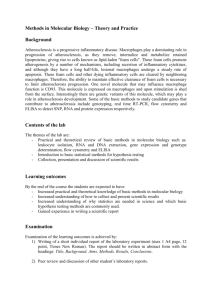
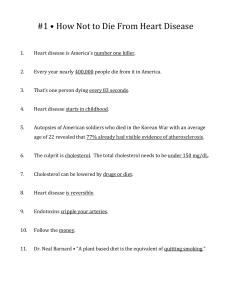
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/230211988 Macrophage Foam Cells Chapter · September 2010 DOI: 10.1002/9780470015902.a0020730 CITATIONS READS 3 3,669 3 authors: Annabel F Valledor Jorge Lloberas University of Barcelona University of Barcelona 63 PUBLICATIONS 3,964 CITATIONS 90 PUBLICATIONS 5,668 CITATIONS SEE PROFILE SEE PROFILE Antonio Celada University of Barcelona 267 PUBLICATIONS 11,259 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: A research study of the intracellular cholesterol metabolism alterations in breast cancer and epithelial thyroid carcinoma: Evaluation of HDL-based therapeutic strategies View project Regulation of immune responses by LXRs View project All content following this page was uploaded by Annabel F Valledor on 27 August 2016. The user has requested enhancement of the downloaded file. Macrophage Foam Cells Advanced article Article Contents Annabel F Valledor, University of Barcelona, Barcelona, Spain Jorge Lloberas, University of Barcelona, Barcelona, Spain Antonio Celada, University of Barcelona, Barcelona, Spain • Introduction • Macrophages • Macrophages and Inflammation • Conversion of Macrophages into Foam Cells Based in part on the previous version of this eLS article ‘Macrophage Foam Cells’ (2010) by Annabel F Valledor, Jorge Lloberas and Antonio Celada. • Macrophages in the Development of Atherosclerotic Lesions • Transcriptional Control to Prevent Foam Cell Formation and the Development of Atherosclerosis • Foam Cells in Other Forms of Chronic Inflammation Online posting date: 16th February 2015 Foam cells are lipid-loaded macrophages that are generated from the massive uptake of modified low-density lipoproteins and the intracytoplasmatic accumulation of cholesteryl esters. Foam cells are present in all stages of atherosclerosis and participate in inflammatory responses and tissue remodelling within the arterial intima. Foam cells can also be generated as a consequence of infection by persistent pathogens, such as Mycobacterium, Chlamydia and Toxoplasma. These pathogens meet nutritional advantages by residing within cells that accumulate lipids. When the immune system is unable to eliminate substances perceived as foreign, it produces a granuloma, composed mostly of macrophages, attempting to wall off the non-self material. This article reviews the processes that lead to the regulation of foam cell formation in atherosclerosis and infection. Introduction In the mid-nineteenth century, Rudolf Virchow postulated that cellular pathology is critical in atherosclerosis (reviewed by Mayerl et al., 2006). However, only in recent years has the inflammatory process leading to atherosclerosis been characterised. Today, we know that foam cells are lipid-laden macrophages present in all stages of atherosclerosis. Foam cells play a major role in the formation of the fatty-streak, the earliest pathological sign of atherosclerosis, and in the progression and pathogenicity eLS subject area: Cell Biology How to cite: Valledor, Annabel F; Lloberas, Jorge; and Celada, Antonio (February 2015) Macrophage Foam Cells. In: eLS. John Wiley & Sons, Ltd: Chichester. DOI: 10.1002/9780470015902.a0020730.pub2 of established atherosclerotic plaques. Thus, foam cells are considered therapeutic targets for the treatment of atherosclerosis (Saha et al., 2009). These cells have also been detected in other forms of chronic inflammation, including septic arthritic lesions and in tissues infected by persistent pathogens such as Mycobacterium, Chlamydia and Toxoplasma (Portugal et al., 2008). Macrophages Macrophages play a critical role in tissue homeostasis and immunity. The use of multicolour fluorescence-activated cell sorting together with adoptive transfer of precursors has helped characterise in vivo differentiation of macrophage populations. Like many other cells in the immune system, blood monocytes and many macrophage subsets originate from pluripotent haematopoietic stem cell within the bone marrow. Successive commitment steps generate macrophage/dendritic cell progenitors that differentiate to monocytes, which then leave the bone marrow and travel through the blood to other tissues in the body (Geissmann et al., 2010). In an adult, the bone marrow releases approximately 5 × 109 monocytes daily and most of these cells are short-lived. Under normal conditions, a few of these monocytes (patrolling monocytes) enter tissues and differentiate into macrophages. Recently, it has been shown that in many tissues (i.e. brain, skin and liver) resident macrophage populations derive from yolk sac precursors that colonise their target tissues during embryogenesis and form stable networks within these tissues by differentiation in situ. Such macrophage populations self-renew in the steady state and do not depend on continuous replacement by the bone marrow (reviewed by Ginhoux and Jung, 2014). Depending on the specific location, resident macrophages are given different names that may be associated with specialised functional activities (e.g. osteoclasts in the bone, alveolar macrophages in the lung, histiocytes in the connective tissue, mesangial cells in the kidney, sinusoidal lining cells in the spleen, microglia in the brain, Kupffer cells in the liver and Langerhans cells in the skin). See also: Macrophages eLS © 2015, John Wiley & Sons, Ltd. www.els.net 1 Macrophage Foam Cells Macrophages are approximately 21 μm in diameter and can be identified by the specific expression of a number of proteins, including CD14, CD11b, F4/80 (mice)/EMR1 (humans), lysozyme M, MAC-3 and CD68 (Yona and Jung, 2010). Macrophages are versatile cells that have multiple activities inside and outside the immune system. The initial function that was associated with these cells is phagocytosis, which is the capacity to engulf and digest pathogens, cellular debris and apoptotic bodies (Paidassi et al., 2009). Phagocytosis is part of the non-specific immune defence response (or innate immunity). After the pathogen is recognised as foreign material by specific pathogen-associated molecular pattern receptors, the phagocytic cell makes temporary extensions of the cell membrane to surround the pathogenic particle and internalise it within vacuoles (phagosomes). Phagosomes then fuse with lysosomes to make phagolysosomes, in which a number of enzymes and other toxic products destroy the microorganisms (Flannagan et al., 2009). ‘Foreign’ proteins derived from these microorganisms are hydrolysed, thus generating peptides (small fragments of proteins). Part of these peptides is released to the extracellular medium as waste. Released peptides can then be recognised by B lymphocytes through their surface immunoglobulins, a process that leads to B lymphocyte activation. Some of the protein fragments are further processed into short peptides inside macrophages (10–14 amino acids in length) and are inserted into the antigen-presenting groove of major histocompatibility complex (MHC) molecules for subsequent export to the cell membrane. These peptide–MHC complexes are then presented to T lymphocytes through a process known as antigen presentation. If the interacting T lymphocyte displays the appropriate T cell receptor (TCR) for the peptide–MHC combination, the T lymphocyte will be activated and stimulated to release cytokines that modulate the immune response (Hume, 2008). These are the early events of the specific immune defence (or adaptive immunity). With the coordinated action of T and B lymphocytes, the process of antigen presentation may result in the production of specific antibodies that attach to antigens on the surface of pathogens (opsonisation). Opsonised particles are more efficiently recognised by macrophages, thus resulting in enhanced phagocytosis and clearance of the foreign particles. See also: Phagocytosis; Phagocytosis: Enhancement During the immune response, macrophages are also involved in the production of pro-inflammatory mediators, including enzymes, nitrogen and oxygen reactive species, complement proteins and cytokines that control the functional activity of other cells. For example, the cytokines tumour necrosis factor α (TNFα) and interleukin-1 beta (IL-1β) released by activated macrophages act in the hypothalamus to induce fever. Overproduction of these cytokines during septic shock can lead to multi-organ failure and the death of the organism (Lloberas and Celada, 2009). See also: Inflammatory Mediators Finally, macrophages are also implicated in the maintenance of homeostasis. For example, spleen macrophages recognise cell surface markers that are expressed on aged red blood cells. After phagocytosis of these cells, some of their contents are recycled, including iron molecules, and later released by macrophages to the plasma depending on the needs of the organism to produce more red blood cells in the bone marrow (Beaumont and Delaby, 2 2009). Macrophages also control lipid metabolism, as described later. See also: Spleen Macrophages and Inflammation Nowadays, we know that inflammation represents a major factor in the development of a number of chronic diseases, such as cancer, metabolic syndrome, autoimmunity and neurodegenerative disorders. For this reason, many novel strategies for therapeutic intervention of several chronic diseases aim at interfering with the inflammatory process, and in particular, with the activities of macrophages. The expression of selected surface molecules allows us to distinguish among different monocyte subsets in circulation. In humans, expression of CD16 (also known as Fc-gamma receptor III, FcγRIII) distinguishes two monocyte subsets. Most of the circulating monocytes (80–90%) are CD14+ /CD16− cells that express high levels of the chemokine receptor CCR2 and low levels of CX3CR1. These monocytes are poor producers of inflammatory cytokines and they preferentially release the anti-inflammatory cytokine IL-10. Conversely, CD16+ monocytes express high levels of CX3CR1 and low levels of CCR2 and account for inflammatory cytokine production. In the mouse, monocyte subsets can be distinguished on the basis of the expression of the Ly6C antigen and of the chemokine receptors CCR2 and CX3CR1. Ly6C− monocytes patrol blood vessels under steady-state conditions, whereas monocytes that express Ly6C and high levels of CCR2 are recruited at sites of inflammation and in lymph nodes and secrete large amounts of inflammatory cytokines (Geissmann et al., 2003; Mantovani et al., 2009). When inflammation takes place, the bone marrow generates Ly6C+ monocytes that strongly interact with endothelial cells lining the blood vessels at the inflammatory loci and then enter the damaged tissue through a process known as extravasation, where they undergo the morphological and functional changes that lead to differentiation into activated tissue macrophages. During the initial phases of the inflammatory process and in response to several cytokines (e.g. interferon γ, IFNγ) or bacterial products such as lipopolysaccharide (LPS), macrophages become ‘classically activated’ and exert strong pro-inflammatory activities through the release of a number of toxic compounds such as nitric oxide (NO) and reactive oxygen species (ROS). During the progression of inflammation, macrophages phagocytose apoptotic bodies derived from neutrophils, macrophages or other cells present at the inflammatory site. Extensive phagocytosis makes macrophages switch phenotype to become anti-inflammatory cells with active roles in tissue repair (Arnold et al., 2007). See also: Inflammatory Mediators Conversion of Macrophages into Foam Cells Macrophages play a major role in lipoprotein homeostasis. Under normal conditions, macrophages take up low-density lipoproteins (LDLs) through LDL receptors (LDLRs). After eLS © 2015, John Wiley & Sons, Ltd. www.els.net Macrophage Foam Cells internalisation, LDL particles are degraded in the lysosomal compartment, where enzymes hydrolyse cholesteryl esters to free cholesterol and fatty acids. Free cholesterol is toxic and needs to be re-esterified into cholesteryl esters for storage as lipid droplets in the cytoplasm. The dynamic balance between the amount of free cholesterol and cholesteryl esters within the cell is regulated by two enzymes located in the endoplasmic reticulum: acyl-coenzyme A:cholesterol acyltransferase-1 (ACAT1) and neutral cholesterol ester hydrolases (nCEH) (reviewed by Li and Palinski, 2006). In normal conditions, free cholesterol and phospholipids are mobilised to the plasma membrane by adenosine triphosphate-binding cassette (ABC) transporters, including ABCA1 and G1, and subsequently transferred to exogenous apolipoprotein acceptors that make up high-density lipoproteins (HDLs). This process is known as cholesterol efflux and it is the first step in reverse cholesterol transport from peripheral tissues to the liver. Human genetic deficiency in ABCA1 leads to Tangier disease, a condition characterised by severe HDL deficiency, the accumulation of foam cells in many tissues and an increased susceptibility to develop atherosclerosis (reviewed by Takahashi et al., 2005). Each of the lipid constituents of LDL, including cholesteryl esters, phospholipids, sterols and triglycerides, can undergo oxidation. Under conditions that lead to the accumulation of oxidised LDL (oxLDL) or other forms of modified LDL, macrophages become highly efficient at taking up these particles through the action of scavenger receptors (SR)-A, −BI and CD36, which have evolved as molecular pattern recognition receptors to mediate phagocytosis of pathogens and apoptotic cells (reviewed by Hazen, 2008). The accumulation of LDL derivatives inside macrophages inhibits the surface expression of classical LDLRs but not of scavenger receptors (Brown and Goldstein, 1986). Thus, macrophages conserve the capacity to accumulate very large amounts of oxLDL-derived lipids and become lipid-loaded foam cells. See also: Macrophages in Lipid and Immune Homeostasis Macrophages in the Development of Atherosclerotic Lesions Atherosclerotic lesions arise in the arterial wall, typically at vessel bifurcations that are exposed to non-laminar blood flow. The intima, the arterial layer adjacent to the lumen, consists of a monolayer of endothelial cells and an internal elastic tissue, which, in humans, is rich in proteoglycans, particularly near branch sites. Lipid accumulation is generally absent from healthy intima, as are macrophages, except for occasional patrolling monocytes. Underneath the intima, a thick arterial media, consisting mainly of smooth muscle cells interwoven with elastin and collagen fibres, conveys mechanical stability to the arterial wall (reviewed by Li and Palinski, 2006). The accumulation of lipids in the arterial intima is dependent on the interaction of LDL particles with proteoglycans within the extracellular matrix. LDL particles may then undergo modification (e.g. oxidation) by endothelial and other arterial cells and initiate an inflammatory process that promotes monocyte recruitment into the vessel wall (Figure 1). Under the effect of oxLDL, endothelial cells express adhesion molecules, including E- and P-selectins, which interact with integrins expressed on the surface of circulating monocytes, thus facilitating monocyte tethering and rolling on the endothelial layer. This process is followed by firm adhesion of monocytes on endothelial cells mediated by endothelial expression of vascular adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1). Finally, transmigration through the endothelium involves the interaction of junctional adhesion molecules (JAM) and connexins (reviewed by Galkina and Ley, 2007). Endothelial transmigration of monocytes is also promoted by chemokines, such as monocyte chemoattractant protein 1 (MCP-1) and Ccl5 (also known as Rantes) (Figure 1). The chemokine C-C receptors CCR2 and CCR5 are expressed in monocytes and play an important role in atherosclerosis by binding to MCP-1 and Ccl5, respectively. Genetic manipulation of these chemokine/receptor systems have been shown to affect plaque size and progression (reviewed by Gautier et al., 2009). Macrophage migration inhibitory factor (MIF) is a cytokine that plays a regulatory role in monocyte adhesion and migration and in macrophage proliferation. Increased expression of MIF has been demonstrated in human atherosclerotic lesions, whereas the absence of the gene encoding MIF reduces atherosclerosis in mice (reviewed by Noels et al., 2009). See also: Atherosclerosis: Pathogenesis, Clinical Features and Treatment Once monocytes have taken residence in the arterial wall intima, they undergo phenotypic transformation into macrophages, internalise large amounts of modified LDLs via scavenger receptors and become foam cells, as described earlier (Figure 1). This is the initial step in formation of the fatty streak in the arterial wall. Thus, a common strategy in reducing the risk of atherosclerosis is currently based on lowering LDL levels in the organism through the use of statins, inhibitors of HMG-CoA reductase, the rate-limiting enzyme involved in the cholesterol biosynthetic pathway. By reducing the cellular capacity to synthesise cholesterol, LDLRs are upregulated, particularly in hepatocytes, and they remove the circulating pro-atherogenic LDL particles more rapidly (Brown and Goldstein, 1986). During progression of the atherosclerotic plaque, invading macrophages and newly formed foam cells secrete ROS and the enzyme 12/15-lipoxygenase (LO) that contributes to enhancing the oxidation of LDL particles. Foam cells also release pro-inflammatory cytokines (including TNF-α, IL-1β and IL-6), chemokines, growth factors, such as platelet-derived growth factors (PDGFs), endothelial-derived growth factor (VEGF) and insulin-like growth factors (IGFs), and enzymes, such as cysteine-, serine- and metallopeptidases, which degrade extracellular matrix components (reviewed by Saha et al., 2009). The combined action of all these molecules enhances the inflammatory process, allowing T lymphocytes, natural killer cells, dendritic cells and mast cells to infiltrate the vascular subendothelium. Furthermore, the proliferation and migration of smooth muscle cells into the intima facilitates the establishment of the atherosclerotic plaque. At later stages of atherosclerosis, foam cells express high levels of cycloxygenases (COX)-1 and -2 (reviewed by Cipollone et al., 2008). These are enzymes that generate pro-inflammatory eLS © 2015, John Wiley & Sons, Ltd. www.els.net 3 Macrophage Foam Cells (b) (a) Vascular lumen Adhesion Migration MCP-1 CCR-2 ox LDL Monocyte Endothelial cells LDL HDL Extracellular matrix Differentiation M-CSF Intima VCAM-1 P-selectin E-selectin ICAM-1 CS-1 mmLDL Proinflamatory process 15 LO iNOS Homeostatic responses apo E ABC-1 ACAT ox LDL TNF-α IL-1β IL-6 Macrophage Foam cell ox LDL uptake CD36 SR-A Media Internal elastic lamina LDL oxidation Smooth muscle cells (c) Figure 1 Mechanisms involved in foam cell formation and development of the atherosclerotic lesion. (a) Microphotograph of the normal intima after oil-red O staining. Very few oil-red O-positive lipid infiltrations are detected in the normal intima. (b) Microphotograph of the earliest stage of an atherosclerotic lesion, the fatty streak, after staining with oil-red O. The fatty streak is characterised by subendothelial accumulation of macrophages/foam cells, which contain massive amounts of lipids, as indicated by oil-red O staining. (c) Atherogenesis is a chronic inflammatory process. Under conditions of hypercholesterolaemia, LDL accumulates in the arterial intima and is progressively oxidised by endothelial and other arterial cells. Endothelial cells also become activated, thus increasing the expression of adhesion molecules, including selectins, VCAM-1 and ICAM-1, on their surfaces. OxLDL and MCP-1 act as chemoattractants for circulating monocytes that then attach to endothelial cells via adhesion molecules. CCR2, the receptor for MCP-1, is upregulated in circulating monocytes and further increases their rate of recruitment. Monocytes transmigrate to the subendothelial space, where they transform into macrophages and begin producing enzymes that oxidatively modify LDL, such as 12/15-LO and enzymes that produce ROS. Oxidised LDL is rapidly taken up by scavenger receptors, such as CD36 and SR-A. The rapid accumulation of cholesteryl esters results in foam cell formation. Infiltrated macrophages and foam cells also participate in the inflammatory process by secretion of pro-inflammatory cytokines, such as TNF-α, IL-1β and IL-6. Homeostatic responses to prevent accumulation of foam cells include upregulation of the expression of molecules that participate in cholesterol efflux to HDL, such as apoE and ABCA1. Original magnification of microphotographs is 40×. (a) and (b) were donated by Andrew C. Li (University of California, San Diego). Reproduced with permission from Glass and Witztum (2001) © Cell Press. prostaglandins and thromboxane A2 (TXA2), which induce vasoconstriction and platelet aggregation. Inflammatory mediators also activate resident cells in the lesion and the secretion of proteolytic enzymes by macrophages contributes to plaque 4 erosion and rupture by forming a surface on which activated platelets may initiate thrombosis and amplify inflammation, thereby leading to stroke and myocardial infarction. See also: Cholesterol and Vascular Disease eLS © 2015, John Wiley & Sons, Ltd. www.els.net Macrophage Foam Cells Transcriptional Control to Prevent Foam Cell Formation and the Development of Atherosclerosis Liver X receptors (LXRs) and peroxisome proliferator-activated receptors (PPARs) are ligand-dependent transcription factors that belong to the nuclear receptor family. LXRs and PPARs positively regulate gene expression by binding as heterodimers with other members of the nuclear receptor family, the retinoid X receptors (RXRs), to specific response elements on the promoter or enhancer regions of their target genes. Several studies suggest that LXRs and PPARs play critical roles in feed-forward mechanisms that regulate cholesterol and fatty acid homeostasis in macrophages in response to rapid changes in cellular lipids (reviewed by Ricote et al., 2004). Two isoforms of LXR have been identified, LXRα and β, both of which are activated by oxidised derivatives of cholesterol (oxysterols) (Repa and Mangelsdorf, 2000). Treatment of cells with oxLDL leads to LXR activation, which suggests that LXR-activating oxysterols are present in oxLDL. LXR agonists induce in vitro cholesterol efflux from macrophages to extracellular apoAI acceptors and inhibit the development of atherosclerosis in mice. Moreover, the transplantation of LXR-deficient bone marrow progenitor cells into either apolipoprotein E (apoE)-deficient or LDLR-deficient mice leads to an increase in atherosclerotic lesions, thereby suggesting that activation of the LXR pathway exerts protective roles that impede the accumulation of excess cholesterol within cells and also prevent foam cell formation and the development of atherosclerosis (Tangirala et al., 2002). In fact, LXR–RXR heterodimers directly upregulate the expression of a number of genes involved in lipid and lipoprotein homeostasis, such as the cholesterol transporters ABCA1 and G1, phospholipid transfer protein (PLTP) and apoE (Figure 2) (reviewed by A-González and Castrillo, 2011). All these molecules participate in promoting cholesterol efflux, thus preventing and/or reducing cholesteryl ester accumulation in arterial wall macrophages. Moreover, the recognition of apoE as part of chylomicron remnants, very low-density lipoproteins (VLDLs) and intermediate density lipoproteins (IDLs) by LDLRs facilitates hepatic uptake of lipoprotein remnants. LXR activation also leads to the coordinated upregulation of other apolipoproteins (apoC-I, apoC-IV and apoC-II) and lipoprotein lipase (LPL), which affect lipoprotein metabolism (Mak et al., 2002). For example, ApoC-II is the obligate cofactor for LPL and is required for LPL-dependent hydrolysis of triglycerides present in chylomicrons, VLDLs and HDLs. Deficiency of apoC-II results in hypertriglyceridaemia (Fojo and Brewer, 1992). More recent studies have also demonstrated that LXR activation leads to increased expression of Mylip/Idol, an E3-ubiquitin ligase that promotes degradation of several members of the LDLR family. Therefore, the LXR pathway not only enhances mechanisms involved in cholesterol efflux but also participates in limiting the uptake of circulating LDL by macrophages and other cells (Zelcer et al., 2009; Hong et al., 2010). Apart from their role in reverse cholesterol transport, LXR agonists induce the expression of the transcription factor sterol response element binding protein (SREBP)-1c, which in turn triggers the expression of enzymes involved in fatty acid synthesis and desaturation and triglyceride formation (Repa et al., 2000). In macrophages, positive regulation of fatty acid biosynthesis and their use in cholesterol sterification may reflect an adaptive mechanism provided by LXRs to buffer the toxic effects of free cholesterol (Tabas, 2002). Moreover, desaturation of fatty acids may provide the cell with ligands for other nuclear receptors, including PPARs (see later discussion). The finding that lipogenesis is strongly activated by available synthetic LXR agonists limits their potential use as anti-atherogenic drugs. However, it may be possible to develop novel ligands that differentially regulate programs of gene expression involved in cholesterol efflux and fatty acid biosynthesis. In the absence of activating ligands, LXR/RXR heterodimers actively repress target genes by binding nuclear receptor co-repressors such as NCoR and SMRT. In LXR-deficient macrophages, NCoR is not recruited to LXR target genes, which leads to derepression of the ABCA1 gene and enhanced cholesterol efflux, but does not result in increased expression of SREBP1c or increased fatty acid biosynthesis (Wagner et al., 2003). Therefore, the generation of selective LXR modulators that disrupt the binding of LXR to co-repressors without leading to co-activator recruitment may provide a strategy to selectively increase ABCA1 expression in macrophages and thus be used for anti-atherogenic purposes without having side effects on lipogenesis. Within the PPAR subfamily, three isoforms have been identified, namely PPARα, 𝛿 and γ. PPARs bind a broad range of fatty acids and their metabolites. While there is some preference for specific fatty acids by each PPAR, when present at sufficiently high concentrations many fatty acids are capable of activating all three PPAR isoforms. PPARs can be also activated by certain eicosanoids, which are produced by metabolism of arachidonic acids and other long-chain polyunsaturated fatty acids (reviewed by Menendez-Gutierrez et al., 2012). PPARα is also the molecular target of fibrates, such as gemfibrizol, which are used clinically to treat hypertriglyceridaemia. Indeed, PPARα regulates the production of enzymes involved in fatty acid β-oxidation and lipoprotein metabolism. Clinical trials examining the effects of fibrates in primary and secondary cardiovascular prevention studies demonstrated a significant reduction in coronary heart disease, with highest efficacy in overweight individuals with insulin resistance and chronic inflammation (reviewed by Bouhlel et al., 2008). PPARγ is activated by thiazolidinediones (TZDs), such as rosiglitazone, which act as insulin sensitisers and have been used in the treatment of type 2 diabetes mellitus. Oxidised lipids present in oxLDL, such as 15-hydroxyeicosatetraenoic acid and 13-hydroxyoctadecadienoic acid, also have the capacity to activate PPARγ (reviewed by Ricote et al., 2004). The scavenger receptor CD36, involved in oxLDL uptake, is a PPARγ target gene (Figure 2). However, despite increased CD36 expression, TZDs do not induce significant cellular cholesterol accumulation (Moore et al., 2008). Indeed, PPARγ agonists reduce carotid artery wall thickening in diabetic patients and direct evidence that PPARγ exerts anti-atherogenic action has been shown in murine models of atherosclerosis (reviewed by Li and Palinski, 2006). eLS © 2015, John Wiley & Sons, Ltd. www.els.net 5 Macrophage Foam Cells oxLDL apoptotic cells Triglyceride-rich lipoproteins LPL SRs CD36 FFAs PGs, LTs Cholesterol Oxysterols PLA2 FAS PPARE TATA PPAR/RXR Cxcl10 MIG IL12p40 iNOS LXRE TATA RXR/LXR CD36 iNOS COX2 LXRα Cpt1 IL-1β Ech1 IL-6 Pex11a MMP-9 LPL MCP-1,-3 MIP-1β Cxcl10 ABCA1 ABCG1 apoE LPL PLTP SREBP1c Mylip/Idol FFAs Cholesterol efflux Cpt1 Ech1 Pex11a Mitochondria β-oxidation ACAT Cholesterol Cholesterol esters ABCA1 apoAI apoE Figure 2 Macrophage responses to PPAR and LXR activation. Macrophages have availability to free fatty acids (FFAs) via the action of fatty acid synthase (FAS) or phospholipase A2 (PLA2) or via LPL-mediated lipolysis of triglyceride-rich lipoproteins. Conversion of FFAs to eicosanoids, such as prostaglandins (PGs) and leucotriens (LTs), provides ligands for PPARs. On the other hand, the uptake of oxLDL by SRs, including CD36, provides oxysterols that can activate LXRs. Activated PPARs and LXRs upregulate the expression of target genes through heterodimerisation with RXR and binding to the response elements PPARE and LXRE, respectively. Both PPARs and LXRs induce the expression of genes involved in macrophage lipid homeostasis (in red). For example, PPARs upregulate the expression of genes involved in mitochondrial β-oxidation, including Cpt1, Ech1 and PexIIa, and LXRs induce the expression of genes that participate in cholesterol efflux, such as ABCA1 and apoE. PPARs and LXRs also participate in modulation of innate and acquired immunity by transrepressing the expression of selective subsets of pro-inflammatory genes each (in blue). MIG, macrophage induced gene; iNOS, inducible nitric oxide synthase; MIP, macrophage inflammatory protein. Adapted from Ricote et al. (2004). © American Heart Association. In agreement with this, reconstitution of the haematopoietic system of LDLR-deficient mice with PPARγ-null bone marrow progenitor cells results in increased atherosclerosis (Chawla et al., 2001). There are several points of cross-talk between PPARs and LXRs in the regulation of cholesterol homeostasis. PPARα and γ induce the expression of ABCA1 and stimulate cholesterol efflux in human primary and THP-1 macrophages through a transcriptional cascade mediated by LXRα (Chawla et al., 2001; Chinetti et al., 2001). Consistent with these findings, basal cholesterol efflux from cholesterol-loaded macrophages to HDL is significantly reduced after disruption of the PPARγ gene (Akiyama 6 et al., 2002). Microarray analysis suggests that most PPARγ target genes, such as CD36, apoE, adipose differentiation-related protein (ADRP), ABCG1, the peroxisomal enzymes Ech1 and Pex11a, α mannosidase II and carnitine palmitoyl transferase (Cpt1), participate in lipid transport and metabolism. Interestingly, some of the target genes for PPARγ are also induced by PPAR𝛿 ligands, suggesting that these two isoforms have overlapping transactivator functions in macrophages (reviewed by Ricote et al., 2004). In addition to the regulation of lipid metabolism, LXRs and PPARγ exert both overlapping and specific repressive actions on transcriptional programs induced during the macrophage eLS © 2015, John Wiley & Sons, Ltd. www.els.net Macrophage Foam Cells response to inflammatory stimuli, affecting a number of genes that code for mediators of innate and acquired immune responses (Ghisletti et al., 2007). Most probably, these effects result from a combination of mechanisms, including nuclear receptor-mediated transrepression. LXRs and PPARγ also exert anti-inflammatory effects in several in vivo murine models of inflammation, including atherosclerosis (reviewed by Ricote et al., 2004). In humans, rosiglitazone reduces the circulating concentrations of inflammatory markers of cardiovascular disease, such as C-reactive protein, matrix metallopeptidase (MMP)-9 and TNF-α, in type 2 diabetic patients (Haffner et al., 2002). In the past few years, significant progress has been made in our understanding of the molecular mechanisms governing the transrepression of inflammatory responses by LXRs and PPARγ. Agonists for LXRs or PPARγ inhibit NF𝜅B-mediated responses through alternative sumoylation-dependent mechanisms. Ligand-dependent conjugation of SUMO2/3 to LXRs or SUMO1 to PPARγ targets them to promoters of genes induced upon toll-like receptor (TLR) engagement, where they prevent the signal-dependent removal of co-repressor complexes (Ghisletti et al., 2007). More recently, LXR has been shown to downregulate a large percentage of the macrophage transcriptional response to IFNγ in a sumoylation-dependent manner, which correlated with reduced recruitment of signal transducer and activator of transcription (Stat)1 to several gene promoters (Pascual-García et al., 2013). These observations led to the notion that LXR and PPAR agonists exert their anti-atherogenic effect not only by promoting cholesterol efflux but also by limiting the production of inflammatory mediators in the arterial wall. Taking all these considerations together, the activation of LXRs and PPARs by constituents of oxLDL or other endogenous ligands should lead to cholesterol efflux and inhibition of macrophage inflammatory responses, thereby preventing foam cell accumulation. However, this protective system cannot compensate the effects of cholesterol-rich western diets indefinitely. The mechanisms that shut off the protective actions of nuclear receptors are not well understood. Interestingly, IFNγ and LPS repress the expression of PPARγ (Welch et al., 2003) and both IFNγ and TLR signalling inhibit macrophage responses to LXR agonists, such as induction of ABCA1 and cholesterol efflux (Castrillo et al., 2003; Pascual-García et al., 2013). These observations suggest that inflammatory events within the arterial wall reciprocally contribute to the inhibition of nuclear receptor action. On the other hand, an LXR transcriptional target, the scavenger glycoprotein AIM (apoptosis inhibitory protein secreted by macrophages)/Sp-α protects macrophages from the apoptotic effects of oxidised lipids (Arai et al., 2005) and recent work has provided evidence that overexpression of human AIM increases foam cell formation by promoting CD36-mediated uptake of oxLDL (Amézaga et al., 2014). On the basis of these observations, it is possible that positive regulation of AIM and CD36 expression by endogenous LXR and PPAR ligands, respectively, in coordination with a local inflammatory environment that inhibits LXR-dependent cholesterol efflux may contribute to the loss of the protective activities mediated by these nuclear receptors during development of atherosclerosis. See also: Nuclear Receptors and Disease; Nuclear Receptor Genes Foam Cells in Other Forms of Chronic Inflammation When the immune system is unable to eliminate substances perceived as foreign, both infectious and non-infectious, it produces a ball-like structure of immune cells attempting to wall off the non-self material. This special type of inflammatory reaction is called granuloma and occurs in a wide variety of diseases (Figure 3). Granuloma is an organised collection composed mostly of macrophages that are typically so tightly clustered that the borders of individual cells are difficult to appreciate and often, but not invariably, fuse to form multi-nucleated giant cells. Granulomas may also contain matrix components, including collagen, and additional cells such as lymphocytes, neutrophils, eosinophils, multi-nucleated giant cells and fibroblasts. T cells of the IFNγ-secreting TH 1 subset surround the granuloma. See also: Immune Mechanisms against Intracellular Pathogens; Inflammation: Chronic During infection, lipid bodies can be generated within infected cells. Formation of lipid bodies in this context is dependent on the activation of TLRs and the presence of pro-inflammatory signals such as TNFα and MCP-1. In infections by Mycobacterium tuberculosis, lipids are overproduced by bacilli that reside within macrophages. These lipids consolidate as multi-vesicular bodies and are subsequently exocytosed to the extracellular milieu (Figure 3). The most bioactive components of these released lipids are trehalose dimycolates (TDM). It has been recently demonstrated that foam cell formation can be specifically induced by oxygenated forms of mycolic acid, such as oxygenated ketomycolic and hydroxyl-mycolic acids. These lipids are synthesised by pathogenic mycobacterial species such as Mycobacterium avium and M. tuberculosis but not by saprophytic species such as M. smegmatis. Foam cells can also be generated by treatment with isolated lipids. Trehalose dimycolate isolated from the cell wall of M. bovis or Calmette–Guérin (BCG) bacilli binds to macrophage receptor with collagenous structure (MARCO) and is internalised by the action of TLR2, thereby leading to foam cell formation. Because trehalose dimycolate is released and captured by infected cells, a large number of macrophages in the lesion become foam cells (Rhoades et al., 2003) (Figure 3). Foam cells are also generated in other infections, such as those caused by Toxoplasma and Chlamydia (Portugal et al., 2008). See also: Immune Mechanisms against Intracellular Pathogens; Tuberculosis: Immunity Electron microscopy has shown that M. tuberculosis is in contact with lipid bodies within foam cells. Interestingly, M. tuberculosis can also survive in adipocytes, cells that store lipids in the adipose tissue. Moreover, lipid inclusions have been found inside the bacilli themselves. Indeed, these bacteria can catabolise cholesterol (Pandey and Sassetti, 2008) and the growth of experimental bacterial strains deficient in cholesterol transporters is hindered in conditions where cholesterol is the source of carbon. Taken together, all these observations suggest that the pathogen uses lipids from the host as a nutrient. Therefore, the pathogen meets nutritional advantages by living within cells that accumulate lipids. This strategy may allow the bacilli to remain in a dormant non-replicative state (Peyron et al., 2008). eLS © 2015, John Wiley & Sons, Ltd. www.els.net 7 Macrophage Foam Cells Mycobacterium tuberculosis Multivesicular bodies exocytosed TLRs SR (MARCO) Granuloma Internalization TDM Macrophage Foam cell Noninfected macrophage (a) TNFα IL-1 IL-6 iNOS COX2 Foam cell IL-12 AP-1 NFκB STAT1 TH1 IFN-γR IFNγ (b) PPAR Infected macrophage TH1 lymphocyte TLRs TH1 lymphocyte Bacterial pathogens Macrophage Figure 3 Foam cell formation in the granuloma during the infection with Mycobacterium tuberculosis. (a) Bacilli that reside within macrophages overproduce lipids such as trehalose dimycolates (TDM) that consolidate as multi-vesicular bodies and are subsequently exocytosed to the extracellular milieu. Through the SRs and TLRs exocytosed bodies are taken up by macrophages that then become foam cells. (b) Cross-talk between macrophages and TH 1 lymphocytes. References A-González N and Castrillo A (2011) Liver X receptors as regulators of macrophage inflammatory and metabolic pathways. Biochimica et Biophysica Acta 1812: 982–994. Akiyama TE, Sakai S, Lambert G, et al. (2002) Conditional disruption of the peroxisome proliferator-activated receptor gamma gene in mice results in lowered expression of ABCA1, ABCG1, and apoE in macrophages and reduced cholesterol efflux. Molecular and Cellular Biology 22: 2607–2619. Amézaga N, Sanjurjo L, Julve J, et al. (2014) Human scavenger protein AIM increases foam cell formation and CD36-mediated oxLDL uptake. Journal of Leukocyte Biology 95: 509–520. Arai S, Shelton JM, Chen M, et al. (2005) A role for the apoptosis inhibitory factor AIM/Spα/Api6 in atherosclerosis development. Cell Metabolism 1: 201–213. Arnold L, Henry A, Poron F, et al. (2007) Inflammatory monocytes recruited after skeletal muscle injury switch into antiinflammatory macrophages to support myogenesis. Journal of Experimental Medicine 204: 1057–1069. Beaumont C and Delaby C (2009) Recycling iron in normal and pathological states. Seminars in Hematology 46: 328–338. Bouhlel MA, Staels B and Chinetti-Gbaguidi G (2008) Peroxisome proliferator-activated receptors – from active regulators of macrophage biology to pharmacological targets in the treatment of cardiovascular disease. Journal of Internal Medicine 263: 28–42. 8 Brown MS and Goldstein JL (1986) A receptor-mediated pathway for cholesterol homeostasis. Science 232: 34–47. Castrillo A, Joseph SB, Vaidya SA, et al. (2003) Crosstalk between LXR and toll-like receptor signaling mediates bacterial and viral antagonism of cholesterol metabolism. Molecular Cell 12: 805–816. Chawla A, Boisvert WA, Lee CH, et al. (2001) A PPAR gamma-LXR-ABCA1 pathway in macrophages is involved in cholesterol efflux and atherogenesis. Molecular Cell 7: 161–171. Chinetti G, Lestavel S, Bocher V, et al. (2001) PPAR-alpha and PPAR-gamma activators induce cholesterol removal from human macrophage foam cells through stimulation of the ABCA1 pathway. Nature Medicine 7: 53–58. Cipollone F, Cicolini G and Bucci M (2008) Cyclooxygenase and prostaglandin synthases in atherosclerosis: recent insights and future perspectives. Pharmacology & Therapeutics 118: 161–180. Flannagan RS, Cosio G and Grinstein S (2009) Antimicrobial mechanisms of phagocytes and bacterial evasion strategies. Nature Reviews. Microbiology 7: 355–366. Fojo SS and Brewer HB (1992) Hypertriglyceridaemia due to genetic defects in lipoprotein lipase and apolipoprotein C-II. Journal of Internal Medicine 231: 669–677. Galkina E and Ley K (2007) Vascular adhesion molecules in atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology 27: 2292–2301. eLS © 2015, John Wiley & Sons, Ltd. www.els.net Macrophage Foam Cells Gautier EL, Jakubzick C and Randolph GJ (2009) Regulation of the migration and survival of monocyte subsets by chemokine receptors and its relevance to atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology 29: 1412–1418. Geissmann F, Jung S and Littman DR (2003) Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity 19: 71–82. Geissmann F, Manz MG, Jung S, et al. (2010) Development of monocytes, macrophages, and dendritic cells. Science 327: 656–661. Ghisletti S, Huang W, Ogawa S, et al. (2007) Parallel SUMOylation-dependent pathways mediate gene- and signalspecific transrepression by LXRs and PPARgamma. Molecular Cell 25: 57–70. Ginhoux F and Jung S (2014) Monocytes and macrophages: developmental pathways and tissue homeostasis. Nature Reviews in Immunology 14: 392–404. Glass CK and Witztum J (2001) Atherosclerosis: the road ahead. Cell 104: 503–516. Haffner SM, Greenberg AS, Weston WM, et al. (2002) Effect of rosiglitazone treatment on nontraditional markers of cardiovascular disease in patients with type 2 diabetes mellitus. Circulation 106: 679–684. Hazen SL (2008) Oxidized phospholipids as endogenous pattern recognition ligands in innate immunity. Journal of Biological Chemistry 283: 15527–15531. Hong C, Duit S, Jalonen P, et al. (2010) The E3 ubiquitin ligase IDOL induces the degradation of the low density lipoprotein receptor family members VLDLR and ApoER2. Journal of Biological Chemistry 285: 19720–19726. Hume DA (2008) Macrophages as APC and the dendritic cell myth. Journal of Immunology 181: 5829–5835. Li AC and Palinski W (2006) Peroxisome proliferator-activated receptors: how their effects on macrophages can lead to the development of a new drug therapy against atherosclerosis. Annual Review of Pharmacology and Toxicology 46: 1–39. Lloberas J and Celada A (2009) p21(waf1/CIP1), a CDK inhibitor and a negative feedback system that controls macrophage activation. European Journal of Immunology 39: 691–694. Mak PA, Laffitte BA, Desrumaux C, et al. (2002) Regulated expression of the apolipoprotein E/C-I/C-IV/C-II gene cluster in murine and human macrophages. A critical role for nuclear liver X receptors alpha and beta. Journal of Biological Chemistry 277: 31900–31908. Mantovani A, Garlanda C and Locati M (2009) Macrophage diversity and polarization in atherosclerosis: a question of balance. Arteriosclerosis, Thrombosis, and Vascular Biology 29: 1419–1423. Mayerl C, Lukasser M, Sedivy R, et al. (2006) Atherosclerosis research from past to present--on the track of two pathologists with opposing views, Carl von Rokitansky and Rudolf Virchow. Virchows Archiv 449: 96–103. Menendez-Gutierrez MP, Roszer T and Ricote M (2012) Biology and therapeutic applications of peroxisome proliferator- activated receptors. Current Topics in Medicinal Chemistry 12: 548–584. Moore GB, Pickavance LC, Briscoe CP, et al. (2008) Energy restriction enhances therapeutic efficacy of the PPARgamma agonist, rosiglitazone, through regulation of visceral fat gene expression. Diabetes, Obesity & Metabolism 10: 251–263. Noels H, Bernhagen J and Weber C (2009) Macrophage migration inhibitory factor: a noncanonical chemokine important in atherosclerosis. Trends in Cardiovascular Medicine 19: 76–86. Paidassi H, Tacnet-Delorme P, Arlaud GJ and Frachet P (2009) How phagocytes track down and respond to apoptotic cells. Critical Reviews in Immunology 29: 111–130. Pandey AK and Sassetti CM (2008) Mycobacterial persistence requires the utilization of host cholesterol. Proceedings of the National Academy of Sciences of the United States of America 105: 4376–4380. Pascual-García M, Rué L, León T, et al. (2013) Reciprocal negative cross-talk between liver X receptors (LXRs) and STAT1: effects on IFN-γ-induced inflammatory responses and LXR-dependent gene expression. Journal of Immunology 190: 6520–6532. Peyron P, Vaubourgeix J, Poquet Y, et al. (2008) Foamy macrophages from tuberculous patients’ granulomas constitute a nutrient-rich reservoir for M. tuberculosis persistence. PLoS Pathogens 4: e1000204. Portugal LR, Fernandes LR, Pietra Pedroso VS, et al. (2008) Influence of low-density lipoprotein (LDL) receptor on lipid composition, inflammation and parasitism during Toxoplasma gondii infection. Microbes and Infection 10: 276–284. Repa JJ, Liang G, Ou J, et al. (2000) Regulation of mouse sterol regulatory element-binding protein-1c gene (SREBP-1c) by oxysterol receptors, LXRalpha and LXRbeta. Genes & Development 14: 2819–2830. Repa JJ and Mangelsdorf DJ (2000) The role of orphan nuclear receptors in the regulation of cholesterol homeostasis. Annual Review of Cell and Developmental Biology 16: 459–481. Rhoades E, Hsu F, Torrelles JB, et al. (2003) Identification and macrophage-activating activity of glycolipids released from intracellular Mycobacterium bovis BCG. Molecular Microbiology 48: 875–888. Ricote M, Valledor AF and Glass CK (2004) Decoding transcriptional programs regulated by PPARs and LXRs in the macrophage: effects on lipid homeostasis, inflammation, and atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology 24: 230–239. Saha P, Modarai B, Humphries J, et al. (2009) The monocyte/macrophage as a therapeutic target in atherosclerosis. Current Opinion in Pharmacology 9: 109–118. Tabas I (2002) Consequences of cellular cholesterol accumulation: basic concepts and physiological implications. Journal of Clinical Investigation 110: 905–911. Takahashi K, Kimura Y, Nagata K, et al. (2005) ABC proteins: key molecules for lipid homeostasis. Medical Molecular Morphology 38: 2–12. Tangirala RK, Bischoff ED, Joseph SB, et al. (2002) Identification of macrophage liver X receptors as inhibitors of atherosclerosis. Proceedings of the National Academy of Sciences United States of America 99: 11896–11901. Wagner BL, Valledor AF, Shao G, et al. (2003) Promoter-specific roles for liver X receptor/corepressor complexes in the regulation of ABCA1 and SREBP1 gene expression. Molecular and Cellular Biology 23: 5780–5789. Welch JS, Ricote M, Akiyama TE, Gonzalez FJ and Glass CK (2003) PPARgamma and PPARdelta negatively regulate specific subsets of lipopolysaccharide and IFN-gamma target genes in macrophages. Proceedings of the National Academy of Sciences United States of America 100: 6712–6717. Yona S and Jung S (2010) LXRMonocytes: subsets, origins, fates and functions. Current Opinion in Hematology 17: 53–59. Zelcer N, Hong C, Boyadjian R and Tontonoz P (2009) LXR regulates cholesterol uptake through Idol-dependent ubiquitination of the LDL receptor. Science 325: 100–104. eLS © 2015, John Wiley & Sons, Ltd. www.els.net 9 Macrophage Foam Cells Further Reading Chinetti-Gbaguidi G and Staels B (2009) Lipid ligand-activated transcription factors regulating lipid storage and release in human macrophages. Biochimica et Biophysica Acta 1791: 486–493. Galkina E and Ley K (2009) Immune and inflammatory mechanisms of atherosclerosis. Annual Review of Immunology 27: 165–197. Greaves DR and Gordon S (2009) The macrophage scavenger receptor at 30 years of age: current knowledge and future challenges. Journal of Lipid Research 50 (Suppl): S282–S286. Korbel DS, Schneider BE and Schaible UE (2008) Innate immunity in tuberculosis: myths and truth. Microbes and Infection 10: 995–1004. 10 McLaren JE and Ramji DP (2009) Interferon gamma: a master regulator of atherosclerosis. Cytokine and Growth Factor Reviews 20: 125–135. Russell DG, Cardona PJ, Kim MJ, et al. (2009) Foamy macrophages and the progression of the human tuberculosis granuloma. Nature Immunology 10: 943–948. Silverstein RL (2009) Inflammation, atherosclerosis, and arterial thrombosis: role of the scavenger receptor CD36. Cleveland Clinic Journal of Medicine 76 (Suppl 2): S27–S30. eLS © 2015, John Wiley & Sons, Ltd. www.els.net View publication stats

![Anti-pan Macrophage antibody [Ki-M2R] ab15637 Product datasheet 1 References 1 Image](http://s2.studylib.net/store/data/012548928_1-267c6c0c608075eece16e9b9ab469ad0-300x300.png)