond to changes in intrathoracic pressure ○ Diagnosis▪ Low serum sodium (dilutional hyponatremia) ▪ Low serum osmolality - Diabetes Insipidus○ Inadequate ADH production ▪ Kidneys are unable to retain water and sodium ○ Etiologies▪ Tumor or Inflammatory conditions □ Cancer, abscesses, meningitis, etc. ▪ Surgery, radiation ▪ TBI ○ Signs & Symptoms▪ Polyuria (3-20 Liters per Day) ▪ Polydipsia ▪ Dryness of mouth & skin ▪ Hypertonic dehydration (hypernatremia) ○ Diagnosis▪ Pale and dilute urine ▪ Low urine specific gravity ▪ Increased serum osmolality ▪ Hypernatremia ○ Treatment▪ Vasopressin & Desmopressin (synthetic ADH supplement) □ Normalizes water excretion ▪ Vasopressin = vasoconstrictor!!! □ Use caution w/ cardiac pts □ Desmopressin = safe w/ no cardiac effects Anterior Pituitary- Produces ACTH, TSH, GH, FSH, LH, & Prolactin - Hormone release follows a circadian rhythm ○ Values are higher in the AM ▪ Do lab tests in the morning ' Patho Page 95 ▪ Do lab tests in the morning ' Growth Hormone- Hypo-secretion can cause: ▪ Shortness ▪ Normal intelligence ▪ Obesity ○ Rx w/ GH injections (DNA recombinant therapy) ▪ Ethical concerns w/ GH supplements in adults - Hypersecretion○ Children▪ Gigantism ▪ Most common cause = Pituitary Adenoma (benign) ▪ Large height of 7-8' ○ Adults▪ Long bones epiphyses are closed… □ Leads to ACROMEGALY -----------------------------------------------------------------------> ▪ Affects hands, FACE, kyphosis, deeper voice, glucose intolerance, ▪ Can enlarge the heart = fatal - Diagnosis○ Draw Hepatic IGF-1 level & GH levels ▪ Hepatic IGF-1 (Liver enzyme) mediates GH activity ○ MRI tumor - Treatment○ Surgical removal of tumor ○ Radiation therapy▪ Can lead to pituitary hypofunction Thyroid- Thyroid Hormone○ Iodine attaches w/ Tyrosine to form T4 (thyroxine) & T3 (triiodothyronine) ▪ T4 is converted to T3 ○ Actions▪ Thyroid hormones are necessary for ALL CELLULAR FXNS □ Strongest Effects on Cardiac, Respiratory, GI, Neuromuscular systems ▪ Increases metabolism & protein synthesis ▪ Responsible for proper Growth & Devo in children □ Including mental and sexual maturity - Children born w/o thyroid hormone will be ID - Calcitonin○ Lowers blood calcium levels ▪ Inhibits calcium resorption from the bone ○ Calcitonin levels increase when serum calcium rises above normal - Hypothyroidism○ 2ND MOST COMMON ENDOCRINE DISORDER ▪ Behind DM ○ Most cases are primary hypothyroidism (thyroid gland is ineffective) ○ Primary Hypothyroidism- (problem w/ thyroid) ▪ Low Thyroid Hormone (T3 & T4) ▪ High TSH from pituitary ○ Etiology▪ Autoimmune destruction of the thyroid gland by antibodies □ Most common in Women after age 50 □ Hashimoto's Thyroiditis- ANTIBODIES MUST BE PRESENT TO BE Dx w/ HASHIMOTO'S ▪ Congenital Hypothyroidism□ Cretinism □ Baby is born w/ inadequate T3 & T4 production d/t problems with their thyroid or absence of the thyroid - Untreated Cretinism = mental retardation if undiagnosed and untreated ▪ Partial or total resection of the thyroid□ Removed d/t cancer or HYPERthyroidism □ Require LIFELONG replacement therapy ○ Signs & Symptoms▪ Goiter- only occurs w/ iodine deficiency ▪ Lower metabolism □ Lower body temp / Cool skin (COLD INTOLERANCE) □ Increased body weight ▪ Weakness ▪ Slow motility/constipation of GIT ▪ Reduced myocardium contractility (decreased cardiac output) ▪ Decreased Liver Function- rise in cholesterol levels ▪ Decreased sex drive □ Irregularities in menstrual flow ▪ CNS depression□ Fatigue □ Slower mental processing □ Memory impairment (if severe hypothyroidism) ○ Myxedema Tissue- -------------------------------------------------------------------------------------> ▪ Unusual fluid retention □ Puffiness of the face □ Periorbital swelling/edema (in severe deficiency) ▪ Myxedema Coma□ Extreme hypothyroidism □ Life-Threatening, severe condition Patho Page 96 Calcium-Bone-IN- Keep CALCIUM INSIDE the BONE □ Puffiness of the face □ Periorbital swelling/edema (in severe deficiency) ▪ Myxedema Coma□ Extreme hypothyroidism □ Life-Threatening, severe condition □ Treat w/ supplemental thyroid hormone ○ Diagnosis▪ High TSH // Low T3 & T4 = PRIMARY ▪ Presence of Thyroid Antibodies = HASHIMOTO's ○ Rx▪ Drugs restore thyroid fxn and replace deficient hormone ▪ Levothyroxine (T4) [Synthroid]□ Drug of choice!!! □ Body takes the T4 and converts it to T3 - Hyperthyroidism○ Most common in women ○ Less common than HYPO-thyroidism ○ Etiology▪ MOST COMMON = Grave's Disease □ Autoimmune etiology □ YOU MUST HAVE ANTIBODIES PRESENT TO Dx w/ GRAVES!!!! - If no antibodies = simply "hyperthyroidism" ▪ Hypofunction of the Pituitary □ Low TSH (trying to slow thyroid down) □ High T3 & T4 (overactive thyroid) ○ Effects▪ Exaggerated target organ response □ Increase HR - HR greater than 100 = decreased cardiac output ▪ Increased BMR ○ Signs & Symptoms▪ Thyrotoxicosis□ Palpitations □ Nervousness □ Fatigued (in both hypo & hyper) □ Diarrhea □ Diaphoresis (in both) - Heat intolerance (compared to cold intolerance in HYPO) □ Weight loss ▪ Exophthalmos ----------------------------------------------------------------------------> ▪ Enlargement of Thyroid (diffuse goiter) ○ Thyroid Storm/Crisis▪ Extreme Hyperthyroidism □ LIFE THREATENING condition □ MEDICAL EMERGENCY ▪ Extreme Tachycardia & Hyperthermia □ Need to be in ICU to regain cardiac control Parathyroid Glands- Secrete Parathyroid Hormone (Parathormone) (PTH) ○ Release is controlled by serum calcium levels ▪ Low serum calcium = increased PTH ▪ High serum calcium = decreased PTH (negative feedback) - PTH works to increase serum calcium levels ○ Bone resorption ○ Absorb from GIT ○ Calcium & Magnesium reabsorption from Kidneys ▪ Coupled w/ phosphate excretion ▪ Abnormal calcium levels d/t PTH can lead to irregular Magnesium & Phosphorus Levels - Hyperparathyroidism○ Excess PTH ○ Etiology▪ Tumors of the Parathyroid ▪ Hyperplasia of Parathyroid ▪ Autoimmune Hypercalcemia○ Effects- Decreased neural excitability & impaired cardiac and smooth muscle fxn ▪ Excessive Osteoclast activity - Muscle weakness □ Loss of bone calcium - Neuromuscular▪ Hypercalcemia ○ Headache, stupor, fatigue ○ Symptoms- Anorexia, constipation, N/V ▪ Bone weakness○ Think of the decreased smooth muscle ability □ Bone pain □ Deformities □ Fractures or H/o Fx ▪ Muscular & Neurological sxs ▪ Kidney stones! - Hypoparathyroidism○ Deficient PTH ○ Etiology▪ Removal of PT glands (secondary to hyperparathyroidism) ○ Results in hypocalcemia ○ Symptoms▪ Increased neuromuscular excitability □ Tetany Patho Page 97 Hypocalcemia- INCREASED Neuromuscular irritability ▪ Removal of PT glands (secondary to hyperparathyroidism) ○ Results in hypocalcemia ○ Symptoms▪ Increased neuromuscular excitability □ Tetany □ Trousseau's & Chvostek sign ▪ Cardiac effects ▪ Skeletal effects (severe, long-term deficits) Adrenal Glands"Add"-ison's = "Add"-renal Glands - Pathway of Hormonal Control ○ Hypothalamus --> Pituitary releases ACTH ---> Target Gland = Adrenal CORTEX to release CORTISOL --> effects all tissues - Primary Adrenal Cortical Insufficiency (Addison's Disease)○ Destruction of all layers of the adrenal gland ▪ DECREASED Glucocorticoids (Cortisol) & Mineralocorticoids (aldosterone) ▪ High ACTH (pituitary compensation) ○ Etiologies▪ Autoimmune = most common ▪ TB (most common before 1950) ▪ Surgical removal of Adrenal Glands (Adrenal cancer) ▪ Bleeding from excessive anticoagulants ▪ AIDS□ Opportunistic infxn targets adrenal glands ▪ Anti-fungal agents & other drugs ○ Signs & Symptoms▪ Hyperpigmentation (bronze, sun-tan) ▪ Increased sodium, chloride, & water excretion (aldosterone deficiency) □ Potassium retention □ Extreme losses can lead to Cardiovascular Collapse (hypovolemic shock) ▪ Poor tolerance to stress (low glucocorticoids/cortisol) ▪ Hypoglycemia (low cortisol production) ▪ Weakness ▪ N/V ▪ Weight loss ○ Diagnosis▪ Cortisol, aldosterone, & ACTH levels ▪ 24 hr urine collection for ACTH ▪ Dexamethasone suppression test □ Measures the negative feedback suppression of ACTH ○ Treatment▪ Life Threatening condition (low sodium & water retention = hypovolemic shock/coma/death) □ MUST HAVE drug replacement of all hormones affected (aldosterone, cortisol, etc.) ▪ Hydrocortisone□ Increase dosage during periods of stress - Secondary Adrenal Cortical Insufficiency○ Etiology▪ Removal of Pituitary Gland results in absent/decreased pituitary (ACTH) production ▪ ACUTE ADRENAL CRISIS□ Most common □ Rapid withdrawal of glucocorticoids (hydrocortisone, prednisone, etc.) - Meds leave Adrenal Gland unable to produce own glucocorticoids - Must GRADUALLY DECREASE glucocorticoid use (scheduled Rx) □ Life Threatening- Cardiovascular collapse - Hypotension - Hypovolemic shock ○ Treatment▪ Immediate resume glucocorticoids □ Begin gradual withdrawal ▪ Administer fluids to prevent CV collapse ○ Teach the pt the importance of following the correct schedule/regimen of their Rx - Treatment for Adrenal Cortical Insufficiency○ Glucocorticoids▪ Hydrocortisone, prednisone ▪ ALWAYS REQUIRED ○ Mineralocorticoids▪ Fludrocortisone ▪ Helps w/ sodium & water retention □ Very useful in elderly CUSHING'S SYNDROME- Glucocorticoid Hormone Excess- Types1. Excessive ACTH production d/t pituitary tumor ▪ Cushing's Disease 2. Excessive cortisol production d/t adrenal tumor 3. Ectopic Cushing Syndrome▪ Non-pituitary tumor causing excess release of ACTH 4. Iantrogenic Cushing Syndrome▪ Results from long term treatment w/ Hydrocortisone meds ▪ Teach pts about the long-term adverse "Cushing-like" effects - Signs & Symptoms○ Wt gain w/ Abdominal obesity ○ Increase in "fat"Patho Page 98 Hypocalcemia- INCREASED Neuromuscular irritability - Cramping!!! - Hyperactive reflexes!!! "ADD"-ison's = "ADD" cortisol & aldosterone ▪ Results from long term treatment w/ Hydrocortisone meds ▪ Teach pts about the long-term adverse "Cushing-like" effects - Signs & Symptoms○ Wt gain w/ Abdominal obesity ○ Increase in "fat"▪ Moon Face ▪ Upper thoracic spine (buffalo hump) ○ High blood glucose = glucose intolerance ▪ Treat w/ insulin ○ Protein wasting- (mimics an excessive STRESS RESPONSE) ▪ Thin arms, legs ▪ Decreased wound healing ▪ Increased bruising ○ Hypokalemia, HTN, increased susceptibility to infxn ○ Extreme emotional lability (mild euphoria to psychotic behavior) - Diagnosis○ 24 hr urine test ▪ Look for increased cortisol ○ Serum ACTH levels (depending on the form of Cushing's they have) ○ MRI, CT for tumors - Treatment = surgical removal of tumors HyperaldosteronismExcess aldosterone production = adrenal gland - Etiologies○ Primary- Aldosterone secreting Adenoma ○ Secondary- Renal ischemia which activates the RAAS ▪ Results in increase in aldosterone ▪ RAAS also causes vasoconstriction - Effects○ Renal retention of sodium & water ○ Excretion of potassium - Signs & Symptoms○ HTN ○ Increased serum sodium & decreased potassium Adrenal Medulla HYPER-Secretion• Pheochromocytoma ○ Benign tumor = most common • Results in excess catecholamine release (norepi & epi) ○ Catecholamines are released from the adrenal medulla • Signs & symptoms○ HTN ○ Diaphoresis Sympathetic Responses!!! ○ Tachycardia ○ Anxiety ○ HA HematopoiesisSickle Cell Anemia- Recessive disorder (must have both recessive genes) ○ Inherited HbS gene ▪ Abnormal Hgb, shaped like an S - Signs and Sxs○ Decreased RBC lifespan (20 days) ○ Chronic hemolytic anemia ○ Vessel Occlusion▪ Irregular shape of RBC can get stuck together or stuck in capillaries/smaller vessels ▪ Get caught and clump together, causing clots □ Causes extreme pain, ischemia - Risk factors for developing a Sickle Cell CRISIS: ○ Cold weather, stress, exertion, infection, other reasons for hypoxia, dehydration, acidosis - Other major complications○ Depending on where occlusion is, that organ will show sxs. ▪ MI, stroke (CVA), infection, pneumonia, bone crises (fx), splenic ischemia, other infarctions to the eyes/kidneys/etc. - Diagnoses○ Analysis of DNA (amniocentesis) ○ Hemoglobin electrophoresis ▪ DNA test to determine the genotype of the hemoglobin (if the HbS gene is present) ○ Screening for all ethnicities done in all states - Treatment○ Supportive care given: no specific treatment, but can treat the associated problems! ▪ Antibiotics (infxn), fully immunized against flu, Hep B, pneumonia ○ Hydroxyurea (drug), blood transfusion (packed RBCs), bone marrow transplant, stem cell transplant, etc. Aplastic Anemia: - Reduction of ALL TYPES OF BLOOD CELLS (WBC, RBC, platelets) ○ Fatal - no blood cell production - Either insidious or acute onset - Etiology○ Most are unknown etiology ○ Exposure to radiation ▪ Radiation/chemotherapy suppress bone marrow Patho Page 99 Moon Face & Buffalo Hump disappear when Cortisol production is "normalized" ▪ Radiation/chemotherapy suppress bone marrow ▪ Cancer treatment = purposeful aplastic anemia ○ Chemicals, toxins that reduce hematopoiesis ○ Benzene, chloramphenicol, AIDS - Signs & Symptoms○ Initial symptoms include that of Anemia ▪ Fatigue, weakness, pallor ○ Petechieae (punctate skin bruising) and Ecchymosis (bruises) due to decreased platelets ▪ Also prone to bleeding from body cavities ○ Increased susceptibility to infxn (decreased WBC's) - Treatment○ Blood transfusions ○ Bone Marrow transplants ○ Immunosuppressive Therapy▪ Prevents the suppression of the hematopoietic stem cells in the bone marrow ○ Antibiotics for possible infxn. ○ Removal of the causative agent (chemotherapy, radiation, etc.) DiabetesType I Diabetes Mellitus- IT IS A MULTIFACTORIAL DISEASE - Most common in younger population (under 30) ○ 3 things cause Islet cell destruction○ Genetic predisposition ▪ Genetics□ Diabetes can aggregate in families □ Concordance rate for twins is 50% □ Exact mode of inheritance is unknown ○ Autoimmunity --------------------------------------------------------------------------------------> ▪ 90% pts have circulating islet cell antibodies within a year of Dx ▪ Approximately 10% have other autoimmune disorders include: □ Grave's Disease, & Addison's Disease ○ Environmental insult/effects ▪ Viruses are suspected as initiators the insult and causes Type I diabetes ▪ There has probably been a long latency period of the virus in the body with subsequent beta cell loss ▪ Chemical toxins - Signs and Sxs○ SIGNS ANS SXS DUE TO AN ABSOLUTE ZERO AMOUNT OF INSULIN ○ Classic Signs & Sxs = polydipsia, polyuria, polyphagia, & weight loss ▪ Increase the eating but losing weight ▪ Glucose is a very large molecule □ As it move through renal tubule, it filters out as urine and it draws water through osmosis. □ Some weight loss is due to the loss of water weight - And also due to the glucose being excreted as urine and not going into the cells for use/storage □ GLUCOSE IS AN OSMOTIC DIURETIC (polyuria) - Causing the thirst, hunger, and weight loss ○ Leaving untreated can progress to Diabetic Ketoacidosis (DKA) ▪ Can lead to coma & death - Treated through INSULIN (primary), Medical Nutrition Therapy (MNT), and physical activity ○ YOU MUST BE TREATED WITH INSULIN No if's and's or but's ○ Physical activity is very important to any Dx/Treatment plan with DM - Blood Glucose Monitoring○ Fasting Blood Glucose as needed to monitor Diagnoses ○ Need blood glucose monitors when injecting insulin ▪ Type I check a minimum of 4 times per day before meals & before bed (ACHS) ○ A1C- check this 3-4 times annually for T1 & T2 ○ Medicare/Medicaid will cover most of these costs Diabetic Ketoacidosis- Occurs when diabetes is out of control ○ More common in Type I - 3 major metabolic problems○ Hyperglycemia!!!!! Dangerously high levels of glucose ○ Ketosis (presence of ketones in the blood) ○ Metabolic acidosis (ketones are acid bodies) ▪ Body tries to normalize the acidosis caused by ketones and depletes the stores of HCO3 - Onset○ Slow onset over several days…… unlike hypoglycemia ○ Risk Factors: ▪ Newly diagnosed ▪ Not taking sufficient insulin (you will die) ▪ Too little exercise, too much food, Stress, infxn □ All of these cause an increase in BG levels - Signs and Symptoms○ Classical Signs of DM ▪ Polyuria, polydipsia, polyphagia ○ Abdominal pain/tenderness ○ Fruity Breath (due to ketones in the blood) ○ Kussmaul's Respirations Patho Page 100 ○ Kussmaul's Respirations ○ Hypotension/hypovolemic (due to polyuria) ○ Decreased Level of Consciousness ▪ Will progress to coma if no intervention (INTERVENTION MUST BE INSULIN) ○ Death can result from metabolic acidosis and hypovolemic shock - Pathogenesis○ See figure --------------------------------------------------------------------------> ○ Body switches from carb metabolism to fat metabolism ○ Ketones are intermediate products from incomplete metabolism of fat ▪ Will be able to measure ketones in the blood and urine (ketonemia & ketonuria) ○ Ketones are acid bodies, causing acidosis ▪ Normal pH is 7.35-7.45 (pH IS LOOOWWWW!!!!!) ○ Kussmaul's Respirations: Body will try to compensate with increasing respirations (very rapid deep respirations) ▪ Body is trying to blow off CO2, to balance the acid levels in the body - Diagnosis○ Hyperglycemia (Blood Glucose above 250 mg/dL) ○ Low Bicarbonate (less than 15) …. Normal = 22-31 ○ Decreased pH/acidic (less than 7.3) ○ Ketonemia & Ketonuria ▪ Ketones are present in the blood and the urine ○ Sodium levels are low & Potassium levels are elevated ▪ DKA causes hyperosmolality of extracellular fluid ▪ Thus Intracellular Water & K+ shifts to the extracellular component ▪ This causes a "pseudo-hyponatremia" due to the intracellular-extracellular fluid shift □ AKA sodium levels are relatively low - Treatment○ GIVE IV INSULIN ○ Replace low electrolytes and monitor Q1H ○ Usually admitted to the ICU ○ Need to identify the underlying cause then treat the cause Chronic Complications of DM- Occurs in both Type I & II DM ○ DM complications are a major cause of blindness, amputations, and the need for dialysis - DM is a major risk factor for development of CAD resulting in MI ○ The most common COD in DM pt.'s is CARDIAC COMPLICATIONS - Types of Chronic Complications: ○ Peripheral Neuropathy (nerve damage… think of foot ulcers, etc.) ○ Nephropathy ○ Retinopathy ○ Skin lesions & foot ulcers - Pathophysiology of Chronic Conditions○ Polyol Pathway▪ Hydroxyl Groups (OH-) on the glucose are converted to Sorbitol & Fructose □ Sorbitol causes swelling and clouding in the lens of the eye (NOT retinopathy) ▪ Polyol Pathway affects the eye lens, kidneys, nerves, & blood vessels ○ Formation of Glycoproteins▪ Glycoproteins are usually found in the basement membranes of capillaries ▪ Increased levels of blood glucose favors the formation of even more of the Glycoproteins □ Causes a disruption of capillary exchange due to narrowing of the vessel ▪ Affects the Eye, Kidney, & Vascular System ○ Tissue oxygenation ▪ RBC dysfunction that interferes with the release of O2 from the hemoglobin ○ Protein Kinase C▪ Protein Kinase C is an intracellular signaling molecule □ Regulates vascular functions: - Permeability, vasodilation, endothelial activation, & growth factor signaling ▪ DM causes an increase in Protein Kinase C □ Activation of PKC in the retina, kidney, & nerves can cause vascular damage □ Also causes disorders in mitochondrial function - Blindness/RetinopathyDon't know statistics, but know the ADA recommendation ▪ Annual dilated pupillary exam ○ Diabetes is the leading cause of new blindness ▪ Review why Retinopathy occurs - Kidney Disease○ Diabetes leading cause of kidney failure (ESRD) ▪ Need an annual microalbumenuria exam □ There should be absolutely no protein in the urine □ Kidneys cannot filter proteins… if there are proteins, then there is a sign of renal failure/disease - Neuropathy○ Majority of DM population has some form of nerve damage ○ Recommendation is to check their feet without shoes/socks at every provider visit ▪ Looking for hair loss, thickened nails, check their sensation ○ Foot and Leg▪ Thickening of the basement membrane of the capillaries supplying the nerve □ Decreased blood flow can lead to necrosis ▪ Demyelination occurs causing a slowing in nerve conduction ▪ Sensory neuropathy = loss of pain/pressure sensation □ Injuries go unnoticed ○ Foot Care- Patho Page 101 □ Decreased blood flow can lead to necrosis ▪ Demyelination occurs causing a slowing in nerve conduction ▪ Sensory neuropathy = loss of pain/pressure sensation □ Injuries go unnoticed ○ Foot Care**SEE SLIDE** ---------------------------------------------------------------------------------------------> ○ Preventing Peripheral Neuropathy▪ Control blood sugar!!!!!! ▪ Daily inspection of feet ▪ Always wear shoes inside and outside ▪ Don't use heating pads ▪ Break in new shoes gradually ▪ Trim nails carefully ImmunityTwo types of Immunology- Innate○ This is the first line of defense ○ Early and rapid and lacks an organized attack (irrational jealous girlfriend) ○ Recognizes Self vs. Nonself Cells ○ This includes the▪ Skin, mucous membranes, phagocytic leukocytes, specialized lymphocytes (NK cells) ▪ Phagocytes and NK cells just blindly rush to the intruder ▪ Some cells eat the intruder, and PRESENT THE ANTIGEN (antigen presenting cells) to the other immune cells - Adaptive○ Specific/acquired ○ Slower to respond, more effective approach (rational jealous girlfriend) ○ Recognizes the threat, plans, and attacks ▪ Specialized cells attack the intruder ○ 2 types of responses▪ Humoral- B-cells create antibodies to fight the intruder ▪ Cell-Mediated- T cells activate phagocytes or kill Host cells which holds the intruder SEE THE IMMUNE SYSTEM FLOW CHART -----------------------------------------------------------------------------------> - Complement cascade- helps out by getting rid of debris ○ Complement are a group of proteins that rid the blood of the debris from phagocytized cells ○ Enhances the antibody response - Antibodies○ Created in response to a specific foreign substance in the body ▪ Antibodies are unique to that specific antigen ▪ Last forever in the body ○ IGM & IGG ▪ Immunoglobin-M & Immunoglobin-G ▪ IGM's indicate initial exposure to an antigen □ "M" = meet… you can only meet someone one time ▪ IGG's are the established antibodies that continue circulating □ "G" = greet… you can greet someone infinite times, but only meet someone one time □ IGG's indicate if someone has immunity over something (titers) ○ Some antibodies can be received from Mother (IGG) or through vaccination (passive immunity) ▪ IGG's cross the placenta and give the baby immunity Adaptive (Acquired) Immune System- Humoral○ Defend in the blood and mucous (humorous) ○ B cells produce antibodies ○ B cells recognize the antigen differentiate into plasma cells and then secrete specific antibodies ○ Antibodies connect to antigens floating in the blood or the SURFACE of cells - Cell-Mediated○ T-cells are located INSIDE the cell (B cells cannot get here) ○ Recognize antigen-presenting cells by receiving the signal from the B-cells ○ Helper T-cells- (CD4) ▪ Helps regulate almost all other immune cells ▪ Release cytokines to help signal antigens for further destruction/help from other immune system cells ○ Cytotoxic T-cells- (CD8) ▪ Kill the intracellular antigens ▪ Inject enzymes into the cell where viruses/cancers/bacteria are and induce apoptosis Immunodeficiency- Primary Immunodeficiency○ Congenital or inherited (rare but there are a lot of these) ▪ Genetic mutations, recessive genes, X-linked disorders, etc. ○ Pathophysiology▪ Mutations cause a lack of development of immune system cells ▪ Mimic the symptoms of autoimmune disorders ○ Early detection is critical because the primary deficiencies are FATAL in Children ▪ Family Hx is important because remember this is GENETIC ○ Notice primary immunodeficiencies by recurrent, persistent, or unusual infxn ▪ They will get the same type of infxn over and over and over ▪ The type of infections can help diagnose the immunodeficiency - Secondary ImmunodeficiencySecondary is acquired Patho Page 102 Basophils & eosinophils = fungal infxn Neutrophils, Basophils, & Eosinophils = Phagocytes ○ Secondary is acquired ▪ AIDS most common secondary immunodeficiency ○ Much more common than primary ○ Caused by a pathogen, aging process, malignancies, malnutrition, drugs, etc. ○ Pathophysiology▪ WBC dysfunction □ There is an overall loss in the amount of IGG's - Makes you more susceptible to secondary infection □ Deficit in T-cell numbers and function (low CD4 & CD8 numbers) ○ No cure for these disorders ○ Congenital transmission is possible (HIV+ mother) ○ Remember…. They are IMMUNOSUPPRESED and susceptible to secondary infxn T-cell deficits leave you more vulnerable to viral & fungal infections & Opportunistic infections B-cell deficits increased bacterial susceptibility - HIV/AIDS○ HIV is the virus that causes AIDS ▪ CD4 count below 200 and/or an opportunistic infxn ○ Transmission▪ Can be transmitted through semen, blood, vaginal fluid, breastmilk □ Sexual contact is the most common transmission method ○ Pathophysiology▪ HIV is a retrovirus that kills immune cells □ CD4 Tcells □ Macrophages □ Dendritic cells ▪ Immune Cell Death results in decreased immune response □ EVEN if the person is ASYMPTOMATIC they will have a decreased immune response ▪ Results in increased susceptibility to many secondary illnesses/infections □ (TB, flu, literally anything…) ○ Stages of HIV1. Primary infection□ Can be asymptomatic or have flu-like symptoms 2. Latency period□ Chronic, asymptomatic period □ Can last for years and years and managed well with correct medical treatment 3. AIDS□ Diagnosed by presence of HIV Virus, AND a CD4 Count below 200 and/or an opportunistic infxn ○ Antiretrovirals▪ Medications to treat HIV ▪ Works to decrease the amount of the virus in the body (HIV) □ Goal is to get an undetectable amount of HIV (viral load) in the body and to increase CD4 Count ▪ 5 Classes of Antiretrovirals- -------------------------------------------------------------------> □ Each class of the drugs try to interrupt the life cycle of the HIV at different points □ Usually combine different types of these drugs to target the HIV replication process at multiple points - HAART (Highly Active Antiretroviral Therapy) = combination of multiple antiretrovirals - Opportunistic Infections○ Decreased levels of the CD4 cells creates susceptible to various conditions that wouldn't be pathogenic in a healthy person ○ Examples▪ Respiratory□ TB, bacterial pneumonia - Higher rate of TB in HIV+ population ▪ GIT□ Oral thrush (esophageal candidiasis) - yeast infxn of mouth/esophagus □ Gastroenteritis □ C.Diff., E.coli, etc. ▪ Nervous□ HANDS - HIV Associated Neurocognitive Disorders - Cognitive impairment w/ motor dysfunction - Behavioral issues - Psychosocial issues - Hallucinations □ Toxoplasmosis □ PML - Progressive Multifocal Leukoencephalopathy - Demyelinates white matter in the CNS ▪ Malignancies□ Some forms of cancer are more common in the HIV+ population □ Kaposi sarcoma □ Non-Hodgkin's Lymphoma ▪ Metabolic□ Wasting syndrome - Involuntary loss of 10% of baseline weight - Think of the stereotypical HIV+ pt that is small, skinny, frail □ Lipodystrophy (body is unable to produce fat) □ Insulin resistance GeneticsRegulation of Gene Expression- There are factors that allow genes and characteristics to be expressed individualistic to each person Patho Page 103 - There are factors that allow genes and characteristics to be expressed individualistic to each person ○ Think of: **no two individuals with Downs are the same** - Induction○ Process by which gene expression is increased ▪ (usually promoted by an external influence) - Gene repression○ Process by which a regulatory gene reduces or prevents expression of a gene Genotype vs. Phenotype: - Genotype- genetic info stored in the basic triplet code on the chromosome - Phenotype- outward expression ○ Don't know genotype, because it can be either homozygous dom. Or heterozygous Expressivity/Penetrance- Transcription factors bind to DNA to regulate time or transcript that activate or repress gene expression ○ Ex: in down's some genes express mildly or severely ▪ Depends on the transcription factors and how they tell the DNA to express/repress the gene - Penetrance○ Specific gene's ability to express itself in a pop that everyone has the genotype ○ Ex: entire pop. Has genotype for 6 fingers ▪ Not everyone in the room will express the phenotype for 6 fingers ▪ 75% penetrance = 75% of population with the genotype will express the phenotype Types of Inheritance- Polygenic○ There are multiple genes at different Loci ▪ Each gene on the loci exerts and additive effect on the expression of the trait ▪ THIS HAS NO ENVIRONMENTAL INFLUENCE ○ Ex: eye color, skin color, etc. ▪ Many genes are acting on this trait ▪ Very complex to guess the phenotype - Multifactorial○ Multiple alleles at different loci affect the outcome ○ INCLUDES ENVIRONMENTAL INFLUENCE ○ Ex: height, diabetes, alcoholism, etc. ▪ Height is multifactorial, because yes it includes genetics, but also environmental (maybe you weren't nourished properly, etc.) Mendel's Laws- Locus- position of a gene on a chromosome (loci = plural) - Allele- Alternate forms of the same gene on the same locus • Dominant/recessive Singe-Gene Disorder- Single gene is affected @ a single locus - Marfan's Syndrome ○ Autosomal Dominant Disorder ▪ Need 1 gene from 1 parent Sex-Linked Diseases- Remember X-linked allow females to be "carriers" but not express• Thus males will AUTOMATICALLY express the gene (if they get that particular X chromosome from the mommy) ------------------------------------------------------------------------------------------------------> ▪ There are 2 dummy, don't forget! One affected one is fine! ▪ Some people have boys that don’t get that X chromosome (lucky bastards) - Hemophilia○ Group of diseases in which blood doesn't clot properly Multifactorial Inheritance Disorders- See definition above! Multifactorial- Examples of Congenital Disorders: ○ Cleft palate, congenital heart disease, Urinary tract malformation - Environmental Factors: ○ Think of it this way: you have the genetic predisposition, but your environmental factors can influence/heighten you risk (HTN, cancer, DM, CAD, etc.) - Environmental Influences on Fetal Development○ Period of Vulnerability ▪ Ex: 2 weeks, the CNS is EXTREMELY vulnerable □ Vulnerability of CNS lasts until the 20-22 wks up to 2 yrs. ▪ Each system has a period of vulnerability ○ Teratogenic Agents: ▪ Alcohol, drugs, radiation, chemicals, infectious agents ○ Exposure to teratogens during period of vulnerability can alter genetic expression of the fetus… damn. ○ Fetal Alcohol Syndrome Autosomal Examples- Human Allelic Disorders (dominant) ○ All you need is 1 gene from 1 parent - Conditions are very rare but commonly expressed - Examples: ○ Achondroplastic Dwarfism ○ Polydactyly ○ Huntington's Disease▪ Autosomal Dominant Nieman-Pick Disease Patho Page 104 ○ Nieman-Pick Disease ▪ Autosomal Recessive ○ Color Blindness: ▪ Sex-linked traits □ More males are affected than females Neurologic SystemStroke- Vascular event that injures brain tissue causing acute-FOCAL neuro deficit ○ Deficits match the territory effected - 4th leading cause of morbidity & mortality - Hemorrhagic Strokes○ Least common but most frequently fatal ○ Spontaneous rupture of cerebral vessel causing hematoma ○ AGE & HTN are MOST COMMON risk factors ○ Etiology▪ Arteriovenous Malformations□ Development in utero of abnormalities in vascular bundles of AV unions □ These can rupture ▪ Trauma ▪ Aneurysm ▪ Drugs (cocaine abuse) ▪ Coagulation disorders ○ Symptoms▪ Sudden SEVERE SEVERE HA at onset □ "worst HA of my life" □ Due to the subarachnoid hemorrhage ▪ Vomiting (increased ICP) ○ Treatment▪ Limit the spread of hematoma ▪ Manage Intracranial Pressure ▪ Surgery□ Resect AVM □ Clip aneurysms ▪ Interventional Radiology- endovascular coiling walls off aneurysm - Ischemic Strokes○ Most common type of CVA ○ Results from obstruction of blood flow d/t thrombosis or emboli ▪ Thrombotic stroke□ Atherosclerotic plaques develop near cerebral vessel bifurcations □ Damage to the vessel wall results in buildup of a clot □ DIABETES & HTN are huge risk factors ▪ Embolic□ Moving clot that migrates to cerebral vessels (most common MCA) □ Cardiac risk factors are most common (A-fib, MI, endocarditis, etc.) ○ Risk Factors▪ FHx ▪ HTN ▪ Obesity ▪ Smoking ▪ A-fib ▪ CKD ○ Transient Ischemic Attacks- --------------------------------------------------------------------------------------> ▪ "Mini-Strokes" ▪ Brief episodes of ischemia w/o infarction ▪ Same as Ischemic Stroke but only PARTIAL blockage ▪ Serve as a warning sign of future stroke □ Most people have stroke w/in 3 mos of TIA - Diagnosis of CVA○ EARLY DETECTION!!!! "Temporarily Reduced Function" ▪ FAST □ Face droop □ Arms drop □ Speech slurred □ Time = 3 hour TPA window ○ Confirm neurological deficits by: ▪ Head CT w/o contrast ▪ Neurological exam - Treatment○ Administer TPA (tissue plasminogen activator)▪ MUST R/O HEMORRHAGIC STROKE FIRST ▪ Need to be given w/in 3 hours of onset of symptoms ○ Salvage brain tissue ○ Prevent secondary strokes ▪ ID risk factors, educate, etc. ○ Minimize long-term disability ▪ Rehab, etc. - Impact of Stroke Location○ Effects are obvious on the OPPOSITE side of the brain ▪ R side CVA = L sided weakness ○ Deficits manifest based on the location of the CVA -------------------------------------------------------> - Nursing Considerations Post CVA- Patho Page 105 - Impact of Stroke Location○ Effects are obvious on the OPPOSITE side of the brain ▪ R side CVA = L sided weakness ○ Deficits manifest based on the location of the CVA -------------------------------------------------------> - Nursing Considerations Post CVA○ Get them mobile w/in 24 hours to prevent further blood clots ○ Assess ADL's ▪ Consult w/ rehab ○ Orient yourself to the non-affected side ▪ Ensures they can hear/see/interact with you ○ Include the family/caregivers in the education - Post Stroke Care○ Risk of recurrence is highest in the first week ○ Admin antiplatelets ○ Reduce modifiable risk factors ▪ HTN, DM management, smoking cessation, etc. ○ Treat underlying medical conditions ○ Consult w/ rehab to build on deficits▪ Motor, language, sensory, cognitive ▪ Dysarthria ▪ Dysphagia ▪ Fine motor skill deficits ▪ Inability to perform ADL's Dementia- Umbrella term that includes: ○ Alzheimer's ○ Lewy body dementia ○ Parkinson's ○ Vascular ○ Etc. - Incidence is increasing as the population ages - Cognitive decline in areas of the brain w/ cognition and memory - Diagnosis○ Based on presenting problem ○ History ○ Neuro exam ○ Brain imaging ○ Behavioral/cognitive functioning - Need to r/o reversible causes of memory loss & cognitive decline -----------------------> ○ Acute infection, trauma, drugs, emotional, etc. - Diagnosing○ Requires 2 components▪ Decline in memory ▪ Decline in at least 1/4 cognitive functions□ Language comprehension / speech □ Process & interpret visual information □ Planning, sound judgements, abstract thought □ Motor functioning - Treating○ Treat underlying causes that can reverse it ▪ B12 deficiency ▪ Hypothyroidism ▪ Drug toxicity ▪ Tumors ○ Treat problematic behaviors▪ Agitation ▪ Sleep disorders ▪ Wandering ▪ Sundowner's Syndrome- in the evening = higher incidence of agitation, confusion, Alzheimer's Disease- Risk increases w/ age - Slow, progressive dementia w/ subtle onset of memory loss - Patho○ Caused by accumulation of amyloid beta peptides ▪ Cause a chain reaction of physical changes to the brain tissue ▪ Axons become entangled □ Prevents communication of these cells and causes cell death ○ Microscopic exam shows Neuritic Plaques, degenerated & tangled axons ○ MRI shows atrophy of cerebral cortex & ventricle enlargement -----------------------------> - Stages of Alzheimer's○ Early▪ Lasts 2-4 years ▪ Short term memory loss ▪ Random detail loss ▪ Personality changes ○ Moderate▪ Lasts 2-10 years ▪ More cognitive impairment ▪ Language deficits ▪ Depression ▪ Unable to perform self-care Severe- Patho Page 106 ○ Severe▪ Lasts 1-3 years ▪ Loss of ability to respond to their environment ▪ Total dependent care needed ▪ Bed ridden ▪ Death - Treatment○ Many medications for Alzheimer's ▪ Aim to decrease Acetylcholine breakdown and preventing the formation of those plaques ○ Can cause N/V, loss of appetite, weakness, etc. - Nursing Considerations○ Biopsychosocial disorder ▪ Affects every aspect of them and their family's life ○ Focus on the things they CAN DO! ○ Support the caregivers ○ Utilize community resources for pt and caregivers Migraine- Men > women - Incidence decrease by Age 50 - Symptoms○ Can have aura or no aura FAMILY HX ▪ Majority of migraines DO NOT have aura - Genetic predisposition > w/ aura than w/o aura ○ SEVERE, pulsatile, throbbing UNILATERAL pain ○ Last about 4-72 hours ▪ Migraines lasting longer than 72 hours = STATUS MIGRANOSIS □ This is a MEDICAL EMERGENCY ○ Aggravated by physical activity ○ Sensitivity to light/sound/smell ○ Visual disturbances ○ N/V - Aura○ Can last from 5 min to 1 hour & develop over 5-20 minutes ○ Precedes migraine ▪ Can have prodromal symptoms days before: □ Fatigue □ Irritability ○ Speech disturbances - Patho○ Hyper-activation of the Trigeminal V ▪ d/t hypersensitivity to environmental stimuli □ Allergies, light, caffeine, etc. ○ Release prostaglandins & other substances that results in vasodilation ▪ Results in Neurogenic Inflammation ▪ Stims the nociceptors and manifests as throbbing pain ○ NSAIDS can prevent prostaglandins and prevent migraines from progressing - Triggers○ Stress ○ Sleep deprivation ○ Alcohol ○ Foods (MSG, cheese, chocolate) ○ Visual stimulation ○ Estrogen ▪ Migraines coincide w/ menstrual cycle ▪ Most migraines (75-80%) go away after pregnancy - Phases○ Prodromal▪ Hrs to days before ▪ Energetic/excitable or depressed/ irritable ▪ Thirsty, cravings ▪ Tired, increased urination ○ Aura▪ Not always present ▪ Flickering lights ▪ Tingling ▪ Speech disturbances ○ Attack▪ Acute phase of the migraine lasting from 4-72 hours ▪ Varies in location ▪ Throbbing pain □ Worsened w/ activity ▪ Sensitivity to light, sound, smells ▪ N/V, syncope, light-headedness ○ Post-dromal▪ Extreme tiredness/Sluggish ▪ Confusion ▪ Head pain exacerbated w/ bending over - Treatment○ Acute (during)▪ Aim to alleviate symptoms ○ Acute Non-responder Care▪ For those that don't respond w/ first treatment ▪ 10 mg IV Reglan (metoclopramide) Patho Page 107 ▪ 10 mg IV Reglan (metoclopramide) □ Relieves nausea & helps w/ absorption of other meds ○ Prophylactic Treatment▪ Use if migraines occur 2-3x per month or migraines are debilitating ▪ Taken daily for months/years ▪ Beta-blockers (propranolol) & anti-seizure meds & anti-depressants ○ Pharmacologic Treatment▪ Non narcotics used for mild-mod pain (best taken early) □ NSAIDS - prevent prostaglandin synthesis ▪ Triptans- (Maxalt = Rizatriptan) □ 1st line defense □ Increase serotonin and promote vasoconstriction ▪ Narcotics- For severe HA □ Ex: Norco/Vicodin ▪ Other□ Midrin (isometheptene) = vasoconstriction □ Ergotamines w/ caffeine = vasoconstriction ○ Non Pharmacologic Treatment▪ Control risk factors & triggers ▪ Behavior interventions□ Stress manage □ Relaxation therapy □ Biofeedback □ Cognitive therapy - Nursing considerations○ Non-oral meds useful for sudden onset HA and N/V (IV Reglan/metoclopramide) ○ Frequent use of acute therapies can cause rebound HA ○ Triptans should be avoided in pt w/ CAD ▪ Causes coronary spasm ○ Ergotamines CONTRAINDICATED in pregnants (uterine contractions) Seizures- Result from abnormal/excessive firing from a group of neurons in the brain ○ Results from alteration of permeability and redistribution of ions and neurotransmitters ▪ AKA… there's a CHEMICAL IMBALANCE in the brain - Signs & Symptoms○ Depend on the type of neurons that are hyperactive ○ Sensory, motor, autonomic, psychic (De Ja Vu, anxiety) - Types○ Provoked▪ Secondary seizures caused by something else □ Infection □ Brain injury □ Drug abuse ○ Unprovoked ▪ Primary/epileptic seizures ▪ Idiopathic ▪ Focal seizures or Generalized Seizures - Provoked Seizures○ Most common = Febrile Seizures ▪ Seizures in children □ 6 mos & 5 yrs ▪ Temp above 104 not related to another metabolic disorder ○ Etiologies▪ Electrolyte imbalances (hyponatremia) ▪ Eclampsia ▪ Hypoxia ▪ Hypoglycemia ▪ Tumors ▪ Meningitis - Unprovoked (Epileptic Seizures)○ Focal Seizure WITHOUT Impairment of Consciousness▪ Begin in 1 part of the brain (localized) ▪ Symptoms□ Aura □ Involuntary muscle movements □ Sensory disturbances □ ANS stimulation (tachycardic, diaphoretic, pupillary changes, etc.) ○ Focal Seizure WITH Impairment of Consciousness▪ Occur in temporal lobe □ Begins UNILATERALLY and can spread to both ▪ Psychomotor symptoms- automatisms/repetitive activities ---------------------------> First ever Seizure Pt in EMU □ Lip smacking □ Patting □ Rubbing clothing □ déjà vu, hallucinations, etc. - Can be confused w/ psychiatric disorders ▪ Postictal Confusion is common ○ Generalized Seizures▪ Generalized = includes both hemispheres of brain at onset ▪ Tonic- stiffening of extremities w/ contractions ▪ Clonic- contractures and relaxations w/ hyperventilation ▪ Tonic Clonic (grand mal) = MOST COMMON □ Generalized seizure w/ extension of extremities w/ LOC Patho Page 108 □ Generalized seizure w/ extension of extremities w/ LOC □ Loss of bladder/bowel control □ Clonic rhythmic contractions & relaxation of extremities ▪ Absence (Petit mal) □ Only in children □ Non-convulsive □ Unresponsive □ Blank stare ▪ Myoclonic□ Brief, involuntary muscle contractions w/o strong extension (tonic) □ Limited to the face, trunk, or extremities ▪ Atonic- "drop attacks" = Caroline = sudden loss of muscle tone ▪ All generalized seizures can be followed by Todd's Paralysis□ Temporary paresis (weakness), aphasia, or hemianopia □ Lasts up to 24 hours - Status Epilepticus○ THIS IS A MEDICAL EMERGENCY ▪ STATUS EPILEPTICUS in Tonic-Clonic Seizures can lead to respiratory failure & death ○ When seizures don't stop after 5 minutes or happen back-to-back w/ no recovery ○ Can occur w/ all generalized seizures ○ Most common in Elderly & Children ○ Treat the underlying cause ▪ Abrupt withdrawal of anti-epileptic drugs ▪ Alcohol withdrawal ▪ Acute neurological illness (meningitis) ▪ Metabolic disorders (hypernatremia, etc.) ▪ Stroke ○ Life support measures & admin meds ▪ Secure an airway!!! ▪ Ativan, Cerebyx, Keppra, Phenobarbital, Propofol, Versed, Ketamine ------------------------------> - Treatment○ Pharmacological▪ Suppress the hyperactive neurons or inhibit transmission of electrical impulses ▪ Benzodiazepines ▪ More than 20 different types of drugs □ Important to limit number of drugs to 1!!! □ These drugs can interact w/ OCP's, affect fertility, and cause birth defects ▪ 65% of pt don't fully respond to anti-epileptic drugs ○ Non-Pharmacological▪ MRI's & EEG's to diagnose □ EEG's are the GOLD STANDARD ▪ Surgery if medications continue to fail ▪ Neurostimulation of Vagal Nerve ▪ Diet modification□ Ketogenic diet = induce ketosis to help prevent seizures Multiple Sclerosis- Autoimmune disorder○ Inflammation and destruction of myelin in the CNS Pregnancy can cause relapse - Progressive, degenerative disorder - Genetic and environmental (smoking, low vitamin D) risk factors ○ Women 2x > Men - Symptoms dependent on location of lesions/plaques formed by broken down myelin ○ Visual changes ○ Speech deficits ○ Muscle weakness ○ Gait issues ○ Depression = 30-50% ▪ d/t impaired fxn - Diagnose ○ MRI ○ Neuro exam ○ Charcot's Neurologic Triad▪ Nystagmus ▪ Intentional tremors ▪ Staccato speech - Treatment○ Treat acute attacks w/ corticosteroids ○ Modify the course of the disease ▪ Interferon B□ Immune booster ▪ Glatiramer Acetate□ Mimics myelin so the body destroys it instead of the actual myelin ○ Treat symptoms ▪ Pain ▪ Fatigue ▪ Depression ▪ Bowel/Bladder dysfunction ▪ Constipation ▪ Tremors Pain- Patho Page 109 Constipation ▪ Tremors PainNerve Fibers- See figure ---------------------------------------------------------------------------------------------------> - A Fibers○ Large, myelinated, Fast, sharp pain ○ Release of glutamate at the synapse with the spinal neurons ○ ASSOCIATED WITH ACUTE PAIN - C Fiber○ Small, nonmyelinated = chronic, slow pain ○ Release glutamate and substance P Pain Mechanisms- Nociceptive Pain○ Initiated by nociceptors in peripheral tissues when there is damage - Neuropathic Pain○ Direct injury or dysfunction of the sensory axons or peripheral/central nerves - Pain threshold○ The amount of stimulus required to elicit a pain response ○ The point at which the nociceptive stimulus is perceived as painful - Pain tolerance○ Maximum intensity/duration of pain that a person is willing to endure before seeking intervention ○ Can't take it anymore! Types of Pain- Cutaneous pain ○ Skin, or sub q tissues (papercuts) ○ Easily localized pain ○ Sharp pain with burning qualities ▪ Can be abrupt or slow onset - Deep somatic ○ Bones, muscles, tendons, joints ○ More diffuse/radiating pain - Visceral ○ Visceral organs ○ One of the most common pains from disease (upset stomach, etc.) - Referred ○ Originates in another place then diffuses to another place where it is perceived Acute Pain vs. Chronic Pain- Acute Pain○ Short-lived, and is resolved when the underlying cause is resolved ("self-limiting") ▪ Initiated by trauma, injury, surgery by activation of nociceptors ○ Initial injury causes nociceptive firing (hyperalgesia), and then a secondary wave of intense acute pain results from secondary responses (inflammation, edema, etc.) ▪ This secondary hyperalgesia can result in the development of chronic pain if not treated properly ○ Treat acute pain preemptively (before it gets too severe) ▪ Increases comfort of the pt and also prevents hypersensitivity of pain centers in the periphery and CNS ▪ Also requires the use of less drugs if treated preemptively - Chronic Pain○ Pain that lasts longer than what is reasonably expected ▪ Pain is sustained by factors that are remote from the initial cause of the pain ○ Most common cause of chronic pain = cancer ○ Highly variable b/w pts▪ Can be unrelenting extreme pain (metastatic bone pain) ▪ Or… continuous w/ periods of escalation (back pain) ○ Serves no protective purpose and interferes w/ QOL & ADL's ▪ Nociceptors are persistently stimulated serving no useful protective purpose ○ Causes psychological, physiological, familial, and economical stress ○ Different Levels of Chronic Pain Sensations▪ Peripheral- (Peripheral Sensitization) □ Persistent stimulation of the peripheral nociceptors □ Inflammatory response increases the sensitivity of the C -Fibers ▪ Peripheral-Central□ Abnormal function of the peripheral and central systems □ Results from destruction of descending-inhibitory pathways (endogenous opioids) and the hyperexcitability/continuous firing of new nociceptors □ Ex: PHANTOM LIMB PAIN ▪ Central□ Due to a disease, injury, lesion of the CNS □ Ex: Multiple Sclerosis ○ Management of chronic pain is a COMPLEX PROCESS: ▪ Depends on a lot of factors□ Cause of the pain □ Underlying health problem □ Life expectancy of the individual ○ Best managed by a multidisciplinary team ▪ Anesthesiology, physicians, nurses, PT, surgeons, case management, etc. Patho Page 110 Inflammation and InfectionInflammation- Reaction of vascularized tissue in response to cell injury/death - Results in○ Increase in inflammatory mediators ○ Movement of fluid and leukocytes from the vascular system to the extravascular tissue ▪ Results in swelling - Inflammatory conditions (-itis) ○ Appendicitis ○ Neuritis - of the nerves ▪ Indicates the body response to an injury/damage/or ischemia Acute Inflammation- Two Stages of Acute Inflammation ○ Vascular stage▪ Increased blood flow (vasodilation, decreased venous return) ▪ Increased vascular permeability □ There is more plasma entering the tissues and leads to edema □ Plasma contains substances that help the tissue heal - Clotting factors help stop bleed and prevent the spread of infection - Antibodies are help to fight infection - Nutrients help feed tissue cells and proteins ○ Cellular Responses▪ Movement of phagocytic leukocytes (mainly neutrophils) from the blood to the injured area □ Margination- slowing of the blood leads to accumulation of WBC □ Transmigration- WBC leave the vessels through the endothelium □ Chemotaxis- WBC follow the chemical trail to get to the site of injury/infection □ Phagocytosis- neutrophils, monocytes, and macrophages are activated and engulf/destroy the microbe/tissues/etc. CARDINAL SIGNS OF INFLAMMATION- All occurs during acute inflammation ○ Happens w/in minutes-hours ○ Acute inflammation is self-limited… ▪ When the cause of inflammation goes away, so does the inflammation - Rubor (redness)- due to vasodilation in the vascular phase - Heat- occurs due to vasodilation in the vascular phase - Swelling- increased fluid in IS space in the vascular phase - Pain- increased fluid in IS space in vascular phase - Loss/Alteration of Function- increased fluid in IS space in the vascular phase Chronic Inflammation- Can last from weeks to years - Etiology○ Low grade inflammation conditions ▪ Obesity ▪ Type II Diabetes ○ Inappropriate activation of immune system (autoimmune disorders) ▪ RA, IBS, Lupus, etc. ○ Persistent infxn - Chronic inflammation results in an increased risk of developing cancer ○ Due to the long term damage to DNA - Usually begins gradually as a low grade fever, etc. that is ASYMPTOMATIC ○ Over time the effects will start to manifest ▪ You may not even know you have chronic inflammation for a long-long time ○ Ex: Lupus, RA, IBS, etc. Know the differences b/w chronic & acute -------------------------------------------------------------------> Fever- Most prominent sign of inflammation - Systemic symptom caused by PYROGENS (released from the WBC) ○ Promotes a hostile environment for pathogens - Four Types○ SEE FIGURE ------------------------------------------------------------------------------> ○ Intermittent Fever▪ Fever spikes and return to normal at least once per 24 hrs ○ Remittent Fever▪ Doesn't return to normal level ▪ Varies just a few degrees in either direction (up/down) ▪ Ex: UTI ○ Sustained Fever▪ Temp stays above normal w/ very little variation □ (usually sustained with <1 degree variability) ▪ Ex: Drug Rxns, hypermetabolic fever ○ Relapsing Fever▪ Episodes of fever that occur days apart from each other ▪ Ex: malaria, Lyme Disease, TB Chain of Infection**NEED ALL OF THESE COMPONENTS TO HAVE AN INFXN Patho Page 111 **NEED ALL OF THESE COMPONENTS TO HAVE AN INFXN - Reservoir○ Natural habitat of the pathogen (humans, food, environment, etc.) ○ Humans can be reservoirs and be asymptomatic (HIV) ▪ Can still spread the disease - Portal of Exit○ Point of escape from the reservoir ○ Respiratory tract, GIT, UT, skin - Means of Transmission○ Transmitting from reservoir to new host ○ Direct contact, droplet, aerosol ▪ Proper hand hygiene/gloving can interrupt the means of transmission - Portal of Entry○ Where the org enters a new host ○ Must find a portal of entry or the org will die ○ Entry route can be the same as the exit route ○ Respiratory, GIT, UT, skin = most common portals of entry - Host Susceptibility○ Host must be susceptible and the org must be able to overcome host defenses Transmission Methods- Direct ○ Close contact (sex, kissing, etc.) ○ Congenital = mom to baby - Indirect = ingestion/inhalation Stages of infectious disease- Incubation○ Pathogen begins replication ○ No recognizable symptoms in the host ○ Can vary in length (hours to months) - Prodromal○ Initial appearance of NONSPECIFIC symptoms ▪ Mild fever, muscle aches, HA, fatigue ○ Person is most contagious in this phase - Acute○ When the host experiences the max impact of infxn ○ Symptoms very specific, pronounced, ▪ Blisters/rash/itching/etc. in Chickenpox - Convalescent○ Containment of the infxn ○ Elimination of the pathogen ○ Repair damaged tissue ○ Symptoms resolve ○ Time varies on the pathogen and the pt immune response - Resolution○ Totally eliminate the pathogen ○ No residual sxs Clinical Manifestations- Symptoms- outward expression of the immune response and the invading organism Specific Reflect the site of infection Nonspecific Shared w/ number of disease (fever, HA) Obvious Chicken pox symptoms are obvious Covert Discrete.. Requires further testing (LAB WORK) to determine infection (Increased WBC count) Cardiovascular- KNOW YOUR FCKIN PHYSIOLOGY **Go back and quickly breeze over the whole section from Exam 3** Infective Endocarditis- Relatively rare but with significant mortality - May evolve over years/months or very quickly - Risk Factors○ Strep throat- Under- treated as a child ▪ AKA the abx therapy is unfinished ○ Drug abuse ○ Congenital heart defects ○ Mitral valve prolapse - Etiology○ Streptococcal with childhood strep ○ Congenital disorders ○ Staph infections in drug abusers ○ Other bacterial, fungal infxn - Patho○ Vegetative lesions form on the valves ▪ Release bacteria into bloodstream ▪ Lesions break off and form an obstruction ○ The lesions grow larger, weigh down the valves and cause: ▪ Regurgitation ▪ Stenosis Patho Page 112 ▪ Stenosis - Signs and Symptoms○ Fever, cough, dyspnea ○ New heart murmur develops when they're older adults ○ Petechieae, splinter hemorrhage (due to obstruction in small vessels) - Treatment○ Must diagnose with blood cultures ○ IV antibiotics for six weeks (a million units of penicillin Q2H intradermal) ▪ High doses of Abx lead to other microbes growing □ Primarily vaginal FUNGAL INFXN □ C. diff, etc. ○ Prophylaxis with certain procedures ○ Valvular replacement may be necessary Arterial Diseases of the Extremities - Peripheral vascular disease (PVD) - Assessment ○ Monitoring capillary refill time ○ Peripheral pulses (strength) ○ Auscultation to hear a bruit ○ Doppler ultrasound Arteriosclerotic Occlusive Disease- also called arteriosclerosis obliterans - Most commonly called (arterial insufficiency) - Symptoms○ Intermittent claudication with walking (gastrocnemius muscle has highest O2 consumption) ○ Cool temperature ○ Limb color blanches with elevation and becomes deep red when leg is in dependent position ▪ Due to autoregulatory increases in blood flow and Increase in gravitational pressure ○ Pain becomes more severe at rest (rest pain) and leg must be lowered to gain relief. ▪ This action increases peripheral perfusion to the area. ○ Diminished or absent peripheral pulses ○ Loss of hair on toes, feet, nails thickened and ridged ○ Arterial ulcers ▪ Very painful, deep, and circular ▪ Tend to be on tips of toes, heel or other pressure areas ▪ Arterial ulcers are CLEAN - but deep and painful ▪ Venous ulcers = gross, jagged edges, purulent ○ Edema is minimal unless kept in dependent position to minimize pain - Treatment ○ Femoropopiteal (Fem-Pop) Bypass graft surgery▪ Use saphenous vein to bypass the occluded area ○ Walking to point of claudication to develop collateral circulation ○ Stop smoking▪ Absolutely necessary!!!!!! THIS IS FOUNDATIONAL TO TREATING ○ Control diabetes mellitus ▪ DM is the #1 CAUSE OF ARTERIAL INSUFFICIENCY Arterial vs Venous Insufficiency - Both may commonly occur simultaneously - Arterial pain is intermittent claudication while venous pain is aching - Arterial -pulses absent; Venous- present - Arterial ulcers are painful while venous ones aren’t if superficial - Arterial ulcers have a black base while venous are beefy red to yellow - Arterial- edema is minimal while in venous edema is moderate to severe (non-pitting) Myocardial Infarction- Death (necrosis) of cardiac tissue due to prolonged ischemia lasting about 20-40 minutes ○ Necrosis = death ○ Ischemia = lack of O2 - Number one killer of Americans - Patho○ Atherosclerotic plaque disrupts circulation and….. ▪ Blood vessel ruptures …or… ▪ Acute coronary thrombosis occurs ○ Three zones of myocardial damage▪ Necrosis□ Inner zone of dead tissue that was ISCHEMIC for 20-40 min □ Cannot be regenerated - Will become scar tissue and won't contract □ Pathological Q wave (more pronounced than in the QRS complex) ▪ Area of Injury□ Cells will die if the ischemia is not stopped IMMEDIATELY - Cells can be saved but won't be strong as before □ Elevated S wave from baseline - The higher the S wave, the worse the injury ▪ Ischemia□ Cells usually doesn't die… □ Can recover fully and work like normal ○ Necrotic areas are cleaned out by macrophages over the next 48 hours ▪ Results in increased Temperature d/t inflammatory process ▪ In about 10 days scar tissue begins forming and is complete in 7 weeks ▪ Scar areas cannot contract or conduct action potentials Patho Page 113 - - - - ▪ Scar areas cannot contract or conduct action potentials □ Seen as "bundle branch blockage" as seen via changes in EKG Signs and Symptoms○ Acute chest pain ▪ Classically radiates to the left arm ▪ Not relieved by Rest or Nitroglycerin (unstable angina) ○ EKG changes ▪ ST elevation ▪ Pathological Q wave ▪ Dysrhythmias (PVC’s) ○ Nausea and vomiting (d/t chest pain) ○ Weakness ○ Pale, cool skin ○ Fever and leukocytosis ○ ESR rises ○ Dyspnea ○ Symptoms of cardiogenic shock with renal shutdown ▪ HIGH % of cardiogenic shock pt will die Diagnosis of MI ○ 12 lead EKG-▪ Pathologic Q wave ▪ ST elevation ○ Enzymes (Bio-Markers)▪ These enzymes are released from dead cells due to necrosis □ You can measure these markers to assess the extent of the necrosis □ The higher the enzyme levels the greater the damage ▪ Elevated Troponin levels □ Troponin > 1 is positive in 1-2 hours - Less than 1 is normal ▪ CK-MB rises □ Sign of muscle metabolism □ CK-MB- heart, 6-8 hrs - CK-MM- skeletal muscle - CK-BB-Brain - CK-MB - cardiac □ CK-MB begins rising in 6-8 hours Location of Myocardial Infarction ○ Depends on which arteries are occluded, ▪ e.g. posterior MI, anterior MI, anterolateral ○ LAD occlusion- is the worst prognosis for immediate death Treatment○ TPA = dissolves the clot ○ Aspirin and other anti-platelet aggregator ○ Heparin - anticoagulant… ▪ Doesn't dissolve current clots but prevents new one ○ Anti-dysrhythmics ○ Beta blockers (decrease HTN) ▪ Works on the ACE enzyme in the RAAS ○ Calcium channel blockers ▪ Decrease BP ○ Nitroglycerine IV ▪ Chest pain and vasodilation (decrease BP) ○ Morphine = chest pain ○ Valium = anxiety ○ Stent to keep artery open ○ PTCA ○ CABG ○ Lifestyle modification education Gastrointestinal, Biliary, Hepatic, etc.- **Section Headers are Highlighted in Yellow Above** Acute pancreatitis GERD C diff Peptic ulcer disease Cholecystitis Hepatitis Diverticulitis Ulcerative colitis ○ Curling's Ulcer StressHormones and the Stress Response (neuroendocrine response)- All of the responses of stress are strongly influenced by the neuroendocrine system ○ These responses result in increased energy for the body to use in the Fight/Flight response - Cortisol = INCREASED RISK OF INFXN Norepinephrine & Epinephrine: - Origin: Locus ceruleus, adrenal medulla - These are the catecholamines - FunctionPatho Page 114 Unstable Angina (Pre-infarction Angina)- Symptoms of chest pain occurring at rest; ○ Prolonged chest pain >15-20 minutes and non-predictable ○ Pain is persistent in UNSTABLE ANGINA even w/ Nitro - Patho: ○ Probably triggered by changes to the unstable Plaque ○ Plaque is changing in nature/shape/form - Treatment of Unstable Angina ○ THIS IS A MEDICAL EMERGENCY ○ Cardiac Catheterization ○ 12 lead (direction) EKG ▪ ST depression ▪ T wave inversion ○ Rx: ▪ IV nitroglycerine to relieve pain □ This is the only Med that might stop the pain ▪ Antiplatelet drugs (aspirin, Plavix) ▪ Calcium channel blockers (-edepines) ▪ TPA instantly dissolves the clots ○ Percutaneous Transluminal Coronary Angioplasty (PTCA or PCI) ○ Stents to keep vessel open ○ CABG will have to be done if stents are ineffective Norepinephrine & Epinephrine: - Origin: Locus ceruleus, adrenal medulla - These are the catecholamines - Function○ Decrease insulin release ○ Increase in glucagon release ▪ Results in elevated blood sugar levels ○ Increase HR, cardiac contractions, ○ Bronchodilation Corticotropin Releasing Hormone- In the hypothalamus - CRH essential in the endocrine component of the neuroendocrine response - Stimulates ACTH to release from the anterior pituitary - Increases ANS activity in the locus ceruleus - CRH acts on the anterior pituitary therefore reproductive processes are affected by this ACTH- Anterior pituitary - Stims the synthesis and release of cortisol from Adrenal Cortex Cortisol- Adrenal cortex - Known as the stress hormone ○ Regulates the stress response - Potentiates the actions of epi and glucagon - Inhibits reproductive hormones and TSH's ○ These are not necessary in times of stress - Produces increased risk of infxn (Decreased immune activity) and decreased inflammation - Increases blood glucose for energy for the body ○ Can help maintain glucose levels and enhances the effects of the catecholamines Aldosterone- Adrenal cortex - Increases sodium reabsorption in the kidneys ○ Water follows salt = increased BP/Blood volume etc. ADH- Also called vasopressin - Hypothalamus, posterior pituitary - Actions○ Increases water reabsorb in kidneys ○ Causes vasoconstriction ○ Stimulates the release of ACTH ▪ Particularly in response to stress/hypotension/fluid volume loss/hemorrhage □ Extreme stress!!! Autonomic Nervous System- Regulates BP, GIT responses to food, focusing eye, thermoreg., etc. - Know the difference b/w sympathetic (fight or flight responses - prepares the body for strenuous physical activity) & parasympathetic (rest & digest - person sitting quietly, resting) Sympathetic Response Parasympathetic Response Dilation pupil Decreased salivation Increased HR & BP Vasoconstriction Pupil constriction Increase salivation Decreased HR Arterial vasodilation Bladder relaxes to fill with urine & NOT PEE!!! Bronchodilation Decrease GIT motility Bladder relaxation Increased GIT motility Bladder constricts to void (parasympathetic) Bladder constriction RespiratoryPneumonia- Inflammatory rxn in the alveoli & interstitial tissue of the lung from a pathogen - 6th leading COD (mostly in elderly) - Frequent complication of Flu & Immunocompromised - Categories of Pneumonia○ Type of Agent▪ Typical = bacteria ▪ Atypical = mycoplasmas or viruses d/t disease condition of lungs (stasis of mucous) ○ Distribution w/in lungs▪ Lobular Pneumonia ▪ Broncho-pneumonia ○ Setting▪ HAI □ Pseudomonas aeruginosa, S. aureus, E. coli □ Medicare doesn't cover health care costs of HAI's ▪ Community Acquired- Patho Page 115 PNEUMONIA = INFLAMMATION ▪ Community Acquired□ Influenza, S. aureus, Mycoplasma pneumoniae, Chlamydia □ Must be Dx w/in 48 hrs of admission □ Pt must not have lived in long-term facility w/in 14 days prior to admit - Patho○ Microbial agents multiply & cause inflammation ▪ Alveolar spaces fill w/ exudate/mucous □ Exudate can solidify and become difficult to expectorate ○ Creates less surface area for gas exchange (results in hypoxemia) - Dx○ Sputum culture & sensitivity ○ Symptomatology ○ CHEST XR Pneumococcal Pneumonia- S. pneumoniae = most common cause of bacterial pneumonia - 4 stages of the disease - Signs & Symptoms○ Fever, chills, malaise ▪ Elderly rarely run fevers!!! □ If they present w/ fever, the infxn is very severe □ Watch for signs of rapid mental deterioration ○ Productive cough ○ Bloody sputum (bloody or rust-tinged) - Rx with ANTIBIOTICS ○ Levofloxacin ○ Piperacillin ○ Cefotaxime ○ Vancomycin ○ Gentamycin - Primarily focus on PREVENTION ○ Pneumococcal vaccination (Elderly 65+ & for those 2+ & immunocompromised) ○ 2 vaccines: both vaccines recommended for elderly 65+ Tuberculosis- #1 COD from a SINGLE organism worldwide ○ Incidence has rapidly declined w/ vaccines but increased again with increase of HIV rates ▪ HIV is most associated w/ TB ○ Increased d/t immigration from countries w/ high incidence/prevalence - Mycobacterium tuberculosis ○ Spread by airborne droplets ▪ Aka… living in close-confined quarters - TB mostly effect lungs but can affect all organs ○ Best survives in oxygen rich environment - Patho○ Macrophages initiated a cell-mediated immune response ▪ Contains the infxn and calls on T-cells ▪ T-cells "approve" the macrophages to initiate cell-mediated response □ Release lytic enzymes and cells undergo apoptosis ▪ This results in the cheese-like appearance of lung tissue in Chest XR ▪ Lasts 3-6 weeks □ Indicates the pt is EXPOSED but they DON'T have ACTIVE TB □ Aka… the TB is walled off and not actively infecting more tissue ○ TB can be latent for a long period of time ▪ Becomes active when the immune mechanisms fail and the TB is released from the walled off protection - Symptoms○ Insidious & Non-specific symptoms ○ Cardinal Signs of TB: ▪ Night Sweats ▪ Weight loss ▪ Fever ▪ Cough □ Once TB spreads to the sputum, it can be transmitted to another person - Diagnosis○ PPD, Chest XR ○ Sputum Tests!!!! - Rx○ Multiple drug combinations are MANDATORY ▪ INH (isoniazid), Rifampin, Pyrazinamide, Ethambutol, Streptomycin for 6+ mos ○ Drug resistant TB is rare… Arterial Blood Gasses- Normal values: ○ pH = 7.35 - 7.45 ○ HCO2 = 22 - 31 ○ PCO2 = 35 - 45 mmHg (indicative of ventilation) ▪ Decrease in ventilation = increase in PCO2 ○ PO2 = 80 - 100 mmHg (indicative of perfusion) - Acid-Base Balance○ First determine Acid/Alkaline per pH level ○ Then determine if PCO2 or HCO3 is altered ▪ PCO2 abnormal = respiratory ▪ HCO3 abnormal = metabolic Patho Page 116 GHON Focus (walled off TB) FOR FUCK'S SAKE, TRENTON….. - a LOW PH = ACID - a HIGH PH = ALKALINE ▪ HCO3 abnormal = metabolic ▪ The "cause" is OPPOSITE of what is NORMAL Fluid & ElectrolytesInterstitial Fluid Exchange: - SEE THE FIGURE ------------------------------------------------------------------------------------------------> - Capillary filtration pressure pushing fluid out ○ Acting against in the interstitial space is "Tissue Hydrostatic Pressure" ○ If you have a lot of water in the IS space, it will push into the vascular space - Capillary colloidal (protein typically albumin) Osmotic Pressure pushing fluid back into the blood stream ○ Pulls water from IS space back into the capillary - Interstitial Pressure opposes the movement of water out of the capillary - ** remember pressure dynamics** ○ Arterial end higher pressure than venous end of capillaries ○ Know the exact numbers and how that relates to electrolytes/fluid balance in the capillaries ○ 120 mmHg in the LV and pushes the blood all the way to the caps. ▪ It is at its lowest point the Rt. Atrium Edema = sign of excess IS fluid - Most common in the feet and legs - Anaphylaxis = edema in the face, throat, eyes, etc. - Etiologies: ○ Increased Hydrostatic pressure ○ Lowered plasma oncotic pressures ▪ Due to decreased amounts of plasma proteins - albumin □ DECREASED CAPILLARY COLLOIDAL OSMOTIC PRESSURE REDUCES THE ABILITY TO SUCK FLUID FROM IS BACK INTO CAPILLARY ○ Increased capillary permeability ▪ Causes solutes to leave the capillary, increase the interstitial osmolality and draw more water in the interstitial spaces; thus causing edema ○ Lymphatic Channel Obstruction ▪ Can be caused by cancer or surgery Sodium- 135-145 Hyponatremia- More common than hypernatremia - Etiologies○ SIADH (increased water retention = dilutional hyponatremia) ○ Vomiting ○ Hypotonic irrigations (enemas) ○ Excessive water intake ○ Near drowning (freshwater) - Signs and Symptoms**most sxs. Are manifestations from the brain!!!*** ○ HA, confusion, lethargy, seizures, coma, death ▪ Neuro sxs ○ Muscle/abdominal cramping ○ N/V ○ Suppression of thirst reflex - Drugs can cause hyponatremia: ○ Diuretics!! ▪ Induces sodium loss to reduce water concentrations - Diagnosis: ○ Serum sodium level = below 135 ○ Serum osmolality below 280 ○ Urine Specific Gravity below 1.010 ○ Decreased Hct & plasma proteins (increased serum water content) - Tx: ○ Treat the underlying cause! ○ Fluid restriction ○ Oral or IV of saline solution (NS) ○ Eat high sodium foods ○ Severe: ▪ Neurological symptoms such as seizures (serum sodium <110) ▪ Treated with hypertonic solution (3-5%) to increase sodium levels and return to normal □ Too much treatment with hypertonic solution can cause a rapid shift of water out of the brain cells and cause permanent brain damage (Karev) Hypernatremia- Sodium levels above 145 mEq/L ○ Serum osmolality above 295 - Etiologies: ○ Tube feedings ▪ Some of the canned foods for tube feedings are high in sodium (need to dilute them) ○ Watery diarrhea ○ IV infusion of hypertonic solution ○ Near drowning (salt water) ○ Inability to respond to thirst ▪ They are relatively hypernatremic due to low fluid levels - Signs and Symptoms○ Thirst Oliguria (inability to form urine) Patho Page 117 ○ Oliguria (inability to form urine) ○ Decrease in skin turgor, salivation ○ Neuro sxs: ▪ HA, agitation, poor reflexes, seizures, coma, death - Assessment: ○ Drugs that cause: ▪ Antibiotics, anything with sodium bicarb, IV NaCl ○ Nursing functions: ▪ Monitor neuro status, seizures, etc. I&O, Vitals, Instruct to avoid high Na+ foods - Diagnoses: ○ Serum sodium above 145 ○ Serum osmolality above 295/300 ○ Urine specific gravity will be high (dehydrated) = 1.025+ - Treatment○ Treat the underlying CAUSE ○ Replace fluids, slowly and carefully ▪ Can be done orally or IV but gradually to avoid Cerebral Edema Potassium: - Normal value = 3.5-5.0 - Dietary Sources of K+ ○ Fruits (think bananas, oranges, etc.) ○ Meats ○ Vegetables Hypokalemia- K+ level below 3.5 - Etiologies: ○ Inadequate Dietary Intake: ▪ Anything that causes poor eating habits □ Anorexia □ NPO □ Unbalanced diet ○ Excess Renal, GI, Skin losses ▪ Potassium wasting diuretics (Lasix & thiazides) ▪ Diarrhea/emesis □ GI secretions are high in K+, therefore unusual wasting can cause hypokalemia - Signs and Symptoms○ Decreased urine specific gravity ▪ Less concentrated urine = lower Specific Gravity ○ GI, Neuromuscular, renal, & Cardiovascular systems are mostly effected ▪ Due to K+ acting on the electrical activity of excitable tissues □ HEART DYSRHYTHMIAS!! - Decreased T-wave ▪ Abdominal distention, CONSTIPATION, diminished bowel sounds (abnormal peristalsis) □ Due to the K+ deficiency acting on the bowels' contractility ▪ Muscle weakness, paralysis - Diagnoses: ○ Lab results ▪ Urine specific gravity ▪ K+ serum level ▪ Serum osmolality ○ Presence of sxs. (T-wave depression) - Treatment: ○ High K+ foods, oral supplements, or IV ▪ K+ must be diluted when given IV (or it will stop the heart) and also needs to be infused not pushed ○ Meds to help treat hypokalemia = K-Dur & IV Potassium Chloride Hyperkalemia- Serum potassium greater than 5.0 - Etiologies: ○ MOST COMMON CAUSE IS DECREASED RENAL FUNCTION ▪ The Kidney is unable to excrete potassium into urine like normal ○ Excess IV administration of K+ or excessive oral ingestion of supplements ○ K+ sparing diuretics (spironolactone) ○ Shift of K+ from intracellular to extracellular (ICF -> ECF) ▪ Crushing injuries, burns, etc. ▪ These types of injuries cause cell death and thus release of K+ into the ECF - Signs and Symptoms○ First symptom is paresthesia (numbness/tingling) ○ HEART DYSRHYTHMIAS ▪ Cardiac conduction is inhibited ▪ Shown through ELEVATED T-WAVES ○ Also GI sxs like in hypokalemia (N/V, intestinal cramping, DIARRHEA~!!!!) ○ Muscle weakness, and decreased neuromuscular excitability ▪ Remember that K+ messes up the electrical activity of the systems ▪ Dyspnea due to respiratory muscle weakness - Diagnosed by looking at lab values, medical history (renal failure, etc.), & EKG findings - Treatment: ○ Limit K+ foods, & sparing meds (spironolactone) ○ Needs something that will remove K from body ▪ Sodium polystyrene (Kaexalate) □ Resin drug that exchanges potassium for sodium, lowering the K+ level ▪ Calcium gluconate- Patho Page 118 Symptoms are like a "HANGOVER"!!! ▪ Calcium gluconate□ Calcium antagonizes the reduced membrane excitability caused by excess K+, and returns excitability/membrane potential to normal - Short-lived solution and thus combined with something that can reduce the ECF concentrations of K+ (insulin) □ Need to monito EKG for hypokalemia (flattened T-wave, etc.) ○ In severe cases, hemodialysis can be used for pt. with renal failure NeoplasmsCancer Stats!!! - #1 cancer = skin cancer ○ Lung Cancer = #1 Cancer COD for MEN & WOMEN - 76% cases are diagnosis after age 55 - Cancer 5 year survival rate = 65% - 2nd COD in USA - Cancer rates higher in males - Incidence & mortality rates are highest in Blacks - Survival of Cancer dependent on○ Poverty ○ Access to care ○ Poor health when diagnosed ○ Comorbidities ○ Differences in cell/tumor biology ○ Later staging of the cancer Incidence & Mortality- Most Common Incidences: ○ SKIN = most common site OVERALL ○ Prostate, Lung, Colorectal = most common site for MALES ○ Breast, Lung, Colorectal = most common site for FEMALES - Most Common Mortalities: ○ #1 COD in both sexes = LUNG CANCER ▪ Males = Lung, prostate, colorectal ▪ Females = Lung, breast, colorectal 6 Hallmarks of Cancer- Self-Sufficiency in emitting growth signals - Limitless replication potential - Insensitivity to regulatory signals - Evading apoptosis - Sustained angiogenesis - Tissue invasion / metastasis ○ Normal cells stop growing when they come into contact with other cells ○ Cancer cells continue to grow and "crowd out" normal cells Early Warning Signs- Unusual bleeding/discharge - Un-healing lesions - Change in bowel habits - Nagging cough / hoarseness - Lumps - Changes in moles/lesions - Dysphagia Symptoms of Most Solid Tumors- Anemia○ Decreased RBC level ○ Tumors is drawing up normal amount of blood and making the body anemic ○ Bone marrow suppression - Anorexia & Cachexia (muscle wasting) - Fatigue and sleep disorders - Compression/obstruction of tissues/organs - Pain (not usually an early symptom) ○ SEVERE PAIN is associated with LATE STAGES of Cancer - Psychosocial integrity & QOL The Cancer Development Process- See figure ----------------------------------------------------------------------------> - Dysplasia - IN SITU STAGE ○ Neoplasm confined to the original site and hasn't spread to surrounding tissue/organs ○ Early stage cancer ○ Malignant cells haven't crossed basement membrane ○ Usually can be surgically removed or treated ▪ It's in one location so it's easy to pluck out ▪ Very low chance of reoccurring □ "Cervical In Situ Cancer = 100% survival rate" - Invasive neoplasm Carcinogenesis- Process by which carcinogens cause normal cells to become cancer cells Carcinogens- (chemical, physical, biological) Patho Page 119 ○ Carcinogens- (chemical, physical, biological) ▪ Colon cancer can be caused by diets high in fats ▪ Diets high in nitrates = high incidence of cancer - Phases of Carcinogenesis-- understand them but don't go crazy -InitiationPromotionTransformationThe higher the amount of POORLY DIFFERENTIATED / UNDIFFERENTIATED Progressioncells = the worse the cancer! Cancer Patho- Genetic damages causes cells to mutate - Cell's revert from a differentiated state to an undifferentiated state - Proliferation of cells is continuous ○ Proliferation = time it takes for the tumor to double in size RenalNephrotic Syndrome- Caused by systemic diseases (DIABETES, lupus, etc.) - Signs & Symptoms○ Lots of protein in the urine ▪ Proteinuria = 3.5 g/day ▪ Hypoalbuminemia = <3 mg/dl ○ Fats in the urine (lipiduria) ○ Hyperlipidemia (high Triglycerides & LDL's) ▪ Results from the liver trying to increase Protein Synthesis ○ Generalized Edema / ascites ▪ Hypoalbuminemia results in decreased colloidal osmotic pressure ○ Dyspnea▪ Results from pulmonary edema & ascites pressing on diaphragm - Protein in the urine is ABSOLUTELY NOT NORMAL ○ Indicates extensive damage to the glomeruli ○ They are super leaky and are allowing proteins to seep out - Complications○ Loss of immunoglobulins (proteins) = increase r/o infxn ○ Increased r/o blood clots, CAD, HTN = loss of clotting factors ○ Anemia (loss of RBC) ○ AKI ---> CKD - Assess the 24 hours urine specimen ○ Pt uses restroom in the morning and the clock starts ▪ Flush… you don't want first sample ○ For the next 24 hrs, every urine sample needs to be collected and refrigerated ▪ Leaving urine out, it will culture and grow bacteria (not accurate) ○ Keep and collect the last urine specimen Patho of renal ?????? Patho Page 120