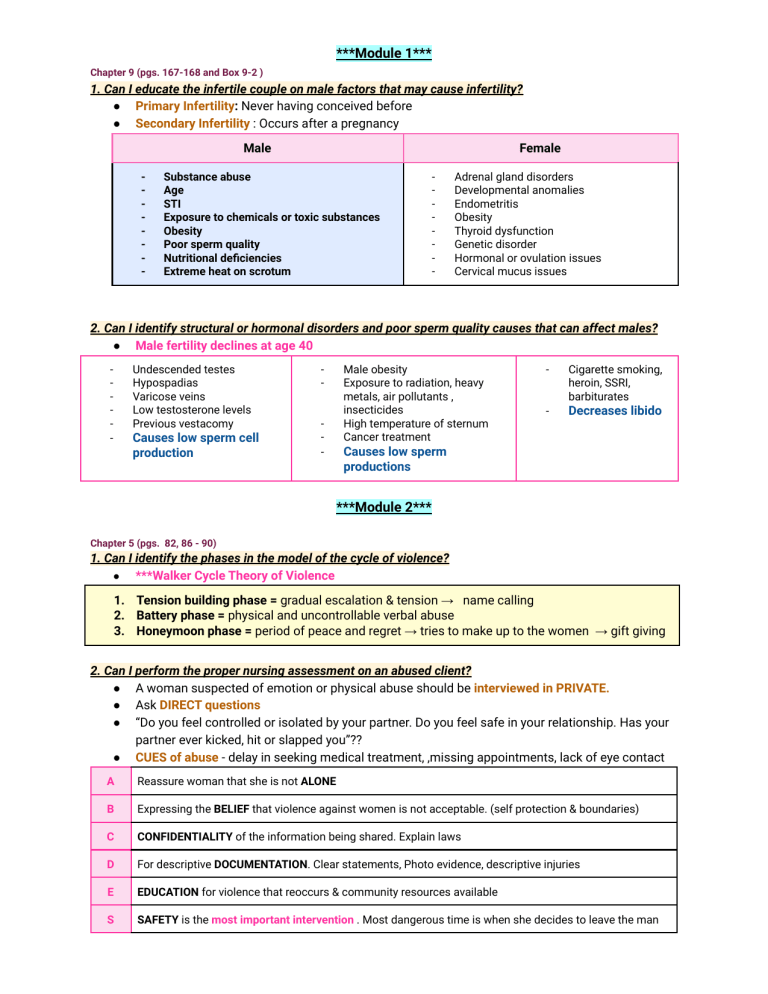
***Module 1*** Chapter 9 (pgs. 167-168 and Box 9-2 ) 1. Can I educate the infertile couple on male factors that may cause infertility? ● Primary Infertility: Never having conceived before ● Secondary Infertility : Occurs after a pregnancy Male - Female Substance abuse Age STI Exposure to chemicals or toxic substances Obesity Poor sperm quality Nutritional deficiencies Extreme heat on scrotum - Adrenal gland disorders Developmental anomalies Endometritis Obesity Thyroid dysfunction Genetic disorder Hormonal or ovulation issues Cervical mucus issues 2. Can I identify structural or hormonal disorders and poor sperm quality causes that can affect males? ● Male fertility declines at age 40 - Undescended testes Hypospadias Varicose veins Low testosterone levels Previous vestacomy Causes low sperm cell production - Male obesity Exposure to radiation, heavy metals, air pollutants , insecticides High temperature of sternum Cancer treatment - Cigarette smoking, heroin, SSRI, barbiturates - Decreases libido Causes low sperm productions ***Module 2*** Chapter 5 (pgs. 82, 86 - 90) 1. Can I identify the phases in the model of the cycle of violence? ● ***Walker Cycle Theory of Violence 1. Tension building phase = gradual escalation & tension → name calling 2. Battery phase = physical and uncontrollable verbal abuse 3. Honeymoon phase = period of peace and regret → tries to make up to the women → gift giving 2. Can I perform the proper nursing assessment on an abused client? ● A woman suspected of emotion or physical abuse should be interviewed in PRIVATE. ● Ask DIRECT questions ● “Do you feel controlled or isolated by your partner. Do you feel safe in your relationship. Has your partner ever kicked, hit or slapped you”?? ● CUES of abuse - delay in seeking medical treatment, ,missing appointments, lack of eye contact A Reassure woman that she is not ALONE B Expressing the BELIEF that violence against women is not acceptable. (self protection & boundaries) C CONFIDENTIALITY of the information being shared. Explain laws D For descriptive DOCUMENTATION. Clear statements, Photo evidence, descriptive injuries E EDUCATION for violence that reoccurs & community resources available S SAFETY is the most important intervention . Most dangerous time is when she decides to leave the man ● Myths & Facts about intimate partner violence **Myths** - Facts IPV occurs in a small % of population Being pregnant protects a women from IPV IPV only occurs in problematic or lower class families Only people who come from abusive families end up in abusive relationship Women would leave the relationship if the abuse was really that bad Only war veterans have PTSD Only men with psychological problems abuse women - - - ½ of the developing countries report 30% of women experience IPV Research suggest that pregnant women are more at risk of IPV IPV occurs regardless of social class Internet and phones have been used by both men and women to harass, monitor and control partners Some survivors of IPV may be diagnosed with PTSD Chapter 7 (pgs. 136-140 and table 7-6) 1. Can I identify the maternal and fetal effects and prevention of TORCH infections? ● TORCH infections from organism are capable of placing placenta Infection Toxoplasmosis Maternal Effects/ - Other Infections - Hepatitis A Hepatitis B - Rubella Cytomegalovirus - - Herpes Genitalis - Fetal Effects Most infections are asymptomatic Acute infection similar to mononucleosis Immune after first episode - Hep A : liver failure (rare), low grade fever, jaundice, RUQ tenderness Hep B : can be transmitted sexually , liver disease like cirrhosis - Rash, fever, mild symptoms such as headache, malaise and arthralgias, swollen lymph nodes - Most are asymptomatic or flu like symptoms Infection can be harbored in cervix - Painful blisters , tender inguinal lymph nodes, fever - - - - Prevention & Counseling Congenital infection is most likely to occur when infection develops 3rd trimester Fetal injury greatest during first trimester if infection occurs , coma, hydrocephalus, death - Hep A: perinatal transmission virtually never occurs Hep B: Infections occur during birth. Maternal vaccination should present no risk to fetus - 50-80% of fetuses exposed to virus will show signs of congenital infection Deafness & eye defect - - - - - - Fetus death, neurological problems, eye abnormalities Hepatosplenomegaly, intracranial calcification - Risk mainly during late pregnancy Congenital infection - - - Good handwashing techniques Eating raw or rare meat and exposure to litter used by cats should be avoided Hep A : Vaccine is available // Spread by fecal oral contact Hep B :Vaccine is available // Passed by contaminated needles, syringes ect. Vaccine is contraindicated in pregnant women, no pregnancy 1 month after vaccine Can breast feed Transmitted from infected organ , blood, sexual contact Wash hands carefully No treatment Acyclovir can be used to treat recurrent outbreaks Transmission greatest in vaginal birth → C section 2. Can I assess the s/s and nursing intervention for a client with bacterial vaginosis and Candidiasis? Disease Symptoms ***Bacterial Vaginosis (most common) - “Fishy odor” Increased thin vaginal discharge (thin, grayish, white) Odor increase after sex Trichomoniasis (STI) - “Strawberry Spots” Greenish copious discharge, malodorous ***Candidiasis - Yeast infection Vulva and pruritus “Cottage cheese” discharge Itching /burning Antibiotics - Metronidazole (flagyl) No need to treat partner *Not recommended to those who are breastfeeding* ↑↑↑ - OTC agents :intravaginal agents → fluconazole “azole” Chapter 12 (pgs. 233 and fig. 12-8) 1. Can I assess fetal development and the impact of teratogens? Ovum (1-2 weeks) - Embryo is NOT usually supcetiple to teratogen Tertagen usually damage all or most cells or damage only a few cell embryo develop w/o defects Embryonic weeks (3-8 weeks) HIGHLY SENSITIVE - Neural tube defects Mental retardation Heart defects, cleft lips, deafness, glaucoma, no limbs Most CRITICAL & vulnerable time for organ development due to cell division Embryo considered human after 8 weeks - Minor birth defects of CNS, teeth, ears, heart Fetus less sensitive to teratogens Fetal Period (9-40 weeks) Chapter 13 (pgs. 249-252, 254-262 and table 13-5 and Terminology handouts) 1. Can I explain the acronym GTPAL and document the results accordingly? 5 digit system that provides more information about the women's obstetric history. May not be considered accurate since it only provides information about births, not pregnancy reaching 20 weeks G - Gravida All pregnancy T - Term: over 37 weeks (37-41 6/7 weeks) P - Preterm : under 37 weeks to 20 (20-36 6/7 weeks) A - Abortion -20 weeks or less Miscarriages or selective L - Living children currently ● Example: A 26 year old female is currently 26 weeks pregnant. She had a misscariage at 10 weeks gestation 5 years ago. She has a three year old who was born at 39 weeks. What is GTPAL? - G=3 , T= 1 P= 0 A=1 L= 1 2.. Can I explain the acronym G/P (Gravidity/ parity) and document the results accordingly? ● 2 digit system abstained during the history assessment interview ● Example : Gravida 1, para 0 ( 1,0) means the woman is pregnant for the first time but has not reached 20 weeks yet Gravidity Parity The number of pregnancies a woman had The number of pregnancies that had reached 20 weeks , doesn't matter if their alive or stillborn 3. Can I assess the integumentary system, and gastrointestinal system of a pregnant client? Skin and Hair - Gastrointestinal Hyperpigmentation Melasma Linea nigra (pigment line on fundus) Striae gravidarum ( stretch marks) Angiomas ( spider veins) Pruritus gravidarum (abdomen itching) Nail and hair grows faster & thicker - N/V Heartburn Delayed peristalsis and gastric emptying Relaxation of cardiac sphincter Hemorrhoids Liver & gallbladder changes Abdominal discomfort from uterus expanding Excessive salivation (ptyalism) 4. Can I distinguish between presumptive, probable, and positive signs of pregnancy? Presumptive Signs (Changes woman experiences) MOMMY - Amenorrhea ( missed period) Nausea/Vomiting Urinary Frequency Hyperpigmentation (melasma, linea nigra, areola) Breast Changes Fatigue Quickening (fetal movement) Probable (Changes examiner observes) DOCTOR - Uterine enlargement Pregnancy test ( detects beta HCG, where occurs after implantation) Changes in Pelvic Organs Hedgar’s sign (softening of uterus) Goodell's Sign (softening of cervix) Chadwick Sign ( Bluish tint) Ballottement (movement of rebound) Braxton Hicks (contractions) Positive (Diagnostic) BABY - Direct visualization of the fetus Fetal heartbeat Palpable fetal movement Chapter 14 (pgs. 264-265, 268-269, (Signs of potential complications) 275, 283, 285, 288 tab 14-2, 14-3, Bx 14-1) 1. Can I assess the importance of fundal height? ● **Fundal Height : estimation of pregnancy: in direct relation to weeks of gestation - Mcdonalds methods Top of fundus to symphysis pubis = centimeter From 18-30 weeks Decreased implications: IUGR, oliogohydraminos Increased implications : Polyhydraminos, multiple gestations Elevated HOB, have knees flexed 2. Can I evaluate the EDB/EDC/EDD (estimate date of birth/estimate date of confinement/estimate date of delivery) using the Nagele’s rule? ● **Naegele Rule - Used Calculate estimated date of birth first day of the clients last menstrual cycle, subtract by 3 months and then add 7 days =Date - 3 months + 7 days = EDB 3. Can I assess first trimester discomfort related to pregnancy and self-management? ● Discomfort related to pregnancy First Trimester - - - - - - Breast changes (pain, tingling & tenderness) - due to hormonal stimulation → supportive maternity bra with pads to absorb discharge Urgency and frequent urination ( bladder reduced by enlarging uterus - empty bladder regularly/kegel exercise) → empty bladder regularly , limit fluid before bedtime, wear perineal pads N/V & fatigue : morning sickness (may be due to increase of estrogen, hcG , hormones) (rest and eat a well balanced diet) Rest as needed, eat small meals, avoid greasy gassy food, dont smoke Excessive salivation (may be due to elevated estrogen level - Chew gum & eat hard candy Gingivitis, hyperemia, bleeding, tender gums (estrogen stimulation) Eat a well balanced diet, eat fruits, brush teeth gently, watch hygiene, avoid infections, dentist Nasal stuffiness: Epistaxis (mucous membrane change related to increased estrogen level) Humidifier, about nose trauma Leukorrhea (hormonal stimulated cervix) Do not douche, wear perineal pad, wipe front to back Emotional lability : mood swings ( hormonal changes, changes in lifestyle) Support groups, communicate concern to partner Second Trimester - - Pigmentation deepens (areola, vulva, linea nigra, melasma, acne, oily skin - melanocyte stimulating hormone) Spider Nevi : around neck, face thorax, arms ( estrogen hormone change) Pruritus (noninflammatory, unknown, keep fingernail short) Palpitations (unknown, contact provider if symptoms of cardiac decomposition) Supine hypotension -pressure from uterus, side lying better ) Faintness ( postural hypotension) Food cravings ( satisfy craving, eat a well balanced diet) Heartburn (progesterone slows GI tract, avoid gassy food, large meals, fat food, antacid btw meals) Constipation ( drink 2L of water, include high fiber diet) Flatulence w/ Belching ( chew food slowly, avoid gas food) Varicose Veins ( avoid standing for a long time) Heachaches → 26 weeks ( emotional tension, try relation therapies) Carpal Tunnel Syndrome (compression due to nerves, elevate arms or splinting) Periodic Numbness & Ligament /Joint pain : stretching due to enlarging uterus - maintain good posture techniques) Third Trimester - - - - - Shortness of breath & dyspnea (expansion of diaphragm by enlarging uterus - keep good posture, dont smoke) Insomnia ( fetal movement, muscle cramps, SOBeffleurage, massage, bath before bedtime) Moodswings & increased anxiety (hormonal and metabolic adaptation) Urinary frequency and urgency returns ( empty bladder regularly and kegel exercise) Perineal discomfort (pressure from enlarging uterus, rest up and use good posture) Braxton Hicks contractions (uterine contractions in preparation for work labor , change positions and rest) Leg cramps when reclining: (due to compression of nerves , dorsiflex foot) Ankle edema (non pitting, can be aggravated due to prolonged standing, lack of exercise , water pooling-ample fluid for natural diuretic affect, diuretic are contraindicated 4. Can I explain maternal adaptation and expecting the pregnancy? 1. Accepting the pregnancy 2. Identifying with maternal role 3. Reordering personal relationships 4. Establishing a relationship with fetus 5. Preparing for birth - Emotional lability : rapid and unpredictable changes in mood Ambivalent feelings : conflicting feelings during pregnancy - Effective communication between expectant mother and mother Most important is the father of the child ( needs to feel loved and valued by partner) Phase 1 The woman accepts the biological fact of pregnancy . “ i am pregnant” Phase 2 The woman accepts the growing fetus as distinct from herself . Usually by 5th month “ i am going to have a baby” Phase 3 The woman prepares realistically for the birth and parenting of a child “ i am going to be a mother” - Watching videos, attending classes, seeking advices 5. Can I explain sibling adaptation to an expecting family? 1 y/o Seems to be unaware 2 y/o Notices changes in mom's appearance. Excitis cleaning behavior sometimes and regress from toilet training and eating 3 -4 y/o Wants to hear stories of their own beginning and accept a comparison of their own development to pregnancy. Listens to fetal heartbeat and feel baby moving School aged Early to Middle Adolescents Late Adolescents Curiosity” how the baby got in and how it will get out” Looks forward to the baby See themselves as mommy/ daddy Preoccupied with establishing their own sexual identiy and can have difficulrt aceepting the idea of sexual activityfrom thei parents Do not seem distrubed due to their focus on making plans for their own lives and realize they soon will leave home 6. Can I instruct a client when to notify the HCP about complications during the first trimester? First Trimester 1. 2. 3. 4. 5. “Severe” Vomiting Chill/Fever Burning on Urination Diarrhea Abdominal Cramps/Vaginal bleeding Causation 1. 2. 3. 4. 5. Hyperemesis Gravidarum Infection Infection Infection Misccarrage/ Ectopic pregnancy (fertilized egg implants & grows outside of uterus) 7. Can I identify each trimester of pregnancy? First Trimester Conception -13 weeks Second Trimester 14 weeks- 26 weeks Third Trimester 27-40 weeks Chapter 15 (pgs. 299-300, 303 table 15-2, 309) 1. Can I instruct a pregnant client on the importance of folate (folic acid)? ● Particular concern during the preconception period ● Folate is the form found naturally in food and folic acid is the form used to fortify grain products and food and vitamins Folic Acid deficiency - 0.4-0.6mg recommended - **High risk of neural tube defects or closure in neral tube→ spina bifida, anencephaly FOODS : organ meat, legumes, broccoli, greens , spinach , avocado, oranges, asparagus, papaya, fortified cereal, dark leafy green, citrus fruit 2. Can I evaluate the proper weight gain during pregnancy? ● ***Recommended weight gain*** ● Normal women with single pregnancy should gain 2-4 lb in first trimester, then 1lb/week after Underweight ( BMI less than 18) 28-40 lbs Normal (BMI 18.5-24.9) ⅔ trimester 1lb/week 25-35 lbs Overweight (BMI 25-25.9) 15-25 lbs Obsese (BMI over = 30) 11-20 lbs - 3. Can I instruct a client on the use of alcohol during pregnancy? ● Alcohol is a teratogen = contraindication during pregnancy ● Increase risk of msiccariage ,stillbirth, preterm pregnancy - No amount of alcohol is safe Fetal alcohol syndrome Alcohol related birth defects, CNS abnormalities, facial dysmorphia, impaired cognitive development, emotional and behavioral issues Chapter 26 (pgs. 565-570, box 26 – 1) 1. Can I identify the indications for a transvaginal ultrasonography (ultrasound)? ● noninvasive, painless, nonradiating ● Optimally used in the first trimester to detect ectopic pregnancy, monitor embryo, help identify abnormalities and help establish gestational age, fetal activity, placental anatomy ● During the 2&3rd trimester, it can be used with abdominal scanning to determine preterm labor First Trimester Second Trimester Third Trimester Confirm pregnancy Establish or confirm dates Confirm gestational age Confirm viability Confirm viability Confirm viability Determine gestational age & multiple pregnancy Detect polyhydramnios (excess amniotic fluid) Detect congenital anomalies Rule out ectopic pregnancy Detect intrauterine growth restriction & congenital anomalies Detect IUGR, placental abruptions, amniotic fluid assessment Determine cause of vaginal bleeding Assess placental location Determine fetal position Visualization for CVS Visualization during amniocentesis Visualization during amniocentesis (done at 8th week) (must be 14 weeks) (must be 14 weeks) 2. Can I identify factors that indicate the need for fetal testing? ● Some Indications for Antepartum testing Systemic lupus erythematosus Autoimmune disease that attacks its own tissues Preeclampsia potential dangerous pregnancy complication characterized by high blood pressure and signs of damage to another organ system Fetal Growth Restriction Fetus is unable to achieve its genetically determined potentially size Cholestasis Pregnancy A liver condition that develops in late pregnancy and triggers INTENSE ITCHING Oligohydramnios (AFI ) Amniotic fluid that is LESS than expected for gestational age Preterm rupture membranes can lead to oligohydramnios Late term or Post term gestation Previous Stillbirth Decreased Fetal Movement Chronic Hypertension/ Diabetes Renal Disease Multiple Gestation 3. Can I evaluate the daily fetal movement count? ● Kick counts : once a day for 60 minutes ● Daily Fetal Movement Count (DFMC) : - minimum of 10 daily movements should be counted per hour* Assess at 28-38 weeks Notify hcp if no movement in 12 hours or less than 3 movement in a hour → needs further evaluation from BPP , nonstress or contraction test Orange juice to stir up the baby Chapter 28 (pgs. 598-600, 603-604, 605-607) 1. Can I evaluate clinical manifestations of possible miscarriage? ● Uterine bleeding ● Uterine contractions ● Abdominal pain ● Signs of misccariage during early pregnancy Miscarriage ( Sponatenous Abortion) - A pregnancy that ends spontaneously before 20 weeks gestations or fetal viability →Threatened: Bleeding or cramping →Inevitable: cannot prevent →Incomplete: partial expulsion →Complete : all expelled →Missed :dies (ultrasound confirmation) - Causes: medical disorder, diabetes, obesity, lupus, alcoholism, toxin, cervical insufficiency Symptoms: heavy menstrual period (6-12 weeks). Severe pain, similar to labor after 12 weeks. Treatment: Oxytocin given to prevent hemorrhage → interventions are similar to labor because fetus must be expelled 2. Can I assess the incidence, s/s, and diagnosis of ectopic pregnancy? ● Ectopic Pregnancy : Fertilized ovum is planted outside of the uterine cavity , endometrial lining of uterus ● Uterus is the only organ capable of containing and sustaining a term pregnancy Incidence - - Leading cause of infertility 1st trimester accounts for 0.5-1.5% are ectopic pregnancy 2% of all in U.S S/S - Diagnosis UNILATERAL PAIN on one side abdominal pain, lower quadrant delayed menses abnormal vaginal bleeding dull to colicky pain - Hcg level higher than 1500 milli units or progesterone levels less than 5ng/ml = suspect disorder Treatment: Methotrexate : dissolves ectopic pregnancy by destroying and dividing cells Transvaginal ultrasound or pelvic examination Removal of entire tube 3. Can I assess the s/s and diagnosis of a hydatidiform mole? ● Abnormal development of placenta ● Complete Mole: empty egg with two sperm “ white grapes”46 chromosome ● Partial Mole: Normal ovum fertilized by two or more sperm, 69 or more chromosome S/S - dark brown vaginal discharge like prune juice, may pass vesicles Uterus or fundal height will be larger than usual (enlarged) Anemia from blood loss Excessive N/V hyperemesis gravidarum Preeclampsia Diagnosis - “Grape like clusters” Tranvaginal ultrasound “Snowstorm pattern” hcG level beyond high or constantly rising during a time it should be declining Intervention - Most molar pregnancy aborted spontaneously Suction curettage Emotional support 4. Can I instruct a client about a cerclage? ● Cerclage placement has been treated for women who have weak cervix or cervical insufficiency - SEWING UP CERVIX “Mcdonalds Techniques” = Suture is placed around the cervix beneath the mucosa to constrict the internal of the cervix Bedrest in recumbent position. Observation and supervision for the remainder of the pregnancy Chapter 29 (pgs. 631-632) 1. Can I assess the s/s of hyperemesis gravidarum? ● N/V begin 4-10 weeks of gestation and usually confined to the first 20 weeks of gestation Hyperemesis Gravidarum - Diet Technique “Excessive , severe vomiting”during pregnancy that causes → weight loss/dehydration electrolyte imbalances nutritional deficiencies and ketonuria Can cause esophageal rupture, Wernicke encephalopathy May have dry mucous membranes, decreased BP, increased HR and poor skin turgor Treatment: Antiemetic therapy & Iv fluids, NPO - Avoid empty stomachs Eat every 2-3 hours Eat high protein Eat dry bland, low fat food Ginger tea Liquids from cup lids Chapter 31 (pgs. 674-675) 1. Can I educate a client on the risk of commonly used drugs? ● Almost all are at risk for preterm birth, misccariage, fetal anomalies Tobacco - Low birth weight Risk of ear infection Respiratory illness SIDS ( sudden infant death) IUGR Thromboembolic problems Alcohol - Marijuana - Lack of definitive evidence Maybe IUGR, maternal health behaviors Fetal alcohol syndrome Neurodevelopmental disorder Birth defect Behavior disorders Fetal death Misccariage, stillbirth & preterm Opioids- Heroin - Cocaine - CNS stimulant Can cross placenta and breast milk Decrease blood flow to uterus Preterm labor & placenta abruptio Hypoxemia in fetus, small gestational age Baby → hypertonic & tremulous Neonatal abstinence syndrome Mom: misscariage, preterm birth, placenta abruptio Meth - Not been clearly identified Maybe lethargy and abnormal heart rate , brain anomalies, preterm birth ***Module 3*** Chapter 13 (pg 250) 1. Can I explain when the expectant woman will feel the baby move and what it is called? ● QUICKENING : flutter feeling and difficult to distinguish between peristalsis - First recognition of fetal movements “feeling of life” Nulliparous: (no births) 18 weeks or later Multiparous: (2+birth before) 14-16 weeks Chapter 14 (pgs 264, 285 and Emergency box page 274 & Table 14-2 1. Can I identify the length of each trimester? First Trimester Conception -13 weeks Second Trimester 14 weeks- 26 weeks Third Trimester 27-40 weeks 2. Can I educate the pregnant woman about normal discomforts of pregnancy? First Trimester - - - - - - - Breast changes (pain, tingling & tenderness) - due to hormonal stimulation Urgency and frequent urination ( bladder reduced by enlarging uterus - empty bladder regularly/kegel exercise) N/V & fatigue : morning sickness (may be due to increase of estrogen, hcG , hormones) (rest and eat a well balanced diet) Excessive salivation (may be due to elevated estrogen level - chew gum, hard candy) Gingivitis, hyperemia, bleeding, tender gums (estrogen stimulation// eat fruits, brush teeth gently) Nasal stuffiness: Epistaxis (mucous membrane change related to increased estrogen level) Leukorrhea (hormonal stimulated cervix) Emotional lability : mood swings ( hormonal changes, changes in lifestyle) Third Trimester Second Trimester - - Pigmentation deepens (areola, vulva, linea nigra, melasma, acne, oily skin - melanocyte stimulating hormone) Resolves 6 weeks after birth, not preventable Spider Nevi : around neck, face thorax, arms ( estrogen hormone change) will eventually fade away Pruritus (a desire to scratch, noninflammatory, unknown) keep fingernail short, lotion, reduce using soap Palpitations (Flutter feeling, unknown, contact provider if symptoms of cardiac decomposition Supine hypotension -pressure from uterus, side lying better or semi sitting with knees flexed Faintness ( postural hypotension) - moderate exercise, deep breathing , avoid sudden posture change Food cravings - not preventable ( satisfy craving, eat a well balanced diet) Heartburn (progesterone slows GI tract, avoid gassy food, large meals, fat food, antacid btw meals) Constipation ( drink 2L of water 8-10 glasses of water,, include high fiber diet) Flatulence w/ Belching ( chew food slowly, avoid gas food) Varicose Veins ( avoid standing for a long time, constrictive clothing, bearing down, rest with legs and hip elevated ) Heachaches → 26 weeks ( emotional tension, try relation therapies) Contact HCP if feeling worst headache ever → preeclampsia Carpal Tunnel Syndrome (compression due to nerves, elevate arms or splinting) Periodic Numbness & Ligament /Joint pain : stretching due to enlarging uterus - maintain good posture techniques, heat may help ) - - - - - - - Shortness of breath & dyspnea (expansion of diaphragm by enlarging uterus - keep good posture, dont smoke) Insomnia ( fetal movement, muscle cramps, SOB- effleurage, massage, bath before bedtime) Moodswings & increased anxiety (hormonal and metabolic adaptation) Urinary frequency and urgency returns ( empty bladder regularly and kegel exercise) Perineal discomfort (pressure from enlarging uterus, rest up and use good posture) Braxton Hicks contractions (uterine contractions in preparation for work labor , change positions and rest) Leg cramps when reclining: (due to compression of nerves , dorsiflex foot) Ankle edema (non pitting, can be aggravated due to prolonged standing, lack of exercise , water pooling-ample fluid for natural diuretic affect, diuretic are contraindicated 3. Can I explain vena cava syndrome and how to manage it? ● Supine hypotension which is a low blood pressure that occurs when a woman is lying on her back ● Pressure of uterus on ascending vena cava ● Reduced uteroplacental and renal perfusion S/S - Intervention Pallor Dizziness Fairness Breathlessness Tachycardia Clammy Sweating - LEFT side position Side lying position or semi sitting posture with knees flexed Position women on her side until s/s resolves FLIP FLUID O2 Chapter 26 [pgs 571-572 (Table 26.2 & Table 26.3) & 575 1. Can I explain a BPP and the indications of results? ● Amniotic fluid must be 2 pts for normal BPP or any Inducing ● Noninvasive dynamic assessment of a fetus based on acute and chronic markers of fetal disease ● Physical examination of fetus ● BPP 8-10 = Normal & low risk for asphyxia ● BPP 4-6 = suspects chronic asphyxia ● BPP 0-2 = strongly suspect asphyxia Variable 2 points 0 Points Fetal breathing movement (FBM) One episode of fetal breathing movements of at least 30-secs in a 30-min observation. Absent fetal breathing movements or less than 30-secs in a 30-min observation Fetal Movements At least three trunk/limb movements in 30-min Fewer than three episodes of trunk/limb movements in 30-min Fetal Tone At least one episode of active extension with return to flexion of fetal limb or trunk Absence of movement or slow extension/flexion Amniotic Fluid Index (AFI) AFI > 5cm or at one pocket > 2cm AF < 5cm or no pocket > 2cm Nonstress Test (NST) FHR Reactive Non Reactive 2. Can I explain the Maternal Assay AFP? ● Maternal serum alpha fetoprotein (***a-Fetoprotein) is USED AS A SCREENING TOOL ONLY ) not diagnosis) for neural tube defects in pregnancy , performed in 15-20 weeks Compared each week with normal values - If AFP is elevated → ultrasound evolution or further testing needed Chapter 27 [pgs 583-586 (Look at all Tables and Boxes 27-1, 2, 3), 592-596 & emergency box] 1. Can I explain and assess the signs and symptoms of Preeclampsia? ● Pregnancy specific condition in which hypertension plus one of the following damage to another organ system at 20 weeks gestations ● Placenta as the root cause , poor perfusion as a result of vasospasm and reduced plasma level Preeclampsia - - Eclampsia Hypertension + 1 or more of the following → Proteinuria +1 → thrombocytopenia → impaired liver function → renal insufficiency, not urination → Hyperreflexia → Pitting edema Complications: CNS irritability, clonus, headaches, hyperreflexia, ankle clonus and seizure, uterine contractions, abdominal pain, spotting, decreased fetal movements 140/90 or higher (BP) +1 Proteinuria Assessment: Edema & DTR assessment, urine dipstick, blood pressure, LOC, ausclate sound breath Low dose of aspirin found to reduce preeclampsia *seizure precaution **Daily fetal movements 10 Adequate bed rest, protein & fluid intake, magnesium sulfate ➔ SEIZURE CAUTION ➔ Development of seizure or coma in women with preeclampsia Have suctioning equipment ready to use Maintain patent airway Blurred vision, tonic contractions alter LOC, right upper Quadrant, abdominal pain TREATMENT = Magnesium sulfate Multiple organ failure = HELLP A variety of preeclampsia that involves hepatic dysfunction - *1 or 2 features for diagnosis ● ● H Hemolysis (rupturing of rbc) EL Elevated Liver Enzymes LP Low Platelets 2. Can I educate the PIH client on the side effects of Magnesium Sulfate? S/s of Magnesium sulfate toxicity? ● Medication of choice for preventing and treating seizure activity , cns depressant, relaxes smooth muscle ● Neuroprotector Normal Adverse side effects - Lethargic Flushed feeling x10 Feeling of warmth Diaphoresis Slurred speech Visual blurring N/V TOXIC S/S - Absent DTR Decreased RR and decreased LOC Crackles Assess respiratory status & urine output less than 30cc Antidote for toxicity : Calcium gluconate /chloride Keep antidote at bedside **Discontinue infusion, notify provider 3. Can I explain the reasons for Magnesium Sulfate administration? - Magnesium Sulfate Medication of choice for preventing and treating seizure activity , cns depressant, relaxes smooth muscle (preeclampsia & eclampsia) Also used as a radioprotector to prevent neonatal morbidity (cerebral palsy ) Anti Seizure/Anticonvulsant Tocolytics Chapter 32 (pgs 686-689 & Medication Guide) 1. Can I assess the pregnant woman before administration of Terbutaline? Terbutaline, a tocolytic, is commonly administered to relax the uterine smooth muscle by stimulating beta 2 receptors. Stops a woman from contraction, slows down labor, delays birth **Antidote → propranolol*** - ***GIVES YOU EXTREME TACHYCARDIA Do not admin to patient who is already TACHY Assess client before Tachycardia Any known HEART DISEASE Preeclampsia with severe features or eclampsia Diabetes Assess for hypoglycemia or hyperglycemia 2. Can I explain Antenatal Glucocorticoid Therapy (Betamethasone)? Betamethasone glucocorticoid: helps accelerate fetal lung maturity by stimulation fetal surfactant productions Given Intramuscular Reduces incidence of respiratory distress syndrome, hemorrhage, death of neonates w/o increasing infection - Can cause HYPERGLYCEMIA in clients Predispose newborn to HYPOGLYCEMIA - *** DO NOT GIVE TO MOTHERS WHO HAVE HYPERTENSION/HYPOTENSION, OR CARDIAC DISEASE Side effects: hypotension, headache, fluzzing, dizziness, nausea 3. Can I evaluate the medication Nifedipine? Nifedipine: CCB is a tocolytic agent that can suppress contractions. Works by preventing calcium from entering smooth muscle, thus reducing contractions - DO NOT ADMIN WITH MAGNESIUM SULFATE - DO NOT ADMIN SUBLINGUALLY - ***Module 4*** Chapter 14 (pg. 275) 1. Can I instruct a client on the Group B Strep screening? Infection Maternal Effects/ Group B streptococcus (3rd trimester) (can be considered as normal flora in women who aren’t pregnant, but can be fatal for baby ) ALL PREGNANT women should gave GBS testing since membranes can rupture - Fetal Effects UTI , choroianminotits (bacteria infection) Postpartum endometritis Sepsis , meningitis ( rare) urine & vaginal culture ***should be screened at 35-37 weeks gestation Intravenous prophylaxis = Penicillin - Preterm birth Can be fatal During active labor need antibiotics Chapter 19 (pgs. 386-387) 1. Can I assess the findings obtained from performing the Leopold Maneuvers? ● **Leopold Maneuver (3rd trimester) - Which fetal part is in the uterine fundus? Where is the fetal back located? What is the presenting fetal part? Fetal size after 24 weeks What's in the fundus, what's the fetal position? Presenting part? Point of maximal intensity of fetal heart is usually directly over the FETAL BACK - Fetal presentation, position, lie , head engagement First A: Fundal Grip : the uterine fundus is palpated to determine which fetal part occupies the fundus = FETAL LIE Note the shape, consistency , mobility of the palpated part ? What's on top of the fundus? Round soft = butt, round firm = head Second B: Lateral grip : Each side of the maternal abdomen is palpated to determine which side is fetal spine or extremities Cephalic, breech, shoulder? FETAL PRESENTATION Smooth or bumpy ? Onto the side, where is the back? Smooth = back , lumpy = extremities *Fetal tones best heard in the back Third C: Pawliks grip: The area above the symphysis pubis is palpated to locate the fetal presenting part and thus determine how far the fetus has descended and whether is engaged? WHAT PART IS PRESENTING OVER THE INLET OF TRUE PELVIS Head engagement? What's in the pelvis? Firm or soft? Fourth D: First pelvic grip. One hand applies pressure on the fundus while the index finger and thumb of the other hand palpate the present part to confirm presentation engagement Cephalic prominence? Where is the head IS IT FLEXED OR EXTENDED? Chapter 21 (pgs. 433-434) 1. Can I assess a client’s rubella and varicella status? ● For women who are not vaccinated or immune = NEGATIVE TITER (1:8/enzymes) Rubella - - Varicella For those who are non immune , SUB-Q injection → postpartum vaccine recommended for protection of future pregnancy **Avoid becoming pregnant for 28 days after being vaccinated Breastfeeding OK Should not be given to immunocompromised pt as the virus sheds in urine and other body fluids - Recommend client to get vaccine before discharge 2nd dose given at postpartum checkup 4-8 weeks **Avoid becoming pregnant for 28 days after being vaccinated 2. Can I instruct a client on the need for RhoGAM? ● When a Rh- mom is pregnant with a Rh+ baby **Rh Immunization - Administration of Rh immune globulin is intended to prevent problems in future pregnancies should the Rh- negative women have Rh-positive fetus Routine antepartum prevention at 28 weeks of gestation in women with Rh negative blood Give standard dose within 72 h after birth if neonate is Rh-positive to mom Observe client 20 minutes after administration Medication is made from human plasma ( consider those who are religious & educate) Coombs Test : screening for Rh incompatibility Rhogam ( for mother rh-, incase fetus is rh+) ● Rh compatibility : done on mom who are rh( -) , check to see if baby is rh (+) ● Protect future pregnancy Detects antibodies that act against the surface of your RBC Leads to fetal anemia ***Rhogam @ 28 weeks as prophylactic & 72 hours after birth(tricks mom into not producing antibodies that fight babies blood) (if mom and dad are negative, baby usually is negative too) Direct Coombs - Done on baby (newborn of baby , mom rH negative) If mom is positive , test doesn't need to be done If mom is negative, test has to be done Indirect Coombs - Done on mom (antibodies that are floating freely in the blood) Chapter 26 (pgs. 573-574, 578-581 and figs 26-9 through 26-12) 1. Can I assess the indication for an amniocentesis in the 2nd, and 3rd trimester? ***Amniocentesis*** (module 2) - To obtain amniotic fluid that contains fetal cells Done with Ultrasonographic visualization Done after 14 weeks when uterus becomes abdominal organ **2nd trimester done for genetic issues ( lung is not mature yet)--> NTD, spina bifida **3rd trimester done to see lung maturity & diagnosis of hemolytic disease Diagnose fetal defects Can determine fetal immaturity Rhogam for Rh negative women after procedure 2. Can I evaluate the results of a CST (contraction stress test)? ● A contraction stress test (oxytocin challenge test) identifies a jeopardized fetus that was stable at rest but shows evidence of compromise after stress ● Can be used with nipple stimulation or IV oxytocin Contraction Stress Test (CST) Contraindications : preterm labor, placenta previa, vasa previa , cervical insufficiency - Negative (GOOD) No late decelerations Associated with good fetal outcomes Minimum of 3 contractions in 10 minutes with NO decelerations Negative= baby can tolerate labor - Positive (BAD) Do not want decelerations Repetitive late decelerations with more than 50% contractions Positive results associated with intrauterine fetal death, IUGR, meconium stained amniotic fluid 3. Can I evaluate the results of a NST (Nonstress test)? ● Checks the well being of the fetus ● Twice a week testing to evaluate fetus heart patterns, movement to simulation, contractions ● 20 - 30 minute process Nonstress Test (NST) Can drink orange juice for stimulation or vibroacoustic stimulation - Mom clicks button when she feels fetal movement Reactive (GOOD) 2 accelerations in a 20 minute period lasting 15 seconds each (15x15) - Nonreactive (BAD)(further eval contraction test or BPP) DOES NOT demonstrate at least two qualifying acceleration within 20 minute period Fetus can be sleeping → give OJ or stimi but still none after 40 minutes total = more eval 3. Can I assess the metabolic changes associated with pregnancy? ( last question moved here) ● Pregnancy is characterized by alterations in glucose metabolism, insulin production and metabolic homeostasis ● Glucose can cross placenta but NOT insulin ● Baby makes their own insulin 1st Trimester Womens metabolic status is influenced by rising levels of estrogen and progesterone - Increase insulin production, use of glucose and tissue glycogen as storage Decrease in levels of blood glucose & liver glucose production Women who are insulin dependent diabetes are prone to HYPOGLYCEMIA 2nd & 3rd Trimester “Diabetogenic effect” on maternal metabolic status - Increased insulin resistance and liver glucose production Decrease in glucose tolerance & liver glycogen storage ENSURES maximum glucose for the fetus - Chapter 28 (607-611) 1. Can I assess the s/s of placenta previa and abruptio placenta? *Placenta Previa* *Abruptio Placentae * Placenta implanted is completely or partially covering the cervix which is close enough to cause bleeding in 2 or 3rd trimester Detachment or tear of placenta from the uterus Signs/Symptoms - PAINLESS - bright red vaginal bleeding - abdominal is relaxed - nontender & soft Fundal height greater than gestational age - At risk = history of c-section & smoking Complications: hemorrhage to mom & preterm baby Interventions Usually given birth by c-section Betamethasone is given Tocolytics to be given if bleeding process with contractions - No rectal or Vagina examination are perfomred Assess maternal vital signs & fetal monitoring Signs/Symptoms - PAINFUL - Sudden onset of intense pain in uterus Pain in one region Board like abdomen w/ or w/o bleeding dark red vaginal bleeding Tenderness Uterine rigidity - At risk = maternal hypertension, cocaine or abdominal trauma , cigarette smoking Complications: hemorrhage to mom, hypovolemic shock, thrombocytopenia. IUGR in fetus, hypoxemia and stillbirth Interventions If mom and baby are stable = monitor - If bleeding is moderate to severe = immediate birth Chapter 29 (pgs. 615-630) 1. Can I evaluate the care management pertaining to the screening for gestational diabetes mellitus ● All pregnant women who do not have gestational diabetes should be screened at 24-28 weeks gestation ● Precondition counseling is recommended for all women of the reproductive age who have diabetes because it is associated with less perinatal mortality and fewer preterm birth and congenital anomalies Medications that carry adverse maternal and fetal outcomes should be changed to ones that are safer but equally effective Discussion of microvascular and macrovascular complications carry a significant risk for maternal morbidity and mortality during pregnancy → coronary artery disease and renal insufficiency Establish glycemic control ideally before conception and plan optimal timing for pregnancy 2. Can I instruct a diabetic client about the importance of preconception counseling and the possible risk factors to the infant? Pregestational Diabetes Mellitus - - - Type 1 or Type 2 diabetes that existed BEFORE pregnancy Women with insulin dependent diabetes are prone to hypoglycemia (also for babies during birth) Mom Complications: c-section, hypertension, preeclampsia, preterm baby, mortality , hydramnios ( too much amniotic fluid) , infections, UTI , stillbirth Baby Complications : macrosomia (sumo heavy baby), shoulder dystocia, congenital anomalies , FGR (fetal growth restriction) , neural tube defects, spina bifida Assessment: urine collection, A1c, baseline renal function Routine every 1-2 weeks for 1st&2nd trimester Routine visit 1-2 times a week for 3rd trimester 60-105mg/dl before meals 140 mg/dl or less after meal 1 hour Skin & foot care is important Average 2200 calories, maintain balanced diet , exercise 30 mins, walking , swimming Gestational Diabetes Mellitus - Diabetes diagnosed during the second half of the pregnancy Screened around 24-28 weeks gestation Glucose tolerance & GTT test - - 1h-glucose test (50-g oral glucose ) → no fasting → 130-140 mg/dl = positive screen → positive continue to step 2 on another day - 3h-glucose test (100-g oral glucose) → overnight fasting → avoid CAFFEINE (increases glucose level) → avoid SMOKING → glucose level drawn 1, 2, and 3 hours later → 2 elevated values from reading = GDM confirmed - - - Mom Complications : preeclampsia, development of type 2 diabetes after pregnancy , preterm, misccariage, hypertension, mortality, hydramnios, shoulder dystocia Baby Complications : not found due to critical formation usually in first trimester for development , congenital malformations , macrosomia, respiratory distress Measure glucose hourly 4. Factors affecting labor : Five P’s of Labor & Birth Passenger (fetus and placenta) -size of the head -fetal presentation : part of the body first felt by the examiner in cervix (cephalic = occipital) (breech = sacrum) (shoulder = scapula) -fetal lie : in relation of the fetus spine to mothers spine (longitudinal , vertical, transverse, horizontal, oblique) (transverse=c section) The fetus Size of the head ( fontanel) Fetal Presentation Fetal Lie Fetal Attitude Vertex Flexed “Head tucked in” Military “Straight” Brow “ hyperextension of face” Face “Face looking at hole” - Fetal Position (Station/engagement) (in relation to moms body) →** Posterior will push against moms coccyx (head on coccyx) & diameter is wider → Where is Occipital in relation to mom? → Anterior is GOOD ROP (Bad) ROT (csection) ROA (Good) OP LOP (Bad) LOT (csection) LOA (Good) OA Complete Breech Incomplete Breech Frank Breech Footling Indian style butt comes out first One straight leg up Both legs straight up, baby folded in half, easier than complete to come out One leg in ischial spine Cord prolapse (can fall through the foot) -fetal attitude : fetal body part to one another -fetal position Passegway (birth canal) Composed of mothers rigidity bone pelvis and the soft tissues of the cervix, the pelvic floor, the vagina and external opening of vagina Powers (contractions) - Engagement : head corresponds at 0 station - Birth canal & Pelvis Gynecoid = Best Position Platypelloid = Worst Position Coccyx = ex. (OP) baby will be pushing on the coccyx - painful - Know the ischial spine ● ● Primary Powers (involuntary): Contractions - signals beginning of labor Frequency, Duration, Intensity, Effacement, Dilations, Ferguson reflex Secondary Powers : Mom pushing / Bearing down / Valsalva maneuvers - When cervix is fully dilated , the women will feel a urge to push and involuntary bear down The urge to push is triggered by the ferguson reflex, when presenting part stretches the pelvic muscles → oxytocin stimulation for contractions Position - Upright positions, All fours, Lithomony, Semirecumbent , Lateral , Squatting, Kneeling Help decrease the cpm[ression of the maternal descending aorta and ascending vena cava that can compromise cardiac output Psychological Response - Cultural beliefs // Anxiety level Environment // All women are different