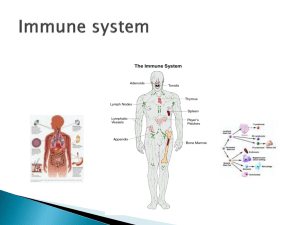
Lecture № 1: Lymphatic System. Lymphoid Organs. Histology of Central Lymphoid Organs. Bone marrow can be red because of the presence of erythrocytes and their precursors, which is indicative of active hemopoiesis; or yellow owing to fat, indicating reduced hemopoiesis. All marrow in newborn humans is red. Fat appears in long bones from the fifth to the seventh year; and by the the age of 18 years, almost all limb marrow is yellow. Hemopoietic marrow in adults is largely restricted to the skull, clavicles, vertebrae, ribs, sternum, and pelvis. The red bone marrow is within the space of bone. It is composed of (a) stromal elements, (b) blood vessels, and (c) developing blood cells at various stages of formation and maturation. Structure of the red bone marrow Bone marrow can be red because of the presence of erythrocytes and their precursors, which is indicative of active hemopoiesis; or yellow owing to fat, indicating reduced hemopoiesis. All marrow in newborn humans is red. Fat appears in long bones from the fifth to the seventh year; and by the the age of 18 years, almost all limb marrow is yellow. Hemopoietic marrow in adults is largely restricted to the skull, clavicles, vertebrae, ribs, sternum, and pelvis. The red bone marrow is within the space of bone. It is composed of (a) stromal elements, (b) blood vessels, and (c) developing blood cells at various stages of formation and maturation. Bone marrow stroma It consists of (1) reticular cells. These cells are branched, with a pale nucleus; they contain many rER cisternae. They form reticulum meshwork.The latter holds the developing blood cells. Functions: (a) formation of the ground substance and reticular fibers (collagen of the 3rd type). The ground substance contains hyaluronic acid, chondroitin sulfate, and heparan sulfate. These glycosaminoglycans may bind growth factors, which control hemopoiesis. Moreover, the ground substance contains laminin and fibronectin, which facilitate adhesion of hemopoietic cells to the marrow stroma, (b) production of special hemopoietic growth factors, (c) by accumulating lipids they may transform into adipocytes found in the bone marrow. (2) osteogenic cells: osteoblasts and osteoclasts; they are situated on the surface of bone trabeculae (endosteum). (3) macrophages. There are two types of macrophages within bone marrow. The first type is represented by fixed macrophagic cells, which remove aged and defective red cells from the circulation by phagocytosis; in addition, these macrophages are involved in the production of some growth factors and, perhaps, facilitate the delivery of reticulocytes to the circulation. The second type of macrophages are nurse cells. The latter seize iron from circulation and convey it to erythroblasts. As a rule, macrophages lie among the erythroblasts, but a macrophage often lies in the center of the erythroblastic islet. The cytoplasm of this macrophage extends out and encloses the surrounding erythroblasts. (4) adipose cells. These cells serve as the sites of fat storage. Moreover, adipose cells take part in the production of some growth factors. It was shown that fat cells aromatize testosterone to estrogen. In some cases, for example, during severe blood loss, these cells lose their fat, thereby decreasing the volume and providing additional space for hemopoiesis. Blood vessels Veins and arteries constitute the vascular compartment of the marrow. The marrow lacks lymphatic vessels. The bone marrow is supplied with medullary branches from the nutrient artery of the bone. A capillary network opens into a well-developed series of thin-walled sinusoids, which empty into a large central sinus. The blood leaves the bone in the emissary vein via the nutrient canal. The bone marrow sinusoids are lined with flat endothelial cells. They lie on a discontinuous basement membrane. In some places the cytoplasm of endothelial cells is so thin that forms “pores” (or “apertures”). Mature blood cells adhere to this pore before being realized into the circulation. Sometimes mature blood cells squeeze through endothelial junctions. Blood cells press to the junction, and the aperture appears. Apertures normally develop only in relationship to the cell passage; they are either occupied by a cell in transit or absent. Developing blood cells form hematopoietic compartments Erythroblasts are produced near sinuses, forming erythroblastic islets. Megakaryocytes lie close against the adventitial surface of the sinusoids. They deliver platelets to the vascular lumen. Since megakaryocytes are large cells, they resist being swept into circulation and prevent vascular leakage. Granulocytes are produced in nests or as dispersed sheets of the cells somewhat away from the vascular sinuses. Lymphocytes (precursors) occur throughout the marrow. Macrophages, reticular, osteogenic, adipose, and vascular cells are all necessary for the formation of the blood cells. They constitute the microenvironment for developing cells. Thymus The thymus is divided into lobes and lobules by connective tissue septa. They extend into the organ from the connective tissue capsule. Each lobule is divided into the peripheral zone called the cortex (it is rich in lymphocytes) and the central zone, namely, medulla (less lymphocytes). The stroma of every thymus lobule consists of branched epithelial cells. These cells are joined together by desmosomes. These epithelial cells form a reticulum (meshwork) within the lobules. That is why they were called reticulo-epithelial cells. They serve as a framework for Tlymphocytes. Macrophages are present within the lobules. Macrophages perform the following functions: (1) phagocytosis and (2) production of the factor stimulating one division and differentiation of Tlymphocytes. It is noteworthy that the phagocytosis of macrophages is unusual. Macrophages will phagocytose only degenerating T-lymphocytes. Large multinucleated cells are present in the outer part of the cortex. As a rule, 20 to 100 Tlymphocytes surround one of these cells. These cells were supposed to secrete some factors for differentiation of T-lymphocytes. These cells were called nurse cells. Some granulocytes, plasma cells, mast cells, and fat cells are present in the thymus. The central zone of every lobule is occupied by reticulo-epithelial cells and lymphocytes. The reticuloepithelial cells of the medulla are less fully branched. The epithelial cells of medulla form thymic corpuscles or Hassall’s corpuscles. These corpuscles consist of epithelial cells tightly wound upon one another in a concentric pattern. The central cells become swollen, calcified, and necrotic. The corpuscle may become keratinized, resembling the epidermis. With age the corpuscles become larger and more prominent. The functions of thymus corpuscles are not known. The development of T-lymphocytes within the thymus T-lymphocyte precursors (II class) migrate to the thymus during embryonic development and some months after birth. At first, these cells appear under the capsule. Proliferation and differentiation of T-lymphocytes (class II and III) begin initially in this part of lobule. Reticuloepithelial cells secrete thymosin and thymopoetin (specific factors for T-lymphocyte differentiation). In adults only lymphoblasts (IV class) are present under the capsule. Lymphoblasts then gradually turn into T-lymphocytes. These T-lymphocytes lie only within the cortex. This differentiation results in the following subclasses of T-lymphocytes: T-killers, T-helpers, and T-supressors. Each type of these lymphocytes has specific receptors. This development of T-lymphocytes was termed antigen-independent proliferation and differentiation. T-lymphocytes of the cortex cannot contact with an antigen due to the presence of the blood–thymic barrier in the cortex. This barrier consists of endothelial cells of capillary, endothelial basement membrane, perivascular connective tissue sheath containing many macrophages and reticulo-epithelial cells, the basement membrane of reticulo-epithelial cells, and the sheath of reticulo-epithelial cells. As T-cells mature and move deep into the cortex, more than 90 to 95% of them die. Macrophages will phagocytose only T-lymphocytes that are confused about self and nonself. If this population of T-cells remains in the thymus, it would cause an autoimmune disease. Thus, only 5 to 10% of T-lymphocytes leave the thymus. These T-cells are mature, but innocent or virginal. They migrate to the peripheral organs of the immune system (spleen, lymph nodes, appendix, etc.), where lymphocytes encounter an antigen. . After this antigen stimulation, antigen-dependent proliferation and differentiation of Tlymphocytes occur in the peripheral organs of the immune system. The thymus reaches its greatest weight at puberty followed by its slow atrophy or age involution. It involves two distinct processes: (1) fatty infiltration and (2) T-lymphocyte decrease (the lobules atrophy, and the septae widen). Although there is considerable age involution, the thymus remains a weighty functional organ. This normal process of slow thymic involution associated with ageing should be distinguished from acute thymic involution or accidental involution. This involution may occur in response to severe disease or stress. During stress many corticosteroids appear in the bloodstream. These hormones induce the lysis of immature T-cells. Thymus gland The thymus is a primary lymphatic organ, present in the superior mediastinum and it is formed of two lobes. Its presence is required for the immune response to be fully established. The thymus gland reaches maturity during childhood and become rudimentary later on at puberty. Although the thymus is packed with lymphocytes, it does not filter lymph. Structure of thymus gland: Thymus gland is formed of stroma and parenchyma - Thymus is covered with thick connective tissue capsule that sends septa into the two lobes which dividing them into incomplete lobules. - Each lobule is divided into peripheral dark stained cortex and central pale stained medulla. - The stroma is formed of reticuloepithelial network that hold lymphocytes. - Cortex: • It is much darker than medulla because of the presence of large number of T-lymphocytes or thymocytes. • Cortex is the site of T-lymphocytes maturation. • The cortex contains also macrophage, and reticuloepithelial cells. • Reticuloepithelium are stellate cells with pale nuclei and long cytoplasmic processes that join together and completely isolate the cortex from the medulla, and are divided into three types; type I, type II, and type III. Structure of the Thymus gland showing incomplete lobule composed of the cortex and medulla. Medulla looked lighter than the cortex and contain thymic or Hassell`s corpuscles - Medulla • It is much lighter than the cortex because of lymphocytes are lass abundant than the cortex, and contain large number of reticuloepithelial cells. • It contains spherical acidophilic structure called thymic or Hassell`s corpuscles, which is found only in the medulla, and appears to be degenerating reticuloepithelial cells. It contains also non-fenestrated blood capillaries that form the thymic barriers. • The reticuloepithelial cells are responsible for the secretion of factors which promote the maturation of the T cells. As the cells mature, they are pushed in towards the medulla, where they enter the blood vessels. Blood thymic barrier: The blood thymus barrier, a continuous endothelium (non-fenestrated), prevents blood borne antigens from reaching the cortex. The capillaries of the medulla are fenestrated and allow T- cells to enter the circulation. Function of the thymus gland: - Thymus gland is essential for T-lymphocyte maturation. - Reticuloepithelial cells act as endocrine gland that secret different hormones required for T-cell maturation such as; thymosin, thymopoietin, thymolin, and thymic humoral factor. Lecture № 2: Lymphatic System. Lymphoid Organs. Histology of Peripheral Lymphoid Organs. - The lymphatic system is vital to the defense mechanism against infectious agents. - The cells which deal with these agents arose, developed, matured, and/or stored in lymphatic tissues. - The lymphatic vessels and lymphoid organs are closely associated with the cardiovascular system. - Lymph itself is a clear and slightly yellowish fluid derived from blood, and contains white blood cells (mainly lymphocytes). - Lymph starts as blood fluid that passes through the tissue spaces and drained back by thin vein like lymphatic vessels, and then re-enter the venous circulation. - There are lymphoid cells in most tissues of the body arranged either loosely as aggregations, formed into encapsulated structures such as lymph nodes, or freely mobile as individual cells. Types of lymphoid tissues: 1- The lymphoid tissue is divided into primary or secondary: - Primary lymphoid tissues are the tissues in which lymphocytes are generated and differentiate into mature lymphocytes: such as bone marrow for B cells, and the bone marrow and the thymus for T cells. - Secondary lymphoid tissues are the tissues in which immune responses are initiated, and the lymphatic vessels that connect them to the tissues and the bloodstream and thus to sites of infection; i.e. secondary lymphoid tissue brings antigen together with lymphocytes. 2- The lymphoid tissue can be divided into diffuse or nodular: - Diffuse lymphatic tissue consists of unorganized aggregation of lymphocytes. These can be found wherever localized conditions have attracted lymphocytes in large numbers, and vary greatly in size. Such aggregations are usually transient features. - Localized or Nodular lymphatic tissue is always found surrounded by diffuse tissue and it is much more organized. The typical example of nodular lymphatic tissue is the germinal center, a highly ordered collection of B-lymphocytes found in some lymphatic organs. Not all lymphatic organs will contain germinal centers. Germinal centers never occur outside of those lymphatic system organs that can provide an appropriate environment for them. Diagrammatic illustration of both diffuse and nodular lymphatic structures The association of nodular/diffuse, germinal center/unorganized tissue can be found in lymph nodes, spleen, thymus gland, tonsils, appendix, and Peyer's patches of the ileum. Spleen The spleen is a complex organ found in the abdominal cavity, carrying out filtration of particles and aged red cells from the blood, and responding to the presence of antigens. The spleen is really part of the circulatory system, but it is always described with the lymphatic organs because of the very large population of lymphocytes found in it. The spleen is a flaccid bag that serves as a storage site for blood. Structure of spleen showing the capsule, trabeculae, red and white pulps Structure of spleen: Spleen is formed of stroma and parenchyma - Spleen has a discrete CT stroma in the form of capsule which sends septa or trabeculae deep into the volume of the organ. The capsule is formed of collagen with some elastic fibers. - Between the trabeculae, there is a network of reticular fibers and reticular cells that form the framework of the spleen. The meshes of this network hold cells of splenic parenchyma. - Parenchyma of spleen is formed of splenic pulps (red pulps and white pulps). • Red pulp consists of splenic cords separated by blood sinusoids. The red pulp is made up of a mesh of leaky sinusoids through which the red cells are squeezed. Many of the cells lining the sinusoids are phagocytic and are able to engulf debris from the blood or fragments of broken red cells. o Splenic cords (Cords of Billroth): Formed of loose meshwork of reticular fibers and reticular cells. The meshwork holds cellular elements of the parenchyma such as T-and B-lymphocytes, plasma cells, and blood cells. o Splenic sinusoids: Vary in shape and size, and are lined by elongated endothelial cells. The sinusoidal wall is leaky, with incomplete basement membrane and lack muscular wall. Structure of splenic parenchyma, showing the capsule, trabeculae, white and red pulps. • White pulp: Splenic artery penetrates the hilum, branched to give trabecular arteries that leave the trabeculae and enter parenchyma, of spleen. The arteries then surrounded by sheath of lymphocytes called peri-arterial lymphatic sheath (PALS). The sheath contains mainly Tlymphocytes (thymus dependent zone), whereas the lymphoid follicles contain Blymphocytes. Splenic circulation Function of spleen: - Filtration of blood from foreign materials. - Disposal of defective blood cells - Spleen is involved in recycling g of iron in the body. - Spleen acts as a reservoir of red blood cells. - Spleen acts as a hemopoietic organ during embryonic life. - Spleen has an immunological response; which contain large number of B- and T-lymphocytes that play an important role in defense mechanism. Lymph nodes The lymph node is the most organized of the lymphatic organs and are found along larger lymphatic vessels. They are bean shaped, with a depression on one side (hilum). Blood vessels enter and leave the lymph node at the hilum, whereas lymphatic vessels enter at the periphery, and exit at the hilum. The lymph nodes act as "filters" for lymph as it passes through. Lymph is pushed through from the periphery of the node to its center, and then continues on its way back to join the venous circulation. Structure of lymph nodes: lymph nodes are formed of stroma and parenchyma - Lymph nodes have a discrete CT stroma in the form of capsule which sends trabeculae deep into the volume of the organ. The capsule acts as an overall envelope for the node, and is composed of dense irregular collagen with a few elastic fibers. Between the trabeculae, there is a network of reticular fibers and reticular cells that form the framework of the lymph node. The meshes of this network are filled with lymphocytes, plasma cells and macrophages. - Lymph sinuses are lymph spaces found in the cortex and medulla and are divided into subcapsular, cortical, and medullary lymph sinuses. Structure of lymph node showing the cortex and medulla, as well as afferent and efferent lymphatic and blood vessels - Parenchyma of lymph nodes are formed of cortex and medulla - Cortex: The cortex is further divided into outer cortex and deep or medullary cortex. • The outer cortex is formed of o Primary lymphoid nodules which contain B-lymphocytes o Secondary lymphoid nodules which contain germinal center. o Internodal lymphoid tissue formed of diffuse lymphoid tissue. • The inner or deep cortex which is formed of diffuse lymphoid tissue that extend towered the medulla to join medullary cords. The inner cortex is the site of Tlymphocytes and is called thymus dependent zone. - Medulla: is formed of aggregation of lymphoid tissues that branch and anastomose to form medullary cords. These cords contain small lymphocytes, plasma cells, and macrophages. Function of lymph nodes: - Filtration of lymph - Lymph nodes are the sites of antigen recognition. Diffuse lymphoid tissues Tonsils Tonsils are found in association with the oral cavity, and can easily be identified by their surface covering of folding mucous membrane (stratified squamous epithelium) with deep crypts between these folds, and lymphoid tissue filling the spaces between them. Tonsils are usually well encapsulated by CT on the side away from the oral cavity; germinal centers are normally present in the lymphoid follicles. Small mucus salivary glands are present below the lymphatic tissue and their ducts open onto the surface of the tonsil. The tonsils contain lymphocytes, macrophages and plasma cells. Structure of the tonsils Aggregated Lymphatic Nodules of the Ileum and Appendix These structures are large enough to be visible with the naked eye as whitish areas on that side of the intestine opposite to its mesenteric attachment. These lymphoid follicles have germinal centers, the site of maturation and development of the B-lymphocytes. This cross section of the ileum nicely displays the aggregated lymphatic nodules (still universally called "Peyer's Patches" despite the official nomenclature rules against eponyms). These are the sites of maturation and development of B-lymphocytes. They're very prominent structures in most species. It's quite common to find germinal centers in them, though as the animal ages the number of germinal centers decreases. In cattle, for example, germinal centers are present at the time of birth and they decline relatively rapidly with age, as the pool of "memory" lymphocytes increases. The Concept of the GALT Tonsils and Peyer's patches, along with all the diffuse lymphatic tissue in the gastrointestinal tract and respiratory system, collectively are labeled Gut Associated Lymphatic Tissue (GALT) or Mucus Associated Lymphatic Tissue (MALT).