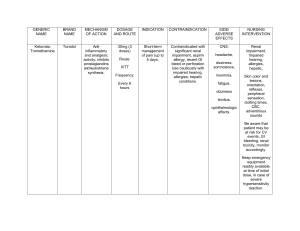
Kidney International, Vol. 54 (1998), pp. 313–327 PERSPECTIVES IN RENAL MEDICINE The clinical spectrum of tubulointerstitial nephritis ASGHAR RASTEGAR and MICHAEL KASHGARIAN Department of Internal Medicine and Department of Pathology, Yale University School of Medicine, New Haven, Connecticut, USA Tubules and interstitium make up approximately 80% of the renal volume, and occupy the compartment referred to as the tubulointerstitium. The interstitium space takes up 13% of rat and up to 17% of dog and rabbit kidneys, including 7 to 9% of renal cortex, 3 to 5% of outer medulla and 30 to 40% of inner medulla and papillary tip [1, 2]. It is made up of both cellular and matrix components. There are two main cell types. (a) Type I interstitial cells are fibroblast-like cells capable of producing and degrading extracellular matrix. The lipid-rich interstitial cells in the inner medulla, a possible source of prostaglandins, are also considered to be a form of type I interstitial cells. (b) Type II interstitial cells, found in all renal zones, include monocyte derived macrophages with capacity for phagocytosis and dendritic antigen-presenting cells found primarily in the cortex. The matrix is made up of a fibrillar net of interstitial and basement membrane collagens and associated proteoglycans, glycoproteins, and interstitial fluid. The interstitial compartment not only provides structural support for the individual nephrons, but also serves as a conduit for solute transport [2]. It is also the site of production of several hormones and cytokines such as erythropoietin and prostaglandins. Renal diseases can broadly be classified as glomerular, vascular, tubulointerstitial or obstructive in origin. Diseases of tubulointerstitial compartment may be the result of primary injury to this compartment or secondary to injury to other compartments. Several studies in patients with a variety of renal diseases have shown that changes in the tubulointerstitial compartment are a better predictor of the severity of renal dysfunction and long-term outcome than changes in other compartments [3–7]. Recent advances in our understanding of the process of injury and repair in general, and tubulointerstitial compartment in particular, Key words: end-stage renal disease, analgesic-induced tubulointerstitial nephritis, urinary tract obstruction, hyperuricemia, nephrocalcinosis, lead nephropathy, sarcoid nephropathy, acute drug-induced tubulointerstitial nephritis. Received for publication September 15, 1997 and in revised form December 30, 1997 Accepted for publication January 1, 1998 © 1998 by the International Society of Nephrology have helped elucidate some of the important pathogenic events leading to tubulointerstitial nephritis (TIN). These advances have been summarized in several excellent reviews [8 –12] and will only be discussed briefly here. This review focuses primarily on clinical aspect of the diseases where the tubulointerstitial compartment is the primary target of the pathogenic process rather than being secondarily involved by damage to the glomerular, vascular compartment or collecting system. The term acute interstitial nephritis was first used a century ago in 1898 by Councilman in describing a group of patients with systemic bacterial infection, primarily scarlet fever and diphtheria. This term was applied to acute inflammation of the kidney characterized by cellular and fluid exudation in the interstitial tissue that was not dependent on the presence of bacteria [13]. For many decades, the term chronic pyelonephritis was used to describe renal diseases associated with chronic injury to interstitum, despite the lack of evidence for the presence of active infection in a majority of the patients. Beginning in early 1950s, the work of Spuhler and Zollinger in Switzerland on the role of analgesics [14, 15], and Henderson and colleagues in Australia on the role of lead in the development of chronic tubulointerstitial nephritis (TIN) [16], provided strong evidence that the so-called chronic pyelonephrits was often not infectious in origin. It is now recognized that TIN represents a group of diseases that are due to a variety of etiologies and pathogenic mechanisms. Given the tight structure-function relationship between glomerular, vascular and tubulointerstitial compartments, a significant overlap exists between the clinical presentation of the diseases initiated in any compartment. In addition, the clinical presentation of TIN depends both on its etiology and the severity of renal dysfunction. Despite this factor, certain findings are more common in these patients than patients with glomerular disease. These include: (1) a lack of significant proteinuria and hypoalbuminemia; (2) the presence of sterile pyuria and white blood cell (WBC) casts rather than hematuria and red blood cell (RBC) casts; (3) the presence of a concentrating defect resulting in polyuria and nocturia; and (4) the presence of other tubular defects such as renal tubular acidosis, salt losing nephropathy and osteomalacia due to long-standing vitamin D 313 314 Rastegar and Kashgarian: Tubulointerstitial nephritis deficiency. These differences become increasingly blurred with progression of renal failure. TUBULOINTERSTITIAL NEPHRITIS Epidemiology of tubulointerstitial nephritis TIN is an important cause of renal failure and end-stage renal disease (ESRD). The incidence of primary TIN varies by geographical area, entry criteria, and mode of diagnosis [17–22]. While renal biopsy remains the gold standard, nephrologists are less likely to biopsy patients with clinical signs and symptoms of TIN than patients with glomerular disease. Therefore, the diagnosis of TIN is often based on epidemiological, clinical and laboratory evaluations rather than renal biopsy. In an autopsy series the incidence of TIN was reported at 1.7% for acute and 0.2% for chronic TIN [23]. In a Finnish study of 314,000 asymptomatic recruits, 174 with hematuria and/or proteinuria were biopsied. Two patients had TIN for a prevalence of 0.7 per 100,000 in this population [24]. Murray and Goldberg reported an incidence of 33% among 320 patients admitted to a teaching hospital over a three year period (1969 to 1972) with a diagnosis of CRF and serum creatinine of greater than 1.3 mg% [17]. The most common causes of TIN were urinary tract obstruction, analgesic abuse, hyperuricemia and nephrocalcinosis. In a similar study from a teaching hospital in North Carolina, TIN was also the most common cause of CRF, accounting for 40.8% of the cases. The most common etiologic diagnosis was analgesic-induced TIN (AITIN), considered as definitive in 26.8% and probable in 14.6% of patients with TIN [25]. In both studies the diagnosis of TIN was primarily based on clinicopathological findings and less commonly on renal biopsy. The incidence of TIN among ESRD patients varies from 42.2% in Scotland [26], 29% in Berlin [20], and 27.5% in Delaware County, Pennsylvania [18] to 25.7% in North Carolina, USA [25]. Rostand et al, in a study from Alabama focusing on racial differences in ESRD, calculated an annual incidence per 100,000 population of 2 for TIN, 2.3 for nephrosclerosis, 1.2 glomerulonephritis and 0.8 for diabetes nephropathy [27]. In a renal biopsy study of 109 patients with unexplained renal failure (GFR , 60 ml/min) and normal size kidney, TIN was the most common diagnosis, and was seen in 29 (27%) of patients [28]. The 1996 United States ESRD Registry Data, however, shows an incidence of only 3% among all patients on dialysis [22]. If obstructive disease and TIN associated with malignancy is also included, the incidence approaches 7.5%, still significantly lower than the above quoted numbers. This difference may be due to several factors including lack of diagnostic precision, the recent increase in the number of patients with diabetes and other systemic diseases on dialysis, and successful prevention and earlier treatment of tubulointerstitial nephritis. Part of the difference is geo- Table 1. WHO classification of tubulointerstitial diseaes Infection Acute infectious tubulointerstitial nephritis Acute tubulointerstitial nephritis associated with systemic infection Chronic infectious Tubulointerstitial nephritis (chronic pyelonephritis) Specific renal infection Drug-induced tubulointerstitial nephritis Acute drug-induced tubulotoxic injury Drug-induced hypersensitivity tubulointerstitial nephritis Chonic drug-induced tubulointerstitial nephritis Tubulointerstitial nephritis associated with immune disorders Induced by antibodies reacting with tubular antigens Induced by autologous or exogenous antigen-antibody complexes Induced by, or associated with, cell-mediated hypersensitivity Induced by immediate (IgE-type) hypersensitvity Obstructive uropathy Vesicoureteral reflux associated nephropathy (reflux nephropathy) Tubulointerstitial nephritis associated with papillary necrosis Heavy metal-induced tubular and tubulointerstitial lesions Acute tubular injury/necrosis Toxic Ischemic Tubular and tubulointerstitial nephropathy caused by metabolic disturbances Hereditary renal tubulointerstitial disorders Tubulointerstitial nephritis associated with neoplastic disorders Tubulointerstitial lesions in glomerular and vascular diseases Miscellaneous disorders Balkan endemic nephropathy graphic in nature, reflecting the role of environmental factors in the development of TIN. Classification of tubulointerstitial nephritis There is no universally acceptable classification of TIN. The most comprehensive is the WHO classification, which uses a pathogenic and when possible an etiologic approach to these diseases (Table 1) [29]. From a practical point of view, we prefer a simpler classification initially dividing TIN into primary and secondary forms, independent of acuity or chronicity of the disease (Table 2). Primary TIN is comprised of diseases where the dominant pathogenic process begins in the tubulointerstitial compartment, only secondarily affecting other compartments. Secondary TIN encompasses diseases where the primary pathogenic process begins in vascular, glomerular or collecting system, followed by damage to the tubulointerstitial compartment. This classification is by no mean all encompassing, and does not recognize diseases that affect more than one compartment simultaneously such as systemic vasculitis, systemic lupus erythematosus (SLE), or human immunodeficiency virus (HIV) associated nephropathy. Pathology of tubulointersitital nephritis Although the tubulointerstitum can only respond in a limited manner to a variety of insults, the pattern of response can help define the acuity of the process, the long-term prognosis and in some patients the pathogenesis and/or etiology of the disorder. The initial division of the Rastegar and Kashgarian: Tubulointerstitial nephritis Table 2. Classification of tubulointerstitial nephritis (TIN) I. Primary TIN 1. Infection (bacterial pyelonephritis, Hantavirus, Leptospirosis) 2. Immune-mediated (Sjögren syndrome, anti-tubular basement membrane disease) 3. Drug-induced (AIN, analgesics-induced IN, lithium, cyclosporine, Chinese herbs) 4. Toxins (lead) 5. Metabolic disorders (gouty nephropathy, hypercalcemic IN, hypokalemoic) 5. Hereditary TIN (Wilson disease, cystinosis, hyperoxaluria) 6. Hematologic disorders (sickle cell disease, Light chain nephropathy, cast nephropathy, light chain deposit diseases, amyloidosis) 7. Miscellaneous (Balkan nephropathy) II. Secondary TIN 1. Glomerular disease 2. Vascular disease 3. Structural disease a. Cystic diseases b. Obstructive disease c. Reflux histologic pattern of TIN is dependent on the presence or absence of a significant inflammatory infiltrate in the interstitium. In diseases where the infiltrate is predominant, the characteristics of the cellular components of the infiltrate further assist in the differentiating types of TIN with differing pathogenesis. The structural changes of tubular injury include cytopathic changes from sublethal injury to necrosis, alteration in growth including atrophy, hypertrophy and simplification and the accumulation of cast material in the tubular lumina. Interstitial changes include edema, leukocytic infiltration and fibrosis. In predominantly non-inflammatory lesions, the nature of the tubular epithelial changes and the presence of renal tubular pigments, cast material, crystals or other inclusions assist in making these differentiations. Using histological criteria, one can classify tubulointerstitial disease in such a manner as to recognize the wide variety of potential etiologic agents and different pathogenic mechanisms that produce similar or identical morphologic patterns. In acute or active forms of interstitial nephritis the interstitium is edematous and there is a cellular infiltrate that may contain lymphocytes, plasma cells or polymorphonuclear leukocytes, including eosinophils. Invasion of the tubules may be seen to resemble the tubulitis of allograft rejection. In more chronic forms, interstitial fibrosis and tubular atrophy is the most prominent feature that may be accompanied by an infiltrate comprised only of small lymphocytes. Marcussen recently has brought attention to a sequence of events where tubulitis eventually leads to tubular destruction and the development of atubular glomeruli. This process contributes both to the histologic picture and the progressive loss of function seen in chronic interstitial nephritis [30]. Pathogenesis of tubulointerstitial nephritis The mechanisms by which various etiologic agents can mediate renal tubulointerstitial injury can either be direct 315 through cytotoxicity or indirect by the induction of systemic inflammatory or immunologic reactions. Direct cytotoxic mechanisms are dose and exposure duration dependent, such as what is seen in analgesic and lead nephropathy. Indirect reactions are often idiosyncratic as occurs in the acute interstitial nephritis associated with nonsteroidal anti-inflamatory agents (NSAIDs). The nature of the injury may be determined to some extent by factors unrelated to the agent such as preexisting renal disease, or extrarenal factors that can affect renal dosage such as abnormal liver function. In addition, the differences in susceptibility of different nephron segments can modify the renal response to these agents, such as with heavy metal exposure. Studies in experimental models and in human disease provide compelling evidence for immune mechanisms of tubulointerstitial disease, and these have been reviewed extensively [9, 31]. These mechanisms are in some instances analogous to immune-mediated glomerular disease involving antibasement membrane antibodies or immune complex deposition. In other instances they are more specific to the structures of the tubulointerstitium and involve antibodies to cell surface antigens, or antigens processed and presented by tubular epithelial or interstitial dendritic cells to the immune system, resulting in cell mediated reactions. In addition, local activation of epithelial, endothelial and interstitial fibroblastic cells results in expression of a variety of cytokines and growth factors such as platelet-derived growth factor (PDGF) and transforming growth factor-B (TGF-B), which can contribute to inflamation and fibrogenesis in the tubulointerstitial compartment [10, 12, 32]. General approach to patients with tubulointerstitial nephritis Diagnosis of TIN should be considered in any patient with unexplained renal failure and/or specific tubular dysfunction. As drugs and toxins are major causes of primary TIN, a complete occupational history, history of drugs ingestion (including over the counter drugs as well as herbal medications) and toxin exposure should be sought. In patients with systemic signs and symptoms known systemic disease, the renal disorder should be considered in the context of a systemic illness. The clinical presentation of TIN reflects the nature of the underlying disease and severity of renal disorder. Although there are significant overlaps between the clinical presentation of glomerular and tubulointerstitial diseases, several features may help differentiate between these two entities. Patients with TIN tend to have less severe systemic hypertension and edema and a slower rate of progression [5, 33]. The initial presentation may be dominated by clinical expression of the tubular defects such as polyuria, nocturia, or abnormal biochemical parameters such as metabolic acidosis and glycosuria [33]. Urinalysis may provide strong evidence for the presence of tubular disorder with low specific gravity, high pH, and presence of 316 Rastegar and Kashgarian: Tubulointerstitial nephritis glucose. Twenty-four-hour urine protein levels are rarely greater than 2.5 g and are commonly below 1.0 g [5]. Urinary sediment varies from bland to active with WBCs and WBC casts rather than RBC and RBC casts. To establish a specific diagnosis, further workup is necessary and should be guided by the clinical history and initial findings. This workup may include specialized imaging, serological, biochemical and toxicological studies and/or renal biopsy. The role of renal biopsy in the diagnosis of TIN has not been systematically examined. In certain circumistances the renal biopsy is carried out to exclude glomerular pathology. In selected patients with possible allergic or granulomatous interstitial nephritis and interstitial nephritis associated with plasma cell dyscrasias, it is often diagnostic. However, in many circumstances such as lithium or lead nephropathy the findings are nonspecific. In summary, the workup of patients suspected of TIN should be guided heavily by the clinical and occupational histories, epidemiology of known diseases, as well as clues offered by the initial workup. The WHO classification (Table 1) and our proposed classification (Table 2) show that the list of disease categories under TIN is very long. This list includes disorders associated with infection, drugs and toxins, metabolic, hematologic and hereditary disorders. To provide an indepth review of the spectrum of TIN, we have chosen to discuss four specific disorders that are either common, and therefore clinically important, and/or exemplify a unique type of injury to the tubulointerstitium. These diseases are analgesic-induced TIN, granulomatous interstitial nephritis of sarcoidosis, lead nephropathy, and drug-induced allergic interstitial nephritis. Due to the limitation of space, several other disorders such as lithium associated TIN, interstitial nephritis due to hematologic disorders, and the recently described interstitial nephritis due Chinese herbs are not included in this review. ANALGESIC-INDUCED TUBULOINTERSTITIAL NEPHRITIS Non-narcotic analgesics are among the most commonly used medications in the world. These drugs, primarily developed in the second half of the nineteenth century, became very popular as single or mixed agents for control of pain. They include salicylates such as aspirin, pyrazolones such as antipyrine, anilides such as phenacetin, and acetoaminophen. Spuhler and Zollinger in the early to mid 1950s reported that 13 of 44 patients in Switzerland with interstitial renal disease habitually consumed analgesics [14, 15]. Although the importance of analgesic ingestion as an etiologic factor was not initially clear, these and other reports published from several other countries raised serious questions about a potential association between the use of these medications and development of renal failure. This association is supported by both epidemiological and ex- perimental studies. In this review we will emphasize the epidemiological data linking analgesic use to TIN. Epidemiology of analgesic-induced tubulointerstitial nephritis The historical prevalence of analgesic-induced tubulointerstitial nephritis (AITIN) in different geographical areas varies widely from 0% in Queenscliff, Australia, 10 to 35% in Switzerland, 33 to 41% in Scandinavia and Wales, to 49% in Brisbane, Australia [34, 35]. The prevalence of AITIN in ESRD patients varies from 1.7% in Philadelphia [18], 10% in North Carolina [25] to 18% in Belgium [33, 36] and 30% in Queensland, Australia [37]. In addition to great variability among different countries and different regions of the same country, there is a significant female preponderance in all series, with a female-to-male ratio as high as 6:1 [34]. Papillary necrosis is a well known component of both clinical as well as experimental AITIN. Epidemiological data support this association with a close concordance in the incidence of papillary necrosis and AATIN. For example, the autopsy-based incidence of papillary necrosis is only 0.2% in the US compared to 21% in Sydney and Brisbane, Australia [32]. The marked variation in the incidence of AITIN and papillary necrosis is best explained by the overall consumption rate of analgesics, especially the combination type containing phenacetin, in a given community [35]. This causal relationship is strengthen by the effect of removal of phenacetin from formulary in many countries beginning in early 1960s [38]. Follow-up reports from Europe [39 – 41], Canada [42], and Australia [43] documented a decrease in the prevalence of AITIN in most, but not all, countries where analgesic mixtures often containing phenacetin were banned. The only prospective cohort study was carried out by Dubach, Rosner and Pfister, who followed 623 female workers with evidence of regular phenacetin use, and 621 age, parity, and in most cases, nationality, marital and work matched controls [44]. Cross sectional data showed that a history of renal disease, prevalence of proteinuria, and abnormal concentrating ability, but not elevated serum creatinine, was more frequent among consumers than nonconsumers. After removal of the subjects with initial renal abnormalities, other subjects were followed for 11 years and multiple indices of renal function and mortality was evaluated. The frequency of low urinary specific gravity and elevated serum creatinine was higher in phenacetin users than controls; (23.2% vs. 6.7% and 6.7% vs. 0.9%, respectively; P , 0.001). The relative risk (RR) for overall mortality was 2.7, for death from renal and urogenital disease 4.3, and for cardiovascular disease 4.5. However, the RR for death from cancer of 2.0 did not achieve significance [44]. In the past one and a half decades, six well designed, case-controlled studies have been published evaluating the Rastegar and Kashgarian: Tubulointerstitial nephritis Table 3. Analgesic use and renal disease, summary of case-control studies Author year/country McCredie 82/Austratia Murray ’83/USA Sandler ’89/USA Pommer ’89/Germany Morlans ’90/Spain Sandler ’91/USA Perneger ’94/USA Patient Controls N 129 223 533 1047 554 Analgesic outcome RR/OR Phen. PN 17 All ESRD 1.08 (NS) 516 AAP Phen. CRF 3.21 5.11 574 517 All ESRD 2.44 340 673 Phen. ASA ESRD 19 2.54 544 516 All CRF 716 361 AAP NSAID ESRD 2.1 2–2.4 8.8 Abbreviations are: RR, risk ratio; OR, odds ratio; PN, papillary necrosis; AAP, acetaminophen; ASA, acetosalicylic acid; Phe, phenacetine containing. P value was significant unless indicated. (See text for references and detail). relationship between analgesics use and renal disease (Table 3). These data are not strictly comparable. The definition of regular or heavy use varies greatly and the amount of ingestion is determined by recall. The end point varies from papillary necrosis, TIN, renal failure, and most commonly ESRD. Control groups were drawn from hospitalized patients [18], a normal population [21, 45, 46], outpatient clinic patients [20], and both normal populations as well as patients with renal failure without papillary necrosis [43]. In addition, Sandler, Burr and Weinberg evaluated the role of NSAIDs and found that renal failure was seen mostly among the older men with heart failure [46]. This effect probably reflects the hemodynamic rather than structural effects of these drugs. Despite these differences, a comparison between these studies is helpful in understanding the role of analgesics not only in the development of AITIN but of renal failure. McCredie et al, in a case control study of 91 patients with definite and 38 patients with probable papillary necrosis with appropriate controls, reported a risk ratio of 17 for association between heavy analgesics use and papillary necrosis [43]. The RR for analgesics not containing phenacetin could not be calculated because of small numbers. Murray et al studied 527 patients from dialysis center in Delaware County and 1047 controls [18]. This study did not find any relationship between analgesics use and ESRD or TIN. In contrast, a similar study from Berlin [20] found a significant relationship between regular analgesic use and ESRD with a RR of 2.44 (1.77 to 3.39) for regular intake of any analgesics and 2.65 for the combination analgesics (the majority containing phenacetin or phenazones). Although 317 the authors indicate that regular analgesic use was reported most frequently in those with the diagnosis of AITIN (63 out of 577 patients), no specific RR is given for this group or the group with nonanalgesic associated TIN. The study by Sandler et al from North Carolina, where the use of analgesics was significantly higher than Delaware county, showed a RR of 1.71 for daily use of any analgesics and 6.06 for phenacetine containing analgesics [21]. This association was strongest for TIN, but present for other renal diseases including diabetic nephropathy as well as glomerulonephritis. Regular analgesic use was much more common in Australia [43, 47], Germany [20], and North Carolina [21] among both control and cases than Philadelphia. The average amount of analgesics consumed by patients in Australia with papillary necrosis was 25.3 kg, while the average in all ESRD patients from Germany was 3.643 kg. In study by Murray et al only 1.7% of cases and 1.9% of control groups had total intake above 3.0 kg [18]. Interestingly, the two control groups in the Australian study had average lifetime consumption of 13.7 and 7.2 kg, while in the German study’s control group it was 0.756 kg. This strongly supports the contention that the difference between the incidence in these four geographical areas reflects the overall incidence of regular analgesic (especially combination analgesics) use in these populations. The heaviest users develop the classical findings of AITIN with clinically diagnosable papillary necrosis and renal failure. It is possible that in areas with low to moderate consumption, the lesion is subclinical and primarily present as progressive renal failure in patients with or without known renal disease. The pathologic lesion in this group of patients is not defined and is presumed to be nonspecific interstitial damage. In addition, the heavy use of analgesics among controls in Australia and Berlin study indicates that either some individuals are resistant to the effect of analgesics or other factors are involved. The studies by Sandler et al [46], Perneger et al [45] and Morlan et al [48], while strengthening the association with combination drugs containing phenacetine, raise questions about the role of other analgesics including acetaminophen, NSAIDs and ASA. Perenger, Whelton and Klag estimated that acetaminophen could account for 8 to 10% of ESRD in the U.S. [45]. The odd ratio (OR) increased from 1.4 (P 5 NS) for those who took up to one pill per day to 2.1 (1.1 to 3.7) for those who took more than one pill per day. The OR for the subgroup who had ingested a cumulative dose of greater than 5,000 pills was 8.8 [42]. The findings in these reports are somewhat weakened by the fact that the data are prone to recall bias, use of telephone interviews as well lack of renal data in control patients. These data, while open to methodological criticism, raise important questions about the role of commonly used over the counter drugs in the general population and patients with underlying renal disease. Although phenacetine is 318 Rastegar and Kashgarian: Tubulointerstitial nephritis Fig. 1. (A) Low power view of the cortex of the kidney of a patient who died of renal failure secondary to analgesic induced tubulointerstitial nephritis. There is extensive interstitial scarring (represented by the green staining of collagen) and tubular atrophy with no significant cellular infiltrate. This cortical change was associated with medullary scars secondary to papillary necrosis (original magnification 350 Masson trichrome). (B) Low power view of a renal biopsy of a patient with renal sarcoidosis. The interstitium contains several confluent non caseating granulomata (arrowhead) and a nonspecific mononuclear infiltrate (original magnification 3100, hematoxylin and eosin stain). (C) High power view of the interstitial infiltrate of a renal biopsy of a patient with acute allergic interstitial nephritis secondary to ingestion of a nonsteroidal anti inflammatory drug. There is interstitial edema and a mixed cellular infiltrate which contains mononuclear cells, polymorhonuclear leukocytes and eosinophils (arrowheads). There is also evidence of tubulitis (tubule identified by T) with foci of individual tubular epithelial cell necrosis (original magnification 3300, hematoxylin and eosin stain). (D) Electron micrograph of the nucleus of a proximal tubular epithelial cell of a patient with lead nephropathy. There is an electron dense intranuclear inclusion (arrowhead) that probably represents a lead metallothionein complex. These inclusions are characteristic of lead toxicity but are not uniformly present in patients with lead nephropathy, especially in advanced disease (original magnification 313,600). usually considered to be the main culprit, the role of other analgesics cannot be ignored. Histopathology of analgesic-induced tubulointerstitial nephritis The earliest lesion described in analgesic nephropathy is capillary sclerosis of the urinary tract mucosa [49, 50]. A similar lesion consisting of peritubular capillary sclerosis is initially seen in the inner medulla and can be produced in experimental animals [51]. This will eventually leads to papillary necrosis followed by interstitial fibrosis. In the cortex there is extensive interstitial scarring that is usually bland with relatively few inflammatory cells, which if present are generally small lymphocytes. Extensive tubular atrophy is also seen (Fig. 1A). Glomerulosclerosis is also present as a secondary change, but more commonly the glomeruli are not damaged and become crowded because of the tubular atrophy. Since renal biopsies rarely give a significant sample of the inner medulla, it is often difficult to assign the relatively nonspecific cortical changes of interstitial fibrosis and tubular atrophy to this entity [52]. Similar lesions are produced in animal models using single or combination analgesics [51, 53, 54]. Thus, the presence of these cortical changes combined with radiologic and/or clinical evidence of papillary necrosis are consistent with the diagnosis of analgesic-induced nephropathy. Pathogenesis of analgesic-induced tubulointerstitial nephritis The pathogenesis of analgesic nephropathy is incompletely understood and no single mechanism seems to explain the findings. Prostaglandin inhibition, direct nephrotoxicity, and immunologic factors have all been suggested as possibilities. For example, it has been suggested that cyclooxygenase inhibition may lead to activation of caspases and apoptosis of cells in the medullary environment with subsequent repair by fibrosis. The bulk of the current evidence, however, points to a mechanism whereby Rastegar and Kashgarian: Tubulointerstitial nephritis a combination of analgesics may exert toxicity by the generation of the metabolites of phenacetin, aspirin, paracetamol, and salicylic acid, which are then concentrated in the medullary interstitium [54 –56]. Here they may be oxidized by prostaglandin endoperoxidase synthase to form even more toxic reactive metabolites that can injure either one or all of the endothelial, tubular or interstitial cellular components [57]. In addition, ASA and NSAIDs inhibit prostaglandin production by inhibition of cyclooxyganase enzymes. Renal blood flow is very dependent on systemic as well as local production of vasodilatory prostoglandins. This is especially true for renal medulla, which normally lives at edge of hypoxia and therefore is more prone to ischemic damage. The final injury is therefore due to both hemodynamic as well as cytotoxic effects of these drugs resulting in papillary necrosis and interestital fibrosis [58]. Clinical features and management of analgesic-induced tubulointerstitial nephritis As a component of analgesic syndrome AITIN presents 2 to 6 times more often in women than men. The major components of this syndrome is headache and/or musculoskeletal pain, epigasteric pain, anemia and renal failure. Abdominal pain is due to analgesic induced gastritis or ulceration resulting in chronic blood loss and iron-deficiency anemia [59]. Urinary findings include sterile pyuria, hematuria, and defects in urinary concentration and acidification. These findings are significantly more common than in patients with glomerular disease [60]. The clinical presentation of the analgesic associated syndrome partly depends on the content of analgesic mixture. Dyspepsia and iron deficiency anemia are more common in aspirin containing mixtures, while methemoglobinemia is a feature of mixtures containing phenacetin or its derivatives. It is estimated that approximately 10% of patients with analgesic syndrome develop ESRD [61]. On a long term basis the clinical signs and symptoms of renal damage dominate, including papillary necrosis, CRF and in a small subgroup, uroepithelial tumors. The diagnosis should be suspected in any individual with unexplained renal failure, especially in the presence of anemia out of proportion to the renal failure, a history of papillary necrosis, or unexplained medullary or papillary calcification. A history of analgesic use is often difficult to get and should be sought initially indirectly by focusing on reasons for taking analgesics [60]. Many of the signs and symptoms associated with AITIN (such as hypertension, anemia, sterile pyuria) do not have adequate specificity and sensitivity to be helpful. Elseviers et al in a series of studies have provided strong evidence that specific anatomic changes, best seen by non-contrast computer tomography (CT scan), has much greater sensitivity and specificity than other clinical signs and symptoms in the diagnosis of ESRD due to AITIN [62, 63]. These changes are: (1) decrease in renal volume; (2) bumpy renal contours; and (3) papillary 319 calcification. In a more recent study these observations were validated in a representative sample of patients with analgesics abuse with ESRD and extended to patients with moderate renal failure [64]. In patients with ESRD, decreased renal volume had the greatest sensitivity at 95% while papillary calcification had the highest specificity at 97%. The combination of small kidneys and a bumpy renal contour or papillary necrosis had a sensitivity and specificity of 90%. In patients with moderate renal failure papillary calcification was most sensitive at 92% and specific at 100%. Combination of papillary necrosis with either a bumpy renal contour or small kidneys did not improve sensitivity or specificity [64]. In clinical practice, however, it is important to remember that the predictive value of this test, like any other diagnostic test, is very much dependent on the prevalence of the disease in the population under study. This test should therefore be utilized only in patients with a reasonable risk for AITIN and not as a general screening test. The course of renal failure is often indolent, progressing over years to decades. If the drug is discontinued early in the course of renal injury, there is often stabilization or improvement in renal function. However, many patients continue to use the drug, despite advice to the contrary, and eventually develop ESRD [65]. The full spectrum of analgesic-associated interstitial damage includes patients who do not fit the classical diagnosis of AITIN. These patients often have other underlying renal diseases and the habitual use of analgesics accelerates the course of renal failure [45, 46, 48]. This group probably represents the majority of patients in countries with low to moderate analgesic use. No specific diagnostic test exists to allow recognition of these patients. We therefore feel that a careful history of analgesics use should be obtained in all patients with renal disease. While intermittent use of these drugs is safe in normal individuals as well as individuals with renal failure, long term use of these drugs (especially combination analgesics) should be avoided as it could result in AITIN or accelerate the course of the underlying renal disease [66, 67]. KIDNEY IN SARCOIDOSIS Sarcoidosis is a systemic disease of unknown etiology characterized by the presence of noncaseating granulomata in affected organs. The clinical presentation is usually dominated by pulmonary, dermal, and ocular involvement. Renal involvement is due to infiltration of renal interstitum by granulomata (Fig. 1B) and/or by granuloma-induced disturbances in calcium homeostasis. Granulomatous interstitial nephritis (GIN) is, however, seen in other diseases including allergic interstitial nephritis, Wegener’s granulomatosis, Berrylliosis, and tuberculosis [63, 68 –70]. The glomeruli are usually normal, however, granulomata can occasionally involve renal vessels. Other findings include 320 Rastegar and Kashgarian: Tubulointerstitial nephritis interstitial fibrosis and tubular atrophy. Interstitial calcification is seen in patients with hypercalcemia and or hypercalciuria. Granulomatous inflammation represents an intense immunologic response to a presumed antigen and consists of a collection of monocyte-derived macrophages and lymphocytes. Activated macrophages, located primarily in the center of the granuloma, are capable of antigen presentation to the lymphocytes and can coalesce into epithelioid or multinuclear giant cells. Lymphocytes are primarily CD4positive helper cells with a small number of CD8-positive suppresser cells forming a ring on the periphery of granuloma. The increase in number of activated macrophages and lymphocytes represents both local proliferation as well as recruitment from the circulating pool. These events are triggered by release of multiple cytokines including interleukin (IL)-1, IL-2, interferon gamma, colony stimulating factor, and chemotactic factor for monocytes. Tissue injury is a byproduct of this intense immunologic activity and involves recruitment of neutrophils capable of tissue necrosis through degranulation. Granulomata eventually undergo resolution by fibrosis. This process involves recruitment of fibroblast into granulomata by multiple cytokines including TGF-B and PDGF. The fibroblast proliferate locally and begin to lay down matrix protein resulting in irreversible fibrosis [71]. Clinical features of sarcoid nephropathy The incidence of renal involvement in sarcoidosis is unknown. A prevalence of 7 and 37% is reported in two autopsy series published over four to five decades ago [72, 73]. Renal involvement however is often clinically silent. LaBecq, Verhaegen and Desmet studied 152 patients and found 75 (49%) with a clinical renal abnormality that was primarily proteinuria and/or abnormal urinary sediments; 21 patients (14%) had renal calculi at some time in the course of the disease. Of the 25 patients who underwent renal biopsy, 10 had epithelioid granulomata [74]. These findings are supported by a smaller study of 42 patients by Romer, 23 of whom had renal abnormalities. Renal biopsy carried out in 15 patients showed GIN in five [75]. GIN usually presents as renal failure progressing over weeks to months. Kenouch and Mery noted that out of 75 reported cases in literature all but three had renal failure at presentation [76]. Proteinuria is mild, however, many patients have tubular defects including diabetes insipidus, renal tubular acidosis, and glycosuria. Macrophages in sarcoid granuloma contain a 1-alpha hydroxylase enzyme capable of activating vitamin D to its active form. The resultant increase in absorption of calcium from the gut causes hypercalcemia and hypercalciuria presenting as nephrolithiasis and/or nephrocalcinosis. The incidence of hypercalciuria is reported to be from 10 to 60%, hypercalcemia at 10%, and nephrocalcinosis at 5% [77]. In a highly selected referral group of 42 patients, Romer noted calcium abnormalities in 19: 3 with hypercalcemia, 4 with hypercalciurias, and 12 with hypercalcemia and hypercalciuria [75]. The macrophage alpha hydroxylase enzyme is unique in that it is not accompanied by the 24-hydroxylase enzyme. It also lacks negative feedback inhibition to its own product. It is, however, very sensitive to inhibition by glucocorticoids [78]. Diagnosis and treatment of sarcoid nephropathy Sarcoid nephropathy should be considered in any patient with unexplained renal failure and hypercalcemia, nephrocalcinosis, renal tubular defect or increased immunoglobulins. These patients often have signs and symptoms of pulmonary, ocular and/or dermal involvement with sarcoidosis. The initial workup should therefore attempt to establish this diagnosis through a standard workup. The presence of granulomata on renal biopsy, while not specific to sarcoidosis, should strongly suggest this diagnosis in an appropriate setting [68, 69]. In patients with known sarcoidosis, sarcoid nephropathy should be considered in the presence of renal failure, hypercalcemia, nephrolithiasis, nephrocalcinosis or renal tubular defects. GIN can be treated effectively with glucocorticoids [75]. Patients often respond quickly with improvement in renal function, however, this depends greatly on the extent and severity of inflammation and fibrosis before treatment is initiated. There are no data regarding the dose or length of the treatment. We recommend the standard anti-inflammatory dose of 1 to 1.5 mg/kg initially continued for eight weeks, followed by slow taper guided by recurrence of signs and symptoms of disease activity. The hypercalcemia/hypercalcuric syndrome also responds quickly to corticosteroid, but a recurrence may occur if the treatment is discontinued rapidly. In general the dose needed to treat this complication is significantly lower than the dose needed to treat GIN, and can be as low as 35 mg of prednisone daily [79]. Chloroquine, by decreasing the level of 1,25 dihydroxycholecalciferol, is an effective therapy for the hypercalcemic/hypercalciuric syndrome [80]. Ketoconazole, an inhibitor of steroidogenesis, has been used in a single patient who could not tolerate corticosteroids. It was effective in decreasing the level of active vitamin D as well as serum and urinary calcium [81]. The length of any of the treatments is dependent on the level of activity of the disease and may be lifelong in a small number of patients. LEAD NEPHROPATHY An abundant heavy metal, lead has been a part of human history for millennia. The major sources of exposure today are through lead-based paints, lead leached into food and beverages during processing and storing, and, increasingly, through industrial and environmental exposure. Lead toxicity affects many organs resulting in encephalopathy, anemia, peripheral neuropathy, gout, and renal failure. Acute Rastegar and Kashgarian: Tubulointerstitial nephritis lead toxicity, often seen in children below six years of age, is primarily due to paint chip pica, and results in severe encephalopathy, seizures and proximal tubular damage presenting as Fanconi syndrome [82]. The blood lead level in these children is usually above 150 mg/dl and the diagnosis is usually apparent. The pathology includes the presence of proximal tubular intranuclear inclusion bodies that resolve with chelation therapy (Fig. 1D). If exposure continues, chronic tubulointerstitial nephritis may develop decades later and present as progressive renal failure and/or hypertension. Epidemiology of lead nephropathy The first case of lead-induced renal cortical atrophy and interstitial fibrosis was reported by Lanceraux in 1863 and 1881. It was found in an artist who habitually had held his painting brush in his teeth [83]. Although lead nephropathy was accepted as a defined entity by the end of the 19th century, it was the epidemic of lead nephropathy in Queensland, Australia that provided the strongest link between lead and chronic TIN. Lead exposure was due to the lead based paints used between 1890 and 1930 [84]. Henderson, among others, noted the excess mortality due to chronic interstitial nephritis to be present in Queensland but not in other parts of Australia. The higher mortality was observed first in the youngest age groups and then later in the oldest age groups. It declined beginning in 1930s, after lead-based paints were banned in 1922 [16]. Henderson traced 354 out of 401 cases of childhood plumbism admitted to Brisbane Children’s Hospital between 1915 to 1935, and noted that of the 165 who had already died, 108 had died of renal or vascular disease and 20 of 187 living individuals had proteinuria and/or hypertension. He then correlated the incidence of granular contracted kidney found at autopsy with the lead content of the skull in Queensland and Sydney, and showed that the lead content of the skull closely correlated with the incidence of renal failure. In addition, 67% of patients with small contracted kidneys in Queensland did not fit into a known renal disease while all the patients in Sydney had a known primary diagnosis. The bone lead content in patients with small contracted kidneys from Queensland was significantly higher than in other patients in either Sydney or Queensland (8 vs. 2 mg/100 g of bone) [85]. Emmerson showed a significantly higher total body lead burden using EDTA mobilization tests in subjects with CTIN of unknown etiology compared to chronic renal failure of known etiology and normal subjects [86]. Chronic lead toxicity in the U.S. is more commonly due to ingestion of illicit alcohol (socalled moonshine) where lead is leached into the product during the distillation process [87, 88]. More recently the major source of lead exposure has shifted from lead-based paint and moonshine to industrial exposure. This type of exposure is often insidious, occurring over very long periods [89 –91]. Weeden, Mallik and Batuman studied 140 321 asymptomatic lead workers, 113 of whom had increased total body lead burden by the EDTA mobilization test. Twenty-one of the 57 patients who had GFR measurements by the iothalamate Na 125I test had values below 90 ml/min/1.73 m2. However, only 3 patients had a serum creatinine above 1.5 mg%. Using stringent criteria, the authors felt that at least 15 of the patients had lead nephropathy [90]. Pinto de Almeida et al screened 52 lead workers in Brazil with high lead exposure and compared their renal function with 44 workers from a paper mill. Renal dysfunction defined as serum creatinine above 1.5 mg% was seen in 17 (32.7%) of the lead workers and 1 (2.3%) of controls. In addition, the exposed group had significantly higher uric acid level than control (6.6 6 1.7 vs. 4.4 6 1.2 mg%, P , 0.001) [91]. Two studies have shown an inverse relationship between low level lead exposure and renal function in general population [92, 93]. In the study of approximately 2,000 civil servants in England, Staessen noted a decrease in GFR by 10 to 13 ml/min with a 10-fold increase in the serum lead level [92]. In another retrospective cohort study of 459 men, a similar rise in the serum lead level was associated with a small but significant increase in serum creatinine equivalent to the expected rise seen with 20 years of aging [93]. No data on bone lead level was provided in either study and no patient developed ESRD. The role of childhood lead exposure in development of CRF remains controversial. The Australian studies by Henderson et al established a causal relationship in that population [16]. Two recent studies evaluating renal function 17 to 50 years after an episode of acute childhood plumbism, however, have failed to show any effect on renal function [94, 95]. The difference between these findings and the findings reported by Henderson and others from Australia probably reflects the greater lead burden in the latter population. The Australian children were exposed to lead paint over a long period of time when the danger of the exposure was unknown [16]. The American studies are a follow up of children diagnosed with acute plumbism and who were probably removed from continuous exposure. These studies are therefore not comparable to the Australian study. Although ESRD is a feature of lead exposure in unique populations [16], its contribution to overall ESRD incidence is not clear. In a study of 135 patients from Belgium, France and Germany, 8 patients (5%) had an iliac bone lead level equivalent to level seen in lead workers. Follow-up data in 6 of these patients verified a history of significant lead exposure with no other renal disease. In this population it is possible that exposure to lead played a significant role in the development of renal failure [96]. In summary, acute childhood plumbism is not associated with renal failure decades later, and low level lead exposure in general population is associated with mild but significant depression of renal function. The role of such exposure in the development of ESRD is at present unclear. 322 Rastegar and Kashgarian: Tubulointerstitial nephritis Pathology of lead nephropathy Renal biopsies have not been carried out systematically in patients with lead nephropathy. Biopsies in 12 patients with subclinical lead nephropathy and mild to moderate decrease in GFR were normal in six and showed primarily focal tubular atrophy and interstitial fibrosis with minimal cellular infiltration in others. Electron microscopy showed mitochondrial swelling, loss of cristae, loss of basal infoldings, and a lysosomal-like structure containing dense bodies in the proximal tubules. Immunofluorescence microscopy showed mild deposits of immunoglobulins and complement in both glomeruli and proximal tubules [90]. The most extensive pathological data are provided by Inglis, Henderson and Emmerson on patients who had died of severe lead exposure in Australia [97]. Kidneys were fibrotic and shrunken, often weighing less than 100 grams. The interstitum showed variable degree of fibrosis with tubular dilation. The vessels had thickened muscular walls with subintimal hyaline deposition in afferent arterioles. The most specific and interesting finding was the disappearance of glomeruli “without trace” noted in a majority of the specimens [97]. It should be noted that these findings are in autopsies of patients who had died of ESRD. Although some of the findings are nonspecific and are seen in any end-stage tubulointerstitial disease, the severity of renal contraction as well and glomerular drop out favors this diagnosis. Clinical features of lead nephropathy Epidemiological studies have firmly established the relationship between chronic lead toxicity and chronic TIN. Renal failure becomes apparent years after the exposure and is associated with gout in up to half of the cases [86]. Although hyperuricemia is common in renal failure, gout is highly unusual and its presence should raise the possibility of lead nephropathy [98, 99]. In addition, patients with primary gout without lead toxicity rarely develop renal failure [100, 101]. Bautman et al studied 44 patients with gout, half with renal failure (serum creatinine . 1.5 mg%). Three-day EDTA mobilization tests resulted in a significantly greater lead excretion in patients with rather than without renal failure (806 6 90 vs. 470 6 52 mg/three days, P , 0.005). Lead excretion in 10 patients with renal failure of other etiologies was similar to patients with gout without renal failure and normal subjects [102]. The diagnosis of lead nephropathy should be considered in any patient with progressive renal failure, mild to moderate proteinuria, significant hypertension, history of gout and appropriate history of exposure. Ultrasonography of the kidneys shows bilaterally small, echogenic kidneys without focal scars. As the blood lead level only reflects recent lead exposure and is usually normal in these patients, the diagnosis should be based on measurement of body lead burden by EDTA mobilization test or measure- ment of bone lead content by bone biopsy. The EDTA test involves administration of 2 grams of EDTA intramuscularly in two divided doses 8 to 12 hours apart and collection of three consecutive 24-hour urine samples. Individuals with a high lead burden will have a cumulative excretion rate of more than 0.6 mg. Renal failure in itself does not increase body lead load but delays lead excretion [102]. The three-day urinary collection, however, assures a complete measurement of excreted lead in these patients. Recently, a new technique using x-ray fluorescence has been utilized to measure the bone lead level [103]. This technique is highly accurate and reproducible and can provide a rapid, noninvasive measure of body lead stores [104]. In general the clinical course of lead nephropathy is slowly progressive and is often dominated by recurrent gouty attacks and hypertension. There is little experience in the therapeutic use of EDTA in patients with chronic renal disease. Weeden et al treated 8 patients with industrial exposure with EDTA injection trice weekly for 6 to 50 months. Four patients improved with a 20% increase in GFR. All these patients had mild renal failure with the lowest GFR of 52 ml/min before treatment. EDTA has no effect on patients with serum creatinine of greater than 3.0 mg% [90]. Hypertension and gout dominate the course, which finally leads to ESRD in a small subgroup. Lead and hypertension Hypertension is a very common feature of lead nephropathy. Association between hypertension without renal failure and low level lead exposure has gained increasing support over the past two decades. In a study of 21 hypertensive patients with no renal disease and 27 with renal disease the three days EDTA mobilization test showed a significantly higher excretion of lead in those with renal failure (860 6 101) than those without renal failure (340 6 39, P , 0.001) and patients with comparable renal failure of known cause (440 6 50) [105, 106]. This relationship has been strengthened by a variety of epidemiological studies done in the past decade [107–110]. In a recent case-control study of 1171 participants in the Normative Aging Study, Hu et al [110] using K-x-ray fluorescence showed that body lead burden was an an independent risk factor along with body mass index and family history of hypertension for the development of hypertension. The link may be through activation of reninangiotensin system [111–113] or through an increase in sodium-lithium countertransport [114]. ACUTE DRUG-INDUCED TUBULOINTERSTITIAL NEPHRITIS It is now widely recognized that a large variety of drugs including b-lactam antibiotics, non-steroidal anti-inflammatory drugs, diuretics, anticonvulsants, and an increasingly diverse group of other drugs can be associated with an allergic acute tubular interstitial nephritis [115–124]. In two Rastegar and Kashgarian: Tubulointerstitial nephritis large unselected renal biopsy series, the incidence of acute interstitial nephritis (AIN) was estimated at 1.2 to 1.3% [23, 125]. Richet et al, in a study of 976 patients with acute renal failure, noted that 14% of 218 biopsies were compatible with this diagnosis for a minimum incidence of 3% in this population [126]. The exact incidence is unknown, as the reported series is small and highly selective and patients with this diagnosis are often not biopsied. Pathology and pathogenesis of acute interstitial nephritis It is likely that this form of interstitial nephritis is immunologically mediated and idiosyncratic in nature. The clinical evidence is circumstantial and consists of the presence of a rash, fever and/or eosinophilia, the occurrence of nephritis in only a minority of exposed individuals independent of the drug dose, the recurrence of the disease upon re-exposure and the response to corticosteroid therapy [127]. The exact immune mechanisms involved have not been clearly defined, but it is likely that cell mediated hypersensitivity is involved since the histologic lesion is very similar to that seen in allograft rejection. One of the most distinguishing features of acute druginduced tubulointerstitial nephritis is the nature of the interstitial infiltrate. The interstitium is edematous, where the tubules are separated by a palely stained interstitium (in contrast to the dense staining of fibrosis) and infiltrated with a significant number of eosinophils and mononuclear cells (Fig. 1C). The infiltrate is characteristically focal, is most prominent at the cortical medullary junction, and often surrounds individual tubules. The mononuclear portion of the infiltrate is predominately lymphocytic with some macrophages and plasma cells, and sometimes forms granulomata. The eosinophils tend to concentrate in small foci and may form the eosinophilic microabscesses. Neutrophils can be present but are uncommon. A second distinguishing characteristic is the presence of tubulitis. Particularly with PAS stains, lymphocytes can be seen invading the tubules beneath the tubular basement membrane. Variable degrees of tubular epithelial cell damage with evidence of regeneration as identified by the presence of mitotically shaped and pleomorphic nuclei are almost always found, but extensive necrosis of the epithelium is rare. Additional evidence that the process is immune mediated has been derived from immunohistochemical analysis of biopsies of such patients. The infiltrate usually has a predominance of T lymphocytes expressing the CD4 antigen, and in most cases there is an enhanced expression of HLA Class II antigens on the tubular epithelium [120 – 130]. Immunofluorescence and electron microscopy of such cases has not revealed the presence of immune deposits, further suggesting that the immune process is cell mediated. The glomeruli are usually not affected and evidence of vasculitis is generally not seen. Although drugs have been implicated in most cases of allergic interstitial nephritis, a similar picture can be found in patients with lupus 323 nephritis [131–133] and rarely in association with antitubular basement membrane antibodies [120]. Biopsy proven instances of acute oliguric tubulointerstitial nephritis with a similar histologic picture but without any known drug exposure have also been reported [124, 134]. One special group includes the association of acute interstitial nephritis with uveitis and bone marrow and lymph node granulomata [135–137]. This syndrome occurs predominately in adolescent girls and young women and with the presence of granulomata in the kidney, and must be distinguished from sarcoid involvement. Clinical features and management of acute interstitial nephritis Although the clinical manifestations may be variable, they are usually heralded by fever, hematuria and/or azotemia. Eosinophilia occurs in a majority of cases. Urinalysis reveals hematuria, sterile pyuria and moderate proteinuria. Eosinophils may be detected in the urinary sediment [138, 139]. A variety of tubular defects including hyporenenimic hypoaldosteronism, salt losing nephropathy [122], and potassium and magnesium wasting [140] have been reported. A skin rash is seen in some patients lending support to the concept that the disease may be immunologically mediated. The azotemia may be severe and patients may present with acute renal failure leading to the use of the renal biopsy as a diagnostic procedure. A unique syndrome of renal failure and nephrotic syndrome is reported in association with NSAIDs [128, 141] and less commonly other drugs [142]. Renal biopsy, in addition to classical findings of allergic interstitial nephritis, shows extensive foot process fusion compatible with nil disease. The diagnosis of AIN is primarily clinical, and is often considered in the setting of rising creatinine in a patient with or without history of chronic renal failure. A minority of patients have a classical triad of skin rash, fever, and eosinophilia initially described with methicillin-induced AIN [117]. Urinalysis shows variable degrees of proteinuria in association with pyuria and hematuria. Using a special stain, Nolan, Angers and Kelleher reported a sensitivity of 91% (10 of 11 patients) and specificity of 85% (69 of 81 controls) for eosinophiluria [139], for a positive predictive value of 43%. Given the spectrum of the disease and lack of standardization of the test, its value in management of patients with AIN should be questioned [127, 138, 143]. In a study of 97 patients, gallium scanning had a sensitivity of 100% and specificity of 91%, which decreased to 85% if the data were limited to biopsy proven patients only [144]. These data have not been independently verified. Renal biopsy remains the gold standard and should be strongly considered in any patient where the exact diagnosis is critical for appropriate management. The course of AIN is highly variable and can lead to irreversible renal failure if the offending agent is not removed. In patients with mild to moderate renal failure, 324 Rastegar and Kashgarian: Tubulointerstitial nephritis discontinuation of the drug is often associated with a return of renal function toward baseline. In two biopsy-proven series with total of 44 patients, 2 developed ESRD, 17 returned to normal renal function, and the remainder recovered significantly but remained with varying degree of renal failure. The recovery rate is probably higher as the preinjury creatinine was not available in all patients [120, 145]. The recovery often takes several weeks and may continue up to a year after discontinuation of offending agent [145]. These two series are too small to develop reliable predictive parameters, however, the severity of initial clinical course, degree of improvement in the initial six to eight weeks and severity of pathological lesion correlated with the final outcome [120, 145]. The role of steroid therapy in the management of these patients is highly controversial. Galpin et al in a study of methicillininduced AIN noted that 8 patients treated with prednisone had greater and faster recovery of their renal function compared to 14 untreated patients [120]. Pusey et al, in another retrospective study, noted that 7 of 7 patients treated with intravenous prednisone recovered, while two untreated patients developed chronic renal failure and one patient had slow recovery [146]. These uncontrolled retrospective studies in highly selected patients do not provide adequate guidelines to clinicians in the management of these patients. Given the suggestive data in literature and until well-controlled prospective studies are done, we recommend a short course of high-dose steroid therapy (1 mg/kg body wt for 2 weeks with a rapid taper) in patients with appropriate clinical and/or histological findings and significant renal failure. In patients with mild renal failure we prefer to discontinue the offending agent and follow the patient closely. CONCLUDING REMARKS Tubulointerstitial diseases represent a group of heterogenous disorders with vaying etiology, pathogenesis and clinical course, and make up a significant percentage of patients with renal disease. Over the past three decades, we have developed an better understanding of the basic mechanism of tubulointerstitial injury as well as epidemiology, clinical presentation and course of specific disorders. As the four disorders discussed in this report shows, many tubulointerstitial disorders are either preventable and/or treatable. In addition, new disorders involving this compartment, such as TIN due to Chinese herbs used for weight loss [147], continue to be described. A better understanding of the epidemiology, pathogenesis, clinical presentation and course of the disease should help us prevent and/or treat this group of disorders. Reprint requests to Asghar Rastegar, M.D., Department of Internal Medicine, Yale University School of Medicine, 333 Cedar St., New Haven, Connecticut 06520, USA. APPENDIX Abbreviations used in this article are: AIN, acute interstitial nephritis; AITIN, analgesic-induced tubulointerstitial nephritis; ASA, acetosalicylic acid; CRF, chronic renal failure; CT, computer tomography; CTIN, chronic tubulointerstitial nephritis; ESRD, end-stage renal disease; GFR, glomerular filtration rate; GIN, granulomatous interstitial nephropathy; HIV, human immunodeficiency virus; IL, interleukin; NSAIDs, nonsteroidal anti-inflammatory drugs; OR, odds ratio; PDGF, platelet-derived growth factor; RBC, red blood cells; RR, relative risk; SLE, systemic lupus erythrematosus; TGF-B, transforming growth factor-B; TIN, tubulointerstitial nephritis; WBC, white blood cells. REFERENCES 1. WOLGAST MA, LARSON M, NYGREN K: Functional characteristics of renal interstitium. Am J Physiol 241(Renal Fluid Electrolyte Physiol 10):F105–F111, 1981 2. LEMLEY KV, KRIZ W: Anatomy of the renal interstitium. Kidney Int 39:370 –381, 1991 3. STRIKER GE, SCHAINUCK LI, CUTLER RE, BENDITT EP: Structuralfunctional correlations in renal diseases. Part 1: A method for assaying and classifying histophatholgic changes in renal disease. Hum Pathol 1:615– 630, 1970 4. MUJAIS S, BATTLE DC: Functional correlates of tubulo-interstitial damage. Semin Nephrol 8:94 –99, 1988 5. EKNOYAN G, MCDONALD MA, APPEL D, TRUONG LD: Chronic tubulo-interstitial nephritis: Correlation between structural and functional findings. Kidney Int 38:736 –743, 1990 6. BOHLE A, MACKENSEN-HAEN S, GISE H: The consequences of tubulointerstitial changes for renal function in glomerulopathies, in Tubulo-Interstitial Nephropathies, edited by AMERIO A., CORTELLI P, MASSRY SE, Boston, Dordrecht, London, Kluwer Academic Press, 1991, pp 29 – 40 7. NATH KA: Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis 20:1–17, 1992 8. WILSON CB: Nephritogenic tubulointerstitial antigens. Kidney Int 39:501–17, 1991 9. NIELSON EG: Pathogenesis and therapy of interstitial nephritis (clinical conference). Kidney Int 35:1257–1270, 1989 10. JONES CL, EDDY AA: Tubulointerstitial nephritis. Pediatr Nephrol 6:572–586, 1992 11. DODD S: The pathogenesis of tubulointerstitial disease and mechanisms of fibrosis. Curr Topic Pathol 88:51– 67, 1995 12. EDDY AA: Experimental insights into the tubulointerstitial disease accompanying primary glomerular lesions. J Am Soc Nephrol 5:1273– 1287, 1994 13. COUNCILMAN WJ: Acute interstitial nephritis. J Exp Med 3:303– 420, 1898 14. ZOLLINGER H, SPUHLER O: Die nicht-eitrige chronische interstitielle Nephritis. Scheizerische Zeitschrift fuer Allgemeine Pathologie 13:807– 811, 1950 15. SPUHLER O, ZOLLINGER HU: Die chronisch-interstitielle nephritis. Zeitschrift fuer Med 151:1–50, 1953 16. HENDERSON DA: Chronic nephritis in Queensland. Aust Ann Med 4:164 –177, 1955 17. MURRAY TG, GOLDBERG M: Analgesic-associated nephropathy in the USA: Epidemiologic, clinical and pathogenetic features. Kidney Int 13:64 –71, 1978 18. MURRAY TG, STOLLEY PD, ANTHONY JC, SCHINNAR R, HEPLERSMITH E, JEFFREYS JL: Epidemiologic study of abuse of analgesics containing phenacetin. N Engl J Med 308:357–362, 1983 19. POMMER W, GLAEDKE G, MOLZAHN M: The analgesic problem in the the Federal Republic of Germany: Analgesic consumption, frequency of analgesic nephropathy and regional differences. Clin Nephrol 26:274 –278, 1986 20. POMMER W, BRONDER E, GREISER E, HELMERT U, JESDINSKY HJ, KLIMPEL A, BORNER K, MOLZAHN M: Regular analgesic intake and the rish of end-stage renal disease. Am J Nephrol 9:403– 412, 1989 21. SANDLER DP, SMITH JC, WEINBERG CR, BUCKALEW VM JR, DENNIS VW, BLYTHE WB, BURGESS WP: Analgesic use and chronic renal disease. N Engl J Med 320:1238 –1243, 1989 Rastegar and Kashgarian: Tubulointerstitial nephritis 22. UNITED STATES RENAL DATA SYSTEM: 1996 Annual Data Report: II. Incidence and prevalence of ESRD. Am J Kidney Dis 28(Suppl 2):S34 –S47, 1996 23. ZOLLINGER HU, MIHATSCH MJ: Renal Pathology in Biopsy. Berlin, Springer-Verlas, 1978, pp 407– 410 24. PETTERSSON G, VONBONSDORFF M, TOMROTH T, LINDHOLM H: Nephritis among young Finnish men. Clin Nephrol 22:217–222, 1984 25. GONWA TA, HAMILTON RW, BUCKALEW VA: Chronic renal failure and end-stage renal disease in northwest North Carolina: Importance of analgesic associated nephropathy. Arch Intern Med 141:462– 465, 1981 26. PENDREIGH DM, HOWITT LF, MACDOUGAL AJ, ROBSON JS, HEASMAN MA, KENNEDY AC, MACLEOD M, STEWART WLD: Survey of chronic renal failure in Scotland. Lancet 1:304 –307, 1972 27. ROSTAND SG, KIRK KA, RUTSKY EA, PATE BA: Racial difference in the incidence of treatment of end-stage renal disease. N Engl J Med 306:1276 –1279, 1982 28. FARRINGTON K, LEVISON DA, GREENWOOD RN, CATTELL WR, BAKER LR: Renal biopsy in patients with unexplained renal impairment and normal kidney size. Quart J Med 70:221–233, 1989 29. CHURG J, COTRAN RS, SAKAGUCHI H, SOBIN LH: Renal Disease Classification and Atlas of Tubulointerstitial Disease. Tokyo, New York, Igaku-Shoin, 1984 30. MARCUSSEN N: Atubular glomeruli in chronic renal disease. Curr Topic Pathol 88:145–175, 1995 31. PALMER B: The tubules in progression of renal failure. J Invest Med 45:346 –361, 1997 32. NATH KA: Reshaping the interstitium by platelet-derived growth factor. Implications for progressive renal disease. Am J Pathol 148:1031–1036, 1996 33. COGAN MG: Tubulo-intersitial nephropathies: A pathophysiological approach — Medical Staff Conference, University of California, San Francisco. West J Med 132:134 –140, 1980 34. MOLZHAN M, POMMER W: Analgesic nephropathy, in Oxford Textbook of Clinical Nephrology, edited by CAMERON S, DAWSON, AM, GRÜNFELD, JP, KERR D, RITZ E, Oxford, Oxford Medical Publication, 1992, pp 803– 819 35. BUCKALEW VM, SCHEY HM: Renal disease from habitual antipyretic analgesic consumption: An assessment of the epidemiologic evidence. Medicine 11:291–303, 1986 36. VANHERWEGHEM JL, EVEN-ADIN D: Epidemiology of analgesic nephropathy in Belgium. Clin Nephrol 17:129 –133, 1982 37. CLUNIE GJA, HARTLEY LCJ, RIBUSH NT, EMMERSON BT, MORGAN TO: An integrated service for treatment of irreversible renal failure. Med J Aust 2:403– 408, 1971 38. NOELS LM, ELSEVIERS MM, DE BROE ME: Impact of legislative measures of the sales of analgesics and the subsequent prevalence of analgesic nephropathy: A comparative study in France, Sweden and Belgium. Nephrol Dial Transplant 10:167–174, 1995 39. NORDERFELD O: Deaths from renal failure in abusers of phenacetincontaining drugs. Acta Med Scand 191:11–16, 1972 40. KASANEN A: The effect of restriction of the sale of phenacetin on the incidence of papillary necrosis established at autopsy. Ann Clin Res 5:369 –374, 1973 41. MABECK CE, WICHMANN B: Mortality from chronic interstitial nephritis and phenacetin consumption in Denmark. Acta Med Scand 205:599 – 601, 1979 42. WILSON DR, GAULT MH: Declining incidence of analgesic nephropathy in Canada. Can Med Assoc J 127:500 –502, 1982 43. MCCREDIE M, STEWART JH, MATHEW TH, DISNEY AP, FORD JM: The effect of withdrawal of phenacetin-containing analgesics on the incidence of kidney and urothelial cancer and renal failure. Clin Nephrol 31:35–39, 1989 44. DUBACH UC, ROSNER B, PFISTER E: Epidemiologic study of abuse of analgesics containing phenacetin. Renal morbidity and mortality (1968 –1979). N Eng J Med 308:357–362, 1983 45. PERNEGER TV, WHELTON PK, KLAG MJ: Risk of kidney failure associated with the use of acetaminophen, aspirin, and nonsteroidal antiinflammatory drugs. N Engl J Med 331:1675–1679, 1994 46. SANDLER DP, BURR FR, WEINBERG CR: Nonsteroidal antiinflammatory drugs and risk of chronic renal failure (see comments). Ann Intern Med 115:165–172, 1991 47. MCCREDIE M, STEWART JLD, MAHONEY JF: Is phenacetin respon- 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 325 sible for analgesic nephrology in New South Wales. Clin Nephro l 17:134 –140, 1982 MORLANS M, LAPORTE JR, VIDAL X, CABEZA D, STOLLEY PD: End-stage renal disease and non-narcotic analgesics: A case control study. Br J Clin Pharmacol 30:717–723, 1990 SCHUBERT GE, BETHKE BA: Capillarosclerosis of the renal pelvis: Autopsy study for estimating the incidence of phenacetin and paracetamol abuse. Eur Urol 12:327–330, 1986 MIHATSCH MJ, HOFER HO, GUDAT F, KNUESL C, TORHORST J, ZOLLINGER HU: Capillary sclerosis of urinary tract and analgesic nephropathy. ztitle of journal? 20:285–301, 1983 BURRELL JH, YONG JLC, MACDONALD GJ: Analgesic nephropathy in Fischer 344 rats: Comparative effects of chronic treatment with either aspirin or paracetamol. Changes in renal structure and urinary concentrating ability in Fischer 344 rats given continuous low doses of aspirin and paracetamol. Pathology 22:33– 44, 1990 MIHATSCH M, TORHORST J: The morpholgic diagnosis of analgesic (phenacetin) abuse. Path Res Pract 164:68 –79, 1979 BURRELL JH, YONG JLC, MACDONALD GJ: Analgesic nephropathy in Fischer 344 rats: Comparative effects of chronic treatment with either aspirin or paracetamol. Pathology 23:107–114, 1991 MOLLAND EA: Experimental renal papillary necrosis. Kidney Int 13:5–14, 1978 BLUEMLE LW JR, GOLDBERG M: Renal accumulation of salicylate and phenacetin: Possible mechanisms in the nephropathy of analgesic abuse. J Clin Invest 47:2507–2514, 1968 DUGGINS GC, MUDGE GH: Analgesics nephropathy; renal distribution of acetaminophen and its conjugates. J Pharmacol Exp Ther 199:1–9, 1976 MOHANDAS J, DUGGIN GG, HORVATH JS, TILLER DJ: Metabolic oxidation of acetaminophen (paracetamol) medicated by cytochrome P-450 mixed-function oxidase and prostaglandin endoperoxide systhetase in rabbit kidney. Toxicol Appl Pharm 61:252–259, 1981 SABATINI S: Pathophysiologic mechanism in analgesic-induced papillary necrosis. Am J Kidney Dis 28(Suppl 1):S34 –S38, 1996 HENRICH WL: Analgesic nephropathy. Am J Med Sci 295:561–568, 1988 NANRA RS: Pattern of renal dysfunction in analgesic nephropathy— Comparison with glomerulonephritis. Nephrol Dial Transplant 7:384 –390, 1992 KINCAID-SMITH P: Analgesics-induced renal disease, in Diseases of the Kidney, edited by SCHRIER RW, GOTTSCHALK CW, Boston, Little, Brown, and Company, 1988, pp 1202–1216 ELSEVIERS MM, BOSTEELS V, CAMBIER P, DE PAEPE M, GODON JP, LINS R, LORNOR W, MATHYS E, MOERENMANS C, ROOSE R, THEELEN JB, VAN CAESBROECK D, VERBANK J, DE BROE ME: Diagnostic criteria of analgesic nephropathy in patients with endstage renal failure–Result of the Belgian Study. Nephrol Dial Transplant 7:479 – 486, 1992 ELSIEVIERS MM, WALLER I, NENOV D, LEVORA J MATOUSOVIC K, TANQUEREL T, POMMER W, SCHARZ A, KELLER E, THIELER H, KOHLER H, LEMONIATOU H, CRESSERI D, BOUCCHI D, FIOCCHI O, JORDANS J, FRANEK E, SILVE FJ FERNANDEZ RUIS EJ, MORLANS M, HELLSTROM M, WAUTERS JP, FELLE D, CASSI HV, DE BROE ME: Evaluation of diagnostic criteria for analgesic nehpropathy in patients with end-stage renal failure: Result of ANNE study. Nephrol Dial Transplant 10:808 – 814, 1995 ELSEVIERS MM, DE SCHEPPER A, CORTHOUTS R, BOSMANS JL, COSYN L, LINS RL, LONROY W, MATHYS E, ROOSE R, VAN CAESBROECK D, WALLER I, HORACKOVA M, SCHWARZ A, SVRECK P, BOUCCHIM D, FRANEK E, MORLANS M, DE BROE ME: High diagnostic performance of CT scan for analgesic nephropathy in patients with incipient to severe renal failure. Kidney Int 48:1316 –1323, 1995 HAUSER AC, DERFLER K, BALCKE P: Progression of renal insufficiency in analgesic nephropathy: Impact of continuous drug abuse. J Clin Epidemiol 44:53–56, 1991 HENRICH WL, AGODOA LE, BARRETT B, BENNETT WM, BLANTZ RC, BUCKALEW VM JR, D’AGATI VD, DE BROE ME, DUGGIN GG, EKNOYAN G, ELSEVIERS MM, GOMEZ A, MATZKE GR, PORTER GA, SABATINI S, STOFF JS, STRIKER GE, WINCHESTER JF: National Kidney Foundation Position Paper. Analgesics and the kidney: Summary and recommendations to the Scientific Advisory Board of 326 67. 68. 69. 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. 87. 88. 89. 90. 91. 92. 93. Rastegar and Kashgarian: Tubulointerstitial nephritis the National Kidney Foundation from an Ad Hoc Committee of the National Kidney Foundation. Am J Kidney Dis 27:162–165, 1996 BENNETT WM, HENRICH WL, STOFF JS: The renal effects of nonsteroidal anti-inflammatory drugs: Summary and recommendations. Am J Kidney Dis 28(Suppl 1):S56 –S62, 1996 MOREL-MARGER LF, MERY JP, MOUGEN WTB, RONCO P, ROLAND J: Granulomatous interstitial nephritis. Adv Nephrol 13:219 –245, 1984 VIERO RM, CAVALLO T: Granulomatous interstitial nephritis. Hum Pathol 26:1347–1353, 1995 CRUZADO JM, POVEDA R, MANA J, CARRERAS L, CARRERA M, GRINYO JM, ALSINA J: Interstitial nephritis in sarcoidosis: Simultaneous multiorgan involvement. Am J Kidney Dis 26:947–951, 1995 SEMENZATO G, AGOSTINIC, CHILOSI M: Immunology and immunopathology, in Sarcoidosis and Other Granulomatous Diseases, edited by JAMES DG, New York, Marcel Dekker, Inc., 1994, pp 153–180 BRANSON JA, PAK JH: Sarcoidosis hepatic involvement: Presentation of a case with fatal liver involvement, including autopsy findings and review of evidence in sarcoid of liver as found in literature. Ann Intern Med 40:111–114, 1954 RICKER W, CLARK M: Sarcoidosis; A clinicopathological review of 300 cases including 22 autopsies. Am J Clin Pathol 19:725, 1949 LABECQ E, VERHAEGEN H, DESMET V: Renal involvement in sarcoidosis. Post Grad Med J 46:526 –529, 1970 ROMER FK: Renal manifestation and abnormal calcium metablolism in sarcoidosis. Quart J Med (New Series) XLIX:195–233-247, 1980 KENOUCH S, MERY JP: Sarcoidosis, in Oxford Textbook of Clinical Nephrology, edited by CAMERON S, DAVISON AM, GRÜNFELD JP, KERR D, RITZ G, Oxford, Oxford Medical Publications, Oxford, 1992, pp 576 –582 HOFFBRAND BI: The kidney in sarcoidosis, in Sarcoidosis and Other Granulamatous Diseases, edited by JAMES DG, New York, Marcel Dekker Inc., 1994, pp 335–344 ADAMS JS, GACAD MA: Characterization of 1 hydroxylation of vitamin D steroids by altered alveoler macrophages from patients with sarcoidosis. Exp Med 161:755–765, 1985 NORDAL KP, DAHL E, HALSE E, AKSNES L, AARSBOG D: Rapid effect of prednisolone on serum 1,25-Dihydroxycholecalciferol levels in hypercalcemic sarcoidosis. Acta Med Scand 218:519 –523, 1985 MCLEARY TJ, JONES G, YIP A, LOHNES D, COHANIM M, YENDT ER: The effect of chloroquine on serum 1,25-dihydroxyvitamin D and calcium metabolism in sarcoidosis. N Engl J Med 315:727–730, 1986 BIA MJ, ANSOGNIA K: Treatment of sarcoid-associated hypercalcemia with ketoconazole. Am J Kidney Dis 18:702–705, 1991 BEATTIE AD, BRIGGS JD: Acute lead poisoning. Quart J Med 4:275–284, 1975 WEDEEN RP: Poison in the Pot: The Legacy of Lead. Carbondale, Southern Illinois University Press, 1984 NYE LJJ: An investigation of the extraordinary incidence of chronic nephritis in young people in Queensland. Med J Aust 2:145–152, 1929 HENDERSON DA: The etiology of chronic nephritis in Queensland. Med J Aust 25:196 –202, 1958 EMMERSON BT: Chronic lead nephropathy. The diagnostic use of calcium EDTA and the association with gout. Aust Ann Med 12:310 –324, 1963 MORGAN JM, HARTLEY MW, MILLER RE: Nephropathy in chronic lead poisoning. Arch Int Med 118:17–29, 1966 BALL GV, MORGAN JM: Chronic lead ingestion and gout. South Med J 61:21–24, 1968 WEEDEN RP, MAESKA JK, WEINER B, LIPAT GA, LYONS MM, VITALE LF, JOSELOW MM: Occupational lead nephropathy. Am J Med 59:630 – 641, 1975 WEDEEN RP, MALLIK DK, BATUMAN V: Detection and treatment of occupational lead nephropathy. Arch Intern Med 139:53–57, 1979 PINTO DE ALMEIDA AR, CARVALHO FM, SPINOLA AG, ROCHA H: Renal dysfunction in Brazilian lead workers. Am J Nephrol 7:455– 458, 1987 STAESSEN JA, LAUWERYS RR, BUCHET JP, RPMDAO D, VANRENTERGEM Y, AMERY A: Impairmant of renal function with increasing blood lead concentrations in the general population. N Engl J Med 327:151–156, 1992 KIM R, ROTNITZKY A, SPARROW D, WEISS ST, WAGNER C, HU H: A 94. 95. 96. 97. 98. 99. 100. 101. 102. 103. 104. 105. 106. 107. 108. 109. 110. 111. 112. 113. 114. 115. 116. 117. 118. 119. longitudenal study of low-level lead exposure and impairment of renal function. The normative age study. JAMA 275:1177–1181, 1996 HU H: A 50-year follow-up of childhood plumbism. Hypertension, renal function, and hemoglobin levels among survivors. Am J Dis Child 145:681– 687, 1991 MOEL DI, SACHS HK: Renal function 17 to 23 years after chelation therapy for childhood plumbism. Kidney Int 42:1226 –1231, 1992 VANDEVYVER FL, D’HAESE PC, VISSER WJ, ELSEVIERS MM, FNIPPENBERG LL, LAMBERTS LV, WEDEEN RP, DE BROE MS: Bone lead in dialysis patients. Kidney Int 33:601– 607, 1988 INGLIS JA, HENDERSON DA, EMMERSON BT: The pathology and pathogenesis of chronic lead nephropathy occurring in Queensland. J Pathol 124:65–76, 1978 THOMAS BK, THOMAS BW: Chronic renal failure with gout: A marker of chronic lead poisoning. Kidney Int 26:319 –323, 1984 CRASWELL PW, BOYLE JP, HEAZLEWOOD VJ, BADDELEY H, LLOYD HM, THOMAS BK, THOMAS BW; Chronic renal failure with gout: A marker of chronic lead poisoning. Kidney Int 26:319 –323, 1984 BERGER L, YU T-F: Renal function in gout, IV. An analysis of 524 gouty subjects including long-term follow-up studies. Am J Med 59:630 – 641, 1975 YU T-F, BERGER L, DORPH DJ, SMITH H: Renal function in gout. V. Factors influencing renal hemodynamics. Am J Med 67:766 –771, 1979 BATUMAN V, MAESAKA JK, HADDAD B, TEPPER E, LANDY E, WEDEEN RP: Role of lead in gouty nephropathy. N Engl J Med 304:520 –523, 1981 KIM R, ARO A, ROTNIZKY A, AMARASIRWADENA C, HU H: K x-ray fluorescence measurements of bone lead concentration: Analysis of low-level data. Phys Med Biol 40:1475–1485, 1995 SOKAS RK, BESARAB A, MCDIARMID MA, SHAPIRO IM, BLOCH P: Sensitivity of in vivo x-ray fluorescence determination of skeletal lead stores. Arch Environ Health 45:268 –272, 1990 BATUMAN V, LANDY E, MAESAKA JK, WEDEEN RP: Contribution of lead to hypertension with renal impairment. N Engl J Med 309:17–21, 1983 BATUMAN V: Lead nephropathy, gout, and hypertension. Am J Med Sci 305:241–247, 1993 HARLAN WR, LANDIS JR, SCHMOUDER RL: The relationship of blood lead and blood pressure in adolescent and adult US population. JAMA 253:530 –534, 1985 PIRKLE JL, SCHWARTZ, J, LANDIS JR, HARLAN W: The relationship between blood lead and blood pressure and its cardiovascular risk implications. Am J Epidemiol 121:246 –258, 1985 SCHWARTZ J: Lead, blood pressure, and cardiovascular disease in men and women. Env Hlth Per 91:17–32, 1991 HU H, ARO A, PAYTON M, KORRICK S, SPARROW D, WEISS ST, ROTNITZKY A: The relationship of bone and blood lead to hypertension. The normative aging study. JAMA 275:1171–1176, 1996 GONZALEZ J, WERK EE, THRASHER K, BEHAR R, LOADHOLT CG: Renin aldosterone system and potassium levels in chronic lead intoxication. So Med J 72:433– 436, 1979 VICTERY W, VANDER AJ, SHULAK JM, SCHOEPS P, JULIUS S: Lead, hypertension and the renin-angiotension system in rats. J Lab Clin Med 99:354 –362, 1982 FLEISCHER N, MOUW DR, VANDER AJ: Chronic effects of lead on renin and renal sodium excretion. J Lab Clin Med 95:759 –769, 1980 BATUMAN V, DREISBACH A, CHUN E, NAUMOFF M: Lead increases red cell sodium-lithium countertransport. Am J Kidney Dis 14:200 – 203, 1989 BALDWIN DS, LEVINE BB, MCCLUSKY RT, GALLO GR: Renal failure and interstitial nephritis due to penicilline and methicilline. N Engl J Med 279:1245–1252, 1968 CHAZAN JA, GARELLA S, ESPARZA A: Acute interstitial nephritis. A distinct clinicopathological entity. Nephron 9:10 –26, 1972 GALPIN JE, SCHINABERGER JH, STANLEY TM, BLUMENKRANTZ MJ, BAYER AS, FRIEDMAN GS, MONTGOMERIE JZ, GUZE LB, COBURN JW: Acute tubulointerstitial nephritis due to methicilline. Am J Med 65:756 –765, 1978 VAN YPERSELE DE STRIHOU C: Acute allergic interstitial nephritis. Kidney Int 16:751–765, 1979 LINTON A, CLARK WF, DRIEDGER AA, TURNBULL I, LINDSEY RM: Rastegar and Kashgarian: Tubulointerstitial nephritis 120. 121. 122. 123. 124. 125. 126. 127. 128. 129. 130. 131. 132. 133. 134. Acute interstitial nephritis due to drugs. Review of literature with a report of none cases. Ann Intern Med 93:735–741, 1980 BRENTJENS J, NOBEL AG: Immunologically mediated lesions of kidney tubules and interstitium in laboratory animals and in man. Semin Immunopathol 5:357–378, 1982 BAUM M, PIEL CF, GOODMAN JR: Antobiotic-associated interstitial nephritis and nephrotic syndrome. Am J Nephrol 6:149 –151, 1986 CAMERON JS: Allergic insterstitial nephritis’ clinical features and pathogenesis. Q J Med 66:97–115, 1988 BUYSEN JG, HOUTHOFF HJ, KREDIET RT, ARISZ L: Acute interstitial nephritis; a clinical and morphological study in 27 patients. Nephrol Dial Transplant 5:94 –99, 1990 GREISING J, TRACHTMAN H, GAUTHIER B, VALDERRAMA E: Acute interstitial nephritis in adolescents and young adults. Child Nephrol Urol 10:189 –195, 1990 LABERKE H-G, BOHLE A: Acute interstitial nephritis: Correlation between clinical and morphological findings. Clin Nephrol 14:263– 273, 1980 RICHET G, SRAER JD, KOURILSBY O, KANFER A, MIGNON F, WITHWORTH J, MOREL-MAROGER L: La ponction biopsy renale dans les insuffisances renales aiguees. Ann Med Interne (Paris) 129:445– 447, 1978 TOTO RD: Review: Acute interstitial nephitis. Am J Med Sci 299: 392– 410, 1990 BENDER WL, WHELTON A, BESCHORNERWE, DARWISH MO, HALL CRAGGS M, SOLEZ K: Interstitial nephritis, proteinuria, and renal failure caused by nonsteroidal anti-inflammatory drugs. Immunologic characterization of inflammatory infilterate. Am J Med 76: 1006 –1012, 1984 BRUNATI C, BRANDO B, CONFALONIERI R, BELLI LS, LAVAGNI MG, MINETTI L: Immunophenotyping of mononuclear cell infilterate associated with renal disease. Clin Nephrol 26:15–20, 1986 CHOW JR, HATLEY B, JAGGER C, DILLY SA: ICAM-1 expression in renal disease. J Clin Pathol 45:880 – 884, 1992 BOUCHER A, DROZ D, ADAFER E, NOEL LH: Characterization of mononuclear cell subsets in renal cellular interstitial infilterates. Kidney Int 29:1043–1049, 1986 KASHGAIAN M: Lupus nephritis: Lessons from the pathology laboratory. Kidney Int 45:928 –938, 1994 MAGIL AB, TYLER M: Tubulo-interstitial disease in lupus nephritis. A morphologic study. Histopathology 8:81– 87, 1984 HAWKINS EP, BERRY PL, SILVA FG: Acute tubulointerstitial nephritis in children: Clinical, morphologic, and lectin studies. A report of Southwest Pediatric Nephrology Study Group. Am J Kidney Dis 14:466 – 471, 1989 327 135. DORBIN RS, VERNIER RL, FISH AL: acute eosinophilic interstitial nephritis and renal failure with bone marrow lymph node granulomas and anterior uveitis, a new syndrome. Am J Med 59:325–333, 1975 136. VANHAESEBROUCK P, CARTON D, DE BEL C, PRAET M, PROESMANS W: Acute tubulo-interstitial nephritis and uveitis syndrome (TINU syndrome). Nephron 40:418 – 422, 1985 137. CACOUB PG, DERTAY G, LE HOANG P, BAUMELOU A, BEAUFILS H, DE GRECO F, ROUSSELI F, JOUNNEAU C, JACOBS C: Idiopathic acute interstitial nephritis associated with anterior uveitis in adults (see comments). Clin Nephrol 31:307–310, 1989 138. CORWIN HL, KORBET SM, SCHWARTZ MM: Clinical correlates of eosinophiluria. Arch Intern Med 145:1097–1099, 1985 139. NOLAN RN, ANGERS MS, KELLEHER SP: Eosinophiluria — A new method of detection and definition of the clinical spectrum. N Engl J Med 315:1516 –1519, 1986 140. BRADEN GL, GERMAIN MJ, FITZGIBBON JP: Impaired potassium and magnesium homeostasis in acute tubulointerstitial nephritis. Nephron 41:273–278, 1985 141. BREZIN JH, KATZ SM, SCHWARTZ AB, CHINITZ JL: Reversible renal failure and nephrotic syndrome associated with nonsteroidal antiinflammatory drugs. N Engl J Med 301:1271–1273, 1979 142. NEUGARTEN J, GALLO GR, BALDWIN DS: Rifampin induced nephrotic syndrome and acute interstitial nephritis. Am J Nephrol 3:38 – 42, 1983 143. RUFFING KA, HOPPES P, BLEND D, CUGINO A, JARJOURA D, WHITTIER FC: Eosinophil in the urine revisited. Clin Nephrol 41:163–166, 1994 144. LINTON AL: Gallium scintingraphy in the diagnosis of acute renal disease. Clin Nephrol 24:312–315, 1986 145. KIDA H, ABE T, TOMOSUGI N, KOSHINO Y, YOKOYAMA H, HATTORI N: Prediction of the long-term outcome in acute interstitial nephritis. Clin Nephrol 22:55– 60, 1984 146. PUSEY CD, SALTISSI D, BLOODWORTH L, RAINFORD DJ, CHRISTIE JL: Drug associated acute interstitial nephritis: Clinical and pathological features and the response to high dose steroid therapy. Quart J Med 52:194 –211, 1983 147. VANHERWEGHEM JL, DEPIERREUX M, TIELMANS C, ABRAMOWICZ D, DRATWA M, JADOUL M, RICHARS C, VANDERVELDE D, VERBELEN D, VANHAELEN-FASSTRE R, VANHEALEN M: Rapidly progressive interstitial renal fibrosis in young women: Association with slimming regimen including Chinese herbs. Lancet 341:387– 391, 1993