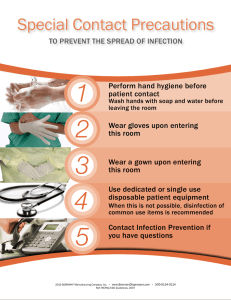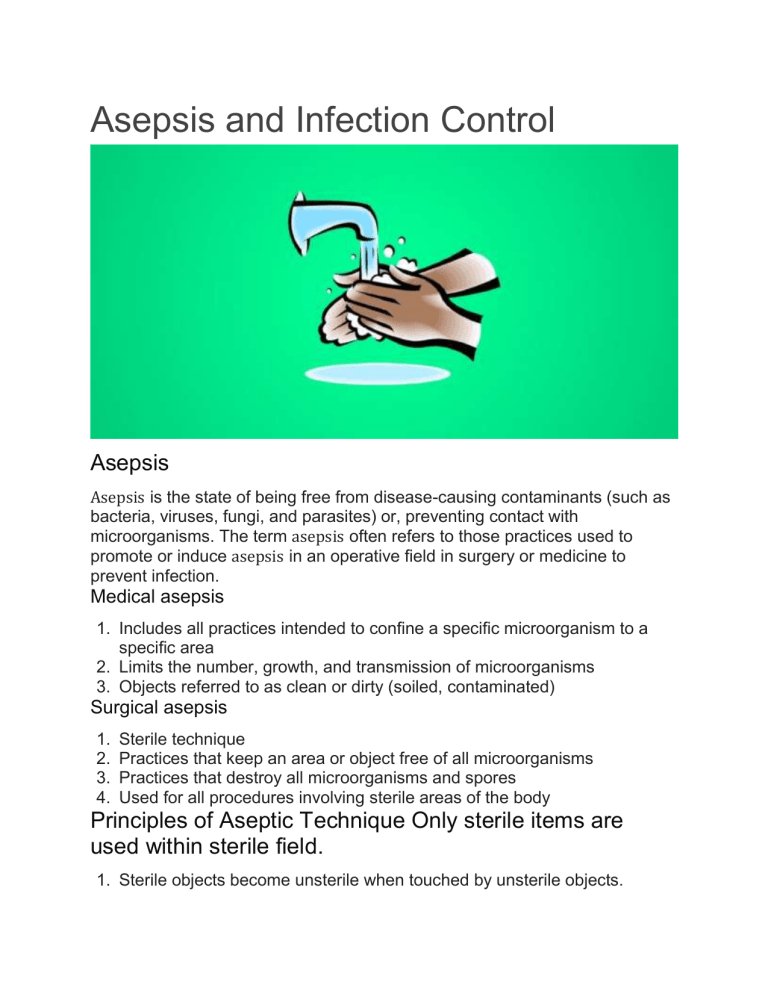
Asepsis and Infection Control Asepsis Asepsis is the state of being free from disease-causing contaminants (such as bacteria, viruses, fungi, and parasites) or, preventing contact with microorganisms. The term asepsis often refers to those practices used to promote or induce asepsis in an operative field in surgery or medicine to prevent infection. Medical asepsis 1. Includes all practices intended to confine a specific microorganism to a specific area 2. Limits the number, growth, and transmission of microorganisms 3. Objects referred to as clean or dirty (soiled, contaminated) Surgical asepsis 1. 2. 3. 4. Sterile technique Practices that keep an area or object free of all microorganisms Practices that destroy all microorganisms and spores Used for all procedures involving sterile areas of the body Principles of Aseptic Technique Only sterile items are used within sterile field. 1. Sterile objects become unsterile when touched by unsterile objects. 2. Sterile items that are out of vision or below the waist level of the nurse are considered unsterile. 3. Sterile objects can become unsterile by prolong exposure to airborne microorganisms. 4. Fluids flow in the direction of gravity. 5. Moisture that passes through a sterile object draws microorganism from unsterile surfaces above or below to the surface by capillary reaction. 6. The edges of a sterile field are considered unsterile. 7. The skin cannot be sterilized and is unsterile. 8. Conscientiousness, alertness and honesty are essential qualities in maintaining surgical asepsis Infection Signs of Localized Infection Localized swelling Localized redness Pain or tenderness with palpation or movement Palpable heat in the infected area Loss of function of the body part affected, depending on the site and extent of involvement Signs of Systemic Infection Fever Increased pulse and respiratory rate if the fever high Malaise and loss of energy Anorexia and, in some situations, nausea and vomiting Enlargement and tenderness of lymph nodes that drain the area of infection Factors Influencing Microorganism’s Capability to Produce Infection Number of microorganisms present Virulence and potency of the microorganisms (pathogenicity) Ability to enter the body Susceptibility of the host Ability to live in the host’s body Anatomic and Physiologic Barriers Defend Against Infection Intact skin and mucous membranes Moist mucous membranes and cilia of the nasal passages Alveolar macrophages Tears High acidity of the stomach Resident flora of the large intestine Peristalsis Low pH of the vagina Urine flow through the urethra NANDA Diagnosis Risk for Infection State in which an individual is at increased risk for being invaded by pathogenic microorganisms Risks factors Inadequate primary defenses Inadequate secondary defenses Related Diagnoses Potential Complication of Infection: Fever Imbalanced Nutrition: Less than Body Requirement Acute Pain Impaired Social Interaction or Social Isolation Anxiety Interventions to Reduce Risk for Infection Proper hand hygiene techniques Environmental controls Sterile technique when warranted Identification and management of clients at risk Chain of Infection 1. The chain of infection refers to those elements that must be present to cause an infection from a microorganism 2. Basic to the principle of infection is to interrupt this chain so that an infection from a microorganism does not occur in client 3. Infectious agent; microorganisms capable of causing infections are referred to as an infectious agent or pathogen 4. Modes of transmission: the microorganism must have a means of transmission to get from one location to another, called direct and indirect 5. Susceptible host describes a host (human or animal) not possessing enough resistance against a particular pathogen to prevent disease or infection from occurring when exposed to the pathogen; in humans this may occur if the person’s resistance is low because of poor nutrition, lack of exercise of a coexisting illness that weakens the host. 6. Portal of entry: the means of a pathogen entering a host: the means of entry can be the same as one that is the portal of exit (gastrointestinal, respiratory, genitourinary tract). 7. Reservoir: the environment in which the microorganism lives to ensure survival; it can be a person, animal, arthropod, plant, oil or a combination of these things; reservoirs that support organism that are pathogenic to humans are inanimate objects food and water, and other humans. 8. Portal of exit: the means in which the pathogen escapes from the reservoir and can cause disease; there is usually a common escape route for each type of microorganism; on humans, common escape routes are the gastrointestinal, respiratory and the genitourinary tract. Asepsis and Infection Control Breaking the Chain of Infection Etiologic agent Correctly cleaning, disinfecting or sterilizing articles before use Educating clients and support persons about appropriate methods to clean, disinfect, and sterilize article Reservoir (source) Changing dressings and bandages when soiled or wet Appropriate skin and oral hygiene Disposing of damp, soiled linens appropriately Disposing of feces and urine in appropriate receptacles Ensuring that all fluid containers are covered or capped Emptying suction and drainage bottles at end of each shift or before full or according to agency policy Portal of exit Avoiding talking, coughing, or sneezing over open wounds or sterile fields Covering the mouth and nose when coughing or sneezing Method of transmission Proper hand hygiene Instructing clients and support persons to perform hand hygiene before handling food, eating, after eliminating and after touching infectious material Wearing gloves when handling secretions and excretions Wearing gowns if there is danger of soiling clothing with body substances Placing discarded soiled materials in moisture-proof refuse bags Holding used bedpans steadily to prevent spillage Disposing of urine and feces in appropriate receptacles Initiating and implementing aseptic precautions for all clients Wearing masks and eye protection when in close contact with clients who have infections transmitted by droplets from the respiratory tract Wearing masks and eye protection when sprays of body fluid are possible Portal of entry Using sterile technique for invasive procedures, when exposing open wounds or handling dressings Placing used disposable needles and syringes in puncture-resistant containers for disposal Providing all clients with own personal care items Susceptible host Maintaining the integrity of the client’s skin and mucous membranes Ensuring that the client receives a balanced diet Educating the public about the importance of immunizations Modes of Transmission 1. Direct contact: describes the way in which microorganisms are transferred from person to person through biting, touching, kissing, or sexual intercourse; droplet spread is also a form of direct contact but can occur only if the source and the host are within 3 feet from each other; transmission by droplet can occur when a person coughs, sneezes, spits, or talks. 2. Indirect contact: can occur through fomites (inanimate objects or materials) or through vectors (animal or insect, flying or crawling); the fomites or vectors act as vehicle for transmission 3. Air: airborne transmission involves droplets or dust; droplet nuclei can remain in the air for long periods and dust particles containing infectious agents can become airborne infecting a susceptible host generally through the respiratory tract Course of Infection 1. Incubation: the time between initial contact with an infectious agent until the first signs of symptoms the incubation period varies from different pathogens; microorganisms are growing and multiplying during this stage 2. Prodromal Stage: the time period from the onset of nonspecific symptoms to the appearance of specific symptoms related to the causative pathogen symptoms range from being fatigued to having a low-grade fever with malaise; during this phase it is still possible to transmit the pathogen to another host 3. Full Stage: manifestations of specific signs & symptoms of infectious agent; referred to as the acute stage; during this stage, it may be possible to transmit the infectious agent to another, depending on the virulence of the infectious agent 4. Convalescence: time period that the host takes to return to the pre-illness stage; also called the recovery period; the host defense mechanisms have responded to the infectious agent and the signs and symptoms of the disease disappear; the host, however, is more vulnerable to other pathogens at this time; an appropriate nursing diagnostic label related to this process would be Risk for Infection Inflammation The protective response of the tissues of the body to injury or infection; the physiological reaction to injury or infection is the inflammatory response; it may be acute or chronic Body’s response 1. The “inflammatory response” begins with vasoconstriction that is followed by a brief increase in vascular permeability; the blood vessels dilate allowing plasma to escape into the injured tissue 2. WBCs (neutrophils, monocytes, and macrophages) migrate to the area of injury and attack and ingest the invaders (phagocytosis); this process is responsible for the signs of inflammation 3. Redness occurs when blood accumulates in the dilated capillaries; warmth occurs as a result of the heat from the increased blood in the area, swelling occurs from fluid accumulation; the pain occurs from pressure or injury to the local nerves. Immune Response 1. The immune response involves specific reactions in the body to antigens or foreign material 2. This specific response is the body’s attempt to protect itself, the body protects itself by activating 2 types of lymphocytes, the T-lymphocytes and B-lymphocytes 3. Cell mediated immunity: T-lymphocytes are responsible for cellular immunity When fungi , protozoa, bacteria and some viruses activate Tlymphocytes, they enter the circulation from lymph tissue and seek out the antigen Once the antigen is found they produce proteins (lymphokines) that increase the migration of phagocytes to the area and keep them there to kill the antigen After the antigen is gone, the lymphokines disappear Some T-lymphocytes remain and keep a memory of the antigen and are reactivated if the antigen appears again. 4. Humoral response: the ability of the body to develop a specific antibody to a specific antigen (antigen-antibody response) B-lymphocytes provide humoral immunity by producing antibodies that convey specific resistance to many bacterial and viral infections Active immunity is produced when the immune system is activated either naturally or artificially. 3. Natural immunity involves acquisition of immunity through developing the disease 4. Active immunity can also be produced through vaccination by introducing into the body a weakened or killed antigen (artificially acquired immunity) 5. Passive immunity does not require a host to develop antibodies, rather it is transferred to the individual, passive immunity occurs when a mother passes antibodies to a newborn or when a person is given antibodies from an animal or person who has had the disease in the form of immune globulins; this type of immunity only offers temporary protection from the antigen. Types of Immunity Active Immunity Host produces antibodies in response to natural antigens or artificial antigens Natural active immunity Antibodies are formed in presence of active infection in the body Duration lifelong Artificial active immunity Antigens administered to stimulate antibody formation Lasts for many years Reinforced by booster Passive Immunity Host receives natural or artificial antibodies produced from another source Natural passive immunity Antibodies transferred naturally from an immune mother to baby through the placenta or in colostrums Lasts 6 months to 1 year Artificial passive immunity Occurs when immune serum (antibody) from an animal or another human is injected Lasts 2 to 3 weeks Nosocomial Infection 1. Nosocomial Infections: are those that are acquired as a result of a healthcare delivery system 2. Iatrogenic infection: these nosocomial infections are directly related to the client’s treatment or diagnostic procedures; an example of an iatrogenic infection would be a bacterial infection that results from an intravascular line or Pseudomonas aeruginosa pneumonia as a result of respiratory suctioning 3. Exogenous Infection: are a result of the healthcare facility environment or personnel; an example would be an upper respiratory infection resulting from contact with a caregiver who has an upper respiratory infection 4. Endogenous Infection: can occur from clients themselves or as a reactivation of a previous dormant organism such as tuberculosis; an example of endogenous infection would be a yeast infection arising in a woman receiving antibiotic therapy; the yeast organisms are always present in the vagina, but with the elimination of the normal bacterial flora, the yeast flourish. Risks for Nosocomial Infections Diagnostic or therapeutic procedures Iatrogenic infections Compromised host Insufficient hand hygiene Factors Increasing Susceptibility to Infection 1. Age: young infants & older adults are at greater risk of infection because of reduced defense mechanisms Young infants have reduced defenses related to immature immune systems In elderly people, physiological changes occur in the body that make them more susceptible to infectious disease; some of these changes are: 3. Altered immune function (specifically, decreased phagocytosis by the neutrophils and by the macrophages) 4. Decreased bladder muscle tone resulting in urinary retention 5. Diminished cough reflex, loss of elastic recoil by the lungs leading to inability to evacuate normal secretions 6. Gastrointestinal changes resulting in decreased swallowing ability and delayed gastric emptying. 2. Heredity: some people have a genetic predisposition or susceptibility to some infectious diseases 3. Cultural practices: healthcare beliefs and practices, as well as nutritional and hygiene practices, can influence a person’s susceptibility to infectious diseases 4. Nutrition: inadequate nutrition can make a person more susceptible to infectious diseases; nutritional practices that do not supply the body with the basic components necessary to synthesized proteins affect the way the body’s immune system can respond to pathogens 5. Stress: stressors, both physical and emotional, affect the body’s ability to protect against invading pathogens; stressors affect the body by elevating blood cortisone levels; if elevation of serum cortisone is prolonged, it decreases the anti-inflammatory response and depletes energy stores, thus increasing the risk of infection 6. Rest, exercise and personal health habits: altered rest and exercise patterns decrease the body’s protective, mechanisms and may cause physical stress to the body resulting in an increased risk of infection; personal health habits such as poor nutrition and unhealthy lifestyle habits increase the risk of infectious over time by altering the body’s response to pathogens 7. Inadequate defenses: any physiological abnormality or lifestyle habit can influence normal defense mechanisms in the body, making the client more susceptible to infection; the immune system functions throughout the body and depends on the following: Intact skin and mucous membranes Adequate blood cell production and differentiation A functional lymphatic system and spleen An ability to differentiate foreign tissue and pathogens from normal body tissue and flora; in autoimmune disease, the body has a problem with recognizing its own tissue and cells; people with autoimmune disease are at increased risk of infection related to their immune system deficiencies. 8. Environmental: an environment that exposes individuals to an increased number of toxins or pathogens also increases the risk of infection; pathogens grow well in warm moist areas with oxygen (aerobic) or without oxygen (anaerobic) depending on the microorganism, an environment that increases exposure to toxic substances also increases risk 9. Immunization history: inadequately immunized people have an increased risk of infection specifically for those diseases for which vaccines have been developed. 10. Medications and medical therapies: examples of therapies and medications that increase clients risk for infection includes radiation treatment, anti-neo-plastic drugs, anti inflammatory drugs and surgery Diagnostic Tests Used to Screen for Infection 1. Signs and symptoms related to infections are associated with the area infected; for instance, symptoms of a local infection on the skin or mucous membranes are localized swelling, redness, pain and warmth 2. Symptoms related to systemic infections include fever, increased pulse & respirations, lethargy, anorexia, and enlarged lymph nodes 3. Certain diagnostic tests are ordered to confirm the presence of an infection. Category-specific Isolation Precautions Strict isolation Contact isolation Respiratory isolation Tuberculosis isolation Enteric precautions Drainage/secretions precautions Blood/body fluid precautions Disease-specific Isolation Precautions Delineate practices for control of specific diseases Use of private rooms with special ventilation Cohorting clients infected with the same organism Gowning to prevent gross soilage of clothes Universal Precautions (UP) Used with all clients Decrease the risk of transmitting unidentified pathogens Obstruct the spread of bloodborne pathogens (hepatitis B and C viruses and HIV) Used in conjunction with disease-specific or category-specific precautions Body Substance Isolation (BSI) Employs generic infection control precautions for all clients Body substances include: Blood Urine Feces Wound drainage Oral secretions Any other body product or tissue Standard Precautions Used in the care of all hospitalized persons regardless of their diagnosis or possible infection status Apply to: Blood All body fluids, secretions, and excretions except sweat (whether or not blood is present or visible) Nonintact skin and mucous membranes Combine the major features of UP and BSI Transmission-based Precautions Used in addition to standard precautions For known or suspected infections that are spread in one of three ways: Airborne Droplet Contact May be used alone or in combination but always in addition to standard precautions Managing Equipment Used for Isolation Clients Many supplied for single use only Disposed of after use Agencies have specific policies and procedures for handling soiled reusable equipment Nurses need to become familiar with these practices Bloodborne Pathogen Exposure Report the incident immediately Complete injury report Seek appropriate evaluation and follow-up Identification and documentation of the source individual when feasible and legal Testing of the source for hepatitis B, C and HIV when feasible and consent is given Making results of the test available to the source individual’s health care provider Testing of blood exposed nurse (with consent) for hepatitis B, C, and HIV – please check these to match style used in book – fairly certain it should be caped antibodies Postexposure prophylaxis if medically indicated Medical and psychologic counseling Puncture/Laceration Encourage bleeding Wash/clean the area with soap and water Initiate first aid and seek treatment if indicated Mucous membrane exposure (eyes, nose, mouth) Flush with saline or water flush for 5 to 10 minutes Postexposure Protocol (PEP) for HIV Start treatment as soon as possible preferably within hours after exposure For “high-risk” exposure (high blood volume and source with a high HIV titer), three drug treatment is recommended For “increased risk” exposure (high blood volume or source with high HIV titer), three-drug treatment is recommended For “low risk” exposure (neither high blood volume nor source with a high HIV titer), two-drug treatment is considered Drug prophylaxis continues for 4 weeks Drug regimens vary and new drugs and regimens continuously being developed HIV antibody tests should be done shortly after exposure (baseline), and 6 weeks, 3 months, and 6 months afterward Postexposure Protocol (PEP) for Hepatitis B Anti-HBs testing 1 to 2 months after last vaccine dose HBIG and/or hepatitis B vaccine within 1 to 7 days following exposure for nonimmune workers Postexposure Protocol (PEP) for Hepatitis C Anti-HCV and ALT at baseline and 4 to 6 months after exposure