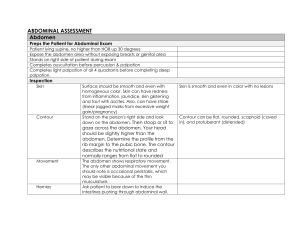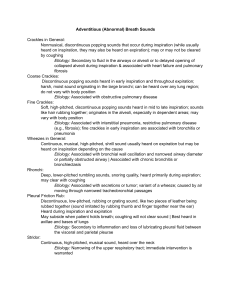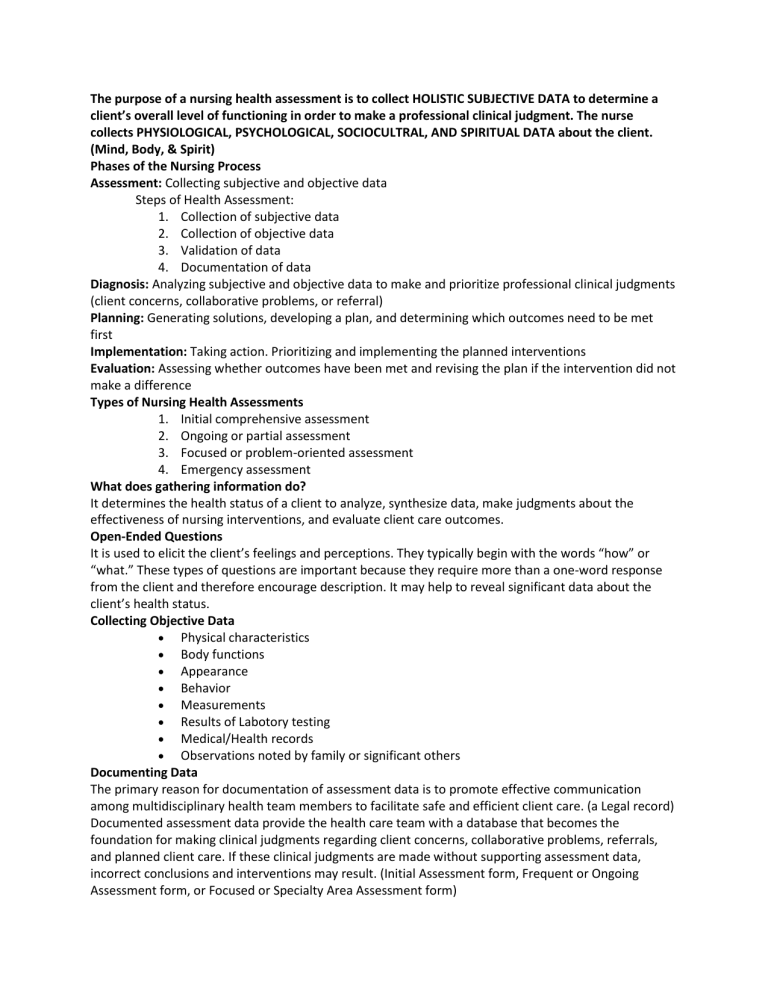
The purpose of a nursing health assessment is to collect HOLISTIC SUBJECTIVE DATA to determine a client’s overall level of functioning in order to make a professional clinical judgment. The nurse collects PHYSIOLOGICAL, PSYCHOLOGICAL, SOCIOCULTRAL, AND SPIRITUAL DATA about the client. (Mind, Body, & Spirit) Phases of the Nursing Process Assessment: Collecting subjective and objective data Steps of Health Assessment: 1. Collection of subjective data 2. Collection of objective data 3. Validation of data 4. Documentation of data Diagnosis: Analyzing subjective and objective data to make and prioritize professional clinical judgments (client concerns, collaborative problems, or referral) Planning: Generating solutions, developing a plan, and determining which outcomes need to be met first Implementation: Taking action. Prioritizing and implementing the planned interventions Evaluation: Assessing whether outcomes have been met and revising the plan if the intervention did not make a difference Types of Nursing Health Assessments 1. Initial comprehensive assessment 2. Ongoing or partial assessment 3. Focused or problem-oriented assessment 4. Emergency assessment What does gathering information do? It determines the health status of a client to analyze, synthesize data, make judgments about the effectiveness of nursing interventions, and evaluate client care outcomes. Open-Ended Questions It is used to elicit the client’s feelings and perceptions. They typically begin with the words “how” or “what.” These types of questions are important because they require more than a one-word response from the client and therefore encourage description. It may help to reveal significant data about the client’s health status. Collecting Objective Data Physical characteristics Body functions Appearance Behavior Measurements Results of Labotory testing Medical/Health records Observations noted by family or significant others Documenting Data The primary reason for documentation of assessment data is to promote effective communication among multidisciplinary health team members to facilitate safe and efficient client care. (a Legal record) Documented assessment data provide the health care team with a database that becomes the foundation for making clinical judgments regarding client concerns, collaborative problems, referrals, and planned client care. If these clinical judgments are made without supporting assessment data, incorrect conclusions and interventions may result. (Initial Assessment form, Frequent or Ongoing Assessment form, or Focused or Specialty Area Assessment form) Muscle Movements Abduction: Moving away from midline of the body Adduction: Moving toward midline of the body Circumduction: Circular motion Inversion: Moving inward Eversion: Moving outward Extension: Straightening the extremity at the joint and decreasing the angle of the joint Flexion: Bending the extremity at the joint and decreasing the angle of the joint Hyperextension: Joint bends greater than 180 degrees Dorsiflexion: Toes draw upward to ankle Plantar flexion: Toes point away from ankle Pronation: Turning or facing downward Supination: Turning or facing upward Protraction: Moving forward Retraction: Moving backward Rotation: Turning of a bone toward the center of the body Internal rotation: Turning of a bone toward the center of the body External rotation: Turning of a bone away from the center of the body Physical Examination Techniques Inspection Palpation Percussion Auscultation Order for Assessing Abdomen Inspection Auscultation Percussion Palpation Types of Palpation Palpation consists of using parts of the hand to touch and feel for the following characteristics: texture, temperature, moisture, mobility, consistency, strength, size, shape, degree of tenderness. Three different parts of the hand – the finger pads, ulnar/palmar surface, and dorsal surface – are used during palpation. Finger pads- Fine discriminations: pulses, texture, size, consistency, shape, crepitus. Ulnar or palmar surface – Vibrations, thrills, fremitus. Dorsal (back) surface: Temperature. Light palpation: There should be very little or no depression (<1 cm). Use this technique to feel pulses, tenderness, surface skin texture, temperature, and moisture. Moderate palpation: Depress the skin surface 1 to 2 cm to feel for easily palpable body organs and masses. Note the size, consistency, and mobility of structures you palpate. Deep palpation: This should be in a surface depression between 2.5 and 5 cm. Nondominant hand -> Dominant hand -> Skin. This allows you to feel very deep organs or structures that are covered by thick muscle. Bimanual palpation: Using two hands, placing one hand on each side of the body part (uterus, breasts, spleen). Use one hand to apply pressure and the other hand to feel the structure. Note the size, shape, consistency, and mobility of the structures you palpate. Acronyms for exploring symptoms, signs, or health concerns Character: Describe nature. Provocative Onset Quality Location Radiates Duration Severity Severity Timing Pattern: What makes it better or worse? Associated factors Normal Breath Sounds Bronchial: Short during inspiration, long in expiration Bronchovesicular: Same during inspiration and expiration Vesicular: Long in inspiration, short in expiration Abnormal Breath Sounds -> Adventitious Breath Sounds Discontinuous sounds Crackles (fine) example: rolling a strand of hair between your fingers High-pitched, short, popping sounds heard during inspiration and not cleared with coughing Crackles occurring late in inspiration are associated with restrictive diseases such as pneumonia and CHF. Crackles occurring early in inspiration are associated with obstructive disorders such as bronchitis, asthma, or emphysema. Crackles (coarse) example: softly separating Velcro Low-pitched, bubbling, moist sounds that may persist from early inspiration to early expiration Indicates pneumonia, pulmonary edema, and pulmonary fibrosis. “Velcro rales” of pulmonary fibrosis are heard louder and closer to stethoscope, usually do not change in location, and more common in clients with long-term COPD Continuous Sounds Pleural friction rub example: sound is much like crackles, only more superficial and occurring during both inspiration and expiration Low-pitched, dry, grating sound Can indicate pleuritis or Dehydration Wheeze (sibilant) High-pitched, musical sounds heard primarily during expiration but may also be heard on inspiration Cases of acute asthma or chronic emphysema Wheeze (sonorous) Low-pitched snoring or moaning sounds heard primarily during expiration but may be heard throughout the respiratory cycle. May be cleared with coughing. Sonorous wheezes are often heard in cases of bronchitis or single obstructions and snoring before an episode of sleep apnea. Stridor is a harsh, honking wheeze with severe broncho laryngospasm, such as occurs with croup. *APEX OF THE LUNGS IS ABOVE THE CLAVICLE Assessing Tonsils In a client who has both tonsils and a sore throat, tonsillitis can be identified and ranked with a grading scale from 1 to 4 as follows: 1+ Tonsils are visible 2+ Tonsils are midway between tonsillar pillars and uvula 3+ Tonsils touch the uvula 4+ Tonsils touch each other Assessing the Uvula A deviated uvula is one that leans to one side or the other. This often occurs if certain cranial nerves are weakened. Asymmetric movement or loss of movement may occur after a cerebrovascular accident (stroke). The palate fails to rise and the uvula deviates to normal side with cranial nerve X (vagus) paralysis. Inspecting Mouth Concerns Leukoplakia (ventral/ surface) Hairy Leukoplakia (lateral surface) Cancer sores Herpes Simplex Type I (cold sores) Assessing Pulses Palpate carotid arteries individually because bilateral palpation could result in reduced cerebral blood flow. If you detect occlusion during auscultation, palpate very lightly to avoid blocking circulation or triggering vagal stimulation and bradycardia, hypotension, or even cardiac arrest. Pulse Amplitude Scale 0 = Absent 1+ = Weak, diminished 2+ = Normal 3+ = Strong 4+ = Bounding Assessing Ascites Ascitic fluid in the abdomen causes generalized protuberance, bulging flanks, and an everted umbilicus. Percussion reveals dullness over fluid (bottom of abdomen and flanks) and tympany over intestines (top of abdomen) Test for shifting dullness. If you suspect that the client has ascites because of a distended abdomen or bulging flanks, perform this special percussion technique. The client should remain supine. Percuss the umbilicus. Note the change from dullness to tympany and mark this point. Now help the client turn onto the side. Percuss the abdomen from the bed upward. Mark the level where dullness changes to tympany. Perform the fluid wave test. The client should remain supine. You will need assistance with this test. Ask the client or an assistant to place the ulnar side of the hand and the lateral side of the forearm firmly along the midline of the abdomen. Firmly place the palmar surface of your fingers and hand against one side of the client’s abdomen. Use your other hand to tap the opposite side of the abdominal wall. Not reliable. Ultrasound is necessary. Lobes of the Brain Frontal: Directs voluntary, skeletal actions. Also influences communication (talking and writing), emotions, intellect, reasoning ability, judgment, and behavior. Contains Broca are, which is responsible for speech. Temporal: Receives and interprets impulses from the ear. Contains Wernicke area, which is responsible for interpreting auditory stimuli. Parietal: Interprets tactile sensations, including touch, pain, temperature, shapes, and two-point discrimination. Occipital: Influences the ability to read with understanding and is the primary visual receptor center. Parts of External Ear Auricle (Pinna) External Auditory Canal Cerumen (wax) Tympanic membrane (eardrum) Layers of Skin The skin is the largest organ of the body. It is a physical barrier that protects the underlying tissues and organs from microorganisms, physical trauma, ultraviolet radiation (UVR), and dehydration. It plays a vital role in temperature maintenance, fluid and electrolyte balance, absorption, excretion, sensation, immunity, and vitamin D synthesis. The skin also provides individual identity to a person’s appearance. 1. Epidermis (outer layer) Consists of dead, keratinized cells that render the skin waterproof that completely replaces every 3 to 4 weeks 2. Dermis (inner layer) Visible patterns known as fingerprints and origin of the sebaceous (oil) glands, sweat glands, and hair follicles 3. Subcutaneous Tissue (beneath the dermis) loose connective tissue containing fat cells, blood vessels, and nerves that conserves internal body heat and protects bones and internal organs Genogram key = Female A/W = Alive and well = Male ( ) = Cause of death or = Deceased -- = Client’s spouse or = client l = Adoption (vertical) Time of day body temperatures (4:00-6:00am) Body temperature is lowest early in the morning (8:00pm-Midnight) Body temperature is the highest late in the evening Areas of Abuse 1. Physical 2. Emotional 3. Sexual 4. Economical Visual Reflexes Pupillary light reflex causes pupils to constrict immediately when exposed to bright light Direct reflex in which constriction occurs in the eye exposed to the light Indirect (Consensual) reflex in which exposure to light in one eye results in constriction of the pupil in the opposite eye Accommodation is a functional reflex allowing the eyes to focus on nearby objects External Genitalia Male Penis Scrotum Female Mons pubis Labia majora Labia minora Clitoris Internal Genitalia Male Testes Spermatic Cord Female Vagina Cervix Uterus Fallopian tubes Ovaries Risk Factors of Cancer Alcohol Tobacco Obesity Old age Hereditary * TEARS COME FROM THE NASAL LACRIMAL GLANDS *REFER TO DOCTOR OR PROVIDER FOR SCREENING OR TEACHING *BREASTS NOT SYMMETRICAL IS NORMAL!