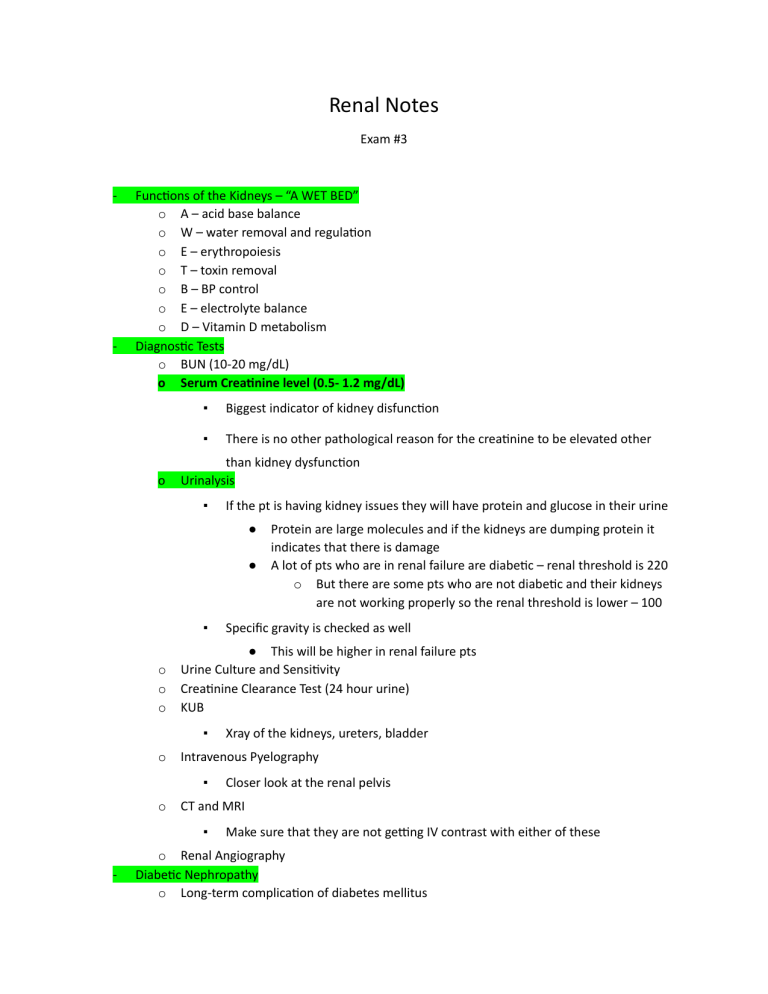
Renal Notes Exam #3 - - Func ons of the Kidneys – “A WET BED” o A – acid base balance o W – water removal and regula on o E – erythropoiesis o T – toxin removal o B – BP control o E – electrolyte balance o D – Vitamin D metabolism Diagnos c Tests o BUN (10-20 mg/dL) o Serum Crea nine level (0.5- 1.2 mg/dL) o ▪ Biggest indicator of kidney disfunc on ▪ There is no other pathological reason for the crea nine to be elevated other than kidney dysfunc on Urinalysis ▪ If the pt is having kidney issues they will have protein and glucose in their urine ● ● ▪ o o o Closer look at the renal pelvis CT and MRI ▪ - Xray of the kidneys, ureters, bladder Intravenous Pyelography ▪ o Specific gravity is checked as well ● This will be higher in renal failure pts Urine Culture and Sensi vity Crea nine Clearance Test (24 hour urine) KUB ▪ o Protein are large molecules and if the kidneys are dumping protein it indicates that there is damage A lot of pts who are in renal failure are diabe c – renal threshold is 220 o But there are some pts who are not diabe c and their kidneys are not working properly so the renal threshold is lower – 100 Make sure that they are not ge ng IV contrast with either of these o Renal Angiography Diabe c Nephropathy o Long-term complica on of diabetes mellitus o Most common cause of renal failure ▪ o o Atherosclero c changes decrease blood to kidney Need smaller doses of insulin as progresses ▪ - most pa ents on dialysis are diabe c r/t kidneys unable to breakdown insulin and excrete it o Chronic renal failure develops Acute Kidney Injury o Old name: Acute renal failure o Sudden loss of kidney func on ▪ o Waste products accumulate ▪ o which leads to azotemia Oliguria ▪ o o rapid onset of hours to days w/output less than 20 ml/hr (norm 30ml/hr) or 400 ml/day May recover-usually reversible Pathophysiology ▪ Reduced blood flow to the kidney from hypovolemia, hypotension, reduced cardiac output & heart failure, obstruc on of the kidney or lower urinary tract from a tumor or bilateral obstruc on of the renal arteries or veins ▪ o Leads to decreased GFR, increased BUN & Crea nine and oliguria Causes ▪ 3 categories lead to acute renal failure ● Prerenal Failure (before the kidneys) MAP<60 o **Remember – this is a problem that is occurring BEFORE it even gets to the kidneys ▪ A low MAP (decreased blood supply) Nephrons in the kidneys are not ge ng good perfusion and this causes the GFR to drop Decreased blood supply to kidneys-low BP in renal artery ● o ▪ when nephrons receive inadequate blood supply they are unable to make urine and waste is not adequately removed o Causes ▪ Hypovolemia ▪ Decreased cardiac output (Shock & Heart failure) ● ▪ Decreased peripheral resistance - vasodila on ▪ Renal vascular obstruc on Intra-renal Failure (w/in the kidneys) o Damage to nephrons from prolonged renal ischemia ▪ Myoglobinuria ● ▪ o Transfusion reac ons Nephrotoxic Injury (more common cause of intra-renal failure) ▪ An bio cs ● ● o o o Vancomycin Gentamicin ▪ NSAIDS ▪ Contrast dye Infec ous Processes ▪ Acute pyelonephri s ▪ Acute glomerulonephri s Autoimmune disorders ▪ ● Can lead to rhabdomyolysis Lupus Post Renal Failure (a er the kidneys) o Obstruc on of urinary collec ng system o Blocks flow or urine from body (Bet/kidney & Urethral meatus) ▪ Urethral obstruc on ▪ Prosta c hypertension ▪ Bladder Cancer ▪ Ureteral obstruc on ▪ Calculi ▪ Abdominal tumor ▪ Spinal Cord disease S/S of AKI ▪ Sudden decrease in urine output (<400 ml in 24 hours) ▪ Anorexia, N/V o ▪ Sudden weight gain ▪ Decrease in LOC ▪ Halitosis ▪ Low BP, Tachycardiac, tachypneic Four Phases of AKI ▪ Ini a on (Onset) Phase ● Starts with ini al insult and ends with oliguria ● Spans several hours to 2 days ● Renal func on begins to deteriorate but renal damage not yet established ● Poten ally reversible during this phase ▪ Oliguric/Anuric Phase ● Increase in serum concentra on of normally excreted products o urea, crea nine, uric acid, K+, Mg ▪ o These will be high in the blood b/c they are normally excreted ● Urine volume lowest ● Lasts 1-3 weeks ● Longer remains in this phase, the greater amount of renal damage ● Uremia and hyperkalemia common during this phase o Watch for dysrhythmias ▪ Diure c Phase ● Renal ssue recovers and repairs itself ● Gradual increase in urine output o GFR is recovering ● May lose large amounts of fluid due to salt and water accumula on leading to dehydra on ▪ Recovery Phase (Convalescent ) ● May take up to 3-12 months ● Laboratory values return to pt’s normal level Medical Management ▪ Objec ves ● ● ▪ Restore normal chemical balance Prevent complica ons un l repair of renal ssue and restora on of renal func on occurs Treat cause ● ● Prerenal o op mizing renal perfusion Postrenal ● ▪ o remove the obstruc on Intrarenal o remove the cause o treat infec on Treatment needs to be suppor ve ● Maintenance of Fluid Balance o Fluid excesses ▪ o Adequate renal blood flow ▪ o IV fluids or transfusions of blood products o Dopamine (low doses) Dietary Management ▪ Adequate energy, protein, and micronutrients to maintain homeostasis ▪ - Diure cs to promote diuresis Caloric requirements met with high carbohydrate meals because carbohydrates have a protein sparing effect ▪ Restrict food and fluids with sodium, potassium and phosphorus Chronic Kidney Disease (CKD) o Defini on ▪ o o o o more months Untreated CKD can result in end stage renal disease Stages based on GFR-normal is 125 ml/min Also called end stage renal disease (ESRD)-Stage 5 CKD Gradual decrease in kidney func on ▪ o o o Umbrella term that describes kidney damage or a decrease in the GFR for 3 or inability to eliminate wastes Irreversible E ology ▪ Diabe c nephropathy ▪ Nephrosclerosis and HTN ▪ Glomerulonephri s ▪ Autoimmune diseases Pathophysiology ▪ Large propor on of nephrons damaged ▪ Progressive disease process ▪ Renal insufficiency: 75% nephrons lost ▪ End-stage: 90% nephrons lost ▪ Uremia: Urea in the blood ● ● ▪ o Uremic frost: frosty appearance of skin caused by wastes coming to skin surface Terminal stage Affects all body systems Assessment and Diagnos c Findings ▪ Fluid accumula on ● ● ▪ Electrolyte imbalances ● ▪ Elevated BUN, crea nine Anuria or oliguria or large vol of urine w/o waste products (rare) Acid-base imbalances ● ● ▪ Mental changes Waste products retained ● ● ▪ Edema HTN Metabolic acidosis o Renal buffering system not working Rapid, deep resp to rid lungs of CO2 to correct acidosis Anemia ● ● Inadequate erythropoie n produc on Dietary deficiencies ▪ Calcium and Phosphorus Imbalance ▪ High magnesium levels ▪ ▪ ▪ ● Avoid antacids ● Anorexia, N/V ● ● Fluid overload Hyperkalemia - Arrhythmias GI CV Respiratory ● ▪ Pulmonary edema Neuromuscular ● Confusion and irritability ▪ Psychosocial ● ▪ Renal ● ● ● ▪ Urine output varies from scant to normal Specific Gravity o varies by cause BUN and serum crea nine levels increase Increase in blood phosphate, decrease in calcium levels ● ● o Decreased concentra on Phosphorus and calcium have a reciprocal rela onship – when one is high the other is low In CKD phosphorus is high, therefore calcium is normally low Medical Management ▪ Emergency Medica ons ● ● ● ● ● IV dextrose and Insulin o Will help bring down high K+ levels 10 % Calcium Gluconate Sodium Polystyrene (Kayexalate) o Binds to K+ and excretes it through BM o Contraindicated in pts w/ a bowel obstruc on or ileus Albuterol o Works similar to insulin – pushes K+ back into the cells o Contraindicated in pts who are tachycardic Bicarbonate o If pt acido c ▪ Maintenance Medica ons ● Calcium & Phosphorus Binders o Calcium ▪ o Given daily to help raise calcium levels Sevelamer (Renagel) ▪ Phosphorous is given when the pt eats b/c there is a lot of phosphorus in foods ● This helps to not raise their phosphorous levels and in turn helps to raise their calcium levels ▪ If the pt is not ea ng they do not need to take this b/c it binds to the phosphorus in foods ▪ ● them An hypertensives o Pts are hypertensive b/c of the fluid reten on o ACE inhibitors are common for renal pts ▪ ● ● Can cause K+ reten on (Monitor) Erythropoie n-Epogen o Pts w/ CKD lack erythropoie n so this helps replace it o Given typically IV on dialysis days o Specific parameters are set by the Dr ▪ ● Milk products and soup have a lot of phosphorus in Make sure to check lab values before administering to avoid clo ng issues! An seizure Agents o Prophylac c o B/c of the toxic build up in the system from CKD pts are more prone to seizures Iron o Indica on – anemia o Don’t give on an empty stomach o Don’t give w/ a phosphorus binder b/c they can prevent the body from absorbing the iron ▪ If ordered together – give phosphorus binder when the pt is ea ng and then give the iron about a half hour to an hour a er they are done ea ng ▪ **Drug therapy always a challenge b/c 2/3 of all drugs or their metabolites are ▪ eliminated by the kidneys Diet ● ● ● ● ● ▪ o High calorie Low protein o unless dialysis – then they can have high protein Low sodium, potassium, phosphorus Increased calcium Vitamins Fluid restric on Nursing Management ▪ Monitor fluid and electrolyte balance ▪ Reduce metabolic rate ▪ Promote pulmonary func on ▪ Prevent infec on ▪ Provide skin care ▪ Provide psychosocial support ▪ Prevent complica ons ● ● ● ● Hyperkalemia Metabolic acidosis Pericardi s Pulmonary edema ● High serum phosphate level Renal Labs Lab Reference Range BUN 10-20 mg/dL Crea nine M: 0.6 – 1.2 mg/dL F: 0.5 – 1.1 mg/dL GFR (glomerular filtra on) >90 mL/min Sodium 136 – 145 mEq/L Calcium 9 – 10.5 mg/dL Potassium 3.5 – 5.0 mEq/L Phosphorous 3.0 – 4.5 mg/dL Magnesium 1.3 – 2.1 mEq/L Urinalysis Specific Gravity 1.00 – 1.04 pH 4.6 – 8 Glucose None Ketones None Protein 0 – 0.8 mg/dL RBC’s 0–2 WBC’s 0–4 Bacteria <1000 colonies/mL Leukocytes None