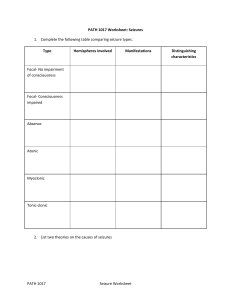
SEIZURES Ecessive neuron discharge Alteration in membrane potential Abnormal cells (epileptic focus) Any with a CNS imbalance can have seizures Though tto be genetic Risk Factors: tumors, vascular d/o, alcohol or drug withdrawal, brain trama, e- imbalance, AV malformations, infections, systemic diseases, uremia, acid/base imbalance, low sodium, heavy metal poisoning S/S Aura: sight, smell, sound, or taste (parietal, occipital have auras) -same every time Involuntary movements Often related to temporal lobe seizures or complex partial seizures Autonomic sx- d/t stimulation of autonomic nervous system -pupil dilation, diaphoresis, etc Post ictal period: flaccid extremities, lethargic or unresponsive for up to several hrs Differential dx: is this seizure related to a dysrhythmia? Syncope related to dysrhythmia v-tach: looks like seizure vasovagal response narcolepsy night terrors or somnambulism panic or rage attack psychogenic symptoms (pseudo-seizures) D41138722 Jubiny@10311992 TIA Migraine Triggers: flashing lights, music, odors, fatigue, stress, illness, fever, menstrual cycle ASK PATIENT WHAT TRIGGERS IT Simple/partial (focal)-: comes from one side of the brain Focal motor: (“marching/jacksonian” or tonic-clonic movement from upper or lower limb) arises from motor strip somatosensory- tingling of contralateral limb, face, or side of body (sensory strip) Autonomic-temporal/posterior frontal lobe-- fight or flight symptoms: sweating, flushing, pallor, epigastric Visual: occipital lobe: flashing lights, unilateral or bilateral blurring, scotomas ( blind spot or partial loss of vision in what is otherwise a perfectly normal visual field) Motor strip- facial grimacing Contraversive-head and eyes turned to opposite side (either side of frontal lobe) Auditory- ringing or hissing noises- temporal lobe Psychic (temporal)-distorted memory, time, déjà vu, hallucinations, frequently turns into complex partial EEG will have discharge sin limited regoin STUDY FOR EXAM- chart below KNOW FOR EXAM: LOBULAR Lobular seizures: FRONTAL: simple or complex, inappropriate behaviors, short length TEMPORAL: automatisms, psychic sx, olfactory or auditory hallucinations PARIETAL: complex that may progress to generalized, usually have auras, visual or auditory hallunications OCCIPITAL: visual auras, visual hallucinations, abnormal eye movements Complex partial: Impairment of consciousness, not wakefulness- not conscious but can be woken ; cognitive, affective sx-dreamy state; blak vacant expression, déjà vu, jamais vu (forget people they know), or fear Psychomotor phenomena: chewing, wetting lips, autonomism (picking at cothing) Dysphagia Formed auditory hallucinations- hears music, etc Formed visual hallucinations-sees house, trees that aren’t there Olfactory hallucinations- bad or unusual smell Can become more complex Involves involuntary motor activities (automatisms) Paranoia, aggression May be confused with psychosis EEG: 2-4Hz spike waves (don’t have to know) Generalized: involves both hemispheres -absence: petit mal- affects kids- staring, eye flutter, lasts 3-30 secs and may happen 100x a day -myoclonic: sporadic jerking or muscle contractions, isolated to one area, seen in encephalopathy -clonic: bilateral rhythmic movement followed by relaxation, eyes roll backward, frothing of mouth, head turning to one side (look at eye to see where they move) -tonic: stiffening of trunk, jaws shut close, incontinence, apneic periods -generalized tonic-clonic (grand-mal): combo of both, may become cyanotic , body limp afterwards, incontinence, snoring, hard to wake up afterwards -atonic-drop seizure- muscles weaken and pt drops to the floor- CAN’T WAKE THEM UP FROM IT GET A GOOD HX OF WHAT THE SEIZURES ARE Status epilepticus Seizure lasts > 5 min, or back-to-back seizures without regaining consciousness in between seizures Usually bc they stopped their AED’s Withdrawal from alcohol or drugs Fever Women with eclampsia Can present with tonic clonic movement MUST HAVE EEG If consciousness not regained after seizure, they could have a general seizure, the consider sub clinical seizure- do diligent assessment Testing for seizures CBC, BMP, toxicology screen Anticonvulsant levels if epileptic-do a level of their usual AED EEG- may miss seizures bc they are so localized or bc the seizure is over and there’s no EEG activity CT of brain and head/trauma MRI- IF FIRST EVER SEIZURE PET scan can find foci if seizing Subdural grids- look for areas where seizure is coming from Treatment: Avoid triggers, manage underlying condition, medical management/drug therapy(meds are decided based on type of seizure as well as if the first line drug worked or not- dilaton, Depakote,Tegretol, Lamictal FIRST LINE AED’S – know for exam Dilantin (phenytoin) – dose of 300-400mg/dL; loading dose 10-20 ; give slow IVP or cardiac arrest<50mg/min, phlebitis Surgical management- candidates are usually focused partial seizures(no generalized seizures); wont have major neuro defects if its done Mapping: done while patient is awake – ID’s visual, motor, sensory areas Wada’s Test: language and memory lcation; put one side of brain to sleep- show them pictures, then wake that side up and ask them if they remember the pictures Lobectomy: lesionectomy, hemispheriectomy (only for infants)-vagal nerve stimulator *ALL PTS AWAKE DURING SURGERY (PUT TO SLEEP TO TAKE OUT PART OF SKULL) Most common tx: Status epilepticus atuvan (lorazepam) 4-8 mgIV, then 1st line AED drug: Phenytoin (dilantin) load 20 mg/kg, then addition dilantin 5-10mg/kg, then intubate and propofol or versed drip then barbituates - know for exam- for emergency situations: IV DILANTIN: know dosage: 300-400mg/d; L:10-20, SE: ataxia, hirsutism, Pearls: give sow IVP or cardiac arrest <50mg/min, phlebitis Propofol can be given -stops muscle movement Lorazepam or midazolam next For exam, just recognize these drugs: Valproate (Depakote) Carbamazepine (Tegretol) Lamotrigine (Lamictal) Managing a seizing patient: Ease patient to floor unless in bed, take off glasses, don’t put anything in their mouth DO NOT RESTRAIN- guide movements to prevent injury Stay with patient and have someone put in PART/rapid response call After seizure put pt on their side Assess for patency of airway before turning them on the side DOCUMENTATION- KNOW FOR EXAM Was the seizure witnessed, who witnesses it ? Warning signs: Any aura, smell? What type of movements? Did eyes deviate? Up, down, straight ahead? Was pt conscious during seizure? Any incontinence? (Indicative of generalized seizure) What was the person’s behavior like after seizure? Aggression, sleepy, manic, crying? Any injuries after? Up on a ladder? Laying on the couch? Treatment done prior to seizure- did patient take an extra dose of their meds after the seizure, or did they get it in the ambulance? The client who just had a three (3)-minute seizure has no apparent injuries and is oriented to name, place, and time but is very lethargic and just wants to sleep. Which intervention should the nurse implement? 1. Perform a complete neurological assessment. 2. Awaken the client every 30 minutes. 3. Turn the client to the side and allow the client to sleep. 4. Interview the client to find out what caused the seizure. 3. Turn the client to the side and allow the client to sleep. (During the postictal (after-seizure) phase, the client is very tired and should be allowed to rest quietly; placing the client on the side will help prevent aspiration and maintain a patent airway.) Differential dx: is this seizure related to a dysrhythmia? Syncope related to dysrhythmia v-tach: looks like seizure vasovagal response narcolepsy night terrors or somnambulism panic or rage attack psychogenic symptoms (pseudo-seizures) D41138722 Jubiny@10311992