COMPARISON OF SHORT-TERM HYPOCALORIC HIGH PROTEIN DIETS
advertisement

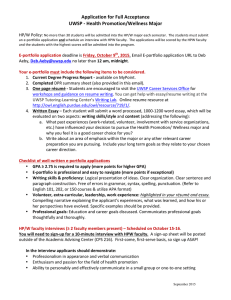
Journal Pre-proof COMPARISON OF SHORT-TERM HYPOCALORIC HIGH PROTEIN DIETS WITH A HYPOCALORIC MEDITERRANEAN DIET: EFFECT ON BODY COMPOSITION AND HEALTH-RELATED BLOOD MARKERS OF OVERWEIGHT AND SEDENTARY YOUNG PARTICIPANTS Konstantinos Feidantsis , Spyridon Methenitis , Kleopatra Ketselidi , Kiriaki Vagianou , Petros Skepastianos , Apostolos Hatzitolios , Alexandros Mourouglakis , Athina Kaprara , Maria Hassapidou , Tzortzis Nomikos , Sousana K. Papadopoulou PII: DOI: Reference: S0899-9007(21)00227-6 https://doi.org/10.1016/j.nut.2021.111365 NUT 111365 To appear in: Nutrition Received date: Revised date: Accepted date: 18 January 2021 11 April 2021 27 May 2021 Please cite this article as: Konstantinos Feidantsis , Spyridon Methenitis , Kleopatra Ketselidi , Kiriaki Vagianou , Petros Skepastianos , Apostolos Hatzitolios , Alexandros Mourouglakis , Athina Kaprara , Maria Hassapidou , Tzortzis Nomikos , Sousana K. Papadopoulou , COMPARISON OF SHORT-TERM HYPOCALORIC HIGH PROTEIN DIETS WITH A HYPOCALORIC MEDITERRANEAN DIET: EFFECT ON BODY COMPOSITION AND HEALTH-RELATED BLOOD MARKERS OF OVERWEIGHT AND SEDENTARY YOUNG PARTICIPANTS, Nutrition (2021), doi: https://doi.org/10.1016/j.nut.2021.111365 This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2021 Published by Elsevier Inc. 1 Highlights 2 Hypocaloric MD provides all the necessary nutrients 3 Hypocaloric MD reduces body mass, fat mass and maintains FFM 4 Hypocaloric MD: beneficial on metabolic and inflammation/muscle damage 5 indices 6 Hypocaloric HP / HPW reduce body mass and FFM, but not fat mass 7 Hypocaloric HP / HPW: adverse on metabolic and inflammation/muscle damage 8 indices 9 1 10 11 COMPARISON OF SHORT-TERM HYPOCALORIC HIGH PROTEIN DIETS 12 WITH A HYPOCALORIC MEDITERRANEAN DIET: EFFECT ON BODY 13 COMPOSITION AND HEALTH-RELATED BLOOD MARKERS OF 14 OVERWEIGHT AND SEDENTARY YOUNG PARTICIPANTS 15 16 Running Title: Hypocaloric Mediterranean and high-protein diets 17 1,2 *, Spyridon Methenitis 1,3 18 Konstantinos Feidantsis 19 Kiriaki Vagianou 20 Mourouglakis 5, Athina Kaprara 6, Maria Hassapidou 1, Tzortzis Nomikos 21 Sousana K. Papadopoulou 1 22 *Authors with equal contribution and should consider as both first authors 1,7 *, Kleopatra Ketselidi 1,7 , , Petros Skepastianos 4, Apostolos Hatzitolios 5, Alexandros 7 & 23 1. Department of Nutrition Sciences and Dietetics, Faculty of Health Sciences, 24 International Hellenic University, P.O.Box 141, 574 00, Sindos, Thessaloniki, 25 Greece 26 27 28 29 30 31 2. Laboratory of Animal Physiology, Department of Biology, Aristotle University of Thessaloniki, GR 54124, Thessaloniki, Greece 3. Sports Performance Laboratory, School of Physical Education & Sports Science, National and Kapodistrian University of Athens, Athens, Greece 4. Department of Biomedical Sciences, Faculty of Health Sciences, International Hellenic University, Sindos Thessaloniki Greece 32 5. Diabetes Center, EASO Obesity Center, First Propedeutic Department of Internal 33 Medicine, Medical School, Aristotle University of Thessaloniki, AHEPA 34 Hospital, Thessaloniki, Greece 35 36 37 38 6. Laboratory of Sports Med, School of Physical Education and Sports Science, Thessaloniki, Aristotle University of Thessaloniki, Greece 7. Department of Nutrition and Dietetics, School of Health Science & Education, Harokopio University of Athens, Athens, Greece 39 2 40 Correspondence: Konstantinos Feidantsis (), email: kfeidant@bio.auth.gr, Tel: 41 00302310998413 42 Abstract 43 The aim of the present study was to compare the short-term effects of hypocaloric 44 Mediterranean and two high protein diets, with and without whey protein 45 supplementation, on body composition, lipidemic profile, inflammation and muscle 46 damage blood indices, in overweight, sedentary, young participants. Thirty-three young, 47 overweight, male and female participants (Age: 22.8±4.8 yrs, Body Mass: 85.5±10.2 kg, 48 Body Fat Percentage: 34.3±8.1%) were randomly allocated to three different hypocaloric 49 (-700 kcal·day-1) diets: (A) Mediterranean Diet (MD; n=10), (B) High Protein (HP; n=10) 50 diet, and (C) High Protein - Whey Supplementation (HPW; n=10) diet. The intervention 51 lasted 6 weeks. Body composition and biochemical indices were evaluated 1 week before 52 and after the nutritional interventions. Body and fat mass were decreased in MD and HP 53 group (p<0.05; -1.7±1.2% - -7.3±4.2%), while no significant decline of fat free mass 54 (FFM) was observed in the MD group. The MD diet beneficially altered the lipid profile 55 (p<0.05) while the HP and HPW diets did not induce significant changes. Subclinical 56 inflammation and muscle damage indices were significantly increased in HP and HPW 57 groups (p<0.05; 7.4±3.5% - 266.6±55.1%), but were decreased in MD group (p<0.05; - 58 33.3±10.1% - 1.8±1.2%). Energy intake of carbohydrates and proteins was significantly 59 related to the changes of body composition and examined biochemical blood markers 60 (p<0.05; r: -0.389 -0.889). Among the three hypocaloric diets, only the MD diet induced 61 positive changes in body composition and the metabolic profile of overweight, sedentary 62 individuals. 63 3 64 Graphical abstract 65 66 67 Keywords: protein supplementation; fat free mass; blood indices; inflammation; obesity 68 Introduction 69 While obesity is closely related to inflammation, oxidative stress, glucose 70 intolerance, metabolic and cardiovascular diseases, with a negative impact on health and 71 health care economics [1, 2, 3], its prevalence arises each year in the developed countries. 72 Thus, scientists investigate the effect of several lifestyle interventions, including energy- 73 restricted diets and exercise, on body weight/fat loss and obesity’s comorbidities. 74 Caloric restriction diets (hypocaloric diets 500-800 kcals·day-1) [4], including 75 hypocaloric Mediterranean Diet (MD) seem to beneficially affect increased body 76 weight/fat [5]. However, an undesired consequence of the negative energy balance is fat 77 free mass (FFM) significant reduction (~25%) [6]. FFM reduction is linked with 78 decreased basal metabolic rate, a down-regulation of muscle protein synthesis and 79 upregulation of muscle protein degradation, thus jeopardizing short and long term 80 benefits of weight reduction. Reduced FFM also increases the risk for the development of 81 several chronic diseases, such as metabolic syndrome and type II diabetes [6, 7, 8, 9, 10]. 82 In recent years, “high protein diets” with additional (beyond Recommended 83 Dietary Allowance - RDA) protein intake, although hypocaloric, are very promising for 4 84 FFM maintenance in athletes and trained individuals. These diets seem to have a direct 85 positive impact on several biological mechanisms, including satiety and energy 86 expenditure increase [e.g. 11, 12, 13]. However, their effects especially in obese or 87 individuals with type II diabetes body composition are discrepant and controversial [14], 88 mostly regarding the lipidemic profile [15], liver and kidney function [16]. Several 89 studies showed that increased amino acids (AA) levels in blood plasma due high protein 90 diets have been linked with increased odds for hyperinsulinaemia, insulin resistance and 91 type II diabetes [17, 18]. In addition, high protein consumption has been linked to 92 increased inflammation and to liver and kidney dysfunction due to an increase of uric 93 acid, an end-product of purine metabolism. On the other hand, isocaloric or hypocaloric 94 Mediterranean Diets (MDs) induce beneficial changes on lipidemic profile and several 95 cardiometabolic risk factors [19, 20, 21]. 96 According to the above, the aim of the present study was to compare the short- 97 term effects of hypocaloric Mediterranean MD and two high protein diets, with and 98 without whey protein supplementation (HPW and HP respectively), on body 99 composition, lipidemic profile, inflammation and muscle damage blood indices, in 100 overweight, sedentary, young participants. 101 102 Methods 103 Nutritional Interventions 104 In an effort to evaluate the short-term effect of MD, HPW and HP diets on body 105 composition, lipidemic profile, inflammation and muscle damage blood indices, in 106 overweight, young, sedentary participants, a 6 week intervention period was selected, 107 according to previous reports [22, 23, 24]. Every week, each one of the participants met 108 with one of the nutritionists of our research team, in order to receive her/his new dietary 109 plan, as well as to discuss possible queries that might affect the results of the study, as 110 well as to verify her/his commitment. Individualized diets were designed weekly for each 111 participant, considering their daily energy expenditure, their resting metabolic rate 112 (RMR) (already evaluated before the intervention), as well as their eating habits and their 113 needs in macro and micronutrients components. For weight loss facilitation, all diets were 114 hypocaloric, aiming to induce a moderately negative energy balance of approximately 5 115 600-700 kcal·day-1 [4]. The nutritional plan included 3 meals and 2 snacks per day. In 116 addition, all diets provided the same caloric intake per day. A detailed presentation of the 117 three nutritional interventions is presented in Table 1. In the MD group, each participant 118 followed a standard hypocaloric MD (Table 1), based on the principles of the 119 Mediterranean Diet, consisting of 58.39±2.12% carbohydrates, 27.95±1.57% fats and 120 15.87±0.49% proteins per day (1.5 g·kg FFM-1·day-1). In both HP and HPW groups, the 121 daily protein intake was set at 2.5 g·kg FFM-1·day-1, in order to protect FFM losses 122 during caloric restricted diets [25]. The calculation of the protein intakes per kg FFM 123 instead of per kg of body mass was selected, because FFM is more metabolically active 124 compared to fat tissue [25] . In addition, protein intake per meal did not exceed 20-30 g, 125 in both HP and HPW groups, as previously proposed [26]. Accordingly, HP and HPW 126 diets consisted of 43.6±2.3% and 44.1±2.3% carbohydrates, 27.4±0.9% and 27.2±0.9% 127 fats, 28.7±1.9% and 28.9±1.4% proteins, respectively (Table 1; no significant differences 128 between HP and HPW groups, p>0.05). The HP and HPW interventions differed only in 129 the dietary source of protein. Specifically, in the HP group, protein was exclusively 130 obtained from food, while in the HPW group, 50% of the daily protein intake was 131 obtained from a whey protein supplement (isolated whey protein formula provided by 132 BioMax BioWhey), in which 25 g consisted of 102 kcal, 1.9 g carbohydrates, 0.6 g fats, 133 and 21 g proteins of which 5 g were branched chain amino acids (BCAA) and 5 g were 134 glutamine. 135 136 All participants, recorded their dietary intake for three consecutive days, two 137 weekdays and one weekend day. An experienced dietitian provided verbal and written 138 instructions for food diaries completion. Food models were used for the estimation of 139 consumed foods’ quantity. Food diaries’ analysis was performed by experienced 140 dietitians via the Food Processor Program (version 7.4, ESHA Research Salem, Oregon) 141 with the inclusion of traditional Greek recipes [9, 27]. The validity and reliability of the 142 used questionnaire have been evaluated in previous studies of our lab [9, 27], and the 143 Intraclass Correlation Coefficient (ICC) ranged from 0.850 to 0.901 (95% CI: Lower = 144 0.80, Upper = 0.92). 145 6 146 Experimental Approach to the Problem 147 Participants were recruited via advertisements in local university-student 148 societies. Those who fulfilled the following inclusion criteria: 1) Body mass index (BMI) 149 > 25 Kg·m-2, 2) absence of systematic exercise training during the previous 12 months 150 and the intervention period 3) weight stability (±2 kg) at least for three months prior to 151 the entrance in the study, 4) absence of metabolic, cardiovascular and/or pulmonary 152 diseases, (5) no supplement consumption, (6) no additional dietary plan for weight loss or 153 maintenance, and 7) age range 18 - 25 years, visited the laboratory for a second time for 154 medical examination and body composition evaluation by bioelectrical impedance 155 analysis (BIA). RMR was evaluated through indirect calorimetry. A completion of a 3- 156 day recall questionnaire, after detailed oral and written explanations, was employed for 157 the assessment of the participants’ dietary habits and physical activity. Each participant 158 was assigned into one of the 3 groups: 1) MD 2) HP and 3) HPW. One week later, 159 participants started their 6-weeks nutritional intervention. During the study, dietary intake 160 and weekly physical activity were evaluated by questionnaires at intervals of 2, 4 and 6 161 weeks, in order to evaluate the compliance to the prescribed dietary schemes. One week 162 after the end of the nutritional intervention, body composition and RMR were re- 163 evaluated, while a second venous blood sample was obtained, after an overnight fast. 164 165 Participants 166 After the initial screening of responders, thirty-three young male (17) and female 167 (16), Caucasian, overweight volunteers, fulfilling the inclusion criteria, provided their 168 written consent to participate in the study. Three participants (one from each group) were 169 excluded from the study. Thus, 30 participants finished the experimental procedure. After 170 the initial evaluations all responders were assigned into 3 groups (each group consisted of 171 5 males and 5 females participants), according to their body fat percentage and fat free 172 mass (FFM; no differences between the groups; p>0.05): (A) MD (n=10; Age: 21.40±2.9 173 yrs, Body Mass: 84.1±8.7 kg, Body Height: 174.20±4.58 cm, Body Fat Percentage: 174 33.0±7.8%), (B) HP (n=10; Age: 23.2±3.1 yrs, Body Mass: 86.7±7.9 kg, Body Height: 175 177.20±5.08 cm, Body Fat Percentage: 34.3±8.1%) and (C) HPW (n=10; Age: 23.10±4.3 176 yrs, Body Mass: 85.7±7.2 kg, Body Height: 175.99±8.12 cm, Body Fat Percentage: 7 177 35.5±9.1%). The initial descriptive characteristics of participants’ body composition in 178 each group are presented in Table 2. All procedures were in accordance with the 179 Declaration of Helsinki and approved by the local university ethics committee, while all 180 participants signed an informed consent before entering in the research procedure. 181 182 Evaluation of Physical Activity, Energy expenditures and Resting Metabolic Rate. 183 Physical activity was recorded via three self-reported questionnaires (2 weekdays 184 and one weekend day) in order to determine participants’ level of physical activity, 185 frequency and duration per day (ICC = 0.95, 95% CI: Lower = 0.90, Upper = 0.98; p < 186 0.0001, n=10) [9, 27, 28], both before the initiation and during the study. Revised tables 187 by Ainsworth et al. [29] were used to estimate the energy cost of each activity. RMR was 188 evaluated through indirect calorimetry (FitMate pro, COSMED, Rome, Italy). The ICCs 189 for this evaluation have been explored in a pilot study from our laboratory, and was 0.897 190 (95% CI: Lower = 0.85, Upper = 0.94; p < 0.0001, n=10). 191 192 Evaluation of body composition and anthropometric characteristics. 193 Height was measured using a stadiometer (SECA 220, Seca Corporation, 194 Columbia, USA), while body mass using a calibrated digital scale (Seca 707, Seca 195 Corporation, Columbia, USA). Body composition was evaluated via BIA (50Hz; 196 Bodystat 1500, Bodystat Ltd) and measurements were analyzed using Bodystat 1500 197 computer software, with the use of specific equations for Caucasian males and females 198 participants (Bodystat 1500 Body Manager, version3.16, 2002, Bodystat Ltd). BIA 199 evaluation was performed according to previous recommendations for the estimation of 200 body fat (percentage and Kg), FFM (percentage and Kg) and total body water (%; 201 bioelectrical impedance vector analysis) according to the manufacture instructions [ICC 202 for body fat = 0.93, (95% CI: Lower = 0.89, Upper = 0.97), LBM =0.98, (95% CI: Lower 203 = 0.95, Upper = 0.99), water = 0.94, (95% CI: Lower = 0.88, Upper = 0.98), p < 0.0001, 204 n = 10] [24]. 205 206 Blood sampling and biochemical assays. 8 207 Venous blood samples were obtained from each subject, after at least 8 hours of 208 fasting, during morning hours (8:00-9:00 am). Complete blood count was determined in 209 EDTA anticoagulated whole blood sample on a Mindray BC-3000 hematology analyzer 210 (Mindray, Shenzhen, China). For biochemical parameter determinations, blood samples 211 were drawn in Vacutainer-type tubes containing clot activator and were centrifuged for 30 212 min. The recovered sera were stored at -40˚C until further analysis. All biochemical 213 parameters were measured through a Mindray BS-300 Chemistry Analyzer (Mindray, 214 Shenzhen, China). Blood analysis was performed with respective reagents for each 215 parameter, together with original calibrators with metrological traceability as well as 216 controls for the above analyzer and according to manufacturers instructions. Moreover, 217 appreciable recovery rates (93.96–98.43%) of all the biochemical parameters examined 218 herein, indicated very good compatibility of extraction media for biochemical analysis. 219 220 Statistical Analyses 221 A post hoc power analysis (G*Power ver 3.1; FrankFaul, Universitat Kiel, 222 Germany), which is ideal for social, behavioral and biomedical sciences [30], was 223 performed, according to the study design, the number of participants that completed the 224 protocols and the evaluations, and the lowest Partial Eta Squared of the significant 225 contrasts or the Pearson’s r correlations coefficient that were found. The results of this 226 analysis revealed that the actual power of the present study results for the contrast 227 between the groups is above 0.890, while for the correlation coefficients ranged between 228 0.857 and 0.912. All data are presented as mean and standard deviation (±SD). Partial eta 229 squared could be used as an indicator of effect size, and it could be classified as small 230 (0.01 to 0.059), moderate (0.06 to 0.137) and large (≥0.138). One-Way and Two-way 231 repeated analysis of variance (ANOVA) followed by Bonferroni Post-Hoc (p ≤ 0.05 was 232 used as a 2-tailed level of significance), and Pearson’s product moment correlation 233 coefficient were used for the investigation of differences and correlations between the 234 groups (SPSS Statistics Ver. 20). The interpretation of the observed correlations was 235 performed according to Hopkins’ ranking: correlations coefficients between 0.3 - 0.5 236 were considered moderate, between 0.51 - 0.70 large, between 0.71 - 0.90 very large, and 237 > 0.91 almost perfect. 9 238 239 Results 240 241 242 No significant differences were found between the groups for the initial 243 evaluations of body composition, RMR and biochemical indices (p>0.05; Table 2). As it 244 was expected the participants of HP and HPW groups consumed lower amounts of 245 carbohydrates but higher amount of proteins compared to the MD participants, as it has 246 been designed (p<0.001; Table 2). The two protein groups did not differ in the protein, 247 carbohydrate and fat intake (p>0.05). 248 Significant body mass, BMI and body fat percentages reductions were observed 249 for the MD and HP groups after the hypocaloric diets (p<0.05; factor Time η2: 0.453 – 250 0.747; Table 2). No significant differences were found for these parameters in the HPW 251 group. A significant time x group interaction was found for the body composition 252 variables (p<0.05; Time x Group Interaction η2: 0.262-0.394). Specifically, the MD 253 group presented higher body mass, BMI and body fat percentage decreases (p<0.001) 254 compared to HP and HPW groups (Table 2). FFM decreased in HP and HPW groups, 255 with HPW achieving the highest decrease. MD group participants had no significant FFM 256 loss. Βody fat percentage differed significantly between HP and HPW, with the HP group 257 achieving higher loss (p<0.001). No significant changes were found for RMR between 258 the groups at any time point (p>0.05; η2: 0.050 – 0.079). However, when the percentage 259 changes were taken into account, it was observed that the HPW group showed the highest 260 RMR reduction (-8.9±2.8%), followed by the HP group (-4.6±2.7%), while the MD 261 group showed a minor, non-significant, increase (1.4±0.9%). 262 Τable 3 depicts blood indices changes evaluated in the present study. Significant 263 beneficial changes were found for triglycerides, total cholesterol (TC), LDL-cholesterol 264 (LDL-C), HDL-cholesterol (HDL-C) and glucose concentrations, mainly after the MD 265 intervention (p<0.01). A significant Time x Group interaction was found for most 266 variables (Table 3). The highest triglycerides, TC and LDL-C reductions and the highest 267 HDL-C increase were exhibited in the MD group (-42.4±15.4% - 18.2±12.9%), followed 268 by HP (-20.4±12.9% - 3.5±3.1%), while the lowest, insignificant changes were observed 10 269 in the HPW group (-8.3±4.4% - 0.5±2.1%). Significant differences between the 270 concentrations as well as the percentage changes of inflammation and muscle damage 271 related blood markers, were found between the groups after the 6week interval (p<0.001; 272 Time η2: 0.159 – 0.607; Time X Group Interaction η2: 0.081 – 0.610; Table 3, Figure 1). 273 The inflammation markers [white blood cells (WBC), C-reactive protein (CRP)] and the 274 muscle damage markers [Creatine kinase (CK), lactate dehydrogenase (LDH)] remained 275 unchanged or significantly decreased in the MD group, while they significantly increased 276 in the HP and HPW groups (Table 3 and Figure 1). Similarly, aspartate transaminase 277 (AST), alanine transaminase (ALT), gamma-glutamyltransferase (γGT), serum albumin 278 (SA) and serum total protein (STP) concentrations were increased only in the HP 279 (4.4±2.1% -33.3±21.4%) and HPW group (13.1±5.5% - 61.0±17.4%) with significant 280 differences between the groups to be found for the post-intervention values (p<0.05; 281 Time η2: 0.199 – 0.457; Time X Group Interaction η2: 0.164 – 0.366; Table 3) as well as 282 for the percentage changes (p<0.001). 283 284 285 When all participants were considered as one group (n=30), significant 286 correlations were found between the daily energy intakes (kcal), and/or the differences of 287 intakes, compared to pre-intervention values, of carbohydrates, proteins and the 288 percentage changes of body composition components, RMR, blood lipids, inflammation 289 and muscle damage related blood markers (p<0.05; Table 4; Figure 1). Specifically, 290 carbohydrate daily energy intake exhibits moderate to large, negative correlations with 291 the percentage changes of body mass, body fat percentage, triglycerides and LDL-C 292 levels (r: -0.389 - 0.600; p<0.05), but large positive relationships with the changes of 293 FFM and RMR (r: 0.889 and 0.599 respectively; p<0.05; Figure 1). In contrast, protein 294 daily energy intake presents a negative correlation with FFM (r: -0.799) and positive 295 correlations with body mass, body fat percentage, triglycerides and LDL-C levels (r: 296 0.389 – 0.518; p<0.05). It must be pointed out though, that due to the fact that all the 297 above parameters decreased after the nutritional interventions, their percentage changes 298 were negative. Thus, when a negative correlation was found, it indicated that participants 299 with higher amounts of carbohydrates or proteins were those with the highest decrease of 11 300 the above parameters, while the positive ones indicated that participants with higher 301 intakes of carbohydrates or proteins were those with the lowest decrease. Large to very 302 large, negative correlations were found between the daily energy intake from 303 carbohydrates and the percentage changes of WBC, Urea (NG), Creatine (Cr), CK, CRP, 304 LDH, uric acid (UA), AST and ALT (r: -0.442 - -0.844; p<0.05; Table 4). 305 Controversially, positive relationships were found between the daily energy intake from 306 proteins and the percentage changes of the above blood indices (r: 0.510 – 0.703; 307 p<0.05). According to these results, the negative relationships between the daily energy 308 intake from carbohydrates and the percentage changes of the blood parameters mentioned 309 above, indicate that participants who receive higher amounts of carbohydrates per day 310 were those who achieved the lowest increases in these parameters, and vice versa for the 311 positive correlations that were found for the protein intake (Figure 2). 312 313 314 315 Discussion 316 Nowadays, it is well described that even in short-term periods almost all types of 317 calorie restriction diets similarly induce body mass reduction [31, 32] which is 318 accompanied by 75% fat mass and 25-30% FFM losses [33]. Although in athletes who 319 undergo systematic heavy training, an increased amount of protein intake (up to 3.4 g·kg 320 FFM-1·day-1) during caloric restriction diets, seems to be very effective in maintaining 321 FFM and performance [e.g. 12, 13, 25, 27], according to the results of the present study, 322 in the absence of any systematic training, increased protein consumption does not seem to 323 have any significant impact on FFM maintenance in sedentary overweight individuals. 324 The results of the present study provide further support to recent meta-analyses [34, 35] 325 indicating that during short term hypocaloric diets (<12 weeks) in non-trained, healthy 326 participants, high protein diets have a small impact on body, fat mass reductions and 327 FFM maintenance compared to normal protein diets. These observations suggest, that 328 during HP and HPW diets, FFM is sacrificed to support hepatic gluconeogenesis 329 production in the expense of the reduced carbohydrate intake [7]. 12 330 Increased consumption of protein, especially when a part comes from whey 331 protein supplementation, raises AA plasma concentrations, which has been linked with 332 suppression of endogenous glucose production, reduced glucose uptake from muscle cells 333 and increase of muscle insulin resistance [19, 36]. AA increased availability, by pyruvate 334 dehydrogenase and hexokinase II inhibition, results in increased AA utilization during 335 mitochondrial oxidation, minimizing glucose and free-fatty acids contributions [37, 38]. 336 Moreover, it seems that HP and HPW groups may have a negative impact on molecular 337 pathways controlling muscle mass maintenance and/or hypertrophy such as those of 338 AKT/mTOR, which is activated by insulin, postprandial increase of extracellular AA, but 339 also from glucose [7, 11, 39]. AA increased availability, results in strong stimulation of 340 mammalian target of rapamycin complex 1 (mTORC1) and its dowstream targets, such as 341 the ribosomal protein S6 kinase beta 1 (p70S6k), which is known to control muscle 342 protein synthesis [7, 11, 39]. Indeed, it seems that there is almost a linear increase of 343 muscle protein synthesis after ingestion of 20-35 g of protein per meal. However, the 344 over-stimulation of p70S6k can trigger a negative-feedback loop, leading to insulin 345 receptor substrate 1 (IRS1)de-phosphorylation, AKT/mTOR pathway unregulated 346 activity, muscle protein synthesis reduction and muscle mass degradation, and insulin 347 resistance and adipogenesis [11, 18, 40]. The above mechanisms may explain FFM 348 highest reductions, fat mass lowest losses and increased fasting glucose values in the HP 349 and HPW groups [40]. On the other hand, the amount of protein intake of the hypocaloric 350 MD, seems to be enough in order to elicit a positive stimulation of muscle protein 351 synthesis, and thus maintain FFM. 352 The low carbohydrate availability of HP and HPW diets may also explain the 353 significant losses of FFM through muscle protein breakdown up-regulation, probably 354 owed to the hyper-activation of adenosine monophosphate-activated protein kinase 355 (AMPK) [7, 8, 10, 40]. During low carbohydrate availability, AMPK activation results in 356 up-regulation of muscle autophagy mechanisms leading to increased AA release in order 357 to support hepatic gluconeogenesis and prevent hypoglycemia [7, 11, 36, 40]. The above- 358 suggested mechanisms are supported by the results of the present study, in which FFM 359 strong reduction is strongly correlated to an increase of all muscle inflammation/damage, 360 protein degradation and hepatic blood indices. In addition, the present study showed that 13 361 when a part of the daily increased protein consumption comes from whey protein 362 supplementation, known for its high availability of BCAA (especially of leucine) [39], 363 the negative effects on FFM and all the evaluated blood markers are maximized, 364 suggesting that the above proposed mechanisms may have even higher activation [11, 18, 365 40]. In contrast, in hypocaloric MD, where the availability of carbohydrates was higher 366 and the protein intake was similar to RDI, the previous mechanisms might exhibit lower 367 activation [39, 40], restraining FFM losses, augmenting fat losses and improving 368 biochemical profile. 369 According to the present results, HP and HPW diets resulted to almost 370 hyperuricemia levels (≥7mg·dL-1 for men and ≥6mg·dL-1 for women) [41, 42], since uric 371 acid as an end product of purine metabolism [19]. Moreover, increased blood uric acid 372 concentrations are related with muscle inflammatory/damage blood indices such as CK 373 and high-sensitivity CRP [43], as also observed in the present study. Uric acid can also 374 inhibit insulin signaling and promote insulin resistance, increasing risk for cardiovascular 375 diseases, metabolic syndrome and type II diabetes especially in over-weight and obese 376 individuals [19, 41, 42]. Uric acid increased concentrations are also linked to reduced fat 377 utilization (as energy substrate), increased conversion of excess glucose into lipids, 378 mitochondrial dysfunction [19, 42], vascular oxidative stress, endothelial dysfunction, 379 coronary artery disease and atherosclerosis [43, 44]. Considering all the above, it seems 380 that uric acid increased levels may mediate for the unfavorable metabolic effects 381 observed after hypocaloric, HP diets in sedentary overweight individuals, observed in the 382 present study. 383 Finally, our results demonstrated that high protein consumption, in parallel with a 384 hypocaloric diet, may attenuate the beneficial effects of energy restriction on lipid profile. 385 In the HP and especially HPW groups, almost all lipidemic profile markers exhibited the 386 lowest positive changes. An important concern about HP diets, especially those rich in 387 animal protein sources poor in complex carbohydrates such as dietary fibers, is their 388 direct correlation with higher cholesterol, saturated fatty acids intake and higher 389 cardiovascular diseases risk [45]. Our findings support researches and meta-analyses [46, 390 47] exhibiting a stronger decrease in TG, LDL-C, HDL-C and no significant effect on 391 surrogate cardiovascular disease outcomes such as blood pressure, TC, LDL-C and CRP 14 392 after low protein and high carbohydrate diet. Thus, this type of hypocaloric diets, in 393 sedentary participants cannot minimize the risks for cardiovascular and metabolic 394 diseases. On the contrary, several studies [e.g. 34, 45] have reported an improvement in 395 TG, TC and LDL-C serum levels when replacing dietary CHO content with PRO. 396 Nonetheless, long-term variations of HP diet on lipid profiles warrant further 397 investigation. 398 Unfortunately, there are some limitations in this study that require consideration. 399 First, our sample of overweight individuals cannot generalize our findings to the general 400 population. However, the results of the present study can be a useful tool for future 401 studies of this kind in order to better establish the association of different dietary 402 intervetions with body and other biochemical indexes, in larger samples which are more 403 coherent to the general population. Second, non compliance, self-reported data, 404 measurement errors and bias of food records could have an impact. Third, due to 405 equipment failure, physical activity could not be evaluated through accelerometer devices 406 but was recorded via recall self-reported questionnaire. 407 The results of the present study suggest that in sedentary overweight individuals, 408 a short-term hypocaloric MD seems to provide all the necessary nutrients that are 409 required to induce significant body and fat mass reductions, with FFM concomitant 410 maintenance, moreover inducing positive changes on lipidemic-glucose profile, hepatic 411 and inflammation/muscle damage related blood indices. Thus, it lowers the risks for 412 chronic metabolic and cardiovascular diseases. In contrast, at least in non-trained 413 overweight individuals, HP and HPW reduced body mass, however favoring the 414 reduction of FFM and not of fat mass, while they have negative effects on lipidemic 415 profile and on health/inflammation/muscle damage blood markers. Particularly, these 416 type of diets also increase uric acid blood concentrations, changes which are related to 417 increased risk for insulin resistance, metabolic syndrome and cardiovascular diseases 418 (Figure 3). Thus, hypocaloric high protein diets, especially with whey protein 419 supplementation, should be avoided, during short-term caloric restriction periods, in non- 420 trained overweight men and women. 421 422 15 423 Approval 424 All procedures were in accordance with the Declaration of Helsinki and approved by the 425 Department of Nutrition Sciences and Dietetics, Faculty of Health Sciences, International 426 Hellenic University, Research Ethics Committee (ref. number 1014/2018), while all 427 participants signed an informed consent before entering the research procedure. 428 429 Authors’ Contribution 430 KF and SM performed part of experiments, analyzed part of the data, designed and 431 supervised the study, researched data and contributed to the writing of the manuscript. 432 KK, KV, PS, AH, AM, AK, TN performed part of the experiments and analysed data. 433 MH contributed to the writing of the manuscript and SKP designed and supervised the 434 study. 435 436 Grants, sponsors, and funding sources: No grant support was received for this study. 437 438 Conflict of Interest: None 439 440 441 442 References 443 [1] Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. (2014) 444 Global, regional, and national prevalence of overweight and obesity in children and 445 adults during 1980–2013: a systematic analysis for the Global Burden of Disease 446 Study 2013. The Lancet 384, 766-781. 447 [2] Albuquerque D, Stice E, Rodríguez-López R, Manco L, Nóbrega C (2015) Current 448 review of genetics of human obesity: from molecular mechanisms to an evolutionary 449 perspective. Mol Genet Genomic 290, 1191-221. 450 [3] Sureshchandra S, Marshall N, Wilson R, Barr T, Rais M, Purnell J, et al. (2018) 451 Inflammatory determinants of pregravid obesity in placenta and peripheral blood. 452 Front Physiol 9, 1089. 16 453 [4] Raynor H, Champagne C (2016) Position of the Academy of Nutrition and Dietetics: 454 interventions for the treatment of overweight and obesity in adults. J Acad Nutr Diet 455 116, 129-147. 456 [5] Muramoto A, Matsushita M, Kato A, Yamamoto N, Koike G, Nakamura M, et al. 457 (2014) Three percent weight reduction is the minimum requirement to improve 458 health hazards in obese and overweight people in Japan. Obes Res Clin Pract 8, 459 e466-e475. 460 [6] Weinheimer E, Sands L, Campbell W (2010) A systematic review of the separate and 461 combined effects of energy restriction and exercise on fat-free mass in middle-aged 462 and older adults: implications for sarcopenic obesity. Nutr Rev 68, 375-388. 463 464 [7] Methenitis S. 2018A Brief Review on Concurrent Training: From Laboratory to the Field. Sports 6, 127. 465 [8] Argilés J, Campos N, Lopez-Pedrosa J, Rueda R, Rodriguez-Mañas L (2016) Skeletal 466 Muscle Regulates Metabolism via Interorgan Crosstalk: Roles in Health and Disease. 467 J Am Med Dir Assoc 17, 789-796. 468 [9] Papadopoulou S, Feidantsis K, Hassapidou M, Methenitis S (2020) The specific 469 impact of nutrition and physical activity on adolescents’ body composition and 470 energy balance. Res Q Exerc Sport DOI: 10.1080/02701367.2020.1773374 471 472 473 474 475 476 477 478 479 480 [10] Pasiakos S, Margolis L, Orr J (2014) Optimized dietary strategies to protect skeletal muscle mass during periods of unavoidable energy deficit. FASEB J 29, 1136-1142. [11] Pesta D, Samuel V (2014) A high-protein diet for reducing body fat: mechanisms and possible caveats. Nutr Metabol 11, 53. [12] Phillips S (2014) A brief review of higher dietary protein diets in weight loss: a focus on athletes. Sports Med 44, 149-153. [13] Phillips S, Chevalier S, Leidy H (2016) Protein “requirements” beyond the RDA: implications for optimizing health. Appl Physiol Nutr Metab 41, 565-572. [14] Cava E, Yeat NC, Mittendorfer B (2017) Preserving healthy muscle during weight loss. Adv Nutr 8, 511-519. 481 [15] Noakes M, Keogh J, Foster P, Clifton P (2005) Effect of an energy-restricted, high- 482 protein, low-fat diet relative to a conventional high-carbohydrate, low-fat diet on 17 483 weight loss, body composition, nutritional status, and markers of cardiovascular 484 health in obese women. Am J Clin Nutr 81, 1298-1306. 485 [16] Antonio J, Ellerbroek A, Silver T, Vargas L, Tamayo A, Buehn R, et al. (2016) A 486 high protein diet has no harmful effects: A one-year crossover study in resistance- 487 trained males. J Nutrition Metab 9104792. 488 489 [17] Rietman A, Schwarz J, Tomé D, Kok F, Mensink M (2014) High dietary protein intake, reducing or eliciting insulin resistance? Eur J Clin Nutr 68, 973. 490 [18] Krebs M, Krssak M, Bernroider E, Anderwald C, Brehm A, Meyerspeer M, et al. 491 (2002) Mechanism of amino acid-induced skeletal muscle insulin resistance in 492 humans. Diabetes 51, 599-605. 493 [19] Zhu Y, Hu Y, Huang T, Zhang Y, Li Z, Luo C, et al. (2014) High uric acid directly 494 inhibits insulin signalling and induces insulin resistance. Biochem Biophys Res 495 Commun 447, 707-714. 496 [20] Manzel A, Muller D, Hafler D, Erdman S, Linker R, Kleinewietfeld M (2014) Role 497 of “Western diet” in inflammatory autoimmune diseases. Curr Allergy Asthma Rep 498 14, 404. 499 [21] Hernáez Á, Castañer O, Elosua R, Pintó X, Estruch R, Salas-Salvadó J, et al. (2017) 500 Mediterranean 501 cardiovascular-risk individuals: a randomized controlled trial. Circulation 135, 633- 502 643. diet improves high-density lipoprotein function in high- 503 [22] González-Pérez J, Sánchez-Leenheer S, Delgado AR, González-Vargas L, Díaz- 504 Zamudio M, Montejo G. et al. (2013) Clinical impact of a 6-week preoperative very 505 low calorie diet on body weight and liver size in morbidly obese patients. Obes Surg 506 23(10), 1624-1631. 507 [23] Kermack AJ, Wellstead SJ, Fisk HL, Cheong Y, Houghton FD, Macklon NS, Calder 508 PC. (2020) The Fatty Acid Composition of Human Follicular Fluid Is Altered by a 509 6‐ Week Dietary Intervention That Includes Marine Omega‐ 3 Fatty Acids. Lipids. 510 [24] Kermack AJ, Lowen P, Wellstead SJ, Fisk HL, Montag M, Cheong Y, et al (2020b) 511 Effect of a 6-week “Mediterranean” dietary intervention on in vitro human embryo 512 development: The Preconception Dietary Supplements in Assisted Reproduction 513 double-blinded randomized controlled trial. Fertil Steril 113(2), 260-269. 18 514 [25] Helms E, Zinn C, Rowlands D, Brown S (2014) A systematic review of dietary 515 protein during caloric restriction in resistance trained lean athletes: a case for higher 516 intakes. Int J Sport Nutr Exerc Metab 24(2), 127-138 517 518 [26] Kim IY, Deutz N, Wolfe R (2018) Update on maximal anabolic response to dietary protein. Clin Nutr 37, 411-418. 519 [27] Papadopoulou S, Dalatsi V, Methenitis S, Feidantsis K, Pagkalos I, Hassapidou M 520 (2017) Nutritional Routine of Tae Kwon Do Athletes Prior to Competition: What Is 521 the Impact of Weight Control Practices? J Am Coll Nutr 36, 448-454. 522 [28] Methenitis S, Zaras N, Spengos K, Stasinaki AN, Karampatsos G, Georgiadis G, et 523 al. (2016) Role of Muscle Morphology in Jumping, Sprinting, and Throwing 524 Performance in Participants With Different Power Training Duration Experience. J 525 Strength Cond Res 30, 807-817. 526 [29] Ainsworth B, Haskell W, Herrmann S, Meckes N, Bassett Jr D, Tudor-Locke C, et 527 al. (2011) Compendium of Physical Activities: a second update of codes and MET 528 values. Med Sci Sports Exerc 43, 1575-1581. 529 [30] Faul F, Erdfelder E, Lang AG, Buchner A. (2007) G* Power 3: A flexible statistical 530 power analysis program for the social, behavioral, and biomedical sciences. Behav 531 Res Methods 39(2), 175-191. 532 [31] de Souza R, Bray G, Carey V, Hall K, LeBoff M, Loria C, et al. (2012) Effects of 4 533 weight-loss diets differing in fat, protein, and carbohydrate on fat mass, lean mass, 534 visceral adipose tissue, and hepatic fat: results from the POUNDS LOST trial. Am J 535 Clin Nutr 95, 614-625. 536 [32] Johnston B, Kanters S, Bandayrel K, Wu P, Naji F, Siemieniuk R, et al. (2014) 537 Comparison of weight loss among named diet programs in overweight and obese 538 adults: a meta-analysis. JAMA 312, 923-933. 539 [33] Wycherley T, Moran L, Clifton P, Noakes M, Brinkworth G (2012) Effects of 540 energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: 541 a meta-analysis of randomized controlled trials. Am J Clin Nutr 96, 1281-1298. 542 543 [34] Clifton P (2012) Effects of a high protein diet on body weight and comorbidities associated with obesity. Br J Nutr 108, S122-S129. 19 544 [35] Morton R, Murphy K, McKellar S, Schoenfeld B, Henselmans M, Helms E, et al. 545 (2018) A systematic review, meta-analysis and meta-regression of the effect of 546 protein supplementation on resistance training-induced gains in muscle mass and 547 strength in healthy adults. Br J Sports Med 52, 376. 548 [36] Bujak A, Crane J, Lally J, Ford R, Kang S, Rebalka I, et al. (2015) AMPK activation 549 of muscle autophagy prevents fasting-induced hypoglycemia and myopathy during 550 aging. Cell Metab 21, 883-890. 551 [37] Bhatia H, Pattnaik B, Datta M (2016) Inhibition of mitochondrial β-oxidation by 552 miR-107 promotes hepatic lipid accumulation and impairs glucose tolerance in vivo. 553 Int J Obes 40, 861. 554 555 556 557 558 559 [38] Duan Y, Li F, Li Y, Tang Y, Kong X, Feng Z, et al. (2016) The role of leucine and its metabolites in protein and energy metabolism. Amino Acids 48, 41-51. [39] Trommelen J, Betz M, van Loon L (2019) The muscle protein synthetic response to meal ingestion following resistance-type exercise. Sports Med 49, 185-197. [40] Saxton R, Sabatini D (2017) mTOR signaling in growth, metabolism, and disease. Cell 168, 960-976. 560 [41] Bhanpuri N, Hallberg S, Williams P, McKenzie A, Ballard K, Campbell W, et al. 561 (2018) Cardiovascular disease risk factor responses to a type 2 diabetes care model 562 including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: 563 an open label, non-randomized, controlled study. Cardiovasc Diabetol 17, 56. 564 [42] Miranda J, Almeida G, Martins R, Cunha M, Belo V, Santos J, et al. (2015) The role 565 of uric acid in the insulin resistance in children and adolescents with obesity. Rev 566 Paul Pediatr 33, 431-436. 567 568 [43] El Din U, Salem M, Abdulazim D (2017) Uric acid in the pathogenesis of metabolic, renal, and cardiovascular diseases: A review. J Adv Res 8, 537-548. 569 [44] Maruhashi T, Hisatome I, Kihara Y, Higashi Y (2018) Hyperuricemia and 570 endothelial function: From molecular background to clinical perspectives. 571 Atherosclerosis 278, 226 - 231. 572 [45] Amini P, Maghsoudi Z, Feizi A, Ghiasvand R, Askari G (2016) Effects of high 573 protein and balanced diets on lipid profiles and inflammation biomarkers in obese 20 574 and overweight women at aerobic clubs: A randomized clinical trial. Int J Prev Med 575 7(1), 110-120. 576 [46] Rolland C, Hession M, Murray S, Wise A, Broom I (2009) Randomized clinical trial 577 of standard dietary treatment versus a low‐ carbohydrate/high‐ protein diet or the 578 LighterLife Programme in the management of obesity. J Diabetes 1, 207-217. 579 [47] Noto H, Goto A, Tsujimoto T, Noda M (2016) Long‐ term Low‐ carbohydrate Diets 580 and Type 2 Diabetes Risk: A Systematic Review and Meta‐ analysis of 581 Observational Studies. J Gen Fam Med 17, 60-70. 582 583 584 585 586 587 588 589 590 591 592 593 594 595 596 597 598 Figure Legends 599 600 Figure 1. Correlation plots between free fat mass percentage changes and (A) Daily 601 carbohydrate energy intakes and (B) Daily protein energy intakes, for the total of 602 participants (n=30) 21 603 604 22 605 Figure 2. Correlation plots between C-reactive protein percentage changes and (A) Daily 606 carbohydrate energy intakes and (B) Daily protein energy intakes, for the total of 607 participants (n=30) 608 609 23 610 Figure 3. Summarized model of the effects of three different hypocaloric (-700 kcal/day) 611 diets, Mediterranean Diet, High Protein diet and High Protein-Whey Supplementation 612 diet on body composition and examined biochemical blood markers. 613 614 615 616 617 Table 1. Characteristics of the three nutritional interventions. Mediterranean (n=10) Regular Intervention Total Daily Energy Expenditure (kcal) Energy Intake (kcal) Energy Balance (kcal) Carbohydrates (g) Carbohydrates (kcal) Carbohydrates as Percentage of Total Calories Intake (%) Groups (Hypocaloric Diets) High Protein (n=10) Regular Intervention High Protein-Whey (n=10) Regular Intervention 2486.17±450.8 2531.96±385.3 2536.74±421.59 2517.54±410.12 2556.01±486.25 2544.82±426.37 9 4 2582.89±614.2 1851.10±438.60 2642.12±407.2 1851.30±424.12 1882.13±417.81 2662.17±587.98 5 * 2 * * 96.72±74.12 110.16±65.98* 106.09±71.02* -642.71±173.23 684.41±182.60* 666.23±190.68* Carbohydrates 258.28±59.14* 341.29±48.34 347.50±55.49 201.88±48.86* M 350.28±66.92 207.55±48.56* M HP, HPW 1365.16±201.3 1081.12±136.59 1390.77±281.9 1401.14±267.68 807.53±95.46* M 830.20±94.24* M 7 * 8 * 52.85±12.60 Fibers (g) 27.59±7.92 Soluble Fibers (g) 4.20±2.55 55.81±2.12* HP, 52.60±15.30 43.62±2.32* M 52.63±14.25 44.11±2.30* M HPW 26.58±10.83 24.90±5.26 M 21.07±7.53 24.28±5.18 M 7.22±2.70* 5.85±2.85 5.27±1.26 4.84±2.16 5.87±1.59 HPW 41.28±4.53* HP, 24 Insoluble Fibers (g) Sugar (g) Monosaccharide s (g) Disaccharides (g) Fat (g) Fat (kcal) Fat as Percentage of Total Calories Intakes (%) Saturated Fatty Acids (g) Monounsaturate d Fatty Acids (g) Polyunsaturated Fatty Acids (g) Trans Fatty Acids (g) Cholesterol (mg) 9.63±7.57 11.29±2.37 8.9±4.06 10.87±3.29 63.71±15.99 61.43±7.89 M 60.44±13.20 61.28±3.52 M HPW 13.35±8.27 18.37±3.58 M 14.31±6.96 18.41±2.94 M 10.59±7.87 16.48±7.96* 7.97±7.99 14.25±2.22* 8.30±5.87 14.73±3.24 93.72±37.59 843.52±100.11 57.5±9.3* 517.5±84.3* 95.47±37.05 859.23±148.21 55.9±10.1* 503.11±87.1* 32.65±10.25 27.95±1.5 32.05±14.41 27.45±0.9 32.27±16.12 26.73±0.9 25.93±12.76 7.81±1.40* 29.07±12.29 7.25±2.62* 28.93±10.56 7.23±3.22* 32.68±15.44 22.58±3.86* 36.50±14.64 27.61±5.96* 37.49±17.71 24.74±5.19* 7.58±4.15 12.06±2.73* 7.12±3.00 12.99±3.01* 8.00±2.56 11.89±5.24* 4.02±3.48 2.11±1.25* 3.89±1.59 1.99±1.52* 5.02±3.25 2.14±1.33* 60.27±20.07 14.80±12.70 12.48±1.47* 49.93±8.06* HP, HPW 21.73±2.69* HP, Fats 94.11±27.28 56.5±8.5* 846.02±109.13 508.18±77.2* Proteins (g) 360.47±99.47 151.29±67.05* 348.11±110.24 147.78±55.22* 364.81±71.11 150.98±43.66* Protein 73.20±14.21 HP, 92.81±30.00 98.21±21.78 133.89±29.78* M 95.06±26.15 134.94±29.80* M HPW Proteins (kcal) 371.24±75.23 Proteins as Percentage of Total Calories Intakes (%) 14.37± 4.12 Med Diet Score Cereals (servings/week) Potatoes (servings/week) Fruits (servings/week) Vegetables (servings/week) Legumes (servings/week) Fish (servings/week) Red Meat (servings/week) Poultry (servings/week) Full-fat dairy products (servings/week) Olive oil (teaspoons/ week) 618 619 620 621 9.11±7.33 32.28±7.25 292.81±63.21 HP, 539.79±129.22* 380.24±80.12 28.93±1.45* M 14.28±8.12 28.68±1.90* M Med Diet Score and Components 44.40±7.25* HP, 30.28±4.88 36.90±4.98 M HPW 30.19±6.20 38.44±4.76 M 15.87±0.49 HP, HPW 392.84±66.66 535.58±119.15* M HPW 14.86±7.77 M 7.95±5.23 31.30±2.21* 9.10±6.98 32.00±6.28* 7.65±5.43 30.60±7.84* 4.00±2.54 6.50±1.88* 4.65±3.65 5.70±1.68* 3.70±1.93 5.45±1.67* 9.45±5.83 21.30±1.47* 10.95±6.29 20.60±1.80* 10.45±6.21 21.60±1.10* 11.45±8.94 27.75±6.63* 11.40±6.85 24.15±5.64* 15.45±10.25 24.80±6.28* 1.80±0.94 1.70±0.63 1.60±0.73 1.67±0.45 1.70±0.99 1.50±0.55 0.85±0.57 2.50±0.55* 1.15±1.00 1.90±0.84 0.90±0.67 1.94±0.47 3.10±2.31 2.75±1.11* M 4.00±1.00 2.00±1.01* M HPW 3.60±2.02 9.30±0.94* M 4.00±2.59 9.25±1.68* M 11.65±7.52 3.25±1.11* 13.90±8.25 2.89±1.25* 12.45±7.99 3.01±1.45* 3.25±2.14 7.00±1.00 4.57±2.82 7.01±0.94 5.50±2.41 6.89±1.25 3.80±1.39 2.90±1.83 1.55±0.63* HP, HPW 4.20±0.94* HP, Values are mean ± SD. (*) denotes the significant differences between pre to post values in each group separately. Letters denote statistical significant difference (p < 0.05) per variable, between the marked groups (where M = Mediterranean Diet, HPW = High Protein-Whey Diet, HP = High Protein). DRI: Dietary Reference Intakes 25 622 623 624 625 626 627 Table 2. Mean values and percentage changes of participants’ anthropometrics characteristics, body composition and resting metabolic rate before and after interventions Mediterranean (n=10) Pre Body Mass (Kg) Body Mass Index (kg·m-2) Percenta ge Body Fat (%) 628 629 630 631 632 633 HPW 4.1±2. 28.4±2.7 26.6±3.1* HP, 2 HPW 27.1±7.9* 5.9±4. 33.0±7.8 HPW 2# HP, Total Body Water (%) 55.4±5.3 58.7±9.1 1.3±1. HP, HPW 1 HP, HPW 6.6±0.6 54.2±7.2 1.2±0. 8 6.4±0.9 HP, 2.0±1. HPW 1 HP, HPW 1.4±0. 1708.9±35 1722.1±32 HP, 9 0.5 5.8 HPW Partial eta squared (η2) Grou TimGrou pX e p Time 86.7±7.9 84.6±10.2*1.7±1. 2M 85.7±7.2 84.3±7.2 1.2±1. 0M 0.71 0.0360.262 4 29.1±2.5 27.9±3.2 2.3±1. 9M 28.7±2.2 27.9±2.1 1.7±1. 5M 0.74 0.1280.315 7 1.7±1. 5# M, HP 0.45 0.2250.394 3 7.9±3. 2M 0.22 0.1910.155 8 52.7±8.5 50.9±6.4 1.8±0. 9 54.4±8.7 52.2±7.4 2.2±1. 1 0.01 0.0340.020 2 6.8±0.8 6.5±0.8* M 4.4±2. 2M 6.9±0.7 6.4±0.5* 5.2±2. M 6M 0.26 0.1800.182 4 1923.4±31 1750.5±2 8.9±2. 6.6 90. 3 8 M, HP 0.05 0.0790.071 0 Post Chang e (% or Δ#) High Protein-Whey (n=10) Chang e (% or Δ#) Pre 32.0±8.7* 2,0±1. 34.3±8.1 HPW 8# M, HPW 60.4±9.8 Resting Metabol ic Rate (kcal·da y-1) Chang e (% or Δ#) 3.5±1. 84.1±8.7 79.6±9.3* HP, 1 Free Fat Mass (kg) Phase Angle (O ) Post High Protein (n=10) Pre 35.5±9.1 Post 33.8±8.9 HP, M HPW 61.5±8.9 57.2±10.1* 4.9±3. M 1M 1905.4±24 1816.7±26 4.6±2. 3.1 9.4 7 M, HPW 59.1±11.2 54.4±7.1* M Values are mean ± SD. Δ: the difference between pre to post values; %: the percentage changes of post compared to pre values. (#) denote Δ. Letters denote statistical significant difference (p < 0.05) per variable, between the marked groups (where M = Mediterranean Diet, HPW = High Protein-Whey Diet, HP = High Protein). (*) denote the significant differences between pre and post intervention values, in each group separately (p<0.05). 26 634 635 Table 3. Mean values and percentage changes of participants’ blood markers before and after interventions Mediterranean (n=10) Pre Triglycerides (mg∙dl-1) Cholesterol (mg∙dl-1) High Density Lipoprotein (mg∙dl-1) Low Density Lipoprotein (mg∙dl-1) Post Chang e (%) 158.2±3091.0±25.4*H 42.4±15 P, HPW .9 .4 HP, HPW 185.7±21145.1±30.4* 21.8±5. HP, HPW .2 6 HP, HPW 38.4±7.9 41.1±7.1*HP,18.2±12 HPW .9 HP, HPW High Protein (n=10) Pre Post Chang e (%) 187.3±31 171.0±24. -8.7±6.2 M .7 9M 188.1±15 181.4±25. -3.5±2.8 M .4 9M 0.19 0.185 0.205 9 38.2±7.1* 3.5±3.1 39.4±10. 39.2±10.9 0.5±5.1 M M,HP 4 0.22 0.201 0.228 2 138.7±31 129.5±50. -6.6±4.9 M,HP .9 9M 0.32 0.421 0.309 1 9.81±11. 5* M 0.25 0.389 0.325 9 9.9±1.1* 54.6±32. HP, M 7 M,HP 0.20 0.159 0.149 9 0.15 0.117 0.241 6 36.9±9.2 M M,HPW 51.1±6.7 54.9±5.8 7.4±3.5 Monocyte (%) Urea (mg∙dl-1) 17.9±10 .9 HP, HPW 5.3±0.9 *HP, 6.2±0.9 14.5±6. HPW 1 HP, HPW HP, 28.8±6.9 -2.1±0.4 29.4±6.2 HPW HP, HPW 34.4±4.2 28.4±7.1* HP, HPW 11.1±8. 8 HP, HPW Creatine 132.4±89101.8±53.9* 25.4±11 HP, HPW -1 .0 Kinase (U∙L ) .2 HP, HPW C-Reactive 0.2±0.1 HP, 0.3±0.1 33.3±10 HPW -1 Protein (mg∙dl ) .1 HP, HPW Creatinine (mg∙dl-1) 0.9±0.1 0.8±0.1 HP, HPW 79.5±9.6 86.4±10.4 8.6±8.4 *M 81.5±6.4 89.5±7.4 6.3±1.5 7.8±1.5* 23.8±18 M, HPW .4 M,HPW 6.4±1.8 0.29 0.302 0.189 0 31.9±13. 3 M,HP 0.19 0.243 0.583 7 42.7±8.2* 40.46±20 M .1 M,HP 0.58 0.371 0.227 4 72.1±36. 4 M,HP 0.60 0.325 0.495 7 130.9±74 169.9±80. 29.7±13 .1 9* M .2 M,HPW 129.9±75 185.4±70. 42.7±16. .6 2* M 6 M,HP 0.23 0.245 0.287 3 66.6±40 0.3±0.1 0.5±0.2* M M,HPW .1 266.6±55 0.3±0.2 1.1±0.3* M .1 M,HP 0.21 0.282 0.341 8 206.5±51 255.6±40. 23.7±9.9 M,HP .8 3* M 0.38 0.401 0.300 1 48.7±17. 5 M,HP 0.28 0.181 0.499 9 40.8±10. 62.7±10.7 53.6±28. 6 * HP, M 2 M,HP 0.73 0.399 0.610 8 40.3±4.6* 14.8±8. M 2M 22.5±10 6.2±1.6 7.6±1.3* M M,HPW .1 30.4±7.4 38.1±7.1* 25.3±14 M .6 M,HPW 36.1±20 1.1±0.3 1.5±0.2* M M,HPW .1 216.1±35189.4±26.3* 12.3±6. HP, HPW .6 7 HP, HPW 212.4±33 235.4±29. 10.9±7. .7 9* M 7 M,HPW 3.8±0.8 HP, -9.5±5.2 30±10.9 4.0±1.4 5.2±0.9* M M,HPW 23.1±10 .7 HP, HPW 42.0±9.1 Gamma- 16.8±6.9 39.1±8.5 20.3±4.3 HPW 30.1±9.1 HP, HPW 18.9±5.0 HP, -6.8±2.3 HPW HP, HPW 16.8±10. 2.3±1.1 17.2±11.7 HP, HPW 5 15.0±9.9 HPW 10.71±4 52.4±9.8 59.9±8.1* 14.3±6.4 M 35.1±5.2 Lactate Dehydrogenase (U∙L-1) Uric Acid (mg∙dl-1) Serum Ammonia (μg∙dl-1) Aspartate Transaminase (U∙L-1) Alanine Transaminase (U∙L-1) 4.2±0.9 Change (%) 0.20 0.227 0.288 0 Neutrophils (%) 55.1±6.9 56.1±7.0 1.8±1.2 Lymphocyte (%) Post 162.3±41 148.8±31. -8.3±4.4 M,HP .7 9* M 142.2±27 121.3±34. 14.6±9. M .6 4 7 M,HPW White Blood Cells (103/μL) Pre Partial eta squared (η2) Grou Tim Grou pX e p Time 159.3±27 126.7±40. 20.4±12 M .4 4* .9 M,HPW 141.7±20110.4±39.4* 22.7±15 HP, HPW .9 .1 HP, HPW 71.9±5.1*HP, 80.1±7.8 14.5±10 HPW .7 6.1±1.4 HP, -3.2±1.1 6.1±1.4 HPW HPW, HP Glucose (mg∙dl1 ) High Protein-Whey (n=10) 50.4±10.0 20.0±12 * M, HPW .2 M,HPW 36.9±7.3 43.6±9.2* 18.1±9.1 M 6.3±1.3 8.3±1.1* M 30.4±7.1 1.1±0.2 1.9±0.2* M 4.1±1.1 6.1±1.5* M 20.7±10. 28.4±15.4 37.3±21 4 *M .4 M 21.8±5.8 31.9±8.8* 46.3±22. M 7M 0.35 0.302 0.329 2 17.1±10. 22.2±14 20.9±7.6 M,HPW 4 .1 15.9±12. 61.0±17. 25.6±12.7 1 4 M,HP 0.21 0.175 0.164 0 25.9±6.3* 51.4±22. M, HP 5 M,HP 0.18 0.199 0.366 16.1±4.7 18.1±5.6 12.4±6. HPW 4 M,HPW 27 17.1±6.0 Glutamyltransfe rase (U∙L-1) Serum Albumin (g∙dl-1) Serum Total Protein (g∙dl-1) 636 637 .1 HP, HPW 4.3±0.1 4.4±0.1 HP, 2.3±0.7 HPW HP, HPW 7.0±0.5 6.9±0.6 HPW -1.2±0.4 HP, HPW 9 4.2±0.1 6.7±0.4 4.9±0.7 M, 16.1±7. HPW 3 M,HPW 7.0±0.2 4.4±2.1 HPW M,HPW 4.3±0.1 6.9±0.5 5.9±0.9* 37.2±13. M, HP 9 M,HP 7.8±0.3* 13.1±5.5 M, HP M,HP 0.19 0.203 0.231 9 0.45 0.221 0.350 7 Values are mean ± SD. Letters denote statistical significant difference (p < 0.05) per variable, between the marked groups (where M = Mediterranean Diet, HPW = High Protein-Whey Diet, HP = High Protein). 638 639 640 641 642 643 644 645 Table 4. Correlations between carbohydrates and protein daily energy intakes and percentage changes of body composition and of selected blood markers after 6 weeks of the nutritional interventions for all participants as a group (n=30). Only significant correlations are presented (p<0.05). Daily Energy (kcal) Percentage Changes (%) Body Mass Body Fat Mass Free Fat Mass Resting Metabolic Rate Triglycerides Low Density Lipoprotein White Blood Cells Urea Creatinine Creatine Kinase C-Reactive Protein Lactate Dehydrogenase Uric Acid Aspartate Transaminase Alanine Transaminase Kcal Difference from Pre Intervention Nutrition (Δkcal) Carbohydrates Proteins Carbohydrates Proteins -0.512 -0.389 0.889 0.518 0.400 -0.799 -0.384 0.400 0.614 0.431 -0.400 0.599 -0.467 0.428 -0.600 0.389 -0.589 -0.666 -0.589 -0.570 0.699 0.703 0.570 0.610 -0.844 0.510 -0.474 0.602 -0.489 0.611 -0.442 0.528 -0.466 0.530 646 647 648 649 28 -0.387 0.397 0.392 -0.403 -0.407 0.415 0.501 -0.514 0.478 0.476 0.372 0.429 0.387 0.401