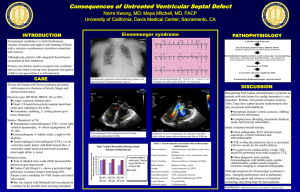
PEDS CARDIAC [SimpleNursing] Congenital Heart Defects Occurs before birth One or more problems within the heart structures changes the way the blood pumps through the heart and into the body - Decreased cardiac output meaning o Less oxygen rich blood goes OUT to the body Risk Factors of CHD: - Genetics: o Family hx of heart disease o Down syndrome - During pregnancy: o Mom develops infection (rubella) o Mom abuses drugs/alcohol o Diabetes Complications of CHD: - Hypoxia RIGHT to left blood flow: TOF, TGA o T – TROUBLE!! o T – TETRALOGY OF FALLOT [TOF] o T – TRANSPOSITION OF THE GREAT VESSELS [TGA] o T – TRUNCUS ARTERIOSUS o T – TRICUSPID ATRESIA - S/S of Hypoxia: o Cyanosis o Poor feeding & poor weight gain o Clubbing fingers o Dyspnea o Tachypnea o Polycythemia increase in red blood cells BLOOD CLOT RISK Report Hgb level over 22 Maintain adequate hydration* to reduce CVA - - CHF [Congestive Heart Failure] LEFT to right: ASD, VSD, PDA, AVSD o Holes in the heart septum that push blood from the LEFT side to the RIGHT side of the heart into the lungs, overloading lungs with TOO much blood flow o HF – heavy fluid o HF – heart failure S/S of CHF: o Weight gain bc of water gain Pale, cool extremities Periorbital Edema Puffiness around the eyes Reduction of number in wet diapers o Diaphoresis o Grunting during feedings Increased efforts on the heart during feeding o Dyspnea o Tachypnea + tachycardia o Poor weight gain [developmentally] Obstructive Defects Right to Left o TROUBLE!!, T+T+T Tetralogy of Fallot o P – Pulmonary Stenosis o R – Right Ventricular Hypertrophy o O – Overriding Aorta o V – VSD [Ventricular Septal Defect] - S/S of TOF: o “TET Spells” hypercyanotic spells *During a TET spell episode: 1. Infants: Knee to chest Older children: Squatting position Prevention of TET spell: 2. DO NOT interrupt sleep ; provide a calm quiet environment upon waking up 3. offer a pacifier during crying 4. small + frequent feedings 5 heart failure signs to report: 5. swaddle or hold the infant during procedures 1. Weight gain o Cyanosis 2. Periorbital edema o Hypoxemia 3. Pale, cool extremities o Clubbing fingernails 4. Reduction in # of wet diapers o Polycythemia = blood clot risk report to HCP if Hgb levels >22 - Treatment of TOF: o Surgical repair Transposition of the Great Vessels o Reversal of the 2 main arteries leaving the heart [pulmonary + aorta] - Treatment of TGA: o Surgical Repair Tricuspid Atresia o Closure of the Tricuspid valve ASD Atrial Septal Defect VSD Ventricular Septal Defect Blood from the RIGHT atrium can’t enter the RIGHT ventricle since tricuspid valve is closed; blood must flow through the hole connecting both atria and then get to the RIGHT ventricle through the VSD Truncus Arteriosus o Connection between the aorta + pulmonary artery + VSD Results in mixing of oxygen rich blood and oxygen poor blood Obstructive Defects Left to Right Blood is pushed from the LEFT side of the heart where its already oxygenated back to the RIGHT side of the heart [AKA Cardiac Shunt] Atrial Septal Defect KEY SIGNS of L to R Cardiac Shunts: *Hole between the Atria 1. Diaphoresis - S/S of ASD: 2. Heart murmur o Murmur 3. Poor weight gain This is normal and to be expected 4. Increased risk for HF + pulmonary HTN - Treatment of ASD: o Closes naturally, on its own o If it DOESN’T, then, surgical repair Ventricular Septal Defect *Hole between the Ventricles - S/S of VSD: o Grunting during feeding o Systolic heart murmur - Treatment of VSD: o Closes naturally o If it DOESN’T, then, surgical repair Patent Ductus Arteriosus *Opening that connects the Aorta to the Pulmonary Artery - S/S of PDA: o Loud machine-like murmur Sounds like a duck “DUCKtus” - Treatment of PDA: o Will close on its own within 48hrs of birth o For PREMATURE BABY: Indomethacin [NSAID] is given to close hole Surgical ligation AtrialVentricular Septal Defect AVSD *this is both ASD+VSD; 2 holes: Atria + Ventricles Typically seen in babies with DOWN SYNDROME Stenosis Stiff valve Stiff + Narrow Pulmonic Stenosis *Pulmonary valve is stiff, small, & narrow *Causes increased pressure and straining on the RIGHT side of the heart *Right ventricle tries to push blood through this tiny opening causing RIGHT ventricular hypertrophy a big hyperinflated heart muscle. - - S/S of Pulmonary Stenosis: o Right ventricular hypertrophy o Loud “systolic ejection” heart murmur Treatment of Pulmonary Stenosis: o Balloon Angioplasty Balloon is inflated in the valve to open the narrowing o Surgical repair valvotomy Aortic Stenosis *Aortic valve has narrowing, which, reduces blood flow to the body - - S/S of Aortic Stenosis: o Decreased cardiac OUTput Means: decreased o2 blood OUT to the body o Activity intolerance o VS: Low BP Tachycardia o Left ventricular hypertrophy Blood backs up into the LEFT ventricle, making heart work harder, forcing the LEFT ventricle to “beef up” and become thick o Pulmonary congestion Blood flow backs up even further, going up into the LEFT atrium and even the lungs, causing congestion inside the lungs Treatment of Aortic Stenosis: o Balloon Angioplasty Balloon is inflated in the valve to open the narrowing o Surgical repair valvotomy Coarctation of the Aorta *Narrowed Aorta decreased cardiac OUTput specifically in the lower extremities *Increased blood flow supplied to upper extremities - - S/S of COA: o Upper extremities: High BP Bounding pulses o Lower extremities: Cool temp Low BP Diminished pulses Treatment of COA: o Balloon Angioplasty Balloon is inflated in the valve to open the narrowing o Stents General Treatments for Congenital Heart Defects: Cardiac catheterization: Inserting a catheter through the femoral artery [near the groin] and up to the Aorta into the heart o BEFORE Cardiac Cath: Assess if allergic to iodine Children must be NPO 4-6 hours Infants must be NPO for shorter than 4-6 hours Report SEVERE diaper rash to HCP Rash can introduce bacteria into the bloodstream o AFTER Cardiac Cath: *PRIORITY ASSESSMENTS: 1. Check pulses start most distal up to cath site a. Normal: weak pulses b. NOT normal: cool, cold, pale extremity 2. Straighten leg for 4-8 hours after procedure 3. Assess incision site for bleeding and infection a. Teach parent NO BATHS to prevent infection - Chest Tube Monitoring during cardiac cath o Placed during cardiac cath surgery to help drain excess fluid and air for lung expansion Remains in place AFTER surgery to help drain excess blood o PRIORITY to report to HCP: 1hr AFTER sx more than 5-10mL/kg of blood 3hr AFTER sx more than 3mL/kg/hr Indicates severe bleeding & cardiac tamponade deadly condition where sac around the heart fills with blood, squeezing the heart to death Can develop QUICKLY in peds EXAMPLE of Cardiac Tamponade: Child weighs 6kg 1hr: 30 – 60mL/kg 3hrs: 6kg x 3mL = 18mL/hr o Total of 54mL in 3hrs - Post-Op Care + Teaching Cardiac Cath o Nurse should elevate HOB to reduce respiratory effort AFTER surgery o Report any fever, warm surgical site, smelly purulent drainage o No heavy lifting of strenuous activity for the first 3-4 weeks Rheumatic Fever ~ occurs when strep throat or scarlet fever are not treated correctly not finishing antibiotics or not treating the infection. ~ untreated infection causes total body inflammation affects blood vessels, joint, skin, brain, and heart, damaging the heart valves - S/S of Rheumatic Fever: o Sore throat o Fever o Joint pain LABS: o Elevated CRP & ESR o Total body inflammation o Hemolytic strep o Shows active strep infection o Antistreptolysin O titer o Shows antibodies from past/previous strep infection - Treatment of Rheumatic Fever: ~ Goal to stop infection and reduce inflammation o Antibiotics o Penicillin o NSAIDS o To reduce inflammation **NEVER GIVE ASPIRIN** Kawasaki Disease *Memory Trick* K-Kawasaki // K-Krazy inflammation ~ inflammation within the blood vessels particularly the coronary arteries, the blood vessels that feed the blood O2. ~ affects lymph nodes, skin, and mucous membranes (inside mouth); aneurysm can develop ~ affects infants, young children, and sometimes teens - - S/S of Kawasaki Disease: o Fever for 3-5 days and unresolved with antipyretics o GALLOP HEART RHYTHM* Interventions for Kawasaki Disease: o Decreased urinary output - Monitor for gallop heart rhythm o Red strawberry tongue* - Monitor for decreased urinary output o Red eyes, lips, hands, and feet - Check temperature regularly o Skin peeling o Joint pain Discharge instructions - Monitor temp at least q6hr for first 48hrs Treatment for Kawasaki Disease: - Report to HCP if fever o IV immunoglobulin [IVIG] To boost antibodies No live vaccines for 11 months after IVIG MMR, Varicella, Influenza o Aspirin To treat inflammation // also an anti-platelet *BE CAUTIONS WITH REYES SYNDROME*