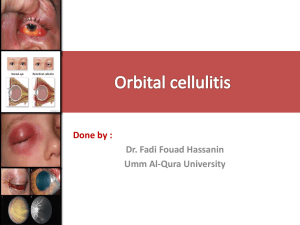
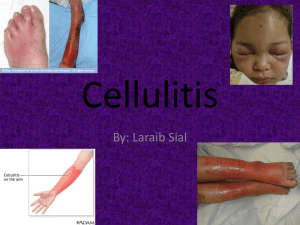
Evidence Based Disease Management Presentation Diagnosis: Cellulitis / Folliculitis ICD-10 Code(s): LO3 Cellulitis and acute lymphangitis L03.0 Cellulitis of finger and toe L03.1 Cellulitis of other parts of limb L03.2 Cellulitis of face L03.3 Cellulitis of trunk L03.8 Cellulitis of other sites L03.9 Cellulitis, unspecified Pathophysiology: Cellulitis is defined as bacterial skin infection. It is a breach to the affected skin such as a fissure, cut, laceration, insect bite or puncture wound. The affected area becomes irritated, swollen and can be painful. There might a microscopic break in the skin barrier. The affected areas can range from face, arms, legs, etc. Individuals with DM are at risk for more sever diseases. Cellulitis should be treated immediately to avoid further infection, which can spread to lymph nodes and bloodstream leading to sepsis. Majority of the cellulitis cases are cuased by Streptococcus pyogenes or by Staphylococcus aureus. Subjective: Clinical presentation can vary per individual and type of incontinence Skin irritated that expand Swelling Tenderness/ Pain Warmth Fever Chills Spots Blisters Skin dimpling Skin discoloration Objective: Varies based on area: Skin barrier affected with rash, redness, swelling, and/or pus Fever with abnormal vital signs such as high BP, HR Diagnostic Studies: Moderate Case CBC ESR and CRP Creatinine levels Severe Case CBC with differential ESR and CRP Creatinine levels Blood cultures Ultrasonography CT/MRI imaging 1 Needle aspiration and biopsy Management: Identify and treat causes Education: o Wash the wound daily with soap and water. o Apply a protective cream (Vaseline, Polysporin) for protection. o Cover the wound with a bandage. Change bandages at least daily. o Signs of infection: Irritation, pain and pus o Elevation of affected body part to reduce edema o Compression therapy o People with Diabetes or poor circulation need additional education: Inspecting feet daily. Moisturizing skin regularly. Trimming fingernails and toenails carefully. Wear footwear and gloves suitable to activities. Promptly treating infections on the skin's surface Drug Therapy: Antibiotic regimens are effective in more than 90% of patients o Mild case dicloxacillin 500mg orally every 6 hrs cephalexin 500 mg orally every 6 hrs cefadroxil 500mg every 12 hrs or 1 g orally once daily If allergic to penicillin: Clindamycin (450mg every 8hrs) or macrolide Treatment of recurrent disease o Daily amoxicillin (250mg BID) or erythromycin (250mg BID) Patients with severe cellulitis require parenteral therapy: o Medications include: Cefazolin 1 or 2 g IV every 8 hrs Nafcillin 1 or 2 g IV every 4 hrs Oxacillin 1 or 2 g IV every 4 hrs o Broad gram-positive, gram-negative, and anaerobic coverage for cases associated with diabetic ulcers o Coverage for MRSA, until culture & sensitivity information available: TMP-SMX Amoxicillin 875mg orally BID plus doxycycline 100mg orally BID For cellulitis involving wounds sustained in an aquatic environment, recommended antibiotic as follows: o Saltwater or brackish water: doxycycline and ceftazidime, or a fluoroquinolone o Freshwater: a third- or fourth-generation cephalosporin (eg, ceftazidime or cefepime) or a fluoroquinolone (eg, ciprofloxacin or levofloxacin) Consult an infectious disease specialist if the patient is not improving with standard treatment. 2 Guidelines/Websites: Medscape: https://emedicine.medscape.com/article/214222-treatment#d1 https://www.cdc.gov/groupastrep/diseases-public/Cellulitis.html https://www.uptodate.com/contents/acute-cellulitis-and-erysipelas-in-adults-treatment Referral: • Follow Up: • • Infectious disease if case is sever Initial f/u 2 weeks If sever case then based on symptoms and healing of wound References Collazos, J., de la Fuente, B., García, A., Gómez, H., Menéndez, C., Enríquez, H., Sánchez, P., Alonso, M., López-Cruz, I., Martín-Regidor, M., Martínez-Alonso, A., Guerra, J., Artero, A., Blanes, M., de la Fuente, J., & Asensi, V. (2018). Cellulitis in adult patients: A large, multicenter, observational, prospective study of 606 episodes and analysis of the factors related to the response to treatment. PLOS ONE, 13(9), e0204036. https://doi.org/10.1371/journal.pone.0204036 Ortiz-Lazo, E., Arriagada-Egnen, C., Poehls, C., & Concha-Rogazy, M. (2019). An update on the treatment and management of cellulitis. Actas Dermo-Sifiliográficas (English Edition), 110(2), 124–130. https://doi.org/10.1016/j.adengl.2019.01.011 Santer, M., Lalonde, A., Francis, N. A., Smart, P., Hooper, J., Teasdale, E., Del Mar, C., Chalmers, J. R., & Thomas, K. S. (2018). Management of cellulitis: Current practice and research questions. British Journal of General Practice, 68(677), 595– 596. https://doi.org/10.3399/bjgp18x700181 Spelman, D., & Baddour, L. M. (2022). Acute cellulitis and erysipelas in adults: Treatment (F. D. Lowy & K. K. Hall, Eds.). UpToDate. Retrieved November 3, 2022, from https://www.uptodate.com/contents/acute-cellulitis-and-erysipelas-in-adultstreatment#:~:text=In%20general%2C%20five%20to%20six,response%20to%20therapy %2C%20or%20immunosuppression. Sullivan, T., & de Barra, E. (2018). Diagnosis and management of cellulitis. Clinical Medicine, 18(2), 160–163. https://doi.org/10.7861/clinmedicine.18-2-160 3