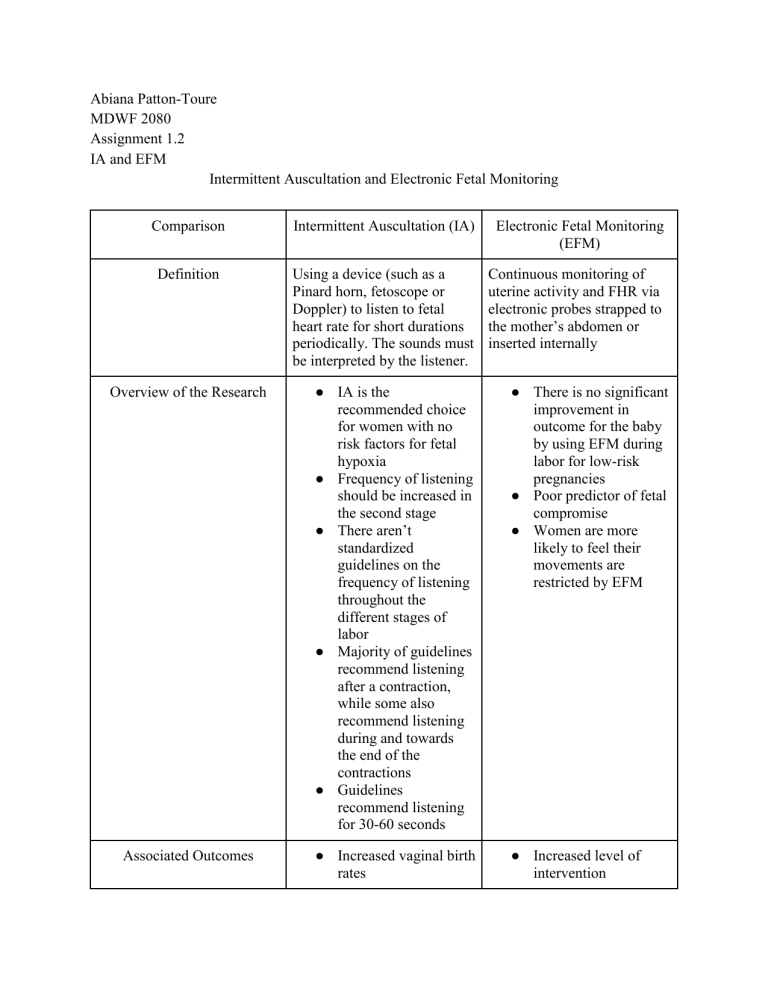
Abiana Patton-Toure MDWF 2080 Assignment 1.2 IA and EFM Intermittent Auscultation and Electronic Fetal Monitoring Comparison Intermittent Auscultation (IA) Electronic Fetal Monitoring (EFM) Definition Using a device (such as a Pinard horn, fetoscope or Doppler) to listen to fetal heart rate for short durations periodically. The sounds must be interpreted by the listener. Continuous monitoring of uterine activity and FHR via electronic probes strapped to the mother’s abdomen or inserted internally Overview of the Research ● IA is the recommended choice for women with no risk factors for fetal hypoxia ● Frequency of listening should be increased in the second stage ● There aren’t standardized guidelines on the frequency of listening throughout the different stages of labor ● Majority of guidelines recommend listening after a contraction, while some also recommend listening during and towards the end of the contractions ● Guidelines recommend listening for 30-60 seconds ● There is no significant improvement in outcome for the baby by using EFM during labor for low-risk pregnancies ● Poor predictor of fetal compromise ● Women are more likely to feel their movements are restricted by EFM Associated Outcomes ● Increased vaginal birth rates ● Increased level of intervention ● Lower neonatal admission to NICUs ○ Epidural ○ Fetal blood sampling ● Increase in operative and assisted delivery rates ● Does not reduce perinatal mortality or the incidence of cerebral palsy When they shouldn’t be used ● When the fetus is atrisk for fetal hypoxia ○ Suspected maternal infection ● Non-reassuring FHT heard ● Against the mother’s wishes ● When there isn’t a clear indication for it ● Against the mother’s wishes Risks ● Heart tones must be interpreted by the listener ● Many practitioners may not listen long enough to get an accurate rate ● Cannot detect decels, accelerations or variability ● May not be heard by all people present ● Lower detection rates of fetal distress ● Low specificity (ability to identify fetuses that aren’t distressed) ● Poor predictive value of adverse fetal outcomes ● High rate of error ● Falsely identifies “fetal distress” ● May induce medical or non-medical anxiety ● Presents a physical barrier to “hands on” support during labor ● Limits mobility ● Diminishes a woman’s confidence in her ability to safely give birth without technology ● Low risk ● Cannot typically ● Linked to reduction in neonatal seizures Benefits interpret decels, acels or variability ● Provides freedom of movement Who is a candidate ● Low-risk clients for labor and birth complications ● Suspected maternal or fetal infection ● Long ROM ● GBS+ (esp. if declining antibiotics) ● Placenta previa or any other suspected placental issues ● Those who IA is not suitable for (potential high BMIs where FHT cannot be heard easily) ● Confined clients ● Clients who prefer the reassurance of EFM ● Clients with hx of PTB, infection, short cervix, pre or post term babies ● Fetuses at-risk for or with known specific genetic defects (i.e congenital heart defects) Additional research ● There is a lack of clear evidence to guide the frequency of IA ●






