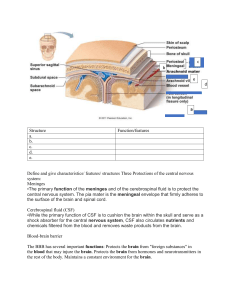
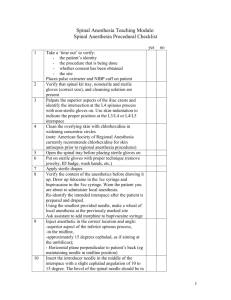
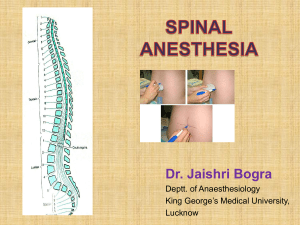
Neuroaxial Anesthesia Definition Temporary loss of sensation due to administration of a local anesthetic drug directly into the central nervous system The anesthetic drug is placed around the nerves of the CNS to prevent pain sensation and muscle relaxation to facilitate surgical procedures These techniques can also be used for analgesic purposes Often administered with opioid analgesics to improve block and provide post operative pain relief Examples include morphine, fentanyl, diamorphine. Clonidine prolongs duration of action of analgesia however it is associated with hypotension. Anatomy Indications Lower abdominal surgeries – Cesarian section Bowel surgery Hernia repair Surgeries of the lower limbs – orthopedic, vascular surgery Surgeries in the perineum – hemorrhoid repair Contraindications Absolute Relative Patient refusal Hypovolemia Lack of cooperation Coagulation disturbances Difficulty with patient positioning Stenotic valvular disease Increased intracranial pressure Bacteremia Infection at site of needle insertion Anatomical abnormalities of the spine Advantages Avoiding airway management concerns that accompany general anesthesia Ability to monitor patient mental status as patient is awake Anesthetic action generally lasts longer than the procedure and offers pain relief Risks and Complications Hypotension Nausea Bradycardia Post dural puncture Headache – associated with larger gauge and type of needle used Cauda equina injury Spinal hematoma Epidural abscess Cardiac arrest – rare Spinal Epidural Sub arachnoid space -Into the CSF Epidural space Loss of motor and sensory function at and below the level of injection Loss of function only at the level of the spinal nerve Must be given only below the level of L3 to avoid damage to spinal cord May be given at cervical, thoracic or lumbar sites Requires lower dose of anesthetic Requires larger volume for same anesthetic effect Faster onset of analgesia Slower onset of analgesia Drugs Both amide and ester anesthetics can be used Bupivacaine is the most common for Neuroaxial anesthesia Baricity Ratio of densities/specific gravity of two solutions – LA vs CSF CSF density is 1.0003 +/- 0.0003 Hyperbaric solutions – higher density than that of CSF and tend to sink and flow in the direction of gravity. Add 5-8% dextrose Isobaric – same density as CSF Hypobaric – Lower density than CSF and these rise in relation to gravitational pull Add distilled water POSTURE is used to control spread Bupivicaine (Marcaine) Amide local anesthetic Hyperbaric solution usually 0.75% is used Prepared alone or with epinephrine Onset of action: 1-17 minutes (route and dose dependent) Duration of action: 2-9 hours (route and dose dependent) Half life: 8.1 hours in neonates and 2,7n hours in adults Metabolism: Hepatic Excretion: renal (6% unchanged) Bupivacaine ctd Side effects: restlessness, anxiety, drowsiness, tinnitus, hypotension, arrhythmias, Adverse effects: seizures, cardio-toxicity and cardiac arrest Contraindications: persons with hypersensitivity reactions to amide group of anesthetics, obstetrical paracervical blocks and Regional anesthesia (biers block) Technique - Equipment Sterile drapes Cleaning solution: Clorhexidine (preferred) or betadine Needles including – Apply local to skin, introducer, spinal needle) Syringes Local anesthetic for skin and soft tissues Types of Needles Tuohy Needle Procedure Sterile PPE is donned and patient is positioned accordingly either sitting up or lateral decubitus position Area is cleaned and draped. ASIS is used as a land mark as it coincides with L3-L4 interspace Palpate spinous processes in the midline Needle is inserted and the correct space is confirmed Confirmation of correct needle insertion Spinal Return of CSF through spinal needle Use of litmus paper – should turn blue Test for glucose using glucometer Epidural Loss of resistance to air or saline ALWAYS aspirate to rule out CSF or blood References Press, C. D., MD. (2015, November 30). Subarachnoid Spinal Block: Overview, Periprocedural Care, Technique. Retrieved July 22, 2018, from https://emedicine.medscape.com/article/2000841-overview?pa=mjq xi1Tamh2AJEV0axMrqyCwMFCRJAufudunlppBmCQ4 rbjc8DNLE5/iq6fCdb243nPhN45bRyFifRUcxgL5uirmrJC0so7wvS3wxSmSU= Spinal anaesthesia. (2018, July 10). Retrieved from https://en.wikipedia.org/wiki/Spinal_anaesthesia (n.d.). Retrieved from https://www.uptodate.com/contents/overview-of-neuraxial-anesthesia#H200678350