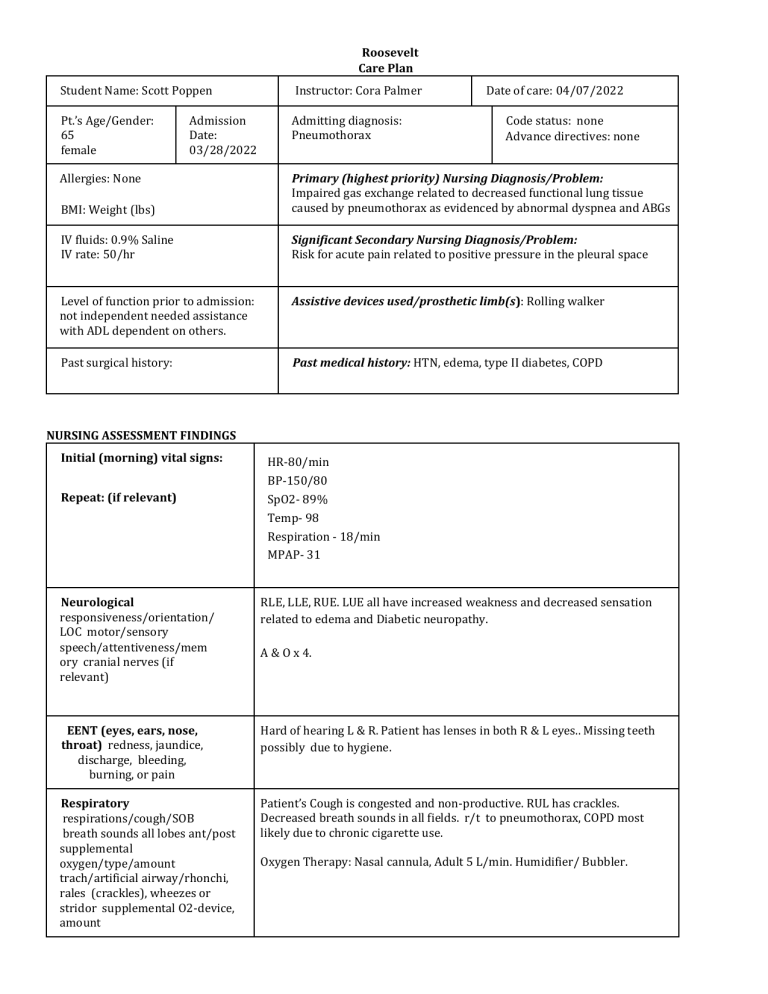
Roosevelt Care Plan Student Name: Scott Poppen Pt.’s Age/Gender: 65 female Admission Date: 03/28/2022 Allergies: None Instructor: Cora Palmer Admitting diagnosis: Pneumothorax Date of care: 04/07/2022 Code status: none Advance directives: none BMI: Weight (lbs) Primary (highest priority) Nursing Diagnosis/Problem: Impaired gas exchange related to decreased functional lung tissue caused by pneumothorax as evidenced by abnormal dyspnea and ABGs IV fluids: 0.9% Saline IV rate: 50/hr Significant Secondary Nursing Diagnosis/Problem: Risk for acute pain related to positive pressure in the pleural space Level of function prior to admission: not independent needed assistance with ADL dependent on others. Assistive devices used/prosthetic limb(s): Rolling walker Past surgical history: Past medical history: HTN, edema, type II diabetes, COPD NURSING ASSESSMENT FINDINGS Initial (morning) vital signs: Repeat: (if relevant) HR-80/min BP-150/80 SpO2- 89% Temp- 98 Respiration - 18/min MPAP- 31 Neurological responsiveness/orientation/ LOC motor/sensory speech/attentiveness/mem ory cranial nerves (if relevant) RLE, LLE, RUE. LUE all have increased weakness and decreased sensation related to edema and Diabetic neuropathy. EENT (eyes, ears, nose, throat) redness, jaundice, discharge, bleeding, burning, or pain Hard of hearing L & R. Patient has lenses in both R & L eyes.. Missing teeth possibly due to hygiene. Respiratory respirations/cough/SOB breath sounds all lobes ant/post supplemental oxygen/type/amount trach/artificial airway/rhonchi, rales (crackles), wheezes or stridor supplemental O2-device, amount Patient’s Cough is congested and non-productive. RUL has crackles. Decreased breath sounds in all fields. r/t to pneumothorax, COPD most likely due to chronic cigarette use. A & O x 4. Oxygen Therapy: Nasal cannula, Adult 5 L/min. Humidifier/ Bubbler. Cardiovascular palpitations/chest discomfort heart sounds/extra sounds rhythm regular/irregular monitor strip interpretation Telemetry monitored. Atrial flutter. Edema dependent, bilateral lower extremities fluid overload. Patient feels right chest sided chest discomfort. Peripheral Vascular skin color nail beds/cap refill/extremity temp radial/dorsalis pedis pulses extremity edema-pitting vs non-pit sacral edema, or discoloration Pitting 3+ in LLE/RLE. Mild edema non pitting in LUE and RUE. Due to fluid volume overload, diabetic neuropathy, lack of mobility. Gastrointestinal/Abdominal characteristics of abdomen, bowel sounds x4 quadrants, tympany, bowel movement abnormalities ostomy, gastric tube, rectal tube feeding tube, gastric tube (PEG) Characteristics of abdomen, round and obese. Firm due to fluid volume overload and poor diet. Bowel sounds normal x4. Normal bowel movements/stools through colostomy. GenitoUrinary urine color/clarity/amount pain/burn/discharge/reten tion indwelling cath/straight cath bladder scan/retention Light amber colored urine. No pain with discharge. Bladder scan 160ml. Retention not present. Intermittent straight catheter. Musculoskeletal range of motion-neck/upper and lower extremities/deformities or injuries/able to bear weight/gait and devices and level of assistance RLE, LLE, RUE, LUE have increased weakness/ decreased sensation r/t edema and Diabetic neuropathy. Unable to bear weight w/o rolling walker. Integumentary/skin assessment Skin color pale or jaundice/temp/moisture turgor/rash/lesions/bruises/wo unds Erythema on feet, peeling. Scaly lower extremity/bilateral. Related to psoriasis and edema. Areas of potential skin breakdown/pressure sores Sacrum is reddened but does blanch. Nares and ears are at risk of skin breakdown due to prolonged nasal cannula use. Calf/thigh/arm DVT assessment +/- Homan’s sign calf/thigh area with pain, redness arm pain/redness Negative Homan’s sign. above IV site; swelling distal to painful area IV Sites/indwelling or implanted lines or ports for medications/fluids assessment of site for redness, tenderness, drainage and description of dressing No abnormal erythema or edema around PIV (right hand 22g). It is locked. Dressing intact. Flushes without resistance. Chest tube- no bleeding/ swelling. Air leak absent r/t pneumothorax. Water seal drainage is below the patient. No evidence of bubbling. Pain Assessment type of pain-describe dull, sharp, etc location/intensity using pain scale Dull aching pain on the right side of thorax. PRIMARY PATIENT PROBLEM/NURSING DIAGNOSIS (problem “related to” and “as evidenced by”) • Impaired gas exchange r/t decreased lung function from pneumothorax and COPD as evidenced by dyspnea, oxygen through nasal cannula and abnormal ABG’s. NG CARE: ENTER INDEPENDENT AND COLLABORATIVE INTERVENTIONS Patient Specific Nursing Intervention(s) ENTER SIX (6) OR MORE INTERVENTIONS Rationale FOR EACH INTERVENTION 1. Checking vital signs- Temp, BP, Resp, Pulse, mPAP every 4 hours. Checking the patient’s vitals at consistent intervals helps to identify complications before they become worse. 2. Change IV line once every 24 hours due to additives in infusion . This will help prevent infection/ incompatibility of drugs. 3. Measure the output of chest tubes and identify characteristics of liquid. This will help to determine if there is any abnormal drainage where pneumothorax is. 4. Bladder Scan PRN- If volume is over 300cc then straight catheter is implemented This will help determine if patient is retaining urine r/t neuropathy/neurogenic bladder 5. Dressings- Apply/ change PRN This intervention promotes wound healing and limits infection. s. 6. Use of incentive spirometry once per shift This will help prevent lung issues such as pneumonia while also increasing the patient’s lung capacity. I Expected Outcome AT LEAST TWO (2) OUTCOMES 1. The patient's lung function will improve. 2. Patient’s edema in LLE & RLE will decrease. Evaluation Strategy FOR EACH OUTCOME Patient oxygenation will decrease from 5 L to 3 L of oxygen through the nasal cannula. This is while maintaining adequate SpO2 in the high 80s-90s. Pitting 3+ in LLE/RLE will decrease to 1+ in the allotted time. ENTER RESOURCE(S) USED AS REFERENCE FOR NURSING DIAGNOSES, INTERVENTIONS, OUTCOMES LISTED ABOVE IN APA FORMAT: 1. activity intolerance- Nursing Diagnosis & Care Plan. (2020, December, 6). Retrieved from https://nurseslabs.com/4-anemia-nursing-care-plans/5/ LABORATORY AND DIAGNOSTIC TEST RESULTS RELATED TO NURSING DIAGNOSIS ABOVE Date Labs/Diagno stics Patient Results Include normal ranges for each Related Pathophysiology Any pathology this test may reveal or help diagnose Nursing Implications CO2 Normal- 22-29 mEq/dL Patient- 34 lungs can't remove enough of the carbon dioxide that the body is producing. Remain alert for complications of respiratory acidosis such as changes in resp, CNS, and cardiovascular function. Arterial HCO3 Normal 22-26 mEq/L Patient- 33 Kidneys are producing more bicarb to counteract the respiratory acidosis. The body is doing what it needs to compensate for respiratory acidosis. Rest, hydration and proper oxygenation is needed. The build up of positive pressure in the pleural space of the right lung is not allowing for proper expansion and ventilation/perfusion. This can lead to atelectasis. Monitor patient for signs of increasing chest pain and or dyspnea.. CT scan Increasing tension in pneumothorax with concern for near or complete collapse of the right lung. SECONDARY PATIENT PROBLEM/NURSING DIAGNOSIS (problem “related to” and “as evidenced by”) ● Acute pain r/t to the positive pressure in the pleural space as evidenced by grimacing and gaurding affected side. NURSING CARE: ENTER INDEPENDENT AND COLLABORATIVE INTERVENTIONS Patient Specific Nursing Intervention(s) ENTER SIX (6) OR MORE INTERVENTIONS Rationale FOR EACH INTERVENTION 1.Checking the patient’s weight daily Will help to see if the patient is depleting or retaining fluid in third place. The reason why is that pneumothorax can negatively impact hemodynamic capabilities and even lead to heart failure. 2. Changing the linen. Checking/ making sure that patient isn't on soiled linens. For a patient who is in bed often due to immobility, linen changes can promote comfort. Moreover, they can help prevent nosocomial infections and skin breakdown. 3. Repositioning the patient every 2 hours. This will help prevent pressure ulcers/ skin breakdown. 4. Keeping the head of the bed above 30 degrees. This intervention will contribute to proper lung expansion. 5. Auscultate breath sounds regularly. This will help in identifying abnormal changes in patients' lung condition. Provides a baseline for pneumothorax resolution 6. Continuous ECG/ telemetry This will help identify early cardiovascular issues due to complications of the patient’s pneumothorax. Expected Outcome AT LEAST TWO (2) OUTCOMES Evaluation Strategy FOR EACH OUTCOME Patient’s weight will be stable and not fluctuate drastically Weighing the patient and make sure she has not gained 2 pounds in a day and or 5 pounds in a week Patient describes satisfactory pain control/management The patient will state a pain level below 3 on a scale of 10. This is compared to a previous baseline pain measurement of 8 out of 10. ENTER RESOURCE(S) USED AS REFERENCE FOR NURSING DIAGNOSES, INTERVENTIONS, AND OUTCOMES LISTED ABOVE IN APA FORMAT: LABORATORY AND DIAGNOSTIC TEST Date daily Labs/Diagnostic s Patient Results Include normal ranges for each Related Pathophysiology Any pathology this test may reveal or help diagnose Nursing Implications What patients may want to know about why the test is done; anything nursing must know to plan and provide care Blood Urea Nitrogen Daily- Normal-around 6 to 24 mg/dL Patient- 35 mg/dL This lab helps determine the kidneys functions and can prevent acute kidney injury. Antibiotics and diuretics can be hard on kidney and had previously sent her into AKI. (CT) coronary angiogram No pulmonary embolism. Right chest tube in place and secure.. Pneumothorax can be caused by a pulmonary embolism and impact cardiorespiratory hemodynamics. Thrombolytics would not be necessary since no embolism is present.. PHARMOCOLOGIC THERAPY Use the chart below to list medications, both SCHEDULED and PRN Medication Name and Dose/Route (generic/trade) Med Type and Reason for Medication Administration (brief reason/include what the med is used for in this patient) Insulin glargine (Lantus) injection 18 Units: dose 18 Units: Subcutaneous: Daily Long Acting Helps to control patient’s blood sugar level due to diabetes Furosemide (LASIX) tablet 30 mg: Oral: Daily Helps treat HTN or any Edema Apixaban (ELIQUIS) tablet 4 mg: Oral 2 Times Daily Treats and prevents blood clots, blood thinner Atrial fib/atrial flutter Albuterol (VENTOLIN) inhaler 1-2 Puff: Every 4 Hours As Needed relaxes muscles in the airways, widening them and allowing more air to flow into the lungs Piperacillin-tazobactam (ZOSYN) 4.2 g/50 mL–IV bag with dextrose: Dose 4.2 g: 12 mL/hr: Intravenous: Every 8 hours Combination of 2 antibiotics. It works by killing the bacteria and preventing their growth. PATIENT EDUCATION/DISCHARGE PLANNING: INFORMATION NEEDED TO PROVIDE INDIVIDUALIZED NURSING CARE Cultural Needs and Implications None Management/Suppor t Systems in Place Patients Family is very close and they visit often. Recommendations for joining a support group for those experiencing lung issues have been given Financial Issues/Concerns none Role Reversal Concerns none Other Issues The patient needs to follow a prescribed diet for diabetes. This will help ensure she does not increase her blood glucose to dangerous levels. This not only includes a reduction in sugar consumption, but also sodium. Plan of Care 2021/CG
