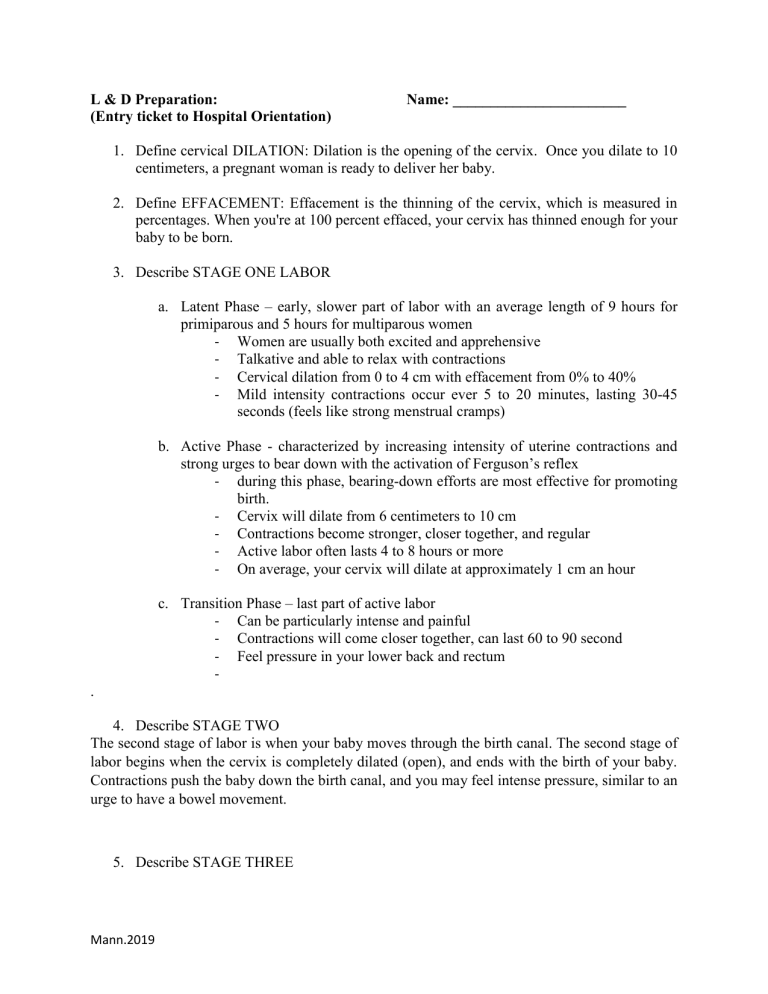
L & D Preparation: (Entry ticket to Hospital Orientation) Name: _______________________ 1. Define cervical DILATION: Dilation is the opening of the cervix. Once you dilate to 10 centimeters, a pregnant woman is ready to deliver her baby. 2. Define EFFACEMENT: Effacement is the thinning of the cervix, which is measured in percentages. When you're at 100 percent effaced, your cervix has thinned enough for your baby to be born. 3. Describe STAGE ONE LABOR a. Latent Phase – early, slower part of labor with an average length of 9 hours for primiparous and 5 hours for multiparous women - Women are usually both excited and apprehensive - Talkative and able to relax with contractions - Cervical dilation from 0 to 4 cm with effacement from 0% to 40% - Mild intensity contractions occur ever 5 to 20 minutes, lasting 30-45 seconds (feels like strong menstrual cramps) b. Active Phase - characterized by increasing intensity of uterine contractions and strong urges to bear down with the activation of Ferguson’s reflex - during this phase, bearing-down efforts are most effective for promoting birth. - Cervix will dilate from 6 centimeters to 10 cm - Contractions become stronger, closer together, and regular - Active labor often lasts 4 to 8 hours or more - On average, your cervix will dilate at approximately 1 cm an hour c. Transition Phase – last part of active labor - Can be particularly intense and painful - Contractions will come closer together, can last 60 to 90 second - Feel pressure in your lower back and rectum . 4. Describe STAGE TWO The second stage of labor is when your baby moves through the birth canal. The second stage of labor begins when the cervix is completely dilated (open), and ends with the birth of your baby. Contractions push the baby down the birth canal, and you may feel intense pressure, similar to an urge to have a bowel movement. 5. Describe STAGE THREE Mann.2019 The third stage of labor is when your uterus continues to contract to push out the placenta (afterbirth) after your baby’s birth. The placenta usually delivers about 5 to 15 minutes after the baby arrives. 6. How is DURATION of contractions measured? Duration is timed from when you first feel a contraction until it is over. This time is usually measured in seconds. 7. How is FREQUENCY of contractions measured? Frequency is timed from the start of one contraction to the start of the next. 8. Describe each of the following FETAL HEART RATE PATTERNS: (THINK VEAL CHOP) a. Accelerations: Accelerations are short-term rises in the heart rate of at least 15 beats per minute, lasting at least 15 seconds. Accelerations are normal and healthy. They tell the doctor that the baby has an adequate oxygen supply, which is critical. b. Early Decelerations: A deceleration is a decrease in the fetal heart rate below the fetal baseline heart rate. An early deceleration is defined as a waveform with a gradual decrease and return to baseline with time from onset of the deceleration to the lowest point of the deceleration >30 seconds. c. Late Decelerations: A late deceleration is a symmetric fall in the fetal heart rate, beginning at or after the peak of the uterine contraction and returning to baseline only after the contraction has ended (Figure 6). The descent and return are gradual and smooth. d. Variable Decelerations: Variable decelerations are irregular, often jagged dips in the fetal heart rate that look more dramatic than late decelerations. Variable decelerations happen when the baby's umbilical cord is temporarily compressed. This happens during most labors. 9. List 3 non-pharmacologic methods of pain control for the laboring woman: Birthing ball, patterned breathing, movement and position changes, counter-pressure, touch and massage, armotherapy 10. List 2 NANDA 2018 nursing diagnoses which may apply to the laboring woman: Mann.2019 • Readiness for enhanced health literacy • Ineffective adolescent eating dynamics • Ineffective child eating dynamics • Ineffective infant eating dynamics • Risk for metabolic imbalance syndrome • Imbalanced energy field • Risk for unstable blood pressure • Risk for complicated immigration transition • Neonatal abstinence syndrome • Acute substance withdrawal syndrome • Risk for acute substance withdrawal syndrome • Risk for surgical site infection • Risk for dry mouth • Risk for venous thromboembolism • Risk for female genital mutilation • Risk for occupational injury • Risk for ineffective thermoregulation 11. What is gestational hypertension? What is Pre-Eclampsia? What is Eclampsia? How do they differ? Gestational hypertension is diagnosed when blood pressure readings are higher than 140/90 mm Hg in a woman who had normal blood pressure prior to 20 weeks and has no proteinuria (excess protein in the urine). Preeclampsia is diagnosed when a woman with gestational hypertension also has increased protein in her urine. Preeclampsia and eclampsia are pregnancy-related high blood pressure disorders. Preeclampsia is a sudden spike in blood pressure. Eclampsia is more severe and can include seizures or coma. Mann.2019