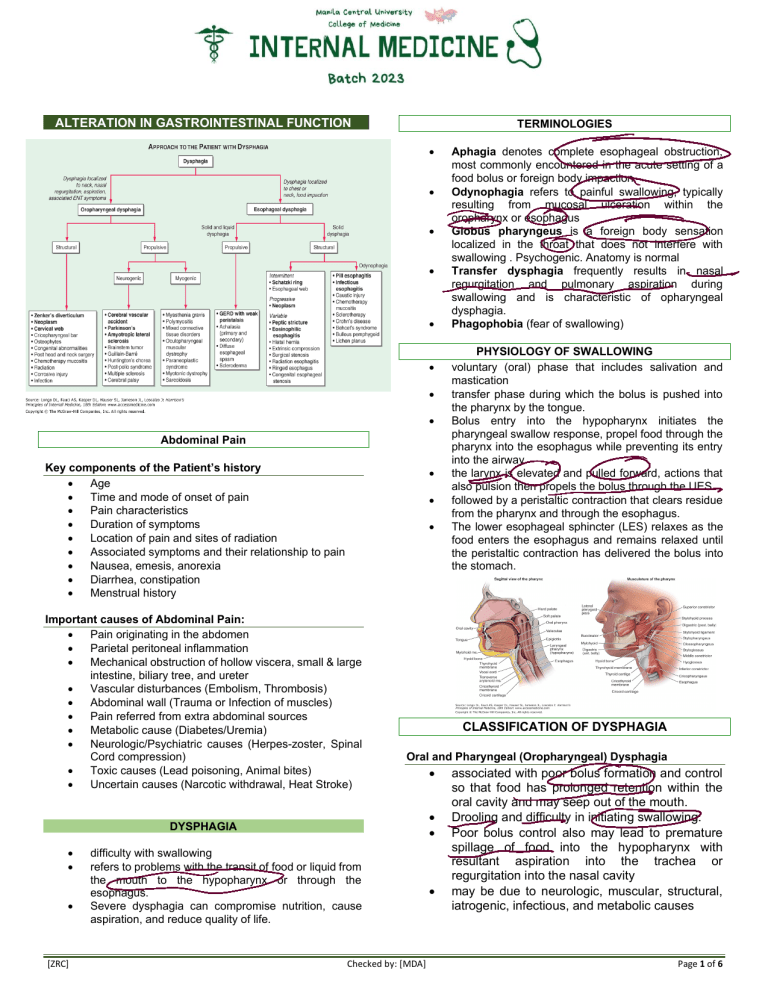
ALTERATION IN GASTROINTESTINAL FUNCTION TERMINOLOGIES • • • • • • • • Abdominal Pain Key components of the Patient’s history • Age • Time and mode of onset of pain • Pain characteristics • Duration of symptoms • Location of pain and sites of radiation • Associated symptoms and their relationship to pain • Nausea, emesis, anorexia • Diarrhea, constipation • Menstrual history • • • Important causes of Abdominal Pain: • Pain originating in the abdomen • Parietal peritoneal inflammation • Mechanical obstruction of hollow viscera, small & large intestine, biliary tree, and ureter • Vascular disturbances (Embolism, Thrombosis) • Abdominal wall (Trauma or Infection of muscles) • Pain referred from extra abdominal sources • Metabolic cause (Diabetes/Uremia) • Neurologic/Psychiatric causes (Herpes-zoster, Spinal Cord compression) • Toxic causes (Lead poisoning, Animal bites) • Uncertain causes (Narcotic withdrawal, Heat Stroke) • [ZRC] PHYSIOLOGY OF SWALLOWING voluntary (oral) phase that includes salivation and mastication transfer phase during which the bolus is pushed into the pharynx by the tongue. Bolus entry into the hypopharynx initiates the pharyngeal swallow response, propel food through the pharynx into the esophagus while preventing its entry into the airway. the larynx is elevated and pulled forward, actions that also pulsion then propels the bolus through the UES followed by a peristaltic contraction that clears residue from the pharynx and through the esophagus. The lower esophageal sphincter (LES) relaxes as the food enters the esophagus and remains relaxed until the peristaltic contraction has delivered the bolus into the stomach. CLASSIFICATION OF DYSPHAGIA Oral and Pharyngeal (Oropharyngeal) Dysphagia • • • DYSPHAGIA • • Aphagia denotes complete esophageal obstruction, most commonly encountered in the acute setting of a food bolus or foreign body impaction. Odynophagia refers to painful swallowing, typically resulting from mucosal ulceration within the oropharynx or esophagus Globus pharyngeus is a foreign body sensation localized in the throat that does not interfere with swallowing . Psychogenic. Anatomy is normal Transfer dysphagia frequently results in nasal regurgitation and pulmonary aspiration during swallowing and is characteristic of opharyngeal dysphagia. Phagophobia (fear of swallowing) difficulty with swallowing refers to problems with the transit of food or liquid from the mouth to the hypopharynx or through the esophagus. Severe dysphagia can compromise nutrition, cause aspiration, and reduce quality of life. Checked by: [MDA] • associated with poor bolus formation and control so that food has prolonged retention within the oral cavity and may seep out of the mouth. Drooling and difficulty in initiating swallowing. Poor bolus control also may lead to premature spillage of food into the hypopharynx with resultant aspiration into the trachea or regurgitation into the nasal cavity may be due to neurologic, muscular, structural, iatrogenic, infectious, and metabolic causes Page 1 of 6 INTERNAL MEDICINE OCTOBER 9, 2020 • • Endocrine / metabolic disorders (Pregnancy, Uremia. Thyroid disorders) Toxins (Liver failure, Alcohol) DYSPEPSIA (GASTROESOPHAGEAL REFFLUX DISEASE) Esophageal Dysphagia • abnormalities of peristalsis and/or deglutitive inhibition, potentially affecting the cervical or thoracic esophagus. • • NAUSEA, VOMITING, AND INDIGESTION • • • • • • Nausea is the subjective feeling of a need to vomit. Vomiting (emesis) is the oral expulsion of gastrointestinal contents resulting from contractions of gut and thoracoabdominal wall musculature. Regurgitation, the effortless passage of gastric contents into the mouth. Rumination is the repeated regurgitation of stomach contents, which may be rechewed and reswallowed. Indigestion is a nonspecific term that encompasses a variety of upper abdominal complaints including nausea, vomiting, heartburn, regurgitation, and dyspepsia Dyspepsia refers to upper abdominal pain or discomfort DYSPEPSIA • • • Types is coordinated by the brainstem and is affected by responses in the gut, pharynx, and thoracoabdominal wall. 1. Uninvestigated Dyspepsia- no work up of upper GI endoscopy done 2. Functional Dyspepsia- patients with dyspepsia but negative upper GI endoscopy DYSPEPSIA (PEPTIC ULCER DISEASE) CAUSES OF VOMITING: 1. 2. Intraperitoneal • Obstructing Disorders (Intestinal Obstruction) • Enteric infections • Inflammatory diseases (Cholecystitis, Pancreatitis, Appendicitis, Hepatitis) • Altered Sensorimotor function (Gastroesophageal reflux disease) Means upper abdominal discomfort. Usually located in the epigastrium Symptoms are: epigastric pain/burning sensation, early satiation, postprandial fullness Common causes • Gastritis, gastric/duodenal ulcers • Work up is upper GI endoscopy, test for Helicobacter pylori infection VOMITING • Symptoms are caused by back flow of gastric acid and other gastric contents into the esophagus due to incompetent barriers at the gastroesophageal junction Heartburn symptoms • epigastric pain aggravated by hunger, relieved by food or antacids DUODENAL BULB ENDOSCOPY: ULCER SEEN ON UPPER GI Extraperitoneal • Cardiopulmonary disease (myocardial infarction) • Labyrinthine disease (Motion sickness) • • • Intracerebral disorders Hemorrhage, Abscess) Psychiatric illness (Depression) Postoperative vomiting (Malignancy, 3. Medications / Metabolic • Drugs (Cancer chemotherapy, antibiotics, cardiac drugs) [ZRC] Checked by: [MDA] Page 2 of 6 INTERNAL MEDICINE • • • • • • • • • • OCTOBER 9, 2020 ALARM SYMPTOMS OF DYSPEPSIA dysphagia Unexplained weight loss Recurrent Vomiting Early satiety Occult or gross gastrointestinal bleeding Jaundice Palpable mass or adenopathy Family history of GI malignancy The presence of Alarm Symptoms suggests malignancy! Proper investigation should be done e.g gastroscopy or upper endoscopy CONSTIPATION • • • persistent, difficult, infrequent, or seemingly incomplete defecation. Less than 3 bowel movements per week complain of excessive straining, hard stools, lower abdominal fullness, or a sense of incomplete evacuation. DIARRHEA • passage of abnormally liquid or unformed stools at an increased frequency Classification : • Acute if <2 weeks • Persistent if 2–4 weeks, and • Chronic if >4 weeks in duration. [ZRC] Checked by: [MDA] Page 3 of 6 INTERNAL MEDICINE OCTOBER 9, 2020 Colonoscopy • • Endoscopic procedure that is used directly to visualiza the colon up to the ileo-cecal valve Used to screen for colonic polyps and colon cancer CAUSES OF ISOLATED HYPERBILIRUBINEMIA • • JAUNDICE due to accumulation of bilirubin in the bloodstream causes yellow pigmentation of plasma, discoloration of heavily perfused tissues Can be detected when serum bililrubin level exceeds 34 to 43 mmol/L (2.0 to 2.5 mg/dl) Indirect Hyperbilirubinemia • Hemolytic disorders • Ineffective erythropoiesis (Cobalamin, folate, iron defeciencies) • Drugs (Rifampicin) • Inherited conditions (Crigler-Najjar, syndrome) Direct hyperbilirubinemia • Dubin- Johnson and Rotor syndrome HEPATOCELLULAR CONDITIONS THAT MAY PRODUCE JAUNDICE • • • • • • CLINICAL SIGNS OF JAUNDICE: • • • Gilbert’s Scleral icteresia – a sensitive sign. Sclera is rich in elastin Darkening of the urine, tea-colored or beer colored Differential dx – carotenemia: only the skin is yellowish but not the sclera Viral hepatitis Hepatitis A,B,C,D,E Alcohol Drug toxicity – isoniazid, acetaminophen Environmental toxins Wilson’s disease Autoimmune hepatiis CHOLESTATIC CONDITIONS THAT MAY PRODUCE JAUNDICE Intrahepatic • Hepatitis • Drug toxicity – erythromycin • TB, Lymphoma, Malaria, Leptospirosis Extrahepatic (seen on ultrasound, CT scan, MRI, ERCP) • Malignant – Cholangiocarcinoma, Pancreatic and Ampullary and Gallbladder CA • Benign - Choledocholithiasis [ZRC] Checked by: [MDA] Page 4 of 6 INTERNAL MEDICINE OCTOBER 9, 2020 ASCITES ERCP (Endoscopic Pancreatography) Retrograde Cholangio CHOLANGIOGRAM • • Accumulation of fluid in the peritoneal cavity Presence of fluid wave and shifting dullness on physical examination PARACENTESIS A simple bedside procedure in which a needle is inserted into the peritoneal cavity and ascitic fluid is removed. APPROACH TO PATIENT WITH JAUNDICE • • • • determine if the patient has an isolated elevation of serum bilirubin. is the bilirubin elevation due to an increased unconjugated or conjugated fraction? If the hyperbilirubinemia is accompanied by other liver test abnormalities is the disorder hepatocellular or cholestatic? If cholestatic, is it intra- or extrahepatic? ABDOMINAL SWELLING CAUSES: 6 F’s • Flatus • Fat • Fluid • Fetus • Feces • Fatal growth (often a neoplasm) [ZRC] SAAG (SERUM-ASCITES ALBUMIN GRADIENT) • SAAG is calculated by subtracting the ascitic albumin from the serum albumin • SAAG > 1.1 g/dl reflect the presence of portal hypertension Checked by: [MDA] Page 5 of 6 INTERNAL MEDICINE OCTOBER 9, 2020 HOW TO PREVENT DIGESTIVE DISEASES Encourage high fiber diet Avoid hepatotoxic drugs, herbal drugs, or food supplements • Screen for colon cancer • Adopt a healthy lifestyle • • References: • • Digestive System PPT lecture 2020 Harrison’s Principle of Internal Medicine 20th edition “Eat your breakfast always” -Zhon Pogi, 2020 [ZRC] Checked by: [MDA] Page 6 of 6


![Dysphagia Webinar, May, 2013[2]](http://s2.studylib.net/store/data/005382560_1-ff5244e89815170fde8b3f907df8b381-300x300.png)