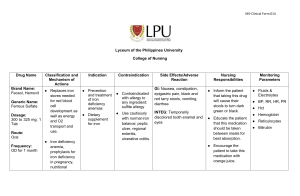
Hematologic Dysfunction Blood consists of two elements: ✓ The liquid is plasma. ✓ Blood Cells. o Plasma contains a percentage of water, mineral salts, Carbohydrates, fats, clotting factors and immunoglobulin and bilirubin. o Blood cells consist of: White blood cells, red blood cells & Platelets. • White Blood Cells: WBC Leucocytes: kills germs that attack the body. o Neutrophils: The cells responsible for "Phagocytosis" increase in proportion in case of bacterial inflammation o Lymphocytes: Cells increase in viral infection o Monocytes: Cells whose function is to eat germs o Eosinophiles: Cells rise in in case of allergies o Basophiles: Its function is not yet specified and contains Histamine. o Bands: Immature white blood cells are high in the case of acute inflammation. • Red blood cells: RBC = Erythrocytes: are flexible and oval biconcave disks cells produced from bone marrow, especially long and flat bones. The action of red blood cells is the transfer of O2 and CO2 Life span is 120 days RBC hemolysis occur in the spleen. • Platelets: small rectangular cells that share the process of blood clotting. Assessment of a child with Hematologic Dysfunction: When the child attends the health center with the parents, the full health history of the child, mother, family, duration of pregnancy, complications during pregnancy, genetic diseases in the family, and presence of family history of blood diseases. After taking health information, the child is conducted a thorough clinical examination starting from: o Head: check the size of the head if proportional with the body, presence of an inflation in forehead indicates the presence of "Thalassemia". o Skin: The color of the skin is pale in cases of blood diseases, yellowish color of mucous membranes and "Conjunctiva" especially in the case of anemia. o Respiratory system: Assesses the child's breathing condition and notes difficulty and rate of breathing. o Heart: Auscultate heart beat and note presence of rapid and deep pulse. o Abdomen: Notice abdominal distention due to enlarged organs such as the spleen and liver. A child with blood diseases suffers from anorexia, nausea, constipation due to slow intestinal movement as a result of hypoxemia, headache, numbness in the fingers due to lack of nerve nutrition, dizziness, muscle weakness and inability to concentrate. • Lab Studies: o ESR, Platelets, CBCD are routinely taken o Blood film inspection is conducted to find out the size and color of red cell which is evidence of the presence of sickle cells, thalassemia. o Reticulocyte’s count: the number of immature blood cells. o Iron and folic acid level. Anemias: If the level of erythrocytes decreases or the hemoglobin ratio decreases, the blood's ability to carry oxygen decrease, thus reducing tissue oxygenation. Anemia is a common disease in the age of infancy and childhood. • Iron Deficiency Anemia: A common disease in children caused by a lack of iron storage and usually at the age of 6 months in children full term while premature babies lack storage at the age of (2-3) months. Causes: o Iron deficiency in the mother o Do not give the baby milk fortified with iron or iron-rich food. o Exposure to chronic bleeding. o Poor iron absorption due to chronic diarrhea and high pH level in the stomach. o Deficiency in folic acid and vitamin B12 Symptoms: anorexia, pallor, poor sucking (infant), rapid fatigue, muscle weakness, head soreness, inability to concentrate, irritability, lower limb ischemia, reduced arterial pressure and increased heartbeat. Diagnosis: o CBCD notes decrease (HCT & Hgb). o Blood Film inspection shows normal red blood cell small in size (Microcytic) and light in color (Hypochromic). o Low MCV o Reticulocyte count increase. o A stool examination is carried out for occult blood in stool for possible gastrointestinal bleeding. o Total iron binding capacity (TIBC). Treatment Iron therapy. Oral ferrous iron salts are the most economical and effective medication for the treatment of iron deficiency anemia; of the various iron salts available, ferrous sulfate is the one most commonly used. Management of hemorrhage. Surgical treatment consists of stopping hemorrhage and correcting the underlying defect so that it does not recur. Diet. The addition of nonheme iron to national diets has been initiated in some areas of the world. The nursing interventions for a child with iron deficiency anemia are: Administer prescribed medications, as ordered: ✓ Administer IM or IV iron when oral iron is poorly absorbed. ✓ Perform sensitivity testing of IM iron injection to avoid risk of anaphylaxis. ✓ Advise patient to take iron supplements an hour before meals for maximum absorption; if gastric distress occurs, suggest taking the supplement with meals — resume to betweenmeals schedule if symptoms subside. ✓ Inform patient that iron salts change stool to dark green or black. ✓ Advise patient to take liquid forms of iron via a straw and rinse mouth with water. Reduce fatigue ✓ Assist the client/caregivers in developing a schedule for daily activity and rest. ✓ Stress the importance of frequent rest periods. ✓ Monitor hemoglobin, hematocrit, RBC count, and reticulocyte counts. ✓ Educate energy-conservation techniques. ✓ Encourage patient to continue iron therapy for a total therapy time (6 months to a year), even when fatigue is no longer present. Educate the client and caregivers about iron deficiency anemia: ✓ Explain the importance of the diagnostic procedures (such as complete blood count), bone marrow aspiration and a possible referral to a hematologist. ✓ Explain the importance of iron replacement/supplementation. ✓ Educate the client and the family regarding foods rich in iron (organ and other meats, leafy green vegetables, molasses, beans). Prevent infection ✓ Assess for local or systemic signs of infection, such as fever, chills, swelling, pain, and body malaise. ✓ Monitor WBC count; anticipate the need for antibiotic, antiviral, and antifungal therapy. ✓ Instruct the client to avoid contact with people with existing infections. ✓ Stress the importance of daily hygiene, mouth care, and perineal care. ➢ Prevent bleeding ✓ Monitor platelet count; instruct the client/caregivers about bleeding precautions. ✓ Anticipate the need for a platelet transfusion once the platelet count drops to a very low value. ✓ Assess the skin for bruises and petechiae. Hemolytic Anemia: Is an anemia caused by the hemolysis of red blood cells. β – Thalassemia (Cooley anemia): The word Thalassemia is derived from the Greek world Thalassa and means the sea. The disease is seen in Mediterranean people such as Lebanon, Italy and Syria. Thalassemia is a hereditary hematology characterized by the production weak red blood cells with rapid destruction. β Thalassemia is the most frequent and widespread type of Thalassemia. • Thalassemia types: o Thalassemia Minor: Characterized by the production of small microcytic red blood cells. o Thalassemia Intermedia: Characterized by severe anemia and spleen enlargement. o Thalassemia Major = Cooley anemia: The most important species, is an acute anemia treated by blood transfusion does not treat blood. Pathophysiology: The Hemoglobin consists of two alpha series (α)and beta (β). Poly Peptide Chain: Is a protein chain of the type α and β. In the case of β - Thalassemia there is a partial or total deficiency in the composition of the β chain, thus adapting the body to this imbalance and increases the production of the α chain leading to the formation of weak red blood cell that is rapidly destructed. Symptoms: ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ Anemia Fever of unknown cause Anorexia Fatigue Enlarged Head Enlarged Maxilla Splenomegaly Hepatomegaly Mongolian eye shape Short stature Flat nose and depressed Delayed sexual growth As anemia progresses, the child will have chronic hypoxia, headache, bone pain, activity intolerance, and anorexia. The bone expands or swells due to increased bone marrow functioning, especially facial bones, making the face shape Mongolian. Diagnosis: Symptoms appear in children after the second half of the first year of life. CBCD: Hgb & Hct, change in RBC properties and short lifespan, RBC. Blood Film Fetal Hgb increases Bilirubin increases Hemoglobin electrophoresis o o o o o Treatment: There is no special treatment for the treatment of β -Thalassemia, it is an incurable disease. o Give blood periodically so as to maintain an Hgb level at least 10.5g/dl, which will reduce risk of cardiomegaly and hepatomegaly, it reduces or prevents bone deformity and improves growth and development. o Give a drug to prevent iron build-up as a result of giving large amounts of blood. This drug is called "Desferal" and it releases excess amounts of iron. o Splenectomy in children with severe spleen enlargement. This process reduces pressure on the abdomen and increases the life of the red blood cells given to the patient. o Vaccine given against: Hemophilus influenza, Meningococcal, Pneumococcal o Give prophylactic antibiotics such as "Penicillin" in case of splenectomy. Nursing care: ✓ Give protein-rich and low-iron food taking into account giving cold meals to avoid ulceration in the mouth. ✓ Give small and multiple meals in addition to increasing fluid intake. ✓ Clean the mouth in case of ulceration ✓ Give oxygen to compensate for the low ability of Hgb to transfer O2. ✓ Avoid contact with infected persons. ✓ Isolation of the patient with low WBC. ✓ Patient support to adapt to treatment ✓ Planning treatment in a way that suits the patient's activities. ✓ Encourage your child to engage in effortless activities. ✓ Encourage parents and children to express their feelings. ✓ Give detailed guidance on the nature of the disease and its treatment methods. ✓ Encouraging parents and guiding them to take care of their child at home, including: • • • • • • Avoid infections. Method of giving "Desferal" (subcutaneous S/C) Give low iron diet and encourage high fluid intake. Practice special activities to avoid fractures, wounds and burns. Monitor signs, symptoms and complications of the disease. Consult doctor in case of complication.