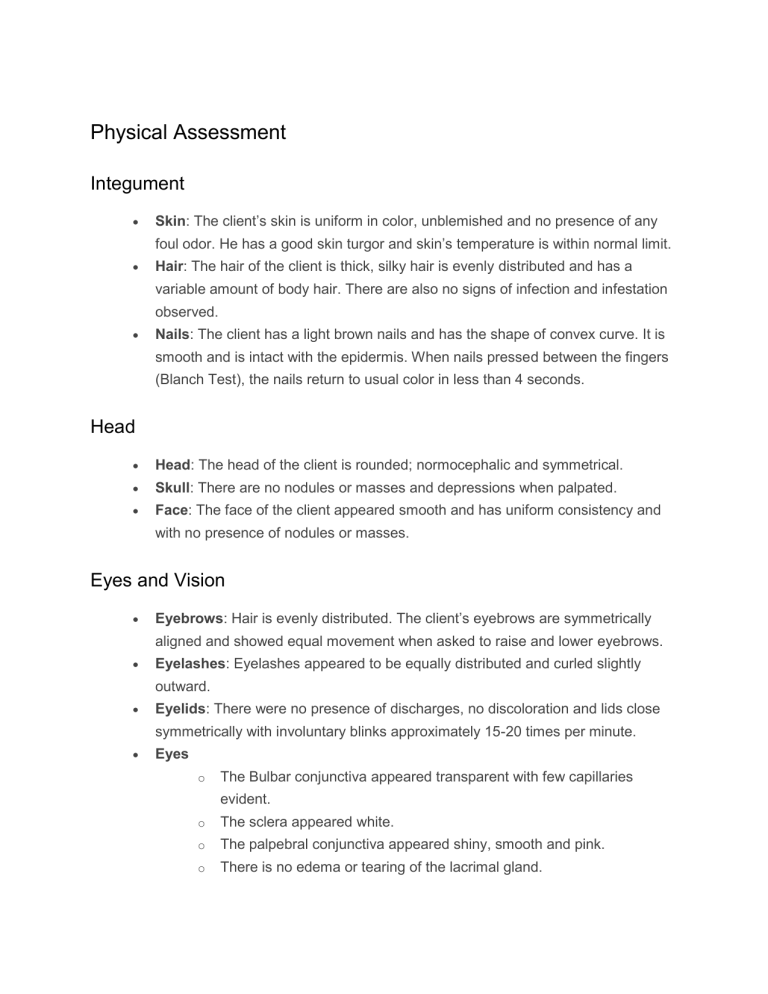
Physical Assessment Integument Skin: The client’s skin is uniform in color, unblemished and no presence of any foul odor. He has a good skin turgor and skin’s temperature is within normal limit. Hair: The hair of the client is thick, silky hair is evenly distributed and has a variable amount of body hair. There are also no signs of infection and infestation observed. Nails: The client has a light brown nails and has the shape of convex curve. It is smooth and is intact with the epidermis. When nails pressed between the fingers (Blanch Test), the nails return to usual color in less than 4 seconds. Head Head: The head of the client is rounded; normocephalic and symmetrical. Skull: There are no nodules or masses and depressions when palpated. Face: The face of the client appeared smooth and has uniform consistency and with no presence of nodules or masses. Eyes and Vision Eyebrows: Hair is evenly distributed. The client’s eyebrows are symmetrically aligned and showed equal movement when asked to raise and lower eyebrows. Eyelashes: Eyelashes appeared to be equally distributed and curled slightly outward. Eyelids: There were no presence of discharges, no discoloration and lids close symmetrically with involuntary blinks approximately 15-20 times per minute. Eyes o The Bulbar conjunctiva appeared transparent with few capillaries evident. o The sclera appeared white. o The palpebral conjunctiva appeared shiny, smooth and pink. o There is no edema or tearing of the lacrimal gland. o Cornea is transparent, smooth and shiny and the details of the iris are visible. The client blinks when the cornea was touched. o The pupils of the eyes are black and equal in size. The iris is flat and round. PERRLA (pupils equally round respond to light accommodation), illuminated and non-illuminated pupils constricts. Pupils constrict when looking at near object and dilate at far object. Pupils converge when object is moved towards the nose. o When assessing the peripheral visual field, the client can see objects in the periphery when looking straight ahead. o When testing for the Extraocular Muscle, both eyes of the client coordinately moved in unison with parallel alignment. o The client was able to read the newsprint held at a distance of 14 inches. Ears and Hearing Ears: The Auricles are symmetrical and has the same color with his facial skin. The auricles are aligned with the outer canthus of eye. When palpating for the texture, the auricles are mobile, firm and not tender. The pinna recoils when folded. During the assessment of Watch tick test, the client was able to hear ticking in both ears. Nose and Sinus Nose: The nose appeared symmetric, straight and uniform in color. There was no presence of discharge or flaring. When lightly palpated, there were no tenderness and lesions Mouth: o The lips of the client are uniformly pink; moist, symmetric and have a smooth texture. The client was able to purse his lips when asked to whistle. o Teeth and Gums: There are no discoloration of the enamels, no retraction of gums, pinkish in color of gums o The buccal mucosa of the client appeared as uniformly pink; moist, soft, glistening and with elastic texture. o The tongue of the client is centrally positioned. It is pink in color, moist and slightly rough. There is a presence of thin whitish coating. o The smooth palates are light pink and smooth while the hard palate has a more irregular texture. o The uvula of the client is positioned in the midline of the soft palate. o The neck muscles are equal in size. The client showed coordinated, Neck: smooth head movement with no discomfort. o The lymph nodes of the client are not palpable. o The trachea is placed in the midline of the neck. o The thyroid gland is not visible on inspection and the glands ascend during swallowing but are not visible. Thorax, Lungs, and Abdomen Lungs / Chest: The chest wall is intact with no tenderness and masses. There’s a full and symmetric expansion and the thumbs separate 2-3 cm during deep inspiration when assessing for the respiratory excursion. The client manifested quiet, rhythmic and effortless respirations. The spine is vertically aligned. The right and left shoulders and hips are of the same height. Heart: There were no visible pulsations on the aortic and pulmonic areas. There is no presence of heaves or lifts. Abdomen: The abdomen of the client has an unblemished skin and is uniform in color. The abdomen has a symmetric contour. There were symmetric movements caused associated with client’s respiration. o The jugular veins are not visible. o When nails pressed between the fingers (Blanch Test), the nails return to usual color in less than 4 seconds. Extremities The extremities are symmetrical in size and length. Muscles: The muscles are not palpable with the absence of tremors. They are normally firm and showed smooth, coordinated movements. Bones: There were no presence of bone deformities, tenderness and swelling. Joints: There were no swelling, tenderness and joints move smoothly. Nursing Assessment in Tabular Form Assessment Findings Integumentary Skin Hair Nails Skull Face When skin is pinched it goes to previous state immediately (2 seconds). With fair complexion. With dry skin Evenly distributed hair. With short, black and shiny hair. With presence of pediculosis Capitis. Smooth and has intact epidermis With short and clean fingernails and toenails. Convex and with good capillary refill time of 2 seconds. Rounded, normocephalic and symmetrical, smooth and has uniform consistency.Absence of nodules or masses. Symmetrical facial movement, palpebral fissures equal in size, symmetric nasolabial folds. Eyes and Vision Hair evenly distributed with skin intact. Eyebrows are symmetrically aligned and have equal movement. Equally distributed and curled slightly outward. Skin intact with no discharges and no discoloration. Lids close symmetrically and blinks involuntary. Eyebrows Eyelashes Eyelids Bulbar conjunctiva Transparent with capillaries slightly visible Palpebral Conjunctiva Shiny, smooth, pink Sclera Appears white. Lacrimal gland, Lacrimal sac, No edema or tenderness over the lacrimal gland and no tearing. Nasolacrimal duct Cornea Assessment Clarity and texture Corneal sensitivity Pupils Visual Fields Visual Acuity Findings Transparent, smooth and shiny upon inspection by the use of a penlight which is held in an oblique angle of the eye and moving the light slowly across the eye. Has [brown] eyes. Blinks when the cornea is touched through a cotton wisp from the back of the client. Black, equal in size with consensual and direct reaction, pupils equally rounded and reactive to light and accommodation, pupils constrict when looking at near objects, dilates at far objects, converge when object is moved toward the nose at four inches distance and by using penlight. When looking straight ahead, the client can see objects at the periphery which is done by having the client sit directly facing the nurse at a distance of 2-3 feet. The right eye is covered with a card and asked to look directly at the student nurse’s nose. Hold penlight in the periphery and ask the client when the moving object is spotted. Able to identify letter/read in the newsprints at a distance of fourteen inches. Patient was able to read the newsprint at a distance of 8 inches. Ear and Hearing Auricles Color of the auricles is same as facial skin, symmetrical, auricle is aligned with the outer canthus of the eye, mobile, firm, non-tender, and pinna recoils after it is being folded. External Ear Canal Without impacted cerumen. Hearing Acuity Test Voice sound audible. Watch Tick Test Able to hear ticking on right ear at a distance of one inch and was able to hear the ticking on the left ear at the same distance Nose and sinuses External Nose Nasal Cavity Symmetric and straight, no flaring, uniform in color, air moves freely as the clients breathes through the nares. Mucosa is pink, no lesions and nasal septum intact and in middle with no Assessment Mouth and Oropharynx Teeth Tongue and floor of the mouth Tongue movement Uvula Gag Reflex Neck Head movement Muscle strength Lymph Nodes Thyroid Gland Thorax and lungs Posterior thorax Spinal alignment Breath Sounds Anterior Thorax Abdomen Abdominal movements Auscultation of bowel sounds Upper Extremities Lower Extremities Findings tenderness. Symmetrical, pale lips, brown gums and able to purse lips. With dental caries and decayed lower molars Central position, pink but with whitish coating which is normal, with veins prominent in the floor of the mouth. Moves when asked to move without difficulty and without tenderness upon palpation. Positioned midline of soft palate. Present which is elicited through the use of a tongue depressor. Positioned at the midline without tenderness and flexes easily. No masses palpated. Coordinated, smooth movement with no discomfort, head laterally flexes, head laterally rotates and hyperextends. With equal strength Non-palpable, non tender Not visible on inspection, glands ascend but not visible in female during swallowing and visible in males. Chest symmetrical Spine vertically aligned, spinal column is straight, left and right shoulders and hips are at the same height. With normal breath sounds without dyspnea. Quiet, rhythmic and effortless respiration Unblemished skin, uniform in color, symmetric contour, not distended. Symmetrical movements cause by respirations. With audible sounds of 23 bowel sounds/minute. Without scars and lesions on both extremities. With minimal scars on lower extremities Assessment Muscles Bones and Joints Mental Status Language Orientation Attention span Level of Consciousness Findings Equal in size both sides of the body, smooth coordinated movements, 100% of normal full movement against gravity and full resistance. No deformities or swelling, joints move smoothly. Can express oneself by speech or sign. Oriented to a person, place, date or time. Able to concentrate as evidence by answering the questions appropriately. A total of 15 points indicative of complete orientation and alertness. Motor Function Gross Motor and Balance Walking gait Standing on one foot with eyes closed Heel toe walking Toe or heel walking Fine motor test for Upper Extremities Finger to nose test Alternating supination and pronation of hands on knees Finger to nose and to the nurse’s finger Fingers to fingers Fingers to thumb Has upright posture and steady gait with opposing arm swing unaided and maintaining balance. Maintained stance for at least five (5) seconds. Maintains a heel toe walking along a straight line Able to walk several steps in toes/heels. Repeatedly and rhythmically touches the nose. Can alternately supinate and pronate hands at rapid pace. Perform with coordinating and rapidity. Perform with accuracy and rapidity. Rapidly touches each finger to thumb with each hand. Fine motor test for the Lower Extremities Pain sensation Able to discriminate between sharp and dull sensation when touched with needle and cotton. Intravenous solutions are used in fluid replacement therapy by changing the composition of the serum by adding fluids and electrolytes. Listed below is a table which may serve as your quick reference guide on the different intravenous solutions. Type Use Increases circulating plasma Special Considerations patients with heart volume when red Normal Saline (NS) 0.9% NaCl in Water Shock Fluid replacement Crystalloid Isotonic (308 mOsm) or hypernatremia, because NSS replaces extracellula in patients r fluid and can lead with diabetic Solution failure, edema, cells are adequate ketoacidosis Hyponatremia Blood transfusions Resuscitation Metabolic Alkalosis Hypercalcemia Water replacement Raises total fluid to fluid overload. 1/2 Normal Saline (1/2 NS) concentrations. in Water dextrose infusion Crystalloid cardiovascular Solution Hypotonic collapse or increase in intracranial pressure. Sodium and trauma, or burns. fluid, but is of less Gastric fluid loss value for from nasogastric replacement of NaCl suctioning or vomiting. Useful for daily maintenance of body chloride depletion (154 mOsm) Don’t use in patients with liver disease, Hypertonic dehydra tion Use cautiously; may cause normal saline solution and before Helpful for Na+ replacement DKA after initial 0.45% NaCl Replaces losses without altering fluid volume Do not use in deficit. Helpful for establishing renal function. Fluid replacement for clients who don’t need extra glucose (diabetics) Has similar electrolyte content with serum but doesn’t contain magnesium. Has potassium there fore don’t use to Lactated Ringer’s (LR) Replaces fluid and patients with renal buffers pH failure as it can Hypovolemia due cause hyperkalemia Normal to third-space saline shifting. disease because the Don’t use in liver with electrolyt Dehydration patient can’t es and buffer Burns metabolize lactate; a Isotonic (275 Lower GI tract fluid functional liver loss converts it to Acute blood loss bicarbonate; don’t mOsm) give if patient’s pH > 75. Normal saline with K+, Ca++, and lactate (buffer) Often seen with surgery D5W Dextrose 5% Raises total fluid Solution is isotonic volume. initially and becomes Helpful in hypotonic when Crystalloid rehydrating and dextrose is solution excretory purposes. metabolized. in water Isotonic (in the bag) *Physiologica Fluid loss Not to be used for and dehydration resuscitation; can Hypernatremia cause hyperglycemi lly hypotonic a (260 mOsm) Use in caution to patients with renal or cardiac disease, can cause fluid overload Doesn’t provide enough daily calories for prolonged use; may cause eventual breakdown of protein. Provides 170-200 calories/1,000cc for energy. Physiologically hypotonic -the dextrose is metabolized quickly so that only water remains – a hypotonic fluid Hypotonic dehydrat ion D5NS Do not use in Replaces patients with cardiac Dextrose 5% fluid sodium, or renal failure in 0.9% chloride, and because of danger saline calories. of heart failure and Temporary pulmonary edema. Hypertonic (560 mOsm) treatment of circulatory insufficiency and Watch for fluid volume overload shock if plasma expanders aren’t available SIADH (or use 3% sodium chloride ). Addisonian crisis DKA after initial treatment with normal saline D5 1/2 NS when glucose falls < solution and halfDextrose 5% normal saline in 0.45% solution – saline prevents hypoglyce Hypertonic mia and cerebral (406 mOsm) edema (occurs In DKA, use only 250 mg/dl Most common postoperative fluid Useful for daily maintenance of body fluids and nutrition, when serum and for rehydration. osmolality is reduced rapidly). Contraindicated in newborns (≤ 28 days of age), even if Same as LR plus separate infusion provides about 180 D5LR lines are used (risk calories per Dextrose 5% in Lactated of fatal ceftriaxone- 1000cc’s. calcium salt Indicated as a Ringer’s source of Hypertonic water, electrolytes (575 mOsm) and calories or as an alkalinizing precipitation in the neonate’s bloodstream). Contraindicated in patients with a agent known hypersensitivity to sodium lactate. Normosol-R Replaces fluid and Not intended to Normosol Isotonic (295 mOsm) buffers pH supplant transfusion Indicated for of whole blood or replacement of packed red cells in acute extracellular the presence of fluid volume losses uncontrolled in surgery, hemorrhage or trauma, burns or severe reductions of shock. red cell volume Used as an adjunct to restore a decrease in circulatory volume in patients with moderate blood loss Common Positions Fowler’s Fowler’s position, is a bed position wherein the head and trunk are raised 40 to 90 degrees. Fowler’s position is used for people who have difficulty breathing because in this position, gravity pulls the diaphragm downward allowing greater chest and lung expansion. In low Fowler’s or semi-Fowler’s position, the head and trunk are raised to 15 to 45 degrees; in high Fowler’s, the head and trunk are raised 90 degrees. This position is useful for patients who have cardiac, respiratory, or neurological problems and is often optimal for patients who have nasogastric tube in place. Using a footboard is recommended to keep the patient’s feet in proper alignment and to help prevent foot drop. Orthopneic or Tripod Orthopneic or tripod position places the patients in a sitting position or on the side of the bed with an overbed table in front to lean on and several pillows on the table to rest on. Patients who are having difficulty breathing are often placed in this position since it allows maximum expansion of the chest. Dorsal Recumbent In dorsal recumbent or back-lying position, the client’s head and shoulders are slightly elevated on a small pillow. This position provides comfort and facilitates healing following certain surgeries and anesthetics. Supine or Dorsal position Supine is a back-lying position similar to dorsal recumbent but the head and shoulders are not elevated. Just like dorsal recumbent, supine position provides comfort in general for patients recover after some types of surgery. Prone In prone position, the patient lies on the abdomen with head turned to one side; the hips are not flexed. This is the only bed position that allows full extension of the hip and knee joints. Prone position also promotes drainage from the mouth and useful for clients who are unconscious or those recover from surgery of the mouth or throat. Prone position should only be used when the client’s back is correctly aligned, and only for people with no evidence of spinal abnormalities. To support a patient lying in prone, place a pillow under the head and a small pillow or a towel roll under the abdomen. Lateral position In lateral or side-lying position, the patient lies on one side of the body with the top leg in front of the bottom leg and the hip and knee flexed. Flexing the top hip and knee and placing this leg in front of the body creates a wider, triangular base of support and achieves greater stability. The greater the flexion of the top hip and knee, the greater the stability and balance in this position. This flexion reduces lordosis and promotes good back alignment. Lateral position helps relieve pressure on the sacrum and heels in people who sit for much of the day or confined to bed rest in Fowler’s or dorsal recumbent. In this position, most of the body weight is distributed to the lateral aspect of the lower scapula, the lateral aspect of the ilium, and the greater trochanter of the femur. Sims’ Position Sims’ is a semi-prone position where the patient assumes a posture halfway between the lateral and prone positions. The lower arm is positioned behind the client, and the upper arm is flexed at the shoulder and the elbow. Both legs are flexed in front of the client. The upper leg is more acutely flexed at both the hip and the knee, than is the lower one. Sims’ may be used for unconscious clients because it facilitates drainage from the mouth and prevents aspiration of fluids. It is also used for paralyzed clients because it reduces pressure over the sacrum and greater trochanter of the hip. It is often used for clients receiving enemas and occasionally for clients undergoing examinations or treatments of the perineal area. Pregnant women may find the Sims position comfortable for sleeping. Support proper body alignment in Sims’s position by placing a pillow underneath the patient’s head and under the upper arm to prevent internal rotation. Place another pillow between legs. Trendelenburg’s Trendelenburg’s position involves lowering the head of the bed and raising the foot of the bed of the patient. Patient’s who have hypotension can benefit from this position because it promotes venous return. Reverse Trendelenburg Reverse Trendelenburg is the opposite of Trendelenburg’s position. Here the HOB is elevated with the foot of bed down. This is often a position of choice for patients with gastrointestinal problems as it can help minimize esophageal reflux. Cheat Sheet for Patient Positions Below is the cheat sheet for the common patient positioning. You can also download the PDF file: Patient Positioning Cheat Sheet (PDF, 142 KB) Condition Bronchoscopy Position After: Semi-Fowler’s Rationale & Additional Info To reduce aspiration risk from difficulty of swallowing During: Flat on bed with arms at sides; kept still. Cerebral angiography After: Extremity in which contrast was injected is kept straight for 6 to 8 hours. Flat, if femoral artery was used. Apply firm pressure on site for 15 minutes after the procedure. Condition Position Rationale & Additional Info Pre-op: surgical table will be moved to various positions during test. Myelogram (air contrast) Post-op: HOB is lower than To disperse dye. trunk. Myelogram (oil-based dye) Pre-op: surgical table will be moved to various positions during test. Post-op: Flat on bed for 6 to To disperse dye.To prevent CSF leakage. 8 hours Myelogram (water-based dye) Pre-op: surgical table will be moved to various positions during test. Post-op: HOB elevated for 8 To prevent dye from irritating the meninges. hours. Liver biopsy During: Supine with RIGHT side of upper abdomen exposed; RIGHT arm raised and extended behind and and overhead and shoulder. After: RIGHT side-lying with To expose the area. To apply pressure and minimize bleeding. pillow under puncture site. Lung biopsy Renal biopsy Flat supine with arms raised above head and hands health together; head and arms on pillow. PRONE with pillow under the abdomen and shoulders. To expose and provide easy access to the area. To expose the area. Don’t sleep on affected side; encourage exercise by squeezing a rubber ball. Arteriovenous fistula Post-op: Elevate extremity Don’t use AV arm for BP reading and venipuncture. Peritoneal Dialysis When outflow is Turning facilitates drainage; Condition Position inadequate: turn patient from side to side. Rationale & Additional Info check for kinks in the tubing. Possible to have abdominal cramps and blood-tinged outflow if catheter was placed in the last 1-2 weeks. Cloudy outflow is never normal. Meniere’s Disease Autografting Internal radiation, during treatment Change position slowly; bedrest during acute phase Immobilize site for 3 to 7 days. Provide protection when ambulating To promote healing and maximal adhesion. To prevent dislodgement of the implant device. Strict bedrest while implant is in place Provide own urinal or bedpan Heart failure with pulmonary edema Sitting up, with legs dangling Myocardial infarction Semi-Fowler’s Pericarditis High-Fowlers, upright leaning forward. Depending on desired outcome. to patient. To decrease venous return and reduce congestion; promotes ventilation and relieves dyspnea. To help lessen chest pain and promote respiration. To help lessen pain. Slight elevation of legs but not above the heart or slightly Peripheral artery disease dependent. To slow or increase arterial return Dangle legs on side of the bed. Shock Flat on bed. To improve or increase circulation. Condition Position Rationale & Additional Info Trendelenburg is no longer a recommended position. Sickle Cell Anemia HOB elevated 30 degrees, avoid knee gatch and putting strain on painful joints Varicose veins, leg ulcers, and venous insufficiency Elevate extremities above heart level. To promote maximum lung expansion and assist in breathing. To prevent pooling of blood in the legs and facilitate venous return; avoid prolonged standing. Bed rest with affected limb elevated. After 24 hours after heparin Deep vein thrombosis therapy, patient can To promote circulation. ambulate if pain level permits. Tracheoesophageal fistula (TEF) Ventriculoperitoneal shunt (for Hydrocephalus treatment) HOB elevated 30-45 degrees. After shunt placement: Place on non-operative side in flat position. To prevent reflux. HOB raised 15-30 degrees if ICP is increased. Avoid rapid fluid drainage. Do not hold infant with head elevated. HyphemaBlood in anterior chamber of eye Abdominal aneurysm Dehiscence Dumping Syndrome, HOB elevated 30-45 degrees, with night shield. Post-op: HOB no more than 45 degrees Place in low-Fowler’s position then raise knees or instruct knees and support them with a pillow. Take meals in reclining To allow the hyphema to settle out inferiorly and avoid obstruction of vision and to facilitate resolution To avoid flexion of the graft. To decrease tension on the abdomen. To delay gastric emptying time. Condition prevention of Position position, lie down for 20-30 minutes after. Rationale & Additional Info Restrict fluids during meals, low carb, low fiber diet in small frequent meals. Evisceration Place in low-Fowler’s position. Instruct not to cough; place on NPO; keep intestines moist and covered with sterile saline until patient can be wheeled to OR. Reverse Trendelenburg, slanted bed with head higher. Gastroesophageal reflux disease (GERD) Pediatric: prone with HOB Hiatal hernia Upright position after meals. Pyloric stenosis RIGHT side-lying position after meals. Extremity burns Elevate extremity. Facial burns or trauma Head elevated Initially place in sitting position or high Fowler’s position with legs dangling. HOB elevated 30-45 degrees; bed rest Autonomic dysreflexia Cerebral aneurysm elevated. To promote gastric emptying and reduce reflux. To prevent gastric content reflux. To facilitate entry of stomach contents into the intestines. To reduce dependent edema and pressure. To reduce edema To reduce blood pressures below dangerous levels and provide partial symptom relief. To prevent pressure on aneurysm site To promote venous return and maintain blood flow to the head. To reduce ICP and encourage blood drainage.Avoid hip and neck flexion which inhibits drainage. To promote venous drainage. Heat stroke Supine, flat with legs elevated. Hemorrhagic stroke HOB elevated 30 degrees. Elevate HOB 30-45 degrees, maintain head midline and in neutral position. Avoid flexion of the neck, head Increased intracranial pressure (ICP) HOB flat in midline, neutral To facilitate venous drainage Ischemic stroke rotation, hip flexion, coughing, sneezing and bending forward. Condition Position position. Rationale & Additional Info and encourage arterial blood flow. Avoid hip and neck flexion which inhibits drainage Seizure Spinal cord injury Side-lying or recovery position. Immobilize on spinal backboard, head in neutral position and immobilized with a firm, padded cervical collar. Must be log rolled without To drain secretions and prevent aspiration. To prevent any movement and further injury. allowing any twisting or bending movements Head injury Buck’s Traction Casted arm Delayed prosthesis fitting Hip fracture Elevate HOB 30 degrees, head should be kept in neutral position. Elevate FOB for countertraction; use trapeze for moving; place pillow beneath lower legs. Elevate at or above level of heart Elevate foot of bed to elevate residual limb. Affected extremity needs to be abducted. To decrease intracranial pressure (ICP).Keep head from flexing or rotating. Avoid frequent suctioning. Ask patient to dorsiflex foot of the affected leg to assess function of peroneal nerve, weakness may indicate pressure on the nerve. To minimize swelling To hasten venous return and prevent edema. Use splints, wedge pillow, or pillows between legs. Avoid stooping, flexion position during sex, and overexertion during walking or exercise. Hip replacement On unaffected side: maintain abduction when in supine position with pillow between legs. Avoid extreme internal or external rotation. Condition Position Rationale & Additional Info HOB raised to 30-45 degrees. Immediate prosthesis fitting Elevate residual limb for 24 hours. Osteomyelitis Support affected extremity with pillows or splints Total hip replacement Help to sitting position; place chair at 90 degrees angle to bed; stand on affected side; pivot patient to unaffected side. To prevent dizziness and orthostatic hypotension. Acute Respiratory Distress Syndrome (ARDS) High Fowler’s To promote oxygenation via maximum chest expansion. Turn to LEFT side or place in Trendelenburg. Patient should be immediately repositioned with the right atrium above the gas entry site so that trapped air will not move into the pulmonary circulation. Air embolism from dislodged central venous line Rigid cast acts to control swelling. To maintain proper body alignment; avoid strenuous exercises. High Fowler’s Tripod position: sitting Asthma position while leaning forward To promote oxygenation via maximum chest expansion. with hands on knees. Chronic Obstructive Pulmonary Disease (COPD) High Fowler’s Orthopneic position To promote maximum lung expansion and assist in breathing. High Fowler’s Emphysema Orthopneic position Pleural Effusion High Fowler’s High Fowler’s Pneumonia Lay on affected side To promote maximum lung expansion To provide maximal To maximize breathing mechanisms. To splint and reduce pain. Condition Position Lay with affected lung up Pneumothorax Pulmonary edema Pulmonary embolism High Fowler’s High Fowler’s, legs dependent position High Fowler’s Turn patient to LEFT side and lower HOB Flail chest High Fowler’s Rib fracture High Fowler’s Contraction stress test (CST) Placed in semi-Fowler’s or side-lying position Cord prolapse Shrimp or fetal position; modified Sims’ or Trendelenburg. Late decelerations (placental insufficiency) Placenta previa Turn mother to her LEFT side. Turn mother to her LEFT side. Sitting position. Variable decelerations (cord compression) Place mother in Trendelenburg position. Spina Bifida Prone (on abdomen). Position on back or in infant seat. Cleft lip (congenital) Hold in upright position while Fetal distress feeding. Prolapsed umbilical cord During labor: Knee-chest Rationale & Additional Info To reduce congestion. To promote maximum lung expansion and assist in breathing. To decrease edema and congestion To promote maximum lung expansion and assist in breathing. To provide maximal comfort and maximize breathing mechanisms. To promote maximum lung expansion and assist in breathing. Monitor for posttest labor onset. To prevent pressure on the cord. If cord prolapses, cover with sterile saline gauze to prevent drying. To reduce compression of the vena cava and aorta. To allow more blood flow to the placenta. To minimize bleeding. To remove pressure off the presenting part of the cord and prevent gravity from pulling the fetus out of the body. To prevent sac rupture. To prevent trauma to suture line. Relieves pressure or gravity Condition Position position or Trendelenburg. Rationale & Additional Info from pulling the cord. Hand in vagina to hold presenting part of fetus off cord. Cardiac catheterization (post) Continuous Bladder Irrigation (CBI) Ear drops Ear irrigation HOB elevated no more than 30 degrees or flat as prescribed.May turn to either side Tape catheter to thigh; no other positioning restrictions Position affected ear uppermost then lie on unaffected ear for absorption. During procedure: Tilt head towards affected ear. After procedure: Lie on affected side for drainage. Eye drops Lumbar puncture Tilt head back and look up, pull lid down. During: Shrimp or fetal position (side-lying with back bowed, knees drawn up to abdomen, neck flexed to rest chin on chest). After: Flat on bed for 4-12 hours. Nasogastric tube insertion High Fowler’s with head tilted forward Nasogastric tube irrigation and tube feedings HOB elevated 30 to 45 degrees; keep elevated for 1 hour after an intermittent feeding. With decreased Affected extremity should be kept straight. Prevents the catheter from being dislodged. Pull outer ear upward and back for adults; upward and down for children. Better visualization and drainage of the medium to the ear canal via gravity. Drop to center of the lower conjunctival sac; blink between drops; press inner canthus near nose bridge for 1-2 min to prevent systemic absorption. To maximize spine flexion. To prevent spinal headache and CSF leakage. Closes the trachea and opens the esophagus; prevents aspiration. To prevent aspiration.Promotes emptying of the stomach and prevents aspiration. Condition Position LOC: RIGHT side-lying with Rationale & Additional Info To prevent aspiration. HOB elevated. With tracheostomy: Maintain in semi-Fowler’s position Paracentesis During: Semi-Fowler’s in bed or sitting upright on side of bed with chair; support the feet. Post: Assist into any comfortable position Postural Drainage Trendelenburg Rectal enema administration Left side-lying (Sims’ position) with right knee flexed. Rectal enemas and irrigation Left side-lying, Sims’ position Sengstaken-Blakemore and Minnesota tubes HOB elevated Empty the bladder before procedure; report elevated temperature; assess for hypovolemia. Lung area needing drainage should be in uppermost position Allows gravity to work into the direction of the colon by placing the descending colon at its lowest point. To allow fluid to flow in the natural direction of the colon. To enhance lung expansion and reduce portal blood flow, permitting esophagogastric balloon tamponade. Before: (1) Sitting on edge of bed while leaning on bedside table with feet supported by stool; or lying in bed on unaffected side with head elevated 45 degrees. Thoracentesis (2) Lying in bed on unaffected side with HOB elevated to Fowler’s. After: Assist patient into any comfortable position Prevent fluid leakage into the thoracic cavity. Condition Position Rationale & Additional Info preferred. Total Parenteral Nutrition (TPN) Vascular extremity graft During insertion: Trendelenburg. Bed rest for 24 hours, keep extremity straight and avoid knee or hip flexion Perineal procedures Lithotomy Appendectomy Post-op: Fowler’s position To prevent air embolism. For maximal adhesion. For better visualization of the area. To relieve abdominal pain and ease breathing. Sleep on unaffected side with a night shield for 1 to 4 weeks. Cataract surgery Semi-Fowler’s or Fowler’s on To prevent edema. back or on non-operative side. HOB elevated 30-45% with head in a midline, neutral position. Craniotomy Never put client on operative To facilitate venous drainage. side, especially if bone was removed. Hemorrhoidectomy Hypophysectomy Surgical removal of the pituitary gland. Infratentorial surgery Incision at back of head, above nape of neck Kidney transplant Laminectomy During: Prone Jackknife position. Provides better visualization of the area. HOB elevated. To prevent increase in ICP. Flat and lateral on either side; avoid neck flexing. To facilitate drainage. Post-op: Semi-Fowler’s, turn from back to non-operative side Back is kept straight.Patient is logrolled if turned. Sit straight in straight-backed To promote gas exchange Condition Position Rationale & Additional Info chair when out of bed or when ambulating. Laryngectomy HOB elevated 30-45 degrees Mastectomy Semi-Fowler’s with arm on affected side elevated. Myringotomy Post-op: semi-Fowler’s position. Post-op: Position on side of affected ear . Bed rest with minimal activity and repositioning. Retinal detachment Area of detachment should Mitral valve replacement be in the dependent position. Supratentorial surgery Incision front of head below hairline Thyroidectomy Tonsillectomy HOB elevated 30-45 degrees; maintain head/neckline in midline neutral position; avoid extreme hip and neck flexion. Post-op: High Fowler’s or semi-Fowler’s. Amputation: above the Turn only on back and on unaffected side. To assist in breathing. To allow drainage of secretions Helps detached retina fall into place. To facilitate drainage. To reduce swelling and edema in the neck area. Avoid extension and To decrease tension on the movement by using suture line and support the sandbags or pillows. head and neck. Post-op: prone or side-lying Side lying with head tucked and legs pulled up or; Bone marrow aspiration/biopsy To maintain airway and decrease edema. To allow lymph drainage. To facilitate drainage and relieve pressure on the neck. To expose the area. Apply pressure to the area Prone with arms folded under after the procedure to stop chin. the bleeding. Elevate for first 24 hours To prevent edema. Condition knee Position using pillow.Position prone twice daily. Rationale & Additional Info To provide for hip extension and stretching of flexor muscles; prevent contractures, abduction Amputation: below the knee Foot of bed elevated for first 24 hours. Position prone daily. To prevent edema. To provide for hip extension.