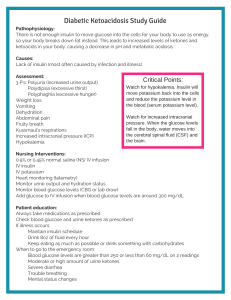
African American/Hispanics more at risk for getting diabetes - Type 1: dependent – for life insulin Type 2: resistant – older age Obesity: #1 risk factor for diabetes A1c is good for hyperglycemia Brain cellularly works with glucose - Brain needs carbs for fuel If you don’t eat, breaks down protein and fat Byproduct of fat metabolism - Ketones Exclusively burning fat and you aren’t breaking down carbs - Type 1 diabetes affected most by ketoacidosis Anybody with diabetes can be ketonic If you start to damage blood supply to the kidney, you go into acute renal dysfunction - Any place in the body that doesn’t perfuse leads to amputation - Lower limbs more commonly affected Neuropathy - Hot things are discouraged for normal sensation - Not able to feel injury, may get worse HgBA1c - Prediabetic depends on this factor Adrenal gland tumor - High BP - High cortisol levels Too much cortisone= high BP Prednisone - Blood sugar is going to increase Hypoglycemia - Fatigue - Lethargic - Shaky - Headache - Syncope - Neuro status is important Hyperglycemia with ketones is DKA - Mgmt. is different - The ketones make it different Pancreas isn’t working appropriately - Glucose Fasting <100 - Take glucose before meals After you eat: 180 Before bedtime - Glucose levels rise A1c: less than or around 7 A1c for diabetes: 5.6 Fasting glucose is elevated 2 hr plasma glucose - Draw it, give them a drink and they stick it at 1 and 2 hours - Goal: do not want to exceed 199 - More with type 2 diabetics Type 1: REQUIRES INSULIN - Fast onset Type 2: progressive, a little at a time - Metformin - Oral hypoglycemic drugs to start, initially may need to convert to insulin or use both Hyperlipidemia, hypercholesteremia, all of it leads to diabetes Type 1’s lose weight because everything is being peed out - They don’t have insulin to manage the food Type 1 have a lot of neuro changes and severe weight loss Diabetics should wear a bracelet - People on insulin they recommend a bracelet D5W: diabetics Bolus: NS Push D50 if someone is unresponsive and hypoglycemic Or glucagon IM if patient doesn’t have an IV site A1c tests for the last 3 months HHS: Clinical manifestations: dehydration, hypotension, tachy, decreased LOC (seizures) Patho: complication of DM. occurs when a blood sugar is topo high for a long period of time leading to severe dehydration. Treatment: Diagnostics: a plasma glucose level >600 mg/dL increased effective plasma osmolality >320 mOsm/kg in the absence of ketoacidosis. - Plasma osmolarity ranging from 300 to 320 mosm/mL A very high blood sugar level (over 600 mg/dL) with low ketone levels (acids in blood and urine) will help make the diagnosis of HHS - Ketones are rarely present in persons with HHS - More dehydrated DKA - Starving in this state Clinical picture: tachypneic to compensate for acidosis pH 7.2, kusmual breaths, fruity breath - Ketones are in the urine CO2 drops Tx: rehydration, reverse the acidosis with fluids and electrolyte replacement, slow rehydration to prevent cerebral edema - With insulin, monitored every hour, insulin drips IV, NPH only one able to be in IV Hyponatremic and hypokalemic for DKA Bacteria loves sugar, recurring yeast infections are common Metformin - Huge GI issues - Take it forever - Stop taking it before contrast dye interacts lactic acidosis renal damage Always has a tray of food before doing the insulin - Make sure the patient likes the food Check urine for ketones!!!!