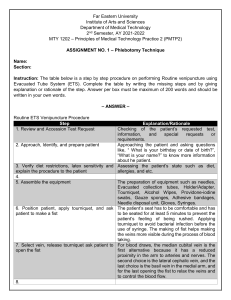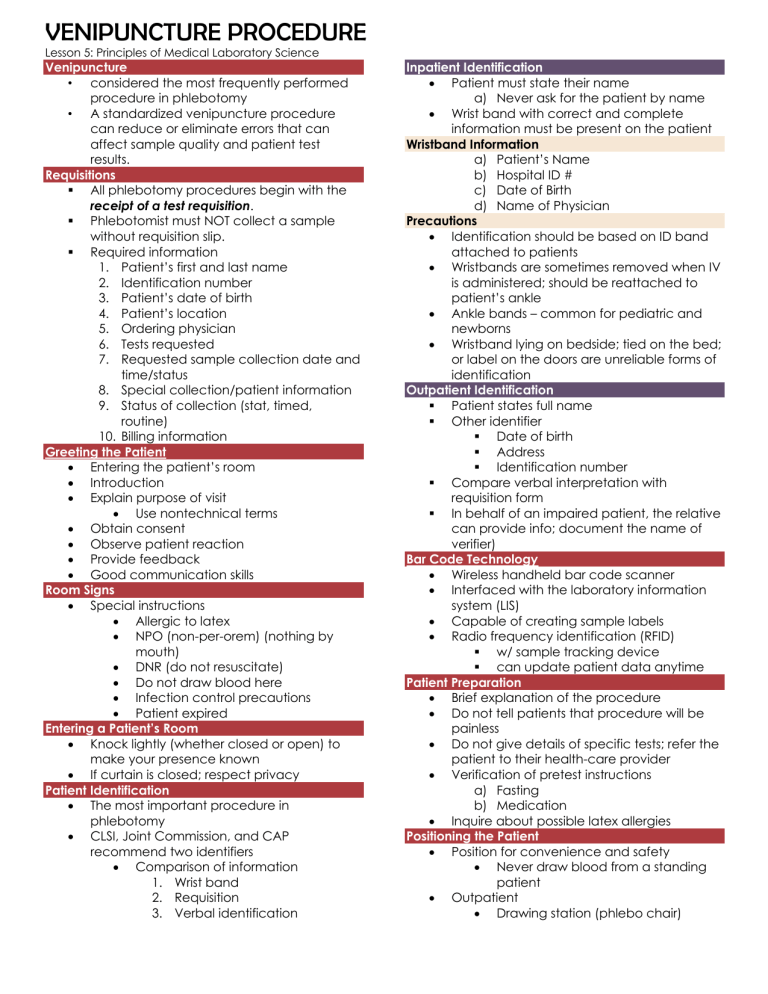
VENIPUNCTURE PROCEDURE Lesson 5: Principles of Medical Laboratory Science Venipuncture • considered the most frequently performed procedure in phlebotomy • A standardized venipuncture procedure can reduce or eliminate errors that can affect sample quality and patient test results. Requisitions § All phlebotomy procedures begin with the receipt of a test requisition. § Phlebotomist must NOT collect a sample without requisition slip. § Required information 1. Patient’s first and last name 2. Identification number 3. Patient’s date of birth 4. Patient’s location 5. Ordering physician 6. Tests requested 7. Requested sample collection date and time/status 8. Special collection/patient information 9. Status of collection (stat, timed, routine) 10. Billing information Greeting the Patient • Entering the patient’s room • Introduction • Explain purpose of visit • Use nontechnical terms • Obtain consent • Observe patient reaction • Provide feedback • Good communication skills Room Signs • Special instructions • Allergic to latex • NPO (non-per-orem) (nothing by mouth) • DNR (do not resuscitate) • Do not draw blood here • Infection control precautions • Patient expired Entering a Patient’s Room • Knock lightly (whether closed or open) to make your presence known • If curtain is closed; respect privacy Patient Identification • The most important procedure in phlebotomy • CLSI, Joint Commission, and CAP recommend two identifiers • Comparison of information 1. Wrist band 2. Requisition 3. Verbal identification Inpatient Identification • Patient must state their name a) Never ask for the patient by name • Wrist band with correct and complete information must be present on the patient Wristband Information a) Patient’s Name b) Hospital ID # c) Date of Birth d) Name of Physician Precautions • Identification should be based on ID band attached to patients • Wristbands are sometimes removed when IV is administered; should be reattached to patient’s ankle • Ankle bands – common for pediatric and newborns • Wristband lying on bedside; tied on the bed; or label on the doors are unreliable forms of identification Outpatient Identification § Patient states full name § Other identifier § Date of birth § Address § Identification number § Compare verbal interpretation with requisition form § In behalf of an impaired patient, the relative can provide info; document the name of verifier) Bar Code Technology • Wireless handheld bar code scanner • Interfaced with the laboratory information system (LIS) • Capable of creating sample labels • Radio frequency identification (RFID) § w/ sample tracking device § can update patient data anytime Patient Preparation • Brief explanation of the procedure • Do not tell patients that procedure will be painless • Do not give details of specific tests; refer the patient to their health-care provider • Verification of pretest instructions a) Fasting b) Medication • Inquire about possible latex allergies Positioning the Patient • Position for convenience and safety • Never draw blood from a standing patient • Outpatient • Drawing station (phlebo chair) VENIPUNCTURE PROCEDURE Lesson 5: Principles of Medical Laboratory Science Arm fully supported and angled downward (allow tubes to fill from bottom up) § This will prevent reflux or anticoagulant carryover between tubes • Use recliner/reclining chair for patients with a history of syncope • Ask patient to make a fist (the other hand can be used for support- placed behind elbow to make the veins easier to locate) • Be alert with patient’s condition during the process • For hospitalized patients; one can place pillow or towel under patient’s arm • If bed rails are lowered return them to the raised position after phlebo • Patient’s should remove anything in the mouth (food, drinks, gums, or thermometer) before veni; they may cause choking. Equipment Selection • Necessary equipment is selected and placed close to the patient • No blood collection tray placed on the bed • Accessible on the same side as your free hand a) Eliminates “reaching across” • Reexamine the requisition • Select appropriate supplies based on patient age and condition a) Correct type and number of evacuated tubes b) Appropriate venipuncture needle and holder c) Antiseptic; Bandaging; Tourniquet • Inspect supplies (i.e., expiration date) • Place tubes in “order of draw” • Keep extra tubes handy Wash Hands and Apply Gloves • Perform in front of patient • Gloves are changed between each patient Tourniquet Application • Impedes venous flow § Allowing accumulation of blood to veins § Easier to locate veins • Allows arterial flow • Maximum allowable duration of tourniquet application is 1 minute • Complications can arise with prolonged application • When used during vein selection; tourniquet must be released and REAPPLIED ONLY AFTER 2 MINUTES • Tourniquet is placed 3 to 4 inches above the puncture site • A tourniquet applied near the venipuncture site may cause vein to collapse • The loop formed should face downward • Free end should be away from the venipuncture area to allow easy removal • Tourniquets should not be applied too tight: § Uncomfortable § Obstruct blood flow to the area • Signs of too tight tourniquet application: § Appearance of small red patches called petechiae § Blanching of the skin around the tourniquet § Inability to feel radial pulse Site Selection § Major veins: antecubital fossa § Median cubital vein § Cephalic vein § Basilic vein “H” and “M” pattern § “H” pattern: (70%) § Median cubital vein; Cephalic vein; Basilic vein § “M” pattern: § cephalic vein; median cephalic median basilic and basilic vein § Other sites § Lower arm veins § Wrist veins § CLSI discourages the use of veins in the underside of the wrist because of the chance to accidentally puncture arteries, nerves or tendons § Hand veins (use butterfly set) Median Cubital Vein • Vein of choice for venipuncture • Located near the center of the antecubital fossa. • It is the most preferred vein because it is: a) large, b) close to the surface of the skin, c) stationary and sufficiently anchored to the tissue for a successful venipuncture • least painful to puncture (less nerve endings) • least likely to bruise § VENIPUNCTURE PROCEDURE Lesson 5: Principles of Medical Laboratory Science Cephalic Vein • Located in the thumb side; • Second-choice vein • More difficult to locate • Fairly well anchored (tendency to move) • Often the only vein that can be felt in obese patients • Easily bruises • Possibility of blood spurt (close to the surface) a) Remedy: lower the angle; use 15 degree angle Basilic Vein • located on the medial side (inner edge) of the antecubital fossa; • last-choice vein; • large and easy to feel; • least firmly anchored; rolls easily; • increase risk of puncturing median nerve and brachial artery • CLSI does not recommend the use of this vein (last resort) • easily bruises (may form hematoma) Locating Suitable Veins • Place tourniquet • Ask patient to close fist • Avoid clenching or pumping of fist • Can increase blood potassium levels “PSEUDOHYPERKALEMIA” PROCEDURE FOR VEIN PALPATION • Veins are located by sight and touch (palpation) • Palpate and trace the path of veins (both vertical and horizontal motion) with the index finger of the non-dominant hand. J Veins feel spongy; resilient; tube/cordlike J Arteries pulsate J Do not use thumb to palpate veins (it has pulse) • Tip: Patients have more prominent veins in the dominant arm. • If superficial veins are not readily apparent you can: J tap the site with index and middle finger J apply a warm, damp washcloth to the site for 5 minutes, or J lower the extremity over the bedside to allow the veins to fill. Cleansing the Site § Antiseptic of choice: 70% isopropyl alcohol (routine) § Manner of Disinfection: CIRCULAR OUTWARD MOTION • Widening concentric circle inside to outside • For dirty skin, repeat the procedure using a new alcohol pad. • Drying time o 30 SECONDS TO 60 SECONDS o Allows for maximum bacteriostatic action o “Drying time is Dying Time” • Failure to completely air dry the site will cause: o Painful; stinging sensation o Hemolysis of sample • Avoid recontamination of site o Do not blow on the site; o Do not fan the area; o Do not dry the area with non-sterile gauze o Do not touch the site again after disinfection • For routine venipuncture, the antiseptic of choice is 70% isopropyl alcohol only. • Never use iodine because it can affect the results of several tests. • Povidone/Tincture of iodine is only used for: o blood culture collection o blood donation Assembly of Puncture Equipment • While alcohol is drying; make a final survey of the things needed • Prepare the syringe; § Needle bore should be in line with the graduations in the barrel • Assemble the needle and the holder properly • Examine defective and expired tubes; have extra tubes at hand Performing the Venipuncture Reapplying tourniquet Confirm puncture site § If necessary; cleanse the gloved palpating finger for additional vein palpation Examine the needle; position the needle “bevel-up” Anchoring the vein § Use non-dominant thumb § One can stretch skin if needed to anchor the needle to the veins Inserting needle § Bevel up § Recommended angle: 15 to 30 degrees § Should be done smoothly § Entering the vein slowly is more painful to the patient; § May cause a spurt of blood at the venipuncture site VENIPUNCTURE PROCEDURE Lesson 5: Principles of Medical Laboratory Science Filling the Tubes § Use thumb to push the tubes § Index and middle fingers can be used to grasp the flared ends of the holder § Tourniquet and fist must be released in one minute time period or until the last tube is filled § TOURNIQUET IS REMOVED FIRST BEFORE REMOVING THE NEEDLE. § The hand holding the needle assembly must remain braced on the patients’ arm to prevent pushing through or pulling out of the needle to the vein. § Tubes must be held in downward angle to prevent reflux § Follow the correct CLSI order of draw § Gentle inversion of tube once filled in the appropriate mark must be performed immediately to avoid clotting of samples and must be done as soon as the tubes are removed § Remove the last evacuated tube first; § Remove the tourniquet § Remove the needle § Failure to remove the tube before removing the needle may cause blood to drip from the end of the needle and may cause contamination of patient’s clothes Technical Tips: § Avoid vigorous mixing of samples because it may cause hemolysis; § Poor mixing may cause clot formation and yield erroneous results. § Allow tubes to fill until the vacuum is exhausted to ensure correct blood is to anticoagulant ratio. Correct Number of Inversions Red (Glass) Light Blue 0x 3-4 x Red (plastic; with clot activator ) Gold/Tiger Top 5x Light green ; Green; Lavender; Pink; Gray; Tan Yellow; Orange; Royal Blue 8x Removal of the needle: • Remove tourniquet first before removing the needle § If not performed correctly; it may cause blood to ooze out from the site and may cause Hematoma which later on can form a bruise • Activate needle safety device if available • Place gauze on venipuncture site • Withdraw the needle in a smooth, swift motion • Apply pressure to site as soon as needle is withdrawn. • Do not apply pressure while the needle is still in the vein. • To avoid hematoma; pressure must be applied until bleeding has stopped (about 2-3 minutes). • Arms must be in a raised; outstretched position. • Bending the elbow will allow blood to leak more easily to tissue and thus can cause hematoma. • A capable patient can be asked to apply pressure to the site. Disposal of the needle: • Upon completion of venipuncture; needles must be properly disposed in an acceptable sharps container. • Under no circumstance should the needle be bent; cut; placed on bed or manually recapped. Labeling of Tubes • Post-collection • Written label • Computer-generated label • Information on label 1. Patients name 2. Patients ID number 3. Date and time of collection 4. Phlebotomist’s initials • Additional information can be present in computer-generated labels. • Inpatient: § After labeling the tubes; compare the label with the patient’s arm band • Outpatient: § Verify the name by showing tube label § Asking the patient to confirm the name on the label • Proper handling of samples must be observed at all times. VENIPUNCTURE PROCEDURE Lesson 5: Principles of Medical Laboratory Science Bandaging the Patient § Bleeding of the venipuncture site lasts for about 5 minutes. § Before applying adhesives; check if bleeding has completely stopped. § Paper tape can be used for those allergic to adhesives. § Instruct patient to remove bandage after an hour and avoid carrying heavy objects during that period. Disposal of Used Supplies § Contaminated supplies (e.g. alcohol pads and gauze -> biohazard bin § Needle caps; paper -> regular waste container § Lastly; remove gloves -> biohazard § Perform hand washing Leaving the patient § Return bed rails to original position § If patients have been fasting and no more procedures are scheduled, they should be instructed to eat. § Before calling the next patient, clean the area first with surface disinfectant. § Say thank you for patient’s cooperation. Completing the Venipuncture Procedure • Transport sample as soon as possible. • Gel-separation tubes must be placed in upright position to facilitate clotting and prevent hemolysis. • CLSI recommends centrifugation and separation of cells from plasma or serum within 2 hours. • Ideally, the samples must reach the lab 45 minutes after blood collection and must be centrifuged on arrival. • Tests most commonly affected by improper processing: o Glucose o Potassium o Coagulation tests • Glycolysis cause false lower glucose values • Hemolysis cause elevated potassium levels • Coagulation factors are destroyed at room temperature for extended periods of time. Drawing Blood from Special Population Pediatric Puncture • Special attention is necessary involving children below two years old • Risk of damage could be permanent if proper procedure is not followed • Risk of anemia is possible since the volume of blood is smaller • The phlebotomist should exhibit warm and caring approach Eutectic mixture of local anesthetics (EMLA)- used for pain interventions; comes in cream or foam Geriatric Puncture • Special attention is necessary involving elderly patients because they may have special conditions • Elderly have thinner skin and smaller muscles which cause vein to roll easily • Healthcare institution has to consider safety issues like space requirement for walkers and wheelchairs and maintenance of non- slip clutter- free floors Long- term Care Patients 1. Dialysis Patients- use the dorsum of the hand to preserve the veins of the arms for hemodialysis access. 2. Long- term care Patients can be assistedliving with the help of relatives 3. Home- care Patients need medical attention and assistance from healthcare professionals from time to time. Phlebotomists are independent, flexible and can carry all necessary equipment with them during house calls. 4. Hospice Patients need end-of-life care and mostly have a prognosis six months or less. 10 COMMANDMENTS OF PHLEBOTOMIST 1. Thou shall protect thyself from injury. 2. Thou shall identify the patients correctly. 3. Thou shall puncture the skin at about a fifteen degree angle. 4. Thou shall glorify the median cubital vein. 5. Thou shall invert tubes with additives immediately after collection. 6. Thou shall collect specimens only from an acceptable site. 7. Thou shall label specimens at the bedside. 8. Thou shall stretch the skin at the puncture site. 9. Thou shall know when to quit. 10. Thou shall treat all patients as if they were family.