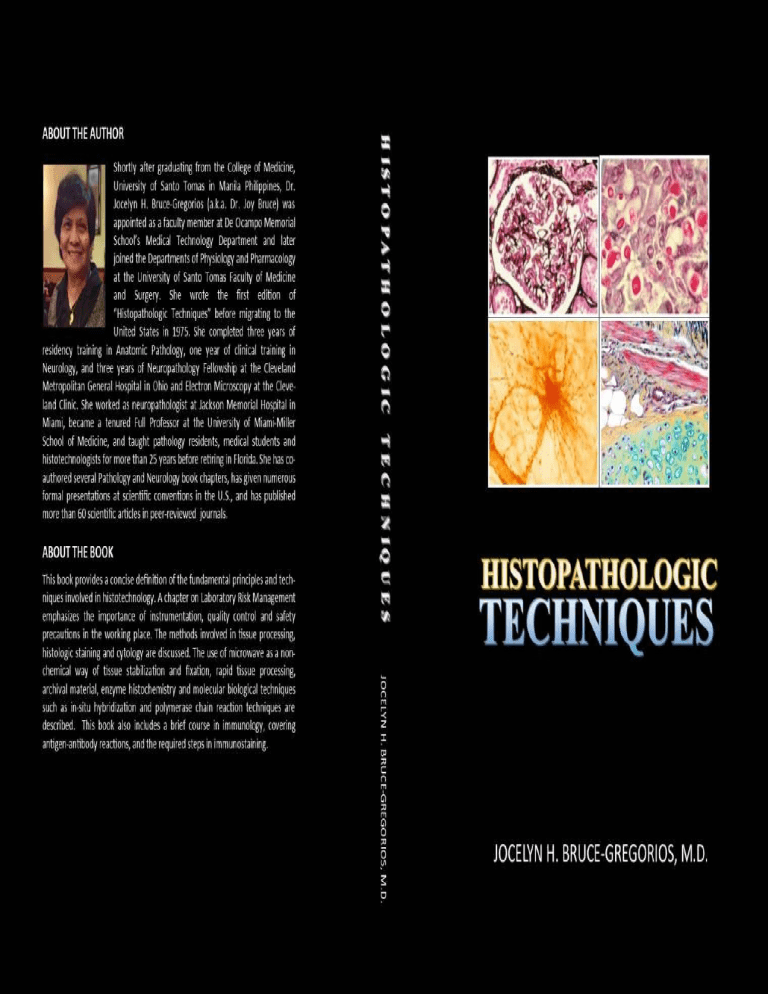
HISTOPATHOLOGIC TECHNIQUES JOCELYN H. BRUCE-GREGORIOS, M.D. MARC-ELI MEDINA FALDAS Contributing Author HISTOPATHOLOGIC TECHNIQUES Copyright by Jocelyn H. Bruce-Gregorios, M.D. All Rights Reserved. No part of this book may be reproduced, stored in retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the authors. Published by: JOCELYN H. BRUCE-GREGORIOS, M.D. U.S. EDITION DEDICATED To JEANNE-JEANNE, MY ANGEL. . . . . To JHAY-JHAY, MY HOPE . . . . To JIM-BOY, MY JOY . . . To MOM AND DAD, MY INSPIRATION PREFACE This book was initially written to provide fundamental knowledge and basic principles designed to help the histotechnologist with common time consuming issues including safety in the laboratory and prevention of artifacts associated with fixation, dehydration, embedding, microtomy and staining of tissues that are important for proper diagnosis of disease. Much of the discussion is centered on techniques and guidelines in tissue processing since the primary work of a histotechnologist is to provide the pathologist with well-preserved and adequately processed material that can be used to make a proper interpretation and diagnosis of disease. While immunohistochemistry and in situ hybridization have replaced many histochemical techniques, some stains remain in wide use today. Various chapters focus on frequently used histochemical methods including their mechanisms, precautions and guidelines for all the steps in the process of staining. Various chapters focus on frequently used histochemical methods including their mechanisms, precautions and guidelines during the process of staining. While immunohistochemistry and in situ hybridization have replaced many histochemical stains, many techniques are still based on established principles that remain in wide use today. It includes a brief course in immunology, covering topics of antigens, antibodies, antigen-antibody reactions, and an explanation of required steps in immunostaining procedures. I am much indebted to Dr. Stephen Vernon, Dr. Parvin Ganjei and Bonnie Cohen who co-authored some of the chapters in the previous edition of this book. For this edition, I am privileged to have Marc-Eli Faldas as my co-author on immunohistochemistry. On a personal level, I dedicate this book to my parents, Marcelo and Jacinta Bruce. I would like to especially thank and acknowledge my sister Evelyn for supporting me in this endeavor, and her twin Eva for serving as my second eye in reviewing this manuscript. As has been in the past, I do not claim originality of the ideas presented in this book, particularly on the techniques that have been established by and adapted from various authorities in the field. Many of the methods described are also being used in the Department of Pathology, University of Miami Miller School of Medicine and Jackson Memorial Hospital. “Histopathologic Techniques” is designed to be a practical reference guide for practicing histotechnologists and students alike. I hope that this book has achieved its purpose. Jocelyn H. Bruce-Gregorios, M.D. Miami, Florida June 2017 TABLE OF CONTENTS 1. 2. 3. 4. 5. 6. Risk Management General safety precautions; Types of Hazards; Chemical Hazards; Labeling; Storage of hazardous chemicals; Physical hazards; Electrical hazards; Biological hazards; Handling spills; First aid measures; Ergonomics; When using a microscope; Maintaining proper posture. Use and Care of the Microscope Compound microscope; Viewing heads; Main framework of compound microscope; Parts of the lens system; Magnification and calibration; Bright field microscopy; Dark field microscopy; Phase contrast microscopy; Polarized light microscopy; Care and maintenance of the compound microscope; Fluorescence microscope; Care and maintenance of fluorescent microscope; Electron microscope; Transmission electron microscope; Scanning electron microscope; Care and maintenance of electron microscope; Radiation safety guidelines. Examination of Fresh Tissue Fine needle aspiration; Core needle biopsy; Incisional biopsy; Excisional biopsy; Punch biopsy; Shave biopsy; Curettings; Teasing or dissociation; Squash preparation; Smear preparation; Streaking; Spreading; Pull-apart; Impression smear; Frozen section; Cold knife procedure; Cryostat procedure; Mounting of tissue block; Freezing previously fixed tissue; Examination of nerve and muscle; Special processing techniques; Freeze drying; Freeze-substitution. Conventional Tissue Processing Fixation; Dehydration; Clearing; Infiltration; Embedding; Sectioncutting; Mounting of tissue cutting; Staining; Automatic tissue processing; Factors that impact processing; Technical considerations. Rapid Tissue Processing Microwave processing; microwave oven; Staining Methods; Vacuum assisted processor; rapid tissue processors; Microwave techniques; Precautionary measures. Fixation Goals of fixation; Objectives of fixation; Methods of fixation; Mechanisms of fixation; Benefits of fixation; Effects of fixatives in general; Characteristics of a good fixative; Types of fixatives; Secondary fixation; Post-chromatization; Washing out; General precautions; Difficulties caused by improper fixation; Fixation artifacts; Lipid fixation; Carbohydrate fixation; Protein fixation; Fixation for electron microscopy; Fixation for immunohistochemistry; Practical consideration; Antigen retrieval; Effect of heat; Microwave fixation. 7. Chemical Fixatives Cross-linking fixatives; Denaturing fixatives; Formaldehyde and formalin; Buffered formalin; Advantages of formalin; Disadvantages of formalin; Factors that influence formalin fixation; Precautions; 10% formol-saline; 10% neutral buffered formalin; Zinc formalin; Formol-sublimate; Paraformaldehyde; Karnovsky’s fixative; Glutaraldehyde; Methyl alcohol; Isopropyl alcohol; Ethyl alcohol; Carnoy’s fixative; Clarke’s solution; Alcoholic formalin; Formol acetic alcohol; Gendre’s fixative; Newcomer’s fluid; Mercuric chloride; Zenker’s solution; Helly’s solution; Lillie’s B-5 fixative; Heidenhain’s Susa; Osmium tetroxide; Fleming’s solution; Chromate fixatives: Chromic acid; Potassium dichromate; Muller’s fluid; Orth’s fluid; Picric acid fixatives: Bouin’s solution; Hollande’s solution; Brasil’s fixative; Glacial acetic acid; Lead fixative; Trichloracetic acid; Acetone; Michel’s solution. 8. Decalcification Acid decalcifying agents; Strong mineral acids; Aqueous nitric acid; Formol nitric acid; Perenyi’s fluid; Phloroglucin Nitric Acid; Hydrochloric acid; Von Eber’s fluid; Formic acid; Formic acidsodium citrate solution; Trichloroacetic acid; Sulfurous acid; Flemming’s fluid; Citric acid-citrate buffer solution; chelating agents; Neutral EDTA; Other techniques; Ion exchange resins; Electrophoresis; Microwave oven decalcification; Factors influencing decalcification; Endpoint of decalcification; Treatment following decalcification; Surface decalcification; Tissue softeners. 9. Dehydration Alcohol; Ethanol; Butyl alcohol; Tertiary butanol; Isopropanol; Pentanol; Acetone; Dioxane; Cellosolve; Triethylphosphate; Tetrahydrofuran; Dehydrating agents for electron microcopy. 10. Clearing Characteristics of a good clearing agents; Xylene; Toluene; Benzene; Chloroform; Cedarwood oil; Aniline oil; Clove oil; Carbon tetrachloride; Tetrahydrofuran; Dioxane; Other xylene substitutes; Terpenes; Limonene; Orange oil; Chlorinated hydrocarbons; Coconut oil; Bleached palm. 11. Impregnation and Embedding Paraffin wax impregnation; Manual processing; Automatic processing; Precautions with automatic processing; Vacuum embedding; Embedding procedure; Practical considerations; Substitutes for paraffin wax; Paraplast; Embeddol; Carbowax; Dimethyl sulfoxide; Celloidin; Nitrocellulose; Gelatin impregnation; Embedding; Embedding molds; Double embedding; Resin embedding; Polyester plastics; Acrylic plastics; Glycol methacrylate; Methyl methacrylate; Practical considerations. 12. Microtomy Rocking microtome; Rotary microtome; Sliding microtome; Freezing microtome; Cold microtome (cryostat); Ultrathin microtome; Care of the microtome; Safety measures; Microtome knives; Honing; Precautions during honing; Stropping; Precautions during stropping; Disposable blades; Glass knives; Diamond knives; Other equipment. 13. Cutting Sections Types of sections; Paraffin sections; Coarse trimming; Fine trimming; Knife clearance and bevel angles; Cutting paraffin embedded sections; Flotation; Mounting sections; Faults/ problems observed during section-cutting; Celloidin embedding. 14. Electron Microscopy Principle of electron microscopy; Transmission electron microscope; Processing of tissue for electron microscopy; Primary fixation; Glutaraldehyde; Paraformaldehyde; Rinsing; Secondary fixation; Dehydration; Infiltration; Embedding; Polymerization; Processing tissue for electron microscopy; Trimming; Ultramicrotomy; Staining ultrathin sections; Lead citrate; Uranyl acetate; Phosphotungstic acid; Problems during processing; Practical considerations; Scanning electron microscope; Fundamental principles of scanning electron 15. 16. 17. 18. microscopy; Preparation of samples for scanning electron microscopy; Cleaning; Drying; Mounting; Gold coating; Radiation safety concerns; Scanning tunneling electron microscope (STEM). Adhesives and Mounting Media Adhesives; Mayer’s egg albumin; Dried albumin; Gelatin; Gelatinformaldehyde mixture; Poly-L-Lysine; APES; Mounting medium; Aqueous mounting media; Glycerin jelly; Farrant’s medium; Apathy’s medium; B run’s fluid; Resinous mounting media; Canada balsam; DPX; XAM; Clarite; Mountants for immunochemical staining; Cover slipping; Ringing; Broken slides. Principles of Staining Staining of paraffin sections; Histological staining; Direct staining; Indirect staining; Accentuator; Mordant; Progressive staining; Regressive staining; Differentiation; Differential staining; Metachromatic staining; Metallic impregnation; Vital staining; Intravital staining; Supravital staining; Hematoxylin and eosin (H&E) staining; Frozen section staining; Precautions in staining; Collodionization of sections; Re-staining of old sections; Histochemical staining; Immunohistochemical staining. Stains and Staining Solutions Natural dyes; Hematoxylin; Cochineal dyes; Orcein; dyes; Acid dyes; Basic dyes; Neutral dyes; Aluminum hematoxylin solutions; Blueing; Ehrlich’s hematoxylin; Harris hematoxylin; Cole’s hematoxylin; Mayer’s hematoxylin; Iron hematoxylin solutions; Regaud’s hematoxylin; Weigert’s hematoxylin; Heidenhain’s hematoxylin; Phosphotungstic acid hematoxylin; Eosin; Aqueous eosin Y; Romanowsky stains; Van Gieson’s stain; Acridine orange; Acridine red 3B; Alcian blue; Alizarin red S; Aniline blue; Azocarmine; Basic fuchsin; Feulgen reagent; Schiff’s reagent; Mallory’s fuchsin stain; Gomori stain; Benzidine; Bismarck brown; Carmine; Giemsa, Gram’s iodine; Masson’s trichrome; Methylene blue; Oil Red O; Osmium tetroxide; Periodic acid Schiff (PAS), Prussian blue, Von Kossa; Wright stain; Lysochromes. Staining of Carbohydrates Periodic Acid Schiff (PAS) reaction; General principles of PAS staining; Schiff reagent; Staining of glycogen; PAS with diastase; Best carmine method; Staining of mucin; Acid mucopolysaccharides; Metachromatic staining; Alcian blue stain; Toluidine blue; Combined Alcian blue-PAS-Hematoxylin stain; Gomori’s aldehyde fuchsin stain; Mucicarmine stain; Colloidal iron technique; Fluorescent acridine orange technique; Neutral mucopolysaccharides. 19. Staining of Lipids Simple lipids; Compound lipids; Derived lipids; Adipose tissue; Lipofuscin; Fat stains and Sudan dyes; Sudan black method; Sudan IV stain for lipids; Oil Red O method; Osmic acid stain for fat; Nile blue sulfate method; Histochemical methods; Free fatty acids; Cholesterol; Cerebrosides; Gangliosides. 20. Staining of Proteins and Nucleic Acids Simple proteins; Conjugated proteins; Derived proteins; Fibrous proteins; Globular proteins; Membrane proteins; Nucleic acids; Principles of staining; Hematoxylin and eosin stain; Histochemical identification of proteins; Alkaline Fast Green method for basic proteins; Peracetic acid-alcian blue for cystine and cysteine; Alcian blue-PAS stain for proteoglycans; Staining of nucleic acids; Feulgen staining for nuclear DNA; Methyl green-pyronin method for RNA and DNA; Fluorescent staining for DNA and RNA; Immunohistochemistry; Antigen retrieval; Electron microscopy; Polyacrylamide gel electrophoresis; In-situ hybridization; Polymerase chain reaction (PCR); Reverse transcription polymerase chain reaction (RT-PCR); In-situ PCR. 21. Enzyme Histochemistry Oxidative enzymes; Dehydrogenases; Staining for succinic dehydrogenase; Oxidases; Cytochrome oxidase; Tyrosinase; Dopa oxidase; Peroxidases; Hydrolytic enzymes; Phosphatases; Alkaline phosphatases; Gomori calcium method for alkaline phosphatase; Acid phosphatase; Gomori lead method for acid phosphatase; 5Nucleotidase; Lead method for 5-nucleotidase; Adenosine triphosphatase (ATPase); ATPase staining pH 9.4, 4.6 and 4.2; Nonspecific esterase; α-naphthyl acetate method for nonspecific esterase; Indoxyl acetate method for nonspecific esterase; Chloroacetate esterase; Acetyl-cholinesterase; Tetrazolium method for monoamine oxidase; Phosphorylase; Aldolase; Sulfatase. 22. Immunohistochemistry Polyclonal antibodies; Monoclonal antibodies; Preparing tissue for immunohistochemistry; Proteolytic enzyme digestion; Paraffin sections; Pre-treatment of tissue sections; Heat-induced epitope removal (HIER); Microwave antigen removal; Pressure cooking antigen removal; Antigens; Epithelial tumor markers; Intermediate filament markers; Neuroendocrine markers; Germ cell tumor markers; Mesenchymal tumor markers; Cell proliferation markers; Cancerassociated genes; Infectious agent markers; Controls; Chromogenic methods; Enzyme labeling; Direct technique; Enhanced polymer onestop staining (EPOS); Indirect technique; Soluble enzyme immune complex technique; Paraffin wax section immunoperoxidase technique; Peroxidase-antiperoxidase (PAP) technique; Blocking unwanted nonspecific staining; Avidin-Biotin Complex (ABC) technique; Labeled Streptavidin Biotin (LSAB) technique; Immunofluorescence method; Direct immunofluorescence technique; Indirect immunofluorescence technique; Frozen section immunofluorescence; In-situ hybridization. 23. Pigments and Minerals Endogenous pigments; Exogenous pigments; Artifact pigments; Hemoglobin; Hemosiderin; Hematoidin; Hematin; Hemozoin; Prussian blue stain; Lillie’s method for ferric and ferrous iron; Perl’s Prussian blue method for hemosiderin; Gomori’s Prussian blue stain for iron; Turnbull’s blue reaction for ferrous iron; Leuco patent blue V stain for hemoglobin; Bile pigments and hematoidin; Modified Fouchet’s technique for liver bile pigments; Gmelin technique for bile and hematoidin; Schmorl’s ferric ferricyanide method for reducing substances; Lipofuscin; Gomori’s aldehyde fuchsin technique for lipofuscin; Mallory’s fuchsin stain for hemofuscin; Melanin; MassonFontana method for melanin; Schmorl’s method; Removal of melanin pigments; Minerals; Calcium deposits on tissues; Modified VonKossa’s method for calcium; Alizarin red S method for calcium; Metal substitution; Copper; Modified Rhodanine technique for copper; Urates and pyrophosphates; Gomori’s methenamine silver stain for urate crystals; Carbon; Formaldehyde deposits; Removing formalin pigments; Mercuric chloride deposits; Osmium tetroxide deposits; Chrome deposits; Silica; Tattoo pigments; Starch or talcum powder. 24. Staining of Bone Marrow and Blood Elements Bone marrow preparations; Bone marrow aspirate; Squash smear; Spread smear; Bone marrow core biopsy; Romanowsky stains; MayGrunwald stain; Jenner stain; Giemsa stain; Wright’s stain; WrightGiemsa stain; May-Grunwald-Giemsa stain; Perl’s Prussian blue stain; Myeloperoxidase stain; Masson’s trichrome stain for GMA plastic bone marrow sections; Ancillary procedures; Lymph node biopsies; Fine needle aspiration; Excisional biopsy; Sentinel lymph node biopsy; Processing lymph node biopsies; Special studies. 25. Staining of Connective Tissue Loose connective tissue; Adipose tissue; Dense connective tissue; Cartilage; Bone tissue; Reticular connective tissue; Elastic tissue; Blood plasma; Reticulin stain; Gomori’s silver impregnation stain; Gordon Sweets’ method; Collagen; Van Gieson’s stain for collagen; Masson’s trichrome stain; Gomori’s one-step trichrome stain; Movat pentachrome stain; Mallory’s aniline blue stain; Azocarmine stain; Elastic stain; Van Gieson stain; Verhoeff’s elastic method; Verhoeff-Van Gieson stain; Aldehyde fuchsin elastic stain; Luna staining method and protocol for elastic fibers and mast cells; Orcein stain; Krajian’s technique; Basement membrane; Jones’ impregnation technique; Fibrin; MSB technique for fibrin; Mallory’s Phosphotungstic acid hematoxylin (PTAH) method; Fibrinoid; Hyalin; Amyloid; Congo red methods; Metachromatic staining; Crystal violet method; Fluorescent staining with Thioflavine-T. 26. Staining of Muscle and Bone Voluntary striated muscle; Involuntary smooth muscle; Striated cardiac muscle; Open muscle biopsies; Needle biopsy samples; Paraffin sections; Cryostat method; Technical considerations; Gomori’s trichrome stain for paraffin sections; Gomori’s trichrome stain for frozen muscle; Mallory’s phosphotungstic acid hematoxylin (PTAH); Periodic Acid Schiff (PAS) stain; Sudan black stain; Oil red O stain; Heidenhain’s iron hematoxylin method; Histochemical stains; Muscle fiber types; ATPase stain; Succinate dehydrogenase stain; NADH stain; α-glycerophosphate dehydrogenase stain; Myophosphorylase stain; Nonspecific esterase; Acid phosphatase; Bone; Schmorl’s picro-thionin method; Ground section preparation of bones; Alizarin red S staining protocol for calcium; Von-Kossa staining protocol for calcium. 27. Staining of Nervous Tissue Central nervous system; Astrocytes; Oligodendrocytes; Microglia; Fixation and processing; Staining techniques; Staining of Nissl bodies; Cresyl fast violet for paraffin sections; Staining of astrocytes; Cajal’s gold sublimate method; Modified PTAH stain for reactive astrocytes; Modified Holzer’s method for astrocytic processes; Staining for oligodendrocytes and microglial cells; Myelin sheath; Weigert-Pal technique for staining normal myelin; Kluver-Barrera Luxol fast blue stain for myelin with Nissl counterstain; Luxol fast blue and H&E stain; Luxol fast blue-PAS-H&E stain; Weil’s method for myelin sheaths; Baker’s chromic-acid hematin method for myelin; Marchi method for degenerating myelin; Microwave modification of Bielschowsky’s technique for neurofibrillary tangles and plaques; Bodian stain for nerve fibers and nerve endings; Sevier-Munger technique; Golgi’s silver staining technique; Modified Golgi method; Glial fibrillary acidic protein; Neu-N antibody staining protocol; Myelin basic protein (MBP) antibody staining protocol; Peripheral nervous system; Fixation and processing; Peripheral myelin in paraffin sections; Methylene blueazure II-basic fuchsin stain; Osmium tetroxide. 28. Staining of Microorganisms Bacteria; Negative staining; Simple staining; Differential staining; Gram stain; Modified Brown-Brenn method; Gram-Twort stain; Mycobacteria; Acid-fast stain; Ziehl-Neelsen stain; Fite stain; Microwave auramine-rhodamine fluorescent technique; Helicobacter pylori; Toluidine blue stain; Cresyl violet acetate method; Legionella pneumophilia; Dieterle method for spirochete; Spirochetes; WarthinStarry method for spirochetes; Steiner and Steiner microwave procedure; Fungi and actinomycetes; Grocott methenamine silver (GMS) stain; Viruses; Lendrum’s Phloxine-Tartrazine method for viral inclusions; Orcein method for hepatitis B-surface antigen; Protozoans; Giemsa stain for parasites. 29. Cytologic Techniques Exfoliative cytology; Smear preparation; Cervical smear; Impression smear; Sputum smear; Bronchoscopy specimens; Smears of gastric secretions and aspirates; Smears of breast secretion; Collection technique; Fine needle aspiration; Slide preparation; Body fluids; Cell suspensions; Preparation of cytospin slides; Urinary tract specimen; Body cavity effusions; Fixation; Wet fixation; Precautions observed during fixation; Staining methods in cytology; Papanicolaou smear; Pap stain procedure for gynecologic specimen; Cells found in cervico- vaginal smears; Vaginal hormonal cytology; Staining procedure for nongynecologic specimens; Modified Papanicolaou staining; MayGrunwald Giemsa stain; Mounting; Immunohistochemistry. CHAPTER 1 RISK MANAGEMENT AND SAFETY IN THE LABORATORY Risk management pertains to the process of ensuring and maintaining personal as well as environmental health and safety in the laboratory. It is everyone's responsibility to minimize risks associated with day-to-day activity by using safety guards and checking the quality of reagents. The first step is to identify all electrical, mechanical and biological hazards that can potentially cause harm in the laboratory. An inventory of chemical reagents must be on hand and obsolete chemicals should be routinely disposed of. Standard operating procedures must be detailed to include control of hazardous substances, risk assessments, and other health and safety information relevant to handling of specimens. One of the most common accidents in the laboratory involves cutting of one's finger or hand on microtome knives. The risk manager should develop a system whereby all incidents and accidents are reported, no matter how small. Each incident should be investigated and, where possible, additional measures should be taken to ensure that the incident does not happen again. A set of written, standardized operating procedures (SOPs) are usually mandated by accrediting or regulatory agencies to ensure that the laboratory is safe. This includes detailed procedures for handling hazardous substances and personal hygiene practices. Records of regulatory compliance, risk assessment, causes and prevention of occupational injury or illness, health and safety training, personal protective equipment and hazardous waste disposal practices must be kept indefinitely. Unidentifiable, questionable, old or obsolete reagents and chemicals in poorly labeled containers should be set aside for disposal. A file of hazardous chemicals from Material Safety Data sheets are now available from databases on the Internet and should be readily accessible in the laboratory. All hazardous agents must be listed and evaluated, including normal use, disposal, and risks associated with spillage. Many laboratories contain significant risks, and the prevention of laboratory accidents requires great care and constant vigilance. The laboratory environment can be a hazardous place to work. Laboratory workers are exposed to numerous potential hazards including chemical, biological, physical and radioactive hazards, as well as musculoskeletal stresses. Many workers are unaware of the potential hazards in their work environment that make them more vulnerable to injury. All laboratories need to have a written program stating the policies, procedures, and responsibilities that serve to protect employees from the health hazards associated with that particular workplace. Measures to protect against laboratory accidents include safety training and enforcement of laboratory safety policies. The following are general safety precautions that must be observed when working in the laboratory: Protect the hands and forearms by wearing either gloves and a laboratory coat or suitable long gloves to avoid contact of the toxic material with the skin. Wash hands frequently throughout the day and before leaving the lab. Procedures involving volatile toxic substances and those involving solid or liquid toxic substances that may result in the generation of aerosols should be conducted in a fume hood or other suitable containment device. The laboratory workplace should be well-ventilated, clean and organized. Smoking, sleeping, eating and drinking are prohibited in the laboratory. Do not store food and drinks in laboratory refrigerators. Do not wear shorts, sandals, or open-toed shoes in laboratory. Minors or personal pets are not permitted in the laboratory. Secure any dangling jewelry, restrain loose clothing, and tie back long hair that might get caught in equipment before starting work. Use of cell phones and music headphones should be avoided while working in the lab. They can be distracting and can increase the potential for an accident to occur. They can also become contaminated if handled while working with hazardous materials. Every instrument used in the laboratory should meet electrical safety specifications and have written instructions regarding its use. Eye wash station, safety shower and first aid kits should be standard facilities in a laboratory. Fire extinguishers, emergency shower systems, emergency eye washers, first aid, emergency blankets, and hoods must be checked monthly. To avoid the unnecessary purchase of chemical materials, a detailed list of chemical materials must be prepared. Only a minimum amount of volatile chemicals must be kept in the laboratory. Chemical material should be stored and safely secured where there is sufficient ventilation. Combustible chemical material must be stored in a heat resistant cabinet. Acids and bases must be separately stored. Every chemical compound used in the laboratory should have a materials safety data sheet on file that specifies the nature, toxicity, and safety precautions to be taken when handling the compound. All chemical material must be labeled with the name, characteristics, danger level, and precautionary measures. Laboratories must have available appropriate protective gears for all individuals: safety devices, goggles, gloves, lab coats, and face-shields. The laboratory must have a method for disposal of hazardous wastes. Collect and seal absorbed material into labelled containers for disposal. Tissues that are collected should be stored in formalin and may be disposed by incineration or by putting them through a "tissue grinder" attached to a large sink (similar to a large garbage disposal unit). Used chemicals must not be released into soil, drains and waterways. Use an absorbent such as sand, “kitty litter” or a commercial product to collect spills and contain spread. One must always be cautious when handling electrical appliances and must be aware of the location of safety devices (fire extinguisher, emergency shower system). Extinguishers with water, carbon dioxide, dry chemical powder or foam are all suitable depending on other products involved in a fire. Fire safety procedures should be posted. There must not be any obstacle in the vicinity of the laboratory door. Avoid handling the sharp ends of instruments. Use forceps or other tools to remove sharp instruments from baskets and autoclaves. Workers should use appropriate hand protection when hands are exposed to hazards such as cuts, lacerations or thermal burns. Laboratory accidents must be documented and investigated with incident reports and industrial accident reports. Obtain medical advice (first aid officer, doctor, poisons information center, ambulance) immediately if major exposure occurs. TYPES OF HAZARDS An important first step in protecting worker health and safety is recognizing workplace hazards. Most hazards encountered fall into three main categories: chemical, physical or biological. Chemical Hazards Cleaning agents and disinfectants, drugs, anesthetic gases, solvents, paints, and compressed gases are examples of chemical hazards. Potential exposures to chemical hazards can occur both during use and with poor storage. The potential for harm or injury could be significant if chemicals are misused or mishandled. The “lab standard” applies to the laboratory use of chemicals and mandates written in the Standard Operating Procedures (SOPs) that address the particular hazards and precautions required for safe use. Explosive chemicals include picric acid. Certain silver solutions may explode upon aging, which is why they should never be stored after use. Oxidizers are harmless by themselves, but may initiate or promote combustion and present a serious fire risk when in contact with certain substances. Examples include sodium iodate, mercuric oxide and chromic acid. Permissible Exposure Limits (PELs), Threshold Limit Values (TLVs), or Occupational Exposure Limits (OELs) are some of the terms used to define the maximum allowable airborne concentration of a chemical (vapor, fume or dust) to which a worker may be exposed. While they represent a concentration at or below which it is safe for most people to work, some individuals may react adversely even below such limits due to hypersensitivity or allergy. Labeling Every chemical should be labeled with certain basic information, including: Chemical name and, if a mixture, names of all ingredients; Manufacturer's name and address if purchased commercially, or name of person making the reagent; Date purchased or made; Expiration date, if known; Hazard warnings and safety procedures. The different types of chemicals include: Irritants are chemicals that cause reversible inflammatory effects at the site of contact with living tissue, especially the skin, eyes and respiratory passages. Corrosive chemicals cause destruction or irreversible alterations when exposed to living tissue, or destroy certain inanimate surfaces (generally metal). A chemical may be corrosive to tissue but not to steel, or viceversa. Few are corrosive to both. Sensitizers cause allergic reactions in some exposed workers, not just in hypersensitive individuals. Sensitization may occur at work because of the high exposure level. Carcinogens are substances that induce tumors, not only in experimental animals but also in humans. Examples of carcinogenic chemicals include chloroform, chromic acid, formaldehyde, nickel chloride and potassium dichromate. Carcinogenic dyes include auramine, basic fuchsin, and any dye derived from benzidine (including Congo red and diaminobenzidine). Toxic materials are capable of causing death by ingestion, skin contact or inhalation at certain specified concentrations. These include methanol, chromic acid, osmium tetroxide and uranyl nitrate. Storage of hazardous chemicals Standard precautions will provide laboratory workers with good protection from most toxic substances. In addition, records that include amounts of material used and names of workers involved should be kept as part of the laboratory notebook record of the project. To minimize hazards from accidental breakage of apparatus or spills of toxic substances in the fume hood, they should be stored in pans or trays made of polyethylene or other chemically resistant material. The apparatus should be mounted above trays of the same type of material. Alternatively, the working surface of the hood can be fitted with a removable liner of adsorbent plastic-backed paper. These materials will contain spilled toxic substances in the absorbent liner and greatly simplify subsequent cleanup and disposal. Any material that comes in contact with toxic substances should be disposed of as a toxic substance. Vapors that are discharged from the apparatus should be trapped or condensed to avoid adding substantial amounts of toxic vapor to the hood exhaust air. Areas where toxic substances are being used and stored must have restricted access, and warning signs must be posted if a special toxicity hazard exists. All volatile substances having high chronic toxicity must be stored in a ventilated storage area. Use a secondary tray or container having sufficient capacity to contain the material in case the primary storage container fails. All containers of substances in this category should have labels that identify the contents and include a warning such as: WARNING! HIGHLY TOXIC OR SUSPECTED CARCINOGEN. Storage areas for substances in this category must have limited access, and special signs should be posted if a special toxicity hazard exists. Any area used for storage of substances of high chronic toxicity must be maintained under negative pressure with respect to the surroundings. Most laboratory chemicals can be safely stored in conventional cabinets. However, storage of chemicals above eye level must be avoided. Dangerous liquids are best stored below countertop height to minimize the risk of bodily exposure in case a bottle is dropped and broken. Dangerous reagents must be stored in plastic or plastic-coated glass bottle. Certain flammable liquids that present unusual fire and explosion risk must never be stored in a refrigerator or freezer unless these appliances are certified as suitable for an explosive atmosphere. Only small quantities must be made available as needed, and they must be used up completely if possible. Do not keep any leftover flammable liquid. Flammable liquids should be stored in cabinets and safety containers that are approved by the Occupational Safety and Health Administration (OSHA). Flammables liquids requiring refrigeration should be stored in either explosionproof or flammable resistant refrigerators and freezers. Most chemicals are readily absorbed through the skin and can cause other health effects and/or contribute to the dose absorbed by inhalation of the chemical from the air. Many studies indicate that absorption of chemicals through the skin can occur without being noticed by the worker. In many cases, skin is a more significant route of exposure than the lung. This is particularly true for non-volatile chemicals which are relatively toxic and which remain on work surfaces for long periods of time. As a general rule during the process of dilution, concentrated acids should be added to water (never water to acid) in order to prevent splashing, and should be done under a chemical fume hood. Hypochlorite solutions are classified as irritants and corrosives. Undiluted bleach solution is corrosive to stainless steel, and thorough rinsing in stainless steel sinks must follow its use to remove the residue. Bleach solutions should not be autoclaved. Never mix different chlorine solutions or store them with cleaning products containing ammonia, ammonium chloride, or phosphoric acid. Combining these chemicals could result in release of chlorine gas, which can cause nausea, eye irritation, tearing, headache, and shortness of breath. These symptoms may last for several hours. A worker exposed to an unpleasantly strong odor after mixing a chlorine solution with a cleaning product should leave the room or area immediately and remain out of the area until the fumes have cleared completely. Cryogens are used to produce substances with temperatures below -153°C (-243°F), such as liquid nitrogen and a boiling point of -196oC (-321°F), that are commonly used in laboratories. Although not a cryogen, solid carbon dioxide or dry ice which converts directly to carbon dioxide gas at -78°C (-109°F) is also often used in laboratories. Cryogens, as well as dry ice, can be hazardous to workers if not handled properly. Dry ice or liquid nitrogen should never be handled with bare hands. Do not pour cold liquid onto the edge of a glass Dewar flask when filling because the flask may break and implode. To dispose of dry ice, allow it to sublimate or evaporate to the atmosphere in a well-ventilated area where CO2 vapor cannot build up. Do not dispose of dry ice in sewers, sinks, or toilets. The extreme cold can fracture ceramic fixtures or crack polyvinyl chloride (PVC) piping. If flushed down plumbing, the gas buildup can cause an explosion. Do not place dry ice in trash cans or similar containers. The extreme cold and resulting condensation can destroy these receptacles. Physical Hazards The most obvious physical hazards are slips and falls from working in wet locations and the ergonomic hazards of lifting, pushing, pulling, and repetitive tasks. Other physical hazards often unnoticed are electrical, mechanical, acoustic, or thermal in nature. Ignoring these can have potentially serious consequences. Many operations in the lab can result in lab workers assuming sustained or repetitive awkward postures such as looking at slides on a microscope for extended periods. What is found acceptable for brief or occasional use may become problematic if performed for long durations or very frequently. Pain is a good indicator that something is wrong. Work must be conducted in a neutral, balanced posture. Containers of sharp objects are found everywhere in pathology laboratories, and following a few safety rules can help prevent accident reports such as getting stuck with a needle or other sharp objects. Only clearly labeled punctureproof and leak proof containers must be used for “sharps”. The container must be replaced when three-fourths full to prevent over-filling. Employees must be trained never to remove the covers of these receptacles or attempt to transfer their content. Inspect all glassware before use. Discard any broken, cracked, or chipped glassware. Many injuries also stem from poor housekeeping. Slips, trips, and falls are very common but can be easily avoided. Start with safe and organized storage areas. Clean the work area throughout the day and before leaving the lab for the day. Keep all aisles and walkways in the lab clear to provide a safe walking surface and an unobstructed exit. Material storage areas should be organized in order not to create hazards. Bags, containers and bundle stored in tiers should be stacked, blocked, interlocked, and limited in height so that they are stable and secured against sliding or collapse. Do not block doors or access to emergency equipment (i.e. fire extinguishers, eyewashes, etc.), emergency shut-offs, and utility controls (i.e. electrical panels). Storage areas should be free from an accumulation of materials that could cause tripping, fire, explosion, or harboring of pests. Work areas must be kept clean and free of unnecessary chemicals. If necessary, clean equipment after use to avoid the possibility of exposing the next person who uses it. Combustibles are substances whose vapors will ignite at or above a certain temperature (or flash point) or in the presence of an ignition source. Combustible liquids pose little risk of fire under routine laboratory conditions, but they will burn readily during a fire. In the USA, OSHA defines "flash point" as 100°F (38°C) while the Department of Transportation defines it as 141°F (or 60.5°C). Flammables have flash points below the temperature specified above, but require specially designed storage rooms, cabinets and containers, to control and prevent vapors from building up around electrical devices that spark. Fire is a serious hazard that one faces in a typical laboratory. While proper procedures and training can minimize the chances of an accidental fire, laboratory workers should still be prepared to deal with a fire emergency when it occurs. In dealing with a laboratory fire, all containers of infectious materials should be placed into autoclaves, incubators, refrigerators, or freezers for containment. Laboratories, especially those using solvents in any quantity, have the potential for causing flash fires, explosion, rapid spread of fire, and high toxicity of products of combustion (heat, smoke, and flame). Electrical Hazards In the laboratory, workers may be exposed to electrical hazards including electric shock, arc blasts, electrocution, fires and explosions. Potential exposures to electrical hazards can result from faulty electrical equipment/instrumentation or wiring, damaged receptacles and connectors, or unsafe work practices. Damaged electrical cords can lead to possible shocks or electrocutions. Electrical hazards are potentially life threatening but can be easily avoided. First, equip all electrical power outlets in wet locations with ground-fault circuit interrupters (GFCIs) to prevent accidental electrocutions. GFCIs are designed to “trip” and break the circuit when a small amount of current begins flowing to ground. Wet locations usually include outlets within six feet of a sink, faucet, or other water source and outlets located outdoors or in areas that get washed down routinely. Specific GFCI outlets can be used individually, or GFCIs can be installed in the electrical panel to protect entire circuits. One will not be protected from electric shock if a 3-pronged plug is not inserted into a 3-prong outlet. Before turning equipment on, all power cords must be checked to be sure that they are in good condition. Another very common electrical hazard is the improper use of flexible extension cords. Avoid using extension cords whenever possible. If you must use one, obtain a heavy- duty one that is electrically grounded, with its own fuse, and install it safely. Extension cords should not go under doors, across aisles, be hung from the ceiling, or plugged into other extension cords. A flexible electrical cord may be damaged by door or window edges, by staples and fastenings, by equipment rolling over it, or simply by aging. Do not use these as a substitute for permanent wiring. The cord insulation should be in good condition and continue into the plug ends. Never repair cracks, breaks, cuts, or tears with tape. Either discard the extension cord or shorten it by installing a new plug end. Take care not to run extension cords through doors or windows where they can become pinched or cut. And always be aware of potential tripping hazards when using them. Use only grounded equipment and tools and never remove the grounding pin from the plug ends. Also, do not use extension cords in a series—just get the right length of cord for the job. If you see a person being electrocuted, DO NOT TOUCH THEM! The electricity can go through you, too. If possible, turn off the power (pull the plug or trip the circuit breaker), or use an item made of non-conductive material (e.g., wooden broom handle) to pry him or her away from the contact. Call 911 immediately. Biological Hazards Biohazards refer to anything that can cause disease in humans, regardless of their source. Biohazards include infectious agents and their toxins as well as contaminated solutions, specimens or objects. Allergens, are one of the most important health hazards, yet they are frequently overlooked. Molds and fungi produce and release millions of spores small enough to be air, water, or insectborne which may have negative effects on human health including allergic reactions, asthma, and other respiratory problems. If biological materials are used in the area, they should not be stored in hallways, in unlocked freezers or in refrigerators. Biohazard signs should be placed in appropriate areas. Pathologists, histotechnologists and technicians may be exposed to a certain level of risk when handling and processing potentially infectious specimen through inhalation of aerosols, contact with non-intact skin and contact with mucous membranes (eyes, nose, mouth). Fresh tissue and body fluids must always be considered potentially infectious, and grossing of specimen has the highest risk of all histological activities. Fixed specimens have a much less risk because nearly all infectious agents are deactivated by histological fixation, although tissues must be thoroughly fixed for this to happen. Complete penetration by alcohol will destroy all infectious agents except prions. Prions are infectious agents that cause spongiform encephalopathies such as Creutzfeld-Jakob disease (CJD), scrapie and mad cow disease. Normal steam sterilization does not inactivate these particles, and common effective treatments like sodium hypochlorite or phenol will create artefacts in tissue. Tissue from patients with suspected CJD can be decontaminated by immersing the specimen in formalin for 48 hours, followed by treatment in concentrated formic acid for 1 hour, and additional formalin fixation for another 48 hours. Small dust-like particles generated from sectioning may become airborne, particularly when performing cryostat sections of fresh tissue. Cryogenic sprays can magnify this risk, and therefore should not be used to freeze potentially infectious tissue. Cutting areas or surfaces may be sterilized with chlorine bleach or a suitable commercial disinfectant, and warning signs should be posted in labs handling infectious materials. Disinfectants should be on hand for sanitizing bench tops and treating spills. Biological safety cabinet(s) must be certified within the last 12 months of use. Handling Spills The laboratory worker must be prepared for potential accidents or spills involving toxic substances. Lab workers must be trained in handling toxic materials and spill clean-up before beginning work with toxic substances. Small spills are defined as those that can be safely handled by the immediate staff. Spill neutralizing and containment kits should be available immediately outside the hazardous work area. These may be commercially purchased or assembled from common materials, and should include protective equipment and clean up aids, such as good quality latex or nitrile gloves similar in thickness to dishwashing gloves, disposable plastic aprons for chemical spills and disposable gowns for biohazards, dustpan and brush for powders, sponges, towels and mops for liquids, adsorbent material (kitty litter or a commercial sorbent), bleach (sodium hypochlorite for biohazards), baking soda for acids, vinegar (5% acetic acid) for alkalis, a commercial neutralizing product, a sealable plastic bucket and heavy plastic bags for containment of the salvaged waste. If the amount of spilled material is limited to a few grams or milliliters, it can be simply wiped off with towel or sponge, while protecting the hands with suitable gloves. The towel or sponge must be disposed of appropriately after use; do not put it into the general trash, and protect the room from its vapors by sealing it within an impermeable plastic bag or container. For significant spills of dangerous materials, all personnel should evacuate the room or immediate vicinity where the accidental spilled occurred, and first aid must be given to anyone who has gotten splashed or is feeling the effects of vapors. If the spill is large, the area must be sealed off and an experienced emergency response team must be called. If there is a major spill outside of the hood, the room or appropriate area should be evacuated and necessary measures should be taken to prevent exposure of other workers. Spills must be cleaned by personnel wearing suitable personal protective apparel. If a spill of a toxic material occurs outside the hood, an air-supplied full-face respirator may be needed. The work space and equipment should be decontaminated with 10% bleach solution. Avoid creating dust. Contaminated pipette tips, tubes, weighing trays, gloves, paper towel, napkins and any other clean up debris must be disposed of as hazardous waste. After removal of gloves, wash hands thoroughly with soap and copious amounts of water. First Aid Measures With laboratory chemicals, the most common accidents requiring first aid are ingestion, eye contact and extensive skin contact. Laboratory technicians and technologists should have basic training in dealing with these situations, and yearly safety training should include first aid information and preparedness in the event of chemical accidents, including accidental ingestion of hazardous chemicals. First aid kits must be easily accessible and refilled on a regular basis. When providing first aid treatment to a person that has been exposed to chemical, infectious or toxic waste products, the following precautions should be observed: • Immediately remove the person from the source of contamination and move to fresh air. • If the person is not breathing, do not use mouth to mouth, or mouth to nose ventilation, because of the danger to the rescuer. Instead, use a resuscitation bag and mask. • If pulse is absent, start external cardiac massage and follow standard Advanced Cardiovascular Life Support (ACLS) guidelines. • Give 100% oxygen by mask if available. • Remove all contaminated clothing and footwear into a sealable collection bag and launder contaminated clothing thoroughly. For accidental skin contact with hazardous chemicals, the affected area should be washed with copious amounts of water for 15-30 minutes. Emergency showers should be as accessible as eye wash stations. If the hazardous substance is not readily water-soluble, use soap with the water wash. Immediately remove contaminated clothing and launder before re-use. Seek medical assistance following skin contact. Splashing of dangerous chemicals into the eyes is also a common accident. Symptoms include redness, pain, blurred vision, and eye damage. All laboratories should be equipped with emergency eyewash stations, either as standing devices or small appliances affixed to sink faucets. Current recommendations are to have such devices no more than 100 feet from hazardous work areas, and the water temperature should be controlled to a range of 15-35°C. In case of accidental splashing, the affected eye should be rinsed for 15-30 minutes, pulling the lids away from the eyeball, prior to seeking emergency health care. Portable eyewash bottles are not recommended because they pour too little liquid and may become contaminated with microorganisms. Ergonomics Laboratory work activities can introduce ergonomic risk factors that are associated with muscular-skeletal disorders. Laboratory-associated ergonomic risks are the same as those found in the office and general industry. These risk factors include awkward or sustained postures, highly repetitive movements, excessive force or strain, contact stresses, and vibration. Awkward postures occur when body parts are positioned away from their neutral position. These postures can put stress on the joint and its associated muscles. Contact stress is a sustained contact between a body part and an external object. Examples include: resting the wrist or forearm against a sharp edge/corner. Duration is the period of time that a body part is exposed to an ergonomic risk factor. Longer durations of exposure increase the severity of the risk. Repetition is the repeated performance of motion that includes other ergonomic risk factors such as force and/or awkward posture. Severity of the risk increases with higher repetition of motions with ergonomic risk factors. Static postures occur when a body part is held in a single position over a long period of time. The severity of a static posture can increase if the posture is awkward, applies continual force, and/or is held for long durations. Examples include: sitting or standing in single position for a long duration. When Using a Microscope Sit close to the work surface. Avoid leaning on hard edges. Keep elbows close to their sides. Adjust chair, workbench, or microscope as needed to maintain an upright head position. Elevate, tilt or move the microscope close to the edge of the counter to avoid bending the neck. Take short breaks. Every 15 minutes, close the eyes or focus on something in the distance. Every 30-60 minutes, get up to stretch and move. Alternate between sitting and standing positions. When possible, plan work tasks to include a variety of movements to avoid static postures or repetitive motions. Avoid contacting or resting wrists or forearms on sharp edges. When seated, the thighs should be parallel to the floor and feet firmly planted on the floor or on a foot rest. Maintaining proper posture: Keep your back straight, maintain all 3 natural curves in your spine. Distribute your weight evenly on both hips. Keep your head and neck aligned over your shoulders. Sit back in your chair; your back should be supported by the seat back. Adjust your chair height so that your hips are slightly higher than your knees. Be sure your feet are supported by the floor or a footrest. Avoid sitting for long periods of time; get up from your chair at least once every hour. Do not twist or bend your back from a seated position. REFERENCES Banks I, Gamble M. (2002) Managing the Laboratory, Chapter 1. In: Bancroft J.D. and Gamble M, eds. Theory and Practice of Histological Techniques, 2nd ed. London: Churchill Livingstone, IL. Berte LM. (2000) New Quality Guidelines for Laboratories. Medical Laboratory Observer, March 2000. "Biological Agents and Biological Toxins". Occupational Safety and Health Administration. Brown P, Gibbs CJ, Gajdusek D, Cathala F, LaBauge R. (1986) Transmission of Creutzfeldt-Jakob disease from formalin-fixed, paraffin-embedded human brain tissue. N Engl J Med 315:1614–5. Centers for Disease Control. (1988) Guidelines for Protecting the Safety and Health of health care workers, CDC Publication # 88-1 19. Washington DC: US Government Printing Office. Dapson RW. (2002) Safety in the laboratory. In: Bancroft, J.D., Gamble, M. Theory and Practice of Histological Techniques, 5th Ed, London: Churchill Livingstone, 1: 1-32. Dapson JC, Dapson RW. (1995) Hazardous Materials in the Histopathology laboratory: regulations, risks, handling and disposal. 3rd Ed. Battle Creek, MI: Anatech ·Ltd. ES&H Manual. (2015) Chapter 29: Safe Handling of cryogenic liquids". Lawrence Berkeley National Laboratory. Personal Protective Equipment (PPE)". Identifying and Evaluating Hazards in Research Laboratories. (2013) Guidelines developed by the Hazards Identification and Evaluation Task Force of the American Chemical Society’s Committee on Chemical Safety: American Chemical Society. Jungbauer FH, van der Harst JJ, Groothoff JW, Coenraads PJ. (2004) Skin protection in nursing work: promoting the use of gloves and hand alcohol. Contact Dermatitis 51:135–40 Kiernan JA. (l999) Histological and Histochemical Methods: Theory and Practice. Laboratory Safety PPE | Yale Environmental Health and Safety". www.ebs.yale.edu. Lunn G, Sansone EB. (1990) Destruction of hazardous chemicals in the Laboratory. New York: John Wiley. Masterton R, Teare L, Richards J. (2002) Hospital Infection Society/Association of Medical Microbiologists. Towards a Consensus II. Workshop I. Hospital-acquired infection and risk management. J Hosp Infect 51:17–20. Montgomery L. (1995) Health and Safety Guidelines for the Laboratory - Chicago: American Society of Clinical Pathologists Press. National Committee for Clinical Laboratory Standards. (1989) Guidelines for Laboratory Safety, Document GPJ7- P. Villanova, PA: NCCLS. National Research Council. (1989) Prudent Practices for Disposal of Hazardous Chemicals from Laboratories. Washington, DC: National Academy Press. Rutala W, Weber D. (1997) Use of inorganic hypochlorite (bleach) in healthcare facilities. Clin Microbiol Rev: 597–610. Sitwell LB, Attack E, Izukawa D. (1988) Creutzfeldt-Jakob disease in histopathology technicians. N Engl J Med 318:854. "Stanford University: SLAC Environment, Safety, and Health Manual, Chapter 36, Stanford University. https://en.wikipedia.org/wiki/Laboratory safety Teare EL, Masterton RG. (2003) Risk management in pathology: J Clin Pathol. 56(3): 161–163. Wilkins D WA, Cossar YE, Miller DC. (1988) Creutzfeldt-Jakob disease in histopathology technicians. N Engl J Med 318:853–4. https://www.lanl.gov/safety/electrical/docs/elec_hazard_awareness_study_guide: "Fire Hazards control". https://www.utexas.edu/safety/ehs/lab/manual/4_guidelines.html http://www.kostic.niu.edu/labsafetyrules.html https://www.osha.gov/Publications/laboratory/OSHAfactsheet-laboratory-safety-ergonomics.pdf . CHAPTER 2 USE AND CARE OF THE MICROSCOPE The microscope is one piece of equipment that is used by both the pathologist and the histotechnologist. The pathologist examines the slide under the microscope to identify a disease process or an abnormality that will directly affect the patient's treatment. The histotechnologist examines the same slide microscopically for quality control to determine whether all technical processes are done properly and if a slide of diagnostic quality has been achieved. It is therefore important for the histotechnologist to be knowledgeable and skilled in the use of the microscope. The microscope enlarges images and allows the visualization of morphologic cellular details that are too small to be seen by the naked eyes. With the aid of lenses, the unstained section allows the majority of light to pass through, but without adequate distinction between various tissue structures. Stains and dyes are used to give contrast to the tissue by creating light absorption of varying degrees, uniquely taken up by each tissue element, and seen microscopically as colors. To be useful, a microscope must accomplish three things: (1) it must magnify the object, (2) it must resolve the details of the object, and (3) it must make these details visible. There are many types of microscopes. The most common (and the first to be invented) is the optical compound microscope, which uses light to image the sample. Other major types of microscopes are the electron microscope (both the transmission electron microscope and the scanning electron microscope), the ultra-microscope, and the various types of scanning probe microscope. COMPOUND MICROSCOPE A compound light microscope is a microscope with more than one lens and its own light source. In this type of microscope, there are ocular lenses in the binocular eyepieces and objective lenses in a rotating nosepiece closer to the specimen. Because it contains its own light source at its base, a compound light microscope is also considered a bright field microscope, which means that the specimen is lit from below and viewed from above. Illumination comes from below and contrast in the sample is caused by absorbance of some of the transmitted light in dense areas of the sample. Bright-field microscopy is the simplest and most popular of all techniques used for illumination of samples in light microscopes. The typical appearance of a bright-field microscopy image is a dark sample on a bright background, hence the name. With bright field illumination, the sample’s contrast comes from its absorption of the light, as opposed to dark field illumination where the contrast comes from the sample scattering the light. The compound microscope consists of the lens system condenser, objective and ocular. The condenser brings the parallel rays of light to a point of focus in the plane of the object. The objective magnifies the object being viewed and focuses a real image in the upper part of the body tube. The ocular further magnifies the image formed by the objective. To effectively use the microscope, it is necessary to know its parts and basics of magnification. The compound microscope currently in use for surgical pathology consists of its framework and its two separate lens system. Viewing Heads Monocular Heads - only use one eyepiece when viewing the specimen. You are restricted if you want to use an LCD camera because this would occupy the eyepiece. However, monocular microscopes are light weight and are inexpensive. Binocular heads have two eyepieces and are more convenient and comfortable to use. It is the most common choice. Trinocular Heads - have a third eyepiece tube that can be used by another person simultaneously or by an LCD camera. The trinocular option is more expensive than the other two types. Usually the heads can be set to a 45 degree or a 30 degree angle with sliding or hinge adjustment for inter-pupillary distance. These options are based on individual preference. The main framework of the Compound Microscope consists of: 1. Base -provides support for the microscope. The base should be large and solid enough to allow the microscope to stand by itself. 2. Arm - supports and holds the magnifying and adjustment system. It can be used as a handle for carrying the microscope. 3. Stage - is the flat platform where the slide is placed for examination. 4. Substage - is located directly under the stage and holds the condenser and diaphragm. 5. Mechanical Stage - permits movement of the stage while holding the slide in the phase of focus. The parts of the lens system are: 1. Nosepiece - is located at the end of the body tube for holding the objectives. 3. Objectives - consist of a system of lenses located at the end of the body tube that is held in place by the nosepiece and is closer to the slide under examination. The purpose of the objective is to increase or decrease magnification. The objectives are mounted on a revolving turret allowing for the change of objectives. When one objective is focused on the turret, all lenses will be approximately in focus. If this is true, the microscope is said to be Par focal. 4. Focal length - is the distance between outer lens of objective and the cover glass of the slide under examination. Fig. 2-1. Compound Microscope Magnification and Calibration Magnification is the process that increases the size of the structure under examination. It is achieved by the use of the microscope's lens system. The total magnification of a microscope is the product of the magnifying power of the objective and eyepiece, with a normal tube length of 160 mm. Example: Objective 40 x Eyepiece 10 Total Magnification 400 x If the microscope is fitted with a draw tube, the body tube length will be increased, and the body tube magnification will also be correspondingly increased. Example: Objective = 40x Eyepiece = 10x Working Tube Length = 180 mm. Normal Tube Length = 160 mm. Objective x Eyepiece x Working Tube Length = Magnification 40 x 10 x 1.25 (180mm/l60mm) = 450x Usually the light source, a light bulb, is built into the base below the substage. The enclosed light source provides a dependable, permanently adjusted, full field illumination for all objectives without refocusing the condenser. Critical microscopy requires a lamp with condensing lens and a diaphragm. The source of illumination should be uniformly intense. It should completely flood the back lens of the condenser with light when the lamp iris diaphragm is open. The object being examined should appear as if it were selfilluminating, without shadows or dark and light areas. Proper illumination requires that the condenser, illuminator, objective and ocular be precisely aligned for the passage of the cone of light. The iris diaphragm of the condenser should also be adjusted for the passage of the light to the object under examination. The condenser located in the substage receives light rays from the source of illumination and forms a cone of light that can be focused on the objective under study by raising or lowering the condenser. For maximum resolution, the cone of light must be wide enough to fill the back of the lens being used. The iris diaphragm of the condenser can be opened or closed to accommodate differing amounts of light for each objective. The resolving power of an objective is its ability to allow the examiner to see two particular points that are close together, as separate and distinct. The amount of detail magnified by the microscope depends on the cone of light that can be collected by the objective. Bright Field Microscopy Bright field microscopy is generally used in compound microscopes, where light is either passed through, or reflected off, a specimen. Illumination is not altered by devices that alter the properties of light (such as polarizers or filters). The name "bright field" is derived from the fact that the specimen is dark and contrasted by the surrounding bright viewing field. Simple light microscopes are sometimes referred to as bright field microscopes where a specimen is placed on the stage of the microscope and incandescent light from the microscope’s light source is aimed at a lens beneath the specimen. This lens is called a condenser. The condenser usually contains an aperture diaphragm to control and focus light on the specimen; light passes through the specimen and then is collected by an objective lens situated in a turret above the stage. The objective magnifies the light and transmits it to an oracular lens or eyepiece and into the user’s eyes. Some of the light is absorbed by stains, pigmentation, or dense areas of the sample and this contrast allows you to see the specimen. Dark Field Microscopy Dark Field illumination is a technique used to observe unstained and transparent samples causing them to be clearly visible and appear brightly lit against a dark, almost purely black background. In bright field illumination, the object is lit from below the stage, resulting in a larger, contrasted image that can be studied. A dark field microscope blocks this central light with a condenser so that only oblique rays hit the object. The principal elements of dark field illumination are the same for both stereomicroscopes and more conventional compound microscopes. Illumination of specimens by dark field requires blocking out of the central light rays along the optical axis of the microscope, which ordinarily pass through and around (surrounding) the specimen. Blocking these light rays allows only those oblique rays originating at large angles to strike the specimen positioned on the microscope stage. When a transparent specimen is placed on the glass microscope stage and observed under dark field illumination, the oblique light rays cross the specimen and are diffracted, reflected, and/or refracted by optical discontinuities (such as the cell membrane, nucleus, and internal organelles) allowing these faint rays to enter the objective. The specimen then appears bright on an otherwise black background. Phase Contrast Microscopy Phase contrast microscopy is an optical microscopy illumination technique in which small phase shifts in the light passing through a transparent specimen are converted into amplitude or contrast changes in the image. It is a type of light microscopy that enhances contrasts of transparent and colorless objects by influencing the optical path of light. The phase contrast microscope is able to show components in a cell or bacteria which would be very difficult to see in an ordinary light or bright field microscope. This microscope technique makes it possible to study the cell cycle in live cells. It reveals many cellular structures that are not visible with a simpler bright field microscope and makes it possible for biologists to study living cells and how they proliferate through cell division. The use of phase contrast does not require staining to view the slide. Fig. 2-2. Phase Contrast Microscope Polarized Light Microscopy The polarized light microscopy is a contrast-enhancing technique that improves the quality of the image obtained with birefringent materials when compared to other techniques such as bright field microscopy, phase contrast microscopy and dark field microscopy. It is designed to examine specimens that are visible primarily due to their optically anisotropic character. It has two essential components: (1) The polarizer situated below the specimen stage usually fixed in the left-to-right, East-West direction, although this is usually rotatable through 360 degrees. (2) The analyzer, usually aligned North-South but again rotatable on some microscopes, is located above the objectives and can be moved in and out of the light path as required. Since the components of a birefringent, anisotropic sample (e.g., urate crystals, striated muscle, amyloid) are aligned at different angles, rotating the polarizer will cause crossed polarizer alignment (where polarization directions of the polarizer and analyzer are 90 degrees apart), and produce kaleidoscopic colors as a result of the interference between light waves passing through the specimen. Care and Maintenance of the Compound Microscope The microscope is a delicate, precisely aligned instrument. A skilled individual should perform preventive care and maintenance of the microscope. Only if the instrument is used correctly and maintained regularly is it capable of producing the best image data possible. Careless, incorrect operation and maintenance techniques not only result in unreliable and poor quality images, but also cause productivity at the microscope to suffer, and the instrument's useful lifetime to be greatly reduced. Always support the microscope when carrying. It should be cradled - one hand holding it by the arm, the other supporting the base. The best way to carry a microscope is in its case. Never disassemble the microscope as doing so may cause electric shock or damage to the microscope. To avoid electric shock or damage to the instrument, unplug the microscope before replacing the bulb. Use only the prescribed halogen or fluorescent bulb. Allow the halogen bulbs to cool before touching. Halogen bulbs become extremely hot and may cause burns if touched. Keep the microscope covered when not in use. Microscope life is extended when they are covered during storage. This should be done even if they are stored in a cabinet. Among several types of plastic cover, those made of softer more flexible material are probably less prone to dust. Lint-free fabric covers are also available, and provide an effective dust barrier that can minimize the need for cleaning the microscope. Never store a microscope with the eyepiece removed or uncovered, since dust will collect in the body tube and be very difficult to clean. Keep the body tube sealed at all times. A microscope that remains unused for a lengthy period of time can accumulate dust and debris from the air. This is aggravated by leaving the instrument uncovered, which can lead to deterioration of image quality even though the instrument may be practically new. Keep the microscope in a dry place. Do not store the microscope in direct sunlight. Sunlight can influence the quality of the specimen imaging. In humid or moist environments, it is advisable to store the microscope in a waterproof container with a drying agent. Never touch the optical lens with bare fingers. Your body produces an oil that smudges the glass. This oil can even etch the glass if left on too long. Use only LENS PAPER to clean the glass. Toilet Paper, Kleenex, and paper towels have fibers than can scratch the lenses. Blemishes such as dust, lint, and smudges on the optical components, as well as scratches in the lenses, filters, prisms, mirrors, and faceplate of the image sensor, tend to degrade overall microscope performance. Dirt must be removed from the microscope frame and mechanical parts by dabbing with a moist paper towel. Dirt that is non-adherent may be removed from less delicate lens surfaces by gentle brushing with a clean camel hair brush or by an air blower, but it must be assured that no oil or similar spray is released from the compressed gas can. Clean smudges, fingerprints, oils, and other contaminants from the lens with clean lens paper or a soft clean cloth moistened with a small amount of absolute alcohol-ether mixture. If an alcohol-ether mixture is unavailable, use isopropyl alcohol. The top lens of the eyepiece should be polished to remove dust or finger marks, and the microscope should be checked for critical illumination. Lenses should be wiped daily and as necessary with fresh lens paper (rough paper or cloth will cause scratching of the lens). Rotation of the eyepiece will show if any dust is present. If so, the eyepiece may need to be dismantled and both lenses cleaned. Substage condenser should be checked for dust. If dust is present on the condenser, the object being viewed will come in and out of focus when racked up and down – always focus UP! The use of immersion oil is essential in maximizing the microscope’s optical performance, but its improper use or failure to immediately remove the oil after each use constitutes the most serious contaminant that must be dealt with in instrument maintenance. Oil that has been stored for more than one or two years may not perform optically the same as fresh oil, and a potential increase in viscosity often makes it more difficult to remove. Consequently, containers of immersion oil should be labeled with the date received, and discarded when necessary. Immersion oil should always be wiped from all surfaces immediately after use even if additional slides are going to be observed. The practice of simply adding additional drops of oil when changing to the next slide results in excess oil accumulating on the microscope. Immersion oil is most safely removed using only lens tissue, without employing any solvents. In the event immersion oil is allowed to harden, moisten a piece of lens paper with a small amount of xylene and use this to re-dissolve and remove the hardened oil. Note: Xylene may leave a film on the lens and may dissolve the cement used to seal the immersion objective. To prevent this, always moisten a second lens paper with alcohol and use it to remove any residual xylene. Repeated use of xylene will destroy lens coatings. Breathe gently on the lens with the mouth open, so that no saliva droplets are expelled. If possible, the mouth should be positioned beneath the level of the objective to further reduce any possibility of droplets landing on the lens. With moisture condensed from the breath as a lubricant and solvent, a fresh piece of lens tissue is used to wipe the lens surface in a circular motion. Optical components should not be immersed in any solvent, and cleaning tissues should only be moistened, never saturated, with a cleaning solution. FLUORESCENCE MICROSCOPE A fluorescence microscope refers to any microscope that uses fluorescence to generate an image. In fluorescence microscopy, many wavelengths of light, ranging from the ultraviolet to the visible can be used to cause samples to fluoresce and allow viewing by eye or with the use of specifically sensitive cameras. When certain compounds are illuminated with high energy light, they emit light of a lower frequency. This effect is known as fluorescence. The fluorescence microscope is a precision instrument intended for microscopic detection of tubercle bacilli in specimens in the routine diagnostic TB laboratory. The use of fluorochromes for staining allows smear examination at lower magnification than is used for light microscopy. Because of the lower magnification, each field examined under fluorescence microscopy is larger in area than that seen with light microscopy, thus reducing the time needed to examine a slide. Fluorescence microscopy requires intense, near-mono-chromatic, illumination which some widespread light sources, like halogen lamps cannot provide. Four main types of light source are used, including xenon arc lamps or mercury-vapor lamps with an excitation filter, lasers, and high-power LEDs. This method can be extremely sensitive, allowing the detection of single molecules. Many different fluorescent dyes can be used to stain different structures or chemical compounds. One particularly powerful method is the combination of antibodies coupled to a fluorophore as in immunostaining. Examples of commonly used fluorophores are fluorescein or rhodamine. Unlike transmitted and reflected light microscopy techniques, fluorescence microscopy only allows observation of the specific structures which have been labeled for fluorescence. For example, observing a tissue sample prepared with a fluorescent DNA stain by fluorescent microscopy only reveals the organization of the DNA within the cells and reveals nothing else about the cell morphologies. Fig 2-3. Fluorescence Microscope Care and Maintenance of a Fluorescence Microscope • Do not place the microscope where it could be exposed to direct sunlight, dust, vibration (e.g. from centrifuges), water (sink, spray from a tap), chemical reagents, or humidity. • It may be possible to repair a faulty microscope by replacing easily removable parts (objectives, eyepieces, light bulbs, fuses); if this does not work, the microscope should be entrusted to a competent person for repair. Never dismantle the microscope. • Accumulated dust within a microscope can deteriorate image quality. Keep all openings covered with dust caps so that dust does not enter the microscope and settle on inaccessible lenses, mirrors, and prisms. If you do not have any dust caps, cover the openings with tape. Remove dust off of the scope’s stage, base, and body with a damp cloth. If necessary, clean off any immersion oil or glycerol smears with ethanol or Sparkle. • Remove both eyepieces and clean their surfaces with a Kimwipe and Sparkle. Blow any dust or dirt out of the insides with an air blower. Fluorescent bulb can be changed only after the light source has been turned off for 30 minutes and the lamp housing is only warm to the touch. It is recommended that the fluorescent bulb be changed after 100 hours of use. This can be observed in the timer located in the fluorescent light power box. The timer should be re-set each time the fluorescent bulb is changed. When changing the 50W mercury fluorescent bulb, do not handle the glass bulb portion but rather handle the metallic base and top of the bulb. If the bulb portion is handled, make sure to wipe it off gently using a tissues moistened with alcohol. Do not touch the lamp with the fingers. Smudges and dirt on the glass bulb will interfere with the light path and will affect the quality of the fluorescence. If the blue light remains weak after a new lamp has been fitted and properly adjusted, there may be another problem such as a blackened heat filter. Discontinue use of the microscope and request repair by a specialist. The light source for the fluorescent light must be switched on and allowed to warm-up for 5 minutes prior to use. Once the fluo-rescent light has been turned on, it cannot be turned off in less than 15 minutes. Make sure to close the shutter slider to shut-off the fluorescent light temporarily during interruption while reading slides to prevent fading of specimen’s fluorescent intensity, and to prolong the life of the burner and the bulbs by avoiding frequent on/off switches. Do not work at the microscope/computer for more than 2 hours without taking a break. Fixed specimens must be mounted with a coverslip, and be sealed, clean and dry. This means that slides must be free from excess mounting media and that nail varnish must have had at least 60 minutes to set. ELECTRON MICROSCOPE An electron microscope is a microscope that uses a beam of accelerated electrons as a source of illumination. Because the wavelength of an electron can be up to 100,000 times shorter than that of visible light photons, the electron microscope has a higher resolving power than a light microscope and can reveal the structure of smaller objects. In many ways, an electron microscope functions similarly to an optical scope except that, instead of visible light, a stream of electrons is used to illuminate the specimen. The electron beam is focused with magnetic lenses. Electron guns emit a flow of electrons of a considerably shorter wave length than visible light and this fact allows an electron microscope to have higher resolution and magnification. Transmission Electron Microscope Transmission Electron Microscope (TEM) works on the same principle as an optical microscope but uses electrons instead of light and electromagnets instead of glass lenses. Use of electrons instead of light allows a much higher resolution, giving a two-dimensional view. Thin slices of specimen are obtained. The electron beams pass through this. It has high magnification and high resolution. A transmission electron microscope can achieve better than 50 nm resolution and magnifications of up to about 10,000,000 x whereas most light microscopes are limited by diffraction to about 200 nm resolution and useful magnifications below 2000 x. Fig. 2-4. Transmission Electron Microscope Scanning Electron Microscope A Scanning Electron Microscope (SEM) uses electron illumination and looks at the surface of bulk objects by scanning the surface with a fine electron beam. The image is seen in 3-D. It has high magnification and high resolution. The specimen is coated in gold and the electrons bounce off to give you an exterior view of the specimen. The pictures are in black and white. Fig. 2-5.Scanning Electron Microscope Because the SEM image relies on surface processes rather than transmission, it is able to image bulk samples up to many centimeters in size and (depending on instrument design and settings) has a great depth of field, and so can produce images that are good representations of the three-dimensional shape of the sample. Another advantage of SEM is its variety called Environmental Scanning Electron Microscope (ESEM) that can produce images of sufficient quality and resolution with the samples being wet or contained in low vacuum or gas. This greatly facilitates imaging biological samples that are unstable in the high vacuum of conventional electron microscopes. Care and Maintenance of the Electron Microscope After long hours of use, contamination may form in the electron beam path in the column due to the accumulation of particles of sample and because of outgassing from evacuated sections. Periodic maintenance by the manufacturer’s service engineers is required to keep each unit of the evacuation system operating correctly so as to maintain the high vacuum. • Never attempt any routine maintenance task without thinking of the possible hazards involved with that task. • Switch off the high voltage and use a vacuum trip to immobilize the high voltage supply when air is let into the gun. • The electron gun is also a source of x-rays. If the gun or condenser area is dismantled for any reason, ensure that it is checked for radiation leaks prior to using the instrument. • Constantly check the rotary pump’s filter. If it becomes discolored or moist with oil, change it! If it smells oil when pumping out a vessel, check the filter and the oil. • The scanning electron’s sputter coater is constantly pumping against the gases given off by specimens and their adhesives. It will be the most contaminated of all the rotary pumps. Even a good filter may be inefficient when the pump oil is severely contaminated, so be sure to have the pump oils changed at least every year. Make sure that the instrument is switched off when changing fuses. Make sure that the rotary pump is switched off before commencing maintenance (belt burns hurt). Use the instrument within the application range and by the method specified in the catalog, instruction manual and other relevant document from the manufacturer. When using the electron microscope, make sure that: The condenser lens movable aperture is completely pulled out from the column. Emission current is greater than 20 µA flowing. Movable aperture is inserted for the purpose of interrupting the electron beam. Unlocking safety devices are used. Filament exchange, specimen exchange, film exchange, and mild baking of the column are maintenance items to be carried out by the user. If filament is broken, loosen the filament centering screw, detach and replace the broken filament, using the protocol supplied by the manufacturer. Observe the following precautions in the use of the side-entry specimen holder: If the specimen is not held firmly by the grid retainer, it will be susceptible to vibration and specimen drift may occur. Also, the specimen may drop into the tilting device. Contamination on the vacuum part of the holder may cause specimen charge-up or contamination and/or specimen drift. Contamination on the O-ring may cause a drop in vacuum level at specimen insertion or unsmooth movement of the specimen stage. Contamination or scratch on the sapphire tip of the holder could result in unsmooth movement of the specimen stage. About once a month, clean especially the vacuum part of the holder tip with gauze that is moistened with absolute ethanol. After cleaning, dry it completely with a dryer. Check for abnormal vibration and sound daily. If there is an abnormality, contact the service engineer. When the compressor is not operated for a long time, the lifetime of the grease used will be shortened due to humidity, so evacuation should be carried out for at least 30 minutes once a month. Troubleshooting of the air compressor by the user should be confined to confirming the symptoms. Inspection and repair by a person other than the service engineers may result in loss of a part related to safety. Insufficient amount of oil can cause a drop in pump performance. And too much oil can result in the oil spattering out. A suitable amount should thus be provided. The oil should normally be changed within 6 months, but if water vapor or a gas harmful to oil has been evacuated, the oil will deteriorate more quickly and cause a drop in pump performance, in which case the oil should be changed more frequently. If the water temperature differs from the room temperature, condensation will form on the cooled sections and this will lead to corrosion. If the difference from room temperature is 5°C or greater, the optional cooling water circulator should be utilized. Check if the cooling tap water flow at the outlet side is low versus the opening of the water supply tap, or if the water temperature is abnormally high. When a filter is used at the water supply side, check the filter for contamination or clogging. When using a cooling water circulator, check for cleanliness of the circulated water, and if contaminated, replace it with distilled water. Contamination of the movable apertures will cause the symptoms explained below and result in image disturbance. Cleaning of the apertures must be done periodically or whenever image disturbance occurs. The lithium battery must be handled separately from general waste matter. When lithium battery replacement is required, be sure to contact the dealer from whom you purchased the instrument or your nearest manufacturer service agent. Entrust the replacement to a qualified service engineer. Axial alignment of the column and electron gun should be carried out at filament exchange or when disassembling the column for cleaning, etc. Since the column axis may deviate, its alignment must be performed by trained technicians or service engineers. Radiation Safety Guidelines for Scanning Electron Microscope (SEM) The radiation safety concerns are related to the electrons that are backscattered from the sample, as well as X-rays produced in the process. Scanning electron microscopes are radiation-generating devices and should be at least inventoried. It is important that the integrity of the shielding is maintained, that all existing interlocks are functioning, and that workers are aware of radiation safety considerations. Safety evaluations should be performed initially when machine is purchased and after machine has been moved. Each machine should be key controlled when not in use. Interlocks, if present, must remain operational unless approved by the Radiation Safety Officer. Shielding must be sufficient to maintain exposure rates less than 0.5 mrem/hr at 5 cm. The SEM user should keep logbook of any maintenance done on machine. The Radiation Safety Officer must be notified if any modifications are made to the interlocks or any other safety devices. The SEM user should also keep a copy of operating and emergency procedures at the accelerator panel. No survey meters or personnel dosimetry are required. REFERENCES Abramowitz A. (1987) in Microscope: Basics and Beyond, The Olympus Corporation, Melville, New York, pages 11-13, 21-26. Boundless. “Dark-Field Microscopy.” Boundless Microbiology. Boundless, Retrieved Aug. 2015. https://www.boundless.com/microbiology/textbooks/boundless-microbiology-textbook/microscopy3/other-types-of-microscopy-30/dark-field-microscopy-244-343. Bradbury S. (1989) An Introduction to the Optical Microscope, Oxford Science Publications, Oxford, United Kingdom, pages 49-57. Bradbury S, Bracegirdle B. (1998) Introduction to Light Microscopy: Microscopy Handbooks, Volume 42, BIOS Scientific Publishers - Springer, Oxford, United Kingdom, pages 69-76. Burgess J. (1987) Under the Microscope: A Hidden World Revealed. CUP Archive. p. 11 Chapman SK. (1986) Maintaining & Monitoring the Transmission Electron Microscope, Oxford University Press, pp 37-39. Douglas B, Murphy. (2002) Fundamentals of light microscopy and electronic imaging. Wiley/IEEE. p. 64. Herman B. (1998) Fluorescence Microscopy, BIOS Scientific Publishers - Springer, Oxford, United Kingdom, pages 17-20. Inoué S, Oldenbourg R. (1995) in Handbook of Optics, Volume II, Bass, M. (ed.), McGraw-Hill, New York, pages 17.12-17.20. Inoué S, Spring K. (1997) Video Microscopy: The Fundamentals, Plenum Press, New York, pages 4959. Keller E. (1998) Cells: A Laboratory Manual, Volume 2: Light Microscopy and Cell Structure, Spector, D., Goldman, R., and Leinwand, L. (eds.), Cold Spring Harbor Press, Cold Spring Harbor, New York, pages 94.9-94.21. Maintenance and repair of laboratory, diagnostic imaging and hospital equipment. Geneva, World Health Organization, 1994. Maintenance manual for laboratory equipment. (2008) 2nd ed. Geneva, World Health Organization. Manual of basic techniques for a health laboratory. (2003) 2nd ed. Geneva, World Health Organization. Marmasse C. (1980) Microscopes and Their Uses, Gordon and Breach, New York, pages 57-106. McCrone W, McCrone L, Delly J. (1984) Polarized Light Microscopy, McCrone Research Institute, Chicago, pages 15-19. McLaughlin R. (1997) Special Methods in Light Microscopy, Microscope Publications, Ltd., Chicago, pages 3-19. Meek GA. (1977) Practical Electron Microscopy for Biologists, John Wiley and Sons, pp 45-46. Ming Chiang Li. (1980) "Electron Interference". L. Marton and Claire Marton. Advances in Electronics and Electron Physics 53. Academic Press. p. 271. Needham G. (1958) The Practical Use of the Microscope, Charles C. Thomas, Springfield, Illinois, pages 230-256. Petrak LJ, Waters JC. (2014) A Practical guide to microscope care and maintenance. In Methods in Cell Biology Chapter 4, Vol 123, pp 55-76. Pluta M. (1988) Advanced Light Microscopy, Volume 1: Principles and Basic Properties, Elsevier, New York, pages 179-239. Pluta M. (1989) Advanced Light Microscopy vol. 2 Specialized Methods, Elsevier. Richardson J. (1991) Handbook for the Light Microscope: A User's Guide, Noyes Publications, Park Ridge, New Jersey, pages 52-80. Rost F, Oldfield R. (2000) Photography with a Microscope, Cambridge University Press, Cambridge, United Kingdom, pages 70-82. Shimizu Y, Takenaka H. (1994) Advances in Optical and Electron Microscopy, Volume 14, Academic Press, New York, pages 249-334. Spencer M. (1982) Fundamentals of Light Microscopy, Cambridge University Press, New York, pages 63-69. Zernike F. (1955) "How I Discovered Phase Contrast". Science 121 (3141): 345–349. www.microscopemaster.com/different-types-of-microscopes.html www.cas.miamioh.edu/mbiws/microscopes/compoundscope.html www.fei.com/introduction-to-electron-microscopy/ www.who.int/entity/diagnostics_laboratory/documents/guidance/guidance2/en/) CHAPTER 3 EXAMINATION OF FRESH TISSUE Histology is the microscopic study of the normal tissues of the body while histopathology is the microscopic study of tissues affected by disease. The procedures adopted for the preparation of material for such studies are known as histologic or histopathologic techniques. The tissues are usually obtained during surgery, biopsy, or autopsy. They range from very large specimens or whole organs to tiny fragments of tissue. The following surgical procedures are usually performed to obtain the specific-types of tissue that are submitted to a histology laboratory for processing: Fine needle aspiration is the simplest, least invasive test and uses the smallest needle to simply remove cells from the area of abnormality. This is not always adequate to obtain a diagnosis, depending on the area to be biopsied. A core needle biopsy removes not only cells, but also a small amount of the surrounding tissue. This provides additional information to assist in the examination of the lesion. An incisional biopsy takes out even more surrounding tissue. It takes out some of the abnormality, but not all. The doctor will slice into the lesion and remove only a portion of it. If the lesion is found to be cancerous, further surgery may be needed to remove or excise the entire lesion. An excisional biopsy generally removes the entire area in question. Punch biopsy is considered the primary technique for obtaining diagnostic full-thickness skin specimens. It requires basic general surgical and suture-tying skills and is easy to learn. The technique involves the use of a circular blade that is rotated down through the epidermis and dermis, and into the subcutaneous fat, yielding a 3- to 4mm cylindrical core of tissue sample. Shave biopsy - where small fragments of tissue are “shaved” from a surface (usually skin). Curettings - where tissue is scooped or spooned to remove tissue or growths from body cavity such as endometrium or cervical canal. Specimens are usually received in fixative (preservative) but sometimes they arrive fresh and must be immediately fixed. Tissue specimens received in the surgical pathology laboratory should have a request form that lists the patient information and clinical history along with a description of the site of origin. The specimens are accessioned by giving them a number that will identify each specimen for each patient. It is important that specimens are properly identified to minimize the risk of mislabeling. Once tissues are removed from the body, their proteins and cells are digested and broken down by their own enzymes, independent of a bacterial action. This process is known as autolysis, which is retarded by cold and accelerated at room temperature. It is more severe in tissues that are rich in enzymes (e.g. liver, brain, and kidney) and less rapid in elastic and collagen tissues. Methods of tissue examination may vary according to the structural and chemical components of the cells to be studied, and depends on the nature and amount of the tissue to be evaluated. Fresh tissues are usually examined when there is an immediate need for evaluation. On the other hand, a better and more effective means of studying tissues, whether normal or abnormal, is by examination of adequately preserved sections and smears that are stained to demonstrate specific structures. The glass slides are then mounted with coverslips for permanent keeping. Examination may be done on fresh or preserved tissues, depending on necessity. Fresh tissues have the advantage of being examined in the living state, thereby allowing protoplasmic activities such as motion, mitosis, a n d phagocytosis to be observed. Its use is limited, however, because of the fact that tissues examined in the fresh state are not permanent, and therefore, are liable to develop the changes that have usually been observed after death. Methods of Fresh Tissue Examination 1. Teasing or Dissociation – is a process whereby a selected tissue specimen is immersed in isotonic salt solution such as normal saline or Ringer’s solution in a petri dish or watch glass, carefully dissected with a needle an d separated by direct or zigzag spread using an applicator stick. Selected pieces of the tissue are transferred carefully to a microscope slide and mounted as a wet preparation underneath a cover glass, care being taken to avoid forming bubbles. It is either stained with a supravital dye or examined unstained by Phase Contrast or Bright Field microscopy. It has the advantage of permitting the cells to be examined in the living state. The use of the phase contrast microscope greatly increases the structural detail of the cells examined in the living state, allowing movement and mitotic division to be observed. The application of certain stains such as methylene blue can be also of great value. The preparations, however, are not permanent. 2. Squash Preparation (Crushing) is a process whereby small pieces of tissue (not more than one mm. in diameter) are placed in a microscopic slide and forcibly compressed with another slide or with a cover glass. If necessary, a supravital stain may be placed at the junction of the slide and the cover glass, and allowed to be absorbed by the tissue through capillary attraction. 3. Smear Preparation – The method of preparing the smear differs depending on the nature of the material to be examined. As a general rule, smears are made either by spreading the selected portion of the specimen over the surface of the slide with a platinum loop. Alternatively, an apposition smear can be made using a second slide to obtain a relatively uniform distribution of secretion. Too thin or too thick smears have to be avoided, since they make the tissues less suitable for examination. Smears may be examined either as fresh preparations similar to that described for teased preparations, or by using a supravital staining technique. Smear preparations can be made permanent by fixing them while still wet, staining them to demonstrate specific structures and inclusions, and mounting the cleared specimen beneath a cover glass with a suitable mounting medium. This is useful for preparing smears of thick secretions such as serous fluids, concentrated sputum, enzymatic lavage samples from the gastrointestinal tract, and blood smears. This technique is especially useful in cytological examinations, particularly for cancer diagnosis. a. Streaking -With an applicator stick or a platinum loop, the material is rapidly and gently applied in a direct or zigzag line throughout the slide, attempting to obtain a relatively uniform distribution of secretion. Too thin or too thick smears have to be avoided, since they make the tissues unsuitable for examination. b. Spreading - A selected portion of the material is transferred to a clean slide and gently spread into a moderately thick film by teasing the mucous strands apart with an applicator stick. It is a little more tedious than streaking, but has the advantage of maintaining cellular interrelationships of the material to be examined. It is especially recommended for smear preparations of fresh sputum and bronchial aspirates, and also for thick mucoid secretions. c. Pull-Apart – This is done by placing a drop of secretion or sediment upon one slide and facing it to another clean slide. The material disperses evenly over the surface of the two slides. Slight movement of the two slides in opposite directions may be necessary to initiate the flow of materials. The two slides are then pulled apart with a single uninterrupted motion, and the specimen is placed under the microscope for immediate examination, or applied with vital stains. 4. Touch Preparation (Impression Smear) – This is a special method of smear preparation whereby the surface of a freshly cut piece of tissue is brought into contact and pressed on to the surface of a clean glass slide, allowing the cells to be transferred directly to the slide for examination by Phase Contrast microscopy or staining for light microscopic study. It has an added advantage in that the cells may be examined without destroying their intercellular relationship. Frozen Section At times during the performance of surgical procedures, it is necessary to get a rapid diagnosis of a pathologic process. The surgeon may want to know if the margins of his resection are free from tumor before closing. An unexpected disease process may be found that requires immediate diagnosis so the surgeon can decide what to do next, or it may be necessary to determine if the appropriate tissue has been obtained for further workup of a disease process. Immediate diagnosis is accomplished through the use of a frozen section, especially in intra-operative pathology to help the surgeon in choosing his next plan of action. It is especially recommended when lipids and nervous tissue elements are to be demonstrated. Frozen sections are usually done on muscle and nerve biopsies as well as on surgically removed tumors. A fresh tissue is frozen on a microtome with C02, or on a cryostat, a cold chamber kept at an atmospheric temperature of -10° to -20° C. The thin frozen sections are mounted on a glass slide, fixed immediately and briefly in liquid fixative, and stained using similar staining techniques as in traditional wax embedded sections. For histochemistry, cryostat sections give much faster results than paraffin sections. However, the morphological detail and resolution of frozen sections are usually inferior compared to the quality of tissue that has been embedded in paraffin. The advantage of the frozen section method is rapid processing time with less equipment requirement, and less need for ventilation in the laboratory. The disadvantage is the relatively poor quality of the final slide. Frozen sections, both fixed and unfixed, have many applications in histotechnology, and are commonly used for: 1. Rapid pathologic diagnosis during surgery 2. Diagnostic and research enzyme histochemistry 3. Diagnostic and research demonstration of soluble substances such as lipids and carbohydrates 4. Immunofluorescent and immunohistochemical staining 5 . Some specialized silver stains, particularly in neuropathology The tissue for freezing should be fresh, and freezing should be done as quickly as possible. Slow freezing can cause distortion of tissue due to ice crystal artifacts. The more commonly used methods of freezing include: 1. Liquid nitrogen 2. Isopentane cooled by liquid nitrogen 3. Carbon dioxide gas 4. Aerosol sprays Liquid nitrogen is generally used in histochemistry and during intraoperative procedures, and is the most rapid of the commonly available freezing agents. Its main disadvantage is that soft tissue is liable to crack due to the rapid expansion of the ice within the tissue, producing ice crystals or freeze artifacts. It also overcools urgent biopsy blocks, causing damage to both block and blade if sectioning is done at -70°C or below . The tissue snap-frozen in liquid nitrogen must therefore be allowed to equilibrate to cryostat chamber temperature before sectioning is attempted. The majority of non-fatty unfixed tissues are sectioned well at temperatures between -10oC and -25°C. One problem with the use of liquid nitrogen is that it causes a vapor phase to form around the tissue, acting as an insulator that causes uneven cooling of tissue, particularly of muscle biopsies, and making diagnostic interpretation difficult. This problem can be overcome by freezing the tissue in Isopentane, OCT, or Freon 2.2 that has a high thermal conductivity. Isopentane is liquid at room temperature. A Pyrex glass beaker containing isopentane is usually suspended in a flask of liquid nitrogen until half-liquid and half-solid stage is reached. The beaker is removed from the liquid nitrogen when small crystals start forming on the side of the beaker (approximately -170°C), and the tissue to be frozen (affixed on a cork disc, aluminum foil or cryostat chuck) is dropped into the cooled liquid isopentane. This is an excellent method for freezing muscle tissue. Tissue blocks can also be frozen by adapting a conventional freezing microtome gas supply of carbon dioxide gas from a C02 cylinder. The use of aerosol sprays has become increasingly popular in recent years, and is adequate for freezing small pieces of tissue except muscle. Quickfreezing spray cans of fluorinated hydrocarbons (e.g., Cryokwik) have a distinct advantage of rapidly freezing blocks of any type of tissue. Fresh, completely unfixed tissues, or tissues that have been briefly treated with formalin may not require embedding anymore; instead they may be frozen and cut in a freezing microtome or cryostat. Two methods of preparing frozen sections may be resorted to: 1. Cold Knife procedure 2. Cryostat procedure (Cold Microtome) Cold Knife Procedure Tissue blocks can be frozen by adapting a conventional freezing microtome gas supply of carbon dioxide gas from a C02 cylinder, or by using a specially made piece of equipment known as cryostat. Almost any microtome can be utilized for the purpose, provided means are made available for freezing and maintaining the specimen and the knife at low temperatures, usually by utilizing the carbon dioxide technique. A piece of filter paper soaked in gum syrup is placed on the microtome stage, and short bursts of C02 are applied, freezing the filter paper to the stage. The selected block of tissue, approximately 3-5 mm. thick, is then oriented on the stage, applied with a few drops of gum syrup and frozen solid with several intermittent bursts of CO2 , each for 1-2 seconds duration, at intervals of around 4 seconds. It should be frozen just to the point where it will be firm enough to section. The tissue is then lifted up to the knife manually and trimmed until the surface is flat. The surface is then warmed with the finger until the hard frozen tissue starts to thaw and becomes visible to the naked eye. This is the DewLine, the point at which sections may then be cut at 10 µm thickness. Sections do not form ribbons but rather stick to the knife blade and should, therefore, be removed with a camel hair brush or finger moistened with water. They are then transferred to a dish of distilled water to separate, and picked up individually for mounting and staining. The water dish is usually placed on a dark or black background, in order to see the sections which are usually colorless or very light in color. Tissues that have been frozen too hard will usually chip into fragments when cut. The surface of the block may then be softened by warming slightly with the ball of the finger or thumb. Tissues that have not been sufficiently frozen will cut thick and crumble, and the block may come away from the stage. More bursts of C02 gas should then be given to refreeze the block. Whether used in a cold environment or not, a different temperature between the tissue and the knife is usually employed, the latter being colder. Using a cold knife in a controlled cold environment, optimum condition for sectioning shall be provided for by the following temperatures: Knife -40° to - 60°C Tissue -5° to - 10°C Environment 0° to - 10°C The success of this procedure depends upon ambient temperature and humidity. It is very hard, if not impossible, to cut sections in a hot or humid environment. Ease of cutting and quality of sections are always improved if done in a cold room. Sections thinner than 6 µ generally cannot be obtained even from tissues that section well, and with ideal conditions for sectioning. Cryostat Procedure This method makes use of the Cryostat, an apparatus used in fresh tissue microtomy. The cryostat consists of an insulated microtome housed in an electrically driven refrigerated chamber and maintained at temperatures near -20°C, where microtome, knife, specimen and atmosphere are kept at the same temperature. The optimum working temperature of cryostat is -18 to -20°C. Majority of the sections can be cut in isothermic conditions, where the temperature for sectioning can be accurately established and controlled. The tissue for freezing should be fresh, and freezing should be done as quickly as possible. Slow freezing can cause distortion of tissue due to ice crystal artifacts. Fig. 3-1. Ice crystal artifacts caused by improper freezing Fresh frozen tissue requires that the tissue be maintained in the frozen solid state during cutting of section, thereby supporting and protecting the tissue from damage and distortion by the knife during the process of cutting. The tissue must be sufficiently cold to prevent compression and displacement of cell and tissue structures as the knife passes thru it. The microtome knife needs to be chilled and maintained at low temperature to prevent complete melting of the tissue, thereby forming a sticky, distorted mass along the knife edge. When the tissue is too cold, on the other hand, resistance to cutting is increased, so that the tissue becomes brittle and is broken down into fragments upon cutting. The cryostat should be left on at all times even when not in use, since it will require several hours to reach operating temperature from a room temperature start. It takes at least one hour for a knife to come down to operating temperature, so that a spare knife should always be kept inside the cryostat cabinet. To ensure that the sections will cut smoothly and freely onto the knife surface, the knife as well as the undersurface and edge of the anti-roll plate must be kept scrupulously clean and dry. Soft tissue paper, either dry or moistened with absolute alcohol, may be used to clean the knife and anti-roll plate. The cryostat should be defrosted during the weekend, including cleaning and oiling of microtome with special lowtemperature oil. The success of fresh tissue sectioning depends to a large extent on the temperature, both of the tissue and of the knife. Certain tissues such as fat or mucin, and hard or dense structures in a soft matrix require much lower temperatures to impart a suitable consistency for cutting. These are sectioned on the cryostat by lowering the tissue or knife temperature or both, either by placing the block holder in a bath of alcohol or acetone containing dry ice, or by exposing the tissue to carbon dioxide. Mounting of Tissue Block Synthetic water-soluble glycols and resins are generally used as mounting media for tissue blocks that need to be sectioned on a cryostat. The O.C.T. (Optimal Cutting Temperature) compound, Lab-Tek Products, Division of Miles Laboratories is especially recommended. It is marketed in convenient 8 oz. plastic dispensers in three temperature ranges, depending on the tissue being cut: -5 to -15°C for brain, lymph nodes, liver, spleen, uterine curetting, soft cellular tumors; -15 to -25°C for non-fatty breast tissue, ovary, prostate, tongue, and GI tract; -35°C for fatty breast and omental tissue. The cryostat is usually set at -18 to -20°C. Preferably, the tissue block should be 2-4 mm. thick in order to minimize the risk of the knife hitting the metal tissue block holder. Small fragments of tissue, such as curettings or brain biopsies, are placed on a thick base of O.C.T. compound. The blocks are then surrounded and covered with an additional matrix of O.C.T. compound, and frozen by liquid nitrogen. The frozen tissue is mounted on the microtome. Both the microtome knife and the tissue block are left in the cryostat for 15 minutes at -20°C, to ensure that they are cooled to the correct temperature. Sections between 5-10 µm are then cut slowly and steadily, removed from the knife with a camel hair brush, attached directly to slides of cover-glasses at room temperature, air dried, and fixed (optional). To mount cryostat sections after cutting, one edge of the glass slide is lowered gently until it is about 1/2 to 1 mm. from the knife face. The section will automatically transfer from the cold knife to the relatively warm slide. The slide should never be pressed down on the section, because this will cause a frost mark to remain where the section rested on the knife. If this happens, the frost mark should be wiped away with soft tissue paper. Overall, cryostat sections provide the simplest, quickest and least laborintensive method for producing frozen sections, and are routinely used for intraoperative and rapid diagnosis of surgical specimen. It should be noted that cryostats cut only individual sections, and do not form ribbons, as in paraffin blocks. Freezing Previously Fixed Tissue Cryostat sections of fresh, unfixed tissue usually attach easily to the slide, even without adhesives, and will preserve enzymes and other substances that may be studied by histochemical techniques. The cryostat is also recommended for any technique requiring cold sectioning of fixed material, e.g., for fats and lipids, and for some special methods for the nervous system. Sections of formalin-fixed tissue, however, may not adhere to the slide, and will fall off or be detached during staining. Clean slides should be coated with albumin or chrome-glycerin jelly so that the fixed tissue will attach to the slide. Another way, albeit cumbersome, is to immerse the tissue block in boiling 10% buffered formalin for 1 to 2 minutes before freezing and sectioning for rapid surgical diagnosis. Special fixatives such as 10% formol calcium at 4°C may be used in histochemistry and for lipid demonstration. Tissues that have been fixed or stored in alcohol should be washed in water for 12-24 hours before sectioning, since alcohol inhibits freezing. Examination of nerve and muscle Muscle and nerve biopsies are divided into separate portions that will allow for formalin fixation and paraffin embedding, unfixed snap-frozen for cryostat sections, fixation and resin embedding for electron microscopy (EM) and, in some rare cases, for biochemical immunoblotting studies. Multiple fixation processes are required because multiple techniques are to be used. The portion of a specimen intended for frozen section should be transported on top of wet ice, on saline-dampened gauze, and rapidly frozen within two hours. Upon receipt in the histology lab, specimen is oriented in O.C.T. (Optimal Cutting Temperature) compound and snap-frozen in liquid nitrogen/ isopentane for optimal results. Orientation, size, and expedient flash freezing are critical to obtaining undamaged sections of unfixed muscle fibers. Do not allow the tissue to freeze slowly or to soak up excess saline, as these will cause artifacts that can be seen microscopically and can interfere with diagnostic interpretation. A portion of the tissue is oriented on a piece of cardboard, fixed with 10% buffered formalin and processed for staining with routine Hematoxylin and Eosin (H&E staining). The biopsy portion for electron microscopy is fixed in a buffered solution of glutaraldehyde and postfixed in osmium tetroxide, usually by a specialist in electron microscopy. In some muscular degenerative disorders, biochemical techniques may also be required. SPECIAL PROCESSING TECHNIQUES For histochemical evaluation involving enzyme studies, the tissue needs to be chemically active, and the important chemical constituents should not have been removed, altered or displaced. In most instances, frozen section is deemed to be the most ideal and preferred means of preserving tissues in order to avoid complete or partial loss of enzymes consequent to chemical fixation. Difficulties, however, arise in obtaining thin and serial sections of uniform thickness; since cut sections of tissue tend to disintegrate and cannot be easily handled without prior fixation. These disadvantages will have to be considered in determining the necessity and advisability of such sections. In addition to fresh frozen tissue sectioning, there are methods that may be resorted to, if chemical fixation of tissue blocks is to be avoided, namely: 1. Freeze-drying 2. Freeze substitution Like fresh frozen sections, these special techniques have the common principle of rapidly preserving the tissue block by freezing (quenching). The aim is to produce instant cessation of cellular activity thereby preventing chemical alteration of tissue and displacement of cellular tissue components. Freezing must be rapid, accomplished within seconds to prevent the formation of ice crystal artefacts in tissue blocks and produce optimum tissue preservation. The freezing agent commonly employed is liquid nitrogen, and the tissue is sectioned into thin slices using a cryostat machine under very low temperature. The use of isopentane, pentane and propane and most recently of dichloro-difluoromethane, which can be cooled to very low temperature in order to retain the fluidity of the freezing agents, have contributed much in giving higher conductivity to this liquefied gas. Freeze-Drying Freeze-drying is a special way of preserving tissues by rapid freezing (quenching) of fresh tissue at -160°C and subsequently removing ice water molecules (dessication) by transferring the still frozen tissue block into a vacuum chamber at a higher temperature, e.g. -40°C (sublimation) without the use of any chemical fixative. This technique is generally not used in routine surgical laboratories, and is restricted to specialized or research laboratories. A tissue around 2 mm. thick is plunged into isopentane or propaneisopentane mixture which has been chilled to -160° to -180°C with liquid nitrogen. This will effectively solidify the tissue in 2-3 seconds, thus preventing the formation of large ice crystals, autolysis and putrefaction. The frozen tissue is then transferred into a high vacuum drying chamber maintained at a temperature of -30° to -40°C depending upon the size of the tissue. Water is sublimated and dehydrated from the tissue, thereby completing the dessication process within 24-48 hours. Once drying is completed, the tissue is removed, fixed and embedded, either in molten paraffin wax, water soluble waxes or celloidin. Infiltration and impregnation are usually performed in a vacuum embedding oven. The tissue is then sectioned in the usual routine manner and specific staining is applied, depending upon individual necessity. This technique is generally time-consuming and expensive. Drying is by far the most time consuming part of the process, as certain tissues contain 7080% water by weight that has to be removed without damage to the tissue. Furthermore, freeze-dried materials are generally more difficult to section than ordinary paraffin blocks. The tissue is brittle and inadequately supported due to the relatively short period for wax impregnation; hence, it is not advisable as a routine procedure. The tissues are usually flattened directly into an albuminous glass slide with the aid of the finger. Water must be avoided and warm alcohol, acetone, mercury are preferred. However, freeze-drying also h a s many outstanding good features. It produces minimum tissue shrinkage, and allows tissues to be processed in a fresh state. It causes minimal chemical change on the cells, most especially on the protein components, and less displacement of tissue and cellular consti tuents. This method avoids the chemical alteration of cellular components, t h e denaturation of proteins, destruction of enzymes, and loss of tissue constituents that usually occur in the usual histological processing. This method is particularly important as far as enzyme studies are concerned. In addition to demonstrating hydrolytic enzymes, mucous substances, glycogen and proteins, freeze-drying may be used for special studies, including: 1. Immunocytochemistry 2. Fluorescent antibody studies of polypeptide and polypeptide hormones 3. Autoradiography 4. Microspectrofluorimetry of autofluorescent substances 5. Formaldehyde-induced fluorescence of biogenic amines (to demonstrate 5-hydroxytryptamine, adrenaline, and other catecholamines) 6. Scanning electron microscopy Freeze-Substitution: Freeze-substitution is a process of dehydration, performed at temperatures low enough to avoid the formation of ice crystals and to circumvent the damaging effects observed after ambient-temperature dehydration. It is similar to freeze-drying in preparing and preserving tissue blocks for subsequent sectioning because both involve the rapid freezing of tissues and the subsequent infiltration and embedding of the frozen tissue block in paraffin or celloidin. The only variation is that the frozen tissue, instead of being subjected to dehydration in an expensive vacuum drying apparatus, is fixed in Rossman's formula or in 1% Acetone and dehydrated in absolute alcohol. Infiltration and embedding is then carried out in the same way as in paraffin section. Freeze-substitution is based on rapid freezing of tissues followed by solution ("substitution") of ice at temperatures well below 0°C. A 1 mm to 3 mm specimen is thrown into 3:1 propane-isopentane that is super cooled by liquid nitrogen to -175°C (with precautions). Cryostat sections are cut 8-10 µm, and transferred to water-free acetone (substituting fluid), and cooled to -70oC for 12 hours to 1 week in order to dissolve ice slowly without distorting tissue structure. The sections are floated onto coverslips or slides and allowed to dry for subsequent histochemical staining. This technique is relatively more economical and less time-consuming than freeze-drying. For best morphological and histochemical preservation, substituting fluids should in general contain both chemical fixing agent and solvent for ice, e.g., 1% solutions of osmium tetroxide in acetone, mercuric chloride in ethanol, or picric acid in ethanol. REFERENCES Andrew W. (1966) Microfabric of Man, Yearbook Medical Publishers, Inc., Chicago. Anderson G, Bancroft J. (2002) Tissue processing and microtomy. In: Bancroft, J .D. Gamble, M. Theory and Practice of Histological Techniques. 5th ed., Churchill Livingstone, London, 100. An Introduction to Specimen Preparation: Geoffrey Rolls Leica Biosystems, Wetzlar, Germany, 30. May 2011 Bancroft JD. (1975) Histochemical Technique. 2nd Ed. London: Butterworths. Bancroft J.D, Cook HC. (1994) Manual of Histological Techniques and their Brown CC. (1969) Primer of Histopathologic Technique, Appleton-Century-Crafts, New York. Brown RW. (2009) Histologic Preparation: Common Problems and their Solutions. CAP Press. Chicago. Pp. 35-42. Carson FL, Hladik C. (2009) Histotechnology: A Self-Instructional Text. 3rd ed., American Society of Clinical Pathology Press. Pearse AGE. (1980) Histochemistry, Theoretical and Applied, 4th ed., Vol 1, Churchill Livingston, Edinburgh. Sheehan DC, Hrapchak B. (1980) Theory and Practice of Histotechnology, 2nd ed., C.V Mosby Co., St Louis. Suvarna SK, Layton C, Bancroft JD. (2013) Bancroft’s Theory and Practice of Histological Techniques, 7th ed., Churchill Livingston Elsevier. CHAPTER 4 CONVENTIONAL TISSUE PROCESSING In order to enable the pathologist to diagnose the presence or absence of disease, the histotechnologist needs to produce a tissue section of good quality that allows for adequate interpretation of microscopic cellular changes. Solid tissues need to be fixed and processed to preserve their structures, and eventually impregnated with an appropriate hardening substance to permit making thin slices suitable for staining and microscopic evaluation. This can be accomplished by preserving and carefully processing solid structures and tissues in the following order: 1. Fixation 2. Decalcification (optional) 3. Dehydration 4. Clearing 5. Impregnation (Infiltration) 6. Embedding 7. Trimming 8. Section-Cutting (Microtomy) 9. Staining 10. Mounting 11. Labeling “Tissue processing” describes the various steps required to take the tissue from fixation to the state where it is completely infiltrated with a suitable histological wax and can be embedded ready for section cutting on the microtome. Once the tissue has been fixed, it must be processed into a form in which it can be made into thin microscopic sections. Wet fixed tissues (in aqueous solutions) cannot be directly infiltrated with paraffin. First, the water from the tissues must be removed by dehydration. This is usually done with increasing concentrations of alcohol (70% to 95% to 100%). Because water and paraffin are not miscible, the specimens must be gradually dehydrated to achieve complete replacement of water with alcohol. Once successfully dehydrated, the next step is called "clearing" and consists of removing the dehydrating agent (alcohol) with a substance that will be miscible with the embedding medium (paraffin). The commonest clearing agent is xylene. Finally, the tissues are infiltrated with an embedding agent (almost always paraffin). Overview of the steps in tissue processing for paraffin sections 1. Fixation It is important that tissues are handled carefully and appropriately fixed as soon as possible after arriving in the laboratory. The specimen is placed in a liquid fixing agent (fixative) such as formaldehyde solution (formalin). This will slowly penetrate the tissue causing chemical and physical changes that will harden and preserve the tissue and protect it against subsequent processing steps. Formalin, usually as a phosphate-buffered solution, is the most popular fixative for preserving tissues that will be processed for paraffin embedding. Ideally, specimens should remain in fixative long enough for it to penetrate the tissue and then for an additional period in order to allow the chemical reactions of fixation to reach equilibrium (fixation time). Fixation is a critical step in the preparation of histological sections. If it is not carried out under optimal conditions or if fixation is delayed, a tissue specimen can be irreversibly damaged. Following fixation, appropriately trimmed specimens are placed in suitable labelled cassettes (small perforated baskets) to segregate them from other specimens. Formalin-fixed, paraffin-embedded tissues may be stored indefinitely at room temperature, and nucleic acids (both DNA and RNA) may be recovered from them decades after fixation. 2. Dehydration Because melted paraffin wax is hydrophobic (not miscible with water), most of the water in a specimen must be removed before it can be infiltrated with wax. This process is commonly carried out by immersing specimens in a series of ethanol (alcohol) solutions with increasing concentration to avoid excessive distortion of tissue until a water-free tissue in alcohol is reached. Water soluble proteins are removed at lower concentrations of ethanol. When ethanol concentration is increased to 100%, certain lipids may be dissolved. A typical dehydration sequence for specimens not more than 4mm thick would be: 70% ethanol 15 min 90% ethanol 15 min 100% ethanol 15 min 100% ethanol 15 min 100% ethanol 30 min 100% ethanol 45 min Fatty tissues such as breast or lipoma may be inadequately processed in what is normally a successful schedule for other tissues. Ethanol is a poor fat solvent. To ensure complete dehydration, a superior fat solvent such as acetone or isopropanol should be added before the final absolute ethanol, and chloroform or trichloroethane used as the transition solvent. 3. Clearing The dehydrated tissue is transferred to an intermediate solvent that is fully miscible with both ethanol and paraffin wax. The term “clearing” has been chosen because many (but not all) clearing agents impart an optical clarity or transparency to the tissue due to their relatively high refractive index. Another important role of the clearing agent is to remove a substantial amount of fat from the tissue which otherwise presents a barrier to wax infiltration. Following the dehydration, the tissue is immersed in one to three different xylene immersions. In these stages, the ethanol is gradually replaced with xylene and when the tissue is embedded, the xylene will then be replaced by the molten paraffin wax. A typical clearing sequence for specimens not more than 4mm thick would be: Xylene 20 min Xylene 20 min Xylene 45 min 4. Infiltration The cleared tissue is infiltrated with a suitable histological wax (usually paraffin) which is liquid at 60°C and then allowed to cool to 20°C in order to solidify into a consistency that allows sections to be cut. These waxes are mixtures of purified paraffin wax and various additives that may include resins such as styrene or polyethylene that allow them to be sectioned thin enough on a microtome, forming ribbons that can flatten fully when floated on a warm water bath. To completely displace the clearing agent, a typical paraffin infiltration sequence of paraffin for specimens not more than 4mm thick would be: Paraffin wax 30 min Paraffin wax 30 min Paraffin wax 45 min 5. Embedding Once the tissue has been processed it is ready to be oriented into a paraffin block and subsequently sectioned. After infiltration with wax, the tissue is oriented and placed in a mold that is filled with molten wax to form a solid tissue block that can later be clamped into a microtome for sectioning. The infiltrated tissue is removed from the cassette and very carefully oriented in a suitably sized metal mold so that the “plane of section” can be determined. Correct orientation of tissue in a mold is the most important step in embedding. Incorrect placement of tissues may result in diagnostically important tissue elements being missed or damaged during microtomy. Usually tissues are embedded with the surface to be cut facing down in the mold. After orienting the section, the mold is filled with molten wax. The main part of the labelled cassette is placed on top of the mold and topped up with more wax. The whole mold is placed on a cold plate to solidify. When this is completed the block with its attached cassette can be removed from the mold and is ready to be sectioned on a microtome. The choice of mold will depend on the type of chuck in the microtome that will be used to section the tissue. Stainless steel, ceramic, paper, plastic, and aluminum foil molds can be used. The basic method is the same for each. Double embedding is the process by which tissues are first embedded or fully infiltrated with a supporting medium such as agar or nitrocellulose, then infiltrated a second time with wax in which they are also embedded. Double embedding in agar-paraffin is a reliable and convenient method of handling minute and friable tissue fragments such as curetting and endoscopic biopsies, which can be lost during tissue processing. It also overcomes the difficulty of manipulating small tissue fragments during embedding and facilitates correct orientation and identification of tissues for histochemistry and immunohistochemistry. The tissues may shrink by the time they are infiltrated with wax, but if adequately processed, they will still show good morphological detail and allow for accurate histopathological evaluation. 6. Section-cutting Once the tissues have been embedded, they must be cut into sections that are thin enough to be placed on a slide. This is done with a microtome. Good microtomy techniques will minimize artifacts that can lead to difficult diagnostic interpretation of special stains. One of the most directly correlated factors is the thickness in which a specimen is cut. Specimens for routine Hematoxylin and Eosin (H&E) are cut 3–5 μm in thickness. Tissues to be examined for amyloid deposits are better sectioned at 8–12 μm, whereas kidney biopsies should be cut at 2 μm for optimal viewing of the structures of glomeruli. Paraffin wax does not provide a sufficiently hard matrix for cutting very thin sections for electron microscopy. Epoxy resins are the most commonly employed embedding media for semi-thin and ultrathin sections, but acrylic resins are also used, particularly where immunohistochemistry is required. Thicker sections (0.35μm to 5μm) of resin-embedded tissue can also be cut for light microscopy. Again, the immiscibility of most epoxy and acrylic resins with water necessitates the use of dehydration, usually with ethanol. The microtome is nothing more than a knife with a mechanism for advancing a paraffin block across the knife. Knives are either of the standard thick metal variety or thin disposable variety (like a disposable razor blade). Usually this distance can be set, for most paraffin embedded tissues at 6 to 8 microns. Plastic blocks (methacrylate, araldite, or epon) are sectioned with glass or diamond knives that can cut sections down to about 1 micron. Thin sections for electron microscopy (0.25 micron) are best done with a diamond knife. The glass slides containing the specimen are then placed in a warm oven for about 15 minutes to help the section adhere to the slide. If this heat might harm such things as antigens for immunostaining, then this step can be bypassed and gluecoated slides can be used instead to pick up the sections. It is important to have a properly fixed and embedded block or much artifact can be introduced during the sectioning. Common artifacts include tearing, ripping, creases, holes or folding of sections, etc. Once sections are cut, they are floated on a warm water bath that helps remove wrinkles. Then they are picked up on a glass microscopic slide. The tissue slide is drained and may be gently heated to evaporate the layer of water between the sections and the glass. When all the water is gone, the slide may be heated enough to melt the wax, a procedure that may improve adhesion. 7. Mounting of Tissue Sections Paraffinized ribbons of serial tissue sections can be removed from the microtome knife as they are cut, by using a wooden tongue depressor blade. In this process, a slight traction is exerted on the end of the ribbon, stretching it gradually over the wooden blade while floating in a warm water bath. The temperature of the warm bath should be kept at 5–10oC below the melting point of the embedding wax. If it is too hot, desiccated-looking sections will result, while cool water baths will produce excessive wrinkling of the tissue. Adding a few drops of ethyl alcohol to the water may facilitate the mounting of tissue sections. The ribbon must not be left in the bath for more than 1 or 2 minutes, or over-hydration of the tissue will be produced, simulating the appearance of edema fluid when examined microscopically. Because tissue sections do not adhere well to untreated glass slides, a bonding agent also must be a component of the water bath. Albumin, and poly-L-lysine are all suitable additives of this type. One of the most serious issues faced in histotechnology is misidentification of tissues, which includes mislabeled specimens, block identification problems, and tissue contaminants. A potentially dangerous mistake that can take place when mounting sections from flotation baths is the “shedding” of friable small tissue fragments that float freely on the surface of the water, and which may be inadvertently picked up when mounting slides from subsequently processed but unrelated cases. Known as ‘‘floaters’’, these tiny pieces of unrelated tissue commonly cause problems in interpretation of the biopsies by the pathologist. For example, a small piece of unrelated cancerous tissue may inadvertently “float” and be deposited on the slides of a subsequent case that is being evaluated for the presence of malignancy. This may lead to an inaccurate diagnosis and result in medicolegal liabilities on both the pathologist and the histotechnologist. Meticulous cleaning of the microtome water bath and frequent clearing or changing of the water will alleviate the danger of rare contaminants being carried over to subsequent sections being mounted. Also, the technologist must routinely skim, or otherwise clear, the surface of the water bath between cases. Another source of floater-type artefact is the ‘‘tongue blade metastasis,’’ wherein tissue adheres to a wooden applicator stick that is used to float successively prepared ribbons from two different cases. In cases where the specimen is limited in size (such as skin, bronchoscopy and gastrointestinal biopsies), it is advisable to save any unmounted paraffin ribbon (with appropriate identification) from such cases for at least a week after they are accessioned, so that remounts can be prepared when additional sections are requested, without the need for further microtomy of the tissue block. 8. Staining The tissue sections mounted on the slide are nearly invisible under a light microscope so they must be stained to create contrast. After drying in a 60oC, the slide is passed through another series of chemical reagents. Xylene removes the paraffin and absolute alcohol removes the xylene. The tissue on the slide is then rehydrated to prepare it for staining. Most staining procedures in the laboratory, aside from antibody-based immunohistochemistry (IHC), use chemicals or dyes that will bind or have affinity for certain components of the cells and extracellular components. The chemical properties of these dyes produce the visual appearance that is seen under the microscope. Different staining procedures are done depending on the tissue component that is being studied. Potential contamination during the staining procedure may be much higher than having “floaters” when mounting sections from a water bath. The tissue is deparaffinized during the first steps in preparing the slides for staining. As the slides are dipped up and down into the staining baths, the deparaffinized tissue can fragment and small dis-cohesive pieces can break free and be lifted on the slide. Contamination in the staining solution is dependent on the volume of slides being stained and the time point during the day that the samples are taken. Because the stainer baths are a potential reservoir of tissue contaminants, changing the staining fluids may alleviate some of the potential for carryover from this source. And, as higher numbers of the contaminating fragments are localized to the first xylenes and alcohols, frequently changing these baths in particular may also be useful. Automatic Tissue Processing Tissue processing can be performed manually (hand processing), but when there is a large volume of tissues that need to be processed, it is more convenient and much more efficient to use an automated tissue processing machine (“tissue processor”). This machine allows the specimens to be infiltrated with a sequence of different solvents finishing in molten paraffin wax. The specimens are in an aqueous environment to start with (water-based) and must be passed through multiple changes of dehydrating and clearing solvents (typically ethanol and xylene) before they can be placed in molten wax (which is hydrophobic and immiscible with water). The duration and step details of the “processing schedule” chosen for a particular batch of specimens will depend on the nature and size of the specimens. The older design of an automatic issue processor is a carousel which contains a cage in which the tissue cassettes are placed. This carousel has a number of glass beakers containing solvents and solutions which ensure that the tissue is dehydrated and cleared ready for paraffin wax embedding. The carousel vertically agitates the cage in each solution before moving on to the next solution in the dehydration/ clearing method. The modern processors have a chamber in which the specimens are held and the different solutions are pumped in and out of the chamber. In general, the whole process takes around six hours and is usually set up to run overnight. Tissues that come off the tissue processor are still in the cassettes and must be manually put into the blocks by a technician who must pick the tissues out of the cassette and pour molten paraffin over them. This "embedding" process is very important, because the tissues must be aligned, or oriented, properly in the block of paraffin. Fig. 4-1. Automatic Tissue Processor Due to the viscosity of molten paraffin wax, some form of gentle agitation is highly desirable. If the processor is to be run overnight, it should be programmed to hold on the first ethanol bath and not finish until the next morning so the specimens do not sit in hot paraffin longer than the time indicated. If specimens are fresh they may incubate in formalin in the first stage on the machine. It is important to not keep the tissues in hot paraffin too long or else they may become hard and brittle. Processed tissues can be stored in the cassettes at room temperature indefinitely. Vacuum infiltration is the impregnation of tissues by a molten medium under reduced pressure. The procedure assists the complete and rapid impregnation of tissues with wax and reduces the time tissues are subjected to high temperatures, thereby minimizing heat-induced tissue hardening, facilitating complete removal of transition solvents, and prolonging the life of wax by reducing solvent contamination. Factors that impact the duration of tissue processing and extent of infiltration 1. Tissue Density and Thickness Variable tissue density affects infiltration and subsequent sectioning of tissues. Spongy tissues (like lungs) are usually more rapidly infiltrated than hard and dense tissues. Thickness of the tissue also influences the rate of reagent diffusion and hence processing time. Tissue thickness should be optimized for particular processing schedules, or alternatively, processing times should be adjusted to accommodate thick, thin or large tissue blocks. 2. Agitation Agitation using manual or automated processors increases the flow of fresh fluids in and around the tissues. Most tissue processing protocols utilize automated processors with vertical or rotary oscillation mechanisms to speed fluid exchange. Without agitation, tissues tend to settle to the bottom of the processing device or become too tightly packed, therefore reducing surface area available for fluid exchange. Fluid interchange between processing reagents and tissues is promoted by exposure of the maximum tissue surface area. Therefore, tissues should be loosely packed in baskets to facilitate exchange of reagents and increase diffusion. Ideally, the cassette perforations should be perpendicular to the fluid flow. If tissues are allowed to settle on the bottom of a container or are too tightly packed, tissue surface area available for fluid exchange will be severely restricted. 3. Temperature Temperatures in the range of 37° to 45°C, for a limited time can speed up fluid penetration and tissue processing protocols. However, heat must be carefully monitored. High temperature can cause the tissue to shrink and to become hard and brittle, while low temperature increases the viscosity of reagents used in tissue processing, thereby reducing the rate of diffusion and increasing processing time. This can be avoided by maintaining embedding waxes 2o to 3°C above their melting points. Tissue shrinkage during infiltration in paraffin wax results mainly the effect of heat on collagen. 4. Vacuum and pressure Reduced pressure can increase the infiltration rate and decrease the time needed to complete steps in tissue processing protocols. High pressure facilitates infiltration of dense specimens with the more viscous embedding media. Vacuum application during tissue infiltration improves processing quality and can aid in removal of trapped air from porous tissue. Using vacuum during tissue processing protocols can reduce the infiltration time when dealing with dense and fatty tissue specimens. Vacuum applied during dehydration, clearing and infiltration improves the quality of processing in tissues such as lung which becomes de-aerated during the process. However, duration of wax infiltration is dependent upon viscosity and is not generally reduced by applying a vacuum. Technical Considerations Baskets and metal cassettes should be clean and wax-free. Tissues should not be packed too tightly in baskets so as to impede fluid exchange. Processors must be free of spilled fluids and accumulated wax accumulations. Fluid levels must be higher than the specimen containers. Timing and delay mechanism must be correctly set and checked against the appropriate processing schedule. A processor log should be kept in which the number of specimens processed, processing reagent changes, temperature checks on the wax baths and the completion of the routine maintenance schedule are recorded as part of quality assurance program. Gentle washing and minimal thickness of cell layers will prevent the cells from detaching during staining. Make sure that there are enough sections to make a diagnosis, and ensure that the reagents have been applied evenly to the slides. Quality of staining can be compromised by inadequate fixation and similarly by poor tissue processing. A good technician must evaluate and determine the processing of choice for each purpose, i.e., special stains on paraffin, frozen or cell smear preparations. Make sure glass slides are clean and free from debris. In general, needle biopsies and bloody specimens should be incubated conservatively, whereas fatty specimens can be processed for longer than average. REFERENCES Brown RW. (2009) Histologic preparations: common problems and their solutions. Northfield, IL: College of American Pathologists. Clayden EC. (1971) Practical section cutting and staining. Edinburgh: Churchill Livingstone, 1971. Carson FL. (2007) Histotechnology. 2nd ed. Chicago: ASCP Press. Carson FL, Hladik C. (2009) Histotechnology: a self-instructional text. 3rd edition. Chicago: ASCP press. Cook DJ. (2006) Introduction to Techniques and Applications, 2nd ed. Oxfordshire, UK: Scion Publishing Ltd. Hegazy R, Hegazy A. (2015) Simplified Method of Tissue Processing (Consuming Time and Chemicals). Ann. of Int. Med. & Den. Res. 1(2):57-61. Henry JB. (1991) Clinical diagnosis and management by laboratory methods. 18th ed. Philadelphia: W.B. Saunders. Histopathology. New York: Churchill Livingstone, 4.2-1 - 4.2-39. John DB, Anderson G. (2002) Theory and Practice of Histological Techniques.5th ed., Chap 6. Tissue Processing and Microtomy including Frozen: Elsevier Churchill Livingstone, Edinburg p. 85-108. Kothar S, Phan JH, Wang MD. (2013) Eliminating tissue-fold artifacts in histopathological whole-slide images for improved image based prediction of cancer grade. J Pathol Inform., vol. 4, p. 22. Meschr A. (2012) Junqueira's Basic Histology: Text & Atlas, 12th edition, Chapter 1. Histology & Its Methods of Study. The McGraw-Hill Companies. Panja P, Sriram G, Saraswathi TR, Sivapathasundharam B. (2007) Comparison of three different methods of tissue processing. J Oral Maxillofac Pathol 11(1):15-17. Smith PJ, Warfield JL. (2005) Tissue processing and embedding in: The science of laboratory diagnosis: Section 1: Histopathology, 1-specimen handling and preparation of routine diagnostic histopathology Crocker J and Burnett D (ed.) 2nd edition, Wiley J & Sons Limited (publishers), England. Spencer LT, Bancroft JD. (2008) Tissue processing in: Theory and Practice of Histological Techniques, Gamble M, Bancroft JD (eds.), Chapter (6th ed., Churchill Livingstone Elsevier Ltd. Suvarna KS, Layton C, Bancroft JD. (2012) Bancroft’s Theory and Practice of Histological Techniques, 7th ed. London, UK: Churchill Livingstone. Winsor L. (1994) Tissue processing. In Woods A and Ellis R eds., Laboratory CHAPTER 5 RAPID TISSUE PROCESSING In conventional laboratories, routine use of formalin fixation, overnight dehydration, paraffin infiltration, manual embedding and sectioning have produced relatively uniform, high-quality tissue sections for histopathologic examination. Frozen sections have been used when there is an urgent need for immediate histopathologic evaluation. In recent years efforts have been made to streamline the processing time by using microwave heating techniques. This continuous throughput Rapid Tissue Processing (RTP) has introduced dramatic changes into the practice of modern histotechnology. As opposed to conventional tissue processors which use a graded series of alcohols, a clearing agent (usually xylene) and embedding medium (usually paraffin wax) in an overnight process, microwave assisted processing allows dehydration to be done in only one step and employs a four step process involving a single change each in ethyl alcohol and isopropanol followed by two changes in paraffin. When exposed to these high microwave temperatures, the alcohols quickly heat and dissipate, while the paraffin remains inert, allowing the paraffin to fully infiltrate the specimen. This eliminates the use of xylene from the process. Processing is undertaken in a dedicated microwave oven which is fitted with precise temperature control and timer, and an interlocked fume extraction system to preclude accidental ignition of solvent vapor. A turntable or in-built radiation dispenser facilitates even reagent heating. Microwave processing can be 60% to 80% faster than conventional processing time with an hourly throughput of up to 120 specimens. The implementation of RTP allows for rapid turnaround of tissue biopsies, is as effective as slower conventional tissue processing, and provides excellent morphology, sharp nuclear detail and crisp cellular images. The reagents used in molecular pathology can preserve DNA, RNA and proteins in the paraffin block, and eliminate the need to use fresh tissue for molecular studies, particularly with respect to the identification of gene activation and detection of gene products such as messenger RNA (mRNA) and proteins. Microwave technique is now commonly employed to unmask or retrieve antigens, using 10 mm. citrate buffer (pH 6.0). Microwave irradiation has been used successfully to expedite tissue fixation and processing. Microwave, a form of electromagnetic wave-induced heat, when applied in histotechnology, yields histologic material of similar or superior quality to that provided by conventional processing methods. Microwave-assisted processing of tissues, from fixation through paraffin, can save time and produce better results, when the proper microwave technology is used. The ability to control temperatures by a number of different parameters (variable wattage, restrictive temperature probe and water recirculation) makes it possible to achieve results that were not formerly available from conventional tissue processing systems. The technology makes it possible to employ any of the routinely used reagents for paraffin processing, and can be applied to accelerate routine, special, and metallic, as well as immunofluorescent stains. Microwave works as a physical agent similar in mechanism to vacuum, oven (heat) and agitation to expedite the movement of molecules, thereby accelerating fixation, decalcification, tissue processing and staining for immunohistochemistry and electron microscopy. Rapid manual microwavestimulated paraffin wax processing of small batches of tissues gives excellent results comparable to tissues processed by longer automated non-microwave methods. Calibration of domestic ovens is essential for optimum results. The accuracy of the temperature probe, duration of cycle time, and net power levels at various settings must be determined before the oven is used to process tissues. The equipment used in rapid tissue processing can vary from kitchen type microwave ovens to sophisticated semi-automated or automated instruments. These systems all use the same basic principles, with some distinctive variations that can accommodate differences in laboratory needs and practice patterns. Microwave excitation of the molecules increases movement in both solutions and tissues, resulting in improved tissue penetration and fixation, with preservation of many tissue antigens of diagnostic interest. Lower temperatures require longer heating times, while higher temperatures require shorter heating time to achieve strong intensity of staining. Microwave processing requires very precise maintenance of temperature, which is not possible with the use of kitchen-type microwave ovens whose temperature and output power (in watts) are not precisely specified, leading to inadvertent overheating and miscalculation of the percentage output power. Because their magnetrons were not precisely controlled, early work with the kitchen type microwaves resulted in uneven heating (uneven distribution of microwave energy) and sometimes unpredictable amounts of delivered energy. Specifically designed microwave units have been developed, which utilize a removable reaction vessel (to hold cassettes), with manual reagent exchanges according to a predetermined schedule. These units represent an economical method for rapid tissue processing, but only on a relatively small scale. They are also relatively labor intensive. Fig. 5-1. Microwave tissue processor http://www.mikronet.com/histology/milestone-histos3-histos5.shtml Unlike domestic microwave ovens, the laboratory microwave oven does not produce hotspots or uneven heating in tissues due to the presence of magnetic stirrer kept beneath which provides an even field of irradiation. The toxic and flammable solvent vapors generated during processing cannot always be adequately vented from domestic ovens and present an ignition hazard if the electrical system is unprotected, unlike laboratory ovens wherein adequate ventilation is created for the escape of fumes. Laboratory microwaves are now specifically designed and equipped with a thermocouple temperature probe and controller to maintain temperatures within a very narrow range of +/- 1°C, thereby producing consistent and reproducible results. Staining methods take much shorter time in a microwave oven compared to conventional tissue processing. In general, microwaved slides have better contrast, more intense staining, and less non-specific staining, compared with conventional metal-staining methods. Calibrated laboratory microwaves equipped with temperature probes and air-bubble agitation device have largely addressed the earlier problems of inconsistent or uneven heating observed when kitchen-type microwaves were originally used. The optimum temperature is 75° to 95oC, for metallic stains, and 55° to 60°C for non-metallic stains. Researchers have found microwave technology to be beneficial in achieving epitope recovery in formalin-fixed tissues for many markers within 10 min to 15 min. An enclosed system similar in configuration to modern vacuum assisted conventional tissue processors has been recently introduced. This instrument, when combined with microwave fixation, can reduce processing time to about 3 hours and may also be used in a formalin free environment. Like traditional instruments, these rapid tissue processors run in 'batch' mode; once the cycle has begun no additional tissues can be added for processing until the cycle is completed. There are some size constraints, as large tissue section (greater than 1.5 mm. thick) may show inadequate or uneven penetration of reagents, leading to incomplete clearing and paraffin impregnation. Large tissue blocks will require special handling to prevent incomplete fixation or tissue clearing. Small blocks such as endoscopic biopsies can be processed in a shorter period using tailor-specific protocol. Fig. 5-2. Sakura Rapid Tissue Processor (http://www.sakura-americas.com/products/processing/xpress-x120/) This system of continuous throughput rapid tissue processing allows for the addition of new specimens to the processor every 15 minutes, as a reaction chamber becomes available. This automated system utilizes computer controlled microwave delivery and temperature controls in a formalin free environment. Reagent volumes are small, and all reagents are relatively inexpensive and non-toxic . Xylene has also been eliminated, and vacuum assisted paraffin impregnation allows for a complete processing cycle of about 60-70 minutes. Current Rapid Tissue Processors use an innovative, low-wattage microwave technology, molecular-friendly reagents and traditional vacuum infiltration techniques to provide consistent, high quality results in record time. It has a continuous efficient workflow, consistent high quality 1-hour processing of up to 120 specimens per hour, maximum standardized same day diagnosis, formalin- and xylene-free processing. Continuous throughput yields up to 960 cassettes in an 8-hour shift, loads up to 40 cassettes approximately every 20 minutes, and immerses specimens for 15 minutes in each of the 4 enclosed processing retorts with the standard program. Several studies have shown that the quality of tissue sections after rapid tissue processing is comparable, and in some cases, superior to conventional tissue processing methods, with no detrimental effects on the commonly used special staining procedures. Immunohistochemical stains can be performed on sections without antigen retrieval in some cases, and with more highly diluted primary antibodies in others. The most dramatic impact of rapid tissue processing has been in the same day turnaround time from receiving the biopsy until microscopic evaluation and completion of surgical pathology reports, a significant departure from conventional surgical pathology practice. Microwave processing can be achieved 60% faster than conventional processing time so that urgent cases can be signed out on the same day. In some institutions the entire sequence of needle biopsy, tissue processing, slide interpretation and immunohistochemistry for receptors has been carried out within about 4 to 5 hours. One critical aspect of using microwave techniques is ensuring that samples have been adequately fixed. While rapid tissue processing by microwave methods can accept a number of different tissue fixatives, non-formaldehyde fixatives have been shown to have several advantages. An alcohol-based fixative has recently been introduced which, when combined with a formalinfree microwave based rapid tissue processing, has been demonstrated to permit the recovery of DNA, RNA, and proteins for molecular analyses. This universal molecular fixative, known as UMFIX (Sakura Finetek USA Inc., Torrance California), is a mixture of methanol and polyethylene glycol, and is an excellent and cost-effective alternative to formalin. UMFIX is non-volatile and active at room temperature. The morphology of UMFIX-exposed tissue is comparable to that fixed in formalin, and high molecular weight RNA is preserved in tissue that is immediately fixed and stored up to 8 weeks at room temperature. The elimination of formalin in both the fixation process and the processing has improved the quality of antigen preservation in the tissue sections. An added benefit is the elimination of noxious formalin fumes from the workplace, as well as expensive ambient air formalin monitoring programs. Each laboratory should evaluate its fixation control methods to optimize the use of microwave processing. Converting to the safer chemicals (i.e., less fumes, non-regulated disposal) may include rotating smaller quantities more often, causing a net increase in chemical consumption. The safety benefits of removing undesired regulated waste in addition to calculating net volumes may offer immediate cost savings. Although mechanical or electrical faults occasionally occur in tissue processors, processing mishaps where tissues are actually compromised, mainly occur because of human error. Inappropriate processing schedule or making fundamental mistake (perhaps in replenishing or sequencing of processing reagents) can result in the production of tissue specimens that cannot be sectioned and therefore will not provide any useful microscopic information to the pathologist. Precautionary Measures: Sections must be thin enough so fixative and dehydrating solutions can penetrate completely (about 1.5 mm.). This may increase the time required in grossing of specimens. Certain tissues (i.e., brain and large tissue blocks) require additional steps before placing into the rapid tissue processor. Continuous flow processing eliminates batching of specimens and necessitates ongoing attention to the instrument. As samples complete the processing cycle, they must be removed from the instrument to accommodate the next basket of cassettes. Paraffin must be added to the microwave in liquid form, as microwave energy will not melt paraffin pellets. Tissue must be brought to the boiling point of the intermedium (82°C for ethyl alcohol and 78°C for isopropanol) in the last step, to "flash evaporate" the remaining ethyl alcohol or propanol. REFERENCES Bejerano P, Khaled A, Ruiz P. (2003) The practice of a novel microwave assisted tissue processing method in transplant biopsies. Modern Pathology. 16:318B. Boon ME, Kok LP, Ouwerkerk-Noordam E. (1986) Microwave-stimulated diffusion for fast processing of tissue: reduced dehydrating, clearing, and impregnating times. Histopathology 10(3):303-309. Boon ME, Kok LP. (2008) Theory and practice of combining coagulant fixation and microwave histoprocessing. Biotech Histochem 83 (6):261-277. Chiu, KY. (1987) Use of microwaves for rapid immunoperoxidase staining of paraffin sections. Med Lab Sci 44:3-5. Emerson LL, Tripp SR, Baird BC, Layfield LJ and Rohr LR. (2006) A comparison of immunohistochemical stain quality in conventional and rapid microwave processed tissues. American Journal of Clinical Pathology 125:176-183. Hafajee ZA, Leong AS. (2004) Ultra-rapid microwave stimulated tissue processing with a modified protocol incorporating microwave fixation. Pathology. 36: 325-329. Hopwood D, Coghill G, Ramsay J, Milne G, Kerr M. (1984) Microwave fixation: its potential for routine techniques, histochemistry, immunocytochemistry and electron microscopy. Histochem J 16:1171-91. Kok LP, Visser PE, Boon ME. (1988) Histoprocessing with the microwave oven: An update. Histochem J 20:323-328. Kok, LP, Boon ME. (1995) Ultrarapid vacuum-microwave histoprocessing. Histochemistry Journal 27: 411. Leong AS. (1991) Microwave fixation and rapid processing in a large throughput histopathology laboratory. Pathology 23:271-3. Leong, AS. (1994) Microwave technology for morphological analysis. Cell vision 1:278-88. Leong AS and Price D. (2004) Incorporation of microwave tissue processing into a routine pathology laboratory: impact on turnaround times and laboratory work patterns. Pathology 36(4):321-324. Mathai AM, Naik R, Pai MR, Rai S, Baliga P. (2008) Microwave histoprocessing versus conventional histoprocessing. Indian J Pathol Microbiol 51 (1):12-16 Morales A, Essenfeld H, Essenfeld E, Duboue MC, Vincek V, Nadji M. (2002) Continuous-specimenflow, high-throughput, 1-hour tissue processing - A system for rapid diagnostic tissue preparation. Arch Pathol Lab Med 126(5):583-590. Morales AR, Nassiri M, Kanhoush R, Vincek V, Nadji M (2004). Experience with an automated microwave-assisted rapid tissue processing method: Validation of histologic quality and impact on the timeliness of diagnostic surgical pathology. Am J Clin Pathol 121:528- 536. Morales AR, Nadji M, Livingstone AS. (2008) Rapid-response, molecular-friendly surgical pathology: a radical departure from the century-old routine practice. J Am Coll Surg 207(3):320-325. Nadji M, Nassiri M, Vincek V, Kanhoush R, Morales AR. (2005) lmmuno-histochemistry of Tissue , Prepared by a Molecular-Friendly Fixation and Processing System. Applied lmmunohistochemistry and Molecular Morphology 13:277. Ragazzini T, Magrini E, Foschini MC, Eusebi V. (2005) The fast-track biopsy (FTB): description of a rapid histology and immunohistochemistry method for evaluation of preoperative breast core biopsies. International Journal of Surgical Pathology 13:247. Rohr LR, Layfield LJ, Wallin D, Hardy D. (2001) A comparison of routine and rapid microwave tissue processing in a surgical pathology laboratory. Quality of histologic sections and advantages of microwave processing. Am J Clin Pathol 115(5):703-708. Shi SR, Key ME, Kalra KL. (1991) Antigen retrieval in formalin-fixed, paraffin embedded tissues: An enhancement method for immunohistochemical staining based on microwave oven heating of tissue sections. Journal of Histochemistry and Cytochemistry 39:741. Tacha DE, Chen T. (1994) Modified antigen retrieval procedure: calibration technique for microwave ovens. Journal of Histotechnoloqy 17: 365. Vernon SE. (2004) Rapid frozen section with universal molecular fixative eliminates formaldehyde and preserves RNA in clinical samples. Pathology International. 54: A141. Vernon SE. (2005) Continuous Throughput Rapid Tissue Processing Revolutionizes Histopathology Workflow, Lab Med. 36(5):300-302 Visinoni F, Milios J, Leong AS-Y, Boon ME, Kok LP, Malcang IF. (1998) Ultra-Rapid Microwavable Pressure-Induced Histoprocessing: Description of a New Tissue Processor. The Journal of Histotechnology 21: 219. Vincek V, Nassiri M, Nadji M, Morales AR. (2003) A tissue fixative that protects macromolecules (DNA, RNA, and Protein) and histomorphology in clinical samples. Laboratory Investigation. 2003; 83:1427-1435. Willis D, Minshew J. (2002) Microwave Technology in the Histology Laboratory. Histologic: Technical bulletin for histotechnology. 35: 1-7. CHAPTER 6 FIXATION The first and most critical step in histotechnology is FIXATION, a process that preserves tissues from decay, thereby preventing autolysis or putrefaction. The quality of the section on the slide is only as good as the quality of the fixed tissue specimen. If fixation is not adequate, the other processes that follow, such as dehydration, clearing, infiltration, embedding, microtomy and staining, will also be inadequate. A poorly processed tissue will make it difficult for the pathologist to render a proper diagnosis. Fixation should be carried out as soon as possible after removal of the tissues (in the case of surgical pathology) or soon after death (in the case of autopsy) to prevent autolysis. Fixation terminates any ongoing biochemical reactions, and may also increase the mechanical strength or stability of the treated tissues. To accomplish this, tissue sections or smears are usually immersed in a fixative fluid, although in the case of smears, merely drying the preparation acts as a form of preservation. The fixatives employed prevent autolysis by inactivating lysosomal enzymes. They stabilize the fine structure, both inside and between cells, by making macromolecules resistant to dissolution by water and other liquids. Fixatives also inhibit the growth of bacteria and molds that give rise to putrefactive changes. The primary goal of fixation is to preserve the morphologic and chemical integrity of the cell in as life-like a manner as possible. The cell is composed of proteins, carbohydrates, lipids and other organic and inorganic substances. These cellular substances are loosely held together in the cellular protoplasm by hydrogen bonds or salt linkages that are in a constant state of chemical and biological equilibrium. With fixation, the shape, structure, intercellular relationship and chemical constituents of tissues are preserved. Fixation prevents degeneration, decomposition, putrefaction, and distortion of tissues after removal from the body. All vital cellular processes stop when the tissue is placed in a fixative. The weak chemical associations are changed into stable complexes that will not break down with further histologic handling. The second goal of fixation is to harden and protect the tissue from the trauma of further handling, so that it is easier to cut and process for microscopy. Fixation allows the tissue to be more properly oriented in the cassette in preparation for paraffin embedding and microtomy. For practical purposes, fixation aims to prevent or arrest the degenerative processes which commence as soon as a tissue is deprived of its blood supply. Autolysis results from tissue digestion by intracellular enzymes that are released when organelle membranes rupture. Bacterial decomposition or putrefaction is brought about by microorganisms which may already be present in the specimen. These are processes that must be prevented. Loss and diffusion of soluble substances must be avoided as much as possible by precipitation or coagulation of these components or by cross-linking them to other insoluble structural components. The tissues must be largely protected against the deleterious effects of tissue processing including infiltration with hot wax, but, more importantly, tissues must retain their reactivity to stains and other reagents including antibodies and nucleic acid probes. It is important to know that a fixative will initially produce a number of changes to the tissues in what is usually an aqueous environment. This will include shrinkage, swelling, and hardening of various components. The tissues will undergo further changes during processing when they are placed in a nonaqueous environment. For example, fixation in 10% buffered formalin will initially cause slight swelling of tissue specimens. During processing, however, the specimen may shrink and lose 20% -30% of its volume. The particular fixative employed will also influence the degree to which individual elements will stain with various histochemical and immuno-histochemical reagents. OBJECTIVES OF FIXATION To Preserve the Tissue Fixation preserves the tissue by stopping all cellular activities so that the cells can be viewed under the microscope as if they are still in their original living state. The tissue must be placed in the appropriate fixative as soon as possible after removal from the body. Leaving a tissue specimen in air for a prolonged period of time will cause it to dry out, and will result in distortion of its morphologic appearance. Leaving the tissue in water (a hypotonic solution) will cause the cell to swell, while a strong salt (hypertonic solution) will cause the cell to shrink. To Prevent Breakdown of Cellular Elements Surgical removal of the tissue from the body will deprive it of oxygen and nutrition, leading to a degradative chemical process or cell death. Every cell in the body has a structure or "suicide sac" within its cytoplasm called lysosome containing hydrolytic enzymes that are released when the integrity of the cell is destroyed. Postmortem decomposition ("autolysis") occurs due to the action of these hydrolytic enzymes. Fixation prevents autolysis by inactivating the lysosomal enzymes, or by chemically altering, stabilizing, and making the tissue components insoluble. Fixation also protects the tissue from further decomposition ("putrefaction") after death due to bacterial or fungal colonization and overgrowth. To Coagulate or Precipitate Protoplasmic Substances Fixation renders insoluble certain tissue components that may otherwise leak out during subsequent histologic handling. METHODS OF FIXATION Fixation of tissues can be achieved by physical or chemical means. Physical methods include heating, microwaving and cryo-preservation (freeze drying). Heat fixation is rarely used on tissue specimens, its application being confined to smears of microorganisms. However, microwave fixation, which can be regarded as a form of heat fixation, is now widely practiced in routine laboratories. Cryopreservation, usually in the form of freeze drying, has some applications in histochemistry but is not usually applied to diagnostic tissue specimens. Chemical fixation is usually achieved by immersing the specimen in the fixative solution (immersion fixation) or, in the case of small animals or some whole organs such as a lung, by perfusing or injecting the vascular system with fixative (perfusion fixation). For some specialized histochemical procedures, fixatives have occasionally been applied in the vapor form. For example, paraformaldehyde and osmium tetroxide can be used to vapor-fix freeze-dried tissues. There are two basic mechanisms involved in fixation: 1. Additive fixation whereby the chemical constituent of the fixative is taken in and becomes part of the tissue by forming cross-links or molecular complexes and giving stability to the protein. (Examples are formalin, mercury, and osmium tetroxide). 2. Non-additive fixation whereby the fixing agent is not incorporated into the tissue, but alters the tissue composition and stabilizes the tissue by removing the bound water attached to H-bonds of certain groups within the protein molecule. Upon removal of water, new cross-links are established within and among the protein molecules that stabilize the intercellular components, prevent autolysis and make them unsuitable for bacterial decomposition. (Examples are alcoholic fixatives) Fixative solutions may contain a single fixative agent dissolved in a solvent such as water or alcohol or more commonly, a buffer solution to stabilize pH. Some popular fixative solutions contain several different fixing agents in combination, the rationale being that the defects in one agent can be compensated for by the addition of another. For example acetic acid is present in some formulations to counter the shrinkage caused by other agents such as ethanol. Benefits of Fixation Allows thin sectioning of tissue by hardening tissue Prevents autolysis and inactivates infectious agents (except prion diseases) Improves cell avidity for special stains Practical Considerations to Optimize Fixation of Tissue Specimens should be transferred to fixative quickly (<1 hour) after surgery as deterioration will commence with the loss of blood supply. Tissues should be fixed in a sufficient volume of solution; generally in a ratio of 20:1 or at least 10:1 fixative to specimen, for penetration to occur in the most efficient manner. Anatomical barriers to fixation must be removed or incised (e.g. fascia, bone, feces, thick tissue) and large specimens must be sectioned or inflated with fixative (e.g. lung) or opened and cleaned (gastrointestinal tract) to allow penetration. Fixatives diluted and/or contaminated by bodily fluids (e.g. bile, blood, feces) will be reduced in concentration and must be replaced to ensure effectiveness. Pinning specimens to a corkboard or inserting a paper or gauze “wick” into tubular structures can improve fixation and reduce tissue distortion. Sufficient time must be allowed for penetration of fixative; rates of penetration vary according to fixative type. The size of tissue blocks should be small enough to allow adequate permeation of fixative (and subsequent processing solutions) through the perforations in cassettes. Prolonged fixation may be more difficult to reverse and may also result in loss of immunohistochemical antigenicity. The tissue hardens upon fixation and remains in whatever shape it was fixed in. This should be considered in those cases where the final orientation of the sections is important. Main Factors Involved in Fixation 1. Volume: The volume of fixative is important. Traditionally, the amount of fixative used has been 10-20 times the volume of tissue to be fixed. As the fixative molecules bind to the tissue, they are eventually depleted. This often causes poor fixation and can result in staining artefacts. One way to partially solve the problem is to change the solution at intervals to avoid exhaustion of the fixative. Agitation will also enhance fixation of the specimen. The most common error in histotechnology is insufficient ratio of tissue volume to fixative volume. 2. Hydrogen Ion Concentration: Fixation is best carried out close to neutral pH, in the range of 6-8. Outside this range, changes may occur that are detrimental to ultrastructural preservation of the tissue. Hypoxia of the tissue lowers the pH, so there must be buffering capacity in the fixative to prevent excessive acidity. Acidity favors formation of formalin-heme pigment that appears as black, polarizable deposits in tissue. Common buffers include phosphate, bicarbonate, cacodylate, and veronal. Commercial formalin is buffered with phosphate at a pH of 7. 3. Temperature: Many laboratories use tissue processors that work at 40°C for regular tissue processing. For electron microscopy and some histochemistry, the ideal temperature is 0-4°C. Generally, fixation at room temperature is sufficient to maintain excellent morphological detail, although some cells such as mast cells are best fixed at room temperature even for electron microscopy. Refrigeration is used to slow down decomposition if the tissue needs to be photographed and cannot be fixed immediately. Cells from different parts of the body decompose at different time intervals. Brain cells, in particular, deteriorate very quickly. On the other hand, bone marrow continues to undergo mitosis (growth) up to 30 minutes after death when refrigerated. Nucleic acids do not react with fixatives to any extent at room temperatures, and chemical reactions including those involved in fixation are more rapid at higher temperatures. The use of heat for fixation in bacteriology and for blood films is well known. Formalin heated to 60°C is sometimes used for the rapid fixation of very urgent biopsy specimens, although the risk of tissue distortion is increased. Increasing the temperature, as with all chemical reactions, will increase the speed of fixation, as long as you don't “cook” the tissue. An increase in temperature can increase the rate of fixation but can also increase the rate of autolysis. 4. Thickness of section: Tissue blocks should be small (e.g. 1 to 2 mm2 for electron microscopy and 2 cm2 wide for light microscopy) and thin (no more than 0.4 cm for light microscopy). These measurements should not be compromised in order to obtain full penetration and satisfactory fixation. Large solid tissue, such as uterus, should be opened or sliced thinly to improve penetration of fixatives. In addition, fecal matter and stomach contents can inhibit the penetration of fixative, as well as damage tissue during sectioning, and therefore must be removed before fixation. Most tissues can be cut and trimmed without prior fixation, except for the brain which is generally soft when unfixed. Brain is usually suspended whole in 10% buffered formalin for 2-3 weeks to ensure fixation and some hardening prior to sectioning. Because of its porous structure, fixation hardens the consistency of the brain and makes it easier to cut. The brain must be fixed before "grossing" or sectioning. An incompletely fixed tissue may lead to improper and incomplete clearing and impregnation, and may later prove to be a hindrance to normal sectioning and staining of specimen. Penetration of tissue depends upon the diffusability of each individual fixative, which is a constant. Formalin and alcohol penetrate the best, and glutaraldehyde the worst. Mercurials and others are somewhere in between. One way to get around this problem is by sectioning the tissues thinly (2 to 3 mm). Penetration into a thin section will occur more rapidly than for a thick section. Formalin penetrates tissues slowly so specimens may need to be opened, incised or sliced and left to fix for an adequate period of time prior to processing. Larger tissues require more fixatives and longer fixation time. Ideally, fixation is done slowly over one day or more. It is not practical or within the realm of patient care to wait any longer than 1 or 2 days, since clinicians generally need prompt diagnosis. To maintain an adequate fixation time of 4 to 6 hours, the recommended size of the tissue is 2 cm2, and no more than 4 mm. thick. A commonly quoted rate of penetration for aldehyde fixative is twoto-three millimeter per hour. Trying to fix very large pieces of tissue runs the risk of under-fixing the interior of the specimen resulting in biologic degradation of the constituent molecules. For solid material (e.g., liver) the longest dimension should not exceed 10-15mm. 5. Osmolality: If cells are fixed in a hypertonic solution, the cells may shrink. If the cells are fixed in a hypotonic solution, the cells may swell and burst. For that reason, we recommend using a normal phosphate buffered saline (PBS) based fixative. Hypertonic solutions give rise to cell shrinkage. Isotonic as well as hypotonic fixatives cause cell swelling and poor fixation. The best results are usually obtained using slightly hypertonic solutions (400-450 mOsm; isotonic solutions are 340 mOsm). Sucrose is commonly added to osmium tetroxide fixatives for electron microscopy. 6. Concentration: Concentration of fixative should be adjusted down to the lowest level possible. Too high a concentration may adversely affect the tissue and produce artefact similar to that caused by excessive heat. Formaldehyde is normally used as a 10% solution, and glutaraldehyde is normally used as a 3% solution. The presence of a buffer causes polymerization of the aldehyde, with consequent decrease in its effective concentration. Low concentrations of glutaraldehyde (0.25%) have been found to be an ideal concentration for immuno-electron microscopy. 7. Duration of fixation: Some tissues take longer to fix than others, depending on their structure. Fibrous organs such as uterus or intestinal tract take longer to fix than small or loosely textured tissues such as biopsies or scrapings. Fixation time can be cut down by using heat, vacuum, agitation or microwave. Primary fixation in buffered formalin is usually carried out for 2-6 hours during the day when the specimen is obtained, but the tissue may remain in fixative over the weekend without much adverse effect. Most of the formalin can be washed out after fixation for 24 hours. Prolonged fixation may cause shrinkage and hardening of tissue, and may severely inhibit enzyme activity and immunological reactions, although washing of the tissue in running water considerably restores the activity of some enzymes. For electron microscopy, it is recommended that diced tissues be fixed for 3 hours and then placed in a holding buffer. 8. Time Interval: Time interval from of removal of tissues to fixation is also important. In order to maintain tissue morphology, samples should be fixed immediately after removal or death to prevent autolysis or putrefaction. The longer the blood supply is interrupted, the poorer will be the quality of tissue. Artefacts will be introduced by drying, so if the tissue is left out in the open, it should be kept moist with saline. If fixation is not carried out under optimal conditions or if fixation is delayed, more cellular organelles will be lost, more nuclear shrinkage and artefactual clumping will occur, and the tissue specimen can be irreversibly damaged. No matter how much care is subsequently taken in tissue processing, microtomy and staining, the morphological and histochemical information obtainable from a poorly fixed specimen will be compromised. It is therefore important that the principles and practice of tissue fixation and the consequences of poor fixation are thoroughly understood by all staff involved in collecting and processing tissue specimens. Effects of Fixatives in General They reduce the risk of infection during handling and actual processing of tissues. They harden soft and friable tissues and make the handling and cutting of sections easier. This is usually accelerated by the action of alcohol during the dehydration process. They make the cells resistant to damage and distortion caused by the hypotonic and hypertonic solutions used during tissue processing. They inhibit bacterial decomposition. They increase the optical differentiation of cells and tissue components thereby rendering them more readily visible during examination. They may act as mordants or accentuators to promote and hasten staining, or they may inhibit certain dyes in favor of another (e.g. formaldehyde intensifies while osmium tetroxide inhibits hematoxylin staining). Characteristics of a Good Fixative It must be cheap. It must be stable. It must be safe to handle. It must kill the cell quickly thereby producing minimum distortion of cell constituents. It must inhibit bacterial decomposition and autolysis. It must produce minimum shrinkage of tissue. It must permit rapid and even penetration of tissues. It must harden tissues thereby making the cutting of sections easier. It must be isotonic, causing minimal physical and chemical alteration of the cells and their constituents. This is not, however, a strict rule since there are some hypotonic solutions (i.e. glacial acetic acid) producing tissue swelling, which are being used in conjunction with hypertonic solutions (e.g. picric acid) causing shrinkage of cells, to produce a compound which would give an optimal effect on the tissue structure. It must make cellular components insoluble to hypotonic solutions and render them insensitive to subsequent processing. It must permit the subsequent application of many staining procedures to facilitate easier and more profitable examination. Types of Fixatives There are four major groups of fixatives, namely the aldehydes, oxidizing agents, alcohol based fixatives and the metallic group of fixatives. The aldehydes (formaldehyde, glutaraldehyde) and oxidizing agents (osmium tetroxide, potassium permanganate) act by cross-linking proteins. Alcohol based fixatives (methyl alcohol, ethyl alcohol, acetic acid) are protein-denaturing agents. Metallic fixatives act by forming insoluble metallic precipitates like mercuric chloride and picric acid. The choice of the fixative is based on tissue and anticipated ancillary tests. 1. According to COMPOSITION A. Simple Fixatives -are made up of only one component substance. I. Aldehydes a. Formaldehyde b. Glutaraldehyde 2. Metallic Fixatives a. Mercuric chloride b. Chromate fixatives 3. Picric acid 4. Acetic acid 5. Acetone 6. Alcohol 7. Osmium Tetroxide B. Compound Fixatives - are those that are made up of two or more fixatives which have been added together to obtain the optimal combined effect of their individual actions upon the cells and tissue constituents. 2. According to ACTION: A. Microanatomical Fixatives -are those that permit the general microscopic study of tissue structures without altering the structural pattern and normal intercellular relationship of the tissues in question. 10% formal saline 10% neutral buffered formalin Heidenhain 's Susa Formal sublimate (formal corrosive) Zenker 's solution Zenker-formal (Kelly 's solution) Bouin's solution Brasil's solution B. Cytological Fixatives - are those that preserve specific parts and particular microscopic elements of the cell itself. 1. Nuclear Fixatives - are those that preserve the nuclear structures (e.g., chromosomes) in particular. They usually contain glacial acetic acid as their primary component due to its affinity for nuclear chromatin. They have a pH of 4.6 or less. Flemming's fluid Carnoy's fluid Bouin's fluid Newcomer's fluid Heidenhain's Susa Many fixatives have been used over the years, specifically for work with nucleic acids, but relatively few (including mercury and chromium salts) are known to react with them chemically. Mercuric chloride has been found to react with viruses, and causes the loss of their infective power. 2. Cytoplasmic Fixatives - are those that preserve cytoplasmic structures in particular. They must never contain glacial acetic acid which destroys mitochondria and Golgi bodies of the cytoplasm. They have a pH of more than 4.6. Flemming's fluid without acetic acid Kelly's fluid Formalin with "post-chroming" Regaud 's fluid (Muller 's fluid) Orth 's fluid For RNA, the precipitant fixatives - ethanol and acetone - give the best quantitative results using frozen tissues as the standard. 3. Histochemical Fixatives - are those that preserve the chemical constituents of cells and tissues. Formal Saline 10% Absolute Ethyl Alcohol Acetone Newcomer's Fluid Secondary Fixation is the process of placing an already fixed tissue in a second fixative in order: To facilitate and improve the demonstration of particular substances. To make special staining techniques possible (with secondary fixative acting as a mordant). To ensure further and complete hardening and preservation of tissues. Secondary fixation may be done before dehydration and on deparaffinized sections before staining, usually with 10% formalin or 10% formol saline as a primary fixative. The tissue may have been placed in a primary fixative for storage, or may require further fixation for special staining. For example, tissue fixed in 10% buffered neutral formalin may require secondary fixation with Zenker's solution (that acts as a mordant) prior to staining with Masson's trichrome (for connective tissue), Mallory's aniline blue stain (for collagen), or phosphotungstic acid-hematoxylin (PTAH) stain (for striated muscle). Post-Chromatization is a form of secondary fixation whereby a primarily fixed tissue is placed in aqueous solution of 2.5-3% potassium dichromate for 24 hours to act as mordant for better staining effects and to aid in cytologic preservation of tissues. Washing out is the process of removing excess fixative from the tissue after fixation in order to improve staining and remove artefacts from the tissues. Several solutions may be used. 1. Tap water is used to remove: a. excess chromates from tissues fixed in Kelly's, Zenker's, and Flemming's solutions b. excess formalin c. excess osmic acid 2. 50-70% alcohol is used to wash out excess amount of picric acid (Bouin's solution). 3. Alcoholic iodine is used to remove excessive mercuric fixatives. General Precautions in Handling and Fixation of Specimens 1. All tissue specimens must be properly labeled and identified. 2. Surgical specimens should be fixed as soon as possible after removal, or refrigerated if fixation is to be delayed, to prevent drying of surface layers and ultimate tissue distortion. 3. If fixation is not immediately possible, refrigerate but do not freeze. Slow freezing of unfixed tissues near 0°C must be avoided since this may promote formation of ice crystal artefacts. Repeated freezing and thawing, on the other hand, will destroy cellular organelles, release 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. enzymes and diffuse soluble components of the cell. Fresh tissue may be infectious. Consider any fresh or incompletely-fixed tissue as potentially infectious to you and other workers in your lab. Drying should be avoided to prevent shrinkage and distortion of tissue with loss of cellular detail. Drying of specimen surfaces will cause permanent damage and may mask any pathological change. Small endoscopic specimens are particularly susceptible to this type of damage. Small tissue biopsies may be placed in a petri dish with moistened filter paper to prevent drying. Distortion, rough handling or other mechanical damage to the tissue will cause permanent morphological changes which can make interpretation difficult. If placed in normal saline solution (NSS) during the operation, autolysis may occur before fixation is carried on. Tissues should not be more than 5 mm. thick except in lung edema (in which case tissue slices may be 1-2 cm. thick), with minimum squeezing and handling. Thin sections allow complete penetration by fixative in a short time. Purulent material, exudates or transudates should be marked and kept for possible cultures, smears and other bacteriologic examination. The amount of fixative must be adequate, approximately 10-20 times the volume of the tissue specimen except in osmium tetroxide which is very expensive, requiring only 5-10 times that of tissue volume for fixation. For prolonged fixation (e.g. museum preparation) volume of fixing fluid should not be less than 50 times that of the tissue. Contamination of fixed tissue with precipitates (e.g. in osmium tetroxide), should be avoided. In most instances, fixed tissues must be washed thoroughly to remove salts and/or pigments before staining. The required period for fixation should not be exceeded since this may cause excessive hardening or brittleness of tissues. Hollow organs (e.g. stomach, intestines) should be packed with cotton soaked in fixative or completely opened before being immersed in adequate fixing solution. Air-filled lungs may float on fixative. To avoid this, the organ may be covered with several layers of gauze to maintain it under surface. Human brains may be suspended by a cord tied under the Circle of Willis to prevent flattening. Intravascular perfusion (washing out of blood with Ringer's lactate) may lead to artifact formation with loss of blood content. Dense tissues such as brains are poorly penetrated, hence 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. require long fixation (usually 2 weeks prior to sectioning). Eyes should not be dissected before they are fixed since this may lead to immediate tissue collapse and wrinkling due to the escape of vitreous humor. They are not, however, easily penetrated due to tough sclera. Formal-alcohol must be injected before immersing the organ in the fixative. Frozen sections may lead to formation of ice crystal artifacts. To avoid rigor contraction and staining of artifacts when fixing muscle, the fresh biopsy material may be stretched by sutures on each end, or laid flat in a moist filter paper before suspending in fixative. Water should not be used for glycogen-containing tissues because glycogen is soluble in water. To assure rapid access of the fixative to all parts of the tissue, the tissue may be minced, that is, small pieces of specimen may be divided into small fragments and transferred to the vial of a fixative by means of a tooth pick. Hard tissues (e.g. cervix, uterine, fibroids, hyperkeratotic skin, fingernails, etc.) may be washed out in running water overnight and immersed in 4% aqueous phenol solution for 1-3 days (Lendrum's method). This will soften the tissue and allow easier sectioning without producing any marked distortion of the inner structures. Presence of mucus prevents complete penetration of fixative; hence, tissues that contain mucus are fixed slowly and poorly. Excess mucus may be washed away with normal saline solution. Fatty tissues should be cut in thin sections and fixed longer. Tissues containing large amount of blood (e.g. blood vessels and spleen) should be flushed out with saline before fixing. The position or shape that is desired for sectioning should be maintained before fixation. For example, a piece of intestine may be stretched out on a piece of paper and placed in the proper sized container, before pouring the fixative over it. The fixative should penetrate from all sides. Always place specimens into containers that already contain fixative. This will prevent adhesion of the specimen to the container. Where possible, hollow organs or specimens with natural cavities should be opened to allow immediate access to the fixative. Gentle agitation (swirling) of the specimen during its first few minutes in fixative will facilitate penetration. An adequate volume is vital (at least 20:1). An excess of fixative is required as its effective components 30. 31. 32. 33. 34. 35. may be depleted as part of the reactions of fixation. Fixatives should be carefully made from reagents of suitable quality, and fresh if so specified. Poor quality reagents can produce poor quality fixation. Some formulated fixatives should be prepared from stock solutions immediately before use because they are unstable (e.g., Helly’s fluid). If a specimen is received in fixative of dubious quality, it must be replaced with fresh fixative. Fixatives should be used only once. Specimens shed cells and tissue fragments into the fixative solution which could contaminate any subsequent specimen. Avoid metal lids. Some fixatives are highly corrosive and will attack metals (e.g., mercury salts). Some fixatives require that specimens be washed in water prior to processing (e.g., Zenker’s or Helly’s) or some other requirement may exist (phosphate may precipitate from buffer in concentrations of alcohol of greater than 70%). All fixatives are toxic and irritant. Anyone using fixatives should be aware of their potential hazards. Difficulties Caused by Improper Fixation: 1. Failure to arrest early autolysis of cells CAUSE: Failure to fix immediately (the tissue was probably allowed to dry before fixing); Insufficient fixative 2. Removal of substances soluble in fixing agent CAUSE: Wrong choice of fixative 3. Presence of artefact pigments on tissue sections CAUSE: Incomplete washing of fixative 4. Tissues are soft and feather-like in consistency CAUSE: Incomplete fixation 5. Loss or inactivation of enzymes needed for study CAUSE: Wrong choice of fixative 6. Shrinkage and swelling of cells and tissue structure CAUSE: Overfixation 7. Tissue blocks are brittle and hard CAUSE: Prolonged fixation Fixation Artifacts Formalin pigment is a well-known artifact that may be produced under acid conditions. The pigment may be eliminated or reduced by fixation in phenolformalin. The use of neutral buffered formalin and phenol-formalin almost completely stops the formation of formalin pigment which occurs with nonbuffered formaldehyde solutions, and also fixes tissues more rapidly. "Crush artifact" may be found in surgical specimens particularly in liver biopsies, associated with an intense eosinophilic staining at the center of the tissue in H&E stained sections. This may be due to partial coagulation of partially fixed protein by ethanol or by incomplete wax impregnation during subsequent histological processing. Lipid Fixation In conventional histopathological techniques, lipids are largely removed during preparation of tissues. Cryostat or frozen sections should be used for demonstrating lipid in tissues, followed by a general lipid stain. Fixatives containing mercuric chloride and potassium dichromate can be effective for preservation of lipids in cryostat sections. In general, phospholipids, which contain amino groups, are fixed by aldehydes. However, formaldehyde has been shown to react with unsaturated fatty acids during histological fixation, so that less lipid can be demonstrated histochemically in tissue that has been stored in formaldehyde for a long time. Baker's formal-calcium may be used to preserve phospholipids. Improved ultrastructural demonstration of lipids has been achieved by post-fixing in imidazole osmium tetroxide. Cholesterol may be fixed with digitonin for ultrastructural demonstration. Carbohydrate Fixation Carbohydrates are hydrophilic; they hold much water in the extracellular space by hydrogen bonding. There is also, of course, much water inside cells, since water accounts for about 60% of the weight of the human body. Alcoholic fixatives are generally recommended for glycogen fixation. Glycogen can be demonstrated satisfactorily enough for diagnosis, although losses of glycogen can be high (60-80%) in aqueous solution. Alcoholic formaldehyde is a better fixative in human skin compared with neutral buffered formaldehyde. The most useful fixatives for preserving glycogen are alcohol-based, such as Rossman's fluid or cold absolute alcohol. This is essential when processing tissues from patients with glycogen storage disease. There is better retention of glycogen if the section is coated with celloidin. Protein fixation Neutral buffered formal saline or formaldehyde vapor are the most commonly used fixatives for amino acid histochemistry. Fixation for Electron Microscopy The most useful primary fixatives for electron microscopy are osmium tetroxide, glutaraldehyde and paraformaldehyde, with the whole procedure performed at 4°C. For routine studies, glutaraldehyde or osmium tetroxide is adequate. For electron histochemistry and electron immunocytochemistry, Karnovsky's paraformaldehyde-glutaral-dehyde is useful. Post-fixation may be achieved with osmium tetroxide. Fixation for Enzyme Histochemistry The general aim of fixation for enzyme histochemistry is to preserve the maximum enzyme activity at its original localization, while also preserving structural integrity. The tissue for study may be fixed in 4% formaldehyde or formal-saline overnight, or fresh frozen cryostat sections may be fixed in acetone or formaldehyde and washed in distilled water prior to enzyme staining. Fixation for Immunofluorescence Immunofluorescence techniques are commonly used in pathology for the demonstration of various antibodies. The preservation of antigenicity has become a very important consideration when choosing a fixative. In many instances, formalin-fixed and paraffin embedded sections may be used. In more sensitive cases, the tissue must be prepared as a cryostat section and fixation limited to a few seconds in absolute methanol or acetone. Insufficient fixation will result in unfixed tissues being damaged by dehydrating fixative effect of ethanol during processing, causing loss of immunohistochemical antigenicity and poorer microtomy. Antigen-retrieval techniques are required for successful immunohistochemistry. Fixation for Immunohistochemistry Fixation is often an important consideration when preserving tissue for immunohistochemistry. Some antibodies cannot recognize antigens if they are cross-linked in a certain manner. Antigen retrieval may be used to uncover antigens after fixation. To ensure free access of the antibody to its antigen, the cells must be fixed and permeabilized. In general, fixation strengths and times are considerably shorter for cells than on the thicker, structurally complex tissue sections. For immunocytochemistry, sample preparation essentially entails fixing the target cells to the slide. Perfect fixation would immobilize the antigens, while retaining authentic cellular and subcellular architecture and permitting unhindered access of antibodies to all cells and subcellular compartments. Wide ranges of fixatives are commonly used, and the correct choice of method will depend on the nature of the antigen being examined and on the properties of the antibody used. Fixation methods fall generally into two classes: organic solvents and crosslinking reagents. Organic solvents such as alcohols and acetone remove lipids and dehydrate the cells, while precipitating the proteins on the cellular architecture. Cross-linking reagents (such as paraformaldehyde) form intermolecular bridges, normally through free amino groups, thus creating a network of linked antigens. Cross-linkers preserve cell structure better than organic solvents, but may reduce the antigenicity of some cell components, and require the addition of a permeabilization step, to allow access of the antibody to the specimen. Fixation with both methods may denature protein antigens, and for this reason, antibodies prepared against denatured proteins may be more useful for cell staining. The mechanism of fixation is dependent on the reagent used. Alcohol based fixation dehydrates cells/tissues, causing proteins to denature and precipitate in situ. Paraformaldehyde causes covalent cross-links between molecules, effectively gluing them together into an insoluble meshwork. Many researchers believe that tissue may be stored indefinitely in 10% neutral buffered formalin without harm. This is partly true; sections cut from such material and stained with a routine histological stain (e.g., Hematoxylin and Eosin) will look fine. Problems, however, will likely arise when such material is used for immunostaining since the cross-linking action continues and may irreversibly change the conformation (i.e., reduce the antigenicity) of antibody targets. Do not over-fix the tissue if it is intended to be used for immunostaining. Fixation method, time, and temperature are variables that need to be considered when developing immunohistochemistry protocols. Significantly altering fixation times between batches of specimens can have major consequences on the quality of immunostaining. Tissue fixation will permeabilize the cells and allow antibodies to access intracellular structures. There are several good reasons to use cryo-preservation rather than chemical fixation, including minimal alteration of the structure of proteins to be identified by immunostaining. Cryopreservation will avoid or reduce the ‘auto fluorescence’ (i.e., high background) that is inherent to formalin fixed paraffin embedded tissue when performing immunofluorescent microscopy. It promotes the preservation of delicate enzymes that are easily destroyed by fixation. Lipid stains (e.g., Oil Red O) require frozen sections since the ethanols used in tissue processing will extract the lipids. The morphology of cryosections, however, is often inferior to paraffin sections. Formalin-fixed-paraffin-embedded tissue sections typically 'auto fluoresce' when viewed under a fluorescent microscope (some tissues are worse than others); for this reason, immunofluorescent (IF) staining is best done on frozen sections. Background auto fluorescence, to a greater or lesser degree, can be suppressed by a post-staining Sudan Black treatment. The appropriate fixation method should be chosen according to the relevant application. 1. Acetone Fixation Fix cells in -20°C acetone for 5-10 minutes. No permeabilization step needed following acetone fixation. 2. Methanol Fixation Fix cells in -20°C methanol for 5-10 minutes. Permeabilization step is needed following methanol fixation. 3. Ethanol Fixation Fix cells in cooled 95% ethanol, 5% glacial acetic acid for 5-10 minutes. 4. Methanol-Acetone Fixation Fix in cooled methanol, 10 minutes at –20 °C. Remove excess methanol. Permeabilize with cooled acetone for 1 minute at –20 °C. 5. Methanol-Acetone Mix Fixation 1:1 methanol and acetone mixture. Make the mixture fresh and fix cells at -20 C for 5-10 minutes. 6. Methanol-Ethanol Mix Fixation 1:1 methanol and ethanol mixture. Make the mixture fresh and fix cells at -20 C for 5-10 minutes. 7. Formalin Fixation Fix cells in 10% neutral buffered formalin for 5-10 minutes. Rinse briefly with PBS. Permeabilize with 0.5% Triton X-100 for 10 minutes. 8. Paraformaldehyde-Triton Fixation Fix in 3-4% paraformaldehyde for 10-20 minutes. Rinse briefly with PBS. Permeabilize with 0.5% Triton X-100 for 10 minutes. 9. Paraformaldehyde-Methanol Fixation Fix in 4% paraformaldehyde for 10-20 minutes. Rinse briefly with PBS. Permeabilize with cooled methanol for 5-10 minutes at –20 °C. Practical Consideration: Do not reuse or save diluted antibodies. The antibodies adhere to the walls of the container and this effectively reduces the titer to zero. Freeze / thaw cycles will destroy antibodies. 'Dirty' (high background) polyclonal antibodies can sometimes be 'cleaned up' by storing the antibody over pieces of fixed tissue. Irrelevant antibodies in the serum may be adsorbed onto the tissue, effectively raising the titer of the specific antibodies. Another way to approach this is to incubate the antibody on a tissue section and then reuse the antibody on a second section. Antigen Retrieval for Immunostaining Antigen-retrieval methods in immunohistochemistry have shown that some of the reactions of fixation are reversible, particularly those of formaldehyde, but there is considerable variation in the quality of antigen preservation with various agents. However, these techniques do not work for all antigens. There are a number of methods commonly used to restore antigenicity. These methods are not generally used when working with cryo-preserved sections. Microwave antigen retrieval is one of several so-called ‘HIER’ (heat induced epitope retrieval) methods. Others include steaming, pressure cookers and autoclaves. Typically, this type of retrieval involves boiling the slides in a pH 6 citric acid buffer for ten minutes, followed by an additional fifteen minutes in the hot buffer. There are instances where changing the pH to 3 (in citric acid buffer) or to 8-9 (in a Tris EDTA buffer) are successful. Partial digestion of tissue sections by enzymatic method with one (or several) enzymes can sometimes be effective. Protocols are provided for pepsin, protease and trypsin. The enzyme concentrations and incubation times given may have to be adjusted. Effect of heat during fixation When the temperature of a fixative is raised or lowered (as is sometimes recommended for particular histochemical procedures), the rate of diffusion into the specimen is affected, as is the rate of the chemical fixation reactions occurring with the various tissue components. Increasing temperature accelerates the process of fixation. Excessive heat however, particularly if it is prolonged, can damage the cells and cause substantial shrinkage and hardening of the specimen. Today, most laboratories carry out primary fixation of specimens at ambient temperature and only after specimens are loaded onto the processor. Temperatures of between 37°C and 45°C are commonly employed. Another problem encountered in using hot fixative solutions to initially fix larger specimens (greater than 3mm thick), is that the outside of the specimen fixes rapidly while it may take quite some time for the fixative to penetrate to the center of the block which then may be poorly fixed or not fixed at all. The blocks will then show an exaggerated “zonal” fixation effect with different morphological and staining characteristics on the outside as compared to the inside of the specimen. MICROWAVE FIXATION The introduction ·of commercial microwave ovens has allowed easy access to controlled heating, thereby overcoming the previous problems of erratic heating brought about by direct flaming. Microwave fixation allows light microscopic techniques used in routine histopathology to be performed adequately. These include the standard stains, special stains, histochemistry for mucous substances, some enzyme histochemistry, and immuno-cytochemical techniques. Heat is considered to be the major factor responsible for the effects of microwaves during tissue fixation. Apart from increasing diffusion rates, heat will increase molecular kinetics and speed up chemical reactions. It is necessary to achieve a temperature in excess of 60°C within the specimen for primary microwave fixation, while lower temperatures may be acceptable for microwave-assisted fixation. Broadly, there are two ways in which microwave technology is used for tissue fixation. Fresh tissue, placed in saline or other isotonic solution, can be irradiated to produce primary fixation (referred to as “microwave fixation” or “microwave stabilization”). No chemical fixative is used at this stage. Alternatively, specimens can be placed in buffered formalin or some other fixative and, at a later stage, microwaved to assist the fixative action of the fixing agent (referred to as ‘microwave-assisted fixation”). In this latter case, the microwaving may be carried out while the tissue is in fixative, in which case there may be some hazard from toxic fumes produced, or the tissue may be transferred back to saline or buffer for the microwave step. Either way, the fixative solution must be present within the tissue for microwave-assisted fixation to occur. Microwave-assisted fixation is much more commonly used than primary microwave fixation. Proprietary fixatives of relatively low toxicity containing glyoxal, have been developed for use in microwave-assisted fixation. The rate at which the microwave energy will generate heat during tissue fixation depends on a number of factors including the power setting and power output of the oven, the volume and nature of the holding solution, the composition, shape and number of containers (including cassettes), the agitation or movement of the containers, and the number, volume and dimensions of the specimens being fixed. After microwaving they should immediately be sliced to 2 mm and placed in 70% ethanol. For microwave assisted fixation, 2 mm thick slices should be prepared from tissues initially fixed in formalin prior to microwave treatment. Because of the many variables involved in microwave fixation, it is vital that every aspect of the technique is fully standardized (including consistent specimen dimensions), that the microwave oven is properly calibrated, and that the staff performing the fixation step fully understands the factors that will influence its outcome. Advantages: 1. The chief advantage of microwave fixation is that the tissue is heated right through the block in a very short time, thereby potentially allowing the study of cellular processes that proceed very rapidly. 2. It is a non-chemical technique that is useful in preserving neurochemical substances in brain, such acetylcholine. 3. It may also be used for the rapid fixation of routine surgical specimens. 4. It significantly reduces the time taken for immuno-histochemistry and insitu hybridization. 5. Microwave treated tissue (at 50oC), post-fixed in osmium tetroxide also gives satisfactory results for electron microscopy. Disadvantages: 1. Microwaves generated by commercial ovens only penetrate tissue to a thickness of 10-15 mm. 2. There is no significant cross-linking of protein molecules, and subsequent chemical fixation may be needed. 3. Viable spores and other pathogens may remain in tissues processed with alcohol-based fixatives or microwaving alone. FIXATIVE: M Phosphate buffered, 40% Formaldehyde (10% formalin buffered to pH 7.3) Expose tissue to formaldehyde, followed by 1.5 minutes of microwave. PROCEDURE: 1. Fix tissue (no more than 5 mm) in formalin solution for 4 hours. 2. Soak blocks in water at room temperature for 1 minute in 100 ml of formalin. 4. Place in microwave, 450 watts, at 55°C for 1.5 to 4 minutes. 5. Remove blocks and slice tissue to 2 mm thick. 6. Place directly in alcohol. REFERENCES Atwood K, Farmilo AJ, Stead RH, Boenisch T. (2003) Fixation & tissue processing. From: Handbook for immunochemical staining methods. 3rd ed. Carpinteria, CA: Dako; p. 18–22, 44–46. Bancroft JD, Gamble M. (2008) Theory and practice of histological techniques. Churchill Livingstone Elsevier, Philadelphia, PA. Ben-Ezra J., Johnson DA., Rossi J. (1991) Effect of fixation on the amplification of nucleic acids from paraffin-embedded material by the polymerase chain reaction. Journal of Histochemistry & Cytochemistry 39(3): 351-354. Brown RW. (2009) Histologic Preparations: Common Problems and Their Solutions. Northfield, IL: College of American Pathologists. Carson FL, Hladik, C. (2009) Histotechnology: A self-instructional text. 3rd edition. Chicago: ASCP Press. Dapson RW. (1993) Fixation for the 1990's: a review of needs and accomplishments. Biotech Histochem 68(2):75-82. Drury RAB, Wallington EA. (1980) Carleton's histological technique. 5th ed., New York: Churchill Livingstone. Eltoum I, Fredenburgh J, Myers RB, Grizzle WE. (2001) Introduction to the theory and practice of fixation of tissues. J Histotechnol 24:173 -190. Eltoum I, Fredenburgh J, Grizzle WE. (2001) Advanced Concepts in Fixation: 1. Effects of Fixation on Immunohistochemistry, Reversibility of Fixation and Recovery of Proteins, Nucleic Acids, and other Molecules from Fixed and Processed Tissues. 2. Developmental Methods of Fixation. J Histotechnol 24(3):201-210. Feder N, Sidman RL (1958): Methods and Principles of Fixation by Freeze-Substitution. J Biophys Biochem Cytol; 4(5): 593–602. Fox CH, Johnson FB, Whiting J, Roller PP. (1985) Formaldehyde fixation. J Histochem Cytochem 33(8):845-853. Grizzle WE. (2009) Special symposium: fixation and tissue processing models. Biotech Histochem 84(5):185-193. Henwood A. (2010) What is the Best Procedure to Remove Formalin Pigment from FormaldehydeAcetic Acid-Alcohol Fixed Tissues? J Histotechnol 33(3):109-111. Hopwood D. (1996) Fixation and fixatives. In Bancroft J and Stevens A. eds. Theory and practice of histological techniques. New York: Churchill Livingstone. Kiernan JA. (2009) Histological and Histochemical Methods. Theory and Practice. 4th ed. Chapters 24, pp 12-73. Bloxham, UK: Scion. Krenacs L, Krenacs T, Stelkovics E, Raffeld M. (2010) Heat-induced antigen retrieval for immunohistochemical reactions in routinely processed paraffin sections. Methods Mol Biol 588: 103119. Leong AS and Gilham PN. (1989) The effects of progressive formaldehyde fixation on the preservation of tissue antigens. Pathology 21(4):266-268. Leong AS-Y. (1994) Fixation and fixatives. In Woods AE and Ellis RC eds. Laboratory histopathology. New York: Churchill Livingstone, 4.1-1 - 4.1-26. Lillie RD, Fullmer HM. (1976) Histopathologic Technic and Practical Histochemistry, 4th ed., New York: McGraw Hill. Mathal A, et al. (2008) Microwave histoprocessing versus conventional histoprocessing. Histopathology Section 51(1):12-16. Medawar PB. (1941) The rate of penetration of fixatives. Journal of the Royal Microscopical Society 61:46-57. Oliver C, Jamur MC. (2010) Fixation and embedding. Methods Mol Biol 588:353-362. Pearse AGE. (1980) Histochemistry, theoretical and applied. London: Churchill Livingstone. Pizzolato P. (1976) Formalin pigment (acid hematin) and related pigments. Am J Med Technol 42(11):436-440. Prento P, Lyon H. (1997) Commercial formalin substitutes for histopathology. Biotech Histochem 72(5):273-282. Sheehan DC, Hrapchak BB. (1980) Theory and Practice of Histotechnology. 2nd ed. St Louis, MO: Mosby. Suvarna KS, Layton C, Bancroft JD. (2012) Bancroft's Theory and Practice of Histological Techniques. Churchill Livingstone. Williams JH, Mepham BL, Wright DH. (1997)Tissue preparation for immunocytochemistry. J Clin Pathol 50; 422-428. Winsor L. Tissue processing. (1994) In Woods A and Ellis R eds. Laboratory histopathology. New York: Churchill Livingstone. CHAPTER 7 CHEMICAL FIXATIVES Tissue preservation requires the use of a fixative that can stabilize the proteins, nucleic acids and internal components of the tissue by making them insoluble. A variety of chemical fixatives are available for use, depending on the type of tissue to be preserved and the cytologic features to be demonstrated. Each fixative preserves morphology differently. Neutral buffered formalin does not provide adequate fixation in some cells and tissues, like connective tissues, mucus, and bone marrow. Fixatives other than alcohol or formalin may be preferred in certain circumstances and may be necessary for special studies and techniques. Substitutes for formalin are available that may provide adequate fixation with reduced risk of occupational health and safety hazards and improvements to staining results. There are two major groups of chemical fixatives, classified according to their mechanism of action: Crosslinking Fixatives (e.g., Aldehydes) that act by creating covalent chemical bonds between proteins in tissue. This anchors soluble proteins to the cytoskeleton, and lends additional rigidity to the tissue. Precipitating (or denaturing) fixatives (e.g., alcoholic fixatives) that act by reducing the solubility of protein molecules and (often) by disrupting the hydrophobic interactions that give many proteins their tertiary structure. The precipitation and aggregation of proteins is a very different process from the crosslinking that occurs with the aldehyde fixatives. Crosslinking fixatives – Aldehydes By far the most commonly used fixative in histology is formaldehyde, which fixes the tissues by forming cross-linkages in the proteins, particularly between lysine residues. This cross-linkage does not harm the structure of proteins greatly, so that antigenicity is not lost. Therefore, formaldehyde is good for immunohistochemical techniques. The standard solution is 10% neutral buffered formalin or approximately 3.7%-4.0% formaldehyde in phosphatebuffered saline. A buffer prevents acidity that would promote autolysis and cause precipitation of formol-heme pigment in the tissues. Its effects are reversible with excess water and the presence of buffer prevents formalin pigmentation. Other benefits of formaldehyde include long term storage and good tissue penetration. It is particularly good for immunohistochemistry techniques, and formaldehyde vapor can be used as a fixative for cell smears. Formaldehyde and Formalin The terms “formalin” and “formaldehyde” are often used interchangeably, although the chemical composition of each fixative is different. Formaldehyde is a gas produced by the oxidation of methyl alcohol, and is soluble in water to the extent of 37-40% weight in volume. The commercially available solution of formaldehyde contains 35-40% gas by weight (equivalent to 40% stock or concentrated formalin). Pure stock solution of 40% formalin is unsatisfactory for routine fixation since high concentrations of formaldehyde tend to over-harden the outer layer of the tissue and affect staining adversely. Formalin is made with formaldehyde but the percentage denotes a different formaldehyde concentration. For example, 10% neutral-buffered formalin (NBF or simply formalin) is really a 4% formaldehyde solution. This is because formalin is prepared from commercial-grade 37 to 40% formaldehyde, by diluting the concentrated formalin 1:10 in phosphate buffer. It is recommended that laboratories avoid the use of concentrated formalin solutions by purchasing commercially prepared 10% formalin. A. Buffered Formalin The most widely used fixative for routine histology is 10% neutral buffered formalin (NBF, approximately 4% formaldehyde), buffered to pH 7 with phosphate buffer. This fixative can effectively prevent autolysis and provide excellent preservation of tissue and cellular morphology. It is considered the fixative of choice for many other procedures that require paraffin embedding, including immunohistochemistry and interphase Fluorescent In-Situ Hybridization (FISH). Formalin usually contains about 10% methanol, which is added by the manufacturer to retard the formation of higher polymers that eventually fall out of solution as paraformaldehyde. Old bottles of formalin, especially after storage in a cold place, often contain deposits of this white powder. For routine fixation in 10% NBF, dissect the specimen as soon as possible and immerse it in a large volume of fixative (at least 10-20x volume of fix to tissue). Place at 4oC and fix ‘overnight’. After fixation, wash the tissue well in several changes of Phosphate Buffered Saline (PBS). The tissue may be stored in cold PBS for short periods of time (2 or 3 days) and will be safe in ethanol since there is no danger of bacterial degradation. However, it should not be stored in 70% ethanol for an extended period. Storage in PBS with sodium azide added at 4oC is a better alternative. The safest of all is to promptly fix, wash and deliver the samples either in phosphate buffered formalin or in alcohol for processing and embedding. Small (10×10×3 mm) pieces fixed in NBF for 12-24 hours will generally show good cytoplasmic preservation and nuclear detail. “Overnight” fixation (i.e., 8-12 hours) is generally indicated for 10 mm thick slices of tissues. Fixation with formaldehyde is largely complete in 24 hours, but cross-linking reactions continue for at least two weeks. Large, soft specimens such as whole human brains require 2-4 weeks in NBF to become firm enough to cut into slices from which samples can be taken for histology. Variations in time and conditions of fixation cause the majority of problems in histochemistry. There is some evidence that aldehydes continue to react with nucleic acids longer than after they are placed in fixative so that up to 30% may be lost during usual fixation. Physical entrapment of these very large molecules by the protein matrix may play a part in the retention of nucleic acids within the tissue. At temperatures normally used for fixation (20o-22°C), native DNA and RNA do not react with formaldehyde. If reaction mixtures are heated, at about 45°C in case of RNA and 65°C for DNA, reaction begins to take place due to the uncoiling of DNA and RNA. A similar phenomenon is observed in the case of reactions between glutaraldehyde and nucleic acids. This is important to note, because only at the elevated temperatures used when tissues are infiltrated with paraffin or resin, can a reaction with any remaining fixative take place. This lack of reaction potentially allows archival material to be used for DNA analysis in disease. For in-situ hybridization, there is no significant difference between fixation in neutral buffered formaldehyde, Bouin’s Solution or zinc formaldehyde. Advantages of using Formalin: 1. It is cheap, readily available, easy to prepare, and relatively stable, especially if stored in buffered solution. 2. It is compatible with many stains, and therefore can be used with various staining techniques depending upon the need of the tissues. 3. It does not over-harden tissues, even with prolonged periods of fixation, as long as solutions are regularly changed. 4. It penetrates tissues well. 5. It preserves fat and mucin, making them resistant to subsequent treatment with fat solvents, and allowing them to be stained for demonstration. 6. It preserves glycogen. 7. It preserves but does not precipitate proteins, thereby allowing tissue enzymes to be studied. It does not make tissues brittle, and is therefore recommended for nervous tissue preservation. 8. It allows natural tissue colors to be restored after fixation by immersing formalin-fixed tissues in 70% alcohol for one hour, and is therefore recommended for colored tissue photography. 9. It allows frozen tissue sections to be prepared easily. 10. It does not require washing out, unless tissues have stayed in formalin for excessively long periods of time. Disadvantages: 1. Fumes are irritating to the nose and eyes and may cause sinusitis, allergic rhinitis, or excessive lacrimation. 2. The solution is irritating to the skin and may cause allergic dermatitis on prolonged contact. 3. It may produce considerable shrinkage of tissues. 4. It is a soft fixative and does not harden some cytoplasmic structures adequately enough for paraffin embedding. 5. If unbuffered: a. Formalin reduces both basophilic and eosinophilic staining of cells, thereby reducing the quality of routine cytologic staining. Acidity of formic acid may, however, be used to an advantage when applying the silver impregnation technique of staining. b. It forms abundant brown pigment granules on blood-containing tissues, e.g., spleen, due to blackening of hemoglobin. 6. Prolonged fixation may produce: a. Bleaching of the specimen and loss of natural tissue colors. b. Dispersal of fat from the tissue into the fluid. c. Dissolution or loss of glycogen, and urate crystals FACTORS THAT INFLUENCE FORMALIN FIXATION Post-Mortem or Post-Surgical Interval. Rapid fixation by formalin is essential because autolysis begins immediately following disruption of blood and can influence the cellular morphology and staining. The time interval between death and fixation should be minimized and controlled whenever possible. If there is a necessary delay in fixation, the tissue should be immersed in cold phosphate-buffered saline (PBS). Tissues should not be allowed to dry before (or after) fixation. For certain studies, vascular perfusion with fixative may be recommended. Composition of Fixative. Formaldehyde fixation is usually optimal near physiological pH and ionic strength. Unfortunately, formalin is not stable and will gradually acidify to form more complex polymers which can have adverse effects on the tissue. This can be minimized by appropriate buffering and addition of small amounts of methanol. Commercial preparations in proper specimen containers are strongly recommended, but should not be used beyond the expiration date (usually 2 years), because of its short life span. Volume of Fixative Tissues should be immersed in a 10-20-fold volume of fixative. Large amounts of blood or protein-rich fluid can decrease the effective fixative concentration. If necessary, this problem can be minimized by briefly washing the tissue with PBS prior to fixation. If the fixative becomes cloudy or bloody after tissue is immersed, the fixative should be changed. Fixation Time. Fixation with 10% NBF at room temperature for a minimum of 24 hours at room temperature is recommended in most instances. However, some bloody, fatty or fetal tissues may require significantly longer fixation, e.g., up to 48- 72 hours. If the fixed tissue shows internal areas with normal coloration upon staining, the tissue should be left in fixation for a longer time period. Small surgical biopsies are sometimes fixed for only 6 hours, but 12 or more hours will often provide a better result. Inadequate-fixation can cause artefacts following exposure to alcohol during the subsequent tissue processing, or it can cause damage during decalcification. Too much-fixation can impair staining, and complicate sectioning. Temperature. An increase in temperature can increase the rate of fixation but can also increase the rate of autolysis. Primary fixation in the cold can slow autolysis, but it also slows the process of fixation, and premature cooling of a specimen in fixative can lead to inadequate fixation. Tissue Thickness. Formalin fixation is dependent on diffusion of the fixative into the tissue. The thicker the tissue, the more time is required to obtain complete penetration and crosslinking of tissue proteins. If the specimen is too thick, the center of the tissue can suffer from autolysis or incomplete fixation. For this reason, tissues should be no thicker than 3-5 mm. Careful slicing of tissues and solid organs before transferring them to fixative can greatly influence the efficiency of fixation by increasing exposed surface area and decreasing total thickness. This is particularly important for fatty, bloody organs and encapsulated tissues. When slicing tissues, it is important to use a sharp, clean blade to minimize compression artifacts. For very soft tissues, it is sometimes helpful to stiffen the tissue by brief fixation prior to cutting of thinner sections and additional fixation. Tubular organs can be cross-sectioned at small intervals to enhance exposure of the lumen to the fixative. Any luminal contents (like feces and mucus) should also be removed. Post-Fixation Storage. Non-coagulant fixatives such as formalin continue to crosslink proteins as long as they are in contact with the tissue. If there is to be a delay in processing after complete fixation (usually 24 hours or more), the fixed tissue can be stored for up to 3 days in the cold in 70% ethanol. However, it is essential that the tissue is completely fixed prior to transfer to the alcohol. Premature transfer of incompletely fixed tissue to alcohol precludes normal tissue processing. Mixture of Fixatives Two aldehyde fixative mixtures have been particularly useful for electron cytochemistry. The best known mixture of fixative is Karnovsky's paraformaldehyde-glutaraldehyde solution. Acrolein is another aldehyde which has been introduced as a mixture with glutaraldehyde or formaldehyde. It penetrates tissues rapidly, preserves morphology and enzyme activity at low concentrations, and may be used for immersion fixation of surgical biopsies. Precautions: 1. Prolonged storage of formaldehyde, especially at very low temperature, may induce precipitation of white para-formaldehyde deposits and produce turbidity although this, in itself, does not impair the fixing property of the solution. Precipitates may be removed by filtration or by addition of I0% methanol. 2. Methanol added as a preservative to formaldehyde will prevent its decomposition to formic acid or precipitation to paraformaldehyde, but it serves to denature protein, thereby rendering formalin unsuitable as a fixative for electron microscopy. 3. Concentrated solutions of formaldehyde must NEVER be neutralized since this might cause violent explosions. 4. Room should be properly ventilated with adequate windows and preferably with an exhaust fan to prevent inhalation of fumes and consequent injury to the eyes and nose. 5. Dermatitis may be avoided by the use of rubber gloves when handling specimens fixed in formalin. 6. The bleaching of tissues may be prevented by changing the fluid fixative every three months. 7. Natural tissue colors may be restored by immersing tissues in 70% alcohol after fixation. 8. Brown or black crystalline precipitate formed by the action of formic acid with blood can be removed from the sections prior to staining by treatment with saturated alcoholic picric acid or a 1% solution of potassium hydroxide in 80% alcohol. The use of neutral (phosphate) buffered formalin will prevent the pigmentation. 9. If fatty tissues are to be stored for a long time, cadmium or cobalt salts can be added to prevent dispersion of fat out into the fluid. 10. After use, formalin should be collected, sealed in appropriately labelled containers and disposed of by a commercial waste service. 11. All empty containers should be washed thoroughly with water. 12. Formalin should not be released into soil, drains and waterways. 13. Acid reaction due to formic acid formation can be buffered or neutralized by adding magnesium carbonate or calcium in a wide-mouth bottle to prevent violent explosion due to insufficient gas space for CO2 release. 14. Calcium acetate may be used to buffer formalin but it leaves a calcium deposit. The greatest amount of calcium deposit appears wherever the tissue is most exposed to the fixative (i.e., periphery of the block, within and around the walls of blood vessels, or in the proximity of hollow structures). 15. To improve staining and produce firmer and harder consistency, tissues fixed in formalin for 1 -2 hours may be placed again in Helly's fluid for 4-6 hours or in formol-sublimate for 4-16 hours (secondary fixation). 16. Formic acid develops over time producing an acidic solution, requiring a buffer to remain neutral pH (7.0). 17. Acidic formalin causes hematin pigment deposition in tissues particularly in hematogenous tissue after storage for extended periods of time. Methods are available to remove hematin but it is better to prevent its deposition by maintaining a neutral pH. 20. If post-fixed in osmic acid, the tissue must not be washed in demineralized water to prevent hypotonicity and bleaching. 22. Fixation of tissue blocks not exceeding 5 mm. in thickness is usually complete in 6-12 hours at room temperature. 10% Formal-Saline FORMULA: 40% formaldehyde: 100 ml Distilled water: 900 ml Sodium dihydrogen phosphate monohydrate: 4 gm Disodium hydrogen phosphate anhydrous 6.5 gm The solution should have a pH of 6.8 Fixation time: 12 – 24 hours Recommended Application: This is a simple microanatomical fixative made up of saturated formaldehyde (40%, by weight volume) diluted to 10% with sodium chloride. This mixture of formaldehyde in isotonic saline was widely used for routine histopathology prior to the introduction of phosphate buffered formalin. It is recommended for fixation of central nervous tissues and general post-mortem tissues for histochemical examination. It is also recommended for the preservation of lipids, especially phospholipids. The buffer tends to prevent the formation of formalin pigment. Many epitopes require antigen retrieval for successful immunohistochemical (IHC) staining procedure following its use. Most pathologists feel comfortable interpreting the morphology produced with this type of fixative. It often produces formalin pigment. Advantages: 1. It penetrates and fixes tissues evenly. 2. It preserves microanatomic and cytologic details with minimum shrinkage and distortion. 3. Large specimens may be fixed for a long time provided that the solution is changed every three months. 4. It preserves enzymes and nucleoproteins. 5. It demonstrates fats and mucin. 6. It does not over-harden tissues, thereby facilitating dissection of the specimen. 7. It is ideal for most staining techniques, including silver impregnation. 8. It allows natural tissue color to be restored upon immersion in 70% alcohol. Disadvantages are similar to formaldehyde with the following additions: 1. It is a slow fixative. The period of fixation is required to be 24 hours or longer. 2. Formal-saline fixed tissues tend to shrink during alcohol dehydration; this may be reduced by secondary fixation. 3. Metachromatic reaction of amyloid is reduced. 4. Acid dye stains less brightly than when fixed with mercuric chloride. 10% Neutral-Buffered Formalin FORMULA: Mix together: Sodium Dihydrogen Phosphate (Na2HPO4), anhydrous, 6.5 gm Sodium Dihydrogen Phosphate (NaH2PO4•H20) 4 gm Distilled water 900 ml Adjust pH to 7.4, then add: 40% formaldehyde 100 ml Advantages are similar to formal-saline with the following additions: 1. It prevents precipitation of acid formalin pigments on postmortem tissue. 2. It is the best fixative for tissues containing iron pigments and for elastic fibers which do not stain well after Susa, Zenker’s or chromate fixation. 3. It requires no post-treatment after fixation and goes directly into 80% alcohol for processing. Disadvantages: 1. It is longer to prepare; hence, is time-consuming. 2. Positivity of mucin to PAS is reduced. 3. It may produce gradual loss in basophilic staining of cells. 4. Reactivity of myelin to Weigert's iron hematoxylin stain is reduced. 5. It is inert towards lipids, especially neutral fats and phospholipids. Zinc formalin (unbuffered) FORMULA: Zinc sulphate 1 gm Deionized water 900 ml Stir until dissolved, then add – 40% formaldehyde 100 ml Recommended Applications Zinc formalin solutions were devised as alternatives to mercuric chloride formulations. They are said to give improved results with immunohistochemistry. There are a number of alternative formulas available some of which contain zinc chloride which is thought to be slightly more corrosive than zinc sulphate. Formol-Corrosive (Formol-Sublimate) FORMULA: Sat. Aq. Mercuric chloride 90 ml. Formaldehyde 40% 10 ml. Fixation time: 3-24 hours Formol-mercuric chloride solution is recommended for routine post-mortem tissues. Advantages: 1. It penetrates small pieces of tissues rapidly. 2. It produces minimum shrinkage and hardening. 3. It is excellent for many staining procedures including silver reticulum methods. 4. It brightens cytoplasmic and metachromatic stains better than with formalin alone. 5. Cytological structures and blood cells are well preserved. There is no need for "washing-out". Tissues can be transferred directly from fixative to alcohol. 6. It fixes lipids, especially neutral fats and phospholipids. Disadvantages: 1. Penetration is slow; hence, tissue sections should not be more than 1 cm thick. 2. It forms mercuric chloride deposits. 3. It does not allow frozen tissue sections to be made. 4. It inhibits the determination of the extent of tissue decalcification. Paraformaldehyde Paraformaldehyde is a polymerized form of formaldehyde, usually obtained as a fine white powder, which depolymerizes back to formalin when heated. It is suitable for paraffin embedding and sectioning, and also for immunocytochemical analysis. Paraformaldehyde fixed samples can also be stained for general histology but the degree of fixation is less vigorous than Bouin’s so the quality of the morphology obtained will be less. This fixative allows for subsequent immuno-detection of certain antigens and should therefore be used when the objective is to study morphology and protein expression simultaneously. Its effects are reversible by excess water and it avoids formalin pigmentation. Other benefits include: Long term storage and good tissue penetration. Karnovsky’s Fixative (4% Paraformaldehyde-1% Glutaraldehyde in 0.1M Phosphate Buffer) Karnovsky’s fixative is a mixture of paraformaldehyde and glutaral-dehyde. It is suitable for use when preparing samples for light microscopy in resin embedding and sectioning, and for electron microscopy. This fixative should always be prepared fresh. To prepare 8 % Paraformaldehyde (PFA): 1. Working in a fume cupboard wearing appropriate PPE, heat up 90 ml of water to 65 °C on a hotplate stirrer. 2. Add 8 g of paraformaldehyde (PFA) powder to the warm water. Use a magnetic stirrer and hotplate to dissolve PFA (approximately 15-20 minutes). 3. Slowly add drops of 1 M sodium hydroxide solution until the solution is clear. Make up to 100 ml with additional water. 4. Filter the fixative and adjust pH to 7.3-7.4. 5. Allow fixative to cool to room temperature. Store at −20 °C in aliquots. Frozen aliquots are stable for up to 6 months. 6. Dispense 25 ml for use in fixative. To prepare 0.2 M phosphate buffer 1. Solution X: Weigh out 35.61 g of disodium monohydrogen phosphate (Na2HPO4.2H2O) ± make up to 1000 ml with distilled H2O, stir until dissolved. 1 year shelf life at room temperature. 2. Solution Y: Weigh out 27.6 g of sodium dihydrogen phosphate (NaH2PO4.H2O) ± make up to 1000 ml with distilled H2O, stir until dissolved. 1 year shelf life at room temperature. 3. Add 40.5 ml of Solution X to 9.5 ml of Solution Y to give 50 ml 0.2 M phosphate buffer 4. Adjust to pH 7.4. This is to be used fresh. To prepare Karnovsky’s Fixative (for 100 ml add the following together) FORMULA: 8 % paraformaldehyde 25 ml 25 % glutaraldehyde 10 ml 0.2 M phosphate buffer 50 ml. Make up to 100 ml with distilled water. This is to be used fresh. Glutaraldehyde Another popular aldehyde for fixation is glutaraldehyde, made up of two formaldehyde residues, linked by a three carbon chain. Glutaraldehyde is a larger molecule than formaldehyde, and so its rate of diffusion across membranes is slower than formaldehyde. Consequently, glutaraldehyde fixation on thicker tissue samples may be hampered, but this problem can be overcome by reducing the size of the tissue sample. One of the advantages of glutaraldehyde fixation is that it causes rapid and irreversible changes, fixes quickly, is well suited for electron microscopy, it fixes well at 4oC, and it gives best overall cytoplasmic and nuclear detail. However, like formaldehyde, glutaraldehyde causes deformation of alpha-helix structure in proteins so it is not good for immunohistochemical staining. Tissues that have been fixed with a glutaraldehyde-based fixative must be treated with inert amine-containing molecules prior to the immunoassay. Free, unsaturated aldehyde groups are available to covalently link amine-containing moieties such as antibodies. The most efficient aldehyde blockers are ethanolamine and lysine. A standard fixative (2% buffered glutaraldehyde) followed by secondary fixation in osmium tetroxide, is satisfactory for electron microscopy. The glutaraldehyde must be cold and buffered and not more than 3 months old. The tissue must be as fresh as possible and preferably sectioned and fixed in glutaraldehyde at a thickness of no more than 1 mm to enhance fixation. It penetrates very poorly, but gives best overall cytoplasmic and nuclear detail. A 2.5% solution is used for small tissue fragments and needle biopsies fixed in 2-4 hours at room temperature. A 4% solution is recommended for larger tissues less than 4 mm thick, fixed in 6-8 hours up to 24 hours. Some fixation protocols call for a combination of formaldehyde and glutaraldehyde so that their respective strengths complement one another. Advantages of Glutaraldehyde over Formalin: 1. It has a more stable effect on tissues, giving a firmer texture with better tissue sections, especially of central nervous tissues. 2. It preserves plasma proteins better. 3. It produces less tissue shrinkage. 4. It preserves cellular structures better; hence, is recommended for electron microscopy. 5. It is more pleasant and less irritating to the nose. 6. It does not cause dermatitis. Disadvantages of Glutaraldehyde over Formaldehyde: 1. It is more expensive. 2. It is less stable. 3. It penetrates tissues more slowly. 4. It tends to make tissue (i.e. renal biopsy) more brittle. 5. It reduces PAS positivity of reactive mucin. This may be prevented by immersing glutaraldehyde-fixed tissues in a mixture of concentrated glacial acetic acid and aniline oil. Precautions: 1. The specimen vial must be kept refrigerated during the fixation process. 2. Solution may be changed several times during fixation by swirling the vials to make sure that the specimen is in contact with fresh solution all the time. PRECIPITATING (ALCOHOLIC) FIXATIVES Alcohols are protein denaturants and are not used routinely for tissues because they cause too much brittleness and hardness. The protein denaturants methanol, ethanol and acetone - are rarely used alone for fixing blocks unless studying nucleic acids. They are also very good for cytologic smears because they act quickly and give good nuclear detail. Spray cans of alcohol fixatives are marketed to physicians doing PAP smears. Alcohol alone (preferably methanol) is suitable for fixing thin layer preparations such as blood films or cell cultures. Solid specimens taken from patients with gout are usually fixed in 95% ethanol for subsequent histochemical detection of sodium urate crystals, which can be dissolved out of the tissue by water. Ethanol appears to give the most usable DNA fragments for polymerase chain reaction (PCR), whereas formaldehyde limits the size of fragments which can be retrieved. Alcohol rapidly denatures and precipitates proteins by destroying hydrogen and other bonds. It must be used in concentrations ranging from 70 to 100% because less concentrated solutions will produce lysis of cells. Ethanol (95%) is fast and cheap. Since smears are only a cell or so thick, there is no great problem from shrinkage, and since smears are not sectioned, there is no problem from induced brittleness. They are not good for electron microscopy, though, because they cause tissue shrinkage . Absolute alcohol can be used to fix and preserve glycogen, pigments, blood, tissue films and smears. The color of the specimen can be preserved for photographic work using 80% alcohol. Sometimes the specimen is taken out from fixative and placed in 80% alcohol to bring out some of the original color. Glycerin is also used in combination with alcohol for this purpose. Alcohol (ethanol or methanol) alone instantly coagulates proteins but causes considerable distortion of the tissue micro-anatomy. These unwanted changes are opposed by dilution of the alcohol with chloroform (immiscible with water), water, and/or acetic acid (which coagulates chromatin and opposes shrinkage) being miscible with water, alcohol and hydrocarbons. There are also many mixtures containing an alcohol (usually ethanol), formalin, acetic acid and 10% to 70% water, where the chemical reactions of formaldehyde with proteins are not retarded by buffering to a near-neutral pH. All these alcoholic fixatives contain acetic acid, which produces characteristic patterns of coagulated nuclear chromatin, facilitating the recognition of cell types. Methyl Alcohol 100% Advantages: 1. It is excellent for fixing dry and wet smears, blood smears and bone marrow tissues. 2. It fixes and dehydrates at the same time. Disadvantages: 1. Penetration is slow. 2. If left in fixative for more than 48 hours, t issues may be over hardened and difficult to cut. Isopropyl Alcohol 95% - is used for fixing touch preparations , although some touch preparations are air dried and not fixed, for certain special staining procedures such as Wright-Giemsa. Ethyl Alcohol - is used at concentrations of 70-100%. If the lower concentrations are used, the RBC's become hemolyzed and WBC's are inadequately preserved. It may be used as a simple fixative. It is, however, more frequently incorporated into compound fixatives for better results. Fixation Time: 18-24 hours Advantages: 1. It preserves but does not fix glycogen. 2. It fixes blood, tissue films and smears. 3. It preserves nucleoproteins and nucleic acids, hence, is used for histochemistry, especially for enzyme studies. 4. It fixes tissue pigments fairly well. 5. It is ideal for small tissue fragments. 6. It may be used both as a fixative and dehydrating agent. Disadvantages: 1. Hemosiderin preservation is less than in buffered formaldehyde. 2. It is a strong reducing agent; hence, should not be mixed with chromic acid, potassium dichromate and osmium tetroxide which are strong oxidizing agents. 3. Lower concentrations (70-80%) will cause RBC hemolysis and inadequately preserve leukocytes. 4. It dissolves fats and lipids, as a general rule. Alcohol-containing fixatives are contraindicated when lipids are to be studied. 5. It causes glycogen granules to move towards the poles or ends of the cells (polarization). 6. Tissue left in alcohol too long will shrink, making it difficult or impossible to cut. 7. It causes polarization of glycogen granules. 8. It produces considerable hardening and shrinkage of tissues. Carnoy’s Fixative FORMULA: Absolute alcohol 60 ml. Chloroform 30 ml. Glacial acetic acid 10 ml. Fixation Time: 1-3 hours Advantages: 1. It is considered to be the most rapid fixative and may be used for urgent biopsy specimens for paraffin processing within 5 hours. 2. It fixes and dehydrates at the same time. 3. It permits good nuclear staining and differentiation. 4. It preserves Nissl granules and cytoplasmic granules well. 5. It preserves nucleoproteins and nucleic acids. 6. It is an excellent fixative for glycogen since aqueous solutions are avoided. 7. It is very suitable for small tissue fragments such as curettings and biopsy materials. 8. Following fixation for one hour, tissues may be transferred directly to absolute alcohol-chloroform mixture, thereby shortening processing time. 9. It is also used to fix brain tissue for the diagnosis of rabies. Disadvantages: 1. It produces RBC hemolysis, dissolves lipids and can produce excessive hardening and shrinkage. 2. It causes considerable tissue shrinkage. 3. It is suitable only for small pieces of tissues due to slow penetration. 4. It tends to harden tissues excessively and distorts tissue morphology. 5. It dissolves fat, lipids, and myelin. 6. It leads to polarization unless very cold temperatures (-70°C) are used. 7. It dissolves acid-soluble cell granules and pigments. Clarke’s solution FORMULA: Ethanol (absolute) 75 ml Acetic acid glacial 25 ml Fixation time: 3 - 4 hours Recommended Applications Clarke’s solution has been used on frozen sections and smears. It can produce fair results after conventional processing if fixation time is kept very short. It preserves nucleic acids but extracts lipids. Tissues can be transferred directly into 95% ethanol. Alcoholic formalin FORMULA: 40% Formaldehyde: 100 ml 95% Ethanol: 900 ml 0.5 g calcium acetate can be added to ensure neutrality Fixation time: 12 – 24 hours Recommended Applications: Alcoholic-formalin combines a denaturing fixative with the additive and cross-linking effects of formalin. It is sometimes used during processing to complete fixation following incomplete primary formalin fixation. It can be used for fixation or post-fixation of large fatty specimens (particularly breast), because it will allow lymph nodes to be more easily detected as it clears and extracts lipids. If used for primary fixation specimens, it can be placed directly into 95% ethanol for processing. Formol-acetic alcohol FORMULA: Ethanol absolute: 85 ml 40% formaldehyde: 10 ml Acetic acid glacial: 5 ml Fixation time: 1 - 6 hours Recommended Applications Formol-acetic acid alcohol is a faster acting agent than alcoholic formalin due to the presence of acetic acid that can also produce formalin pigment. It is sometimes used to fix diagnostic cryostat sections. If used for primary fixation, the specimens can be placed directly into 95% ethanol for processing. Gendre's Fixative FORMULA: 95% Ethyl alcohol saturated with picric acid 80 ml. Strong formaldehyde solution 15 ml. Glacial acetic acid 5 ml. Post-fixation with phenol-formalin for 6 hours or more can enhance immunoperoxidase studies on the tissues, and in some cases, electron microscopy, if it is necessary at a later time to establish a diagnosis. Advantages: 1. Fixation is faster (fixation time is reduced to one-half). 2. It can be used for rapid diagnosis because it fixes and dehydrates at the same time, e.g., in the frozen section room. 3. It is good for preservation of glycogen and for micro-incineration technique (the burning of a minute tissue specimen for identification of mineral elements from the ashes). 4. It is used to fix sputum, since it coagulates mucus. Disadvantages: 1. It produces gross hardening of tissues. 2. It causes partial lysis of RBC. 3. Preservation of iron-containing pigments is poor. 4. Formaldehyde does not give as good a morphological picture as glutaraldehyde. 5. Formaldehyde causes little cross-linking under usual fixation conditions where low concentrations of proteins are used, while glutaraldehyde is most effective at cross-linking. Newcomer's Fluid FORMULA: Isopropyl alcohol 60 ml. Propionic acid 30 ml. Petroleum 30 ml. Ether 10 ml. Acetone 10 ml. Dioxane 10 ml. Fixation time: 12-18 hours at 3°C Advantages: 1. It is recommended for fixing mucopolysaccharides and nuclear proteins. 2. It produces better reaction in Feulgen stain than Carnoy's fluid. 3. It acts both as a nuclear and histochemical fixative. METALLIC FIXATIVES Mercurials fix tissues through an unknown mechanism that increases staining brightness and gives excellent nuclear detail. However, mercurials penetrate poorly and produce tissue shrinkage. Their best application is for fixation of hematopoietic and reticuloendothelial tissues. 1. Mercuric Chloride Mercuric chloride is the most common metallic fixative, frequently used in saturated aqueous solutions of 5-7%. Mercuric chloride is widely used as a secondary fixative reacting with a number of amino acid residues and accompanied by spectroscopic changes, probably due to reaction with histidine residues. Mercuric chloride-based fixatives are used as an alternative to formaldehyde-based fixatives to overcome poor cytological preservation and include such well-known fixatives as B-5 and Zenker's solution. They penetrate relatively poorly and cause some tissue hardness, but give excellent nuclear detail. These fixatives work by additive and coagulative means. The major advantages of using these fixatives include good penetration resulting in more intense immunostaining and the preservation of cytological detail that allow for easier morphological interpretation. These fixatives often contain neutral salt to maintain tonicity and can be mixed with other fixatives to provide a balanced solution. Their best application is for fixation of hematopoietic and reticuloendothelial tissues. Mercuric chloride penetrates poorly and produces shrinkage of tissues, so it is usually combined with other fixative agents. Tissues fixed with mixtures containing mercuric chloride (except Susa) contain black precipitates of mercury. Mercury deposits are removed from deparaffinized sections before staining, by treating the section with 0.5% iodine solution in 70% ethanol for 510 minutes. Sections are rinsed in water, decolorized for 5 minutes in 5% sodium thiosulfate and washed in running water. Following mercuric chloride post-fixation, the ultrastructural preservation is poor, but trichrome staining methods also work well and many immunoperoxidase techniques are satisfactory. If the glacial acetic acid is replaced by 5 ml of formalin (37–40% formaldehyde), the resulting solution is Helly's fixative, sometimes also called "Formol-Zenker". Helly’s fixative is stable for only a few hours because the formaldehyde and dichromate components react, producing formic acid and chromic ions; the orange solution becomes greenish. Advantages: 1. It penetrates and hardens tissues rapidly and well. 2. Nuclear components are shown in fine detail. 3. It precipitates all proteins. 4. It has a greater affinity to acid dyes and is preferred in lieu of formaldehyde for cytoplasmic staining. 5. Trichrome staining is excellent. 6. It is the routine fixative of choice for preservation of cell detail in tissue photography. 7. It permits brilliant metachromatic staining of cells. 8. It is recommended for renal tissue, fibrin, connective tissue and muscle. Disadvantages: 1. It causes marked shrinkage of cells (this may be counteracted by addition of acid). 2. It rapidly hardens the outer layer of the tissue with incomplete fixation of the center; therefore, thin sections should be made. 3. Penetration beyond the first 2-3 millimeters is slow; hence, not more than 5 mm. thickness of tissues should be used. 4. If left in fixative for more than 1-2 days, the tissue becomes unduly hard and brittle. 5. It prevents adequate freezing of fatty tissues and makes cutting of frozen tissues difficult. 6. It causes considerable lysis of red blood cells and removes much iron from hemosiderin. 7. It is inert to fats and lipids. 8. It leads to the formation of black granular deposits in the tissues. 9. It reduces the amount of demonstrable glycogen. 10. Compound solutions containing mercuric chloride deteriorate rapidly upon addition of glacial acetic acid to formalin. 11. It is extremely corrosive to metals. Precautions: 1. Sections must be cleared of mercury deposits before immunostaining. Black deposits may be removed by adding saturated iodine solution in 95% alcohol, the iodine being decolorized with absolute alcohol in the subsequent stages of dehydration. 2. Compound solutions must always be freshly prepared. 3. The use of metallic forceps and of metal caps to cover the bottles containing the fixative should be avoided. 4. Contact of mercuric fixatives with personal jewelries should be avoided. 5. Mercury-containing solutions (Zenker's or B-5) should always be discarded into proper containers. Mercury, if poured down a drain, will form amalgams with the metal that build up and cannot be removed. Zenker's Solution FORMULA: Mercuric chloride 5 gm Potassium dichromate 2.5 gm Distilled water 100 ml Acetic acid, glacial 5 ml (to be added just before use) Heat, cool, filter in brown bottle. Wash sample for 24 hours with distilled water after fixation. Fixation time: 12-24 hours Advantages: 1. It produces a fairly rapid and even fixation of tissues. 2. Stock solutions keep well without disintegration. 3. It is recommended for trichrome staining. 4. It permits brilliant staining of nuclear and connective tissue fibers. 5. It is recommended for congested specimens (such as lung, heart and blood vessels) and gives good results with PTAH and trichrome staining. 6. It is compatible with most stains. 7. It may act as a mordant to make certain special staining reactions possible. 8. It is a stable fixative that can be stored for many years. Disadvantages: 1. Penetration is poor. 2. It is not stable after addition of acetic acid. 3. Prolonged fixation (for more than 24 hours) will make tissues brittle and hard. 4. It causes lysis of red blood cells and removes iron from hemosiderin. 5. It does not permit cutting of frozen sections. 6. It has the tendency to form mercuric pigment deposits or precipitates. 7. Tissue must be washed in running water for several hours (or overnight) before processing. Insufficient washing may inhibit or interfere with good cellular staining. Precautions: 1. Do not let tissues stay in solution for more than 24 hours. 2. Solutions must always be freshly prepared. 3. Tissues should be cut thin (2-3 mm.) and hollow organs should be opened to promote complete penetration and fixation. 4. Tissues must be washed out thoroughly in running water to permit good staining. 5. It produces mercury pigment which should be removed from sections prior to staining and can produce chrome pigment if tissue is not washed in water prior to processing. After water washing, tissue should be stored in 70% ethanol. 6. Mercuric deposits may be removed by immersing tissues in alcoholic iodine solution prior to staining, through a process known as dezenkerization. Chemically, de-zenkerization is done by oxidation with iodine to form mercuric iodide, which can be subsequently removed by treatment with sodium thiosulfate, using the following procedure: 1. Bring slides to water. 2. Immerse in Lugol's iodine (5 minutes). 3. Wash in running water (5 minutes). 4. Immerse in sodium thiosulfate 5% (5 minutes). 5. Wash in running water (5 minutes). 6. Proceed with required water soluble stain. Zenker-Formol (Helly’s) Solution FORMULA: Mercuric chloride, 5 gm Potassium dichromate, 2.5 gm Distilled water, 100 ml 40% formaldehyde 5 ml (to be added immediately before use) Heat, cool, filter in brown bottle. Wash sample for 24 hours with distilled water after fixation. Fixation time: 4 – 24 hours Practical Applications: Zenker’s solution is an excellent fixative for bone marrow, extramedullary hematopoiesis and intercalated discs of cardiac muscle. However, it produces mercury pigment which should be removed from sections prior to staining and it can produce chrome pigment if tissue is not washed in water prior to processing. After water washing, fixed tissue should be stored in 70% ethanol. Because of the low pH of this fixative, formalin pigment may also occur. Never use metal forceps to handle tissue. Advantages: 1. It is an excellent microanatomic fixative for pituitary gland, bone marrow and blood containing organs such as spleen and liver. 2. It penetrates and fixes tissues well. 3. Nuclear fixation and staining with Helly’s solution is better than with Zenker's. 4. It preserves cytoplasmic granules well. Disadvantages: The disadvantages of Helly's solution are similar to Zenker's except that brown pigments are produced if tissues (especially blood containing organs) are allowed to stay in the fixative for more than 24 hours due to RBC lysis. This may be removed by immersing the tissue in saturated alcoholic picric acid or sodium hydroxide. Lillie’s B-5 Fixative Lillie’s B5 fixative is 4% aqueous formaldehyde with 0.22M mercuric chloride and 0.22M acetic acid. This mixture enhances nuclear detail, which is important for identifying normal and abnormal cell types in bone marrow (hematopoietic tissue) specimens. The coagulation of nuclear chromatin is an effect of the acetic acid. The mercuric chloride ensures rapid structural stabilization and also facilitates bright staining by many of the dyes used in microtechnique. The reasons for this effect on stainability are not understood. A dirty looking brown crystalline precipitate, probably mercurous chloride (Hg2Cl2) forms in all parts of tissues fixed in mixtures containing HgCl2. It is called mercury pigment and before staining must be removed by sequential treatments with iodine and sodium thiosulfate solutions. Because it contains mercury, B-5 is subject to toxic waste disposal regulations, which apply to the fixative solution and every solution thereafter that has been contaminated with mercury. FORMULA: B-5 Stock solution Mercuric chloride: 12 g Sodium acetate anhydrous: 2.5 g Distilled water: 200 ml Working solution: (prepare immediately before use) B-5 stock solution: 20 ml 40% formaldehyde: 2 ml Fixation time: 4 – 8 hours Practical Applications: 1. Despite its mercuric chloride content and consequent problems with disposal, this solution is popular for fixation of hematopoietic, bone marrow biopsies and lymphoid tissue. 2. Rapid fixation can be achieved in 1 1/2 - 2 hours. 3. It produces excellent nuclear detail, provides good results with many 4. 5. 6. 7. 8. 9. special stains, and is recommended for immunohisto-chemical staining. Sections will require the removal of mercury pigment prior to staining. Tissue should not be stored in this fixative but placed in 70% ethanol instead. Over-fixation hardens the tissue and makes cutting difficult. The two working solutions are kept separate, since the mixture is unstable. Mix just prior to use. Some B-5 solutions will form precipitate on standing, but this is of no consequence. As with all mercuric chloride fixatives, the mercury pigment can be removed by de-zenkerization. Heidenhain's Susa Solution – is recommended mainly for tumor biopsies especially of the skin; it is an excellent cytologic fixative. FORMULA: Mercuric chloride 45 gm Sodium chloride 5 gm Trichloroacetic acid 20 gm Glacial acetic 40 ml Acid Formaldehyde 40% 200 ml 40% Distilled water 800 ml Fixation time: 3-12 hours Advantages: 1. It penetrates and fixes tissues rapidly and evenly. 2. It produces minimum shrinkage and hardening of tissues due to the counter-balance of the swelling effects of acids and the shrinkage effect of mercury. 3. It permits most staining procedures to be done, including silver impregnation, producing brilliant results with sharp nuclear and cytoplasmic details. 4. It permits easier sectioning of large blocks of fibrous connective tissues. 5. Susa-fixed tissues may be transferred directly to 95% alcohol or absolute alcohol, thereby reducing processing time. Disadvantages: 1. Prolonged fixation of thick materials may produce considerable shrinkage, hardening and bleaching; hence, tissues should not be more than 1 cm. thick. 2. RBC preservation is poor. 3. Some cytoplasmic granules are dissolved. 4. Mercuric chloride deposits tend to form on tissues; these may be removed by immersion of tissues in alcoholic iodine solution. 5. Weigert's method of staining elastic fibers is not possible in Susa fixed tissues. Precautions: After using Heidenhain's Susa fixative, the tissue should be transferred directly to a high-grade alcohol, e.g. 96% or absolute alcohol, to avoid undue swelling of tissues caused by treatment with low-grade alcohol or water. OXIDIZING AGENTS Oxidizing agents include permanganate fixatives (potassium permanganate), potassium dichromate, chromic acid and osmium tetroxide. The oxidizing fixatives can react with various side chains of proteins and other biomolecules, allowing formation of crosslinks that stabilize tissue structure but cause extensive denaturation despite preserving fine cell structure and are used mainly as secondary fixative. Osmium Tetroxide (Osmic Acid; OsO4) This is a pale yellow powder which dissolves in water (up to 6% at 20°C) to form a strong oxidizing solution. Fixation with osmium tetroxide or postosmication of glutaraldehyde-fixed tissue causes the complete denaturation of protein. Potassium permanganate and potassium dichromate are also oxidizing agents but are less reactive towards proteins than is osmium tetroxide. Osmium tetroxide is traditionally used in electron microscopy both as a fixative and a heavy metal stain. Osmium tetroxide is a good fixative and excellent stain for lipids in membranous structures and vesicles. The most prominent staining in adherent human cells (HeLa) is seen on lipid droplets. Some intracellular structures are also visualized. Osmium tetroxide functions as a secondary fixative by reacting with lipids. It is believed that the unsaturated bonds of fatty acids are oxidized by OSO4 and it is reduced to a black metallic osmium (MW 254.2) which is electron dense and adds contrast to biological tissues (secondary stain). Visualized cellular structures depend on the fixation protocols. In glutaraldehyde fixation, the nucleoli are visible, but overall nuclear staining is weak. In paraformaldehyde fixation, the nuclear staining becomes more prominent, but some intracellular structures are lost. As a first choice, fixing tissues with a combination, glutaraldehyde and paraformaldehyde are recommended. Osmium tetroxide penetrates slower than glutaraldehyde (0.5 mm/hr.) and the tissue takes on a progressively blackened appearance depending upon their lipid content. Fixation experiments with buffered OsO4 solutions have shown that the appearance of the fixed cells is conditioned by the pH of the fixative; thus, 1% OsO4 buffered at pH 7.3-7.5 with acetate-veronal buffer is recommended as an appropriate fixative for electron microscopy. Procedure: 1. Wash the sample four times with PBS. 2. Fix with 2% Paraformaldehyde, 0.1% Glutaraldehyde in PBS for 30 minutes. 3. Wash four times with PBS. 4. Wash four times with double distilled water. 5. Prepare 0.1% OsO4 solution by diluting the 4% stock solution in double distilled water. 6. Incubate the sample with 0.1% OsO4 for 30 minutes. 7. Wash four times with double distilled water. Advantages: 1 It fixes conjugated fats and lipids permanently by making them insoluble during subsequent treatment with alcohol and xylene. Fats form hydrated osmium dioxide, are stained black and therefore are easier to identify. 2. It preserves cytoplasmic structures well, e.g. Golgi bodies and mitochondria. 3. It fixes myelin and peripheral nerves well, hence, it is used extensively for neurological tissues. 4. It produces brilliant nuclear staining with safranin. 5. It adequately fixes materials for ultrathin sectioning in electron microscopy, since it rapidly fixes small pieces of tissues and aids in their staining. 6. It precipitates and gels proteins. 7. It shows uniformly granular nuclei with clear cytoplasmic background. 8. Some tissues (e.g. adrenal glands) are better fixed in vapor form of osmium tetroxide. This eliminates "washing out" of the fixed tissues. 9. Osmium tetroxide completely permeabilizes cell membranes. The osmolarity of the fixative vehicle or solute is relatively unimportant. 10. It penetrates tissue blocks in a gradient and in large samples the center of the block may not be as well fixed as the peripheral areas. 11. Over-fixation with osmium tetroxide may result in extraction of cell components during dehydration and increases the hardness and brittleness of the tissue (for most tissues, 1mm blocks, should not be exposed to osmium for less than 0.5 or more than 1.5 hours). Disadvantages: 1. It is very expensive. 2. It is a poor penetrating agent, suitable only for small pieces of tissues (2-3 mm. thick). 3. It is readily reduced by contact with organic matter and exposure to sunlight, forming a black precipitate which settles at the bottom of the container. 4. Prolonged exposure to acid vapor can irritate the eye, producing conjunctivitis, or cause the deposition of black osmic oxide in the cornea, producing blindness. 5. It inhibits hematoxylin and makes counterstaining difficult. 6. It is extremely volatile. Precautions: I. Eyes and skin may be protected by working in a fume hood or wearing protective plastic masks or gloves while using osmium tetroxide. 2. It should be kept in a dark-colored, chemically clean bottle to prevent evaporation and reduction by sunlight or organic matter. 3. It should be kept in a cool place or refrigerated to prevent deterioration. 4. Addition of saturated aqueous mercuric chloride solution (0.5 to 1 ml/100 ml of stock solution) will prevent its reduction with formation of black deposits. 5. Black osmic oxide crystals may be dissolved in cold water. 6. To prevent contact of tissues with black precipitate formed in the bottom of the jar, the tissues may be wrapped in cotton gauze and suspended in the fluid by means of a thread. 7. Osmic acid-fixed tissues must be washed in running water for at least 24 hours to prevent formation of artefacts. Flemming's Solution is the most common chrome-osmium acetic acid fixative used, recommended for nuclear preparation of such sections. FORMULA: Aqueous chromic acid 15 ml. 1% Aqueous osmium tetroxide 4 ml. 2% Glacial acetic acid 1 ml. Fixation time: 24 - 48 bouts Advantages: 1. It is an excellent fixative for nuclear structures, e.g. chromosomes. 2. It permanently fixes fat. 3. Relatively less amount of solution is required for fixation (less than 10 times the volume of the tissues to be fixed). Disadvantages: 1. It is a poor penetrating agent; hence, is applicable only to small pieces of tissues. 2. The solution deteriorates rapidly and must be prepared immediately before use. 3. Chromic-osmic acid combinations depress the staining power of hematoxylin (especially Ehrlich's hematoxylin). 4. It has a tendency to form artifact pigments; these may be removed by washing the fixed tissue in running tap water for 24 hours before dehydration. 5 It is very expensive. Flemming's solution without acetic acid - is made up only of chromic and osmic acid, recommended for cytoplasmic structures particularly the mitochondria. The removal of acetic acid from the formula serves to improve the cytoplasmic detail of the cell. Fixation time: 24 - 48 hours Advantages and Disadvantages: same as Flemming's solution. CHROMATE FIXATIVES Chromic Acid - is used in 1-2% aqueous solution, usually as a constituent of a compound fixative. It precipitates all proteins and adequately preserves carbohydrates. It is a strong oxidizing agent; hence, a strong reducing agent (e.g. formaldehyde) must be added to chrome-containing fixatives before use in order to prevent counteracting effects and consequent decomposition of solution upon prolonged standing. Potassium Dichromate -is used in a 3% aqueous solution. I. It fixes but does not precipitate cytoplasmic structures. 2. It preserves lipids. 3. It preserves mitochondria (If used in pH 4.5-5.2, mitochondria is fixed. If the solution becomes acidified, cytoplasm, chromatin bodies and chromosomes are fixed but mitochondria are destroyed). Regaud’s (Muller's) Fluid FORMULA: Potassium dichromate 3% 80 ml Strong formaldehyde 40% 20 ml (To be added just before use). Fixation time: 12-48 hours Advantages: 1. It penetrates tissues well. 2. It hardens tissues better and more rapidly than Orth's fluid. 3. It is recommended for the demonstration of chromatin, mitochondria, mitotic figures, Golgi bodies, RBC and colloid-containing tissues. Disadvantages: 1. It deteriorates and darkens on standing due to acidity; hence, the solution must always be freshly prepared. 2. Penetration is slow, hence, tissues should not be thicker than 2-3 mm. 3. Chromate-fixed tissues tend to produce precipitates of sub-oxide, hence should be thoroughly washed in running water prior to dehydration. 4. Prolonged fixation blackens tissue pigments, such as melanin; this may be removed by washing the tissues in running tap water prior to dehydration. 5. Glycogen penetration is poor; it is therefore, generally contraindicated for carbohydrates. 6. Nuclear staining is poor. 7. It does not preserve fats. 8. It preserves hemosiderin less than buffered formalin. 9. Intensity of PAS reaction is reduced. Orth's Fluid FORMULA: Potassium dichromate 2.5% 100ml Sodium sulfate (optional) 1gm Strong formaldehyde 40% 10 ml (To be added just before use). Fixation time: 36-72 hours Advantages: 1. It is recommended for study of early degenerative processes and tissue necrosis. 2. It demonstrates rickettsiae and other bacteria. 3. It preserves myelin better than buffered formalin. Disadvantages: Same as in Regaud's fluid. PICRIC ACID FIXATIVES Picrates include fixatives with picric acid. Foremost among these is Bouin's solution that does almost as well as mercurials with nuclear detail but does not cause as much hardness. Picrates penetrate tissue well to react with histones and basic proteins, form crystalline picrates with amino acids and precipitate all proteins. It is a good fixative for connective tissue, preserves glycogen well, and extracts lipids to give superior results in immunostaining of biogenic and polypeptide hormones. However, it causes a loss of basophilia unless the specimen is thoroughly washed following fixation. Picric acid is an explosive hazard in dry form. As a solution, it stains everything it touches yellow, including skin. Like mercuric chloride, picric acid enhances subsequent staining, especially with anionic (“acid”) dyes. Picric Acid is normally used in strong saturated aqueous solution (approximately I %). Picric acid also dyes the tissues, but the yellow color may be removed by treatment with another acid dye or lithium carbonate. Tissues fixed with picric acid retain little affinity for basic dyes. It preserves glycogen well but causes considerable shrinkage of tissue. Washing with changes of 50% and 70% ethanol will remove most of the yellow color, but the excess picrate may be removed more easily from the sections when the paraffin wax has been removed. Picric acid is only sold in the aqueous state. When it dries out, it becomes explosive. Paraffin sections of formaldehyde fixed tissues are usually immersed for a few hours in a picric acid solution (Bouin’s fluid is commonly used) before Trichrome staining. Trichrome stains use combinations of anionic dyes with phosphotungstic or phosphomolybdic acid to impart contrasting colors to cytoplasm, collagen fibers and other components of tissues. Bouin's Solution The complementary effects of the three ingredients of Bouin’s solution work well together to maintain morphology. Specimens are usually fixed in Bouin’s solution for 24 hours. Prolonged storage in this acidic mixture causes hydrolysis and loss of stainable DNA and RNA. Thorough washing after fixation is necessary. FORMULA: Picric acid saturated aqueous soln. (2.1%) 75 ml 40% formaldehyde 25 ml Acetic acid glacial 5 ml Fixation time: 4 – 18 hours Store at room temperature Practical Applications: Bouin's Solution is recommended for fixation of embryos and pituitary biopsies. It gives very good results with tissue that is subsequently stained with trichrome. It preserves glycogen well but usually lyses erythrocytes. It is sometimes recommended for gastro-intestinal tract biopsies, animal embryos and endocrine gland tissue. It stains tissue bright yellow due to picric acid. Excess picric should be washed from tissues prior to staining with 70% ethanol. Because of its acidic nature, it will slowly remove small calcium deposits and iron deposits. Advantages: 1. It is an excellent fixative for glycogen demonstration. 2. It penetrates tissues well and fixes small tissues rapidly. 3. The yellow stain taken in by tissues prevents small fragments from being overlooked. 4. It allows brilliant staining with the trichrome method. 5. It is suitable for Aniline stains (Mallory's, Heidenhain's or Masson's methods). 6. It precipitates all proteins. 7. It is stable. Disadvantages: 1. It causes RBC hemolysis and reduces the amount of demonstrable ferric iron in tissue. 2. It is not suitable for frozen sections because it causes frozen sections to crumble when cut. 3. Prolonged fixation makes tissues hard, brittle and difficult to section. Tissues should not be allowed to remain in the fluid for more than 12-24 hours (depending on size). 4. Picrates form protein precipitates that are soluble in water; hence, tissues must be first rendered insoluble by direct immersion in 70% ethyl alcohol. 5. Picric acid fixed tissues must never be washed in water before dehydration. 6. Picric acid will produce excessive staining of tissues; to remove the yellow color, tissues may be placed in 70% ethyl alcohol followed by 5% sodium thiosulfate and then washed in running water. 7. Picric acid is highly explosive when dry, and therefore must be kept moist with distilled water or saturated alcohol at 0.5 to 1% concentration during storage. 8. It alters and dissolves lipids. 9. It interferes with Azure eosin method of staining; hence, tissues should be thoroughly washed with alcohol. Hollande’s Solution FORMULA: Copper acetate: 25 gm Picric acid: 40 gm 40% formaldehyde: 100 ml Acetic acid: 15 ml Distilled water: 1000 ml Dissolve chemicals in distilled water without heat. Fixation time: 4 – 18 hours Practical Applications: It is recommended for gastro-intestinal tract specimens and fixation of endocrine tissues. It produces less lysis than Bouin’s Solution. It has some decalcifying properties. The fixative must be washed from tissues if they are to be put into phosphate buffered formalin on the processing machine because an insoluble phosphate precipitate will form. Gendre’s solution FORMULA: 95% Ethanol saturated with picric acid 800 ml 40% formaldehyde 150 ml Acetic acid glacial 50 ml Fixation time: 4 - 18 hours Practical Application: This is an alcoholic Bouin’s solution that appears to improve upon ageing. It is highly recommended for the preservation of glycogen and other carbohydrates. After fixation the tissue is placed into 70% ethanol. Residual yellow color should be washed out before staining. Advantages: 1. It produces minimal distortion of micro-anatomical structures and can be used for general and special stains. (The shrinking effect of picric acid is balanced by the swelling effect of glacial acetic acid.) 2. It is an excellent fixative for preserving soft and delicate structures (e.g. endometrial curettings). 3. It penetrates rapidly and evenly, and causes little shrinkage. 4. Yellow stain is useful when handling fragmentary biopsies. 5. It permits brilliant staining of tissues. 6. It is the preferred fixative for tissues to be stained by Masson's trichrome for collagen, elastic or connective tissue. (If tissue is fixed in formalin, a pre-treatment in Bouin’s solution (as mordant prior to trichrome stain) is recommended. 7. It preserves glycogen. 8. It does not need "washing out". Disadvantages: 1. It penetrates large tissues poorly; hence, its use is limited to small fragments of tissue. 2. Picrates are soluble in water; hence, tissues should not be washed in running water but rather transferred directly from fixative to 70% alcohol. 3. It is not suitable for fixing kidney structures, lipid and mucus. 4. It destroys cytoplasmic structures, e.g. mitochondria. 5. It produces RBC hemolysis and removes demonstrable ferric iron from blood pigments. 6. It reduces or abolishes Feulgen reaction due to hydrolysis of nucleoproteins. Brasil's Alcoholic Picroformol Fixative FORMULA Formaldehyde 37% 2040 ml. Picric acid 80 gm. Ethanol or isopropyl alcohol 6000 ml. Trichloroacetic acid 65 gm. Overnight tissue fixation by automatic processing technique may utilize 3-4 changes of Brasil's fixative at 1/2 to 2 hours each, succeeded directly by absolute alcohol. Advantages: 1. It is better and less "messy" than Bouin's solution. 2. It is an excellent fixative for glycogen. GLACIAL ACETIC ACID Acetic acid is a colorless liquid that when undiluted is also called “Glacial” Acetic Acid because it is a water-free (anhydrous) acetic acid that freezes and solidifies at about 16°C. Acetic acid does not have much effect on proteins, other than to enable swelling by the absorption of water. Its major effect is to precipitate DNA, which is split off from nucleoprotein. For this reason, acetic acid is valuable for the preservation of nuclei, and is often added to fixatives specifically to do that. Acetic acid is not used alone for fixation but is incorporated into other fixatives to form a compound solution, most commonly at a concentration of approximately 5%. Advantages: 1. It fixes and precipitates nucleoproteins. 2. It precipitates chromosomes and chromatin materials; hence, is very useful in the study of nuclear components of the cell. In fact, it is an essential constituent of most compound nuclear fixatives. 3. It causes tissues (especially those containing collagen) to swell. This property is used in certain compound fixatives to counteract the shrinkage produced by other components (e.g. mercury). Disadvantages: 1. When combined with Potassium Dichromate, the lipid-fixing property of the latter is destroyed (e.g. Zenker's fluid). 2. It is contraindicated for cytoplasmic fixation since it destroys mitochondria and Golgi elements of cells. 3. Concentrated acetic acid is corrosive to skin and must, therefore, be handled with appropriate care, since it can cause skin burns, permanent eye damage, and irritation to the mucous membranes. These burns or blisters may not appear until hours after exposure. 4. Latex gloves offer no protection, so especially resistant gloves, such as those made of nitrile rubber, are worn when handling the compound. LEAD FIXATIVES Lead fixatives are used in 4% aqueous solution of basic lead acetate. Lead oxaloacetate, a primary reaction product precipitate for the visualization of the activity of glutamic oxaloacetic transaminase in tissue sections, is stable at a slightly alkaline pH. At concentrations which are used for tissue fixation, a slight inhibitory effect on glutamic oxaloacetic transaminase activity is produced by acetone while a glutaraldehyde-formaldehyde mixture results in marked reduction of activity. Advantages: 1. It is recommended for acid mucopolysaccharides. 2. It fixes connective tissue mucin. Disadvantage: It takes up C02 to form insoluble lead carbonate especially on prolonged standing. This may be removed by filtration or by adding acetic acid drop by drop to lower the pH and dissolve the residue. TRICHLOROACETIC ACID Trichloroacetic Acid (TCA) is a reagent that is used for the precipitation of proteins and nucleic acids. It is also used as a decalcifier and fixative in microscopy. Addition of TCA to a final concentration of 10% (w/v) will precipitate most proteins from solution. The excess TCA can be removed from protein pellets by washes with buffer. For the precipitation of nucleic acids, a 5% solution of ice cold TCA has been used. It is sometimes incorporated into compound fixatives. Advantages: 1. It precipitates proteins. 2. Its marked swelling effect on tissues serves to counteract shrinkage produced by other fixatives. 3. It may be used as a weak decalcifying agent. 4. Its softening effect on dense fibrous tissues facilitates preparation of such sections. Disadvantage: It is a poor penetrating agent, hence, is suitable only for small pieces of tissues or bones. ACETONE Acetone is not recommended as morphological fixative for tissue blocks, mainly because of its shrinkage and poor preservation effects. Its use is reserved for the fixation of cryostat sections or for tissues in which enzymes have to be preserved. Acetone is almost always used alone and without dilution; it fixes by dehydration and precipitation. It is used to fix specimens at cold temperatures (0 to 4°C). Fixation time may vary from several minutes (for cell smears, cryostat sections) to several hours (1-24 hours for small tissue blocks). Advantages: 1. It is recommended for the study of water diffusible enzymes especially phosphatases and lipases. 2. It is used in fixing brain tissues for diagnosis of rabies. 3. It is used as a solvent for certain metallic salts to be used in freeze substitution techniques for tissue blocks. Disadvantages: 1. It produces inevitable shrinkage and distortion. 2. It dissolves fat. 3. It preserves glycogen poorly. 4. It evaporates rapidly. MICHEL’S SOLUTION Michel’s Solution provides a stable medium for transport of fresh unfixed tissues, such as renal, skin and oral mucosa biopsies, which will undergo subsequent frozen section and immunofluorescence studies. Michel’s Transport Medium is not suitable for transporting cells for flow cytometry or for tissues used for fluorescent in-situ hybridization (FISH). It is not a fixative, and is not suitable for any other use (particularly, for transporting living cells for flow cytometry). It should be kept refrigerated (not frozen) until use. Specimens may be kept in it at room temperature for 5 days while in transport until they can be delivered to the reference laboratory. This simple salt solution maintains pH, but does not kill most pathogens. Specimens received in transport medium should be washed in three changes of washing solution (10 minutes for each wash). It is not suitable for FISH studies. Procedure: 1. Bring aliquot of Michel Transport Medium or a pre-filled Michel Transport Medium Vial to room temperature prior to use. Michel Transport Medium is routinely stored at 4°C. During refrigerated storage some precipitation may develop on the container bottom. Precipitation should re-dissolve by allowing the solution to reach room temperature prior to use. 2. Place fresh tissue in an adequate amount of Michel Transport Medium, insuring that the specimen will be totally submerged in fluid during transport. Tissue that has been previously frozen will not provide optimal testing results and should not be used with Michel Transport Medium. 3. Store and/or transport tissue in Michel Transport Medium up to a maximum of five days. Care should be taken to maintain cool to ambient temperatures of 4°C to 22°C during transport. Tissues transported in Michel Transport Medium at room temperature for 5 days prior to fixation and routine processing should provide satisfactory histological results although morphology detail will not be equal to that of expediently fixed and processed tissue. 4. Upon receipt, wash the tissue held in Michel Transport Medium in three changes of Michel Wash Solution for 10 minutes each change. 5. Freeze tissue per laboratory protocol. 6. Tissue placed in Michel Transport Medium may be subsequently processed for light or electron microscopy. Wash tissue for 2-3 minutes in tap water and place in appropriate fixative prior to processing. REFERENCES Atwood K, Farmilo AJ, Stead RH, Boenisch T. (2003) Fixation & tissue processing. From: Handbook for Immunochemical Staining Methods. 3rd ed. Carpinteria, CA: DAKO; 18–22, 44–46. Bancroft JD, Gamble M. (2008) Theory and practice of histological techniques. Churchill Livingstone Elsevier, Philadelphia, PA. Brown RW. (2009) Histologic preparations: common problems and their solutions. Northfield, IL: College of American Carson, FL, Hladik C. (2009) Histotechnology: A Self Instructional Text. 3rd ed. Chicago, IL: ASCP Press. Dapson RW. (1993) Fixation for the 1990's: a review of needs and accomplishments. Biotech Histochem 68(2):75-82. Dapson RW. (2007) Glyoxal fixation: how it works and why it only occasionally needs antigen retrieval. Biotechnic & Histochemistry 82(3): 161-166. Drury RAB, Wallington EA. (1980) Carleton's histological technique. 5th ed. New York: Churchill Livingstone. Eltoum I, Fredenburgh J, Myers RB, Grizzle WE. (2001) Introduction to the theory and practice of fixation of tissues. J Histotechnol 24:173 -190. Eltoum I, Fredenburgh J, Grizzle WE. (2001) Advanced concepts in fixation: 1. Effects of fixation on immunohistochemistry, reversibility of fixation and recovery of proteins, nucleic acids, and other molecules from fixed and processed tissues. 2. Developmental methods of fixation. J Histotechnol 24:201-210. Fox CH, Johnson FB, Whiting J, Roller RP. (1985) Formaldehyde fixation. J Histochem Cytochem 33: 845-853, 1985. Grizzle WE. (2009) Special symposium: fixation and tissue processing models. Biotech Histochem 84(5):185-193. Henwood A (2010). What is the Best Procedure to Remove Formalin Pigment from FormaldehydeAcetic Acid-Alcohol Fixed Tissues? J Histotechnol 33(3):109-111. Hopwood, D. (1969) Fixatives and fixation: a review. Histochemical Journal 1: 323-360. Hopwood D. (1996) Fixation and fixatives. In Bancroft J and Stevens A. eds. Theory and practice of histological techniques. New York: Churchill Livingstone. Hwang, BJ. Chu, G. (1996) Trichloroacetic Acid Precipitation by Ultracentrifugation to Concentrate Dilute Protein in Viscous Solution. Biotechniques, 20(6), 982-984. Karnovsky, M.J. (1965): A Formaldehyde-Glutaraldehyde Fixative of High Osmolarity for use Electron Microscopy. 1. Cell Biol. 27,137 A. Kiernan, JA. (2000) Formaldehyde, formalin, paraformaldehyde and glutaraldehyde: What they are and what they do. Microscopy Today 00-1 pp. 8-12 Kiernan, JA. (2009) Histological and Histochemical Methods. Theory and Practice. 4th ed. chapters 24, pp 12-73. Bloxham, UK: Scion. Leong AS-Y. (1994) Fixation and fixatives. In Woods AE and Ellis RC eds. Laboratory histopathology. New York: Churchill Livingstone 4.1-1 - 4.1-26. Lillie RD, Fullmer HM. (1976) Histopathologic Technic and Practical Histochemistry. 4th ed., New York: McGraw-Hill. p. 54–57. Michel B, Milner Y, David K. (1972) Preservation of tissue-fixed immunoglobulins in skin biopsies of patients with lupus erythematosus and bullous diseases. A preliminary report. J. Invest. Dermatol. 59: 449-452 Oliver C, Jamur MC. (2010) Fixation and embedding. Methods Mol Biol 588:353-362. Pearse AG. (1980) Histochemistry: Theoretical and Applied. 4th ed. Vol. 1. Edinburgh: ChurchillLivingstone. Porter KR, Kallman F. (1953) The properties and effects of osmium tetroxide as a tissue fixative with special reference to its use for electron microscopy. Experimental Cell Research. 4(1): 127-141. Prento P, Lyon H. (1997) Commercial formalin substitutes for histopathology. Biotech Histochem 72(5):273-282. Puchtler H, Waldrop FS, Meloan SN, Terry MS, Connor HM. (1970) Methacarn (methanol-carnoy) fixation: practical and theoretical considerations. Histochemie 21: 97-116. Sheehan DC, Hrapchak BB. (1980) Theory and Practice of Histotechnology. 2nd ed. St Louis, MO: Mosby. Suresh B. (2003) "Acetic Acid". Chemicals Economic Handbook. SRI International. Suvarna KS, Layton C, Bancroft JD. (2012) Bancroft's Theory and Practice of Histological Techniques. Churchill Livingstone. Thavarajah, R., Mudimbaimannar, V. et al. (2012) Chemical and physical basics of routine formaldehyde fixation. J Oral Maxillofac Pathol. 16(3): 400–405 Waldrop FS, Puchtler, Terry MS. (1969) Removal of acid hematin-type pigments from sections; efficacy of alcoholic picric acid solution. Stain Technol 44(6):279-281. CHAPTER 8 DECALCIFICATION Decalcification is the removal of calcium ions from a bone or calcified tissue through a histological process that makes them flexible and easier to cut. Decalcification adjusts the hard substance of bones to the softness of paraffin embedding medium. Bones are the main object of decalcification in a surgical pathology laboratory, but other specimens, such as teeth, calcified tumors and calcified heart valves also require this procedure. Decalcification enables the histotechnologist to cut soft sections of the bone using the microtome, so that they can be processed like any other soft tissue of the body. Fine detail radiographs are often used to assist in the selection of appropriate bone specimens for processing. If the calcified areas in tissue specimens are substantial, it may be impossible to obtain decent sections without first decalcifying the entire specimen. One alternative is to apply “surface decalcification” to a paraffin block, allowing sections to be obtained where the presence of calcium was not anticipated when the specimen was processed. Decalcification is a lengthy procedure, as bone pieces have to be left in the decalcifying agent for several days or even weeks, depending on the size of the tissue. Many of the grossing and cutting techniques for bone require the use of a high-speed saw and/or long periods in a decalcifying solution, prior to reducing the specimen to a size that can be easily processed, embedded and sectioned. The poor quality of thin sections obtained from these methods often contribute to the already difficult task of evaluating the pathology and making a correct diagnosis. A low speed saw may be sufficient to routinely and rapidly reduce undecalcified surgical specimens of hard tissue, to a thickness of 2–3 mm, without compromising the integrity of the tissue. In choosing a technique and processing method, consideration must be given to the type of investigation being carried out. For example, if a metabolic bone disease is being investigated and it is necessary to differentiate mineralized bone from osteoid, or if morphometric measurements are required, it may be necessary to retain and demonstrate the mineral content by producing sections of “un-decalcified” bone. As mineralized bone is such a hard material, there is a limited range of techniques available to produce sections from it. After fixation, it can be directly sawn into thin wafers and then ground using abrasive surfaces to produce thin “ground” sections. The principle of decalcification is fairly simple. Strong mineral acids, such as 10% hydrogen chloride (HCl), or weak organic acids, such as 5-10% formic acid (HCOOH), form soluble calcium salts in an ion exchange that moves calcium into the decalcifying solution. The same final effect makes 14% ethylene diamino tetracetic acid (EDTA) an ideal chelating agent that sequesters metallic ions, including calcium, in aqueous solutions. It is also possible to prepare bone specimens by infiltrating them with acrylic or epoxy resins which, when polymerized, have a hardness equivalent to that of mineralized bone and hence do not require decalcification at all. Make sure that the tissue has been adequately fixed and rinsed well to prevent any undesired reaction with the decalcifying agent. Buffered formalin is a satisfactory fixative for bone but where the preservation of bone marrow is important, some laboratories use alternatives such as zinc formalin mixtures, B5, formol-acetic alcohol (Davidson’s fixative), or Bouin’s solution. In order to protect the cellular and fibrous elements of bone from damage caused by the acids used as decalcifying agents, it is particularly important to thoroughly fix these specimens prior to decalcification. Decalcification should be done after fixation and before impregnation, to ensure and facilitate the normal cutting of sections and to prevent obscuring the microanatomic detail of such sections by bone dust and other cellular debris. Inadequate decalcification may result in poor cutting of hard tissues and damage to the knife edge during sectioning. There are certain specimens e.g., bones, teeth and other calcified tissues like tuberculous lungs, which contain some amount of calcium that is apt to interfere with the accurate evaluation and examination of histologic sections. Hence, one must see to it that all such extraneous materials have been removed before proceeding to the next step in the tissue processing. Poorly-fixed specimens become macerated during decalcification and stain poorly afterwards. This is very noticeable in areas containing bone marrow. It is therefore common practice for laboratories to extend fixation times for bone specimens before commencing decalcification. It is important to provide ready access for the fixative to penetrate the bone, so skin and soft tissue should be removed from large specimens if practicable. Bone specimens should be sawn into thin slices as soon as possible to enhance fixation and an adequate volume of fixative provided. High-quality fine tooth saws should be used to prepare bone slices. Coarse saws can cause considerable mechanical damage and force bone fragments into the soft tissues present in the specimen. Cartilage does not require any softening, except if some calcified areas are present. It is a waste of time to put toenails in decalcification solution, because they are composed of insoluble keratin filaments. After fixation, depending on the amount of adjusted soft tissue, the toenail should be rinsed off with soapy water once it becomes pliable. There are three main types of decalcifying agents: Those based on strong mineral acids Those based on weaker organic acids Those composed of chelating agents. The acids make up a solution of calcium ions while the chelating agents take up the calcium ions. Dilute mineral acids (hydrochloric or nitric) or formic acid can be used effectively if the end point of decalcification is monitored carefully. Nuclear and cytoplasmic detail are compromised if specimens are exposed for too long to acidic decalcifying agents, which can extract RNA and remove the purine and pyrimidine bases from DNA. It is also imperative to wash the acid out of the tissue. ACID DECALCIFYING AGENTS Acid decalcifying agents are the most widely used agents for routine decalcification of large amounts of bony tissues because they are stable, readily available, and relatively inexpensive as compared to other decalcifying agents. As soon as fixation is complete, the selected pieces of tissues are usually placed in a gauze bag and suspended in liberal amounts of decalcifying solution by means of a thread to ensure complete decalcification and to protect the tissue from any precipitate that might be settled at the bottom of the container. Due to the corrosive action of the acid, it is recommended that the thread be dipped in melted paraffin wax and that use of metal cap containers be avoided. Strong Mineral Acids Strong acids such as hydrochloric or nitric acid at concentrations up to 10% are the most rapid in action but if used longer than necessary will rapidly cause a loss of nuclear staining and can macerate tissues. It is important that an appropriate end-point test is used to minimize exposure of the specimens to these agents. Generally proprietary decalcifiers that are claimed to be rapid in action are based on strong acids, most commonly hydrochloric acid, and should be used conservatively with attention to the provided instructions if good results are to be obtained. Rapid decalcifying agents are more likely to adversely affect any subsequent staining. This is especially noticeable in cell nuclei due to failure of nuclear chromatin to take up hematoxylin and other basic dyes as readily as soft tissues that have not been exposed to acid solutions or decalcifiers. Staining by acid dyes will be less affected, although eosin can produce a deep, brick red stain without differential shading. These effects of decalcifying agents on H&E staining can be reduced by post-decalcification and removal, and by appropriately adjusting the staining procedure. I. NITRIC ACID Nitric acid is the most common and the fastest decalcifying agent used so far, utilized both as a simple solution or combined with other reagents. This may be used as simple aqueous solutions with recommended concentrations of 510%. It is a very rapid decalcifying agent, producing minimal distortion and is, therefore, recommended for routine purposes. It has, however, the disadvantage of inhibiting nuclear stains and destroying tissues, especially in concentrated solutions. The endpoint of decalcification must be carefully watched for, to prevent progressive tissue damage and impaired staining. This may be prevented by combining nitric acid with formaldehyde or alcohol. Aqueous Nitric Acid Solution 10% FORMULA: Concentrated nitric Acid 10 ml. Distilled water added up to 100 ml. DECALCIFICATION TIME: 12-24 hours Advantages: 1. It is rapid in action. 2. It produces minimum distortion of tissues. 3. It produces good nuclear staining (although less than in slower acting agents). 4. The acid may be easily removed by 70% alcohol. 5. It is recommended for urgent biopsy, and for needle and small biopsy specimens to permit rapid diagnosis within 24 hours or less. 6. It can be used for large or heavily mineralized cortical bone specimen if decalcification progress is carefully monitored by a decalcification endpoint test. Disadvantages: 1 Prolonged decalcification may lead to tissue distortion. 2. It can seriously damage tissue stainability. 3. It imparts a yellow color with nitrous acid, thereby impairing the staining reaction of the tissue. 4. Old nitric acid solution is particularly damaging and should be replaced with fresh stock solution. 5. Strong acids tend to be more damaging to tissue antigens for immunohistochemical staining, and enzymes may be totally lost. Formol-Nitric Acid FORMULA: Concentrated nitric acid 10 ml. Strong formaldehyde, 40% 5 ml. Distilled water 85 ml. DECALCIFICATION TIME: 1-3 days Advantages: 1. It is rapid-acting; hence, is recommended for urgent biopsies. 2. Nuclear staining is relatively good. 3. It produces less tissue destruction than 10% aqueous nitric acid. Disadvantages: 1. The yellow color imparted by nitrous acid formation will impair staining reaction of the cell. This may be prevented by neutralizing the tissue with 5% sodium sulfate and washing in running tap water for at least 12 hours. Addition of 0.1% urea to pure concentrated nitric acid will also make discoloration disappear without considerably affecting the efficiency of the decalcifying solution. 2. The solution should be used inside a fume hood. Perenyi’s Fluid FORMULA: Nitric acid 10% 40 ml. Chromic acid 0.5% 30 ml. Absolute ethyl alcohol 30 ml. Mix shortly before use. Chromic acid must be collected for proper disposal. DECALCIFICATION TIME: 2 - 7 days Advantages: 1. It is recommended for routine purposes. 2. It decalcifies and softens tissues at the same time. 3. Nuclear and cytoplasmic staining is good. 4. Maceration is avoided due to the presence of chromic acid and alcohol. Disadvantages: 1. It is a slow decalcifying agent for dense bones; hence, is not recommended for urgent diagnosis. 2. Complete decalcification cannot be determined by chemical test because a precipitate is formed upon the addition of ammonia to Perenyi's fluid even in the absence of calcium ion. This may be dissolved by adding glacial acetic acid drop by drop. About 0.5 ml. of saturated aqueous ammonium oxalate is then added to the solution. Reappearance of a white precipitate within 30 minutes will reaffirm the presence of calcium in the agent, signifying that decalcification is still incomplete. Phloroglucin-Nitric Acid FORMULA: Concentrated nitric acid 10 ml. Phloroglucin 1 gm. Nitric acid 10% 100 ml. (To be added after disappearance of dense white fumes formed by combining the first two ingredients.) DECALCIFICATION TIME: 12-24 hours Advantage: It is the most rapid decalcifying agent so far, recommended for urgent cases. Disadvantages: 1. Nuclear staining is poor. 2. Prolonged decalcification produces extreme tissue distortion. 3. Yellow color must be neutralized with 5% sodium sulfate and thoroughly washed with running tap water for at least 24 hours. 4. Complete decalcification cannot be determined by chemical means. When decalcification is complete, the acid must be removed by three changes of 70% to 90% ethanol, since washing in watery solutions will lead to excessive swelling and deterioration of tissue. When the sections are cut, the slides are brought to water and placed in 1% aqueous lithium carbonate for I hour, washed in later for 15 minutes, and then stained. II. HYDROCHLORIC ACID Hydrochloric acid (HCI) is inferior compared to nitric acid in its role as a decalcifying agent because of its slower action and greater distortion of tissue produced on the decalcified section. However, it produces good nuclear staining and if used in 1% solution with 70% alcohol, may be recommended for surface decalcification of the tissue blocks. Rapid proprietary solutions usually contain hydrochloric acid, whereas slow proprietary mixtures contain buffered formic acid or formalin/formic acid. Dilution of a proprietary HCl is not deleterious for effective decalcification or staining, and this is an option if a strong mixture is considered too concentrated. Von Ebner's Fluid FORMULA: Saturated aqueous solution of NaCl 50 ml. 36% concentrated hydrochloric acid 8 ml. Distilled water 50 ml. Advantages: 1. It permits relatively good cytologic staining. 2. It is a moderately rapid decalcifying agent. 3. It does not require washing out before dehydration. 4. It is recommended for teeth and small pieces of bone. Disadvantage: The extent of decalcification cannot be measured by a chemical test. WEAK ACIDS such as formic acid are popular and are widely used for decalcification. Organic acids such as acetic and formic acid are better suited to bone marrow, since they are not as harsh. However, they act more slowly on dense cortical bone. Other acids such as trichloracetic acid (TCA) have also been used. Picric acid and acetic acid are not used alone as decalcifying agents, but are found as components of Carnoy's and Bouin's fixatives. These fixatives may act as incidental, albeit, weak decalcifiers, and can be used in urgent cases when there is only minimal calcification. III. FORMIC ACID Formic acid is a moderate-acting decalcifying agent which produces better nuclear staining with less tissue distortion, and is safer to handle than nitric acid or hydrochloric acid. It is recommended for routine decalcification of postmortem research tissues, although not suitable for urgent examinations. Formic acid can be used as a simple 10% aqueous solution or combined with formalin or with a buffer. It is slower than the strong acid agents, but it is much gentler in action and less likely to interfere with nuclear staining. Formic acid in a 10% concentration is the best all-around decalcifier. Some commercial solutions are available that combine formic acid with formalin to fix and decalcify tissues at the same time. Formic acid is the only weak acid used extensively as a primary decalcifying agent. Addition of citrate probably accelerates decalcification by chelating the calcium as it is liberated from the bone. FORMULA: Formic acid (Sp. grav. 1.20) 10 ml. Normal saline 10% 90 ml. DECALCIFICATION TIME: 2-7 days Advantages: 1. It may be used both as a fixative and decalcifying agent. 2. It permits excellent nuclear and cytoplasmic staining. 3. It is recommended for small pieces of bones and teeth. 4. It is suitable for most routine surgical specimens, particularly when immunohistochemical staining is needed. Disadvantages: 1. It is relatively slow; hence, is not suitable for urgent specimens. Decalcification may be hastened by increasing the proportion of formic acid to 25 ml. However, such concentration may make the solution opaque, thereby interfering with the staining results. 2. It requires neutralization with 5% sodium sulfate, and washing out to remove the acid from the tissue. Formic Acid-Sodium Citrate Solution FORMULA: Aqueous sodium citrate 20% 50 ml. Formic acid 45% 50 ml. DECALCIFICATlON TIME: 3 -14 days Advantages: 1. It permits better nuclear staining than nitric acid method. 2. It is recommended for autopsy materials, bone marrow, cartilage and tissues studied for research purposes. Disadvantages: 1. It is relatively slow; hence, is not recommended for routine purposes and for dense tissues. 2. It requires neutralization with 5% sodium sulfate. IV. TRICHLOROACETIC ACID FORMULA: Trichloroacetic acid 5 gm. Formal saline 10% 95 ml. DECALCIFICATION TIME: 4- 8 days Advantages: 1. It permits good nuclear staining. 2. It does not require washing out; the excess acid may be removed by several changes of 90% alcohol, thus improving tissue dehydration. Disadvantages: 1. It is a weak decalcifying agent, not used for dense tissues, and is suitable only for small spicules of bone. 2. It is very slow-acting; hence, is not recommended for urgent examinations. SULFUROUS ACID -is a very weak decalcifying solution suitable only for minute pieces of bone. V. CHROMIC ACID (FLEMMING'S FLUID) FORMULA: Chromic acid % 15 ml. Osmium tetroxide 4 ml. 2% Glacial acetic acid 1 ml. Advantages: 1. It may be used both as a fixative and decalcifying agent. 2. It may be used for decalcifying minute bone spicules. Disadvantages: 1. Nuclear staining with hematoxylin is inhibited. 2. It tends to undergo reduction and forms precipitates at the bottom of the container thus requiring frequent changes of solution. 3. Insoluble pigments are formed when decalcified tissue is dehydrated with alcohol; hence, tissues must be washed out prior to dehydration. 4. Degree of decalcification cannot be measured by the routine chemical test. Caution: Chromic acid is an environmental toxin. 1. Chromic acid is highly corrosive to skin and mucous membranes. 2. It is carcinogenic. 3. Suitable protective material is not readily available or practical for laboratory use. 4. Drain disposal is not a legitimate option for any solution containing chromium, including subsequent processing of fluids following fixation or rinses following staining procedures involving chromium. VI. CITRIC ACID-CITRATE BUFFER SOLUTION (pH 4.5) FORMULA: Citric acid (monohydrate) aqueous solution 7% 5.0 ml. Ammonium citrate (anhydrous) aqueous solution 7.4% 95.0 ml. Zinc sulfate aqueous solution. 1% 0.2 ml. Chloroform (as preservative) - a few drops DECALCIFICATION TIME: 6 days Advantages: 1 It permits excellent nuclear and cytoplasmic staining. 2. It does not produce cell or tissue distortion. Disadvantage: Its action is too slow for routine purposes. DECALCIFYING AGENTS – CHELATING AGENTS Chelating agents are substances which combine with calcium ions and other salts (e.g. iron and magnesium deposits) to form weakly dissociated complexes and facilitate removal of calcium salt. The most common chelating agent in the market is ethylene diamine tetra acetic acid (EDTA) salt, with the commercial name of Versene, recommended only for detailed microscopic studies. Although EDTA is traditionally referred as "acid", it does not act like inorganic or organic acids but it binds metallic ions, notably calcium and magnesium. EDTA combines with calcium, forming an insoluble nonionized complex (which is why it is also used as an anticoagulant and water softener). It works by capturing the calcium ions from the surface of the apatite crystal, slowly reducing its size. If preservation of nuclear DNA is important, or if histochemical methods for nucleic acids or enzyme activities are intended, a chelating agent is preferred to an acid. Usually the disodium salt of EDTA is used, with the pH adjusted to a level between 7 and 8. Decalcification by EDTA takes much longer than decalcification by acids – weeks rather than days. Acids have some effects on the stainability of the tissue. Despite the physical methods having definite advantages, especially in the speed of processing, the general surgical pathology practice does not use them, for many reasons. They require closer monitoring, cleaning and maintenance of the equipment involved. Because the process is very slow but very gentle (weeks may be required depending on the size of the specimen), this reagent is not suitable for urgent specimens. It is more appropriate for research applications where very high quality morphology is required or particular molecular elements must be preserved for techniques such as immunohistochemistry (IHC), Fluorescent In Situ Hybridization (FISH) or Polymerase Chain Reaction (PCR). It is used at a concentration of approximately 14% as a neutralized solution. The rate at which EDTA will decalcify is pH dependent. It is generally used at pH7.0. It works more rapidly at pH10 but some tissue elements can be damaged at alkaline pH. EDTA does not work in formic acid with pH 3 as a decalcifier. Neutral EDTA, though being a slow decalcifying agent, gives excellent results for soft-tissue integrity, and best quality of both soft-tissue and hard-tissue staining. The optimal pH is 7-7.6, so it is necessary to maintain this narrow window. EDTA works too slowly under pH 5, owing to insolubility, but over pH 8, tissue maceration starts due to alkaline sensitive protein bonds. Loaded with undistributed calcium, the solution can precipitate at the bone surface, which requires more intensive agitation and more intensive post- decalcification rinsing. The tissue is usually placed in EDTA from 1-3 weeks for small specimens, but it may take 6-8 weeks or longer to totally decalcify dense cortical bone. The solution should be changed every 3 days, and in the final stage, every day, to facilitate decalcification. At present, the application of EDTA as a decalcifying agent in a routine setting is hampered by the long time required for incubation. However, new methods, such as decalcification in EDTA using a microwave oven, addition of ammonium hydroxide to the EDTA solution, electrolytic decalcification, or a one-step fixation–decalcification in formalin mercuric chloric acid solution, which also appears suitable for mRNA In Situ Hybridization, might reduce the time of decalcification considerably. Neutral EDTA EDTA disodium salt 250 gm Distilled water 1750 ml Bring to pH 7.0 by adding sodium hydroxide (about 25 gm will be needed). Neutral EDTA acts slowly but causes little tissue damage. Conventional stains are largely unaffected. Advantages: 1. It permits excellent staining results. 2. It produces minimal cell and tissue distortion. 3. It forms minimal histological artifacts, usually caused by production of CO2 bubbles. 4. Extent of decalcification can be measured by routine chemical test. 5. EDTA is an excellent bone decalcifier for enzyme or immuno- histochemical staining, and for electron microscopy. 6. Enzymes require specific pH conditions in order to maintain activity, and EDTA solutions can be adjusted to a specific pH for enzyme staining. Disadvantages: 1. It is very slow, and is therefore not recommended for urgent and routine purposes. 2. It causes slight tissue hardening. 3. EDTA inactivates alkaline phosphatase activity, which can be restored by addition of magnesium chloride. Other techniques for increasing the efficiency of decalcification Sonication with EDTA has been successfully used to accelerate decalcification of trephine specimens for subsequent molecular analysis. During the process, the temperature must be carefully controlled. Microwave treatment has been used with hydrochloric acid decalcifiers but the raised temperature may damage morphology and cause staining artefacts. Ion-exchange resins have been incorporated into some decalcification protocols. They are added to the container holding the decalcifier and take up the ionized calcium, thereby maintaining the effectiveness of the acid. If acid decalcifiers are used in adequate volumes and replaced regularly, the use of such resins is probably unnecessary. Electrolytic decalcification in which the bone is placed in acid decalcifier and attached to an electrode through which current is applied is a technique that has not found wide acceptance because of the potential to cause heat damage to the specimen. ION EXCHANGE RESIN Ion exchange resin (ammonium form of polystrene resin) hastens decalcification by removing calcium ions from formic acid-containing decalcifying solutions, thereby increasing solubility from the tissue. It is not recommended for fluids containing mineral acids such as nitric acid or hydrochloric acid. A layer of the ion exchange resin, about 1/2 inch thick is spread over the bottom of the container to be used and the specimen is placed on top of it. The decalcifying agent is then added, usually 20-30 times the volume of the tissue. The tissue may be allowed to stay in solution for 1-14 days. The degree of decalcification may then be measured by physical or X-ray method. The resin that has been previously used may later be reactivated by immersing it in N/10 HCl twice and washing it with distilled water three times. Advantages: 1. Cellular detail is well-preserved. 2. Daily washing of solutions is eliminated. 3. It permits excellent staining results. 4. Decalcification is hastened. 5. It produces minimal cell and tissue distortion. 6. It forms minimal histological artifacts, usually caused by production of CO2 bubbles. 7. Extent of decalcification can be measured by routine chemical test. Disadvantages: 1. The degree of decalcification cannot be measured by chemical means. 2. It is very slow, and is therefore not recommended for urgent and routine purposes. 3. It causes slight tissue hardening. ELECTROPHORESIS (ELECTRICAL IONIZATION) Electrophoresis is a process whereby positively charged calcium ions are attracted to a negative electrode and subsequently removed from the decalcifying solution . The time required for decalcification is thereby shortened due to the heat and electrolytic reaction produced in the process. The principle is similar to that of chelating agents, with the main difference that this process utilizes electricity and is dependent upon a supply of direct current to remove the calcium deposits. Solution Used for Electrolytic Decalcification Formic acid 88% 100 ml. Concentrated hydrochloric acid 80 ml. Distilled water 1000 ml. This method is satisfactory for small bone fragments, processing only a limited number of specimens at a time. Good cytologic and histologic details are, however, not always preserved in tissues that have been electrically decalcified. MICROWAVE OVEN DECALCIFICATION The microwave oven has been used quite often for tissue processing, but there are very few studies describing its use in decalcification of bone or teeth. Microwave oven decalcification is faster than routine decalcification irrespective of the decalcifying agents used. The tissue preservation and staining efficacy is good in microwave nitric acid decalcification compared to routine nitric acid decalcification. Both formic acid and EDTA show good tissue preservation and staining efficacy irrespective of the method used (manual vs microwave). Microwave decalcification is a novel technique compared to the manual method. In this method, hard tissues are placed in the decalcifying agent in a microwave oven for intermittent periods with regular changes of the solution till the end point is reached. Microwave irradiation has been shown to speed up the process of decalcification significantly–from days to hours. The use of a Microwave Histoprocessor does not adversely affect cell morphology. The quality of microwave-fixed tissues, at the respective optimal time points, is comparable with routinely fixed tissues. With the ability to have entirely fixed tissues 3 hours after autopsy, tissues can be harvested in the morning, placed on the processor in the afternoon, and embedded the following morning. The uniformity of the section’s thickness is always desirable, but it becomes a serious requirement with implementation of microwave- assisted processing. It is unreasonable to make a section too thin (less than 3 mm). Uniform 3-5 mm sections are optimal for decalcification with or without microwave- accelerated processing. There are many technical details pertaining to how to get a uniform representative bone section. Factors influencing the rate of decalcification The rate of decalcification may be influenced by several factors, and ways may be devised to speed up or slow down this process. The concentration and volume of decalcifying agent and temperature at which the reaction takes place are important considerations. Concentration. The concentration of active agent will affect the rate at which calcium is removed. In general, more concentrated acid solutions decalcify bone more rapidly, but are more harmful to the tissue. This is especially true of aqueous acid solutions, as various additives such as alcohol or buffers that protect the tissues may slow down the decalcification process. High concentrations and greater amount of fluid will increase the speed of the process. Rapid depletion of an acid or chelator by their reaction with calcium can be avoided by using large volumes of fluid compared with the volume of tissue, and by changing the solution several times during the decalcification process. The recommended ratio of fluid to tissue volume for decalcification is 20 to 1. Fluid access As with fixation, a fresh decalcifier should have ready access to all surfaces of the specimen. This will enhance diffusion and penetration into the specimen and will facilitate solution, ionization and removal of calcium. Decalcification may be hastened by suspending the tissue in decalcifying solution for greater fluid access. As soon as fixation is complete, the selected pieces of tissues are usually placed in a gauze bag and suspended in liberal amount of decalcifying solution by means of a thread to ensure complete decalcification and protect the tissue from any precipitate that may be settled at the bottom of the container. Due to the corrosive action of the acid, it is recommended that the thread be dipped in melted paraffin wax and that use of metal cap containers be avoided. Size and consistency Increase in size and consistency of tissues will require longer periods for complete decalcification. Dense bone tissues usually require up to 14 days or longer in order to complete the process. In such cases, the solution should be changed daily to ensure better penetration and to test for the degree of decalcification. Agitation. Gentle agitation may increase the rate of decalcification. Mechanical agitation and moving of the tissue in solution usually influences fluid exchange, accelerates the rate of diffusion and speeds up the decalcification process. Gentle fluid agitation is achieved by low-speed rotation, rocking, stirring or bubbling air into the solution. Sonication vigorously agitates both specimen and fluid, and may cause disruption of tissue, with formation of cellular debris on the floor of container. Temperature. Increased temperature will hasten decalcification, but it will also increase the damaging effects of acids on tissue. At 37°C, there will be impaired nuclear staining of Van Gieson's stain for collagen fibers. At 55°C, the tissue will undergo complete digestion within 24-48 hours. Microwave, sonication and electrolytic methods produce heat, and must be carefully monitored to prevent excessive temperatures that damage tissue. Conversely, lower temperature decreases reaction rates. The optimum temperature so far recommended is the room temperature range of 18°C -30°C. Determining the end-point of decalcification Prolonged decalcification of tissue is liable to prevent hydrolysis and lead to maceration and destruction of tissue components which are poorly stained. Overdecalcification, particularly with the strong acid decalcifiers, spoils the staining of basophilic elements such as cell nuclei and in certain circumstances can cause maceration of the softer tissue elements. On the other hand, when the tissue is allowed to stay in the decalcifying agent for a very short period of time, decalcification may be incomplete thereby interfering with the normal cutting of sections and staining of specimens. If high-quality results are to be obtained from decalcified tissue, it is important to determine the point at which all the calcium has been removed because, from this point on, tissue damage seems to occur at an increasing rate. There are several methods to check if the end point of decalcification has been reached: Physical tests require manipulation, bending, probing or trimming of the specimen to “feel” for remaining calcified areas. While this method may be successful in experienced hands it is generally considered to be unreliable. Mechanical damage can occur during bending or probing and small deposits of calcium can easily be missed. A method of determining the endpoint by carefully weighing the specimen after rinsing and blotting has also been described, and may be an effective method for large specimens. An alternate method of evaluating tissues mechanically is by pricking the tissue with a fine needle or a probe. This method is apt to produce needle tract artifacts and destroy important cellular details. Pricking, slicing, bending or squeezing tissue can disrupt soft tumor from the bone or cause false positive microfractures of fine trabeculae, leading to a potential misdiagnosis. Aside from this disadvantage, small calcified foci may not even be detected. A simple chemical test can be applied when some acid decalcifiers are used (particularly formic acid). The decalcifying fluid is usually changed every 24 -48 hours and the chemical test is performed on the discarded fluid. A piece of blue litmus paper is added to a test tube containing 5 ml. of the discarded decalcifying agent (the litmus paper will turn red due to the acidity of the fluid). Strong ammonia is then added drop by drop until the fluid is neutralized (this can be detected by the change in color of the litmus paper from red to blue, indicating alkalinity). The presence of cloudiness indicates that there is still calcium found in the solution. The tissue is then immersed in a new solution of decalcifying agent. If the solution remains clear after neutralization with concentrated ammonia, 0.5 ml. of saturated aqueous solution of ammonium oxalate is added and the solution is allowed to stand for 30 minutes. Cloudiness will signify incomplete calcium removal; hence, the need for further decalcification. If the solution remains clear after 30 minutes, decalcification is considered to be complete. This test is cumbersome and useless in the every- day practice of surgical pathology when many samples are placed in the decalcification solution simultaneously. It is definitely more objective than the bubble method which includes the observation of carbon- dioxide bubbles at the surface of the bone during acid decalcification. If chemical method of determination is to be done, the decalcifying agent should be prepared with distilled water, since false positive readings may be produced by the calcium ions present in tap water. It is unsuitable for solutions containing over 10% acid, although these could be diluted and result in a less sensitive test. The best method, particularly with large specimens such as femoral heads, is to X-ray the specimen. This is a very expensive although the most ideal, most sensitive and most reliable method of determining extent of decalcification due to its ability to detect even the smallest focus of calcium which appears opaque in an X-ray plate. A good-quality X-ray will clearly reveal tiny residual calcium deposits and allow further treatment if required. It is an excellent method for following the process of decalcification of large specimens such as femoral heads. It is, however, not recommended for mercuric chloride-fixed tissues due to the latter's characteristic radio-opacity which will interfere with the correct interpretation of the plate. Treatment following decalcification and prior to processing Various methods for neutralizing residual acid decalcifier before processing have been published, including extensive washing in tap water or the application of alkaline solutions. After decalcification is complete, the acid can be removed from tissues or neutralized chemically by immersing the decalcified bone in either saturated lithium carbonate solution or 5-10% aqueous sodium bicarbonate solution for several hours. Generally a short, effective wash in tap water should be sufficient as any remaining acid will be removed during processing. Adequate water rinsing can usually be accomplished in 30 minutes for small samples and 1-4 hours for larger specimens. Samples that need to be immediately processed, such as small needle biopsies, can be blotted or quickly rinsed with water to remove acid from the surface, before transferring the specimen to a dehydrating fluid. It is important to remove the bulk of the decalcifier to avoid contaminating the processing reagents and the processor with acid. Application of vacuum during wax infiltration should improve the quality of the finished blocks. Acid decalcified tissues for frozen sections must be thoroughly washed in water or stored in formol-saline containing 15% sucrose or phosphate-buffered saline (PBS) with 15-20% sucrose at 4°C before freezing. Tissues decalcified in EDTA solutions should not be placed directly into 70% alcohol, because this will cause residual EDTA to precipitate in the alcohol and within the tissue. Rinsing the decalcified tissue with water or storing overnight in formol-saline or phosphate buffered saline (PBS) will prevent the formation of crystalline precipitate. Surface decalcification This is a method of dealing with small unexpected deposits of calcium that may be encountered in paraffin blocks. When the paraffin-embedded block has been trimmed, the tissue surface may reveal small foci of calcification and may cause resistance or a "grating" sensation when sectioned with a microtome knife. If this is encountered, the block can be removed from the chuck and placed face down on a pad of cotton or gauze saturated with 10% hydrochloric acid for approximately one hour. This surface treatment will allow the decalcifier to penetrate a small distance into the block and dissolve the calcium. The block can then be thoroughly rinsed in water to remove residual acid, chilled and sectioned. Careful realignment of the block will be required because the decalcifier will penetrate a very small distance into the block allowing only a couple of sections to be taken. The staining properties of the tissue will be affected after this procedure, so that allowances in staining need to be made to achieve optimum results. TISSUE SOFTENERS Unduly hard tissues which are liable to damage the microtome knives may require tissue softeners, aside from decalcification. Perenyi's fluid may act both as a decalcifying agent and tissue softener. To soften unduly hard tissues, selected portions are left in the fluid for 12-24 hours and dehydrated in the usual manner; or the cut surface of the block may be submerged in the fluid for 1-2 hours before sectioning, to facilitate easier cutting of tissues. Washing out and immersion of fixed tissues in 4% aqueous phenol solution for 1-3 days may also cause considerable tissue softening and easier sectioning of blocks without producing marked deleterious effects and tissue distortion. Other substances which may be used as tissue softeners are Molliflex, 2% hydrochloric acid, or 1% hydrochloric acid in 70% alcohol. Tissues immersed in Molliflex may appear swollen and soapy. This does not, however, affect the normalizing and subsequent staining of tissue sections. REFERENCES Brain, E.B. (1966) The Preparation of Decalcified Sections. Springfield, IL: C.C. Thomas, 86. Callis G, Sterchi D. (1998) Decalcification of Bone: Literature Review and Practical Study of Various Decalcifying Agents, Methods, and Their Effects on Bone Histology. The Journal of Histotechnology 21:49-58. Callis, GM. (2002) Bone. In: Bancroft, J.D., Gamble, M. Theory and Practice of Histological Techniques. 5th Ed., Churchill Livingstone, London, 269. Carson FL. (2007) Histotechnology. 2nd ed. Chicago: ASCP Press. Clayden EC. (1971) Practical section cutting and staining. Edinburgh: Churchill Livingstone. Culling CF. (1974) Handbook of Histopathological and Histochemical Techniques. 3rd ed. Butterworth, London, 65. Dotti LB, Paparo GB, Clarke BE. (1951) The use of ion exchange resin in decalcification of bone. American Journal of Clinical Pathology, 21: 475. Karpagaselvi S, Jayalakshmi K, Archana P, Lokesh P, Srinivas J, Lakshmi K. (2012) Evaluation and comparison of decalcification agents on the human teeth. J Oral Maxillofac Pathol. 16(2): 222–227. Mawhinney, W.H., Richardson, E., Malcolm, A.J. (1984) Control of rapid nitric acid decalcification. Journal of Clinical Pathology, 37: 1409. Moore RJ. (1994) Bone. In Woods AE and Ellis RC eds. Laboratory histopathology. New York: Churchill Livingstone, 7.2-10. Page KM. (1996) Bone: In Bancroft JD and Stevens A, eds. Theory and Practice of Histological Techniques. New York: Churchill Livingstone. Prasad P, Donoghue M. (2013) A comparative study of various decalcification techniques. Indian J Dent Res 24:302-8 Reineke T, Jenni B, Abdou MT et al. (2006) Ultrasonic Decalcification Offers New Perspectives for Rapid FISH, DNA, and RT_PCR Analysis in Bone Marrow Trephines Am J Surgical Pathology 30. Rolls GO. (2011) Difficult Blocks and Reprocessing. Leica Microsystems. Sanderson, C, Radley K, Mayton L. (1995) Ethylenediamine tetracetic acid in ammonium hydroxide for reducing decalcification time. Biotechnics and Histochemistry, 70: 18. Sanderson C. (1997) Entering the realm of mineralized bone processing: A review of the literature and techniques. Journal of Histotechnology, 20(3): 259. Sangeetha R, Uma K, Chandavarkar V. (2013) Comparison of routine decalcification methods with microwave decalcification of bone and teeth. Oral Maxillofac Pathol. 17(3): 386–391. Schenk RK, Olah AJ, Herrmann W. (1984) Preparation of calcified tissues for light microscopy. In: Dickson, G. (ed.) Methods of Calcified Tissue Preparation. Elsevier, Amsterdam, 1. Skinner RA, Hickmon SG, Lumpkin CK, Aronson J, Nicholas RW. (1997) Decalcified Bone: Twenty Years of Successful Specimen Management. The Journal of Histotechnology 20: 267-277. Sobel AE, Hanok A. (1951) Rapid method for determining ultramicro quantities of calcium and magnesium. Archives of Pathology, 44: 92. Stevenson A., Lowe J, Bancroft JD. (1996) Bone. In: Bancroft, J.D. Stevens, A. (eds.) Theory and Practice of Histological Techniques. 2nd Ed. Churchill Livingstone, London, 320. Vardaxis NJ. (1997) Pathology for the health sciences. Melbourne: Macmillan Australia Pty Ltd. Wallington EA. (1972) Histological Methods for Bone. London: Butterworths. Young B, Heath JW. (2000) Wheater's Functional Histology. 4th ed. Edinburgh: Churchill Livingstone. CHAPTER 9 DEHYDRATION As soon as the tissue has been fixed, and the bones and teeth have been decalcified, it is necessary to remove the fixative and water from the specimen and replace them with dehydrating fluid in preparation for impregnation. This process of removing intercellular and extracellular water from the tissue following fixation and prior to wax impregnation is known as "dehydration”, and the solutions utilized to make this possible are called "Dehydrating Agents". Many of these dehydrating agents are alcohols of various types that are generally used in increasing strengths to remove aqueous tissue fluids with little disruption to the tissue caused by diffusion currents. It is important to distinguish between drying and dehydration. Drying is the removal of water by evaporation from a solid, semi-solid or liquid. Solid tissues should NEVER be allowed to air dry. Dehydration involves slow substitution of the water in the tissue with an organic solvent. Most dehydrating agents are strong organic solvents that bring about some shrinkage and extraction of cell components. To minimize these effects, dehydrating agents are used in a graded series for short periods of time, and water is gradually replaced so that violent osmotic changes do not produce distortions. Characteristics of an Ideal Dehydrating Solution: 1. It should dehydrate rapidly without producing considerable shrinkage or distortion of tissues. 2. It should not evaporate very fast. 3. It should be able to dehydrate even fatty tissues. 4 It should not harden tissues excessively. 5. It should not remove stains. 6. It should not be toxic to the body. 7. It should not be a fire hazard. As a general rule, whatever dehydrating agent is used, the amount in each step should not be less than 10 times the volume of the tissue in order to ensure complete penetration of the tissue by the dehydrating solution. It is also important to keep the dehydration times as brief as possible to minimize the risk of extracting cellular constituents. Almost any water miscible, anhydrous fluid can be used as a dehydrating agent providing that it does not damage the tissue proteins and is also miscible with the fluids to be used subsequently. Cost may also be a factor. Commonly Used Dehydrating Agents Are: 1. Alcohol (most common) 2. Acetone 3. Dioxane 4. Cellosolve 5. Triethyl phosphate 6. Tetrahydrofuran ALCOHOL Ethyl alcohol (ethanol) is the alcohol recommended for routine dehydration of tissues. It is a clear, colorless, flammable fluid. It is considered to be the best dehydrating agent because it is fast-acting, it mixes with water and many organic solvents, and it penetrates tissues easily. It is not poisonous and not very expensive. Methyl alcohol is a toxic dehydrating agent, primarily employed for blood and tissue films and for smear preparations. Butyl alcohol, which is utilized in plant and animal micro-techniques, is a slow dehydrating agent, producing less shrinkage and hardening than ethyl alcohol and is recommended for tissues which do not require rapid processing. It is not advisable to transfer fixed tissues directly from water or aqueous fixative directly into absolute ethanol. Doing so causes a rapid removal of water which can distort the appearance of more delicate cells and structures. It is advisable to remove water gently and allow the tissue to slowly adjust to its removal. The more delicate the tissue, the more gently this should be done, but there is no hard and fast rule. In most instances, dehydration starts by placing the fixed specimen in 70% ethyl alcohol in water, progressing through 95% ethyl alcohol to 100% ethyl alcohol. For delicate tissues, particularly embryonic tissues, dehydration starting with 30% ethanol is recommended. Under no circumstances should a formalinfixed tissue be transferred directly to higher grades of alcohol, e.g. 85-95% alcohol, because this is liable to produce considerable shrinkage and hardening of tissues leading to distortion. Concentrated alcohols (95% or absolute) tend to harden only the surface of the tissue while the deeper parts are not completely penetrated. This will result in a relatively unequal impregnation of tissue with consequently poor cutting of sections. To avoid this, 70% or lower concentrations of alcohol, gradually increased to 95%, are used. The strength of initial alcohol required in each concentration will depend upon the size, and nature of each tissue and fixative used. Generally, smaller and more delicate tissues require lower concentrations and shorter intervals bet ween changes of succeeding ascending grades of alcohol. A very concentrated solution (above 80%) makes tissues hard, brittle and difficult to cut. Prolonged storage in lower concentrations of alcohol (below 70%) tends to macerate the tissue. The tissue may be stored in 70-80% alcohol, although not for very long periods of time, since this may later interfere with the staining properties of the specimen. Although the tissue reaches the final stage of dehydration in 100% ethanol, it’s not possible to proceed straight to wax embedding-- ethanol and wax don’t mix! This is where ‘clearing’ comes in. The term ‘clearing’ refers to the property of the solvents used- -when they have a relatively high refractive index and when tissue is immersed in them, the tissue becomes transparent and clear. For tissue preparation, one to two hours in each solution should be adequate. Tissues with a high water content such as embryo tissue would require a much shorter time. To ensure complete removal of water during dehydration, use at least two changes of 100% ethanol of at least one half hour each. Never leave tissues in 95 or 100% ethanol more than a total of 2 hours or the tissues will harden. Tissues can be stored in 70% ethanol at any time during an interruption in the routine. The following is a general schedule (time in hours) for alcohol dehydration of big tissues according to the type of fixative used: Susa, 10% Zenker Bouin's Carnoy or Flemming's Formolor Fluid Formol Fluid Saline Helly's Sublimate Running Water Alcohol 30% Alcohol 50% Alcohol 70% Alcohol 90% Absolute Alcohol (1) 1-12 1-12 1-6 1/2-3 1-6 1/2-3 3-12 1-6 3-12 1/2-3 3-12 1-6 3-12 1-6 1-3 1-2 1-2 1-2 1-2 1-2 Absolute Alcohol (2) Absolute Alcohol (3) 1-2 1-2 1-2 1-2 1-2 1-2 1-2 1-2 1-2 1-2 At this point all but a tiny residue of tightly bound (molecular) water should have been removed from the specimen. A typical dehydration sequence for specimens not more than 4mm thick would be: 70% ethanol 15 min 90% ethanol 15 min 100% ethanol 15 min 100% ethanol 15 min 100% ethanol 30 min 100% ethanol 45 min A temperature of 37°C will hasten dehydration time and is especially used for tissue sections that require urgent examinations such as fragmentary biopsies. To insure complete dehydration, a layer of anhydrous copper sulfate, about 1/4 inch deep is placed in the bottom of the container and covered with filter paper. This will accelerate dehydration by removing water from the dehydrating fluid. A blue discoloration of copper sulfate crystals will indicate full saturation of dehydrating fluids with water. Alcohol is then discarded and changed with a fresh solution. Ethanol (ethyl alcohol) Boiling point 78.3° C Advantages: Nontoxic Miscible in all proportions with water Little shrinkage if graded alcohols are used Can be used on eyes and embryos, if graded alcohols are used Fast acting Still considered best dehydrating solution Reliable Appears to cause less extraction of cellular components in general than other agents Inexpensive and easily obtained Disadvantages: Expensive Long periods i n absolute ethanol will cause excessive shrinkage and hardening May be difficult to obtain May have prohibitive taxes that necessitate troublesome book-keeping Extracts methylene blue and other thiazine dyes from sections Extracts more lipids than acetone May cause more shrinkage of specimen May react with an unreduced 0s04 remaining in specimen Only slightly miscible with most resins Butanol (butyl alcohol) Boiling point 117.7° C Advantages: Less shrinkage and hardening than with ethyl Excellent for slow processing Miscible with paraffin Disadvantages: Odorous Slow-acting Long periods of infiltration necessary Dehydrating power low Tertiary butanol (butyl alcohol) Boiling point 82.8° C Advantages: Universal solvent—acts as dehydrating and clearing agent May be used in staining series as a dehydrating agent Mixes with water, ethanol, xylene, and paraffin in all Disadvantages: Odorous More expensive than butanol Primary infiltration must be done in half tertiary butanol and half paraffin, prior to paraffin impregnation Reagent tends to solidify at room temperature or below 25° C Isopropanol (isopropyl alcohol) Boiling point 82.3° C Advantages: Excellent substitute for ethanol Less shrinkage and hardening than ethanol No government restrictions on its use Sufficiently water-free to use in place of absolute ethanol Lillie considers it “the best all- around substitute for ethyl alcohol” Less expensive than tax-free alcohol Disadvantages: • Cannot be used in the celloidin technic since nitrocellulose is insoluble in it • Cannot be used for preparing staining solutions, since dyes are not soluble in it Pentanol (amyl alcohol) Boiling point 128° C Advantages: Miscible with 90% alcohol, toluene and xylene Dissolves paraffin wax Disadvantages: Toxic Cannot be used in poorly ventilated rooms Not miscible with water ACETONE (Boiling point 56° C) Acetone is a cheap, rapid-acting dehydrating agent utilized for most urgent biopsies which it dehydrates in 1/2 to 2 hours. Acetone is a clear, colorless fluid that mixes with water, ethanol and most organic solvents. Acetone is more miscible with epoxy resins than alcohol, but is highly flammable and requires considerable care in handling. It is rapid in action but penetrates tissues poorly and causes brittleness in tissues that are placed in acetone for prolonged period of time. Most lipids are removed from tissues with this dehydrating agent. Its use has been limited only to small pieces of tissues due to its extreme volatility and inflammability. Because of considerable tissue shrinkage produced, acetone is not recommended for routine dehydration purposes. Advantages: Rapid dehydrating agent Less expensive than ethanol Does not extract methylene blue and other dyes from stained sections May cause less shrinkage of specimen than ethanol Not reactive with 0s04 remaining in specimen. Miscible with most embedding resins. Disadvantages: Requires a clearing agent Volume must be 20 times that of the tissue Best processing requires a graded series of a mixture of acetone and xylene before one can go into paraffin Needs good ventilation Evaporates rapidly Flammable Absolute acetone is easily contaminated with water, resulting in complete dehydration. Uranyl acetate and phosphotungstic acid are only soluble in dilute solutions of acetone. DIOXANE (Diethylene Dioxide) Refractive index 1.42; Boiling point 101.5° C Dioxane is an excellent dehydrating and clearing agent readily miscible in water, melted paraffin, alcohol and xylol. It produces less tissue shrinkage as compared to alcohol dehydration. Tissues can be left in this reagent for long periods of time without affecting the consistency or staining properties of the specimen. Because dioxane is miscible with both water and paraffin, tissues may be placed directly into the solution after washing out. However, tissue sections dehydrated with dioxane tend to ribbon poorly. Aside from being expensive, dioxane is also extremely dangerous, and this is its main disadvantage. Its vapor produces a cumulative and highly toxic action in man; hence, it should not be used routinely. The laboratory room should be properly ventilated, and all residues should be washed down in the sink. It should not be recycled as the risk of creating explosive peroxides increases greatly. The following is an example of a time schedule for dehydration with dioxane Graupner's Method): (1st) pure dioxane solution 1 hour (2nd) pure dioxane solution 1 hour (3rd) pure dioxane solution 2 hours (1st) Paraffin wax 15 minutes (2nd) Paraffin wax 45 minutes (3rd) Paraffin wax 2 hours Embed in mold and cool in water. In another method (Weiseberger's method), the tissue is wrapped in a gauze bag and suspended in a bottle containing dioxane and a little anhydrous calcium oxide. Water is displaced from the tissue by dioxane and in turn absorbed by calcium oxide or quicklime. Dehydration period ranges from 3-24 hours. Tissues which have been treated with a chromate fixative, e.g. Regaud's or Moller's fluid, should be thoroughly washed in running tap water prior to treatment with dioxane in order to remove the chromate. Advantages: Universal solvent—it dehydrates and clears Miscible with water, alcohol, xylene, and paraffin Does not harm tissue over long time periods Faster dehydrant than ethanol Disadvantages: Needs large volume for dehydration Costs about for times more than does absolute alcohol Must be used in well-ventilated rooms Cumulatively toxic Odorous Distorts tissue-containing cavities CELLOSOLVE (Ethylene glycol monoethyl ether) Boiling point 156.4° C Cellosolve dehydrates rapidly. The tissue may be transferred from water or normal saline directly to cellosolve and stored in it for months without producing hardening or distortion. CAUTION: Ethylene glycol ethers are combustible at 110-120°F and are toxic by inhalation, skin contact and ingestion. Following exposure, the reproductive, fetal, urinary and blood systems are particularly vulnerable to their toxic side effects. If it cannot be avoided, propylene-based glycol ethers should be used instead of ethylene-based glycol ethers. Advantages: Rapid dehydrating agent Tissue may remain in it for months without injury Avoids distortion and does not require graded dilutions Disadvantages: Expensive Rapidly absorbs water from the air Requires clearing agent TRIETHYLPHOSPHATE- Boiling point 215° C When tissues are fixed, washed and transferred directly into triethyl phosphate solution for dehydration, it removes water very readily and produces very little distortion and hardening of tissue. It is soluble in alcohol, water, ether, benzene, chloroform, acetone and xylene. It is used to dehydrate sections and smears following certain stains and produces minimum shrinkage. Advantages: May be used in routine paraffin technic Displaces water readily with slight distortion Does not harden tissue excessively May be used as a dehydrating solution in the staining sequence Soluble in alcohols, benzene, toluene, xylene, ether, chloroform Disadvantages: None TETRAHYDOFURAN (THF) Tetrahydrofuran (THF) is a reagent that both dehydrates and clears tissues since it is miscible in both water and paraffin. It can dissolve many substances including fats and is in itself miscible with lower alcohols, ether, chloroform, acetone, benzene and xylene. It may be used for demixing, clearing and dehydrating paraffin sections before and after staining. It causes less shrinkage and easier cutting of sections with fewer artifacts. It does not dissolve out aniline dyes. In fact, most staining procedures give improved results with tetrahydrofuran. THF is toxic if ingested or inhaled. Vapors cause nausea, dizziness, headache and anesthesia. It is an eye and skin irritant, and prolonged exposure (up to 6 months) may cause conjunctival irritation. Because of this and its rather offensive odor, processing with THF should be done in a well- ventilated room. Although Teflon gloves may be suitable, the use of THF should be avoided if possible, as there is no practical way to absolutely protect skin against contact. Advantages: Miscible in all proportions with water, ether, chloroform, acetone, and the hydrocarbons xylene, toluene, and benzene Rapid without excessive shrinkage and hardening Low toxicity; low fire and explosion hazard Not toxic Better results than most universal solvents Solvents of mounting media Disadvantages: Odorous- should be used in well-ventilated room • Evaporates rapidly Dyes are not soluble in tetrahydrofuran DEHYDRATING AGENTS FOR ELECTRON MICROSCOPY Tissue processing for transmission electron microscopy (TEM) is commonly accomplished using ethanol as a dehydrating solvent and propylene oxide as a transition fluid. Both solvents have some undesirable properties: ethanol solubilizes lipids; propylene oxide is completely miscible with embedding resins and, because of its low viscosity, it can infiltrate tissues readily and reduce the viscosity of embedding resin mixtures. However, it is highly flammable, volatile, toxic, and potentially carcinogenic. It is very reactive even at low temperatures, may combine with reactive groups in cells, and may cause certain cytochemical and staining reactions. Traces may be retained in polymerized resin. It may react with epoxy groups and partially inhibit polymerization which adversely affects hardness and cutting properties of blocks. Acetonitrile is a good substitute for propylene oxide. It is reported to be non-carcinogenic, less toxic and not as flammable as propylene oxide. It is freely miscible with water, alcohols, acetone, and epoxy resins. It does not interfere with epoxy polymerization; and the resulting cured resins have excellent cutting quality and beam stability. Acetonitrile is also an excellent dehydrating agent whose use does not necessitate modification of current techniques. Most importantly, the low solubility of phospholipids in acetonitrile limits the loss of membrane lipids and, hence, leads to a better preservation of tissue features. It is also used as a dehydrating agent for cells prepared for Scanning Electron Microscopy (SEM). REFERENCES Anderson G, Bancroft J. (2002) Tissue processing and microtomy. In: Bancroft, J.D., Gamble, M. Theory and Practice of Histological Techniques. 5th Ed., Churchill Livingstone, London, 100. Baker FJ. (1962) Progress in Medical Laboratory Technology, Vol. 1, Butterworths and Company, London. Baker FJ. (1962) Progress in Medical Laboratory Technology, Vol. 2, Butterworths, London. Baker FJ, Silverton RE, Luckcock ED. (1966) Introduction to Medical Laboratory Technology, Butterworths, London. Baker RD. (1967) Postmortem Examination, Specific Methods and Procedures. W.B. Saunders, London and Philadelphia. Bancroft JD, Cook HC. (1994) Manual of Histological Techniques and the ir Diagnostic Application, Churchill Livingstone, Edinburgh. Brown CC. (1969) Primer of Histopathologic Technique. Appleton-Century-Crafts, New York. Drury RAB, Wallington EA. (1980) Carlton’s Histological Technique. 5t11 ed. Oxford University Press, London. Baker JR. (1958) Principles of Microbiological Microtechnique. Mehuen & Co., Ltd., London. Clark G. ed. (1960) Staining Procedures Used by the Biological Stain Commission, 3rd ed. William & Wilkins, Baltimore. Culling CFA. (1974) Handbook of Histopathological and Histochemical Techniques, 3rd ed. Butterworth, Massachusetts. Drury RAB, Wallington EA. (1967) Carleton s Histological Technique, 4th ed. University Press, Oxford. Edwards HH, Yeh YY, Tarnowski BI, Schonbaum GR. (1992) Acetonitrile as a substitute for ethanol/propylene oxide in tissue processing for transmission electron microscopy: comparison of fine structure and lipid solubility in mouse liver, kidney, and intestine. Microsc Res Tech 21(1):39-50. Holshek JG, Akins RE. (1994): Acetonitrile is better than ethanol as a dehydrating agent for cells prepared for SEM. Proc Mic Soc of Amer, 52nd Annual Mtg, San Francisco Press, ed GW Bailey and AJ Garrett-Reed, pp 324-325. Lillie RD, Fullmer HM. (1976) Histopathologic Technic and Practical Histochemistry, 4th ed. McGraw-Hill Book Co., New York. Mollenhauer HH. (1993) Artifacts caused by dehydration and epoxy embedding in transmission electron microscopy. Microsc Res Tech. 26(6):496-512. Raphael SS. (1983) Processing tissues for histotechnology. In: Raphael SS et al, eds. Lynch s Medical Laboratory Technology, 4th ed. W.B. Saunders Co., Philadelphia, Chapt 32,759. Sheehan DC, Hrapchak BB, Eds. (1980) Theory and Practice of Histotechnology, 2nd ed. CV Mosby Co., St. Louis. Stratton CJ, Erickson TB, Wetzstein HY. (1982) The lipid solubility of fixative, staining and embedding media, and the introduction of LX-112 and poly/bed-812 as dehydrants for epoxy resin embedment. Tissue Cell. 14(1):13-24. Tarnowski BI, Schonbaum GR. (1984) Acetonitrile: substitute for propylene oxide in tissue processing for transmission electron microscopy. Proc 42nd Ann Meeting Elec Mic Society of America, p 38 CHAPTER 10 CLEARING Although the dehydrated tissue is now essentially water-free, it still cannot be infiltrated with wax because wax and ethanol are largely immiscible. An intermediate solvent that is fully miscible with both ethanol and paraffin wax is needed to remove alcohol and other dehydrating solutions from tissues prior to embedding (usually in paraffin wax), and from finished slides prior to mounting. They are also used after sectioning to remove paraffin wax after cutting on the microtome. Clearing (de-alcoholization) is the process whereby alcohol or a dehydrating agent is removed from the tissue and replaced with a substance that will dissolve the wax with which the tissue is to be impregnated (e.g. paraffin) or used as the medium on which the tissue is to be mounted (e.g. Canada balsam). Aside from removing alcohol, a clearing agent must also be miscible with Canada balsam and other resins that are used for mounting sections. This stage in the process is called “clearing” because many (but not all) clearing agents impart an optical clarity or transparency to the tissue due to their relatively high refractive index. This change in appearance is often used as an indication of the effectiveness or completeness of the clearing process. Because of the high refractive indices of most reagents used for de-alcoholization, tissues, particularly embryos and parasites, become transparent so that the internal structures become visible to the naked eye. Another important role of the clearing agent is to remove a substantial amount of fat from the tissue which otherwise presents a barrier to wax infiltration. The most commonly used clearing agent for this purpose is xylene. Glycerin and gum syrup are used when the tissue is to be cleared directly from water, as in a frozen section. No de-alcoholization is involved in this process. Characteristics of a Good Clearing Agent: It should be miscible with alcohol to promote rapid removal of the dehydrating agent from the tissue. It should be miscible with, and easily removed by melted paraffin wax and/or by mounting medium to facilitate impregnation and mounting of sections. It should not produce excessive shrinkage, hardening or damage of tissue. It should not dissolve out aniline dyes. It should not evaporate quickly in a water bath. It make tissues transparent. The choice of a clearing agent depends upon the following: The type of tissues to be processed, and the type of processing to be undertaken The processor system to be used Intended processing conditions such as temperature, vacuum and pressure Safety factors Cost and convenience Speedy removal of dehydrating agent Ease of removal by molten paraffin wax Minimal tissue damage Clearing fluids with a low boiling point are generally more readily replaced by melted paraffin, although chloroform which has a lower boiling point than xylene in fact takes longer than the latter to clear. Viscosity also affects the speed of penetration of the clearing agent. Prolonged exposure to most clearing agents causes the tissue to become brittle and therefore more difficult to cut. A. Xylene (Xylol) Xylene is a colorless clearing agent that is most commonly used in histology laboratories. Clearing time is usually 1/2 to 1 hour. It is used for clearing, both for embedding and mounting procedures. It is generally suitable for most routine histologic processing schedules of less than 24 hours, and when the tissue block size is less than 5 mm. in thickness. Xylene is reasonably cost effective and works well for short-term clearing of small tissue blocks. Xylene is one of the routinely used chemical in histology and pathology laboratories because of its vital role in the paraffin wax tissue processing method. It is mostly used as a clearing agent during tissue processing and as a dewaxing agent during staining. It is also used in cover slipping, in cleaning tissue processors, as solvent to remove synthetic immersion oil from the microscope objective and in recycling of used slides. However, several toxicities believed to be caused by intermediate products of xylene metabolism such as methyl benzaldehyde have been reported. These include central nervous system disorders, respiratory depression, abdominal pain, dryness and redness of skin, dermatitis, liver diseases, nephrotoxicity, conjunctivitis, and teratogenic and fetotoxic effects. Advantages: It is the most rapid clearing agent, suitable for urgent biopsies which it clears within 15-30 minutes. It makes tissues transparent. It is miscible with absolute alcohol and paraffin. It does not extract out aniline dyes. For mounting procedures, it does not dissolve celloidin and can, therefore, be used for celloidin sections. It evaporates quickly in paraffin oven and can, therefore, be readily replaced by wax during impregnation and embedding. It is cheap. Disadvantages: It is highly inflammable and should be appropriately stored. If used longer than 3 hours, it makes tissues excessively hard and brittle. It causes considerable hardening and shrinkage of tissues; hence, is not suitable for nervous tissues and lymph nodes. Xylene becomes milky when an incompletely dehydrated tissue is immersed in it. Xylene may irritate eyes, nose and respiratory tract. It can be absorbed through the skin and cause dermatitis. At high concentrations, it is toxic and narcotic. Special Handling Procedures and Storage Requirements: • Keep container tightly closed to prevent xylene from subliming and entering the atmosphere. • Only non-sparking tools may be used to handle xylene. • Store in a cool and dry area away from incompatible substances (i.e. oxidizing agents, strong acids). • Store xylene in a flammable liquid storage cabinet. • Wash hands thoroughly after handling xylene (even if gloves were used). • Remove contaminated clothing and wash before reuse. • Keep away from heat, sparks, flames, sources of ignition (including empty containers that will retain product residue). • Transport chemicals in closed containers, in the smallest amounts possible, and use aids such as carts, chemical transport carriers, etc. • It is highly recommended that all chemicals be stored below eye level so cracking or leaking containers are immediately visible and there is less potential for chemicals falling onto lab workers when pulling from shelves. B. Toluene Toluene is better at preserving tissue structure and is more tolerant of small amounts of water left behind in the tissues than xylene. However, toluene is more expensive than xylene and more toxic, so toluene is less commonly used. Toluene may be used as a substitute for xylene or benzene for clearing both during embedding and mounting processes. Time recommended for clearing is 1 -2 hours. Advantages: It is miscible with both absolute alcohol and paraffin. It acts fairly rapidly and is recommended for routine purposes. Tissues do not become excessively hard and brittle even if left in toluene for 24 hours. Clears overnight. It is not carcinogenic. Disadvantages: It is slower than xylene and benzene. It tends to acidify in a partially filled vessel. Highly concentrated solutions will emit fumes that are toxic upon prolonged exposure. It is more expensive. C. Benzene Benzene is preferred by some as clearing agent in the embedding process of tissues because it penetrates and clears tissues rapidly. It used to be a popular routine clearing agent until recently when its highly carcinogenic properties were recognized. Its use for clearing purposes is therefore strongly discouraged. Advantages: It is rapid acting, hence is recommended for urgent biopsies (15-60 minutes) and routine purposes. It volatilizes rapidly in paraffin oven and is therefore easily eliminated from the tissue. It is miscible with absolute alcohol. It does not make tissues hard and brittle. It causes minimum shrinkage. It makes tissues transparent. It clears overnight. Disadvantages: It is highly flammable. If a section is left in benzene for a long time, considerable tissue shrinkage may be observed. Hence, tissues should be transferred to paraffin wax as soon as possible. Excessive exposure to benzene may be extremely toxic to man and may become carcinogenic or it may damage the bone marrow resulting in aplastic anemia. If ever benzene is to be used for clearing, the laboratory should be well-ventilated. D. Chloroform Chloroform, when used for clearing of tissues during the embedding process, is slower in action than xylene, but causes less brittleness. Thicker tissue blocks, even those up to I cm. in thickness, can be processed. However, tissues placed in chloroform do not become translucent. Advantages: It is recommended for routine work (6-24 hours). It is miscible with absolute alcohol. It is recommended for tough tissues (e.g. skin, fibroid and decalcified tissues) for nervous tissues, lymph nodes and embryos because it causes minimum shrinkage and hardening of tissues. It is suitable for large tissue specimens. It is not inflammable. Disadvantages: It is relatively toxic to the liver after prolonged inhalation; this may be prevented by adequate room ventilation. Wax impregnation after chloroform clearing is relatively slow. It does not make tissues transparent. It is not very volatile in paraffin oven; hence, it is difficult to remove from paraffin sections. It may even produce considerable deterioration of the wax. Its vapor may attack the rubber seal used in vacuum impregnating bath. Complete clearing is difficult to evaluate. Tissues tend to float in chloroform; this may be avoided by wrapping the tissues with absorbent cotton gauze to facilitate sinking of the section in solution. It evaporates quickly from a water bath. E. Cedarwood Oil Cedarwood oil is used to clear both paraffin and celloidin sections during the embedding process. It is especially recommended for central nervous system tissues and cytological studies, particularly of smooth muscles and skin. It requires two changes in clearing solution. Clearing is usually complete in 2-3 days. Advantages: It is very penetrating. It is miscible with 96% alcohol which it removes readily. It clears celloidin in 5-6 days. It causes minimal shrinkage of tissues. Tissues may be left in oil indefinitely without considerable damage and distortion. It does not dissolve out aniline dyes. It makes tissues transparent. It does not harden tissues. It does not interfere too seriously with paraffin penetration if it is not completely removed. Clearing with cedarwood oil often improves cutting of the sections. Disadvantages: It is an extremely slow clearing agent, hence, it is not recommended for routine purposes. It is slightly slower in penetrating than benzene. It is hard to eliminate from the tissues in paraffin bath, making the wax impregnation process very slow. This may be improved or hastened by transferring the specimen from oil to benzene for 1/2 hour before finally placing the tissue in wax. Quality is not always uniform and good. Tissues cleared in cedarwood oil initially float before gradually staying to the bottom as clearing proceeds. Hence, the tissue may dry out before it is completely cleared. This can be prevented by superimposing absolute alcohol on the surface of the clearing agent. Once saturated, the specimen should then be transferred to a fresh solution of cedarwood oil. Cedarwood oil becomes milky upon prolonged storage and should be filtered before use. Cedarwood oil that has been previously used to clear acetic-alcohol fixed tissues may produce crystals with a melting point of approximately 35°C and therefore interfere with adequate clearing of tissue. The solution must be heated to 200°C in order to dissolve the crystals and restore the solution to its normal state. It is very expensive. F. Aniline oil This is not normally utilized as a routine clearing agent but it is recommended for clearing embryos, insects and very delicate specimens, due to its ability to clear 70% alcohol without excessive tissue shrinkage and hardening. G. Clove oil This reagent causes minimum shrinkage of tissues. However, its quality is not guaranteed due to its tendency to become adulterated. Wax impregnation after clearing with clove oil is slow and difficult. Tissues become brittle, aniline dyes are removed, and celloidin is dissolved. All of these, in addition to the expensiveness of the solution, make it unsuitable for routine clearing purposes. H. Carbon tetrachloride Carbon Tetrachloride may be used in clearing tissues for embedding. Its properties are very similar to that of chloroform although it is relatively cheaper. Its disadvantage is the same as that of chloroform. It produces considerable tissue hardening, and is dangerous to inhale on prolonged exposure due to its highly toxic effects. I. Tetrahydrofuran Tetrahydrofuran is superior to ordinary dehydrating and clearing agents due to its ability to perform two processes at the same time, thereby shortening the total processing time and allowing more time for fixation. It is non-toxic but has offensive odor and should be used in a well-ventilated room. J. Dioxane Dioxane is miscible both with water and paraffin. It is used primarily when time is important because the tissues may be embedded with paraffin within 4 hours after fixation. The tissues are transferred to dioxane straight from Bouin's fluid or a formalin fixative. The dioxane is changed 3 times within 4 hours and the tissues are transferred directly to paraffin (3 changes are made in a total of 90 minutes). Dioxane causes greater shrinkage than xylene does. In addition, it is dangerous. Fumes of dioxane are toxic to human especially to the liver. Other Xylene Substitutes The reported toxicity and environmental pollution from unsafe disposal of xylene led to its substitution with other less-toxic substitutes such as limonene reagents, mineral oil mixtures, 1.7% dish washing solution, vegetable oils and coconut oil. Though these substitutes exist, their availability in commercial quantities in developing countries has hampered their use. All the xylenesubstitutes have to be analyzed thoroughly, before concluding which alternative is better. Terpenes are isoprene polymers found in essential oils originally derived from plants, though some are now synthesized. They are the earliest transition solvents to be used in histology and include turpentine and oils of bergamot, cedarwood, clove, lemon, oreganum and sandalwood. In general the natural oils are not highly pure compounds but contain several substances. Many terpenes clear tissues and celloidin sections from 80%-95% alcohol, render tissues transparent and have a slow gentle non-hardening action. Most are generally regarded as safe though some have particularly strong odors which can be overpowering, requiring good laboratory ventilation. Terpenes are moderately effective solvents, but they too are considered toxic. Solvents in this class also dry slowly, leave an oily residue on slides and are relatively expensive. One of the recommended xylene substitutes from the terpene family is Limonene, a volatile oil found in citrus peels which goes by several trade names. It is a natural oil found in the skins of citrus fruits, such as lemons or oranges, and in cooking is usually referred to as lemon or orange zest. Limonene is obtained industrially by the steam distillation of orange peel which is a byproduct of the orange juice industry. It is a clear, colorless fluid with a distinctly citrus aroma, not unpleasant to most people, although some do not like it. Limonene is often sold as a xylene replacement and some technologists substitute it for xylene in other uses, but this is not universally successful. When used as the clearant immediately prior to cover slipping, there are some reports that the mounting medium, usually dissolved in either toluene or xylene, does not mix well with the limonene. In such cases, replacing the limonene with xylene or toluene, or quickly dipping the section in either one just prior to cover slipping should be effective. This does, of course, defeat the purpose of the replacement to a certain degree. Orange oil based clearing agents offer the clearing action with the lowest hazard rating of all xylene alternatives. It is excellent for preserving fine tissue structure, and can often be used in place of xylene with no alteration of protocol. In using a product containing orange oils, it is important to use a product which has been rigorously purified then stabilized. Orange oils that are neither pure nor stable can break down to produce compounds which will interfere with staining procedures. Chlorinated hydrocarbons can be effective solvents, but they are considered toxic chemicals, posing serious health risks. Government regulations have restricted most of the effective solvents in this class. Coconut oil is an efficient substitute for xylene, as it is non-hazardous, less expensive and causes less shrinkage of the tissue. It can be used as a dealcoholization agent in the histopathological laboratory, without losing the quality of the histological details. The only drawback associated with coconut oil, is its tendency to get solidified at a lower temperature. However, this can be overcome by performing the clearing procedure in an incubator, maintaining the required temperature. Substitution of the conventional xylene with bleached palm oil as a clearing agent during tissue processing and as a dewaxing agent during staining gives good tissues, sections and histological slides. In addition, bleached palm oil is nontoxic, nonhazardous, nonflammable, bio-degradable, economic, easy to handle, and readily available. REFERENCES Anderson K, Fuxe K, Nilsen OG. (1981) Production of discrete changes in dopamine and noradrenaline levels and turnover in various parts of the rat brain following exposure to xylene. Toxicol Appl Pharmacol. 60:535–48. Anderson G, Bancroft J. (2002) Tissue processing and microtomy. In: Bancroft, J.D., Gamble, M. Theory and Practice of Histological Techniques. 5th Ed., Churchill Livingstone, London, 100. Andre GG, Wenger JB, Rebolloso D, Arrington JB, Mehm WJ. (1994) Evaluation of clearing and infiltration mixtures (CIMs) as xylene substitutes for tissue processing. J Histotechnol. 17:137–42. Ankle MR, Joshi PS. (2011) A study to evaluate the efficacy of xylene-free hematoxylin and eosin staining procedure as compared to the conventional hematoxylin and eosin staining: An experimental study. J Oral Max Pathol. 15:161–7. Atlanta: Georgia. (1993) Toxicological profile for xylene, U.S Department of Health and Human Services, public health service, Agency for toxic substance and disease registry. Baker FJ. (1962) Progress in Medical Laboratory Technology, Vol. 1, Butterworths and Company, London. Baker FJ. (1962) Progress in Medical Laboratory Technology, Vol. 2, Butterworths, London. Baker FJ, Silverton RE, Luckcock ED. (1966) Introduction to Medical Laboratory Technology, Butterworths, London. Baker RD. (1967) Postmortem Examination, Specific Methods and Procedures. W.B. Saunders, London and Philadelphia. Bancroft JD, Cook HC. (1994) Manual of Histological Techniques and their Diagnostic Application. Churchill Livingstone, Edinburgh. Brown CC. (1969) Primer of Histopathologic Technique. Appleton-Century-Crafts, New York. Buesa RJ. (2000) Mineral oil: The best xylene substitute for tissue processing yet. J Histotechnol. 23:143–9. Buesa RJ, Maxim VP. (2009) Histology without xylene. Ann Diagn Pathol.13:246–56. Culling, C.F.A. (1974) Handbook of Histopathological and Histochemical Techniques, 3rd ed., Butterworths, Massachusetts. Drury RAB, Wallington EA. (1967) Carleton’s Histological Technique, 4th ed. University Press, Oxford. Drury RAB., Wallington EA. (1980) Carlton s Histological Technique. 5th ed. Oxford University Press, London. Erickson T, Amed V, Leibach SJ, Bushnik P, Saxon A, Hryhorczuk DO, et al. (1994) Acute bone marrow toxicity and pancytopenia following exposure to lead chromate, xylene, and significant changes in the amounts of neurotransmitter and related substances in rat brain induced by subacute exposure to low levels of toluene and xylene. Ind Health. 21:143–51 Kandyala R, Raghavendra SP, Rajasekharan ST. (2010) Xylene: ethylbenzene in a degloving injury. Am J Hematol. 47:257–61. Falkeholm L, Grant CA, Magnusson A, Möller E. (2001) Xylene-free method for histological preparation: A multicentre evaluation. Lab Invest. 81:1213–21. Hipolito RN. (1980) Xylene poisoning in laboratory workers: Vase reports and discussion. Lab Med. 11:593–5. Honma T, Sudo A, Miyagawa M, Sato M, Hasegawa H. (1983An overview of its health hazards and preventive measures. J Oral Max Pathol. 14:1–5 Lab-Tek Products, Division of Miles Laboratories Inc., Naperville, Ill. 60540. Raphael, S.S. (1983) Processing tissues for histotechnology. In: Raphael SS et al, eds. Lynch s Medical Laboratory Technology, 4t11 ed. Chapt 32, W.B. Saunders Co., P hiladelphia, 759. Lillie RD, Fullmer HM. (1976) Histopathologic Technic and Practical Histochemistry, 4t11 ed. McGraw-Hill Book Co., New York. Lyon H, Holm I, Prento P, Balslev E. (1995) Non-hazardous organic solvents in the paraffin embedding technique: A rational approach. Histochem Cell Biol.103:263–9. Rasmussen B, Hjort K, Mellerup I, Sether G, Christensen N. (1992) Vegetable oils instead of xylene in tissue processing. Acta Pathol Microbio Immunol Scandinavica. 100:827–31. Reinherdt PA, Leonard KL, Ashbrook PC. (1996) Pollution prevention and waste minimization in laboratories. Vol. 3. Florida: CRC press, Lewis Publishers; Xylene substitutes; p. 346. Revilla AS, Pestana CR, Pardo-Andreu GL, Santos AC, Uyemura SA, Gonzales ME, et al. (2007) Potential toxicity of toluene and xylene evoked by mitochondrial uncoupling. Toxicol in vitro. 21:782– 8. Savoleinen H, Pfaffli P. (1980) Dose dependent neurochemical changes during short term inhalation exposure to xylene. Arch Toxicol. 1980; 45:117–22 Sheehan DC, Hrapchak BB, Eds. (1980) Theory and Practice of Histotechnology, 2nd ed. CV Mosby Co., St. Louis. Smith J. (2007) Freeman Hospital, Osteo-articular Histology Laboratory, Newcastle upon Tyne, UK, 2Royal Victoria Infirmary, Biopsy Laboratory, Histopathology Department, Newcastle upon Tyne, UK. Uchida Y, Nakatsuka H, Ukai H, Watanabe T, Liu YT, Huang MY. (1993) Symptoms and signs in workers exposed predominantly to xylene. Int Arch Occup Environ Health. 64:597–605. CHAPTER 11 IMPREGNATION AND EMBEDDING Impregnation (Infiltration) is the process whereby the clearing agent is completely removed from the tissue and replaced by a medium that will completely fill all the tissue cavities and give a firm consistency to the specimen. This allows easier handling and cutting of suitably thin sections without any damage or distortion to the tissue and its cellular components. Embedding (Casting or Blocking) is the process by which the impregnated tissue is placed into a precisely arranged position in a mold containing a medium which is then allowed to solidify. Ideally, an infiltrating and embedding medium should be: soluble in processing fluids suitable for sectioning and ribboning molten between 30°C and 60°C translucent or transparent; colorless stable homogeneous capable of flattening after ribboning non-toxic odorless easy to handle inexpensive The medium used to infiltrate the tissue is usually the same medium utilized for impregnation, and for general purposes is known as an Embedding Medium. There are generally four types of impregnation and embedding medium, namely: 1. Paraffin wax 2. Celloidin (collodion) 3. Gelatin 4. Plastic PARAFFIN WAX IMPREGNATION Paraffin is the simplest, most common and best embedding medium used for routine tissue processing. Paraffin wax is a polycrystalline mixture of solid hydrocarbons produced during the refining of coal and mineral oils. It is solid at room temperature but melts at temperatures up to about 65°C or 70°C. Paraffin wax can be purchased with melting points at different temperatures, the most common for histological use being about 56°C to 58°C. At its melting point, it tends to be slightly viscous, but this decreases as the temperature is increased. The traditional advice with paraffin wax is to use this about 2°C above its melting point. Wax hardness (viscosity) depends upon the molecular weight of the components and the ambient temperature. To decrease viscosity and improve infiltration of the tissue, technologists often increase the temperature to above 60°C or 65°C. High molecular weight mixtures melt at higher temperatures than waxes comprised of lower molecular weight fractions. Paraffin wax is traditionally marketed by its melting points which range from 39°C to 68°C. Tissue-wax adhesion depends upon the crystal morphology of the embedding medium. Small, uniform sized crystals provide better physical support for specimens through close packing. Crystalline morphology of paraffin wax can be altered by incorporating additives which result in a less brittle, more homogeneous wax with good cutting characteristics. There is consequently less deformation during thin sectioning. Setting temperature does not appreciably affect crystal size. Advantages: 1. Thin individual serial sections may be cut with ease from the majority of tissues without distortion. 2. The process is very rapid, allowing sections to be prepared within 24 hours. 3. Tissue blocks and unstained mounted sections may be stored in paraffin for an indefinite period of time after impregnation without considerable tissue destruction. 4. Because formalin-fixed, paraffin-embedded tissues may be stored indefinitely at room temperature, and nucleic acids (both DNA and RNA) may be recovered from them decades after fixation, they are an important resource for historical studies in medicine. 5. Many staining procedures are permitted with good results. Disadvantages: 1. Overheated paraffin makes the specimen brittle. 2. Prolonged impregnation will cause excessive tissue shrinkage and hardening, making the cutting of sections difficult. 3. Inadequate impregnation will promote retention of the clearing agent. Tissues become soft and shrunken, and tissue blocks crumble when sectioned and break up when floated out in a water bath. 4. Tissues that are difficult to infiltrate, e.g. bones, teeth, brains and eyes, need long immersion for proper support; otherwise, they will crumble on sectioning. Prolonged immersion in paraffin, on the other hand, is not advisable. 5. Paraffin processing is not recommended for fatty tissues. The dehydrating and clearing agents used in the process dissolve and remove fat from the tissues. After being completely cleared, the tissue is submerged in two or more changes of melted paraffin wax, either in a paraffin oven or in an incubator which has been regulated at 55-60°C. The duration and number of changes required for thorough impregnation of tissue depends on: – Size and type of tissues: Longer time is required for thicker tissues. Use of vacuum imbedding: Vacuum reduces the time required for complete impregnation. Clearing agent employed Common waxes have melting points of 45°C, 52°C, 56°C and 58°C. The 56°C wax is normally used for routine work. In a laboratory with temperature ranging from 20-24°C, paraffin wax with a melting point of 54-58°C is indicated. If the laboratory temperature is between 15-18°C, the melting point of wax to be used should be between 50 and 54°C. Hard tissues require wax with a higher melting point than soft tissues. There are three ways by which paraffin wax impregnation and embedding of tissues may be performed: 1. By manual processing 2. By automatic processing 3. By vacuum embedding 1. Manual Processing At least four changes of wax are required at 15 minutes intervals in order to insure complete removal of the clearing agent from the tissue. The specimen is then immersed in another fresh solution of melted paraffin for approximately 3 hours to insure complete embedding or casting of tissue. The following is an example of a time schedule for manual processing of tissues about 3 mm. thick: Fixation: 10% Buffered Formalin 24 hours Dehydration: 70% Alcohol 6 hours 95% Alcohol 12 hours 100%Alcohol 2 hours 100% Alcohol 1 hour 100%Alcohol 1 hour Clearing: Xylene or Toluene 1 hour Xylene or Toluene 1 hour Impregnation: Paraffin wax 15 minutes Paraffin wax 15 minutes Paraffin wax 15 minutes Paraffin wax 15 minutes Embedding: Paraffin wax 3 hours 2. Automatic Processing This method makes use of an automatic tissue processing machine (i.e., Autotechnicon) which fixes, dehydrates, clears and infiltrates tissues, thereby decreasing the time and labor needed during the processing of tissues. This results in a more rapid diagnosis with less technicality. Usually, only 2- 3 changes of wax are required to remove the clearing agent and properly impregnate the specimen. This is made possible due to constant tissue agitation which accelerates and improves tissue penetration giving rise to more consistent results. One example of an automatic tissue processing machine is the Elliott Bench-Type Processor. The machine is mounted on rollers to permit the turning of platforms and easy access to beakers and wax baths. It makes use of 12 individual processing steps, with ten 1-liter capacity glass beakers and two thermostatically controlled wax baths with a safety device cut-out switch to protect the wax against over-heating. A transfer arm controlled by electrical current moves the tissues from one processing reagent to another (by clock schedules). It can be removed by raising a spring-loaded plunger in the center of the cover plate, thereby allowing the tissue to be arranged manually anytime during the processing. Agitation of fluid is accompanied by a continuous vertical movement or rotation of the specimen carrier by a mechanism connected to the transfer arm. An electrical clock connected to a metal disc notched in positions of 15 minutes or more, serves to control the time needed for each processing step. The clock rotates and sets the transfer arm and mechanism into motion, moving the tissue to the next position. A delay mechanism is provided in instances where processing time may exceed 24 hours. REAGENT PROCESSING TIME Schedule 1 Schedule 2 Schedule 3 10% Buffered Formalin 2 hrs. 2 hrs. 2 hrs. 10% Buffered Formalin 70% Alcohol 2 hrs . 2 hrs. 2 hrs. 2 hrs . 2 hrs. 2 hrs. Absolute Alcohol (1) 1 hr. 3 hrs. Absolute Alcohol (2) 1 hr. 3 hrs. 2 hrs. 2 hrs. Absolute Alcohol (3) 1 hr. 3 hrs. 2 hrs. Xylene or Toluene (1) 1 hr. Xylene or Toluene (2) 1 hr. Benzene (1) 30 mins. Benzene (2) 1 hr. Chloroform ( I ) 2 hrs. Chloroform (2) 2 hrs. Chloroform (3) 2 hrs. Wax (1) 2 hrs. 3 hrs. 2 hrs. Wax (2) 3 hrs. 3 hrs. 2 hrs. TABLE 11-1. Sample Time Table for Automatic Processing of tissues 3-5 mm. thick Precautions with Automatic Processing The frequency with which fluids are changed depends on the number and sizes of the tissues processed. The presence of any odor in the clearing agent during final paraffin wax bath indicates that the paraffin wax needs to be changed. Dehydrating fluids should be changed frequently since dehydration is the most critical stage of tissue processing and inadequate dehydration is difficult to correct once the tissue is in paraffin. The first 100% ethanol bath should be discarded, and the others moved down, so that the final bath has fresh 100% ethanol after two complete processing runs of loads of at least three-quarters capacity. The clearing agent and the dilute ethanols should be changed at least once a week. To avoid spillage, fluid and wax containers must be filled to the appropriate level and correctly located in the machine. Wax accumulating on any surface or beaker leads must be removed and any spillage should be wiped away. Wax bath thermostats should be set at least 3 degrees above the melting point of the wax, and timing should be checked when loading the machine, especially if the machine is equipped with a delay mechanism. Due to the viscosity of molten paraffin wax, some form of gentle agitation is highly desirable. If the processor is to be run overnight it should be programmed to hold on the first ethanol bath and not finish until the next morning so the specimens do not sit in hot paraffin longer than the time indicated. If specimens are fresh they may incubate in formalin in the first stage on the machine. It is important to not keep the tissues in hot paraffin too long or else they become hard and brittle. Processed tissues can be stored in the cassettes at room temperature indefinitely. 3. Vacuum Embedding Vacuum embedding involves wax impregnation under negative atmospheric pressure inside an embedding oven. It reduces the time Fig 11 -1. Tissue processor with vacuum and fume control when tissues are subjected to high temperatures thus minimizing heat-induced tissue hardening. It facilitates complete removal of transition solvents, and prolongs the life of wax by reducing solvent contamination. Vacuum hastens the removal of air bubbles and clearing agent from the tissue block, thereby promoting a more rapid wax penetration of the tissue. This technique is particularly recommended for urgent biopsies, for delicate tissues such as lung, brain, connective tissues, decalcified bones, eyes, spleen and central nervous system. Vacuum infiltration requires a vacuum infiltrator or embedding oven, consisting of wax baths, fluid trap and vacuum gauge, to which a vacuum of up to 760 mm Hg is applied using a water or mechanical pump. Modern tissue processors are equipped to deliver vacuum, or vacuum and pressure, to all or some reagent stations during the processing cycle. Fig. 11-2. Vacuum embedding oven With vacuum embedding, the time required for complete impregnation is reduced by 25% -75% of the normal time required for tissue processing. The tissue is not over-exposed to heat; brittleness, shrinkage and hardening of tissues consequent to overheating is therefore prevented. The tissue can also be transferred after clearing to a heated bath of paraffin wax from which air can be evacuated. The vacuum embedding oven consists of a flat-bottomed heavy brass chamber covered with a heavy glass lid resting on a wide and thick rubber valve which produces an airtight seal when the chamber is being used. The vacuum chamber is enclosed in a thermostatically controlled water-jacket, usually maintained at a temperature of 2-4°C above the melting point of the wax. The degree of the vacuum should not exceed 500 mm. Hg. A stopcock is provided to prevent water from being sucked back into the trap bottle and vacuum chamber when the water or suction pump is closed. Embedding Procedure: After fixation and dehydration, proceed as follows: 1. Clear in two changes of xylene, for 1 hour each. 2. Place the tissue in molten wax, in vacuum chamber and make the oven airtight. Exhaust the air slowly by means of a vacuum pump or Venture suction pump until there is a negative pressure of 400 to 500 mm. mercury. 3. Leave for 15 minutes, then slowly readmit air until normal atmospheric pressure is reached. 4. 5. 6. 7. 8. Place the tissue in fresh wax. Repeat steps 3 and 4. Place the tissue into fresh wax. Repeat step 3 and leave for 30 to 45 minutes. Bring to normal atmospheric pressure and embed the tissue. NOTE: The exhaustion and readmission of air must be gradual or the specimen may be ruined. Of the three methods of paraffin wax impregnation, vacuum impregnation gives the fastest result. Total impregnation time, however, generally depends upon the nature and size of the tissues to be processed, and the type of cleari ng agents to be used. Larger and denser tissue blocks (e.g. bones, fibroids, brains) usually require longer periods and more frequent changes of wax. Benzene and xylene are easily removed from the tissues while chloroform and cedarwood oil are more difficult to remove and require more frequent wax changes. Addition of benzene may hasten displacement of cedarwood oil with less tissue shrinkage. Practical Considerations Since prolonged treatment in melted paraffin causes shrinkage and hardening of tissues, making cutting difficult, the tissue should not be left in the paraffin oven for more than 4 hours. The shorter the time in the hot oven with adequate paraffin impregnation and evaporation of clearing agent, the better it is for the tissue. Tissues become increasingly harder and more brittle as they are heated. Infiltration in overheated paraffin (above 60°C) will also produce shrinkage and hardening of tissues and destroy lymphoid tissues completely. To avoid this, the paraffin oven must be maintained at a temperature 2 to 5°C above the melting point of paraffin to be used for impregnation. Paraffin wax must be pure, i.e. free from dust, water droplets and other foreign matter. Fresh wax should be filtered before use in a wax oven at a temperature 2°C higher than its melting point. Wax that has been trimmed away from the impregnated tissue may be melted and filtered for future use, with a coarse filter paper, e.g. Green's No. 904. When wax has been reused, some amount of water inevitably is mixed with it. If excessive, this may impair the impregnating capacity of the medium and prevent formation of a good tissue block. Water must therefore be removed by heating the wax to 100 -105°C, thereby raising its melting point. Paraffin wax may be used only twice, after which, fresh wax must be utilized. When using an automatic tissue processing machine, wax usually becomes admixed with the clearing agent, especially in the first beaker; hence, water must be discarded. For fixed knife microtomes, a relatively hard wax with a higher melting point is recommended. Heavier microtome knives require harder paraffin wax than lighter ones. SUBSTITUTES FOR PARAFFIN WAX Paraplast is a mixture of highly purified paraffin and synthetic plastic polymers, with a melting point of 56-57°C. It is more elastic and resilient than paraffin wax thereby permitting large dense tissue blocks such as bones and brain to be cut easily with the same result as in double embedding. Blocks obtained are more uniform than with any other medium, with better ribboning of sections. Serial sections may be cut with ease, without cooling the tissue block, thereby preventing the formation of ice crystal artefacts. No deposit is left on the slide after staining, and no special processing schedule is required. It is soluble in common clearing agents and follows the same time schedule for paraffin impregnation, and does not tend to crack like other paraffin wax substitutes. Generally, Paraplast with a melting point of 56 to 58oC is recommended. During the winter, 54 to 56oC Paraplast may be used if the tissue is cut in a cool room. During the summer it may be necessary to use 60 to 63oC, although this is to be avoided if possible in order to not to "cook" the tissue. "Cooked" tissue does not section well or, if it does, it does not stain well and most details are destroyed. Embeddol is synthetic wax substitute similar to Paraplast with a melting point of 56-58°C. It is less brittle and less compressible than Paraplast. Bio/aid is a semisynthetic wax recommended for embedding eyes. Tissue Mat is a product of paraffin, containing rubber, with the same property as Paraplast. Ester Wax has a lower melting point (46-48°C), but it is harder than paraffin. It is not soluble in water, but is soluble in 95% Ethyl Alcohol and other clearing agents; hence, it can be used for impregnation without prior clearing of the tissue. Cellosolve (ethylene glycol monoethyl ether) or xylene may be used as clearing agents, if indicated. In such instances, removal of the clearing agent must be gradual; that is, the tissue must be placed in a solution containing equal proportion of clearing agent and ester wax for 3- 6 hours before finally transferring it to pure wax. Three to four changes of wax are required to ensure complete tissue impregnation. Sectioning of ester wax-impregnated tissues should be done on a heavy duty microtome (e.g. sliding or sledge type microtome) due to the relative hardness of the wax. Water Soluble Waxes are plastic polymers, mostly polyethylene glycols with melting points of 38-42°C or 45-56°C. Polymer waxes are incorporated in the majority of proprietary histological paraffin wax blends presently available to improve adhesion, hardness and plasticity. The most commonly used is Carbowax, a polyethylene glycol containing 18 or more carbon atoms, which appears solid at room temperature. It is soluble in and miscible with water; hence does not require dehydration and clearing of the tissue. The tissues are fixed, washed out and transferred directly into the melted Carbowax. Processing time is reduced with the special advantage that harmful effects produced by ordinary dehydrating agents are consequently avoided. It does not remove neutral fats and lipids which are soluble in reagents used for routine processing with paraffin, hence, allowing these substances to be demonstrated in thin sections. Tissues are not exposed to too much heat so that excessive hardening, shrinkage and brittleness of tissue is avoided; hence, making Carbowax technique suitable for many enzyme histochemical studies. Cytologic details are excellently preserved. For routine processing, four changes of Carbowax, one each in 70% and 90% and 2 times in I 00% concentration, at a temperature of 56°C are used, at 30 minutes, 45 minutes and 1 hour (with agitation), respectively. Specimens are then embedded in fresh Carbowax at 50°C and rapidly cooled in a refrigerator. Due to its hygroscopic nature, Carbowax is very easily dissolved in water. Hence care must be taken to avoid contact of the block with water or ice. Tissue sections are very difficult to float out and mount due to its extreme solubility in water, dehydrating and clearing agents. Adding soap to water or using 10% Polyethylene Glycol 900 in water will reduce tissue distortion and promote flattening and "floating out" of sections. Dimethyl sulphoxide (DMSO) added to proprietary blends of plastic polymer paraffin waxes reduces infiltration times and facilitates thin sectioning. DMSO scavenges residual transition solvent and probably alters tissue permeability by substituting for or removing bound water thus improving infiltration. Some individuals who handle DMSO-paraffin wax may experience an unpleasant and annoying oyster or garlic taste probably caused by DMSO metabolites. Possible health risks associated with the use of DMSO-paraffin wax are minimal if correct laboratory hygiene is observed. CELLOIDIN IMPREGNATION Celloidin (Collodion) is a purified form of nitrocellulose soluble in many solvents, suitable for specimens with large hollow cavities which tend to collapse, for hard and dense tissues such as bones and teeth and for large tissue sections of the whole embryo. It is supplied in thin (2%), medium (4%) or thick (8%) solutions of cellulose dissolved in equal parts of ether and alcohol. This is used mainly for preparing soft tissue sections of mixed consistency such as eyes and brain. No heat is required, and the resultant block has a rubbery consistency which gives good support to the tissues. Disadvantages include inability to cut thin sections, storage of blocks in alcohol and speed of technique (which can take several weeks or months). Advantages: 1. It permits cutting of tissue sections which are thicker than in paraffin wax, and is recommended for processing of neurological tissues. 2. Its rubbery consistency allows tissue blocks that are either very hard or of varying consistency, to be cut without undue distortion. 3. Dense tissues which are hard to infiltrate (e.g. bones and brain) and specimens which tend to collapse easily due to air spaces (e.g. eyes) are supported better, thereby avoiding the crumbling of tissues during sectioning. When eye sections are embedded by the paraffin method, the retina may be detached from the harder tissues (e.g. sclera and choroid) that encircle it. The cedarwood oil used in the dry celloidin technique helps to soften the brittle layers. 4. I t does not require heat during processing; hence, producing minimum shrinkage and tissue distortion especially for cutting large bone sections. It is, therefore, recommended in cases when minimum shrinkage is required and wh en frozen section technique cannot be done. Disadvantages: 1. Celloidin impregnation is very slow (lasting for several days or weeks). 2. Very thin sections (less than I 0 µ) are difficult to cut. 3. Serial sections are difficult to prepare. 4. Vapor of the ether solvent is very flammable; hence, it should never be used near an open flame. 5. Photomicrographs are difficult to obtain. 6. It is very volatile and therefore must be kept in bottles with groundglass stoppers to prevent evaporation. Two methods are used for celloidin impregnation of tissue: Wet Celloidin Method - is recommended for bones, teeth, large brain sections and whole organs. After the usual fixation and dehydration of the tissue, it is placed in equal parts of ether and alcohol for 12-24 hours. The tissue is then placed in thin celloidin (2-4%) for 5-7 days, transferred to medium celloidin (4-6%) for another 5-7 days, drained off and poured with thick celloidin (8-12%) until the specimen has become impregnated, usually between 3-5 days. The specimen is removed from the celloidin, transferred to an embedding medium containing freshly poured thick celloidin and kept in a tightly covered jar or dessicator in order to evaporate the alcohol-ether solvent. The dessicator top is removed for a few seconds, time and again, to admit fresh air and harden the tissue block. Evaporation must be gradual to achieve a consistent, uniform degree of hardness throughout the block and prevent the formation of air bubbles. When the ball of the finger leaves no mark on the surface of the tissue block, evaporation and consequently, embedding, is considered to be complete. The tissue block is then stored in 70-80% alcohol until ready for cutting. This is done to avoid dehydration and shrinkage of tissues. Dry Celloidin Method is preferred for processing of whole eye sections. The principle and procedure of this method is similar to wet celloidin method, except that 70% alcohol is not used for storage before cutting. Instead, Gilson's mixture, made up of equal parts of chloroform and cedarwood oil, is added to the celloidin block before hardening, to make the tissue transparent. The dry method does not make use of alcohol due to the presence of cedarwood oil in the block. Nitrocellulose Low Viscosity Nitrocellulose (L.V.N.) is another form of celloidin soluble in equal concentration of ether and alcohol, with a lower viscosity, allowing it to be used in higher concentrations and still penetrate tissues rapidly. Because of this, many workers prefer L.V.N. to the ordinary celloidin for impregnation and embedding. It forms a harder tissue block and makes cutting of thinner sections possible. The tendency of tissues to crack may be prevented by adding plasticizers (e.g. oleum ricini or castor oil) when embedding chrome-mordanted tissues. Low viscosity nitrocellulose is more explosive than celloidin and should therefore be handled with care. When dry, striking or dropping the container will cause the substance to explode. It is usually marketed while wet with alcohol. The container must be kept tightly covered and protected from sunlight to avoid evaporation of alcohol. When no longer needed for future use, the nitrocellulose should be carefully destroyed, since the material becomes increasingly dangerous as the alcohol continues to evaporate . GELATIN IMPREGNATION Gelatin impregnation is rarely used except when dehydration is to be avoided and when tissues are to be subjected to histochemical and enzyme studies. It is used as an embedding medium for delicate specimens and frozen tissue sections because it prevents fragmentation of tough and friable tissues when frozen sections are cut. It is water-soluble, and does not require dehydration and clearing, although fixatives (such as 10% formalin) should still be washed out by running water whenever indicated. It has a low melting point and does not cause over-hardening of tissues by heating. After the fixative has been completely washed out, the tissue is placed in 10% gelatin with 1% phenol for 24 hours, transferred to 20% gelatin with 1% phenol for the next 12 hours, and finally to another fresh solution of 20% gelatin with 1% phenol which is then allowed to cool in a refrigerator until impregnation and embedding are completed. Gelatin-embedded tissues are then transferred to l 0% formalin for 12-24 hours in order to harden the tissue. Tissues should not be more than 2-3 mm. thick since gelatin-embedded specimens are harder to freeze than non-impregnated tissues. The 1 % phenol serves to prevent the growth of molds. Excess gelatin may be removed by floating the sections oh to paper and trimming them with scissors. The volume of the impregnating medium should be at least 25 times the volume of the tissue. EMBEDDING After impregnation, the tissue is placed into a mold containing the embedding medium and this medium is allowed to solidify. Ideally the embedding medium should match the tissue type in strength and hardness. If the embedding medium is too soft for the material, the tissue will not be supported and sections will be torn or shredded. If the medium is too hard for the tissue, sections will be brittle and will shatter. To infiltrate the tissues with supporting embedding medium, tissues must be free of all water (since usually embedding medium is not miscible with water). Paraffin embedded tissues are arranged at the bottom of the mold together with their proper labels and immersed in melted paraffin at a temperature between 5-10°C above its melting point and then cooled rapidly in a refrigerator at -5°C or immersed in cold water to solidify. This will allow hardening of tissues, giving them a firmer consistency and better support, thereby facilitating the cutting of sections. The process by which a tissue is arranged in precise positions in the mold during embedding, on the microtome before cutting, and on the slide before staining, is known as Orientation. Generally speaking, the surface of the section to be cut should be placed parallel to the bottom of the mold in which it is oriented. Several types of Blocking-out Molds may be used: 1. Leuckhart’s Embedding Mold - consists of two L-shaped strips of heavy brass or metal arranged on a flat metal plate and which can be moved to adjust the size of the mold to the size of the specimen . Blocks produced are even, with parallel sides, and with a fairly shaped initial setting of the wax. The mold is adjustable to give a wide variety of sizes to fit the size of the tissue block for casting. It is recommended for routine use, although, too slow and cumbersome for use in a busy laboratory. 2. Compound Embedding Unit is made up of a series of interlocking plates resting on a flat metal base, forming several compartments. It has the advantage of embedding more specimens at a time, thereby reducing the time needed for blocking. 3. Plastic Embedding Rings and Base Mold -consist of a special stainless steel base mold fitted with a plastic embedding ring, which later serves as the block holder during cutting. One model, the so-called Tissue Tek, is equipped with a warm plate to manage the impregnated specimen, and a cold plate at -5°C for rapid solidification of the block. It consists of a white plastic cassette mold with detachable, perforated stainless steel hinge and Snap-On lid, used to hold the tissue specimen through-out fixation, dehydration, clearing and wax impregnation. With the Tissue Tek system, the specimen is placed on the base mold, the plastic embedding ring is placed in position, filled up with wax, and then placed on a small cool area to allow the wax in the base of the mold to semi-harden. This will allow easy orientation of the block. Once the tissue has been properly oriented, the base of the cassette is placed on top and together, they are placed on the cold plate so that the paraffin wax can cool and harden quickly. After the paraffin wax has solidified (usually 5 minutes), the block is taken out together with the embedding ring and is immediately ready for cutting without having to undergo trimming or mounting, thereby saving time and effort. The advantages of Tissue Tek include ease of use, less paraffin wax needed, faster embedding, firmly attached tissue and holder, and permanent identification. It produces easier orientation when resectioning of tissue is required, and blocks can be filed immediately after sectioning. 4. Disposable Embedding Molds a. Peel-Away disposable thin plastic embedding molds, available in 3 different sizes, are simply peeled off one at a time, as soon as the wax has solidified, giving perfect even block without trimming. It may be placed directly in the chuck or block holder of the microtome. b. Plastic Ice Trays -such as those used in ordinary refrigerators may be recommended for busy routine laboratories. Each compartment may be utilized for embedding one tissue block, which may then be removed by bending the plastic tray once the wax has solidified or by smearing the inner mold with glycerin or liquid paraffin before embedding. c. Paper Boats are normally utilized for embedding celloidin blocks but are equally useful for paraffin wax blocks. They have the advantage of being cheap and easy to make. They provide easy and accurate identification of specimen, thereby avoiding confusion and interchange of tissue blocks. Rapid embedding of small or large volume of individual specimen is possible, since paper molds can be made to suit any size of tissue. To mark the position of small tissues in the paraffin block, a mark such as an "X" is drawn with soft lead pencil on the inner surface of the bottom of the boat. This will attach and be visible on the wax block when solidified and removed from the paper boat. Embedding molds should bear the case number, and other identification data of the tissue block within. Once tissues have been embedded, they may be stored in a cool place indefinitely until they are cut. The choice of embedding mold will depend on the type of chuck in the microtome you will use to section the tissue. Stainless steel, ceramic, paper, plastic, and aluminum foil molds can be used. The basic method is the same for each. 1. Open cassette to view tissue sample and choose a mold that best corresponds to the size of the tissue. A margin of at least 2 mm of paraffin surrounding all sides of the tissue gives best cutting support. Discard cassette lid. 2. Put small amount of molten paraffin in mold, dispensing from paraffin reservoir. 3. Using warm forceps, transfer tissue into mold, placing cut side down, as it was placed in the cassette. 4. When the tissue is in the desired orientation, add the labeled tissue cassette on top of the mold as a backing. Press firmly. 5. Hot paraffin is added to the mold from the paraffin dispenser. Be sure there is enough paraffin to cover the face of the plastic cassette. 6. Cool the top surface of the Paraplast by blowing gently on it. Tissues at this stage are very brittle and should be handled with care. If necessary, fill cassette with paraffin while cooling, keeping the mold full until solid. 7. Cool thoroughly in cold running tap water. If you use ice water for the final cooling, you may split the block owing to too rapid shrinkage. Paraplast naturally splits in the line of least resistance-right through the tissue 8. Paraffin should solidify in 30 minutes. When the wax is completely cooled and hardened (30 minutes) the paraffin block can be easily popped out of the mold; the wax blocks should not stick. If the wax cracks or the tissues are not aligned well, simply melt them again and start over. 9. If you use plastic cups, the Paraplast block can be removed as soon as it is cooled. The stainless steel mold should slip off easily when cool and can be used again. It is important to work quickly while transferring specimens or wax from oven because wax hardens quickly. Always remember to put wax container back into oven immediately and close oven door between transfers. Figure 11-3. Orienting and embedding on the block Orientation of tissues in the Paraplast block is important for tissues such as an artery or fallopian tube so that they can be properly placed in a predetermined plane, such as cross sections. Also, trimming is excessively difficult in a block embedded with two or more tissues if they are not carefully lined up before the Paraplast is cooled. Celloidin or Nitrocellulose Embedding Method used to be recommended for embedding hard tissues such as bones and teeth, and for large sections of whole organs like the eye, since the delicate layers of the eyeball are difficult to keep i ntact when other media are used. Tissues are em bedded in shallow tins of enamel pans which are covered by sheets of weighted glass. Bell jars can be used to control the rate or evaporation of the sol vent. The use of celloidin is discouraged now because of the special requirements needed for processing and the limited use of these types of sections in neuropathology. Double-Embedding is the process by which tissues are first embedded or fully infiltrated with a supporting medium such as agar or nitrocellulose, then infiltrated a second time with paraffin wax in which they are subsequently embedded. This is used to facilitate cutting of large blocks of dense firm tissues like the brain. They are also recommended for making small sections of celloidin blocks. A shortcoming of using agar as the pre-embedding media is that certain tissues shrink during the embedding process, and the agar-based pre-embedding media limits tissue expansion during slide mounting, resulting in difficulties with the tissue sample adhering to the microscope slide. The availability of paraffin waxes containing different types of resins has made this technique obsolete. PLASTIC (RESIN) EMBEDDING The introduction of plastic resin embedding media has provided superior results for light microscopic studies, particularly in hard tissues such as undecalcified bone and for high resolution light microscopy of tissue sections thinner than the usual 4-6 µm, such as renal biopsies a n d bone marrow biopsies. Plastics are classified into epoxy, polyester, or acrylic, based on their chemical composition. Epoxy embedding plastics are made up of a carefully balanced mixture of epoxy plastic, catalysts and accelerators. Three types of epoxy plastics are used in microscopy, i.e., those based on either bisphenol A (Araldite), or glycerol (Epon), or cyclohexene dioxide (Spurr). Infiltration by Araldite is slow, partly because the epoxy plastic itself is a large molecule. The glycerol-based epoxy plastics (Epon) have a lower viscosity but are often sold as mixtures of isomers. Cyclohexene dioxide-based plastics (Spurr) can be obtained pure, have very low viscosity, and infiltrate fastest. Spurr’s Resin is a Low Viscosity mixture which provides rapid infiltration of tissues. It's easy to prepare and mixes rapidly. This resin is compatible with ethanol so no change to propylene oxide is needed prior to infiltration. Polymerization at 60°C is recommended. Epoxy plastics have several disadvantages. They are hydrophobic and subsequent oxidation by peroxide to correct this may produce tissue damage. Epoxide groups may reduce antigenicity of embedded tissue, and may compromise the result of immunohistochemical staining. More importantly, epoxy resins may cause sensitization if absorbed by skin or inhalation. The components of many epoxy plastics are toxic and one of its components, vinyl cyclohexane dioxide (VCD) is known to be carcinogenic. For protection, gloves should always be worn when handling these plastics, and adequate facilities including an operational fume hood must be provided to remove the toxic vapors and properly dispose of toxic waste. Polyester plastics were originally introduced for electron microscopy in the mid- 1950s, but have been superseded by more superior epoxides, and are now seldom used. Acrylic plastics are made up of esters of acrylic or methacrylic acid, and are used extensively for light microscopy. Polyglycol methacrylate (GMA) has proved to be a popular embedding medium for light microscopy because it is extremely hydrophilic, allowing many staining methods to be applied, yet tough enough when dehydrated to section well on most microtomes. The polar water soluble, 2-hydroxyethyl methacrylate, commonly known as "glycol methacrylate", or GMA, has found an increasing number of applications for the embedding of biological tissue for transmission electron microscopy (TEM), for the preservation and observation of fine structure not previously subjected to solvent dehydration. GMA forms only non-crosslinked straight chains on polymerization and therefore requires no hardener. GMA and specifically low acid GMA offers a number of advantages over other systems: • Dehydration of tissues can be made directly in aqueous dilutions of GMA or optionally in organic solvents. • GMA does not need to be water-free and indeed it works best with at least some water present. • Infiltration of tissue with monomer can be performed at room temperature or lower. • Polymerization of GMA can be performed at ambient temperature of 0°C with UV radiation to 60°C in an oven. • Thin sections of polymerized GMA can be cut with glass or diamond knives. • Sections from Low Acid GMA, unlike ordinary technical grade GMA, resist the uptake of stain, thereby reducing greatly the occurrence of non-specific background staining. • Enzyme digestion, a variety of stains and immunological localizations may be performed on thick sections of GMA without removal of the plastic. Benzoyl peroxide is added to the plastic as a catalyst that decomposes to form phenyl radicals acting as an active site for the polymerization of acrylics. Unlike epoxy plastics, the viscosity of acrylic plastic is low so that short infiltration times are possible, although the size and nature of tissue, along with processing and embedding temperature will affect the times required for infiltration and embedding. Radicals can be produced spontaneously by heat or light, so that acrylic plastics and their monomers should be stored in dark bottles in a cool place to prevent premature polymerization. Acrylic plastics based on methyl methacrylate (MMA) are also widely used because of its hardness as the ideal embedding medium for undecalcified bone and is widely used for bone histomorphometry and bone marrow hematopathology. Compared to water-soluble methacrylates (e.g., glycol methacrylate, GMA), MMA offers a variety of advantages. MMA penetrates tissues better than GMA and the histological quality of bone sections is generally higher in MMA-embedded bone samples compared to GMA-embedded specimens. GMA forms crosslinks during polymerization of the plastic so that removal of the resin from tissue sections is not possible for GMA-embedded material. MMA, on the other hand, can easily and completely be removed from tissue sections. This results in superior staining characteristics and excellent morphological detail. However, conventional MMA embedding causes almost complete loss of enzyme activity and protein antigenicity in the tissues, and therefore precludes the use of histochemical and immunohistological methods. In general, it is preferable to use acrylic plastic sections when high resolution light microscopy is required, because of their ease of handling and the quality of staining achieved. However, all acrylic hydrophilic media (including glycol methacrylate) are insoluble so that all staining occurs with the plastic in situ. Because of this, the embedding medium itself may become stained, or the matrix may act as a physical barrier to particular molecules causing problems during imm unohistochemical staining. The alternative use of h ydrophobic methyl methacrylate permits the plastic to be dissolved, and for certain techniques, this may be a very useful property. PRACTICAL CONSIDERATIONS: Specimen should only be processed under an operational fume hood. Processing is best achieved if the specimen is agitated continuously on a roller mixer. Small aliquots of benzoyl peroxide should be dried carefully away from direct heat and sunlight as it is potentially explosive. It is important that no water is present before dissolving the catalyst (2 minutes) in the infiltrating solution. It m ust be completely dissolved in the infiltrating solution, and this may take up to 30 minutes. The acrylic plastic mixes are best prepared only in the quantity required, preferably using a large glass vial. It is advisable to measure the quantities volume by weight. Any waste solutions containing plastic components must be handled and discarded in accordance with local and legal requirements. REFERENCES Anderson G. Bancroft J. (2002) Tissue processing and microtomy. In: Bancroft, J.D., Gamble, M. Theory and Practice of Histological Techniques. 5'h Ed., Churchill Livingstone, London, 100. Atwood K, Farmilo AI, Stead Rh, Boenisch T. (2003) Fixation & tissue processing. From: handbook for immunochemical staining methods. 3rd ed. Carpinteria, CA: DAKO. p. 18–22. Baker JR. (1958) Principles of Microbiological Microtechnique. Mehuen & Co., Ltd., London. Baker FJ. (1962) Progress in Medical Laboratory Technology, Vol. 1, Butterworths and Company, London. Baker FJ. (1962) Progress in Medical Laboratory Technology, Vol. 2, Butterworths, London. Baker FJ, Silverton RE, Luckcock ED. (1966) Introduction to Medical Laboratory Technology, Butterworths, London. Baker, R.D. (1967) Postmortem Examination, Specific Methods and Procedures. W.B. Saunders, London and Philadelphia. Bancroft J.D., Cook H.C. (1994) Manual of Histological Techniques and their Diagnostic Application. Churchill Livingstone, Edinburgh. Brown, C.C. (1969) Primer of Histopathologic Technique. Appleton-Century-Crafts, New York. Brown RW. (2009) Histologic preparations: common problems and their solutions. Northfield, IL: College of American Pathologists. Carson FL, Hladik, C. (2009) Histotechnology: a self-instructional text. 3rd ed., Chicago: ASCP Press. Clark G, ed.: (1960) Staining Procedures Used by the Biological Stain Commission, 3rd ed. William & Wilkins, Baltimore. Culling, CFA. (1974) Handbook of Histopathological and Histochemical Techniques, 3rd ed. Butterworths, Massachusetts. Dapson RW. (2007) Glyoxal fixation: how it works and why it only occasionally needs antigen retrieval. Biotechnic & Histochemistry 82(3): 161-166. Drury RAB, Wallington EA. (1967) Carleton s Histological Technique, 4th ed. University Press, Oxford. Drury R.A.B., Wallington E.A. (1980) Carlton s Histological Technique. 5th ed. Oxford University Press, London. Fox, CH, Johnson FB, Whiting J, Roller RP. (1985) Formaldehyde fixation. J Histochem Cytochem 33: 845-853. Henry JB. (1991) Clinical diagnosis and L aboratory methods. 18th ed. Philadelphia: W.B. Saunders p. 621–622. Horobin RW, Tomlinson A. (1976). The influence of the embedding medium when staining sections for electron microscopy: the penetration of stains into plastic section. .Journal of Microscopy 108: 6978. Kiernan JA. (2009) Histological and Histochemical Methods. Theory and Practice. 4th ed. chapters 2-4, pp 12-73. Bloxham, UK: Scion. Lillie RD, Fullmer, HM. (1976) Histopathologic Technic and Practical Histochemistry. 4th ed. New York: McGraw hill Book Co., New York. Lab-Tek Products, Division of Miles Laboratories Inc., Naperville, Ill. 60540. Raphael, S.S. (1983) Processing tissues for histotechnology. In: Raphael SS et al, eds. Lynch s Medical Laboratory Technology, 4t11 ed. Chapt 32, W.B. Saunders Co., Philadelphia, 759. Pearse AGE. (1980) Histochemistry: Theoretical and Applied. 4th ed. Vol. 1. Edinburgh: ChurchillLivingstone. Sheehan DC, Hrapchak BB, Eds. (1980) Theory and Practice of Histotechnology, 2nd ed. CV Mosby Co., St. Louis, MO. CHAPTER 12 MICROTOMY The process by which processed tissue, most commonly a paraffin embedded tissue, is trimmed and cut into uniformly thin slices or "sections" to facilitate studies under the microscope is known as Microtomy. The basic instrument used is a microtome that is capable of cutting a section at a predetermined thickness by sliding the block into a cutting tool, usually a steel knife, glass or diamond blade, which is fixed and attached to the machine. The microtome consists of three essential parts, namely: 1. Block Holder - where the tissue is held in position. 2. Knife Carrier and Knife - for actual cutting of tissue sections. 3. Pawl, Ratchet Feed Wheel and Adjustment Screws - to line up the tissue block in proper position with the knife, adjusting the proper thickness of the tissue for successive sections. Whatever the type of microtome is used, the principle remains essentially the same, that is, a spring-balanced teeth or pawl is brought into contact with, and turns a ratchet feed wheel connected to a micrometer screw, which is in turn rotated, moving the tissue block at a predetermined distance towards the knife for cutting sections at uniform thickness. There are five (5) kinds of microtomes: 1. Rocking microtome – for cutting serial sections of large blocks of paraffin embedded tissues. 2. Rotary microtome - for cutting paraffin embedded sections. 3. Sliding microtome - for cutting celloidin embedded sections. 4. Freezing microtome -for cutting unembedded frozen sections. 5. Cryostat or cold microtome – for cutting frozen sections 6. Ultrathin microtome - for cutting sections for Electron Microscopy. 1. Rocking (Cambridge) Microtome This was invented by Paldwell Trefall in 1881, the simplest among the different types of microtomes. This consists of a heavy base and two arms the lower arm resting on pivots and a supporting column, and attached to the micrometer screw, at the base of which is found the ratchet wheel with feed mechanism. The upper arm, carrying the block holder on one end by means of a screw, is connected to a lever by a piece of nylon thread. Fig. 12-1. Rocking Microtome When the lever is pulled forward, the pawl is brought in contact with the ratchet wheel to which the millhead micrometer screw is attached. The ratchet wheel is turned, rotating the micrometer screw. The lower arm is elevated, which in turn raises the upper arm at its fulcrum, thereby carrying the chuck or block holder forward, towards the knife. As the pressure on the operating handle or lever is released, the tension on the spring causes the upper arm to return to its normal position; in an arc of a circle. A section is thereby cut as the tissue passes to the knife edge in a slightly curved plane, in 10-12 u thickness. The Cambridge rocking microtome, available in two sizes, has been used to cut small and large blocks of paraffin tissues. It is theoretically not recommended for serial sections since tissues are cut in slightly curved planes. It is not currently favored by most laboratories because of the restrictions in size of tissue block that can be cut, and the difficulty of reorienting the block. B. Rotary (Minot) Microtome This was invented by Minot in 1885-86 to cut paraffin embedded tissues, and is currently the most common type used for both routine and research laboratories, especially for sectioning paraffin-embedded tissues. Electrically driven rotary microtomes are also now available and can be ideally used to produce ribbons for serial sections. Fig. 12-2. Rotary Microtome In the rotary microtome, the device operates with a staged rotary action such that the actual cutting is part of the rotary motion. In a rotary microtome, the knife is fixed in a horizontal position and the principle of section cutting is shown in the image above. Although the flywheel in many microtomes can be operated manually, they are generally automated or semi-automated. Typically, sections are cut between 3 and 5 µm using paraffin wax for diagnostic histology although thinner sections can be attained if samples are embedded in synthetic resin. It is different from the rocking microtome in that the knife and the block holder are brought together by upward and vertical motions, cutting sections in a perfectly flat plane, thereby allowing excellent serial sections to be cut. It is heavier and more stable than the rocking microtome, is more complex in design and construction, and is therefore more expensive. It may be used for cutting large blocks of tissues although results are better when the sliding microtome is used. The knife is placed in a blade-up position and is therefore relatively dangerous. Both manual and electrically driven models are now available for cutting ultrathin sections and for cryostat use. A heavier knife is used, so there is less vibration. The cutting angle (tilt) of knife is adjustable, so it can cut harder tissue. It can cut celloidin-embedded sections by using a special holder to set the knife obliquely. 3. Sliding microtome This was developed by Adams in 1789. There are two types of this microtome. One model, the Base-Sledge Microtome, consists of two movable pillars holding the adjustable knife clamps, allowing the knife to be set at an angle for cutting celloidin sections. The chuck or block holder is set on a heavy metal base which can be moved backwards and forwards under the knife. The Base-Sledge microtome is favored in laboratories where very hard tissue or large blocks are usually sectioned. Such a machine is suited for sectioning specimens embedded in all forms of media, especially for cutting sections from tough tissue blocks which may offer great resistance to the knife. Larger sections are more easily cut with the knife, set at an angle due to less resistance offered by the block. It was originally designed for cutting sections of very large blocks (whole brain). Sections are cut in a perfectly flat plane, thereby making excellent serial tissue sections. It is comparatively heavier and more stable than the ordinary sliding microtome. The angle of the knife is adjustable. The knife used is long (24 cm), hence it requires less honing. The knife holding clamps are adjustable and allow the tilt and the angle (slant) of the knife to be easily set. Modern models of heavy duty base sledge microtomes are electrically driven and are ideal for resin-embedded decalcified bone. The second type, the Standard Sliding microtome, is different from the base sledge microtome because with this instrument, the block remains stationary while the knife is moved backward and forward during the process of sectioning. It was developed mainly for cutting celloidin embedded tissue blocks and is inherently more dangerous because of the movable knife, which makes it difficult to attach knife guards. Fig. 12-3. Sliding Microtome In both of these machines, the knife can be set obliquely for celloidin sections or straight for large refractory paraffin blocks, cutting both large and small tissues with ease; it is especially recommended for cutting extremely hard and rough tissue blocks. It is the most dangerous type of microtome due to the movable exposed knife. A slow but very steady motion is therefore required to manipulate the instrument. D. Freezing Microtome Fig. 12-4. Freezing Microtome This was invented by Queckett in 1848. The stage for block holder is hollow and perforated around its perimeter, attached to a reinforced flexible lead pipe thru which carbon dioxide passes from a cylinder. A simple lever operated valve allows the release of rapid, intermittent bursts of carbon dioxide which will freeze the block holder and the tissue evenly. A second cooling device for lowering the temperature of the knife is also incorporated in most machines to facilitate sectioning. The knife holder is attached to a lever which is in turn connected to the pawl. When the operating handle is moved back, the knife is moved back to its original position, away from the block. The lever, is in turn, moved causing the pawl to get in contact with the ratchet feed wheel and thereby turn the micrometer screw. The block holder is then raised towards the knife at a predetermined thickness. By pulling the operating handle forward, a section is cut as the knife edge slices thru the raised tissue block. The microtome is firmly clamped on to the edge of the bench for use, or mounted on especially constructed shelf, with C02 cylinder below. It is used to cut undehydrated thin to semi-thin sections of fresh, frozen tissues, especially in instances when rapid diagnosis is required, when histological demonstration of fat is needed, when certain neurological structures are to be studied, and when sensitive tissue constituents to be studied are damaged or destroyed by heat. Although other microtomes can be modified for cutting frozen section, this type will give the best results and is used almost universally. The freezing microtome is equipped with a stage upon which tissue can be quickly frozen using either liquid carbon dioxide, from a cylinder, or a low temperature recirculating coolant. The cutting action of the freezing microtome differs from those described previously as in this case the knife is moved whilst the tissue block remains static, same as sliding microtome. E. The Cryostat or Cold Microtome Fig. 12-5. Cryostat The Cryostat is a refrigerated apparatus used for freezing the tissue into the block holder to the correct degree of hardness that allows for easier and faster sectioning. It consists of a microtome, usually a rotary microtome, kept inside a cold chamber which has been maintained at a temperature between -5° to -30°C (average is -20°C) by an adjustable thermostat, capable of freezing fresh tissues within 2-3 minutes, and cutting sections of 4 µ with ease. All the controls in the microtome are operated from outside the refrigerated cabinet. The cryostat provides a means of preparing thin sections of fresh frozen tissues especially for fluorescent antibody staining techniques or histochemical enzyme studies. It is most commonly used for rapid preparation of urgent tissue biopsies for intraoperative diagnosis. It is often housed in the frozen section room close to the operating room to allow direct consultation between surgeon and pathologist. Sections are usually transferred directly from the microtome knife to a slide or cover glass, all of which are maintained at a low temperature. E. Ultrathin microtome Fig. 12-6. Ultrathin Microtome An ultrathin microtome equipped with a glass or gem grade diamond knife is used to cut very thin sections (typically 60 to 100 nanometer) of tissue embedded in epoxy resin. Sections are stained with an aqueous solution of an appropriate heavy metal salt and examined with a transmission electron microscope (TEM). The ultrathin microtome is also used with its glass knife or an industrial grade diamond knife to cut semi-thin sections prior to thin sectioning. These semi-thin sections are generally 0.5 to 1 µm thick and are mounted on a glass slide and stained to locate areas of interest under a light microscope prior to thin sectioning for the TEM. Thin sectioning for the TEM is often done with a gem quality diamond knife. CARE OF THE MICROTOME After sectioning, all the accumulated paraffin and small pieces of tissues must be brushed away with a soft brush and not allowed to stay in the microtome, since this may later interfere with the cutting of tissue blocks. After carefully drying the machine and knife holder, the parts should be wiped with xylol. Prolonged and continuous application of the painted parts with xylene should, however, be avoided since this reagent is capable of removing the paint. Movable portions should be oiled thoroughly to prevent rusting The microtome must always be covered when not in use, to prevent accumulation of dust and other dirt which may later on interfere with the normal sectioning of tissues. The microtome should be placed on a stable bench, away from air drafts, doorways and passing staff. Any air movement from air conditioners or other causes can make section handling very difficult. Always remove the knife or blade before cleaning. The knife holder can easily be removed to facilitate access for cleaning. No fluid must enter the inside of the instrument during cleaning. When cleaning the blade avoid dragging anything along the cutting edge. Even cellulose fibers can cause damage to the blade. Have the instrument inspected at least once a year by a qualified service technician. Safety Measures: It is very important that staff are not distracted when using the microtome because of the risks of injury from extremely sharp blades. It is preferable to have non-slip flooring in the vicinity of microtomes because, inevitably, wax fragments will find their way onto the floor where they can produce a slippery surface. Use forceps or brush instead of fingers to pick up sections or wax fragments from blade or block face. Use hand wheel lock when changing blocks. The knife or blade should be removed from the microtome when the instrument is left unattended or when cleaning the instrument. MICROTOME KNIVES Trimming and section-cutting are done with a microtome knife, which is available in three basic types or shapes: 1. Plane-Concave Knife (usually 25 mm. in length) - One side of the knife is flat while the other is concave. Less concave sides are recommended for cutting celloidin-embedded tissue blocks on a sliding microtome. More concave sides are used to cut paraffin sections on base-sledge, rotary or rocking microtome. 2. Biconcave Knife (usually 120 mm. in length) - with both sides concave, recommended for cutting paraffin - embedded sections on a rotary microtome. 3. Plane-Wedge Knife (usually 100 mm. in length) have both sides straight, recommended for frozen sections or for cutting extremely hard and tough specimens embedded in paraffin blocks, using a base sledge type or sliding microtome. Plane-wedge and plane-concave knives are usually provided with backs, to maintain the correct bevel angle throughout honing. Detachable handles may be attached to the knife during sharpening. There is a cutting facet (bevel) found on the tapered edge of all knives, the sides of which are more acutely inclined towards each other than the side proper, forming the actual cutting edge of all knives. The angle formed between the cutting edges is known as the "Bevel Angle", normally about 27° to 32°. Such angle is maintained for each knife by means of a slide-on back, a spring-loaded semi-circular metal sheet slipped on to the knife with one or more plane surfaces (plane-wedge or plane-concave) to hold the cutting edge at a constant, correct angle during the process of honing and stropping. Each knife should have its own corresponding back which should not be interchanged with another, to keep the bevel angle. A good cutting edge should be made of good quality steel. Too soft cutting edges are likely to become dull easily, while too hard edges are likely to produce nicks or jagged edges and irregularities on the knife edge, thereby producing tears or striation on the tissue sections during cutting. A good cutting edge must be able to cut good sections from a paraffin wax block about 2-3 microns thick, without any serration noted on examination. Safety razor blades may be used for partially calcified materials, paraffin and frozen sections. They are readily replaced when dull, and produce similarly good tissue sections as those cut with microtome knives. They are, however, unsatisfactory for sections less than 10 µ. Theoretically, the perfect and optimum cutting angle is obtained when the sides of the wedge knife are inclined at an angle of about 15°, causing maximum penetration of the tissues and minimizing distortion. To prevent uneven sections, or alternate thin and thick sections, the knife should be inclined with a 5-10° clearance angle from the cutting plane so that the cutting facet will not compress the block during the process of cutting. The cutting edge must be thinner than the section being cut. A good cutting edge must be sharp enough to cut good sections from a paraffin wax block at 4 µ thick without causing serrations. The knife or blade should be removed from the microtome when the instrument is left unattended or when cleaning the instrument. This is best done by unclamping the blade, then using the blade ejector on the left side of the guard to start moving the blade laterally out of the clamp. It can then be grasped with forceps (not fingers) and safely removed. Used blades should be disposed of appropriately in a “sharps” container or into the “used blades” slot in the base of the blade dispenser. Never place a knife or blade on the bench or in a box with the cutting edge facing up. HONING AND STROPPING Badly nicked knives with blunted ends have to undergo sharpening in order to ensure optimum sectioning of tissue blocks and prevent gross irregularities on the tissue sections. Jagged edges, if not corrected, will produce tears or striations in tissue sections. Sharpening of the knife involves two stages: Honing (Hard Sharpening) Honing involves the removal of gross nicks on the knife edge (Coarse Honing) to remove blemishes, and grinding the cutting edge of the knife on a stone (Honing Proper) to acquire an even edge. The degree of sharpness is proportional to the fineness of the abrasive used in sharpening. This procedure makes use of a hone, a natural sharpening stone or hard grinding surface (carborundum), which serves to remove nicks and irregularities on the knife edges. Several types of hones may be used: 1 Belgium Yellow - for manual sharpening when cutting edge has been rendered blunt or nicked. This type usually gives the best result. 2. Arkansas - gives more polishing effect than the Belgium Yellow. 3. Fine carborundum - is much coarser than the first two types and is used only for badly nicked knives followed by either one of the first two knife sharpeners. The surface of the hone is wiped clean with a soft cloth moistened with xylene in order to remove the scattered small particles of stones and metal. It is then covered with a thin film of Mineral and Clove Oil, Xylene, Liquid Paraffin or Soapy Water for lubrication. The knife is fitted to its corresponding back, placed on one end of the hone, and with the cutting knife edge first, the "heel" (handle end) is drawn obliquely or diagonally towards the operator on the stone until the "toe" (head portion) is reached. The knife is then turned over, and the other surface is again drawn forward, EDGE FIRST, with a HEEL TO TOE direction. Hone is placed on non-skid surface. A damp cloth may be used-to prevent movement of the hone. Light lubricating oil or soapy water is used for lubrication. . Fig. 12-7. Honing technique The knife complete with handle and backing sheath is laid on the Hone with the cutting edge facing away from the operator and the heel roughly at the center of the nearest end of hone. The knife is held with thumb on the back and forefinger on the front surface. The knife is pushed forward diagonally from heel to toe to the other end of the hone, turned over on its back and moved across the hone until the heel is in the center with the cutting edge leading and then brought back diagonally. It is then turned across the hone to its original position Such sequence forms a double stroke, with a knife held obliquely, taking the same precaution to hone the entire length of the knife. Honing is then continued until all the teeth in the knife edge have been eradicated. In the case of the Minot or plane-wedge knife, the knife is turned over so as to sharpen the other surface every I0-20 strokes. For plane-concave knives, only the concave surface should be rubbed on the Hone. A flat circular glass plate with finely powdered aluminum oxide made into paste with water (used as an abrasive) may be used for grinding and removing nicks. Diamantine may also be used for final polishing. The plate glass is usually 1/4 to 3/ 8 inch thick, about 14 inches long and 1-2 inches wider than the length of the knife blade to be sharpened. Due to the plate's relatively greater width, the knife blade does not have to be held obliquely, but is pushed and pulled forward and backward at right angles to the transverse diameter of the plate. Mechanical honing with machines may make use of a vibrating frosted glass plate or a wheel driven by an electrical motor. The knife is pressed against the flat side of a rotating glass wheel which is being driven by a mechanical device. Approximately 30 double strokes are given each side of the knife to which very gentle pressure is applied. The use of knife sharpening machines, although quite expensive, is usually time-saving and produce well sharpened knives with uniform bevels. Precautions during Honing: The hone should be long enough (about 8" x 3") to allow the whole length of the knife edge to be sharpened in a single stroke and wide enough to sufficiently support and prevent the rocking of the knife. The hone should be lubricated with warm soapy water or fine oil before using. It is then washed, preferably with water, to remove all metal particles that may have been collected during the process. The washing fluid used must flow rapidly enough so that the metal chips are removed between strokes and a clean hone is presented every time. The pressure on the knife should be gentle and steady to keep it from rocking. The number of strokes usually amounts to 20-30 times in each direction, depending upon the condition of the knife. Badly nicked knives require greater and longer honing than less irregular knives. The hone should be cleaned before, during, and after use. A black film that develops in the hone usually is imparted by the knife that is being sharpened, and should be brushed out with a good nailbrush in running water, which may either be plain or soapy, until the hone is thoroughly cleaned. After its use, the hone must be washed with warm soapy water, dried, and kept in a box to protect it from dust while it is not in use. After honing, wipe off the oil or soap from the knife with xylene. Then strop it thoroughly. TROPPING Stropping is the process whereby the "burr" formed during honing is removed and the cutting edge of the knife is polished. The purpose of stropping is to polish and sharpen the cutting edge, while that of honing is to remove the irregularities from the knife. If the knife has become dull and blunt, but is free from nicks or teeth, it is usually only necessary to strop it. For delicate work, the knife is stropped before every object is sectioned. A paddle strop made up of the best quality horse leather, firmly attached to a solid back, in order to prevent sagging is preferred. The procedure is the reverse of honing. The knife is first fitted with its appropriate knife back, then laid obliquely on the strop and with the cutting edge behind, (EDGE LAST) is pushed backward and drawn forward in a TOE TO HEEL direction. Around 40120 double strokes are usually required. Fig. 12-8. Stropping Technique In the case of plane-wedge or Minot knives, the knife is turned around at the end of each stroke so as to sharpen each surface alternately. For planeconcave knives, only the concave surface should be stropped. Precautions Observed in Stropping: The knife should always be wiped clean with a soft cloth before and after a series of stropping strokes and before changing from a coarse to a fine strop to remove particles which may have been taken off the knife. After stropping is satisfactorily completed, the knife edge is then oiled or greased to prevent it from rusting. Then, the knife is kept covered in a suspension box to prevent the settling of dust and grit on its surface, causing damage to the knife edge. The knife should not be allowed to rest on its sides since this may also damage the cutting edge. Pressure during the first stropping strokes should be quite light, since the natural compressibility of the leather is what actually does the work. Only a gentle pressure should be applied while the knife is held steady on the strop, since a slip may cut the strop and damage the cutting edge. Speed in stropping should be avoided. One full second should be allowed for each stroke to avoid injury to the strop and the knife. Leather strops are usually dry and require oiling before they are used. Strops are usually treated with vegetable oil (e.g. castor oil) applied into the back of the strop, NOT the surface. The strop should not be used for at least 24-48 hours after treatment. Too much oil will make the stropping surface slippery and will render the procedure unsatisfactory. To remove excessive oil from the strop, its surface is scraped with a blunt instrument, e.g. the back of the knife. Mineral oil is not recommended and should NEVER come in contact with a strop since it will tend to blister and destroy the leather. One drop of mineral oil will spoil the polish of that area, and produce a permanent blemish on the strop. Stropping surfaces should be firm and not loose, to prevent the turning of the knife's edge. Hence, strops are usually mounted on a wooden canvass and covered with a flat pad to prevent them from sagging. Wax must not be allowed to come in contact with the strop. With an applicator, the used knife blade should be washed and flushed with xylene. The knife is then dried off, by wiping the knife on a soft paper or cloth (NEVER wipe the paper or cloth on the knife). The procedure is again repeated with fresh xylene and a fresh sheet of paper or both, until all the wax has been removed. Disposable Blades Sharpening (honing) and polishing (stropping) are no longer common practice in most modern laboratories because of the availability of disposable knives that are cheaper to use than conventional steel knives. They have a sharp cutting edge that can cut 2-4 µ thick sections with ease. Some microtome manufacturers have also now incorporated a disposable blade holder in place of a knife holder. Magnetic knives are also now available that can attach to some blade holders and are particularly suitable for use in the cryostat. Glass Knives Glass knives are generally used for trimming and semi-thin sectioning of tissue blocks for electron microscopy. They are prepared from commercially available 40 x 2.5 cm. plate glass strips that have been washed with detergent, rinsed in distilled water and alcohol, and dried with lint-free paper. Cleaned strips are clamped into a knife maker, scored with a tungsten carbide wheel, cracked to form 25 x 25 mm square pieces, and further broken into two triangular shaped knives using even pressure. Glass knives should be prepared and stored in dust-free boxes with lids, just before use, to avoid contamination. Diamond Knives Diamond knives are used to cut any type of resin block for electron microscopy. When supplied by manufacturers, they are already mounted in a metal block designed to fit directly into the knife holder of the ultrathin microtome. Diamond knives are brittle and expensive, but very durable, and the cutting edge must be kept clean to make it cut longer and to avoid damage during sectioning. OTHER EQUIPMENT In addition to the microtome and the microtome knife, the following items are also required during the process of sectioning: Waterbath - The thermostatically controlled type is preferable, but if this is unavailable, water from a hot water tap can be used although this can give rise to air bubbles which may be trapped under cut sections. The temperature of the water should be between 5 and 10°C below the melting point of the paraffin wax. Alcohol or small quantities of detergent may be added for reducing surface tension and allowing the section to flatten out with greater ease. Drying oven or hot plate - Small drying ovens are now available, incorporating a fan, especially designed for drying tissue section on slides. With a temperature setting at the melting point of the wax no obvious damage is done to the sections and drying is complete in 30 minutes. A hot plate may also be used instead of a drying oven. For more delicate tissues such as brain, a lower drying temperature is used to avoid splitting and cracking of the section due to excessive heat. In such cases, 37oC for 24 hours or longer is recommended. Forceps (fine pointed or curved) and squirrel hair brush - These tools are needed for handling sections during cutting, and for removing folds and creases on the sections during "floating out" in water bath. Clean Slides - For routine work, 76 x 25 mm. slides that are 1.0 -1.2 mm thick are usually preferred because they do not break easily. Frost-ended slides are generally used, where the identification number of the section can be inscribed with a pencil. Automatic slide labeling machines are also now available. Equipment such as a slide rack is made on the assumption that regular slides have been used. Larger size of slides are used for sections of eyes or CNS tissues when these will not fit on the regular The quality of sections cut on a microtome suffer badly from several (avoidable) causes. Things to avoid include: fecal material in intestine, especially in the colon where this material is very hard; hair is particularly bad it can be removed using a razor blade or clippers. Hair can also sometimes be inadvertently included with organs. Please be careful during dissections; sutures, thread or staples should be removed from the specimen prior to cutting with the knife. REFERENCES Bancroft JD. (1975) Histochemical Technique, 2nd ed. Butterworths, London. Bancroft JD, Cook HC. (1994) Manual o Histological Techniques and their Diagnostic Application. Churchill Livingstone, Edinburgh. Bancroft JD, Hand NM. (1987) Enzyme Histochemistry. Royal Microscopical Society Handbook 14. Oxford Science, Oxford. Brown RW, ed. (2009) Histologic Preparations: Common Problems and Their Solutions. Northfield, IL: CAP Press; 2009. Carson FL. (1997) Histotechnology. A Self-Instructional Text, 2nd ed. ASCP Press, Chicago. Carson FL, Hladik C. (2010) Histotechnology, A Self-Instructional Text. 3rd ed. Chicago, IL: ACSP Press. Culling CFA, Allison RT, Barr WT. (1985) Cellular Pathology Technique. 4th ed. London: Butterworths. Leica Microsystems. (2008) Instruction Manual Leica RM2235 V1.3 Nussloch: Leica Microsystems, 2008. Leica Microsystems website. Available at: http://www.leica-microsystems.com. Lubatschowski H. (2007) Laser Microtomy, Wiley-VCH Verlag, Biophotonics, S. 49-51. Mailhiot MA. (2005) Microtomy. It’s all about Technique! National Society for Histotechnology. Merryman HT. (1960) Principles of freeze drying. Annals of the New York Academy of Sciences. 85, 630. Peachey Lee D. (1958) "Thin Sections: A study of section thickness and physical distortion produced during microtomy" J. Biophysic. & Biochem. Cytol. 4(3): 233–242 Pearse AGE. (1980) Histochemistry, Theoretical and Applied, 4th ed. Vol 1. Churchill Livingstone, Edinburgh. Porter KR, Blum J. (2005) Article first published online: The Anatomical Record. Vol 117, Issue 4 Rolls G. (2008) 101 Steps to Better Histology. Melbourne: Leica Microsystems, 2008. Rolls GO, Farmer NJ, Hall JB. (2008) Artifacts in Theory and Practice of Histotechnology. 2nd ed. Columbus, OH: Battelle Press. Santoianni RA, Hammami A. (1990) Nuclear Bubbling an Overlooked Artifact. The Journal of Histotechnology, 13; 135-136. Sheehan DC, Hrapchak B. (1980) Theory and Practice of Histotechnology, 2nd ed. C.V. Mosby Co., St. Louis, pp 79-82. CHAPTER 13 CUTTING SECTIONS Sectioning is a process whereby tissues are cut into uniformly thin slices or "sections" with the aid of a microtome, to facilitate the studies under the microscope. Three general types of tissue sections may be made: 1. PARAFFIN SECTIONS - for paraffin embedded tissue blocks which may be cut by rocking and rotary microtome. 2. CELLOIDIN SECTIONS - for celloidin embedded tissues which are usually cut by means of the sliding microtome. 3. FROZEN SECTIONS - which may be cut from tissues that have been fixed and frozen with CO2 or for fresh or fixed tissues frozen with the cryostat. PARAFFIN SECTIONS Once the tissues have been embedded and the wax has solidified, the wax block is removed from the mold, the identification number is noted and the excess wax is cut off from the block to expose the tissue surface in preparation for actual cutting. This procedure is known as TRIMMING. Only thin slices are taken out at a time to prevent the block from cracking. The sides, top and bottom of the tissue block are trimmed until perfectly level and all sides are parallel, almost to the edge of the tissue. An old knife or blade may be used for this procedure, but it must still be relatively sharp to avoid damage to the tissue. When using the coarse feed, avoid cutting unintentional thick sections as this will damage the knife and possibly the block face. Depending upon the size and orientation of the tissue sample, shave conservatively into the block surface taking appropriate cuts that may measure between 4-60 micrometers. Samples of small biopsy tissue may be trimmed only to the depth of the first representation of several levels that will be collected. Since tissue is completely surrounded by paraffin, it is useful to uncover the surface of the block to reveal the tissue. Coarse facing is done on the microtome at approximately 30 microns at a time until the entire tissue surface is exposed. Care should be taken to avoid removing too much tissue in this step. Tissue that was embedded improperly may not reveal the entire tissue surface and will have to be re-embedded. Since tissue is completely surrounded by paraffin, it is useful to uncover the surface of the block to reveal the tissue. Coarse facing is done on the microtome at approximately 30 microns at a time until the entire tissue surface is exposed. Care should be taken to avoid removing too much tissue in this step. Tissue that was embedded improperly may not reveal the entire tissue surface and will have to be re-embedded. After coarse trimming, a heated spatula is held between the tissue block and the block holder until the wax begins to melt. The spatula is then withdrawn and the block is gently pressed into position. The block is allowed to harden for cutting proper by facing them down in ice cold water or refrigerator for 5-10 minutes. Placing blocks in a freezer can cause surface cracking, where the friable tissue separates from the surrounding wax cohesive sections become difficult to obtain. Cooling both the tissue and the wax will give them a similar consistency, and make sectioning easier. Re-chilling of the block may be required if the block face becomes warm or if deeper levels are required. The block is then placed in the microtome for fine trimming and cutting. Fine trimming may be done by either setting the thickness adjuster at 15 mm or by advancing the block using the coarse feed mechanism. The knife is usually tilted at 0-1 5° angulation on a microtome to allow a clearance angle between the cutting facet and the tissue block. Biconcave knives require smaller clearance angles than wedge-shaped knives. Fig. 13-1. Knife Clearance and Bevel Angles The block that is clamped on the chuck must be retracted enough to ensure that the knife does not touch the chuck or block on initial down stroke. The surface block is then trimmed away until the entire tissue surface has been partly exposed. The block is advanced into the knife and cutting is continued until complete sections come out of the block and a regular cutting rhythm is maintained. The cutting rate depends upon the type of the tissue, the size of the block, and the model or type of the microtome that is used. Sections usually form ribbons due to slight heat generated between the block and the knife edge during the process of cutting. Sections are cut between 4-6µ in thickness for routine histologic procedures, after the block has been fixed and secured to the block holder. The micrometer gauge is set to the required thickness and the knife is positioned in such a way that the center of the blade is in line with the block and the knife has been securely clamped in place . The actual thickness of the first couple of sections in a ribbon may be thicker than indicated because of thermal expansion when cutting a cold paraffin block. Using the microtome handle, try to cut in a slow and consistent manner don’t start and stop while the blade is cutting a block as this may produce horizontal lines across the block and the sections (and very slight changes in thickness). Sectioning is generally improved when the specimen and the wax are well matched in hardness. It is for this reason that most paraffin blocks must be cold when sections are cut. The actual method used to chill the block is important. Cold wax provides better support for the harder elements in a specimen allowing thinner sections to be obtained. Place the blocks on a cold plate or a cold wet surface for a few minutes (such as the surface of melting ice). Water penetrates a small distance into the block face, swelling tissues and making them more amenable to cutting. This is particularly important to over-dehydrated, dry or crumbly tissues. Incomplete sections are discarded. Complete ribbons are picked up at once with a camel hair brush, or a pair of forceps. Tissues which tend to crumble (e.g. blood clots, bone marrow) or do not form a smooth flat surface can be sectioned with ease, by exhaling gently into the block surface while the section is being cut slowly, to reduce the effects of static electricity. Successive sections will usually stick edge-to-edge due to local pressure with each cutting stroke, thereby forming a ribbon. Generally a slow, uniform cutting stroke produces the best results and the least compression. Do not stop and restart during a cutting stroke as this will produce bands of different thickness across the section. Fig. 13-2. Cutting Paraffin-Embedded Sections The practice of gently breathing on the face of a chilled block immediately before cutting each section, is common in some laboratories. The application of warm, moist breath tends to make sections more cohesive, but it also causes thermal expansion thus making the section thicker. Debris adhering to upper or lower edges of the block, or the back of the blade, can make it difficult to obtain cohesive ribbons and cause the ribbon to lift off the blade on the upstroke. If debris is present clear it away, re-chill the block and start again. Sections are removed in ribbons of ten to allow easy location of serial sections. The sections are then floated out on a water bath set at 45-50°C, approximately 6-10°C lower than the melting point of the wax used for embedding the tissue. This is to flatten the sections and prepare them for mounting onto the slides. Folds and creases may be removed by stretching the sections gently with a pair of dissecting needles or forceps. Bubbles may be teased out from beneath the sections by means of the same needle. Sections should not be left on the water bath for a long time (30 seconds will be enough) to avoid undue expansion and distortion of tissue. A section is selected for staining and picked up onto a clean slide in a vertical position. The slide is immersed in the water bath in a near vertical position as close as possible to the section. When the slide touches the section, it is lifted vertically out of water and drained. Sections may also be flattened out by placing them on a slide which has been flooded with 20% alcohol, producing convection currents which will serve to remove the creases in the tissue within a few seconds. Sections are very easily damaged when dislodging wrinkles or bubbles with brush or forceps. Examine each section as it floats on the water surface as imperfections can be readily seen. Leave the section on the water surface just long enough for it to flatten. Overexpansion can spoil the morphology in susceptible sections. Fig. 13-3. Floating Paraffin Embedded Sections Flotation should expand the section to its original dimensions and ensure that it is completely flat. The temperature will need to be 5 - 9 ˚C below the melting point of the wax. Make sure the water is clean and free of bubbles. To promote efficient drainage and to prevent the section from slipping down the slide, remove slides vertically from the water. After floating and mounting the paraffin sections from each block, use lint-free Kleenex or Kim-wipe to thoroughly wipe clean the surface of the water and the edges of the flotation bath to prevent floaters or cross-contamination. The mounted section is then placed in a 70oC paraffin oven for 20 minutes or until water droplets are no longer visible on the slides. Besides the paraffin oven which is maintained at a temperature of 2-5°C above the melting point of the paraffin used, small thermostatically controlled incubators may be used, regulated at 37°C, and at 45-55°C, for enzyme digestion, chemical extraction, metallic impregnation and enzyme localization techniques. Hot plates are not recommended because they can cause overheating and there is a risk of dust falling onto the section during the drying period. Excessive heat can cause droplets of water underneath a section to boil and this will cause damage. Proper drying ensures that sections are completely dehydrated, free of heat damage, flat and unlikely to lift during staining. Drain excess water from beneath the section before drying. Dry sections for between 5 and 30 minutes. Some delicate specimens will produce best results when dried at 37oC for a longer time (several hours to overnight). Metal racks with 25-slide divisions are used to store the mounted sections during the drying process which usually takes about 5 minutes in the heated oven. Once dry, the whole rack of slides can be taken for manual batch staining or placed on an automated staining machine. Staining of serial sections should never be attempted unless they are completel y dried. Overheating should be avoided because it will distort the tissue and melt some of the structures like collagen. Slides must always be grease- and dust-free and stored and handled correctly. If staining is to include antigen retrieval (IHC), enzyme pretreatment (ISH), or prolonged incubation steps, charged slides or an adhesive must be used. Some special stains, particularly those that employ alkaline reagents, can also cause sections to lift. Extended storage (usually more than 3 days) of unstained formalin-fixed paraffin embedded slides should be avoided as this may result in the loss of antigens. While not established, vacuum sealing and refrigeration may help preserve some unstable antigens. For nucleic acid extraction sections, allow the individual sections to roll up naturally and place them directly into sterile microfuge tubes ready for nucleic acid extraction. The extraction buffer can be added directly to the microfuge tube in order to preserve the molecular integrity of the sample. When cutting sections for DNA or RNA extraction, all instruments and equipment must be pre-cleaned and wiped down with RNAse-away before and between each specimen. Gloves must be worn. Molecular grade water must be used for floating sections for RNA extraction. Faults/Problems Observed during Section-Cutting Difficulties encountered during cutting of sections are mostly due to faults encountered during the processing of tissues or due to some faults in the technique or cutting itself. Therefore, it must be evaluated and corrected on a case-tocase basis, if good tissue sections are to be made. Below is a summary of the most common problems that can be identified at the microtome. Many microtomy problems have several causes so it is best to address them one at a time until the problem is resolved. Fig. 13-4. Section detached from the slide due to faulty processing PROBLEM Sections fail to form ribbons Sections roll up on cutting so that they adhere and get broken against the knife edge Ribbon is curved, REASON REMEDY Surfaces and edges of the block are not Re-trim the block parallel Horizontal surface Re-adjust and reof the block is not orient the block parallel to the knife Coat horizontal Paraffin wax is too edges of the block hard with wax of lower melting point Knife is tilted too Reduce the tilt much Readjust the Sections are too thickness of the thick sections Knife is dull Hone and strop Knife is blunt Sharpen the knife Tilt of knife is too Reduce the tilt great Knife edge is dirty Clean the knife edge Adjust the knife so Blunt or dull spot that knife edge will on the knife, present a uniformly producing an sharp edge to the irregular knife edge block, or sharpen crooked or uneven instead of straight Sections are compressed, wrinkled or jammed Edges of the block are not parallel but round or wedge shaped Knife is not parallel to the block Knife is blunt or dull Paraffin block is warm and soft Knife edge is coated with paraffin Sections are too thin Microtome set screw is loose Tilt of knife is too vertical Sections are squashed (width of each section is less than that of the block) A hole is formed in the section Sections of unequal thickness are produced Bevel of knife is lost due to incorrect sharpening Re-trim the block Readjust the knife and block Re-sharpen the knife Cool the block on ice water until firm Clean the knife edge Readjust thickness of the section Tighten the screw Reduce the tilt Re-sharpen, using a knife back or automatic knife sharpener Re-embed in freshly filtered wax if necessary Bubble or dirt formed in the embedding medium Tissue is not processed properly and will not form a Re-process tissue section (especially if center is raw) Under-processed portion of tissue Re-process tissue bursts on contact with warm water Once embedded in paraffin wax, decalcification is Hard spot in tissue impractical; use a due to calcium base-sledge microtome with a wedge knife Tilt of knife is too great or bevel is not cleared, hence Reduce the tilt object is compressed against the knife edge Clamp set screw on knife or block Tighten the screw holder is loose Cut blocks into smaller fragments Soften the blocks in Blocks are too hard detergent or phenol Breathe out or blow gently on the bock Static electricity due and knife to break up to low atmospheric static electricity, or boil water in the Sections adhere to the humidity room to increase knife or other parts of humidity the microtome Knife edge is dirty Clean the knife edge Knife edge is dull Sharpen the knife Knife tilt is too Reduce the tilt great Nicks or damage on Sharpen the knife the knife edge Re-embed in freshly Ribbon is split or Dirty embedding filtered wax lengthwise vertical scratches are seen on Clean knife edge Knife edge is dirty sections with xylene Tilt of knife is too Reduce the tilt great Knife tilt is too Reduce the tilt great Sections are lifted Knife is dull Sharpen the knife from the knife on Paraffin is too soft upstrokes Cool paraffin wax in or room temperature ice water is warm Tilt of knife is too small, paraffin Resistance is felt on block is therefore the lower part of the compressed against Increase the tilt section during cutting the base of the knife towards the end of stroke Knife edge vibrates Treat with phenol Horizontal or parallel due to hardness of during processing or lines or furrows across tissue collodionize the section Tilt of knife is too ("chatters") are seen Reduce the tilt great Knife is blunt Sharpen the knife Adjust the knife so that knife edge will Knife is not present a uniformly clamped properly sharp edge to the block, or sharpen Section cut is sometimes thin, Knife or block Tighten adjusting sometimes thick holder is loose and locking screws Blocks are too large Knife makes a hard metallic scraping or ringing sound on backstroke, when section is cut Frozen tissue crumbles and comes off the block holder when cut Frozen tissue chips into fragments when cut Ribbons are crooked Sections are too thick On trimming, tissue smells of clearing agent Tissue is opaque, section cutting is difficult due to presence of alcohol Tissue shrinks away from wax when trimmed Knife tilt is too small that block is compressed by bevel and section is not cut Tilt of knife is too slanted or too big Increase the tilt Readjust the tilt Tissue is too hard Take fresh block treated with phenol during processing Knife blade is too thin Change the knife Freezing is not adequate Refreeze the tissue block Tissue is frozen too much Warm the tissue with the fingers Top and bottom edges of block are not parallel to edge of blade/sides of block are not perpendicular to the blade Wrong micrometer setting Adjust the block holder to make the block edges parallel to the knife Microtome needs recalibration Block is trimmed down nearest to the tissue. Remaining wax is melted on Clearing agent not embedding oven and completely removed paraffin due to insufficient impregnation is impregnation repeated, changing the paraffin at least once before embedding Repeat clearing; if object has already been embedded, Insufficient clearing prolong clearing up to 12 hours, then reembed Insufficient dehydration, Repeat the whole therefore procedure incomplete clearing and impregnation On trimming, wax appears crystalline Contaminated wax Block not cooled rapidly enough Paraffin block, after cooling, is moist and crumbles Insufficient paraffin Re-embed in freshly filtered wax Re-embed in freshly filtered wax Repeat paraffin impregnation, then re-embed CELLOIDIN EMBEDDING Celloidin embedding is a slow process, usually taking weeks, and does not produce sections as thin as those produced by paraffin embedding. The advantage of celloidin embedding is that it completely avoids the use of heat at any stage. As a consequence, heat produced artifacts are avoided. In particular, shrinkage is absolutely minimal, if there is any, and structural relationships of the various types of tissue components can be seen clearly. The disadvantages are the longer time to cut, the thickness of the sections, the necessity for staining to be done on free floating section, the inconvenience of having to store the blocks in sealed jars with tight lids to prevent complete evaporation of 70% ethanol, the resulting restrictions on the type of staining methods that may be used. Celloidin may be purchased either as a solution or as a solid, damped with a liquid (usually ethanol) to reduce flammability. The stock purchased as a solution may be in an undesirable solvent and it is often the practice to evaporate the solvent to obtain dry celloidin, which is then weighed and re-dissolved in the appropriate solvent. Celloidin is used in form of solution, usually in a 1:1 mixture of ethanol-ether at concentrations of 2%, 4% and 8%. The fastest way to dissolve celloidin is to soak it first in half the final volume of anhydrous ethanol to soften it (50 mL for each 8 grams celloidin) with intermittent mixing in a tightly stoppered container. The next day, an equal volume of diethyl ether is added and intermittently mixed until an evenly consistent solution is obtained. The 2% and 4% solutions may then be made by simple dilution of the 8% solution with an equal parts mixture of ethanol and diethyl ether. The evaporation to dryness is done slowly at room temperature, without additional heat and in an explosion safe environment as a fire safety precaution. The solution should be transparent, without undissolved material, and should be stored in a completely closed container which is ether resistant. For delicate tissues, gradual dehydration with several changes of alcohol is strongly recommended to avoid distortion from removing the water too fast. No clearing agent is used with celloidin and following dehydration with absolute ethanol, the tissue may be placed in ethanol-ether. Ether is a lipid solvent and will remove much of the fat from the tissue. Denser tissues take a longer to infiltrate it must be left to infiltrate. When infiltration is complete, the block has to be cast and hardened. Paper boats have the advantage in that they may be cut off if the paper does not peel away easily. Some thick celloidin is poured into the bottom of a boat, then the tissue is oriented, and more celloidin poured in to cover the tissue. After filling the boat with thick celloidin, it is placed under a bell jar with a base that ensures air is excluded. Each day the top of the jar is lifted a little for a few minutes so that evaporated ethanol-ether can escape. More solvent will evaporate from the block each day, evaporating the solvent off slowly and ensuring that the celloidin thickens and hardens evenly throughout the tissue. Evaporating it too fast will result in the outside of the block becoming hard while the inside is still soft. The slow method of hardening the block allows the increasing concentration of celloidin to get into the block and give additional support to the tissue. The embedding process takes time and is complete when the block is sufficiently hard, often judged by pressing it with a finger nail without leaving an impression. Hardening of the celloidin block may be hastened by placing a small open container of chloroform under the bell jar. The chloroform will saturate the atmosphere and harden the celloidin without further evaporation. As the block hardens the celloidin will shrink. If at any time the celloidin shrinks enough to expose the tissue, more celloidin should be poured in to cover it. At the end of the hardening process there should be sufficient celloidin to allow for trimming the back of the block flat so that it may act as a base for glueing the block to a wooden holder for sectioning. Once hardened, the block is removed from the paper boat, preferably by peeling, but it can be cut away with a sharp blade if necessary. The block is then trimmed, leaving about 3 -5 mm of celloidin all around the tissue, then a distinctive cut is made on one corner for orientation. The back is trimmed flat and the block is placed into 70% ethanol until ready to be sectioned. The blocks are trimmed in the same manner as in paraffin blocks, but they do not require hardening by chilling before cutting. Tissues embedded in celloidin are usually sectioned with a sliding microtome, where the block is mounted to a holding platform facing upwards and some thick celloidin is placed onto the holder, positioning the block so that it will meet the knife as wanted, and the assembly is left until the attachment is firm. The knife is held at a significant slant so that most of the blade edge is used during the cutting stroke, and is quite long, often in excess of 25 cm. The face of the block is lubricated with 70% ethanol and the knife drawn across the top of the block at a strong slant, shaving off a section, which is immediately removed and placed in 70% ethanol. The surface of the block is then re-lubricated for the next cutting stroke. To avoid dehydration and shrinkage, section cutting is usually done wet, which means that the block is lubricated with a fluid, usually 60-70% ethanol, and is not allowed to dry out. This makes section cutting somewhat messy and quite a bit slower than the dry sectioning used with paraffin. Celloidin sections do not come off in ribbons and tend to roll up during cutting, and moistening the block and section with alcohol by means of a camel hair brush will serve to flatten the sections on the knife. After cutting the sections, they are immediately collected into 70% alcohol instead of being mounted on to glass slides. They are then stored in the same solution in jars with tightly fitting lids, and finally mounted on to slides after they have been stained. They are usually stained free floating and put on slides at the same time as the coverslip is applied. This makes it difficult to prepare serial sections as each section must be stored in individual, appropriately numbered containers. Small batches of 5 or more sections may be prepared, stored in the same alcohol that was used for lubrication, and never be allowed to become dry. REFERENCES Baker FJ. (1962) Progress in Medical Laboratory Technology, Vol. 1, Butterworths, London. Bancroft JD. (1975) Histochemical Technique. 2nd Ed. Butterworths, London. Bancroft JD, Cook HC. (1994) Manual of Histological Techniques and their Diagnostic Application. Churchill Livingstone, Edinburgh. Brown RW. (2009) Histologic Preparations: Common Problems and their Solutions. Northfield, IL: College of American Pathologists. Carson FL, Hladik C. (2009) Histotechnology: a self-instructional text. 3rd edition. Chicago: ASCP press. Culling CFA, Allison RT, Barr WT. (1985) Cellular Pathology Technique. 4th ed. London: Butterworths. Drury RAB, Wallington EA. (1967) Carleton's Histological Technique, 4th ed. Oxford University Press., New York. Fischer AH, Jacobson KA, Rose J, Zeller R. (2008) Cutting sections of paraffin-embedded tissues. Cold Spring Harbor Protocol. John DB, Anderson G. (2002) Theory and Practice of Histological Techniques.5th ed. Chapt 6. Tissue Processing and Microtomy including Frozen: Elsevier Churchill Livingstone, Edinburg; p. 85-108. Leica Microsystems. (2008) Instruction Manual Leica RM2235 V1.3 Nussloch: Leica Microsystems. Levinson SA, Macfate RP. (1969) Clinical Laboratory Diagnosis, 7th Ed., Lea and Febiger, Philadelphia. Lillie RD. (1965) Histopathologic Technique and Practical Histochemistry, 3rd Ed., Blakiston Division, McGraw-Hill, New York, Toronto, Sydney, London. Lillie RD, Fullmer HM. (1976) Histopathologic Technic and Practical Histochemistry. 4th ed. New York: McGraw hill. Lynch MJ, Raphael SS, Mellor LD, Spare PO, Inwood MJ. (1969) Medical Laboratory Technology and Clinical Pathology, 2nd Ed., W.B. Saunders Company, Philadelphia, London, Toronto. Mailhiot MA. (2005) Microtomy, It’s All About Technique! National Society of Histotechnology. Rolls G. (2008) 101 Steps to Better Histology. Melbourne: Leica Microsystems. Sheehan DC, Hrapchak BB. (1980) Theory and Practice of Histotechnology. 2nd ed. St Louis, MO: Mosby. Suvarna SK, Layton C, Bancroft JD. (2012) Bancroft’s Theory and Practice of Histological Techniques. 7th ed. Churchill Livingston, Elsevier. CHAPTER 14 ELECTRON MICROSCOPY The electron microscope is a type of microscope that uses a beam of electrons to create an image of the specimen. It is capable of much higher magnifications and has a greater resolving power than a light microscope, allowing it to see much smaller objects in finer detail. All electron microscopes use electromagnetic and/or electrostatic lenses to control the path of electrons. Glass lenses, used in light microscopes, have no effect on the electron beam. Principle of Electron Microscopy The basic design of an electromagnetic lens is a solenoid (a coil of wire around the outside of a tube) through which one can pass a current, thereby inducing an electromagnetic field. The electron beam passes through the center of such solenoids on its way down the column of the electron microscope towards the sample. Electron beams are used in electron microscope to illuminate the specimen and thus create an image. Since the wavelength of electrons are 100,000 times shorter than visible light the electron microscopes have much greater resolving power. Light microscopes show limited resolution compared to electron microscopes. Light microscopes have a resolution of 200nm and can magnify up to 2,000 x. Electron microscopes can achieve a resolution of 0.2nm and magnifications up to 2,000,000 x. Electron microscopes use a beam of electrons to illuminate the specimen instead of light as in light microscopy. The electron microscopes are of the following types: • Transmission electron microscope • Scanning electron microscope • Scanning tunneling electron microscope TRANSMISSION ELECTRON MICROSCOPE In transmission electron microscope (TEM), the source of illumination is a high voltage beam of electrons of very short wavelength, emitted from a tungsten filament at the top of a cylindrical column. The electron beam that has been partially transmitted through the very thin (and so semitransparent for electrons) specimen carries information about the structure of the specimen. The spatial variation in this information (the "image") is then magnified by a series of magnetic lenses until it is recorded by hitting a fluorescent screen, photographic plate, or light sensitive sensor such as a CCD (charge-coupled device) camera. The whole optical system of the microscope is enclosed in vacuum. Air must be evacuated from the column to create a vacuum so that the collision of electrons with air molecules and hence the scattering of electrons are avoided. Along the column, at specific intervals magnetic coils are placed. Just as the light is focused by the glass lenses in a light microscope, these magnetic coils in the electron microscope focus the electron beam. The magnetic coils placed at specific intervals in the column acts as an electromagnetic condenser lens system. The specimen is stained with an electron dense material and is placed in the vacuum. In transmission electron microscopy (TEM), electrons are transmitted through a plastic-embedded specimen, and an image is formed. TEM enables the resolution and visualization of detail not apparent via light microscopy, even when combined with immunohistochemical analysis. TEM is used to study the morphology of cells and their organelles, and in the identification and characterization of viruses, bacteria, protozoa and fungi. There are a number of drawbacks to the TEM technique. Many materials require extensive sample preparation to produce a sample thin enough to be electron transparent, which makes TEM analysis a relatively time consuming process with a low throughput of samples. The structure of the sample may also be changed during the preparation process. The field of view is relatively small, raising the possibility that the region analyzed may not represent the whole sample. There is potential that the sample may be damaged by the electron beam, particularly in the case of biological materials. For all practical purposes, living tissues or cells cannot be viewed under the TEM since the specimens are subjected to such high vacuum, heat and intense radiation from the electron beam. This would suffice to kill the cells either by volatilization of water (and other low melting point substances), denaturation from heat, or by ionizing radiation. There are four parts for a transmission electron microscope: • Electron source • Electromagnetic lens system • Sample holder • Imaging system The electron source is an electron gun which consists of a tungsten filament. This filament emits electrons when it is heated. The beam of electrons are then focused on the specimen by the condenser which consists of electromagnets called magnetic lenses. The sample holder consists of a mechanical arm which holds the specimen. The imaging system also consists of electromagnetic lens system and a screen which has a phosphorescent plate. The plate glows when hit by the electrons after passing through the specimen. PROCESSING OF TISSUE FOR ELECTRON MICROSCOPY FIXATION - This is done to preserve the sample and to prevent further deterioration so that it appears as close as possible to the living state, although it is dead now. It stabilizes the cell structure. There is minimum alteration to cell morphology and volume. Glutaraldehyde is often used as the fixative in TEM. Fixation is the first and most important step in any EM study, since mistakes made at this point render the whole project useless. The main purpose of fixation is to cross-link cellular structures into a matrix in order to preserve the structure of the cells with no changes in morphology, volume, or spatial relationships, and with minimum loss of cellular constituents. It also serves to protect and stabilize cellular structures from changes during subsequent treatments and from irradiation by the electron beam. Primary fixation • Fix specimen with 2.5% glutaraldehyde in 100 mM phosphate buffer at pH 7.0 2-24 hours (2-3 preferred) is usually started at room (or physiological) temperature and after 15-30 min then continued at 4°C. (Fixation at 4°C slows down autolytic processes and reduces tissue shrinkage). The time of fixation is dependent upon the dimensions of the sample to be fixed. The largest recommended size is 1 mm3, when there is optimal penetration. • Wash in 200 mM phosphate buffer that has been adjusted to the osmolarity of the sample to prevent tissue damage Glutaraldehyde, a di-aldehyde, preserves the tissue’s ultrastructure well but penetrates slower than the monoaldehyde, paraformaldehyde. Glutaraldehyde is used alone for small pieces of material, but a mixture of the two aldehydes may be used to fix larger tissues. Glutaraldehyde is fairly stable in concentrated form and at cold temperatures (-20°C). At room temperature and especially when diluted to working strength (1-3%), it is unstable and impurities and polymers accumulate. Paraformaldehyde is a monoaldehyde and penetrates faster than glutaraldehyde, but results in poorer ultrastructure. A solution is to use a mixture of both aldehydes as in perfusion fixation. RINSING - It is necessary to wash or rinse the specimen following primary aldehyde fixation and before post-fixation with osmium tetroxide. This step removes traces of aldehyde that would contaminate the tissue, forming a precipitate between the aldehyde and osmium during the secondary fixation step. The samples should be washed with a buffer to maintain the pH after fixation. For this purpose, sodium cacodylate buffer is often used which has an effective buffering range of 5.1-7.4. The sodium cacodylate buffer thus prevents excess acidity which may result from tissue fixation during microscopy. The type of buffer in which the fixatives are made up can affect the appearance of the specimen. Veronal buffers (containing barbitals) should not be used with aldehyde fixatives, and phosphate buffering may form a precipitate in the presence of calcium and uranyl ions. If the specimen is known to contain these ions, use a different buffer (e.g., Tris, HEPES, cacodylate). One advantage of cacodylate and HEPES buffer is that CaCl2 and/or MgCl2 can be added to the primary fixative. Calcium (and Mg) ions reduce the extraction of cellular components and enhance the retention of phospholipids. Also, the use of phosphate buffers with the glutaraldehyde fixative occasionally causes a precipitin to form during the second fixation step with osmium tetroxide. To prevent this, wash the specimen with saline or water after the first fixation so as to remove all traces of the phosphate. This problem rarely arises however and its cause is not understood. POST-FIXATION (SECONDARY FIXATION) with osmium tetroxide (OsO4) increases the stability and contrast of fine structure. OsO4 helps in the stabilization of many proteins by transforming them into gels without destroying the structural features. Tissue proteins stabilized by OsO4 are not coagulated by alcohols during dehydration. Osmium tetroxide reacts with unsaturated lipids, is electron-dense, and stains phospholipids of the cell membrane. The tissue is post-fixed with 1% osmium tetroxide in 100 mM phosphate buffer for 1-2 hours at 4°C, and then washed at least 5 times in distilled water to remove all excess phosphate ions and prevent uranyl acetate from being precipitated. This step is followed by dehydration through an ascending concentration series of solvent before embedding in resin DEHYDRATION - The water content in the tissue sample should be replaced with an organic solvent since the epoxy resin used in infiltration and embedding step are not miscible with water The tissue is dehydrated through a series of ethanols or acetones and propylene oxide. Acetone is preferred as there is less lipid loss than with ethanol dehydration. Maximum dehydration times are given below. • 30% Acetone or Ethanol 10 min. • 50% Acetone or Ethanol 20 min. • 70% Acetone or Ethanol 20 min. • 90% Acetone or Ethanol 20 min. • 100% Acetone, 3 × 20 min. • 100% Acetone 20 min. Propylene oxide is commonly used in the preparation of biological samples for electron microscopy, to remove residual ethanol previously used for dehydration. In a typical procedure, the sample is first immersed in a mixture of equal volumes of ethanol and propylene oxide for 5 minutes, and then four times in pure oxide, 10 minutes each. Since propylene oxide is much more volatile than ethanol or acetone, be careful not to allow the sample to be exposed to the air as damage will occur due to the rapid evaporation of the solvent. The samples can be fixed and dehydrated using ethanol as described above. However, after fully dehydrating the samples, the cells can be released from the plastic using propylene oxide. By gently pipetting propylene oxide over the cells, they will detach from the plastic either as individual cells or in ribbons. The detached cells should be pelleted and washed several times with propylene oxide to remove and solubilize the plastic before embedding. INFILTRATION - Epoxy resin is used to infiltrate the cells. It penetrates the cells and fills the space to give hard plastic material which will tolerate the pressure of cutting. The epoxy resin used for the 50:50 mixture can be from the frozen resin stock. There are several epoxy resins to choose from that have different viscosities. The less viscous epoxy resins (e.g., Spurr resin) have a carcinogenic component and are useful for hard material like bone but should be used and disposed of with care. Since most plastics dissolve in acetone and propylene oxide, the samples must be dehydrated using ethanol and a series of resin-ethanol mixes used during the infiltration process (instead of the more usual resin-propylene oxide mixes). Embedding is done using flat molds. EMBEDDING - The purpose of the embedding medium is to provide a stable, hard matrix throughout a tissue or cell in order that very thin sections may be cut. Paraffin wax is not firm enough for ultrathin sections and it will melt under the electron beam. There are many types of plastic resins available for embedding tissue. The three principal types of resins used for embedding ultrathin sections are the epoxy resins, polyester resins and methacrylate resins. The most commonly used resins are the epoxides, Epon and Araldite. They have adequate viscosity and are fairly stable under the intense electron beam. The two key advantages of acrylic or methacrylate-based resins over epoxy-based resins are that they are more hydrophilic and in some cases, can be polymerized at low temperatures. POLYMERIZATION – In this step, tissues embedded in the resin (wrapped in aluminum foil) are allowed to set overnight at room temperature and then placed in an oven at 60°C for 2-3 days. Specimens are placed in appropriate molds, such as Beem capsules. Blocks may be sectioned the following morning and polymerized further if necessary. A good test for correct polymerization is to try and dent one of the side ridges of the tip of the capsule with a fingernail (after removing the capsule from the mold). If there is an indentation from the fingernail the polymerization at 60°C should continue until the capsule is hard enough to show no indentations. To remove the capsule from the mold, carefully cut the mold lengthwise with a razor blade and peel the cut edges from the top (not the tip) of the capsule. The capsule can then be easily removed. If the side facets near the tip show cracks and/or bulging, it usually indicates too rapid polymerization. Processing tissue for electron microscopy • Fix tissues in a mixture of 2.5% glutaraldehyde, 2% (para) formaldehyde in 100 mM cacodylate buffer (pH 7.0) with 2 mM CaCl2 and 0.2% picric acid. • After an initial 30 min fixation, cut the specimens into small (1 mm3) pieces and continue fixation in fresh fixative for 16-24 h at 4°C. • Wash briefly with 200 mM cacodylate buffer (pH 7.0). • Post-fix with 1% osmium tetroxide in 100 mM cacodylate buffer (pH 7.0); 2 h at 4°C. • Wash with excess distilled water [to remove any free cacodylate and/or phosphate ions]. • En bloc stain with 2.0% aqueous uranyl acetate for 2 h at 4°C (in dark). • Dehydrate with acetone (or ethanol), propylene oxide and embed in resin. TRIMMING - Excess plastic surrounding the tissue must be trimmed away in a fashion that will yield a square or rectangular sections. Trim the capsule while viewing under the dissecting microscope using old glass knives or knives not suitable for sectioning. The capsule mold must be trimmed to a pyramid where the pyramid tip and sides are exposed tissue. The angle of the pyramid sides (called facets) should be about 45°. Too steep of an angle will not allow enough lateral support when sectioning while too flat (or low) of an angle will cause the "face" being sectioned to enlarge too quickly during sectioning. Use smooth slicing (not chiseling) strokes that cut through the plastic in one stroke. Take very thin slices so as to leave a smooth side surface (important for good sectioning). Fig. 14-1. Sectioning epon-embedded tissues for electron microscopy Sectioning (Ultramicrotomy) - The specimen must be cut into very thin sections for electron microscopy so that the electrons are semitransparent to electrons. These sections are cut on an ultramicrotome which is a device with a glass or diamond knife. For best resolution the sections must be 30 to 60 nm. Most problems with microtomy arise due to improper water level, too fast a cutting stroke, wrong knife angle (this should be about 5°) and a dull knife edge. It is extremely important that the first section using the new area of the knife be as thin as possible. Otherwise the knife edge will dull. After centering the sections they may be adhered to the proper grid by grasping the grid in fine tweezers (Pick up the grid only by the very edge) and bending the grid against the bottom of the petri dish so that it may be placed dull side down on the surface of the water and sections. The resin block can be made ready for the sectioning by trimming it at the tip with a razor blade or black trimmer so that the smallest cutting face is available. Fix the block to an ultra-microtome and cut the sections. Sections float onto a surface of liquid held in trough and remain together in a form of ribbon. Freshly distilled water is generally used to fill the trough. If a noticeable amount of water has evaporated from the boat causing a more concave surface, it is advisable to add a small amount of water to the boat so the surface is nearly level before moving the sections. The ultrathin sections are collected on grids for examination. Grids are manufactured of various metals, e.g., copper, nickel, and gold and are available in different designs including square mesh, hexagonal mesh, and parallel bars. Copper is the most common choice for grids and may be used with or without a support film. The sections often have a tendency to roll up like a scroll. This can be prevented by using a new knife edge and a slow smooth cutting stroke. The sections are then placed on a clean microscope slide with enough water present to permit positioning of the sections in an orderly arrangement. The slide is dried, lightly heat fixed and stained for 5 minutes with Toluidine blue. Most biological EM work is done on small (several millimeters) copper discs called grids cast with a fine mesh. This mesh can vary a lot depending on the intended application, but is usually about 15 squares per millimeter (400 squares per inch). On top of this grid, a thin layer of carbon is deposited by evaporating carbon graphite onto it. It is on this thin carbon film that the sample will then rest so that it can be examined in the microscope. Carbon is generally a hydrophobic substance (that is, it repels water), and if a drop of water is placed on it, the water will want to minimize its contact with the carbon. To make the surface more accessible to water and the suspended sample, the carbon needs to be made hydrophilic. This is accomplished by glow discharging. In glow discharging, the carbon coated grids are placed inside a partly evacuated chamber connected to a power supply. When high voltage is applied between the cathode and anode at each end of the chamber, the electron potential ionizes the gas within the chamber. These negatively charged ions then deposit on the carbon, giving the carbon film an overall hydrophilic (water attracting) surface. Staining Ultrathin Sections Although secondary fixation in osmium tetroxide provides some areas of electron density, this is usually not sufficient to provide high contrast, high definition images. A number of staining techniques are available to enhance the contrast of areas of interest. These fall into two major categories. 1) Positive Stains - deposit electron dense material on the area of interest, so that it stands out as a dark area on a light background. The stains most commonly used are uranyl acetate and lead citrate. Both metals apparently bind at sites of osmium deposition and lead also binds with and stains nucleic acids and glycogen. Uranyl acetate is used as a positive stain for EM. Uranyl ions react strongly with phosphate and amino groups, staining DNA and some proteins. Organelles composed of membranes are not stained well. Note that the starting material is radioactive. Lead citrate may also be employed as a positive stain and binds lead ions to negative ions, producing a general increase in contrast. 2) Negative Stains - penetrate and darken the interstices between areas of interest, which then appear light on a dark background. In negative stain microscopy, the electron beam primarily interacts with the stain. When stain is added to a sample, the stain surrounds the sample but is excluded from the volume occupied by the sample; hence the use of the term 'negative stain'. Some suitable negative stains include ammonium molybdate, uranyl acetate, uranyl formate, phosphotungstic acid, osmium tetroxide, and osmium ferricyanide. These have been chosen because they scatter electrons strongly and also adsorb to biological matter well. The structures which can be negatively stained are much smaller than those studied with the light microscope. Here, the method is used to view viruses, bacteria, bacterial flagella, and proteins or protein aggregates, which all have a low electronscattering power. Some stains, such as osmium tetroxide and osmium ferricyanide, are very chemically active. As strong oxidants, they cross-link lipids mainly by reacting with unsaturated carbon-carbon bonds, and thereby both fix biological membranes in place in tissue samples and simultaneously stain them. Lead Citrate is perhaps the best stain available since it can be used at a high pH and stains a wide variety of cellular components including nuclear components, ribosomes, membranes, microfilaments and glycogen. Aqueous solutions of lead salts and saturated solutions of lead hydroxide have been used as stains to enhance the electron-scattering properties of components of biological materials examined in the electron microscope. Saturated solutions of lead hydroxide, while staining more intensely than either lead acetate or monobasic lead acetate, form insoluble lead carbonate upon exposure to air. Care must be taken since lead citrate will react with atmospheric CO2 to form a fine precipitate of lead. Uranyl acetate may be used during the dehydration process by making the 50% acetone up to 2% with the stain. Uranyl acetate is not soluble in pure acetone. An aqueous solution of 2% concentration can be used to float or dip sections mounted on grids. Epon and Araldite do not take up aqueous stains well unless they are alkaline. Organic solvent solutions will usually leave a fine precipitate on the sections and is not often used. Rinse the solutions well with distilled water. Phosphotungstic acid may be used as a "negative" stain in that it does not bind particularly well to anything but instead causes areas other than cellular (organic) material to appear dark. It is especially useful for viewing molecules such as proteins (e.g., antibody, DNA) and suspensions of subcellular structures such as membranes (e.g., mitochondria - elementary particles, etc.) Usually a 1- 2% aqueous solution is used to stain a tissue block during dehydration for about 30 minutes. Excess dye is rinsed off with distilled water and the sections are then destained (removing excess stain in the sections) with ethanol (90-95%) for 2 minutes. The slide is dried and a cover slip is secured with a small drop of the pure plastic mixture used for the embedding procedure. A vial of this mixture (with DMP-30 added) may be kept for several months in the freezer (-20°C). The section may be viewed to see if they are of appropriate quality and can be labeled and stored after curing the plastic mixture (used for mounting the cover slip) on a warming plate set at 60°C. Problems during processing of tissues for electron microscopy: 1. Poor fixation can cause autolytic or postmortem changes (e.g. dilated mitochondria, widened extracellular spaces). a. Check the fixation protocol, particularly the timing between acquisition of the material and immersion fixation where postmortem changes may have occurred. b. Check the buffer pH and osmolarity. 2. Soft blocks—where an impression in the resin remains when a fingernail is pressed into it. This is because poor polymerization and is usually caused by out of-date accelerator. Replace accelerator every 6 mo. If soft blocks persist, increase infiltration times and/or gradually increase the resin/solvent ratio during the infiltration phase (e.g., 20:80, 40:60, 60:40, and 80:20). 3. Brittle tissue blocks in the center when cut. This may occur in one block of a batch due to poor infiltration of that solitary block or it may occur in a complete batch of blocks. If a whole batch of blocks are brittle, this may be due to poor dehydration caused by one of several things: a. analytical grade solvents were not used; b. incorrect concentrations of solvents were used; or dehydration times were too short. 4. Hard tissue (, e.g., bone or calcified tissue) blocks are fragile and break easily when cut due to poor infiltration. a. Omit the accelerator from the resin during all infiltration steps and infiltrate at 60°C before final embedding in complete resin as normal. b. Use a resin with a lower viscosity, e.g., the epoxy resin Spurr or an acrylic resin such as LR White. c. Digest hard walls, e.g., plant material but this may damage the ultrastructure. 5. Unrelated electron dense material (approximately 10 nm) throughout specimen when examined under the electron microscope may be caused by lead citrate stain. Check the support film or resin without tissue for the material. If stain is absent, there may have been a contaminant in glutaraldehyde, osmium, and phosphate. If stain is present on the empty grid, repeat the staining procedure on unstained grids and take more care not to introduce CO2 from breath. Practical Considerations and Safety Precautions • Tissue specimen should be cut into 1 mm pieces/blocks. Bigger specimen will result in incomplete infiltration therefore interfering final quality of results. • Analytical grade reagents must be used for all solutions, e.g., buffers and stains. • Glutaraldehyde must be EM grade. • Ultramicrotome knives should be examined using the back light (if available) to ensure the edge is sharp and dust free. • The uranyl acetate stains must be made fresh before use. • Most of the chemicals used for processing specimens for electron microscopy are extremely hazardous. • Glutaraldehyde, formaldehyde and osmium tetroxide are volatile and should be handled in a fume hood. The stock solution of glutaraldehyde (even when purchased new) should be checked often for impurities. If impurities have accumulated to unacceptable levels, the glutaraldehyde can be easily redistilled in a vented fume hood with the distillate collected at 100oC in small fractions until the pH of the distillate is less than 4.0. It is then convenient to freeze several aliquots at -20°C at which it is chemically stable for many months. Osmium is extremely dangerous, the crystals, liquid and vapors are all hazardous. The vapors can fix the cornea and lens of the eye and both vapors and liquid are absorbed rapidly and act as a nerve gas. Use only with proper ventilation (e.g., fume hood). It usually is purchased in crystalline form in pre-weighed sealed glass ampoules. Always prepare the fixative solution in a fume hood. The unused osmium tetroxide solution should be stored at 4°C in a scrupulously clean, foil wrapped 50ml volumetric flask that is tightly corked (do not use ground glass or rubber stoppers). The osmium solution will appear purple or violet in color when degraded or "exhausted". It should be carefully pipetted into a flask containing 95% ethanol. This will degrade the osmium for later disposal. Keep this waste flask in the fume hood at all times. • The epoxy resins used to embed the specimens are potentially more dangerous than the fixatives. In contrast to fixatives, whose actions are immediate and apparent, the consequences of exposure to the resins are not apparent for years. Therefore be careful with all resins prior to polymerization into hard blocks. Epoxy resins can be irritating to skin and eyes; use with caution. Many epoxides are known to be carcinogenic. The polymerized capsule however is not carcinogenic. Use acetone on a cloth or wipe to remove any resins from your skin. Lead is a cumulative toxin, so skin contact must be avoided. Most of chemicals used for processing specimens for electron microscopy are extremely hazardous, especially glutaraldehyde, formaldehyde, osmium tetroxide, embedding medium in liquid form, lead citrate, uranyl acetate. Extreme care should be taken when handling these chemicals. All steps must be performed in a fume hood and gloves should be worn all the time. Osmium tetroxide, glutaraldehyde, propylene oxide/resin waste should be collected in bottles for safe disposal. SCANNING ELECTRON MICROSCOPE (SEM) The Scanning Electron Microscope (SEM) scans the surface of coated specimens with an electron beam and by detecting electrons scattered (reflected) by the object, forms an image on a TV like monitor. This image is usually aesthetically pleasing and has a resolution of 50 µ and up. Unlike the Transmission Electron Microscope, where the electrons in the primary beam are transmitted through the sample, the Scanning Electron Microscope (SEM) produces images by detecting secondary electrons which are emitted from the surface due to excitation by the primary electron beam. Generally, the image resolution of an SEM is at least an order of magnitude poorer than that of a TEM. However, because the SEM image relies on surface processes rather than transmission, it is able to image bulk samples up to many centimeters in size and (depending on instrument design and settings) has a great depth of field, and so can produce images that are good representations of the three-dimensional shape of the sample. Another advantage of SEM is its variety called environmental scanning electron microscope (ESEM) can produce images of sufficient quality and resolution with the samples being wet or contained in low vacuum or gas. This greatly facilitates imaging biological samples that are unstable in the high vacuum of conventional electron microscopes. Areas ranging from approximately 1 cm to 5 microns in width can be imaged in a scanning mode using conventional SEM techniques (magnification ranging from 20X to approximately 30,000X, spatial resolution of 50 to 100 nm). The SEM is also capable of performing analyses of selected point locations on the sample; this approach is especially useful in qualitatively or semi-quantitatively determining chemical compositions, crystalline structure, and crystal orientations. Fundamental Principles of Scanning Electron Microscopy (SEM) The SEM is an instrument that produces a largely magnified image by using electrons instead of light to form an image. A beam of electrons is produced at the top of the microscope by an electron gun. The electron beam follows a vertical path through the microscope, which is held within a vacuum. The beam travels through electromagnetic fields and lenses, which focus the beam down toward the sample. Once the beam hits the sample, electrons and X-rays are ejected from the sample. Detectors collect these X-rays, backscattered electrons, and secondary electrons and convert them into a signal that is sent to a screen similar to a television screen. This produces the final image. Accelerated electrons in an SEM carry significant amounts of kinetic energy, and this energy is dissipated as a variety of signals produced by electronsample interactions when the incident electrons are decelerated in the solid sample. Secondary electrons and backscattered electrons are commonly used for imaging samples: secondary electrons are most valuable for showing morphology and topography on samples and backscattered electrons are most valuable for illustrating contrasts in composition in multiphase samples (i.e. for rapid phase discrimination). As the excited electrons return to lower energy states, they yield X-rays that are of a fixed wavelength. Thus, characteristic Xrays are produced for each element in a mineral that is "excited" by the electron beam. Magnification in a SEM can be controlled over a range of up to 6 orders of magnitude from about 10 to 500,000 times. Unlike optical and transmission electron microscopes, image magnification in the SEM is not a function of the power of the objective lens. SEMs may have condenser and objective lenses, but their function is to focus the beam to a spot, and not to image the specimen. Depending on the instrument, resolution will vary between less than 1nm and 20nm. In addition to its high resolving capability, the SEM also has a great depth of field, giving the characteristic three-dimensional appearance that is useful for understanding the surface structure of a specimen. The SEM has a monitor from which we as the operators view the specimen. The image is derived from the detection of excited electrons that are being bounced off the gold specimen at varying speeds and signals. The two detectors pick up the electron signals and via an analog/ digitizing process the image is viewed on a monitor screen, captured and stored as a digital image (varying resolutions) on the computer’s hard drive. Preparation of Samples for Scanning Electron Microscopy Because the SEM utilizes vacuum conditions and uses electrons to form an image, special preparations must be done to the sample. All water must be removed from the samples because the water would vaporize in the vacuum. For most protocols, SEM specimens need to be electrically conductive. For this reason, non-conductive and semi-conductive SEM specimens require the deposition of a thin surface layer of metal. This also increases the amount of secondary electrons that can be detected from the surface of the specimen in the SEM. 1. Fixation The fixation technique is designed to preserve the cellular structure of the specimen so when observed under the SEM the dead specimen will (should) resemble that of a live specimen. Various chemicals processes are used to fix the specimen. These chemicals are very dangerous to human health and care must be taken when dealing with them. 2. Extracting the required part of the specimen There are various ways of extracting the selected part of tissue that needs to be scanned, including manual dissection (simply cut and pull the wanted part carefully away from the body) and chemical dissection (use chemicals which eat away the soft body material leaving only the wanted hard bodied sections such as the exoskeleton). 3. Cleaning There are three major ways for cleaning specimens: a) Manual: this is where the dirt is picked off the specimen by very thin forceps and ultrafine pins. The dirt can also be removed by an eyelash, this is effective for delicate specimens. b) Vibration: the grime can be removed by using a sonicator which sends a high vibration frequency through the specimen shaking off the dirt. This method is ideal for hard bodied specimens. c) Chemical: various chemicals can be employed to actively remove the waxy layer on the surface of the specimens. Others simply dissolve or loosen the unwanted surface grime. 4. Drying The SEM works under a vacuum so it is essential that the specimen is completely dry. Otherwise, the specimen will simply collapse or blow up in the vacuumed chamber. There are several ways to dry the specimens: a) Air dried: many hard bodied specimens i.e., insects are dried on capture so once cleaned they can be simply placed into the SEM b) Critical Point dried: this complicated process involves the replacement of liquid in the cells with gas. This process creates a completely dry specimen with minimal or no cellular distortion. c) Chemically dried: the wet specimen can be put through an alcohol dehydration series which replaces the water with alcohol and then the alcohol is slowly evaporated off leaving a dried specimen. 5. Mounting The specimen is set on an aluminum stub to stabilize it in one place for viewing and maneuvering in the SEM chamber; to avoid the specimen from disappearing when being gold coated; and to reduce the amount of handling of the specimen. The stub is often a small, flat, round piece of metal that has a stem (looks like a flattened mushroom). The basic method of attachment is to glue the specimen or bits of the specimen to the stub which has been covered with double sided sticky tape and a thin layer of foil to ensure that the specimen (which is not conductive) will be grounded or earthed to the stub, and that electron charging of the specimen in the SEM chamber is reduced. 6. Gold Coating: The gold splutter coater is a machine that is used to coat the mounted specimens in gold before they go into the SEM. There are two detectors in the SEM chamber that are used to detect the two types of electrons that are bouncing of the gold metal specimen. It is these electrons - secondary and backscatter that go to make up an image of the specimen. If the specimen is not finely covered with a metal like gold it will produce a very poor signal so that the image will be very dark and perhaps not even there. Fig. 14-2. Gold Sputter Coater Radiation safety concerns The radiation safety concerns are related to the electrons that are backscattered from the sample, as well as X-rays produced in the process. Most scanning electron microscopes are extremely well shielded and do not produce exposure rates greater than background. However, scanning electron microscopes are radiation-generating devices and should be at least inventoried. It is also important that the integrity of the shielding is maintained, that all existing interlocks are functioning, and that workers are aware of radiation safety considerations. SCANNING TUNNELING ELECTRON MICROCOPE (STEM) The Scanning Tunneling Electron Microscope (STEM) is a type of electron microscope that shows three-dimensional images of a sample. In the STEM, the structure of a surface is studied using a stylus that scans the surface at a distance of only an atom’s diameter. Electrons tunnel between the surface and the stylus, producing an electrical signal. The stylus is extremely sharp, with its tip being formed by one single atom. The stylus is raised and lowered in order to keep the signal constant and main the distance. This enables the stylus to follow even the smallest details of the surface it is scanning. A profile of the surface is created, and from that, a computer-generated contour map of the surface is produced. This technique has been used in the study of DNA molecules. REFERENCES Antonovsky A. (1984) "The application of colour to SEM imaging for increased definition". Micron and Microscopica Acta 15 (2):77–84. Chapman SK. (1986) Maintaining & Monitoring The Transmission Electron Microscope, Oxford University Press, 1986 pp 37-39. Dahl R, and Staehelin LA. (1989) J. Electron Microsc. Tech. 13, 165-174. Danilatos GD. (1986) "Colour micrographs for backscattered electron signals in the SEM". Scanning 9 (3): 8–18. Erlandson RA. (1994) Diagnostic transmission electron microscopy of tumors: with clinicopathological, immunohistochemical, and cytogenetic correlations, New York: Raven Press. xvii, 857. Erlandson RA. (2003) Role of Electron Microscopy in Modern Diagnostic Surgical Pathology, in Modern Surgical Pathology, Weidner, et al., Editors. Saunders: Philadelphia, PA. p. 81-89. Erni R, Rossell MD, Kisielowski C, Dahmen U. (2009). "Atomic-Resolution Imaging with a Sub-50pm Electron Probe". Physical Review Letters 102 (9). Eyden B. (2002) Electron microscopy in the diagnosis of tumours. Curr Diag Pathol 8: p. 216-24. Ghadially FN. (1997) Ultrastructural Pathology of the cell and matrix, 4. Ed. Vol. 1, Boston: Butterworth-Heinemann. Glauert AM. (1974) Fixation, dehydration and embedding of biological specimens, in Practical Methods in Electron Microscopy, vol. 3, part I, North-Holland, Amsterdam. Hall J L, Hawes C. (eds.) (1991) Electron Microscopy of Plant Cells, Academic, London, England. Hayat MA. (1981) Principles and Techniques of Electron Microscopy. Biological Applications, 2nd ed. Vol. 1. Baltimore: University Park Press. Hayat MA. (2000) Principles and Techniques of electron microscopy: biological applications. 4th ed., New York: Cambridge University Press. Li MC. (1980) "Electron Interference". In L. Marton and Claire Marton. Advances in Electronics and Electron Physics 53. Academic Press. p. 271. Luft JH. (1961) "Improvements in epoxy resin embedding methods". The Journal of biophysical and biochemical cytology 9 (2). p. 409. Meek GA. (1977) Practical Electron Microscopy For Biologists, John Wiley and Sons, pp 4546. Murphy DB. (2002). Fundamentals of light microscopy and electronic imaging. Wiley/IEEE. p. 64. Reid N. (1974) Ultramicrotomy, in Practical Methods in Electron Microscopy, vol. 3, part II, NorthHolland, Amsterdam. Robards AW, Wilson AJ. (1993) Basic Biological Preparation Techniques for TEM, in Procedures in Electron Microscopy, Wiley, England, ch. 5. Robards AW, Sleytr UB. (1985) In "Practical Methods in EM" (A. M. Glauert, ed.), Vol. 10, pp. 309324 Elsevier, Amsterdam. Rudenberg J, Gunther H, Rudenberg PG. (2010) "Chapter 6 – Origin and Background of the Invention of the Electron Microscope: Commentary and Expanded Notes on Memoir of Reinhold Rüdenberg". Advances in Imaging and Electron Physics 160. Elsevier. Shimizu Y, Takenaka H. (1994) in: Advances in Optical and Electron Microscopy, Volume 14, Academic Press, New York, pages 249-334 (1994). Stirling JW, Curry A. (2007) Quality standards for diagnostic electron microscopy. Ultrastruct Pathol 31(5): p. 365-7. Tucker JA. (2000) The continuing value of electron microscopy in surgical pathology. Ultrastruct Pathol 24(6): p. 383-89. Wagner BE, Curry A. (2002) The usefulness of electron microscopy in diagnosing and investigating infectious diseases. Curr Diagn Pathol 8: p. 232-40. CHAPTER 15 ADHESIVES AND MOUNTING MEDIA Mounting is the last step in tissue processing that results in a permanent histological preparation suitable for microscopy, after adhesion of the sections on to the slide and appropriate staining of the tissue. After cutting, sections are floated out on a water-bath. Bubbles accumulating under the ribbon may be removed with a smooth teasing needle, care being taken not to tear the section. Bubbles may also be removed by pulling the ribbon very gently across the long edge of a glass slide held below the section in the water bath. When the sections chosen have flattened out, the numbered slide is immersed in the water bath and the section is fished out and drained. After draining, the sections are fixed to the slides. This can be done either by leaving the slides in a 37°C incubator overnight, by placing the slides in a wax oven at 56° to 60°C for 2 hours, or by drying the slides on a hot plate at 45° to 55°C for 30 to 45 minutes. For more delicate tissues like the CNS tissue or brain, a longer drying time at lower temperature (e.g. 37°C for 24 hours or longer) is recommended to avoid splitting and cracking of the section due to excess heat. Another alternative to drying is by the use of adhesives. To promote adhesion of sections, adhesives may be spread thinly and evenly on a clean grease-free slide which is then gently approximated to the end of the ribbon, and drawn upwards in a near vertical motion. ADHESIVES An adhesive is a substance which can be smeared on to the slides so that the sections stick well to the slides. The choice of slide and adhesive will be influenced by the staining methods to be subsequently applied. Slides must always be grease- and dust- free and stored and handled correctly. If staining is to include antigen retrieval (IHC), enzyme pretreatment for in-situ hybridization (ISH), or prolonged incubation steps, charged slides or an adhesive must be used. Some special stains, particularly those that employ alkaline reagents, can also cause sections to lift. Slides must always be accurately and appropriately labelled in a manner compliant with local regulations. Adhesives are not necessary for routine staining, provided that the slides are clean and free from grease. However, they are essential for methods that require exposure of sections to acids and alkalis (especially ammoniacal silver solutions) during staining. In such cases, the amount of adhesives applied on the slide should be kept to a minimum, since they are prone to contamination and bacterial growth that might be confused with real tissue organisms demonstrated by Gram and PAS stains. If clean grease-free slides are used and sections are adequately dried, the sections will not float off during staining and adhesive will not be necessary. There are still certain instances when sections may float from the slide: For urgent cryostat sections to be submitted for immunocytochemistry For central nervous system tissues For tissues containing blood clot For tissues which have been decalcified When sections are to be subjected to high temperatures The most commonly use adhesive is Albumin. Albumin solution is prepared by mixing equal parts of glycerin, distilled water and white of eggs, then filtered through coarse filter paper and a crystal of Thymol is added. One disadvantage of using albumin is that it retains some of the stain and gives a dirty background. Thymol resistant organisms growing in the adhesive have been known to contaminate gram-stained sections and cause confusion during microscopic examination. Poly-L-lysine, also a favorite adhesive, can be bought as a 0.1 % solution and further diluted (1 in 10 with distilled water) when ready to use. Sections are coated with this dilute poly-L-lysine and allowed to dry. With time, the adhesive ability of this substance slowly loses its effectiveness. Therefore the coated slides should be used within a few days. Aminopropyltriethoxysilane (APES) is a better section adhesive and coated slides can be stored for a long time. Slides are dipped in 2% APES in acetone drained then dipped in acetone, drained again and finally dipped in distilled water. It is invaluable in cytology particularly for cytosine preparation of proteinaceous or bloody material. 1. Mayer's Egg Albumin FORMULA: Egg White 50 cc. Glycerin 50 cc. Filter and add about 100 mg. crystals of thymol to prevent the growth of molds. Mayer's egg albumin is the most commonly used because it is very easy to make, is convenient, and is relatively inexpensive. A drop of Mayer's egg albumin is usually smeared into the clean glass slide before sections are oriented. Sections which have been creased on cutting may be stretched by gentle heating before attaching them into slides. During staining, the excess of albumin may also take up the stain and interfere with diagnosis; hence, it should be wiped off from the slide to remove any excessive solution. For celloidin sections, egg albumin is smeared on the slide. The section is then transferred from 95% alcohol bath to the slide, pressed flat on the slide with a smooth filter paper coated with thin celloidin mixture. 2. Dried Albumin - dried, and stored in 70% alcohol until it is ready for staining. FORMULA Dried albumin 5 gm Sodium chloride 5 gm Dissolve in 100 cc. of Distilled Water and add crystals of thymol. 3. Gelatin (1%) FORMULA: Gelatin 1 gm Distilled water 100 ml Glycerol 15 ml Phenol Crystal 2 gm Adding up to 30 ml of 1% aqueous gelatin to the water in a floating out bath and mixing it well is a most convenient alternative to direct coating of slides. 4. Gelatin-formaldehyde mixture FORMULA: 1% gelatin 5 ml 2% formaldehyde 5 ml Coat the slides with the above mixture. Allow coated slides to dry at 37°C for one hour or overnight before use. 5. Poly-L-Lysin e This aqueous detergent can be purchased as a 0.1% solution which is further diluted 1:10 with distilled water (final dilution to 0.01%) prior to use. Sections are coated with this diluted poly-L-lysine and allowed to dry. This is widely used as a section adhesive in immunohistochemistry. PolyL-lysine coated slides must be used within a few days after they are prepared, since its effectiveness as an adhesive slowly decreases in time. 6. APES (3-aminopropylthriethoxysilane) APES-coated slides are very useful in cytology, particularly for cytospin preparations of proteinaceous or bloody material. The slides are dipped in 2% APES in acetone, drained, dipped in acetone, drained again, and finally dipped in distilled water. They are then placed upright in a rack and allowed to dry. APES-coated slides are better than poly-L-lysine coated slides because they can be stored for a long time without losing their adhesiveness. MOUNTING MEDIUM If an unmounted stained section is seen in the microscope, differences in light refraction between the glass slides and the tissue components, may lead to difference in length dispersion; hence, very little microscopic detail can usually be appreciated. Tissues should therefore be impregnated with a transparent medium that has an index of refraction close to that of the glass and the tissue. The mounting medium bonds specimen, slide and coverslip together with a clear durable film. A mounting medium is usually a syrupy fluid applied between the section and the coverslip after staining, setting the section firmly, preventing the movement of the coverslip. It protects the stained section from getting scratched, to facilitate easy handling and storage of the slides, and to prevent bleaching or deterioration due to oxidation, thereby preserving the slides for permanent keeping. The mounting medium also helps prevent the distortion of image during microscopic examination. Mounting media are often chosen for a specific refractive index (R.I.), which can enhance specimen details or make them invisible. Materials like glass become totally invisible if immersed in a solution of the same refractive index. Refractive index is important because it governs the contrast between the cellular detail and the background, and also the transparency of the observed sample against the bright field of the microscope. The mounting media must always have an RI higher than the mounted sample to impart more transparency. The slide carrying the section to be mounted is taken from the last xylene bath with the forceps. Excess xylene is wiped off from the back of the slide and from around the section. A drop of mounting medium is placed down the center of the slide. A clean, dry cover glass is placed on the edge of the slide and gradually inclined downward until it touches the mounting medium and gently pressed on to the slide while the mounting medium quickly spreads through the whole area of the section. The slide may then be incubated at 37°C for 12-24 hours after mounting, to harden the medium. Do not use immersion oil on an uncovered slide. If in a hurry to view a specimen under oil immersion, mount the slip and handle the mount carefully, keeping it horizontal. Oil can be applied, but do not attempt to wipe it off until the mounting medium is cured - at least overnight or an hour on a hotplate or in an oven. Do not store mounted slides vertically for 2 days if cured at room temperature. Excessive mounting medium will cause it to ooze out of the sides of the cover glass, and should be carefully wiped with a fine cloth moistened with xylene. Excessive blotting, on the other hand, will dry up the section, causing shrinkage and cracking of the specimen. If the section has to be remounted, the cover glass may be removed by soaking in xylene. Excess xylene, if not removed, will mix with the mountant and form bubbles on the slide. Too little mounting medium may also cause improper setting of the coverslip or formation of bubbles on the section, which can be teased out by gently pressing on the cover glass with a pointed forceps or mounting needle. Setting may be hastened in a hot oven at 50°C for 2 hours. Characteristics of a good mounting medium: 1. It should be colorless and transparent. 2. It should be freely miscible with xylene and toluene. 3. It should not dry to a non-stick consistency and harden relatively quickly. 4. It should protect the section from physical damage and chemical activity (oxidation and changes in pH). 5. It should be resistant to contamination (particularly microorganism growth). 6. It should not cause shrinkage and distortion of tissues. 7. It should not leach out any stain or affect staining. 8. It should not change in color or pH. 9. It should be compatible with the adhesive in use. 10. It should set without crystallizing, cracking or shrinking (or otherwise deform the tissue being mounted) and not react with, leach or induce fading in stains and reaction products (including those from enzyme histochemical, hybridization, and immunohistochemical procedures). A mounting medium should be chosen that will not fade the particular stains used; for example, basic aniline dyes should be mounted in non-acid containing mountants. Preparations showing the Prussian blue reaction should be mounted in non-reducing media. The mounting medium is usually dispensed from the stock bottles into screw cap collapsible tin tubes. This will keep the mountant clean and prevent the concentration and thickening of the solution subsequent to evaporation. Slides should be properly labeled with an identifying case number on the side of the mounted coverslip to. As a general rule, a paper label bearing the patient's name, section number and preferably the staining method used, is attached to the slide for proper identification, while also avoiding any damage to the sections caused by wiping the "wrong" side of the slide. Mounting media may be divided into two main groups: a. Aqueous Media b. Resinous Media AQUEOUS MOUNTING MEDIA Aqueous mounting medium are used for mounting sections from distilled water when the stains would be decolorized or removed by alcohol and xylene as would be the case with most of the fat stains (Sudan methods) or for metachromatic staining of amyloid. They are usually made up of gelatin, glycerin jelly or gum arabic (to solidify the medium), glycerol (to prevent cracking and drying of the preparation), sugar (to increase the refractive-index), and a preservative solution. Following are examples of common aqueous mounting media: 1. Water - has a low refractive index, is moderately transparent and evaporates easily, hence is good only for temporary mounting. Also, water does not allow tissues to be examined under the oil immersion lens. In a wet mount, the specimen is suspended in a drop of liquid (usually water) 2. located between slide and cover glass. The water refractive index of the water improves the image quality and also supports the specimen. In contrast to permanently mounted slides, wet mounts cannot be stored over extended time periods, as the water evaporates. Glycerin - may also be used as a preservative. It has a high index of refraction and provides greater visibility if slightly diluted with water (for moist sections). This is a very suitable semi-permanent mounting medium with a refractive index of 1.46, sets quite hard, and will keep sections mounted for years, especially if sealed on the edges with paraffin wax. It is miscible with water, is inexpensive, and is non-poisonous. It is also not necessary to treat the specimens with alcohol or organic solvents, which may introduce artifacts and remove pigments. This is usually regarded as the standard mountant for fat stains. The disadvantage is, that it is difficult to prepare slides that are truly permanent in nature. Because it is a thick liquid, it can slowly run off a slide that is tilted. A proper sealing of the cover slip corners is absolutely necessary if one wants to store the slides over extended periods. Do not stack slides for long as the pressure will squeeze glycerin from the mounts. Glycerin will eventually evaporate and air will penetrate under the cover slip. Glycerin can be attacked by microorganisms, so one can optionally add a crystal of thymol to avoid bacteria and fungi. As with other solvents it is used because it is cheap, safe and quick to use with little preparation. Ringing the coverslip with a hydrophobic seal will extend the life of mounted sections, although cationic dyes will diffuse into the medium over time. Phosphate buffered glycerol (RI = 1.47) is commonly used to mount sections for immunofluorescence and glycerol may be added to other agents to retard drying and cracking. GLYCERIN JELLY (KAISER'S 1880) (Refractive Index 1.47) FORMULA: Gelatin 10 gm. Glycerol 70 ml. Distilled water 60 ml. Phenol crystals (preservative) 0.25 gm. Gelatin is added to distilled water and incubated in a water bath at 60°C until dissolved. Glycerol and then phenol crystals are added and mixed. The solution is labeled, and stored in a refrigerator at 40°C. For use, the gelatin must be heated in a water bath or incubator at 60°C to melt. Too much gelatin makes the jelly difficult to melt and included bubbles found on the slide will not burst. The melted medium should not be shaken or stirred before use, if formation of air bubbles is to be avoided. Glycerin jelly is the standard mounting medium used when dehydration and clearing with xylene cannot be made (as in fat stains). Pure glycerin has the highest index of refraction and thus provides the best viewing and may be optimal for critical or irreplaceable material, because old material, when glycerin is mostly evaporated, is easily retrieved with hot water or steam. The disadvantage is that it should be melted before use (due to the presence of gelatin). Stains mounted on glycerin jelly tend to fade. Polyvinyl alcohol, often used as a mountant in immunofluorescence microscopy, has been recommended as an alternative for glycerine jelly. The mountant is not set in the desired amount of hardness and therefore requires "ringing". 3. FARRANT'S MEDIUM (Refractive Index 1.43) FORMULA: Gum arabic 50 gm. Distilled water 50 ml. Glycerol 50 ml. Sodium merthiolate 0.025 gm. Dissolve gum arabic in distilled water with gentle heating and add glycerol and sodium merthiolate. Mix well and label. This gum arabic medium does not solidify upon storage and therefore does not need to be heated before use. However, it takes a longer time to harden and may therefore require ringing. Arsenic trioxide may be used as a substitute of sodium merthiolate for preservation of the medium. Addition of 50 gm. potassium acetate will produce a neutral (pH 7.2) instead of an acid (pH 4.4) medium, and therefore, will raise the refractive index to 1.44. 4. APATHY'S MEDIUM (Refractive Index 1.52) FORMULA: Pure gum arabic (crystals not powder) 50 gm. Pure cane sugar or sucrose 50 gm. Distilled water 50 ml. Thymol crystals 0.05 gm. This medium is used for methylene blue-stained nerve preparations and as a general purpose aqueous mountant. It is one of the most useful aqueous mountants for fluorescent microscopy, being virtually nonfluorescent. Von Apathy’s medium is not compatible with normal histological stains. The pH of the medium is near 4.0 (highly acidic) so stains fade or bleed into the medium. Addition of 50 grams potassium acetate, 20 grams of calcium chloride or 10 grams sodium chloride can raise the pH to near 7.0 and will prevent "bleeding" of metachromatic stains for amyloid. The medium sets quite hard, has a higher refractive index, and does not require ringing. 5. BRUN'S FLUID FORMULA: Glucose 24 gm. Glycerine 6 ml. Spirits of camphor 6 ml. Distilled water 84 ml. Mix, shake well, and filter. Store the solution in a well-stoppered bottle. Brun's Fluid is recommended for mounting frozen sections from water. Frozen sections that are mounted directly from water or paraffin sections which require dehydration and clearing, usually should be mounted on glycerin, gum syrup or Brun's fluid. RESINOUS MOUNTING MEDIA Sections of tissue embedded in plastic compounds (such as epoxy resins) can be successfully mounted in liquid resin of the same type. Sections should be completely dry before applying mountant, which is best set using the same conditions prescribed for tissue blocks. Resinous media are used for preparations that have been dehydrated and cleared in xylene or toluene, and are recommended for majority of staining methods. They may be divided into natural and synthetic resins. The most important synthetic resins are used for embedding undecalcified bones, and for electron microscopy. Canada Balsam (Refractive Index 1.524) Canada Balsam is a natural resin extracted from the Canadian tree, Abus Balsamea, usually dissolved in xylene in an incubator at 37°C or paraffin oven at 58 °C, and filtered, obtaining the desired consistency by controlled evaporation of the solvent. The solution can be made neutral or acid by adding excess amounts of calcium carbonate or salicylic acid, allowing the mixture to settle, decanting the supernatant liquid into a stock bottle, and discarding the residue. It is a transparent, almost colorless oleoresin that adheres firmly to glass and sets to a hard consistency without granulation. However, it darkens slightly with age and slowly becomes acid because it oxidizes xylene, thereby causing gradual fading of many stains. The harmful solvents which, constitute a health hazard such as xylene, may limit the use of Canada Balsam as a mounting medium. The use of nontoxic solvents like histomount instead of xylene like histomount may be less of a health hazard but may cause other problems such as slow hardening and premature darkening. Benzene may be substituted for xylene as a solvent. The medium can only be neutralized temporarily since the mixture becomes acidic and changes into a brown color upon storage. Calcium carbonate chips may be added to maintain its neutral reaction. The solution acidifies and darkens with age and upon exposure to sunlight, for which reason it should be kept in a dark glass bottle. Stains are usually not preserved due to acidity on prolonged exposure. Canada balsam is recommended for whole mounts and for thick sections because it does not shrink much. It sets hard without granulation; it is, however, quite expensive. As Canada Balsam does not mix with water, mounting in it implies the use of a sequence of dehydration, starting with low grade alcohols, followed by high grade alcohols, absolute alcohol, mixed clearing agents plus alcohol, clearing agents, clearing agents mixed with xylene, pure xylene, and balsam dissolved in xylene. Toluene or benzene could be used instead of xylene. DPX - (Dibutyl Phthalate and Xylene) (Refractive Index 1.532) This is a resinous medium recommended for small tissue sections but not for whole mounts because of shrinkage produced on drying; hence, it should be used in excess amounts. It is a colorless, neutral medium in which most standard stains are well preserved. It is prepared by dissolving the common plastic, polystyrene, in a suitable hydrocarbon solvent (usually xylene). It tends to set quickly and, in doing so, often retract from the edge of the coverslip. It has a greater advantage over Canada balsam in that slides can be cleaned of excess mountant simply by stripping it off after cutting around the edge of coverslip. XAM (Refractive Index 1.52) Xam is a synthetic resin mixture in xylene, available in a pale yellow or colorless solution. It dries quickly without retraction, and preserves stains well. Sections are quickly mounted from xylene. CLARITE (Refractive Index 1.544) Clarite (or Clarite X) is a synthetic resin which is soluble in xylene (it is used as a 60% solution in xylene), and is generally preferred over D.P.X. Other recommended synthetic mounting media include Permount (made by Fisher Scientific), H.S.R. (Harleco Synthetic Resin), and Clearmount (Gurr). Mountants for immunochemical staining The choice of mounting medium following immunochemical staining is largely dictated by the label (and in the case of enzymatic labels, the chromogen) used to visualize the antigen. Aqueous mounting medium is generally suitable for all enzymatic label/chromogen combinations and fluorescent labels. Specimens mounted in such media are mounted straight from the aqueous phase (with no dehydration or clearing). Aqueous mounting media for phycobiliprotein fluorescent labels (phycoerythrin, phycocyanin) must not contain glycerol as this quenches the staining intensity. Similarly, exposure to excitation light of most fluorescent labels results in diminished staining, a process known as photo bleaching. Apathy’s medium (Refractive Index 1.52) is the most useful aqueous mountant for fluorescent microscopy, being virtually non-fluorescent. Polyvinyl alcohol (Refractive Index 1.5) is an alternative for glycerine jelly, commonly used for fluorescent labels with paraphenylene-diamine as antifading agent. Ready-touse anti-fading kits are also commercially available. Cover slipping The stained section on the slide must be covered with a thin piece plastic or glass to protect the tissue from being scratched, to provide better optical quality for viewing under the microscope, and to preserve the tissue section for years to come. The stained slide must go through the reverse process that it went through from paraffin section to water. The stained slide is taken through a series of alcohol solutions to remove the water, then through clearing agents to a point at which a permanent resinous substance beneath the glass coverslip, or a plastic film, can be placed over the section. Bubbles under the coverslip may form when the mounting media is too thin, and as it dries air is sucked in under the coverslip. Contamination of clearing agents or cover slipping media may also produce a bubbled appearance under the microscope. Ringing Ringing is the process of sealing the margins of the cover-slip to prevent the escape of fluid or semi-fluid mounts and evaporation of mountant, to fix the coverslip in place, and to prevent sticking of the slides upon storage. The term “ringing” originated because round coverslips were initially used and the coating applied in the form of a circle or “ring.” A liquid preparation sealed well with nail polish could last some months. Paraffin wax may be applied with a ringing iron and is satisfactory as a temporary ringing agent. The ringing media used may be Kronig cement made up of two parts paraffin wax mixed with 4-9 parts powdered colophonium resin, heated and filtered. Also available are cellulose adhesives such as Durofix. Broken Slides Mounting a broken slide on to another clean xylene-moist slide with a drop of mounting media (Clarite or Permount) may be sufficient for immediate examination while a new section is being cut and stained. If an important slide is broken and replacement is not available, the section (if still intact) may be transferred to another slide. The coverslip can be removed by soaking in xylene, and placing the broken slide in the incubator at 37°C until all the mountant has been removed. The whole slide is then covered with a mixture of 6 parts butyl acetate and 1 part durofix and left in the incubator for 30 minutes until the mixture hardens into a film. Using a sharp scalpel blade, the hardened film is cut around the section, and the slide is placed in cold water until the film and section float off. The film containing the section is mounted on a clean slide, placed in the 37°C incubator until dry, washed gently with butyl acetate, then washed well with xylene, and mounted in Clarite or Permount. REFERENCES Bancroft JD. (1975) Histochemical Technique. 2nd Ed., Butterworths, London. Bancroft JD, Cook HC. (1994) Manual of Histological Techniques and their Diagnostic Application. Churchill Livingstone, Edinburgh. Bancroft JD, Stevens A. (1996) Theory and Practice of Histological Techniques. 3rd ed. Edinburgh: Churchill Livingstone; p. 734-6. Brown HJ. (1951). Experiences in the use of polyvinyl alcohol as a mountant. Microscope 8: 263-265. Espada J, Juarranz A, Galaz S, Cañete M, Villanueva A, Pacheco M, et al. (2005) Non-aqueous permanent mounting for immunofluorescence microscopy. Histochem Cell Biol 123:329-34. Farrington M. (1989) Notes on a method of making fluid mounts. Balsam Post 11: 22. Fidiam JF. (1993). Brief history of mounting specimens for the microscope. Balsam Post 21: 5-9. Fink S. (1987) Some new methods for affixing sections to glass slides. Stain Technology 62: 27-32, 9399, 349-354. Franklin AL, Filion WG. (1985) A new technique for retarding fading of fluorescence: DPX-BME. Stain Technol 60:125-35. Frison E. (1955) Some further experiments with synthetic resins as mounting media of high and low refractive indices. Microscope 10: 204-210. Gerakaris JG. (1984) Slide ringing revisited. Microscope 32: 259-264. Gray P, Wess G. (1950) The use of polyvinyl alcohol and its derivatives as microscopical mounting media. Part 1: Water miscible mounting media. Journal of the Royal Microscopical Society; 70: 287-90 Heimer GV, Taylor CE. (1974) Improved mountant for immunofluorescence preparations. J Clin Pathol 27:254-6. Loveland RP, Centifanto YM. (1986) Mounting media for microscopy. Microscope 34: 181-241. Luna LG. (1960) Manual of Histologic and Special Staining Techniques. 2nd ed. New York: The Blakiston Division McGraw Hill Book Co. Lynch MJ, Raphael SS, Mellor LD, Spare PO, Inwood MJ. (l969) Medical Laboratory Technology and Clinical Pathology, 2nd Ed., W.B. Saunders, Philadelphia, London, Toronto. Renshaw S. (2007) Immunochemical staining techniques. Immunochemistry: methods Express. Bloxham: Scion Publishers; p. 46-95. Wells J. (1978) The use of nail varnish in microscopy. Microscopy 33: 5. Welsby FW. (1955) Experiments with Canada Balsam. Microscope 10: 255-258. CHAPTER 16 PRINCIPLES OF STAINING Staining is the process whereby tissue components are made visible in microscopic sections by direct interaction with a dye or staining solution. A colored compound is used to produce a contrast between different tissues and cellular components based on their varying affinities for most dyes and stains, so morphologic changes are more easily identified, physical characteristics and structural relationships of tissues and their cells can be evaluated, and the presence or absence of disease can be established. Most cells are colorless and transparent, and therefore histological sections have to be stained in some way to make the cells visible. The same is true of components of the extracellular matrix. Because different parts of the cell are biochemically different, they take up specific stains to varying degrees. The main reason why cells are stained is to enhance contrast and visualization of the cell or certain cellular components under a microscope. Cells may be stained to highlight metabolic processes, to differentiate between live and dead cells in a specimen, to demonstrate the relationship between internal and external structures of the cells, and to identify different types of cells. A histologic stain is the purified form of a coloring agent or crude dye that is generally applied in an aqueous solution. The actual staining process may involve immersing the sample (before or after fixation and mounting) in dye solution. Certain parts of cells and tissues that are acidic in character (e.g. nucleus) have greater affinity for basic dyes, while basic constituents (e.g. cytoplasm) take more of the acid stains. Individual variation of the tissue constituents regarding these properties will consequently produce variation in colors under the microscope. Many dyes, however, require the use of a mordant a chemical compound that reacts with the stain to form an insoluble, colored precipitate on the tissue and make the staining reaction possible. When excess dye solution is washed away, the mordanted stain remains. It is important to remember that the colors of stains are not the real color of a particular tissue, and that a structure that appears as one color using one stain, may be a quite different color using another stain. The great majority of routine histology is done with hematoxylin and eosin (H&E) staining, because it is quick, cheap and informative. It involves the use of two contrasting stains, e.g., hematoxylin which stains the nuclear detail, and eosin which brings out the cytoplasmic detail of the cell and the tissue's architecture. STAINING OF PARAFFIN SECTIONS Paraffin wax is poorly permeable to most staining solutions and should therefore be removed from the section prior to staining. This is usually done by immersing the paraffin section in a solvent (e.g. xylene) two times, at 1-2 minutes duration each, for sections up to 10 micron thick. Xylene is not miscible with aqueous solutions and low graded alcohol, and should therefore be subsequently removed with absolute alcohol, followed by descending grades of alcohol to prevent damage and detachment of sections. The alcohol is then finally replaced with water before actual staining of section is performed. Such procedure is the exact reverse of impregnation and may be summed up by the phrase "Sections to Water". After the section is cut and mounted on the slide, it is drained and dried thoroughly to ensure that all moisture between the section and slide has evaporated, and that the section is firmly attached to the slide. If drying is not complete, the section (or part of it), especially from bone and nervous tissue, may become detached from the slide during the process of staining, usually after adding the acid differentiator. If an alcoholic stain is to be used, there is no more need to replace the alcohol with water. After deparaffinization with xylene, the section is transferred to decreasing grades of alcohol, and in such instances, the term "Sections to Alcohol" is used, and the staining procedure is subsequently done unless the tissue has been fixed in mercuric chloride solution, in which case, the section is taken “to water”. After staining, the section is again dehydrated with increasing grades of alcohol and cleared with two changes of xylene to prepare the section for mounting, since most mountants are miscible in xylene. The second change of xylene will also raise the refractive index of the glass slide, thereby reducing light refraction during microscopic examination. The stained section may be left in xylene for an indefinite period of time until it is finally mounted on the slide. The section should not be allowed to stay in alcohol for a Jong time because many stains are usually removed by prolonged immersion in alcohol. Sections may float off the slide during staining if the slides are dirty or greasy, or if the sections have not been left in the paraffin oven long enough to dry and be fixed in the slide. Sections must be left in the oven for a minimum of 30 minutes before they are finally stained to avoid such problems. HISTOLOGICAL STAINING Histological staining is the process whereby the tissue constituents and general relationship between cell and tissue are demonstrated in sections by direct interaction with a dye or staining solution, producing coloration of the active tissue component. Micro-anatomic stains, bacterial stains and specific tissue stains (e.g. muscles, connective tissue and neurologic stains) fall into this category. Histologists have developed many stains which are suited to particular purposes, allowing cell structures to be differentiated. It is important to remember that the colors of stains are not the real color of a particular tissue, and that a structure that appears as one color using one stain, may be a quite different color using another stain. METHODS OF STAINING Direct Staining: Direct staining is the process of giving color to the sections by using aqueous or alcoholic dye solutions. In simple (or direct) staining only one dye is used, which is washed away after 30–60 seconds, prior to drying and examination. The molecules that make up basic dyes have a positive charge. This is important because the cell wall and cytoplasm of bacterial cells have a negative charge. The positively charged dye is attracted to the negatively charged cells, enhancing the ability of the stain to stick to and color the cells. Methylene blue is a classic example of a simple stain. This blue stain will color all cells blue, making them stand out against the bright background of the light microscope. Indirect Staining: Indirect staining is the process whereby the action of the dye is intensified by adding another agent or a MORDANT which serves as a link or bridge between the tissue and the dye, to make the staining reaction possible. By itself, the dye may stain only weakly, if at all. The mordant combines with a dye to form a colored "lake", which in turn combines with the tissue to form a "tissuemordant-dye-complex" that is rendered insoluble in ordinary aqueous and alcoholic solvents. This allows subsequent counterstaining and dehydration to be carried out easily. It is an integral part of the staining reaction itself, without which no staining could possibly occur. A mordant may be applied to the tissue before the stain, or it may be included as part of the staining technique, or it may be added to the dye solution itself. Examples of mordants are potassium alum with hematoxylin in Ehrlich's hematoxylin, and iron in Weigert's hematoxylin. Fig. 16-1. Mordant and Accentuator An ACCENTUATOR, on the other hand, is not essential to the chemical union of the tissue and the dye. It does not participate in the staining reaction, but merely accelerates the reaction. Examples are potassium hydroxide in Loeffler's methylene blue and phenol in carbol thionine and carbol fuchsin. PROGRESSIVE STAINING Progressive staining is the process whereby tissue elements are stained in a definite sequence, and the staining solution is applied for specific periods of time or until the desired intensity of coloring of the different tissue elements is attained. Once the dye is taken up by the tissue, it is not washed or decolorized. The differentiation or distinction of tissue detail relies solely on the selective affinity of the dye for different cellular elements. REGRESSIVE STAINING With this technique, the tissue is first overstained to obliterate the cellular details, and the excess stain is removed or decolorized from unwanted parts of the tissue, until the desired intensity of color is obtained. Routine Hematoxylin and Eosin (H&E) staining is the most common method utilized for microanatomical studies of tissues, using the regressive staining which consists of overstaining the nuclei, followed by removal of superfluous and excessive color of the tissue constituent by acid differentiation. DIFFERENTIATION (DECOLORIZATION) is the selective removal of excess stain from the tissue during regressive staining in order that a specific substance may be stained distinctly from the surrounding tissues. A staining procedure that differentiates or distinguishes between types of bacteria is termed as a differential staining technique. Methods for simple staining impart same color to all bacteria and other biological material, may cause slight variation in shade. On the other hand, differential staining methods impart a distinctive color only to certain types of bacteria. In some techniques, the stains are applied separately, while in other they are applied as a combined stain. Differential Staining uses more than one chemical stain to better differentiate between various microorganisms or structures/cellular components of a single organism. This is usually done by washing the section in simple solution (e.g. water or alcohol), or by the use of acids and oxidizing agents. In general, if the primary stain used is a basic dye, the differentiation is carried out by an acid solution, while alkaline medium is used for differentiation after applying an acidic dye. Alcohol acts as a differentiator for both basic and acidic dyes, probably by simply dissolving out the excess dye. Differential staining is also used to detect abnormalities in the proportion of different white blood cells in the blood. The process or results are called a WBC differential. This test is useful because many diseases alter the proportion of certain white blood cells. A mordant can act as a differentiating agent. Mordants such as iron alum can also oxidize hematoxylin to a soluble, colorless compound, so that the tissue component becomes decolorized. On the other hand, if a section that has been stained by a mordant dye is allowed to remain in a differentiating agent such as 1 to 2% alcohol, all the dye will be removed. This is actually done as a preliminary step in re-staining a faded slide. Differentiation is usually controlled by following exact times specified for staining, or by examination under the microscope. One commonly recognizable use of differential staining is the Gram stain. Gram staining uses two dyes: Crystal violet and Fuchsin or Safranin (the counterstain) to differentiate between Gram-positive bacteria (large Peptidoglycan layer on outer surface of cell) and Gram-negative bacteria. METACHROMATIC STAINING Most dyes stain tissues orthochromatically, i.e., in color shades that are similar to the color of the dye itself. Metachromatic staining technique entails the use of specific dyes which differentiate particular substances by staining them with a color that is different from that of the stain itself (metachromasia). Tissue components combine with these dyes to form a different color from the surrounding tissue. This is particularly employed for staining cartilage, connective tissues, epithelial mucins, mast cell granules, and amyloid. At its simplest, the actual staining process may involve immersing the sample (before or after fixation and mounting) in dye solution, followed by rinsing and observation. Many dyes, however, require the use of a mordant: a chemical compound that reacts with the stain to form an insoluble, colored precipitate. When excess dye solution is washed away, the mordanted stain remains. Although methyl violets, of which crystal violet is one, do give metachromatic staining, they are not considered to be the most effective for the purpose. The azures or toluidine blue are more effective usually. The exception is for amyloid, when significant metachromasia is given by amyloid deposits using crystal or methyl violets. METALLIC IMPREGNATION Metallic Impregnation is a process where specific tissue elements are demonstrated, not by stains, but by colorless solutions of metallic salts which are thereby reduced by the tissue, producing an opaque, usually black deposit on the surface of the tissue or bacteria. Specific tissue elements are demonstrated, not by stains, but by colorless solutions of metallic salts which are thereby reduced by the tissue, producing an opaque, usually black deposit on the surface of the tissue or bacteria. Ammoniacal silver, for example, is reduced by argentaffin cells (e.g. in melanin and intestinal glands), forming black deposits seen under the microscope. A metallic impregnating agent is different from a stain in that it is not absorbed by the tissue, but is held physically on the surface as a precipitate or as a reduction product in certain tissue components. The most valuable metals for this purpose are gold (gold chloride) and silver (silver nitrate). Metallic silver deposits are sometimes adventitiously formed in sections; hence, all reagents to be used should be chemically pure, glassware should be clean and a formalin-laden atmosphere which is apt to precipitate such pigment disposition should be avoided. Also, since ammoniacal silver solutions are potentially explosive, care should be taken to prepare all solutions in clean containers just before use, and silvered glassware should be avoided. Flexible plastic containers may be used instead. Solutions should never be exposed to sunlight if explosion is to be avoided, and all unused reagents should be immediately inactivated by sodium chloride or dilute hydrochloric acid solution and discarded. The use of metallic instruments should be avoided when handling sections for metallic impregnation. VITAL STAINING Vital staining is the selective staining of living cell constituents, demonstrating cytoplasmic structures by phagocytosis of the dye particle (cytoplasmic phagocytosis), or by staining of pre-existing cellular components (true vital staining), as in the staining of mitochondria by Janus green. Vital stains are excluded by the living cells but taken up by the already dead cells as in the vital staining of reticulo-endothelial system with trypan blue, or propidium iodide for eukaryotic cells. The usual purpose is to reveal cytological details that might otherwise not be apparent; however, staining can also reveal where certain chemicals or specific chemical reactions are taking place within cells or tissues. The nucleus of a living cell is resistant to vital stains, and therefore is not demonstrated. In fact, demonstration of nuclear structures during vital staining suggests permeability of the membrane of the dye, signifying the death of the cell. INTRAVITAL STAINING Intravital staining of living cells is done by injecting the dye into any part of the animal body (either intravenous, intraperitoneal or subcutaneous), producing specific coloration of certain cells, particularly those of the reticulo-endothelial system. Common dyes used are lithium, carmine and India ink. SUPRAVITAL STAINING Supravital staining is a method of staining used in microscopy to examine living cells that have been removed from an organism. It differs from intravital staining, which is done by injecting or otherwise introducing the stain into the body. Those that enter and stain living cells are called supravital stains (e.g. New Methylene Blue and Brilliant Cresyl Blue for reticulocyte staining). However, these stains are eventually toxic to the organism, some more so than others. Partly due to their toxic interaction inside a living cell, when supravital stains enter a living cell, they might produce a characteristic pattern of staining different from the staining of an already fixed cell (e.g. "reticulocyte" look versus diffuse "polychromasia"). To achieve desired effects, the stains are used in very dilute solutions ranging from 1:5,000 to 1:50,000. Note that many stains may be used in both living and fixed cells. Thin slices of tissues are placed in small staining dishes and enough staining solution is added to cover the tissue. Common dyes used are: 1 Neutral red -probably the best vital dye. 2. Janus green-especially recommended for mitochondria. 3. Trypan blue -one gram of dye is dissolved in 100 ml. of sterile distilled water to be used immediately; it is dangerous to allow the suspension to stand for more than one hour, because it is likely to become toxic to the cell. 4. Nile blue 5. Thionine 6. Toluidine blue HEMATOXYLIN AND EOSIN (H & E) Staining Hematoxylin and Eosin (H&E) staining is the corner stone of tissue-based diagnosis. The process stains thin tissue sections so that pathologists can visualize tissue morphology. The process uses a hematoxylin dye to stain cell nuclei (and other parts) blue and an eosin dye to stain other structures pink or red. Hematoxylin binds strongly to acids and consequently binds to nuclear DNA and stains nuclei blue. Properly applied, this technique provides exceptional detail of tissue structure and the makeup of the cells. This detail is required for tissue-based diagnosis, particularly in the detection and classification of infection, cancer or metabolic disease. Routine H&E staining plays a significant role in tissue-based diagnosis by coloring otherwise transparent tissue sections, and allowing cell structures including the cytoplasm, nucleus, and organelles and extra-cellular components to be clearly visible under the microscope. In a histology laboratory, all specimens are initially stained with H&E and additional stains are only ordered if additional information is needed to provide a more detailed analysis. Staining with H&E is very reliable although it does show some variation depending on the exact formulation of the stain, and the stain density is considerably affected by the thickness of the sections – thicker sections take up more stain. It is also generally done before any additional staining techniques, because histology with H&E can confirm the basic tissue type and help to localize the lesion. (The term lesion is used by pathologists to indicate any area of damage, infection, inflammation, tumor, necrosis or otherwise abnormal tissue.). Since most cell structures are transparent, very little detail of the structure can be seen, unless the cells are stained. The same is true of components of the extracellular matrix. Because different parts of the cell are biochemically different, they take up specific stains to varying degrees. ROUTINE H&E STAINING in Paraffin Embedded Section (Regressive Staining) Fixation: Most fixatives can be used except osmic acid solutions which inhibit hematoxylin. Procedure: 1. Clear paraffin embedded sections in first xylene bath for 3 minutes. 2. Transfer to second xylene bath for 2 to 3 minutes. 3. Immerse in first bath of absolute ethyl alcohol for 2 minutes. 4. Transfer to a bath of 95% ethyl alcohol for 1 or 2 minutes. 5. Rinse in running water for 1 minute. 6. Stain with Harris alum hematoxylin for 5 minutes (Ehrlich's hematoxylin requires 15-30 minutes). 7. Wash in running tap water to remove excess stain. 8. Differentiate in 1% acid-alcohol (1 ml concentrated HCl to 99 ml. of 80% ethyl alcohol) for 10-30 sec. monitoring the changes in color microscopically until only the nuclei are stained. 9. Rinse in tap water. 10. Blue in ammonia water (average of 5 minutes) or 1% aqueous lithium carbonate until the sections appear blue (about 30 seconds). 11. Wash in running water for 5 minutes. 12. Counterstain with 5% aqueous eosin for 5 minutes. If alcoholic eosin is used, the time can be reduced to 30 seconds or 1 minute. 13. If aqueous eosin is used, wash and differentiate in tap water under microscope control until the nuclei appear sharp blue to blue black and the rest of the tissue appear in shades of pink. If alcoholic solution is used, differentiate with 70% alcohol. 14. Dehydrate, clear and mount. NOTE: For tissues fixed with mercuric chloride, the staining time in hematoxylin should be increased slightly while duration of eosin staining should be reduced. The mercury should be removed using a 0.5% solution of iodine in 80 to 95% alcohol and rinsed in water. The iodine is then removed by placing the slide in 3% sodium thiosulfate solution for 1 to 5 minutes and washing it well in running water for 3 to 5 minutes. Alternatively, mercury deposits may be removed after sections are hydrated, by immersing the sections in Gram's or Lugol's iodine for 5 minutes, followed by sodium thiosulfate and subsequently washing the section in water prior to staining. Staining may be prolonged for chromium and osmium fixed tissues (e.g. Flemming's fluid), for tissues subjected to long acid decalcification, and after prolonged storage in acid formalin or 70% alcohol. FROZEN SECTION STAINING Frozen sections mounted on the slides may be stained as in paraffin sections although the duration of staining is usually shorter. Sections may be mounted in an aqueous medium directly from water if necessary. Frozen sections may be stained by picking up sections on albuminized slides and drying them quickly or by simple direct staining on a wet slide with an eye dropper. The following staining methods are commonly employed for frozen sections, the choice depending upon the personal preference of the pathologist and the type of tissue section to be stained. 1. Hematoxylin-Eosin method 2. Thionine method 3. Polychrome Methylene Blue method 4. Alcoholic Pinacyanol method (used also for supravital staining of mitochondria and primarily for color sensitization in photography) H & E staining of Frozen Sections for Rapid Diagnosis (Progressive Staining) 1. Orient section in the block and freeze with liquid nitrogen. 2. Cut cryostat sections at 5-10 micron. 3. Mount sections on to albuminized slides and dip in 10% formalin to fix. 4. Rinse rapidly in water. 5. Stain with Harris hematoxylin for 30-45 seconds. 6. Rinse in tap water. 7. Blue in ammonia water for 5 seconds. 8. Rinse in tap water. 9. Counterstain with 5% aqueous eosin or 1% alcohol eosin for one minute. 10. Rinse in tap water. 11. Dehydrate in increasing concentrations of alcohol. 12. Clear with xylene. 13. Mount with cover slide. It is somewhat less favored than regressive staining due to the difficulty of producing sufficiently intense progressive staining of cell structures without staining other parts, thereby resulting in diffused color and obscured details. For convenience, reagents for this rapid H&E stain are generally arranged in sequence using a series of Coplin jars. This method takes only 5-10 minutes and produces well-differentiated sections that are semi-permanent and can be stored. The remaining portion of tissue must be kept for routine processing and are made for comparison with frozen sections. Fig. 16-2. Passing slides through a series of solutions Precautions in Staining Stains on the skin should be avoided not only because they are signs of poor technique but because stains are health hazards per se, being slowly absorbed by the skin and eventually producing side effects. Stains may be effectively removed from the skin by prompt topical application of 0.5% acid alcohol, followed by rinsing with tap water. Failure of staining may be due to paraffin, fixative, or decalcifying solution that has not been thoroughly washed out and removed. Early fixation in alcohol before paraffin embedding may have been incorrect, for which no remedy can be made. Alternatively, the staining solution may be faulty. Hematoxylin solutions may not have been properly and sufficiently ripened. Hematoxylin must not be used too soon after preparation to ensure complete ripening. Impurities found in the dye or in the water solvent will affect not only the solubility of the dye but even the intensity of the staining reaction, necessitating purification and filtering of the dye. Stains that have already been deteriorated should be replaced. If, after staining, sections are fuzzy and do not appear clear under the microscope, xylol should be replenished. There may be water in the absolute alcohol, moisture in the coverslip, or too much egg albumin on the slide, thereby obliterating the image of the stained tissue. And often, acid-alcohol decolorizer may not have been completely removed, or a film from alkaline alcohol may have been carried along. To remedy the condition, the section is placed in a Coplin jar containing xylol to dissolve the adhesive. The slide is run back thru the various processes up to the point where the fault was; a fresh solution is used, and the tissue is re-stained. Stains may be saved and used again for as long as they have not lost their staining properties. Sections are usually rinsed with distilled water before placing them in used stains. Formation of precipitate in staining solution and poor staining results signify loss of staining property and hence, the stain should be discarded and replaced with a fresh solution. Failure of sections to remain on the slide during staining could have been due to a dirty or oily slide. Slides may have been carried thru the first alcohol baths too fast, resulting in a rapid but incomplete dehydration; or paraffin sections may not have been thoroughly spread on the slide when mounted. Albumin fixative may be too old, as suggested by the loss of its clear color, or by emission of an odor. To avoid this, adhesives should be prepared in small amounts (around 1 ounce) which may last for 2-3 months. COLLODIONIZATION OF SECTIONS Paraffin ribbons containing air bubbles, torn or inadequately infiltrated sections are likely to float from the slide when deparaffinized and stained. They are more firmly attached by coating the slide with dilute (thin) celloidin solutions, a process known as collodionization, which is also recommended for sections that will be subjected to strong alkaline or acid solutions and for tissues that contain glycogen for demonstration. Procedure: 1. Deparaffinize in xylene. 2. Dehydrate thru absolute alcohol. 3. Dip individual slides in Coplin jar containing dilute ether alcohol solution. 4. Dip in dilute ether solution of celloidin (thin celloidin). 5. Hold slide on one end for 1/2 to 1 minute to drain or until the section begins to whiten around the edges. 6. Wipe off the back of the slide and place in 80% alcohol for 3-5 minutes to harden the celloidin. 7. Stain as desired. Sections may be transferred from one solution to another with a bent glass rod (as in frozen sections), but because they are thicker, they may be handled by means of forceps instead. Cellulose nitrate (celloidin) is soluble in absolute alcohol, and will be removed if absolute alcohol is used in the final dehydration prior to clearing of stained sections. Instead, sections treated with 95% alcohol may be transferred to a mixture of equal parts of chloroform, absolute alcohol and xylene (C.A.X,) then treated with xylene and mounted in Xam. RE-STAINING OF OLD SECTIONS Old, bleached or faded sections may be re-stained: the slide is usually immersed in xylene for 24 hours, or gently heated until the mounting medium begins to bubble. The coverslip may then be removed by lifting it with a dissecting needle. The section is placed in xylene for up to 24 hours to remove the remaining balsam and then brought down to water. It is placed in a 0.5 potassium permanganate solution for 5-10 minutes, rinsed in tap water and subsequently immersed in 5% oxalic acid for 5 minutes or until the section is decolorized. After washing it again in running tap water for another 5 minutes, the section may then be re-stained with the appropriate staining technique. HISTOCHEMICAL STAINING (HISTOCHEMISTRY) Histochemical staining is the process whereby various constituents of tissues are studied thru chemical reactions that will permit microscopic localization of a specific tissue substance. Chemical ions such as calcium, molecules such as bile pigments, and biopolymers such as cellulose, DNA and specific enzymes are among the tissue components that can be identified using histochemical staining techniques. In enzyme histochemistry, the active staining reagent serves as a substrate upon which the enzymes act, and the final coloration produced is from the substrate rather than the tissue. In many instances, histochemical methods used to stain several chemical constituents will also ultimately stain the tissue itself, thereby producing an overlapping of techniques. The staining techniques employed for histochemistry are also usually applied for staining of histologic structures. Examples of such type of stains are Perl's Prussian blue reaction for hemoglobin, and Periodic Acid Schiff staining for carbohydrates. IMMUNOHISTOCHEMICAL (IHC) STAINING is a combination of immunologic and histochemical techniques using a wide range of polyclonal or monoclonal, fluorescent labeled or enzyme-labeled antibodies to detect and demonstrate tissue antigens (e.g., proteins) and phenotypic markers under the microscope. Immunohistochemical staining is widely used in the diagnosis of abnormal cells such as those found in cancerous tumors, in the localization of biomarkers and differentially expressed proteins in different parts of a biological tissue, and in the detection of specific molecular markers that are characteristic of particular cellular events such as proliferation or cell death (apoptosis). Visualizing an antibody-antigen interaction can be accomplished in a number of ways. In most cases, an antibody is conjugated to an enzyme, such as peroxidase, that can catalyze a color-producing reaction. Alternatively, the antibody can also be tagged with a fluorophore, such as fluorescein or rhodamine. Immunohistochemical staining techniques are used to label defined antigens with monoclonal and polyclonal antibodies. Commercially produced antibodies most frequently originate from mice, and less frequently from rabbits. The degree of autolysis or putrefaction, the selection of fixation medium, fixation duration, incubation period, and concentration of the selected antibodies can be crucial factors that can affect the results of immunohistochemical staining protocols. Unlike conventional histological staining methods, immunohistochemical techniques are based on antigen–antibody bindings, which can be affected by inappropriate fixative selection and duration. The current recommendation for immunohistochemical techniques is a maximum of 4% neutral buffered formaldehyde solution and, for some antibodies, fixation time can be up to a maximum of 48 h. Microwave-based fixation of tissue in formaldehyde may have an adverse effect on immunohistochemical staining. REFERENCES Baker JR. (1958) Principles of Biological Microtechnique. London: Methuen, 89: 238. Bancroft JD, Stevens A, editors. (1996) Theory and practice of histological techniques. 4th ed., New York: Churchill Livingstone. Bancroft JD, Gamble M, eds (2002) Theory and Practice of Histological Techniques. 5th ed. London: Churchill-Livingstone. Bettinger CH, Zimmermann HW. (1991) New investigations on hematoxylin, hematein, & hemateinaluminium complexes. 1. Hematin-aluminium complexes and hemalum staining. Histochemistry, 96: 215. Beveridge TJ. (2001) "Use of the Gram stain in microbiology". Biotech Histochem 76 (3): 111–8. Black J. (2012) Microbiology: Principles and exploration. 8th ed. John Wiley & Sons. p. 68. Carson FL. (1996) Histotechnology: a self-instructional text. 2nd ed. Chicago: American Society of Clinical Pathologists Press. Carson FL, Hladik C. (2009). Histotechnology: A Self-Instructional Text. 3rd ed. American Society of Clinical Pathologists Press. Clark G. (1981) Staining Procedures, 4th ed., Baltimore: Williams & Wilkins, p. 412. Culling CF. (1974) Handbook of Histopathological and Histochemical Techniques. 3rd ed., Butterworth, London, 65. Horobin RW. (2002) Theory of Staining and its Practical Implications. Chapt 7, In: Theory and Practice of Histological Techniques, 2nd ed. Churchill Livingstone, London, 109. Horobin RW, Kiernan JA. (2002) Conn's Biological Stains. A Handbook of Dyes Stains and Fluorochromes for Use in Biology and Medicine. 10th ed. Oxford. Junquera LC, Carneiro J. (1980) Basic histology. 3rd ed. Los Altos, CA: Lange Medical Publications. Kiernan JA. (2008) Histological and Histochemical Methods. Theory and Practice. Bloxham, UK: Scion. Lee GL. (1992) Histopathologic methods and color atlas of special stains and tissue artifacts. Gaithersburg, MD: American Histolabs Inc., Publications Division. Lillie RD. (1965) Histopathologic Technic and Practical Histochemistry, 3rd edition, McGraw-Hill Book Co., New York. Lillie RD. (1969) H.J Conn's Biological Stains, 8th ed., Williams and Wilkins Co., Baltimore. Lillie RD, Fullmer HM. (1976) Histopathologic Technic and Practical Histochemistry, 4th ed., McGraw-Hill Book Co., New York. Luna LG. Manual of Histologic Staining Methods of the Armed Forces Institute of Pathology, third edition, McGraw Hill Lynch MJ, Raphael SS, Mellor LD, Spare PD and Inwood MJ. (1969) Medical Laboratory Technology and Clinical Pathology, 2nd edition, WB Saunders Co., Philadelphia London Toronto Marshall PN, Horobin RW. (1973) The mechanism of action of 'mordant' dyes - a study using preformed metal complexes. Histochemie, 35: 361. McManus JFA, Mowry RW. (1964) Staining Methods. Histologic and Histochemical. Harper & Row, London. Pearse AGE. (1980) Histochemistry, Theoretical and Applied, Vol. 2, 4th ed., Churchill Livingstone, Edinburgh. Pearse AGE. (1985) Histochemistry, Theoretical and Applied, Vol. 3, 4t11 ed., Churchill Livingstone, Edinburgh. Penney DP, Powers JM, Frank M, Churukian C. (2002) Biotech Histochem 77 (5–6): 237–275. Reynolds JI, Moyes RB, Breakwell DP. (2009) "Differential staining of bacteria: acid fast stain". Current Protocols in Microbiology. Appendix 3: Appendix 3H. Ryan KJ, Ray CG. eds. (2004) Sherris Medical Microbiology (4th ed.) McGraw Hill. pp. 232–3. Sheehan DC, Hrapchak BB. (1980) Theory and practice of histotechnology. 2nd ed. St. Louis, MO: The C.V. Mosby Company. Suvarna SK, Layton C, Bancroft JD. (2013) Bancroft’s Theory and Practice of Histological Techniques. 7th ed. Churchill Livingstone, Elsevier. Wells J. (1988) A Technique for Staining the Superficial Cells of Plucked Hair Follicles and Other Solid Tissues, Stain Technology, Vol 63, No3. CHAPTER 17 STAINS AND STAINING SOLUTIONS Biological stains or coloring substances are prepared from dyes which may generally be divided into two categories: 1. Natural dyes - e.g., cochineal dyes, logwood dyes, and vegetable extracts 2. Synthetic (artificial) dyes - e.g., aniline or coal tar dyes NATURAL DYES Natural dyes are those obtained from plants and animals, previously utilized for dyeing of wool and cotton. Among the most common natural dyes available are: 1. Hematoxylin 2. Cochineal dyes and its derivatives 3. Orcein 4. Saffron 1. HEMATOXYLIN Hematoxylin is a natural dye derived by extraction from the core or the heartwood of a Mexican tree known as "Hematoxylin Campechianum”. It is by far the most valuable staining reagent used by the cytologist due to its powerful nuclear and chromatin staining capacity, and its striking polychrome properties which may be produced with proper differentiation. It may be used after almost any fixative and is a permanent stain. Hematoxylin itself is not a true basic dye. The active coloring agent is hematin, which is formed by the oxidation of hematoxylin, a process known as "ripening." This is usually accomplished by exposing the substance to air and sunlight, thereby oxidizing hematoxylin (natural ripening). Such a process is slow and takes as long as 3-4 months, but it can be accelerated by adding strong oxidizing agents such as hydrogen peroxide, mercuric oxide, potassium permanganate, sodium perborate or sodium iodate which converts hematoxylin to hematin almost instantaneously by chemical oxidation (artificial ripening), so that the staining solution is ready for use immediately after preparation. It is essential that the oxidant be used in correct amount, since excessive oxidation (over-ripening) leads to production of other useless compounds. Using the least amount of oxidant will result in satisfactory staining and longer life of the stain. Ripened hematoxylin is seldom used alone due to its inherent low affinity for the tissue itself. It is most frequently used in combination with alum, iron, chromium and copper salts, which act as mordants catalyzing or forming links between the hematin stain and the tissue. Mordants are substances that combine with the tissue and the staining solution, forming a "bridge" that allows staining reaction to take place. Alum hematoxylin stains are recommended for progressive staining of tissues, and are usually counterstained with Eosin, Congo Red and Safranin. Both the Ehrlich’s solution and the Harris’ solution contain Alum Hematoxylin. Rapid ripening of Ehrlich’s reagent, however, is brought about by the addition of Sodium Iodate; while Harris solution is ripened with Mercuric Chloride. Iron hematoxylin compounds are used only for differential or regressive staining, using Acid-Alcohol as a differentiating agent. An example of an Iron Hematoxylin compound is Weigert’s Stain using Iron (Ferric) Chloride. Copper hematoxylin solutions are utilized for the study of spermatogenesis. Hematoxylin and eosin (H&E) staining protocol is used frequently in histology to examine thin sections of tissue. Hematoxylin stains cell nuclei blue, while eosin stains cytoplasm, connective tissue and other extracellular substances pink or red. Eosin is strongly absorbed by red blood cells, coloring them bright red. In a skillfully made H & E preparation the red blood cells are almost orange, and collagen and cytoplasm (especially muscle) acquire different shades of pink. When the staining is done by a machine, the subtle differences in eosinophilia are often lost. Hematoxylin stains the cell nucleus and other acidic structures (such as RNA-rich portions of the cytoplasm and the matrix of hyaline cartilage) blue. In contrast, eosin stains the cytoplasm and collagen pink. 2. COCHINEAL DYES Cochineal dye is an old histologic dye extracted from the female cochineal bug (Coccus Cacti), which is treated with alum to produce the dye, carmine. It is widely used as a powerful chromatin and nuclear stain for fresh material and smear preparations. When combined with picric acid (picrocarmine), it is extensively used in neuropathological studies; and when combined with aluminum chloride (Best's carmine stain), it is used for the demonstration of glycogen. 3. ORCEIN Orcein is a vegetable dye extracted from certain lichens which are normally colorless, but which, when treated with ammonia and exposed to air, produce blue or violet colors. It is a weak acid, is soluble in alkali, and is mainly used for staining elastic fibers. Litmus is also obtained from lichens, treated with lime and soda, and exposed to ammonia and air. It is, however, not used as a cytological stain because of its poor staining property. It is instead, used mainly as an indicator. SYNTHETIC DYES Synthetic dyes are sometimes known as "Coal Tar Dyes" since they were originally manufactured from substances that have been taken from coal tar. They are derived from the hydro-carbon benzene (C6H6), and are collectively known as Aniline Dyes. Chromophores are substances with definite atomic groupings and are capable of producing visible colors. Simple benzene compounds which contain such substances are known as chromogens. These are different from the dyes in that any color that they impart to the tissue is not permanent and can, therefore, be easily removed. Before a chromogen can properly be called a dye, it must have the property of retaining its color in the tissue. This property is acquired by the addition of an auxochrome, an auxiliary radical or substance which imparts to the compound the property of electrolytic dissociation, thereby altering the shade of the dye, enabling it to form salts with another compound, and ultimately retaining its color. A dye, therefore, should consist of a chromophore and an auxochrome group attached to a hydrocarbon benzene ring. The coloring property is attributed to the chromophore, and the dyeing property to the salt-forming auxochrome. Depending on where the coloring substance (chromophore) is found, dyes may be classified into three groups: 1. Acid Dyes - where the active coloring substance is found in the acid component, and the inactive base, e.g. acid fuchsin, is usually the sodium salt of a sulfonate of rosaniline. One example of such a dye is picric acid, which has the ability to form salt with an alkali. Picric acid is outstanding in the sense that it is the only substance so far that can fix, differentiate and stain tissue all by itself. It may be employed as a counterstain to basic cytoplasmic stains, to acid fuchsin in Van Gieson's connective tissue staining, or to crystal violet for the microscopic study of fungi. It may also be used as a fixative, as a decalcifying agent, or as a tissue softener. Trichloracetic acid, picric acid and chromium-fixed tissues usually take in acidic dyes more readily. Basic cell structures (collagen, eosinophilic granules of leukocytes, etc.) have an affinity for the acid dye ions and are regarded as acidophilic. 2. Basic Dyes - where the active coloring substance is found in a basic component that combines with the acid radical (usually taken from sulfuric, acetic or hydrochloric acid). An example of a basic nuclear stain is methylene blue, which may be used both as an indicator and as a dye. It is very widely used in microbiology for bacterial staining. Tissues fixed with mercuric chloride and formaldehyde usually favor staining with basic dyes. Acidic cell structures (chromatin, mucus, cartilage matrix etc.) have an affinity for basic dye ions and are therefore regarded as basophilic. 3. Neutral Dyes - are formed by combining aqueous solutions of acid and basic dyes, capable of staining cytoplasm and nucleus simultaneously and differentially. Because they are made up of large molecular complexes, neutral dyes are insoluble or barely soluble in water, but they are usually soluble in alcohol. Ethyl alcohol or acetic acid-fixed tissues, on the other hand, readily take in both basic and acidic dyes. Examples of neutral dyes are Romanowsky dyes used in hematology, Giemsa's stain, and Irishman's stain for leukocyte differentiation. COMMON STAINING SOLUTIONS HEMATOXYLIN Hematoxylin is the staining solution most commonly used for routine histologic studies. The mordants used to demonstrate nuclear end cytoplasmic structures are alum and iron, forming lakes or colored complexes (dyemordant-tissue complexes), the color of which will depend on the salt used. Aluminum salt lakes are usually colored blue while ferric salt lakes are colored blue-black. The most commonly used staining system is called H&E (Hematoxylin and Eosin). H&E contains the two dyes hematoxylin and eosin. Hematoxylin can be considered as a basic dye (general formula for basic dyes is: Cl- dye). Hematoxylin is actually a dye called hematin (obtained from the log-wood tree) used in combination with aluminum ions (Al3+). It is used to stain acidic (or basophilic) structures a purplish blue. (Hematoxylin is not strictly a basic dye, but it is used with a 'mordant' that makes this stain act as a basic dye. The mordant (aluminum salts) binds to the tissue, and then hematoxylin binds to the mordant, forming a tissue-mordant-hematoxylin linkage). Eosin is an acidic dye: it is negatively charged (general formula for acidic dyes is: Na+ dye-). It stains basic (or acidophilic) structures red or pink. This is also sometimes termed 'eosinophilic'. Thus the cytoplasm is stained pink, by H&E staining. Thus the nucleus is stained purple by H&E staining. This means that the nucleus, and parts of the cytoplasm that contain RNA stain up in one color (purple), and the rest of the cytoplasm stains up a different color (pink). Aluminum Hematoxylin Solutions Aluminum (alum) hematoxylin stains are recommended for progressive staining of tissues, (i.e. staining for a predetermined time to adequately stain the nuclei but leave the background tissue relatively unstained, to be later counterstained with eosin, Congo red or safranin). The alum hematoxylins can also be used for regressive staining, meaning that the section is overstained, and then di fferentiated in acid alcohol followed by "blueing". Aluminum salts give a blue lake, and increase the selectivity for nuclei, especially if acid is added or is used as a differentiating agent. The two main alum hematoxylin solutions employed are Ehrlich's hematoxylin and Harris hematoxylin solutions. Rapid ripening of Ehrlich's reagent is brought about by the addition of sodium iodate; while Harris solution is ripened with mercuric chloride. Alum or potassium aluminum sulfate, when used as the mordant, usually dissociates in an alkaline solution, combining with -OH of water to form insoluble aluminum hydroxide. In the presence of excess acid, aluminum hydroxide cannot be formed, with ultimate failure of aluminum hematoxylin dye-lake to form, due to lack of -OH ions. Hence, acid solutions of alum hematoxylin become red. During staining, alum hematoxylin stained sections are usually passed on to an alkaline solution (e.g. 1% hydroxide) in order to neutralize the acid and free the OH group, to form an insoluble blue aluminum hematin-tissue-lake. Such procedure is known as blueing. For blueing of alum-hematoxylin -stained sections, warm (40° to 50°C) tap water is commonly used, since it is generally sufficiently alkaline. When tap water is not sufficiently alkali ne, or is even acid, and is unsatisfactory for blueing hematoxylin, lithium carbonate (1% w/v in water), bicarbonate (0.2 to 0.5% w/v in tap water), and potassium or sodium acetate may be used. Alternatively, Scott's Tap Water Substitute (T.W.S.) consisting of 33.5 gm. NaHC04 and 20 grams MgS04, in 1000 cc of water, with thymol (to inhibit the formation of molds), is used to accelerate blueing of thin paraffin sections. Blueing with ammonia, lithium carbonate or Scott's Tap Water Substitute has more rapid action (about 15, 30 and 60 seconds respectively), compared to the 5 to 15 minutes required for warm tap water to "blue" hematoxylin. Ammonia water, used to blue stains, may be prepared by mixing 2 cc. of strong ammonium hydroxide with 98 cc of tap water. Ammonia (0.5 to 1% in 80% alcohol) may be "hard" on delicate tissues and may loosen and cause sections to fall off the slides during staining. Lithium carbonate has a tendency to form crystalline deposits unless the slides are agitated in it and washed well afterwards. The use of very cold water slows down the process while warming accelerates it. In fact, the use of very cold water (below 10°C) for blueing sections may even produce pink artifact discolorations on the tissue. Ehrlich's Hematoxylin FORMULA: Hematoxylin 2 gm Absolute ethyl alcohol 100 ml Aluminum potassium Sulfate 15 gm approximately Glycerin 100 ml Distilled water 100 ml Glacial acetic acid 10 ml Dissolve hematoxylin in absolute ethyl alcohol with gentle heat. Dissolve the potassium alum in distilled water and glycerin with gentle heating and shake (glycerin is added to slow the oxidation process and prolong the shelf life of hematoxylin). Mix the two solutions and add glacial acetic acid. Expose to air and sunlight for several weeks or months in a flask lightly plugged with cotton, shaking daily. Transfer in a well-stoppered bottle and store in a warm place. This naturally ripening alum hematoxylin takes about 2 months to ripen, but its staining property will last for months or years. Hematoxylin may be partially oxidized iodate to hasten ripening by addition of 0.3 gm Sodium, but this will also inevitably shorten the shelf life of the stain. As hematoxylin solution becomes oxidized, the color of the solution will change from purplish to deep red, while the pungent odor of acetic acid will be replaced by a pleasant aroma. Glycerin acts as a stabilizer, retards evaporation of the solution, and appears to slow down ripening, so that it may be added 4-6 weeks after the initial preparation. Ehrlich's hematoxylin is generally used for regressive staining, and differentiated with I % hydrochloric acid in 70% alcohol (acidalcohol) until the nucleus is selectively stained. Mucopolysaccharide substances such as cartilage and cement lines of bones are also stained intensely blue. It is suitable for tissues that have been subjected to acid decalcification, and is especially useful for tissues that have been become acidic during prolonged storage in formalin. Ehrlich's hematoxylin is not an ideal stain for frozen sections. Staining time is usually 15-40 minutes. Harris Hematoxylin FORMULA: Hematoxylin 1 gm Absolute ethyl alcohol 10 ml Ammonium/Potassium alum 20 gm Distilled water 190 ml Mercuric oxide (red) 0.5 gm Glacial acetic acid 10 ml Dissolve hematoxylin in absolute ethyl alcohol with gentle heating. Dissolve ammonium or potassium alum in distilled water on a large (500 ml. capacity) boiling flask or beaker. Add hematoxylin solution and boil. Add mercuric oxide and plunge immediately into cold water for rapid cooling. A large beaker should be used, because the violent liberation of oxygen will cause the solution to explode from a narrow-mouthed flask. The solution should assume a dark purple color when ripened by mercuric oxide. The addition of 4% glacial acetic acid will give a more precise nuclear staining. The solution is then filtered and transferred into a well-stoppered bottle. Harris hematoxylin is a good regressive stain that may either be used immediately or stored for future use, since it remains stable for a long time (about 6 months). Since most of the alcohol is evaporated in the process of boiling, 10 ml. of ethyl alcohol may be added to the final solution, to help prevent the growth of molds. The precipitate that forms on prolonged storage should be filtered off before use. Harris hematoxylin is widely used for routine nuclear staining, in exfoliative cytology, and for staining of sex chromosomes. The usual staining time is 5-20 minutes, depending on the batch and age of stain, the nature of tissue, and the degree of staining required. Best results are obtained when the solution is made every 2 or 3 months. The formation of precipitate in the stored staining solution indicates deterioration in nuclear staining property. The stain should be filtered before use, and staining time may need to be increased at this stage. Cole's Hematoxylin Cole's hematoxylin is another alum hematoxylin solution recommended for routine purposes, especially used in sequence with Celestine blue. This alum hematoxylin is artificially ripened with an alcoholic iodine solution. It is ready for immediate use, but may need filtering after storage, as with Harris hematoxylin. FORMULA: Hematoxylin 1.5 gm 1% Iodine in 95% Alcohol 50 ml Sat. Aq. Ammonium Alum 700 ml Distilled Water 250 ml Dissolve hematoxylin in warm distilled water and mix with iodine. Add alum solution and boil. Cool and filter before use. Staining time is 10 minutes. Mayer's Hematoxylin This is an alum hematoxylin that is chemically ripened with sodium iodate. Like any alum hematoxylin, it can be used as a regressive stain, but it is also useful as a progressive stain. It is used as a n uclear counterstain to demonstrate the presence of cytoplasmic glycogen by special stain. It is also used in instances when acid-alcohol differentiation might destroy or decolorize the stained cytoplasmic components like mucopolysaccharides. It is used in Celestine Blue hemalum method of nuclear staining. FORMULA: Hematoxylin 1 gm Sodium iodate 0.2 gm Potassium alum 50 gm Citric acid 1 gm Chloral hydrate 50 gm Distilled water 1000 ml Allow hematoxylin, alum and sodium iodate to dissolve in water overnight. Add chloral hydrate and citric acid. Boil for 5 minutes and cool. The addition of sodium iodate immediately ripens the hematoxylin. Citric acid is usually added after potassium alum has been dissolved (by shaking the solution); however, the addition of 20 ml. glacial acetic acid seems to give better nuclear staining and a more stable solution. Chloral hydrate is added to the final solution as a preservative. One disadvantage of Mayer's hematoxylin is that it can be stored only for 3 to 6 months at the most. Iron Hematoxylin Solutions Iron hematoxylin compounds are used only for differential or regressive staining, using acid-alcohol as a differentiating agent. Two main iron hematoxylin solutions are employed for routine work in the laboratory: Weigert's Solution, using ferric ammonium chloride, and Heidenhain's solution, using ferric ammonium sulfate (iron alum) as mordants. The dye lake obtained when ferric salts are used as mordants is an intense blue-black one. They can be applied to tissues fixed in virtually all fixatives, producing permanent stains, provided all iron mordants have been wiped out. Tissues that have been stored in alcohol for years and which would ordinarily fail to stain, will normally take iron hematoxylin. Tissue structures are stained blackish or grayish, according to the extent of differentiation, producing minimal eyestrain; hence, making it useful for photomicrography. Solutions prepared with correct or optimal amounts of iron salts (0.5 g. metallic iron for each 1 gram of hematoxylin) are used for dense, regressive staining (e.g. myelin methods) . The stain becomes more selective for nuclei if acid or an excess of ferric salt is added. Ferric salts ripen hematoxylin rapidly and are active oxidizing agents; hence, they do not keep well as a prepared mixture. In mixtures of hematoxylin and ferric salts, the insoluble lake gradually precipitates out, so that premixed stains are not very stable. Regaud's Hematoxylin for Mitochondria: Among the many methods used to demonstrate mitochondria by light microscopy, the most permanent and the simplest is Regaud's modification of iron hematoxylin on sections of material fixed in potassium dichromate and formalin and subsequently mordanted in dichromate. After staining, the slides are differentiated to remove the hematoxylin from most cytoplasmic components other than mitochondria. Unfortunately, the results are not uniform: some cells will be over-stained and some under-stained. Therefore a number of microscopic fields should be examined. Weigert's Hematoxylin Solution FORMULA: SOLUTION A: Hematoxylin 1 gm Absolute ethyl alcohol ml SOLUTION B: 30% anhydrous ferric chloride 4 ml Concentrated hydrochloric acid 1 ml Distilled water 100 ml Hematoxylin is dissolved in alcohol with gentle heating, while ferric chloride, hydrochloric acid and water are mixed in a different container. Both solutions are stable and may be stored separately for 6 weeks before use. Ferric chloride is usually added to the staining solution just before use, by mixing equal parts of the two solutions to produce a deep black mixture. The working solution will remain active for 1-2 days. It changes color from a deep blueblack-violet, through violet, purple, brown and yellowish brown within 2 to 3 weeks, as it becomes less and less stable. A solution that has turned brown should be discarded. Weigert's solution is the standard iron hematoxylin stain used in the laboratory, especially for demonstrating muscle fibers and connective tissues. It is particularly recommended when the preceding stains contain acid (e.g. Van Gieson stain containing picric acid) which decolorizes nuclei stained with alum hematoxylin. Heidenhain's Hematoxylin It is a popular cytological stain, especially for the study of mitosis. It can be used after almost any fixative. Chromatin material (nuclear network and chromosomes) blue black. FORMULA: MORDANT DIFFERENTIATOR: Ferric ammonium sulfate 2.5 gm Distilled water 100 ml HEMATOXYLIN STAIN: Hematoxylin 1.5 gm 95% ethyl alcohol 10 ml Distilled water 90 ml Hematoxylin is dissolved in ethyl alcohol and added with water, allowed to ripen for 4-5 weeks, and stored in tightly stoppered bottles. This iron hematoxylin uses ferric ammonium sulfate as oxidant/mordant, and the same solution as the differentiating fluid. The mordant differentiator is used separately during the process of staining, instead of being added to the solution. Heidenhain's solution is a cytological stain recommended for regressive staining of thin sections. After staining, all components are black or dark grey black. The hematoxylin staining is moved progressively from different tissue structures at different rates using the iron alum solution. Differentiation can be more easily controlled if the differentiating iron alum solution is diluted with an equal volume of distilled water or an alcoholic picric acid solution. It is utilized for the demonstration of both nuclear and cytoplasmic inclusions such as chromatin, chromosomes, nucleoli, centrosomes, and mitochondria. Voluntary muscle striations and myelin are also well stained. Phosphotongstic Acid Hematoxylin (PTAH) There are many variants of the original Mallory PTAH technique, combining hematoxylin with 1% aqueous phosphotungstic acid, which acts as a mordant. Natural ripening of the tungsten hematoxylin solution is achieved with light and air, but will take some months to ripen. FORMULA: Hematoxylin 1 gm Phosphotungstic acid 20 gm Distilled Water 1000 ml Dissolve the solids in separate portions of distilled water. Add together and stand in the light to ripen for several weeks. Immediate ripening may be obtained by adding 50 ml of 0.25% aqueous potassium permanganate after the two solutions are mixed, so that stain can be used the next day, although peak staining activity is not reached until after 7 days. When hematin is used instead of hematoxylin to prepare a staining solution, the oxidation process is not necessary and the staining solution can be used immediately, but its staining activity is comparatively short-lived. The color of the solution ranges from reddish-brown to purple, although this is not a reliable guide for the study of stained tissues. Nuclei, fibrin, muscle striations, and myofibrils are colored blue while collagen, bone and cartilage take an orange-red or brownish red to deep brick-red stain. Staining is usually progressive, hence, microscopic examination of the materials every hour is recommended. Ninety-five percent alcohol usually removes the red component of the stain, so that dehydration and rinsing of sections should be brief. Phosphotungstic acid hematoxylin stain usually demonstrates structures in paraffin as well as celloidin and frozen sections. Staining time is usually 12-24 hours. EOSIN Eosin is one of the most valuable stains used for differentially staining connective tissues and cytoplasm. It is a red general cytoplasmic stain that combines with hemoglobin to give an orange color. It is an acid dye and the terms acidophilic, oxyphilic and eosinophilic are often used interchangeably. It may be used after any fixative and is routinely used in histopathology as a counterstain to hematoxylin, imparting a pink or red color to cytoplasmic material, cell membranes, and some extracellular structures. It is commonly used as a background stain because it gives a pleasing and colorful contrast to nuclear stains, particularly in chromate and picric acid fixed tissues, and in acid decalcified materials which are strongly stained with eosin. Yellowish (Eosin Y) -is the most commonly used. It is readily soluble in water, less in alcohol, available in both aqueous and alcoholic solutions, showing a green yellow fluorescence especially in alcoholic medium. The aqueous stain is generally used as a I % solution for 15 seconds to 3 minutes, depending on the tissue, type of fixative and intensity of color desired. Slightly longer staining time is required after formalin than after Zenker’s solution. The other eosin compound is Eosin B (eosin bluish or imperial red); it has a very faint bluish cast. The two dyes are interchangeable, and the use of one or the other is more a matter of preference and tradition. Eosin S and Eosin B are now rarely used. 5% Aq ueous Eosin Y FORMULA: Eosin Y 5 gm Distilled water 100 ml Dissolve in water by gentle heating. Cool and filter. Thymol crystals may be added to prevent formation of molds. Eosin, Stock Alcoholic Solution FORMULA: Eosin Y 1 gm Distilled water 20 ml 95% alcohol 80 ml Dissolve Eosin Y in water by gentle heating. Cool and add alcohol. For use, one part of the stock solution is usually diluted with three parts of 80% alcohol. Addition of 0.5 ml. glacial acetic acid for every 100 ml. of stain will usually give a deeper red stain to the tissue. Differentiation of the eosin stain ing occurs in the subsequent tap water wash, and a little further differentiation occurs through the alcohols. Combining eosin Y and phloxine B produces a cytoplasmic stain that demonstrates various tissue components more dramatically. Eosin-Phloxine B Solution FORMULA: 1% phloxine 10 ml 1% eosin Y 100 ml 95% alcohol 780 ml Glacial Acetic Acid 4 ml Romanowsky Stains The Romanowsky stains are all based on a combination of eosinate (chemically reduced eosin) and methylene blue (sometimes with its oxidation products azure A and azure B). Common variants include Wright's stain, Jenner's stain, Leishman stain and Giemsa stain. All are used to examine blood or bone marrow samples. They are preferred over H&E for inspection of blood cells because different types of leukocytes (white blood cells) can be readily distinguished. All are also suited to examination of blood to detect blood-borne parasites like malaria. OTHER STAINS Acid Fuchsin-Picric Acid (Van Gieson’s Stain) is a mixture of picric acid and acid fuchsin for demonstration of connective tissues. FORMULA: Picric acid, saturated aqueous solution 100 ml Acid fuchsin (1 % aqueous solution) 5 ml The solution weakens after long standing and may be strengthened by adding a few drops of fresh acid fuchsin. Acid Fuchsin (Masson Stain) may be used to stain collagen, smooth muscle, or mitochondria. Acid fuchsine is used as the nuclear and cytoplasmic stain in Mallory's trichrome method. Acid fuchsine stains cytoplasm in some variants of Masson's trichrome. In Van Gieson's picro-fuchsin, acid fuchsin imparts its red color to collagen fibers. Acid fuchsin is also a traditional stain for mitochondria. FORMULA: Acid fuchsin 1 gm Glacial acetic acid 1 ml Distilled water to make 100 ml Picro-Fuchsin Solution FORMULA: 1% Acid fuchsin 13 ml Saturated aqueous picric acid 87 ml ACRIDINE ORANGE is a basic acridine fluorochrome which permits discrimination between dead and living cells, giving green fluorescence for DNA and a red fluorescence for RNA. It is a nucleic acid selective fluorescent cationic dye useful for cell cycle determination. When bound to DNA, it is very similar spectrally to fluorescein. Like fluorescein, it is also useful as a nonspecific stain for backlighting conventionally stained cells on the surface of a solid sample of tissue (fluorescence backlighted staining). ACRIDINE RED 3B is used to demonstrate deposits of calcium salts and possible sites of phosphatase activities. ALCIAN BLUE - is a complex, water-soluble phthalocyanin dye, similar to chlorophyll, which stains acid mucopolysaccharides by forming salt linkages with them. It is an excellent stain because it is simple, it produces a striking blue color, and it is resistant to various counterstaining procedures. It is more specific for connective tissue and epithelial mucin due to its use as an acid solution. Alcian blue is often combined with PAS, as it stains acidic mucins blue, whereas PAS stains neutral mucins red, hence it can be used to distinguish elements of the extracellular matrix. FORMULA: Alcian blue 1 gm Glacial acetic acid 1 ml Distilled water add up to 100 ml ALIZARIN RED S forms an orange-red lake with calcium at a pH of 4.2. It works best with small amounts of calcium (such as in Michaelis-Gutman bodies). The alizarin method is also used on the Dupont ACA analyzer to measure serum calcium photometrically. ANILINE BLUE is a cytoplasmic stain used for counterstaining of epithelial sections. FORMULA: Aniline blue 1 gm Distilled water 97.5 ml Glacial acetic acid 2.5 ml AZOCARMINE: Nuclei are deep red; cytoplasm is a pale red. BASIC FUCHSIN - is a plasma stain utilized also for deep staining of acidfast organisms, for mitochondria, for differentiation of smooth muscles with the use of picric acid. It is a main constituent of Feulgen's and Schiff's reagent for the detection of aldehydes, of Van Gieson's solution for connective tissues, mucin, and for elastic tissue staining. a. CARBOL-FUCHSIN FORMULA: Basic fuchsi n 1 gm Phenol crystals 5 gm Absolute ethyl alcohol 10 ml Distilled water 100 ml Grind basic fuchsin and phenol together in a mortar. Add alcohol and then water. Boil in a beaker and stand for 24 hours to cool. Filter before use. 2. COLEMAN'S FEULGEN REAGENT FORMULA: Basic fuchsin 1 gm Sodium metabisulphite 1 gm 1N hydrochloric acid 10 ml Distilled water 200 ml Boil water, remove from heat and add basic fuchsin. Cool and add sodium metabisulphite and hydrochloric acid. Stand for 24 hours and filter through activated charcoal to get a colorless filtrate. Store in a refrigerator. c. SCHIFF'S REAGENT FORMULA: Basic fuchsin 1 gm Sodium metabisulfite anhydrous 1 gm Distilled water 200 ml Normal hydrochloric acid 20 ml Boil water. Add basic fuchsin and dissolve by stirring. Cool to 50°C, filter and add hydrochloric acid. Cool to 25°C and add sodium metabisulphite. Let stand for 24 hours until the solution becomes pale-straw in color. Filter through activated charcoal to form a colorless filtrate. Store in a refrigerator. d. MALLORY'S FUCHSIN STAIN FORMULA: Basic fuchsin 0.5 gm 95% ethyl alcohol 50 ml Distilled water 50 ml Dissolve fuchsin in alcohol by gentle heating. Add water, cool, and filter. e. ALDEHYDE FUCHSIN (GOMORl'S STAIN) FORMULA: Concentrated hydrochloric acid 1 ml Paraldehyde 1 ml 0.5% basic fuchsin in 70% alcohol 100 ml Stand at room temperature for 24 hours until the mixture becomes deep purple in color. Store in refrigerator. BENZIDINE is used for staining hemoglobin. FORMULA: Solution A Benzidine 0.5 gm Absolute alcohol 50 ml Sodium nitroprusside 0.1 gm Distilled water up to 100 ml Dissolve benzidine in alcohol. Dissolve sodium nitroprusside in 10 ml. distilled water. Mix and make up to 100 ml. with the remaining distilled water. Solution B Absolute alcohol 50 ml Glacial acetic acid 2 ml Hydrogen peroxide 30% 0.5 ml Sodium nitroprusside 0. 1 gm Distilled water up to 100 ml Both solutions A and B should be freshly prepared. BISMARCK BROWN - is used as a contrast stain for Gram's technique, in acid fast and Papanicolau method, and for staining diphtheria organisms. CARMINE - is used as a chromatin stain for fresh materials in smear preparations. It is slightly soluble in water at a neutral reaction, and usually kept in ammoniacal solution which changes its properties due to oxidation. The most important component of carmine is carminic acid, which is also useful in industry and analytical chemistry. It can be used for determining the presence of certain metal ions, such as aluminum. A dry powder is often prepared in the form of carmine aluminum calcium lake ("carmine alum lake"). It is usually combined with aluminum chloride to stain glycogen (Best Carmine solution). Best Carmine Stain (Stock Solution) FORMULA: Carmine 2 gm Potassium carbonate 1 gm Potassium chloride 5 gm Distilled water 60 ml Concentrated ammonia 20 ml Grind carmine in a mortar and add potassium carbonate and potassium chloride to water. Boil gently in a large flask (to avoid frothing) for 5 minutes. Cool and add ammonia. Store in a dark bottle inside the refrigerator. Stain will keep well for about 3 months after preparation. Best Carmine Working Solution FORMULA: Best carmine (stock solution) 2 parts Ammonia concentrated 2 parts Absolute methyl alcohol 3 parts Best's Differentiator FORMULA: Absolute methyl alcohol 40 ml Absolute ethyl alcohol 80 ml Distilled water 100 ml CARMALUM (MAYER'S) SOLUTION -is a mordanted dye acting as a basic dye and staining acidic substances. FORMULA: Carminic acid 0.5 gm Potassium alum 5 gm Distilled water 100 ml Salicylic acid 0.05 gm Sodium salicylate 0.25 gm Warm the solution to dissolve the constituents. Filter when cool, then add salicylic acid and sodium salicylate. CELESTINE BLUE - Celestine Blue is an oxazine dye used as an alternative to iron hematoxylin nuclear stain, producing a strong and precise nuclear stain that is resistant to decolorization by succeeding acid stains and solutions. Celestine blue forms a strong staining lake with iron alum, acting as a mordant to bind hematoxylin. It is resistant to strong acid dyes, and is recommended for routine staining of fixed sections, giving a good nuclear definition when used in conjunction with alum hematoxylin. FORMULA: Ferric ammonium sulfate 5 gm Distilled water 100 ml Celestine blue 0.5 gm Glycerin 14 ml Dissolve ferric ammonium sulfate in water overnight at room temperature. Add Celestine blue; Boil for 3 minutes. Cool and filter, then add glycerin. CONGO RED - is best known as an indicator, but may be utilized as a stain for axis cylinders in embryos. It is used as a 4% aqueous solution in staining elastic tissues and myelin. Congo red is used to identify deposits of protein in tissue called amyloid. CRESYL VIOLET - is commonly used in histology to stain nervous tissues. Cresyl violet stains the acidic components of the neuronal cytoplasm (specifically Nissl bodies) a violet color. CRYSTAL VIOLET - is a nuclear or chromatin stain used for staining amyloid in frozen sections and platelets in blood. Gentian violet is the staining solution formed by the mixture of crystal violet, methyl violet and dexterin. ETHIDIUM BROMIDE intercalates and stains DNA, providing a fluorescent red-orange stain. Although it will not stain healthy cells, it can be used to identify cells that are in the final stages of apoptosis –such cells have much more permeable membranes. Consequently, ethidium bromide is often used as a marker for apoptosis in cells populations and to locate bands of DNA in gel electrophoresis. The stain may also be used in conjunction with acridine orange (AO) in viable cell counting. This EB/AO combined stain causes live cells to fluoresce green whilst apoptotic cells retain the distinctive red-orange fluorescence. GIEMSA STAIN – consists of a mixture of methylene-blue and eosin, and it is used for staining blood to differentiate leukocytes. It is mostly used on methanolfixed blood films, where it stains erythrocytes pink and the different types of leukocyte, allowing their identification according to size and shape of their nuclei. It also binds to some pathogens, including spirochetes (syphilis), trypanosomes (sleeping sickness and Chagas disease) and plasmodium (malarial parasites). In addition it can also be used to stain some bacteria in tissue sections pink, and it is therefore particularly useful if infection is suspected. FORMULA: Giemsa stain 1 gm Glycerin 66 ml Absolute methyl alcohol 66 ml Mix glycerin and Giemsa stain and place in oven at 60°C for 30 minutes to 2 hours then add methyl alcohol. GOLD SUBLIMATE - is the stain used for metallic impregnation, made up of gold chloride and mercuric chloride. FORMULA: Mercuric chloride 0.4 gm Distilled water 60 ml 1% Gold chloride (brown) 10 ml Dissolve mercuric chloride in water by gentle heating. Cool and add gold chloride, store in a dark place, or mix immediately before use. IODINE - is probably the oldest of all stains, originally used for microscopic study of starch granules. It stains amyloid, cellulose, starch, carotenes and glycogen. It is widely used for removal of mercuric fixative artefact pigments, and as a reagent to alter crystal and methyl violet so that they may be retained by certain bacteria and fungi. It may also be used in the form of aqueous or alcoholic solutions. Gram's Iodine - is used to identify and differentiate bacteria. For example, staphylococci, streptococci and pneumococci are gram-positive and stain a deep blue, whereas coliforms and Neisseria are gram-negative and stain pink. FORMULA: Iodine 1 gm. Potassium iodide 2 gm. Distilled water 300 ml. Dissolve potassium iodide in a little water. Add iodine and dissolve in the remaining water. Gram's Iodine is used in Gram Weigert method of staining microorganisms and fibrin in tissue sections. Lugol's solution or Lugol's iodine Lugol’s solution is a brown solution that turns black in the presence of starches and can be used as a cell stain, making the cell nuclei more visible. Iodine is also used as a mordant in Gram's staining, it enhances dye to enter through the pore present in the cell wall/membrane. FORMULA: Iodine 1 gm Potassium iodide 1 gm Distilled water 100 ml Lugol's Iodine is used as a test for glycogen, amyloid, and corpora amylacea. JANUS GREEN B - is used for demonstrating mitochondria during intravital staining. MALACHITE GREEN - has sometimes been used for staining erythrocytes is a weakly basic dye used as a contrast stain for staining ascaris eggs and erythrocytes, and as a bacterial spore stain; it is also used both as a decolorizer and as a counterstain. By itself, this dye is not all that good for general microscopy, being perhaps in the same category as tartrazine. Like tartrazine, malachite green is primarily a counterstain; this means it gives general color to areas that have either failed to take up some other, more specific stain or which have been subjected to de-staining. FORMULA: 2% aqueous malachite green 220 ml Glacial acetic acid 30 ml Glycerol, C.M. Mix and store in a colored bottle. MASSON’S TRICHROME is (as the name implies) a three-color staining protocol. The recipe has evolved from Masson's original technique for different specific applications, but all are well-suited to distinguish cells from surrounding connective tissue. Most recipes produce red keratin and muscle fibers, blue or green staining of collagen and bone, light red or pink staining of cytoplasm, and black cell nuclei. METHYL GREEN - stains chromatin green in the presence of an acid. It gives false positive reactions with certain secretions such as mucin. Methyl green is used commonly with bright-field microscopes to dye the chromatin of cells so that they are more easily viewed. METHYLENE BLUE - is a common basic nuclear stain employed with eosin to provide marked differentiation of various structures in the tissue. It usually contains some azures or methylene violet. Methylene blue stains acidic cell parts (like the nucleus) blue and is a good counterstain with Eosin Y. It can be substituted for Janus Green B stain or Carmine stain. This methylene blue stain is a 1% aqueous solution. "Polychroming" involves the oxidation of methylene blue, resulting in loss of methyl groups and leaving lower homologues of the dye (azures) and deaminized oxidation products (thiazoles). The resulting mixture of methylene blue, azures and thiazoles is known as polychrome methylene blue. It stains nuclei blue while cartilage matrix, mucin, mast cell granules and connective tissues generally take a reddish-violet color. It is a valuable stain for plasma cells and may also be employed in cytological examinations of fresh sputum for malignant cells, as a bacterial stain for evaluation and differentiation of bacterial organisms, for diagnosis of diphtheria, and for vital staining of the nervous tissue. FORMULA: Methylene blue 1 gm Potassium carbonate 1 gm Distilled water 100 ml Mix in a flask that has been lightly plugged with the cotton or gauze and let stand at 37°C for weeks to oxidize. For use, dilute in 1:5 or 1:10 dilution with distilled water. This solution is available commercially. For rapid diagnosis, frozen sections are stained with polychrome methylene blue for I/2 to 1 minute, rinsed and mounted in an aqueous mountant, blotted dry, or cleared in xylene and mounted in Clarite, Permount or H.S.R. Mallory's Phloxine Methylene Blue Stain - originally known as EosinMethylene Blue (EMB) method, this technique produces a sharp nuclear stain and reveals with marked differentiation the various structures in the tissues, which should be fixed in Zenker's fluid. METHYLENE VIOLET - is a metachromatic dye formed whenever methylene blue is heated in fixed alkali or alkali carbonate, coloring nuclei of leukocytes reddish-purple in the presence of methylene blue. NILE RED (also known as Nile blue oxazone) is formed by boiling Nile blue with sulfuric acid. This produces a mix of Nile red and Nile blue. Nile red is a lipophilic stain; it will accumulate in lipid globules inside cells, staining them red. Nile red can be used with living cells. It fluoresces strongly when partitioned into lipids, but practically not at all in aqueous solution. OIL RED O is a dye that is more soluble in fat than in water or alcohols, hence it is used as a stain for neutral lipids. For example when myelin is broken down in the CNS, in diseases such as multiple sclerosis, macrophages take up the lipid-rich debris and stain strongly with this dye. The oil red O stain can identify neutral lipids and fatty acids in smears and tissues. Fresh smears or cryostat sections of tissue are necessary because fixatives containing alcohols, or routine tissue processing with clearing, will remove lipids. The ORO is a rapid and simple stain. It can be useful in identifying fat emboli in lung tissue or clot sections of peripheral blood. ORCEIN --is an excellent stain for elastic fibers, and is especially recommended in dermatological studies due to its ability to demonstrate the finest and most delicate fibers in the skin. OSMIUM TETROXIDE Osmic Acid or Osmium Tetroxide (OsO4) is a selective stain for unsaturated lipids and for lipoproteins such as myelin, which it stains black. Osmic acid, aside from being used as a fixative especially for electron microscopy, may be used to stain fat, although other substances are also stained simultaneously, thereby preventing specific staining of lipids to be done. Fat, which reduces osmium tetroxide to osmium dioxide, is stained black, and may be demonstrated from the tissue by using chrome-osmium solutions or by the frozen section method. PERIODIC ACID SCHIFF (PAS) is an all-around useful stain for many things. It stains glycogen, mucin, mucoprotein, glycoprotein, basement membranes, capsules, and blood vessels as well as fungi and intracellular carbohydrates such as glycogen in hepatocytes. Cells that secrete mucus are also strongly stained. A pre-digestion step with amylase will remove staining for glycogen. This method depends on the selective oxidation by periodic acid of free hydroxyl groups on two adjacent hydroxyl groups converting the alcohols to aldehydes. The aldehydes are then detected by the Schiff reagent, which stains them reddish purple. Other tissue components stain according to the counterstain used. Lead-hematoxylin or another basic stain is often the counterstain. PHOSPHOTUNGSTIC ACID - is a common negative stain for viruses, nerves, polysaccharides, and other biological tissue materials. This is an ideal stain for the demonstration of striated muscle fibers and mitochondria, which stain blue. A counterstain is often not used. PICRIC ACID - is employed as a contrast stain to acid fuchsin, for the demonstration of connective tissue (Van Gieson's stain), as a cytoplasmic stain in contrast to basic dyes, as a counterstain to crystal violet, as a tissue fixative, and as a decalcifying agent. PRUSSIAN BLUE - is an insoluble colored salt of ferric ferrocyanide (an iron cyanide compound) normally utilized for the manufacture of paints, but may be used for microanatomical color contrast of specimens and for demonstration of the blood and lymph vessels by injection (intravital staining). RHODAMINE B - is used with osmic acid to fix and stain blood and glandular tissues. SAFRANIN (or Safranin O) - is a nuclear stain. It produces red nuclei, and is used primarily as a counterstain. Safranin may also be used to give a yellow color to collagen. SILVER NITRATE - is used in 10% aqueous solution to prepare various dilutions to be used in identification of spirochetes, reticulum and other fiber stains. TOLUIDINE BLUE - is a nuclear stain for fixed tissues, used as a substitute for thionine in fresh frozen tissue sections. It is recommended for staining of Nissl granules or chromophilic bodies. It is a particularly versatile dye that stains nuclei blue, and can be used to differentiate different types of granules (e.g. within mast cells). Because it can permeate the resins that are used to embed sections for electron microscopy, it is often used as a preliminary stain, to identify sections that will later be examined by electron microscopy. VAN GIESON STAIN - binds to collagen in the extracellular matrix, staining it pink. Often it is combined with a stain for elastic fibers (elastic van Gieson) which stain black, allowing the two major elements of connective tissue to be differentiated. VICTORIA BLUE - is used for demonstration of neuroglia in frozen sections. VON KOSSA STAIN - is a silver reduction method that demonstrates phosphates and carbonates, but these are usually present along with calcium. This stain is most useful when large amounts are present, as in bone. WRIGHT STAIN - causes blood cells to exhibit four major staining properties that allow the cell types to be distinguished. Basophilia (affinity for methylene blue), azurophilia (affinity for the oxidation products of methylene blue called azures, which are reddish purple), acidophilia (affinity for eosin), and neutrophilia (affinity for a complex of dyes in the mixture, which are pale lilac). In a stained blood smear, erythrocytes bind eosin and appear orange to pink, nuclei purplish blue, basophilic granules very dark bluish purple, eosinophilic granules red to red-orange, neutrophilic granules reddish-brown to lilac, platelets violet to purple, and lymphocyte cytoplasm stains pale blue. OIL SOLUBLE DYES (LYSOCHROMES) Lysochromes (oil soluble dyes) are not real dyes in the usual sense of the word because they do not have auxochrome groups. They give color to lipids simply because they are more soluble in lipid medium of the tissues, than in their medium of 70% alcohol. Oil soluble dyes are available in the form of Sudan Black B. Sudan III and Sudan IV (Scharlach R), used for the demonstration of intracellular fats which are colored black, orange, and red, respectively. In order to penetrate fats, the oil soluble dyes (Sudan dyes) must be dissolved in organic sol vent, although the solvent vehicle (usually ethanol, isopropanol or propylene glycol) should be sufficiently dilute (aqueous) to avoid extracting the lipids themselves. Sudan Black Sudan Black is a stain that colors fat droplets black and is the most sensitive of the oil soluble dyes. It possesses two secondary amino groups per molecule, making it a slightly basic dye which may cause non-specific staining. Because of this molecular structure, Sudan black has a much greater affinity for phospholipids than other lysochromes -coloring neutral lipids (triglycerides) by simple dissolution of the dye. It has the added advantage of being a more sensitive coloring agent. The ability of fats to adsorb Sudan Black is related to dye concentration, temperature and physical state of the fats. Maximal dye uptake occurs when fat reaches its melting point, so that lipids that are liquid or semi-liquid at staining temperature will be stained while those that are crystalline or solid will not be affected by the dye. Sudan Black is prepared as a 0.5% solution boiled in 70% ethanol for 10 minutes under a reflux condenser, and filtered before use. It is a very unstable solution and should be discarded if the usual blue-black color turns brownish black. It usually imparts a black color on intracellular lipids, and is recommended for paraffin sections especially for tissues fixed in formol calcium with post chroming, demonstrating lipids that are resistant to paraffin embedding. Unlike the other Sudan dyes, Sudan Black B stains phospholipids as well as neutral fats. Sudan black B does not stain crystalline cholesterol, and free fatty acids tend to be soluble in the ethanolic dye bath. Sudan IV Sudan IV (Scharlach R) is different from Sudan Black because it has no secondary amino group and it does not color phospholipids or the fine lipid droplets. It is prepared by saturating the dye (Scharlach R) in one part of 2% benzoic acid (in 70% alcohol), and one part of acetone, forming a very stable solution which may be used repeatedly as long as it is filtered. Addition of benzoic acid intensifies fat and prevents rapid deterioration of the solutions. It is recommended for staining triglycerides (neutral lipids), giving them a deep and intense red stain. Sudan Ill Sudan III was the first Sudan dye to be introduced into histochemistry. It is also fat soluble, and is good as a fat stain for central nervous system tissues, giving a less deep and lighter orange stain compared to the darker staining Sudan IV. CHIEF SOLVENTS USED FOR STAINS 1. WATER - should always be distilled unless otherwise stated. 2. ALCOHOL - Ethyl alcohol may be used in various concentrations. Methyl alcohol, if to be used, is usually absolute, and is indicated especially in the preparation of blood stains, for which reason, it should be acetone free. 3. ANILINE WATER -Ten ml. of aniline is added to every 1/2 to 1 liter of hot distilled water, shaken, cooled, and filtered. 4. PHENOL - is used in aqueous solution of 0.5 - 5%. REFERENCES Baker JR. (1962) Experiments on the action of mordants. 2. Aluminium haematein. Quart J Microsc Sci; 103: 493-517. Bancroft JD, Gamble M, eds. (2002) Theory and Practice of Histological Techniques. 5th ed. London: Churchill-Livingstone. Bergey, DH, Holt JG, Noel RK, Sneath PHA. (1994) Bergey's Manual of Determinative Bacteriology (9th ed.) Lippincott Williams & Wilkins. Beveridge TJ. (2001) "Use of the Gram stain in microbiology". Biotech Histochem 76 (3): 111–8. Carson FL, Hladik C. (2009) Histotechnology: a Self-instructional Text. 3rd ed. Chicago, IL: ASCP Press. Clark G. (1981) Staining Procedures, 4th ed., Baltimore: Williams & Wilkins, p. 412. Conn, JI. (1969) Biological Stains, 8th ed., Williams and Wilkins Co. Baltimore. Davies JA, Anderson GK, Beveridge TJ, Clark HC. (1983) "Chemical mechanism of the Gram stain and synthesis of a new electron-opaque marker for electron microscopy, which replaces the iodine mordant of the stain". Journal of bacteriology 156 (2): 837–45. Gill GW. (2010) Gill hematoxylins: first person account. Biotech Histochem 85(1):7-18. Gill GW. (2010B) H&E staining: oversight and insights. DAKO Connection. 14:104-114. Gilliland JW, Dean WW, Stastny M, Lubrano G. (1979) Stabilized Romanowsky blood stain. Stain Technol 54:141–150. Horobin RW, Murgatroyd LB. (1968) The composition and properties of Gallocyanin-chrome alum stains. Histochem J 1:36–54. Horobin RW, Walter K. (1987) Understanding Romanowsky staining. I: The Romanowsky-Giemsa effect in blood smears. Histochemistry 86:331–336. Horobin RW, Kiernan JA. (2002) Conn's Biological Stains. A Handbook of Dyes Stains and Fluorochromes for Use in Biology and Medicine. 10th ed. Oxford: BIOS. Kiernan JA. (2008) Histological and Histochemical Methods. Theory and Practice. Bloxham, UK: Scion. Lillie RD. (1977) Conn's biological stains, 9th ed. Williams & Wilkins, Baltimore. Lillie RD, Pizzolato P, Donaldson PT. (1975) Hematoxylin substitutes: a survey of mordant dyes tested and consideration of the relation of their structure to performance as nuclear stains. Stain Technol 51:25–41. Llewellyn BD. (2009) Nuclear staining with alum hematoxylin. Biotechnic & Histochemistry. 84(4):159-177. Luna LG. (ed.) (1969) Manual of Histologic Staining Methods of the Armed Forces Institute of Pathology. The Blakiston Division, New York, 1969, 3rd ed. Marshall PN. (1976) The composition of stains produced by the oxidation of methylene blue. Histochem J 8:431–442. Marshall PN. (1978) Romanowsky-type stains in haematology. Histochem J 10:1–29. Marshall PN, Horobin RW. (1973) The mechanism of action of “mordant” dyes — a study using preformed metal complexes. Histochemie 35:361–371. Marshall PN, Horobin RW. (1973) Measurements of the affinities of basic and “mordant” dyes for various tissue substrates. Histochemie 36:303–312. Marshall PN, Horobin RW. (1974) A simple assay procedure for mixtures of hematoxylin and hematein. Stain Technol 49:137–142. Marshall PN, Lewis SM. (1975) A technique for distinguishing between Methylene Violet and Methylene Violet Bernthsen. Stain Technol 50:51–53. McManus JFA, Mowry RW. (1960) Staining Methods: Histologic and Histochemical. Paul B. Hoeber Inc., New York. Meloan SN, Puchtler H. (1974) Ion alizarin blue S stain for nuclei. Stain Technol 49:301–304. Penney DP, Poers JM, Frank M, Churukian C. (2002) Biotech Histochem 77 (5–6): 237–275. Pfuller U, Franz H, Preiss A. (1977) Sudan Black B: chemical structure and histochemistry of the main blue components. Histochemistry 54:327–333. Proctor GB, Horobin RW. (1987) Basic fuchsin homologues. Are pure dyes really necessary? Med Lab Sci 44:398–400. Puchtler H, Meloan SN, Waldrop FS. (1986) Application of current chemical concepts to metalhematein and — brazilein stains. Histochemistry 85:353–364. Reynolds JI, Moyes RB, Breakwell DP. (2009) "Differential staining of bacteria: acid fast stain". Current Protocols in Microbiology. Appendix 3: Appendix 3H. Ryan KJ, Ray CG. (editors) (2004). Sherris Medical Microbiology (4th ed.) McGraw Hill. pp. 232–3. Schulte E. (1986) Hematoxylin and the Feulgen reagent. In: Boon ME, Kok LP (eds.) Standardization and quantitation of diagnostic staining in cytology. Coulomb Press, Leiden, pp 9–15. Schulte E, Wittekind D. (1989) Standardization of the Feulgen-Schiff technique: staining characteristics of pure fuchsin dyes. Histochemistry 91:321–331. Schulte E, Wittekind D. (1989) The influence of Romanowsky-type stains on nuclear and cytoplasmic features of cytological specimens. Anal Cell Pathol 1:83–86. Scott JE. (1967) On the mechanism of the Methyl Green-Pyronin stain for nucleic acids. Histochemie 9:30–47. Scott JE. (1972b) The histochemistry of Alcian Blue, note on the presence and removal of boric acid as a major diluent in Alcian Blue 8GX. Histochemie 29:129–133. Wittekind D. (1979) On the nature of Romanowsky dyes and the Romanowsky-Giemsa effect. Clin Lab Haematol 1:247–262. Wittekind D, Kretschmer V, Sohmer I. (1982) Azure B-Eosin Y stain as the standard RomanowskyGiemsa stain. Br J Haematol 1:391–393. Wittekind D, Kretschmer V. (1987) On the nature of Romanowsky-Giemsa staining and the Romanowsky-Giemsa effect. II. A revised Romanowsky-Giemsa staining procedure. Histochem J 19:399–401. Yasumatsu H. (1977) Stain using celestine blue B as substitute nuclear stain in routine cytologic examinations. Acta Cytologica 21:173–174. CHAPTER 18 STAINING OF CARBOHYDRATES Carbohydrates are the main sources of energy in the body, mobilized in the form of monosaccharides (glucose) and stored in the form of polysaccharides, either in pure form (glycogen), or bound to other substances (mucin). Glycogen is made up of polysaccharides of glucose, and is normally stored in the liver, heart and skeletal muscle, but it may be abnormally present in certain diseases. Mucin is made up of hexosamines (neutral mucopolysaccharides) or mucus that is secreted by the goblet cells of intestinal mucosa, respiratory lining cells and certain glands, or found in intercellular substances and connective tissue fibers. Both glycogen and mucin are stained by the Periodic Acid-Schiff (PAS) technique. Periodic Acid Schiff (PAS) Reaction Periodic Acid Schiff is a histochemical stain that will demonstrate carbohydrates and other substances in the tissue. The PAS technique uses periodic acid to specifically oxidize the 1,2 glycol group of polysaccharides and mucin, liberating aldehydes that are required for the coloration of Schiff's reagent, thereby producing a red magenta or purplish-pink color. The treatment with periodic acid oxidizes some of the carbohydrates in the tissue to aldehydes. The carbohydrates involved are 1-2 glycols. Since not all carbohydrates include this structure, the PAS is not a method for carbohydrates in general but only for those which contain 1-2 glycols or closely related structures, including polysaccharides, mucopoly- saccharides, glycoproteins and glycolipids. The essential point is that treatment must be able to produce an aldehyde on the carbohydrate component. As a general rule, the intensity of PAS reaction is proportional to the content of sugars (glucose, galactose, mannose, methylpentose, fucose and hexosamines) present in the reacting substance. In order to have a PAS-positive staining reaction, oxidation must occur to produce aldehyde. Oxidation may continue beyond the aldehyde stage, and in such cases, the result will be negative since this PAS reaction is specific for glycol or glycol amino group where oxidation does not proceed beyond the aldehyde stage. Periodic acid is not the only oxidizing agent that has been recommended for the oxidation of carbohydrates although it is certainly the most used and arguably the most effective. Periodic acid has been less popular for fungal cell walls as staining of carbohydrates in the background may diminish the contrast between the background pink and the deeper pink of the fungal cell wall. To overcome this, the oxidant used for fungi is often chromic acid (chromium trioxide in water) which is different from periodic acid in that it continues to oxidize the aldehydes it produces. Over oxidation will eventually lead to a pale or false negative reaction. Some other oxidizing agents have been used as well including permanganic acid, performic acid, peracetic acid and lead tetracetate. Although valuable for specific purposes, these are not in common use. Periodic acid is generally applied to the sections as a 0.5 to 1.0% aqueous solution for 2 to 20 (average 5) minutes at room temperature. Oxidation beyond 10 minutes increases basophilic methylene blue staining-probably due to acidification of sulfhydryl groups into sulfonic acid. This can be manifested by increased affinity of the nuclei for hematoxylin counterstain. A temperature above 25°C which markedly accelerates the reaction, causing oxidation not only of aldehydes but also of other groups, e.g., sulfhydryl and disulfide. Solution must be discarded if it turns brown in color. Most fixatives can be used with this staining technique, except those that contain osmic acid, chromates and permanganates. Routine fixation and decalcification of bone will cause considerable loss of PAS positivity. PAS stain can be used to demonstrate the following substances: (1) Polysaccharides: These macromolecules are composed of monosaccharide units joined by covalent bonds. The main polysaccharide identified through histology staining is glycogen, which is present in numerous tissues, including skeletal muscle, cardiac muscle, liver, and kidney. (2) Neutral mucus substances: PAS is also commonly used to stain and identify glycoproteins, glycolipids, and neutral mucins, which are produced by epithelial cells in different organs. (3) Tissue basement membranes: These PAS-positive thin layers of reticular connective tissue anchor and support epithelium and endothelium to underlying connective tissue. (4) Fungal organisms: The cell walls of some living fungal organisms contain high levels of carbohydrate, and also stain positive with PAS. General Principles of the PAS Stain The reactivity of the PAS technique is based on the structure of the monosaccharide units. The stain involves periodic acid acting as an agent to oxidize the carbon-to-carbon bonds between two adjacent hydroxyl groups. This produces aldehyde groups in the tissue section that then reacts with Schiff reagent (made up of a mixture of basic fuchsin, hydrochloric acid, and sodium metabisulphite). The basic fuchsin in the mixture reacts with newly formed aldehyde groups in the tissue and produces a bright magenta color when the section is rinsed in water. The intensity of the color is proportional to the concentration of hydroxyl groups originally present in the monosaccharide units. Hematoxylin is typically used as a counter stain to visualize other tissue elements. However, when PAS is used to demonstrate fungal organisms, a light green counter stain is preferred. Diastase (alpha-amylase) digestion may also be used to assist in the diagnosis of glycogen storage diseases. Diastase hydrolyses and extracts starch, glycogen, and breakdown products of tissue polysaccharides. When compared to a slide of tissue containing glycogen, a diastase extraction slide will have no visible PAS stain. After examining routine hematoxylin and eosin-stained sections, the pathologist can order a PAS stain to help with the diagnosis of: Glycogen storage diseases: These are conditions in which excessive quantities of glycogen are stored in the liver, muscles, or kidney. PAS is often routinely used in the clinic to demonstrate glycogen accumulation in biopsies of these tissues. Tumors: Glycogen granules can also be present in some tumors, including some of those that arise in tissues such as the pancreas, lung, and bladder. Fungal infection: PAS can be used to visualize some fungal organisms in tissue sections. Basement membranes: PAS can be used to highlight abnormal basement membrane abnormalities – such as in glomerular diseases in the kidney. Schiff Reagent The essential component of Schiff reagent is basic fuchsin, which is a mixture of three dyes (rosanilin, pararosanilin and magenta II). Sulfur dioxide converts the magenta-colored basic fuchsin into colorless leukofuchsin. Reoxidation by slow exposure to light and air or by addition of periodic acid will restore the colorless leukofuchsin to the magenta colored basic fuchsin. A good quality Schiff's reagent should be made from pararosaniline rather than basic fuchsin, i.e. the specific component of basic fuchsin which produces the brightest staining solution. Beware of dye batches which give a brown solution when first made. Only a water clear or pale amber solution is acceptable. Although this brown discoloration may be removed with activated charcoal, the original depth of brown is indicative of the amount of nonpararosanilin components present in the dye. If large amounts of charcoal are needed to remove the brown color, or the charcoal has to be allowed to stay in the solution for longer than about a minute to make it water clear, then it is quite possible that the staining abilities of the Schiff's reagent may be compromised. The most common application for Schiff's reagent is the Periodic Acid Schiff, or PAS, reaction. This is a technique for the demonstration of carbohydrates in tissue sections. The purpose of the periodic acid is to oxidize some of the tissue carbohydrates. This produces aldehyde groups, which can then condense with Schiff's reagent forming a bright red coloration and demonstrating the tissue component to which the carbohydrate is attached. Schiff reagent can be prepared in different ways: (1) by using thionyl chloride to release sulfur dioxide; (2) by adding sodium or potassium metabisulfite; or (3) by using sulfur dioxide gas. All of these methods utilize the same principle of sulfuration in order to rearrange the chromophore group that is present in basic fuchsin. Any excess sulfur remaining in solution, together with any nonspecific yellow dye contaminant that is sometimes present in fuchsin, is absorbed and removed by subsequent treatment with activated charcoal. Schiff reagent is stored in the refrigerator so it is important to allow the reagent to come to room temperature before use. Failure to do so may result in weak staining. It is also important to store Schiff reagent in a tightly closed container when not in use so that the solution remains potent and stable. Barger and de Lamater Method (1948) 1. Dissolve 1 g. basic fuchsin in 400 ml. boiling distilled water. (Remove the flask of water from the bunsen burner just before adding the basic fuchsin, to prevent splashing of solution.) 2. Cool to 50°C and filter. 3. Add 1 ml. thionyl chloride to the filtrate. 4. Stopper, shake, and then let stand in the dark for 12 hours. 5. Add 2 gm. activated charcoal to decolorize, shake for l minute, and filter into a brown stock bottle. 6. Store in the dark at 0 to 4°C. 7. Allow the aliquot required to reach room temperature before use. De Tomasi-Coleman Method (1939) 1. Dissolve l gm. basic fuchsin in 200 ml. of boiling distilled water, shaking for 5 minutes. 2. Cool to 50°C and filter. 3. To the warm filtrate add 20 ml. of 1 M HCl (98.3 ml. HCl, sp gr 1.16, made to 1000 ml. with distilled water). 4. Cool to 25°C. 5. Add l gm. anhydrous sodium or potassium metabisulfite. 6. Let stand in the dark for 16 to 24 hours (solution will be orange or straw-colored). 7. Add 2 gm. activated charcoal to decolorize, shake for l minute, and filter into a brown stock bottle. 8. Store in the dark at 0 to 4°C. 9. Allow the aliquot to reach room temperature before use. Both Schiff reagents are stable and may last up to 6 months. However, it is preferable to make fresh reagent every month. The reagent should be discarded when it begins to form a color. Aside from running control sections when staining, reactivity of the Schiff reagent may be tested by adding a few drops of the reagent to 10 cc of 37- 40% formaldehyde. Rapid development of a reddish purple color means that the Schiff reagent is still good and usable. If the reaction is delayed and the resultant color is deep blue-purple, the solution is breaking down and should be discarded. STAINING OF GLYCOGEN Glycogen is the main storage form of glucose, manufactured and stored chiefly in the liver, but is also found normally in less quantity in muscles, parathyroid and cartilage. Glycogen is very soluble in water and insoluble in alcohol. Theoretically, therefore, alcoholic solutions are supposed to be the best fixatives and aqueous fixatives are not suitable. This is not entirely observed in practice because glycogen is ultimately lost no matter what fixative is used. Glycogen is often admixed with protein and lipids and hence is also coated with a protein membrane during protein fixation, thereby preventing further loss of glycogen. Furthermore, formalin and picric acid tend to bind glycogen with proteins. Although alcohol renders glycogen insoluble, it penetrates the tissues slowly; hence, preserves only the glycogen on the surface of the block. It also causes polarization or streaming of glycogen to one end of the cell, causing glycogen to appear in the form of clusters of large coarse granules along the margins of the cell. For adequate demonstration of glycogen, thin slices of tissues should be as fresh as possible, and should be immediately placed in the fixative at 4°C to prevent rapid breakdown of glycogen into glucose, due to the action of strong glycogenolytic enzymes particularly in the liver. For routine processing, the following fixatives are recommended, i.e., acetic acid, alcohol formalin, Bouin's, Brasil's, Kelly's and Gendre's solution. From the fixative, the tissue blocks should go directly into absolute alcohol. If minimal loss of glycogen is desired, it is advisable to float the sections onto 75% ethanol when cutting, and also to mount them on slides from 75% ethanol. Because of its water solubility, rinsing of tissues in normal saline before fixing should be avoided. For staining, blocks should be fixed in absolute alcohol to prevent dissolving water soluble glycogen. A positive control section should always be treated in parallel with the section being examined, to ensure that the staining technique is working. PERIODIC ACID-SCHIFF REACTION (McManus 1948, Carson 1983) Fixation: 10% neutral buffered formalin or Bouin’s solution. Sections: 4-5 µm Paraffin Solutions: Periodic Acid, 0.5% Solution Periodic acid 2.5 gm Distilled water 500 ml 1N Hydrochloric Acid Hydrochloric acid, conc. 83.5 ml Distilled water 916.45 ml Add acid to the water and mix well. Potassium Metabisulphite, 0.55% Potassium metabisulphite 2.75 gm Distilled water 500 ml Schiff Reagent Distilled water 800 ml Basic fuchsin 4 gm Sodium metabisulphite 4 gm 1N Hydrochloric acid 80 ml Heat water to the boiling point. Remove from flame, add basic fuchsin, and again heat solution to boiling point. Cool the solution to 50oC and then filter. Add 80 ml of 1N HCl, cool completely, and then add 4 gm of sodium metabisulphite. Let the solution stand in the dark overnight; it should turn light amber. Add 2 m of activated charcoal and shake for 1 minute. Filter the solution, and store in the refrigerator. The solution should be stable for 2-4 months. Method: 1. Bring sections to water. 2. Oxidize in 5 minutes in 0.5% aqueous periodic acid. 3. Wash in running water for 5 minutes and rinse in 3 changes of distilled water. 4. Place in Schiff's reagent for 10-20 minutes (10 minutes for frozen sections). Schiff reagent should be allowed to warm to room temperature before use. 5. Wash for 30 minutes in running water or rinse three times in 0.5% aqueous sodium metabisulfite, freshly prepared, and wash in running water for 10 minutes. (The metabisulfite rinse is optional, to remove excess leucofuchsin which might regain color on oxidation and cause false positive staining). 6. Wash in running tap water or 10 minutes to develop full color 7. Optional: Counterstain in Harris hematoxylin with acetic acid (2 ml acetic acid and 48 ml hematoxylin) for ½ minute. 8. Wash in tap water, "blue" in Scott's tap water substitute, and wash for 5 minutes in running tap water. 9. Dehydrate in increasing concentrations up to absolute alcohol, clear and mount in Clarite or Permount. Results: PAS-positive substances red or magenta red Nuclei blue NOTES: The method described gives maximum reaction but may produce a little background coloration. Alcoholic PAS reaction uses buffered alcoholic solution of periodic acid and reducing sulfite rinse. Mucoproteins are the most common PAS positive substances, e.g., mucin and intestinal mucoid secretions, tracheobronchial aspirates, and hyaline casts (kidney). Carbohydrates, glycoproteins, glycolipids, unsaturated lipids and phospholipids are also PAS positive, provided they are retained in the section. PAS-positive staining can also be found in certain bacteria, fungi, kerasin, connective tissue mucin, basement membrane, thyroid and cartilage. The PAS reaction is a useful indicator for glycogen when the technique incorporates a diastase digestion stage. Fig. 18-1. PAS Stain - Liver PAS with Diastase Method for Glycogen Demonstration Periodic Acid Schiff (PAS) stain is widely used for demonstration of glycogen. However, because of the fact that many other substances are also demonstrated, control sections should be processed simultaneously for proper evaluation. The section serving as control is treated with diastase (human saliva) or 0.1% malt diastase in distilled water to remove glycogen. For practical purposes, PAS reaction with and without diastase is considered as a specific test for glycogen. Glycogen is readily digested with amylase. Malt diastase is extracted from malt and contains both alpha- and beta- amylases. It is the commonly employed enzyme for glycogen digestion because it is easy to use, stable and comparatively cheap. Saliva containing ptyalin (salivary amylase) is also a highly effective means of digesting glycogen in tissue sections. However, most workers prefer the commercial diastase because it is easier to standardize. Fixation: Helly's Fluid Solution: Diastase 1 gm. Distilled water 100 ml. Method: 1 Sections to water. 2. Treat the control with saliva or I % malt diastase in distilled water. 3. Wash in running tap water for 5 minutes. 4. 0.5% periodic Acid for 5 minutes. 5. Rinse in distilled water. 6. Schiff's reagent for 5 minutes. 7. Rinse in 3 changes of sulfurous acid for 3 minutes each. 8. Wash in running tap water for 5 minutes. 9. Harris hematoxylin for 30 seconds. 10. Blue" in running tap water for 5 minutes. 11. Dehydrate, clear and mount. Results: Nuclei blue Glycogen red NOTE: The diastase digestion step should be performed with solutions that have been preheated to 37° C for one hour prior to use. The strength of the diastase solution should be optimized to give complete glycogen digestion. Concentrations (w/v) of 0.1% – 1.0% are commonly used. The diastase should be dissolved in a phosphate buffer with a pH of around 6.0 for maximum effectiveness. Diastase dissolved in water may not give adequate performance. PAS Technique with diastase control is the method of choice for glycogen staining. Substances that are positive to Schiff's reagent without periodic acid oxidation are not necessarily carbohydrates. Hence, controls should be included to show substances that are only positive to Schiff after specific oxidation. Other methods used for staining glycogen are: 1. Best Carmine Method 2. Langhan's Iodine stain Best Carmine Method (Modified Sheehan 1980, Luna 1992) Best Carmine is a good staining technique due to the affinity of alkaline carminic acid for glycogen, producing a bright red color. Ehrlich's hematoxylin is used as a counterstain, coloring the nuclei blue. Although carminic acid is believed to be the essential ingredient, carmine is generally used in its place because the acid form is more expensive and not necessarily more effective. Potassium carbonate and potassium chloride salts are added to the stock solution to inhibit any non-specific background carmine staining due to electrostatic bonding between the negatively charged carmine and the basic proteins found in tissue. This method is selective but not as highly specific for glycogen as the PAS method with and without diastase. Mast cell granules, fibrin and mucin are also stained, albeit weakly. Fixation: 10% neutral formalin, absolute alcohol, formol-saline, or Carnoy's fluid. Sections: Celloidin sections are the best. Paraffin sections should be covered with a thin layer of celloidin before staining (celloidinization) to prevent the loss of sections from the slide due to the ammoniacal staining solution, and to preserve glycogen. Celloidinization of Slides 1. Sections to absolute alcohol. 2. Place sections in 1% celloidin in equal parts of absolute ethyl alcohol and ether for 5 minutes. 3. Wipe dry the back of the slide and without allowing celloidin to dry, transfer the slide to 80% ethyl alcohol for 5 minutes. Solutions: Carmine Stock Solution: Carmine 2 gm Potassium carbonate 1 gm Potassium chloride 5 gm Distilled water 60 ml Boil gently for 5 minutes, using a large flask to avoid spilling. Cool and add 20 ml. concentrated ammonia. Filter and store in a dark container at 4°C. (The solution should be usable for several months.) Carmine Working Solution: Stock solution 5 ml Concentrated ammonia 12.5 ml Methanol 12.5 ml The working solution should be filtered before use. Best's Differentiator Methanol 40 ml Ethanol 80 ml Distilled water 100 ml Method: 1. Rinse celloidinized slide briefly in water. 2 Stain with Harris hematoxylin for 5 minutes or Mayer hematoxylin for 15 minutes. 3. Wash in running water for 15 minutes. 4. Stain in working solution of Best carmine, in a small closed jar for 30 minutes. 5. Differentiate in Best's differentiator for 30 seconds or until no more color comes away. 6. Rinse rapidly in 80% alcohol, or place immediately in 95% alcohol. 9. Remove or dissolve celloidin film by transferring the section to alcohol ether mixture. 10. Dehydrate in absolute alcohol, clear and mount. Results: Nuclei blue or grayish blue Glycogen pink to red Mucin weak red Fig. 18-2. Best Carmine stain - Liver NOTES: Staining may be improved by reducing the amount of ammonia or methyl alcohol. Celloidin film, if too thick, may become insoluble after Best carmine staining, particularly if saliva has been used as control. This is quite impossible to remove completely. In such cases, the stained section should be examined thru the portion of the film that tends to be lightly stained. Failure to stain may be due to using old deteriorated stock solution, or to washing the section in water instead of alcohol or differentiator immediately after staining with carmine. The section should not be allowed to dry following staining with carmine, but should be washed immediately in alcohol or differentiator. Staining should be carried out in a closed container (e.g., Coplin jar) as the highly volatile ammonia readily evaporates, causing the carminic acid to precipitate out of the solution. STAINING OF MUCIN Mucins are polysaccharides bound to other substances (the nature of which serves as the basis for their classification), forming the ground substance of connective tissues primarily. Mucins usually take up a light pink color with eosin when stained with H&E, unless Ehrlich's hematoxylin (alkaline) is used, in which case acid mucopolysaccharides especially from connective tissue will stain bluish or basophilic. They may be precipitated by dilute acetic acid and dissolved by dilute alkali; hence, alkaline fixatives are usually contraindicated. Formalin and Carnoy's fluid are recommended for fixation although prolonged storage in formalin tends to reduce the strength of PAS reaction of mucin. Hydration with 0.2.N NaOH for 10-15 minutes before staining may be done to regain PA.S reaction although such procedure almost invariably causes detachment of sections from the slide. There are a variety of mucin stains, all attempting to demonstrate one or more types of mucopolysaccharide substances in tissues. The types of mucopolysaccharides are as follows: • Neutral mucopolysaccharides - These substances contain hexoses as their second carbohydrate component, are less distributed and less important than acid mucopolysaccharides, and found in epithelial and intestinal glands. • Acid (simple, or non-sulfated) - Are the typical mucins of epithelial cells containing sialic acid. They stain with PAS, Alcian blue at pH 2.5, colloidal iron, and metachromatic dyes. They resist hyaluronidase digestion. • Acid (simple, mesenchymal) - These contain hyaluronic acid and are found in tissue stroma. They do not stain with PAS, but do stain with Alcian blue at pH 2.5, colloidal iron, and metachromatic dyes. They digest with hyaluronic acid. They can be found in sarcomas. • Acid (complex, or sulfated, epithelial) - These are found in adenocarcinomas. PAS is usually positive. Alcian blue is positive at pH 1, and colloidal iron, mucicarmine, and metachromatic stains are also positive. They resist digestion with hyaluronidase. • Acid (complex, connective tissue) - Found in tissue stroma, cartilage, and bone and include substances such as chondroitin sulfate or keratan sulfate. They are PAS negative but do stain selectively with Alcian blue at pH 0.5. Acid Mucopolysaccharides They are polysaccharides with hexuronic acid as secondary carbohydrate constituent, bound to sulfuric acid esters and proteins. They comprise mainly of hyaluronic acid (connective tissue mucin usually formed by fibroblasts), heparan sulfate (usually found in aorta, cardiac connective tissues and mast cells) and chondroitin sulfate (found in cartilage). They comprise the intercellular or ground substance all throughout the body, particularly between connective tissue elements such as reticulum, elastin and collagen. They are also especially found in synovial fluid, vitreous humor and Wharton's jelly of the umbilical cord. Acid mucopolysaccharides are the only large group of carbohydrate compounds that are not strongly PAS positive. They may, however, be well demonstrated by the following staining methods: 1. Metachromatic staining 1. Toluidine blue and Azure A 2. Uranyl nitrate- Azure method 2. Alcian blue technique 3. Colloidal iron technique 4. Aldehyde fuchsin stain 5. Mucicarmine stain 6. Fluorescent acridine orange technique Metachromatic Staining Acid mucin is metachromatic (producing a color that is different from that normally exhibited by the dye), while neutral mucin is not. The most useful metachromatic dye for acid mucin is Azure A. In the Azure A metachromatic technique, the intensity of staining appears to be due to the initial potassium permanganate oxidation step which aids in uptake of dye by the tissue. The alcohol-fastness and increased brightness of metachromasia is due to the addition of uranyl nitrate that acts as a mordant-type differentiator. For metachromatic staining, mercurial fixatives are used. Uranyl nitrate Azure method gives excellent results with connective tissue mucins and is the only method that is alcohol-fast, allowing permanent preparations to be made easily. Toluidine blue is a basic thiazine metachromatic dye with high affinity for acidic tissue components and nucleic acids. It stains nucleic acids blue and polysaccharides purple. It is also used to highlight tissue components such as cartilage or certain types of mucin. With mucopolysaccharidosis (characterized by abnormal deposition of mucopolysaccharides or glycosaminoglycans in connective tissues and hepatocytes), it is necessary to avoid aqueous solutions during fixation, processing and section preparation. The tissue should be either fixed in an alcoholic fixation (i.e. Carnoy's fluid) or received fresh for cryostat sectioning. Metachromatic Toluidine Blue Method Section: Frozen section Solution: 0.25% toluidine blue in pH 4.5 buffer Method: I. Prepare 15 µm thick fresh cryostat sections (preferably snap-frozen). 2. Stain with toluidine blue solution for 10 seconds only. 3. Blot dry, dehydrate rapidly through absolute alcohol. 4. Clear and mount in a synthetic mountant. Results: Mucopolysaccharide red purple Tissue background blue Alcian Blue Technique, pH 2.5 (Luna 1968; Carson 1983) Alcian blue is a histological dye that forms electrostatic bonds with certain tissue components containing either carboxyl or sulfate groups (such as sulfated or acid mucins which are specifically and intensely stained. Alcian blue is the most popular method for general demonstration of acid mucopolysaccharides, using 3% acetic acid at pH 2.5. Fixation: 10% neutral-buffered formalin or Bouin’s solution Sections: 4-5 µm paraffin sections Solution: Acetic Acid, 3% Solution Glacial acetic acid 15 ml Distilled water 485 ml Alcian Blue, 1% Solution Alcian Blue-8GX 5 gm Acetic acid, 3% solution 500 ml Adjust the pH to 2.5, filter, and add a few crystals of thymol Nuclear-Fast Red (Kernechtrot) Solution Nuclear fast-red (Kernechtrot) 0.5 gm Aluminum sulfate 25 gm Distilled water 500 ml Dissolve the aluminum sulfate in the distilled water, and then add the nuclear-fast red. Heat the solution until the nuclear-fast red has dissolved. Cool, filter, and add a few grains of thymol as preservative. Method: 1. Deparaffinize and hydrate sections to distilled water. 2. Place slides in 3% acetic acid solution for 3 minutes. 3. Place slides in alcian blue solution for 30 minutes at room temperature or for 15 minutes in a 37oC water bath. 4. Rinse sections briefly in 3% acetic acid solution to remove excess alcian blue. 5. Wash slides in running tap water for 10 minutes. 6. Rinse in distilled water. 7. Counterstain in nuclear-fast red solution for 5 minutes. 8. Wash in running tap water for at least 1 minute. 9. Dehydrate in 2 changes each of 95% alcohol and absolute alcohol. 10. Clear in xylene and mount in synthetic resin. Results: Acid mucins blue Nuclei red Avoid celloidinization of slides as the alcian dyes are strongly retained by celloidin. Fig. 18 - 3. Alcian Blue stain in myxoid chondroma Combined Alcian Blue-PAS-Hematoxylin Technique for acid and neutral mucins (Luna 1968; Carson 1983) This combined technique is useful for demonstrating the presence of any mucin, especially for separating acid mucins and neutral mucins. The rationale is that by first staining all acid mucins with alcian blue, those acid mucins which are also PAS-positive will not react in the subsequent PAS reaction. Thus, only the neutral mucins will be stained by PAS, while acid mucins will be stained by alcian blue. Fixative: 10% neutral-buffered formalin or Zenker’s solution Sections: 4-5 µm paraffin sections Solutions: Acetic Acid, 3% Solution Glacial acetic acid 3 ml Distilled water 100 ml Alcian Blue, pH 2.5 Alcian blue 5 gm Acetic acid, 3% solution 500 ml Periodic Acid, 0.5% Solution Periodic acid 2.5 gm Distilled water 500 ml Stock Reducing Rinse Solution Sodium metabisulphite 10 gm Distilled water 100 ml Working Reducing Rinse Stock reducing rinse 2.5 ml Distilled water 50 ml Prepare just before use. Schiff Reagent Distilled water 800 ml. Basic fuchsin 4 gm Sodium metabisulphite 4 gm 1N Hydrochloric acid 80 ml Heat water to the boiling point. Remove from flame, add basic fuchsin, and again heat solution to boiling point. Cool the solution to 50oC and then filter. Add 80 ml of 1N HCl, cool completely, and then add 4 gm of sodium metabisulphite. Let the solution stand in the dark overnight; it should turn light amber. Add 2 m of activated charcoal and shake for 1 minute. Filter the solution, and store in the refrigerator. The solution should be stable for 2-4 months. Method: 1. Deparaffinize sections and bring to water. 2. Place sections in 3% acetic acid for 1 minute. 3. Stain sections in alcian blue for 30 minutes. 4. Wash sections in running tap water, then rinse in distilled water. 5. Place section in 05% periodic acid for 10 minutes. 6. Wash slides in running tap water for 5 minute, then rinse in distilled water. 7. Place slides in Schiff reagent for 10 minutes. 8. Place slides in reducing rinse for 5 minutes. 9. Wash in running tap water for 10 minutes. 10. Stain sections with Harris hematoxylin containing acetic acid (48 ml hematoxylin in 2 ml glacial acetic acid) for ½ to 1 minute. (Optional) 11. Dehydrate in 2 changes each of 95% and absolute alcohols clear in xylene, and mount with synthetic resin. Results: Acid mucins blue Neutral mucins magenta Mixtures of above the color will range from blue-purple through purple to a violet or mauve color, depending on dominant component Nuclei pale blue It is important to stain only lightly with hematoxylin to distinguish it from alcian blue staining. Ehrlich's hematoxylin should be avoided as a counterstain, as it will also stain some mucins and will complicate the final result. Fig. 18-4. Alcian Blue-PAS Stain (Acid mucin- blue; Neutral mucin-magenta) Gomori's Aldehyde Fuchsin Stain Aldehyde fuchsin was first introduced by Gomori in 1950 as an elastic tissue stain. It employs basic fuchsin plus aldehyde to demonstrate sulfurcontaining compounds .The blueing of basic fuchsin is due to its combining with a mixture of acid-alcohol and paraldehyde, forming acetaldehyde which then condenses with the amino groups of the basic fuchsin. In the presence of strong mineral acid, basic fuchsin forms intensely purplish dyes with certain aldehydes. A number of other tissue components are equally stained, including acid mucopoly-saccharides, sulfated mucosubstances, pancreatic islets of Langerhans, thyrotrophic hormones, and secretory substances. It is also used to stain mast cells, particularly when no counterstaining is done. Aldehyde fuchsin has a greater affinity for sulfated mucins, which are stained purple, while the carboxylate forms (sialomucins, e.g. submandibular salivary gland and intestinal goblet cell) only will be stained blue after subsequent counterstaining with alcian blue. Mucicarmine Stain Adding aluminum hydroxide to carmine (Southgate 1927) has improved the ability of carmine solution (Mayer 1896) to stain for mucin, probably with the rationale that aluminum salts in the solution will form a chelate compound with carmine, which then binds to the mucin-containing tissue. Its large molecular size also allows the dye complex to penetrate and bind to acidic mucins but not to other acidic substances such as nucleic acids. Southgate's mucicarmine technique is useful for staining encapsulated fungi, e.g. Cryptococcus neoformans. Preparing the Stain: 1. Grind 1 gm. carmine and place in a large (500 ml.) conical flask. 2. Add 100 ml. of 50% alcohol and mix. 3. Add 1 g. aluminum hydroxide and mix 4. Add 0.5 g. anhydrous aluminum chloride. 5. Mix and boil gently for 2 Yi minutes. 6. Cool, filter and store at 4°C. The mucicarmine solution will usually keep for 6 months or so at 4°C before its stain properties deteriorate. Solutions more than 6 months old should be discarded. Method: 1. Deparaffinize section and bring to water. 2. Stain the nuclei with Mayer's hematoxylin (not Ehrlich's hematoxylin). Differentiate well and blue in the usual way. 3. Stain with mucicarmine for 20 minutes. 4. Wash in water. Rinse in absolute alcohol. 5. Clear in xylene and mount. Results: Mucins red Nuclei blue Background unstained NOTE: Ehrlich's hematoxylin should be avoided as a counterstain because certain mucins pick up the hematoxylin and consequently will not be stained. As a general mucin technique, the combined alcian blue-PAS technique will be more informative in establishing the presence or absence of tissue mucins. Fig. 18-5. Cryptococcus Neoformans (Mucicarmine stain) Colloidal (Dialyzed) Iron Technique The colloidal iron technique works on the principle that at a low pH, colloidal iron will be adsorbed onto tissue containing acid mucins, and subsequently visualized by conversion to ferric ferrocyanide (prussian blue) using the conventional Perl's technique. The dialyzed iron-prussian blue can be combined with PAS reaction to give color differentiation between acid and neutral mucins. This has greater sensitivity and intensity of reaction compared to alcian blue staining, but is a more complex and time-consuming method. Iron particles are stabilized in ammonia and glycerin and are attracted to acid mucopolysaccharides. It requires formalin fixation. Phospholipids and free nucleic acids may also stain. The actual blue color comes from a Prussian blue reaction. The tissue can be pre-digested with hyaluronidase to provide more specificity. Fluorescent Acridine Orange Technique Acridine orange is a fluorescent stain (fluorochrome) that can be used to demonstrate acid mucins. Mucin in a section stained with iron hematoxylin and acridine orange gives a selective brilliant orange fluorescence, while other fluorescence in the tissue are subdued by iron hematoxylin and are therefore colored black. The disadvantage is that fluorescent staining is temporary and will only last for about 2 hours once the section is mounted. Fixation: Formalin and other fixatives, except heavy metals. Sections: Frozen or paraffin Sections Method: 1. Sections to water. 2. Place in 4% aqueous iron hemalum for 5-10 minutes. 3. Wash briefly in running tap water. 4. Stain in 0.1% aqueous acridine orange for 1% minutes. 5. Wash briefly and mount in glycerin. 6. Examine immediately in a fluorescence microscope. Results: Acid mucopolysaccharides Black Fungi Greenish red flourescence Background Reddish orange fluorescence Neutral Mucopolysaccharides They can be found in glands of the GI tract (notably esophagus and stomach) and in prostate. They stain red with PAS and can be distinguished from acid mucopolysaccharides because they do not stain with Alcian blue, colloidal iron, mucicarmine, or metachromatic dyes. The neutral mucopolysaccharides are glycol proteins poor in sulphuric and uronic acids, containing 20–50% protein. Up to 80 per cent of the polysaccharides in human cervical mucus from the midcycle consists of a neutral mucopolysaccharide which contains as constituents methylpentose, galactose, and hexosamine. The combination of the alcian blue and the PAS techniques can be used as a means of distinguishing neutral mucins from acid mucins. In most protocols, sections are stained with the standard alcian blue (pH 2.5) method followed by the PAS technique. The alcian blue at a pH of 2.5 will stain all acid mucins deep blue but will not color the neutral mucins. The subsequent application of the PAS technique will stain the neutral mucins bright magenta. Tissues or cells that contain both neutral and acidic mucins may demonstrate a dark blue or purple coloration. REFERENCES Bancroft JD. (1975) Histochemical Techniques. London, Butterworths. Bancroft JD, Cook HC. (1994) Manual of Histochemical Techniques and their Diagnostic Application. Churchill Livingstone, Edinburgh. Carson FL, Pikett JP. (1983) Histochemistry. In: Race GJ, ed. Laboratory Medicine, Philadelphia, PA: Harper & Row. Carson FL. (1997) Histotechnology. A Self-Instructional Text. 2nd ed. Chicago: American Society of Clinical Pathologists. Charman J, Reid L. (1972) The effect of decalcifying fluids on the staining of epithelial mucins by alcian blue. Stain Technology, 47: 173. Clark G. (1981) Staining Procedures (4th ed). Baltimore, Williams and Wilkins. Cook HC. (1959) A comparative evaluation of the histological demonstration of mucin. Journal of Medical Laboratory Technology, 16: 1. Culling CFA. (1963) Handbook of histopathological techniques Ed. 2 Butterworths, London, UK. Culling CFA. (1974) Handbook of histopathological and histochemical techniques Ed. 3. Butterworths London, UK. Dapson RW. (2005) Dye-tissue interactions: mechanisms, quantification and bonding parameters for dyes used in biological staining. Biotech Histochem 80(2):49-72. Dapson RW. (2007) The history, chemistry and modes of action of carmine and related dyes. Biotech Histochem 82:173–187. Drury RAB, Wallington EA. (1967) Carleton’s Histological Technique (4th ed.) New York, Oxford University Press, 1967. Goldstein DJ, Horobin RW. (1974) Rate factors in staining with alcian blue. Histochemical Journal, 6: 157. Gomori G. (1950) A new histochemical test for glycogen and mucin. American Journal of Clinical Pathology 16: 177. Grocott RG. (1955) A stain for fungi in tissue sections. American Journal of Clinical Pathology, 25: 975. Hale CW. (1946) Histochemical demonstration of acid mucopolysaccharides in animal tissue. Nature (London), 157: 802. Hicks JD, Matthaei E. (1958) A selective fluorescence stain for mucin. Journal of Pathology and Bacteriology, 75: 473. Itikawa 0, Oguru Y. (1954) Simplified manufacture and histochemical use of the Schiff reagent. Stain Technology, 29: 9. Kiernan JA. (2008) Histological and Histochemical Methods: Theory and Practice. 4th ed. Bloxham, UK: Scion. Chapter 11, pp. 274-306). Kiernan JA. (2010) Carbohydrate histochemistry. Connection (Dako scientific magazine) 14:68-78. Lane RF, Tripp EJ. (1971) Basic fuchsin and the preparation of Schiff's reagent. Med Lab Technol. 28(1):26-34. Lillie RD. (1954) Histologic Technic, 2nd ed., McGraw-Hill, New York and Maidenhead. Lillie R.D. (1969) H.J. Conn s Biological Stains. Williams & Wilkins, Baltimore. Luna LG. (1968) Histologic Staining Methods of the Armed Forces Institute of Pathology, 3rd ed., New York, NY; McGraw-Hill Book Co. Luna LG. (1992) Histopathologic Methods and Color Atlas of Special Stains and Tissue Artifacts. Gaithersburg, MD: American Histolabs Inc. McManus FA. (1948) Histological and histochemical uses of periodic acid. Stain Technol 23:99. McManus JFA, Mowry RW. (1960) Staining Methods: Histologic and Histochemical. New York: Hoeber (Chapter 13, pp. 124-151). Mowry RW. (1978) Alcian blue techniques for the histochemical study of acidic carbohydrates, Journal of Histochemistry and Cytochemistry, 4: 407. Pearse AGE. (1968) Histochemistry: Theoretical and Applied (3rd ed.), Vol. 1. London, Churchill Livingstone. Pearse AGE. (1972) Histochemistry: Theoretical and Applied, Churchill Livingstone, Edinburgh. Pearse AGE. Histochemistry (1985) Theoretical and Applied, 4th ed. Vol. 2. Analytical Technique. Edinburgh: Churchill-Livingstone, pp .675-785. Reid H, Clamp JR. (1978) The biochemical and histochemical nomenclature of mucus. British Medical Bulletin 34: 1. Rosai J. (2004) Special techniques in surgical pathology, in Rosai J (ed): Rosai and Ackerman’s Surgical Pathology (9th ed). Philadelphia, PA, Mosby pp 38–41. Scott JE, Dorling J. (1965) Differential staining of acid glycosaminoglycans (mucopolysaccharides) by alcian blue in salt solutions. Histochemie 5: 22. Schulthorpe HH. (1978) Metachromasia. Medical Laboratory Sciences, 35: 365. Sheehan DC, Hrapchak BB. (1980) Theory and Practice of Histotechnology, 2nd ed. Columbus OH: Battelle Press. Southgate HW. (1927) Note on preparing mucicarmine. Journal of Pathology and Bacteriology 30:729. Spicer SS, and Meyer DB. (l960) Histochemical differentiation of acid mucopolysac-charides by means of combined aldehyde fuchsin-alcian blue staining. American Journal of Clinical Pathology 33: 453. Sheehan DC, Hrapchak BB. (1980) Theory and Practice of Histotechnology (2nd ed). St. Louis, MO, C.V. Mosby Company, 1980. CHAPTER 19 STAINING OF LIPIDS In histotechnology, the word lipid refers to all fat and fat like, or fat containing substances. This includes triglycerides, fatty acids, lipoproteins and glycolipids. Lipids or fats are generally classified into simple lipids, compound lipids, and derived lipids. They all have a common property of solubility in organic solvents and insolubility in water. 1. Simple lipids (neutral fat) are esters of fatty acids with alcohols and are usually found in the body as energy stores in adipose tissue. Triglycerides are esters of fatty acids with glycerol constituents, serving as storage fats in animals with high solubility for certain nonionic colored substances (lysochromes) stainable by Sudan Black B, Sudan IV and Oil Red 0. 2. Compound lipids consist of a fatty acid, an alcohol and one or more other groups such as phosphorus or nitrogen. They are generally found in the central nervous system. a. Phospholipids are the important components of cellular membranes particularly found in mitochondria and nervous tissue elements and are readily stained by Sudan Black B and acid hematin. b. Glycolipids are composed of fatty acids and hexoses, possessing characteristics of both lipids and carbohydrates and are therefore stained by Sudan Black B and PAS techniques. 3. Derived lipids are fatty acids that are derived from hydrolysis of simple and compound lipids. Examples are cholesterol, bile acids, sex hormones and adrenocortical hormones. Adipose Tissue Adipose tissue or fat is distributed throughout the body in distinct “white” and “brown” adipose tissue depots. White adipose tissue (WAT) is largely composed of unilocular lipid-filled adipocytes that specialize in lipid storage, whereas brown adipose tissue (BAT) is largely composed of multilocular adipocytes that specialize in lipid burning. Fat cells appear as “signet rings” on H&E stain because large lipid droplet displace the nucleus and remainder of the cytoplasm to the edge of the cell. With standard methods of fixation, lipids are largely lost from tissues during processing. The clear areas in the section are truly empty, because the triglycerides in the fat droplet are soluble in the organic solvents used during processing of the section, and are therefore removed from the section. Fig. 19-1. Adipose tissue or Fat (H&E stain) Lipid bodies, also named lipid droplets or adiposomes, are distributed in the cytoplasm as roughly spherical organelles lacking a delimiting classical bilayer membrane, but surrounded by an outer monolayer of phospholipids, which at least in some cells may have a unique fatty acid composition. Cytoplasmic lipid droplets are neutral lipids, usually triacylglycerols or cholesteryl esters. Because lipid bodies can be destroyed by drying or fixation and staining with alcoholbased reagents, there are consequently some methodological limitations to their study. Lipids are difficult to demonstrate histologically because they dissolve in the solvents used for paraffin processing and, to a lesser degree, in celloidin processing. Frozen sections may be required in order to stain for lipids. Triglycerides are always completely removed in properly cleared and paraffin infiltrated blocks. It should be noted, however, that lipids bound to other materials, such as lipoproteins, lipofuscins and myelin may not be completely removed by solvents used during paraffin processing and significant amounts may still be present in the tissue sections. Lipids are best demonstrated on cryostat sections of fresh unfixed tissue since there is no really good fixative available. Formalin only preserves those lipids that are already more or less firmly bound to proteins (such as lipofuscins and granules of leukocytes). Lipochrome (lipofuscin) pigments are the breakdown products within cells from oxidation of lipids and lipoproteins. They are the wear-and-tear pigments found most commonly in heart, liver, CNS, and adrenal cortex. Lipofuscins (lipochrome pigments) are PAS positive and variably acid fast. They stain with Ziehl-Neelsen. In addition lipofuscin is Sudan black B and Sudan Red positive. Lipochrome can be demonstrated by Schmorl's method which also stains for melanin. Lipochrome may also exhibit a strong orange auto fluorescence in formalin-fixed, unstained paraffin sections. Fig. 19-2. Lipochrome (lipofuscin) appearing as brown pigments. H&E stain of liver Lipids present in fat embolism, fatty liver and atheroma may be fixed for staining in paraffin sections by exposing the sections to an emulsion of linoleic acid and lecithin in 70% ethylene glycol at 56oC for 3 days. These tissues are then treated with 2% chromic acid at 4°C for 24 h followed by 24 h in 5% sodium bicarbonate, with appropriate rinsing between solutions. Paraffin sections of these tissues then stained with a lipid-soluble dye such as Oil Red O. The demonstration of fat embolism with good quality tissue detail is made practical by the method, which is convenient and inexpensive. Phospholipids and neutral fats will be lost during routine dehydration and embedding unless they are treated with potassium dichromate or osmic acid, which are the only agents that truly fix lipids. Oxidation of phospholipids by chromate fixation renders them non-extractable by alcohol, toluene, xylene or paraffin. However, they both greatly alter the chemical reactivity of the lipids, which can adversely affect staining. Formol-calcium is the fixative of choice for lipid histochemistry, and is prepared by adding 2% calcium acetate to 10% formalin. To preserve the lipids, polyethylene glycols (carbowaxes) are sometimes used in lieu of the usual dehydration and embedding process. However, this technique is not widely utilized, and in most centers, neutral fats are still best demonstrated in frozen sections of fixed or unfixed tissue. Formol-calcium fixed tissue blocks are also suitable for cryostat sections, and should be mounted on chrome-gelatin coated slides, because fixation causes the endogenous tissue proteins to lose their adhesive properties. In general, histochemical techniques are the common methods of choice for demonstrating lipids in tissue sections. These are usually complemented by other biochemical techniques and chromatography for specific identification and possible quantification of the lipid demonstrated by microscopy. Fat Stains and Sudan Dyes Sudanophilia is the property of tissues to be stained with fat or oil-soluble dyes, regardless of the type of dye used, due to their essential lipid nature. The staining is based on the greater physical solubility of the dye in lipid substances than in the usual aqueous-alcoholic or acetone-alcoholic medium in which they are dissolved. Staining with these dyes is regarded as specific for lipids, especially for simple lipids (neutral fat). Oil soluble dyes are usually divided into the main groups: 1. Basic Aryl amines with very low water solubility: a. Sudan Black B - most sensitive lipid stain known b. Sudan Red VII B 2. B-Naphthols such as the original diazo dyes a. Sudan III (C.I. No. 26100) b. Sudan IV (Scharlach B) C.I. No. 26105 - staining fats with a more brilliant or deeper red color than Sudan III which stains lipids orange-red. Sudan dyes are a group of lipid soluble solvent dyes often called lysochromes. Sudan III was the first of these dyes to be introduced in 1896, followed by Sudan IV (Scharlach R) in 1901. Sudan III is predominantly used for staining triglycerides in animal tissues (frozen sections). With the use of certain solvents, may also be used to stain some protein bound lipids in paraffin sections. The most sensitive and versatile of all these dyes is Sudan Black B, which was introduced in 1935. Unlike other Sudan dyes, Sudan Black B stains phospholipids as well as neutral fats. However, Sudan Black B does not stain crystalline cholesterol, and free fatty acids tend to be dissolved in the alcoholic dye bath. These drawbacks can be overcome by pre-treating the tissue with bromine to make the unsaturated lipids insoluble in organic solvents. The uptake of Sudan black B by partition from dilute solution is a specific test for lipid, but in normally fixed tissue most of the structural lipid is ‘bound’ and is not accessible to the dye. For frozen sections, cut tissues about 15 micra thick are usually stained with. Scharlach R or with Oil Red 0, which stains neutral fats and lipofuscin well. Oil Red O is used to demonstrate the presence of fat or lipids in fresh, frozen tissue sections. Oil Red O is a fat-soluble diazo dye, and is classified as one of the Sudan dyes which have been in use since the late 1800s. Like most stains used to detect lipids, Oil Red O is not a true special stain, since it can’t form bonds with lipid components. It is actually a pigment that functions as an oil-soluble colorant, and the technique represents a physical method of staining. For general use, 70% alcohol is an adequate solvent for Oil Red 0 and Sudan black. Containers should always be kept covered except when the tissue is being placed into and taken out of solution to prevent evaporation, particularly of their alcoholic component. Sudan Black Method for Lipids (Suvarna 2013) Fixation: Formaldehyde calcium with post-chroming Section: Unfixed cryostat sections preferred, or frozen sections post-fixed in formol calcium Method: 1. Sections from water to 50% and 70% alcohol. 2. Stain for up to 2 hours in saturated Sudan Black B in 70% ethanol. 3. Place in 70% alcohol for 5 seconds only to remove excess surface dye. (Longer periods will remove the color). 4. Immerse in 50% alcohol for I minute. 5. Wash in distilled water for 2 minutes. 6. Counterstain with Mayer's carmalum for 2 1/2 minutes. 7. Wash in distilled water for 2 minutes. 8. Mount in aqueous mounting medium. Results: Lipids blue black Nuclei Red Sudan IV (Scharlach R) Stain for Lipids Fixation: 10% Formalin Sections: Frozen sections Method: Collect 10 µ frozen sections in distilled water. 1. Place in 50% alcohol for 1 minute. 2. Place in 70% alcohol for 1 minute. 3. Immerse in Sudan IV or Scharlach R (Oil Red 0 may be used) for 5-10 minutes. 4. Dip in 70% alcohol for 1minute (Longer periods will remove the color.). 5. Counterstain with Harris hematoxylin for 2 minutes. 6. Differentiate in 1% acid alcohol until only the nuclei are stained blue/ black under microscopic control. 7. "Blue" in tap water for 5 minutes. 8. Rinse in distilled water. 9. Mount sections on to slide from distilled water to an aqueous mounting medium. Results: Lipids (mainly triglycerides) - red Nuclei - blue/black NOTE: Scharlach R (Sudan IV) is the most commonly used stain, producing a rapid and permanent coloration of lipid. The addition of benzoic acid to the staining solution materially intensifies the resulting color and prevents deterioration. True fats stain intensely while cholesterol stains less intensely. Oil Red 0 Method in Dextrin (modified by Churukian 2000) Oil Red 0 is closely related to Sudan dyes and was introduced in 1926 by French. It was popularized in 1943 by Lillie and Ashburn who advocated its use as a 50 to 60% fresh aqueous dilution of a saturated 99% isopropanol stock solution. Oil Red 0 stains neutral fats and lipofuscin well. The basis for staining lipids with an oil-soluble dye lies in its increased solubility in fatty substances as opposed to the dye solvents which are used in routine tissue processing. The choice of solvent for this reaction is also critical, since it must be able to extract excess dye without dissolving the lipid to be stained- propylene glycol is the preferred solvent for this technique. The end result is that fat and lipids in tissue sections stain bright red, and nuclei stain blue. Although other stains are available to help detect the presence of lipids in tissues, the intensity of its red coloration makes Oil Red O the preferred choice. Fixation: Fresh frozen or frozen sections post-fixed in neutral buffered formalin Sections: 5 µm sections mount on slides, air dry Solutions: Dextrin Solution Dextrin 1 gm Distilled water 100 ml Oil Red O stock solution Oil Red O 0.5gm Isopropanol 100ml Dissolve the dye in isopropanol using gentle heat in water bath. Oil Red O working solution Stock Oil Red O solution 30ml Dextrin 20ml Allow to stand for a day or more. Stable or months, filter before use. Method: 1. Place slides directly into filtered 0.5% Oil Red O in dextrin. Stain for 20 minutes, rinse with running water briefly. 2. Counterstain with Gill II hematoxylin for 20-30 seconds. Rinse with water, blue, coverslip with aqueous mounting media. Results Lipid red Nuclei blue Fig. 19-3. Oil-Red-O stain of liver Osmic Acid Stain for Fat Osmium tetroxide (osmic acid) is not a dye but is an unstable oxide which is reduced to a permanent black substance by unsaturated fats and fatty acids. It is used as a fixative for electron microscopy and in histochemistry, and for demonstration of unsaturated fats, with the disadvantage that other substances may also be stained simultaneously. Lipids may be demonstrated by fixing the tissue in chrome-osmium solutions or by using frozen section. Reduction of osmium by thiocarbohydrazide highly enhances lipid labeling. After formol/ glutaraldehyde fixation much of the lipid in the tissues is ‘bound’ and does not take up osmium. It can be unmasked by a saturated aqueous solution of thymol. Osmium taken up by tissue proteins at neutral pH is only a small fraction of that taken up by the lipid. Blackening of osmium tetroxide by unsaturated lipid is too unpredictable to demonstrate lipid in tissues. Direct fixation with neutral osmium tetroxide is an effective method for visualizing lipid for the electron microscope, but the poor penetration of tissue by osmium limits its use for light microscopy. . Fixation: 10% formalin Section: Cryostat section Method: 1. Collect frozen sections at l0 µ in distilled water. 2. Immerse in l % osmium tetroxide in the dark for 12-18 hours. 3. Wash in distilled water. 4. Wash thoroughly in tap water for 3 hours. 5. Counterstain if desired with l % safranin for l minute. 6. Rinse in distilled water. 7. Rinse in 70% alcohol. 8. Mount on to slides. 9. Blot dry. 10. Dehydrate rapidly, clear and mount. Results: Nuclei yellow-orange Fats black Fig. 19-4. Osmium Stain, peripheral nerve myelin Nile Blue Sulfate Method for Fats Nile blue sulfate is a dye capable of differentiating two lipid classes simultaneously by the action of its two components: a red oxazone which dissolves neutral lipids, and a blue oxazine which is basic and reacts with phospholipids and free fatty acids. Nile blue sulfate can be used as a preliminary indicator of the type of lipid present in the tissue section. Nile red is an excellent stain that is present as a minor component of commercial preparations of the non-fluorescent lipid stain Nile blue. Nile red is intensely fluorescent and, if proper spectral conditions are chosen, it can serve as a sensitive vital stain for the detection of cytoplasmic lipid droplets. Nile red provides resolution of cytoplasmic lipid droplets in tissues equal to, if not better than, that obtained with the non-fluorescent dye Oil red 0. Histochemical Methods Unlike the fat stains described above, histochemical methods involve chemical reactions with specific groups, radicals or bonds in the lipid molecule. Many of these methods are utilized mainly for research studies. Free Fatty Acids The histochemical demonstration of free acids is based on the observation that free fatty acids bind heavy metal ions such as copper to form soaps which can then be stained with Weigert's lithium hematoxylin, dimethylaminobenzidine rhodamine, or rubeanic acid. Calcium and iron deposits will also bind with copper, but can be distinguished from lipid by their persistence in a de-lipidized control section. They can be extracted with either 1% hydrochloric acid (for calcium) or 5% oxalic acid (for iron salts). Cholesterol Most of the earlier methods for demonstrating cholesterol were ineffective unless cholesterol had been oxidized, either chemically with ferric salts or by long exposure to atmospheric oxygen. An enzymatic method introduced by Emeis et al in 1977 based on the production of H2O2 from free cholesterol by cholesterol oxidase. It involves a two-stage procedure in which esterified cholesterol is initially hydrolyzed to its free sterol by means of a cholesterol esterase. Cholesterol is then oxidized by a cholesterol oxidase to release hydrogen peroxide, which reacts simultaneously with diaminobenzidine to produce an insoluble brown polymer at the site of cholesterol. Cholesterol esters can be demonstrated as cholesterol after hydrolysis by cholesterol ester hydrolase and has also been detected with the use of enzyme cholesterol esterase. These methods are of limited practical use because the reagents are expensive, and the procedures are too complex for routine light microscopy. An enzymatic method for the histochemical localization of cholesterol is presented. It makes possible the localization of free cholesterol, cholesterol esters, or both and is compatible with routine histological staining procedures. Cerebrosides The sulfate esters of cerebrosides (sulfatides) are generally deposited in brain and other organs of patients with sulfatide storage disease known as metachromatic leukodystrophy. Cerebrosides and related lipids are stained by the Periodic Acid Schiff (PAS) method, designed to stain mucopolysaccharides, and can be distinguished from glycogen by removal with diastase. Staining with cresyl violet produces a metachromatic orange color on sulfatides, in contrast to the orthochromatic purple color of other, less acidic myelin lipids. Toluidine blue is a standard metachromatic dye for acidic polymers, and imparts a yellow brown or purplish color to sulfatide deposits. The section is dehydrated with acetone to eliminate the metachromasia induced by less acidic groups. Gangliosides Neurons may have significant ganglioside storage giving rise to cells suggestive of gangliosidoses, but storage may not be obvious particularly in subtypes without mental retardation. The stored gangliosides are PAS (+), sudanophilic (+), and Luxol fast blue (+). Fig. 19-5. Abnormal metabolism and neuronal storage of fats in Gaucher’s disease (PAS stain) Gangliosides present in storage diseases like Tay-Sach's disease and Gm1 gangliosidosis are stained with conventional PAS method. They are distinguished from other glycolipids by their constituents, neuraminic acid and sialic acid. A modified PAS method reduces the concentration of the oxidizing agent (periodate) from 1 to 0.01% to stain sialo-groups that are oxidized more rapidly than other sugar glycoside. This modified PAS stain has been used to demonstrate gangliosides (the only glycolipids that contain sialic acids) within neurons in Tay-Sach's disease. REFERENCES Adams CWM. (1959) A histochemical method for the simultaneous demonstration of normal and degenerating myelin. Journal of Pathology and Bacteriology 77: 648. Adams CWM, Bayliss OB. (1968) Lipid histochemistry. In: Glick, D. and Rosenbaum, RM. (eds.) Techniques of Biochemical and Biophysical Morphology, vol.2. Wiley-Interscience, New York, 99. Bancroft JD, Stevens A. (1990) Theory and practice of histological techniques. 3rd ed. Churchill Livingstone. Bayliss High OB. (1981) The histochemical versatility of Sudan Black B. Acta Histochimica. Suppl.Band. XXIV, 5: 247. Callis G, Chifelle TL, et al. (1951) Propylene and ethylene glycol as solvents for Sudan IV and Sudan Black B. Stain Technology, 26: 51. Churukian CJ. (2000) Manual of the special stains laboratory, 8th ed. University of Rochester, Rochester NY. Dunnigan MG. (1968) The use of Nile blue sulphate in the histochemical identification of phospholipids. Stain Technology, 43: 249. Emeis JJ, Van Gent CM, Van Sabben CM. (1977) An enzymatic method for the histochemical localization of free and esterified cholesterol separately. Histochem J. 9(2):197-204. Gomori G. (1952) In: Microscopic Histochemistry. Chicago University Press, Chicago. Holczinger L. (1959) Histochemical demonstration of free fatty acids. Acta Histochem. 13; 8:167-75. Jones D. (1969) The reactions of formaldehyde with unsaturated fatty acids during histological fixation. Histochemical Journal. 1: 359. Jones ML. Lipids. Chapt 11 in: Bancroft J.D. and Gamble M, eds., Theory and Practice of Histological Techniques, 2nd ed., Churchill Livingstone, London, 201. Lillie RD. (1965) In: Histopathologic Technique and Practical Histochemistry, 3rd ed., Blakiston, New York. Menschik Z. (1953) Nile Blue histochemical method for phospholipids. Stain Technology 28: 13. Pearse AGE. (1951) A review of modem methods in histochemistry. Journal of Clinical Pathology, 4:1. Pearse AGE. (1985) vol. 2, Chapt 16. In: Histochemistry, Theoretical and Applied 4th ed., Churchill Livingstone, Edinburgh. Roussouw DJ, Chase CC et al. (1976) The histochemical localization of cholesterol in formalin-fixed and fresh frozen sections. Stain Technology, 51: 143. Sheehan DC, Hrapchak BB. (1980) Theory and Practice of Histotechnology, 2nd ed., Mosby, St. Louis. Suvarna SK, Layton C, Bancroft JD. (2013) Bancroft’s Theory and Practice of Histological Techniques, 7th ed. Churchill Livingstone, Elsevier. Tracy RE and Walia P. (2002) A method to fix lipids for staining fat embolism in paraffin sections. Histopathology 41: 75-79. Tracy RE and Walia P. (2004). Lipid fixation for fat staining in paraffin sections applied to lesions of atherosclerosis. Virchows Arch. 445(1):22-6. Epub 2004 Jun 2. Wigglesworth VB. (1957) The use of osmium in the fixation and staining of tissues. Proceedings of the Royal Society (London), 8147: 185. Wigglesworth VB. (1988) Histological staining of lipids for light and electron microscope. Biological Reviews. 63: 3, 417–431. CHAPTER 20 STAINING OF PROTEINS AND NUCLEIC ACIDS Protein is the basic component of living cells and is made of carbon, hydrogen, oxygen, nitrogen and one or more chains of amino acids linked by peptide bonds. Based on chemical composition, they occur in tissues either as: 1) Simple proteins: On hydrolysis they yield only the amino acids and occasional small carbohydrate compounds. Examples are: albumins, globulins, structural proteins, enzymes, histones and protamines. Simple proteins can be demonstrated in tissue by histologic methods, amino acid histochemical methods, enzyme histochemical methods, and immunocytochemical methods. 2) Conjugated proteins: These are simple proteins combined with some non-protein material in the body to form complex proteins. Examples are: lipoproteins, mucoproteins, nucleoproteins, glycoproteins, and phosphoproteins. 3) Derived proteins: These are proteins derived from simple or conjugated proteins by physical or chemical means. Examples are: denatured proteins and peptides. The three types of proteins based on physical configuration are fibrous, globular, and membrane. 1) Fibrous Proteins form muscle fiber, tendons, connective tissue and bone. Examples of fibrous proteins are actin, collagen, elastin, fibronectin, myosin, tau, tropomyosin and tubulin. The organic portion, or protein fibers, found in connective tissues are either collagen, elastic, or reticular fibers. Fibrous proteins are often structural, such as collagen, the major component of connective tissue, or keratin, the protein component of hair and nails. Collagen fibers provide strength to the tissue, preventing it from being torn or separated from the surrounding tissues. Histologic methods involve the demonstration of fibrous proteins based on the physical configuration of their molecules, rather than their chemical composition. Fibrous proteins can be demonstrated by selective staining with small or large molecule dyes (trichrome method), and silver impregnation (reticulin method), and specific dye-protein interactions (e.g., Congo red stain for amyloid). 2) Globular proteins are more water soluble than the other classes of proteins and they have several functions including transporting, catalyzing, and regulating. Almost all globular proteins are soluble and many are enzymes. Globular proteins are found in blood and tissue fluids in amorphous globular form with very thin or non-existent membranes. Examples of globular proteins are albumins, alpha globulin, beta globulin, fibrin, gamma globulin, hemoglobin immunoglobulins and myoglobin. 3) Membrane Proteins play several roles including relaying signals within cells, allowing cells to interact, and transporting molecules. Membrane proteins often serve as receptors or provide channels for polar or charged molecules to pass through the cell membrane. Examples of membrane proteins include c-myc, estrogen receptor, glycophorin D, histones, hydrolases, oxidoreductases, and p53. NUCLEIC ACIDS Nucleic acids are usually combined with basic proteins to form nucleoproteins. They consist of alternate sugar and phosphate groups, with a nitrogenous base attached to each sugar group. There are two major nucleic acids. Deoxyribonucleic acid (DNA) contains a 5-carbon sugar deoxyribose, and is mainly found in the nucleus of the cell. The four nitrogenous bases of DNA are purines (adenine and guanine) and pyrimidines (thymine and cytosine). Ribonucleic acid (RNA) is found in the cytoplasm, and to a lesser extent in the nucleus, particularly in the nucleolus. It contains ribose sugar with attached nitrogenous bases of purines (adenine and guanine) and pyrimidines (uracil and cytosine). Principles of Staining Staining depends largely on the attachment of dyes to proteins that have both positively and negatively charged groups. Phosphate groups of DNA also are important in nuclear staining. A tissue section contains many proteins that differ in their isoelectric points. At an ideal pH, certain tissue components will show a relative acidophilia whereas others display a relative basophilia. If the pH is adjusted outside the range of about 4 - 8, some groups cease to ionize altogether, and their staining is inhibited almost completely. For carboxyl groups the relevant pH is about 4 and below. As the pH alters, there is an impact on staining, but the impact is gradual. When the pH is at 1.5, no carboxyl groups are involved with staining. However, phosphate radicals are still ionizable at that pH and nuclear staining can still be done, although it tends to be highly selective. Adding a very small amount of acetic acid to 1%-2% aqueous solutions of neutral red, or the addition of borax to methylene blue can sharpen nuclear staining. This small amount of acid slightly inhibits the ionic staining of background tissues, making the largely unaffected ionic nuclear staining appear more prominent. The final pH is usually about 4, depending on the buffering capacity of other ingredients. This increases the ionization of tissue amino groups. Similarly, minor adjustments to make solutions more alkaline can be done with compounds such as sodium tetraborate (borax) or sodium carbonate. Acidophilic dyes are attracted to acidic substances, such as mitochondria and collagen which are anionic (negatively charged) at physiologic pH. Many proteins are acidophilic at physiologic pH. The aniline dye, eosin, is an acid dye that stains cytoplasm, muscle, and connective tissues various shades of pink and orange. Eosin is a red or pink stain that is Acidic / Negative. It binds to acidophilic substances (such as proteins - which are basic and positively charged).Commonly substituted acid dyes include orange G or phyloxine. Eosin is an acid aniline dye that will bind to and stain basic structures (or negatively charged structures), such as cationic amino groups on proteins. Cytoplasm, muscle, connective tissue, colloid, red blood cells and decalcified bone matrix all stain pink to pink/orange/red with eosin. For acidic dyes, the dye in question can often in addition be selective for particular acidophilic components. I.e. a technique called the Mallory staining technique uses three acidic dyes: aniline blue, acid fuchsin and orange G, which selectively stain collagen, cytoplasm and red blood cells respectively. Most proteins in the cytoplasm are basic because they are positively charged due to the arginine and lysine amino acid residues. These form salts with acid dyes containing negative charges, like eosin. Therefore, eosin binds to these amino acids/proteins and stains them pink. This includes cytoplasmic filaments in muscle cells, intracellular membranes, and extracellular fibers. Basophilic dyes are attracted to basic substances, which are cationic (positively charged) at physiologic pH. Proteins are basophilic at a pH lower (more acidic) than their isoelectric point. When the environmental pH is below a protein's isoelectric point, the protein is negatively charged and hence basophilic. DNA/RNA in the nucleus, and RNA in ribosomes in the rough endoplasmic reticulum are both acidic because the backbones of nucleic acids are negatively charged due to presence of phosphate groups. The negatively charged acidic backbones form salts with basic dyes containing positive charges. Therefore, dyes like hematoxylin will bind to DNA and RNA and stain them violet. Proteoglycans are basophilic due to sugars and esterified sulfates which are negative at physiologic pH. For basic dyes, the reaction of the anionic groups of cells (these include the phosphate groups of nucleic acids, sulphate groups of glycosaminoglycans, and carboxyl groups of proteins) depends on the pH at which they are used. Hematoxylin (derived from hematein) is not strictly a basic dye, but it is used with a 'mordant' that makes this stain act as a basic dye that is generally used in combination with aluminum ions. The mordant (aluminum salt) binds to the tissue, and then hematoxylin binds to the mordant, forming a tissue-mordanthematoxylin linkage. DNA (heterochromatin and the nucleolus) in the nucleus, and RNA in ribosomes and in the rough endoplasmic reticulum are both acidic, so nuclear heterochromatin stains blue and the cytoplasm of cells rich in ribonucleoprotein also stains blue or purple. The cytoplasm of cells with minimal amounts of ribonucleoprotein tends to be lavender in color. This difference in staining intensity is useful in differentiating one tissue from another. Common basic dyes often substituted for hematoxylin include methylene blue, toluidine blue, thionine, carmine, basic fuchsin, and azure II. It may be used after any fixation except fixation with osmium tetroxide. Frequently, basic dyes (methylene blue, toluidine blue, thionine) will react with a specific tissue component and impart to it a color different from that of the dye itself. This phenomenon is called metachromasia and the cell or tissue components that exhibit it are said to be metachromatic. Hematoxylin & Eosin Stain (H & E) The staining method involves application of hemalum, a complex formed from aluminum ions and hematin (an oxidation product of hematoxylin). Hemalum colors nuclei of cells (and a few other objects, such as keratohyalin granules and calcified material) blue. The nuclear staining is followed by counterstaining with an aqueous or alcoholic solution of eosin Y, which colors eosinophilic structures in various shades of red, pink and orange. The staining of nuclei by hemalum occurs due to binding of the dye-metal complex to DNA, but nuclear staining can be obtained after extraction of DNA from tissue sections. The mechanism is different from that of nuclear staining by basic (cationic) dyes such as thionine or toluidine blue. Staining by basic dyes occurs only from solutions that are less acidic than hemalum, and it is prevented by prior chemical or enzymatic extraction of nucleic acids. There is evidence to indicate that coordinate bonds, similar to those that hold aluminum and hematein together, bind the hemalum complex to DNA and to carboxy groups of proteins in the nuclear chromatin. The eosinophilic structures are generally composed of intracellular or extracellular protein. Most of the cytoplasm is eosinophilic. Red blood cells are stained intensely red. Histochemical Identification of Proteins Histochemical methods are used to demonstrate the presence of amino acid molecules rather than whole protein molecules. They are based upon identification of specific linkages or groups within the amino acid molecule such as the protein bound amino groups (e.g. in lysine), phenyl groups (e.g. in tyrosine), disulfides and sulfhydryl linkages (e.g., in cystine and cysteine), indole groups (e.g., in tryptophan and tryptamine) and guanidyl groups (e.g., in arginine). Methods for histochemical detection of specific proteins or of characteristic groups in proteins are few, and some of those presently available are somewhat cumbersome for routine histological use, or result in formation of highly unstable color complexes. If the various amino acids in tissues are to be demonstrated histochemically, it is important to avoid fixatives such as mercuric chloride which react with amino acid groups. Neutral buffered formol saline is the most commonly used fixative for amino acid histochemistry. Many of the microscope slides are prepared using material embedded in plastic rather than in paraffin. The plastic embedding medium (glycol methacrylate) is commonly used in histology and pathology because some of the artifacts (shrinkage and distortion) caused by hot paraffin can be largely avoided. Furthermore, plastic embedded sections can be cut at 1 or 2 micrometers thick, allowing for improved visualization of the tissue. Because H&E stains can be problematic with methacrylate, some of the plastic embedded material is stained using a combination of substitute dyes that look similar to H&E but without the problems. Staining of ribboned epon sections 0.3-2 μ thick with two intense acid dyes, Aniline Blue Black and Coomassie Brilliant Blue R 250 for light microscopy allows precise localization of proteins and, because the sections are ribboned, facilitates three-dimensional visualization of the structures involved. The dyes may be used in combination with the periodic acid-Schiff reaction and with autoradiography. Alkaline Fast-Green Method for Basic Proteins (especially protamines and histones) Fast Green is an acid dye that stains basic groups in the tissues, particularly basic protamines and histones which have higher isoelectrical points than the pH of the staining solution. All other proteins have lower isoelectric points: their basic groups are not ionized and therefore will not stain. Trichloracetic acid is used to remove nucleic acid which would otherwise mask the basic group of protamines and histones. Peracetic Acid-Alcian Blue for Cystine and Cysteine Peracetic Acid oxidizes cystine and cysteine, forming strong cysteic acid which is stained blue-green by a basic dye. Sakaguchi’s test for arginine uses NaOH, sodium hypochlorite (Milton's reagent) and pyridine chloroform, producing orange-red color on objects containing arginine. The mechanism is not known. Proteins with enzyme properties can be demonstrated by histochemical methods, based on their effect on specific substrates. Recently developed immunocytochemical methods have also been successful in identifying and localizing specific proteins such as immunoglobulins, enzymes and hormones. Proteoglycans Proteoglycans are proteins that are heavily glycosylated. The basic proteoglycan unit consists of a "core protein" with one or more covalently attached glycosaminoglycan chain(s). The chains are long, linear carbohydrate polymers that are negatively charged under physiological conditions due to the occurrence of sulfate and uronic acid groups. Proteoglycans occur in the connective tissue and are a major component of the extracellular matrix. The protein component of proteoglycans is synthesized by ribosomes and translocated into the lumen of the rough endoplasmic reticulum. An inability to break down proteoglycans is characteristic of a group of genetic disorders, called mucopoly-saccharidoses. The inactivity of specific lysosomal enzymes that normally degrade glycosaminoglycans leads to the accumulation of proteoglycans within cells causing a variety of disease symptoms, depending upon the type of proteoglycan that is not degraded. Alcian Blue-PAS Staining for Proteoglycans This is a combined method utilizing the properties of both the PAS and Alcian blue methods to demonstrate the full complement of tissue proteoglycans. The rationale of the technique is that by first staining all the acidic mucins with Alcian blue, those remaining acidic mucins which are also PAS positive will be chemically blocked and will not react further during the technique. Those neutral mucins which are solely PAS positive will subsequently be demonstrated in a contrasting manner. Where mixtures occur, the resultant color will depend upon the dominant moiety. STAINING OF NUCLEIC ACIDS Demonstration of nucleic acids depends upon either reaction of the dyes with the phosphate groups, or production of aldehydes from the sugar (deoxyribose). No histochemical methods are available to demonstrate the nitrogenous base. • Feulgen technique - demonstrates sugar • Methyl green pyronin technique - demonstrates phosphate • Acridine orange (by fluorescent method) • Gallocyanin-chrome alum method demonstrates both DNA and RNA This last staining method does not separate the two nucleic acids since it stains both DNA and RNA blue, and suitable extraction technique must be used. DNA is demonstrated by the Feulgen technique which uses 1 M HCl at 60°C to hydrolyze and break the purine-deoxyribose bond, thereby exposing the aldehydes which are then stained by Schiff's reagent. RNA is demonstrated by the methyl green-pyronin technique where methyl green stains the nuclei by binding preferentially and specifically to DNA, while pyronin binds to RNA and stains the cytoplasm red. Phosphate groups of DNA and RNA are acidic and combine with hematoxylin and other basic dyes by salt linkages. Nucleic acids are best preserved in alcoholic and acidic fixatives (especially Carnoy's fluid that contains both alcohol and glacial acetic acid). Formalin is an acceptable fixative, but has only limited reaction with DNA and RNA. Strong inorganic acids such as nitric or hydrochloric acid will extract nucleic acids, and should be avoided. A number of routine histological fixatives such as Zenker's, Susa's, and Carnoy's do not allow specific nuclear staining. The presence of mercuric chloride in Zenker's and Susa's fluids is apt to introduce a staining artefact since a divalent metal ion might serve as a link between carboxyl groups and acid dye ions. Feulgen Staining for Nuclear DNA (Pearse 1968; Carson 1983) Feulgen stain is a staining technique used to identify chromosomal material or DNA in cell specimens. Acid hydrolysis removes purine bases from the DNA, thereby unmasking free aldehyde groups. Feulgen reaction allows DNA in situ to be specifically stained based on the reaction of Schiff or Schiff-like reagents with the free aldehyde groups in proportion to the DNA concentration in the cell which results in the purple staining. RNA is not hydrolyzed by the HCl treatment and, thus, the reaction is DNA-specific. The specimen is subjected to warm (60°C) hydrochloric acid, then to Schiff reagent. Optionally, the sample can be counterstained with Light Green SF yellowish. Finally, it is dehydrated with ethanol, cleared with xylene, and mounted in a resinous medium. DNA should be stained red. The background, if counterstained, is green. The Feulgen reaction is considered to be specific for DNA. The other nucleic acid, RNA, does not react the same way either because the acid hydrolysis causes it to dissolve away, or because of the hydroxyl group present in ribose which has lost its oxygen in deoxyribose. It is important to note, however, that if acid hydrolysis is applied for too long, especially at elevated temperature, then DNA also can be completely removed, and this is a known source of failure in the technique. It depends on acid hydrolysis of DNA, therefore fixing agents using strong acids should be avoided. FIXATION: Zenker’s, Carnoy’s, Formalin, Kelly's, Regaud's, Flemming’s, and Susa (except Bouin's and Brasil's fixatives due to their acid components which may hydrolyze nucleic acid in varying degrees and duration). 5µ paraffin sections of neutral buffered formalin fixed tissue are suitable. Fixatives containing strong acids should be avoided as this method depends on the acid hydrolysis of DNA, and acids in some fixatives may prehydrolyze the tissue (such as picric acid in Bouin's aqueous formal-picricacetic mixture). Formula: Solution A (1 M hydrochloric acid) Hydrochloric acid (concentrated) 83.5 ml Distilled water 916.5 ml Solution B: Schiff's reagent (to prepare) Boil 200ml of distilled water, remove flask from Bunsen and add 1g of basic fuchsin. Allow to cool to 50°C. Add 2g of potassium metabisulphate while mixing. Cool to room temperature and add 2ml of concentrated hydrochloric acid mix and stand in the dark overnight. Add a large amount of activated charcoal, shake well and filter. The solution should be clear/pale yellow. Store at 4°C Solution C: Bisulfite Solution 10% potassium metabisulfite 10 ml 1M hydrochloric acid 10 ml Distilled water 180 ml Method: 1. Deparaffinize sections to water. 2. Rinse sections in 1 M HCl at room temperature. 3. Place sections in 1 M HCl at 60°C for 8 minutes (for Carnoy or formalin fixed tissue). 4. Rinse in 1 M HCl at room temperature for 1 minute. 5. Transfer sections to Schiff's reagent for 45 minutes. 6. Rinse sections in bisulfite solution for 2 minutes. 7. Repeat wash in bisulfite solution for 2 minutes. 8 Repeat wash in bisulfite solution (3rd wash) for 2 minutes. 9. Rinse well in distilled water. 10. Counterstain (optional) in 1% light green for 2 minutes. 11. Wash in water. 12. Dehydrate through alcohols to xylene and mount. Fig. 20-1. Feulgen Reaction Results: DNA red purple Cytoplasm green NOTES: 1. Specific hydrolysis time should be observed, based on fixative used. Tissue fixed with formaldehyde vapor should be hydrolyzed for 30 to 60 minutes, while tissue fixed in Zenker solution should be hydrolyzed for only 5 minutes. 2. After immersing the slide in Schiff's reagent, it is usually flooded with bisulfite solution before transferring it to water, to remove the excess Schiff's reagent from the section, while preventing its oxidation back to basic fuchsin. If a slide is transferred directly to water from Schiff's reagent, basic fuchsin will form again, producing a false positive result. Methyl Green-Pyronin method for RNA and DNA (from Bancroft & Cook 1994) Methyl green-pyronin method uses the basic dyes to produce a differential staining reaction for DNA and RNA, respectively. Methyl green is highly selective for DNA, coloring it green due to the binding of anionic phosphate group with the stain. Pyronin is somewhat specific for RNA, giving it a pinkish red color. Methyl green-pyronin stain is also utilized to detect the presence of plasma cells and lymphocytes. Fixation: 10% Formalin, absolute alcohol, Zenker's fluid, or Carnoy's fluid Staining solution: 2% methyl green (chloroform washed) 9 ml 2% pyronin Y 4 ml Acetate buffer pH 4.8 23 ml Glycerol 14 ml Mix well before use. Method: 1. Sections to water. 2. Rinse in acetate buffer pH 4.8. 3. Place in staining solution for 25 minutes. The staining solution used for plasma cells works better on Zenker fixed materials. 4. Rinse in buffer. 5. Blot dry. 6. Rinse in 93% alcohol, then in absolute alcohols. 7. Clear in xylene and mount with appropriate medium. Results: DNA (Chromatin) Green or blue-green RNA (Nucleoli) Rose-red; Granules Dark rose-red Plasma cell cytoplasm Purple Fluorescent Staining for DNA and RNA Fluorochromes are fluorescent dyes which emit light or visible radiation energy when excited by light of shorter wave length, either visible or ultraviolet. Disadvantages associated with fluorescent labels include the need for a special light' source, limited morphology because of poor counterstaining, fading of the signal on storage, and intrinsic tissue auto fluorescence that is increased by fixation. Several fluorochrome tracers are presently available: 1. Fluorescein is still the most widely used fluorochrome, because of its wide absorption spectrum and blue light range. Its characteristic apple green emission is rarely seen as "auto fluorescence" in mammalian tissue, which is often blue in color. 2. Rhodamine conjugates absorb maximally in green light, exhibiting an orange-red emission, and are commonly used in two-color techniques. 3. Acridine Orange is the most commonly used fluorochrome to demonstrate DNA and RNA in fresh or fixed tissues, combining with nucleic acids in cells by salt linkages and cohesion. DNA emits a yellowgreen fluorescence while RNA is stained brick to orange-red. This is used for screening of cervical smears for cancer cells. While it has been used in exfoliative cytology and with alcohol fixed tissues, the results are not permanent and the technique does not work on formalin-fixed tissues. 4. Acriflavine, as a 0.01% alcoholic solution, can be used as an alternative to basic fuchsin in Schiff's reagent, for the Feulgen technique of acid hydrolysis. DNA is stained by a fluorescent yellow color in this Feulgentype reaction. Immunohistochemistry Immunohistochemical staining of tissue sections is perhaps the most commonly applied protein immunostaining technique. While the first cases of immunohistochemical staining used fluorescent dye, other non-fluorescent methods using enzymes such as peroxidase and alkaline phosphatase are now used. These enzymes are capable of catalyzing reactions that give a colored product that is easily detectable by light microscopy. Immuno-electron microscopy allows the detection of specific proteins in ultrathin tissue sections. Antibodies labelled with heavy metal particles (e.g. gold) can be directly visualized using transmission electron microscopy. While powerful in detecting the sub-cellular localization of a protein, immuno-electron microscopy can be technically challenging, expensive, and require rigorous optimization of tissue fixation and processing methods. Antigen Retrieval Formalin-fixed, paraffin-embedded (FFPE) tissues may be stored indefinitely at room temperature, and nucleic acids (both DNA and RNA) may be recovered from them decades after fixation. Many antigens can be successfully demonstrated in formalin-fixed paraffin-embedded tissue sections. However, some antigens will not survive even moderate amounts of aldehyde fixation. Under these conditions, tissues should be rapidly fresh frozen in liquid nitrogen and cut with a cryostat. The disadvantages of frozen sections include poor morphology, poor resolution at higher magnifications, difficulty in cutting over paraffin sections, and the need for frozen storage. The detection of many antigens can be dramatically improved by antigen retrieval methods that act by breaking some of the protein cross-links formed by fixation to uncover hidden antigenic sites. Electron Microscopy For electron microscopy, the most commonly used fixative is glutaraldehyde, usually as a 2.5% solution in phosphate buffered saline. These fixatives preserve tissues or cells mainly by irreversibly cross-linking proteins. The main action of these aldehyde fixatives is to cross-link amino groups in proteins through the formation of methylene bridges (-CH2-), in the case of formaldehyde, or by a C5H10 cross-links in the case of glutaraldehyde. This process, while preserving the structural integrity of the cells and tissue can damage the biological functionality of proteins, particularly enzymes, and can also denature them to a certain extent. This can be detrimental to certain histological techniques. Further fixatives are often used for electron microscopy such as osmium tetroxide or uranyl acetate. Phosphotungstic acid has long been used as a protein precipitant for positive staining of whole muscle and collagen fibrils. Phosphotungstic acid acts as an anionic stain for the positively charged groups of protein and has been used sporadically as a positive stain in tissue sections, usually as an adjunct to other stains after osmium tetroxide fixation. Phosphotungstic acid in aqueous solution serves as a single and reliable stain for aldehyde-fixed tissue, with a view to its potential use in quantitative electron microscopy. After aldehyde-fixation, treatment with phosphotungstic acid in aqueous acidic medium produces an intense electron-opaque stain with minimal distortion of organelles. Mitochondrial matrix, cisternae of the endoplasmic reticulum, and the Z-band of muscle are densely stained. The intensity of stain reflects the concentration of protein based on the quantitative reaction of phosphotungstic acid with the positively charged groups, and can provide a basis for the use of the method in quantitative electron microscopy, particularly on thin sections. Polyacrylamide Gel Electrophoresis Polyacrylamide gel electrophoresis (PAGE) is a technique that is widely used to separate biological macromolecules, usually proteins or nucleic acids, according to their electrophoretic mobility. Following electrophoresis, the gel may be stained (for proteins, most commonly with Coomassie Brilliant Blue R-250, ethidium bromide; or silver stain), allowing visualization of the separated proteins. After staining, different biomolecules appear as distinct bands within the gel. It is common to run molecular weight size markers of known molecular weight in a separate lane in the gel to calibrate the gel and determine the approximate molecular mass of unknown biomolecules by comparing the distance traveled relative to the marker. DNA is demonstrated by the following extraction techniques: • Digestion Method: Pure deoxyribonuclease will digest DNA and pure ribonuclease will digest RNA • Chemical Methods using: o 10% perchloric acid at 4oC overnight to remove RNA o Trichloroacetic acid o Hydrochloric acid Stains that allow visualization of the protein pattern in the gel. • Coomassie Stains The most popular anionic protein dye, Coomassie Brilliant Blue, stains almost all proteins. Coomassie Brilliant Blue: R-250 (R for reddish) offers shorter staining times than G-250 (G for greenish). Coomassie dyes are also the favorite stains for mass spectrometry and protein identification. Ethylene Bromide Ethidium bromide is a sensitive, easy stain for DNA. The major drawback to ethidium bromide is that it is a potent mutagen. Solutions must be handled with extreme caution, and decontaminated prior to disposal. The dye may be run in the gel with the DNA if desired, eliminating a separate staining/de-staining process, and nondestructive nature of ethidium bromide staining have made it the standard stain for double stranded DNA. • Silver Stains Silver stains offer the highest sensitivity, although protocols are often time-consuming, complex, and do not offer sufficient reproducibility for quantitative analysis. Protein sensitivity to silver stain offers sensitivity that exceeds that of Coomassie and is equivalent to most fluorescent stains. Fluorescent Stains These stains are ideal for protein study but are more expensive than Coomassie or silver stains and require either a CCD (charge-coupled device) camera or fluorescence scanner for gel imaging. A silver staining technique has been widely used to detect DNA fragments with high sensitivity on polyacrylamide gels. The conventional procedure of the silver staining is tedious, which takes about 40–60 min and needs five or six kinds of chemicals and four kinds of solutions. Eliminating ethanol, acetic acid, and nitric acid precession before silver impregnation and using minimal AgNO3 dose on polyacrylamide gel results in a golden yellow staining and transparent background with high sensitivity of the silver-stained DNA. Silver staining aids the visualization of targets of intracellular and extracellular cellular components such as DNA and proteins, such as type III collagen and reticulin fibers in microscopy of histological sections; in temperature gradient gel electrophoresis; and in polyacrylamide gels. It is also used in karyotyping. Silver nitrate stains the nucleolar organization region (NOR)-associated protein, producing a dark region wherein the silver is deposited and denoting the activity of RNA genes within the NOR. Silver stains are also employed in applications that previously employed radiolabeling because they can achieve comparable levels of detection without the environmental and economic concerns associated with the use of radioisotopes. Silver stain is more sensitive and stains lower (2-5 ng) concentrations of single stranded and double stranded DNA 2-5 ng protein, compared to ethidium bromide (10 ng double stranded DNA) and Coomassie blue (>= 60 ng protein). Silver staining relies on the reduction of silver cations to insoluble silver metal by nucleic acids which are deposited in gel, creating a “latent image” that then becomes visible by soaking the gel in a solution of silver cations and a reducing agent. The silver granules in the latent image catalyze the further reduction and deposition of silver from the solution. Bands manifest as dark brown or black regions which appear before significant background develops. Development of the bands is stopped by altering the pH of the gel to a point where silver reduction is no longer favored. IN-SITU HYBRIDIZATION The definitive, most sensitive technique for identifying DNA is in-situ hybridization. The technique uses a labeled complementary DNA, RNA or modified nucleic acids strand (or probe) to localize a specific DNA, RNA, nucleic acid sequence or gene expression within a cell, in contrast with immunohistochemistry, which usually localizes proteins in tissue sections. After hybridizing a labeled complementary DNA or, a complementary RNA (riboprobe) to the target sequence at elevated temperature, the excess probe is washed away (after prior hydrolysis using RNase in the case of unhybridized, excess RNA probe), and the probe that was labeled with either radio-, fluorescent- or antigen-labeled bases (e.g., digoxigenin) is localized and quantified in the tissue either by autoradiography, fluorescence microscopy, or immunohistochemistry, respectively. The target nucleic acid is retained in-situ and is not degraded by nucleases, so that it becomes accessible for hybridization to the probe. There are two basic ways to visualize the RNA and DNA targets in situ—by fluorescence (FISH) and by chromogenic (CISH) detection. In situ hybridization (FISH) multiple targets can be visualized simultaneously and co-localized multiple gene expression patterns within a single specimen using spectrally distinct fluorophore labels for each different hybridization probe. Chromogenic in situ hybridization (CISH) reveals genetic information in the context of tissue morphology using methods that already available in histology lab. Markers used to detect the target molecule include isotopes, chromogenic and fluorescent digoxigenin (DIG). Genes and their transcripts can now be demonstrated by insitu nucleic acid hybridization techniques for specific identification of DNA and RNA sequences. In-situ hybridization has become applicable in routine laboratories due to the introduction of recombinant DNA technology (by which sequences of nucleic acids, either DNA or RNA, could be amplified by cloning and purified to very high levels), and nick translation methods (incorporating labeled nucleotides into purified DNA and synthesizing a biotinylated nucleotide) for non-radioactive in-situ labeling. In-situ hybridization involves the pre-treatment of cellular preparations to unmask the target nucleic acids, and hybridization of a nucleic acid probe, of complementary base sequence, to the target cell. This enables specific nucleic acid sequences or "genes", such as DNA of specific viruses, to be demonstrated and localized inside individual cells and viewed under the microscope. The technique is now widely used for the detection of abnormal genes, identification of viral infection, and for tumor phenotyping. Nonradioactive in situ hybridization, can be combined with immunochemistry to identify specific DNA or RNA molecules with fluorescent probes or tags that can be used for immuno-fluorescence and enzyme-linked fluorescence signal amplification (especially alkaline phosphatase and tyramide signal amplification). DNA in the sample is easy is a highly stable molecule and can be easily preserved in the sample for subsequent in-situ hybridization. On the other hand, preserving RNA is much more difficult due to presence of RNase enzyme that may be found on glassware, in reagents and on the operator and their clothing. RNase will quickly destroy any RNA in the cell or the RNA probe itself. Therefore, users must ensure they use sterile techniques, gloves, and solutions to prevent RNase from contaminating and destroying the probe or tissue RNA. For good results, older slides should not be stored dry at room temperature. They should be stored either in 100% ethanol at -20°C, or in a plastic box covered in saran wrap at -20°C or -80°C. Slides stored in this way can be used for several years. RNA probes should be between 250 to 1500 bases in length. Probes approximately 800 bases long exhibit the highest sensitivity and specificity. Ideally transcription templates should allow for transcription of both probe (antisense strand) and negative control (sense strand) RNAs. DNA probes can also provide high sensitivity for in situ hybridization. However, they do not hybridize as strongly to the target mRNA molecules as RNA probes. Therefore, formaldehyde should not be used in the post hybridization washes when using DNA probes. Fig. 20-2. Localization by in situ hybridization of amplified ribosomal DNA Specificity of the probe is extremely important. If the exact nucleotide sequence of the mRNA or DNA in the cell is known, a precise complementary probe can be designed. If over 5% of the base pairs are not complementary, the probe will hybridize only loosely to the target sequence. This means the probe is more likely to be washed away during wash and detection steps and the probe may not be detected, or only some of the sites may be detected and the labeling will not be an accurate representation. Polymerase Chain Reaction (PCR) In-situ hybridization techniques are now also supplemented by the polymerase chain reaction (PCR) method whereby a single copy or a few copies of a piece of DNA can be amplified across several orders of magnitude, generating thousands to millions of copies of a particular DNA sequence. In-situ PCR potentially provides a means of detecting single copies of nucleic acid sequences in cellular preparations. The method relies on thermal cycling, through cycles of repeated heating and cooling of the reaction for DNA melting and enzymatic replication of the DNA. Primers (short DNA fragments) containing sequences complementary to the target region along with a DNA polymerase, which the method is named after, are key components to enable selective and repeated amplification. As PCR progresses, the DNA generated is itself used as a template for replication, setting in motion a chain reaction in which the DNA template is exponentially amplified. Three major steps are involved in a Polymerase Chain Reaction. These three steps are repeated for 30 or 40 cycles and done on an automated cycler, a device which rapidly heats and cools the test tubes containing the reaction mixture. Each step -- alteration of structure (denaturation), annealing (joining), and extension takes place at a different temperature: 1) Denaturation - The DNA is heated at 95oC, breaking the weak hydrogen bonds that hold the double-stranded DNA, thereby creating two separate single stranded DNA. 2) Primer Annealing - At medium temperatures, around 54oC, the mixture is cooled, allowing primers to bind (anneal) to their complementary single-stranded DNA "template" (The template is the sequence of DNA to be copied.) On the small length of double-stranded DNA (the joined primer and template), the polymerase attaches and starts copying the template. 3) Extension - The reaction is then heated to 72oC, the optimal temperature for DNA polymerase to act, and DNA building blocks complementary to the template are coupled to the primer, making a double stranded DNA molecule and adding nucleotides onto the primer in a sequential manner, using the target DNA as template. With one cycle, a single segment of double-stranded DNA template is amplified into two separate pieces of double-stranded DNA. These two pieces are then available for amplification in the next cycle. As the cycles are repeated, more and more copies are generated and the number of copies of the template is increased exponentially. The cycles are done on an automated cycler, a device which rapidly heats and cools the test tubes containing the reaction mixture. The PCR amplification of target nucleic acid sequence is more sensitive than other hybridization methods, but may produce false positive results due to contamination and non-specific priming. Reverse transcription polymerase chain reaction (RT-PCR), one of many variants of polymerase chain reaction (PCR), is the most sensitive technique for mRNA detection and quantitation currently available. In RT-PCR, the RNA template is first converted into a complementary DNA (cDNA) using a reverse transcriptase. The cDNA is then used as a template for exponential amplification using PCR. The first step in RT-PCR uses reverse transcriptase and a primer to anneal and extend a desired mRNA sequence. If the mRNA is present, the reverse transcriptase and primer will anneal to the mRNA sequence and transcribe a complimentary strand of DNA. This strand is then replicated with primers and Taq Polymerase, and the standard PCR protocol is followed. This protocol copies the single stranded DNA millions of times in a small amount of time to produce a significant amount of DNA. In Situ PCR In Situ Polymerase Chain Reaction (In situ PCR) is a powerful method that detects minute quantities of rare or single-copy number nucleic acid sequences in frozen or paraffin-embedded cells or tissue sections for the localization of those sequences within the cells. In this method, the polymerase chain reaction actually takes place in the cell on a slide, and the product can be visualized in the same way as in traditional in situ hybridization. Either DNA or RNA can be detected through the combined examination of PCR/RT-PCR and Histology. The ability to identify individual cells, expressing or carrying specific genes of interest in a latent form in a tissue section under the microscope provides a visual account of silent genes, and allows the determination of various aspects of normal versus pathological conditions, or latent versus active viral replication. The principle of this method involves tissue fixing (to preserve the cell morphology) and subsequent treatment with proteolytic digestion (to provide access for the PCR reagents to the target DNA). The target sequences are amplified by those reagents and then detected by standard immunocytochemical protocols. In situ PCR combines the sensitivity of PCR or RT-PCR amplification along with the ability to perform morphological analysis on the same sample, and thus it is an attractive tool in diagnostic applications. One of the most prominent applications is the detection of infectious disease agents including HIV-1, HBV, HPV, HHV-6, CMV, and EBV. Successful in situ hybridization and PCR can be done with unfixed, frozen tissue or after fixation in acetone, ethanol, or buffered formalin. Fixatives that include a heavy metal or picric acid do not allow for PCR because of the rapid and extensive degradation of the DNA. 100% detection of the target is achieved only when prolonged formalin fixation is followed by protease digestion. PCR in situ hybridization is best used to detect DNA in paraffin-embedded tissue sections. As with standard in situ hybridization or PCR, variables that can affect in situ PCR results include type of fixative and time of fixation, protease digestion, and the composition of the amplifying solution and oligoprobe cocktail. REFERENCES Alfert M, Geschwind I. (1953) A selective staining method for the basic proteins of cell nuclei. Proceedings of the Natl Academy of Sciences 39 (10): 991-998; Angerer LM, Angerer RC. (1992) In situ hybridization to cellular RNA with radiolabeled RNA probes. In: Wilkinson DG (ed). In situ Hybridization: A Practical Approach, University Press, Oxford, 15. Baker JR. (1962) Experiments on the action of mordants. 2. Aluminium-haematein. Quart. J. Microsc. Sci. 103: 493-517. Bancroft JD. (2002) Proteins and nucleic acids. Chapt 12, pp 231 -242. In: Theory and Practice of Histological Techniques. 5th ed., Churchill Livingstone, Elsevier. Bancroft JD. (2002) Enzyme histochemistry and its diagnostic implications. Chap. 27, pp. 593-620. In: Theory and Practice of Histological Techniques. 5t1i ed. Churchill Livingstone, Elsevier. Bancroft JD. (1975) Histological Techniques, 2ru1 ed. London; Butterworths. Bancroft JD, Cook HC. (1994) Manual of Histological Techniques and Their Diagnostic Applications. Churchill Livingstone, Edinburgh. Bancroft JD, Hand NM. (1987) Enzyme Histochemistry. R.M.S. Handbook No. 14. Oxford Science Publications, Oxford. Bassam BJ, Caetano-Anolles G, Gresshoff PM. (1991) Fast and sensitive silver staining of DNA in polyacrylamide gels, Anal. Biochem. 196 (1991) 80–83. Bertalanffy FD, Von Nagy KP. (1962) Fluorescence microscopy and photomicrography with acridine orange. Medical Radiography and Photography, 38: 82. Carson FL, Pickett JP. (1983) Histochemistry. In Race GJ, ed. Laboratory Medicine. Philadelphia, PA: Harper & Row. Cook HC. (1974) Manual of Histological Demonstration Techniques. Butterworths, London. Dubowitz V. (1985) Muscle Biopsy: A Practical Approach. Bailliere Tindall, London. Elias, JM. (1969) Effects of temperature, post-staining rinses and ethanol-butanol. Dehydrating mixtures in methyl green pyronin staining. Stain Technology 44:201. Filipe MI, Lake BD, eds. (1983) Histochemistry in Pathology. Churchill Livingstone, Edinburgh. Fisher D. (1968) Protein staining of ribboned epon sections for light microscopy. Histochemie 16(1), 92-96 Glenner GG, Burtner HJ, Brown GW. (1957) The histochemical demonstration of monoamine oxidase activity by tetrazolium salts. Journal of Histochemistry and Cytochemistry, 5: 591. Glenner G, Lillie RD. (1959) Observations on the diazotization-coupling reaction for the histochemical demonstration of tyrosine: metal chelation and formazan variants. Journal of Histochemistry and Cytochemistry, 7: 416. Gomori G. (1950) An improved histochemical technique for acid phosphatase. Stain Technology. 25: 81. Gomori G. (1951) Alkaline phosphatase of cell nuclei. Journal of Laboratory and Clinical Medicine. 37: 526. Gomori G. (1952) Histochemistry of esterases. International Review of Cytology. 1: 323. Goody WW, Cheng L, Lewin KJ. (1987) In situ viral DNA hybridization in diagnostic surgical pathology. Human Pathology 18: 497-1. Greer CE, Peterson SL, Kiviat NB, Manos MM. (1991) PCR amplification from paraffin-embedded tissues: Effects of fixative and fixative times. Am. J. Clin. Pathol. 95: 117-124. Holt SJ, Withers RFJ. (1952) Cytochemical localization of esterases using indoxyl derivatives. Nature, 170: 1012. Hudson P, Penshcow J et al. (1981) Hybridization histochemistry: use of recombinant DNA as a "homing probe" for tissue localization of specific mRNA populations. Endocrinology 108: 353. James J, Tas J. (1984) Histochemical protein methods. RMS Handbook D4. University Press, London: Oxford. Kiernan JA. (2008) Histological and Histochemical Methods: Theory and Practice. 4th ed. Bloxham, UK: Scion. Komminoth P, Long AA. (1993) In situ polymerase chain reaction. An overview of methods, applications and limitations of a new molecular technique. Virchows Archiv B Cell Pathology 64: 67. Lee CI, Levin A, Branton D. (1987) Copper staining: a five-minute protein stain for sodium dodecyl sulfate-polyacrylamide gels. Anal Biochem. 166(2):308-12. Levinson JJ, Retzel S, McCormick JJ. (1977) An improved acriflavine-feulgen method. Journal of Histochemistry and Cytochemistry, 25: 355. Lillie RD, Pizzolato P, Donaldson PT. (1976) Nuclear stains with soluble metachrome mordant lake dyes. The effect of chemical endgroup blocking reactions and the artificial introduction of acid groups into tissues. Histochemistry 49: 23-35. Llewellyn BD. (2009) Nuclear staining with alum-hematoxylin. Biotech. Histochem. 84: 159-177. Lojda Z, Gossrau R, Schiebler TH. (1979) Enzyme Histochemistry: A Laboratory Manual. SpringerVerlag, Heidelberg. Lowe JB. (1986) Clinical applications of gene probes in human genetic disease, malignancy, and infectious disease. Clinica Chimica Acta 157. Marshall PN, Horobin RW (1973) The mechanism of action of "mordant" des - a study using preformed metal complexes. Histochemie 35: 361-371. Mitchell BS, Dhami D, Schumacher U. (1992) In situ hybridization: a review of methodologies and applications in the biomedical sciences. Medical Laboratory Sciences 49: l07. Nuovo GJ, Gallery F, MacConnell P, Becker J, Bloch W. (1991) An improved technique for the detection of DNA by in situ hybridization after PCR amplification. Am. J. Pathol.139: 1239-1244. Nuovo GJ, Gallery F, Horn R, MacConnell P, Bloch W. (1993) Importance of different variables for optimizing in situ detection of PCR-amplified DNA. Nuovo GJ, Gallery F, MacConnell P, Braun A. (1994) In situ detection of PCR-amplified HIV-1 nucleic acids and tumor necrosis factor RNA in the central nervous system. Am. J. Pathol. 144: 659-666. Nuovo GJ. (1994) PCR in situ hybridization: Protocols and applications, 2nd ed. Raven Press, New York. Pearse AGE. (1951) Review of modem methods in histochemistry. Quarterly Journal of Microscopical Science, 92: 393. Pearse AGE. (1960) Histochemistry: Theoretical and Applied, 2nd Ed., J and A Churchill, London. Pearse AGE. (1968) Histochemistry, Theoretical and Applied. 3n1 ed., Churchill, London, vol. 1. Pearse AGE. (1972) Histochemistry, Theoretical and Applied. 3rd ed., Churchill Livingstone, Edinburgh, vol. 2. Pringle JH, Barker S, et al. (1992) Demonstration of Epstein-Barr virus in tissue sections by in situ hybridization for viral RNA. Journal of Pathology 167 (Suppl), 133A. Puchtler H, Meloan SN, Waldrop FS. (1986) Application of current chemical concepts to metalhaematein and -brazilein stains. Histochemistry 85: 353-364. Qu L, Li X, Wu G, Yang N. (2005) Efficient and sensitive method of DNA silver staining in polyacrylamide gels, Electrophoresis 26: 99–101. Sanguinetti CJ, Dias Neto E, Simpson AGD. (1994) Rapid silver staining and recovery of PCR products separated on polyacrylamide gels, BioTechniques 17: 914–921. Silverman L, Glick D. (1969) The reactivity and staining of tissue proteins with phosphotungstic acid. J Cell Biol 40(3) 761-767 Sumner AT, Sumner BEH. (1969) Laboratory Manual in Histochemistry, 1st ed., Blackwell Scientific Publications, Oxford and Edinburgh. Tokuda Y, Nakamura T, Satonaka K, et al. (1990) Fundamental study on the mechanism of DNA degradation in tissues fixed in formaldehyde. Journal of Clinical Pathology, 43: 748. Warford A, Lauder I. (1991) In situ hybridization in perspective. Journal of Clinical Pathology 44: 177. Weiss LP, Tsou KC & Seligman AM. (1954) Histochemical demonstration of protein bound amino groups. Journal of Histochemistry and Cytochemistry 2: 29. CHAPTER 21 ENZYME HISTOCHEMISTRY Enzyme histochemistry serves to detect early metabolic changes in biopsy and autopsy tissue before manifestation on H&E staining or immunohistochemistry. For critical enzyme histochemistry, it is essential not to inactivate an appreciable proportion of the enzyme to be studied, especially 'soluble' enzymes, such as alkaline phosphatase. The precision of the histochemical localization varies inversely with the length of time required in the incubation medium to achieve an appreciable response. Enzymes are tissue components that serve as catalysts for most biological reactions. They may be bound to specific cell components (such as mitochondrial enzymes) or may be free and soluble in the cytoplasm and body fluids. With few exceptions (e.g., chloroacetate esterase), frozen sections are generally required for histochemical demonstration of enzymes. Tissues frozen to -70°C or below are usually well preserved, with little loss of enzyme activity. The use of unfixed frozen sections is confined to enzymes extremely sensitive to denaturation such as the dehydrogenases. Disadvantages of unfixed frozen sections include mechanical disruption by freezing and thawing, uneven section thickness, and diffusion of soluble enzymes and co-factors leading to loss of reproducibility and false localization. Although, ideally, enzyme histochemistry should be performed on unfixed sections, so as to avoid potential artifacts inherent in chemical fixation, it is usually considered necessary to briefly fix sections in order to stop the 'soluble' enzymes from becoming lost into the incubation medium. In general, the best fixative for all enzymes is chilled acetone, which, of all fixatives, causes the least inactivation. Cytological details are not so good but they are satisfactory for most purposes if the slices are thin enough (not over 3 mm. in thickness). Acetone is especially recommended when staining for acid phosphatase. For other enzymes, cold 90-100% ethyl alcohol is preferable because it gives a better cytological fixation and the tissue is easier to handle. Most hydrolytic enzymes are reasonably resistant to formalin and can be fixed in 10 per cent formalin (preferably adjusted to pH 6-6.5 with a small amount of phosphate buffer). Methyl alcohol is entirely unsuitable as a fixative, because it destroys most enzymes. Metal precipitation is the most common technique for histochemical demonstration of enzymes, based on simultaneous capture or coupling, which involves the use of a suitable substrate and a diazonium salt. The primary reaction product ("coupler"), formed by the hydrolytic reaction between substrate and the enzyme, combines with the diazonium salt to produce a highly colored and insoluble final reaction product. The substrate must be soluble in water and in the buffer medium used, to allow maximum hydrolysis by the enzyme. Another technique uses soluble substrates which undergo molecular rearrangement to give a colored insoluble reaction product after enzyme hydrolysis. Enzymes for which histochemical techniques are known belong in one of the two groups: (1) Oxidative enzymes (2) Hydrolytic enzymes OXIDATIVE ENZYMES Oxidative enzymes (i.e. tyrosinase, peroxidase, monoamine oxidase, cytochrome oxidase) catalyze the reaction between substrate and atmospheric oxygen. They can be demonstrated by simultaneous coupling method, which involves oxidation of the substrate and subsequent reduction of a tetrazolium salt, resulting in the formation of a relatively insoluble formazan deposit at the site of enzyme activity. The two tetrazolium salts commonly used as hydrogen acceptors are monotetrazolium (MTT) which forms a lipid-soluble finely granular formazan, and ditetrazolium chloride-nitro (NBT) that forms a lipidinsoluble, highly colored formazan deposit on the site of enzyme activity. The oxidative enzymes fall into three groups: (a) Dehydrogenases, (b) oxidases, and (c) peroxidases a) Dehydrogenases The dehydrogenases catalyze the transfer of hydrogen to immediate acceptors other than oxygen and peroxides, although the ultimate acceptor may be oxygen. They require coenzymes, and some of them are also linked to the diaphorase or cytochrome systems. Dehydrogenases are enzymes that remove hydrogen from the substrate and transfer it along a hydrogen acceptor (oxidative) pathway. The released hydrogen is accepted by the coenzymes NAD or NADP, or the dehydrogenase enzyme itself can act as an acceptor, in which case no coenzyme is required. They can be demonstrated by the transferring the released hydrogen ions into tetrazolium salt to produce formazan deposits. They are rather delicate enzymes which are largely destroyed by any sort of fixation and completely destroyed by embedding. They are rapidly inactivated even on standing. NADH diaphorase demonstrates mitochondria and the fine detail of the sarcoplasmic reticulum of the fiber. It is used to detect very minor or early structural abnormality in the sarcoplasmic reticulum network of the fiber, as well as mitochondrial abnormalities. The principle of their demonstration is the observation of the change in color of suitable hydrogen acceptors when they are reduced by the enzyme. The three main types of compounds used are: (1) Methylene blue - is reduced to colorless leuco-methylene blue and thus indicating the sites of activity by bleaching. The methylene blue technique is not recommended because the negative image does not permit good localization of the enzyme, and the method is cumbersome. (2) Tetrazolium method - where the substrates are reduced to bright red, purplish, or blue formazans, which are insoluble in water and soluble in fats. The tetrazolium method is the most sensitive and results in excellent localization of the enzyme, except for an occasional secondary staining of fat droplets by formazan. The formation of dye should be quite noticeable after about 5-10 minutes of incubation if good active material is used. (3) Tellurite - reduced to insoluble black elementary tellurium. The tellurite method is considerably less sensitive, but it gives nice, sharp pictures. Even without the use of any substrate, positive reactions will be obtained in most cases on account of the presence of various endogenous substrates in the tissues, which can be avoided by rinsing the sections before incubation. The optimum pH for the enzymatic activity is pH 7.3-7.6. The tissue need not be absolutely fresh; refrigeration for 4 hours at 4°C does not cause any noticeable loss of activity. Fixation in chilled acetone for 4 hours causes only 40 percent inactivation of the enzyme. Use frozen sections 25-50 µ thick because thinner sections often fail to stain. Incubation time at 37°C. Range from 20 minutes to 3 hours. Elementary tellurium is black or brown-black. The sections can be counterstained with hematoxylin or carmine; they should be mounted in glycerol or glycerol-jelly. b) Oxidases Oxidases are a group of enzymes having in common the property of catalyzing the oxidation of various substrates, mainly phenols and amines, in the presence of atmospheric oxygen. Substrate specificity is usually only relative since the same enzyme can attack a number of substrates (although while the same substrate may be attacked by a number of different enzymes. Polyphenol oxidases (PPOs) are enzymes belonging to a group of coppercontaining metalloproteins. They are members of the oxido-reductases that catalyze the oxidation of a wide range of phenolic compounds by utilizing molecular oxygen. The ability of polyphenol oxidases to act on phenolic compounds makes them highly useful biocatalysts for various biotechnological applications. Indophenol oxidase (Cytochrome oxidase) Indophenol Oxidase (Cytochrome Oxidase) is a copper-yielding cytochrome complex that catalyzes the oxidation of ferrocytochrome c to produce ferricytochrome c and 2H2O. It forms part of Complex IV of the respiratory chain. A deficiency of one or more of the polypeptides of this complex results in neuronal loss in the brain leading to psychomotor retardation and neurodegenerative disease. To stain for cytochrome oxidase, a mixture of solutions of a phenol or naphthol and an aromatic diamine is slowly oxidized on exposure to air, with the formation of intensely colored (usually blue) indophenol dyes, most of which are insoluble in water but very soluble in oils and fats. The reaction is immediate in the presence of strong oxidants, such as dichromate or hypochlorite. Cytochrome oxidase is a sensitive enzyme that is readily destroyed by drying and by fixation with formalin. Tyrosinases Tyrosinases are copper containing monooxygenases that catalyze the production of melanin and other pigments from tyrosine by oxidation. If uncontrolled, increased tyrosinase activity may result in increased melanin synthesis thereby causing melanoma. Decreasing tyrosinase activity has been targeted to prevent conditions related to the hyperpigmentation of the skin. Tyrosinase deficiency is associated with various forms of albinism. Ltyrosinase is the initial substrate for melanin biosynthesis and its conversion to dopaquinone is catalyzed by tyrosinase, whose expression is reported in melanocytes and melanomas. The loss of activity with heat and marked reduction of activity in slightly acid solution are properties common to all known tyrosinases. An improved histochemical method for demonstrating tyrosinase activity has been described which utilizes small amounts of dopa to shorten the induction period for the enzymatic oxidation of tyrosine. This method is a rapid, reproducible and specific way to localize tyrosinase in tissue section. The histochemical tyrosine-dopa method for tyrosinase has greater specificity than the dopa oxidase method; it is more rapid, more reproducible and more sensitive than the method using tyrosine alone as substrate; it is simpler, more direct and more rapid than the auto-radiographic-histochemical method. Dopa oxidase Melanin pigment is formed from the amino acid, dihydroxy-phenylalanine (DOPA), by the action of a specific oxidative enzyme (dopa oxidase) that is responsible for the oxidation of l-tyrosine to dopa and dopa quinone. L-DOPA is produced from the amino acid L-tyrosine by the enzyme tyrosine hydroxylase and is the precursor to the neurotransmitters dopamine, norepinephrine (noradrenaline), and epinephrine (adrenaline) collectively known as catecholamines. A specific dopa oxidase, which does not act on any substrate except dopa, is easily inactivated by chemical and physical agents, and is present only in cells concerned with the elaboration of melanin (chromatophores). To demonstrate dopa oxidase, use frozen sections of fresh material or of tissue fixed for only a few hours in 5 per cent formalin. Longer fixation may cause partial inactivation of the enzyme. The sections are rinsed very briefly in distilled water and transferred a 0.1 per cent solution of dihydroxyphenylalanine, buffered with a phosphate buffer to pH 7.3-7.5, in an open dish for 4-5 hours. Temperature should be between 20° and 37°C. It is advisable to change the incubating solution once or twice to avoid the deposition of a melanin precipitate (by spontaneous oxidation of the substrate). At pH 7.7 the reaction is much faster (about 1 hour), but the danger of precipitates is also increased. Rinse sections, counterstain as desired, dehydrate, and mount. The sites of dopa oxidase activity will appear dark brown-gray or brown-black. For greater contrast, melanin formed during the reaction can be blackened by silver c) Peroxidases Peroxidases are heme-containing enzymes that use hydrogen peroxide as the electron acceptor to catalyze a number of oxidative reactions. Enzymes of the peroxidase group catalyze the reduction or transfer of oxygen from hydrogen peroxide and other peroxides to a variety of substrates. This biochemical function confers them a role in many different and important biological processes including defense mechanisms and immune response. Chemically, most if not all of the peroxidases appear to be heme proteins. They are quite resistant to various chemical and physical agents, especially to acids and heat. For the histochemical demonstration of peroxidase, benzidine, naphthol, and various leuco-dyes are utilized in the presence of hydrogen peroxide. Benzidine is oxidized to a blue or brown dye; naphthol to a purple-black one, while leuco-dyes are re-colorized to their original shades. It is important to run controls without peroxide because positive reactions may be obtained even in its absence Myeloperoxidase is a peroxidase enzyme that is most abundantly expressed in neutrophil granulocytes (a subtype of white blood cells). It is a lysosomal protein stored in azurophilic granules of the neutrophil and released into the extracellular space during degranulation. It has a heme pigment, which causes its green color in secretions rich in neutrophils, such as pus and some forms of mucus. It also oxidizes tyrosine to tyrosyl radical using hydrogen peroxide as an oxidizing agent. As a hemoprotein, hemoglobin can, in the presence of hydrogen peroxide, also act as a peroxidase. The peroxidase properties of hemoglobin, when it reacts with physiologic oxidants such as hydrogen peroxide, have been advocated to propagate oxidative cell and tissue damage. Horse radish peroxidase is, a heme-containing enzyme that utilizes hydrogen peroxide to oxidize a wide variety of organic and inorganic compounds; it is commercial used as a component of clinical diagnostic kits and for immunoassays. Peroxidase stain is a method for demonstrating peroxidase granules in some neutrophils and in eosinophils where the enzyme promotes the oxidation of benzidine by hydrogen peroxide. In the benzidine reaction the optimal concentration of hydrogen peroxide is about 0.01 M in the case of myeloid granules and much higher, about 0.1 M, in the case of hemoglobin. The activity of myeloid granules is rapidly destroyed by heating to 75°-80°C or by extraction with a warm chloroform-methyl alcohol mixture. The activity of hemoglobin is entirely resistant to these influences. Smears are fixed with acetone, alcohol, or formalin-alcohol (1:10). For tissues the same fixatives or formalin-saline are recommended. It is important that the fixative should not hemolyze the red cells, thereby causing a diffusion of the reaction for hemoglobin. Frozen sections, are the best, although in most cases excellent results are obtained after celloidin- or paraffin-embedding. HYDROLYTIC ENZYMES Hydrolytic enzymes are complex catalytic proteins that use water to break down protein, carbohydrate, nucleic acids, starch, fats, phosphate esters and other molecules into their simplest units. Most of the hydrolytic enzymes demonstrable histochemically belong to the group of esterase; that is, they hydrolyze esteric linkages. Depending on the substrate, hydrolysis yields an acid ion and an alcohol or a phenol (or, in the case of phosphamidase, an acid and an amide). Reactions have been devised for the demonstration of either the acid or the alcoholic moiety. The acids are demonstrated by their regular precipitation reactions with metal ions, most often calcium, lead; cobalt, iron, and copper. The precipitate formed is usually colorless and not easily seen under the microscope. Therefore, it must be transformed into a colored, easily observable compound. In the case of the heavier metals the sections can be treated directly with a suitable reagent. Soluble sulfides, for example, will transform precipitates of lead, cobalt, iron and copper into blackish, exceedingly insoluble sulfides. The alcoholic (or phenolic) moiety can be demonstrated only if it is a thioalcohol or a naphthol. Some thio-alcohols form highly insoluble precipitates with heavy metals; naphthols can be visualized as azo dyes. Under suitable conditions, diazonium salts will couple with aromatic amines and hydroxy compounds (and, in addition, with a number of heterocyclic compounds) to form brightly colored, very insoluble azo dyes. Hydroxides (phenols and naphthols) couple optimally at an alkaline reaction (pH 8 and up), whereas amines couple at an acid reaction (pH 3-5). Phosphatases Phosphatases are enzymes capable of hydrolyzing organic phosphate esters. Alkaline phosphatases exhibit maximum activity at a higher pH (9.0) while acid phosphatases exhibit peak activity at a lower pH (around 5.0). Of the large variety of phosphatases, histochemical methods are available for nonspecific alkaline phosphatase, for 5- nucleotidase, acid phosphatase, and phosphamidase. Some of the phosphatases (hexosediphosphatase, and adenosine triphosphatase of muscle) are so sensitive that they will not tolerate fixation and/or embedding. All fixatives cause considerable inactivation of both alkaline and acid phosphatase. Good results may be obtained with refrigerated tissue fixed as late as 48 hours after removal, although there may be some blurring of the picture, owing to diffusion of the enzyme. Alkaline Phosphatases Phosphatases with a pH optimum around 9 occur in most organs. The largest group, the nonspecific enzyme(s), will hydrolyze any monoester of phosphoric acid and, in addition, nucleic acids. As a rule, aromatic esters are hydrolyzed optimally at a higher pH (9.7-10) than aliphatic ones (pH 8.1- 9). All enzymes of the group are activated by Mg. Frozen sections show a higher activity than embedded tissues. However, there is a danger of loss of enzyme by diffusion, since fixation in acetone or alcohol will not render the enzyme completely and irreversibly insoluble. Alkaline phosphatase is not too sensitive to minor variations in temperature; incubation at any temperature between 30° and 45°C will do. The cheapest and easiest available substrate is glycerophosphate, any commercial brand of which can be used; the recommended concentration is 0.01-0.03 M. The histochemical technique used for demonstrating the enzyme, alkaline phosphatase, blackens the cells and tissue containing the enzyme. In general, the degree of blackness is correlated with the quantity of enzyme present. Exact localization is complicated by the fact that the enzyme may shift its intracellular position during the histological procedure. Sections are incubated in a solution consisting of sodium glycerophosphate and calcium nitrate. Through the action of the phosphatase, calcium phosphate is precipitated in those regions where the enzyme is present. For visualization in sections, the calcium phosphate is converted into cobalt phosphate and finally into cobalt sulfide, which is black. The calcium phosphate method is based on the principle that, if sections are incubated with glycerophosphate at an alkaline reaction in the presence of Ca++ ions, the phosphate ions liberated will be precipitated at the site of formation as insoluble Ca phosphate. The latter is then transformed, in a second step, into metallic silver or black cobalt sulfide. The pH of the solution should be between 9 and 9.8. Below pH 9 the intensity of the reaction rapidly declines. Only sites of highest activities will be stained after short periods, of incubation (up to 2 hours), and on greatly prolonged incubation diffusion artifacts may become very disturbing. Borax is better avoided because it inhibits the hydrolysis of glycerophosphate and of certain other substrates and because of its incompatibility with higher concentrations of Ca++. The concentration of the buffer should be 0.05-0.1 M. Gomori calcium method for alkaline phosphatase (Bancroft 2008) This technique is used to demonstrate the enzyme, alkaline phosphatase. It blackens the cells and tissue containing the enzyme. In general, the degree of blackness is correlated with the quantity of enzyme present. Exact localization is complicated by the fact that the enzyme may shift its intracellular position during the histological procedure. Sections are incubated in a solution consisting of sodium glycerophosphate and calcium nitrate. Through the action of the phosphatase, calcium phosphate is precipitated in those regions where the enzyme is present. For visualization in sections, the calcium phosphate is converted into cobalt phosphate and finally into cobalt sulfide, which is black. The technique involves simultaneous coupling reaction with sodium Bglycerophosphate as the substrate that is hydrolyzed by the enzyme to produce phosphate ions. This primary reaction product (phosphate) reacts with calcium ions to form calcium phosphate, which is then treated with cobalt nitrate to produce cobalt phosphate, which becomes visible as a black precipitate when treated with dilute ammonium sulfide. Fixation: Formol calcium at 4°C Sections: Prefixed cryostat sections preferred Solutions: Incubating medium 2% sodium B-glycerophosphate 2.5 ml 2% sodium veronal 2.5 ml 2% calcium nitrate 5.0 ml 1% magnesium chloride 0.25 ml Distilled water 1.25 ml The final pH of the incubating medium should be between 9.0 and 9.4. The sodium veronal acts as the buffer vehicle, while magnesium chloride acts as an enzyme activator. Method: 1. After suitable fixation, bring sections to water. 2. Place in incubating medium at 37°C for 25 minutes to 6 hours, depending on type of section. (Cryostat sections require the shortest time.) 3. Wash well in distilled water. 4. Treat sections with 2% cobalt nitrate for 3 minutes. 5. Wash well twice in distilled water. 6. Immerse sections in 1% ammonium sulfide for 2 minutes. 7. Wash well in distilled water. 8. Counterstain in 2% methyl green (chloroform extracted). 9. Wash well in running tap water. 10. Mount in glycerin jelly. Results: Alkaline phosphatase activity brownish-black Nuclei green Acid Phosphatase Acid phosphatase reaction: This histochemical technique is used to recognize lysosomes due to their acid phosphatase content. Sections are incubated in a solution containing a lead phosphate. The phosphate is released by enzymatic activity of acid phosphatase (lysosomal enzyme) and is precipitated as lead phosphate, and is then converted to lead sulfide, a black deposit. Acid phosphatase stain is used to o identify macrophages in necrotic fibers and abnormal lysosomal activity in muscle fibers. Acid phosphatases, as a rule, are not activated by Mg and almost invariably are greatly inhibited by fluoride. The original histochemical method for acid phosphatase utilizes the hydrolysis, of glycerophosphate at pH 5 in the presence of Pb++ ions. Fixation in cold acetone and embedding in paraffin are recommended. Gomori Lead method for acid phosphatase (Bancroft 2008) This technique is used to demonstrate lysosomes due to their acid phosphatase content. Sections are incubated in a solution containing a lead phosphate. The phosphate is released by enzymatic activity of acid phosphatase (lysosomal enzyme) and is precipitated as lead phosphate, and is then converted to lead sulfide a black deposit. In this metal precipitation technique, sodium B-glycerophosphate is used as the substrate in a buffer medium at pH 5.0 to form phosphate ions as the primary reaction product, which is then treated with lead ions to form lead phosphate as final reaction product. Treatment with ammonium sulfide allows the precipitate of lead sulfide to be demonstrated and seen at the site of enzyme activity. Fixation: Formol calcium at 4°C Sections: Prefixed cryostat sections preferred Solutions: Incubating Medium: 0.05 M acetate buffer pH 5.0 10 ml. Sodium B-glycerophosphate 32 mg. Lead nitrate 20 mg. The lead nitrate must be dissolved in the buffer before sodium Bglycerophosphate is added. The pH of the incubating medium should be approximately 5.0. Method: 1. After suitable fixation, bring sections to water. 2. Place sections in incubating medium at 37°C for 30 minutes to 2 hours. 3. Wash in distilled water. 4. Immerse in 1% ammonium sulfide (fresh) for 2 minutes. 5. Wash well in distilled water. 6. Counterstain in 2% methyl green. 7. Wash in tap water. Results: Acid phosphatase activity black Nuclei green Technical Considerations: Fixation of thin blocks in cold acetone, rapid embedding at a temperature not exceeding 56° C, and the use of recently cut sections and of the correct substrate mixture will produce good results in a vast majority of instances; however, occasional unexplainable failures cannot be eliminated completely. Toluene or xylene should not be used; they will cause some fading of the stain. Above pH 6, the activity of alkaline phosphatase rapidly increases, and one may obtain combination pictures of the distributions of acid and alkaline phosphatase. The choice of substrates is rather limited because the lead salts of most phosphoric esters are very insoluble at pH 5 or higher. 5-Nucleotidase The substrates of the enzyme are 5-nucleotides (muscle adenylic acid, inosinic acid and, possibly, adenosine triphosphoric acid). The pH optimum is around 7.8, but the enzyme is quite active even at pH 9. The histochemical method for 5-nucleotidase is very similar to the method for alkaline phosphatase; in fact, it may be identical except for the substrate. At this pH +/- 8.3, the 5nucleotidase is fully active, while the activity of alkaline phosphatase is only about one-third of the maximum. A slight disadvantage of this low pH is a tendency toward diffusion artifacts. It can be offset almost completely by a sufficiently high concentration of Ca ions. While nonspecific alkaline phosphatase will attack both glycerophosphate and the two nucleotides, 5nucleotidase cannot hydrolyze substrates other than 5-nucleotide. Lead method for 5-nucleotidase (Wachstein & Meisel 1957) In this metal precipitation technique, the substrate adenosine-5-phosphate is hydrolyzed by the enzyme to phosphate ions in the presence of magnesium which serves as an activator. The primary reaction product (phosphate) is precipitated by lead ions to produce lead phosphate, which is then converted to brown lead sulfide precipitate following treatment with ammonium sulfide. Fixation: Unfixed preferred, or formol calcium at 4°C Sections: Cryostat, free floating Incubating Medium: 1.25% adenosine-5-phosphate 4 ml 0.2M Tris buffer, pH 7.2 4 ml 2% lead nitrate 0.6 ml 0.1 M magnesium sulfate 1 ml Distilled water 0.5 ml Method: 1. Place in incubating medium at 37°C for 30 minutes to 1 hour. 2. Fix in formol saline if unfixed sections are used. 3. Transfer sections with glass rod to distilled water. 4. Repeat wash in fresh distilled water. 5. Treat with 1% ammonium sulfide for 3 minutes. 6. Wash well in distilled water. 7. Repeat wash. 8. Mount on microscope slides and allow to partially dry. 9. Mount in glycerin jelly. Result: 5-nucleotidase blackish-brown deposits. Note: Free floating cryostat sections of unfixed materials are recommended because of considerable loss of enzyme activity when prefixed sections are used. Adenosine Triphosphatase (ATPase) (Dubowitz 1985; Carson 1983) ATPase methods are used in combination to distinguish between Type 1 and Type 2 fibers, and to further subdivide the Type 2 fibers into 2A, 2B and 2C subtypes. This distinction is diagnostically important since some muscle diseases have characteristic patterns of loss, atrophy or grouping of specific fiber types or subtypes. Some types of structural fiber abnormality (e.g., periodic paralysis) are also demonstrated by the ATPase methods. The technique for demonstrating ATPase involves metal precipitation, using the adenosine triphosphate as substrate to form phosphate as primary reaction product. The phosphate ion is then precipitated either by lead to form lead phosphate, which is converted to dark brownish-black precipitate after treatment with ammonium sulfide. An alternative way of precipitating phosphate is by calcium-cobalt method (as with alkaline phosphatase) whereby calcium is added to form calcium phosphate, which is then treated with cobalt nitrate to produce a precipitate of cobalt phosphate. For skeletal muscle biopsies, the substrate is incubated at different pH levels (pH 9.4 using 0.1 M glycine buffer, or pH 4.2 and pH 4.6 using 0.1M veronal-acetate to distinguish between type 1, and types 2A, 2B and 2C fibers.) Nonspecific esterase: Nonspecific esterase stain is used to identify cell types containing esterases that have a characteristic ability to split esters under particular conditions. Increased staining is seen in sites of lysosomal and macrophage activity. In one staining method, α-naphthyl acetate is enzymatically hydrolyzed, liberating a free naphthol compound. This then couples with a diazonium compound, forming dark brown-red or black colored deposits at sites of non-specific esterase activity. This enzyme is detected primarily in monocytes, macrophages and histiocytes, and is normally absent in granulocytes. Neuromuscular and myotendinous junction are also positive for esterase: α- Napththyl acetate method for nonspecific esterase (Bancroft 2008) This method uses α-naphthyl acetate as a substrate that releases α-naphthol during enzyme hydrolysis. The α-naphthol is then coupled with a suitable diazonium salt (fast blue B or pararosanilin-HCl) to produce an insoluble dye at the site of enzyme activity. Fixation: Formal calcium at 4°C Sections: Prefixed cryostat preferred. Solutions: a. Substrate solution α- naphthyl acetate 50 mg Acetone 5 ml b. Buffer solution Disodium hydrogen phosphate 2.83 gm Distilled water 100 ml c. Sodium nitrite solution Sodium nitrite 400 mg Distilled water 10 ml d. Pararosanilin-HCl stock solution Pararosanilin hydrochloride 2 gm 2 M hydrochloric acid 50 ml Heat gently, cool to room temperature and filter e. Distilled water Incubating medium: Solution a 0.25 ml Solution b 7.25 ml Solution c 0.4 ml Solution d 0.4 ml Solution e 2.5 ml Equal parts of solutions (c) and (d) should be mixed together before adding to the incubation medium. Adjust pH to 7.4 with additional solution (b) if necessary. Method: 1. After suitable fixation, bring sections to water. 2. Incubate sections in incubating medium at 37°C for 2 to 20 minutes. 3. Wash in running water. 4. Counterstain in 2% methyl green (chloroform extracted). 5. Wash well in tap water. 6. Dehydrate rapidly through fresh alcohol to xylene and mount in DPX. Results: Esterase reddish brown Nuclei green lndoxyl acetate method for nonspecific esterase (Holt 1958; Bancroft 2008) This technique uses bromo-indoxyl acetate as the substrate to produce bromoindoxyl which is then oxidized to an insoluble azo dye. Fixation: Formol calcium at 4°C Sections: Prefixed cryostat preferred Incubating Medium: 5 bromo-4-chloro-indoxyl acetate 1 mg Ethanol 0.1 ml Tris buffer (0.2M), pH 7.2 2 ml Potassium ferricyanide 17 mg Potassium ferrocyanide 21 mg Calcium chloride 11 mg Distilled water 7.9 ml The 5-bromo-4-chloro-indoxyl acetate is dissolved in ethanol and the buffer is then added. The remaining chemicals are dissolved in the distilled water and the solution is mixed. The final solution must be freshly prepared just prior to use. Method: 1. Bring prefixed cryostat sections to water. 2. Incubate sections in incubating medium at 37°C for 15 to 60 minutes. 3. Rinse in tap water. 4. Counterstain in Mayer's carmalum for 5 minutes. 5. Rinse in tap water. 6. Mount in glycerin jelly or dehydrate, clear in xylene and mount in DPX. Results: Esterase activity blue Nuclei red Chloroacetate esterase Also called specific esterase, naphtol AS-D chloroacetate esterase is a useful stain that facilitates the identification of neutrophil polymorphs in both frozen and paraffin sections. Chloroacetate is enzymatically hydrolyzed by "specific esterase," liberating a free naphthol compound. This then couples with a diazonium compound, forming highly colored deposits at sites of enzyme activity. This enzyme is usually considered specific for cells of granulocytic lineage and may be used to detect neutrophils in peripheral blood, bone marrow or tissue sections which have been paraffin embedded. Chloroacetate Esterase (Leder 1979; Carson 1983) Sections: Frozen or 4µm paraffin sections to demonstrate mast cells and cells of granulocytic lineage. Formula: Veronal Acetate Stock Solution. Na acetate (trihydrate) 1.94 g or (anhydrous) 1.2 g Na di-ethyl barbiturate (sodium barbitone) 2.9 g Distilled water 100 ml Veronal Buffer pH 9.1 Veronal acetate stock soln. 50.0 ml Distilled water 197.5 ml 0.1N HCl (COSHH C H I) 2.5 ml To prepare 4% Pararosaniline (Basic Fuchsin) stock Pararosanilin 2 g Distilled water 40 ml. Heat until almost boiling, cool to room temperature. Then Add 2 N HCl 10 ml. Filter into bottle. Pararosanilin (Basic Fuchsin) Solution Equal amounts of A and B (i.e. 4 drops of each using a 1 ml disposable pipette). (A) 4% Pararosanilin in 20% HCl (B) 4% Na nitrite (0.04 g/ml) Method 1. Fix cryostat section in buffered formalin or take paraffin sections to water. 2. In a 50 ml beaker take 4 drops 4% Pararosanilin hydrochloride solution, add 4 drops freshly prepared 4% Na nitrite solution, and mix for 1 min. The mixture should turn straw colored. 3. Add 20 ml Veronal acetate buffer solution pH 9.1 adjust to pH 6.3 using N HCl. 4. Weigh out 0.01g Naphthol AS-D chloroacetate and dissolve in 0.5 ml Dimethyl formamide. 5. Add this solution to the Pararosanilin/Buffer mixture, the resulting solution should turn flocculent pale pink in color. 6. Filter onto slides and leave 20-30 min at room temperature. 7. Wash in water. 8. Lightly counterstain with Hematoxylin. 9. Wash in water, do not differentiate, blue in Scott’s tap water. 10. Dehydrate clear and mount in Permount. 1. 2. 3. 4. 5. One change of 70% ethanol – 10 Dips Two changes of 95% ethanol – 10 Dips each Two changes of 100% ethanol – 10 Dips each Three changes of Xylene – 10 Dips each Coverslip with Permount Fig. 21 -3. Chloroacetate Esterase stain in bone marrow biopsy Results Chloroacetate esterase activity reddish brown Nuclei blue Precaution: Basic Fuchsin (Pararosanilin) (as dry powder) is a toxic carcinogen. Wear face mask when weighing out dye and make up solutions in fume cupboard. After any powder is weighed out, it must be put into the solute straight away and work bench must be wiped clean. Acetylcholinesterase Acetylcholinesterase is an enzyme present in nervous tissue, muscle, and red blood cells that catalyzes the hydrolysis of acetylcholine to choline and acetic acid. It is found at mainly neuromuscular junctions and cholinergic brain synapses, where it terminates synaptic transmission. During neurotransmission, acetylcholine is released from the nerve into the synaptic cleft and binds to acetylcholine receptors on the post-synaptic membrane, relaying the signal from the nerve. Acetylcholinesterase, also located on the post-synaptic membrane, terminates the signal transmission by hydrolyzing acetylcholine. The presence of acetylcholinesterase (AChE) activity in amniotic fluid is associated with open neural tube defects. Increased acetylcholinesterase expression is also associated with congenital absence of colonic ganglion cells and is a basis for the diagnosis of Hirschsprung’s disease. Acetycholinesterase Stain (Lowe 1995) Sections: Unfixed cryostat or cold Formol calcium/gum sucrose fixed sections. Solutions: Incubating solution. Acetyl thiocholine iodide 5mg 0.1M acetate buffer (pH.6.0) 6.5ml 0.1m sodium citrate (2.94g/100ml) 0.5ml 30mM copper sulphate (0.58g/100ml) 1.0ml Distilled water 1.0ml 5mM potassium ferricyanide (0.165g/100ml) 1.0ml Add in order, mixing well at each stage Method: 1. Incubate in solution a. at 37ƒC for 15-120 minutes. 2. Rinse in distilled water. 3. Counterstain in Hematoxylin. 4. Dehydrate, clear. Mount sections in DPX Results: Cholinesterase activity Red/brown. Fig. 21 -4. Intestinal biopsy showing acetylcholinesterase staining of ganglion cells Notes: 1. Care should be taken when using cholinesterase inhibitors as they are extremely toxic. 2. Unfixed cryostat sections of rectal biopsy take one hour. 3. Unfixed cryostat sections of muscle biopsy take one and half to two hours. 4. RBC membranes contain acetylcholinesterase and may simulate nerve fibers 5. Areas with strong acetylcholinesterase activity are resistant to dehydration. Tetrazolium method for Monoamine Oxidase (Glenner 1957) This enzyme is involved in the breakdown of adrenaline and 5 hydroxytryptamine. It is demonstrated by the oxidation of tetra nitro- blue tetrazolium (TNBT). Sections: Unfixed cryostat Incubating Medium: Tryptamine hydrochloride 25 mg. Sodium sulfate 4 mg. Tetra nitro-blue tetrazolium (TNBT) 5 mg. 0.1 M phosphate buffer, pH 7.6 5 ml. 0.2 Distilled water 15 ml. Method: 1. Place sections in incubating medium at 37°C for 45 minutes. 2. Wash in running tap water for 2 minutes. 3. Place sections in 10% formol-saline for 30 minutes. 4. Wash well in tap water for 2 minutes. 5. Mount in glycerin jelly. Results: Monoamine oxidase activity bluish black Phosphorylase Phosphorylase is an enzyme that, in the presence of inorganic phosphate, catalyzes the conversion of glycogen into glucose-1-phosphate. Phosphorylases catalyze the breakdown of glycogen in liver and muscle. The phosphorylase of skeletal muscle occurs in two forms, the active form (phosphorylase-a) and a much less active form (phosphorylase-b). Phosphorylase kinase is an enzyme that uses ATP to phosphorylate phosphorylase b and thus reform phosphorylase a, the active form of phosphorylase. Phosphorylase-b kinase activity, as present in resting muscle in the non-activated form, appears to be ample to account for the fast appearance of phosphorylase-a observed with muscle contraction Phosphorylase also distinguishes between type 1 and 2 fibers of skeletal muscle but fades very quickly. It is used to exclude McArdle’s disease, a primary phosphorylase deficiency. Muscle biopsies of McArdle's patients are characterized by subsarcolemmal storage of normal glycogen and by absent stain with the histochemical phosphorylase reaction. In some patients, however, it is possible to find scattered fibers with positive phosphorylase staining. The underlying principle is that phosphorylase catalyzes the breakdown of glucose-1phosphate to glucose and phosphate ions. The glucose is subsequently stained with iodine to give a purple color. Phosphorylase Stain (Meijer 1968) Sections: Unfixed cryostat Incubating Solution (add the reagents in the following order) 0.1 M acetate buffer, pH 5.9 100 ml 0.1 M magnesium chloride 10 ml Glucose-1-phosphate 1 gm Glycogen (oyster/rabbit liver) 20 mg. ATP salt 50 mg Sodium fluoride 1.8 gm Ethanol 20 ml Polyvinyl pyrrolidine 9 gm Store at -20oC. Method: 1. Incubate in solution at 37oC for 90 minutes. 2. Wash in 40% ethanol for 5 seconds; air dry. 3. Fix in ethanol for 3 minutes; air dry. 4. Wash in 1:30 Lugol’s iodine for 5 minutes. 5. Mount in 9:1 glycerine jelly/Lugol’s iodine. Results: Phosphorylase activity blue/black Notes: The solution is kept in a closed Columbia jar and is frozen after each incubation. Replace when its potency is diminished. Aldolase Demonstration of aldolase is based on the fact that the enzyme splits hexose diphosphate into two molecules of triose phosphate. The latter hydrolyzes spontaneously at an alkaline reaction, and the phosphate liberated is visualized much as in the regular method for alkaline phosphatase. lodoacetate and fluoride are added to the incubating mixture to prevent the dismutation of triose phosphate and the hydrolysis of hexose diphosphate by alkaline phosphatase, respectively. Frozen sections must be used, because paraffin sections give no reaction. Sulfatase Sulfatases hydrolyzing sulfates of phenols and of thioglucosides are quite resistant to dehydration by acetone. The concentration of enzyme is very low (maximum, 50-60 ^M of substrate hydrolyzed per gram of tissue and per hour; in most cases activity is very much lower, usually around 1 per cent of the phosphatase activity). The method demonstrates the sulfate ion by precipitating it with benzidine; the latter is then demonstrated with y8-naphthoquinone sulfonate. These methods seem to work with acetone-fixed, unembedded tissue only. Incubation of fresh tissue in the presence of 6-bromo-2-naphthylsulphate for 3 hours gives a very pale blue particulate localization of the stain for aryl sulfatase. REFERENCES Andrea M, Giuliana S, Annachiara N, Marina F. (1999) McArdle’s Disease: The Unsolved Mystery of the Reappearing Enzyme. Am J Pathol. 154(6): 1893–1897. Bancroft JD. (1960) Theory and practice of histological techniques. 6th edition. London, Churchill. Bancroft JD, Gamble M. (2008) Theory and Practice of Histological Techniques. Elsevier Health Sciences, 409-410. Beckstead JH, Bainton DF. (1980) Enzyme histochemistry on bone marrow biopsies: Reactions useful in the differential diagnosis of leukemia and lymphoma applied to 2-micron plastic sections. Blood 55:386, 1980 Bitensky L, Cohen S. (1965) The histochemical demonstration of alkaline phosphatase in unfixed frozen sections. [Quart. J. Micr. Sci., 106(2), .193-196. Carson FL, Pickett JP. (1983) Histochemistry. In: Race GJ, ed. Laboratory Medicine. Philadelphia PA: Harper & Row. Chilosi M, Pizzolo G, Menestrina F, Iannucci AM, Bonetti F, Fiore-Donati L. (1981) Enzyme histochemistry on normal and pathologic paraffin-embedded lymphoid tissue Am J Clin Pathol 76(6):729-36. Chilosi M, Menestrina F, Pizzolo G, Maconi A, Iannucci A, Bonetti F, Fiore-Donati L. (1981) Fluoride resistant alpha-naphthyl acetate esterase and combined enzyme histochemistry in the study of normal and pathologic lymphoid tissues. Basic Appl Histochem. 25(1):39-50. Davis BJ, Ornstein L. (1959) High resolution enzyme localization with a new diazo reagent, hexazonium pararosaniline. J. Histochem. Cytochem. 7,297. Dubowitz V. (1985) Muscle Biopsy. A Practical Approach, 2nd ed. Philadelphia, PA: Bailliere Tindall. Glenner GG, Burtner HJ, Brown GW. (1957) The histochemical demonstration of monoamine oxidase activity by tetrazolium salts. J. Histochem. Cytochem. 5, 591–600. Gomori G. (1952) Acid Phosphatase. In Microscopic Histochemistry. p189. University of Chicago Press. Grogg E, Pearse AGE. (1952) A critical study of the histochemical techniques for acid phosphatase with a description of an azo dye method. J. Path. Bact. 64, 627. Hardonk MJ, Koudstaal J. (1976) Enzyme histochemistry as a link between biochemistry and morphology. Prog Histochem Cytochem. Holt SJ. (1958) Indigogenic staining methods for esterases. In General Cytochemical Methods, vol. I, pp. 375-398. Ed. by J. F. Danielli. New York: Academic Press Inc. Holt SJ. (1963) Some observations on the occurrence and nature of esterases in lysosomes. In The Lysosornes Ed. by A. V. S. de Reuck and M. P. Cameron. P. I 14. London: J. and A. Churchill Ltd. Hoshino M, Kobayashi H. (1971) The use of glycol methacrylate as an embedding medium for the histochemical demonstration of acid phosphatase activity. J Histochem Cytochem 19:575. Kass L. (1977) Esterase reactions in acute myelomonocytic leukemia. Am J Clin Pathol 67:485. Kugler P. (1988) Quantitative enzyme histochemistry in the brain. Histochemistry 90(2), 99-107. Lauren J, Sweeney PD. (2004) An introductory biology lab that uses enzyme histochemistry to teach students about skeletal muscle. Advan in Physiol Edu 28:23-28. Leder LD. (1979): The chloroacetate esterase reaction. A useful means of histological diagnosis of hematological disorders from paraffin sections of skin. Am J Dermatopathol 1: 39. Li CY, Lam KW, Yam LT. (1973) Esterases in human leukocytes. J Histochem Cytochem 21:1. Lowe J. (1995) Histopathology. (www.nottingham.ac.uk) University of Nottingham Lutty GA, McLeod DS. (2005) Phosphatase enzyme histochemistry for studying vascular hierarchy, pathology, and endothelial cell dysfunction in retina and choroid. Vision Research 45(28): 3504–3511. Meier-Ruge WA, Bruder E. (2008) Current Concepts of Enzyme Histochemistry in Modern Pathology. Path obiology 75:233-243. Meijer AEFH. (1968) Improved histochemical method for the demonstration of the activity of α glucan phosphorylase. Histochemie 12, 244. Nachlas MM, Tsou KC, De Souza E et al. (1957) Cytochemical demonstration of succinic dehydrogenase by the use of a new p-nitrophenyl substituted ditetrazole. J Histochem Cytochem 5:420 Okun MR, Edelstein L, Niebauer G, Hamada G. (1969) The Histochemical Tyrosine-Dopa Reaction for Tyrosinase and its use in Localizing Tyrosinase Activity in Mast Cells. The Journal of Investigative Dermatology 53, 39–45 Pearse AGE. (1960) Histochemistry, Theoretical and Applied. London: J. and A. Churchill Ltd. Pinkus GS, Said JW. (1977) Profile of intracytoplasmic lysozyme in normal tissues, myeloproliferative disorders, hairy cell leukemia, and other pathologic processes. Am J Pathol 89: 351. Pinkus GS, Hargreaves HK, McLeod JA, Nadler LM, Rosenthal DS, Said JW. (1979) Alpha-Naphthyl acetate esterase activity--a cytochemical marker for T lymphocytees. Correlation with immunologic studies of normal tissues, lymphocytic leukemias, non-Hodgkin's lymphomas, Hodgkin's disease, and other lymphoproliferative disorders. Am J Pathol. 97(1):17-41. Rutenberg AM, Cohen NRB, Seligman AM. (1952) Histochemical demonstration of aryl sulphatase. Science, N. Y. 116, 539. Rutenberg AM, Seligman AM. (1955) The histochemical demonstration of acid phosphatase by a postincubation coupling technique. J. Histochem. Cytochem. 3, 455. Rutenburg AM, Rosales CL, Bennett JM. (1965) An improved histochemical method for the demonstration of leukocyte alkaline phosphatase activity: Clinical application. J Lab Clin Med 65:698. Sargaiyan V, Bansal A. (2014) Enzyme Histochemistry: A Review. J Adv Med Dent Science 2(2):191195. Vorbnrodt, A. (1961) Histochemical studies on the intracellular localization of acid deoxyribonuclease. J, Histochem. Cytochem. 9, 647. Wachstein M, Meisel E. (1957) Histochemistry of hepatic phosphatases at a physiologic pH with special reference to the demonstration of bile canaliculi. Amer. J. Clin. Path. 27, 13–23. Wachstein M, Meisel E, Falcon C. (1961) Histochemistry of thiolacetic acid esterase: a comparison with non-specific esterase with special regard to the effect of fixatives and inhibitors on intracellular localization. J. Histochem Cytochem 9, 325. William J. Howat WJ, Wilson BA. (2014) Tissue fixation and the effect of molecular fixatives on downstream staining procedures. Methods 70(1):12–19 Wyllie RG. (1965) Fixation in Enzyme Histochemistry. Nature 207, 93 – 94. CHAPTER 22 IMMUNOHISTOCHEMISTRY Jocelyn H. Bruce and Marc-Eli Faldas Immunohistochemical techniques are now routinely used for the identification of specific or highly selective cellular epitopes or antigens in frozen or paraffin-embedded tissues. Immunocytochemistry can also be used to detect organisms in cytologic preparations such as fluids, sputum samples, and fine needle aspirates. These immunologic techniques make use of antigenantibody interactions, whereby the site of antigen binding is demonstrated by direct labeling of the antibody, or by means of a secondary labeling method. Antibodies belong to the class of serum proteins known as immunoglobulins. IgG is the most commonly used antibody for immunocytochemistry. An epitope is the structural part of the antigen that reacts with an antibody. Immunohistochemistry (IHC) combines anatomical, immunological and biochemical techniques to identify discrete tissue components by the interaction of target antigens with specific antibodies tagged with a visible label. IHC makes it possible to visualize the distribution and localization of specific cellular components within cells and in the proper tissue context. While there are multiple approaches and permutations in IHC methodology, all of the steps involved are separated into two groups: sample preparation and labeling. IHC is used for disease diagnosis, drug development and biological research. Using specific tumor markers, physicians use IHC to diagnose a cancer as benign or malignant, determine the stage and grade of a tumor, and identify the cell type and origin of a metastasis to find the site of the primary tumor. IHC is also used in drug development to test drug efficacy by detecting either the activity or the up- or down-regulation of disease targets. Immunofluorescence is often, but not always performed on frozen tissue due to the high background auto-fluorescence seen in formalin fixed paraffin embedded tissue. Samples are prepared on individual slides, or multiple samples can be arranged on a single slide for comparative analysis, such as with tissue microarrays. IHC slides can be processed and stained manually, while technological advances now provide automation for high-throughput sample preparation and staining. Samples can be viewed by either light or fluorescence microscopy, and advances in the last 15 years have improved the ability to capture images, quantitate mult-0parametric IHC data and increase the collection of that data through high content screening. Polyclonal Antibodies Polyclonal antibodies are produced by immunizing an animal with a purified specific molecule (immunogen) that contains the antigen of interest, and collecting immunoglobulin-rich serum after the animal has produced humoral antibody against the antigen. The most frequently used animal for the production of polyclonal antibodies is the rabbit, followed by goat, pig, sheep, horse, guinea pig and others. Because polyclonal antibodies are produced by different cells of the animal, they are immunochemically not identical to each other, and they react with various epitopes on the antigen against which they are raised. Some of the polyclonal antibodies may cross-react with other molecules and cause nonspecific staining, requiring their purification by absorption with the appropriate antigen, or antibody dilution to eliminate the unwanted reaction. Monoclonal Antibodies Animals immunized with the specific immunogen will produce numerous clones of plasma cells (polyclonal) that in turn will produce the antibody. Monoclonal antibodies are the products of an individual clone of plasma cells. Hybridoma and cloning techniques have been developed to produce monoclonal antibodies that do not cross-react with other molecules. Antibodies from a given clone are immunochemically identical and react with a specific epitope on the antigen against which they are raised. Mice are currently used almost exclusively for the production of monoclonal antibodies. Propagation can be carried out in culture medium or by transplantation of the hybridoma into the peritoneal cavity of syngeneic mice from where the antibodies are harvested. This has dramatically increased the quantities and number of specific monoclonal antibodies available for immunohistochemistry. Preparing tissue for immunohistochemistry In certain instances, the tissue must be prepared as a cryostat section and fixed for a few seconds in absolute methanol or acetone, to preserve immunological activity and prevent destruction of some of the labile antigenic sites. However, immunofluorescence and immuno-peroxidase techniques may also be done on formaldehyde-fixed and paraffin embedded sections. Many masked antigens can now be retrieved in routinely processed tissue by (1) proteolytic enzyme digestion, (2) microwave antigen retrieval, (3) microwave and trypsin antigen retrieval or (4) pressure cooker antigen retrieval. Proteolytic Enzyme Digestion Formalin fixed paraffin sections are usually pre-treated with proteolytic enzymes to break down formalin cross-linking, unmask and allow certain antigenic sites to be exposed. Proteolytic enzyme digestion is especially useful for demonstrating heavy chain immunoglobulins, complement and specific antigens (such as cytokeratin) in formalin-fixed paraffin-embedded biopsies. The most common enzymes used are trypsin and protease. Before pretreatments are employed, the sections are deparaffinized, taken to alcohol and, in the case of peroxidase labeling, treated with 0.5% methanol in hydrogen peroxide for 10 to 15 minutes to destroy endogenous peroxidase activity. The slides are then washed in running water and taken to distilled water. The trypsin method uses 0.1% trypsin in 0.1 % calcium chloride in distilled water, adjusted to pH 7 .8 with sodium hydroxide, and preheated at 37°C. The slides are also preheated at 37°C in distilled water before placing in freshly prepared trypsin solution. After a predetermined period of time, the slide is transferred to cold running water to terminate enzyme digestion. The protease method uses 0.05 to 0.1% protease in distilled water, adjusted to pH 7.8 with sodium hydroxide. The section is preheated at 37°C in distilled water and placed in protease solution for a shorter period of time due to its faster rate of enzyme digestion. Paraffin Sections 1. Deparaffinize sections in xylene 2 times for 5 minutes each time. 2. Hydrate with 100% ethanol 2 times for 3 minutes each time. 3. Hydrate with 95% ethanol for 1 minutes. 4. Rinse in distilled water. 5. Follow procedure for pretreatment as required. Pre-treatment of Tissue Sections Antigenic determinants masked by formalin-fixation and paraffinembedding often may be exposed by epitope unmasking, enzymatic digestion or saponin, etc. Do not use this pretreatment with frozen sections or cultured cells that are not paraffin-embedded. Procedure 1. Rinse sections in PBS-Tween 2 times for 2 minutes each time. 2. Serum Blocking: Incubate sections with normal serum block – species same as secondary antibody, for 30 minutes to block non-specific binding of immunoglobulin. Note: This protocol uses avidin-biotin detection system. Avidinbiotin block may be needed based on tissue type. Normal serum block should be used prior to avidin-biotin block. 3. Primary Antibody: Incubate sections with primary antibody at appropriate dilution in primary antibody dilution buffer for 1 hour at room temperature or overnight at 4 °C. 4. Rinse in PBS-Tween 20. 5. Peroxidase Blocking: Incubate sections in peroxidase blocking solution for 10 minutes at room temperature. 6. Rinse in PBS-Tween 20. 7. Secondary Antibody: Incubate sections with biotinylated secondary antibody at appropriate dilution in PBS for 30 minutes at room temperature. 8. Rinse in PBS-Tween 20 3 times for 2 minutes each time. 9. Detection: Incubate sections in streptavidin-HRP in PBS for 30 minutes at room temperature. 10. Rinse in TBS 3 times for 2 minutes each time. 11. Chromogen/Substrate: Incubate sections in DAB solution for 1-3 minutes. 12. Rinse in PBS-Tween 20 2 times for 2 minutes each time. 13. Counterstain if desire. 14. Rinse in distilled water. 15. Dehydrate through 95% ethanol for 2 minutes, then 100% ethanol for 2 times 3 minutes each time. 16. Clear in xylene. 17. Coverslip with mounting medium. Heat-induced epitope retrieval (HIER) Heat-induced epitope retrieval (HIER), a simple laboratory technique that has become an essential part of many immunohistochemistry and in situ hybridization procedures, is a pretreatment method used to improve staining results. Heat, coupled with specific buffered solutions, is utilized to recover antigen reactivity in formalin fixed paraffin embedded tissue. It reverses the formaldehyde mediated chemical modifications of the antigen through either of the following processes. First and foremost, thermal energy breaks the crosslinks that bind surrounding proteins or peptides to the antigen which lead to the “opening” or “unmasking” the epitope. And, second, thermal energy removes bound calcium ions from the sites of cross-links since several HIER buffers, such as EDTA and citrate, act as calcium chelators. HIER heating sources include the microwave, vegetable steamer, pressure cooker and water bath. In general, the higher the temperature of the HIER solutions, the more effective the recovery of the epitope is. While each of these heating sources is suitable for HIER, there are advantages as well as drawbacks associated with each source. For example, often, the microwave distribution of heat within a microwave is uneven or inconsistent which results in a lack of reproducibility as to staining intensities. In contrast, the pressure cooker, steamer and water bath produce uniform and consistent heat distribution. However, while the higher temperatures produced by the pressure cooker are advantageous since, in a short period of time, an effective recovery of epitope reactivity can be readily achieved, damage or distortion to the morphology of connective tissues can also occur. Heat-Induced Epitope Retrieval (HIER) www.rndsystems.com Reagents Required for Heat-induced Epitope Retrieval: • 10 x Antigen Retrieval Solution: o Antigen Retrieval Reagent-Basic o Antigen Retrieval Reagent-Acidic o Antigen Retrieval Reagent-Universal • Deionized H2O • 1 x PBS: 0.137 M NaCl, 0.05 M NaH2PO4, pH 7.4 Equipment: • Polypropylene Coplin staining jar (or equivalent) • Water bath at 92-95°C Procedure: 1. Make working dilutions by mixing 1 part of 10X Antigen Retrieval concentrate with 9 parts of deionized water. 2. Preheat retrieval solution to 92-95°C. This may be achieved by placing a polypropylene Coplin staining jar filled with retrieval solution into a water bath. Note: Heating may cause cracking of glass staining dishes. 3. Immerse slides into preheated retrieval solution for 2-10 minutes. Note: Since the effect of antigen retrieval reagents depends on their temperature (90-100 °C) and incubation time (up to 30 minutes), optimal conditions should be determined by the individual investigator. Cryostat sections are more sensitive to damage by retrieval solution than paraffin-embedded tissues. To avoid tissue damage, it may be necessary to shorten the incubation time to 2-5 minutes. 4. After the incubation is finished, remove the Coplin jar with retrieval solution and slides from the water bath, and let it cool to room temperature. 5. Gently rinse the slides with deionized water and then with PBS. Note: Because tissues may be loosened after the retrieval procedure, avoid vigorous rinsing to prevent detachment from the slides. Microwave Antigen Retrieval Microwave antigen retrieval is a relatively new technique that involves the boiling of formalin-fixed deparaffinized sections in certain solutions, such as 0.01 M-citrate buffer (pH 6.0), EDTA at pH 8.0 or Tris EDTA (pH or 10.0). Many antigens thought previously to be either lost or destroyed by routine histological processing techniques can be retrieved by microwave oven heating. Antibodies such as the proliferation markers (Ki-67 and MIB-1), hormone receptors (ER and PR), growth factor receptors (HER-2/neu) and others which were previously thought to be applicable only to frozen sections, are demonstrated well on paraffin sections after heat pre-treatment. Most antigen retrieval methods apply temperatures near the boiling point of water. The optimal length of exposure to heat may vary from 10 to 60 minutes and depends to some extent on the length of formalin fixation. The most satisfactory time period appears to be 20 minutes for most antigens and fixation protocols. Care should be taken not to allow the sections to dry after heating, as this destroys antigenicity. Boiling of poorly fixed material often damages nuclear details. Fibrous and fatty tissues tend to detach from the slide. This can be prevented by mounting the sections on slides with a strong adhesive (such as Vectabond), or dipping Vectabond-coated slides in I0% formol saline for 1 to 2 minutes and air drying before picking up sections. Amplification of nucleic acids from paraffin-embedded material by the polymerase chain reaction (PCR) is increasingly being used to detect viral genomes and oncogene mutations. On amplifying DNA, consistent product was seen in the ethanol and Omnifix specimens up to 72 hr. of fixation time. On amplifying RNA, a product could be detected even after 1 week of fixation in ethanol or Omnifix, and after 48 hr. in the formalin-fixed tissue. Bouin's and B-5 tissues give consistent results only after 6 hr. of fixation. The choice of fixative and fixation time are critical factors influencing the outcome of PCR amplification of nucleic acids from paraffin-embedded material. Pressure Cooking Antigen Retrieval Pressure cooking antigen retrieval is another alternative that appears to be less time consuming and allows for more consistent recovery of many antigens, compared to large batch microwave oven technique. In the large batch microwave oven technique, heating temperature is not uniformly distributed and slides are subjected to "hot spots" and "cold spots" resulting in inconsistent antigen recovery. Antigens Primary antibodies against numerous antigens are now available in the market, and are widely used for diagnosis of tumors, determination of tumor type, the evaluation of prolife-ration potential, identification of infectious agents, prognostic and therapeutic implications, and many other aspects of diagnostic pathology. Epithelial tumor markers: 1. Keratin is a highly sensitive marker for epithelial cells, and is present in epithelial tumors (carcinoma). Certain non-epithelial tumors (such as mesotheliomas and non-seminomatous germ cell tumors) also stain positive for keratin, and may be distinguished from carcinoma by applying an additional panel of antibodies. a) CK7 (Cytokeratin 7) is more frequently found in carcinomas of the lung, breast, uterus and ovaries (serous tumors). These tumors are typically negative for CK20. b) CK20 (Cytokeratin 20) is more common in carcinomas of the colon and stomach. These tumors are usually negative for CK7. c) Transitional cell carcinomas of the bladder and mucinous ovarian tumors are usually positive for both CK7 and CK20. d) Renal cell carcinomas, hepatocellular carcinomas, prostatic adenocarcinomas, thyroid carcinomas and squamous cell carcinomas (skin, lung and esophagus) are usually negative for either CK7 or CK20. 2. EMA (Epithelial membrane antigen) is a high molecular weight protein that is helpful in determining the site of tumor. It is positive for adenocarcinomas of the breast, lung and kidneys but more often nonreactive for hepatocellular carcinomas, adrenal carcinomas or embryonal carcinomas, and negative for non-epithelial tumors (sarcomas, lymphomas, melanomas) and other tumors (meningiomas, mesotheliomas, anaplastic large cell lymphomas, and plasma cell tumors). 3. CEA (Carcinoembryonic antigen) is an oncofetal antigen that is present in carcinomas of the gastrointestinal tract, pancreas, lung, breast, ovary, uterus and cervix. It is especially useful for differentiating between adenocarcinoma (CEA-positive) and mesothelioma (CEA-negative). Prostate, thyroid and renal carcinomas are usually non-reactive to CEA. 4. TTF-1 (Thyroid transcription factor-1) is useful in distinguishing lung adenocarcinomas from mesotheliomas. It is positive in thyroid, lung and neuroendocrine tumors (medullary thyroid carcinomas, carcinoid tumors and small cell tumors of the lung). 5. PSA (Prostate specific antigen) is extremely useful in the diagnosis of prostatic adenocarcinoma. It is also positive in certain pancreatic and salivary gland tumors. Intermediate Filament Markers 1. Actin is a contractile intermediate filament protein present in muscle and some non-muscle tissue. It is a sensitive marker for muscle differentiation and can be used to identify tumors derived from smooth, skeletal and cardiac muscle. 2. Vimentin is a 57kD intermediate filament that is present in normal mesenchymal cells and their neoplastic counterparts (i.e., sarcoma, melanoma, lymphoma, leukemia, seminoma, and some neural tumors). Melanomas and schwannomas always stain positive for vimentin, so that a negative staining may be used to exclude the diagnosis. It is almost always present in tissue sections because of the background stromal elements, and has limited use as a stand-alone stain, but it can be very helpful when combined with other specific tumor markers. 3. Desmin is a 53 kD intermediate filament expressed by smooth and striated (skeletal and cardiac) muscle. It is considered to be highly specific for myogenic tumors, including leiomyoma (smooth muscle tumor) and rhabdomyosarcoma (skeletal muscle tumor). It is also used to demonstrate the myogenic component of mixed tumors (i.e., carcinosarcomas or malignant mixed mesodermal tumors). 4. Glial fibrillary acidic protein (GFAP) is a 51 kD intermediate filament protein expressed by central nervous system glial cells, particularly astrocytes. It is most widely used to confirm the diagnosis of astrocytoma (but may also be present in certain cases of ependymomas, oligodendrogliomas and medulloblastomas). Non-CNS tumors (meningiomas, metastatic carcinomas and lymphomas) stain negative for GFAP. 5. Neurofilament (NF) is expressed in cells of neural origin, particularly neurons, neuronal processes, peripheral nerves, sympathetic ganglia, adrenal medulla and neuroendocrine cells. Tumors that show neuronal or neuroendocrine differentiation (e.g., neuroblastomas, ganglioneuromas, neuromas, chemodectomas, and pheochromocytomas) will stain positive for neurofilament. 6. S-100 protein is a low molecular weight calcium-binding protein that is expressed in CNS glial cells, Schwann cells, melanocytes, histiocytes, chondrocytes, skeletal and cardiac muscle, myoepithelial cells and some epithelial cells of breast, salivary and sweat gland epithelium. Neuroendocrine markers: 1. Neuron-specific enolase (NSE) is an isoenzyme marker whose presence in tissue provides strong evidence of neural or neuroendocrine differentiation. 2. Chromogranin is found in the neural secretory granules of endocrine tissues, and is recognized as a marker for neuroendocrine differentiation. Immunoreactivity is typically granular and its distribution is similar to that seen with silver staining methods such as Grimelius stain. A combination of keratin and chromogranin positivity is typical of neuroendocrine carcinoma. Chromogranin positivity with a negative keratin stain is typical of paraganglioma. 3. Synaptophysin is a 38 kD transmembrane protein associated with presynaptic vesicles of neurons. It has been identified in normal neurons and neuroendocrine cells. Germ cell tumor markers Non-seminomatous germ cell tumors (i.e. embryonal carcinomas, teratomas, choriocarcinomas, and endodermal sinus or yolk sac tumors) generally stain positive for epithelial markers (keratin). For more specific classification, the following germ cell tumor markers are used: 1. HCG (Human chorionic gonadotropin) is synthesized by placental syncytiotrophoblasts, and is a marker for choriocarcinoma. 2. APP (Alpha-fetoprotein) is synthesized by normal liver hepatocytes, and is used as a marker for endodermal sinus tumors showing yolk sac differentiation. Embryonal carcinomas and teratomas containing these elements, as well as hepatocellular carcinomas will also stain positive for APP. 3. PLAP (Placenta-like alkaline phosphatase) is produced by the placental syncytiotrophoblasts in late pregnancy, and is used as a marker for germ cell tumors, particularly germinomas. Most embryonal carcinomas, choriocarcinomas and endo-dermal sinus tumors will also stain positive for this antibody. PLAP is positive in majority of seminomas. Mesenchymal tumor markers 1. Myogenic tumors - Tumors of skeletal muscle origin are positive for muscle-specific actin and desmin and/or other muscle markers such as myo-D1, myoglobin and myogenin. 2. Fibrohistiocytic tumors - The use of histiocytic markers such as CD68, or FAM 56, combined with more nonspecific proteolytic enzymes such as alpha-1-antitrypsin and alpha-1-antichymotrypsin may be helpful in the diagnosis of malignant fibrohistiocytic sarcomas. An undifferentiated component of sarcoma may react only with vimentin. 3. Vascular tumors - Endothelial markers for vascular tumors (such as angiosarcomas) include Factor VII-related antigen, CD31 and Ulex Europaeus 1 (UEA). 4. Melanomas - Melanocytes are derived from neural crest and will be reactive for S100 protein. The intensity of staining for S100 is usually inversely proportional to the melanin content of the tumor. Melanosome (HMB-45) is a widely used, highly sensitive and highly specific marker for the diagnosis of melanoma. Melan-A (MART-1) also encodes a melanoma-specific antigen that is present in normal pigmented cells of skin and retina as well as in certain adrenocortical tumors. 5. Lymphomas - The best screening marker for lymphoma is LCA (leukocyte common antigen), also known as CD45. For immunophenotypic subclassification of lymphoma, the most common markers used include those for T cells (CD3, CD4, CDS), B cells (CD19, CD20, CD23), Reed-Sternberg cells (CD15, CD30), and immunoglobulin light and heavy chains. Cell Proliferation Markers Ki-67 (MIB-1) and PCNA (proliferating cell nuclear antigen) are the most common immunohistochemical markers used to assess proliferation of tumor cells. Increased expression of these antigens is usually associated with greater aggressiveness and higher likelihood of recurrence of metastasis. Cancer-associated genes The development and progression of a malignant phenotype of human tumors is related to abnormalities of structure or activity of proto-oncogenes and/or mutation of tumor suppressor genes such as p53. Many cellular oncogenes, including c-erbB-2, c-myc and ras have been found to be activated in cancer, particularly of the breast. Infectious Agent Markers Antigenic markers are now available for a number of infectious agents, including hepatitis A virus, hepatitis B surface and core antigens, hepatitis C virus, human papilloma virus, cytomegalovirus, Epstein-Barr virus, toxoplasma, pneumocystis carinii, helicobacter pylori, cryptosporidium, cryptococcus neoformans, histoplasma, entamoeba histolytica, and mycobacteria. For mycobacteria, immunohistochemical techniques are more sensitive, the results are obtained faster than with tissue culture, and they are easier to read than acid-fast stains. Controls It is essential to use positive and negative controls when processing tissue sections for immunohistochemistry, in order to test for specificity of the antibodies involved, and to avoid misinterpretations due to false positive or false negative results. To be specific, the immunohistochemical technique must not cause staining in the absence of the primary antiserum. The staining should be inhibited when the primary antibody is adsorbed by the relevant antigen prior to its use, but it should not be inhibited when the primary antibody is absorbed by other related or unrelated antigen. 1. Positive Control: It is always advisable to use, as positive control, a section that is known and proven to contain the antigen in question because absence of staining in a test section does not necessarily mean that the antigen is absent in the tissue being studied. 2. Negative Control: This can be done using a parallel section from the tissue, and either omitting the primary antibody from the staining schedule or replacing the specific primary antibody by an immunoglobulin that is directed against an unrelated antigen. 3. Internal Tissue Control: Also named as "built in" control, this eliminates the variable of tissue fixation between specimens and controls but it contains the target antigen, not only in the tissue elements under investigation, e.g. tumors, but also in adjacent normal tissue element. One example is the presence of S-100 protein in both melanoma and normal tissue elements, such as peripheral nerves and melanocytes. Chromogenic Method Chromogenic (brightfield) and fluorescence detection techniques are used in the determination of the presence and subcellular location of an increasing number of proteins within a single biopsy. Chromogenic multiimmunohistochemical staining is based on immunoenzymatic reaction with chromogen and enzyme. Chromogenic IHC staining can generate dense deposits that are easy to detect but difficult to quantitate, because of nonlinear optical effects and low achievable dynamic ranges. In facilitating chromogenic detection, the primary antibody, secondary antibody, or streptavidin is conjugated to an enzyme. Horseradish peroxidase (HRP) and alkaline phosphatase, which convert 3,3' diaminobenzidine (DAB) and 3-amino-9ethylcarbazole (AEC), into brown and red end products, respectively are commonly used enzymes. When a soluble organic substrate is applied, the enzyme reacts with the substrate to generate an insoluble colored product that is localized to the sites of antigen expression. Chromogenic detection is considered to be a more sensitive method than immunofluorescence. It requires only a typical light microscope unlike fluorescence microscopy which requires a specialized light source and filter sets. Chromogenic detection, however, is less convenient because it includes more incubation and blocking steps. Like immunofluorescence, it allows for the visualization of multiple antigens, but only if the antigens are confined to different locations in the cell and tissue because overlapping colors may obscure results. An advantage of DAB chromogenic staining is that the colored precipitate formed during the reaction between HRP and DAB is not sensitive to light and the slides can be stored for many years. Enzyme Labeling Enzymes are widely used in immmunohistochemistry, and are usually incubated with a chromogen using standard histochemical method to produce a stable colored reaction. Enzyme labeling of antibodies with horseradish peroxidase, followed by staining with appropriate substrate or chromogen mixture such as diaminobenzidine (DAB), will produce an insoluble dark brown reaction end product, and allow labeled cells to be counterstained with hematoxylin and other nuclear stains. The optimal incubation time for linking antibodies with peroxidase conjugates is 30 to 60 minutes at room temperature. Direct Technique The traditional direct technique of doing immunohistochemistry is to conjugate the primary antibody directly to the label, such as a fluorochrome or horseradish peroxidase. The main advantage of using directly labeled antibody is that it is simple and quick, because it requires only one application of the reagent, followed by the appropriate chromogen substrate solution. However, it is less sensitive compared to indirect techniques that involve 2 or 3 stages of conjugation and staining. This carries the risk of not detecting small amounts of antigen that could be crucial in making the diagnosis. The method is no longer sufficiently sensitive for today's demands. Enhanced Polymer One-Step Staining (EPOS) method The Enhanced Polymer One-Step Staining (EPOS) method, marketed by Dako A/S, is a new direct technique whereby a large number of primary antibody molecules and peroxidase enzymes are attached to a dextran polymer "backbone" or "spine molecule". The chief advantage of the EPOS technology is the reduced number of incubation steps of the staining protocol required, so that rapid staining is completed in a single step within 10 minutes. In addition to an average of 70 molecules of enzyme, 10 molecules of antibody can be attached to the spine molecule. It is more sensitive than the traditional direct technique, and is suitable for frozen section immunohistochemistry. Conjugation of both antirabbit and anti-mouse secondary antibodies renders the system useful for both polyclonal and monoclonal antibodies. Because these systems avoid the use of (strept) avidin and biotin, nonspecific staining that results from endogenous biotin is eliminated. The main disadvantage is the limited number of primary antibodies commercially available for this system. Fig. 22-1. Immunohistochemistry - Direct Technique General EPOS Procedure (Peroxidase) 1. Quench for endogenous peroxidase activity (optional). 2. Rinse with and place in wash buffer for 3 to 5 minutes. 3. Incubate with EPOS conjugate for 10 to 60 minutes. 4. Rinse with and place in wash buffer for 3 to 5 minutes. 5. Incubate with substrate-chromogen for 5 to 15 minutes. 6. Counterstain (optional) and coverslip. Indirect Technique The indirect technique of immunohistochemistry is a 2 or 3 step procedure that involves application of the unconjugated primary antibody, followed by a labeled antibody directed against the first antibody. It is relatively inexpensive, and is more sensitive than the traditional direct technique because several secondary antibodies are likely to react with a number of different epitopes of the primary antibody, thereby amplifying the signal as more enzyme molecules are attached per target site. Horseradish peroxidase is the most commonly used enzyme for indirect antibody enzyme-complex techniques. Fig. 22-2. Immunohistochemistry- Indirect Technique Two-step Indirect Technique In this technique, an unconjugated primary antibody first binds to the antigen. An enzyme-labeled secondary antibody directed against the primary antibody (now the antigen) is then applied, followed by the substratechromogen solution. If the primary antibody is made in rabbit or mouse, the secondary antibody must be directed against rabbit or mouse immunoglobulins, respectively. Cross-reactivity is eliminated by using preabsorbed secondary antiserum (i.e., antiserum that has been absorbed with immunoglobulins from the species under investigation). Three-step Indirect Technique In this technique, a second enzyme-conjugated antibody is added to the previously described indirect technique. The addition of a third layer of antibody serves to further amplify the signal, since more antibodies are capable of binding to the previously bound secondary reagent. Soluble Enzyme Immune Complex Techniques (Unlabeled Antibody Techniques) These techniques utilize preformed soluble enzyme-anti-enzyme immune complex. The staining sequence involves the use of an unconjugated primary antibody, a secondary antibody, the soluble enzyme-anti-enzyme complex, and the substrate solution. Paraffin Wax Section Immunoperoxidase Technique Paraffin wax section immunoperoxidase technique remains a standard method among most laboratories, especially in combination with frozen section processing for immunofluorescence of renal and skin biopsies. Routinely fixed, paraffin-embedded specimens combine good morphology with localization of various cell and tissue markers. It does not require an expensive fluorescence microscope, it can be adapted as a diagnostic procedure for formalin-fixed, paraffin embedded specimen, and immunolabeling can be correlated with morphology. However, it is more time consuming than frozen-section immunofluorescence. Especially for renal and skin biopsies, proteolytic enzyme digestion is necessary, and is best achieved by using trypsin, chymotrypsin or protease. Nonimmune serum is required to block nonspecific staining, especially when polyclonal antibodies are employed. Avidin-biotin labeling, especially with peroxidase, is currently the most popular system used in diagnostic laboratories. The most popular fixative for paraffin embedded sections is neutral buffered formalin. There may be shrinkage or distortion during fixation or subsequent paraffin-embedding, but generally, formalin-based fixatives are excellent for most immunostains. Although some antigens are not well demonstrated after fixation in formaldehyde-based fixatives, many can be demonstrated after the use of appropriate pretreatment methods, such as proteolytic enzyme digestion and/or antigen retrieval, particularly if polyclonal antisera are used. Mercuric chloride-based fixatives such as formol sublimate and B5 have gained some popularity because they improve cytological preservation and minimize the distortion associated with formaldehyde-based fixatives. They cause considerable hardening of tissue because of their coagulative properties, allowing thin slices to be made. These types of fixatives are particularly suitable for the demonstration of intracytoplasmic antigens. B5 is widely recommended for the fixation of lymph node biopsies, both to improve the cytological detail and to enhance immunoreactivity with the antiimmunoglobulin antisera used in phenotyping B cell lymphomas. B5-fixed, paraffin embedded tissue sections show excellent results with cytoplasmic immunoglobulins. However, surface membrane immuno-globulin is not stained as readily. As a general rule, enzyme pretreatments do not improve, and may actually hinder immunostaining of tissue fixed in mercuric chloride-based coagulative fixatives. Alcohol is not widely used as a fixative for routine histological techniques because of its poor penetrating ability. However, small pieces of tissue are fixed rapidly and show good cytological preservation. Since alcohols are coagulant fluids and do not form additive compounds, they permit good antibody penetration and do not block immunoreactive determinants. Alcohol fixation is more commonly used in research laboratories where the size of specimens and handling requirements are different from those observed in routine histopathology. It is also generally applied to frozen sections or smears. Preparing paraffin wax sections for immunostaining 1 Cut 3-S µm sections and place on cleaned glass slides. Vectabond or APES-coated slides may be used to assist with section adhesion. 2. Place sections at 60°C microwave oven overnight (if processing sections without adhesives) or at 56°C for 1 to 2 hours (if Vectabond- or APEScoated slides are used). Heating on a hot plate at high temperature is not recommended because it can be detrimental to the antigen. 3. Deparaffinize sections in xylene and bring to absolute alcohol. 4. Block endogenous peroxidase activity by incubating in 0.5% hydrogen peroxide in methanol for 10 minutes. 5. Rehydrate, wash well in running water and transfer to tris-buffered saline (TBS). 6. To retrieve antigen: a. Preheat slides at 37°C in distilled water. b. Transfer to freshly prepared trypsin solution at 37°C for 15 to 120 minutes (depending on specimen size, duration of fixation and rate of fixation), using 0.1% trypsin in 0.1% calcium chloride in distilled water, adjusted to pH 7.8 using 0.1M NaOH and preheated at 37°C. c. Terminate trypsin enzyme digestion by transferring the sections to cold running tap water. Peroxidase-Antiperoxidase (PAP) Technique The peroxidase-antiperoxidase (PAP) technique is an indirect antibody enzyme-complex technique where the soluble peroxidase-antiperoxidase complex is bound to unconjugated primary antibody (e.g. rabbit anti-human IgG) by a second layer of "bridging" antibody usually a swine anti-rabbit antibody) that then binds to both the primary antibody and the rabbit PAP complex. Fig. 22-3. Peroxidase-Anti-Peroxidase (PAP) Technique Horseradish peroxidase is the most widely used enzyme for labeling. Combining horseradish peroxidase with the most common chromogen, diaminobenzidine (DAB), results in a stable, insoluble dark brown reaction end product when antigen is present in the tissue. To block endogenous peroxidase activity, the sections are pre-incubated in absolute methanol containing hydrogen peroxide. Alkaline phosphatase antibodies raised in mouse, by the same principle, can also be used to form alkaline phosphatase-anti-alkaline phosphatase complexes (APAAP). The major advantage of APAAP procedure compared to the PAP technique is the lack of interference from endogenous peroxidase activity. APAAP technique is recommended for use on blood and bone marrow smears because of the potential distraction of endogenous peroxidase activity on PAP staining. Endogenous alkaline phosphatase activity is usually blocked by adding levamisole to the substrate solution. Peroxidase-Antiperoxidase (PAP) Technique for Paraffin Sections Solutions: Buffer Wash: O.OO5M Tris buffered saline TBS) Tris-Buffered Saline Wash (O.OO5M TBS) Distilled water 1 liter Sodium chloride 8 gm TRIS (hydroxymethyl methylamine) 0.6 gm M HCl 4.4 ml. If necessary, adjust final pH to 7.6 with either 1 M HCl or 0.2 M Tris solution. Substrate: DAB (Diaminobenzidine tetrahydrochloride) Tris-HCL Buffer (recommended for DAB) 0.2 M Tris (containing 24.228 g/l) 12 ml 0.1 M HCl 19 ml. Distilled water 19 ml. DAB Solution DAB 5 mg. Tris-HCI buffer (pH 7.6) 10 ml. H2O2 0.1 ml. (Freshly prepared and added just before use) Method: 1. Bring sections to Tris-buffered saline (TBS). 2. Drain off and wipe around section. 3. Incubate with 1:10 dilution of normal swine serum for 10 minutes. Drain, but do not wash off before applying primary antibody. 4. Incubate in optimally diluted rabbit primary antibody for 30 to 60 minutes. 5. Gently wash in TBS. 6. Incubate in optimally diluted swine anti-rabbit antibody for 30 minutes. 7. Gently wash in TBS. 8. Incubate in optimally diluted rabbit peroxidase anti-peroxidase for 30 minutes. 9. Gently wash in TBS. 10. Incubate in freshly prepared DAB solution at room temperature until a dark brown reaction product is obtained, usually after 5 to 10 minutes. The reaction end-product resists alcohol dehydration and clearing in xylene. 11. Rinse in TBS and wash in running water. 12. Counterstain in hematoxylin. 13. Dehydrate, clear and mount. Practical Considerations 1. Antigen-antibody reactions are reversible, and simple immune complexes formed on the tissue may dissociate during the washing cycles used while performing immunohistochemistry. 2. Low salt concentrations as well as low temperatures will reduce the likelihood of weak staining due to dissociation of already formed immune complex. 3. Monoclonal antibodies, compared to polyclonal antibodies, depend more on environmental factors such as pH and solute for optimum performance. When using monoclonal antibodies, high salt concentrations, high temperature and very low pH should be avoided during the washing of specimens to avoid loss of staining due to weakening the antigen-antibody bond. 4. The recommendations for handling and storage given by the manufacturer on specification sheets and on vial labels should always be followed in order to achieve optimal performance for the reagents used in immunohistochemistry. 5. Refrigerators and freezers used for storage of immunochemicals should be monitored for accurate and consistent temperatures. 6. Store most pre-diluted ("ready to use") antibodies, their conjugates, and monoclonal antibody solutions at 2-8°C because freezing and thawing will reduce their effectiveness. 7. Concentrated protein solutions such as antisera and immunoglobulin fractions should be stored in aliquots and frozen at -20°C or below to prevent cycles of repeated freezing and thawing. 8. Frozen protein solutions should be brought to room temperature slowly, and temperatures above 25°C should be avoided. 9. Reagent contamination can be avoided by the use of disposable clean pipette tips. 10. Higher concentrations of specific antibodies (and higher affinities) allow for the shortening of incubation time. 11. The optimal incubation time for most primary antibodies is 20 to 30 minutes at room temperature (20 to 22°C). Overnight (18 hour) incubation of sections at 4°C will increase the sensitivity of the procedure with some monoclonal antibodies, particularly those against cell membrane antigens. To accomplish this, adequate amounts of the primary antibody are applied, the section is covered with a cover glass, and the slide is stored horizontally in a regular refrigerator. 12. It is possible to decrease the incubation time to 5 to 10 minutes by increasing the temperature to 37°C. Slides incubated for extended periods or at 37°C should be placed in a humidity chamber to prevent evaporation and drying of the tissue sections. Immunostaining in higher temperatures will have unpredictable and sometimes cause false negative results. 13. Low levels of antigens may not be detected, and may result in false negative staining. Increasing the concentration of the primary antibody or prolonging incubation with primary antibody overnight at 4°C or at ambient temperature, can enhance staining. 14. Inhibiting endogenous enzyme activity, especially peroxidase and alkaline phosphatase, prior to staining can eliminate false-positive reactions. a. Endogenous enzyme peroxidase can be blocked by pre-incubating the sections in absolute methanol containing 0.5% hydrogen peroxide for 10 minutes at room temperature. b. Most endogenous alkaline phosphatase activity can be blocked by adding 1 mm. concentration of levamisole to the final incubating medium. 15. Non-specific uptake of antigen can cause high levels of background staining. This can be due to apparent affinity of collagen, reticulin and other tissue components for immuno-globulin, or due to nonimmunological binding of specific immune sera within the tissue section. 16. Inadequate or delayed fixation may give rise to false-positive results due to passive uptake of plasma proteins, including immunoglobulins by the cells. 17. Misinterpretation resulting from false-positive reactions can be avoided by using an anti-albumin control. 18. In general, it is the first immune sera applied that gives rise to high levels of non-specific binding. Background staining can be reduced by incubating the sections in an immunoglobulin that will not react or interfere with the primary specific antiserum, such as normal whole serum from the species in which the second (bridging) antibody is raised. 19. Nonspecific background staining can be reduced by adding a blocking serum to the diluted primary antiserum, or by using primary antiserum at high dilutions, or by enzymatic digestion or by adding a detergent such as Triton X. 20. When alkaline phosphatase serves as an enzyme label in the procedure, avoid using phosphate buffers as they inhibit the activity of the enzyme. 21. Sodium azide, an antibacterial agent present in many commercially prepared buffers, can prevent binding of the peroxidase enzyme to its substrate and inhibit color development. Its use in wash and diluent buffers should be avoided. 22. Common chromogens for peroxidase are diaminobenzidine (DAB) and aminoethylcarbazole (AEC), both of which should be made fresh immediately before use. Failure to add hydrogen peroxide to either of these solutions is a common oversight, particularly or beginners, and results in total lack of staining of all slides, including positive controls. 23. Etching a circle around the tissue section with a diamond pen will prevent diffusion of reagent over the entire slide, thereby saving precious antibody. Blocking of Unwanted Non-specific Staining Unwanted non-specific staining, a common problem in immunohistochemistry experiments, generally occurs when there is binding of the primary antibody to amino acids other than those within the desired epitope of the antigen. In the context of antibody-mediated antigen detection, nonspecific binding causes high background staining that can mask the detection of the target antigen. Thus, how to block non-specific interactions without reducing the antibody-epitope binding is the challenge to overcome in this case. Sources of unwanted non-specific staining include endogenous enzymes or fluorochromes, endogenous biotin, endogenous antibody binding activity and cross reactivity of the secondary reagents with endogenous proteins. They result in high background causing difficulties in visualizing the antigen of interest in its appropriate cellular location. However, the use of a blocking reagent prior to incubation of the sample with the primary antibody can effectively block nonspecific staining interactions. Common blocking buffers include normal serum, non-fat dry milk, BSA or gelatin, and commercial blocking buffers with proprietary formulations are available for greater efficiency. Avidin-Biotin Complex (ABC) Techniques The Avidin-Biotin Complex technique uses avidin (derived from egg white) because of its marked affinity for biotin, a low molecular weight vitamin that can be easily conjugated to antibodies and enzyme markers. Variants of the avidin-biotin system include peroxidase and alkaline phosphatase, either directly bound to avidin or streptavidin (a similar molecule extracted from the culture broth of the bacterium streptomyces avidini. Alternatively, the enzymes are biotinylated and the avidin-binding sites are occupied by the biotinylated label, forming the avidin-biotin complex. These are supplied commercially as two separate reagents, biotinylated label and avidin or streptavidin, and are added together 30 minutes before use. The basic sequence of staining consists of primary antibody, biotinylated secondary antibody, followed either by the preformed (strept) avidin-biotinenzyme complex of the avidin-biotin complex (ABC) technique or by the enzyme labeled streptavidin. Formation of ABC complex requires that the solutions of the (strept)avidin and biotinylated enzyme are mixed and prepared at least 30 minutes before use. All incubations are carried out at room temperature. TISSUE Fig. 22-4. Avidin-Biotin Complex (ABC) Technique Method: 1. Paraffin section or frozen section to water and rinse in PBS-Tween 20 twice for 2 minutes each time. 2. Perform antigen retrieval if necessary. 3. Incubate sections in normal serum – species the same as secondary antibody. Note: Since this protocol uses avidin-biotin detection system, avidin/biotin block may be needed based on tissue type. 4. Incubate sections in primary antibody at appropriate dilution for 1 hour at room temperature or overnight. Note: No serum blocking is needed if antibody diluent is used. 5. Rinse in PBS-Tween 20 buffer 3 times for 2 minutes each time. 6. Incubate sections in peroxidase blocking solution for 10 minutes at room temperature. Note: For acetone fixed frozen sections, perform this peroxidase blocking step using 0.3% H2O2 in methanol prior to primary antibody incubation to avoid tissue destruction. 7. Rinse in PBS-Tween 20 buffer 3 times for 2 minutes each time. 8. Incubate sections in biotinylated secondary antibody in PBS for 30 minutes at room temperature. 9. Rinse in PBS-Tween 20 buffer 3 times for 2 minutes each time. 10. Incubate sections in ABC-Peroxidase Solution for 30 minutes at room temperature. 11. Rinse in PBS-Tween 20 buffer 3 times for 2 minutes each time. 12. Incubate sections in peroxidase substrate solution. 13. Rinse in PBS-Tween 30 buffer 3 times for 2 minutes each time. 14. Counterstain with counterstain solution. 15. Rinse in running tap water for 2-5 minutes. 16. Dehydrate through 95% ethanol for 1 minute, and then 100% ethanol 2 times for 3 minutes each time. 17. Clear in xylene 2 times for 5 minutes each time. 18. Coverslip. Labeled Streptavidin Biotin Technique (LSAB Procedure) A labeled avidin-biotin (LAB) method has been recently introduced and is found to be 4 to 8 times more sensitive than the old ABC method. Also, avidin has now been largely replaced by the use of streptavidin, leading to the labeled streptavidin-biotin (LSAB) method. The staining sequence consists of primary rabbit (or mouse) antibody, biotinylated anti-rabbit (or anti-mouse) immunoglobulin and streptavidin-enzyme conjugate. The color reaction is then developed with the appropriate substrate/ chromogen, such as horseradish peroxidase. Method: 1. Paraffin section or frozen section to water and rinse in PBS-Tween 20 times for 2 minutes each time. 2. Perform antigen retrieval if necessary. 3. Incubate sections in normal serum – species same as secondary antibody. Note: since this protocol uses avidin-biotin detection system, avidin/biotin block may be needed based on tissue type. 4. Incubate sections with primary antibody at appropriate dilution for 1 hour at room temperature or overnight. No serum blocking is needed if antibody diluent is used. 5. Rinse in PBS-Tween 20 buffer 3 times for 2 minutes each time. 6. Incubate sections in peroxidase blocking solution for 10 minutes at room temperature. Note: For acetone fixed frozen sections, perform this peroxidase blocking step using 0.3% H2O2 in methanol prior to primary antibody incubation to avoid tissue destruction. 7. Rinse with PBS-Tween 20 buffer 3 times for 2 minutes each time. 8. Incubate sections in Biotinylated secondary antibody in PBS for 30 minutes at room temperature. 9. Rinse with PBS-Tween 20 buffer 3 times for 2 minutes each time. 10. Incubate sections in HRP-Streptavidin solution for 30 minutes at room temperature. 11. Rinse with PBS-Tween 20 buffer for 3 times for 2 minutes each time. 12. Incubate sections in peroxidase substrate solution. 13. Rinse with PBS-Tween 20 buffer for 3 times for 2 minutes each time. 14. Counterstain with hematoxylin. 15. Rinse in running tap water for 2-5 minutes. 16. Dehydrate through 95% ethanol for 1 minute, and then 100% ethanol 2 times for 3 minutes each time. 17. Clear in xylene 2 times for 5 minutes each time. 18. Coverslip. Immunofluorescence Method Immunofluorescence technique has become an emerging prime alternative to chromogenic approaches to IHC as it has the ability to generate highresolution images for protein localization studies and also the capacity to quantitate the fluorescent signal. Immunofluorescent methods are extensively used to detect antibodies, particularly for the diagnosis of glomerular disease in frozen sections of renal biopsies. It is also applied to skin biopsies of patients with systemic lupus and vasculitis, to examine the pattern of deposition of immunoglobulins. In addition, technical advances in microscope development and fluorophore have widened the selection of colors to use for both single- and multi-color fluorescence microscopy greater than ever. Immunofluorescence (IF) method is used in the evaluation of cells in suspension, cultured cells, tissue, beads and microarrays for the detection of specific proteins on both fresh and fixed samples. Its practical application in laboratory include: (a) the analysis of antigens in fresh, frozen or fixed tissues, sub-cellular localization of antigens in tissue culture monolayers and observation of bacterial or parasitic specimens, (b) detection and localization of the presence or absence of specific DNA sequences on chromosomes; and, (c) defining the spatial-temporal patterns of gene expression within cells/tissues. Fluorescence and phosphorescence are both types of luminescence. When molecules with luminescent properties absorb light, they emit light of a different wavelength. In the immunofluorescence method, antibodies are chemically conjugated to fluorescent dyes such as fluorescein isothiocyanate or tetramethyl rhodamine isothiocyanate. These labeled antibodies bind (directly or indirectly) to the antigen of interest which allows for antigen detection through fluorescence techniques. The fluorescence can then be quantified using a flow cytometer, array scanner or automated imaging instrument, or visualized using fluorescence or confocal microscopy. Successful immunofluorescent techniques depend on adequate preservation of substrate antigens, adequacy of antibody conjugate, careful staining and incubation procedures, and quality of the fluorescence microscope. Direct immunofluorescence technique for solid tissue biopsies This is usually performed on thin (2 to 5 µm) cryostat sections of fresh unfixed material, mounted on slides that have been previously coated with gelatin adhesive or poly-L-lysine (supplied by Sigma) at 1:10 dilution. In this technique, the tissue is reacted directly with a fluorescein-conjugated antibody specific for the material being sought within the tissue. Solutions: Tris-Buffered Saline Wash (0.005M TBS) Distilled water 1 liter Sodium chloride 8 gm TRIS (hydroxymethyl methylamine) 0.6 gm 1M HCl 4.4 ml If necessary, adjust final pH to 7.6 with either 1 M HCl or 0.2M Tris solution. Substrate: DAB (Diaminobenzidine tetrahydrochloride) DAB 5 mg Tris-HCl buffer (pH 7.6) 10 ml Horse radish peroxidase 0.1 ml (Freshly prepared and added just before use.) Method: 1. Bring sections to Tris-buffered saline (TBS), drain off, and incubate in non-immune serum. 2. Drain off and wipe around section. 3. Incubate in optimally diluted peroxidase-labeled primary antibody for 1-15 hours (traditional direct method) at ambient temperature or 4°C; or in EPOS peroxidase pre-diluted antibody (DAKO) for 1-2 hours at ambient temperature (enhanced polymer one-step method). 4. Gently wash in TBS. 5. Incubate in freshly prepared DAB solution at room temperature until a dark brown reaction product is obtained, usually after 5 to 10 minutes. The reaction end-product resists alcohol dehydration and clearing in xylene. 6. Rinse in TBS and wash in running water. 7. Dehydrate through 95% ethanol for 1 minute, and then 100% ethanol 2 times for 3 minutes each time. 8. Clear in xylene 2 times for 5 minutes each time. 9. Coverslip. Results: Apple-green fluorescence when fluorescein is used as fluoro-chrome; Orange-red fluorescence with rhodamine conjugates Fig. 22-5. Fluorescein-conjugated antibody against cytoplasmic immunoglobulin in a patient with lymphocytic lymphoma and macroglobulinemia Notes: 1. The slides may be stored at 4°C for one year, but may show decreased fluorescent staining. 2. Avoid direct sunlight on the slides at all times. 3. Cover slip should not be moved or maneuver when mounting, to prevent distortion of the tissue. 4. The tissue sections must be kept moist at all times to prevent artefactual staining. 5. Conjugates prepared from poor quality antibody tend to produce inferior results, often with weak positive results against high levels of background staining. Indirect immunofluorescence technique The indirect immunofluorescence technique is mainly used for the detection of autoantibodies in the patient's serum, including the anti-nuclear antibody (ANA), anti-mitochondrial antibody (AMA), and liver-kidney microsomal antibody. Frozen Section Immunofluorescence Immunocytochemistry can also be employed to identify antigens in fresh frozen sections. Frozen section immunofluorescence is a relatively simple, rapid and sensitive technique that is easily reproducible, particularly among histopathologists who are experienced with fluorescent antibody techniques. However, immunofluorescent labeling requires considerable skill, is not permanent, and often fades within days after the sections have been immunostained. It also requires the use of a costly fluorescence microscope, which can be a major drawback. It is always advisable to also process part of the biopsy for paraffin wax immunohistochemistry in order to visualize and correlate labeling with the morphology of the tissue that is being studied. Cryostat sections give much better antigen preservation than paraffin sections. Additionally, fixative can be used with cryostat sections, so that a different and optimal fixative can be selected for each antigen, all taken from the same block. Fresh tissue should be frozen immediately and rapidly. A 1.0 x 1.0 x 0.3 cm block of fresh tissue can be snap-frozen by immersing it directly in liquid nitrogen, although a mixture of isopentane and liquid nitrogen will result in a more uniform freezing of tissue and better preservation of histomorphology. OCT can be used as a supporting media to facilitate preparation of good quality frozen sections. However, prolonged storage of OCT-embedded frozen tissue will cause gradual loss of cellular antigens, while snap-frozen fresh tissue, without supporting media, can be stored at -70°C for long periods of time without appreciable antigen loss. Acetone is generally used as fixative to preserve the antigen, to destroy harmful infective agents, and to allow a wide range of primary antibodies to be employed without destroying many of the epitopes. Sections are fixed in absolute acetone at room temperature for 30 minutes, and air-dried for a few minutes prior to immunostaining. Cell surface antigens are best preserved in sections fixed briefly in cold acetone (5 minutes at 4°C). Good results are also obtained in frozen sections fixed for a few minutes in ethanol, formalin and picric acid paraformaldehyde. Between each step of the staining technique, sections require several brief washing with Tris Buffered Saline (TBS) to prevent one reagent from contaminating another. Excess buffer is then drained, and the area around the section is wiped dry. Thin sections and extended drying period prevent the artifacts often seen in frozen-section immunostains of lymphoid tissues fixed in acetone. Extending the drying period to 48 hours will usually result in improved morphology. Slide Preparation of Frozen Sections 1. Snap-freeze fresh tissues in liquid nitrogen or isopentane pre-cooled in liquid nitrogen, embedded in OCT compound in cryomolds. 2. Store frozen blocks at -80oC. 3. Cut 4-8 m thick cryostat sections. 4. Mount cryostat sections on either super-frost plus slides or gelatin coated slides. 5. Store slides at – 80oC. 6. Prior to staining, warm slides at room temperature for 30 minutes and fix in ice cold acetone for 5 minutes. Air dry for 30 minutes. 7. Wash in PBS. IN-SITU HYBRIDIZATION In-situ hybridization shares some similarities with the antigen-antibody reaction that forms the basis for immunohistochemistry. However, it is based on the specificity of the interaction of a probe with the target nucleic acid, rather than the target protein or immunogen. As with immunohistochemistry, optimal results for in-situ hybridization will be achieved only with carefully fixed and processed tissue samples. Formalin fixed paraffin-embedded material appears to be the best choice in a diagnostic setting. Pre-treatment digestion with protease enzyme is required for all cross linked samples to remove proteins and make the target more accessible to the probe. Because of unavoidable variations in tissue fixation and processing, the use of an endogenous positive control probe is absolutely essential. In an aqueous environment, the thermodynamically stable conformation of a nucleic acid is that of a double-stranded helix. A double-stranded molecule may be separated or denatured into two single strands that disrupt the stabilizing hydrogen bond between complementary bases, i.e., adenine pairs with thymine (or uracil) and cytosine with guanine. Heat and formamide, which both break hydrogen bonds, are the commonly used denaturants. When complementary strands from two different sources are mixed and the denaturants are removed, some of the double-stranded structures will be composed of one strand from each source, forming molecules known as "hybrids". In a hybridization assay, the two sources are the target (sample) and the probe nucleic acids. A probe is simply a known fragment of nucleic acid with a label that can be detected in some fashion. It forms a hybrid molecule with a sample that contains nucleic acids complementary to its sequence. The process of searching a sample for specific nucleic acid sequences is termed "hybridization reaction". Majority of the probes now available are produced either by recombinant nucleic acid technology or through chemical synthesis. Cloned probes consist of a known segment of DNA inserted into a plasmid vector that is propagated by growth in bacterium, resulting in a double-stranded DNA probe which must be denatured before use. Other plasmid vectors contain RNA promoter regions that permit generation of single-strand RNA probes, RNA probes require careful handling and storage to prevent degradation. RNA is much more unstable than DNA, and enzymes that digest RNA (known as RNase) are virtually present everywhere. The use of RNA probes therefore dictate use of sterile technique and preparation of reagents and glassware to remove RNase. All hybridization assays require the probe and the sample nucleic acid to be mixed under conditions that will allow complementary base-pairing as well as a method to detect that hybridization has occurred. The general steps of insitu hybridization are basically similar to the steps followed for immunohistochemistry. Detection of radio-labeled probes is usually achieved with autoradiography. Detection of affinity-labeled probes is achieved with methods similar to those previously discussed for immunohistochemistry. Non-isotopic labeling has been initially achieved through the production of biotin-labeled analogue of deoxyuridine triphosphate. Biotin itself cannot generate signals, so that polynucleotides with biotin incorporated into their structure are detected indirectly through high-affinity interaction with avidin or streptavidin chemically linked or complexed to a colorimetric enzyme or fluorescence tags. Alkaline phosphatase systems with tartrazine substrates are reported to yield good results. In most applications, the amount of antigen greatly exceeds the amount of nucleic acid target in tissues, so that low background is essential for optimal results. Fig. 22- 6. In-Situ Hybridization Although numerous well-characterized primary antibodies for immunohistochemistry are now readily available through commercial sources, nucleic acid probes are only beginning to be developed. The lack of commercial reagents is one of the most significant factors limiting the diagnostic application of in-situ hybridization in many laboratories. REFERENCES Adams JC. (1992) Biotin amplification of biotin and horseradish peroxidase signals in histochemical stains. J Histochemistry and Cytochemistry 40: 1457. Battifora H. (1991): Assessment of antigen damage in immunohistochemistry. American Journal of Clinical Pathology 96: 669. Baker JR. (1970) Principles of Biological Microtechnique. Methuen, London. Boenisch, T. (2001) Dako Handbook on lmmunochemical Staining Methods. 3rd ed. DakoCytomation, Carpinteria, California. Bullock GR, Petrusz P, eds. (1982) Techniques in Immunocytochemistry. Academic Press, London, Vol 1. Chan JKC. (2000) Advances in immunohistochemistry. Impact on surgical pathology practice. Sem. Diagn. Pathol. 17(3): 17–77. Chaubert P, Bertholet MM, Correvon M, Laurini S, Bosman FT. (1997) Simultaneous double immunoenzymatic labeling: a new procedure for the histopathologic routine. Mod Path. 10: 585-591. Cordel JL, Falini B, Erber WN, et al. (1984) lmmunoenzymatic labeling of monoclonal antibodies using immune complexes of alkaline phosphatase and monoclonal anti-alkaline phosphatase (APAAP complexes). Journal of Histochemistry and Cytochemistry 32: 219. Elias JM. (1990) Immunohistopathology: A Practical Approach to Diagnosis. Chicago, ASCP. Elias JM, Gown AM, Nakamura RM, et al. (1989): Quality control in immunohistochemistry: Report of a workshop sponsored by the Biological Stain Commission. American Journal of Clinical Pathology 92: 836. Eng LF, Shiubra LA, et al. (eds). (1988) Glial fibrillary acidic protein: A review of structure, function and clinical application: In: Neuron and Glial Proteins: Structure, Function and Clinical Application. San Academic Press, Diego, CA. Fox CH, Johnson FB, et al. (1985): Formaldehyde fixation. Journal of Histochemistry and Cytochemistry 33: 845. Giorno R. (1984) Diagnostic Immunology 2: 151. Guestdon JL, Ternyck T, Avrameas S. (1979) The use of avidin-biotin interaction in immunoenzymatic techniques. Journal of Histochemistry and Cytochemistry 27: 1131. Hsu SM. (1988) The use of monoclonal antibodies and immunohistochemical techniques in lymphomas. Review and outlook. Hematology Pathology 2: 183. Hsu SM, Raine L, Fanger H. (1981) Use of avidin-biotin-peroxidase complex (ABC) in immunoperoxidase techniques: A comparison between ABC and unlabeled antibody (PAP) procedures. Journal of Histochemistry and Cytochemistry 29: 577. Kok LP, Boon ME. Physics of microwave technology in histochemistry. Histochemistry J 22: 381. Larsson L. (1988) Immunohistochemistry: Theory and Practice. Boca Raton, Florida, CRC. Larsson L. (1993) Tissue preparation methods for light microscopic immunohistochemistry. Applied Immunohistochemistry 1: 2. Larsson LI. (1988) In: Larsson LI. Immunocytochemistry: Theory and Practice. Boca Raton: CRC Press, 147. Leong AS, Milios JI, Duncis CG. (1988) Antigen preservation in microwave irradiated tissues: A comparison with formaldehyde fixation. Journal of Pathology 156: 275. Lillie RD. (1965) Histopathologic Technic and Practical Histochemistry, 3rd ed., McGraw Hill, New York. Login GR, Schnitt SJ, Dvorak AM. (1987) Rapid microwave fixation of human tissues for light microscopic immunoperoxidase identification of diagnostically useful antigens. Laboratory Investigation 57: 585. McGadey J. (1970) A tetrazolium method for non-specific alkaline phosphatase. Histochemie 23: 180. Mepham BL. (1982) Influence of fixatives on the immunoreactivity of paraffin sections. Histochemistry Journal 14: 731. Moll R, Franke WW et al. (1982) The catalog of human cytokeratins: Patterns of expression in normal epithelia, tumors and cultured cells. Cell 31: 11. Nadji M, Ganjei P. (1990) American Journal of Clinical Pathology, 94: 470. Nakane PK, Pierce GB. Jr (1966) Enzyme-labeled antibodies: preparation and application for the localization of antigens. Journal of Histochemistry and Cytochemistry 14: 929. Nakane PK, Pierce GBJ. (1967) Enzyme-labeled antibodies for the light and electron microscopic localization of tissue antigens. Journal of Cell Biology 33: 308. Okoye J, Natuanya IN. (2015) Immunohistochemistry: A Revolutionary Technique in Laboratory Medicine. Clinical Medicine and Diagnostics. 5(4): 60-69. Polak JM, Van Noorden S. (eds). (1986) Immunocytochemistry: Modern Methods and Applications. Bristol: Wright. Ponder BA, Wilkinson MM. (1991) Journal of Histochemistry and Cytochemistry, 29: 981, Ramos-Vara JA, Miller MA. (2014) When tissue antigens and antibodies get along: the technical aspects of Immunohistochemistry. Vet. Pathol. 51: 42-87. Reimer HM, Wick MR. In: Wick MR, Siegal GP, eds. Monoclonal Antibodies in Diagnostic Immunohistochemistry. New York: Marcel Decker, l. Shabnam J, Ira JB. (2004) Beyond Hematoxylin and Eosin. The Role of Immunohistochemistry in Surgical Pathology. Cancer Invest. 22 (3): 445–465. Shi SR, Key ME, Kalra KL. (1991): Antigen retrieval in formalin-fixed, paraffin embedded tissues: An enhancement method for immunohistochemical staining based on microwave oven heating of tissue sections. Journal of Histochemistry and Cytochemistry 39: 741. Shi SR, Cote RJ, Taylor CR. (1997) Antigen retrieval immunohistochemistry: past, present, and future. J Histochem Cytochem 45:327–343. Sternberger LA, Hardy PHJ et al. (1970) The unlabeled antibody enzyme method of immunohistochemistry: Preparation and properties of soluble antigen-antibody complex (horseradish peroxidase/anti-horseradish peroxidase) and its use in identification of spirochetes. Journal of Histochemistry and Cytochemistry 18: 315. Steward MW, Steensgaard J. (1983) Antibody Affinity: Thermodynamic Aspects and Biological Significance. Boca Raton: CRC Press. Swanson PE. (1988): Foundations of immunohistochemistry: A practical review. American Journal of Clinical Pathology 90: 333. Taylor CR, Cote RJ. (1994) Immunomicroscopy: A Diagnostic Too/for the Surgical Pathologist, 2nd ed. Philadelphia, WB Saunders. Taylor CR, Shi SR, Cote RJ. (1996) Antigen retrieval for immunohistochemistry: Status and need for greater standardization. Applied Immunohistochemistry 4: 144. Van der Loos CM. (2008) Multiple immunoenzyme staining: methods and visualizations for the observation with spectral imaging. J. Histochem. Cytochem. 56:313-328. Protocol for the Preparation and Fluorescent IHC Staining of Paraffin-embedded Tissue Sections https://www.rndsystems.com/resources/protocols/protocol-preparation-and-fluorescent-ihc-stainingparaffin-embedded-tissue Protocol for the Preparation and Fluorescent IHC Staining of Frozen Tissue Sections https://www.rndsystems.com/resources/protocols/protocol-preparation-and-fluorescent-ihc-stainingfrozen-tissue-sections Protocol for the Preparation and Chromogenic IHC Staining of Paraffin-embedded Tissue Sections https://www.rndsystems.com/resources/protocols/protocol-preparation-and-chromogenic-ihcstaining-paraffin-embedded-tissue Protocol for the Preparation and Chromogenic IHC Staining of Frozen Tissue Sections https://www.rndsystems.com/resources/protocols/protocol-preparation-and-chromogenic-ihcstaining-frozen-tissue-sections Blocking of Unwanted Non-specific Staining http://www.ihcworld.com/_protocols/general_IHC/ihc_blocking.htm https://www.rndsystems.com/resources/protocols/preventing-non-specific-staining http://www.dako.com/08002_03aug09_ihc_guidebook_5th_edition_chapter_17.pdf http://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learningcenter/protein-biology-resource-library/pierce-protein-methods/overview-immunohistochemistry.html Immunoenzyme Staining http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2326109/ Immunoenzyme (HRP) Method http://link.springer.com/article/10.1007/BF02889950 http://link.springer.com/article/10.1007/BF00679982#page-1 http://jhc.sagepub.com/content/27/4/832.short http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2326109/ http://www.ihcworld.com/_protocols/general_IHC/immunoenzyme_pod.htm http://www.biotechniques.com/multimedia/archive/00074/CRI-FP-Microscopy_74545a.pdf Immunoenzyme (AP) Method http://www.ihcworld.com/_protocols/general_IHC/immunoenzyme_ap.htm http://www.ncbi.nlm.nih.gov/pubmed/6198355 http://www.ncbi.nlm.nih.gov/pubmed/2416713 http://link.springer.com/article/10.1007%2FBF01002537#page-1 Double Immunohistochemistry Staining Protocol http://www.biotechniques.com/multimedia/archive/00074/CRI-FP-Microscopy_74545a.pdf http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3347652/ http://www.dako.com/08002_03aug09_ihc_guidebook_5th_edition_chapter_15.pdf. http://www.ihcworld.com/_protocols/general_IHC/double_ihc.htm http://www.abcam.com/kits/enzymatic-double-staining-ihc-kits http://www.abcam.com/protocols/immunocytochemistry-immunofluorescence-protocol Immunohistochemistry Double Staining Method http://jhc.sagepub.com/content/30/10/1079.short http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1877425/pdf/amjpathol00113-0101.pdf http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1880629/pdf/amjpathol00130-0094.pdf https://www.kpl.com/docs/techdocs/HISTODS.PDF Chromogenic IHC Staining https://www.rndsystems.com/resources/protocols/detection-visualization-antibody-binding http://www.nature.com/labinvest/journal/v95/n4/full/labinvest20152a.html http://www.sciencedirect.com/science/article/pii/S1046202314002837 http://www.nature.com/nbt/journal/v24/n8/full/nbt0806-914.html http://www.biositehisto.com/services-and-quality/immunohistochemistry/ Chromogenic IHC Staining of Paraffin-Embedded Tissue Sections http://www.biotechniques.com/multimedia/archive/00074/CRI-FP-Microscopy_74545a.pdf https://www.rndsystems.com/resources/protocols/protocol-preparation-and-chromogenic-ihc-stainingparaffin-embedded-tissue http://www.nature.com/modpathol/journal/v18/n10/full/3800417a.html/ajp.amjpathol.org/article/S00029440 (10)64785-2/fulltext http://dspace.bibliotecainnsz.org/bitstream/handle/123456789/13417/1054G.pdf?sequence=1 https://www.rndsystems.com/resources/protocols/graphic-protocol-preparation-and-chromogenic-ihcstaining-paraffin-embedded-tissue-sections https://www.rndsystems.com/resources/protocols/protocol-preparation-and-fluorescent-ihc-stainingparaffin-embedded-tissue Chromogenic IHC Staining of Frozen Tissue Sections https://www.rndsystems.com/resources/protocols/protocol-preparation-and-fluorescent-ihc-stainingfrozen-tissue-sections https://www.rndsystems.com/resources/protocols/graphic-protocol-preparation-and-chromogenic-ihcstaining-frozen-tissue-sections http://www.novusbio.com/support/support-by-application/immunohistochemistry-frozen/protocol.html https://www.rndsystems.com/resources/protocols/protocol-preparation-and-chromogenic-ihc-stainingfrozen-tissue-sections Immunofluorescence http://www.dako.com/08002_03aug09_ihc_guidebook_5th_edition_chapter_10.pdf Fluorescent IHC Staining of Paraffin-Embedded Tissue Sections https://www.rndsystems.com/resources/protocols/graphic-protocol-preparation-and-fluorescent-ihcstaining-paraffin-embedded https://www.jove.com/video/5064/immunohistochemistry-protocol-for-paraffin-embedded-tissuesections http://www.abcam.com/ps/pdf/protocols/ihc_p.pdf Fluorescent IHC Staining of Frozen Tissue Section https://www.rndsystems.com/resources/protocols/graphic-protocol-preparation-and-fluorescent-ihcstaining-frozen-tissue-sections http://njms.rutgers.edu/research/gause/FStaining_Protocol.pdf http://www.sciencegateway.org/protocols/pdf/ihc_icc_protocol_guide.pdf http://www.cellsignal.com/contents/resources-protocols/immunohistochemistry-protocol-(frozen)/ihcfrozen Heat-Induced Epitope Retrieval (HIER) http://www.leicabiosystems.com/pathologyleaders/technical-brief-of-heat-induced-epitope-retrieval/ http://www.ihcworld.com/_protocols/epitope_retrieval/overview.htm https://www.rndsystems.com/resources/protocols/protocol-heat-induced-epitope-retrieval-hier http://info.ebioscience.com/bid/101985/IHC-Antigen-Retrieval-What-is-it-and-when-should-you-use-it CHAPTER 23 PIGMENTS AND MINERALS Abnormal insoluble yellow, brown or black pigment deposits that can be seen without staining, are frequently encountered in tissues submitted for histologic processing. Pigmentation is the process by which substances that absorb visible light and produce color are deposited in the body in normal or abnormal situations. Pigments can occur in normal or in pathological conditions and can be classified into three major categories: endogenous, exogenous and artefacts of fixation. 1. Endogenous pigments are produced within the tissue to serve a physiological function, or may be by-products of normal metabolism. They are further subdivided into hematogenous or blood-derived pigments (hemosiderin, hemoglobin, bile pigment), nonhematogenous (such as melanin, lipofuscin and chromaffin), and endogenous minerals (such as iron, calcium and copper). Endogenous pigments become pathologic when they are deposited in excessive quantity or found in abnormal locations. 2. Exogenous pigments- Exogenous pigments consist of foreign materials, usually minerals introduced to the body thru air, food, medication and injections. Examples of exogenous pigments are tattoos, asbestos, carbon, silica, iron and silver. Carbon is the most common exogenous pigment, appearing as jet black pigments in lung sections and bronchial glands of chronic smokers. Iron may be present as an endogenous pigment in the liver in case of iron overload, or may be an exogenous pigment in the case of shrapnel wound. 3. Artifact pigments – usually lie on top of tissue instead of within the cell. They are produced in tissues during processing and most commonly result from fixation. Formalin pigment occurs when tissue is fixed in acidic formaldehyde solutions. ENDOGENOUS PIGMENTS Hematogenous pigments are naturally formed within the tissues, usually by hemoglobin breakdown caused by excessive blood destruction due to bacteria, parasites and poisons. 1. Hemoglobin - is the oxygen-containing conjugated protein found normally in red blood cells and is responsible for transporting oxygen from lungs to other parts of the body. It is the only hematogenous pigment that is present in normal tissue, i.e., the red blood cell. It consists of a colorless protein component and a pigmented portion containing iron. Hemoglobin stains vividly with acid (anionic dyes) such as eosin after formalin fixation, but is poorly stained after "Susa" fixation. Red blood cells are stained black by Heidenhain's iron hematoxylin, and blue by Mallory's phosphotungstic acid hematoxylin. 2. Hemosiderin - is the most common hemoglobin derivative and the ironcontaining pigment of hemoglobin. It is seen as yellow to brown granule, and is normally found inside the cells (macrophages) that have phagocytized and degraded hemoglobin. It is made up of free iron in the form of ferric hydroxide bound to protein complexes, and can be identified in organs such as the liver, spleen, and bone marrow. Ferritin, which is not colored, is not the only component of hemosiderin. Glycoproteins are also present, and the deposits give a positive periodic acid Schiff reaction. Hemosiderosis may be attributed to transfusion, excess dietary iron consumption, or the breakdown of red blood cells. Hemosiderin-laden macrophages in the lung are sometimes known as heart failure cells because they are present as a result of failure of the left side of the heart to pump blood from the pulmonary vasculature. Hemosiderin is soluble, may be removed by acids, and maybe demonstrated histochemically by Prussian blue reaction. Hemosiderin-laden macrophages containing ferric ions combined with acid solutions of ferrocyanide will give ferric ferrocyanide, a bright blue pigment known as Prussian blue. It can be removed from tissue section by 10% sulfuric acid. It is insoluble in alkalis and soluble in either 0.4 M aqueous oxalic acid (six hours) or 0.06M sodium dithionite in acetate buffer, pH 4.5 (five minutes). Dilute hydrochloric acid is sufficient to liberate loosely bound ferric iron, such as hemosiderin, from its protein component. 3. Hematoidin - is the iron-free pigment of hemoglobin, found in places where there is poor oxygenation, participating in the formation of bile pigment. Hematoidin is derived from red blood cells and occurs as yellowish or greenish granules or masses. It is chemically the same as bilirubin and can be demonstrated by Hall’s method. It occurs in pathological conditions such as infarcts and in areas of hemorrhage and thrombosis, usually appearing within macrophages as yellow brown granules. Hematoidin can also be found in old hemorrhagic areas in the brain. 4. Hematin - is hemoglobin minus the globin molecule, found in old blood clots, but may be encountered in malaria, pernicious anemia, and toxic hemolysis. 5. Hemozoin - is the black granule formed by malarial parasites living in red blood cells, and may be removed by alcoholic picric acid method. Hemozoin (malaria pigment) may be seen in the liver, spleen, bone marrow, lymph nodes, and brain capillaries. It is similar to formalin pigment, but may be differentiated from formalin pigment by its location and distribution. This pigment can be removed by treating the section with alcoholic picric acid or with 10% ammonium hydroxide in 70% alcohol for 5 to 15 minutes. Fig. 23-1. Brownish-black hemozoin granules of malarial parasite in intravascular red blood cells Prussian blue stain is the classic method for demonstrating iron in tissues. The Prussian blue stain is not a true special staining technique but rather, a histochemical reaction used to detect the presence of iron in tissues. It is an extremely sensitive test, and can even detect single granules of iron in cells. This histochemical method is based on the unmasking of ferric iron by dilute hydrochloric acid which is a component of the acid ferrocyanide solution. Tissue sections are treated with hydrochloric acid to denature the binding proteins of the hemosiderin molecule, and thereby release ferric (3+) ions. Potassium ferrocyanide is then introduced. The ferric ions combine with this solution, resulting in the formation of ferric ferrocyanide, an insoluble bright blue pigment – otherwise known as Prussian blue. The optimal pH for the Prussian blue reaction appears to be 1.5. Prussian blue is insoluble in acids but soluble in alkalis. The commonly used red counterstains are applied from acid solutions; neutral red and the aluminum complex of nuclear fast red both contrast well with Prussian blue. Eosin can be used if contrast between nuclei, cytoplasm and collagen is not needed. Lillie’s Method for Ferric and Ferrous Iron (Lillie 1976) Sections: Paraffin 6 microns. Solutions: Potassium Ferrocyanide Solution: Potassium Ferrocyanide 0.4 gm Hydrochloric Acid 40 ml Prepare fresh, just before use. Potassium Ferricyanide Solution: Potassium Ferricyanide 0.4 gm Hydrochloric Acid 40 ml. Prepare fresh, just before use. Method: 1. Deparaffinize and hydrate to distilled water. 2. For Ferric Iron, place in Potassium Ferrocyanide Solution for 1 hour. For Ferrous Iron, place in Potassium Ferricyanide Solution for 1 hour. 3. Wash well in 1% Acetic Acid. 4. Stain for 10 minutes in Basic Fuchsin Solution. 5. Rinse in distilled water. (For critical work, omit this step.) 6. Dehydrate in 95% alcohol, absolute alcohol and clear in xylene two changes each. 7. Mount with Permount. Results: Ferric iron Dark Prussian blue Ferrous iron Dark Turnbull’s blue Background light Red Perl's Prussian Blue Method for Hemosiderin (ferric iron) (Perls 1867; Suvarna 2013) Fixation: Neutral Formalin or other fixatives except acid fixative and potassium dichromate Sections: The method works well on all types of sections. Solution: Acid ferrocyanide Solution: 1% aqueous potassium ferrocyanide 20 ml 2% aqueous hydrochloric acid 20 ml Preferably freshly prepared just before use. Method: 1. Sections to water. 2. Treat sections with freshly prepared acid ferrocyanide solution for 10 to 30 minutes. 3. Wash in distilled water. 4. Counterstain the nuclei with eosin, 0.5% aqueous neutral red, or 0.1% nuclear fast red. 5. Wash rapidly in distilled water. 6. Dehydrate, clear and mount in neutral mounting medium. Results: Hemosiderin and ferric salts stain deep blue. Other pigments retain their n atural color. Tissues and nuclei stain red (according to counterstain). Notes: 1. Depending on the amount of ferric iron present, it may be necessary to vary the staining times. 2. Sharpest staining is given by a modified technique, placing sections in 10% potassium ferrocyanide for 10 minutes, then adding 1/2 volume of 10% HCI, and leaving the sections in the mixture for 20- 30 minutes. The result is improved because potassium ferrocyanide diffuses more slowly than HCI, and if mixed with the latter offhand, may be late for reaction with ferric ions. This modification gives the ferrocyanide time to diffuse in the tissue before ferric salts are liberated. 3. It is essential to have a positive control with all test sections. 4. Freshly formed deposits of iron may be dissolved in the hydrochloric acid. Gomori's Prussian blue Stain for Iron (Luna 1968) Fixation: Alcohol or l 0% formalin Sections: Paraffin sections cut at 6 microns Solution: Nuclear Fast Red Dissolve 0.1 gm. nuclear fast red in 100 cc. of 5% aluminum sulfate with aid of heat. Cool and filter. Add a grain of thymol as preservative. Keep well at room temperature. Method: 1. Immerse slides in equal parts of 20% hydrochloric acid and 10% potassium ferrocyanide mixed immediately before use in chemically cleaned glassware for 20 minutes. 2. Wash thoroughly in distilled water. Do not use tap water. 3. Counterstain in nuclear fast red for 2 minutes. 4. Rinse in distilled water. 5. Dehydrate, clear and mount. Results: Iron pigments bright blue Nuclei red Cytoplasm pink to rose Turnbull's Blue Reaction for Ferrous Iron (Hemosiderin) Turnbull's Blue method is rarely used in routine histology since ferrous iron is less commonly found than ferric iron. The reaction depends upon the union of ferrous Iron with potassium ferricyanide to form a blue precipitate of complex ferrous ferricyanide. Ferrous salts are stained blue while other pigments remain unstained. Turnbull's Blue for Ferrous Iron (Culling 1974) The method is very similar to Perls' Prussian blue, but uses potassium ferricyanide instead of ferrocyanide. The ferrous iron reacts with the potassium ferricyanide to form ferrous ferricyanide. This is an insoluble, blue compound known as Turnbull's blue. The intensity of the color gives some indication as to amount, but it is qualitative only. Fixation: Neutral buffered formalin Sections: 5µ paraffin sections of fixed tissue are suitable. Avoid iron containing materials and jars while fixing as these may contaminate the tissue. Acid containing fixatives may remove some of the iron deposits, but apart from that most are satisfactory. Solutions Neutral red Stock solution A Potassium ferricyanide 20 gm Distilled water 100 ml Stock solution B Hydrochloric acid, conc. 1 ml Distilled water 100 ml Working solution Stock solution A 1 volume Stock solution B 1 volume Method 1. Bring sections to distilled water with xylene and ethanol. 2. Place into the working solution for 15 minutes. 3. Rinse with distilled water. 4. Wash well with tap water. 5. Stain with neutral red for one minute. 6. Rinse well with tap water. 7. Dehydrate with ethanol. 8. Clear with xylene. Results: Ferrous iron – blue Nuclei – red Notes: 1. The working solution should be made immediately before use. 2. Avoid washing with tap water before placing into the working solution, as rust in the water or tap fixtures could cause false positive staining. 3. Wash well at step 3, as traces of iron will form a granular red deposit with neutral red. Fig. 23 - 2 .Prussian Blue Stain for Iron Leuco patent blue V Stain for Hemoglobin (Dunn and Thompson 1946; Suvarna 2013) Fixation: Formalin Solutions: Stock Solution: 1% aqueous patent blue V (CI 42045) 25 ml Powdered zinc 2.5 gm Glacial acetic acid 0.5 ml Mix well on a magnetic stirrer. The solution will become pale greenblue. Filter and store in a refrigerator at 3-6oC. The solution is stable for about 1 week. Working Solution: Stock solution 10 ml Glacial acetic acid 2 ml 3% hydrogen peroxide 1 ml Prepare immediately before use. Method: 1. Take test and control sections to distilled water. 2. Stain in patent blue solution for 5 minutes at room temperature. 3. Rinse in distilled water. 4. Lightly counterstain in 0.5% aqueous neutral red or 0.1% aqueous nuclear fast red for 1 minute. 5. Rinse in distilled water. 6. Dehydrate, clear and mount I synthetic resin. Results: Hemoglobin peroxidase (RBCs and neutrophils) dark blue Nuclei red Note: 1. Fixation in excess of 36 hours may give rise to unreliable results. Bile Pigments and Hematoidin Removal of iron from the heme of hemoglobin due to degradation of red blood cells, results in the formation of biliverdin, a green compound that is transported to the liver, where is it further reduced to bilirubin that is orange in color. Bilirubin is a bile pigment that is excreted by the hepatocytes of the liver, removed from circulation in the blood and secreted into the duodenum as a component of bile. When bilirubin is not excreted by hepatocytes, jaundice or yellowing of the skin can occur. Bile pigments contain both conjugated and unconjugated bilirubin, biliverdin and hematoidin, all of which are chemically distinct and show different physical properties. In H&E stained section of the liver, bile if present is seen as small yellow-brown globules, first in the liver cells or hepatocytes, and later in the bile canaliculi. Biliverdin and bilirubin are considered bile pigments. Bile pigments can vary in color from yellowish-brown to green. Jaundice, a yellow discoloration of the skin, is caused by excess bile pigment in patients with liver failure, hemolytic anemia, or when there is an obstruction in the flow of bile from the liver to bilirubin. In the liver, bile pigments appear in hepatocytes as yellowbrown globules which is sometimes difficult to distinguish from lipofuscins that are also commonly seen within the cells. Both pigments appear yellow brown on H&E stained paraffin sections (the green color of biliverdin is often masked by eosin), and can be positive with Schmorl's ferric ferricyanide reduction test. Lipofuscin is autofluorescent while bile pigments are not. The most commonly used method for demonstration of bile pigments is Hall’s modified Fouchet technique in which the pigment is converted to the green color of biliverdin and blue cholecyanin by the oxidative reaction of the ferric chloride in the presence of trichloroacetic acid (Fouchet’s reagent). The tissue section is then counterstained with Van Gieson’s solution. Only bile and bile pigments in the liver are detected using this special staining technique. It is applied to paraffin sections of formaldehyde-fixed tissue. The Gmelin’s technique is used to demonstrate bile pigments in other locations outside the liver. Small amounts of bile pigments are lost during routine tissue processing and staining because of their slight solubility in organic solvents. Large deposits of bile pigments, however, can resist these processing procedures. It is recommended that two control sections be processed with the test section. Both sections should be oxidized with Fouchet’s reagent, but only one should be counterstained with Van Gieson’s. The second section should not be counterstained. A more reliable result can be obtained if fresh Fouchet’s reagent is prepared on the day it is to be used. Modified Fouchet's Technique for Liver Bile Pigments (Hall 1960) Fixation: Any fixative is suitable. Sections: Any section is suitable. Solutions: Fouchet's solution 25% aqueous trichloroacetic acid 36 ml 10% aqueous ferric chloride 4 ml Freshly prepared before use. Van Gieson’s stain Dissolve 100 mg . of acid fuchsin (Cl 42685) in l 00 ml. of saturated aqueous picric acid. Method: l. Take test and control sections to distilled water. 2. Treat with the freshly prepared Fouchet's solution for l 0 minutes. 3. Wash well in running tap water for 1 minute. 4. Rinse in distilled water. 5. Counterstain with van Gieson’s solution for 2 m inutes. 6. Dehydrate, clear and mount in synthetic resin Results: Bile pigments emerald to blue Muscle green yellow Collagen red Notes: 1. Two control sections should be stained with the test section: one stained with Fouchet's reagent and van Gieson, and one with Fouchet's reagent only. 2. Hematoidin is not likely to show any color change with this method. This pigment can be shown using the Gmelin or Stein techniques. Gmelin Technique for Bile and Hematoidin (Suvarna 2013) This method shows an identical result with liver bile, gallbladder bile and hematoidin. Gmelin's Test, if positive, is diagnostic for bile pigments, although the result produced is only temporary. The reaction depends on progressive oxidation of bilirubin to blue-green biliverdin by addition of nitric acid, changing the yellowish brown pigment to blue and purple; then to green color within seconds. The results may be unreliable, and it is advisable to repeat the test at least three times before a negative result is reported. Other oxidizing agents used are ferric salts, iodine and potassium dichromate. Sections: Paraffin, frozen or cryostat Method: 1. Sections to distilled water and mount in distilled water. 2. Place mounted section under the microscope using an objective with reasonable working distance. 3. Place 2-3 drops of concentrated nitric acid to one side of the cover glass and draw under the cover glass by means of a piece of blotting paper on the opposite side. 4. Remove excess solution and observe pigment for color changes. Results: Bile pigments will gradually produce the following spectrum of color change: yellow-green-blue-purple-red Notes: 1. This method is not permanent, thus preventing storage of sections. Schmorl's Ferric Ferricyanide Method for Reducing Substances (Lillie 1954) This technique involves the reduction of ferricyanide to ferrocyanide with the production of Prussian blue in the presence of ferric salts (the Schmorl's reaction). This type of reaction is seen with bile, some lipofuscins, neuroendocrine cell granules and also melanin. Fixation: 10% buffered formalin is best. Sections: Paraffin Solutions: Freshly prepared 0.4% aqueous potassium ferricyanide 4 ml. Freshly prepared 1% aqueous ferric chloride (Or 1% ferric sulfate) 30 ml. Use this solution soon after mixing. Method: 1. Take test and control sections to distilled water. 2. Treat sections with ferric-ferricyanide solution for 5 to l 0 minutes. 3. Wash well in running tap water for several minutes to ensure that all residual ferricyanide is completely removed from the section. 4. Lightly counterstain with 0.5% aqueous neutral red or 0.1% aqueous nuclear fast red for 5 minutes. 5. Dehydrate, clear and mount in synthetic resin. Results: Bile, lipofuscins and melanin dark blue Argentaffin cells, chromaffin dark blue Thyroid colloid dark blue Nuclei red Notes: 1. The time for reaction to take place depends on the substance to be demonstrated. Melanin reacts more quickly than lipofuscin and may require less staining time. This fact should not be taken as a definitive diagnostic pointer but only as a general guideline. 2. Control sections should always match the test sections. Hence, a lipofuscin control should not be used if the test pigment is thought to be melanin. Lipofuscin (hemofuscin) Fig. 23-3. Lipofuscin H & E Stain Lipofuscin is a yellow-brown to reddish-brown pigment that is due to a slow and progressive oxidation of lipids and lipoproteins. Lipofuscin is known as “wear and tear pigment” or “brown atrophy” that is usually associated with aging. It represents the indigestible, lipid containing remnants of autophagic vacuoles formed during the cellular aging or atrophy and is formed in long-lived metabolically active, but not mitotically active, cells. It can be found in hepatocytes, cardiac muscle cells, adrenal cortex, brain, spinal cord, bone marrow, kidney and other organs. Normal lipofuscin contains fatty acids that are closely associated with protein. This association allows most of the pigment to remain in place during passage through the solvents used in paraffin embedding. It can be stained with oil-soluble dyes in frozen sections and with basic fuchsin in paraffin embedded tissue. It is often reacts with a variety of histochemical and staining methods, including stains for lipids, the Schmorl’s ferric-ferricyanide reduction technique, the Fontana Masson silver stain method, Gomori 's aldehyde fuchsin, methyl green, and occasionally with the Periodic Acid Schiff (PAS)method. Some lipofuscin can be stained with Sudan black B and carbol fuchsin in a modified Ziehl-Neelsen stain. Gomori's Aldehyde Fuchsin Technique for Lipofuscin (Gomori 1950) Fixation: Any fixative Sections: Works well on all types of sections Solutions: Acidified potassium permanganate solution (0.25% aqueous potassium permanganate in 0.1% sulfuric acid). 2% aqueous oxalic acid Aldehyde fuchsin Aldehyde Fuchsin: Dissolve 1 gm. pararosanilin (Cl 42500) in 100 ml. aqueous 70% ethanol. Add 1 ml. concentrated hydrochloric acid and 1 ml paraldehyde, shaking mixture thoroughly. Stand for 2 to 3 days at room temperature or preferably longer, near natural light, to allow the solution to blue. Store solution at 4°C. The solution will remain viable for approximately 2 months. Any increase in the background staining will indicate deterioration of the staining solution. Method: 1. Sections to distilled water. 2. Treat with acidified potassium permanganate solution for 5 minutes. 3. Wash well in distilled water and treat for 2 minutes with oxalic acid solution to bleach the section. 4. Wash well in distilled water. 5. Rinse in 70% ethyl alcohol. 6. Stain section in aldehyde fuchsin for 5 minutes. Longer staining times will be needed as the solution ages. 7. Rinse in 70% ethyl alcohol followed by rinsing in three changes of distilled water. 8. Counterstain with 0.1% aqueous tartrazine (Cl 19140) in 0.2% acetic acid for 1 minute. 9. Rinse well in distilled water. 10. Dehydrate, clear and mount in synthetic resin. Results: Lipofuscin purple Background yellow Notes: 1. Paraldehyde should be freshly opened. Acetaldehyde may be used if paraldehyde is not available. 2. Other tissue constituents, such as beta cells of the pancreas and pituitary, elastin, sulfated mucins and neurosecretory granules will also stain with this method. Mallory's Fuchsin Stain for Hemofuscin Pigment (Mallory 1961; Luna 1968) Fixation: Zenker’s, Absolute Alcohol or 10% Buffered Neutral Formalin. Sections: Paraffin @ 6 microns. Method: 1. Deparaffinize and hydrate to distilled water. 2. Stain in Alum Hematoxylin until the nuclei stand out sharply. Wash thoroughly in water. 3. Stain in Basic Fuchsin, 0.5% for 30 minutes. Wash in water. 4. Differentiate in 95% alcohol until hemofuscin granules stand out sharply against a gray background. 5. Dehydrate in absolute alcohol, and then clear in Xylene, two changes each. 6. Mount with Permount. Results: Nuclei blue Hemofuscin red Hemosiderin unstained Melanin Melanin is an autogenous pigment (brown or black), normally found in the skin, eyes and in pigment-bearing neurons within the brainstem, such as the locus ceruleus and the substantia nigra. It is formed by melanocytes when tyrosine is converted to dihydroxyphenylalanine (DOPA) by tyrosinase, and then into melanin, packaged into protein containing granules called melanosomes. It is soluble in strong alkali, and does not react with iron or fat stain. Pathological deposition of melanin occurs in benign lesions such as a nevus or "mole", or in malignant tumors such as melanoma. A high percentage of amelanotic melanomas can be identified with the monoclonal antibodies HMB-45, Melan A, and NSE. The commonly used Fontana-Masson ("melanin stain") method relies upon the melanin granules to reduce ammoniacal silver nitrate (but argentaffin, chromaffin, and some lipochrome pigments also will stain black as well). Schmorl's method uses the reducing properties of melanin to stain granules blue-green. The most specific method of all is an enzyme histochemical method called DOPA-oxidase. It requires frozen sections for best results, but paraffin sections of well-fixed tissues may be used. The stain works because the DOPA substrate is acted upon by DOPA-oxidase in the melanin-producing cells to produce a brownish black deposit. Two methods are commonly used: The MassonFontana silver method and Schmorl’s ferric ferricyanide reaction. Substances, such as melanin, which have the ability to bind and reduce silver without the use of a separate reducing agent are said to be argentaffin, which means possessing the ability to reduce silver without the aid of light or a reducing agent. The Fontana-Masson method is an argentaffin procedure Chromaffin cells, also known as pheochromocytes, are neuro-endocrine cells found mostly in the medulla of the adrenal glands. They release catecholamines: 80% of Epinephrine (Adrenaline) and 20% of Norepinephrine (Noradrenaline) into systemic circulation. They are named as such because they can be visualized by staining with chromium salts. Chromium salts oxidize and polymerize catecholamines to form a brown color, most strongly in the cells secreting noradrenaline. They can be demonstrated by Schmorls' staining solution that contains ferric chloride and potassium ferricyanide. However, because other pigments give a positive reaction with Schmorl’s technique, a melanin bleach procedure with potassium permanganate and oxalic acid should also be done. Melanin is not extracted by acid treatments that remove formalin pigment. They are resistant to fat solvents such as acetone but are soluble, to varying degrees, with hydrogen peroxidase, potassium permanganate and chromic acid. In cases when melanin pigment obscures cellular detail, melanin pigment can be bleached with potassium permanganate and oxalic acid solutions or 12-24 hours. Melanin bleaching can be performed on free floating frozen or paraffin sections. The darker the melanin pigment the longer the bleach will take to decolorize the pigment. Masson-Fontana Method for Melanin (Masson 1928; Lillie 1965) Certain tissue components are argentaffin; that is, they possess the ability to bind silver from a solution and to reduce it to visible metallic silver without the need for a separate reducing agent. A 10% neutral buffered formalin can be used as a fixative. Avoid alcohol because it dissolves argentaffin granules. Melanin has the ability to reduce solutions of ammoniacal silver nitrate to metallic silver. Fixation: Formalin Sections: Standard paraffin sections Solutions: Preparation of Silver Solution: To 20 mL of 10 % silver nitrate add concentrated ammonia drop by drop until the formed precipitate almost dissolves. A faint opalescence is evident when the end point is reached. If too much ammonia is added, 10% silver nitrate can be added drop by drop until the faint opalescence is obtained. To this silver solution add 20 mL of distilled water and filter. Store in a dark bottle. The solution will last for about four weeks in fridge 4oC. 5 % Sodium Thiosulsulfate 1 % Neutral Red Methods: 1. Deparaffinize and hydrate to distilled water. 2. Treat with silver solution a) 45 mins at 56øC to demonstrate melanin b) At room temperature over-night in the dark to demonstrate argentaffin. 3. Wash well in several changes of distilled water. 4. Treat with 5% sodium thiosulfate for 2 minutes. 5. Wash in tap water. 6. Counterstain in 1% neutral red (aqueous) for 3 minutes. 7. Wash in tap water. 8. Dehydrate through graded alcohols to Histoclear. 9. Mount in Safety-mount. Results: Melanin black Argentaffin granules black Nuclei red Notes: 1. Use only thoroughly clean glassware, as the silver solution will react with any residual contaminant left on the glassware. 2. Prolonged exposure to ammoniacal silver solution at 56°C may give rise to a fine deposit over the section. 3. Argentaffin cells in intestinal epithelium, chromaffin granules and lipofuscin may give positive silver reactions. Silver solutions may become explosive (see Metallic Impregnation). 4. In cases where there seems to be confusion regarding the nature of the pigment present in the tissue, melanin may have to be removed during staining without interfering with other pigments, to assess whether the pigment in question is melanin or not. Fig. 23 -4. Masson Fontana Stain for Melanin Schmorl’s Method In Schmorl’s technique, sections are immersed in a solution containing ferric chloride and potassium ferricyanide. Melanin reduces ferric ions (Fe3+) to ferrous ions (Fe2+), and the ferrous iron then combines with ferricyanide. The expected product is ferrous ferricyanide, a blue pigment known as Turnbull’s blue. In fact, the product is the same as Prussian blue, which is formed when ferric ions combine with ferrocyanide ions. Prussian blue is ferric ferrocyanide, occurring in crystals that also contain water molecules and sodium or potassium ions. The color is associated with the occurrence of iron in both oxidation states (+2 and +3) in the same molecule. The final step is application of aluminum-nuclear fast red or a similar counterstain. As with the Masson-Fontana method, this reaction is not melanin-specific and may stain other elements, such as argentaffin, chromaffin cells and some types of lipofuscin. Removal of Melanin Pigments (Bleaching) (Preece 1959) Melanin can be bleached by strong oxidizing agents such as potassium permanganate. Specimen: Standard paraffin sections, formalin fixed Control: H&E without bleaching procedure, and H&E with bleaching procedure for each case Solutions: 0.25% Potassium Permanganate Distilled water 38 ml Stock 5% Potassium Permanganate 2 ml 5% Oxalic Acid Oxalic Acid 25 gm Distilled water 500 ml Methods: 1. Deparaffinize and hydrate to distilled water. 2. Oxidize in permanganate for 30 minutes. 3. Wash with water. 4. Bleach in oxalic acid until white. 5. Proceed staining as desired. Results: Skin melanin is bleached within 30 minutes MINERALS In histology and histopathology, minerals refer to substances detected by forming colored reaction products specific to metal ions or inorganic anions. They serve as catalytic agents in many of the biological reactions in the body, including muscle responses, neuronal signaling, hormone production, digestion and nutrient processing. The most common minerals that can be demonstrated by special staining techniques are calcium, iron and copper. Calcium Deposits on Tissues Calcium is present in hydroxyapatite, the insoluble mineral of bones and teeth. Abnormal deposits of calcium phosphate or carbonate can be associated with necrotic tissue in lesions of atherosclerosis, hyperparathyroidism, nephrocalcinosis, sarcoidosis, tuberculosis, and in some tumors. Calcium phosphate crystals can form in the cartilage of joints in a condition known as chondrocalcinosis or pseudo gout. Acidic fixatives such as Bouin’s fluid have the potential to dissolve calcified deposits and must therefore be avoided. Neutral buffered formaldehyde is a suitable fixative. Calcium salts of phosphates and carbonates in tissues are stained deep purplish blue in routine hematoxylin and eosin. Because calcium oxalate is birefringent, it can be identified easily by polarization. The other calcium salts are not birefringent and will not polarize. There are two histochemical methods that are routinely used to stain calcium. These are alizarin red S and the von Kossa techniques. Alizarin red S is an anionic anthraquinone dye that forms sparingly soluble salts with calcium ions. At pH 4.8 or 6.1, alizarin red S gives an orange color with calcified deposits. The yellow component is attributed to impurities in the dye. If staining is carried out at pH 4.8 or 6.1, the reaction must be monitored microscopically and stopped, usually after one or two minutes, before diffusion artifacts appear, indicating partial dissolving of calcium phosphate or carbonate before precipitation of Ca2+ by the dye. Amino groups of proteins in the tissue also bind the dye and must be removed by differentiation, leaving a pink background stain. The modified technique (method of Puchtler) uses alizarin red S at pH 9 allowing both the sulphonate group on carbon 3 and the ionized hydroxy group on carbon 2 to participate in salt formation with calcium. The impurities do not react at this higher pH, and the resulting calcium salt has a deep red color. An alkaline pH also prevents most of the background staining and obviates the need for differentiation. A disadvantage of staining with any alkaline solution is the risk of sections detaching from the slides. With the stain at pH 9, diffusion does not occur and the slides may, with advantage, be left in the solution for an hour. Calcium deposits are stained orange-red with alizarin red S and are birefringent. When staining for calcium with alizarin red S, slides are taken to 95% alcohol and then placed in staining solution. If the slides are allowed to remain in any of the other solutions, there will be a loss of some or all calcium. The von Kossa technique for demonstrating calcium involves replacement of the anionic part of calcium salts with silver. Silver is made visible following reduction by exposure to bright light. The Von Kossa calcium stain is an indirect method for identifying calcium in tissue. The primary calcium salts in tissue are calcium phosphate and calcium carbonate. In this technique, silver is substituted for calcium and is then reduced to metallic silver with sunlight. The metallic silver marks the location of the calcium in the tissue. This stain is most useful when large amounts are present, as in bone. Fig. 23-5. Microcalcification in oligodendroglioma (brain tumor) Soluble calcium salts (CaCl3, calcium sulfate, calcium lactate) are non-ionized or bound to protein, and may be demonstrated by: a. Gypsum method - which depends upon the formation of Gypsum crystals when sulfuric acid is added to calcium. b. Oxalate method - Insoluble calcium salts (calcium phosphate, calcium carbonate) are soluble in weak acids, and hence should be fixed in a neutral solution. They can be demonstrated thru calcium-dye-lake reactions or by metal substitution. Modified Von-Kossa’s Method for Calcium (Lillie 1965; Carson 1996) Specimen: Standard paraffin section Control: Calcium in tissue. Solutions: 5 % aqueous silver nitrate Silver nitrate 5 gm Distilled water 100 ml 5 % Sodium thiosulfate Sodium thiosulfate 5 gm Distilled water 100 ml 1 % Neutral Fast Red Neutral Fast Red 0.5 gm Aluminum sulfate 25 gm Distilled water 500 ml Dissolve the aluminum sulfate in distilled water and then dissolve the nuclear fast red in this solution using heat. Cool, filter, and add a few grains of thymol as preservative. Method: 1. Deparaffinize and hydrate to distilled water. Rinse well in distilled water. 2. Place in Silver nitrate solution and expose to strong light for 10 to 20 minutes. If the day is overcast longer incubation will be necessary. Check the slides periodically and stop the reaction when the calcium salts are brown-black. 3. Rinse sections in distilled water. 4. Place slides in 5% sodium thiosulfate for 2 to 3 minutes. 5. Wash slides in distilled water. 6. Counterstain in nuclear fast red for 5 minutes. 7. Wash sections well in water. 8. Dehydrate and clear in 2 changes each of 95% alcohol, absolute alcohol, and xylene. 9. Mount with synthetic resin. Results: Mineralized bone Black Osteoid Red Nuclei blue Calcium-dye lake reaction is particularly recommended for staining skeletal system in embryos and fetuses. The most common methods are: Routine Hematoxylin & Eosin methods staining calcium salts deep purplish blue. Sodium alizarin red S method using alizarin red S with dilute ammonium hydroxide; an orange red color develops within 30 seconds to 5 minutes on a faint pink background. Alizarin Red S Method for Calcium (Dahl 1952; Luna 1968) Fixation: 95% ethyl alcohol or I 0% buffered neutral formalin Sections: Paraffin sections at 6 microns 1% Alizarin red S Solution (CI 58005) Alizarin red S 1 gm. Distilled water 100 ml. Ammonium hydroxide (0.1%) 10 ml. Stir dye into the distilled water so that only a few small grains of dye remain undissolved. Add 10 ml. of 0.1% ammonium hydroxide slowly with constant stirring. Resulting pH should be 6.35 - 6.5. Solution is stable for one month. 0.05% fast green FCF (CI 42053) in 0.2% acetic acid Method: 1. Deparaffinize and hydrate to 95% alcohol (drain off excess 95% alcohol). 2. Place in Alizarin Red S solution for 1 to 5 minutes. 3. Remove excess stain with distilled water by quick rinse. 4. Counterstain in fast green solution for 1 minute. 5. Rinse in three changes of distilled water. 6. Dehydrate in 95% alcohol and, absolute alcohol. 7. Clear in two changes of xylene and mount in Permount. Results: Calcium salts intense reddish-orange Background pale green Notes: 1. Staining time is dependent on the amount of calcium present. 2. Calcium deposits are birefringent after staining with Alizarin red S. Metal Substitution Metal substitution is an indirect method of staining calcium whereby silver is substituted for calcium salts found in tissues, forming silver salts of carbonates, phosphates or oxalates, which are then reduced to black metallic silver by light. Urates may also be blackened by this method. To differentiate the salts, a control section should be treated with saturated aqueous lithium carbonate which usually dissolves urates. Copper Copper is an essential nutrient, being a component of cytochromes and many oxidoreductase enzymes. Copper in small amounts is present in the liver and is hardly detectable by standard staining methods, except in third trimester fetal liver. Pathologically, the accumulation of copper is associated with Wilson’s disease. This is a recessively inherited metabolic disorder in which a transporter protein in liver cells fails to move copper into the bile and fails to combine copper with ceruloplasmin, the copper-binding protein of blood plasma. Copper accumulations are seen also in primary biliary cirrhosis and some other liver disorders. The rubeanic acid and rhodanine stains are utilized to detect the cytoplasmic accumulation of copper in the liver. Dithiooxamide (also known as rubeanic acid) gives a stable dark green polymeric product that can be mounted in a resinous medium. The reagent p-dimethylaminobenzidine rhodanine (DMABR) gives a red product that dissolves in organic solvents and therefore requires an aqueous mounting medium. Both require long (overnight) incubation to develop the colors. The sensitivity of the dithiooxamide method can be increased by prolonging the incubation to 72 hours. Lindquist's rhodanine method, considered to be the most sensitive and specific one, is the special staining technique of choice for demonstrating copper. When counterstaining the rhodanine copper stain, Mayer or LillieMayer hematoxylin should be used. Harris hematoxylin can also be used if it is diluted with equal parts distilled water. Care must be taken not to over counterstain because this will "mask" the red stained copper. Lindquist's Modified Rhodanine Technique for Staining Copper (Lindquist 1969; Sheehan 1980) Solutions: Rhodanine Stock Solution 5-p-Dimethylaminobenzidine rhodanine 0.05 gm Absolute ethanol 25 ml Prepare fresh and filter prior to use. Rhodanine Working Solution Rhodanine stock solution 5 ml 2% Sodium acetate trihydrate 45 ml Borax Solution Disodium tetraborate 0.5 gm Distilled water 100 ml Method: 1. Take sections to water. 2. Incubate in the rhodanine working solution for 3 hours at 56°C or overnight in a 37°C oven. 3. Rinse well in several changes of distilled water. 4. Stain in dilute Mayer hematoxylin for 10 minutes. 5. Briefly rinse in distilled water and place immediately in borax solution for l 0 seconds. 6. Rinse well in distilled water. 7. Mount with Apathy's mounting media. Results: Copper and copper associated protein red to orange-red Nuclei blue Bile green Notes: Apathy's media is preferred for mounting to prevent fading of copper in archived material which might happen with other synthetic mountants. Formalin used for demonstrating arsenic in tissues must contain copper acetate. Arsenic in tissues will react with copper acetate to form green cupric acetoarsenate. After cover slipping, fading of the stained copper may occur if the copper concentration within the tissue is low. If the tissue section is overstained with hematoxylin, the copper may be difficult to visualize. Urates and Pyrophosphates Monosodium urate, the crystallized form of uric acid that circulates as a breakdown product of purine (nucleic acid) metabolism, is usually deposited in joints and kidneys of patients with gout. The color of crystalline urate is characteristically yellow but can vary from colorless to brown, depending on the thickness of the crystals. Pathologically, crystallization or increased urate in the blood predisposes a patient to gout, poor kidney function, kidney stones and arthritis. Urate crystals are soluble in aqueous solutions and slightly soluble in weak alcoholic solutions. Therefore, tissues must be fixed in 95% or absolute alcohol to prevent leaching of urates. Sodium urate crystals can be visualized on a hematoxylin & eosin (H&E) stained slide under a polarized light with a red compensator. The urates will demonstrate a negative yellow or blue birefringence, based on the alignment of the urate crystals. A special staining technique, Gomori’s methenamine-silver method, can also be used to identify urate crystals in tissue sections. Tissue sections are placed into a methenamine-silver solution. Urates, like melanin, can bind silver from silver solutions and reduce it directly to metallic silver. After reducing the silver, sodium thiosulfate is used to remove the unreduced silver from the tissue sections. The section is then counterstained with light green. Methenamine silver stains urates black on a green background. Chondrocalcinosis (pseudogout) is a disease that results from deposition of calcium pyrophosphate crystals in joint cartilage, and may mimic gout. A polarizing microscope fitted with a quartz first order red compensator is useful in differentiating between urate crystals of gout and pyrophosphate crystals of pseudogout. Pyrophosphate crystals exhibit positive birefringence while urate crystals will show negative birefringence. Urates can also be extracted by saturated aqueous lithium carbonate solution while pyrophosphate crystals are not extracted. Staining of Uric Acid and Urates Uric acid and urates are soluble in water, so much of the material will be lost during normal aqueous fixation and subsequent processing. Staining with eosin only (no hematoxylin) provides limited contact with water. 95% alcohol is recommended as the most suitable fixative for the specific demonstration of urates. These specimens should be processed on a day cycle starting at absolute alcohol. Avoid prolonged floating-out of section on water bath. Gomori’s Methenamine Silver Stain for Urate Crystals (Pearse 1985, Sheehan 1980) Fixation: Absolute Alcohol at 4°C for overnight. Sections: Paraffin at 4-5 microns Solutions: Methenamine-Silver Nitrate Stock Solution Silver Nitrate, 5% aq. 5ml Methenamine, 3%, aq 100ml Methenamine-Silver Nitrate Working Solution Methenamine Silver-Nitrate Stock Soln 25ml Distilled Water 25ml Sodium Borate, 5% aq 2ml Prepare fresh prior to use. Do not use if cloudy. Method: 1. Deparaffinize to Xylene and rinse with 3 changes of absolute alcohol. 2. Place slides in preheated working methenamine silver. 3. Incubate for 30 minutes at 60ºC. 4. Rinse sections is distilled water. 5. Tone with 0.1% Gold Chloride for 5 minutes. 6. Give sections 4 or 5 rinses of distilled water. 7. 3% Sodium Thiosulfate for 5 minutes. 8. Wash in tap water for 5 minutes. 9. Rinse in distilled water. 10. Counterstain in Light Green working solution for 2 minutes. 11. Dehydrate, clear and mount. Results: Urate Crystals Black Background Green Carbon Carbon is the most commonly seen exogenous mineral in tissues, and is easily recognized in stained tissue sections, such as lung and adjacent lymph nodes of urban dwellers and tobacco smokers. Black pigmentation of the lung (anthracosis) is also seen as a result of massive deposition of carbon in coal workers. The lung disease known as Coal worker's pneumoconiosis is caused by inhalation of silica, which is found in association with coal and other minerals. Carbon is extremely inert and cannot be demonstrated with conventional histochemical methods. It may be confused with melanin, which is dissolved by bleaching agents while carbon is not. Carbon is insoluble in concentrated sulfuric acid and all other acid and alkaline solution. Carbon appears as anthracotic pigment in the lungs. It can be distinguished from melanin by doing a melanin bleach. Poorly fixed tissues may contain formalin-heme pigment, which is black and finely granular, but this is widely scattered in the tissues without regard to cellular detail. Formalin-heme pigment is also birefringent on polarization. ARTIFACT PIGMENTS Artifacts that appear in stained slides may result from a number of causes including improper fixation, the type of fixative, poor dehydration, improper reagents, or poor microtome sectioning. These pigments, when viewed microscopically, commonly appear to lie on top of the tissue and not within the cell. Artefact pigments may be deposited during fixation of tissue with formalin, mercuric chloride, chromium or osmic acid, which may later on interfere with good staining results if not properly and completely washed out. Highly colored, usually amorphous, granular, sometimes crystalline (crystal-violet) stain precipitates may be seen in sections due to faulty staining techniques, e.g. when saturated alcoholic stain solutions are allowed to evaporate in a warm, dry atmosphere. Acid alcohol is perhaps the most common solution used for removing excess stains in sections, particularly on H&E series: 1. Dip sections quickly in 0.5% or 1% acid alcohol. 2. Wash immediately thoroughly in running water to stop the acid action. 3. Place sections in either of the following solutions for 5-15 minutes: a) Tap water alkalinized with a few drops of ammonia water. b) Running tap water c) Lithium Carbonate This will neutralize the acid and restore the purple color of the solution. 4. Wash slides in running tap water to remove the alkaline solution. A. Formaldehyde deposits Formalin deposits appear as fine, dark-brown or black crystal-like precipitates, often with no relationship to the tissue (i.e., the precipitate appears adjacent to tissues or within interstices or vessels) especially in postmortem and blood-containing tissues fixed with acid formaldehyde. The deposits are breakdown products of laked hemoglobin, found maximally around blood vessels and congested tissues, e.g. liver and spleen. They form when the formalin buffer is exhausted and the tissue becomes acidic, which promotes the formation of a complex of heme and formalin. The pigment deposits are birefringent in polarized light. Formalin pigments may be prevented by using neutral or buffered formalin. Malaria pigments can be distinguished from formalin pigments by being intracellular. Both of them are most effectively removed by treating unstained tissue sections with saturated alcoholic picric acid. These pigment artefacts are found in tissues that have been fixed in simple formalin fixatives, such as 10% formalin and 10% formal saline. As these solutions age, formic acid develops from the formaldehyde content and lowers the pH. This in turn causes crystals of formalin pigment, or acid formaldehyde hematin, to be deposited throughout the tissues. This is more common in tissues that are bloody, but it will occur in nearly all tissues eventually, especially when they are stored in those solutions for extended periods. Fig. 23-6 Formalin H & E Stain Formalin pigment may be easily stopped from forming by using 10% neutral buffered formalin (NBF) as the fixative. Since its formation is dependent on an acidic pH, buffering to pH7 effectively stops it. However, it may still form if tissues are stored in NBF for much extended periods without changing the solution. The NBF should be changed every six months at a minimum. Doing so effectively stops formalin pigment from forming. Fig. 23-7. Formalin Auto fluorescence In small amounts the pigment does not interfere with slide examination, but large amounts can be distracting. It may be removed from sections prior to staining quite easily by immersing in ethanolic picric acid, a method given below. It may also be removed with alkalis such as 1% sodium hydroxide in absolute ethanol, but these very frequently cause sections to detach from slides and should be avoided. Removing formalin pigment (Suvarna 2013, Kiernan 1999) Method 1 1. Bring sections to water via xylene and ethanol. 2. Place into 1.8% picric acid in absolute alcohol for 1 hour. 3. Optionally, treat with saturated aqueous lithium carbonate to remove picric acid discoloration. 4. Wash well with water. 5. Continue with the staining method. Method 2 Solution: Alcohol-Ammonia Solution 95 % alcohol 50 mL Concentrated ammonia (0.880) 15 mL Mix before use. Method: 1. Deparaffinize and hydrate to distilled water. 2. Place in Alcohol-ammonia solution for 1 (one) hour. 3. Wash in water. 4. Stain using H&E or other technique. Method 3 Solution: Ammonia Water 28% 2 ml Alcohol 70% 100 ml Method: 1. Place in solution for 30-60 minutes. 2. Rinse and place in 1% aqueous acetic acid. 3. Wash thoroughly in tap water and stain as desired. Method 4 Solution: Hydrogen Peroxide 3% Aqueous 50 ml Acetone 50 ml Ammonium Hydroxide 28% 1 ml Method: 1. Place in solution for 5- 10 minutes. 2. Wash thoroughly in running tap water and stain as desired. Removing Formalin Pigment (Garvey’s Technique): Solutions: Alkylphenol ethoxylate (APE) Phenol 5 ml HCl 5 ml Absolute ethanol 90 ml Method: 1. Place sections in alkylphenol ethoxylate (APE) for 5 minutes. 2. Wash in water for 5 minutes. • 3. Treat with 5% potassium permanganate for 2 minutes, 4. Wash in water for 2 minutes. 5. Decolorize in 5% oxalic acid, 2 minutes. 1. M e rc u r i c C h l o r i d e D e p o s i t s ( K i e r n a n 1 9 9 9 , D r u r y 1 9 8 0 ) The presence of large irregular clumps of black precipitate on slides of tissues fixed in a mercurial fixative suggests that the tissues were not "dezenkerized" prior to staining. These black precipitates will also appear white with polarized light microscopy. These deposits occur in all tissues fixed in liquids containing mercuric chloride, including B5, Heidenhain’s Susa, Helly’s and Zenker’s fluid. Addition of a few drops of saturated alcoholic iodine solution during dehydration will remove the pigment but will tend to make tissues brittle during sectioning. Hence, final removal of the mercurial deposit by subsequent bleaching with a weak sodium thiosulfate (hypo) after sectioning and before staining is recommended. Method 1 1. Deparaffinize slides thru xylol, absolute and 95% alcohol. 2. Place in alcoholic iodine solution (0.5% iodine in 80% alcohol) for 5-10 minutes to remove the deposit. 3. Wash in water and rinse in 80% alcohol. 4. Place in a 5% solution of sodium thiosulfate for 2-5 minutes. 5. Wash thoroughly in running water to remove the Sodium Thiosulfate. 6. Stain as desire Method 2 Solutions: Lugol’s Iodine Iodine 1.0 g Potassium iodide 2.0 g Distilled water 100 mL 5 % Aqueous Sodium Thiosulfate Method: 1. Bring sections to water. 2. Place in Lugol's iodine for 15 minutes. 3. Wash in water. 4. Place in thiosulphate for 3 minutes. 5. Wash in water. 6. Stain with H&E or other technique. 3. Osmium Tetroxide Deposits (Ellis 1979) Osmic acid appears as black deposits on tissues which have not been properly washed out. To remove by bleaching, the following procedures may be availed of: Method 1 1. Sections to 70% alcohol. 2. Place the tissue in solution containing 2 ml. of Hydrogen Peroxide and 70% Alcohol (48 ml.) 3. Expose to sunlight for 15-30 minutes to bleach. 4. Take down to water and wash thoroughly. Method 2 1. Sections to water. 2. Place in 0.5% potassium permanganate for 5 minutes. 3. Wash in water. 4. Place in sulfurous acid until thoroughly bleached. 5. Wash thoroughly in water. 4. Chrome deposits appear as fine brown or black granules in chromate (i.e., Zenker’s) fixed tissues. They may be removed from the tissues by washing them out from sections with the use of acid alcohol. Chrome deposits can be prevented by washing tissue in running tap water prior to dehydration. 5. Silica is found most commonly in the lungs and associated lymph nodes of stone grinders. In coal miners, it occurs together with carbon, which presents as anthracosis. Silica pigment occurs as grayish crystals that are birefringent. Asbestos is a special type of long-thin silica crystal found in the lungs and associated lymph nodes of asbestos workers. Mesotheliomas are tumors of the serous membranes (peritoneum, pericardium and pleura) that are often related to asbestos exposure. In tissue, these irritant crystals are found in the form of fibers coated with a protein-iron-calcium matrix, giving them a barbell shape appearance. The characteristic shape and light brown color make it easy to identify them in routine hematoxylin and eosin sections. They are called "ferruginous bodies" because they give a positive reaction with Prussian blue staining for ferric iron. It is not anisotropic and, therefore, cannot be demonstrated by polarized light. Inhaled asbestos fibers become coated with a complex containing hemosiderin which can be demonstrated with the Prussian blue reaction. 6. Tattoo pigments are usually applied to skin but may also be used to mark anatomic or surgical landmarks and help .the tissue during gross dissection, embedding, and in final histologic sections. The ink may be applied to color the entire outside perimeter of the specimen, using single or multiple colored inks. To be effective, the tissue markers should be insoluble in fixative solutions, processing solutions, and the embedding media; must not react with histologic stains or obscure cellular details; and must be clearly visible both through the naked eye , or under the microscope. Black or bright blue ink is often preferred. 7. Starch or talcum powder is a pigment usually introduced by talc from the gloves of a surgeon, nurse, or pathologist. This pigment is PAS- and GMSpositive and can be easily identified by its characteristic appearance, which includes a “Maltese cross” configuration when polarized. Talcum powder has an affinity for the dyes auramine O and rhodamine B, and will fluoresce yellow when viewed with a fluorescence microscope. REFERENCES Bancroft JD, Cook HC. (1994) Manual of Histological Techniques and their Diagnostic Application. Edinburg: Churchill Livingstone. Bancroft JD, Stevens A, eds. (1996) Theory and practice of histological techniques. 4th ed. New York: Churchill Livingstone. Bancroft JD, Gamble M. (2002). Theory and Practice of Histological Techniques. 5th ed. London, England: Churchill-Livingstone. Bancroft JD, Gamble M. (2008) Theory and Practice of Histological Techniques. 6th ed. Oxford: Churchill Livingstone Elsevier. 252-253. Barrett AM. (1944) On the removal of formaldehyde-produced precipitate from sections. J Pathol Bacteriol 56(1):135-136. Carson FL. (1996) Histotechnology: a self-instructional text. 2nd ed. Chicago: American Society of Clinical Pathologists Press. Carson FL, Hladik C. (2009) Histotechnology: A Self-Instructional Text. 3rd ed. Chicago, Ill.: American Society of Clinical Pathologists, 23-24, 254-255. Chio KS, Reiss U, Fletcher B, Tappel AL. (1969) Peroxidation of subcellular organelles: formation of lipofuscin-like pigments. Science 166:1535-1536. Churukian CJ. (2000) Manual of the Special Stains Laboratory, Rochester: University of Rochester. Churukian CJ. (2002) Pigments and Minerals. Chapter 13 in Bancroft JD, Gamble M (eds). Theory and Practice of Histological Techniques, 5th ed. London: Churchill Livingstone. pp. 243-267. Churukian CJ. (2005) Manual of the Special Stains Laboratory. 10th ed. Rochester, NY: University of Rochester. Culling CFA. (1974): Handbook of Histopathological and Histochemical Techniques. 3rd ed. London: Butterworths; pp. 384–385. Culling CFA. (1974) Handbook of Histopathological and Histochemical Techniques. 3rd ed. London, England: Butterworth; 386. Dahl LK. (1952) A simple and sensitive histochemical method for calcium. J Exp Med 95: 474-479. Drury RAB, Wallington EA. (1980) Carleton's histological technique Ed. 5 Oxford University Press, Oxford, UK. Ellis EA, Anthony DW. (1979) A method for removing precipitate from ultrathin sections resulting from glutaraldehyde-osmium tetroxide fixation. Stain Technol 54(5):282-5. Garvey W. (1991) Modification of the Mayer haematoxylin stain. J Histotechnol 13:163–165. Gomori G. (1936) Microchemical demonstration of iron. Am J Pathol 13: 655. Gomori G. (1950) Aldehyde fuchsin: a new stain for elastic tissues. American Journal of Pathology 13: 655 Gomori G. (1951) Histochemical Staining Methods. In: Vischer, MB (eds). Methods in medical research, vol.4. Year Book Publishers, Chicago, p 14 Grocott, RG. (1955) A stain for fungi n tissue sections and sears. Am J Clin Pathol 25: 975. Hall MJ. (1960) A staining reaction for bilirubin in sections of tissue. Am J Clin Pathol 34: 313-316. Henwood A. (2010) What is the Best Procedure to Remove Formalin Pigment from FormaldehydeAcetic Acid-Alcohol Fixed Tissues? The Journal of Histotechnology 33(3): 109-111. Irons RD, Schenk EA, Lee JC. (1977) Cytochemical methods for copper: semiquantitative screening procedure for identification of abnormal copper levels in the liver. Arch Pathol Lab Med. 101:298-301. Kiernan JA. (1999) Histological and histochemical methods: Theory and practice, Ed. 3 Butterworth Heinemann, Oxford, UK. Kiernan JA. (2008) Histological and Histochemical Methods: Theory and Practice 4th ed. Bloxham, UK: Scion. (Chapter 13, pp. 337-353). Landas SK, Schelper RL, Tio FO, Bennett-Gray J. (1986) Staining properties of melanin and lipofuscin pigments. Am J Clin Pathol 86(4):556–557. Lee GL. (1992) Histopathologic methods and color atlas of special stains and tissue artifacts. Gaithersburg, MD: American Histolabs Inc., Publications Division. Lillie, R.D. (1954) Histopathologic Technic and Practical Histochemistry, Philadelphia, Bladiston Co. Lillie RD. (1965) Histopathologic Technic and Practical Histochemistry 3rd ed. Philadelphia, PA: Blakiston. Lillie RD, Fullmer HM, eds. (1976) Histopathologic Technic and Practical Histochemistry. 4th ed. New York, NY: McGraw-Hill; Lindquist RR. (1969) Studies on the pathogenesis of hepatolenticular degeneration, II: cytochemical methods for the localization of copper. Arch Pathol. 87:370-379. Luna LD. (1968) Manual of Histologic Staining Methods of the Armed Forces Institute of Pathology, 3rd ed. New York: McGraw-Hill. Mallory FB. (1961) Pathological Technique, Hafner Publ. Co., NY, p 136. Mallory FB, Parker F. (1939) Fixing and staining methods for lead and copper in tissues. American Journal of Pathology 16: 516. Masson P. (1928) Carcinoids and nerve hyperplasia of the appendicular mucosa. Am J Pathol 4: 181. Pearse AGE. (1953) Histochemistry, Theoretical and Applied. Churchill, London. Rodriguez HA, McGavran MH. (1969) A modified DOPA reaction for the diagnosis and investigation of pigment cells. American Journal of Clinical Pathology, 52: 219. Pearse AGE. (1985) Histochemistry, Theoretical and Applied 4th ed. Edinburgh: Churchill Livingstone. Vol. 2, Chapter 20, pp. 973-1033. Preece A. (1959) A manual for histologic technicians. Little, Brown. Prophet E, Mills B, Arrington J, Soblin L. (1992) Laboratory methods in Histotechnology. Washington, DC: Armed Forces Institute of Pathology. Prota, G. (1995) The chemistry of melanins and melanogenesis. Progress in the Chemistry of Organic Natural Products 64:93-148. Puchtler H, Meloan SN, Terry MS.(1969) On the history and mechanism of alizarin and alizarin red S stains for calcium. J Histochem Cytochem 17:110-124. Sheehan D, Hrapchak B. (1973) Theory and practice of histotechnology. St. Louis, MO: CV Mosby Company Sheehan DC, Hrapchak BB. (1980) Theory and Practice of Histotechnology. 2nd ed. St. Louis: Mosby 130, 214, 220-221. Suvarna SK, Layton C, Bancroft JD. (2013) Bancroft’s Theory and Practice of Histological Techniques: Churchill Livingstone, Elsevier. Thornburg LP, Beissenherz M, Dolan M, Raisbeck MF. (1985) Histochemical demonstration of copper and copper-associated protein in the canine liver. Vet Pathol 22:327-332. Tseng CH. (1983) A new method of removal of formalin pigment. Am J Med Technol 49:435–436. Waldrop FS, Puchtler H, Terry MS. (1969) Removal of acid hematin type pigments from sections; efficacy of alcoholic picric acid solution. Stain Technol 44:279–281. Wilcox WR, Khalaf A, Weinberger A, Kippen I, Klinenberg JR.(1972) Solubility of uric acid and monosodium urate. Mol and Biol Eng 10:522-531. Yasue T. (1969). Histochemical identification of calcium oxalate. Acta Histochem Cytochem 2(3):8395. CHAPTER 24 STAINING OF BONE MARROW AND BLOOD ELEMENTS Bone marrow may be processed as a touch or smear preparation, or in the form of biopsy. Bone marrow aspirates stained by Romanowsky techniques are currently used as a main diagnostic tool by the hematopathologist. Bone marrow biopsy is usually indicated when material cannot be obtained by aspiration ("dry tap"), as in aplastic anemia and myelofibrosis, or when visualization of bone marrow structure is required, as in lipid storage diseases, malignancy or metastatic disease. New and improved trephine biopsy needles have been developed to produce a good length core of distortion-free bone marrow tissue that can be stained with hematoxylin and eosin or with Romanowsky-like stains. A limited number of histochemical techniques can also be applied to examine hematopoietic elements in architecturally wellpreserved marrow spaces. Bone marrow biopsy also demonstrates the topographic distribution of cell types which cannot be obtained by bone marrow aspiration. Bone Marrow Preparations Examination of the bone marrow aspirate and trephine biopsy is essential for the diagnosis of bone marrow and malignant hematologic disorders (including acute and chronic leukemias, myelodysplastic syndromes, chronic myeloproliferative disorders, lymphomas, and plasma cell myeloma. Additional investigations including flow cytometric immunophenotyping, cytochemistry, FISH, and molecular genetics can be performed on the bone marrow aspirates. Bone Marrow Aspirate Bone marrow smears should be prepared immediately following aspiration. Smears prepared from EDTA samples should be made as soon as possible to reduce storage artefact. To prepare smears, the aspirate should be expelled into a small plastic or siliconized glass dish, and a Pasteur pipette is used to draw up particles, which are placed on glass slides and then smeared. Alternatively, a drop of aspirate can be placed on each glass slide and the excess blood drained off the slide by tipping the slide, or aspirated with a Pasteur pipette or plastic syringe, before making the smear. A minimum of six smears and two particle squash (‘crush’) slide preparations should be made. Particle clot preparations may provide additional information and can be made if a trephine biopsy is not taken or if one suspects that the biopsy was not adequate. Bone marrow smears or touch preparations are air-dried, fixed and stained using standard methods for blood smear, such as Wright's or Giemsa's stain. A blood or marrow smear or touch prep should not be sprayed with or dipped in a fixative such as hairspray, alcohol or formalin. The Romanowsky stains used in hematology will only work on air dried material that is relatively fresh (less than one month old). For bone marrow biopsies, Zenker's solution is recommended for fixing, since this will decalcify tiny bony spicules which may have been admixed with the blood clot. A piece of bone marrow is removed and sliced thinly, and fixed with Zenker's fluid and acetic acid for 14-24 hours to decalcify the cancellous bone. The section is then washed in running water for 3-6 hours, and processed as for a bone marrow smear. Bone marrow smears are usually made at the bedside, directly after aspiration of the bone marrow. At the bedside, 1 ml of the aspirate is added to a snap cap vial containing 1.8% EDTA, mixed well, and sent to the laboratory. Using a Pasteur pipette that has been rins ed previously with EDTA solution, an aliquot of the aspirate is transferred to a watch glass. I f the watch glass is gently tilted, blood will run to one side and marrow particles will be visible. Any excess blood can be gently blotted away using filter paper, taking care not to touch the marrow particles or contaminate one's hands with blood . The particles are transferred to glass slides, from which smears can be made: 1. Squash smear: Squash the marrow particles with another slide and pull to the end of the marrow slide. This type of preparation often causes considerable cellular artifact. The squash preparation is useful for the assessment of cellularity, megakaryocyte numbers, focal disease (e.g. lymphoma, plasma cell myeloma, mast cells, metastatic carcinoma, storage histiocytes, and granulomas) and fibrotic marrows. 2. Spread smear: The marrow particles are placed at one end of the slide and spread with another slide as for a blood smear. This allows excellent detail of individual cell morphology. Two air-dried smears and one squash slide should be fixed with fresh acetone-free absolute methanol and stained with a Romanowsky stain, such as May-Grunwald Giemsa or Wright Giemsa stain. A methanol-fixed smear and a squash slide should be stained with Prussian blue (Perls’ reaction) and counterstained with nuclear fast red. All bone marrow smears should be cover slipped using a mounting medium that hardens and dries rapidly. Mounting media may contain toxic organic compounds such as toluene or xylene and should be handled with appropriate safety precautions. Additional slides may be used for cytochemistry (e.g. myeloperoxidase or nonspecific esterases), immunohistochemistry, fluorescent in situ hybridization, or archived as unfixed, unstained smears, as required. Unfixed and unstained aspirate smears stored at room temperature for long periods may give variable results on retrospective Giemsa staining. Aspirate slides fixed in absolute methanol preserve DNA (and possibly many antigens) for future FISH, or DNA extraction and subsequent PCR amplification. For cases with suspected acute leukemia, cytochemical stains for myeloperoxidase and nonspecific esterases (e.g. α-naphthyl butyrate esterase) are recommended. Bone Marrow Trephine (Core) biopsy The BM trephine biopsy may be performed either before or after the aspirate. Trephine sections are particularly useful for the assessment of overall marrow architecture and cellularity and provide greater sensitivity for the assessment of focal lesions and patchy infiltrates. The length of the core from an adult should be at least 2 cm. A shorter core (e.g. 1 cm) may sometimes contain sufficient diagnostic information. The biopsy specimen shrinks by approximately 20% after processing. However, the larger the amount of tissue that is biopsied, the greater is the likelihood of a focal lesion (e.g. lymphoma, metastatic tumor, granulomas) being detected. A standard fixative for trephine core biopsy is neutral buffered formalin is the standard fixative for trephine core biopsies. Other fixatives commonly used include zinc formaldehyde, B5 (mercuric chloride, sodium acetate and formalin), acetic acid-zinc-formalin, isotonic buffered formalin, Bouin’s fixative (picric acid, acetic acid and formaldehyde), or formaldehyde and glutaraldehyde. Fixation time varies from 1 to 24 hours depending on the fixative used. Although B5 gives good morphology with a short turnaround time (TAT), it contains mercuric chloride causing safety and environmental concerns. Touch imprints should be made from the trephine biopsy prior to placing in the core tissue in fixative. Imprints are especially important if there is a ‘dry tap’ on bone marrow aspiration. Imprints are made by gently touching the fresh unfixed core on the slide, or the slide on the core. The imprints are fixed and stained using the same method as for aspirate smear and squash preparations. If bone is to be studied, a small piece of bone marrow attached to a thin hard bone is decalcified for 24-48 hours. Both organic and mineral acids are commonly used for decalcification of bone marrow specimens. Organic acids (e.g., formic and acetic) decalcify slower than mineral acids (e.g., HCL and nitric). Over-decalcification of tissue with acids, particularly mineral acids, results in tissue destruction so that tissue in acid decalcifiers should not be left unchecked for extended periods (e.g., over a weekend). Tissue suspension, mild agitation, gentle mixing or air bubble percolation, will ensure an even distribution of decalcifying acid around bone sample. For decalcification, the following solutions used are EDTA, formic acid, acetic acid, picric acid, or nitric acid. Decalcification time varies depending on the type of decalcifying agent and the size of the biopsy specimen. Decalcification with EDTA results in better preservation of nucleic acids, but is slower than with other acid reagents. Sections should not be left in solution for a longer period of time since this may injure, if not destroy, the cellular detail of the bone marrow. The section is washed thoroughly after decalcification, cleared, embedded in paraffin and stained as required. The recommended thickness of sections is two to three microns. Hematoxylin and eosin, and the Van Gieson stains are the methods available for routine use. In order to protect the cellular and fibrous elements of bone from damage caused by the acids used as decalcifying agents, it is particularly important to thoroughly fix these specimens prior to decalcification. Poorly-fixed specimens become macerated during decalcification and stain poorly afterwards. This is very noticeable in areas containing bone marrow. It is therefore common practice to extend fixation times for bone specimens before commencing decalcification. Decalcification results in the leaching out of some storage iron from the core biopsy, and nitric acid and hydrochloric acid have been reported to diminish the acid fastness of mycobacteria resulting in false negative results. However, acid fastness is retained when decalcification is in formic acid, sodium citrate or citric acid buffer. Bone marrow core biopsy specimens can also be embedded in plastic. Plastic embedding gives good cytological detail, does not require decalcification and may be useful for the evaluation of metabolic bone diseases and histochemical reactions that are removed by the decalcification process. Decalcification chelates storage iron and may affect morphology and cytological detail and the ability to perform histochemistry and immunohistochemistry. The undecalcified resin-embedded trephines have replaced the older techniques that employ decalcification and paraffin embedding. Except for the demonstration of iron and reticulin, much of the cytological details necessary for diagnosis of hematopoietic disorders can be obtained from marrow biopsies stained by H&E technique. The Giemsa stain may be helpful for identifying plasma cells, mast cells, lymphoid cells, eosinophils, and for distinguishing between myeloblasts and proerythroblasts. Another useful method involves staining of granulopoietic precursor granules in glycol methacrylate sections, using toluidine blue and eosin. Toluidine blue is the most useful and informative stain for plastic-embedded tissue sections. If the stain is heated and used at high alkaline pH, it easily penetrates the plastic and stains various tissue components a blue color of differing shades and intensities, with no appreciable staining of the embedding medium . Cytologic dysplasia, the morphologic hallmark of myelodysplastic syndromes, is best defined in bone marrow aspirate samples with MayGrünwald Giemsa stain. Hematoxylin and eosin stain (H&E), Giemsa, Gomori’s silver impregnation technique and Perls’ stain in combination with immunostaining are also common methods used to study myelodysplastic syndrome. Reticulin stain is particularly useful in the detection of myelofibrosis, since the reticulin content is greatly increased in this disease. Reticulin is also slightly increased with increasing cellularity of the marrow, as seen in conditions such as leukemia and lymphoma. A bone marrow section previously shown to have increased reticulin should be included as a positive control since silver impregnation staining methods are fixation dependent. A trichrome stain may be used to identify collagen fibrosis, which is readily recognized in well-stained H&E specimens. Romanowsky Stains Romanowsky stains consist of methylene blue/azure B and eosin, dissolved in acetone-free methanol. They include Jenner, Giemsa, May Grunwald and Leishman stains. Jenner ( 1889) found that a precipitate formed by mixing eosin and methylene blue could be dissolved in methyl alcohol to form a useful stain that combines the properties of the two dyes. Romanowsky (1890) found that better staining resulted when old (ripened and therefore "polychromed") methylene blue solutions were added to eosin and the precipitate was dissolved in methyl alcohol. Modern Romanowsky techniques, such as Wright's and Leishman's stains, are basically similar to Romanowsky's original method. The main difference lies in the manner and method of polychroming methylene blue. With Leishman's stain, methylene blue is polychromed by heating a 1% solution with 0.5% sodium carbonate at 65°C for 12 hours, after which further ripening is allowed to proceed for 10 days before it is mixed with an equal volume of 0.1% eosin B. Preparation of Solutions of Romanowsky Dyes May–Grünwald Stain: Weigh out 0.3 g of the powdered dye and transfer to a conical flask of 200–250 ml capacity. Add 100 ml of methanol and warm the mixture to 50°C. Allow the flask to cool to c 20°C and shake several times during the day. After letting it stand for 24 h, filter the solution. It is then ready for use, no ‘ripening’ being required. Jenner’s Stain: Prepare a 5 g/l solution in methanol in exactly the same way as described earlier for the May–Grünwald stain. Giemsa’s Stain: Weigh 1 g of the powdered dye and transfer to a conical flask of 200– 250 ml capacity. Add 100 ml of methanol and warm the mixture to 50°C; keep at this temperature for 15 min with occasional shaking, then filter the solution. It is then ready for use, but it will improve on standing for a few hours. Azure B–Eosin Y Stock Solution The stock solution includes azure B, tetrafluoroborate or thiocyanate (Color index 52010), >80% pure, and eosin Y (Color index 45380), >80% pure. Wright's Stain (Hope 1978) Methylene blue is polychromed by heating with sodium bicarbonate. It may be purchased in solution ready for use, or as a powder, 1.0 gm. which is carefully dissolved in 600 ml. of methyl alcohol. Principle: The eosinates of polychromed methylene blue are dissolved in absolute methyl alcohol. When this solution is placed on a dried blood smear, the methyl alcohol acts as the fixative, and the dissolved dye begins the staining process. After from one to three minutes, the stain is diluted with an equal volume of distilled water. This differentially stains the cytoplasmic granules and is allowed to act for about three minutes. It is then poured off and the preparation is washed briefly in tap water and allowed to dry. Fixation: Streak thin (approximately one cell thick) smears across a sterile slide by means of a second slide or cover glass. Air dry quickly. Method: 1. Place the air-dried smear, film side up, on a staining rack. 2. Cover the smear with undiluted Wright stain and leave for 1 minute. The methyl alcohol fixes the smear. 3. Dilute with distilled water (approximately equal volume) until a metallic scum appears. Allow this diluted stain to act for 2 1/2 to 5 minutes. 4. Without disturbing the slide, flood with distilled water and wash until the thinner parts of the film are pinkish red. 5. If distilled water does not give adequate differentiation, a phosphate buffer (pH 6.4 to 6.5) should be used, at least for washing, but possibly also for diluting the stain (step 3). Results: Erythrocytes yellowish-red Polymorphonuclears: Nucleus dark purple Polymorphonuclears: Granules reddish-lilac Polymorphonuclears: Cytoplasm pale-pink Eosinophils: Nuclei blue Eosinophils: Granules red to orange-red Eosinophils: Cytoplasm blue Basophils: Nucleus purple to dark blue Basophiles: Granules very dark purple Lymphocytes: Nuclei dark purple Lymphocytes: Cytoplasm sky blue Platelets violet to purple granules In general, Wright's stains are somewhat empirical mixtures of polychromed dyes, so that one batch may differ from one another. A stock solution can be stored, although "ripening' or polychroming continues during storage, and poor results are obtained if the stock staining solution becomes contaminated with water. The working solution, i.e., 10 ml. stock solution to 90 ml. phosphate buffered distilled water (pH 6.8), should be freshly made immediately prior to use. All Romanowsky stains have a tendency to precipitate, and must be filtered before use. Wright's or Wright-Giemsa stains are usually the preferred staining method for bone marrow aspirate smears. Both are methanol-based staining solutions. Since Wright's stains are methanol based they do not require a fixation step prior to staining, although you might prefer to do so first to reduce water artifact that can occur on humid days or with aged stain. Giemsa Stain (Lillie 1965, 1977) Giemsa's stain is a member of the Romanowsky group of stains, which are defined as being the black precipitate formed from the addition of aqueous solutions of methylene blue and eosin, dissolved in methanol. Instead of empirically polychromed dyes, this stain employs various azure compounds (thionine and its methyl derivatives) with eosin and methylene blue. It is best purchased commercially in solution. Solutions: Giemsa's stain, stock solution – obtain from commercial sources. Giemsa reagent improves with age. Giemsa stain, working solution Giemsa stock solution 40 drops Distilled water 40 ml The diluted stain keeps well, but is best made up fresh each time. Acetic acid 0.5% Method: 1. Bring sections to distilled water. 2. Stain with diluted Giemsa's stain made up fresh. 3. Rinse in distilled water. 4. Differentiate with 0.5% aqueous acetic acid. 5. Dehydrate rapidly. 6. Clear and mount. Results Bile pigments green Collagen, muscle, bone pale pink Micro-organisms fungi, parasites purplish-blue Starch granules, cellulose sky blue Pigments (native color is yellow/brown, or green if fixed in dichromate containing fixative Nuclei dark blue to violet Erythrocytes salmon pink Cytoplasm varying light blue shades Notes: 1. The staining is usually performed at room temperature overnight. Increasing the stain temperature shortens staining time. 2. By itself, Giemsa stains red cells and neutrophil granules poorly, but azurophil granules (red) are well stained. It is not commonly used alone in hematology, but is an excellent stain for inclusion bodies if the smears are allowed to stain in dilute Giemsa stain for 12 to 18 hours. 3. Differentiation with acetic acid will vary according to the staining time and temperature, but it is generally achieved within 30 secs. The differentiating agent removes only the blue dye component, thus increasing the apparent intensity of the red component. Wright-Giemsa or Jenner-Giemsa Stain This combination of a Romanowsky stain with another stain (such as Giemsa) improves the staining of cytoplasmic granules. Wright's and WrightGiemsa stains, when performed properly, will give sharp and clear cytoplasmic, nuclear, and granule detail. It is advisable to keep a separate stock of Wright's stain for bone marrow staining at least 6 months before use to allow it to ripen. The most important components of these stains are oxidized methylene blue, azure B and eosin Y dyes. The eosin Y dye stains the cytoplasm of cells and orange to pink color. The methylene blue and azure B dyes stain the nucleus varying shades of blue to purple. Romanowsky stains are used to perform differential white blood cell counts and to study red blood cell morphology. Abnormal granulocyte, lymphocyte or monocyte cell counts may be used to facilitate the diagnosis of diseases such as leukemia or bacterial infections. In the dip method of staining, the smears are first dipped in methanol to fix the specimens and then placed in Wright's or Wright-Giemsa stain for 10-15 minutes to stain. The smears are next moved to a mixture of stain and 6.8 pH phosphate buffer (usually one part stain to 2-3 parts buffer) and allowed to stain for at 20-30 minutes. After staining, they are given a quick rinse in distilled water and allowed to air dry before mounting or cover-slipping. When using a staining rack, the marrow slides or coverslips are first flooded with enough stain to cover the slide and stained for 10-15 minutes. Then, a 6.8 pH buffer is carefully added without overflowing and gently mixed by blowing until a green metallic sheen forms. This is allowed to stand for 2030 minutes and then rinsed off with distilled water. The slides or coverslips are then air dried and mounted. Results: Nuclei purple/blue Cytoplasm pink/blue Eosinophils pink/red Fig. 24-1. Bone Marrow Aspirate (Wright-Giemsa Stain) May-Grunwald-Giemsa Stain (Luna 1968) This gives slightly better results than the Jenner-Giemsa. Method: 1. Fix air-dried smears in methyl alcohol for 5 minutes. 2. Transfer to May-Grunwald stain (another Romanowsky dye) freshly diluted with 1 or 2 volumes of buffered distilled water (pH 6.8). Leave for 3 to 5 minutes. 3. Transfer, without washing, to fresh diluted Giemsa and allow to stain for 7 to 15 minutes. 4. Differentiate by washing quickly in three changes of buffered (pH 6.8) distilled water and place in a fourth change of buffered water for 3 to 12 minutes. (Monitor degree of differentiation under low power microscope). 5. Stand the slide on end to dry. Notes: 1. The use of Coplin jars for staining will minimize the possibility of precipitation of stain on the glass slide. If this occurs, the slide can be re-immersed in methanol and in preferred Romanowsky stain. 2. Differentiation in phosphate buffer can be adjusted to suit personal preference in the balance between blue staining and the eosin staining. 3. It is essential that the slide is completely dry before mounting. Perls’ Prussian blue Iron Stain Iron staining on bone marrow aspirate smears is commonly part of the standard order protocol for bone marrows aspirates. Bone marrow aspirates are more sensitive than trephine biopsy sections for the detection of hemosiderin when the biopsy specimens are decalcified in formic acid. The detection of hemosiderin in a Perls’ stained bone marrow aspirate is regarded as the gold standard by which other tests for iron deficiency or depletion are assessed. The section is treated with dilute hydrochloric acid to release ferric ions from binding proteins. These ions then react with potassium ferrocyanide to produce an insoluble blue compound (the Prussian blue reaction). This procedure is particularly helpful when evaluating patients with anemia, iron overload, and myelodysplasia. , etc. In the adult setting, it is commonly performed on the bone marrow biopsy, but can be requested on the aspirates as well. Mercurial fixatives seem to do a better job of preserving iron in bone marrow than formalin. A Prussian blue stain should be performed on a bone marrow smear for the evaluation of storage iron and sideroblasts. A bone marrow smear with increased iron stores should be included as a positive control. Core biopsy sections are less reliable than the aspirate for the assessment of storage iron, since decalcification removes storage iron. Myeloperoxidase (MPO) stain (Kaplow 1965) This stain is helpful in identifying cytoplasmic granules characteristic of myeloid cells. This is useful when there are large, immature white blood cells in the peripheral blood, to differentiate myeloid leukemia cells from those of lymphoid origin. The demonstration of peroxidase granules in certain leukocytes (myeloid cells) depends on their content of an iron-porphyrin-containing enzyme (peroxidase) that promotes the oxidation of benzidine by hydrogen peroxide. Copper sulfate then forms a blue-green compound with the oxidized benzidine and renders the granules visible. Fixative: 40% formaldehyde 1 part 95% ethanol 9 parts Staining Solution: 30% Ethanol 100 ml Benzidine hydrochloride 0.3 gm 3.8% zinc sulfate 1.0 ml Sodium acetate 1 gm 1 N Sodium hydroxide 1.5 ml 3% hydrogen peroxide (10 vols.) 1.7 ml Counterstain: Giemsa stain diluted 1 in 10 with buffered distilled water, pH 6.8 Incubation mixture: 30 % ethyl alcohol 100 ml Benzidine dihydrochloride 0.3 gm 0.132 M (3.8 % w/v) ZnSO4 .7 H20 1.0 ml Sodium acetate 1.0 gm 3 per cent hydrogen peroxide 0.7 ml 1.0 N sodium hydroxide 1.5 ml Safranin 0 0.2Gm The reagents should be added in the order listed, mixing well with each addition. The benzidine salt may contain a small amount of inert residue which will not go into solution. A precipitate forms upon addition of the zinc sulfate. This dissolves upon addition of the remaining reagents. Omit the safranin if a nuclear counterstain is not required. The final pH is 6.00 ± .05. The solution should be filtered and stored in a capped Coplin jar or bottle at room temperature. The same solution can be used over and over again for as long as 6 months. Method: 1. Use fresh smears of blood or bone marrow imprints. Activity may be preserved for as long as 3 weeks if preparations are stored in the dark. Venous or peripheral blood is equally satisfactory. Heparin, oxalate and EDTA are not inhibitory. 2. Fix slides for 60 seconds at room temperature in 10 per cent formalethanol. (10 ml. of 37 per cent formaldehyde and 90 ml. of absolute ethyl alcohol). Wash for 15 to 30 seconds with gently running tap water. Shake off excess water. 3. Place wet slides in incubation mixture in a Coplin jar for 30 seconds at room temperature. 4. Wash briefly (5 to 10 seconds) in running tap water, dry and examine. 5. If greater nuclear detail is desired, the stained preparations may be recounterstained in 1% aqueous cresyl violet acetate for 1 minute, or in freshly prepared Giemsa stain for 10 minutes. (Wright’s stain is less satisfactory as a counterstain.) Fig. 24-2. Bone Marrow Aspirate – Myeloperoxidase Stain Results: Myeloid cells (except basophils) are positive (i.e., peroxidase activity is shown by the presence of green to dark blue granules in the cytoplasm). Eosinophils are stained most intensely and are often tinged brown-black or green-black. The cytoplasm of neutrophils is filled with blue dye. Basophils, lymphocytes and erythroblasts are negative. Monocytes show slight peroxidase activity. Masson’s Trichrome Stain for GMA Plastic Bone Marrow Sections (Churukian 2009) Sections: Undecalcified glycol methacrylate embedded bone marrow sections cut at 4 μm. Solutions: Modified Weigert’s Iron Hematoxylin Solution A Hematoxylin 2.0 gm Alcohol, 90% 100.0 ml Solution B Ferric chloride, FeCl3.6H20, 62% aqueous 4.0 ml Distilled water 95.0 ml HCL concentrated 1.0 ml Working Modified Weigert’s Iron Hematoxylin Equal parts of Solution A and Solution B Biebrich Scarlet-Acid Fuchsin Solution Biebrich scarlet, C.I. 26905 0.45 gm Acid fuchsin, C.I. 42685 0.05 gm Acetic acid, glacial 0.50 ml Phosphomolybdic-Phosphotungstic Acid Solution Phosphomolybdic acid 2.5 gm Phosphotungstic acid 2.5 gm Distilled water 100.0 ml Aniline Blue Solution Aniline blue, C.I. 42755 1.0 gm Distilled water 40.0 ml Acetic acid, glacial 0.8 ml 1% Acetic Acid Solution Acetic acid, glacial 1.0 ml Distilled water 99.0 ml Method: 1. Place in modified Weigert’s iron hematoxylin for 5 minutes. 2. Wash briefly in running tap water and rinse in two changes of distilled water. 3. Decolorize with 0.5% hydrochloric acid in 70% alcohol for 5 seconds. 4. Wash in running tap water for 30 seconds and rinse in two changes of distilled water. 5. Place in Biebrich scarlet-acid fuchsin solution for 30 minutes. 6. Rinse in three changes of distilled water. 7. Place in phosphomolybdic-phosphotungstic acid for 10 minutes. 8. Rinse in two changes of distilled water. 9. Place in aniline blue solution for 7 minutes. 10. Rinse in two changes of distilled water. 11. Place in 1% acetic acid for 1 minute. 12. Rinse in three changes of distilled water and air dry. 13. Dip in xylene and mount with synthetic resin. Results: Osteoid seams red Mineralized bone blue Nuclei dark gray Ancillary Procedures Immunohistochemistry is not routinely performed but may be required for the determination of the lineage and differentiation stage of normal or abnormal cells or cellular infiltrates, as well as for detection of residual disease, specific cell phenotype, extent of disease and prognostic markers. Immunochemistry can be performed by immunoperoxidase or immunoalkaline phosphatase methods. For specimens to be used for immunohistochemistry, a prolonged fixation in 10% NBF may be detrimental (e.g., loss of antigenic epitopes due to continued amino group cross-linking and alteration of tertiary protein structure). Transferring the tissue to 70% ethanol after a 12-hour fixation reduces fixationrelated effects. In-situ hybridization can be performed on bone marrow biopsies but may not be possible when tissues are fixed or decalcified. Although the morphology is not comparable to that of semi-thin sections, formalin fixation provides superior antigen and DNA preservation as compared with picric acid or mercury-based fixative. Metallic fixatives such as Zenker’s and B-5 degrade DNA and impair subsequent molecular diagnostic testing. This limitation is circumvented by fixation in a zinc formalin fixative such as B-plus Fix. LYMPH NODE BIOPSIES A lymph node biopsy removes all or part of the lymph node to be looked at under a microscope for signs of infection or a disease, such as cancer. Other tests may also be used to check the lymph tissue sample, including a culture, genetic tests, or tests to study the body's immune system camera.gif (immunological tests). There are several ways to do a lymph node biopsy. Fine-needle aspiration - a long thin needle is inserted into a lymph node to remove a sample of cells or tissue, Open (excisional) biopsy - a small cut is made in the skin and one or more lymph nodes are taken. Sentinel lymph node (SLN) biopsy - is a new technique that is increasingly used in cancer patients. The so-called sentinel lymph node is the first one to receive lymphatic fluid draining from a cancer site, and can predict whether cancer is likely to be found in the rest of the lymphatic system without removing all of the nearby nodes. If the sentinel node contains no cancer cells, the other lymph nodes are likely to be clear, and a complete lymph node dissection may be unnecessary. If the sentinel node tests positive for cancer, however, all nearby nodes must be removed. The most important aspect of the sentinel node examination is careful attention to slicing the SLN no thicker than 2.0 mm and correct embedding of the slices to assure that all macro-metastases larger than 2.0 mm are identified. Immunohistochemistry, performed with both antibodies S-100 and HMB-45, combined with careful conventional histopathology based on multiple sections, is currently the most reliable method to assess metastatic melanoma in sentinel lymph node. This allows more accurate diagnostic and prognostic staging. Processing Lymph Node Biopsies Samples need to be processed such that the following investigations can be carried out if required: • Microscopy on appropriately fixed and stained tissue samples • Immunological investigation by immunohistochemistry and/or FC • Cytogenetic analysis by Giemsa-banding (G-banding) • FISH on cell suspensions, films, imprints or paraffin sections • Molecular genetic analysis by polymerase chain reaction (PCR), real-time PCR (RT-PCR) or gene sequencing Lymph nodes may be received as complete nodes or as needle core biopsy specimens. In the absence of gross tumor, the entire node is cut into 3- to 4-mm slices in the longitudinal or transverse plane, taking care to process different surfaces for microscopic examination. If the node is so small that it cannot be sliced in this manner, it may be totally submitted as one piece. In the presence of visible tumor within a single lymph node, one or several routine sections to demonstrate the tumor and its possible extra-nodal extension. Every node must be submitted for processing. Lymph node dissections are best processed fresh, although the specimen may be fixed for paraffin or plastic embedding and morphological examination. Submitting fresh tissue facilitates the use of specialist techniques such as cytogenetic analysis, allows the storing of frozen material where appropriate and enables optimal fixation for paraffin embedding and processing. If a frozen section is performed, the results of frozen section will guide the subsequent approach. If a lymphoproliferative disorder is suspected at the time of frozen section, it is important to ensure that sufficient fresh unfrozen tissue is kept for routine histopathology. The process of freezing and subsequent thawing for fixation and processing will interfere with both morphological and immunohistochemical analysis. If macroscopic examination of a larger node leads to the detection of a possible infective focus, a small piece of the fresh tissue should be sent for microbiological culture. If tuberculosis or fungal infection is suspected, the fixed sample should be placed in formalin for 48 hours. Also, if HIV is suspected most laboratories would expect the node to be fixed for 48 hours prior to processing. Cytological diagnosis based on morphology and confirmation by a positive Ziehl-Neelsen stain for acid-fast bacilli is a time-tested method for the diagnosis of tuberculous lymphadenitis, it has low sensitivity. Auramine-rhodamine stain is considered better than routine Ziehl-Neelsen stain in sensitivity, but is less specific. During paraffin sectioning, the tissue is cut at several levels. At least 10 intervening sections from the ribbon should be prepared, using coated or charged glass slides, and stored unstained. These are invaluable if a small infiltrate is noted in any one level, or unexpected features suspicious of lymphoma are found, requiring subsequent immunohistochemical analysis. Lymph node sections are stained using the standard H&E stain. Reticulin staining may be helpful in assessing the follicular architecture. Immunohistochemical staining and other specialized techniques may be used but are not mandatory unless indicated. The specimen may be fixed in formalin to allow paraffin or plastic embedded sections for morphological analysis. Small samples such as needle core biopsies may be insufficient material for any additional investigations. However, if large enough, a whole fresh lymph node can be can be divided so that part of the specimen can be fixed for histological sections and part can be used fresh for other investigations. Fig. 24-3. Lymph node biopsy – H & E Stain The tissue sampled for paraffin blocks needs to be 3 mm thick. The tissue needs to be in fixative for 24-48 hours for adequate preservation of cytological detail. Prolonged fixation makes immunochemistry more difficult and recovery of DNA from paraffin blocks unreliable. A sample of fresh tissue should be rapidly frozen and stored for subsequent analysis if required such as DNA analysis. The use of paraffin embedding after decalcification alone is cheaper and is most suitable for DNA extraction, but plastic embedding gives improved morphology and can now be used with a wide variety of antibodies as well as for DNA based tests. Specimen preparation with hematoxylin and eosin (H&E) staining remains the gold standard for histologic interpretation of lymph node material. However, both serial sectioning and immunohistochemical staining for breast cancer or melanoma-associated tumor markers (e.g., the highly sensitive S-100 and the highly specific MART-1) facilitate the detection of metastatic tumor. Rapid immunohistochemistry aims to improve the accuracy of frozensection diagnoses. Rapid immunostaining of frozen sections may be possible using the enhanced polymer one-step staining (EPOS) system (Dako) with antibodies against leucocyte common antigen (LCA), cytokeratin (CK), and antimelanoma (MEL) after fixing samples in 100% acetone for 20 seconds (CK, LCA) or two minutes (MEL), followed by incubation of the primary antibody and development of the chromogen reaction with 3 3,' diaminobenzidine (DAB) for three and five minutes at 37°C, respectively. For rapid intraoperative diagnosis of lymph node micrometastasis, combining anti-cytokeratin antibodylabeled nano-crystal beads with rapid hematoxylin and eosin (H&E) staining on the same section, referred to as the rapid double staining (RDS) technique has also been reported. Special Studies A fresh sample of the specimen in tissue culture medium should be sent for optional cytogenetic analysis. Cells left for more than a few hours without being placed in culture medium will be unlikely to yield useful cytogenetic information. Tissue imprints should be made from all fresh biopsies so that they can be examined by targeted fluorescent in situ hybridization (FISH) if necessary. Cytogenetic analysis may not be necessary if H & E stained sections show reactive changes or evidence of metastatic disease. If the lymph node is fresh, make up to five imprints from the lymph node and preserve for FISH analysis where available. The imprints are initially air-dried. The dried imprint can then be fixed in chilled methanol-acetic acid (3:1) for 15– 30 minutes and stored at –20ºC in a desiccated chamber. Cytogenetic or FISH analysis should be used as adjuncts for the diagnosis of Burkitt’s lymphoma, but should not be requested as a routine investigation on all samples. Sections for FISH should be thinly sliced (2-4 microns). Protease digestion times will vary depending on the thickness of the section, so that additional sample subjected to longer protease digestion may need to be submitted if hybridization fails. The use of PCR for specific translocations such as t(14:18) and for detection of T cell receptor clonality and B cell clonality, based on T-cell receptor and immunoglobulin heavy and light chain gene rearrangement, are all important parts of the diagnostic study. No diagnostic material should be discarded until all investigations are complete. REFERENCES Ashton-Key M, Diss TC, Isaacson PG, Smith ME. (1995) A comparative study of the value of immunohistochemistry and the polymerase chain reaction in the diagnosis of follicular lymphoma. Histopathology, 27, 501-508. Association of Directors of Anatomic and Surgical Pathology (2001). ADASP recommendations for processing and reporting lymph node specimens submitted for evaluation of metastatic disease. Am J Surg Pathol 25:961-3. Bain BJ. (2001) Bone marrow trephine biopsy. J Clin Pathol, 54, 737-742. Bain BJ. (2001a) Bone marrow aspiration. Journal of Clinical Pathology 54, 657–663. Bain BJ, Clark DM, Lampert IA, Wilkins BS. (2001) Bone Marrow Pathology, 3rd ed. pp. 1–499. Blackwell Science, Oxford, UK. Bain BJ. (2006) Blood Cells: A Practical Guide. 4th ed. Hoboken, NJ: Wiley-Blackwell. Bainton DF, Farquhar MG. (1968) Differences in enzyme content of azurophil and specific granules of polymorphonuclear leucocytes. I. Histochemical staining of bone marrow smears. II. Cytochemistry and electron microscopy of bone marrow cells. Journal of Cell Biology 39: 286. Bancroft JD, Cook HC, eds. (1994) Manual of Histological Techniques and Their Diagnostic Application, pp. 1–457. Churchill Livingstone, London. Bauermeister DE. (1971) Quantitation of bone marrow reticulin – a normal range. American Journal of Clinical Pathology 56, 24–31. Beckstead JH, Halverson PS, Reis CA, Bainton DF. (1981) Enzyme histochemistry on and immunohistochemistry on biopsy specimens of pathologic human bone marrow. Blood 57:1088–98. Beckstead JH. (1994) A simple technique for preservation of fixation-sensitive antigens in paraffinembedded tissues. J Histochem Cytochem 42: 1127–34 Block M, Smaller V and Brown J. (1953) An adaptation of the Maximow technique for preparation of sections of hematopoietic tissues. Journal of Laboratory and Clinical Medicine 42: 145. Blythe D, Hand NM, Jackson P, Barrans SL, Bradbury RD, Jack AS. (1997) Use of methyl methacrylate resin for embedding bone marrow trephine biopsy specimens. J Clin Pathol, 50, 45-49. Bonds LA, Barnes P, Foucar K, et al. (2005) Acetic acid-zinc-formalin: a safe alternative to B-5 fixative. Am J Clin Pathol 124:205 – 211. Brown RS, Edwards J, Bartlett JW, et al. (2002) Routine acid decalcification of bone marrow samples can preserve DNA for FISH and CGH studies in metastatic prostate cancer. J Histochem Cytochem 50: 113–5. Brynes RK, McKenna RW, Sundberg RD. (1978) Bone marrow aspiration and trephine biopsy: an approach to a thorough study. American Journal of Clinical Pathology 70, 753–759. Burgio VL Magrini V, Ciardini L, Pezzoni G. (1984) An enzyme-histochemical approach to the study of the human bone marrow stroma. Acta Haematologica 71: 73. Burkhardt R, Frisch B, Bartl R. (1982) Bone biopsy in haematological disorders. J Clin Pathol, 35, 257284. Campbell JK. Matthews JP, Seymour JF, Wolf MM, Juneja SK. (2003) Optimum trephine length in the assessment of bone marrow involvement in patients with diffuse large cell lymphoma. Ann Oncol, 14, 273-276. Chilosi M, Lestani M, Pedron S, et al. (1994) A rapid immunostaining method for frozen sections. Biotech Histochem 69:235–9. Churukian CJ. (2009) Method of the histochemical stains and diagnostic application, Dept of Pathology and Lab Medicine, Univ of Rochester, NY, 2nd web edition. Clark G, ed. (1973) Staining Procedures, 3rd ed., Williams & Wilkins, Baltimore, pp. 131-132. Dancy JT, Denbelbeiss KA, Harker LA. (1976) Section preparation of human marrow for light microscopy. Journal of Clinical Pathology 76: 729. DePalma L. (1996) The effect of decalcification and choice of fixative on histiocytic iron in bone marrow core biopsies. Biotech Histochem 71: 57–60. Dunphy C, O’Malley D, Perkins S, et al. (2007) Analysis of immunohistochemical markers in bone marrow sections to evaluate for myelodysplastic syndromes and acute myeloid leukemias. Appl Immunohistochem Mol Morphol 15:154-159. Falini B, Martelli MF, Tarallo F, et al. ( 1984) Immunohistological analysis of human trephine biopsies using monoclonal antibodies. British Journal of Haematology 56: 365. Fleming MD, Kutok JL, Skarin AT. (2002) Examination of the bone marrow. In: Blood: Principles and Practice of Hematology (eds. R.I. Handin, S.E. Lux & T.P. Stossel), pp. 59–79. Lippincott Williams & Wilkins, Philadelphia, Gala JL, Chenut F, Hong KB, et al. (1997) A panel of antibodies for the immunostaining of Bouin’s fixed bone marrow trephine biopsies. J Clin Pathol 50:521–4 Gebhard S, Benhattar J, Bricod C, et al. (2001) Polymerase chain reaction in the diagnosis of T-cell lymphoma in paraffin-embedded bone marrow biopsies: a comparative study. Histopathology 38:37–44 Gomori G. (1937). Silver impregnation of reticulin in paraffin sections. Am J Clin Pathol 13: 993-1002. Fend F, Gschwendtner A, Gredler E, et al. (1994) Detection of monoclonal B-cell populations in decalcified, plastic-embedded bone marrow biopsies with the polymerase chain reaction. Am J Clin Pathol 102:850–5. Horny HP, Sotlar K, Valent P. (2007) Diagnostic value of histology and immunohistochemistry in myelodysplastic syndromes. Leuk Res 31:1609-1616. Fend F, Bock O, Kremer M, et al. (2005) Ancillary techniques in bone marrow pathology: molecular diagnostics on bone marrow trephine biopsies. Virchows Arch 447:909 –919. Horobin RW, Walter KJ. (1987) Understanding Romanowsky staining. Microscopica Acta. 79:153–156. Hoppe BR, Lassen ED. (1978) Blood Smears and the Use of Wright's Stain. Iowa State University Veterinarian 40(3): 113-116. Hoyer PE, Lyon H, Jakobsen P, et al. (1986) Standardized Methyl Green-Pyronin Y procedures using pure dyes. Histochemical Journal 18: 90. Huissen CH and Kuijpers EW. (1991) Quick cytochemical staining of blood and bone marrow cells in a microwave oven. Clinical and Laboratory Haematology 13: 197. Jatoi A, Dallal GE, Nguyen PL. (1999) False-negative rates of tumor metastases in the histologic examination of bone marrow. Modern Pathology 12, 29–32. Kaplow LS. (1965) Simplified Myeloperoxidase Stain Using Benzidine Dihydrochloride. Blood 26(2): 215-219. Kennedy A and Foulis AK. (1989) Use of microwave oven improves morphology and staining of cryostat sections. Journal of Clinical Pathology 42: 101. Klevesath MB, Bobrow LG, Pinder SE, Purushotham AD. (2005) The value of immunohistochemistry in sentinel lymph node histopathology in breast cancer. British Journal of Cancer (2005) 92, 2201– 2205. Kremer M, Quintanilla-Martinez L, Nahrig J, et al. (2005). Immunohistochemistry in bone marrow pathology: a useful adjunct for morphologic diagnosis. Virchows Arch 447:920–37. Krenacs T, Bagdi E, Stelkovics E, et al. (2005) How we process trephine biopsy specimens: epoxy resin embedded bone marrow biopsies. J Clin Pathol 58:897–903. Lan HY, Wei M, Nikolic-Paterson DJ, et al. (1995) A novel, simple, reliable and sensitive method for multiple immunoenzyme staining: use of microwave oven heating to block antibody crossreactivity and retrieve antigens. J Histochem Cytochem 43:97–102. Lee SH, Erbert WN, Portwit A, Toonagas M, Peterson LC. (2008) ICSH guidelines for the standardization of bone marrow specimens and reports. Blackwell Publishing Ltd, Int. Journal of Laboratory. Hematology. 30, 349–36. Lewis SM, Bain BJ, Bates I, eds. (2006) Practical Haematology, 10th ed, pp. 1–722. Churchill Livingstone, London. Lillie RD. (1977) H.J. Conn's Biological Stains, 9th edition, Williams and Wilkins. Lloyd RV, Schmidt K, Blaivas L, et al. (1985) A rapid immunostaining method utilizing preformed antibody–avidin–biotin–peroxidase complexes. Am J Clin Pathol 83: 636–9. Luna LG, ed. (1968) Manual of Histologic Staining Methods of the Armed Forces Institute of Pathology, 3rd ed. McGraw-Hill, New York, pp212-122. Masson PJ. (1929) Some histological methods. Trichrome stainings and their preliminary technique. J. Tech. Methods 12:75-90, 1929 McCluggage WG, Roddy S, Whiteside C, et al. (1995) Immunohistochemical staining of plastic embedded bone marrow trephine biopsy specimens after microwave heating. J Clin Pathol 48: 840–4 Milan L, Trachtenberg MC. (1981) Ultrasonic decalcification of bone. Am J Surg Pathol 5: 573–9. Mullink H, Henzen-Logmans SC, Tadema TM, et al. (1985) Influence of fixation and decalcification on the immunohistochemical staining of cell-specific markers in paraffin-embedded human bone biopsies. J Histochem Cytochem 33:1103–94. Nagasaka T, Lai R, Chen YY, et al. (2000) The use of archival bone marrow specimens in detecting Bcell non-Hodgkin’s lymphomas using polymerase chain reaction methods. Leuk Lymphoma 36:347–52 Peterson LC, Agosti SJ, Hoyer JD. (2002) Protocol for the examination of specimens from patients with hematopoietic neoplasms of the bone marrow: a basis for checklists. Archives of Pathology and Laboratory Medicine 126, 1050–1056. Peterson LC, Brunning RD. (2001) Bone marrow specimen processing. In: Neoplastic Hematopathology (ed. D. Knowles), pp. 1391–1405. Lippincott Williams & Wilkins, Philadelphia, PA. Pujara KM, Bhalara RV, Dhruva GA. (2014) A study of bone marrow iron storage in hematological disorder. Int J Health Allied Sci 3:221-4. Richter T, Nährig J, Komminoth P, Kowolik J, Werner M. (1999) Protocol for ultrarapid immunostaining of frozen sections. J Clin Pathol 52:461–463. Strauchen JA. (1984) Lectin receptors as markers of lymphoid cells. I. Demonstration in tissue sections by peroxidase technique. American Journal of Pathology 116: 297. Stuart-Smith SE, Hughes DA, Bain BJ. (2005) Are routine iron stains on bone marrow trephine biopsy specimens necessary? J Clin Pathol 58:269–72. Toda H, Minamiya Y, Kagaya M, Nanjo H, Akagami Y, Saito H, Ito M, Konno H, Motoyama S, Ogawa J. (2011) A Novel Immunohistochemical Staining Method Allows Ultrarapid Detection of Lymph Node Micrometastases While Conserving Antibody. Acta Histochemica et Cytochemica. 44(3) 133-139. Toth B, Wehrmann M, Kaiserling E, et al. (1999) Immunophenotyping of acute lymphoblastic leukaemia in routinely processed bone marrow biopsy specimens. J Clin Pathol 52:688–92. Tsutsumi Y, Serizawa A, Kawai K. (1995). Enhanced polymer one step staining (EPOS) for proliferating cell nuclear antigen (PCNA) and Ki-67 antigen: application to intraoperative frozen diagnosis. Pathol Int 45:108–11 Van Zee KJ, et.al. (2003) "A Nomogram for Predicting the likelihood of Additional Nodal Metastasis in Breast Cancer Patients with a Positive Sentinel Node Biopsy", Ann Surg Oncol 10(10):1140-1151. Veronesi U, Paganelli G, Galimberti V, et al. (1997) Sentinel-node biopsy to avoid axillary dissection in breast cancer with clinically negative lymph-nodes. Lancet 349: 1864–7. Vincic L, Weston S, Riddell RH. (1989) Bone core biopsies. Plastic or paraffin? Am J Surg Pathol, 13, 329- 334. Weaver DL. (2010) Pathology evaluation of sentinel lymph nodes in breast cancer: protocol recommendations and rationale). Modern Pathology 23, S26–S32 Weiss DJ. (1987) A review of the techniques for preparation of histopathologic sections of bone marrow. Vet Clin Pathol 16:90–94. Werner M, Kaloutsi V, Walter K, et al. (1992) Immunohistochemical examination of routinely processed bone marrow biopsies. Pathol Res Pract 188:707–13 Wester K, Asplund A, Backvall H, et al. (2003) Zinc-based fixative improves preservation of genomic DNA and proteins in histoprocessing of human tissues. Lab Invest 83:889–99 Wickham CL, Sarsfield P, Joyner MV, et al. (2000) Formic acid decalcification of bone marrow trephines degrades DNA: alternative use of EDTA allows the amplification and sequencing of relatively long PCR products. Mol Pathol 53:336 Woronzoff-Dashkoff KK. (2003) The Wright–Giemsa stain. Secrets revealed. Clinics in Laboratory Medicine 22, 15– 23. CHAPTER 25 STAINING OF CONNECTIVE TISSUE Connective tissue constitutes a non-living framework within the various organs, and is made up of various cell components that are found in between other tissues everywhere in the body. It is one of the four types of biological tissue that support, connect, or separate different types of tissues and organs in the body. The other three types are epithelial, muscle, and nervous tissue. Organs represent various combinations of these four basic tissue types, which thus comprise the entire body. Each tissue type retains its connective tissue forms a framework upon which epithelial tissue rests and within which nerve tissue and muscle tissue are embedded. In the central nervous system the outer membranes, the meninges that cover the brain and spinal cord are composed of connective tissue. Blood vessels and nerves travel through connective tissue. The individual bones of the skeleton are held firmly together by ligaments, and muscles are attached to bone by tendons, both of which are examples of dense connective tissue in which many fiber bundles are associated in parallel array to provide great tensile strength. The most common connective tissue cells are fibroblasts (which secrete collagen and other elements of the extracellular matrix), adipocytes (mesenchymal cells which store fat) mast cells, macrophages and lymphocytes (cells with immune function which participate in inflammation). Connective tissue matrix has a ground substance, consisting of water that is stabilized by and fibers stabilized by glycosaminoglycans, proteoglycans, and glycoproteins. In some areas, the connective tissue is loosely organized and highly cellular; in others, its fibrous components predominate; and in still others, the ground substance may be its most conspicuous feature. The anatomical classification of the various types of connective tissue is based largely upon the relative abundance and arrangement of these components. Individual connective tissue cells are normally separated from one another by varying amounts of extracellular matrix. 1. Loose connective tissue connects the epithelial surfaces to the underlying structures and permits free passage of nutrients. It appears as a loose network of numerous bundles of collagenous fibers with some elastic and reticular fibers, admixed with fibroblasts, and small 2. 3. 4. 5. blood vessels as well as lymphatic vessel. One very specific type of loose connective tissue is the basement membrane, which is the welldefined layer of extracellular matrix that serves as a base for epithelial tissues. Adipose tissue is derived from areolar tissue, made up mostly fat cells surrounded by a well-developed network of reticular fibers, and is associated with some capillaries and lymphatic vessels. Adipose or fat cells are connective-tissue cells that receive glucose and fatty acids from the blood and convert them to lipid, which accumulates in the body of the cell as a large oil droplet. This distends the cell and imposes upon it a spherical form. The nucleus is displaced to the periphery, and other metabolically active constituents of the cell are confined to a thin rim of cytoplasm around the large central droplet of lipid. Where they accumulate in such large numbers that they become the predominant cellular element, they constitute the fat or adipose tissue of the body. Dense connective tissue is made up of organized, dense masses of collagenous fibers and fibroblasts that are oriented in the same direction, as seen in the tendons and ligaments that support and connect skeletal muscles to the skeleton because of their tensile strength. The ubiquitous fibroblasts are the principal active cells of connective tissue, occurring as long spindle-shaped cells stretched along bundles of collagen fibrils. When organs are injured, cells known as fibrocytes, which reside in the stroma, are stimulated to develop into fibroblasts. The fibroblasts then migrate into the defect and deposit an abundance of new collagen, known as dense connective tissue that forms a fibrous scar. Cartilage is a fairly dense network of collagenous fibers encased in or mixed with an amorphous or homogenous intercellular substance of chondroitin sulfate. It has abundant ground substance and a consistency of gel that makes the tissue rigid and resistant to compression. The cells of cartilage, called chondrocytes, are isolated in small lacunae within the matrix. Cartilage is enclosed by the perichondrium, a dense fibrous layer lined by cells that have the capacity to secrete hyaline matrix. The cartilaginous skeletal elements present in fetal life are subsequently replaced by bone. Cartilage develops from mesenchymal cells that differentiate into chondroblasts, mature into chondrocytes, and lay down intercellular substance. Bone tissue is a type of mineralized connective tissue that contains collagen and calcium phosphate, a mineral crystal. Bone tissue itself is mostly extracellular material composed of a hard, mineralized form of calcium phosphate. Interspersed within the hard extracellular component of bone are osteocytes which are mature bone cells. Osteocytes are the cells which secrete the calcium phosphate that hardens and forms the bones. Calcium phosphate gives bone its firmness. 6. Reticulin (Reticular Connective Tissue) made up of reticular fibers are distinguished by their tendency to form fine-meshed networks around cells and cell groups and by virtue of their property of staining black, because of adsorption of metallic silver, when they are treated with alkaline solutions of reducible silver salts. Reticulin is made up of extracellular delicate fine branching fibers. They are usually not visible in routine hematoxylin-eosin staining method. The reticulin fibers are argyrophylic and therefore are best stained by silver impregnation technique. They may have a faint pinkish color with van Gieson's stain. Periodic Acid Schiff (PAS) also stains reticulin purplish red. This is not, however, a satisfactory stain due to the delicate nature of the reticulum fibers. 7. Elastic Tissue is present in the skin, ligaments, aorta, arterial elastic lamina, and lung. Elastic fibers are composed of the protein elastin that are highly distensible and, when broken, recoil like rubber bands. The elastin that is found in the walls of arteries withstands the hemodynamic stresses that the flow of blood imposes on the artery wall. They are, in part, responsible for the loss of elasticity of the skin and of the bloodvessel walls in old age. They are made up of fine, intertwining wavy filaments that are insoluble in organic and inorganic solvents (unlike collagen that is soluble in 2% acetic acid). They are extremely resistant to hot water, to strong alkali, and even to digestion with the proteolytic enzyme trypsin. They can be digested, however, by a specific enzyme, elastase, present in the pancreas. 8. Blood Plasma is the watery component that serves as the matrix of blood containing many dissolved substances, such as proteins, glucose, mineral ions, hormones, carbon dioxide. The cells found within this matrix are red and white blood cells, as well as platelets. Plasma, which constitutes 55% of blood fluid, is mostly water (92% by volume) is the main medium for excretory product transportation), and blood cells themselves. Reticulin Stain Silver impregnation techniques for staining of reticulin depend on local reduction and selective precipitation of silver by the carbohydrate aldehyde groups of reticulin. Most are prepared by producing a precipitate from silver nitrate with sodium, potassium, or ammonium hydroxide or with lithium or sodium carbonate. Ammoniacal solution of silver carbonate is reduced by reticulin to dark brown silver oxide which is precipitated on the fibers, and then reduced to black metallic silver by formalin. Unreduced silver is removed by sodium thiosulfate solution. Toning with yellow gold chloride is a valuable step in removing the yellowish discoloration in the background caused by colloidal metallic silver, which is replaced with gold chloride. Toning gives a very pale gray background, which is better for photography and which also improves subsequent counterstaining. Reticular fibers are commonly demonstrated by the use of stains involving silver solutions. These stains rely on the impregnation of silver ions to the fibers and subsequent reduction of those silver ions to their visible metallic form. Reticular fibers are argyrophilic in that they possess the ability to adsorb silver from solution but are unable to reduce it to visible metallic form without the use of a reducing solution to drive the reaction. Demonstration of reticular fibers generally employs an ammoniacal silver solution as a source of silver ions. An ammoniacal silver solution consists of a strong base (ammonium hydroxide) added to an aqueous silver nitrate solution to form a silver diamine complex. This method commonly calls for oxidation and sensitization of tissue prior to application of this complex. Oxidation (potassium permanganate/periodic acid) enhances subsequent staining, while the sensitizing agent (uranyl nitrate/dilute silver nitrate) initially binds to the tissue component of interest. Silver ions provided by the ammoniacal silver solution impregnate the fibers and replace the sensitizer in the metal-organic compound. Subsequently, by the action of a reducing agent (formalin), the silver diamine complex is reduced to visible metallic form. Metallic silver is converted by use of a toning reagent (gold chloride) to metallic gold, which is more stable and offers better contrast and clarity. Unreduced silver and excess gold chloride are removed (sodium thiosulfate), and the tissue section is then counterstained, if desired. Nuclear fast red or light green counterstains are commonly used. Gomori's Silver Impregnation Stain for Reticulin (Gomori 1937, Suvarna 2013, Luna 1986) Reticulin stains are silver stains based on the argyrophilic properties of reticulin fibers. Reticulin fibres have little natural affinity for silver solutions so, they must be treated with a suitable solution, (2.5% iron alum) and potassium permanganate to sensitize areas within the fibres where silver deposition can be initiated. The silver is in a form readily able to precipitate as metallic silver (diamine silver solution). The optimal pH for maximum uptake of silver ions is pH 9.0. A reducing agent, formalin, causes deposition of silver in the form of metal. Any excess silver in the unprecipitated state is removed by treating with sodium thiosulfate solution. “Toning” with gold chloride renders the preparation permanent by replacing silver metal with metallic gold and changes the color of reticulin fibers from brown to black. The two most common reticulin stains are the Gomori’s stain and Gordon & Sweet’s stain. Fixation: Formalin Preparation of Solution: 1. Add 4 to 5 ml. of 10% potassium hydroxide to 20 ml. of 10% silver nitrate solution. Mark the fluid level on the flask and pour off the supernatant. 2. Wash the precipitated silver with distilled water once or twice until the water is quite clear, and fill up to the fluid level with fresh distilled water. This step will result in a cleaner background. 3. With continuous shaking, add 28% ammonia water, drop by drop, until the precipitate is all dissolved. 4. Carefully add 10% silver nitrate solution, drop by drop, until the precipitate that forms easily disappears on shaking. 5. Make the solution up to twice its volume with distilled water; i.e., add an equal volume of water. 6. If stored in a well-stoppered bottle in the dark, the solution may be used for 2 days. Method: 1. Bring paraffin sections of formalin-fixed material down to water. 2. Oxidize in 0.5% aqueous potassium permanganate for 1 to 2 minutes. 3. Rinse in tap water for 2 minutes. 4. Place in 2% aqueous potassium metabisulfite for 1 minute, or until colorless. 5. Wash in tap water for 2 to 5 minutes. 6. Place in 2% aqueous ferric ammonium sulfate for 1 minute to sensitize. 7. Wash in tap water for 2 minutes and then for 30 seconds in each of two changes of distilled water. 8. Allow impregnation in the silver solution for 1 minute. 9. Rinse in distilled water for 20 seconds. 10. Reduce for 3 minutes in 20% formalin (10 ml. formaldehyde with 40 ml. distilled water). 11. Wash in tap water for 3 minutes. 12. Tone in 0.2 gold chloride solution for 10 minutes. 13. Rinse in distilled water. 14. Place in 2% aqueous potassium metabisulfite for 1 minute to reduce toning. 15. Fix in 2% aqueous sodium thiosulfate (hypo) for 1 minute. 16. Wash in tap water for 2 minutes. 17. Dehydrate, clear, and mount. Results: Reticulin fibers black Note: All ammoniacal silver solutions must be prepared fresh, to avoid formation of explosive silver compounds with aging. All glassware used, especially before and for the silver bath and for the preparation of the silver solutions, must be thoroughly washed with nitric acid and then rinsed in several changes of distilled water. The forceps used for handling slide during processing should be nonmetallic, i.e., plastic, until after the sodium thiosulfite stage, to prevent the nonspecific precipitation of silver on the slide. Washing of the sections with distilled water must be thorough, especially before impregnation. Dust (not light) is the greatest single factor that causes deterioration and precipitation of silver solutions, and therefore must be avoided. Avoid splashing or using glass rods without careful washing between solutions. Use glass-distilled water to avoid precipitating silver. Mount the paraffin sections well to an albuminized slide and thoroughly dry before staining the section, to prevent detaching them from the slides due to the high alkalinity of the silver solutions. Inactivate any unused solution by adding excess of sodium chloride solution or of dilute hydrochloric acid. Ensure that both the ammonium hydroxide and potassium hydroxide are fresh and full strength. Keep both well stoppered when not in use. Ammoniacal silver solutions can be explosive when allowed to dry. Immediately after use neutralize the silver solution with saturated sodium chloride and discard. For the ammonium hydroxide, pour sufficient for use from the stock bottle into a beaker, then immediately re-stopper the stock bottle. Do not return excess ammonium hydroxide to the stock bottle. After making the ammoniacal silver solution, smell the solution to ensure it has only a faint smell of ammonia. If the smell of ammonia is strong it indicates that too much ammonium hydroxide has been adde d. If so, it is preferable to make the solution again. Improperly made ammoniacal silver solutions can affect the quality of the impregnation. Untoned sections give dark brown reticulin fibres on a paler brown background. Toning for about 15 seconds to produce brown-black reticulin fibres on a pale grey-brown background. The staining solution (silver nitrate, potassium hydroxide, and ammonia water) should be carefully prepared to avoid having silver precipitate. Clean glassware (used for preparing silver solution) with glassware cleaning solution. Wash thoroughly before use with tap water and use distilled water for the final rinse. It is important not to over dissolve the precipitate at any stage as this will result in a decrease in sensitivity Silver nitrate crystals stored at room temperature will gradually take on a grayish-violet color. This does not occur when silver nitrate is kept refrigerated, even after several years. Fig. 25-1. Reticulin stain of liver biopsy showing the fine interlobular septae Reticulin Stain -Gordon and Sweets’ Method (1936) (Suvarna 2013, Carson 2009) In this method, the tissue is oxidized by potassium permanganate to enhance subsequent staining of reticular fibers. The excess permanganate solution is removed by oxalic acid. The iron alum serves as sensitizer and is subsequently replaced by silver solution to form silver oxide. Silver from silver oxides is selectively deposited on the reticulin fibres, which appear black after conversion to reduced silver, by the reducing agent (formalin). Gold chloride is used as a toner to give a clearer background and unreduced silver is removed by treatment with sodium thiosulphate. Specimen: Standard paraffin sections Fixation: 10% neutral buffered formalin Reagents: (A) Silver Solution: To 5mL of 10% Silver nitrate solution add strong ammonia until the precipitate formed is just dissolved. Avoid excess of ammonia. Add 5mL of 3% Sodium hydroxide solution. Re-dissolve the precipitate by adding strong ammonia drop by drop until the resultant solution retains a faint opalescence. If at this stage any excess ammonia is present, indicated by the absence of opalescence, add a few drops of 10% silver nitrate solution to produce a light precipitate. Make up to 50 mL with distilled water. Store in a dark bottle at 4øC - keeps 3 months. Filter before use (approximately 2 mL per slide). Note: All glassware should be rinsed in distilled water and dried before use. (B) Acidified Potassium Permanganate 0.5% Potassium permanganate 190 mL 3% Sulphuric acid 10 mL (C) 1 % Oxalic Acid (D) 4 % Iron alum (Ammonium Ferric Sulphate) (E) 10 % Formalin (not buffered) - dilute in tap water not distilled (F) 0.2 % Gold Chloride (Sodium Chloro-aurate) (G) 5 % Sodium Thiosulfate (H) 1 % Neutral Red (C.I. 50040) Procedure: 1. Deparaffinize and hydrate to distilled water 2. Acidified potassium permanganate 2 min 3. Wash in water 4. 1 % Oxalic acid 2 min 5. Wash well in distilled water 6. 4 % Iron alum 10 min 7. Wash in distilled water 8. Silver solution (filter 2mLs per slide) 1 min 9. Rinse in distilled water 10. 10 % Formalin 2 min 11. Wash in water followed by distilled water 12. 0.2 % Gold chloride 2 min 13. Rinse in distilled water 14. 5 % (Sodium thiosulphate) 2 min 15. Wash in water 16. Counterstain with 1 % Neutral Red 2 min 17. Dehydrate rapidly, clear and mount Note: Dehydrate rapidly as the neutral red counterstain is removed in alcohol. Use PLASTIC forceps, not metal. Results: Reticulin fibers Black Nuclei Black Background Red COLLAGEN Collagen forms a coarser extracellular framework than reticulin. Collagenous fibers are found in ligaments, tendons, cartilage and bone. Its doubly refractile, coarse connective tissue fibers stain yellow, lavender or brown on silver impregnation, and red with van Gieson 's stain. Collagen and most reticulin fibers stain selectively with acid aniline dyes (aniline blue, acid fuchsin, methyl blue or indigo carmine) from fairly strong acid solutions. The most commonly used acid is picric acid, which also acts as a counterstain for muscle and cytoplasm. Collagen may be differentially stained by any of the following techniques: 1. Van Gieson's stain 2. Masson's Trichrome stain 3. Mallory's Aniline Blue stain 4. Azocarmine stain 5. Krajian's Aniline Blue stain Van Gieson's Stain for Collagen (Carson 2009) Van Gieson's Stain is the simplest method of differential staining of collagen and other connective tissue that uses a mixture of picric acid and acid fuchsin. In van Gieson stained preparations collagen stains dark red while other tissue components appear in varying shades of grey (nuclei) and yellow (cytoplasm). Areas of dense regular connective tissue are usually easy to identify in these preparations. Coarse collagen fibers are aligned with each other with only very narrow opens spaces between them. Like in most other connective tissues, there will be only a few cells between the fibers. Their cytoplasm is difficult to identify but the nuclei can be seen scattered among the collagen fibers. Nuclei are often elongated, and their long axis runs parallel to the course of the collagen fibers. Fixation: Mercuric chloride fixative, although formol-saline also gives good results. Solution: Saturated aqueous picric acid 95 ml. 1 % acid fuchsin 5 ml This may be kept as a stock solution, but a freshly prepared solution of 10 ml. saturated aqueous picric acid and 1.5 ml. of 1 % acid fuchsin may give better staining quality. Method: 1. Sections to alcohol. 2. Stain with Weigert's iron hematoxylin for 15 minutes. 3. Wash in running water for 15 minutes. 4. Rinse with distilled water. 5. Place in Van Gieson's stain for 5 minutes. 6. Rinse in distilled water. a. Rinse rapidly in 70% alcohol. b. Dehydrate rapidly in absolute alcohol, clear and mount in neutral balsam. Acid medium, if used for mounting, will make stains fade rapidly. Results: Nuclei brownish black to black Collagen (fibrous connective tissue) pink or deep red Muscle, Cytoplasm, RBC and Fibrin Yellow Notes: 1. If the duration of staining is strictly followed, there is no need to differentiate in 1% acid alcohol. The sections are instead, differentiated by picric acid in the Van Gieson Stain. 2. Differentiation of collagen and smooth muscles may be accomplished in steps 5 and 6. Van Gieson's stain consists of acid fuchsin (readily soluble in alcohol) and picric acid (readily soluble in water). Washing with appropriate solvent will accentuate one and remove the other. 3. Nuclei are stained with alum hematoxylin, but are readily decolorized by picric acid. Iron hematoxylin may be used. 4. Young fibrils do not take the deep red stain imparted to mature collagen. Masson's Trichrome Stain (Luna 1968, Sheehan 1980) This is often used to stain connective tissue. Trichrome - means the technique produces three colors. Nuclei and other basophilic structures are stained blue, cytoplasm, muscle, erythrocytes and keratin are stained bright-red. Collagen is stained green or blue, depending on which variant of the technique is used. Masson 's trichrome stain uses dyes in acid solution involving nuclear staining with iron hematoxylin, followed by cytoplasmic staining with a red dye (e.g., Ponceau phosphotungstic acid, phosphomolydic acid or both, and fixed staining of fibers with a blue or green stain (e.g. aniline blue or light green). With the Masson’s trichrome stain Bouin’s solution is used initially as a mordant to link the dye molecules to the tissue components of interest. Nuclei are stained with Weigert’s hematoxylin, an iron hematoxylin, which is resistant to decolorization by subsequent acidic staining solutions. Application of Biebrich-scarlet-acid-fuchsin stains all acidophilic tissue elements such as cytoplasm, muscle and collagen. Subsequent treatment by phosphomolybdic/ phosphotungstic acid serves as a decolorizer causing the Biebrich-scarlet-acidfuchsin to diffuse out of the collagen fibers while leaving the muscle cells red. Subsequent application of aniline blue or methyl blue will stain the collagen after which, 1% acetic acid is employed to properly differentiate the tissue section. The Masson’s trichrome stain consists of sequential staining with iron hematoxylin which stains nuclei black; Biebrich scarlet which stain cytoplasm including muscle red and aniline blue or aniline light green which stain collagen blue or green respectively. The classic nuclear stain for the trichrome technique is either Weigert’s or Heidenhain’s iron hematoxylin. Unlike aluminum-based hematoxylins, the iron hematoxylin is more resistant and therefore is not decolorized by the subsequent acid staining solutions. Mercuric chloride or picric acid fixation (Bouin’s solution) gives best results. If tissue was fixed in neutral buffered formalin, staining is enhanced by using Bouin's fluid as a mordant. Fixation: Zenker, Helly, Bouin's and formol sublimate solutions are strongly recommended. Formalin-fixed sections should be premordanted in Bouin's fluid for 1 hour at 56°C or overnight at room temperature prior to staining. Sections: Paraffin sections. Solutions: Solution A Acid fuchsin 0.5 gm. Glacial acetic acid 0.5 ml. Distilled water 100 ml. Solution B Phosphomolybdic acid 1.0 gm. Distilled water 100 ml. Solution C Methyl blue 2.0 gm. Glacial acetic acid 2.5 ml. Distilled water 100 ml. Method: 1. Sections to water. 2. Wash until the yellow color (from Bouin's) is gone, or remove mercury deposits with iodine-thiosulfate sequence, as i ndicated. 3. Stain the nuclei either with Weigert's iron hematoxylin for 10 to 30 minutes 4. Wash in water. 5. Differentiate the nuclear stain with 1 % acid alcohol. 6. Wash in running tap water for 10 minutes until bl ue . 7. Rinse in distilled water. 8. Stain with acid fuchsin solution (A) for 5-10 minutes. 9. Rinse in distilled water. 10. Treat with phosphomolybdic acid mordant (B) for 5 minutes or until collagen is decolorized, and only muscle, RBC and fibrin remain. Discard acid solutions after use. 11. Rinse in distilled water. 12. Counterstain in methyl blue solution (C) for 5 to 10 minutes. 13. Wash well in 1% acetic acid for 1 to 3 minutes. 14. Blot, dehydrate in absolute alcohol, clear and mount. Results: Muscle, RBC and keratin red Nuclei blue-black Collagen and mucus blue Notes: • Fixing the tissue with 10% neutral buffered formalin will not yield optimal trichrome staining results. The longer those tissues remain in formalin fixatives, the less effective the staining will be. After formalin fixation, mordanting the tissue sections with a picric acid solution such as Bouin’s will enhance the trichrome staining intensity. The recommended fixatives for trichrome staining are Bouin’s, Zenker’s, Formal-mercury, Zinc formalin and Picro-mercuric alcohol. • In order to achieve both adequate and even staining of connective tissue fibers the dyes utilized in the trichrome techniques are prepared as low pH solutions, usually in the range of 1.5 - 3.0. Fig. 25-2. Masson Trichrome stain showing fibrosis in a muscle biopsy GOMORI'S ONE-STEP TRICHROME STAIN (Gomori 1950b, Sheehan 1980) The Gomori’s One-Step method is a one-step method where a plasma stain (chromotrope 2R) and a connective tissue fiber stain (fast green FCF, light green, or aniline blue) are combined in a solution of phosphotungstic acid to which glacial acetic acid has been added. Phosphotungstic acid favors the red staining of muscle and cytoplasm. The tungstate ion is specifically taken up by collagen, and the connective tissue fiber stain is subsequently bound to this complex. Specimen: Standard paraffin section of well-fixed tissue or alcohol-fixed smear. Fixative: Bouin’s Solution - Preheated to 56 -60oC. Solutions: Weigert’s Iron Hematoxylin Working Solution Gomori’s Trichrome Stain Chromotrope 2R 0.6 g Light green CI 42095 0.3 g Glacial acetic acid 1.0 mL Phosphotungstic acid 0.8 g Distilled water 100 mL 1% Glacial Acetic Acid Solution Procedure: 1. Deparaffinize and hydrate to distilled water. 2. Place in Bouin's fixative in oven at 56øC for one hour. 3. Wash well in running water until sections are clear. 4. Stain in Weigert's iron haematoxylin working solution for 10 minutes. 5. Rinse in tap water. 6. Stain in Gomori's trichrome stain for 15 to 20 minutes. 7. Rinse in 1% acetic acid (or use acid-alcohol in linear stainer). 8. Rinse in distilled water. 9. Dehydrate and clear in 95% ethyl alcohol, absolute ethyl alcohol and xylene, 2 changes each, for 2 minutes each. 10. Mount with safety-mount. Results: Muscle fibers red Collagen green Nuclei blue to green Notes: Gomori's chromium haematoxylin may be substituted for the Weigert's iron haematoxylin Aniline blue can be substituted for the light green. Slides may be left in Bouin's solution overnight at room temperature. If sections are too red, differentiate in 100 mL of 1% acetic acid to which 0.7 g of phosphotungstic acid has been added. Russell’s modification of the Movat pentachrome stain (Movat 1955, Luna 1992) PRINCIPLE: Acidic mucosubstances are stained by alcian blue. The alkaline alcohol solution that follows converts the alcian blue to monastral fast blue, which is insoluble. Complete conversion is necessary because alcian blue will be decolorized during the remainder of the procedure. Iron hematoxylin is used to stain the elastic fibers, which are then differentiated with ferric chloride (see the Verhoeff method). Sodium thiosulfate removes any residual iodine. Crocein scarlet and acid fuchsin are acid dyes that stain muscle, cell cytoplasm, collagen, and ground substance. Phosphotungstic acid differentiation removes the stain from the collagen and ground substance. The acetic acid removes the phosphotungstic acid, and collagen is then counterstained with alcoholic safran. Fixative 10% neutral buffered formalin is preferred. Sections: Cut paraffin sections at 4 - 5 μm. Reagents Alcian blue, 1% solution Alcian blue-GS 1 g Distilled water 100 ml Glacial acetic acid 1 ml Mix well and store at room temperature. Alkaline alcohol solution Ammonium hydroxide 10 ml Alcohol, 95% 90 ml Prepare fresh. Iodine-iodide solution Iodine 2 g Potassium iodide 4 g Distilled water 100 ml Add the iodine and potassium iodide to ~25 mL of water and mix until dissolved. Add the remaining water. Absolute alcoholic hematoxylin, 10% solution Hematoxylin 10 g Absolute alcohol 100 ml Mix until dissolved. Cap tightly and store at room temperature. Ferric chloride, 10% solution Ferric chloride 10 g Distilled water 100 ml Mix until dissolved and store at room temperature. Working hematoxylin solution Absolute alcoholic hematoxylin 10% 25 ml Absolute alcohol 25 ml Ferric chloride, 10% aqueous 25 ml Iodine-iodide solution 25 ml Prepare just before use. Ferric chloride, 2% (for differentiation) Ferric chloride, 10% solution 10 ml Distilled water 40 ml Prepare just before use. Sodium thiosulfate, 5% solution Sodium thiosulfate 5 g Distilled water 100 ml Mix until dissolved and store at room temperature. Crocein scarlet-acid fuchsin solution Solution A (stock) Crocein scarlet 1 gm Distilled water 99.5 ml Glacial acetic acid 0.5 ml Mix until dissolved and store at room temperature. Solution B (stock) Acid fuchsin 0.1 g Distilled water 99.5 ml Glacial acetic acid 0.5 ml Mix until dissolved, and store at room temperature. Working solution Solution A 40 ml Solution B 10 ml Prepare just before use. Phosphotungstic acid, 5% solution Phosphotungstic acid 5 g Distilled water 100 ml Mix until dissolved and store at room temperature. Alcoholic safran solution Safran du Gatinais 6 g Absolute alcohol 100 ml Place in an air-tight container, and mix well. Keep at 56°C58°C for 48 hours, and keep tightly closed in a brown bottle to prevent hydration or evaporation. Procedure: 1. Deparaffinize and hydrate to distilled water 2. Stain in alcian blue for 20 minutes 3. Wash in running tap water for 5 minutes 4. Place slides in alkaline alcohol for 30 minutes 5. Wash in running tap water for 10 minutes 6. Rinse in distilled water 7. Stain in working hematoxylin solution for 15 minutes 8. Rinse in several changes of distilled water 9. Differentiate in 2% aqueous ferric chloride until the elastic fibers contrast sharply with the background 10. Rinse in distilled water 11. Place slides in sodium thiosulfate for 1 minute 12. Wash in running tap water for 5 minutes; rinse in distilled water 13. Stain in Crocein scarlet-acid fuchsin solution for 1 minute 14. Rinse in several changes of distilled water 15. Rinse in 0.5% acetic acid solution for 30 seconds 16. Place slides in 5% phosphotungstic acid solution, 2 changes of 5 minutes each 17. Rinse in 0.5% acetic acid solution 18. Rinse in 3 changes of absolute alcohol 19. Stain in alcoholic safran solution for 15 minutes 20. Rinse in 3 changes of absolute alcohol 21. Clear in 2 or 3 changes of xylene and mount with synthetic resin Results: Nuclei and elastic fibers Black Collagen Yellow Ground substance and mucin Blue Fibrinoid, fibrin Intense red Muscle Red Fig. 25-3. Movat Pentachrome Stain Mallory's Aniline Blue Stain (Luna 1968, Rowley Bio.com) Several modifications of the original method have been developed. It is often used to differentiate acidophilic extracellular fibers from acidophilic cytoplasm. Basic ingredients are acid fuchsin, aniline blue, orange G and phosphotungstic acid. Collagen and reticular fibers stain blue; nuclei and smooth muscle stain red; elastic fibers stain pink; red blood cells and myelin stain orange. Modified Mallory's aniline blue stain is not absolutely differential because in addition to collagen fibers and reticulum, it also stains hyaline fibrils, fibroglia fibrils, smooth and striated muscle fibers and amyloid. To bring out the collagen fibrils as sharply as possible, omit the staining with acid fuchsin. Then the nuclei and cytoplasm will stain yellow, and the blue fibrils and reticulum will stand out more prominently. This is an excellent and colorful method of demonstrating connective tissue fibers. Fixation: Zenker’s (F-155A +F-155B) Sections: 6 µm paraffin Method: 1. Deparaffinize and hydrate to distilled water. 2. Place in Lugol’s Iodine for 15 minutes. Rinse in tap water. 3. Place in 5% Sodium Thiosulfate for 3 minutes. Wash in tap water for 10 minutes or longer. Rinse in distilled water. 4. Acid Fuchsin Solution for 1 to 5 minutes. Standing with Acid Fuchsin Solution may be omitted if it is desired that collagen fibers stand out more sharply. 5. Transfer directly to Anilne Blue-Orange G Solution for 30 to 60 minutes or longer. 6. Dehydrate in 95% alcohol, absolute alcohol, and clear in Xylene, two changes each. 7. Mount with Permount. Results: Nuclei, fibrin, muscle fibers red Collagen blue Cartilage, bone, mucus varying shades of blue Blood, myelin yellow Elastic fibers pale pink/yellow or unstained Azocarmine Stain This is Heidenhain's modification of Mallory's aniline blue stain, using azocarmine dye for counterstaining. It is a valuable stain showing minute details of connective tissue and of renal glomerular basement membrane as well. Amyloid connective tissues and mucous colloid will take the deep blue stain. Nuclei are colored red. Elastic Stain Elastic fibers are composed of the protein elastin and offer the greatest flexibility among the fiber types. Elastic fibers allow tissue to stretch and are located in the skin and walls of blood vessels. The presence of elastic tissue is recognized in acid-treated fresh preparations by a refractile appearance in contrast to the swollen glassy form of collagen. Elastic tissue is isotropic and gives a yellowish fluorescence in ultraviolet light (blue if unstained). In the presence of ferric salts (oxidizers), elastic fibers stain with basic fuchsin, with or without resorcin. From acidic solutions, the fibers are stained selectively by the weak acid orcein. Among the common staining methods used for elastic fibers are the following: 1. Weigert's Elastic Tissue stain 2. Taenzer-Unna Orcein method 3. Verhoeff 's stain 4. Gomori 's Aldehyde-Fuchsin stain 5. Krajian 's method Weigert's Resorcin-Fuchsin Elastic Tissue Stain (Weigert 1898, Suvarna 2013) The tissue is placed in Weigert's stain, made up of basic fuchsin, resorcin and ferric chloride, differentiated with acid-alcohol, and counterstained with neutral red, H&E, or hematoxylin and van Gieson's stain. Fixation: Tissues are fixed in formalin or alcohol. Zenker-fixed tissues stain slowly and have a greater tendency to cause diffuse coloring of collagen fibrils. Sections: Thin paraffin sections. Solution: Weigert Resorcin-Fuchsin To 100 ml of distilled water, add 1 gm of basic fuchsin and 2 gm of resorcin. Boil. Add 12.5 ml of freshly prepared 30% ferric chloride solution. Continue boiling for 5 minutes. Cool and filter, discarding the filtrate. Dissolve the whole precipitate in 100 ml of 95% ethanol, using a hot plate or water bath for controlled heating. Add 2 ml of concentrated hydrochloric acid. As an improved solvent, the precipitate may be dissolved in: 2-methoxyethanol 50 ml Distilled water 50 ml Concentrated hydrochloric acid 2 ml Staining time is reduced with this solvent. Method: 1. Sections to 95% alcohol. 2. Place in a closed container of stain for 1-3hours at room temperature, or for 1 hour at 56°C. 3. Rinse in tap water. 4. Remove background stain by washing well in 1% acid-alcohol. 5. Rinse well in tap water. 6. Counterstain as desired (van Gieson, eosin or trichrome methods are acceptable. 7. Dehydrate through ascending concentrations of alcohol. 8. Clear in xy len e and mount in permanent mounting medium. Results: Elastic fibers appear brown to purple or with blue-black with methyl violet on a clear background. Other structures are colored depending on the counterstain used. The nuclei may be stained red with carmine before or after staining of fibers. Carmine stain is quite hard to obtain after Zenker fixation. A light stain with alum hematoxylin is preferable. Van Gieson Stain (Mallory 1961, Sheehan 1980, Carson 2009) The tissue is overstained with a soluble lake of hematoxylin ferric chloride-iodine. Both ferric chloride and iodine serve as mordants, but they also have an oxidizing function that assists in converting hematoxylin to hematein. Because this method requires that the sections be overstained and then differentiated, it is a regressive method. Differentiation is accomplished by using excess mordant, or ferric chloride, to break the tissue-mordant-dye complex. The dye will be attracted to the larger amount of mordant in the differentiating solution and will be removed from the tissue. The elastic tissue has the strongest affinity for the iron-hematoxylin complex and will retain the dye longer than the other tissue elements. This allows other elements to be decolorized and the elastic fibers to remain stained. Sodium thiosulfate is used to remove excess iodine. Although van Gieson solution is the most commonly used counterstain, other counterstains may be used. In a strongly acidic solution, collagen is selectively stained by acid fuchsin, an acid aniline dye. Saturated picric acid provides the necessary acidic pH and also acts as a stain for muscle and cytoplasm. The low pH is very important, as selective staining of collagen will not occur at higher pH levels. Acid fuchsin being a larger molecular size is restricted to more permeable collagen fibres whereas the diffusible picric acid penetrates the compact muscle, cytoplasm and red cells. If the picric acid solution is not saturated, collagen may stain pale pink to pale orange, and collagen, cytoplasm, and muscle may all stain the same color. The addition of 0.25 mL of hydrochloric acid to 100 mL of van Gieson solution will sharpen the differentiation between collagen and muscle. Fixation: 10% neutral buffered formalin Specimen: 4-5 µm paraffin sections Reagents: Weigert’s Iron Hematoxylin (These solutions may be kept for approximately 6 months). Solution A Hematoxylin 1 gm 95% alcohol 100 ml Filter. Allow to ripen naturally for four weeks before use. Solution B Ferric chloride, 29% aqueous solution 20 ml Distilled water 475 ml Glacial acetic acid 5 ml Working Solution Mix equal volumes of (1) and (2) prior to use. This mixture should be a violet black colour and must be discarded if it is brown. Acid Fuchsin, 1% Solution Acid fuchsin 1 gm Distilled water 100 ml Picric Acid, Saturated Solution Picric acid 13 gm Distilled water 1000 ml Stir the solution using a mechanical stirrer for several hours. Some picric acid should remain undissolved in the bottom of the flask. The solubility of picric acid is 1.23 gm/100 ml water at 20oC. The amount used may have to be adjusted, depending on whether water has been added to the stock powder to ensure that the water content does not drop below at least 10%. Van Gieson’s Solution Acid fuchsin, 1% solution 5 ml Picric acid, saturated solution 95 ml Procedure: 1. Deparaffinize and hydrate to distilled water. 2. Stain sections with Weigert's Iron Haematoxylin for 10 to 20 mins. Sections should be overstained, as they will be slightly decolorized by the picric acid. 3. Wash in water for 10 minutes until nuclei are dark blue-black and the background a paler blue-black. 4. Stain with Van Gieson's solution for 5 minutes. Discard solution. 5. Place slides in 95% alcohol. 6. Dehydrate, clear with xylene, and mount with synthetic resin. Notes: Acid fuchsin is extracted by water and picric acid by alcohol, hence rapid washing, blotting and brief dehydration are advised. Iron haematoxylin is used in preference to alum haematoxylin as it is more resistant to extraction by picric acid. Results: Nuclei Brown - black Collagen Red Muscle, RBCs, cytoplasm Yellow Verhoeff's Elastic Method (Mallory 1961, Sheehan 1980, Carson 2009) Although there are numerous special stains for identification of elastic fibers, Verhoeff Van Gieson stain is most commonly used because it is quick, and produces intense staining of elastic fibers that are not easily distinguished by H&E staining. It involves two steps: 1. Overstaining with a compound solution made up of haematoxylin, ferric chloride and iodine. The latter two components act as mordants to fix the haematoxylin stain to the tissues, and also act as oxidizing agents to help convert haematoxylin to haematein. Since elastin has a strong affinity for the iron-haematoxylin complex in the stain, it holds the dye longer than other tissue components. Elastin therefore remains stained even after other tissue elements are decolorized. 2. Differentiation uses excess ferric chloride mordant to breakdown the tissue-mordant-dye complex. Sodium thiosulfate is used to remove excess iodine, and the van Gieson counterstain is used to produce contrast with the haematoxylin stain. Elastic fibers and cell nuclei are stained black by the Verhoeff component while collagen and muscle are stained red by the van Gieson counterstain, which also results in yellow staining of cell cytoplasm and other tissue components. Fixation: Formalin Section: Paraffin Reagents: Solution A Hematoxylin 5 g. Absolute alcohol 100 ml. Solution B Ferric chloride 10 g. Distilled water 100 ml. Solution C (Lugol's iodine solution) Iodine 1 g Potassium iodide 2 g Distilled water 100 ml. Solution D (WORKING SOLUTION) Solution A 20 ml. Solution B 8 ml. Solution C 8 ml. Add in the above order, mixing between additions. Method: 1. Bring sections to water. 2. Stain in Verhoeff's solution until the sections are black (15 to 45 minutes). 3. Rinse in water. 4. Differentiate in 2% aqueous ferric chloride with agitation for a few minutes, checking by rinsing in distilled water and examining under low power microscope-until only elastic fibers and nuclei are black and other tissues are gray. Should the section be over-differentiated, it may be returned to Verhoeff's solution for further staining. 5. Rinse in water and then in 95% ethanol to remove iodine. 6. Wash in water for 5 minutes. 7. Counterstain with van Gieson for 1 to 2 minutes. (Eosin may also be used as counterstain). 8. Differentiate in 95% ethanol, dehydrate, clear and mount. Results: Elastic fibers black Nuclei gray to black Collagen red Cytoplasm and muscle yellow Notes: Bulk staining is not possible due to the differentiation involved in this technique. Careful differentiation of each section is required, to ensure that the fine fibres are stained and at the same time a welldifferentiated background is obtained. Elastic staining is extracted by the Van Gieson counterstain, therefore the section should be underdifferentiated with ferric chloride. Pre-treatment with 1% potassium permanganate for 5 minutes, followed by oxalic acid, improves sharpness and intensity of staining. It is imperative that each section be differentiated microscopically. To prepare Verhoeff elastic staining solution, the reagents must be added in the order given, with mixing after each addition, or poor staining may result. The staining jar that contained Verhoeff solution may be cleaned easily by transferring the 2% ferric chloride to the jar for a few minutes before discarding the solution. For optimum results, slides must be individually differentiated, because the time of differentiation is somewhat dependent on the amount of elastic tissue present. Do not depend on the control for timing the differentiation of all sections. Because proper differentiation is sometimes difficult, it is helpful to use duplicate sections differentiated to a slightly different end point. Verhoeff-Van Gieson (VVG) Staining Protocol for Elastic Fibers (Sheehan 1980, Carson 2009) The tissue is stained with a regressive hematoxylin, consisting of ferric chloride and iodine. The differentiating is accomplished by using excess mordant (ferric chloride) to break the tissue-mordant dye complex. The dye will be attracted to the larger amount of mordant in the differentiating solution and will be removed from the tissue. The elastic tissue has the strongest affinity of the iron-hematoxylin complex and will retain the dye longer than the other tissue elements. This method is used for identifying elastic fibers in tissues such as skin, aorta, etc. on formalin-fixed, paraffin-embedded sections, and may be used for frozen sections as well. The elastic fibers will be stained blue-black and background will be stained yellow. The Verhoeff-Van Gieson (VVG) staining method relies on ferric chloride and iodine to act as a mordant that links hematoxylin dye molecules to tissue components and an oxidizer that converts hematoxylin to hematein. Elastic fibers have the strongest affinity for the hematoxylin-ferric chloride iodine solution which is used to overstain the entire tissue section. Therefore, the elastic fibers retain the dye even after a diluted solution of ferric chloride is used to break the tissue-mordant-dye complex in the other tissue elements. The result is a positive staining reaction that highlights and differentiates elastic fibers from other tissue elements. Fixation: 10% formalin. Section: paraffin sections at 5 um. Reagents: 5% alcoholic hematoxylin: Hematoxylin 5 g 100% alcohol 100 ml Mix to dissolve with the aid of gentle heat. Filter. 10% aqueous ferric chloride (prepare fresh, not necessary): Ferric chloride 10 g Distilled water 100 ml Weigert’s iodine solution: Potassium iodide 2 g Iodine 1 g Distilled water 100 ml Use 4 ml of distilled water to dissolve potassium iodide. And then add iodine. Once iodine is dissolved, dilute this solution by adding 96 ml of distilled water. This solution may be prepared fresh as needed or made in larger quantities and stored in brown bottle in the dark at room temperature. Verhoeff’s Working Solution: The working staining solution should be made up fresh for best results. It will not stain satisfactorily if it is kept more than one working day. Prepare the working solution by adding in order the following reagents: 5% alcoholic hematoxylin 20 ml 10% ferric chloride 8 ml Weigert’s iodine solution 8 ml Mix the above amounts (or needed proportions thereof) well. Solution should be jet black. Use immediately and discard after use. 2% aqueous ferric chloride (prepare fresh, not necessary): 10% ferric chloride from above 10 ml Distilled water 50 ml 5% aqueous sodium thiosulfate: Van Gieson’s counterstain: 1% aqueous acid fuchsin 5 ml Saturated aqueous picric acid 100 ml For nervous tissues, it may be prepared as follows: 1% aqueous acid fuchsin 15 ml Saturated aqueous picric acid 50 ml Distilled water 50 ml Procedure: 1. Deparaffinize and hydrate slides to distilled water. 2. Stain in Verhoeff’s solution for 1 hour. Tissue should be completely black. 3. Rinse in tap water with 2-3 changes. 4. Differentiate in 2% ferric chloride for 1-2 minutes. 5. Stop differentiation with several changes of tap water and check microscopically for black elastic fiber staining and gray background. It is better to slightly under differentiate the tissue, since the subsequent Van Gieson’s counterstain can extract the elastic stain somewhat. 6. Wash slides in tap water. 7. Treat with 5% sodium thiosulfate for 1 minute. Discard solution. 8. Wash in running tap water for 5 minutes. 9. Counterstain in Van Gieson’s solution for 3-5 minutes. 10. Dehydrate quickly through 95% alcohol, 2 changes of 100% alcohol. 11. Clear in 2 changes of xylene for 3 minutes each. 12. Coverslip with resinous mounting medium. Results: Elastic fibers blue-black to black Nuclei blue to black Collagen red Other tissue elements - yellow Fig. 25-3. Elastic layer of arterial wall (Elastic Van Gieson Stain) Aldehyde fuchsin elastic stain (Gomori 1950a, Sheehan 1980) Hydrochloric acid and paraldehyde are added to an alcoholic solution of basic fuchsin to form aldehyde fuchsin. Schiff bases are formed by the aldehyde and the fuchsin, and staining is intensified by prior oxidation. Fixative: 10% neutral buffered formalin is preferred; chromate fixatives should be avoided. Formalin and Bouin fixed tissues will how a colorless background and mercury fixed tissue show a pale lilac background. Section: Paraffin sections at 4 - 5 μm. Reagents: Aldehyde fuchsin solution Pararosanilin (basic fuchsin, CI 42500) 1 gm Ethyl alcohol, 70% 200 ml Hydrochloric acid, concentrated 2 ml Paraldehyde (must be fresh) 2 ml Mix well and let stand at room temperature for 2 - 3 days or until the stain is deep purple. Store in the refrigerator. Light green stock solution Light green SF yellowish 0.2 gm Distilled water 100 ml Glacial acetic acid 0.2 ml Mix well. Light green working solution Light green stock solution 10 ml Distilled water 50 ml Procedure: 1. Deparaffinize sections and hydrate to 70% alcohol. 2. Stain sections in aldehyde fuchsin solution for 10 – 40 minutes; with good solutions, 10 minutes is usually sufficient for staining 3. Rinse off the excess stain with 70% alcohol. 4. Wash the sections in water and check microscopically for staining of elastic fibers. If a deeper stain is desired, rinse sections briefly in 70% alcohol and return to the aldehyde fuchsin. If further differentiation is needed, return sections to the 70% alcohol. Differentiation is stopped by rinsing the sections with distilled water. The stain may be filtered and reused. 5. Rinse the sections with distilled water. 6. Counterstain sections with the light green working solution for 1 to 2 minutes; discard the solution. 7. Dehydrate in 2 changes each of 95% and absolute alcohols, clear in xylene, and mount with synthetic resin. Results: Elastic fibers Deep blue to purple Other tissue elements Green Notes: • The paraldehyde used for preparation of the aldehyde fuchsin reagent should be fresh. Do not use reagent that was opened previously. • Old solutions of aldehyde fuchsin may not stain well, and the staining time may need to be prolonged. • Rosaniline (CI 42510) is not satisfactory • The shelf life of aldehyde fuchsin may be prolonged by refrigerating a small amount and freezing aliquots of the remainder. Luna Staining Method and Protocol for Elastic Fibers and Mast Cells (Luna 1992) This method is used for identifying elastic fibers and mast cells on formalinfixed, paraffin-embedded tissue sections, and may be used for frozen sections as well. The elastic fibers and mast cells will be stained purple and the nuclei will be stained black and the background stained yellow. Fixation: 10% formalin. Section: paraffin sections at 5 um. Reagents: Aldehyde Fuchsin Solution: Basic fuchsin 1 gm 70% Ethyl alcohol 200 ml Hydrochloric acid, concentrated 2 ml Paraldehyde 2 ml Let stand for 2-3 days. Filter just before use. Store solution at 4 C and it will be good for a few weeks. Iron Hematoxylin Working Solution, Weigert's: Stock solution A: 1 g hematoxylin in 100 ml 95% alcohol. Stock solution B: 4ml 29% ferric chloride in 95 ml distilled water, then add 1 ml concentrated hydrochloric acid. Working solution: mix equal parts of stock solution A and B. This working solution is reusable within 3 months. Methyl Orange Solution: Methyl orange (Sigma) 0.25 gm Alcohol (95%) 100 ml Mix well and filter before use. Procedure: 1. Deparaffinize and hydrate sections to 95% alcohol. 2. Stain sections in aldehyde fuchsin solution for 30 minutes. 3. Rinse in 95% alcohol, 3 changes (for differentiation as well). 4. Stain in Weigert’s iron hematoxylin working solution for 10 minute. 5. Wash in running tap water for 10 minutes. 6. Rinse in 95% alcohol. 7. Counterstain in methyl orange solution for 5 minutes. 8. Dehydrate through 95% alcohol, absolute alcohol for 2 changes, 3 minutes each. 9. Clear in xylene, 2 changes, and 3 minutes each. 10. Coverslip with resinous mounting medium. Results: Elastic fibers purple Mast cells purple Nuclei black Background yellow Orcein (Taenzer-Unna Orcein Method) Orcein is a naturally occurring vegetable dye, which has now been synthesized. It is used to stain for elastic fibers, especially in dermatology due to demonstration of the finest and most delicate fibers found in the skin. The tissue is stained with Orcein, differentiated with acid-alcohol and counterstained with methylene blue or alum hematoxylin. Elastic fibers stain dark-brown while nuclei are stained blue. Variations between batches of dye may produce erratic results with occasional insufficient staining. Krajian's Technique This is a rapid method for staining elastic fibers, fibrin and amyloid, employing Congo red. Elastic fibers appear bright red; fibrin and connective tissues will appear dark blue; RBC will be colored orange-yellow. BASEMENT MEMBRANE Basement membranes are found throughout the body as a resilient matrix made up of carbohydrate complexes, microfibrils and fibrous elements separating connective tissues from epithelial, endothelial, or mesothelial cells. The thickness of basement membrane varies from 15 to 50 nm. The glomerular basement membrane is particularly thick, and measures up to 350 nm in a healthy adult. The Jones methenamine silver stain is excellent for the demonstration of glomerular and tubular basement membranes of kidney biopsies. Basement membranes are commonly demonstrated with a silver stain employing a methenamine silver solution. Methenamine silver methods rely on the oxidation of carbohydrates within the tissue to form aldehyde groups. These groups will directly act to reduce silver ions from the methenamine silver solution to metallic silver. The ability to bind silver ions from solution and independently reduce silver to a visible metallic form is referred to as argentaffin. The use of sensitizing and reducing solutions are not necessary with this method. Basement membranes may also be demonstrated using the Periodic Acid- Schiff (PAS) technique. It is particularly useful for demonstration of the glomerular basement membrane of the kidney, due to its carbohydrate content, although electron microscopy seems to be the most informative. Basement membranes are not readily stained and are difficult to distinguish on H&E stains, although they are more conspicuous in the renal glomeruli, particularly in disorders where they can be markedly thickened such as in diabe