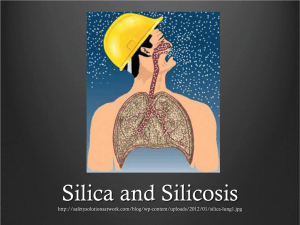
Poverty & occupation health: Silicosis Created: 06 February 2012 Silicosis – a Hidden, Lethal Weapon Targeting Mine Workers Silicosis is a disease found in workers in industry – in factories and mines with a lot of dust. Such facilities are found in many pre-industrial countries, and are often tucked away out of sight. Silicosis is caused by dust-sized particles of silicon getting into the lungs, day after day. In Myanmar it is associated especially with mines, with workers active below ground, working at from ten to over a thousand feet beneath the surface. There, air quality is poor even before work starts. Workers drill the stone to make holes for the sticks of dynamite used to blow up big chunks of stone. Drilling creates dust, and breathing is difficult, unless the mine owners install a proper ventilation or cleaning system. For example, some drilling machines spray water on the dust so that is cleansed from the air. Alternatively, workers can wear masks; but in poor countries these are usually ordinary surgical masks. When drilling starts, the dust settles on the surgical mask, preventing normal breathing, so workers take them off. Many people with silicosis show no symptoms for years. Symptoms of silicosis start with coughing. X-rays are used to identify the disease and show clearly a dark colour around the lungs. This is often interpreted as tuberculosis (TB) with health staff prescribing the appropriate medicines. But when a silicosis patient takes tablets for TB, it worsens the illness and patients may die within six months after taken them. Mineworkers in Myanmar call the symptoms “gun disease” while the drilling machine is called the ”gun”… If too many people die, if their colleagues recognize the problem and try to avoid the job of drilling, the mine owners then offer a bonus (sometimes double their wages) if they continue drilling. The disease progresses even when exposure stops. The patients die within one or two years after the appearance of symptoms. (refs. 6 & 7) Silicosis is one of the oldest occupational health problems and according to WHO still kills thousands of workers every year in every corner of the world (ref. 1). From 1991 to 1995 China reported over 24,000 deaths each year. Thailand has nearly seven thousand stone factories with 1.7 million workers. Between 9% to 21% of the workers at any time will have silicosis, depending on the grinding methods used; most of them do not show symptoms but they are none the less sick (ref. 3). Silicosis is a global disease rooted in the social, political and developmental situation of each nation. It is disappearing in the North – the USA in 1999 reported only 1,877 deaths. Safety precautions in the workplace have made the difference. But in the South it continues. Sufferers of silicosis are mostly lower-level workers. Most of them are poor and may are migrant, with low levels of education. But they are of the age to have young families. They are ignorant about their rights or how to organise protection in the work place. Although trade unions are vital in this process, the price paid for improving conditions is high. According to an ILO report, two hundred trade unionists are murdered every year across the world (ref. 8). Control of this disease is affected by the legislative system. Silicosis needs stricter legislation. It is more serious wherever the following factors are weak or missing – labour laws, investigative structures in departments of Health & Labour, safety procedures at the workplace, and the control of bribery between business owners and the authorities. Silicosis affects men who have little control over the circumstances of the workplace. A country's economic strength is its workforce and it is puzzling that a disease which removes such a number of male workers continues to be ignored. It is a concern mainly to the owners of businesses. Some of these business people are unaware of the severity of the disease; some may know but are negligent. Profit outweighs the safety of their workers. Silicosis is preventable by the supply and use of expensive technology which will reduce the profits of owners and shareholders. Intervention in a specific mine The writer participated in a health development project for two years in Myanmar. Mines can be found in many places in Myanmar extracting valuable minerals such as gold, gems, and jade. When the writer was working in the mining areas four years ago, he visited gold and ruby mines. He found that the workers had no proper preventive materials to shield them from the dust. They received only basic hospital masks of thin paper and cloth which do not filter dust properly. Additionally the drilling machines often do not have the water pumping accessories called wet drilling systems because of the cost and the need for additional apparatus. When the workers wear the hospital masks in deep mines, they cannot breath normally; the dust covers the masks especially during drilling. As a consequence, they take the masks off and continue their work without them. And the dust is breathed in. The writer was involved in the first-aid training conducted in the mining area for the mine workers by an NGO (Project Inform). The training covered occupational health problems with the aim of prevention. As a result of the training, some mine managers and mine owners were willing to provide the proper industrial masks for their workers. In Myanmar at that time, these kinds of industrial masks were not popular, although there are many mines in Myanmar and it is difficult to find proper masks in the market. This lack of popularity may be one of the reasons why other mine owners do not provide these masks. Although the writer did not interview workers suffering from silicosis at the time, he did so later. The workers had been working at drilling in the mines and had complained of symptoms that were diagnised as TB. Most of them got no compensation; some of them received no treatment at all from the health facility in the mine. The majority got some treatment at a township hospital nearby. They were treated as TB patients because of the similarity of the symptoms and the TB-like shadows on the X-rays. So they got anti-TB tablets. When they took them, their symptoms become worse and they died three or four months later. It is not known whether the mine owner or managers are still providing their workers with effective masks today; the writer was not able to return. He has met people still working in those areas who say that the situation is not much improved There are many ways in which the Silicosis issue in Myanmar can be handled. Firstly, labour law and safety procedures must be developed or activated at the workplace especially where drilling machines are used. Workplace inspection should be conducted regularly by the relevant health department inspectors who should also check whether the proper materials and tools are being used. Effective machinery and preventive materials must be in place and need to be checked regularly. The mine workers need to be educated about all relevant occupational health issues. Treatment for Silicosis should be upgraded and people need to be referred to a center with higher levels of treatment if necessary. A pension and/or a relevant compensation procedure should be established for workers who suffer from Silicosis. In conclusion, Silicosis is an incurable lung disease which progressively worsens. The sufferers from Silicosis are mostly poor, often migrant workers, with lower levels of education or knowledge. They also often have young families. There are problems of apathy in the minds of owners and managers. Weak or inactive labour laws worsen the situation. Although there are some improvements for compensation for Silicosis sufferers in Africa (Mining Weekly, 15 November 2004, 2013: Deadline for breaking silicosis grip, www.smianalytical.co.za), there is still a long way to go to overcome the problem of silicosis in workplaces around the world. References: 1. World Health Organization 2. International Labor Organization 3. Journal of Mineral dusts and prevention of silicosis vol 4; No.2, September 1997; “Clinical cases of silicosis in Thailand”; P. Youngchaiyud & A. Nana 4. Project Inform 5. US National Library of medicine and National Institute of health 6. www.unaids.org/documents/20101123_FS_Asia_em_en.pdf 7. www.safaids.net/node/1042 8. www.gmhazards.org.uk/ILOfigs.doc Source: https://www.networklearning.org/ngo-fields/poverty-income-generation/197-poverty-occupationhealth-silicosis Written by Aung Ko Ko (naturekoko@gmail.com)